User login
Five prognostic indexes come up short for planning early CLL treatment
Prognostic indexes have been developed recently to assess time to first treatment in early-stage chronic lymphocytic leukemia (CLL) patients. However, none of five indexes evaluated in a study showed more than a moderate prognostic value or were precise enough to permit clinical decisions to be made, according to a report by Spanish researchers.
Their study, published in Clinical Lymphoma, Myeloma and Leukemia, examined the comparative prognostic value of five prognostic indexes – the CLL-IPI, the Barcelona-Brno, the IPS-A, the CLL-01, and the Tailored approach – on evaluating 428 Binet A CLL patients from a multicenter Spanish database which contained the relevant necessary clinical and biological information. The predictive value of the scores was assessed with Harrell´s C index and receiver operating characteristic curve (area under the curve, AUC).
The researchers found a significant association between time to first treatment and risk subgroups for all the indexes used. The most accurate index was the IPS-A (Harrell´s C, 0.72; AUC, 0.76), followed by the CLL-01 (Harrell´s C, 0.69; AUC, 0.70), the CLL-IPI (Harrell´s C, .69; AUC, 0.69), the Barcelona-Brno (Harrell´s C: 0.67, AUC, 0.69) and the Tailored approach (Harrell´s C, 0.61 and 0.58, AUCs, 0.58 and 0.54).
However, the concordance between four of the five indexes (the Tailored approach was not included for technical reasons) compared was low (44%): 146 cases were classified as low risk with all four indexes tested, 36 as intermediate risk, and 4 as high risk. In the remaining 242 patients (56%) at least one discrepancy was detected in the allocation among prognostic subgroups between the indexes. However, only 12 patients (3%) were allocated as low and high risk at the same time with different indexes, showing the extremes of the discordance.
These data suggest that, although all of these indexes “significantly improve clinical staging and help physicians in routine clinical practice, it is necessary to harmonize larger cohorts of patients in order to define the best index for treatment decision making in the real world,” the authors stated.
“All the models had a moderate prognostic value to predict time to first therapy. ... None of them was precise enough to allow clinical decisions based exclusively on it,” the authors concluded.
The study was supported by grants from the Spanish government and a variety of nonprofit institutions. The authors reported no commercial disclosures.
SOURCE: Gascon y Marín IG et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 13. doi: 10.1016/j.clml.2020.03.003.
Prognostic indexes have been developed recently to assess time to first treatment in early-stage chronic lymphocytic leukemia (CLL) patients. However, none of five indexes evaluated in a study showed more than a moderate prognostic value or were precise enough to permit clinical decisions to be made, according to a report by Spanish researchers.
Their study, published in Clinical Lymphoma, Myeloma and Leukemia, examined the comparative prognostic value of five prognostic indexes – the CLL-IPI, the Barcelona-Brno, the IPS-A, the CLL-01, and the Tailored approach – on evaluating 428 Binet A CLL patients from a multicenter Spanish database which contained the relevant necessary clinical and biological information. The predictive value of the scores was assessed with Harrell´s C index and receiver operating characteristic curve (area under the curve, AUC).
The researchers found a significant association between time to first treatment and risk subgroups for all the indexes used. The most accurate index was the IPS-A (Harrell´s C, 0.72; AUC, 0.76), followed by the CLL-01 (Harrell´s C, 0.69; AUC, 0.70), the CLL-IPI (Harrell´s C, .69; AUC, 0.69), the Barcelona-Brno (Harrell´s C: 0.67, AUC, 0.69) and the Tailored approach (Harrell´s C, 0.61 and 0.58, AUCs, 0.58 and 0.54).
However, the concordance between four of the five indexes (the Tailored approach was not included for technical reasons) compared was low (44%): 146 cases were classified as low risk with all four indexes tested, 36 as intermediate risk, and 4 as high risk. In the remaining 242 patients (56%) at least one discrepancy was detected in the allocation among prognostic subgroups between the indexes. However, only 12 patients (3%) were allocated as low and high risk at the same time with different indexes, showing the extremes of the discordance.
These data suggest that, although all of these indexes “significantly improve clinical staging and help physicians in routine clinical practice, it is necessary to harmonize larger cohorts of patients in order to define the best index for treatment decision making in the real world,” the authors stated.
“All the models had a moderate prognostic value to predict time to first therapy. ... None of them was precise enough to allow clinical decisions based exclusively on it,” the authors concluded.
The study was supported by grants from the Spanish government and a variety of nonprofit institutions. The authors reported no commercial disclosures.
SOURCE: Gascon y Marín IG et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 13. doi: 10.1016/j.clml.2020.03.003.
Prognostic indexes have been developed recently to assess time to first treatment in early-stage chronic lymphocytic leukemia (CLL) patients. However, none of five indexes evaluated in a study showed more than a moderate prognostic value or were precise enough to permit clinical decisions to be made, according to a report by Spanish researchers.
Their study, published in Clinical Lymphoma, Myeloma and Leukemia, examined the comparative prognostic value of five prognostic indexes – the CLL-IPI, the Barcelona-Brno, the IPS-A, the CLL-01, and the Tailored approach – on evaluating 428 Binet A CLL patients from a multicenter Spanish database which contained the relevant necessary clinical and biological information. The predictive value of the scores was assessed with Harrell´s C index and receiver operating characteristic curve (area under the curve, AUC).
The researchers found a significant association between time to first treatment and risk subgroups for all the indexes used. The most accurate index was the IPS-A (Harrell´s C, 0.72; AUC, 0.76), followed by the CLL-01 (Harrell´s C, 0.69; AUC, 0.70), the CLL-IPI (Harrell´s C, .69; AUC, 0.69), the Barcelona-Brno (Harrell´s C: 0.67, AUC, 0.69) and the Tailored approach (Harrell´s C, 0.61 and 0.58, AUCs, 0.58 and 0.54).
