User login
CBT for depression: What the evidence says
Major depressive disorder (MDD) has a devastating impact on individuals and society because of its high prevalence, its recurrent nature, its frequent comorbidity with other disorders, and the functional impairment it causes. Compared with other chronic diseases, such as arthritis, asthma, and diabetes, MDD produces the greatest decrement in health worldwide.1 The goals in treating MDD should be not just to reduce symptom severity but also to achieve continuing remission and lower the risk for relapse.2
Antidepressants are the most common treatment for depression.3 Among psychotherapies used to treat MDD, cognitive-behavioral therapy (CBT) has been identified as an effective treatment.4 Collaborative care models have been reported to manage MDD more effectively.5 In this article, we review the evidence supporting the use of CBT as monotherapy and in combination with antidepressants for acute and long-term treatment of MDD.
Acute treatment: Not too soon for CBT
Mild to moderate depression
Research has indicated that for the treatment of mild MDD, antidepressants are unlikely to be more effective than placebo.6,7 Studies also have reported that response to antidepressants begins to outpace response to placebo only when symptoms are no longer mild. Using antidepressants for patients with mild depression could therefore place them at risk of overtreatment.8 In keeping with these findings, the American Psychiatric Association (APA) has recommended the use of evidence-based psychotherapies, such as CBT, as an initial treatment choice for patients with mild to moderate MDD.9
Two recent studies have suggested that the combination of CBT plus antidepressants could boost improvement in psychosocial functioning for patients with mild MDD.10,11 However, neither study included a group of patients who received only CBT to evaluate if CBT alone could have also produced similar effects. Other limitations include the lack of a control group in one study and small sample sizes in both studies. However, both studies had a long follow-up period and specifically studied the impact on psychosocial functioning.
Moderate to severe depression
Earlier depression treatment guidelines suggested that antidepressants should be used to treat more severe depression, while psychotherapy should be used mainly for mild depression.12 This recommendation was influenced by the well-known National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program, a multicenter randomized controlled trial (RCT) that used a placebo control.13 In this study, CBT was compared with antidepressants and found to be no more effective than placebo for more severely depressed patients.13 However, this finding was not consistent across the 3 sites where the study was conducted; at the site where CBT was provided by more experienced CBT therapists, patients with more severe depression who received CBT fared as well as patients treated with antidepressants.14 A later double-blind RCT that used experienced therapists found that CBT was as effective as antidepressants (monoamine oxidase inhibitors), and both treatments were superior to placebo in reducing symptoms of atypical depression.15
Another placebo-controlled RCT conducted at 2 sites found that CBT was as effective as antidepressants in the treatment of moderately to severely depressed patients. As in the NIMH Treatment of Depression Collaborative Research Program trial,13 in this study, there were indications that the results were dependent on therapist experience.16 These findings suggest that the experience of the therapist is an important factor.
A recent meta-analysis of treatments of the acute phase of MDD compared 11 RCTs of CBT and second-generation antidepressants (selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and other medications with related mechanisms of action).17 It found that as a first-step treatment, CBT and antidepressants had a similar impact on symptom relief in patients with moderate to severe depression. Patients treated with antidepressants also had a higher risk of experiencing adverse events or discontinuing treatment because of adverse events. However, this meta-analysis included trials that had methodological shortcomings, which reduces the strength of these conclusions.
Continue to: Patients with MDD and comorbid personality disorders have been...
Patients with MDD and comorbid personality disorders have been reported to have poorer outcomes, regardless of the treatment used.18 Fournier et al19 examined the impact of antidepressants and CBT in moderately to severely depressed patients with and without a personality disorder. They found that a combination of antidepressants and CBT was suitable for patients with personality disorders because antidepressants would boost the initial response and CBT would help sustain improvement in the long term.
Presently, the APA suggests that the combination of psychotherapy and antidepressants may be used as an initial treatment for patients with moderate to severe MDD.9 As research brings to light other factors that affect treatment outcomes, these guidelines could change.
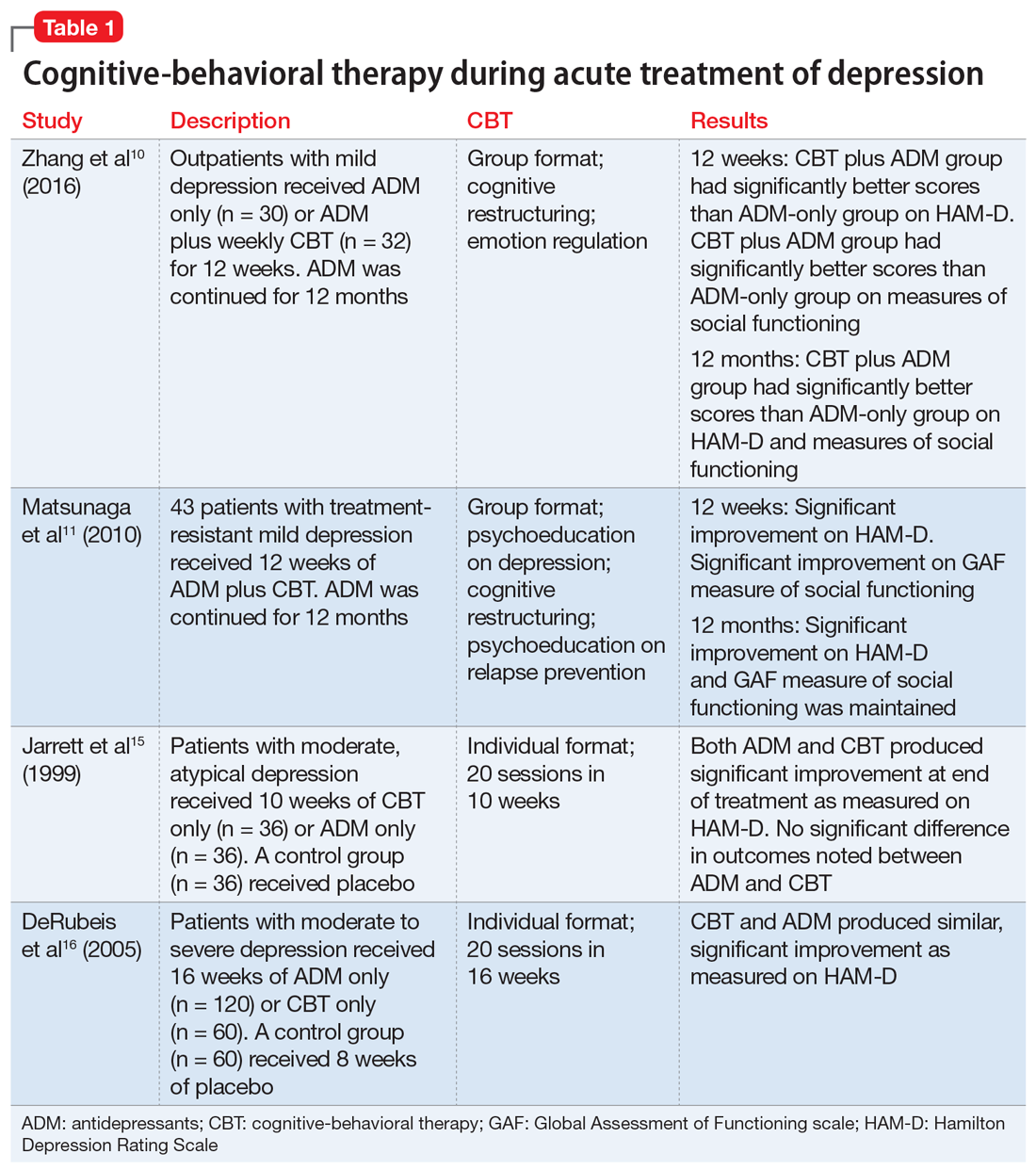
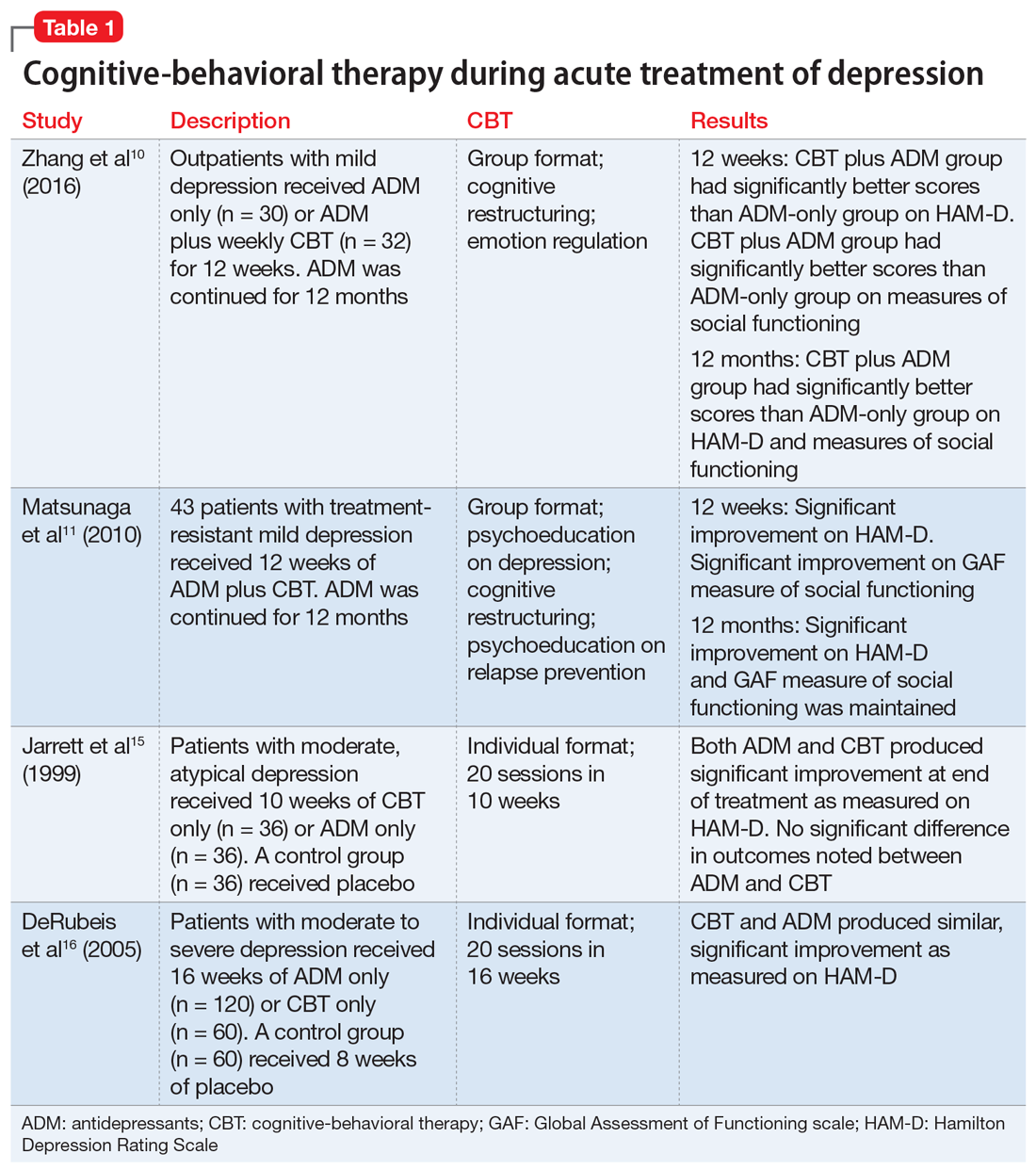
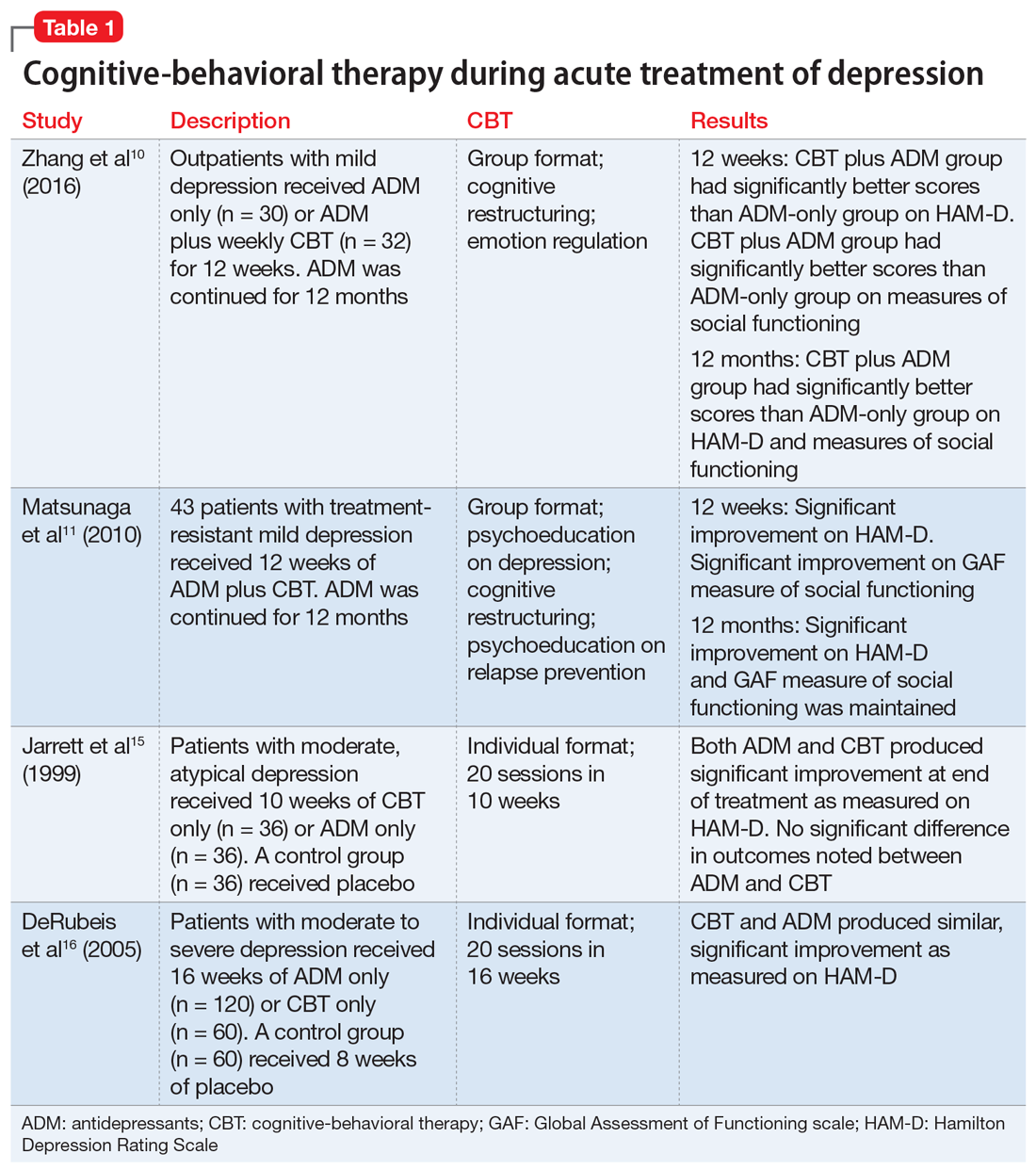
Table 110,11,15,16 summarizes the findings of select studies evaluating the use of CBT for the acute treatment of depression.
