User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


COVID-19–positive or exposed? What to do next
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
With new cases of COVID-19 skyrocketing to more than 240,000 a day recently in the U.S., many people are facing the same situation: A family member or friend tests positive or was exposed to someone who did, and the holiday gathering, visit, or return to work is just days or hours away. Now what?
New guidance issued Dec. 27 by the Centers for Disease Control and Prevention shortens the recommended isolation and quarantine period for the general population, coming after the agency shortened the isolation period for health care workers.
This news organization reached out to two infectious disease specialists to get answers to questions that are frequently asked in these situations.
If you have tested positive for COVID-19, what do you do next?
“If you have tested positive, you are infected. At the moment, you are [either] symptomatically affected or presymptomatically infected,’’ said Paul A. Offit, MD, director of the Vaccine Education Center and professor of pediatrics at Children’s Hospital of Philadelphia. At that point, you need to isolate for 5 days, according to the new CDC guidance. (That period has been shortened from 10 days.)
Isolation means separating the infected person from others. Quarantine refers to things you should do if you’re exposed to the virus or you have a close contact infected with COVID-19.
Under the new CDC guidelines, after the 5-day isolation, if the infected person then has no symptoms, he or she can leave isolation and then wear a mask for 5 days.
Those who test positive also need to tell their close contacts they are positive, said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
According to the CDC, the change to a shortened quarantine time is motivated by science ‘’demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of the illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.”
If you have been exposed to someone with COVID-19, what do you do next?
“If they are vaccinated and boosted, the guidance says there is no need to quarantine,” Dr. Adalja said. But the CDC guidance does recommend these people wear a well-fitting mask at all times when around others for 10 days after exposure.
For everyone else, including the unvaccinated and those who are more than 6 months out from their second Pfizer or Moderna vaccine dose, or more than 2 months from their J&J dose, the CDC recommends a quarantine for 5 days – and wearing a mask for the 5 days after that.
On a practical level, Dr. Adalja said he thinks those who are vaccinated but not boosted could also skip the quarantine and wear a mask for 10 days. Dr. Offit agrees. Because many people exposed have trouble quarantining, Dr. Offit advises those exposed who can’t follow that guidance to be sure to wear a mask for 10 days when indoors. The CDC guidance also offers that as another strategy – that if a 5-day quarantine is not feasible, the exposed person should wear a mask for 10 days when around others.
But if someone who was exposed gets symptoms, that person then enters the infected category and follows that guidance, Dr. Offit said.
When should the person who has been exposed get tested?
After the exposure, ‘’you should probably wait 2-3 days,” Dr. Offit said. “The virus has to reproduce itself.”
Testing should be done by those exposed at least once, Dr. Adalja said.
“But there’s data to support daily testing to guide their activities, but this is not CDC guidance. Home tests are sufficient for this purpose.”
At what point can the infected person mingle safely with others?
“Technically, if asymptomatic, 10 days without a mask, 5 days with a mask,” said Dr. Adalja. “I think this could also be guided with home test negativity being a gauge [as to whether to mingle].”
A version of this article first appeared on WebMD.com.
COVID-19 antigen tests may be less sensitive to Omicron: FDA
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Rapid antigen tests for COVID-19 might be less effective at detecting the Omicron variant that is spreading rapidly across the United States, according to the Food and Drug Administration.
Early data suggest that COVID-19 antigen tests “do detect the Omicron variant but may have reduced sensitivity,” the FDA said in a statement posted Dec. 28 on its website.
The FDA is working with the National Institutes of Health’s Rapid Acceleration of Diagnostics (RADx) initiative to assess the performance of antigen tests with patient samples that have the Omicron variant.
The potential for antigen tests to be less sensitive for the Omicron variant emerged in tests using patient samples containing live virus, “which represents the best way to evaluate true test performance in the short term,” the FDA said.
Initial laboratory tests using heat-activated (killed) virus samples found that antigen tests were able to detect the Omicron variant.
“It is important to note that these laboratory data are not a replacement for clinical study evaluations using patient samples with live virus, which are ongoing. The FDA and RADx are continuing to further evaluate the performance of antigen tests using patient samples with live virus,” the FDA said.
Testing still important
The agency continues to recommend use of antigen tests as directed in the authorized labeling and in accordance with the instructions included with the tests.
They note that antigen tests are generally less sensitive and less likely to pick up very early infections, compared with molecular tests.
The FDA continues to recommend that an individual with a negative antigen test who has symptoms or a high likelihood of infection because of exposure follow-up with a molecular test to determine if they have COVID-19.
An individual with a positive antigen test should self-isolate and seek follow-up care with a health care provider to determine the next steps.
The FDA, with partners and test developers, are continuing to evaluate test sensitivity, as well as the best timing and frequency of antigen testing.
The agency said that it will provide updated information and any needed recommendations when appropriate.
A version of this article first appeared on Medscape.com.
Earlier lung cancer detection may drive lower mortality
of data from the Surveillance, Epidemiology, and End Results (SEER) registries published in JAMA Network Open. Between 2006 and 2016, a stage shift occurred with an increase in stage 1 and 2 diagnoses and a decrease in stage 3 and 4 diagnoses.
While targeted therapy and immunotherapy have rightfully been credited with improved NSCLC survival, the new results underline the importance of screening, according to study author Emanuela Taioli, MD, PhD, director of the Institute for Translational Epidemiology and the associate director for population science at the Tisch Cancer Institute at Mount Sinai, New York.
She noted that the average survival for stage 1 or stage 2 patients was 57 months, but just 7 months when the stage diagnosis was 3 or 4. “So being diagnosed with stage 1 and 2 is a major driver of better survival,” said Dr. Taioli in an interview.
The study included 312,382 individuals diagnosed with NSCLC (53.4% male; median age, 68). Incidence-based, 5-year mortality declined by 3.7% (95% confidence interval, 3.4%-4.1%). Stage 1 or 2 diagnoses increased from 26.5% to 31.2% of diagnoses between 2006 and 2016 (average annual percentage change, 1.5%; 95% CI, 0.5%-2.5%).
“Immunotherapy is a very exciting field. And it is an important contributor for people who have a disease that can be treated with immunotherapy, so that’s why people focus on that. But if you can diagnose the cancer earlier, that’s the best bet,” Dr. Taioli said.
Unfortunately, many patients and physicians haven’t received that message. Even though computed tomography lung cancer screening is covered by Medicare for current or former smokers, only about 7% of eligible patients undergo annual screening. Dr. Taioli said that a belief persists that lung cancer is so deadly that early detection isn’t effective.
But advances in therapy and surgery have changed that outlook. “It’s not true anymore. People don’t know, and physicians are not educated to the idea that lung cancer can be diagnosed earlier and save lives,” she said.
People who have quit smoking may be relatively easy to convince. “They made a big step, because quitting smoking is incredibly hard. I think they will be amenable to screening because they are in a phase [of life] in which they want to take care of themselves. The physician should really explain the benefits, and I don’t think they do it very clearly now,” Dr. Taioli said.
The study is limited by its retrospective nature, and it did not include information on diagnostic method or many NSCLC risk factors.
Dr. Taioli has no relevant financial disclosures.
of data from the Surveillance, Epidemiology, and End Results (SEER) registries published in JAMA Network Open. Between 2006 and 2016, a stage shift occurred with an increase in stage 1 and 2 diagnoses and a decrease in stage 3 and 4 diagnoses.
While targeted therapy and immunotherapy have rightfully been credited with improved NSCLC survival, the new results underline the importance of screening, according to study author Emanuela Taioli, MD, PhD, director of the Institute for Translational Epidemiology and the associate director for population science at the Tisch Cancer Institute at Mount Sinai, New York.
She noted that the average survival for stage 1 or stage 2 patients was 57 months, but just 7 months when the stage diagnosis was 3 or 4. “So being diagnosed with stage 1 and 2 is a major driver of better survival,” said Dr. Taioli in an interview.
The study included 312,382 individuals diagnosed with NSCLC (53.4% male; median age, 68). Incidence-based, 5-year mortality declined by 3.7% (95% confidence interval, 3.4%-4.1%). Stage 1 or 2 diagnoses increased from 26.5% to 31.2% of diagnoses between 2006 and 2016 (average annual percentage change, 1.5%; 95% CI, 0.5%-2.5%).
