User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


White House announces vaccination plans for younger children
States were allowed to begin preordering the shots this week. But they can’t be delivered into kids’ arms until the FDA and CDC sign off. The shots could be available in early November.
“We know millions of parents have been waiting for COVID-19 vaccine for kids in this age group, and should the FDA and CDC authorize the vaccine, we will be ready to get shots in arms,” Jeff Zients, the White House COVID-19 response coordinator, said at a briefing Oct. 20.
Asked whether announcing plans to deliver a vaccine to children might put pressure on the agencies considering the evidence for their use, Mr. Zients defended the Biden administration’s plans.
“This is the right way to do things: To be operationally ready,” he said. Mr. Zients said they had learned a lesson from the prior administration.
“The decision was made by the FDA and CDC, and the operations weren’t ready. And that meant that adults at the time were not able to receive their vaccines as efficiently, equitably as possible. And this will enable us to be ready for kids,” he said.
Pfizer submitted data to the FDA in late September from its test of the vaccine in 2,200 children. The company said the shots had a favorable safety profile and generated “robust” antibody responses.
An FDA panel is scheduled to meet on Oct. 26 to consider Pfizer’s application. The CDC’s Advisory Committee on Immunization Practices will meet the following week, on Nov. 2 and 3.
Laying the groundwork
Doctors applauded the advance planning.
“Laying this advance groundwork, ensuring supply is available at physician practices, and that a patient’s own physician is available to answer questions, is critical to the continued success of this rollout,” Gerald Harmon, MD, president of the American Medical Association, said in a written statement.
The shots planned for children are 10 micrograms, a smaller dose than is given to adults. To be fully immunized, kids get two doses, spaced about 21 days apart. Vaccines for younger children are packaged in smaller vials and injected through smaller needles, too.
The vaccine for younger children will roll out slightly differently than it has for adults and teens. While adults mostly got their COVID-19 vaccines through pop-up mass vaccination sites, health departments, and other community locations, the strategy to get children immunized against COVID is centered on the offices of pediatricians and primary care doctors.
The White House says 25,000 doctors have already signed up to give the vaccines.
The vaccination campaign will get underway at a tough moment for pediatricians.
The voicemail message at Roswell Pediatrics Center in the suburbs north of Atlanta, for instance, warns parents to be patient.
“Due to the current, new COVID-19 surge, we are experiencing extremely high call volume, as well as suffering from the same staffing shortages that most businesses are having,” the message says, adding that they’re working around the clock to answer questions and return phone calls.
Jesse Hackell, MD, says he knows the feeling. He’s the chief operating officer of Pomona Pediatrics in Pomona, N.Y., and a spokesperson for the American Academy of Pediatrics.
“We’re swamped now by kids who get sent home from school because they sneezed once and they have to be cleared before they can go back to school,” he said. “We’re seeing kids who we don’t need to see in terms of the degree of illness because the school requires them to be cleared [of COVID-19].”
Dr. Hackell has been offering the vaccines to kids ages 12 and up since May. He’s planning to offer it to younger children too.
“Adding the vaccines to it is going to be a challenge, but you know we’ll get up to speed and we’ll make it happen,” he said, adding that pediatricians have done many large-scale vaccination campaigns, like those for the H1N1 influenza vaccine in 2009.
Dr. Hackell helped to draft a new policy in New York that will require COVID-19 vaccines for schoolchildren once they are granted full approval from the FDA. Other states may follow with their own vaccination requirements.
He said ultimately, vaccinating school-age children is going to make them safer, will help prevent the virus from mutating and spreading, and will help society as a whole get back to normal.
“We’re the vaccine experts in pediatrics. This is what we do. It’s a huge part of our practice like no other specialty. If we can’t get it right, how can anyone else be expected to?” he said.
A version of this article first appeared on WebMD.com.
States were allowed to begin preordering the shots this week. But they can’t be delivered into kids’ arms until the FDA and CDC sign off. The shots could be available in early November.
“We know millions of parents have been waiting for COVID-19 vaccine for kids in this age group, and should the FDA and CDC authorize the vaccine, we will be ready to get shots in arms,” Jeff Zients, the White House COVID-19 response coordinator, said at a briefing Oct. 20.
Asked whether announcing plans to deliver a vaccine to children might put pressure on the agencies considering the evidence for their use, Mr. Zients defended the Biden administration’s plans.
“This is the right way to do things: To be operationally ready,” he said. Mr. Zients said they had learned a lesson from the prior administration.
“The decision was made by the FDA and CDC, and the operations weren’t ready. And that meant that adults at the time were not able to receive their vaccines as efficiently, equitably as possible. And this will enable us to be ready for kids,” he said.
Pfizer submitted data to the FDA in late September from its test of the vaccine in 2,200 children. The company said the shots had a favorable safety profile and generated “robust” antibody responses.
An FDA panel is scheduled to meet on Oct. 26 to consider Pfizer’s application. The CDC’s Advisory Committee on Immunization Practices will meet the following week, on Nov. 2 and 3.
Laying the groundwork
Doctors applauded the advance planning.
“Laying this advance groundwork, ensuring supply is available at physician practices, and that a patient’s own physician is available to answer questions, is critical to the continued success of this rollout,” Gerald Harmon, MD, president of the American Medical Association, said in a written statement.
The shots planned for children are 10 micrograms, a smaller dose than is given to adults. To be fully immunized, kids get two doses, spaced about 21 days apart. Vaccines for younger children are packaged in smaller vials and injected through smaller needles, too.
The vaccine for younger children will roll out slightly differently than it has for adults and teens. While adults mostly got their COVID-19 vaccines through pop-up mass vaccination sites, health departments, and other community locations, the strategy to get children immunized against COVID is centered on the offices of pediatricians and primary care doctors.
The White House says 25,000 doctors have already signed up to give the vaccines.
The vaccination campaign will get underway at a tough moment for pediatricians.
The voicemail message at Roswell Pediatrics Center in the suburbs north of Atlanta, for instance, warns parents to be patient.
“Due to the current, new COVID-19 surge, we are experiencing extremely high call volume, as well as suffering from the same staffing shortages that most businesses are having,” the message says, adding that they’re working around the clock to answer questions and return phone calls.
Jesse Hackell, MD, says he knows the feeling. He’s the chief operating officer of Pomona Pediatrics in Pomona, N.Y., and a spokesperson for the American Academy of Pediatrics.
“We’re swamped now by kids who get sent home from school because they sneezed once and they have to be cleared before they can go back to school,” he said. “We’re seeing kids who we don’t need to see in terms of the degree of illness because the school requires them to be cleared [of COVID-19].”
Dr. Hackell has been offering the vaccines to kids ages 12 and up since May. He’s planning to offer it to younger children too.
“Adding the vaccines to it is going to be a challenge, but you know we’ll get up to speed and we’ll make it happen,” he said, adding that pediatricians have done many large-scale vaccination campaigns, like those for the H1N1 influenza vaccine in 2009.
Dr. Hackell helped to draft a new policy in New York that will require COVID-19 vaccines for schoolchildren once they are granted full approval from the FDA. Other states may follow with their own vaccination requirements.
He said ultimately, vaccinating school-age children is going to make them safer, will help prevent the virus from mutating and spreading, and will help society as a whole get back to normal.
“We’re the vaccine experts in pediatrics. This is what we do. It’s a huge part of our practice like no other specialty. If we can’t get it right, how can anyone else be expected to?” he said.
A version of this article first appeared on WebMD.com.
States were allowed to begin preordering the shots this week. But they can’t be delivered into kids’ arms until the FDA and CDC sign off. The shots could be available in early November.
“We know millions of parents have been waiting for COVID-19 vaccine for kids in this age group, and should the FDA and CDC authorize the vaccine, we will be ready to get shots in arms,” Jeff Zients, the White House COVID-19 response coordinator, said at a briefing Oct. 20.
Asked whether announcing plans to deliver a vaccine to children might put pressure on the agencies considering the evidence for their use, Mr. Zients defended the Biden administration’s plans.
“This is the right way to do things: To be operationally ready,” he said. Mr. Zients said they had learned a lesson from the prior administration.
“The decision was made by the FDA and CDC, and the operations weren’t ready. And that meant that adults at the time were not able to receive their vaccines as efficiently, equitably as possible. And this will enable us to be ready for kids,” he said.
Pfizer submitted data to the FDA in late September from its test of the vaccine in 2,200 children. The company said the shots had a favorable safety profile and generated “robust” antibody responses.
An FDA panel is scheduled to meet on Oct. 26 to consider Pfizer’s application. The CDC’s Advisory Committee on Immunization Practices will meet the following week, on Nov. 2 and 3.
Laying the groundwork
Doctors applauded the advance planning.
“Laying this advance groundwork, ensuring supply is available at physician practices, and that a patient’s own physician is available to answer questions, is critical to the continued success of this rollout,” Gerald Harmon, MD, president of the American Medical Association, said in a written statement.
The shots planned for children are 10 micrograms, a smaller dose than is given to adults. To be fully immunized, kids get two doses, spaced about 21 days apart. Vaccines for younger children are packaged in smaller vials and injected through smaller needles, too.
The vaccine for younger children will roll out slightly differently than it has for adults and teens. While adults mostly got their COVID-19 vaccines through pop-up mass vaccination sites, health departments, and other community locations, the strategy to get children immunized against COVID is centered on the offices of pediatricians and primary care doctors.
The White House says 25,000 doctors have already signed up to give the vaccines.
The vaccination campaign will get underway at a tough moment for pediatricians.
The voicemail message at Roswell Pediatrics Center in the suburbs north of Atlanta, for instance, warns parents to be patient.
“Due to the current, new COVID-19 surge, we are experiencing extremely high call volume, as well as suffering from the same staffing shortages that most businesses are having,” the message says, adding that they’re working around the clock to answer questions and return phone calls.
Jesse Hackell, MD, says he knows the feeling. He’s the chief operating officer of Pomona Pediatrics in Pomona, N.Y., and a spokesperson for the American Academy of Pediatrics.
“We’re swamped now by kids who get sent home from school because they sneezed once and they have to be cleared before they can go back to school,” he said. “We’re seeing kids who we don’t need to see in terms of the degree of illness because the school requires them to be cleared [of COVID-19].”
Dr. Hackell has been offering the vaccines to kids ages 12 and up since May. He’s planning to offer it to younger children too.
“Adding the vaccines to it is going to be a challenge, but you know we’ll get up to speed and we’ll make it happen,” he said, adding that pediatricians have done many large-scale vaccination campaigns, like those for the H1N1 influenza vaccine in 2009.
Dr. Hackell helped to draft a new policy in New York that will require COVID-19 vaccines for schoolchildren once they are granted full approval from the FDA. Other states may follow with their own vaccination requirements.
He said ultimately, vaccinating school-age children is going to make them safer, will help prevent the virus from mutating and spreading, and will help society as a whole get back to normal.
“We’re the vaccine experts in pediatrics. This is what we do. It’s a huge part of our practice like no other specialty. If we can’t get it right, how can anyone else be expected to?” he said.
A version of this article first appeared on WebMD.com.
Fungal infection can mimic lung cancer metastases
A fungal infection typically seen in the lungs may have a variety of unusual clinical presentations elsewhere in the body, even raising suspicion of cancer in some cases, a medical resident reported at the annual meeting of the American College of Chest Physicians.
In one recent and unusual presentation, a 58-year-old woman with persistent headaches had skull lesions on computed tomography (CT) was eventually diagnosed with disseminated coccidioidomycosis (Valley fever), a fungal infection endemic to the Southwestern U.S.
The imaging pattern of her head CT was initially concerning for cancer metastasis, according to Sharjeel Israr, MD, a third-year internal medicine resident at Creighton University in Phoenix, Ariz.
However, the subsequent chest CT revealed a suspicious chest mass. A biopsy of that mass led to the correct diagnosis of disseminated coccidioidomycosis, according to Dr. Israr, who presented the case report in an e-poster at the CHEST meeting, which was held virtually this year.
Mistaken identity
Coccidioidomycosis, caused by the fungus Coccidioides, usually affects the lungs, according to the Centers for Disease Control and Prevention. However, in severe cases it can spread to other parts of the body. In those cases, it’s referred to as disseminated coccidioidomycosis.
Arizona accounted for about 10,000 out of 18,000 reported Valley fever cases in 2019, according to the latest statistics from the CDC.
Coccidioidomycosis is frequently mistaken not only for cancer, but also for rheumatic conditions and bacterial infections, according to Valley fever specialist John Galgiani, MD, director of the Valley Fever Center for Excellence at the University of Arizona in Tucson.
“Where Valley fever is common, it should very frequently be in the differential for masses that are thought to be cancer,” Dr. Galgiani said in an interview. “This case is a good example of that.”
Challenging case
In an interview, Dr. Israr said the case was challenging to crack despite the fact that Valley fever is very common in Phoenix.