However, the concordance between four of the five indexes (the Tailored approach was not included for technical reasons) compared was low (44%): 146 cases were classified as low risk with all four indexes tested, 36 as intermediate risk, and 4 as high risk. In the remaining 242 patients (56%) at least one discrepancy was detected in the allocation among prognostic subgroups between the indexes. However, only 12 patients (3%) were allocated as low and high risk at the same time with different indexes, showing the extremes of the discordance.
These data suggest that, although all of these indexes “significantly improve clinical staging and help physicians in routine clinical practice, it is necessary to harmonize larger cohorts of patients in order to define the best index for treatment decision making in the real world,” the authors stated.
“All the models had a moderate prognostic value to predict time to first therapy. ... None of them was precise enough to allow clinical decisions based exclusively on it,” the authors concluded.
The study was supported by grants from the Spanish government and a variety of nonprofit institutions. The authors reported no commercial disclosures.
SOURCE: Gascon y Marín IG et al. Clin Lymphoma Myeloma Leuk. 2020 Apr 13. doi: 10.1016/j.clml.2020.03.003.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
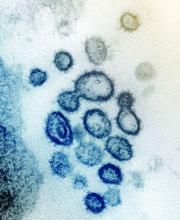
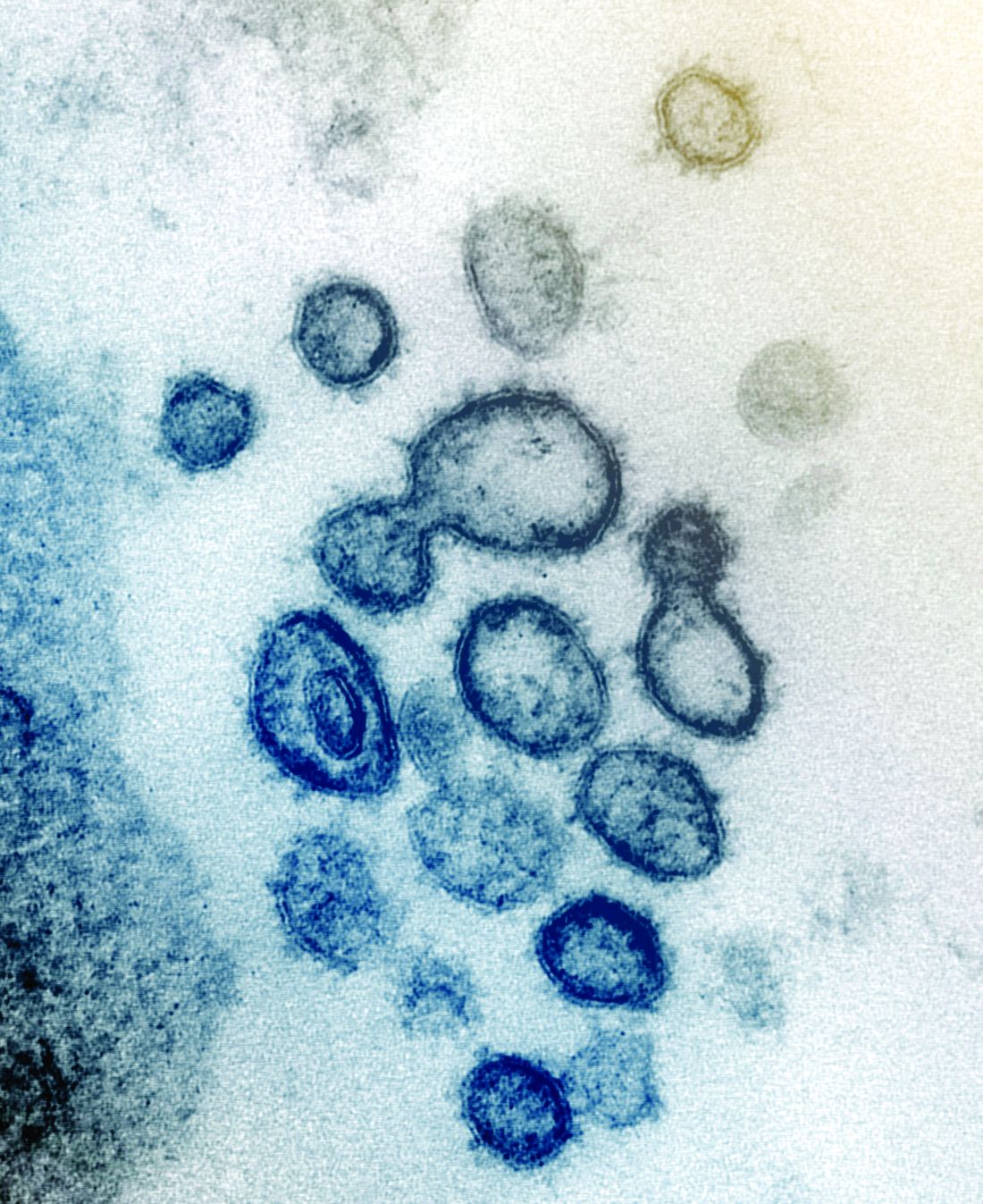
Database will collect data on COVID-19 in patients with MS
The COViMS (COVID-19 Infections in Multiple Sclerosis and Related Diseases) database is gathering information from patients throughout the United States and will soon gain access to Canadian data. Data from patients with CNS demyelinating diseases such as neuromyelitis optica and myelin oligodendrocyte glycoprotein antibody diseases also will be included in COViMS. Amber Salter, PhD, MPH, the director of the North American Research Committee on MS (NARCOMS) is supervising the data collection and analyses.
“COViMS will provide valuable insight on how COVID-19 affects people with MS, including if certain disease-modifying treatments incur special risks,” said June Halper, CEO of CMSC, in a press release.