CBT’s role in long-term treatment
Recurrence and relapse are major problems associated with MDD. The large majority of individuals who experience an episode of depression go on to experience more episodes of depression,20 and the risk of recurrence increases after each successive episode.21
To reduce the risk of relapse and the return of symptoms, it is recommended that patients treated with antidepressants continue pharmacotherapy for 4 to 9 months after remission.9 Maintenance pharmacotherapy, which involves keeping patients on antidepressants beyond the point of recovery, is intended to reduce the risk of recurrence, and is standard treatment for patients with chronic or recurrent MDD.22 However, this preventive effect exists only while the patient continues to take the medication. Rates of symptom recurrence following medication withdrawal are often high regardless of how long patients have taken medications.23
Continue to: Studies examining CBT as a maintenance treatment...
Studies examining CBT as a maintenance treatment—provided alone or in combination with or sequentially with antidepressants—have found it has an enduring effect that extends beyond the end of treatment and equals the impact of continuing antidepressants.24-27 A recent meta-analysis of 10 trials where CBT had been provided to patients after acute treatment found that the risk of relapse was reduced by 21% in the first year and by 28% in the first 2 years.28
Studies have compared the prophylactic impact of maintenance CBT and antidepressants. In an early study, 40 patients who had been successfully treated with antidepressants but had residual symptoms were randomly assigned to 20 weeks of CBT or to clinical management.29 By the end of 20 weeks, patients were tapered off their antidepressant. All patients were then followed for 2 years, during which time they received no treatment. At the 2-year follow-up, the CBT group had a relapse rate of 25%, compared with 80% in the antidepressant group.29 Weaknesses of this study include a small sample size, and the fact that a single therapist provided the CBT.
This study was extended to a 6-year follow-up; antidepressants were prescribed only to patients who relapsed. The CBT group continued to have a significantly lower relapse rate (40%) compared with the antidepressant group (90%).30
In another RCT, patients with depression who had recovered with CBT or medication continued with the same treatment during a maintenance phase.26 The CBT group received 3 booster sessions during the next year and antidepressant group received medication. At the end of the second year (without CBT or medication) CBT patients were less likely to relapse compared with patients receiving antidepressants. The adjusted relapse rates were 17.3% for CBT and 53.6% for antidepressants.26
An RCT that included 452 patients with severe depression used a long intervention period (up to 42 weeks) and a flexible treatment algorithm to more closely model the strategies used in clinical practice.31 Patients were randomly assigned to antidepressants only or in combination with CBT. At the end of 12 months, outcome assessment by blinded interviewers indicated that patients with more severe depression were more likely to benefit from the combination of antidepressants and CBT (76.9% vs 60.3%) and those with severe, non-chronic depression received the most benefit (79.5% vs 62.8%). The lack of a CBT-only group limits the generalizability of these findings. Neither patients nor clinicians were blinded to the treatment assignment, which is a common limitation in psychotherapy studies but could have contributed to the finding that combined treatment was more effective.
Continue to: Some evidence suggests...
Some evidence suggests that augmenting treatment as usual (TAU) with CBT can have a resilient protective impact that also intensifies with the number of depressive episodes experienced. In an RCT, 172 patients with depression in remission were randomly assigned to TAU or to TAU augmented with CBT.32 The time to recurrence was assessed over the course of 10 years. Augmenting TAU with CBT had a significant protective impact that was greater for patients who had >3 previous episodes.32
Another long-term study assessed the longitudinal course of 158 patients who received CBT, medication, and clinical management, or medication and clinical management alone.33 Patients were followed 6 years after randomization (4.5 years after completion of CBT). Researchers found the effects of CBT in preventing relapse and recurrence persisted for several years.33
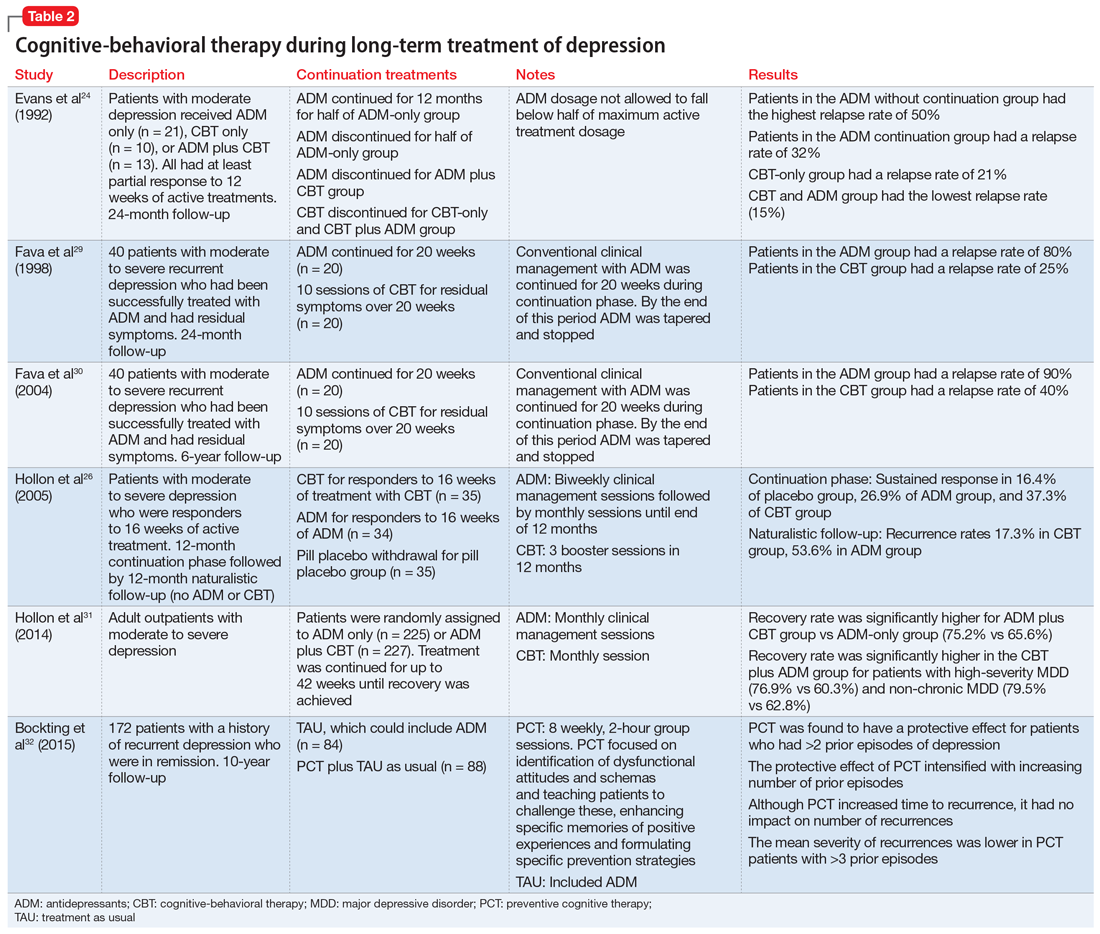
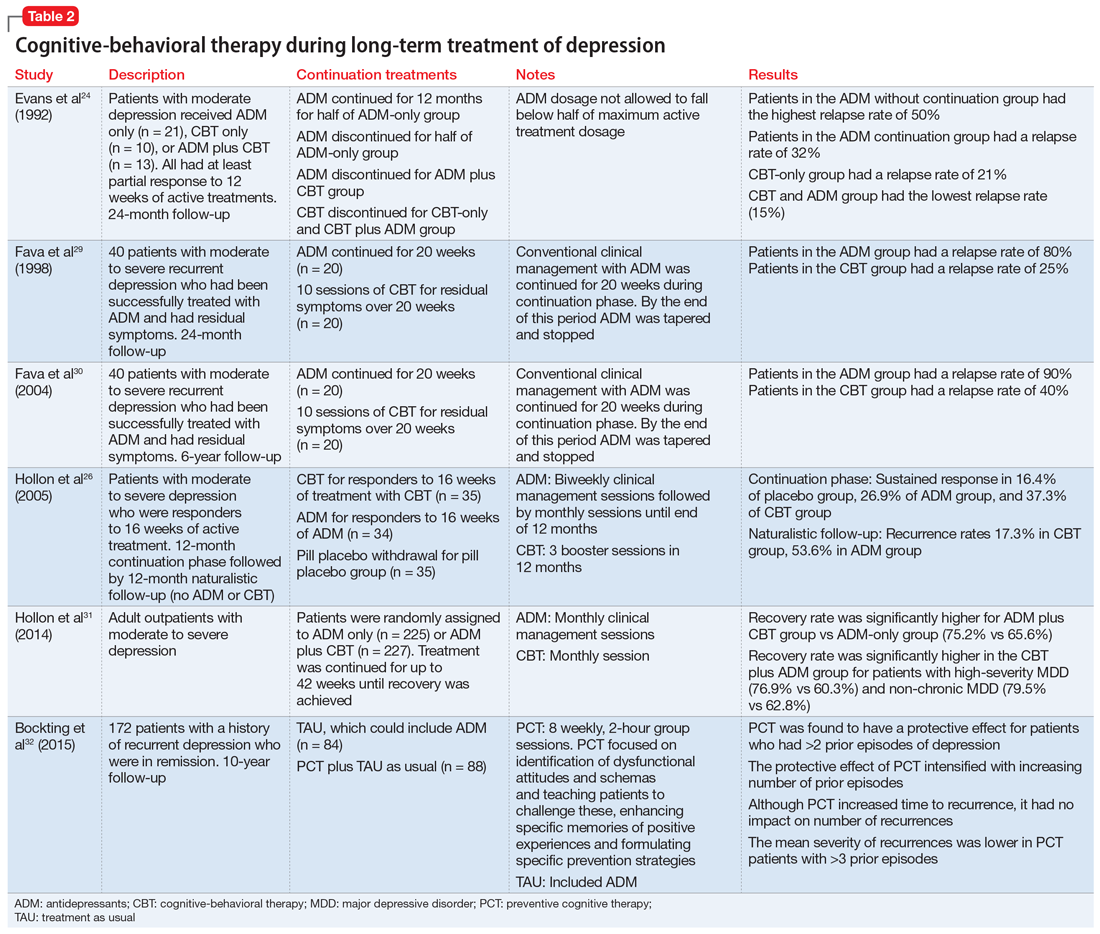
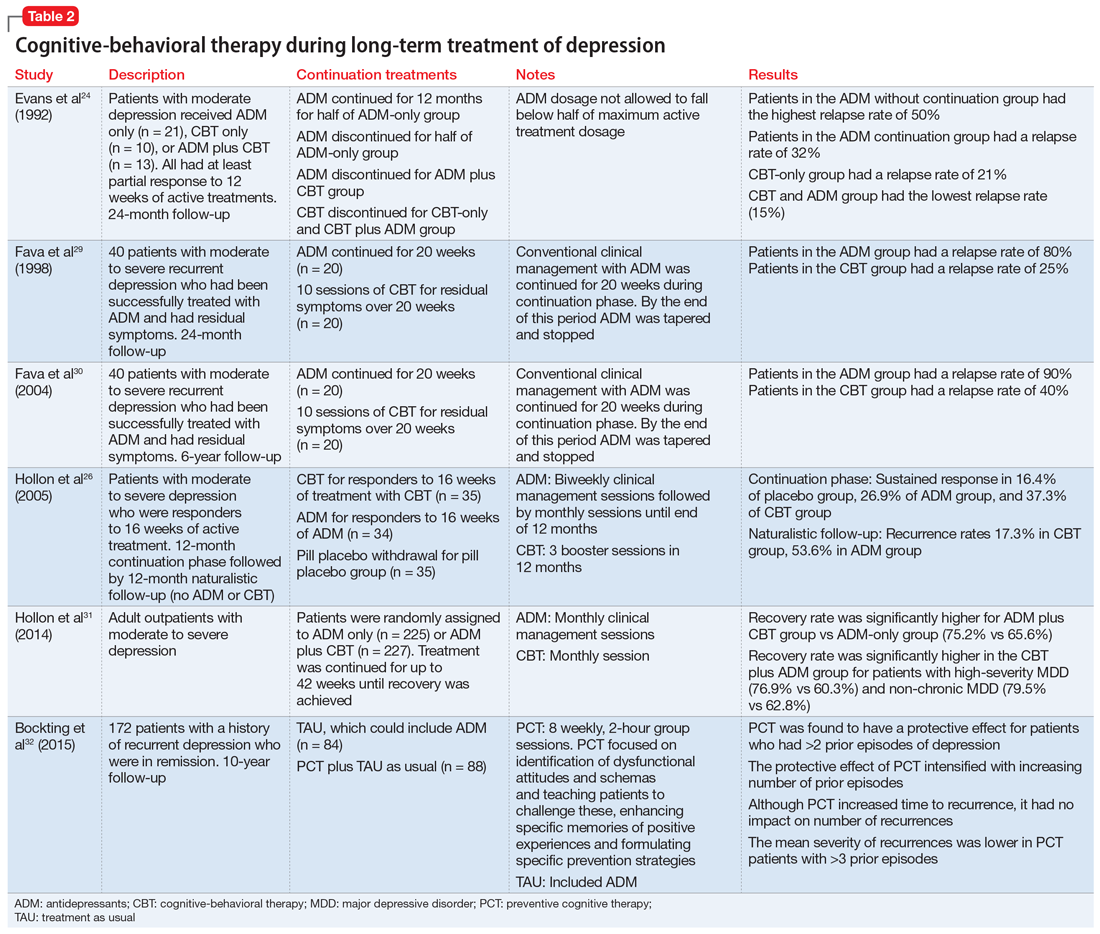
Table 224,26,29-32 summarizes the findings of select studies evaluating the use of CBT for the long-term treatment of depression.