“It was definitely on the differential from the get-go, but it was very, very low our differential, just based on the presentation that she had,” said Dr. Israr.
The patient had history of diabetes and presented with headaches for 4 weeks. However, she had no pulmonary symptoms or meningeal signs, according to Dr. Israr.
A head CT revealed multiple osseous skull lesions and a left temporal lobe lesion.
“The fact that this patient had lesions in the skull, specifically, is something that raised our initial red flags for cancer – especially since she presented with just a headache as her only complaint,” he said.
The imaging pattern was concerning for metastasis, according to Dr. Israr, particularly since a subsequent CT of the chest showed multiple pulmonary nodules plus a 7.7-cm mass in the right lower lobe.
Once the biopsy confirmed coccidioidomycosis, the patient was started on fluconazole 600 mg twice daily, according to Dr. Israr.
Although severe disseminated coccidioidomycosis can be difficult to treat, the lung lesion had decreased in size from 7.7 cm to 4.2 cm about 3 months later, Dr. Israr said.
“At the end of the day, she didn’t have cancer, and it’s something that we’re treating and she’s actually doing better right now,” Dr. Israr said in the interview.
Dr. Israr and coauthors of the case reported they had no relevant relationships to disclose.
A fungal infection typically seen in the lungs may have a variety of unusual clinical presentations elsewhere in the body, even raising suspicion of cancer in some cases, a medical resident reported at the annual meeting of the American College of Chest Physicians.
In one recent and unusual presentation, a 58-year-old woman with persistent headaches had skull lesions on computed tomography (CT) was eventually diagnosed with disseminated coccidioidomycosis (Valley fever), a fungal infection endemic to the Southwestern U.S.
The imaging pattern of her head CT was initially concerning for cancer metastasis, according to Sharjeel Israr, MD, a third-year internal medicine resident at Creighton University in Phoenix, Ariz.
However, the subsequent chest CT revealed a suspicious chest mass. A biopsy of that mass led to the correct diagnosis of disseminated coccidioidomycosis, according to Dr. Israr, who presented the case report in an e-poster at the CHEST meeting, which was held virtually this year.
Mistaken identity
Coccidioidomycosis, caused by the fungus Coccidioides, usually affects the lungs, according to the Centers for Disease Control and Prevention. However, in severe cases it can spread to other parts of the body. In those cases, it’s referred to as disseminated coccidioidomycosis.
Arizona accounted for about 10,000 out of 18,000 reported Valley fever cases in 2019, according to the latest statistics from the CDC.
Coccidioidomycosis is frequently mistaken not only for cancer, but also for rheumatic conditions and bacterial infections, according to Valley fever specialist John Galgiani, MD, director of the Valley Fever Center for Excellence at the University of Arizona in Tucson.
“Where Valley fever is common, it should very frequently be in the differential for masses that are thought to be cancer,” Dr. Galgiani said in an interview. “This case is a good example of that.”
Challenging case
In an interview, Dr. Israr said the case was challenging to crack despite the fact that Valley fever is very common in Phoenix.
“It was definitely on the differential from the get-go, but it was very, very low our differential, just based on the presentation that she had,” said Dr. Israr.
The patient had history of diabetes and presented with headaches for 4 weeks. However, she had no pulmonary symptoms or meningeal signs, according to Dr. Israr.
A head CT revealed multiple osseous skull lesions and a left temporal lobe lesion.
“The fact that this patient had lesions in the skull, specifically, is something that raised our initial red flags for cancer – especially since she presented with just a headache as her only complaint,” he said.
The imaging pattern was concerning for metastasis, according to Dr. Israr, particularly since a subsequent CT of the chest showed multiple pulmonary nodules plus a 7.7-cm mass in the right lower lobe.
Once the biopsy confirmed coccidioidomycosis, the patient was started on fluconazole 600 mg twice daily, according to Dr. Israr.
Although severe disseminated coccidioidomycosis can be difficult to treat, the lung lesion had decreased in size from 7.7 cm to 4.2 cm about 3 months later, Dr. Israr said.
“At the end of the day, she didn’t have cancer, and it’s something that we’re treating and she’s actually doing better right now,” Dr. Israr said in the interview.
Dr. Israr and coauthors of the case reported they had no relevant relationships to disclose.
A fungal infection typically seen in the lungs may have a variety of unusual clinical presentations elsewhere in the body, even raising suspicion of cancer in some cases, a medical resident reported at the annual meeting of the American College of Chest Physicians.
In one recent and unusual presentation, a 58-year-old woman with persistent headaches had skull lesions on computed tomography (CT) was eventually diagnosed with disseminated coccidioidomycosis (Valley fever), a fungal infection endemic to the Southwestern U.S.
The imaging pattern of her head CT was initially concerning for cancer metastasis, according to Sharjeel Israr, MD, a third-year internal medicine resident at Creighton University in Phoenix, Ariz.
However, the subsequent chest CT revealed a suspicious chest mass. A biopsy of that mass led to the correct diagnosis of disseminated coccidioidomycosis, according to Dr. Israr, who presented the case report in an e-poster at the CHEST meeting, which was held virtually this year.
Mistaken identity
Coccidioidomycosis, caused by the fungus Coccidioides, usually affects the lungs, according to the Centers for Disease Control and Prevention. However, in severe cases it can spread to other parts of the body. In those cases, it’s referred to as disseminated coccidioidomycosis.
Arizona accounted for about 10,000 out of 18,000 reported Valley fever cases in 2019, according to the latest statistics from the CDC.
Coccidioidomycosis is frequently mistaken not only for cancer, but also for rheumatic conditions and bacterial infections, according to Valley fever specialist John Galgiani, MD, director of the Valley Fever Center for Excellence at the University of Arizona in Tucson.
“Where Valley fever is common, it should very frequently be in the differential for masses that are thought to be cancer,” Dr. Galgiani said in an interview. “This case is a good example of that.”
Challenging case
In an interview, Dr. Israr said the case was challenging to crack despite the fact that Valley fever is very common in Phoenix.
“It was definitely on the differential from the get-go, but it was very, very low our differential, just based on the presentation that she had,” said Dr. Israr.
The patient had history of diabetes and presented with headaches for 4 weeks. However, she had no pulmonary symptoms or meningeal signs, according to Dr. Israr.
A head CT revealed multiple osseous skull lesions and a left temporal lobe lesion.
“The fact that this patient had lesions in the skull, specifically, is something that raised our initial red flags for cancer – especially since she presented with just a headache as her only complaint,” he said.
The imaging pattern was concerning for metastasis, according to Dr. Israr, particularly since a subsequent CT of the chest showed multiple pulmonary nodules plus a 7.7-cm mass in the right lower lobe.
Once the biopsy confirmed coccidioidomycosis, the patient was started on fluconazole 600 mg twice daily, according to Dr. Israr.
Although severe disseminated coccidioidomycosis can be difficult to treat, the lung lesion had decreased in size from 7.7 cm to 4.2 cm about 3 months later, Dr. Israr said.
“At the end of the day, she didn’t have cancer, and it’s something that we’re treating and she’s actually doing better right now,” Dr. Israr said in the interview.
Dr. Israr and coauthors of the case reported they had no relevant relationships to disclose.
REPORTING FROM CHEST 2021
Pfizer offers refund if drug ‘doesn’t work’
The high cost of new cancer drugs has been the subject of many debates and discussions, but the issue remains largely unresolved.
Now, one pharmaceutical company is offering a refund if its drug “doesn’t work.”
For what it says is the first time in the industry,
“Through this pilot program, Pfizer will offer a warranty to patients and health plans -- Medicare Part D, commercial and those who pay cash -- who are prescribed Xalkori for an FDA [US Food and Drug Administration]–approved indication,” said a company spokesperson.
Although Pfizer claims that its pilot program is a first in the industry, there have been others that are similar.
In 2017, Novartis offered something similar for tisagenlecleucel (Kymriah), the CAR T-cell therapy that launched with a daunting price tag of $475,000. After receiving backlash over the cost, Novartis announced that if the drug does not work after the first month, patients pay nothing.
Italy has been using this system for several years. Pharmaceutical companies must refund money if the drug fails to work. In 2015, the state-run healthcare system collected €200 million ($220 million) in refunds.
Pfizer pledge
Crizotinib is a selective tyrosine kinase inhibitor used mainly in the treatment of metastatic non–small cell lung cancer for patients whose tumors are positive for ALK or ROS1, as detected by an FDA-approved test. This indication was approved a decade ago. Another indication, ALK-positive anaplastic large cell lymphoma, was added earlier this year.
Details of the Pfizer Pledge are posted on Pfizer’s website. Eligible patients are those for whom crizotinib is discontinued before the fourth 30-day supply is dispensed by the patient’s pharmacy.
“The warranty will reimburse an amount equal to the cost paid for the medicine,” the spokesperson added. “The insurance-backed warranty pilot program will be insured and managed by AIG.”
This program is only available for patients who reside in the United States.
If use of crizotinib is discontinued and documentation of ineffectiveness is provided, Pfizer will refund the out-of-pocket amount that was paid for up to the first three bottles (30-day supply) of crizotinib, up to a maximum of $19,144 for each month’s supply, or a total of $57,432. Pfizer will also refund the cost that was paid by Medicare or a commercial insurer.
“Also, we have made sure to develop a program that also allows for Medicare patients to be eligible, since they are exempt from copay cards and at risk for significant financial burden when starting an oncology treatment,” said the spokesperson.
The pilot program is available to patients who began taking crizotinib from June 1, 2021, through December 31, 2021.
So far, Pfizer is offering this warranty only for crizotinib, but that may change in the future.
“Once the pilot is complete, we will assess learnings and consider whether to build a more robust, scalable program capable of supporting multiple products,” the Pfizer spokesperson commented.
Previous scheme ended in court
Pfizer had previously tried a different approach to reducing drug costs: it had attempted to offer copay support programs to Medicare patients who were prescribed its cardiac drug tafamidis (Vyndaqe, Vyndamax).
Tafamidis, launched in 2019, is used for patients with transthyretin amyloid cardiomyopathy. For those patients, it has been shown to reduce all-cause mortality and cardiovascular hospitalizations. It costs about $225,000 a year and has been described as the most expensive cardiovascular drug in the United States.
Earlier this month, a court dismissed Pfizer’s challenge to an anti-kickback law that prevented the company from offering copay support programs to Medicare patients.
The judge ruled that Pfizer’s plan to offer direct payments to patients violated a federal ban on “knowingly or willfully” providing financial support to induce drug purchases, even in the absence of corrupt intent.
Pharmaceutical manufacturers are forbidden from subsidizing copayments for Medicare beneficiaries but are allowed to donate to independent nonprofit organizations that offer copay assistance. Pfizer sued the U.S. Department of Health and Human Services in June 2020 to get a court ruling that their proposed programs were legal.
The new pledge program for crizotinib operates from a different premise, the Pfizer spokesperson commented.
A version of this article first appeared on Medscape.com.
The high cost of new cancer drugs has been the subject of many debates and discussions, but the issue remains largely unresolved.
Now, one pharmaceutical company is offering a refund if its drug “doesn’t work.”
For what it says is the first time in the industry,
“Through this pilot program, Pfizer will offer a warranty to patients and health plans -- Medicare Part D, commercial and those who pay cash -- who are prescribed Xalkori for an FDA [US Food and Drug Administration]–approved indication,” said a company spokesperson.
Although Pfizer claims that its pilot program is a first in the industry, there have been others that are similar.
In 2017, Novartis offered something similar for tisagenlecleucel (Kymriah), the CAR T-cell therapy that launched with a daunting price tag of $475,000. After receiving backlash over the cost, Novartis announced that if the drug does not work after the first month, patients pay nothing.
Italy has been using this system for several years. Pharmaceutical companies must refund money if the drug fails to work. In 2015, the state-run healthcare system collected €200 million ($220 million) in refunds.
Pfizer pledge
Crizotinib is a selective tyrosine kinase inhibitor used mainly in the treatment of metastatic non–small cell lung cancer for patients whose tumors are positive for ALK or ROS1, as detected by an FDA-approved test. This indication was approved a decade ago. Another indication, ALK-positive anaplastic large cell lymphoma, was added earlier this year.
Details of the Pfizer Pledge are posted on Pfizer’s website. Eligible patients are those for whom crizotinib is discontinued before the fourth 30-day supply is dispensed by the patient’s pharmacy.
“The warranty will reimburse an amount equal to the cost paid for the medicine,” the spokesperson added. “The insurance-backed warranty pilot program will be insured and managed by AIG.”
This program is only available for patients who reside in the United States.
If use of crizotinib is discontinued and documentation of ineffectiveness is provided, Pfizer will refund the out-of-pocket amount that was paid for up to the first three bottles (30-day supply) of crizotinib, up to a maximum of $19,144 for each month’s supply, or a total of $57,432. Pfizer will also refund the cost that was paid by Medicare or a commercial insurer.