“Immunotherapy is a very exciting field. And it is an important contributor for people who have a disease that can be treated with immunotherapy, so that’s why people focus on that. But if you can diagnose the cancer earlier, that’s the best bet,” Dr. Taioli said.
Unfortunately, many patients and physicians haven’t received that message. Even though computed tomography lung cancer screening is covered by Medicare for current or former smokers, only about 7% of eligible patients undergo annual screening. Dr. Taioli said that a belief persists that lung cancer is so deadly that early detection isn’t effective.
But advances in therapy and surgery have changed that outlook. “It’s not true anymore. People don’t know, and physicians are not educated to the idea that lung cancer can be diagnosed earlier and save lives,” she said.
People who have quit smoking may be relatively easy to convince. “They made a big step, because quitting smoking is incredibly hard. I think they will be amenable to screening because they are in a phase [of life] in which they want to take care of themselves. The physician should really explain the benefits, and I don’t think they do it very clearly now,” Dr. Taioli said.
The study is limited by its retrospective nature, and it did not include information on diagnostic method or many NSCLC risk factors.
Dr. Taioli has no relevant financial disclosures.
of data from the Surveillance, Epidemiology, and End Results (SEER) registries published in JAMA Network Open. Between 2006 and 2016, a stage shift occurred with an increase in stage 1 and 2 diagnoses and a decrease in stage 3 and 4 diagnoses.
While targeted therapy and immunotherapy have rightfully been credited with improved NSCLC survival, the new results underline the importance of screening, according to study author Emanuela Taioli, MD, PhD, director of the Institute for Translational Epidemiology and the associate director for population science at the Tisch Cancer Institute at Mount Sinai, New York.
She noted that the average survival for stage 1 or stage 2 patients was 57 months, but just 7 months when the stage diagnosis was 3 or 4. “So being diagnosed with stage 1 and 2 is a major driver of better survival,” said Dr. Taioli in an interview.
The study included 312,382 individuals diagnosed with NSCLC (53.4% male; median age, 68). Incidence-based, 5-year mortality declined by 3.7% (95% confidence interval, 3.4%-4.1%). Stage 1 or 2 diagnoses increased from 26.5% to 31.2% of diagnoses between 2006 and 2016 (average annual percentage change, 1.5%; 95% CI, 0.5%-2.5%).
“Immunotherapy is a very exciting field. And it is an important contributor for people who have a disease that can be treated with immunotherapy, so that’s why people focus on that. But if you can diagnose the cancer earlier, that’s the best bet,” Dr. Taioli said.
Unfortunately, many patients and physicians haven’t received that message. Even though computed tomography lung cancer screening is covered by Medicare for current or former smokers, only about 7% of eligible patients undergo annual screening. Dr. Taioli said that a belief persists that lung cancer is so deadly that early detection isn’t effective.
But advances in therapy and surgery have changed that outlook. “It’s not true anymore. People don’t know, and physicians are not educated to the idea that lung cancer can be diagnosed earlier and save lives,” she said.
People who have quit smoking may be relatively easy to convince. “They made a big step, because quitting smoking is incredibly hard. I think they will be amenable to screening because they are in a phase [of life] in which they want to take care of themselves. The physician should really explain the benefits, and I don’t think they do it very clearly now,” Dr. Taioli said.
The study is limited by its retrospective nature, and it did not include information on diagnostic method or many NSCLC risk factors.
Dr. Taioli has no relevant financial disclosures.
FROM JAMA NETWORK OPEN
Coronavirus can spread to heart, brain days after infection
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
The coronavirus that causes COVID-19 can spread to the heart and brain within days of infection and can survive for months in organs, according to a new study by the National Institutes of Health.
The virus can spread to almost every organ system in the body, which could contribute to the ongoing symptoms seen in “long COVID” patients, the study authors wrote. The study is considered one of the most comprehensive reviews of how the virus replicates in human cells and persists in the human body. It is under review for publication in the journal Nature.
“This is remarkably important work,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, told Bloomberg News. Dr. Al-Aly wasn’t involved with the NIH study but has researched the long-term effects of COVID-19.
“For a long time now, we have been scratching our heads and asking why long COVID seems to affect so many organ systems,” he said. “This paper sheds some light and may help explain why long COVID can occur even in people who had mild or asymptomatic acute disease.”
The NIH researchers sampled and analyzed tissues from autopsies on 44 patients who died after contracting the coronavirus during the first year of the pandemic. They found persistent virus particles in multiple parts of the body, including the heart and brain, for as long as 230 days after symptoms began. This could represent infection with defective virus particles, they said, which has also been seen in persistent infections among measles patients.
“We don’t yet know what burden of chronic illness will result in years to come,” Raina MacIntyre, PhD, a professor of global biosecurity at the University of New South Wales, Sydney, told Bloomberg News.
“Will we see young-onset cardiac failure in survivors or early-onset dementia?” she asked. “These are unanswered questions which call for a precautionary public health approach to mitigation of the spread of this virus.”
Unlike other COVID-19 autopsy research, the NIH team had a more comprehensive postmortem tissue collection process, which typically occurred within a day of the patient’s death, Bloomberg News reported. The researchers also used a variety of ways to preserve tissue to figure out viral levels. They were able to grow the virus collected from several tissues, including the heart, lungs, small intestine, and adrenal glands.
“Our results collectively show that, while the highest burden of SARS-CoV-2 is in the airways and lung, the virus can disseminate early during infection and infect cells throughout the entire body, including widely throughout the brain,” the study authors wrote.
A version of this article first appeared on WebMD.com.
Children and COVID: Nearly 200,000 new cases reported in 1 week
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
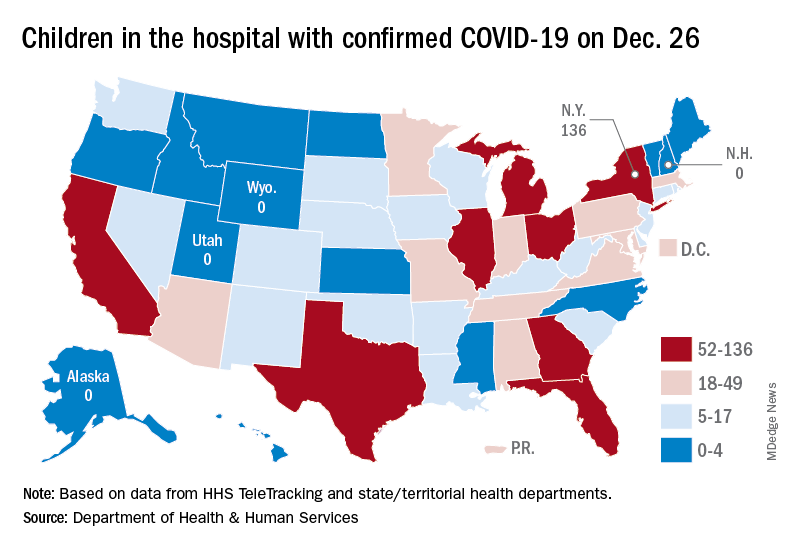
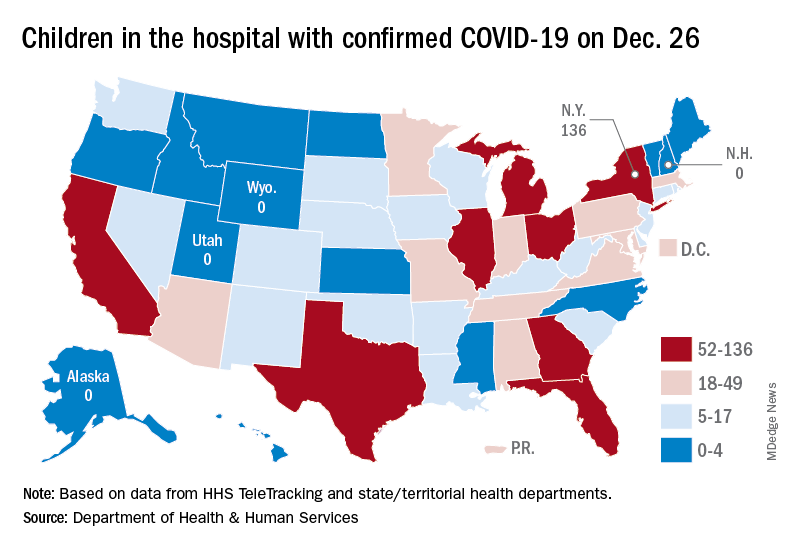
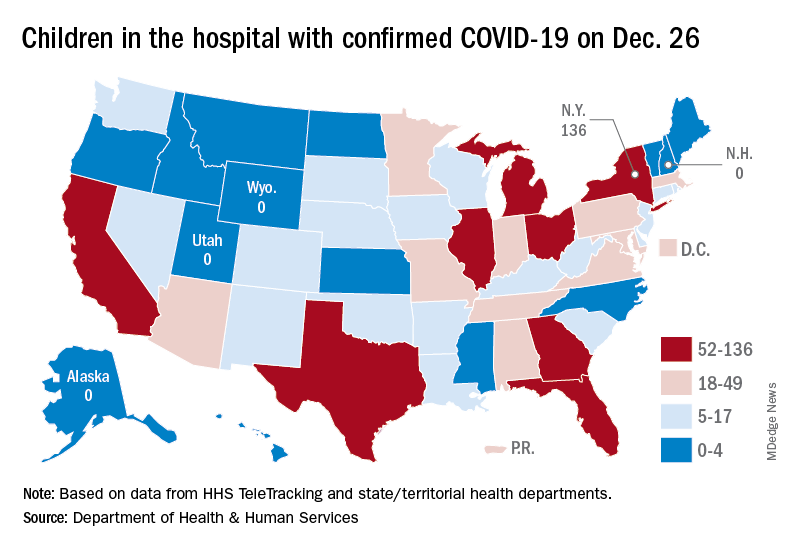
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
Does atopic dermatitis pose an increased risk of acquiring COVID-19?