Limitations of long-term studies
Studies that have examined the efficacy of adding CBT to antidepressants in the continuation and maintenance treatment of patients with MDD have had some limitations. The definitions of relapse and recurrence have not always been clearly delineated in all studies. This is important because recurrence rates tend to be lower, and long-term follow-up would be needed to detect multiple recurrences so that their incidence is not underestimated. In addition, the types of CBT interventions utilized has varied across studies. Some studies have employed standard interventions such as cognitive restructuring, while others have added strategies that focus on enhancing memories for positive experiences or interventions to encourage medication adherence. Despite these limitations, research has shown promising results and suggests that adding CBT to the maintenance treatment of patients with depression—with or without antidepressants—is likely to reduce the rate of relapse and recurrence.
Consider CBT for all depressed patients
Research indicates that CBT can be the preferred treatment for patients with mild to moderate MDD. Antidepressants significantly reduce depressive symptoms in patients with moderate to severe MDD. Some research suggests that CBT can be as effective as antidepressants for moderate and severe MDD. However, as the severity and chronicity of depression increase, other moderating factors need to be considered. The expertise of the CBT therapist has an impact on outcomes. Treatment protocols that utilize CBT plus antidepressants are likely to be more effective than CBT or antidepressants alone. Incorporating CBT in the acute phase of depression treatment, with or without antidepressants, can have a long-term impact. For maintenance treatment, CBT alone and CBT plus antidepressants have been found to help sustain remission.
Continue to: Bottom Line
Bottom Line
Cognitive-behavioral therapy (CBT) can be an effective treatment for patients with major depressive disorder, regardless of symptom severity. The expertise of the clinician who provides CBT has a substantial impact on outcomes. Combination treatment with CBT plus antidepressants is more likely to be effective than either treatment alone.
Related Resources
- Flynn HA, Warren R. Using CBT effectively for treating depression and anxiety. Current Psychiatry. 2014;13(6):45-53.
- Ijaz S, Davies P, Williams CJ, et al. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2018;5:CD010558.
1. Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851-858.
2. Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: remission and beyond. JAMA. 2003;289(23):3152-3160.
3. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
4. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
5. Oxman TE, Dietrich AJ, Schulberg HC. Evidence-based models of integrated management of depression in primary care. Psychiatr Clin North Am. 2005;28(4):1061-1077.
6. Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
7. Paykel ES, Hollyman JA, Freeling P, et al. Predictors of therapeutic benefit from amitriptyline in mild depression: a general practice placebo-controlled trial. J Affect Disord. 1988;14(1):83-95
8. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
9. Practice guideline for the treatment of patients with major depressive disorder, 3rd ed. Arlington, VA: American Psychiatric Association; 2010.
10. Zhang B, Ding X, Lu W, et al. Effect of group cognitive-behavioral therapy on the quality of life and social functioning of patients with mild depression. Shanghai Arch Psychiatry. 2016;28(1):18-27.
11. Matsunaga M, Okamoto Y, Suzuki S et.al. Psychosocial functioning in patients with treatment-resistant depression after group cognitive behavioral therapy. BMC Psychiatry. 2010;10:22.
12. American Psychiatric Association. Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry. 1993;150(suppl 4):1-26.
13. Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry. 1989;46(11):971-982; discussion 983.
14. Jacobson NS, Hollon SD. Prospects for future comparisons between drugs and psychotherapy: lessons from the CBT-versus-pharmacotherapy exchange. J Consult Clin Psychol. 1996;64(1):104-108.
15. Jarrett RB, Schaffer M, McIntire D, et al. Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1999;56(5):431-437.
16. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):409-416.
17. Amick HR, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015;351:h6019. doi: 10.1136/bmj.h6019.
18. Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry. 2006;188(1):13-20.
19. Fournier JC, DeRubeis RJ, Shelton RC, et al. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br J Psychiatry. 2008;192(2):124-129.
20. Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156(7):1000-1006.
21. Solomon DA, Keller MB, Leon AC, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry. 2000;157(2):229-233.
22. Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48(9):851-855.
23. Thase ME. Relapse and recurrence of depression: an updated practical approach for prevention. In: Palmer KJ, ed. Drug treatment issues in depression. Auckland, New Zealand: Adis International; 2000:35-52.
24. Evans MD, Hollon, SD, DeRubeis RJ, et al. Differential relapse following cognitive therapy and pharmacotherapy for depression. Arch Gen Psychiatry. 1992;49(10):802-808.
25. Vittengal JR, Clark LA, Dunn TW, et al. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75(3):475-488.
26. Hollon SD, DeRubeis RJ, Shelton RC, et al. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):417-422.
27. Paykel ES, Scott J, Teasdale JD, et al. Prevention of relapse in residual depression by cognitive therapy: a controlled trial. Arch Gen Psychiatry. 1999;56(9):829-835.
28. Clarke K, Mayo-Wilson E, Kenny J, et al. Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2015;39:58-70.
29. Fava GA, Rafanelli C, Grandi, S, et al. Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Arch Gen Psychiatry. 1998;55(9):816-820.
30. Fava GA, Ruini C, Rafanelli C, et al. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry. 2004;161(10):1872-1876.
31. Hollon SD, DeRubeis RJ, Fawcett J, et al. Effect of cognitive therapy with antidepressant medications vs antidepressants alone on the rate of recovery in major depressive disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(10):1157-1164.
32. Bockting CL, Smid NH, Koeter MW, et al. Enduring effects of preventive cognitive therapy in adults remitted from recurrent depression: a 10 year follow-up of a randomized controlled trial. J Affect Disord. 2015;185:188-194.
33. Paykel ES, Scott J, Cornwall PL, et al. Duration of relapse prevention after cognitive therapy in residual depression: follow-up of controlled trial. Psychol Med. 2005;35(1):59-68.
Major depressive disorder (MDD) has a devastating impact on individuals and society because of its high prevalence, its recurrent nature, its frequent comorbidity with other disorders, and the functional impairment it causes. Compared with other chronic diseases, such as arthritis, asthma, and diabetes, MDD produces the greatest decrement in health worldwide.1 The goals in treating MDD should be not just to reduce symptom severity but also to achieve continuing remission and lower the risk for relapse.2
Antidepressants are the most common treatment for depression.3 Among psychotherapies used to treat MDD, cognitive-behavioral therapy (CBT) has been identified as an effective treatment.4 Collaborative care models have been reported to manage MDD more effectively.5 In this article, we review the evidence supporting the use of CBT as monotherapy and in combination with antidepressants for acute and long-term treatment of MDD.
Acute treatment: Not too soon for CBT
Mild to moderate depression
Research has indicated that for the treatment of mild MDD, antidepressants are unlikely to be more effective than placebo.6,7 Studies also have reported that response to antidepressants begins to outpace response to placebo only when symptoms are no longer mild. Using antidepressants for patients with mild depression could therefore place them at risk of overtreatment.8 In keeping with these findings, the American Psychiatric Association (APA) has recommended the use of evidence-based psychotherapies, such as CBT, as an initial treatment choice for patients with mild to moderate MDD.9
Two recent studies have suggested that the combination of CBT plus antidepressants could boost improvement in psychosocial functioning for patients with mild MDD.10,11 However, neither study included a group of patients who received only CBT to evaluate if CBT alone could have also produced similar effects. Other limitations include the lack of a control group in one study and small sample sizes in both studies. However, both studies had a long follow-up period and specifically studied the impact on psychosocial functioning.
Moderate to severe depression
Earlier depression treatment guidelines suggested that antidepressants should be used to treat more severe depression, while psychotherapy should be used mainly for mild depression.12 This recommendation was influenced by the well-known National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program, a multicenter randomized controlled trial (RCT) that used a placebo control.13 In this study, CBT was compared with antidepressants and found to be no more effective than placebo for more severely depressed patients.13 However, this finding was not consistent across the 3 sites where the study was conducted; at the site where CBT was provided by more experienced CBT therapists, patients with more severe depression who received CBT fared as well as patients treated with antidepressants.14 A later double-blind RCT that used experienced therapists found that CBT was as effective as antidepressants (monoamine oxidase inhibitors), and both treatments were superior to placebo in reducing symptoms of atypical depression.15
Another placebo-controlled RCT conducted at 2 sites found that CBT was as effective as antidepressants in the treatment of moderately to severely depressed patients. As in the NIMH Treatment of Depression Collaborative Research Program trial,13 in this study, there were indications that the results were dependent on therapist experience.16 These findings suggest that the experience of the therapist is an important factor.
A recent meta-analysis of treatments of the acute phase of MDD compared 11 RCTs of CBT and second-generation antidepressants (selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and other medications with related mechanisms of action).17 It found that as a first-step treatment, CBT and antidepressants had a similar impact on symptom relief in patients with moderate to severe depression. Patients treated with antidepressants also had a higher risk of experiencing adverse events or discontinuing treatment because of adverse events. However, this meta-analysis included trials that had methodological shortcomings, which reduces the strength of these conclusions.
Continue to: Patients with MDD and comorbid personality disorders have been...
Patients with MDD and comorbid personality disorders have been reported to have poorer outcomes, regardless of the treatment used.18 Fournier et al19 examined the impact of antidepressants and CBT in moderately to severely depressed patients with and without a personality disorder. They found that a combination of antidepressants and CBT was suitable for patients with personality disorders because antidepressants would boost the initial response and CBT would help sustain improvement in the long term.
Presently, the APA suggests that the combination of psychotherapy and antidepressants may be used as an initial treatment for patients with moderate to severe MDD.9 As research brings to light other factors that affect treatment outcomes, these guidelines could change.
Table 110,11,15,16 summarizes the findings of select studies evaluating the use of CBT for the acute treatment of depression.