“Also, we have made sure to develop a program that also allows for Medicare patients to be eligible, since they are exempt from copay cards and at risk for significant financial burden when starting an oncology treatment,” said the spokesperson.
The pilot program is available to patients who began taking crizotinib from June 1, 2021, through December 31, 2021.
So far, Pfizer is offering this warranty only for crizotinib, but that may change in the future.
“Once the pilot is complete, we will assess learnings and consider whether to build a more robust, scalable program capable of supporting multiple products,” the Pfizer spokesperson commented.
Previous scheme ended in court
Pfizer had previously tried a different approach to reducing drug costs: it had attempted to offer copay support programs to Medicare patients who were prescribed its cardiac drug tafamidis (Vyndaqe, Vyndamax).
Tafamidis, launched in 2019, is used for patients with transthyretin amyloid cardiomyopathy. For those patients, it has been shown to reduce all-cause mortality and cardiovascular hospitalizations. It costs about $225,000 a year and has been described as the most expensive cardiovascular drug in the United States.
Earlier this month, a court dismissed Pfizer’s challenge to an anti-kickback law that prevented the company from offering copay support programs to Medicare patients.
The judge ruled that Pfizer’s plan to offer direct payments to patients violated a federal ban on “knowingly or willfully” providing financial support to induce drug purchases, even in the absence of corrupt intent.
Pharmaceutical manufacturers are forbidden from subsidizing copayments for Medicare beneficiaries but are allowed to donate to independent nonprofit organizations that offer copay assistance. Pfizer sued the U.S. Department of Health and Human Services in June 2020 to get a court ruling that their proposed programs were legal.
The new pledge program for crizotinib operates from a different premise, the Pfizer spokesperson commented.
A version of this article first appeared on Medscape.com.
The high cost of new cancer drugs has been the subject of many debates and discussions, but the issue remains largely unresolved.
Now, one pharmaceutical company is offering a refund if its drug “doesn’t work.”
For what it says is the first time in the industry,
“Through this pilot program, Pfizer will offer a warranty to patients and health plans -- Medicare Part D, commercial and those who pay cash -- who are prescribed Xalkori for an FDA [US Food and Drug Administration]–approved indication,” said a company spokesperson.
Although Pfizer claims that its pilot program is a first in the industry, there have been others that are similar.
In 2017, Novartis offered something similar for tisagenlecleucel (Kymriah), the CAR T-cell therapy that launched with a daunting price tag of $475,000. After receiving backlash over the cost, Novartis announced that if the drug does not work after the first month, patients pay nothing.
Italy has been using this system for several years. Pharmaceutical companies must refund money if the drug fails to work. In 2015, the state-run healthcare system collected €200 million ($220 million) in refunds.
Pfizer pledge
Crizotinib is a selective tyrosine kinase inhibitor used mainly in the treatment of metastatic non–small cell lung cancer for patients whose tumors are positive for ALK or ROS1, as detected by an FDA-approved test. This indication was approved a decade ago. Another indication, ALK-positive anaplastic large cell lymphoma, was added earlier this year.
Details of the Pfizer Pledge are posted on Pfizer’s website. Eligible patients are those for whom crizotinib is discontinued before the fourth 30-day supply is dispensed by the patient’s pharmacy.
“The warranty will reimburse an amount equal to the cost paid for the medicine,” the spokesperson added. “The insurance-backed warranty pilot program will be insured and managed by AIG.”
This program is only available for patients who reside in the United States.
If use of crizotinib is discontinued and documentation of ineffectiveness is provided, Pfizer will refund the out-of-pocket amount that was paid for up to the first three bottles (30-day supply) of crizotinib, up to a maximum of $19,144 for each month’s supply, or a total of $57,432. Pfizer will also refund the cost that was paid by Medicare or a commercial insurer.
“Also, we have made sure to develop a program that also allows for Medicare patients to be eligible, since they are exempt from copay cards and at risk for significant financial burden when starting an oncology treatment,” said the spokesperson.
The pilot program is available to patients who began taking crizotinib from June 1, 2021, through December 31, 2021.
So far, Pfizer is offering this warranty only for crizotinib, but that may change in the future.
“Once the pilot is complete, we will assess learnings and consider whether to build a more robust, scalable program capable of supporting multiple products,” the Pfizer spokesperson commented.
Previous scheme ended in court
Pfizer had previously tried a different approach to reducing drug costs: it had attempted to offer copay support programs to Medicare patients who were prescribed its cardiac drug tafamidis (Vyndaqe, Vyndamax).
Tafamidis, launched in 2019, is used for patients with transthyretin amyloid cardiomyopathy. For those patients, it has been shown to reduce all-cause mortality and cardiovascular hospitalizations. It costs about $225,000 a year and has been described as the most expensive cardiovascular drug in the United States.
Earlier this month, a court dismissed Pfizer’s challenge to an anti-kickback law that prevented the company from offering copay support programs to Medicare patients.
The judge ruled that Pfizer’s plan to offer direct payments to patients violated a federal ban on “knowingly or willfully” providing financial support to induce drug purchases, even in the absence of corrupt intent.
Pharmaceutical manufacturers are forbidden from subsidizing copayments for Medicare beneficiaries but are allowed to donate to independent nonprofit organizations that offer copay assistance. Pfizer sued the U.S. Department of Health and Human Services in June 2020 to get a court ruling that their proposed programs were legal.
The new pledge program for crizotinib operates from a different premise, the Pfizer spokesperson commented.
A version of this article first appeared on Medscape.com.
No benefit from lower temps for out-of-hospital cardiac arrest
The results “do not support the use of moderate therapeutic hypothermia to improve neurologic outcomes in comatose survivors of out-of-hospital cardiac arrest,” write the investigators led by Michel Le May, MD, from the University of Ottawa Heart Institute, Ontario, Canada.
The CAPITAL CHILL results were first presented at the American College of Cardiology (ACC) 2021 Scientific Sessions in May.
They have now been published online, October 19, in JAMA.
High rates of brain injury and death
Comatose survivors of OHCA have high rates of severe brain injury and death. Current guidelines recommend targeted temperature management at 32°C to 36°C for 24 hours. However, small studies have suggested a potential benefit of targeting lower body temperatures.
In the CAPITAL CHILL study of 367 OHCA patients who were comatose on admission, there were no statistically significant differences in the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days with mild-versus-moderate hypothermia.
The primary composite outcome occurred in 89 of 184 (48.4%) patients in the moderate hypothermia group and 83 of 183 (45.4%) patients in the mild hypothermia group — a risk difference of 3.0% (95% confidence interval [CI], 7.2% - 13.2%) and relative risk of 1.07 (95% CI, 0.86 - 1.33; P = .56).
There was also no significant difference when looking at the individual components of mortality (43.5% vs 41.0%) and poor neurologic outcome (Disability Rating Scale score >5: 4.9% vs 4.4%).
The baseline characteristics of patients were similar in the moderate and mild hypothermia groups. The lack of a significant difference in the primary outcome was consistent after adjusting for baseline covariates as well as across all subgroups.
The rates of secondary outcomes were also similar between the two groups, except for a longer length of stay in the intensive care unit in the moderate hypothermia group compared with the mild hypothermia group, which would likely add to overall costs.
The researchers note that the Targeted Hypothermia vs Targeted Normothermia After Out-of-Hospital Cardiac Arrest (TTM2) trial recently reported that targeted hypothermia at 33°C did not improve survival at 180 days compared with targeted normothermia at 37.5°C or less.
The CAPITAL CHILL study “adds to the spectrum of target temperature management, as it did not find any benefit of even further lowering temperatures to 31°C,” the study team says.
They caution that most patients in the trial had cardiac arrest secondary to a primary cardiac etiology and therefore the findings may not be applicable to cardiac arrest of all etiologies.
It’s also possible that the trial was underpowered to detect clinically important differences between moderate and mild hypothermia. Also, the number of patients presenting with a nonshockable rhythm was relatively small, and further study may be worthwhile in this subgroup, they say.
For now, however, the CAPITAL CHILL results provide no support for a lower target temperature of 31°C to improve outcomes in OHCA patients, Dr. Le May and colleagues conclude.
CAPITAL CHILL was an investigator-initiated study and funding was provided by the University of Ottawa Heart Institute Cardiac Arrest Program. Dr. Le May has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The results “do not support the use of moderate therapeutic hypothermia to improve neurologic outcomes in comatose survivors of out-of-hospital cardiac arrest,” write the investigators led by Michel Le May, MD, from the University of Ottawa Heart Institute, Ontario, Canada.
The CAPITAL CHILL results were first presented at the American College of Cardiology (ACC) 2021 Scientific Sessions in May.
They have now been published online, October 19, in JAMA.
High rates of brain injury and death
Comatose survivors of OHCA have high rates of severe brain injury and death. Current guidelines recommend targeted temperature management at 32°C to 36°C for 24 hours. However, small studies have suggested a potential benefit of targeting lower body temperatures.
In the CAPITAL CHILL study of 367 OHCA patients who were comatose on admission, there were no statistically significant differences in the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days with mild-versus-moderate hypothermia.
The primary composite outcome occurred in 89 of 184 (48.4%) patients in the moderate hypothermia group and 83 of 183 (45.4%) patients in the mild hypothermia group — a risk difference of 3.0% (95% confidence interval [CI], 7.2% - 13.2%) and relative risk of 1.07 (95% CI, 0.86 - 1.33; P = .56).
There was also no significant difference when looking at the individual components of mortality (43.5% vs 41.0%) and poor neurologic outcome (Disability Rating Scale score >5: 4.9% vs 4.4%).
The baseline characteristics of patients were similar in the moderate and mild hypothermia groups. The lack of a significant difference in the primary outcome was consistent after adjusting for baseline covariates as well as across all subgroups.
The rates of secondary outcomes were also similar between the two groups, except for a longer length of stay in the intensive care unit in the moderate hypothermia group compared with the mild hypothermia group, which would likely add to overall costs.
The researchers note that the Targeted Hypothermia vs Targeted Normothermia After Out-of-Hospital Cardiac Arrest (TTM2) trial recently reported that targeted hypothermia at 33°C did not improve survival at 180 days compared with targeted normothermia at 37.5°C or less.
The CAPITAL CHILL study “adds to the spectrum of target temperature management, as it did not find any benefit of even further lowering temperatures to 31°C,” the study team says.
They caution that most patients in the trial had cardiac arrest secondary to a primary cardiac etiology and therefore the findings may not be applicable to cardiac arrest of all etiologies.
It’s also possible that the trial was underpowered to detect clinically important differences between moderate and mild hypothermia. Also, the number of patients presenting with a nonshockable rhythm was relatively small, and further study may be worthwhile in this subgroup, they say.
For now, however, the CAPITAL CHILL results provide no support for a lower target temperature of 31°C to improve outcomes in OHCA patients, Dr. Le May and colleagues conclude.
CAPITAL CHILL was an investigator-initiated study and funding was provided by the University of Ottawa Heart Institute Cardiac Arrest Program. Dr. Le May has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The results “do not support the use of moderate therapeutic hypothermia to improve neurologic outcomes in comatose survivors of out-of-hospital cardiac arrest,” write the investigators led by Michel Le May, MD, from the University of Ottawa Heart Institute, Ontario, Canada.
The CAPITAL CHILL results were first presented at the American College of Cardiology (ACC) 2021 Scientific Sessions in May.
They have now been published online, October 19, in JAMA.
High rates of brain injury and death
Comatose survivors of OHCA have high rates of severe brain injury and death. Current guidelines recommend targeted temperature management at 32°C to 36°C for 24 hours. However, small studies have suggested a potential benefit of targeting lower body temperatures.
In the CAPITAL CHILL study of 367 OHCA patients who were comatose on admission, there were no statistically significant differences in the primary composite outcome of all-cause mortality or poor neurologic outcome at 180 days with mild-versus-moderate hypothermia.
The primary composite outcome occurred in 89 of 184 (48.4%) patients in the moderate hypothermia group and 83 of 183 (45.4%) patients in the mild hypothermia group — a risk difference of 3.0% (95% confidence interval [CI], 7.2% - 13.2%) and relative risk of 1.07 (95% CI, 0.86 - 1.33; P = .56).
There was also no significant difference when looking at the individual components of mortality (43.5% vs 41.0%) and poor neurologic outcome (Disability Rating Scale score >5: 4.9% vs 4.4%).
The baseline characteristics of patients were similar in the moderate and mild hypothermia groups. The lack of a significant difference in the primary outcome was consistent after adjusting for baseline covariates as well as across all subgroups.
The rates of secondary outcomes were also similar between the two groups, except for a longer length of stay in the intensive care unit in the moderate hypothermia group compared with the mild hypothermia group, which would likely add to overall costs.