According to the best available evidence, patients with atopic dermatitis (AD) do not appear to face an increased risk of acquiring COVID-19 or becoming hospitalized because of the virus.
“This is an area that will continue to evolve, and further understanding will improve the health care advice that we provide to our patients,” Jacob P. Thyssen, MD, PhD, DmSci, said at the Revolutionizing Atopic Dermatitis virtual symposium. “The general recommendation for now is to continue systemic AD treatments during the pandemic, but the risk of acquiring COVID-19 is different for different drugs.”
According to Thyssen, professor of dermatology at the University of Copenhagen, early management guidance from the European Task Force on Atopic Dermatitis (ETFAD), the European Academy of Allergy and Clinical Immunology (EAACI), and the International Eczema Council (IEC) state that patients with AD who are on biologics or immunosuppressants should continue treatment if they are not infected with COVID-19. For example, the EIC statement says that the IEC “does not recommend temporary interruption of systemic AD treatments affecting the immune system in patients without COVID-19 infection or in those who have COVID-19 but are asymptomatic or have only mild symptoms.”
Guidelines from the EAACI recommend that patients with AD who become infected with COVID-19 withhold biologic treatment for a minimum of 2 weeks until they have recovered and/or have a negative SARS-CoV-2 test.
“However, if you have more severe respiratory disease, the advice to dermatologists is to consult with an infectious medicine specialist or a pulmonologist,” Dr. Thyssen said. “That’s out of our specialty realm. But in terms of AD, there’s no reason to stop treatment as long as the patient has mild symptoms or is asymptomatic. AD patients treated with immunosuppressive agents may have a higher risk of COVID-19 complications. Treatment with traditional immunosuppressant medications does increase the risk of infections. But what about COVID-19?”
Traditional systemic immunosuppressive therapies in AD with azathioprine, cyclosporine, and methotrexate suppress the immune system for 1-3 months, Dr. Thyssen continued. “We do know that vaccination response is reduced when using these agents,” he said. “The half-life of dupilumab [Dupixent] is 12-21 days. It takes about 13 weeks before dupilumab is completely out of the system, but it’s such a targeted therapy that it doesn’t lead to any broad immunosuppression.”
Meanwhile, the half-life of JAK inhibitors such as baricitinib (Olumiant) is about 13 hours. “It’s a broader immune suppressant because there will be off-target effects if you have a high dose, but it’s much more specific than the traditional immunosuppressants,” he said. “We now have JAK1 and JAK2 inhibitors in AD, which do not interfere with vaccine responses to the same degree as traditional immunosuppressants.”
To evaluate the risk for COVID-19 in patients with AD, researchers from the Center for Dermatology Research at the University of Manchester, United Kingdom, performed a cross-sectional study of 13,162 dermatology patients seen in the U.K. between June 2018 and Feb. 2021. Of the 13,162 patients, 624 (4.7%) had AD. They found that 4.8% of patients without a history of COVID-19 infection had AD, compared with 3.4% with a history of COVID-19. The risk for COVID-19 in patients with AD was similar to that of controls (adjusted odds ratio, 0.67).
Authors of a separate cross-sectional study published in May evaluated the health insurance medical records of 269,299 patients who were tested for SARS-CoV-2 across University of California Medical Centers. Of these, 3.6% had a positive test for SARS-CoV-2. Of 5,387 patients with AD, the infection rate was 2.9%, which was lower than in those without AD (3.7%; P = .0063). Hospitalization and mortality were not increased in patients with AD.
Another study, a case-control of more than 4.6 million HMO patients in Israel, found that the intake of systemic corticosteroids, older age, comorbid cardiovascular diseases, metabolic syndrome, and COPD were independent predictors of COVID-19–associated hospitalization. Mortality as a result of COVID-19 was independently predicted by metabolic syndrome and COPD but not by any AD-related variables.
“So, for our AD patients out there, there is no need to fear that they develop a COVID-19 infection or have a severe course, but we do have a few medications that would slightly increase the risk,” Dr. Thyssen said.
In another analysis, researchers evaluated Symphony Health–derived data from the COVID-19 Research Database to evaluate the risk for COVID-19 infection in adults with AD. The AD cohort included 39,417 patients, and the cohort without AD included 397,293 patients. Among AD patients, 8,180 were prescribed prednisone, 2,793 were prescribed dupilumab, 714 were prescribed methotrexate, and 512 were prescribed cyclosporine. The risk for COVID-19 was slightly increased in the AD cohort compared with the non-AD cohort (adjusted incidence rate ratio [IRR], 1.18; P < .0001).
“There can be various explanations for this,” Dr. Thyssen said. “I still think we should maintain that AD itself is not a risk factor for COVID-19, but some of the medications may slightly increase the risk.”
In other findings, the investigators observed that treatment with dupilumab versus no systemic medication decreased the risk for COVID-19 by 34% (adjusted IRR, 0.66; P < .0001), as did methotrexate by 18% (adjusted IRR 0.82; P = .32). However, compared with no systemic medication, the use of prednisone slightly increased the risk of COVID-19 (adjusted IRR, 1.13; P = .03), as did the use of cyclosporine (adjusted IRR, 1.20; P = .32) and azathioprine (adjusted IRR, 1.61; P = .16).
More recently, researchers evaluated the records of 1,237 patients with moderate-to-severe AD (aged 9-95 years) to assess the self-reported severity of COVID-19 symptoms among those who received dupilumab versus other treatments.
Of the 1,237 patients with AD, 632 were on dupilumab, 107 were on other systemic treatments, and 498 were on limited or no treatment. Patients treated with dupilumab were less likely to report moderate-to-severe COVID-19 symptoms compared with patients who were on other systemic treatments, or limited/no treatments.
Vaccines and AD
Dr. Thyssen pointed out that the risk-benefit ratio of currently approved COVID-19 vaccines is better than the risk for an infection with SARS-CoV-2. “AD is not a contraindication to vaccination,” he said. “COVID-19 vaccine does not cause AD worsening since the vaccination response is mainly Th1 skewed.” He added that systemic immunosuppressants and JAK inhibitors used to treat AD may attenuate the vaccination response, but no attenuation is expected with dupilumab. “The half-life of JAK inhibitors is so short that vaccination followed by 1 week of pause treatment is a good strategy for patients.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi-Genzyme.