CBT’s role in long-term treatment
Recurrence and relapse are major problems associated with MDD. The large majority of individuals who experience an episode of depression go on to experience more episodes of depression,20 and the risk of recurrence increases after each successive episode.21
To reduce the risk of relapse and the return of symptoms, it is recommended that patients treated with antidepressants continue pharmacotherapy for 4 to 9 months after remission.9 Maintenance pharmacotherapy, which involves keeping patients on antidepressants beyond the point of recovery, is intended to reduce the risk of recurrence, and is standard treatment for patients with chronic or recurrent MDD.22 However, this preventive effect exists only while the patient continues to take the medication. Rates of symptom recurrence following medication withdrawal are often high regardless of how long patients have taken medications.23
Continue to: Studies examining CBT as a maintenance treatment...
Studies examining CBT as a maintenance treatment—provided alone or in combination with or sequentially with antidepressants—have found it has an enduring effect that extends beyond the end of treatment and equals the impact of continuing antidepressants.24-27 A recent meta-analysis of 10 trials where CBT had been provided to patients after acute treatment found that the risk of relapse was reduced by 21% in the first year and by 28% in the first 2 years.28
Studies have compared the prophylactic impact of maintenance CBT and antidepressants. In an early study, 40 patients who had been successfully treated with antidepressants but had residual symptoms were randomly assigned to 20 weeks of CBT or to clinical management.29 By the end of 20 weeks, patients were tapered off their antidepressant. All patients were then followed for 2 years, during which time they received no treatment. At the 2-year follow-up, the CBT group had a relapse rate of 25%, compared with 80% in the antidepressant group.29 Weaknesses of this study include a small sample size, and the fact that a single therapist provided the CBT.
This study was extended to a 6-year follow-up; antidepressants were prescribed only to patients who relapsed. The CBT group continued to have a significantly lower relapse rate (40%) compared with the antidepressant group (90%).30
In another RCT, patients with depression who had recovered with CBT or medication continued with the same treatment during a maintenance phase.26 The CBT group received 3 booster sessions during the next year and antidepressant group received medication. At the end of the second year (without CBT or medication) CBT patients were less likely to relapse compared with patients receiving antidepressants. The adjusted relapse rates were 17.3% for CBT and 53.6% for antidepressants.26
An RCT that included 452 patients with severe depression used a long intervention period (up to 42 weeks) and a flexible treatment algorithm to more closely model the strategies used in clinical practice.31 Patients were randomly assigned to antidepressants only or in combination with CBT. At the end of 12 months, outcome assessment by blinded interviewers indicated that patients with more severe depression were more likely to benefit from the combination of antidepressants and CBT (76.9% vs 60.3%) and those with severe, non-chronic depression received the most benefit (79.5% vs 62.8%). The lack of a CBT-only group limits the generalizability of these findings. Neither patients nor clinicians were blinded to the treatment assignment, which is a common limitation in psychotherapy studies but could have contributed to the finding that combined treatment was more effective.
Continue to: Some evidence suggests...
Some evidence suggests that augmenting treatment as usual (TAU) with CBT can have a resilient protective impact that also intensifies with the number of depressive episodes experienced. In an RCT, 172 patients with depression in remission were randomly assigned to TAU or to TAU augmented with CBT.32 The time to recurrence was assessed over the course of 10 years. Augmenting TAU with CBT had a significant protective impact that was greater for patients who had >3 previous episodes.32
Another long-term study assessed the longitudinal course of 158 patients who received CBT, medication, and clinical management, or medication and clinical management alone.33 Patients were followed 6 years after randomization (4.5 years after completion of CBT). Researchers found the effects of CBT in preventing relapse and recurrence persisted for several years.33
Table 224,26,29-32 summarizes the findings of select studies evaluating the use of CBT for the long-term treatment of depression.
Limitations of long-term studies
Studies that have examined the efficacy of adding CBT to antidepressants in the continuation and maintenance treatment of patients with MDD have had some limitations. The definitions of relapse and recurrence have not always been clearly delineated in all studies. This is important because recurrence rates tend to be lower, and long-term follow-up would be needed to detect multiple recurrences so that their incidence is not underestimated. In addition, the types of CBT interventions utilized has varied across studies. Some studies have employed standard interventions such as cognitive restructuring, while others have added strategies that focus on enhancing memories for positive experiences or interventions to encourage medication adherence. Despite these limitations, research has shown promising results and suggests that adding CBT to the maintenance treatment of patients with depression—with or without antidepressants—is likely to reduce the rate of relapse and recurrence.
Consider CBT for all depressed patients
Research indicates that CBT can be the preferred treatment for patients with mild to moderate MDD. Antidepressants significantly reduce depressive symptoms in patients with moderate to severe MDD. Some research suggests that CBT can be as effective as antidepressants for moderate and severe MDD. However, as the severity and chronicity of depression increase, other moderating factors need to be considered. The expertise of the CBT therapist has an impact on outcomes. Treatment protocols that utilize CBT plus antidepressants are likely to be more effective than CBT or antidepressants alone. Incorporating CBT in the acute phase of depression treatment, with or without antidepressants, can have a long-term impact. For maintenance treatment, CBT alone and CBT plus antidepressants have been found to help sustain remission.
Continue to: Bottom Line
Bottom Line
Cognitive-behavioral therapy (CBT) can be an effective treatment for patients with major depressive disorder, regardless of symptom severity. The expertise of the clinician who provides CBT has a substantial impact on outcomes. Combination treatment with CBT plus antidepressants is more likely to be effective than either treatment alone.
Related Resources
- Flynn HA, Warren R. Using CBT effectively for treating depression and anxiety. Current Psychiatry. 2014;13(6):45-53.
- Ijaz S, Davies P, Williams CJ, et al. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2018;5:CD010558.
Major depressive disorder (MDD) has a devastating impact on individuals and society because of its high prevalence, its recurrent nature, its frequent comorbidity with other disorders, and the functional impairment it causes. Compared with other chronic diseases, such as arthritis, asthma, and diabetes, MDD produces the greatest decrement in health worldwide.1 The goals in treating MDD should be not just to reduce symptom severity but also to achieve continuing remission and lower the risk for relapse.2
Antidepressants are the most common treatment for depression.3 Among psychotherapies used to treat MDD, cognitive-behavioral therapy (CBT) has been identified as an effective treatment.4 Collaborative care models have been reported to manage MDD more effectively.5 In this article, we review the evidence supporting the use of CBT as monotherapy and in combination with antidepressants for acute and long-term treatment of MDD.
Acute treatment: Not too soon for CBT
Mild to moderate depression
Research has indicated that for the treatment of mild MDD, antidepressants are unlikely to be more effective than placebo.6,7 Studies also have reported that response to antidepressants begins to outpace response to placebo only when symptoms are no longer mild. Using antidepressants for patients with mild depression could therefore place them at risk of overtreatment.8 In keeping with these findings, the American Psychiatric Association (APA) has recommended the use of evidence-based psychotherapies, such as CBT, as an initial treatment choice for patients with mild to moderate MDD.9
Two recent studies have suggested that the combination of CBT plus antidepressants could boost improvement in psychosocial functioning for patients with mild MDD.10,11 However, neither study included a group of patients who received only CBT to evaluate if CBT alone could have also produced similar effects. Other limitations include the lack of a control group in one study and small sample sizes in both studies. However, both studies had a long follow-up period and specifically studied the impact on psychosocial functioning.
Moderate to severe depression
Earlier depression treatment guidelines suggested that antidepressants should be used to treat more severe depression, while psychotherapy should be used mainly for mild depression.12 This recommendation was influenced by the well-known National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program, a multicenter randomized controlled trial (RCT) that used a placebo control.13 In this study, CBT was compared with antidepressants and found to be no more effective than placebo for more severely depressed patients.13 However, this finding was not consistent across the 3 sites where the study was conducted; at the site where CBT was provided by more experienced CBT therapists, patients with more severe depression who received CBT fared as well as patients treated with antidepressants.14 A later double-blind RCT that used experienced therapists found that CBT was as effective as antidepressants (monoamine oxidase inhibitors), and both treatments were superior to placebo in reducing symptoms of atypical depression.15
Another placebo-controlled RCT conducted at 2 sites found that CBT was as effective as antidepressants in the treatment of moderately to severely depressed patients. As in the NIMH Treatment of Depression Collaborative Research Program trial,13 in this study, there were indications that the results were dependent on therapist experience.16 These findings suggest that the experience of the therapist is an important factor.
A recent meta-analysis of treatments of the acute phase of MDD compared 11 RCTs of CBT and second-generation antidepressants (selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and other medications with related mechanisms of action).17 It found that as a first-step treatment, CBT and antidepressants had a similar impact on symptom relief in patients with moderate to severe depression. Patients treated with antidepressants also had a higher risk of experiencing adverse events or discontinuing treatment because of adverse events. However, this meta-analysis included trials that had methodological shortcomings, which reduces the strength of these conclusions.
Continue to: Patients with MDD and comorbid personality disorders have been...
Patients with MDD and comorbid personality disorders have been reported to have poorer outcomes, regardless of the treatment used.18 Fournier et al19 examined the impact of antidepressants and CBT in moderately to severely depressed patients with and without a personality disorder. They found that a combination of antidepressants and CBT was suitable for patients with personality disorders because antidepressants would boost the initial response and CBT would help sustain improvement in the long term.
Presently, the APA suggests that the combination of psychotherapy and antidepressants may be used as an initial treatment for patients with moderate to severe MDD.9 As research brings to light other factors that affect treatment outcomes, these guidelines could change.
Table 110,11,15,16 summarizes the findings of select studies evaluating the use of CBT for the acute treatment of depression.
CBT’s role in long-term treatment
Recurrence and relapse are major problems associated with MDD. The large majority of individuals who experience an episode of depression go on to experience more episodes of depression,20 and the risk of recurrence increases after each successive episode.21
To reduce the risk of relapse and the return of symptoms, it is recommended that patients treated with antidepressants continue pharmacotherapy for 4 to 9 months after remission.9 Maintenance pharmacotherapy, which involves keeping patients on antidepressants beyond the point of recovery, is intended to reduce the risk of recurrence, and is standard treatment for patients with chronic or recurrent MDD.22 However, this preventive effect exists only while the patient continues to take the medication. Rates of symptom recurrence following medication withdrawal are often high regardless of how long patients have taken medications.23
Continue to: Studies examining CBT as a maintenance treatment...
Studies examining CBT as a maintenance treatment—provided alone or in combination with or sequentially with antidepressants—have found it has an enduring effect that extends beyond the end of treatment and equals the impact of continuing antidepressants.24-27 A recent meta-analysis of 10 trials where CBT had been provided to patients after acute treatment found that the risk of relapse was reduced by 21% in the first year and by 28% in the first 2 years.28
Studies have compared the prophylactic impact of maintenance CBT and antidepressants. In an early study, 40 patients who had been successfully treated with antidepressants but had residual symptoms were randomly assigned to 20 weeks of CBT or to clinical management.29 By the end of 20 weeks, patients were tapered off their antidepressant. All patients were then followed for 2 years, during which time they received no treatment. At the 2-year follow-up, the CBT group had a relapse rate of 25%, compared with 80% in the antidepressant group.29 Weaknesses of this study include a small sample size, and the fact that a single therapist provided the CBT.
This study was extended to a 6-year follow-up; antidepressants were prescribed only to patients who relapsed. The CBT group continued to have a significantly lower relapse rate (40%) compared with the antidepressant group (90%).30
In another RCT, patients with depression who had recovered with CBT or medication continued with the same treatment during a maintenance phase.26 The CBT group received 3 booster sessions during the next year and antidepressant group received medication. At the end of the second year (without CBT or medication) CBT patients were less likely to relapse compared with patients receiving antidepressants. The adjusted relapse rates were 17.3% for CBT and 53.6% for antidepressants.26
An RCT that included 452 patients with severe depression used a long intervention period (up to 42 weeks) and a flexible treatment algorithm to more closely model the strategies used in clinical practice.31 Patients were randomly assigned to antidepressants only or in combination with CBT. At the end of 12 months, outcome assessment by blinded interviewers indicated that patients with more severe depression were more likely to benefit from the combination of antidepressants and CBT (76.9% vs 60.3%) and those with severe, non-chronic depression received the most benefit (79.5% vs 62.8%). The lack of a CBT-only group limits the generalizability of these findings. Neither patients nor clinicians were blinded to the treatment assignment, which is a common limitation in psychotherapy studies but could have contributed to the finding that combined treatment was more effective.
Continue to: Some evidence suggests...
Some evidence suggests that augmenting treatment as usual (TAU) with CBT can have a resilient protective impact that also intensifies with the number of depressive episodes experienced. In an RCT, 172 patients with depression in remission were randomly assigned to TAU or to TAU augmented with CBT.32 The time to recurrence was assessed over the course of 10 years. Augmenting TAU with CBT had a significant protective impact that was greater for patients who had >3 previous episodes.32
Another long-term study assessed the longitudinal course of 158 patients who received CBT, medication, and clinical management, or medication and clinical management alone.33 Patients were followed 6 years after randomization (4.5 years after completion of CBT). Researchers found the effects of CBT in preventing relapse and recurrence persisted for several years.33
Table 224,26,29-32 summarizes the findings of select studies evaluating the use of CBT for the long-term treatment of depression.