The researchers note that the Targeted Hypothermia vs Targeted Normothermia After Out-of-Hospital Cardiac Arrest (TTM2) trial recently reported that targeted hypothermia at 33°C did not improve survival at 180 days compared with targeted normothermia at 37.5°C or less.
The CAPITAL CHILL study “adds to the spectrum of target temperature management, as it did not find any benefit of even further lowering temperatures to 31°C,” the study team says.
They caution that most patients in the trial had cardiac arrest secondary to a primary cardiac etiology and therefore the findings may not be applicable to cardiac arrest of all etiologies.
It’s also possible that the trial was underpowered to detect clinically important differences between moderate and mild hypothermia. Also, the number of patients presenting with a nonshockable rhythm was relatively small, and further study may be worthwhile in this subgroup, they say.
For now, however, the CAPITAL CHILL results provide no support for a lower target temperature of 31°C to improve outcomes in OHCA patients, Dr. Le May and colleagues conclude.
CAPITAL CHILL was an investigator-initiated study and funding was provided by the University of Ottawa Heart Institute Cardiac Arrest Program. Dr. Le May has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sleep apnea has many faces
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Fortunately her problem stemmed from sleep apnea, and resolved with continuous positive airway pressure (CPAP) therapy.
Wallace and Bucks performed a meta analysis of 42 studies of memory in patients with sleep apnea and found sleep apnea patients were impaired when compared to healthy controls on verbal episodic memory (immediate recall, delayed recall, learning, and recognition) and visuospatial episodic memory (immediate and delayed recall).1 A meta-analysis by Olaithe and associates found an improvement in executive function in patients with sleep apnea who were treated with CPAP.2 I think this is worth considering especially in your patients who have subjective memory disturbances and do not appear to have a mild cognitive impairment or dementia.
About 15 years ago I saw a 74-year-old man for nocturia. He had seen two urologists and had a transurethral resection of the prostate (TURP) without any real change in his nocturia. I trialed him on all sorts of medications, and he seemed to improve temporarily a little on trazodone (went from seven episodes a night to four).
Eventually, after several years, I sent him for a sleep study. He had severe sleep apnea (Apnea Hypopnea Index, 65; O2 saturations as low as 60%). With treatment, his nocturia resolved. He went from seven episodes to two each night.
Zhou and colleagues performed a meta-analysis of 13 studies looking at the association of sleep apnea with nocturia.3 They found that men with sleep apnea have a high incidence of nocturia.
Miyazato and colleagues looked at the effect of CPAP treatment on nighttime urine production in patients with obstructive sleep apnea.4 In this small study of 40 patients, mean nighttime voiding episodes decreased from 2.1 to 1.2 (P < .01).
I have seen several patients with night sweats who ended up having sleep apnea. These patients have had a resolution of their night sweats with sleep apnea treatment.
Arnardottir and colleagues found that obstructive sleep apnea was associated with frequent nocturnal sweating.5 They found that 31% of men and 33% of women with OSA had nocturnal sweating, compared with about 10% of the general population.
When the OSA patients were treated with positive airway pressure, the prevalence of nocturnal sweating decreased to 11.5%, which is similar to general population numbers. Given how common both sleep apnea and night sweats are, this is an important consideration as you evaluate night sweats.
I have seen many patients who have had atrial fibrillation and sleep apnea. Shapira-Daniels and colleagues did a prospective study of 188 patients with atrial fibrillation without a history of sleep apnea who were referred for ablation.6 All patients had home sleep studies, and testing was consistent with sleep apnea in 82% of patients.
Kanagala and associates found that patients with untreated sleep apnea had a greater chance of recurrent atrial fibrillation after cardioversion.7 Recurrence of atrial fibrillation at 12 months was 82% in untreated OSA patients, higher than the 42% recurrence in the treated OSA group (P = .013) and the 53% recurrence in control patients.
I think sleep apnea evaluation should be strongly considered in patients with atrial fibrillation and should be done before referral for ablations.
Pearl: Consider sleep apnea as a possible cause of or contributing factor to the common primary care problems of cognitive concerns, nocturia, night sweats, and atrial fibrillation.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Wallace A and Bucks RS. Memory and obstructive sleep apnea: a meta-analysis. Sleep. 2013;36(2):203. Epub 2013 Feb 1.
2. Olaithe M and Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep. 2013;36(9):1297. Epub 2013 Sep 1.
3. Zhou J et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020 Dec;24(4):1293-8.
4. Miyauchi Y et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology 2015;85:333.
5. Arnardottir ES et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: the Icelandic sleep apnoea cohort. BMJ Open. 2013 May 14;3(5):e002795. BMJ Open 2013;3:e002795
6. Shapira-Daniels A et al. Prevalence of undiagnosed sleep apnea in patients with atrial fibrillation and its impact on therapy. JACC Clin Electrophysiol. 2020;6(12):1499. Epub 2020 Aug 12.
7. Kanagala R et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589. Epub 2003 May 12.
Children and COVID: Vaccinations lower than ever as cases continue to drop
As the COVID-19 vaccine heads toward approval for children under age 12 years, the number of older children receiving it dropped for the 10th consecutive week, based on data from the Centers for Disease Control and Prevention.
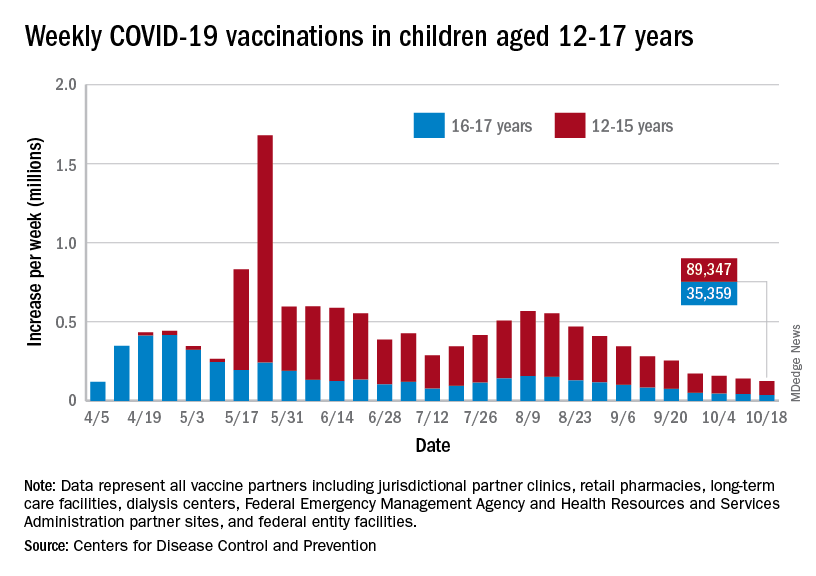
Over 47% of all children aged 12-17 years – that’s close to 12 million eligible individuals – have not received even one dose of COVID-19 vaccine, and less than 44% (about 11.1 million) were fully vaccinated as of Oct. 18, the CDC reported on its COVID Data Tracker.
, when eligibility expanded to include 12- to 15-year-olds, according to the CDC data, which also show that weekly vaccinations have never been lower.
Fortunately, the decline in new cases also continued, as the national total fell for a 6th straight week. There were more than 130,000 child cases reported during the week of Oct. 8-14, compared with 148,000 the previous week and the high of almost 252,000 in late August/early September, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
That brings the cumulative count to 6.18 million, with children accounting for 16.4% of all cases reported since the start of the pandemic. For the week of Oct. 8-14, children represented 25.5% of all COVID-19 cases in the 46 states with up-to-date online dashboards, the AAP and CHA said, noting that New York has never reported age ranges for cases and that Alabama, Nebraska, and Texas stopped reporting over the summer.
Current data indicate that child cases in California now exceed 671,000, more than any other state, followed by Florida with 439,000 (the state defines a child as someone aged 0-14 years) and Illinois with 301,000. Vermont has the highest proportion of COVID-19 cases occurring in children (24.3%), with Alaska (24.1%) and South Carolina (23.2%) just behind. The highest rate of cases – 15,569 per 100,000 children – can be found in South Carolina, while the lowest is in Hawaii (4,838 per 100,000), the AAP and CHA reported.
The total number of COVID-related deaths in children is 681 as of Oct. 18, according to the CDC, with the AAP/CHA reporting 558 as of Oct. 14, based on data from 45 states, New York City, Puerto Rico, and Guam. The CDC reports 65,655 admissions since Aug. 1, 2020, in children aged 0-17 years, and the AAP/CHA tally 23,582 since May 5, 2020, among children in 24 states and New York City.
As the COVID-19 vaccine heads toward approval for children under age 12 years, the number of older children receiving it dropped for the 10th consecutive week, based on data from the Centers for Disease Control and Prevention.
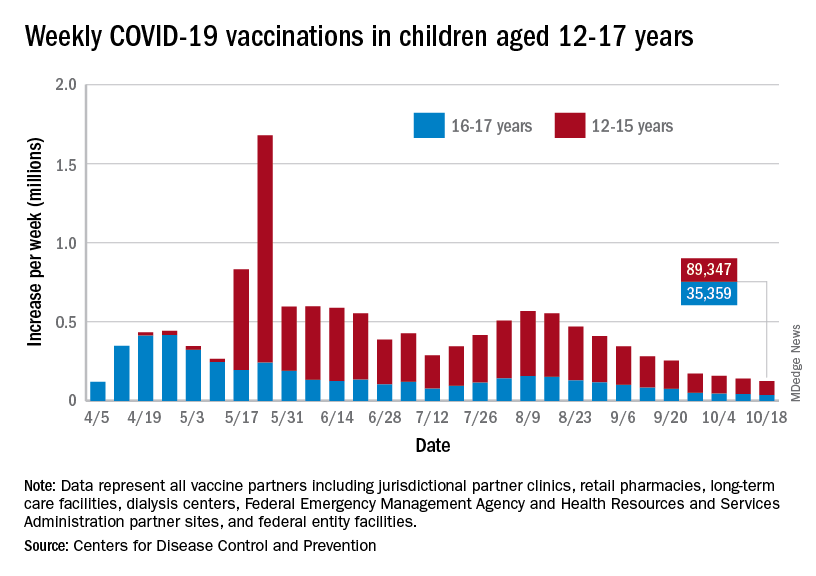
Over 47% of all children aged 12-17 years – that’s close to 12 million eligible individuals – have not received even one dose of COVID-19 vaccine, and less than 44% (about 11.1 million) were fully vaccinated as of Oct. 18, the CDC reported on its COVID Data Tracker.
, when eligibility expanded to include 12- to 15-year-olds, according to the CDC data, which also show that weekly vaccinations have never been lower.
Fortunately, the decline in new cases also continued, as the national total fell for a 6th straight week. There were more than 130,000 child cases reported during the week of Oct. 8-14, compared with 148,000 the previous week and the high of almost 252,000 in late August/early September, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
That brings the cumulative count to 6.18 million, with children accounting for 16.4% of all cases reported since the start of the pandemic. For the week of Oct. 8-14, children represented 25.5% of all COVID-19 cases in the 46 states with up-to-date online dashboards, the AAP and CHA said, noting that New York has never reported age ranges for cases and that Alabama, Nebraska, and Texas stopped reporting over the summer.
Current data indicate that child cases in California now exceed 671,000, more than any other state, followed by Florida with 439,000 (the state defines a child as someone aged 0-14 years) and Illinois with 301,000. Vermont has the highest proportion of COVID-19 cases occurring in children (24.3%), with Alaska (24.1%) and South Carolina (23.2%) just behind. The highest rate of cases – 15,569 per 100,000 children – can be found in South Carolina, while the lowest is in Hawaii (4,838 per 100,000), the AAP and CHA reported.
The total number of COVID-related deaths in children is 681 as of Oct. 18, according to the CDC, with the AAP/CHA reporting 558 as of Oct. 14, based on data from 45 states, New York City, Puerto Rico, and Guam. The CDC reports 65,655 admissions since Aug. 1, 2020, in children aged 0-17 years, and the AAP/CHA tally 23,582 since May 5, 2020, among children in 24 states and New York City.
As the COVID-19 vaccine heads toward approval for children under age 12 years, the number of older children receiving it dropped for the 10th consecutive week, based on data from the Centers for Disease Control and Prevention.