The project began when CMSC and NMSS established independent registries of epidemiologic data related to MS and COVID-19. The two groups soon began communicating and included other researchers, who also were considering establishing registries, in their discussions. In addition, representatives of the Cleveland Clinic verbally agreed to share data that they have been collecting with the COViMS registry. “The fast-moving, almost parallel, efforts led to this collaboration,” said Gary Cutter, PhD, professor of biostatistics at the University of Alabama at Birmingham. “This in itself is noteworthy because all of this took place within an incredibly short time from inception to the initiation of data collection.”
The effects of SARS-CoV-2 infection on the health of patients with MS is little understood. In North America, no reporting system had been organized to gather information on these patients and track outcomes. Such a system could influence the treatment of people with MS who become infected with the novel coronavirus or other similar future viruses. The COViMS registry is intended to define the impact of COVID-19 on patients with MS and ascertain how factors such as age, comorbidities, and MS treatments affect outcomes of COVID-19. “The estimated median age of MS patients in the U.S. is about 52 years, thus putting many at increased risk just due to age,” said Dr. Cutter.
“People with MS and their health care providers need evidence-based guidance to provide optimal MS care during the COVID-19 pandemic, and the COViMS database will help answer the many pressing questions,” said Bruce Bebo, executive vice president of research for the NMSS, in a press release.
The two organizations encourage neurologists and other health care providers who treat patients with MS and documented COVID-19 infection to complete a Case Report Form on the COViMS website, which includes answers to frequently asked questions, a sample CRF, and other resources. The website will provide real-time data once registry participation is underway.
The COViMS (COVID-19 Infections in Multiple Sclerosis and Related Diseases) database is gathering information from patients throughout the United States and will soon gain access to Canadian data. Data from patients with CNS demyelinating diseases such as neuromyelitis optica and myelin oligodendrocyte glycoprotein antibody diseases also will be included in COViMS. Amber Salter, PhD, MPH, the director of the North American Research Committee on MS (NARCOMS) is supervising the data collection and analyses.
“COViMS will provide valuable insight on how COVID-19 affects people with MS, including if certain disease-modifying treatments incur special risks,” said June Halper, CEO of CMSC, in a press release.
The project began when CMSC and NMSS established independent registries of epidemiologic data related to MS and COVID-19. The two groups soon began communicating and included other researchers, who also were considering establishing registries, in their discussions. In addition, representatives of the Cleveland Clinic verbally agreed to share data that they have been collecting with the COViMS registry. “The fast-moving, almost parallel, efforts led to this collaboration,” said Gary Cutter, PhD, professor of biostatistics at the University of Alabama at Birmingham. “This in itself is noteworthy because all of this took place within an incredibly short time from inception to the initiation of data collection.”
The effects of SARS-CoV-2 infection on the health of patients with MS is little understood. In North America, no reporting system had been organized to gather information on these patients and track outcomes. Such a system could influence the treatment of people with MS who become infected with the novel coronavirus or other similar future viruses. The COViMS registry is intended to define the impact of COVID-19 on patients with MS and ascertain how factors such as age, comorbidities, and MS treatments affect outcomes of COVID-19. “The estimated median age of MS patients in the U.S. is about 52 years, thus putting many at increased risk just due to age,” said Dr. Cutter.
“People with MS and their health care providers need evidence-based guidance to provide optimal MS care during the COVID-19 pandemic, and the COViMS database will help answer the many pressing questions,” said Bruce Bebo, executive vice president of research for the NMSS, in a press release.
The two organizations encourage neurologists and other health care providers who treat patients with MS and documented COVID-19 infection to complete a Case Report Form on the COViMS website, which includes answers to frequently asked questions, a sample CRF, and other resources. The website will provide real-time data once registry participation is underway.
The COViMS (COVID-19 Infections in Multiple Sclerosis and Related Diseases) database is gathering information from patients throughout the United States and will soon gain access to Canadian data. Data from patients with CNS demyelinating diseases such as neuromyelitis optica and myelin oligodendrocyte glycoprotein antibody diseases also will be included in COViMS. Amber Salter, PhD, MPH, the director of the North American Research Committee on MS (NARCOMS) is supervising the data collection and analyses.
“COViMS will provide valuable insight on how COVID-19 affects people with MS, including if certain disease-modifying treatments incur special risks,” said June Halper, CEO of CMSC, in a press release.
The project began when CMSC and NMSS established independent registries of epidemiologic data related to MS and COVID-19. The two groups soon began communicating and included other researchers, who also were considering establishing registries, in their discussions. In addition, representatives of the Cleveland Clinic verbally agreed to share data that they have been collecting with the COViMS registry. “The fast-moving, almost parallel, efforts led to this collaboration,” said Gary Cutter, PhD, professor of biostatistics at the University of Alabama at Birmingham. “This in itself is noteworthy because all of this took place within an incredibly short time from inception to the initiation of data collection.”
The effects of SARS-CoV-2 infection on the health of patients with MS is little understood. In North America, no reporting system had been organized to gather information on these patients and track outcomes. Such a system could influence the treatment of people with MS who become infected with the novel coronavirus or other similar future viruses. The COViMS registry is intended to define the impact of COVID-19 on patients with MS and ascertain how factors such as age, comorbidities, and MS treatments affect outcomes of COVID-19. “The estimated median age of MS patients in the U.S. is about 52 years, thus putting many at increased risk just due to age,” said Dr. Cutter.
“People with MS and their health care providers need evidence-based guidance to provide optimal MS care during the COVID-19 pandemic, and the COViMS database will help answer the many pressing questions,” said Bruce Bebo, executive vice president of research for the NMSS, in a press release.
The two organizations encourage neurologists and other health care providers who treat patients with MS and documented COVID-19 infection to complete a Case Report Form on the COViMS website, which includes answers to frequently asked questions, a sample CRF, and other resources. The website will provide real-time data once registry participation is underway.