A version of this article first appeared on Medscape.com.
According to the best available evidence, patients with atopic dermatitis (AD) do not appear to face an increased risk of acquiring COVID-19 or becoming hospitalized because of the virus.
“This is an area that will continue to evolve, and further understanding will improve the health care advice that we provide to our patients,” Jacob P. Thyssen, MD, PhD, DmSci, said at the Revolutionizing Atopic Dermatitis virtual symposium. “The general recommendation for now is to continue systemic AD treatments during the pandemic, but the risk of acquiring COVID-19 is different for different drugs.”
According to Thyssen, professor of dermatology at the University of Copenhagen, early management guidance from the European Task Force on Atopic Dermatitis (ETFAD), the European Academy of Allergy and Clinical Immunology (EAACI), and the International Eczema Council (IEC) state that patients with AD who are on biologics or immunosuppressants should continue treatment if they are not infected with COVID-19. For example, the EIC statement says that the IEC “does not recommend temporary interruption of systemic AD treatments affecting the immune system in patients without COVID-19 infection or in those who have COVID-19 but are asymptomatic or have only mild symptoms.”
Guidelines from the EAACI recommend that patients with AD who become infected with COVID-19 withhold biologic treatment for a minimum of 2 weeks until they have recovered and/or have a negative SARS-CoV-2 test.
“However, if you have more severe respiratory disease, the advice to dermatologists is to consult with an infectious medicine specialist or a pulmonologist,” Dr. Thyssen said. “That’s out of our specialty realm. But in terms of AD, there’s no reason to stop treatment as long as the patient has mild symptoms or is asymptomatic. AD patients treated with immunosuppressive agents may have a higher risk of COVID-19 complications. Treatment with traditional immunosuppressant medications does increase the risk of infections. But what about COVID-19?”
Traditional systemic immunosuppressive therapies in AD with azathioprine, cyclosporine, and methotrexate suppress the immune system for 1-3 months, Dr. Thyssen continued. “We do know that vaccination response is reduced when using these agents,” he said. “The half-life of dupilumab [Dupixent] is 12-21 days. It takes about 13 weeks before dupilumab is completely out of the system, but it’s such a targeted therapy that it doesn’t lead to any broad immunosuppression.”
Meanwhile, the half-life of JAK inhibitors such as baricitinib (Olumiant) is about 13 hours. “It’s a broader immune suppressant because there will be off-target effects if you have a high dose, but it’s much more specific than the traditional immunosuppressants,” he said. “We now have JAK1 and JAK2 inhibitors in AD, which do not interfere with vaccine responses to the same degree as traditional immunosuppressants.”
To evaluate the risk for COVID-19 in patients with AD, researchers from the Center for Dermatology Research at the University of Manchester, United Kingdom, performed a cross-sectional study of 13,162 dermatology patients seen in the U.K. between June 2018 and Feb. 2021. Of the 13,162 patients, 624 (4.7%) had AD. They found that 4.8% of patients without a history of COVID-19 infection had AD, compared with 3.4% with a history of COVID-19. The risk for COVID-19 in patients with AD was similar to that of controls (adjusted odds ratio, 0.67).
Authors of a separate cross-sectional study published in May evaluated the health insurance medical records of 269,299 patients who were tested for SARS-CoV-2 across University of California Medical Centers. Of these, 3.6% had a positive test for SARS-CoV-2. Of 5,387 patients with AD, the infection rate was 2.9%, which was lower than in those without AD (3.7%; P = .0063). Hospitalization and mortality were not increased in patients with AD.
Another study, a case-control of more than 4.6 million HMO patients in Israel, found that the intake of systemic corticosteroids, older age, comorbid cardiovascular diseases, metabolic syndrome, and COPD were independent predictors of COVID-19–associated hospitalization. Mortality as a result of COVID-19 was independently predicted by metabolic syndrome and COPD but not by any AD-related variables.
“So, for our AD patients out there, there is no need to fear that they develop a COVID-19 infection or have a severe course, but we do have a few medications that would slightly increase the risk,” Dr. Thyssen said.
In another analysis, researchers evaluated Symphony Health–derived data from the COVID-19 Research Database to evaluate the risk for COVID-19 infection in adults with AD. The AD cohort included 39,417 patients, and the cohort without AD included 397,293 patients. Among AD patients, 8,180 were prescribed prednisone, 2,793 were prescribed dupilumab, 714 were prescribed methotrexate, and 512 were prescribed cyclosporine. The risk for COVID-19 was slightly increased in the AD cohort compared with the non-AD cohort (adjusted incidence rate ratio [IRR], 1.18; P < .0001).
“There can be various explanations for this,” Dr. Thyssen said. “I still think we should maintain that AD itself is not a risk factor for COVID-19, but some of the medications may slightly increase the risk.”
In other findings, the investigators observed that treatment with dupilumab versus no systemic medication decreased the risk for COVID-19 by 34% (adjusted IRR, 0.66; P < .0001), as did methotrexate by 18% (adjusted IRR 0.82; P = .32). However, compared with no systemic medication, the use of prednisone slightly increased the risk of COVID-19 (adjusted IRR, 1.13; P = .03), as did the use of cyclosporine (adjusted IRR, 1.20; P = .32) and azathioprine (adjusted IRR, 1.61; P = .16).
More recently, researchers evaluated the records of 1,237 patients with moderate-to-severe AD (aged 9-95 years) to assess the self-reported severity of COVID-19 symptoms among those who received dupilumab versus other treatments.
Of the 1,237 patients with AD, 632 were on dupilumab, 107 were on other systemic treatments, and 498 were on limited or no treatment. Patients treated with dupilumab were less likely to report moderate-to-severe COVID-19 symptoms compared with patients who were on other systemic treatments, or limited/no treatments.
Vaccines and AD
Dr. Thyssen pointed out that the risk-benefit ratio of currently approved COVID-19 vaccines is better than the risk for an infection with SARS-CoV-2. “AD is not a contraindication to vaccination,” he said. “COVID-19 vaccine does not cause AD worsening since the vaccination response is mainly Th1 skewed.” He added that systemic immunosuppressants and JAK inhibitors used to treat AD may attenuate the vaccination response, but no attenuation is expected with dupilumab. “The half-life of JAK inhibitors is so short that vaccination followed by 1 week of pause treatment is a good strategy for patients.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi-Genzyme.
A version of this article first appeared on Medscape.com.
According to the best available evidence, patients with atopic dermatitis (AD) do not appear to face an increased risk of acquiring COVID-19 or becoming hospitalized because of the virus.
“This is an area that will continue to evolve, and further understanding will improve the health care advice that we provide to our patients,” Jacob P. Thyssen, MD, PhD, DmSci, said at the Revolutionizing Atopic Dermatitis virtual symposium. “The general recommendation for now is to continue systemic AD treatments during the pandemic, but the risk of acquiring COVID-19 is different for different drugs.”
According to Thyssen, professor of dermatology at the University of Copenhagen, early management guidance from the European Task Force on Atopic Dermatitis (ETFAD), the European Academy of Allergy and Clinical Immunology (EAACI), and the International Eczema Council (IEC) state that patients with AD who are on biologics or immunosuppressants should continue treatment if they are not infected with COVID-19. For example, the EIC statement says that the IEC “does not recommend temporary interruption of systemic AD treatments affecting the immune system in patients without COVID-19 infection or in those who have COVID-19 but are asymptomatic or have only mild symptoms.”
Guidelines from the EAACI recommend that patients with AD who become infected with COVID-19 withhold biologic treatment for a minimum of 2 weeks until they have recovered and/or have a negative SARS-CoV-2 test.
“However, if you have more severe respiratory disease, the advice to dermatologists is to consult with an infectious medicine specialist or a pulmonologist,” Dr. Thyssen said. “That’s out of our specialty realm. But in terms of AD, there’s no reason to stop treatment as long as the patient has mild symptoms or is asymptomatic. AD patients treated with immunosuppressive agents may have a higher risk of COVID-19 complications. Treatment with traditional immunosuppressant medications does increase the risk of infections. But what about COVID-19?”