Limitations of long-term studies
Studies that have examined the efficacy of adding CBT to antidepressants in the continuation and maintenance treatment of patients with MDD have had some limitations. The definitions of relapse and recurrence have not always been clearly delineated in all studies. This is important because recurrence rates tend to be lower, and long-term follow-up would be needed to detect multiple recurrences so that their incidence is not underestimated. In addition, the types of CBT interventions utilized has varied across studies. Some studies have employed standard interventions such as cognitive restructuring, while others have added strategies that focus on enhancing memories for positive experiences or interventions to encourage medication adherence. Despite these limitations, research has shown promising results and suggests that adding CBT to the maintenance treatment of patients with depression—with or without antidepressants—is likely to reduce the rate of relapse and recurrence.
Consider CBT for all depressed patients
Research indicates that CBT can be the preferred treatment for patients with mild to moderate MDD. Antidepressants significantly reduce depressive symptoms in patients with moderate to severe MDD. Some research suggests that CBT can be as effective as antidepressants for moderate and severe MDD. However, as the severity and chronicity of depression increase, other moderating factors need to be considered. The expertise of the CBT therapist has an impact on outcomes. Treatment protocols that utilize CBT plus antidepressants are likely to be more effective than CBT or antidepressants alone. Incorporating CBT in the acute phase of depression treatment, with or without antidepressants, can have a long-term impact. For maintenance treatment, CBT alone and CBT plus antidepressants have been found to help sustain remission.
Continue to: Bottom Line
Bottom Line
Cognitive-behavioral therapy (CBT) can be an effective treatment for patients with major depressive disorder, regardless of symptom severity. The expertise of the clinician who provides CBT has a substantial impact on outcomes. Combination treatment with CBT plus antidepressants is more likely to be effective than either treatment alone.
Related Resources
- Flynn HA, Warren R. Using CBT effectively for treating depression and anxiety. Current Psychiatry. 2014;13(6):45-53.
- Ijaz S, Davies P, Williams CJ, et al. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2018;5:CD010558.
1. Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851-858.
2. Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: remission and beyond. JAMA. 2003;289(23):3152-3160.
3. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
4. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
5. Oxman TE, Dietrich AJ, Schulberg HC. Evidence-based models of integrated management of depression in primary care. Psychiatr Clin North Am. 2005;28(4):1061-1077.
6. Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
7. Paykel ES, Hollyman JA, Freeling P, et al. Predictors of therapeutic benefit from amitriptyline in mild depression: a general practice placebo-controlled trial. J Affect Disord. 1988;14(1):83-95
8. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
9. Practice guideline for the treatment of patients with major depressive disorder, 3rd ed. Arlington, VA: American Psychiatric Association; 2010.
10. Zhang B, Ding X, Lu W, et al. Effect of group cognitive-behavioral therapy on the quality of life and social functioning of patients with mild depression. Shanghai Arch Psychiatry. 2016;28(1):18-27.
11. Matsunaga M, Okamoto Y, Suzuki S et.al. Psychosocial functioning in patients with treatment-resistant depression after group cognitive behavioral therapy. BMC Psychiatry. 2010;10:22.
12. American Psychiatric Association. Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry. 1993;150(suppl 4):1-26.
13. Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry. 1989;46(11):971-982; discussion 983.
14. Jacobson NS, Hollon SD. Prospects for future comparisons between drugs and psychotherapy: lessons from the CBT-versus-pharmacotherapy exchange. J Consult Clin Psychol. 1996;64(1):104-108.
15. Jarrett RB, Schaffer M, McIntire D, et al. Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1999;56(5):431-437.
16. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):409-416.
17. Amick HR, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015;351:h6019. doi: 10.1136/bmj.h6019.
18. Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry. 2006;188(1):13-20.
19. Fournier JC, DeRubeis RJ, Shelton RC, et al. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br J Psychiatry. 2008;192(2):124-129.
20. Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156(7):1000-1006.
21. Solomon DA, Keller MB, Leon AC, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry. 2000;157(2):229-233.
22. Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48(9):851-855.
23. Thase ME. Relapse and recurrence of depression: an updated practical approach for prevention. In: Palmer KJ, ed. Drug treatment issues in depression. Auckland, New Zealand: Adis International; 2000:35-52.
24. Evans MD, Hollon, SD, DeRubeis RJ, et al. Differential relapse following cognitive therapy and pharmacotherapy for depression. Arch Gen Psychiatry. 1992;49(10):802-808.
25. Vittengal JR, Clark LA, Dunn TW, et al. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75(3):475-488.
26. Hollon SD, DeRubeis RJ, Shelton RC, et al. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):417-422.
27. Paykel ES, Scott J, Teasdale JD, et al. Prevention of relapse in residual depression by cognitive therapy: a controlled trial. Arch Gen Psychiatry. 1999;56(9):829-835.
28. Clarke K, Mayo-Wilson E, Kenny J, et al. Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2015;39:58-70.
29. Fava GA, Rafanelli C, Grandi, S, et al. Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Arch Gen Psychiatry. 1998;55(9):816-820.
30. Fava GA, Ruini C, Rafanelli C, et al. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry. 2004;161(10):1872-1876.
31. Hollon SD, DeRubeis RJ, Fawcett J, et al. Effect of cognitive therapy with antidepressant medications vs antidepressants alone on the rate of recovery in major depressive disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(10):1157-1164.
32. Bockting CL, Smid NH, Koeter MW, et al. Enduring effects of preventive cognitive therapy in adults remitted from recurrent depression: a 10 year follow-up of a randomized controlled trial. J Affect Disord. 2015;185:188-194.
33. Paykel ES, Scott J, Cornwall PL, et al. Duration of relapse prevention after cognitive therapy in residual depression: follow-up of controlled trial. Psychol Med. 2005;35(1):59-68.
1. Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851-858.
2. Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: remission and beyond. JAMA. 2003;289(23):3152-3160.
3. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
4. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
5. Oxman TE, Dietrich AJ, Schulberg HC. Evidence-based models of integrated management of depression in primary care. Psychiatr Clin North Am. 2005;28(4):1061-1077.
6. Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
7. Paykel ES, Hollyman JA, Freeling P, et al. Predictors of therapeutic benefit from amitriptyline in mild depression: a general practice placebo-controlled trial. J Affect Disord. 1988;14(1):83-95
8. Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265-1273.
9. Practice guideline for the treatment of patients with major depressive disorder, 3rd ed. Arlington, VA: American Psychiatric Association; 2010.
10. Zhang B, Ding X, Lu W, et al. Effect of group cognitive-behavioral therapy on the quality of life and social functioning of patients with mild depression. Shanghai Arch Psychiatry. 2016;28(1):18-27.
11. Matsunaga M, Okamoto Y, Suzuki S et.al. Psychosocial functioning in patients with treatment-resistant depression after group cognitive behavioral therapy. BMC Psychiatry. 2010;10:22.
12. American Psychiatric Association. Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry. 1993;150(suppl 4):1-26.
13. Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry. 1989;46(11):971-982; discussion 983.
14. Jacobson NS, Hollon SD. Prospects for future comparisons between drugs and psychotherapy: lessons from the CBT-versus-pharmacotherapy exchange. J Consult Clin Psychol. 1996;64(1):104-108.
15. Jarrett RB, Schaffer M, McIntire D, et al. Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1999;56(5):431-437.
16. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):409-416.
17. Amick HR, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015;351:h6019. doi: 10.1136/bmj.h6019.
18. Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry. 2006;188(1):13-20.
19. Fournier JC, DeRubeis RJ, Shelton RC, et al. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br J Psychiatry. 2008;192(2):124-129.
20. Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156(7):1000-1006.
21. Solomon DA, Keller MB, Leon AC, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry. 2000;157(2):229-233.
22. Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48(9):851-855.
23. Thase ME. Relapse and recurrence of depression: an updated practical approach for prevention. In: Palmer KJ, ed. Drug treatment issues in depression. Auckland, New Zealand: Adis International; 2000:35-52.
24. Evans MD, Hollon, SD, DeRubeis RJ, et al. Differential relapse following cognitive therapy and pharmacotherapy for depression. Arch Gen Psychiatry. 1992;49(10):802-808.
25. Vittengal JR, Clark LA, Dunn TW, et al. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75(3):475-488.
26. Hollon SD, DeRubeis RJ, Shelton RC, et al. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):417-422.
27. Paykel ES, Scott J, Teasdale JD, et al. Prevention of relapse in residual depression by cognitive therapy: a controlled trial. Arch Gen Psychiatry. 1999;56(9):829-835.
28. Clarke K, Mayo-Wilson E, Kenny J, et al. Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2015;39:58-70.
29. Fava GA, Rafanelli C, Grandi, S, et al. Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Arch Gen Psychiatry. 1998;55(9):816-820.
30. Fava GA, Ruini C, Rafanelli C, et al. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry. 2004;161(10):1872-1876.
31. Hollon SD, DeRubeis RJ, Fawcett J, et al. Effect of cognitive therapy with antidepressant medications vs antidepressants alone on the rate of recovery in major depressive disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(10):1157-1164.
32. Bockting CL, Smid NH, Koeter MW, et al. Enduring effects of preventive cognitive therapy in adults remitted from recurrent depression: a 10 year follow-up of a randomized controlled trial. J Affect Disord. 2015;185:188-194.
33. Paykel ES, Scott J, Cornwall PL, et al. Duration of relapse prevention after cognitive therapy in residual depression: follow-up of controlled trial. Psychol Med. 2005;35(1):59-68.
How to adapt cognitive-behavioral therapy for older adults
Some older patients with depression, anxiety, or insomnia may be reluctant to turn to pharmacotherapy and may prefer psychotherapeutic treatments.1 Evidence has established cognitive-behavioral therapy (CBT) as an effective intervention for several psychiatric disorders and CBT should be considered when treating geriatric patients (Table 1).2
Table 1
Indications for CBT
| Mild to moderate depression. In the case of severe depression, CBT can be combined with pharmacotherapy |
| Anxiety disorders, mixed anxiety states |
| Insomnia—both primary and comorbid with other medical and/or psychiatric conditions |
| CBT: cognitive-behavioral therapy |
Research evaluating the efficacy of CBT for depression in older adults was first published in the early 1980s. Since then, research and application of CBT with older adults has expanded to include other psychiatric disorders and researchers have suggested changes to increase the efficacy of CBT for these patients. This article provides:
- an overview of CBT’s efficacy for older adults with depression, anxiety, and insomnia
- modifications to employ when providing CBT to older patients.
The cognitive model of CBT
In the 1970s, Aaron T. Beck, MD, developed CBT while working with depressed patients. Beck’s patients reported thoughts characterized by inaccuracies and distortions in association with their depressed mood. He found these thoughts could be brought to the patient’s conscious attention and modified to improve the patient’s depression. This finding led to the development of CBT.
CBT is based on a cognitive model of the relationship among cognition, emotion, and behavior. Mood and behavior are viewed as determined by a person’s perception and interpretation of events, which manifest as a stream of automatically generated thoughts (Figure).3 These automatic thoughts have their origins in an underlying network of beliefs or schema. Patients with psychiatric disorders such as anxiety and depression typically have frequent automatic thoughts that characteristically lack validity because they arise from dysfunctional beliefs. The therapeutic process consists of helping the patient become aware of his or her internal stream of thoughts when distressed, and to identify and modify the dysfunctional thoughts. Behavioral techniques are used to bring about functional changes in behavior, regulate emotion, and help the cognitive restructuring process. Modifying the patient’s underlying dysfunctional beliefs leads to lasting improvements. In this structured therapy, the therapist and patient work collaboratively to use an approach that features reality testing and experimentation.4
Figure
The cognitive model of CBT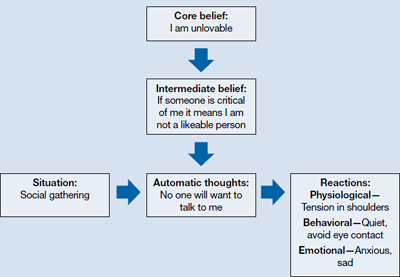
CBT: cognitive-behavioral therapy
Source: Adapted from reference 3
Indications for CBT in older adults
Depression. Among psychotherapies used in older adults, CBT has received the most research for late-life depression.5 Randomized controlled trials (RCTs) have found CBT is superior to treatment as usual in depressed adults age ≥60.6 It also has been found to be superior to wait-list control7 and talking as control.6,8 Meta-analyses have shown above-average effect sizes for CBT in treating late-life depression.9,10 A follow-up study found improvement was maintained up to 2 years after CBT, which suggests CBT’s impact is likely to be long lasting.11
Thompson et al12 compared 102 depressed patients age >60 who were treated with CBT alone, desipramine alone, or a combination of the 2. A combination of medication and CBT worked best for severely depressed patients; CBT alone or a combination of CBT and medication worked best for moderately depressed patients.