CAR T-cell therapy effective for r/r B-cell lymphoma of the GI tract
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
FROM CYTOTHERAPY
Lymphocyte, monocyte data can predict treatment response in follicular lymphoma
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Pandemic necessitates new strategies to treat migraine
Patients with migraine who are unable to continue preventive procedures such as onabotulinumtoxinA injections during the COVID-19 pandemic may be at risk of worsening migraine, according to an article published March 30 in Headache. To address this scenario, including monoclonal antibodies against calcitonin gene-related peptide (CGRP) or the CGRP receptor, the authors said.
“This is a particularly vulnerable time for individuals with migraine and other disabling headache disorders, with many physical and mental stressors, increased anxiety, and changes in daily routine which may serve as triggering factors for worsening headache,” said lead author Christina L. Szperka, MD, director of the pediatric headache program at Children’s Hospital of Philadelphia, and colleagues.
Acute treatment
The authors described potential treatment regimens based on their experience as headache specialists and the experiences of their colleagues. For acute therapy options, NSAIDs, triptans, and neuroleptics may be used in combination when needed. Medications within the same drug category should not be combined, however, and triptans, dihydroergotamine, and lasmiditan should not be coadministered within 24 hours. Since the 2015 American Headache Society guideline for the acute treatment of migraine, the Food and Drug Administration has approved additional acute migraine medications, including ubrogepant, rimegepant, and lasmiditan, the authors said. The agency also cleared several neuromodulation devices for the acute treatment of migraine.
Although few drugs have been studied as treatments for unusually prolonged severe headaches, headache doctors often recommend NSAIDs before patients seek care at an emergency department or infusion center, the authors said. NSAID options include indomethacin, ketorolac, naproxen, nabumetone, diclofenac, and mefenamic acid. Neuroleptics also may be used. “Long-acting triptan medications can be used as bridge therapies, as is often done in the treatment of menstrually related migraine or in the treatment of medication overuse headache,” they said. “We propose a similar strategy can be trialed as a therapeutic option for refractory or persistent migraine.”
The authors also described the use of antiepileptics and corticosteroids, as well as drugs that may treat specific symptoms, such as difficulty sleeping (hydroxyzine or amitriptyline), neck or muscle pain (tizanidine), and aura with migraine (magnesium). Clinicians should avoid the use of opioids and butalbital, they said.
Preventive treatment
“While the injection of onabotulinumtoxinA is an effective treatment for chronic migraine, the procedure can put the patient and the provider at higher risk of COVID-19 given the close contact encounter,” wrote Dr. Szperka and colleagues. “We believe that other migraine preventive treatments should be utilized first when possible.” Since the publication of a guideline on preventive migraine therapies in 2012, the FDA has approved additional preventive therapies, including the anti-CGRP monoclonal antibodies erenumab‐aooe, galcanezumab‐gnlm, fremanezumab‐vfrm, and eptinezumab‐jjmr. “The first three are intended for self‐injection at home, with detailed instructions available for each product on its website,” they said.
Among angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), candesartan has evidence of efficacy and tolerability in migraine prevention. Lisinopril has been considered possibly effective. “There has been recent concern in the media about the possibility of these medications interfering with the body’s response to COVID‐19,” the authors said, although this theoretical concern was not based on experimental or clinical data. “For patients in need of a new preventive therapy, the potential for benefit with an ACE/ARB must be weighed against the theoretical increased risk of infection.”
In addition, studies indicate that melatonin may prevent migraine with few side effects and that zonisamide may be effective in patients who have an inadequate response to or experience side effects with topiramate.
Policy changes and telehealth options
Effectively treating patients with migraine during the pandemic requires policy changes, according to the authors. “Migraine preventive prior authorization restrictions need to be lifted for evidence‐based, FDA‐approved therapies; patients need to be able to access these medications quickly and easily. Patients should not be required to fail older medications,” they said. “Similarly, in order to permit the transition of patients from onabotulinumtoxinA to anti‐CGRP [monoclonal antibodies], insurers should remove the prohibition against simultaneous coverage of these drug classes.” Insurers also should loosen restrictions on the off-label use of acute and preventive medication for adolescents, Dr. Szperka and coauthors suggest.
“In the era of COVID‐19, telehealth has become an essential modality for most headache specialists, given the need for providers to take significant precautions for both their patients and themselves, limiting touch or close contact,” they said. Patients with headache may warrant additional screening for COVID-19 as well. “As headache has been reported as an early symptom of COVID‐19, patients with worsening or new onset severe headache should be reviewed for exposure risk and any other symptoms which may be consistent with COVID‐19 infection,” the authors said.
There was no direct funding for the report. Dr. Szperka and a coauthor receive salary support from the National Institutes of Health. Dr. Szperka also has received grant support from Pfizer, and her institution has received compensation for her consulting work for Allergan. Several coauthors disclosed consulting and serving on speakers’ bureaus for and receiving research support from various pharmaceutical companies.
SOURCE: Szperka CL et al. Headache. 2020 Mar 30. doi: 10.1111/head.13810.
Patients with migraine who are unable to continue preventive procedures such as onabotulinumtoxinA injections during the COVID-19 pandemic may be at risk of worsening migraine, according to an article published March 30 in Headache. To address this scenario, including monoclonal antibodies against calcitonin gene-related peptide (CGRP) or the CGRP receptor, the authors said.
“This is a particularly vulnerable time for individuals with migraine and other disabling headache disorders, with many physical and mental stressors, increased anxiety, and changes in daily routine which may serve as triggering factors for worsening headache,” said lead author Christina L. Szperka, MD, director of the pediatric headache program at Children’s Hospital of Philadelphia, and colleagues.
Acute treatment
The authors described potential treatment regimens based on their experience as headache specialists and the experiences of their colleagues. For acute therapy options, NSAIDs, triptans, and neuroleptics may be used in combination when needed. Medications within the same drug category should not be combined, however, and triptans, dihydroergotamine, and lasmiditan should not be coadministered within 24 hours. Since the 2015 American Headache Society guideline for the acute treatment of migraine, the Food and Drug Administration has approved additional acute migraine medications, including ubrogepant, rimegepant, and lasmiditan, the authors said. The agency also cleared several neuromodulation devices for the acute treatment of migraine.