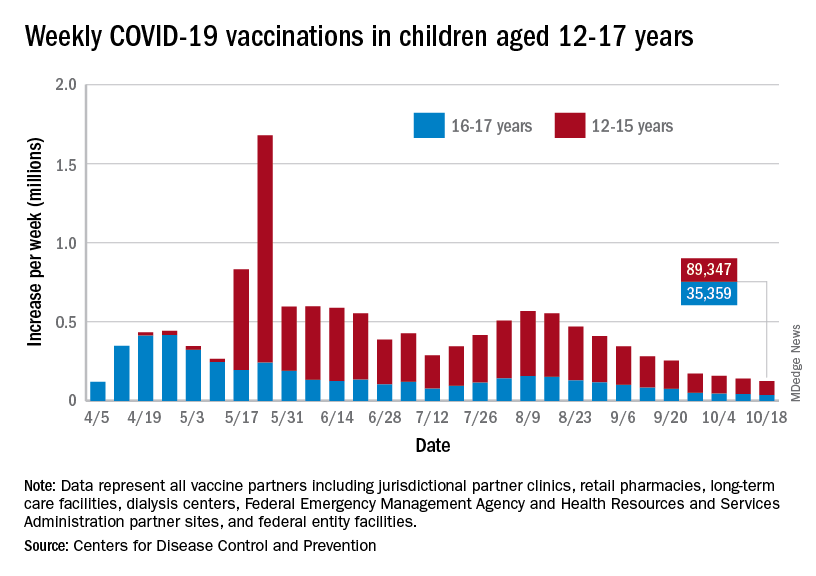
Over 47% of all children aged 12-17 years – that’s close to 12 million eligible individuals – have not received even one dose of COVID-19 vaccine, and less than 44% (about 11.1 million) were fully vaccinated as of Oct. 18, the CDC reported on its COVID Data Tracker.
, when eligibility expanded to include 12- to 15-year-olds, according to the CDC data, which also show that weekly vaccinations have never been lower.
Fortunately, the decline in new cases also continued, as the national total fell for a 6th straight week. There were more than 130,000 child cases reported during the week of Oct. 8-14, compared with 148,000 the previous week and the high of almost 252,000 in late August/early September, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
That brings the cumulative count to 6.18 million, with children accounting for 16.4% of all cases reported since the start of the pandemic. For the week of Oct. 8-14, children represented 25.5% of all COVID-19 cases in the 46 states with up-to-date online dashboards, the AAP and CHA said, noting that New York has never reported age ranges for cases and that Alabama, Nebraska, and Texas stopped reporting over the summer.
Current data indicate that child cases in California now exceed 671,000, more than any other state, followed by Florida with 439,000 (the state defines a child as someone aged 0-14 years) and Illinois with 301,000. Vermont has the highest proportion of COVID-19 cases occurring in children (24.3%), with Alaska (24.1%) and South Carolina (23.2%) just behind. The highest rate of cases – 15,569 per 100,000 children – can be found in South Carolina, while the lowest is in Hawaii (4,838 per 100,000), the AAP and CHA reported.
The total number of COVID-related deaths in children is 681 as of Oct. 18, according to the CDC, with the AAP/CHA reporting 558 as of Oct. 14, based on data from 45 states, New York City, Puerto Rico, and Guam. The CDC reports 65,655 admissions since Aug. 1, 2020, in children aged 0-17 years, and the AAP/CHA tally 23,582 since May 5, 2020, among children in 24 states and New York City.
National Academies issue guidance for childhood COVID-19 vaccines
While the U.S. Food and Drug Administration has yet to give the green light to COVID-19 vaccination for children who are under age 12, it is expected that approval will be granted. In anticipation of the FDA’s go-ahead, which is expected in the coming weeks, a new “rapid expert consultation” has identified “actionable guidance” that state and local decision-makers can use to communicate with the public. The goal is to build confidence in and promote the uptake of COVID-19 vaccines, especially for parents who are contemplating vaccinating their children.
They note that key factors in decision-making concern vaccine side effects, the efficacy of the vaccine in children, availability of research in their child’s age group, research conducted by the parents themselves, and recommendations by the child’s health care provider.
“One of the reasons that the COVID vaccine only became available for children 12 and over months after it was approved for adults is that it takes time and many, many trial participants who are closely monitored before the vaccine ever reaches the general public,” said Nusheen Ameenuddin, MD, MPH, MPA, an assistant professor of pediatrics at the Mayo Clinic, Rochester, Minn. “We continue to talk to parents about the fact that the vaccines have been very safe and effective in this group, and even though people are concerned about side effects, they are much milder and less frequent than the effects of the disease itself.”
Dr. Ameenuddin noted that the lack of data in this age group can be concerning for parents. “It’s not like other vaccines which have been available for a long time, and the clinical trial data are still limited for this age group,” she said. “But I think the main point that practitioners need to emphasize is that, even though the vaccine is new, the science for this vaccine has been around for about a decade.”
The unique circumstances of a pandemic, she pointed out, allowed for important information about effectiveness, safety, and side effects to be obtained more quickly from clinical trial data.
“We have really good evidence for kids 12 and over, about safety and effectiveness, and even though children are not small adults and have their own unique physiology, this has provided a good starting point to suggest that kids slightly younger will also respond well to the vaccines,” said Dr. Ameenuddin, who is also chair of the American Academy of Pediatrics Council on Communications and Media. “As we learn more, we can start gathering more information about even younger kids to ensure that the right dosage and spacing of vaccines can provide maximum vaccine effectiveness and protection from disease.”
The guidance was published Oct. 13 by the National Academies of Sciences, Engineering, and Medicine.
The rapid expert consultation was produced through the Societal Experts Action Network, an activity of the National Academies that is sponsored by the NASEM and the Alfred P. Sloan Foundation. The goal of SEAN is to connect researchers in the social, behavioral, and economic sciences with decision-makers to respond to policy questions related to the COVID-19 pandemic.
In their expert consultation, the authors emphasize that vaccination is critical for decreasing transmission and controlling infection, as well as limiting the emergence of future serious variants. As of Oct. 3, 2021, about 65% of the U.S. population had received at least one dose of the vaccine, and the rate has begun to lag in many areas of the country. There are a variety of reasons for vaccine hesitancy, they note, including perception of low risks from COVID-19 or of high risks from COVID-19 vaccines, exposure to media, political agendas, lack of confidence in science, and distrust of the medical establishment. The Pfizer/BioNTech vaccine is currently authorized for emergency use for individuals 12 years of age and older and fully approved for those aged 16 and older, while the Moderna and the Johnson & Johnson vaccines are authorized for emergency use for those 18 years of age and older.
Many children between the ages of 12 and 17 have not been vaccinated, and the major concerns reported by parents include not knowing enough about the long-term effects of the COVID-19 vaccine in children (88%), concerns about children experiencing serious side effects (79%), and concerns that the COVID-19 vaccine might negatively affect future fertility (73%).
The National Academies have previously released two other “rapid expert consultations” which have addressed building vaccine confidence, and both reports provide key strategies for communicating information about COVID-19 vaccines. In this paper, the focus was on communicating with parents to gain confidence in the vaccine and address concerns.
Key points
The key strategies highlighted for communicating with parents include the following:
- Emphasizing safety and efficacy: Parents should be informed about the ongoing research and clinical trials that will answer more questions about the vaccine and that there is continued monitoring for any safety risks. Pointing to the safety data from the clinical trials for 12- to 17-year-olds, and the lack of serious adverse events from the vaccine in this age group may help alleviate concerns.
- CalibriEncouraging parents to talk with a primary care provider: Research shows that parents trust family physicians and other health care practitioners to provide them with accurate information about vaccines. Local, state, and national leaders can provide messaging templates and other resources to health care professionals who are engaged in these conversations.
- Leveraging social networks to influence parents’ vaccination decisions: Parents are influenced by their social network connections. It is important to engage these networks, especially with members of their community who are considered trustworthy and influential. Social networks may also be very diverse, and include family members, friends, coworkers, social media, and members of their religious community.
While the guidance states that different groups of parents will require different messaging, they suggest that communication can begin with a focus on the things that vaccination can accomplish. In addition to preventing infection with COVID-19, it will allow children to attend school in person and participate in extracurricular activities such as sports, without risking their health. “One thing I’ve learned over several years of working with vaccine-hesitant parents is that you have to tailor each approach to the individual,” said Dr. Ameenuddin. “Different people have different concerns, and first and foremost, it’s important to listen.”
For some parents, emphasizing that the more people that can be vaccinated and the sooner it can be done, the sooner everyone can return to a normal life is a good approach, she added. “I think it’s important to emphasize both the individual and communal benefits of vaccines, but that won’t necessarily reach every person with concerns. I think it’s important to find out what is most important to individuals and work from there to find a way to connect with that family to encourage vaccination.”
Dr. Ameenuddin has no disclosures.
While the U.S. Food and Drug Administration has yet to give the green light to COVID-19 vaccination for children who are under age 12, it is expected that approval will be granted. In anticipation of the FDA’s go-ahead, which is expected in the coming weeks, a new “rapid expert consultation” has identified “actionable guidance” that state and local decision-makers can use to communicate with the public. The goal is to build confidence in and promote the uptake of COVID-19 vaccines, especially for parents who are contemplating vaccinating their children.
They note that key factors in decision-making concern vaccine side effects, the efficacy of the vaccine in children, availability of research in their child’s age group, research conducted by the parents themselves, and recommendations by the child’s health care provider.
“One of the reasons that the COVID vaccine only became available for children 12 and over months after it was approved for adults is that it takes time and many, many trial participants who are closely monitored before the vaccine ever reaches the general public,” said Nusheen Ameenuddin, MD, MPH, MPA, an assistant professor of pediatrics at the Mayo Clinic, Rochester, Minn. “We continue to talk to parents about the fact that the vaccines have been very safe and effective in this group, and even though people are concerned about side effects, they are much milder and less frequent than the effects of the disease itself.”
Dr. Ameenuddin noted that the lack of data in this age group can be concerning for parents. “It’s not like other vaccines which have been available for a long time, and the clinical trial data are still limited for this age group,” she said. “But I think the main point that practitioners need to emphasize is that, even though the vaccine is new, the science for this vaccine has been around for about a decade.”
The unique circumstances of a pandemic, she pointed out, allowed for important information about effectiveness, safety, and side effects to be obtained more quickly from clinical trial data.
“We have really good evidence for kids 12 and over, about safety and effectiveness, and even though children are not small adults and have their own unique physiology, this has provided a good starting point to suggest that kids slightly younger will also respond well to the vaccines,” said Dr. Ameenuddin, who is also chair of the American Academy of Pediatrics Council on Communications and Media. “As we learn more, we can start gathering more information about even younger kids to ensure that the right dosage and spacing of vaccines can provide maximum vaccine effectiveness and protection from disease.”
The guidance was published Oct. 13 by the National Academies of Sciences, Engineering, and Medicine.
The rapid expert consultation was produced through the Societal Experts Action Network, an activity of the National Academies that is sponsored by the NASEM and the Alfred P. Sloan Foundation. The goal of SEAN is to connect researchers in the social, behavioral, and economic sciences with decision-makers to respond to policy questions related to the COVID-19 pandemic.
In their expert consultation, the authors emphasize that vaccination is critical for decreasing transmission and controlling infection, as well as limiting the emergence of future serious variants. As of Oct. 3, 2021, about 65% of the U.S. population had received at least one dose of the vaccine, and the rate has begun to lag in many areas of the country. There are a variety of reasons for vaccine hesitancy, they note, including perception of low risks from COVID-19 or of high risks from COVID-19 vaccines, exposure to media, political agendas, lack of confidence in science, and distrust of the medical establishment. The Pfizer/BioNTech vaccine is currently authorized for emergency use for individuals 12 years of age and older and fully approved for those aged 16 and older, while the Moderna and the Johnson & Johnson vaccines are authorized for emergency use for those 18 years of age and older.
Many children between the ages of 12 and 17 have not been vaccinated, and the major concerns reported by parents include not knowing enough about the long-term effects of the COVID-19 vaccine in children (88%), concerns about children experiencing serious side effects (79%), and concerns that the COVID-19 vaccine might negatively affect future fertility (73%).
The National Academies have previously released two other “rapid expert consultations” which have addressed building vaccine confidence, and both reports provide key strategies for communicating information about COVID-19 vaccines. In this paper, the focus was on communicating with parents to gain confidence in the vaccine and address concerns.
Key points
The key strategies highlighted for communicating with parents include the following:
- Emphasizing safety and efficacy: Parents should be informed about the ongoing research and clinical trials that will answer more questions about the vaccine and that there is continued monitoring for any safety risks. Pointing to the safety data from the clinical trials for 12- to 17-year-olds, and the lack of serious adverse events from the vaccine in this age group may help alleviate concerns.
- CalibriEncouraging parents to talk with a primary care provider: Research shows that parents trust family physicians and other health care practitioners to provide them with accurate information about vaccines. Local, state, and national leaders can provide messaging templates and other resources to health care professionals who are engaged in these conversations.
- Leveraging social networks to influence parents’ vaccination decisions: Parents are influenced by their social network connections. It is important to engage these networks, especially with members of their community who are considered trustworthy and influential. Social networks may also be very diverse, and include family members, friends, coworkers, social media, and members of their religious community.
While the guidance states that different groups of parents will require different messaging, they suggest that communication can begin with a focus on the things that vaccination can accomplish. In addition to preventing infection with COVID-19, it will allow children to attend school in person and participate in extracurricular activities such as sports, without risking their health. “One thing I’ve learned over several years of working with vaccine-hesitant parents is that you have to tailor each approach to the individual,” said Dr. Ameenuddin. “Different people have different concerns, and first and foremost, it’s important to listen.”