CBT is an option when treating depressed medically ill older adults. Research indicates that CBT could reduce depression in older patients with Parkinson’s disease13 and chronic obstructive pulmonary disease.14
As patients get older, cognitive impairment with comorbid depression can make treatment challenging. Limited research suggests CBT applied in a modified format that involves caregivers and uses problem solving and behavioral strategies can significantly reduce depression in patients with dementia.15
Anxiety. Researchers have examined the efficacy of variants of CBT in treating older adults with anxiety disorders—commonly, generalized anxiety disorder (GAD), panic disorder, agoraphobia, subjective anxiety, or a combination of these illnesses.16,17 Randomized trials have supported CBT’s efficacy for older patients with GAD and mixed anxiety states; gains made in CBT were maintained over a 1-year follow-up.18,19 In a meta-analysis of 15 studies using cognitive and behavioral methods of treating anxiety in older patients, Nordhus and Pallesen16 reported a significant effect size of 0.55. In a 2008 meta-analysis that included only RCTs, CBT was superior to wait-list conditions as well as active control conditions in treating anxious older patients.20
However, some research suggests that CBT for GAD may not be as effective for older adults as it is for younger adults. In a study of CBT for GAD in older adults, Stanley et al19 reported smaller effect sizes compared with CBT for younger adults. Researchers have found relatively few differences between CBT and comparison conditions—supportive psychotherapy or active control conditions—in treating GAD in older adults.21 Modified, more effective formats of CBT for GAD in older adults need to be established.22 Mohlman et al23 supplemented standard CBT for late-life GAD with memory and learning aids—weekly reading assignments, graphing exercises to chart mood ratings, reminder phone calls from therapists, and homework compliance requirement. This approach improved the response rate from 40% to 75%.23
Insomnia. Studies have found CBT to be an effective means of treating insomnia in geriatric patients. Although sleep problems occur more frequently among older patients, only 15% of chronic insomnia patients receive treatment; psychotherapy rarely is used.24 CBT for insomnia (CBT-I) should be considered for older adults because managing insomnia with medications may be problematic and these patients may prefer nonpharmacologic treatment.2 CBT-I typically incorporates cognitive strategies with established behavioral techniques, including sleep hygiene education, cognitive restructuring, relaxation training, stimulus control, and/or sleep restriction. The CBT-I multicomponent treatment package meets all criteria to be considered an evidence-based treatment for late-life insomnia.25
RCTs have reported significant improvements in late-life insomnia with CBT-I.26,27 Reviews and meta-analyses have also concluded that cognitive-behavioral treatments are effective for treating insomnia in older adults.25,28 Most insomnia cases in geriatric patients are reported to occur secondary to other medical or psychiatric conditions that are judged as causing the insomnia.25 In these cases, direct treatment of the insomnia usually is delayed or omitted.28 Studies evaluating the efficacy of CBT packages for treating insomnia occurring in conjunction with other medical or psychiatric illnesses have reported significant improvement of insomnia.28,29 Because insomnia frequently occurs in older patients with medical illnesses and psychiatric disorders, CBT-I could be beneficial for such patients.
Good candidates for CBT
Clinical experience indicates that older adults in relatively good health with no significant cognitive decline are good candidates for CBT. These patients tend to comply with their assignments, are interested in applying the learned strategies, and are motivated to read self-help books. CBT’s structured, goal-oriented approach makes it a short-term treatment, which makes it cost effective. Insomnia patients may improve after 6 to 8 CBT-I sessions and patients with anxiety or depression may need to undergo 15 to 20 CBT sessions. Patients age ≥65 have basic Medicare coverage that includes mental health care and psychotherapy.
There are no absolute contraindications for CBT, but the greater the cognitive impairment, the less the patient will benefit from CBT (Table 2). Similarly, severe depression and anxiety might make it difficult for patients to participate meaningfully, although CBT may be incorporated gradually as patients improve with medication. Severe medical illnesses and sensory losses such as visual and hearing loss would make it difficult to carry out CBT effectively.
Table 2
Contraindications for CBT
| High levels of cognitive impairment |
| Severe depression with psychotic features |
| Severe anxiety with high levels of agitation |
| Severe medical illness |
| Sensory losses |
| CBT: cognitive-behavioral therapy |
Adapting CBT for older patients
When using CBT with older patients, it is important to keep in mind characteristics that define the geriatric population. Laidlaw et al30 developed a model to help clinicians develop a more appropriate conceptualization of older patients that focuses on significant events and related cognitions associated with physical health, changes in role investments, and interactions with younger generations. It emphasizes the need to explore beliefs about aging viewed through each patient’s socio-cultural lens and examine cognitions in the context of the time period in which the individual has lived.
Losses and transitions. For many older patients, the latter years of life are characterized by losses and transitions.31 According to Thompson,31 these losses and transitions can trigger thoughts of missed opportunities or unresolved relationships and reflection on unachieved goals.31 CBT for older adults should focus on the meaning the patient gives to these losses and transitions. For example, depressed patients could view their retirement as a loss of self worth as they become less productive. CBT can help patients identify ways of thinking about the situation that will enable them to adapt to these losses and transitions.
Changes in cognition. Changes in cognitive functioning with aging are not universal and there’s considerable variability, but it’s important to make appropriate adaptations when needed. Patients may experience a decline in cognitive speed, working memory, selective attention, and fluid intelligence. This would require that information be presented slowly, with frequent repetitions and summaries. Also, it might be helpful to present information in alternate ways and to encourage patients to take notes during sessions. To accommodate for a decline in fluid intelligence, presenting new information in the context of previous experiences will help promote learning. Recordings of important information and conclusions from cognitive restructuring that patients can listen to between sessions could serve as helpful reminders that will help patients progress. Phone prompts or alarms can remind patients to carry out certain therapeutic measures, such as breathing exercises. Caretakers can attend sessions to become familiar with strategies performed during CBT and act as a co-therapist at home; however, their inclusion must be done with the consent of both parties and only if it’s viewed as necessary for the patient’s progress.
Additional strategies. For patients with substantial cognitive decline, cognitive restructuring might not be as effective as behavioral strategies—activity scheduling, graded task assignment, graded exposure, and rehearsals. Because older adults often have strengthened dysfunctional beliefs over a long time, modifying them takes longer, which is why the tapering process usually takes longer for older patients than for younger patients. The lengthier tapering ensures learning is well established and the process of modifying dysfunctional beliefs to functional beliefs continues. Collaborating with other professionals—physicians, social workers, and case managers—will help ensure a shared care process in which common goals are met.
The websites of the Academy of Cognitive Therapy, American Psychological Association, and Association for Behavioral and Cognitive Therapies can help clinicians who do not offer CBT to locate a qualified therapist for their patients (Related Resources).
- Academy of Cognitive Therapy. www.academyofct.org.
- American Psychological Association. www.apa.org.
- Association for Behavioral and Cognitive Therapies. www.abct.org.
- Laidlaw K, Thompson LW, Dick-Siskin L, et al. Cognitive behaviour therapy with older people. West Sussex, England: John Wiley & Sons, Ltd; 2003.
Drug Brand Name
- Desipramine • Norpramin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Landreville P, Landry J, Baillargeon L, et al. Older adults’ acceptance of psychological and pharmacological treatments for depression. J Gerontol B Psychol Sci Soc Sci. 2001;56(5):P285-P291.
2. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
3. Beck JS. Cognitive conceptualization. In: Cognitive therapy: basics and beyond. 2nd ed. New York NY: The Guilford Press; 2011:29–45.
4. Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York, NY: The Guilford Press; 1979.
5. Areán PA, Cook BL. Psychotherapy and combined psychotherapy/pharmacotherapy for late-life depression. Biol Psychiatry. 2002;52(3):293-303.
6. Laidlaw K, Davidson K, Toner H, et al. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late-life depression. Int J Geriatr Psychiatry. 2008;23(8):843-850.
7. Floyd M, Scogin F, McKendree-Smith NL, et al. Cognitive therapy for depression: a comparison of individual psychotherapy and bibliotherapy for depressed older adults. Behavior Modification. 2004;28(2):297-318.
8. Serfaty MA, Haworth D, Blanchard M, et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009;66(12):1332-1340.
9. Pinquart M, Sörensen S. How effective are psychotherapeutic and other psychosocial interventions with older adults? A meta-analysis. J Ment Health Aging. 2001;7(2):207-243.
10. Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: a meta-analysis. Aging Ment Health. 2007;11(6):645-657.
11. Gallagher-Thompson D, Hanley-Peterson P, Thompson LW. Maintenance of gains versus relapse following brief psychotherapy for depression. J Consult Clin Psychol. 1990;58(3):371-374.
12. Thompson LW, Coon DW, Gallagher-Thompson D, et al. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. Am J Geriatr Psychiatry. 2001;9(3):225-240.
13. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry. 2011;168(10):1066-1074.
14. Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med. 2001;31(4):717-723.
15. Teri L, Logsdon RG, Uomoto J, et al. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52(4):P159-P166.
16. Nordhus IH, Pallesen S. Psychological treatment of late-life anxiety: an empirical review. J Consult Clin Psychol. 2003;71(4):643-651.
17. Gorenstein EE, Papp LA. Cognitive-behavioral therapy for anxiety in the elderly. Curr Psychiatry Rep. 2007;9(1):20-25.
18. Barrowclough C, King P, Colville J, et al. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol. 2001;69(5):756-762.
19. Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71(2):309-319.
20. Hendriks GJ, Oude Voshaar RC, Keijsers GP, et al. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2008;117(6):403-411.
21. Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71(1):31-40.
22. Dugas MJ, Brillon P, Savard P, et al. A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behav Ther. 2010;41(1):46-58.
23. Mohlman J, Gorenstein EE, Kleber M, et al. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry. 2003;11(1):24-32.
24. Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151(5):640-649.
25. McCurry SM, Logsdon RG, Teri L, et al. Evidence-based psychological treatments for insomnia in older adults. Psychol Aging. 2007;22(1):18-27.
26. Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851-2858.
27. Morgan K, Dixon S, Mathers N, et al. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess. 2004;8(8):iii iv, 1-68.
28. Nau SD, McCrae CS, Cook KG, et al. Treatment of insomnia in older adults. Clin Psychol Rev. 2005;25(5):645-672.
29. Rybarczyk B, Stepanski E, Fogg L, et al. A placebo-controlled test of cognitive-behavioral therapy for comorbid insomnia in older adults. J Consult Clin Psychol. 2005;73(6):1164-1174.
30. Laidlaw K, Thompson LW, Gallagher-Thompson D. Comprehensive conceptualization of cognitive behaviour therapy for late life depression. Behav Cogn Psychother. 2004;32(4):389-399.
31. Thompson LW. Cognitive-behavioral therapy and treatment for late-life depression. J Clin Psychiatry. 1996;57(suppl 5):29-37.
Some older patients with depression, anxiety, or insomnia may be reluctant to turn to pharmacotherapy and may prefer psychotherapeutic treatments.1 Evidence has established cognitive-behavioral therapy (CBT) as an effective intervention for several psychiatric disorders and CBT should be considered when treating geriatric patients (Table 1).2
Table 1
Indications for CBT
| Mild to moderate depression. In the case of severe depression, CBT can be combined with pharmacotherapy |
| Anxiety disorders, mixed anxiety states |
| Insomnia—both primary and comorbid with other medical and/or psychiatric conditions |
| CBT: cognitive-behavioral therapy |
Research evaluating the efficacy of CBT for depression in older adults was first published in the early 1980s. Since then, research and application of CBT with older adults has expanded to include other psychiatric disorders and researchers have suggested changes to increase the efficacy of CBT for these patients. This article provides:
- an overview of CBT’s efficacy for older adults with depression, anxiety, and insomnia
- modifications to employ when providing CBT to older patients.
The cognitive model of CBT
In the 1970s, Aaron T. Beck, MD, developed CBT while working with depressed patients. Beck’s patients reported thoughts characterized by inaccuracies and distortions in association with their depressed mood. He found these thoughts could be brought to the patient’s conscious attention and modified to improve the patient’s depression. This finding led to the development of CBT.