Although few drugs have been studied as treatments for unusually prolonged severe headaches, headache doctors often recommend NSAIDs before patients seek care at an emergency department or infusion center, the authors said. NSAID options include indomethacin, ketorolac, naproxen, nabumetone, diclofenac, and mefenamic acid. Neuroleptics also may be used. “Long-acting triptan medications can be used as bridge therapies, as is often done in the treatment of menstrually related migraine or in the treatment of medication overuse headache,” they said. “We propose a similar strategy can be trialed as a therapeutic option for refractory or persistent migraine.”
The authors also described the use of antiepileptics and corticosteroids, as well as drugs that may treat specific symptoms, such as difficulty sleeping (hydroxyzine or amitriptyline), neck or muscle pain (tizanidine), and aura with migraine (magnesium). Clinicians should avoid the use of opioids and butalbital, they said.
Preventive treatment
“While the injection of onabotulinumtoxinA is an effective treatment for chronic migraine, the procedure can put the patient and the provider at higher risk of COVID-19 given the close contact encounter,” wrote Dr. Szperka and colleagues. “We believe that other migraine preventive treatments should be utilized first when possible.” Since the publication of a guideline on preventive migraine therapies in 2012, the FDA has approved additional preventive therapies, including the anti-CGRP monoclonal antibodies erenumab‐aooe, galcanezumab‐gnlm, fremanezumab‐vfrm, and eptinezumab‐jjmr. “The first three are intended for self‐injection at home, with detailed instructions available for each product on its website,” they said.
Among angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), candesartan has evidence of efficacy and tolerability in migraine prevention. Lisinopril has been considered possibly effective. “There has been recent concern in the media about the possibility of these medications interfering with the body’s response to COVID‐19,” the authors said, although this theoretical concern was not based on experimental or clinical data. “For patients in need of a new preventive therapy, the potential for benefit with an ACE/ARB must be weighed against the theoretical increased risk of infection.”
In addition, studies indicate that melatonin may prevent migraine with few side effects and that zonisamide may be effective in patients who have an inadequate response to or experience side effects with topiramate.
Policy changes and telehealth options
Effectively treating patients with migraine during the pandemic requires policy changes, according to the authors. “Migraine preventive prior authorization restrictions need to be lifted for evidence‐based, FDA‐approved therapies; patients need to be able to access these medications quickly and easily. Patients should not be required to fail older medications,” they said. “Similarly, in order to permit the transition of patients from onabotulinumtoxinA to anti‐CGRP [monoclonal antibodies], insurers should remove the prohibition against simultaneous coverage of these drug classes.” Insurers also should loosen restrictions on the off-label use of acute and preventive medication for adolescents, Dr. Szperka and coauthors suggest.
“In the era of COVID‐19, telehealth has become an essential modality for most headache specialists, given the need for providers to take significant precautions for both their patients and themselves, limiting touch or close contact,” they said. Patients with headache may warrant additional screening for COVID-19 as well. “As headache has been reported as an early symptom of COVID‐19, patients with worsening or new onset severe headache should be reviewed for exposure risk and any other symptoms which may be consistent with COVID‐19 infection,” the authors said.
There was no direct funding for the report. Dr. Szperka and a coauthor receive salary support from the National Institutes of Health. Dr. Szperka also has received grant support from Pfizer, and her institution has received compensation for her consulting work for Allergan. Several coauthors disclosed consulting and serving on speakers’ bureaus for and receiving research support from various pharmaceutical companies.
SOURCE: Szperka CL et al. Headache. 2020 Mar 30. doi: 10.1111/head.13810.
Patients with migraine who are unable to continue preventive procedures such as onabotulinumtoxinA injections during the COVID-19 pandemic may be at risk of worsening migraine, according to an article published March 30 in Headache. To address this scenario, including monoclonal antibodies against calcitonin gene-related peptide (CGRP) or the CGRP receptor, the authors said.
“This is a particularly vulnerable time for individuals with migraine and other disabling headache disorders, with many physical and mental stressors, increased anxiety, and changes in daily routine which may serve as triggering factors for worsening headache,” said lead author Christina L. Szperka, MD, director of the pediatric headache program at Children’s Hospital of Philadelphia, and colleagues.
Acute treatment
The authors described potential treatment regimens based on their experience as headache specialists and the experiences of their colleagues. For acute therapy options, NSAIDs, triptans, and neuroleptics may be used in combination when needed. Medications within the same drug category should not be combined, however, and triptans, dihydroergotamine, and lasmiditan should not be coadministered within 24 hours. Since the 2015 American Headache Society guideline for the acute treatment of migraine, the Food and Drug Administration has approved additional acute migraine medications, including ubrogepant, rimegepant, and lasmiditan, the authors said. The agency also cleared several neuromodulation devices for the acute treatment of migraine.
Although few drugs have been studied as treatments for unusually prolonged severe headaches, headache doctors often recommend NSAIDs before patients seek care at an emergency department or infusion center, the authors said. NSAID options include indomethacin, ketorolac, naproxen, nabumetone, diclofenac, and mefenamic acid. Neuroleptics also may be used. “Long-acting triptan medications can be used as bridge therapies, as is often done in the treatment of menstrually related migraine or in the treatment of medication overuse headache,” they said. “We propose a similar strategy can be trialed as a therapeutic option for refractory or persistent migraine.”
The authors also described the use of antiepileptics and corticosteroids, as well as drugs that may treat specific symptoms, such as difficulty sleeping (hydroxyzine or amitriptyline), neck or muscle pain (tizanidine), and aura with migraine (magnesium). Clinicians should avoid the use of opioids and butalbital, they said.