For some parents, emphasizing that the more people that can be vaccinated and the sooner it can be done, the sooner everyone can return to a normal life is a good approach, she added. “I think it’s important to emphasize both the individual and communal benefits of vaccines, but that won’t necessarily reach every person with concerns. I think it’s important to find out what is most important to individuals and work from there to find a way to connect with that family to encourage vaccination.”
Dr. Ameenuddin has no disclosures.
While the U.S. Food and Drug Administration has yet to give the green light to COVID-19 vaccination for children who are under age 12, it is expected that approval will be granted. In anticipation of the FDA’s go-ahead, which is expected in the coming weeks, a new “rapid expert consultation” has identified “actionable guidance” that state and local decision-makers can use to communicate with the public. The goal is to build confidence in and promote the uptake of COVID-19 vaccines, especially for parents who are contemplating vaccinating their children.
They note that key factors in decision-making concern vaccine side effects, the efficacy of the vaccine in children, availability of research in their child’s age group, research conducted by the parents themselves, and recommendations by the child’s health care provider.
“One of the reasons that the COVID vaccine only became available for children 12 and over months after it was approved for adults is that it takes time and many, many trial participants who are closely monitored before the vaccine ever reaches the general public,” said Nusheen Ameenuddin, MD, MPH, MPA, an assistant professor of pediatrics at the Mayo Clinic, Rochester, Minn. “We continue to talk to parents about the fact that the vaccines have been very safe and effective in this group, and even though people are concerned about side effects, they are much milder and less frequent than the effects of the disease itself.”
Dr. Ameenuddin noted that the lack of data in this age group can be concerning for parents. “It’s not like other vaccines which have been available for a long time, and the clinical trial data are still limited for this age group,” she said. “But I think the main point that practitioners need to emphasize is that, even though the vaccine is new, the science for this vaccine has been around for about a decade.”
The unique circumstances of a pandemic, she pointed out, allowed for important information about effectiveness, safety, and side effects to be obtained more quickly from clinical trial data.
“We have really good evidence for kids 12 and over, about safety and effectiveness, and even though children are not small adults and have their own unique physiology, this has provided a good starting point to suggest that kids slightly younger will also respond well to the vaccines,” said Dr. Ameenuddin, who is also chair of the American Academy of Pediatrics Council on Communications and Media. “As we learn more, we can start gathering more information about even younger kids to ensure that the right dosage and spacing of vaccines can provide maximum vaccine effectiveness and protection from disease.”
The guidance was published Oct. 13 by the National Academies of Sciences, Engineering, and Medicine.
The rapid expert consultation was produced through the Societal Experts Action Network, an activity of the National Academies that is sponsored by the NASEM and the Alfred P. Sloan Foundation. The goal of SEAN is to connect researchers in the social, behavioral, and economic sciences with decision-makers to respond to policy questions related to the COVID-19 pandemic.
In their expert consultation, the authors emphasize that vaccination is critical for decreasing transmission and controlling infection, as well as limiting the emergence of future serious variants. As of Oct. 3, 2021, about 65% of the U.S. population had received at least one dose of the vaccine, and the rate has begun to lag in many areas of the country. There are a variety of reasons for vaccine hesitancy, they note, including perception of low risks from COVID-19 or of high risks from COVID-19 vaccines, exposure to media, political agendas, lack of confidence in science, and distrust of the medical establishment. The Pfizer/BioNTech vaccine is currently authorized for emergency use for individuals 12 years of age and older and fully approved for those aged 16 and older, while the Moderna and the Johnson & Johnson vaccines are authorized for emergency use for those 18 years of age and older.
Many children between the ages of 12 and 17 have not been vaccinated, and the major concerns reported by parents include not knowing enough about the long-term effects of the COVID-19 vaccine in children (88%), concerns about children experiencing serious side effects (79%), and concerns that the COVID-19 vaccine might negatively affect future fertility (73%).
The National Academies have previously released two other “rapid expert consultations” which have addressed building vaccine confidence, and both reports provide key strategies for communicating information about COVID-19 vaccines. In this paper, the focus was on communicating with parents to gain confidence in the vaccine and address concerns.
Key points
The key strategies highlighted for communicating with parents include the following:
- Emphasizing safety and efficacy: Parents should be informed about the ongoing research and clinical trials that will answer more questions about the vaccine and that there is continued monitoring for any safety risks. Pointing to the safety data from the clinical trials for 12- to 17-year-olds, and the lack of serious adverse events from the vaccine in this age group may help alleviate concerns.
- CalibriEncouraging parents to talk with a primary care provider: Research shows that parents trust family physicians and other health care practitioners to provide them with accurate information about vaccines. Local, state, and national leaders can provide messaging templates and other resources to health care professionals who are engaged in these conversations.
- Leveraging social networks to influence parents’ vaccination decisions: Parents are influenced by their social network connections. It is important to engage these networks, especially with members of their community who are considered trustworthy and influential. Social networks may also be very diverse, and include family members, friends, coworkers, social media, and members of their religious community.
While the guidance states that different groups of parents will require different messaging, they suggest that communication can begin with a focus on the things that vaccination can accomplish. In addition to preventing infection with COVID-19, it will allow children to attend school in person and participate in extracurricular activities such as sports, without risking their health. “One thing I’ve learned over several years of working with vaccine-hesitant parents is that you have to tailor each approach to the individual,” said Dr. Ameenuddin. “Different people have different concerns, and first and foremost, it’s important to listen.”
For some parents, emphasizing that the more people that can be vaccinated and the sooner it can be done, the sooner everyone can return to a normal life is a good approach, she added. “I think it’s important to emphasize both the individual and communal benefits of vaccines, but that won’t necessarily reach every person with concerns. I think it’s important to find out what is most important to individuals and work from there to find a way to connect with that family to encourage vaccination.”
Dr. Ameenuddin has no disclosures.
Life-threatening paradoxical bronchospasm may escape recognition in patients with COPD or asthma
according to a researcher who reviewed spirometry test results from U.S. military veterans.
Nearly 1.5% of the tests met the criteria for paradoxical bronchospasm, which refers to airway constriction that may rapidly occur after inhalation of a short-acting beta2 agonist (SABA) such as albuterol.
However, none of those reports alluded to paradoxical bronchospasm, said investigator Malvika Kaul, MD, fellow in the department of pulmonary and critical care at the University of Illinois at Chicago and the Jesse Brown Veterans Affairs Medical Center, also in Chicago.
“Paradoxical bronchospasm was neither recognized nor reported in any spirometry test results,” Dr. Kaul said in an online poster presentation at the annual meeting of the American College of Chest Physicians, held virtually this year.
By recognizing paradoxical bronchospasm, health care providers could address its clinical implications and identify potential alternative management options, according to Dr. Kaul.
“We hope in the future, education of clinicians about this phenomena is emphasized,” Dr. Kaul said in her presentation.
Recognizing paradoxical bronchospasm
In an interview, Dr. Kaul said she began researching paradoxical bronchospasm after encountering a patient who had an acute reaction to albuterol during a pulmonary function test.
“I was not taught about it, and I wasn’t recognizing that pattern very frequently in my patients,” she said.
Prescribing information for Food and Drug Administration–approved SABAs include a warning that life-threatening paradoxical bronchospasm may occur, said Dr. Kaul.
If paradoxical bronchospasm occurs, the patient should discontinue the medication immediately and start on alternative therapy, according to the available prescribing information for albuterol sulfate.
Paradoxical bronchospasm has been linked to worsened respiratory outcomes, including more frequent exacerbations, in patients with obstructive lung diseases, according to Dr. Kaul.
Two previous large studies pegged the prevalence of paradoxical bronchospasm at around 4.5% in patients with COPD or asthma, but “it has not been reported or addressed in high-risk population, such as veterans who have high prevalence of obstructive lung diseases like COPD,” Dr. Kaul said.
Latest study results
Dr. Kaul described a retrospective analysis of 1,150 pre- and postbronchodilator spirometry tests conducted in patients with COPD or asthma at the Jesse Brown VA Medical Center between 2017 and 2020.
A positive paradoxical bronchodilator response was defined as a decrease of least 12% and 200 mL in forced expiratory volume in 1 second and forced vital capacity from baseline after four puffs of albuterol were inhaled, Dr. Kaul said.
Out of 18 reviewed spirometry results that met the criteria, none of the test results reported or recognized paradoxical bronchospasm, according to Dr. Kaul.
Those meeting the criteria were predominantly COPD patients, according to Dr. Kaul, who said 12 had an underlying diagnosis COPD, 4 had asthma, and 2 had COPD and asthma.
Of the 18 patients, 13 were African American, and all but 1 of the 18 patients had a current or past smoking history, according to reported data.
A history of obstructive sleep apnea was reported in nine patients, and history of gastroesophageal reflux disease was also reported in nine patients. Eleven patients had emphysema.
Greater awareness needed
Results of this study emphasize the need to recognize potential cases paradoxical bronchospasm in clinical practice, as well as a need for more research, according to Allen J. Blaivas, DO, FCCP, chair of the CHEST Airway Disorders NetWork.
“It’s something to be on the alert for, and certainly be aware that, if your patient is telling you that they feel worse, we shouldn’t just pooh-pooh it,” said Dr. Blaivas, who is medical director of the intensive care unit at the East Orange campus of the VA New Jersey Health Care System.
Further research could focus on breaking down whether patients with suspected paradoxical bronchospasm are using metered-dose inhalers or nebulizers, whether or not they are also taking inhaled corticosteroids, and whether prospective testing can confirm paradoxical bronchospasm in patients who report tightness after using a SABA, he said in an interview.
Dr. Kaul and coauthor Israel Rubinstein, MD had no relevant relationships to disclose. Dr. Blaivas had no relevant relationships to disclose.
according to a researcher who reviewed spirometry test results from U.S. military veterans.
Nearly 1.5% of the tests met the criteria for paradoxical bronchospasm, which refers to airway constriction that may rapidly occur after inhalation of a short-acting beta2 agonist (SABA) such as albuterol.
However, none of those reports alluded to paradoxical bronchospasm, said investigator Malvika Kaul, MD, fellow in the department of pulmonary and critical care at the University of Illinois at Chicago and the Jesse Brown Veterans Affairs Medical Center, also in Chicago.
“Paradoxical bronchospasm was neither recognized nor reported in any spirometry test results,” Dr. Kaul said in an online poster presentation at the annual meeting of the American College of Chest Physicians, held virtually this year.
By recognizing paradoxical bronchospasm, health care providers could address its clinical implications and identify potential alternative management options, according to Dr. Kaul.
“We hope in the future, education of clinicians about this phenomena is emphasized,” Dr. Kaul said in her presentation.
Recognizing paradoxical bronchospasm
In an interview, Dr. Kaul said she began researching paradoxical bronchospasm after encountering a patient who had an acute reaction to albuterol during a pulmonary function test.
“I was not taught about it, and I wasn’t recognizing that pattern very frequently in my patients,” she said.
Prescribing information for Food and Drug Administration–approved SABAs include a warning that life-threatening paradoxical bronchospasm may occur, said Dr. Kaul.
If paradoxical bronchospasm occurs, the patient should discontinue the medication immediately and start on alternative therapy, according to the available prescribing information for albuterol sulfate.
Paradoxical bronchospasm has been linked to worsened respiratory outcomes, including more frequent exacerbations, in patients with obstructive lung diseases, according to Dr. Kaul.
Two previous large studies pegged the prevalence of paradoxical bronchospasm at around 4.5% in patients with COPD or asthma, but “it has not been reported or addressed in high-risk population, such as veterans who have high prevalence of obstructive lung diseases like COPD,” Dr. Kaul said.
Latest study results
Dr. Kaul described a retrospective analysis of 1,150 pre- and postbronchodilator spirometry tests conducted in patients with COPD or asthma at the Jesse Brown VA Medical Center between 2017 and 2020.
A positive paradoxical bronchodilator response was defined as a decrease of least 12% and 200 mL in forced expiratory volume in 1 second and forced vital capacity from baseline after four puffs of albuterol were inhaled, Dr. Kaul said.
Out of 18 reviewed spirometry results that met the criteria, none of the test results reported or recognized paradoxical bronchospasm, according to Dr. Kaul.
Those meeting the criteria were predominantly COPD patients, according to Dr. Kaul, who said 12 had an underlying diagnosis COPD, 4 had asthma, and 2 had COPD and asthma.
Of the 18 patients, 13 were African American, and all but 1 of the 18 patients had a current or past smoking history, according to reported data.
A history of obstructive sleep apnea was reported in nine patients, and history of gastroesophageal reflux disease was also reported in nine patients. Eleven patients had emphysema.