CBT is based on a cognitive model of the relationship among cognition, emotion, and behavior. Mood and behavior are viewed as determined by a person’s perception and interpretation of events, which manifest as a stream of automatically generated thoughts (Figure).3 These automatic thoughts have their origins in an underlying network of beliefs or schema. Patients with psychiatric disorders such as anxiety and depression typically have frequent automatic thoughts that characteristically lack validity because they arise from dysfunctional beliefs. The therapeutic process consists of helping the patient become aware of his or her internal stream of thoughts when distressed, and to identify and modify the dysfunctional thoughts. Behavioral techniques are used to bring about functional changes in behavior, regulate emotion, and help the cognitive restructuring process. Modifying the patient’s underlying dysfunctional beliefs leads to lasting improvements. In this structured therapy, the therapist and patient work collaboratively to use an approach that features reality testing and experimentation.4
Figure
The cognitive model of CBT
CBT: cognitive-behavioral therapy
Source: Adapted from reference 3
Indications for CBT in older adults
Depression. Among psychotherapies used in older adults, CBT has received the most research for late-life depression.5 Randomized controlled trials (RCTs) have found CBT is superior to treatment as usual in depressed adults age ≥60.6 It also has been found to be superior to wait-list control7 and talking as control.6,8 Meta-analyses have shown above-average effect sizes for CBT in treating late-life depression.9,10 A follow-up study found improvement was maintained up to 2 years after CBT, which suggests CBT’s impact is likely to be long lasting.11
Thompson et al12 compared 102 depressed patients age >60 who were treated with CBT alone, desipramine alone, or a combination of the 2. A combination of medication and CBT worked best for severely depressed patients; CBT alone or a combination of CBT and medication worked best for moderately depressed patients.
CBT is an option when treating depressed medically ill older adults. Research indicates that CBT could reduce depression in older patients with Parkinson’s disease13 and chronic obstructive pulmonary disease.14
As patients get older, cognitive impairment with comorbid depression can make treatment challenging. Limited research suggests CBT applied in a modified format that involves caregivers and uses problem solving and behavioral strategies can significantly reduce depression in patients with dementia.15
Anxiety. Researchers have examined the efficacy of variants of CBT in treating older adults with anxiety disorders—commonly, generalized anxiety disorder (GAD), panic disorder, agoraphobia, subjective anxiety, or a combination of these illnesses.16,17 Randomized trials have supported CBT’s efficacy for older patients with GAD and mixed anxiety states; gains made in CBT were maintained over a 1-year follow-up.18,19 In a meta-analysis of 15 studies using cognitive and behavioral methods of treating anxiety in older patients, Nordhus and Pallesen16 reported a significant effect size of 0.55. In a 2008 meta-analysis that included only RCTs, CBT was superior to wait-list conditions as well as active control conditions in treating anxious older patients.20
However, some research suggests that CBT for GAD may not be as effective for older adults as it is for younger adults. In a study of CBT for GAD in older adults, Stanley et al19 reported smaller effect sizes compared with CBT for younger adults. Researchers have found relatively few differences between CBT and comparison conditions—supportive psychotherapy or active control conditions—in treating GAD in older adults.21 Modified, more effective formats of CBT for GAD in older adults need to be established.22 Mohlman et al23 supplemented standard CBT for late-life GAD with memory and learning aids—weekly reading assignments, graphing exercises to chart mood ratings, reminder phone calls from therapists, and homework compliance requirement. This approach improved the response rate from 40% to 75%.23
Insomnia. Studies have found CBT to be an effective means of treating insomnia in geriatric patients. Although sleep problems occur more frequently among older patients, only 15% of chronic insomnia patients receive treatment; psychotherapy rarely is used.24 CBT for insomnia (CBT-I) should be considered for older adults because managing insomnia with medications may be problematic and these patients may prefer nonpharmacologic treatment.2 CBT-I typically incorporates cognitive strategies with established behavioral techniques, including sleep hygiene education, cognitive restructuring, relaxation training, stimulus control, and/or sleep restriction. The CBT-I multicomponent treatment package meets all criteria to be considered an evidence-based treatment for late-life insomnia.25
RCTs have reported significant improvements in late-life insomnia with CBT-I.26,27 Reviews and meta-analyses have also concluded that cognitive-behavioral treatments are effective for treating insomnia in older adults.25,28 Most insomnia cases in geriatric patients are reported to occur secondary to other medical or psychiatric conditions that are judged as causing the insomnia.25 In these cases, direct treatment of the insomnia usually is delayed or omitted.28 Studies evaluating the efficacy of CBT packages for treating insomnia occurring in conjunction with other medical or psychiatric illnesses have reported significant improvement of insomnia.28,29 Because insomnia frequently occurs in older patients with medical illnesses and psychiatric disorders, CBT-I could be beneficial for such patients.
Good candidates for CBT
Clinical experience indicates that older adults in relatively good health with no significant cognitive decline are good candidates for CBT. These patients tend to comply with their assignments, are interested in applying the learned strategies, and are motivated to read self-help books. CBT’s structured, goal-oriented approach makes it a short-term treatment, which makes it cost effective. Insomnia patients may improve after 6 to 8 CBT-I sessions and patients with anxiety or depression may need to undergo 15 to 20 CBT sessions. Patients age ≥65 have basic Medicare coverage that includes mental health care and psychotherapy.
There are no absolute contraindications for CBT, but the greater the cognitive impairment, the less the patient will benefit from CBT (Table 2). Similarly, severe depression and anxiety might make it difficult for patients to participate meaningfully, although CBT may be incorporated gradually as patients improve with medication. Severe medical illnesses and sensory losses such as visual and hearing loss would make it difficult to carry out CBT effectively.
Table 2
Contraindications for CBT
| High levels of cognitive impairment |
| Severe depression with psychotic features |
| Severe anxiety with high levels of agitation |
| Severe medical illness |
| Sensory losses |
| CBT: cognitive-behavioral therapy |
Adapting CBT for older patients
When using CBT with older patients, it is important to keep in mind characteristics that define the geriatric population. Laidlaw et al30 developed a model to help clinicians develop a more appropriate conceptualization of older patients that focuses on significant events and related cognitions associated with physical health, changes in role investments, and interactions with younger generations. It emphasizes the need to explore beliefs about aging viewed through each patient’s socio-cultural lens and examine cognitions in the context of the time period in which the individual has lived.
Losses and transitions. For many older patients, the latter years of life are characterized by losses and transitions.31 According to Thompson,31 these losses and transitions can trigger thoughts of missed opportunities or unresolved relationships and reflection on unachieved goals.31 CBT for older adults should focus on the meaning the patient gives to these losses and transitions. For example, depressed patients could view their retirement as a loss of self worth as they become less productive. CBT can help patients identify ways of thinking about the situation that will enable them to adapt to these losses and transitions.
Changes in cognition. Changes in cognitive functioning with aging are not universal and there’s considerable variability, but it’s important to make appropriate adaptations when needed. Patients may experience a decline in cognitive speed, working memory, selective attention, and fluid intelligence. This would require that information be presented slowly, with frequent repetitions and summaries. Also, it might be helpful to present information in alternate ways and to encourage patients to take notes during sessions. To accommodate for a decline in fluid intelligence, presenting new information in the context of previous experiences will help promote learning. Recordings of important information and conclusions from cognitive restructuring that patients can listen to between sessions could serve as helpful reminders that will help patients progress. Phone prompts or alarms can remind patients to carry out certain therapeutic measures, such as breathing exercises. Caretakers can attend sessions to become familiar with strategies performed during CBT and act as a co-therapist at home; however, their inclusion must be done with the consent of both parties and only if it’s viewed as necessary for the patient’s progress.
Additional strategies. For patients with substantial cognitive decline, cognitive restructuring might not be as effective as behavioral strategies—activity scheduling, graded task assignment, graded exposure, and rehearsals. Because older adults often have strengthened dysfunctional beliefs over a long time, modifying them takes longer, which is why the tapering process usually takes longer for older patients than for younger patients. The lengthier tapering ensures learning is well established and the process of modifying dysfunctional beliefs to functional beliefs continues. Collaborating with other professionals—physicians, social workers, and case managers—will help ensure a shared care process in which common goals are met.
The websites of the Academy of Cognitive Therapy, American Psychological Association, and Association for Behavioral and Cognitive Therapies can help clinicians who do not offer CBT to locate a qualified therapist for their patients (Related Resources).
- Academy of Cognitive Therapy. www.academyofct.org.
- American Psychological Association. www.apa.org.
- Association for Behavioral and Cognitive Therapies. www.abct.org.
- Laidlaw K, Thompson LW, Dick-Siskin L, et al. Cognitive behaviour therapy with older people. West Sussex, England: John Wiley & Sons, Ltd; 2003.
Drug Brand Name
- Desipramine • Norpramin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Some older patients with depression, anxiety, or insomnia may be reluctant to turn to pharmacotherapy and may prefer psychotherapeutic treatments.1 Evidence has established cognitive-behavioral therapy (CBT) as an effective intervention for several psychiatric disorders and CBT should be considered when treating geriatric patients (Table 1).2
Table 1
Indications for CBT
| Mild to moderate depression. In the case of severe depression, CBT can be combined with pharmacotherapy |
| Anxiety disorders, mixed anxiety states |
| Insomnia—both primary and comorbid with other medical and/or psychiatric conditions |
| CBT: cognitive-behavioral therapy |
Research evaluating the efficacy of CBT for depression in older adults was first published in the early 1980s. Since then, research and application of CBT with older adults has expanded to include other psychiatric disorders and researchers have suggested changes to increase the efficacy of CBT for these patients. This article provides:
- an overview of CBT’s efficacy for older adults with depression, anxiety, and insomnia
- modifications to employ when providing CBT to older patients.
The cognitive model of CBT
In the 1970s, Aaron T. Beck, MD, developed CBT while working with depressed patients. Beck’s patients reported thoughts characterized by inaccuracies and distortions in association with their depressed mood. He found these thoughts could be brought to the patient’s conscious attention and modified to improve the patient’s depression. This finding led to the development of CBT.
CBT is based on a cognitive model of the relationship among cognition, emotion, and behavior. Mood and behavior are viewed as determined by a person’s perception and interpretation of events, which manifest as a stream of automatically generated thoughts (Figure).3 These automatic thoughts have their origins in an underlying network of beliefs or schema. Patients with psychiatric disorders such as anxiety and depression typically have frequent automatic thoughts that characteristically lack validity because they arise from dysfunctional beliefs. The therapeutic process consists of helping the patient become aware of his or her internal stream of thoughts when distressed, and to identify and modify the dysfunctional thoughts. Behavioral techniques are used to bring about functional changes in behavior, regulate emotion, and help the cognitive restructuring process. Modifying the patient’s underlying dysfunctional beliefs leads to lasting improvements. In this structured therapy, the therapist and patient work collaboratively to use an approach that features reality testing and experimentation.4
Figure
The cognitive model of CBT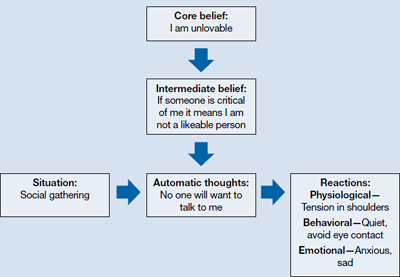
CBT: cognitive-behavioral therapy
Source: Adapted from reference 3
Indications for CBT in older adults
Depression. Among psychotherapies used in older adults, CBT has received the most research for late-life depression.5 Randomized controlled trials (RCTs) have found CBT is superior to treatment as usual in depressed adults age ≥60.6 It also has been found to be superior to wait-list control7 and talking as control.6,8 Meta-analyses have shown above-average effect sizes for CBT in treating late-life depression.9,10 A follow-up study found improvement was maintained up to 2 years after CBT, which suggests CBT’s impact is likely to be long lasting.11
Thompson et al12 compared 102 depressed patients age >60 who were treated with CBT alone, desipramine alone, or a combination of the 2. A combination of medication and CBT worked best for severely depressed patients; CBT alone or a combination of CBT and medication worked best for moderately depressed patients.
CBT is an option when treating depressed medically ill older adults. Research indicates that CBT could reduce depression in older patients with Parkinson’s disease13 and chronic obstructive pulmonary disease.14
As patients get older, cognitive impairment with comorbid depression can make treatment challenging. Limited research suggests CBT applied in a modified format that involves caregivers and uses problem solving and behavioral strategies can significantly reduce depression in patients with dementia.15
Anxiety. Researchers have examined the efficacy of variants of CBT in treating older adults with anxiety disorders—commonly, generalized anxiety disorder (GAD), panic disorder, agoraphobia, subjective anxiety, or a combination of these illnesses.16,17 Randomized trials have supported CBT’s efficacy for older patients with GAD and mixed anxiety states; gains made in CBT were maintained over a 1-year follow-up.18,19 In a meta-analysis of 15 studies using cognitive and behavioral methods of treating anxiety in older patients, Nordhus and Pallesen16 reported a significant effect size of 0.55. In a 2008 meta-analysis that included only RCTs, CBT was superior to wait-list conditions as well as active control conditions in treating anxious older patients.20
However, some research suggests that CBT for GAD may not be as effective for older adults as it is for younger adults. In a study of CBT for GAD in older adults, Stanley et al19 reported smaller effect sizes compared with CBT for younger adults. Researchers have found relatively few differences between CBT and comparison conditions—supportive psychotherapy or active control conditions—in treating GAD in older adults.21 Modified, more effective formats of CBT for GAD in older adults need to be established.22 Mohlman et al23 supplemented standard CBT for late-life GAD with memory and learning aids—weekly reading assignments, graphing exercises to chart mood ratings, reminder phone calls from therapists, and homework compliance requirement. This approach improved the response rate from 40% to 75%.23
Insomnia. Studies have found CBT to be an effective means of treating insomnia in geriatric patients. Although sleep problems occur more frequently among older patients, only 15% of chronic insomnia patients receive treatment; psychotherapy rarely is used.24 CBT for insomnia (CBT-I) should be considered for older adults because managing insomnia with medications may be problematic and these patients may prefer nonpharmacologic treatment.2 CBT-I typically incorporates cognitive strategies with established behavioral techniques, including sleep hygiene education, cognitive restructuring, relaxation training, stimulus control, and/or sleep restriction. The CBT-I multicomponent treatment package meets all criteria to be considered an evidence-based treatment for late-life insomnia.25
RCTs have reported significant improvements in late-life insomnia with CBT-I.26,27 Reviews and meta-analyses have also concluded that cognitive-behavioral treatments are effective for treating insomnia in older adults.25,28 Most insomnia cases in geriatric patients are reported to occur secondary to other medical or psychiatric conditions that are judged as causing the insomnia.25 In these cases, direct treatment of the insomnia usually is delayed or omitted.28 Studies evaluating the efficacy of CBT packages for treating insomnia occurring in conjunction with other medical or psychiatric illnesses have reported significant improvement of insomnia.28,29 Because insomnia frequently occurs in older patients with medical illnesses and psychiatric disorders, CBT-I could be beneficial for such patients.