Preventive treatment
“While the injection of onabotulinumtoxinA is an effective treatment for chronic migraine, the procedure can put the patient and the provider at higher risk of COVID-19 given the close contact encounter,” wrote Dr. Szperka and colleagues. “We believe that other migraine preventive treatments should be utilized first when possible.” Since the publication of a guideline on preventive migraine therapies in 2012, the FDA has approved additional preventive therapies, including the anti-CGRP monoclonal antibodies erenumab‐aooe, galcanezumab‐gnlm, fremanezumab‐vfrm, and eptinezumab‐jjmr. “The first three are intended for self‐injection at home, with detailed instructions available for each product on its website,” they said.
Among angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), candesartan has evidence of efficacy and tolerability in migraine prevention. Lisinopril has been considered possibly effective. “There has been recent concern in the media about the possibility of these medications interfering with the body’s response to COVID‐19,” the authors said, although this theoretical concern was not based on experimental or clinical data. “For patients in need of a new preventive therapy, the potential for benefit with an ACE/ARB must be weighed against the theoretical increased risk of infection.”
In addition, studies indicate that melatonin may prevent migraine with few side effects and that zonisamide may be effective in patients who have an inadequate response to or experience side effects with topiramate.
Policy changes and telehealth options
Effectively treating patients with migraine during the pandemic requires policy changes, according to the authors. “Migraine preventive prior authorization restrictions need to be lifted for evidence‐based, FDA‐approved therapies; patients need to be able to access these medications quickly and easily. Patients should not be required to fail older medications,” they said. “Similarly, in order to permit the transition of patients from onabotulinumtoxinA to anti‐CGRP [monoclonal antibodies], insurers should remove the prohibition against simultaneous coverage of these drug classes.” Insurers also should loosen restrictions on the off-label use of acute and preventive medication for adolescents, Dr. Szperka and coauthors suggest.
“In the era of COVID‐19, telehealth has become an essential modality for most headache specialists, given the need for providers to take significant precautions for both their patients and themselves, limiting touch or close contact,” they said. Patients with headache may warrant additional screening for COVID-19 as well. “As headache has been reported as an early symptom of COVID‐19, patients with worsening or new onset severe headache should be reviewed for exposure risk and any other symptoms which may be consistent with COVID‐19 infection,” the authors said.
There was no direct funding for the report. Dr. Szperka and a coauthor receive salary support from the National Institutes of Health. Dr. Szperka also has received grant support from Pfizer, and her institution has received compensation for her consulting work for Allergan. Several coauthors disclosed consulting and serving on speakers’ bureaus for and receiving research support from various pharmaceutical companies.
SOURCE: Szperka CL et al. Headache. 2020 Mar 30. doi: 10.1111/head.13810.
FROM HEADACHE
Amid coronavirus concerns, researchers urge mental health interventions for patients with dementia
according to a letter published online ahead of print March 30 in Lancet. Consistent with recommendations from Alzheimer’s Disease International and other dementia experts, teams that include mental health professionals, social workers, nursing home administrators, and volunteers should collaborate to provide mental health care for people with dementia. Experts in dementia should lead each team and support team members from other disciplines, wrote Huali Wang, MD, chair of clinical research at Peking University Institute of Mental Health in Beijing, and colleagues.
Interventions could be administered through telehealth, said the authors. Teams led by mental health professionals could use electronic media to provide self-help guidance for reducing stress, such as relaxation or meditation exercise. These teams also could use telephone hotlines to support behavioral management, and psychological counselors could provide online consultations for caregivers in nursing homes or in the community. “We encourage people who have a parent with dementia to have more frequent contact or spend more time with their parent, or to take on some of the caregiving duties so as to give the carer some respite time,” wrote Dr. Wang and colleagues.
Many local authorities are banning visits to nursing home residents to reduce the latter’s risk of COVID-19 infection. As a consequence, these elderly people are becoming more isolated, and anxiety is increasing among nursing home staffs.
In China, five organizations, including the Chinese Society of Geriatric Psychiatry and Alzheimer’s Disease Chinese, responded to the COVID-19 outbreak by publishing recommendations for providing mental health and psychosocial support. Groups of providers from various disciplines offered free counseling services for people with dementia and their caregivers. “These approaches minimized the complex impact of both COVID-19 outbreak and dementia,” wrote the authors.
“China has contained the epidemic, and business is starting to return to normal,” they continued. “We believe that learning lessons from China would empower the world to tackle the COVID-19 pandemic, with little risk of compromising the quality of life of people living with dementia and their carers.”
Dr. Wang has received lecture fees from Eisai China and Lundbeck China. She owns the copyright for the neuropsychiatric symptoms individualized management system. Her coauthors reported serving as advisory board members and receiving fees from companies such as Biogen, Novartis, and Genentech.
SOURCE: Wang H et al. Lancet. 2020 Mar 30. doi: 10.1016/S0140-6736(20)30755-8.
according to a letter published online ahead of print March 30 in Lancet. Consistent with recommendations from Alzheimer’s Disease International and other dementia experts, teams that include mental health professionals, social workers, nursing home administrators, and volunteers should collaborate to provide mental health care for people with dementia. Experts in dementia should lead each team and support team members from other disciplines, wrote Huali Wang, MD, chair of clinical research at Peking University Institute of Mental Health in Beijing, and colleagues.
Interventions could be administered through telehealth, said the authors. Teams led by mental health professionals could use electronic media to provide self-help guidance for reducing stress, such as relaxation or meditation exercise. These teams also could use telephone hotlines to support behavioral management, and psychological counselors could provide online consultations for caregivers in nursing homes or in the community. “We encourage people who have a parent with dementia to have more frequent contact or spend more time with their parent, or to take on some of the caregiving duties so as to give the carer some respite time,” wrote Dr. Wang and colleagues.