Greater awareness needed
Results of this study emphasize the need to recognize potential cases paradoxical bronchospasm in clinical practice, as well as a need for more research, according to Allen J. Blaivas, DO, FCCP, chair of the CHEST Airway Disorders NetWork.
“It’s something to be on the alert for, and certainly be aware that, if your patient is telling you that they feel worse, we shouldn’t just pooh-pooh it,” said Dr. Blaivas, who is medical director of the intensive care unit at the East Orange campus of the VA New Jersey Health Care System.
Further research could focus on breaking down whether patients with suspected paradoxical bronchospasm are using metered-dose inhalers or nebulizers, whether or not they are also taking inhaled corticosteroids, and whether prospective testing can confirm paradoxical bronchospasm in patients who report tightness after using a SABA, he said in an interview.
Dr. Kaul and coauthor Israel Rubinstein, MD had no relevant relationships to disclose. Dr. Blaivas had no relevant relationships to disclose.
according to a researcher who reviewed spirometry test results from U.S. military veterans.
Nearly 1.5% of the tests met the criteria for paradoxical bronchospasm, which refers to airway constriction that may rapidly occur after inhalation of a short-acting beta2 agonist (SABA) such as albuterol.
However, none of those reports alluded to paradoxical bronchospasm, said investigator Malvika Kaul, MD, fellow in the department of pulmonary and critical care at the University of Illinois at Chicago and the Jesse Brown Veterans Affairs Medical Center, also in Chicago.
“Paradoxical bronchospasm was neither recognized nor reported in any spirometry test results,” Dr. Kaul said in an online poster presentation at the annual meeting of the American College of Chest Physicians, held virtually this year.
By recognizing paradoxical bronchospasm, health care providers could address its clinical implications and identify potential alternative management options, according to Dr. Kaul.
“We hope in the future, education of clinicians about this phenomena is emphasized,” Dr. Kaul said in her presentation.
Recognizing paradoxical bronchospasm
In an interview, Dr. Kaul said she began researching paradoxical bronchospasm after encountering a patient who had an acute reaction to albuterol during a pulmonary function test.
“I was not taught about it, and I wasn’t recognizing that pattern very frequently in my patients,” she said.
Prescribing information for Food and Drug Administration–approved SABAs include a warning that life-threatening paradoxical bronchospasm may occur, said Dr. Kaul.
If paradoxical bronchospasm occurs, the patient should discontinue the medication immediately and start on alternative therapy, according to the available prescribing information for albuterol sulfate.
Paradoxical bronchospasm has been linked to worsened respiratory outcomes, including more frequent exacerbations, in patients with obstructive lung diseases, according to Dr. Kaul.
Two previous large studies pegged the prevalence of paradoxical bronchospasm at around 4.5% in patients with COPD or asthma, but “it has not been reported or addressed in high-risk population, such as veterans who have high prevalence of obstructive lung diseases like COPD,” Dr. Kaul said.
Latest study results
Dr. Kaul described a retrospective analysis of 1,150 pre- and postbronchodilator spirometry tests conducted in patients with COPD or asthma at the Jesse Brown VA Medical Center between 2017 and 2020.
A positive paradoxical bronchodilator response was defined as a decrease of least 12% and 200 mL in forced expiratory volume in 1 second and forced vital capacity from baseline after four puffs of albuterol were inhaled, Dr. Kaul said.
Out of 18 reviewed spirometry results that met the criteria, none of the test results reported or recognized paradoxical bronchospasm, according to Dr. Kaul.
Those meeting the criteria were predominantly COPD patients, according to Dr. Kaul, who said 12 had an underlying diagnosis COPD, 4 had asthma, and 2 had COPD and asthma.
Of the 18 patients, 13 were African American, and all but 1 of the 18 patients had a current or past smoking history, according to reported data.
A history of obstructive sleep apnea was reported in nine patients, and history of gastroesophageal reflux disease was also reported in nine patients. Eleven patients had emphysema.
Greater awareness needed
Results of this study emphasize the need to recognize potential cases paradoxical bronchospasm in clinical practice, as well as a need for more research, according to Allen J. Blaivas, DO, FCCP, chair of the CHEST Airway Disorders NetWork.
“It’s something to be on the alert for, and certainly be aware that, if your patient is telling you that they feel worse, we shouldn’t just pooh-pooh it,” said Dr. Blaivas, who is medical director of the intensive care unit at the East Orange campus of the VA New Jersey Health Care System.
Further research could focus on breaking down whether patients with suspected paradoxical bronchospasm are using metered-dose inhalers or nebulizers, whether or not they are also taking inhaled corticosteroids, and whether prospective testing can confirm paradoxical bronchospasm in patients who report tightness after using a SABA, he said in an interview.
Dr. Kaul and coauthor Israel Rubinstein, MD had no relevant relationships to disclose. Dr. Blaivas had no relevant relationships to disclose.
FROM CHEST 2021
Mortality in 2nd wave higher with ECMO for COVID-ARDS
For patients with refractory acute respiratory distress syndrome (ARDS) caused by COVID-19 infections, extracorporeal membrane oxygenation (ECMO) may be the treatment of last resort.
But for reasons that aren’t clear, in the second wave of the COVID-19 pandemic at a major teaching hospital, the mortality rate of patients on ECMO for COVID-induced ARDS was significantly higher than it was during the first wave, despite changes in drug therapy and clinical management, reported Rohit Reddy, BS, a second-year medical student, and colleagues at Thomas Jefferson University Hospital in Philadelphia.
During the first wave, from April to September 2020, the survival rate of patients while on ECMO in their ICUs was 67%. In contrast, for patients treated during the second wave, from November 2020 to March 2021, the ECMO survival rate was 31% (P = .003).
The 30-day survival rates were also higher in the first wave compared with the second, at 54% versus 31%, but this difference was not statistically significant.
“More research is required to develop stricter inclusion/exclusion criteria and to improve pre-ECMO management in order to improve outcomes,” Mr. Reddy said in a narrated poster presented at the annual meeting of the American College of Chest Physicians, held virtually this year.
ARDS severity higher
ARDS is a major complication of COVID-19 infections, and there is evidence to suggest that COVID-associated ARDS is more severe than ARDS caused by other causes, the investigators noted.
“ECMO, which has been used as a rescue therapy in prior viral outbreaks, has been used to support certain patients with refractory ARDS due to COVID-19, but evidence for its efficacy is limited. Respiratory failure remained a highly concerning complication in the second wave of the COVID-19 pandemic, but it is unclear how the evolution of the disease and pharmacologic utility has affected the clinical utility of ECMO,” Mr. Reddy said.
To see whether changes in disease course or in treatment could explain changes in outcomes for patients with COVID-related ARDS, the investigators compared characteristics and outcomes for patients treated in the first versus second waves of the pandemic. Their study did not include data from patients infected with the Delta variant of the SARS-CoV-2 virus, which became the predominant viral strain later in 2021.
The study included data on 28 patients treated during the first wave, and 13 during the second. The sample included 28 men and 13 women with a mean age of 51 years.
All patients had venovenous ECMO, with cannulation in the femoral or internal jugular veins; some patients received ECMO via a single double-lumen cannula.
There were no significant differences between the two time periods in patient comorbidities prior to initiation of ECMO.
Patients in the second wave were significantly more likely to receive steroids (54% vs. 100%; P = .003) and remdesivir (39% vs. 85%; P = .007). Prone positioning before ECMO was also significantly more frequent in the second wave (11% vs. 85%; P < .001).
Patients in the second wave stayed on ECMO longer – median 20 days versus 14 days for first-wave patients – but as noted before, ECMO mortality rates were significantly higher during the second wave. During the first wave, 33% of patients died while on ECMO, compared with 69% in the second wave (P = .03). Respective 30-day mortality rates were 46% versus 69% (ns).
Rates of complications during ECMO were generally comparable between the groups, including acute renal failure (39% in the first wave vs 38% in the second), sepsis (32% vs. 23%), bacterial pneumonia (11% vs. 8%), and gastrointestinal bleeding (21% vs. 15%). However, significantly more patients in the second wave had cerebral vascular accidents (4% vs. 23%; P = .050).
Senior author Hitoshi Hirose, MD, PhD, professor of surgery at Thomas Jefferson University, said in an interview that the difference in outcomes was likely caused by changes in pre-ECMO therapy between the first and second waves.
“Our study showed the incidence of sepsis had a large impact on the patient outcomes,” he wrote. “We speculate that sepsis was attributed to use of immune modulation therapy. The prevention of the sepsis would be key to improve survival of ECMO for COVID 19.”
“It’s possible that the explanation for this is that patients in the second wave were sicker in a way that wasn’t adequately measured in the first wave,” CHEST 2021 program cochair Christopher Carroll, MD, FCCP, from Connecticut Children’s Medical Center in Hartford, said in an interview.
The differences may also have been attributable to changes in virulence, or to clinical decisions to put sicker patients on ECMO, he said.
Casey Cable, MD, MSc, a pulmonary disease and critical care specialist at Virginia Commonwealth Medical Center in Richmond, also speculated in an interview that second-wave patients may have been sicker.
“One interesting piece of this story is that we now know a lot more – we know about the use of steroids plus or minus remdesivir and proning, and patients received a large majority of those treatments but still got put on ECMO,” she said. “I wonder if there is a subset of really sick patients, and no matter what we treat with – steroids, proning – whatever we do they’re just not going to do well.”
Both Dr. Carroll and Dr. Cable emphasized the importance of ECMO as a rescue therapy for patients with severe, refractory ARDS associated with COVID-19 or other diseases.
Neither Dr. Carroll nor Dr. Cable were involved in the study.
No study funding was reported. Mr. Reddy, Dr. Hirose, Dr. Carroll, and Dr. Cable disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For patients with refractory acute respiratory distress syndrome (ARDS) caused by COVID-19 infections, extracorporeal membrane oxygenation (ECMO) may be the treatment of last resort.
But for reasons that aren’t clear, in the second wave of the COVID-19 pandemic at a major teaching hospital, the mortality rate of patients on ECMO for COVID-induced ARDS was significantly higher than it was during the first wave, despite changes in drug therapy and clinical management, reported Rohit Reddy, BS, a second-year medical student, and colleagues at Thomas Jefferson University Hospital in Philadelphia.
During the first wave, from April to September 2020, the survival rate of patients while on ECMO in their ICUs was 67%. In contrast, for patients treated during the second wave, from November 2020 to March 2021, the ECMO survival rate was 31% (P = .003).
The 30-day survival rates were also higher in the first wave compared with the second, at 54% versus 31%, but this difference was not statistically significant.
“More research is required to develop stricter inclusion/exclusion criteria and to improve pre-ECMO management in order to improve outcomes,” Mr. Reddy said in a narrated poster presented at the annual meeting of the American College of Chest Physicians, held virtually this year.
ARDS severity higher
ARDS is a major complication of COVID-19 infections, and there is evidence to suggest that COVID-associated ARDS is more severe than ARDS caused by other causes, the investigators noted.
“ECMO, which has been used as a rescue therapy in prior viral outbreaks, has been used to support certain patients with refractory ARDS due to COVID-19, but evidence for its efficacy is limited. Respiratory failure remained a highly concerning complication in the second wave of the COVID-19 pandemic, but it is unclear how the evolution of the disease and pharmacologic utility has affected the clinical utility of ECMO,” Mr. Reddy said.
To see whether changes in disease course or in treatment could explain changes in outcomes for patients with COVID-related ARDS, the investigators compared characteristics and outcomes for patients treated in the first versus second waves of the pandemic. Their study did not include data from patients infected with the Delta variant of the SARS-CoV-2 virus, which became the predominant viral strain later in 2021.
The study included data on 28 patients treated during the first wave, and 13 during the second. The sample included 28 men and 13 women with a mean age of 51 years.
All patients had venovenous ECMO, with cannulation in the femoral or internal jugular veins; some patients received ECMO via a single double-lumen cannula.
There were no significant differences between the two time periods in patient comorbidities prior to initiation of ECMO.
Patients in the second wave were significantly more likely to receive steroids (54% vs. 100%; P = .003) and remdesivir (39% vs. 85%; P = .007). Prone positioning before ECMO was also significantly more frequent in the second wave (11% vs. 85%; P < .001).
Patients in the second wave stayed on ECMO longer – median 20 days versus 14 days for first-wave patients – but as noted before, ECMO mortality rates were significantly higher during the second wave. During the first wave, 33% of patients died while on ECMO, compared with 69% in the second wave (P = .03). Respective 30-day mortality rates were 46% versus 69% (ns).
Rates of complications during ECMO were generally comparable between the groups, including acute renal failure (39% in the first wave vs 38% in the second), sepsis (32% vs. 23%), bacterial pneumonia (11% vs. 8%), and gastrointestinal bleeding (21% vs. 15%). However, significantly more patients in the second wave had cerebral vascular accidents (4% vs. 23%; P = .050).