Traditional systemic immunosuppressive therapies in AD with azathioprine, cyclosporine, and methotrexate suppress the immune system for 1-3 months, Dr. Thyssen continued. “We do know that vaccination response is reduced when using these agents,” he said. “The half-life of dupilumab [Dupixent] is 12-21 days. It takes about 13 weeks before dupilumab is completely out of the system, but it’s such a targeted therapy that it doesn’t lead to any broad immunosuppression.”
Meanwhile, the half-life of JAK inhibitors such as baricitinib (Olumiant) is about 13 hours. “It’s a broader immune suppressant because there will be off-target effects if you have a high dose, but it’s much more specific than the traditional immunosuppressants,” he said. “We now have JAK1 and JAK2 inhibitors in AD, which do not interfere with vaccine responses to the same degree as traditional immunosuppressants.”
To evaluate the risk for COVID-19 in patients with AD, researchers from the Center for Dermatology Research at the University of Manchester, United Kingdom, performed a cross-sectional study of 13,162 dermatology patients seen in the U.K. between June 2018 and Feb. 2021. Of the 13,162 patients, 624 (4.7%) had AD. They found that 4.8% of patients without a history of COVID-19 infection had AD, compared with 3.4% with a history of COVID-19. The risk for COVID-19 in patients with AD was similar to that of controls (adjusted odds ratio, 0.67).
Authors of a separate cross-sectional study published in May evaluated the health insurance medical records of 269,299 patients who were tested for SARS-CoV-2 across University of California Medical Centers. Of these, 3.6% had a positive test for SARS-CoV-2. Of 5,387 patients with AD, the infection rate was 2.9%, which was lower than in those without AD (3.7%; P = .0063). Hospitalization and mortality were not increased in patients with AD.
Another study, a case-control of more than 4.6 million HMO patients in Israel, found that the intake of systemic corticosteroids, older age, comorbid cardiovascular diseases, metabolic syndrome, and COPD were independent predictors of COVID-19–associated hospitalization. Mortality as a result of COVID-19 was independently predicted by metabolic syndrome and COPD but not by any AD-related variables.
“So, for our AD patients out there, there is no need to fear that they develop a COVID-19 infection or have a severe course, but we do have a few medications that would slightly increase the risk,” Dr. Thyssen said.
In another analysis, researchers evaluated Symphony Health–derived data from the COVID-19 Research Database to evaluate the risk for COVID-19 infection in adults with AD. The AD cohort included 39,417 patients, and the cohort without AD included 397,293 patients. Among AD patients, 8,180 were prescribed prednisone, 2,793 were prescribed dupilumab, 714 were prescribed methotrexate, and 512 were prescribed cyclosporine. The risk for COVID-19 was slightly increased in the AD cohort compared with the non-AD cohort (adjusted incidence rate ratio [IRR], 1.18; P < .0001).
“There can be various explanations for this,” Dr. Thyssen said. “I still think we should maintain that AD itself is not a risk factor for COVID-19, but some of the medications may slightly increase the risk.”
In other findings, the investigators observed that treatment with dupilumab versus no systemic medication decreased the risk for COVID-19 by 34% (adjusted IRR, 0.66; P < .0001), as did methotrexate by 18% (adjusted IRR 0.82; P = .32). However, compared with no systemic medication, the use of prednisone slightly increased the risk of COVID-19 (adjusted IRR, 1.13; P = .03), as did the use of cyclosporine (adjusted IRR, 1.20; P = .32) and azathioprine (adjusted IRR, 1.61; P = .16).
More recently, researchers evaluated the records of 1,237 patients with moderate-to-severe AD (aged 9-95 years) to assess the self-reported severity of COVID-19 symptoms among those who received dupilumab versus other treatments.
Of the 1,237 patients with AD, 632 were on dupilumab, 107 were on other systemic treatments, and 498 were on limited or no treatment. Patients treated with dupilumab were less likely to report moderate-to-severe COVID-19 symptoms compared with patients who were on other systemic treatments, or limited/no treatments.
Vaccines and AD
Dr. Thyssen pointed out that the risk-benefit ratio of currently approved COVID-19 vaccines is better than the risk for an infection with SARS-CoV-2. “AD is not a contraindication to vaccination,” he said. “COVID-19 vaccine does not cause AD worsening since the vaccination response is mainly Th1 skewed.” He added that systemic immunosuppressants and JAK inhibitors used to treat AD may attenuate the vaccination response, but no attenuation is expected with dupilumab. “The half-life of JAK inhibitors is so short that vaccination followed by 1 week of pause treatment is a good strategy for patients.”
Dr. Thyssen disclosed that he is a speaker, advisory board member, and/or investigator for Asian, Arena, Almirall, AbbVie, Eli Lilly, LEO Pharma, Pfizer, Regeneron, and Sanofi-Genzyme.
A version of this article first appeared on Medscape.com.
FROM REVOLUTIONIZING AD 2021
What causes cancer? There’s a lot we don’t know
People with cancer are often desperate to know what caused their disease. Was it something they did? Something they could have prevented?
In a recent analysis, experts estimated that about 40% of cancers can be explained by known, often modifiable risk factors. Smoking and obesity represent the primary drivers, though a host of other factors – germline mutations, alcohol, infections, or environmental pollutants like asbestos – contribute to cancer risk as well.
But what about the remaining 60% of cancers?
The study suggests that, And a small but significant number may simply be caused by chance.
Here’s what experts suspect those missing causes might be, and why they can be so difficult to confirm.
Possibility 1: Known risk factors contribute more than we realize
For certain factors, a straight line can be drawn to cancer.
Take smoking, for instance. Decades of research have helped scientists clearly delineate tobacco’s carcinogenic effects. Researchers have pinpointed a unique set of mutations in the tumors of smokers that can be seen when cells grown in a dish are exposed to the carcinogens present in tobacco.
In addition, experts have been able to collect robust data from epidemiologic studies on smoking prevalence as well as associated cancer risks and deaths, in large part because an individual’s lifetime tobacco exposure is fairly easy to measure.
“The evidence for smoking is incredibly consistent,” Paul Brennan, PhD, a cancer epidemiologist at the World Health Organization’s International Agency for Research on Cancer, said in an interview.
For other known risk factors, such as obesity and air pollution, many more questions than answers remain.
Because of the limitations in how such factors are measured, we are likely downplaying their effects, said Richard Martin, PhD, a professor of clinical epidemiology at the University of Bristol (England).
Take obesity. Excess body weight is associated with an increased risk of at least 13 cancers. Although risk estimates vary by study and cancer type, according to a global snapshot from 2012, being overweight or obese accounted for about 4% of all cancers worldwide – 1% in low-income countries and as high as 8% in high-income countries.
However, Dr. Brennan believes “we have underestimated the effect of obesity [on cancer].”
A key reason, he said, is most studies use body mass index to determine whether someone is overweight or obese, but BMI is a poor measure of body fat. BMI does not differentiate between fat and muscle, which means two people with the same height and weight can have the same BMI, even if one is an athlete who eats lean meats and vegetables while the other lives a sedentary life and consumes large quantities of processed foods and alcohol.
On top of that, studies often only calculate a person’s BMI once, and a single measurement can’t tell you how a person’s weight has fluctuated in recent years or across different stages of their life. However, recent analyses suggest that obesity status over time may be more relevant to cancer risk than one-off measures.
In addition, many studies now suggest that alterations to our gut microbes and high blood insulin level – often seen in people who are overweight or obese – may increase the risk of cancer and speed the growth of tumors.
When these additional factors are considered, the impact of excess body fat may ultimately play a much more significant role in cancer risk. In fact, according to Dr. Brennan, “if we estimate [the effects of obesity] properly, it might at some point become the main cause of cancer.”
Possibility 2: Environmental or lifestyle factors remain under the radar
Researchers have linked many substances we consume or are exposed to in our daily lives – air pollution, toxins from industrial waste, and highly processed foods – to cancer. But the extent or contribution of potential carcinogens in our surroundings, particularly those found almost everywhere at low levels, is still largely unknown.