Good candidates for CBT
Clinical experience indicates that older adults in relatively good health with no significant cognitive decline are good candidates for CBT. These patients tend to comply with their assignments, are interested in applying the learned strategies, and are motivated to read self-help books. CBT’s structured, goal-oriented approach makes it a short-term treatment, which makes it cost effective. Insomnia patients may improve after 6 to 8 CBT-I sessions and patients with anxiety or depression may need to undergo 15 to 20 CBT sessions. Patients age ≥65 have basic Medicare coverage that includes mental health care and psychotherapy.
There are no absolute contraindications for CBT, but the greater the cognitive impairment, the less the patient will benefit from CBT (Table 2). Similarly, severe depression and anxiety might make it difficult for patients to participate meaningfully, although CBT may be incorporated gradually as patients improve with medication. Severe medical illnesses and sensory losses such as visual and hearing loss would make it difficult to carry out CBT effectively.
Table 2
Contraindications for CBT
| High levels of cognitive impairment |
| Severe depression with psychotic features |
| Severe anxiety with high levels of agitation |
| Severe medical illness |
| Sensory losses |
| CBT: cognitive-behavioral therapy |
Adapting CBT for older patients
When using CBT with older patients, it is important to keep in mind characteristics that define the geriatric population. Laidlaw et al30 developed a model to help clinicians develop a more appropriate conceptualization of older patients that focuses on significant events and related cognitions associated with physical health, changes in role investments, and interactions with younger generations. It emphasizes the need to explore beliefs about aging viewed through each patient’s socio-cultural lens and examine cognitions in the context of the time period in which the individual has lived.
Losses and transitions. For many older patients, the latter years of life are characterized by losses and transitions.31 According to Thompson,31 these losses and transitions can trigger thoughts of missed opportunities or unresolved relationships and reflection on unachieved goals.31 CBT for older adults should focus on the meaning the patient gives to these losses and transitions. For example, depressed patients could view their retirement as a loss of self worth as they become less productive. CBT can help patients identify ways of thinking about the situation that will enable them to adapt to these losses and transitions.
Changes in cognition. Changes in cognitive functioning with aging are not universal and there’s considerable variability, but it’s important to make appropriate adaptations when needed. Patients may experience a decline in cognitive speed, working memory, selective attention, and fluid intelligence. This would require that information be presented slowly, with frequent repetitions and summaries. Also, it might be helpful to present information in alternate ways and to encourage patients to take notes during sessions. To accommodate for a decline in fluid intelligence, presenting new information in the context of previous experiences will help promote learning. Recordings of important information and conclusions from cognitive restructuring that patients can listen to between sessions could serve as helpful reminders that will help patients progress. Phone prompts or alarms can remind patients to carry out certain therapeutic measures, such as breathing exercises. Caretakers can attend sessions to become familiar with strategies performed during CBT and act as a co-therapist at home; however, their inclusion must be done with the consent of both parties and only if it’s viewed as necessary for the patient’s progress.
Additional strategies. For patients with substantial cognitive decline, cognitive restructuring might not be as effective as behavioral strategies—activity scheduling, graded task assignment, graded exposure, and rehearsals. Because older adults often have strengthened dysfunctional beliefs over a long time, modifying them takes longer, which is why the tapering process usually takes longer for older patients than for younger patients. The lengthier tapering ensures learning is well established and the process of modifying dysfunctional beliefs to functional beliefs continues. Collaborating with other professionals—physicians, social workers, and case managers—will help ensure a shared care process in which common goals are met.
The websites of the Academy of Cognitive Therapy, American Psychological Association, and Association for Behavioral and Cognitive Therapies can help clinicians who do not offer CBT to locate a qualified therapist for their patients (Related Resources).
- Academy of Cognitive Therapy. www.academyofct.org.
- American Psychological Association. www.apa.org.
- Association for Behavioral and Cognitive Therapies. www.abct.org.
- Laidlaw K, Thompson LW, Dick-Siskin L, et al. Cognitive behaviour therapy with older people. West Sussex, England: John Wiley & Sons, Ltd; 2003.
Drug Brand Name
- Desipramine • Norpramin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Landreville P, Landry J, Baillargeon L, et al. Older adults’ acceptance of psychological and pharmacological treatments for depression. J Gerontol B Psychol Sci Soc Sci. 2001;56(5):P285-P291.
2. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
3. Beck JS. Cognitive conceptualization. In: Cognitive therapy: basics and beyond. 2nd ed. New York NY: The Guilford Press; 2011:29–45.
4. Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York, NY: The Guilford Press; 1979.
5. Areán PA, Cook BL. Psychotherapy and combined psychotherapy/pharmacotherapy for late-life depression. Biol Psychiatry. 2002;52(3):293-303.
6. Laidlaw K, Davidson K, Toner H, et al. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late-life depression. Int J Geriatr Psychiatry. 2008;23(8):843-850.
7. Floyd M, Scogin F, McKendree-Smith NL, et al. Cognitive therapy for depression: a comparison of individual psychotherapy and bibliotherapy for depressed older adults. Behavior Modification. 2004;28(2):297-318.
8. Serfaty MA, Haworth D, Blanchard M, et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009;66(12):1332-1340.
9. Pinquart M, Sörensen S. How effective are psychotherapeutic and other psychosocial interventions with older adults? A meta-analysis. J Ment Health Aging. 2001;7(2):207-243.
10. Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: a meta-analysis. Aging Ment Health. 2007;11(6):645-657.
11. Gallagher-Thompson D, Hanley-Peterson P, Thompson LW. Maintenance of gains versus relapse following brief psychotherapy for depression. J Consult Clin Psychol. 1990;58(3):371-374.
12. Thompson LW, Coon DW, Gallagher-Thompson D, et al. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. Am J Geriatr Psychiatry. 2001;9(3):225-240.
13. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry. 2011;168(10):1066-1074.
14. Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med. 2001;31(4):717-723.
15. Teri L, Logsdon RG, Uomoto J, et al. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52(4):P159-P166.
16. Nordhus IH, Pallesen S. Psychological treatment of late-life anxiety: an empirical review. J Consult Clin Psychol. 2003;71(4):643-651.
17. Gorenstein EE, Papp LA. Cognitive-behavioral therapy for anxiety in the elderly. Curr Psychiatry Rep. 2007;9(1):20-25.
18. Barrowclough C, King P, Colville J, et al. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol. 2001;69(5):756-762.
19. Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71(2):309-319.
20. Hendriks GJ, Oude Voshaar RC, Keijsers GP, et al. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2008;117(6):403-411.
21. Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71(1):31-40.
22. Dugas MJ, Brillon P, Savard P, et al. A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behav Ther. 2010;41(1):46-58.
23. Mohlman J, Gorenstein EE, Kleber M, et al. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry. 2003;11(1):24-32.
24. Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151(5):640-649.
25. McCurry SM, Logsdon RG, Teri L, et al. Evidence-based psychological treatments for insomnia in older adults. Psychol Aging. 2007;22(1):18-27.
26. Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851-2858.
27. Morgan K, Dixon S, Mathers N, et al. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess. 2004;8(8):iii iv, 1-68.
28. Nau SD, McCrae CS, Cook KG, et al. Treatment of insomnia in older adults. Clin Psychol Rev. 2005;25(5):645-672.
29. Rybarczyk B, Stepanski E, Fogg L, et al. A placebo-controlled test of cognitive-behavioral therapy for comorbid insomnia in older adults. J Consult Clin Psychol. 2005;73(6):1164-1174.
30. Laidlaw K, Thompson LW, Gallagher-Thompson D. Comprehensive conceptualization of cognitive behaviour therapy for late life depression. Behav Cogn Psychother. 2004;32(4):389-399.
31. Thompson LW. Cognitive-behavioral therapy and treatment for late-life depression. J Clin Psychiatry. 1996;57(suppl 5):29-37.
1. Landreville P, Landry J, Baillargeon L, et al. Older adults’ acceptance of psychological and pharmacological treatments for depression. J Gerontol B Psychol Sci Soc Sci. 2001;56(5):P285-P291.
2. Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685-716.
3. Beck JS. Cognitive conceptualization. In: Cognitive therapy: basics and beyond. 2nd ed. New York NY: The Guilford Press; 2011:29–45.
4. Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York, NY: The Guilford Press; 1979.
5. Areán PA, Cook BL. Psychotherapy and combined psychotherapy/pharmacotherapy for late-life depression. Biol Psychiatry. 2002;52(3):293-303.
6. Laidlaw K, Davidson K, Toner H, et al. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late-life depression. Int J Geriatr Psychiatry. 2008;23(8):843-850.
7. Floyd M, Scogin F, McKendree-Smith NL, et al. Cognitive therapy for depression: a comparison of individual psychotherapy and bibliotherapy for depressed older adults. Behavior Modification. 2004;28(2):297-318.
8. Serfaty MA, Haworth D, Blanchard M, et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009;66(12):1332-1340.
9. Pinquart M, Sörensen S. How effective are psychotherapeutic and other psychosocial interventions with older adults? A meta-analysis. J Ment Health Aging. 2001;7(2):207-243.
10. Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: a meta-analysis. Aging Ment Health. 2007;11(6):645-657.
11. Gallagher-Thompson D, Hanley-Peterson P, Thompson LW. Maintenance of gains versus relapse following brief psychotherapy for depression. J Consult Clin Psychol. 1990;58(3):371-374.
12. Thompson LW, Coon DW, Gallagher-Thompson D, et al. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. Am J Geriatr Psychiatry. 2001;9(3):225-240.
13. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry. 2011;168(10):1066-1074.
14. Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med. 2001;31(4):717-723.
15. Teri L, Logsdon RG, Uomoto J, et al. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52(4):P159-P166.
16. Nordhus IH, Pallesen S. Psychological treatment of late-life anxiety: an empirical review. J Consult Clin Psychol. 2003;71(4):643-651.
17. Gorenstein EE, Papp LA. Cognitive-behavioral therapy for anxiety in the elderly. Curr Psychiatry Rep. 2007;9(1):20-25.
18. Barrowclough C, King P, Colville J, et al. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol. 2001;69(5):756-762.
19. Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71(2):309-319.
20. Hendriks GJ, Oude Voshaar RC, Keijsers GP, et al. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2008;117(6):403-411.
21. Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71(1):31-40.
22. Dugas MJ, Brillon P, Savard P, et al. A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behav Ther. 2010;41(1):46-58.
23. Mohlman J, Gorenstein EE, Kleber M, et al. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry. 2003;11(1):24-32.
24. Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151(5):640-649.
25. McCurry SM, Logsdon RG, Teri L, et al. Evidence-based psychological treatments for insomnia in older adults. Psychol Aging. 2007;22(1):18-27.
26. Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851-2858.
27. Morgan K, Dixon S, Mathers N, et al. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess. 2004;8(8):iii iv, 1-68.
28. Nau SD, McCrae CS, Cook KG, et al. Treatment of insomnia in older adults. Clin Psychol Rev. 2005;25(5):645-672.
29. Rybarczyk B, Stepanski E, Fogg L, et al. A placebo-controlled test of cognitive-behavioral therapy for comorbid insomnia in older adults. J Consult Clin Psychol. 2005;73(6):1164-1174.
30. Laidlaw K, Thompson LW, Gallagher-Thompson D. Comprehensive conceptualization of cognitive behaviour therapy for late life depression. Behav Cogn Psychother. 2004;32(4):389-399.
31. Thompson LW. Cognitive-behavioral therapy and treatment for late-life depression. J Clin Psychiatry. 1996;57(suppl 5):29-37.