Senior author Hitoshi Hirose, MD, PhD, professor of surgery at Thomas Jefferson University, said in an interview that the difference in outcomes was likely caused by changes in pre-ECMO therapy between the first and second waves.
“Our study showed the incidence of sepsis had a large impact on the patient outcomes,” he wrote. “We speculate that sepsis was attributed to use of immune modulation therapy. The prevention of the sepsis would be key to improve survival of ECMO for COVID 19.”
“It’s possible that the explanation for this is that patients in the second wave were sicker in a way that wasn’t adequately measured in the first wave,” CHEST 2021 program cochair Christopher Carroll, MD, FCCP, from Connecticut Children’s Medical Center in Hartford, said in an interview.
The differences may also have been attributable to changes in virulence, or to clinical decisions to put sicker patients on ECMO, he said.
Casey Cable, MD, MSc, a pulmonary disease and critical care specialist at Virginia Commonwealth Medical Center in Richmond, also speculated in an interview that second-wave patients may have been sicker.
“One interesting piece of this story is that we now know a lot more – we know about the use of steroids plus or minus remdesivir and proning, and patients received a large majority of those treatments but still got put on ECMO,” she said. “I wonder if there is a subset of really sick patients, and no matter what we treat with – steroids, proning – whatever we do they’re just not going to do well.”
Both Dr. Carroll and Dr. Cable emphasized the importance of ECMO as a rescue therapy for patients with severe, refractory ARDS associated with COVID-19 or other diseases.
Neither Dr. Carroll nor Dr. Cable were involved in the study.
No study funding was reported. Mr. Reddy, Dr. Hirose, Dr. Carroll, and Dr. Cable disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For patients with refractory acute respiratory distress syndrome (ARDS) caused by COVID-19 infections, extracorporeal membrane oxygenation (ECMO) may be the treatment of last resort.
But for reasons that aren’t clear, in the second wave of the COVID-19 pandemic at a major teaching hospital, the mortality rate of patients on ECMO for COVID-induced ARDS was significantly higher than it was during the first wave, despite changes in drug therapy and clinical management, reported Rohit Reddy, BS, a second-year medical student, and colleagues at Thomas Jefferson University Hospital in Philadelphia.
During the first wave, from April to September 2020, the survival rate of patients while on ECMO in their ICUs was 67%. In contrast, for patients treated during the second wave, from November 2020 to March 2021, the ECMO survival rate was 31% (P = .003).
The 30-day survival rates were also higher in the first wave compared with the second, at 54% versus 31%, but this difference was not statistically significant.
“More research is required to develop stricter inclusion/exclusion criteria and to improve pre-ECMO management in order to improve outcomes,” Mr. Reddy said in a narrated poster presented at the annual meeting of the American College of Chest Physicians, held virtually this year.
ARDS severity higher
ARDS is a major complication of COVID-19 infections, and there is evidence to suggest that COVID-associated ARDS is more severe than ARDS caused by other causes, the investigators noted.
“ECMO, which has been used as a rescue therapy in prior viral outbreaks, has been used to support certain patients with refractory ARDS due to COVID-19, but evidence for its efficacy is limited. Respiratory failure remained a highly concerning complication in the second wave of the COVID-19 pandemic, but it is unclear how the evolution of the disease and pharmacologic utility has affected the clinical utility of ECMO,” Mr. Reddy said.
To see whether changes in disease course or in treatment could explain changes in outcomes for patients with COVID-related ARDS, the investigators compared characteristics and outcomes for patients treated in the first versus second waves of the pandemic. Their study did not include data from patients infected with the Delta variant of the SARS-CoV-2 virus, which became the predominant viral strain later in 2021.
The study included data on 28 patients treated during the first wave, and 13 during the second. The sample included 28 men and 13 women with a mean age of 51 years.
All patients had venovenous ECMO, with cannulation in the femoral or internal jugular veins; some patients received ECMO via a single double-lumen cannula.
There were no significant differences between the two time periods in patient comorbidities prior to initiation of ECMO.
Patients in the second wave were significantly more likely to receive steroids (54% vs. 100%; P = .003) and remdesivir (39% vs. 85%; P = .007). Prone positioning before ECMO was also significantly more frequent in the second wave (11% vs. 85%; P < .001).
Patients in the second wave stayed on ECMO longer – median 20 days versus 14 days for first-wave patients – but as noted before, ECMO mortality rates were significantly higher during the second wave. During the first wave, 33% of patients died while on ECMO, compared with 69% in the second wave (P = .03). Respective 30-day mortality rates were 46% versus 69% (ns).
Rates of complications during ECMO were generally comparable between the groups, including acute renal failure (39% in the first wave vs 38% in the second), sepsis (32% vs. 23%), bacterial pneumonia (11% vs. 8%), and gastrointestinal bleeding (21% vs. 15%). However, significantly more patients in the second wave had cerebral vascular accidents (4% vs. 23%; P = .050).
Senior author Hitoshi Hirose, MD, PhD, professor of surgery at Thomas Jefferson University, said in an interview that the difference in outcomes was likely caused by changes in pre-ECMO therapy between the first and second waves.
“Our study showed the incidence of sepsis had a large impact on the patient outcomes,” he wrote. “We speculate that sepsis was attributed to use of immune modulation therapy. The prevention of the sepsis would be key to improve survival of ECMO for COVID 19.”
“It’s possible that the explanation for this is that patients in the second wave were sicker in a way that wasn’t adequately measured in the first wave,” CHEST 2021 program cochair Christopher Carroll, MD, FCCP, from Connecticut Children’s Medical Center in Hartford, said in an interview.
The differences may also have been attributable to changes in virulence, or to clinical decisions to put sicker patients on ECMO, he said.
Casey Cable, MD, MSc, a pulmonary disease and critical care specialist at Virginia Commonwealth Medical Center in Richmond, also speculated in an interview that second-wave patients may have been sicker.
“One interesting piece of this story is that we now know a lot more – we know about the use of steroids plus or minus remdesivir and proning, and patients received a large majority of those treatments but still got put on ECMO,” she said. “I wonder if there is a subset of really sick patients, and no matter what we treat with – steroids, proning – whatever we do they’re just not going to do well.”
Both Dr. Carroll and Dr. Cable emphasized the importance of ECMO as a rescue therapy for patients with severe, refractory ARDS associated with COVID-19 or other diseases.
Neither Dr. Carroll nor Dr. Cable were involved in the study.
No study funding was reported. Mr. Reddy, Dr. Hirose, Dr. Carroll, and Dr. Cable disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
States can reserve COVID shots for kids 5-11 this week
States can preorder COVID-19 vaccine doses for younger children this week as they begin to set up vaccination campaigns for ages 5-11.
Vaccine advisory groups for the FDA and CDC are scheduled to discuss and approve the Pfizer shot for kids in the next three weeks. To help states and cities prepare for the rollout, the CDC issued guidance on how to set up expanded vaccination programs.
Immunization program managers can begin ordering doses on Wednesday, according to the guidance. The vials won’t be delivered until the FDA and CDC authorize the shot, but registering now will help federal officials ship doses quickly once they’re available.
Pharmacies in every state will be able to give COVID-19 shots to children, but they can only use doses that are prepared specifically for children. Ages 5-11 will need a 10-microgram dose, which is one-third of the dose administered to ages 12 and older. The guidance warns that doctors should not try to split up or fraction the adult doses.
The CDC guidance also recommends that pediatricians and family practice doctors should serve as primary places to give shots to kids. The document mentions other options, such as vaccination clinics at schools, but doesn’t endorse them as the first choice for vaccinating kids.
The CDC hasn’t yet addressed questions around whether kids should be required to get vaccinated to attend school. The decision will likely be left to state and city officials.
Federal health officials aren’t yet sure how many parents and guardians will seek shots for their younger kids right away, the AP reported. Demand may be high at first for some families, but it may not be as high as when shots first became available for adults, Marcus Plescia, MD, chief medical officer of the Association of State and Territorial Health Officials, told The Associated Press.
“We’re going to have potentially a very busy, and perhaps modestly chaotic time,” he said.
When vaccines were first authorized for adults, hospitals and pharmacies received priority for ordering shots. Some doctors felt left out. This time, however, the CDC has said that pediatricians will receive higher priority and be able to receive shipments quickly.
As the vaccine rollout begins, health officials should consider logistical concerns to address racial and economic disparities for younger kids, Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation and a former acting director of the CDC, told the AP.
If parents or guardians can’t leave work to take their kids to a pharmacy or doctor’s office, for instance, their kids may not receive a shot quickly – or at all.
“It’s really important that we recognize the barriers to vaccinations,” he said.
A version of this article first appeared on WebMD.com.
States can preorder COVID-19 vaccine doses for younger children this week as they begin to set up vaccination campaigns for ages 5-11.
Vaccine advisory groups for the FDA and CDC are scheduled to discuss and approve the Pfizer shot for kids in the next three weeks. To help states and cities prepare for the rollout, the CDC issued guidance on how to set up expanded vaccination programs.
Immunization program managers can begin ordering doses on Wednesday, according to the guidance. The vials won’t be delivered until the FDA and CDC authorize the shot, but registering now will help federal officials ship doses quickly once they’re available.
Pharmacies in every state will be able to give COVID-19 shots to children, but they can only use doses that are prepared specifically for children. Ages 5-11 will need a 10-microgram dose, which is one-third of the dose administered to ages 12 and older. The guidance warns that doctors should not try to split up or fraction the adult doses.
The CDC guidance also recommends that pediatricians and family practice doctors should serve as primary places to give shots to kids. The document mentions other options, such as vaccination clinics at schools, but doesn’t endorse them as the first choice for vaccinating kids.
The CDC hasn’t yet addressed questions around whether kids should be required to get vaccinated to attend school. The decision will likely be left to state and city officials.
Federal health officials aren’t yet sure how many parents and guardians will seek shots for their younger kids right away, the AP reported. Demand may be high at first for some families, but it may not be as high as when shots first became available for adults, Marcus Plescia, MD, chief medical officer of the Association of State and Territorial Health Officials, told The Associated Press.
“We’re going to have potentially a very busy, and perhaps modestly chaotic time,” he said.
When vaccines were first authorized for adults, hospitals and pharmacies received priority for ordering shots. Some doctors felt left out. This time, however, the CDC has said that pediatricians will receive higher priority and be able to receive shipments quickly.
As the vaccine rollout begins, health officials should consider logistical concerns to address racial and economic disparities for younger kids, Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation and a former acting director of the CDC, told the AP.
If parents or guardians can’t leave work to take their kids to a pharmacy or doctor’s office, for instance, their kids may not receive a shot quickly – or at all.
“It’s really important that we recognize the barriers to vaccinations,” he said.
A version of this article first appeared on WebMD.com.
States can preorder COVID-19 vaccine doses for younger children this week as they begin to set up vaccination campaigns for ages 5-11.
Vaccine advisory groups for the FDA and CDC are scheduled to discuss and approve the Pfizer shot for kids in the next three weeks. To help states and cities prepare for the rollout, the CDC issued guidance on how to set up expanded vaccination programs.
Immunization program managers can begin ordering doses on Wednesday, according to the guidance. The vials won’t be delivered until the FDA and CDC authorize the shot, but registering now will help federal officials ship doses quickly once they’re available.
Pharmacies in every state will be able to give COVID-19 shots to children, but they can only use doses that are prepared specifically for children. Ages 5-11 will need a 10-microgram dose, which is one-third of the dose administered to ages 12 and older. The guidance warns that doctors should not try to split up or fraction the adult doses.
The CDC guidance also recommends that pediatricians and family practice doctors should serve as primary places to give shots to kids. The document mentions other options, such as vaccination clinics at schools, but doesn’t endorse them as the first choice for vaccinating kids.
The CDC hasn’t yet addressed questions around whether kids should be required to get vaccinated to attend school. The decision will likely be left to state and city officials.
Federal health officials aren’t yet sure how many parents and guardians will seek shots for their younger kids right away, the AP reported. Demand may be high at first for some families, but it may not be as high as when shots first became available for adults, Marcus Plescia, MD, chief medical officer of the Association of State and Territorial Health Officials, told The Associated Press.
“We’re going to have potentially a very busy, and perhaps modestly chaotic time,” he said.
When vaccines were first authorized for adults, hospitals and pharmacies received priority for ordering shots. Some doctors felt left out. This time, however, the CDC has said that pediatricians will receive higher priority and be able to receive shipments quickly.
As the vaccine rollout begins, health officials should consider logistical concerns to address racial and economic disparities for younger kids, Richard Besser, MD, president and CEO of the Robert Wood Johnson Foundation and a former acting director of the CDC, told the AP.
If parents or guardians can’t leave work to take their kids to a pharmacy or doctor’s office, for instance, their kids may not receive a shot quickly – or at all.
“It’s really important that we recognize the barriers to vaccinations,” he said.
A version of this article first appeared on WebMD.com.