One simple reason is the effects of many of these substances remain difficult to assess. For instance, it is much harder to study the impact of pollutants found in food or water, in which a given population will share similar exposure levels versus tobacco, where it is possible to compare a person who smokes a pack of cigarettes a day with a person who does not smoke.
“If you’ve got exposures that are ubiquitous, it can be difficult to discern their [individual] roles,” Dr. Martin said. “There are many causes that we [likely] don’t really know because everyone has been exposed.”
On the flip side, some carcinogenic substances that people encounter for limited periods might be missed if studies are not performed at the time of exposure.
“What’s in the body at age 40 may not reflect what you were exposed at age 5-10 on the playground or soccer field,” said Graham Colditz, MD, PhD, an epidemiologist and public health expert at Washington University, St. Louis. “The technology keeps changing so we can get better measures of what you’ve got exposure to today, but how that relates to 5, 10, 15 years ago is probably very variable.”
In addition, researchers have found that many carcinogens do not cause specific mutations in a cell’s DNA; rather, studies suggest that most carcinogens lead to cancer-promoting changes in cells, such as inflammation.
“We need to think of how potential carcinogens are causing cancer,” Dr. Brennan said. Instead of provoking mutations, potential carcinogens may use a “whole other kind of pathway.” When, for instance, inflammation becomes chronic, it may spur a cascade of events that ultimately leads to cancer.
Finally, not much is known about what causes cancers in low- and middle-income countries. Most of the research to date has been in high-income countries, such the United States, Australia, and parts of Europe.
“There’s a real lack of robust epidemiological studies in other parts of the world, Latin America, Africa, parts of Asia,” Marc Gunter, PhD, a molecular epidemiologist at the IARC, told this news organization.
Possibility 3: Some cancers occur by chance
When it comes to cancer risk, an element of chance may be at play. Cancer can occur in individuals who have very little exposure to known carcinogens or have no family history of cancer.
“We all know there are people who get cancer who eat very healthy diets, are never overweight, and never smoke,” Dr. Gunter said. “Then there are people on the other end of the extreme who don’t get cancer.”
But what fraction of cancers are attributable to chance?
A controversial 2017 study published in Science suggested that, based on the rate of cell turnover in healthy tissues in the lung, pancreas, and other parts of the body, only about one-third of cancers could be linked to environmental or genetic factors. The rest, the authors claimed, occurred because of random mutations that accumulated in a person’s DNA – in other words, bad luck.
That study brought on a flood of criticism from scientists who pointed to serious flaws in the work that led the researchers to significantly overestimate the share of chance-related cancers.
The actual proportion of cancers that occur by chance is much lower, according to Dr. Brennan. “If you look at international comparisons [of cancer rates] and take a conservative estimate, you see that maybe 10% or 15% of cancers are really chance.”
Whether some cancers are caused by bad luck or undiscovered risk factors remains an open question.
But the bottom line is many unknown causes of cancer are likely environmental or lifestyle related, which means that, in theory, they can be altered, even prevented.
“There is always going to be some element of chance, but you can modify your chance, depending on your lifestyle and maybe other factors, which we don’t fully understand yet,” Dr. Gunter said.
The good news is that, when it comes to prevention, there are many ways to modify our behaviors – such as consuming fewer processed meats, going for a daily walk, or getting vaccinated against cancer-causing viruses – to improve our chances of living cancer free. And as scientists better understand more about what causes cancer, possibilities for prevention will only grow.
“There is a constant, slow growth [in knowledge] that is lowering the overall risk of cancer,” Dr. Brennan said. “We’re never going to eliminate cancer, but we will be able to control it as a disease.”
A version of this article first appeared on Medscape.com.
People with cancer are often desperate to know what caused their disease. Was it something they did? Something they could have prevented?
In a recent analysis, experts estimated that about 40% of cancers can be explained by known, often modifiable risk factors. Smoking and obesity represent the primary drivers, though a host of other factors – germline mutations, alcohol, infections, or environmental pollutants like asbestos – contribute to cancer risk as well.
But what about the remaining 60% of cancers?
The study suggests that, And a small but significant number may simply be caused by chance.
Here’s what experts suspect those missing causes might be, and why they can be so difficult to confirm.
Possibility 1: Known risk factors contribute more than we realize
For certain factors, a straight line can be drawn to cancer.
Take smoking, for instance. Decades of research have helped scientists clearly delineate tobacco’s carcinogenic effects. Researchers have pinpointed a unique set of mutations in the tumors of smokers that can be seen when cells grown in a dish are exposed to the carcinogens present in tobacco.
In addition, experts have been able to collect robust data from epidemiologic studies on smoking prevalence as well as associated cancer risks and deaths, in large part because an individual’s lifetime tobacco exposure is fairly easy to measure.
“The evidence for smoking is incredibly consistent,” Paul Brennan, PhD, a cancer epidemiologist at the World Health Organization’s International Agency for Research on Cancer, said in an interview.
For other known risk factors, such as obesity and air pollution, many more questions than answers remain.
Because of the limitations in how such factors are measured, we are likely downplaying their effects, said Richard Martin, PhD, a professor of clinical epidemiology at the University of Bristol (England).
Take obesity. Excess body weight is associated with an increased risk of at least 13 cancers. Although risk estimates vary by study and cancer type, according to a global snapshot from 2012, being overweight or obese accounted for about 4% of all cancers worldwide – 1% in low-income countries and as high as 8% in high-income countries.
However, Dr. Brennan believes “we have underestimated the effect of obesity [on cancer].”
A key reason, he said, is most studies use body mass index to determine whether someone is overweight or obese, but BMI is a poor measure of body fat. BMI does not differentiate between fat and muscle, which means two people with the same height and weight can have the same BMI, even if one is an athlete who eats lean meats and vegetables while the other lives a sedentary life and consumes large quantities of processed foods and alcohol.
On top of that, studies often only calculate a person’s BMI once, and a single measurement can’t tell you how a person’s weight has fluctuated in recent years or across different stages of their life. However, recent analyses suggest that obesity status over time may be more relevant to cancer risk than one-off measures.
In addition, many studies now suggest that alterations to our gut microbes and high blood insulin level – often seen in people who are overweight or obese – may increase the risk of cancer and speed the growth of tumors.
When these additional factors are considered, the impact of excess body fat may ultimately play a much more significant role in cancer risk. In fact, according to Dr. Brennan, “if we estimate [the effects of obesity] properly, it might at some point become the main cause of cancer.”
Possibility 2: Environmental or lifestyle factors remain under the radar
Researchers have linked many substances we consume or are exposed to in our daily lives – air pollution, toxins from industrial waste, and highly processed foods – to cancer. But the extent or contribution of potential carcinogens in our surroundings, particularly those found almost everywhere at low levels, is still largely unknown.
One simple reason is the effects of many of these substances remain difficult to assess. For instance, it is much harder to study the impact of pollutants found in food or water, in which a given population will share similar exposure levels versus tobacco, where it is possible to compare a person who smokes a pack of cigarettes a day with a person who does not smoke.
“If you’ve got exposures that are ubiquitous, it can be difficult to discern their [individual] roles,” Dr. Martin said. “There are many causes that we [likely] don’t really know because everyone has been exposed.”
On the flip side, some carcinogenic substances that people encounter for limited periods might be missed if studies are not performed at the time of exposure.
“What’s in the body at age 40 may not reflect what you were exposed at age 5-10 on the playground or soccer field,” said Graham Colditz, MD, PhD, an epidemiologist and public health expert at Washington University, St. Louis. “The technology keeps changing so we can get better measures of what you’ve got exposure to today, but how that relates to 5, 10, 15 years ago is probably very variable.”
In addition, researchers have found that many carcinogens do not cause specific mutations in a cell’s DNA; rather, studies suggest that most carcinogens lead to cancer-promoting changes in cells, such as inflammation.
“We need to think of how potential carcinogens are causing cancer,” Dr. Brennan said. Instead of provoking mutations, potential carcinogens may use a “whole other kind of pathway.” When, for instance, inflammation becomes chronic, it may spur a cascade of events that ultimately leads to cancer.