Many local authorities are banning visits to nursing home residents to reduce the latter’s risk of COVID-19 infection. As a consequence, these elderly people are becoming more isolated, and anxiety is increasing among nursing home staffs.
In China, five organizations, including the Chinese Society of Geriatric Psychiatry and Alzheimer’s Disease Chinese, responded to the COVID-19 outbreak by publishing recommendations for providing mental health and psychosocial support. Groups of providers from various disciplines offered free counseling services for people with dementia and their caregivers. “These approaches minimized the complex impact of both COVID-19 outbreak and dementia,” wrote the authors.
“China has contained the epidemic, and business is starting to return to normal,” they continued. “We believe that learning lessons from China would empower the world to tackle the COVID-19 pandemic, with little risk of compromising the quality of life of people living with dementia and their carers.”
Dr. Wang has received lecture fees from Eisai China and Lundbeck China. She owns the copyright for the neuropsychiatric symptoms individualized management system. Her coauthors reported serving as advisory board members and receiving fees from companies such as Biogen, Novartis, and Genentech.
SOURCE: Wang H et al. Lancet. 2020 Mar 30. doi: 10.1016/S0140-6736(20)30755-8.
according to a letter published online ahead of print March 30 in Lancet. Consistent with recommendations from Alzheimer’s Disease International and other dementia experts, teams that include mental health professionals, social workers, nursing home administrators, and volunteers should collaborate to provide mental health care for people with dementia. Experts in dementia should lead each team and support team members from other disciplines, wrote Huali Wang, MD, chair of clinical research at Peking University Institute of Mental Health in Beijing, and colleagues.
Interventions could be administered through telehealth, said the authors. Teams led by mental health professionals could use electronic media to provide self-help guidance for reducing stress, such as relaxation or meditation exercise. These teams also could use telephone hotlines to support behavioral management, and psychological counselors could provide online consultations for caregivers in nursing homes or in the community. “We encourage people who have a parent with dementia to have more frequent contact or spend more time with their parent, or to take on some of the caregiving duties so as to give the carer some respite time,” wrote Dr. Wang and colleagues.
Many local authorities are banning visits to nursing home residents to reduce the latter’s risk of COVID-19 infection. As a consequence, these elderly people are becoming more isolated, and anxiety is increasing among nursing home staffs.
In China, five organizations, including the Chinese Society of Geriatric Psychiatry and Alzheimer’s Disease Chinese, responded to the COVID-19 outbreak by publishing recommendations for providing mental health and psychosocial support. Groups of providers from various disciplines offered free counseling services for people with dementia and their caregivers. “These approaches minimized the complex impact of both COVID-19 outbreak and dementia,” wrote the authors.
“China has contained the epidemic, and business is starting to return to normal,” they continued. “We believe that learning lessons from China would empower the world to tackle the COVID-19 pandemic, with little risk of compromising the quality of life of people living with dementia and their carers.”
Dr. Wang has received lecture fees from Eisai China and Lundbeck China. She owns the copyright for the neuropsychiatric symptoms individualized management system. Her coauthors reported serving as advisory board members and receiving fees from companies such as Biogen, Novartis, and Genentech.
SOURCE: Wang H et al. Lancet. 2020 Mar 30. doi: 10.1016/S0140-6736(20)30755-8.
REPORTING FROM THE LANCET
One-third of high-risk CLL patients received treatment counter to recommendations
Approximately , according to a study based upon data from the informCLL registry. In addition, low levels of prognostic marker testing in these patients was a concern.
Researchers assessed data from 840 enrolled CLL patients, of whom 459 (55%) were previously untreated, and 381 (45%) had relapsed/refractory disease. In terms of therapy, chemoimmunotherapy was more common in previously untreated patients, compared with relapsed/refractory patients (42% vs. 23%), whereas ibrutinib was more frequently used in relapsed/refractory vs. previously untreated patients (51% vs. 39%), according to the researchers.
Fluorescent in situ hybridization (FISH) testing, TP53 mutation, and immunoglobulin heavy chain somatic hypermutation biomarker testing were performed infrequently across all patients at registry enrollment, according to the authors.
Among patients who were tested, the rate of mutated TP53 was the same for previously untreated (14/54; 26%) and relapsed/refractory patients (9/35; 26%). In those patients who were tested, 34% with del(17p), a chromosomal deletion, and 26% of mutated TP53 patients received chemoimmunotherapy combinations. The authors stated that this was concerning in that it contradicts consensus guidelines based on data from several clinical studies. Chemoimmunotherapy is not recommended for these high-risk patients because of poor disease and survival outcomes with this treatment strategy, according to the authors.
“Current clinical practice is not keeping pace with recommendations and guidelines for prognostic
marker testing and subsequent selection of appropriate therapy,” the authors stated.
“Even with the approval of novel agents and updated guidelines, low rates of prognostic biomarker testing may lead to suboptimal therapy choices for patients with unknown risk status. In addition, we note that the presence of high-risk features (del(17p) and TP53) is unfortunately not translating to choosing the optimal therapy for these patients,” the researchers concluded.
The study was sponsored by an AbbVie Company and Janssen. The authors reported consulting and grants from these and other pharmaceutical companies.
SOURCE: Mato AR et al. Clin Lymphoma Myeloma Leuk. 2020;20(3):174-83.
Approximately , according to a study based upon data from the informCLL registry. In addition, low levels of prognostic marker testing in these patients was a concern.
Researchers assessed data from 840 enrolled CLL patients, of whom 459 (55%) were previously untreated, and 381 (45%) had relapsed/refractory disease. In terms of therapy, chemoimmunotherapy was more common in previously untreated patients, compared with relapsed/refractory patients (42% vs. 23%), whereas ibrutinib was more frequently used in relapsed/refractory vs. previously untreated patients (51% vs. 39%), according to the researchers.
Fluorescent in situ hybridization (FISH) testing, TP53 mutation, and immunoglobulin heavy chain somatic hypermutation biomarker testing were performed infrequently across all patients at registry enrollment, according to the authors.
Among patients who were tested, the rate of mutated TP53 was the same for previously untreated (14/54; 26%) and relapsed/refractory patients (9/35; 26%). In those patients who were tested, 34% with del(17p), a chromosomal deletion, and 26% of mutated TP53 patients received chemoimmunotherapy combinations. The authors stated that this was concerning in that it contradicts consensus guidelines based on data from several clinical studies. Chemoimmunotherapy is not recommended for these high-risk patients because of poor disease and survival outcomes with this treatment strategy, according to the authors.
“Current clinical practice is not keeping pace with recommendations and guidelines for prognostic
marker testing and subsequent selection of appropriate therapy,” the authors stated.
“Even with the approval of novel agents and updated guidelines, low rates of prognostic biomarker testing may lead to suboptimal therapy choices for patients with unknown risk status. In addition, we note that the presence of high-risk features (del(17p) and TP53) is unfortunately not translating to choosing the optimal therapy for these patients,” the researchers concluded.
The study was sponsored by an AbbVie Company and Janssen. The authors reported consulting and grants from these and other pharmaceutical companies.
SOURCE: Mato AR et al. Clin Lymphoma Myeloma Leuk. 2020;20(3):174-83.
Approximately , according to a study based upon data from the informCLL registry. In addition, low levels of prognostic marker testing in these patients was a concern.
Researchers assessed data from 840 enrolled CLL patients, of whom 459 (55%) were previously untreated, and 381 (45%) had relapsed/refractory disease. In terms of therapy, chemoimmunotherapy was more common in previously untreated patients, compared with relapsed/refractory patients (42% vs. 23%), whereas ibrutinib was more frequently used in relapsed/refractory vs. previously untreated patients (51% vs. 39%), according to the researchers.
Fluorescent in situ hybridization (FISH) testing, TP53 mutation, and immunoglobulin heavy chain somatic hypermutation biomarker testing were performed infrequently across all patients at registry enrollment, according to the authors.
Among patients who were tested, the rate of mutated TP53 was the same for previously untreated (14/54; 26%) and relapsed/refractory patients (9/35; 26%). In those patients who were tested, 34% with del(17p), a chromosomal deletion, and 26% of mutated TP53 patients received chemoimmunotherapy combinations. The authors stated that this was concerning in that it contradicts consensus guidelines based on data from several clinical studies. Chemoimmunotherapy is not recommended for these high-risk patients because of poor disease and survival outcomes with this treatment strategy, according to the authors.
“Current clinical practice is not keeping pace with recommendations and guidelines for prognostic
marker testing and subsequent selection of appropriate therapy,” the authors stated.
“Even with the approval of novel agents and updated guidelines, low rates of prognostic biomarker testing may lead to suboptimal therapy choices for patients with unknown risk status. In addition, we note that the presence of high-risk features (del(17p) and TP53) is unfortunately not translating to choosing the optimal therapy for these patients,” the researchers concluded.
The study was sponsored by an AbbVie Company and Janssen. The authors reported consulting and grants from these and other pharmaceutical companies.
SOURCE: Mato AR et al. Clin Lymphoma Myeloma Leuk. 2020;20(3):174-83.
CBT by phone reduces depression in Parkinson’s disease
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
FROM NEUROLOGY
Case study shows CLL may mask COVID-19 infection
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
FROM THE LANCET HAEMATOLOGY
FDA removes pregnancy category C warning from certain MS medications
The FDA based the decision on data from more than 1,000 real-world pregnancies, including pregnancies from a large epidemiologic study and published studies over several decades, which found no connection between use of interferon-beta products during early pregnancy and an increased risk of major birth defects, according to the FDA.
As a result, the labels for both medications will no longer have the pregnancy category C designation; however, patients should continue to notify their health care provider if they are pregnant or plan to become pregnant.
The FDA decision to remove the warning follows a similar decision by the European Medicines Agency last year.
“Many women with MS are diagnosed during their childbearing years. With this important update for Plegridy and Avonex, healthcare providers have more data to inform appropriate treatment paths for patients who may be pregnant or planning for pregnancy,” said Bernd Kieseier, MD, MHBA, executive director and head of global MS at Worldwide Medical, Biogen, in a press release.
The FDA based the decision on data from more than 1,000 real-world pregnancies, including pregnancies from a large epidemiologic study and published studies over several decades, which found no connection between use of interferon-beta products during early pregnancy and an increased risk of major birth defects, according to the FDA.
As a result, the labels for both medications will no longer have the pregnancy category C designation; however, patients should continue to notify their health care provider if they are pregnant or plan to become pregnant.
The FDA decision to remove the warning follows a similar decision by the European Medicines Agency last year.
“Many women with MS are diagnosed during their childbearing years. With this important update for Plegridy and Avonex, healthcare providers have more data to inform appropriate treatment paths for patients who may be pregnant or planning for pregnancy,” said Bernd Kieseier, MD, MHBA, executive director and head of global MS at Worldwide Medical, Biogen, in a press release.
The FDA based the decision on data from more than 1,000 real-world pregnancies, including pregnancies from a large epidemiologic study and published studies over several decades, which found no connection between use of interferon-beta products during early pregnancy and an increased risk of major birth defects, according to the FDA.
As a result, the labels for both medications will no longer have the pregnancy category C designation; however, patients should continue to notify their health care provider if they are pregnant or plan to become pregnant.
The FDA decision to remove the warning follows a similar decision by the European Medicines Agency last year.
“Many women with MS are diagnosed during their childbearing years. With this important update for Plegridy and Avonex, healthcare providers have more data to inform appropriate treatment paths for patients who may be pregnant or planning for pregnancy,” said Bernd Kieseier, MD, MHBA, executive director and head of global MS at Worldwide Medical, Biogen, in a press release.