Finally, not much is known about what causes cancers in low- and middle-income countries. Most of the research to date has been in high-income countries, such the United States, Australia, and parts of Europe.
“There’s a real lack of robust epidemiological studies in other parts of the world, Latin America, Africa, parts of Asia,” Marc Gunter, PhD, a molecular epidemiologist at the IARC, told this news organization.
Possibility 3: Some cancers occur by chance
When it comes to cancer risk, an element of chance may be at play. Cancer can occur in individuals who have very little exposure to known carcinogens or have no family history of cancer.
“We all know there are people who get cancer who eat very healthy diets, are never overweight, and never smoke,” Dr. Gunter said. “Then there are people on the other end of the extreme who don’t get cancer.”
But what fraction of cancers are attributable to chance?
A controversial 2017 study published in Science suggested that, based on the rate of cell turnover in healthy tissues in the lung, pancreas, and other parts of the body, only about one-third of cancers could be linked to environmental or genetic factors. The rest, the authors claimed, occurred because of random mutations that accumulated in a person’s DNA – in other words, bad luck.
That study brought on a flood of criticism from scientists who pointed to serious flaws in the work that led the researchers to significantly overestimate the share of chance-related cancers.
The actual proportion of cancers that occur by chance is much lower, according to Dr. Brennan. “If you look at international comparisons [of cancer rates] and take a conservative estimate, you see that maybe 10% or 15% of cancers are really chance.”
Whether some cancers are caused by bad luck or undiscovered risk factors remains an open question.
But the bottom line is many unknown causes of cancer are likely environmental or lifestyle related, which means that, in theory, they can be altered, even prevented.
“There is always going to be some element of chance, but you can modify your chance, depending on your lifestyle and maybe other factors, which we don’t fully understand yet,” Dr. Gunter said.
The good news is that, when it comes to prevention, there are many ways to modify our behaviors – such as consuming fewer processed meats, going for a daily walk, or getting vaccinated against cancer-causing viruses – to improve our chances of living cancer free. And as scientists better understand more about what causes cancer, possibilities for prevention will only grow.
“There is a constant, slow growth [in knowledge] that is lowering the overall risk of cancer,” Dr. Brennan said. “We’re never going to eliminate cancer, but we will be able to control it as a disease.”
A version of this article first appeared on Medscape.com.
People with cancer are often desperate to know what caused their disease. Was it something they did? Something they could have prevented?
In a recent analysis, experts estimated that about 40% of cancers can be explained by known, often modifiable risk factors. Smoking and obesity represent the primary drivers, though a host of other factors – germline mutations, alcohol, infections, or environmental pollutants like asbestos – contribute to cancer risk as well.
But what about the remaining 60% of cancers?
The study suggests that, And a small but significant number may simply be caused by chance.
Here’s what experts suspect those missing causes might be, and why they can be so difficult to confirm.
Possibility 1: Known risk factors contribute more than we realize
For certain factors, a straight line can be drawn to cancer.
Take smoking, for instance. Decades of research have helped scientists clearly delineate tobacco’s carcinogenic effects. Researchers have pinpointed a unique set of mutations in the tumors of smokers that can be seen when cells grown in a dish are exposed to the carcinogens present in tobacco.
In addition, experts have been able to collect robust data from epidemiologic studies on smoking prevalence as well as associated cancer risks and deaths, in large part because an individual’s lifetime tobacco exposure is fairly easy to measure.
“The evidence for smoking is incredibly consistent,” Paul Brennan, PhD, a cancer epidemiologist at the World Health Organization’s International Agency for Research on Cancer, said in an interview.
For other known risk factors, such as obesity and air pollution, many more questions than answers remain.
Because of the limitations in how such factors are measured, we are likely downplaying their effects, said Richard Martin, PhD, a professor of clinical epidemiology at the University of Bristol (England).
Take obesity. Excess body weight is associated with an increased risk of at least 13 cancers. Although risk estimates vary by study and cancer type, according to a global snapshot from 2012, being overweight or obese accounted for about 4% of all cancers worldwide – 1% in low-income countries and as high as 8% in high-income countries.
However, Dr. Brennan believes “we have underestimated the effect of obesity [on cancer].”
A key reason, he said, is most studies use body mass index to determine whether someone is overweight or obese, but BMI is a poor measure of body fat. BMI does not differentiate between fat and muscle, which means two people with the same height and weight can have the same BMI, even if one is an athlete who eats lean meats and vegetables while the other lives a sedentary life and consumes large quantities of processed foods and alcohol.
On top of that, studies often only calculate a person’s BMI once, and a single measurement can’t tell you how a person’s weight has fluctuated in recent years or across different stages of their life. However, recent analyses suggest that obesity status over time may be more relevant to cancer risk than one-off measures.
In addition, many studies now suggest that alterations to our gut microbes and high blood insulin level – often seen in people who are overweight or obese – may increase the risk of cancer and speed the growth of tumors.
When these additional factors are considered, the impact of excess body fat may ultimately play a much more significant role in cancer risk. In fact, according to Dr. Brennan, “if we estimate [the effects of obesity] properly, it might at some point become the main cause of cancer.”
Possibility 2: Environmental or lifestyle factors remain under the radar
Researchers have linked many substances we consume or are exposed to in our daily lives – air pollution, toxins from industrial waste, and highly processed foods – to cancer. But the extent or contribution of potential carcinogens in our surroundings, particularly those found almost everywhere at low levels, is still largely unknown.
One simple reason is the effects of many of these substances remain difficult to assess. For instance, it is much harder to study the impact of pollutants found in food or water, in which a given population will share similar exposure levels versus tobacco, where it is possible to compare a person who smokes a pack of cigarettes a day with a person who does not smoke.
“If you’ve got exposures that are ubiquitous, it can be difficult to discern their [individual] roles,” Dr. Martin said. “There are many causes that we [likely] don’t really know because everyone has been exposed.”
On the flip side, some carcinogenic substances that people encounter for limited periods might be missed if studies are not performed at the time of exposure.
“What’s in the body at age 40 may not reflect what you were exposed at age 5-10 on the playground or soccer field,” said Graham Colditz, MD, PhD, an epidemiologist and public health expert at Washington University, St. Louis. “The technology keeps changing so we can get better measures of what you’ve got exposure to today, but how that relates to 5, 10, 15 years ago is probably very variable.”
In addition, researchers have found that many carcinogens do not cause specific mutations in a cell’s DNA; rather, studies suggest that most carcinogens lead to cancer-promoting changes in cells, such as inflammation.
“We need to think of how potential carcinogens are causing cancer,” Dr. Brennan said. Instead of provoking mutations, potential carcinogens may use a “whole other kind of pathway.” When, for instance, inflammation becomes chronic, it may spur a cascade of events that ultimately leads to cancer.
Finally, not much is known about what causes cancers in low- and middle-income countries. Most of the research to date has been in high-income countries, such the United States, Australia, and parts of Europe.
“There’s a real lack of robust epidemiological studies in other parts of the world, Latin America, Africa, parts of Asia,” Marc Gunter, PhD, a molecular epidemiologist at the IARC, told this news organization.
Possibility 3: Some cancers occur by chance
When it comes to cancer risk, an element of chance may be at play. Cancer can occur in individuals who have very little exposure to known carcinogens or have no family history of cancer.
“We all know there are people who get cancer who eat very healthy diets, are never overweight, and never smoke,” Dr. Gunter said. “Then there are people on the other end of the extreme who don’t get cancer.”
But what fraction of cancers are attributable to chance?
A controversial 2017 study published in Science suggested that, based on the rate of cell turnover in healthy tissues in the lung, pancreas, and other parts of the body, only about one-third of cancers could be linked to environmental or genetic factors. The rest, the authors claimed, occurred because of random mutations that accumulated in a person’s DNA – in other words, bad luck.
That study brought on a flood of criticism from scientists who pointed to serious flaws in the work that led the researchers to significantly overestimate the share of chance-related cancers.
The actual proportion of cancers that occur by chance is much lower, according to Dr. Brennan. “If you look at international comparisons [of cancer rates] and take a conservative estimate, you see that maybe 10% or 15% of cancers are really chance.”
Whether some cancers are caused by bad luck or undiscovered risk factors remains an open question.
But the bottom line is many unknown causes of cancer are likely environmental or lifestyle related, which means that, in theory, they can be altered, even prevented.
“There is always going to be some element of chance, but you can modify your chance, depending on your lifestyle and maybe other factors, which we don’t fully understand yet,” Dr. Gunter said.
The good news is that, when it comes to prevention, there are many ways to modify our behaviors – such as consuming fewer processed meats, going for a daily walk, or getting vaccinated against cancer-causing viruses – to improve our chances of living cancer free. And as scientists better understand more about what causes cancer, possibilities for prevention will only grow.
“There is a constant, slow growth [in knowledge] that is lowering the overall risk of cancer,” Dr. Brennan said. “We’re never going to eliminate cancer, but we will be able to control it as a disease.”
A version of this article first appeared on Medscape.com.
COVID booster protection may wane in about 10 weeks, new data show
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
, according to new data from Britain.
U.K. health officials shared the data just before Christmas and noted that there haven’t been enough severe cases of the Omicron variant to calculate how well boosters protect against severe disease. But they believe the extra shots provide significant protection against hospitalization and death.
“It will be a few weeks before effectiveness against severe disease with Omicron can be estimated,” U.K. Health Security Agency officials wrote in the report. “However, based on experience with previous variants, this is likely to be substantially higher than the estimates against symptomatic disease.”
Since countries began reporting Omicron cases in November, multiple studies have suggested the variant is better at escaping antibodies from vaccination and previous infection, according to the New York Times. The U.K. report adds to that, noting that both the initial vaccine series and booster doses were less effective and faded faster against the Omicron variant than the Delta variant.
Among those who received two doses of the AstraZeneca vaccine, a booster of the Pfizer or Moderna vaccine was 60% effective at preventing symptomatic disease 2 to 4 weeks after the shot. But after 10 weeks, the Pfizer booster was 35% effective, and the Moderna booster was 45% effective. (The AstraZeneca vaccine is not authorized in the United States, but the Johnson & Johnson shot uses a similar technology, the New York Times reported.)
Among those who received three Pfizer doses, vaccine effectiveness was 70% about a week after the booster but dropped to 45% after 10 weeks. At the same time, those who received an initial two-dose series of the Pfizer vaccine and then a Moderna booster seemed to have 75% effectiveness up to 9 weeks.
The report was based on an analysis of 148,000 Delta cases and 68,000 Omicron cases in the United Kingdom through Dec. 20. So far, the U.K. health officials wrote, Omicron infections appear to be less severe and less likely to lead to hospitalization than Delta infections. At that time, 132 people with lab-confirmed Omicron had been admitted to hospitals, and 14 deaths had been reported among ages 52-96.
“This analysis is preliminary because of the small numbers of Omicron cases currently in hospital and the limited spread of Omicron into older age groups as yet,” the report said.
The reinfection rate has also increased for the Omicron variant, the report found. Among the 116,000 people who had an Omicron infection, about 11,000 -- or 9.5% -- were linked to a previously confirmed infection, which is likely an undercount of reinfections. In the data analyzed, 69 Omicron cases were a third episode of COVID-19 infection, and 290 cases occurred 60-89 days after a first infection.
A version of this article first appeared on WebMD.com.
Remdesivir may keep unvaccinated out of the hospital: Study
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
The antiviral remdesivir, an intravenous drug given mostly to seriously ill COVID-19 patients in hospitals, could keep unvaccinated people who become infected out of the hospital if given on an outpatient basis, a new study says.
Researchers studied 562 unvaccinated people from September 2020 to April 2021, according to the study published in the New England Journal of Medicine. The study determined the risk of hospitalization or death was 87% lower in study participants who were given remdesivir than participants who received a placebo.
All participants were at high risk of developing severe COVID-19 because of their age – they were over 60 – or because they had an underlying medical condition such as diabetes or obesity.
An important caveat: The findings are based on data collected before the Delta variant surged in the summer of 2021 or the Omicron variant surged late in the year, the Washington Post reported.
The new study says the drug could be helpful in keeping vaccinated as well as unvaccinated people out of the hospital – an important factor as the Omicron surge threatens to overwhelm health systems around the world.
Remdesivir could be a boon for COVID-19 patients in parts of the world that don’t have vaccines or for patients with immunocompromised systems.
“These data provide evidence that a 3-day course of remdesivir could play a critical role in helping COVID-19 patients stay out of the hospital,” Robert L. Gottlieb, MD, PhD, the therapeutic lead for COVID-19 research at Baylor Scott & White Health in Dallas, said in a news release from Gilead Pharmaceuticals. “While our hospitals are ready to assist patients in need, prevention and early intervention are preferable to reduce the risk of disease progression and allow patients not requiring oxygen to recover from home when appropriate.”
Remdesivir was the first antiviral for COVID-19 authorized by the Food and Drug Administration. It was given to then-President Donald Trump when he was hospitalized with COVID-19 in October 2020.
Gilead released the study findings in September.
A version of this article first appeared on WebMD.com.
Not all patients with community-acquired pneumonia respond to adjunctive dexamethasone
Key clinical point: Neutrophil count, white blood cell (WBC) count, or neutrophil-lymphocyte ratio (NLR) may help in ascertaining which patients hospitalized for community-acquired pneumonia (CAP) would benefit from adjunctive oral dexamethasone therapy.
Main finding: Among patients with a high neutrophil count, WBC count, or NLR who did not die in hospital, those who received dexamethasone had a shorter median length of stay (LOS) than those who received placebo (4 days vs. 6 days), whereas patients with low values for these parameters showed no difference in LOS between those receiving placebo and dexamethasone (P < .05).
Study details: Findings are from a post hoc analysis on 354 out of the 401 non-ICU patients with CAP included in the randomized placebo-controlled Santeon-CAP trial who were randomly assigned to receive either placebo or oral dexamethasone.
Disclosures: The study was sponsored by St. Antonius research fund. The authors declared no conflicts of interests.
Source: Wittermans E et al. Eur J Intern Med. 2021 (Nov 12). Doi: 10.1016/j.ejim.2021.10.030.
Key clinical point: Neutrophil count, white blood cell (WBC) count, or neutrophil-lymphocyte ratio (NLR) may help in ascertaining which patients hospitalized for community-acquired pneumonia (CAP) would benefit from adjunctive oral dexamethasone therapy.
Main finding: Among patients with a high neutrophil count, WBC count, or NLR who did not die in hospital, those who received dexamethasone had a shorter median length of stay (LOS) than those who received placebo (4 days vs. 6 days), whereas patients with low values for these parameters showed no difference in LOS between those receiving placebo and dexamethasone (P < .05).
Study details: Findings are from a post hoc analysis on 354 out of the 401 non-ICU patients with CAP included in the randomized placebo-controlled Santeon-CAP trial who were randomly assigned to receive either placebo or oral dexamethasone.
Disclosures: The study was sponsored by St. Antonius research fund. The authors declared no conflicts of interests.
Source: Wittermans E et al. Eur J Intern Med. 2021 (Nov 12). Doi: 10.1016/j.ejim.2021.10.030.
Key clinical point: Neutrophil count, white blood cell (WBC) count, or neutrophil-lymphocyte ratio (NLR) may help in ascertaining which patients hospitalized for community-acquired pneumonia (CAP) would benefit from adjunctive oral dexamethasone therapy.
Main finding: Among patients with a high neutrophil count, WBC count, or NLR who did not die in hospital, those who received dexamethasone had a shorter median length of stay (LOS) than those who received placebo (4 days vs. 6 days), whereas patients with low values for these parameters showed no difference in LOS between those receiving placebo and dexamethasone (P < .05).
Study details: Findings are from a post hoc analysis on 354 out of the 401 non-ICU patients with CAP included in the randomized placebo-controlled Santeon-CAP trial who were randomly assigned to receive either placebo or oral dexamethasone.
Disclosures: The study was sponsored by St. Antonius research fund. The authors declared no conflicts of interests.
Source: Wittermans E et al. Eur J Intern Med. 2021 (Nov 12). Doi: 10.1016/j.ejim.2021.10.030.

