User login
Sharon Worcester is an award-winning medical journalist for MDedge News. She has been with the company since 1996, first as the Southeast Bureau Chief (1996-2009) when the company was known as International Medical News Group, then as a freelance writer (2010-2015) before returning as a reporter in 2015. She previously worked as a daily newspaper reporter covering health and local government. Sharon currently reports primarily on oncology and hematology. She has a BA from Eckerd College and an MA in Mass Communication/Print Journalism from the University of Florida. Connect with her via LinkedIn and follow her on twitter @SW_MedReporter.
Precision medicine in rheumatology: Enormous opportunity exists
Advances in precision medicine present enormous opportunity for rheumatology, but optimizing its benefits requires more input from the specialty and a sharper focus on related training for rheumatologists, according to Judith A. James, MD, PhD.
Precision medicine is getting a great deal of attention and is an exciting area, but it is already widely used in the field; think treat-to-target in rheumatoid arthritis, autoantibody testing for patient stratification across various conditions, and individual monitoring and dose escalation to achieve optimal uric acid levels in gout patients, Dr. James, professor of medicine and associate vice provost of clinical and translational science at the University of Oklahoma, Oklahoma City, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“We have historically ... actually had the highest number of FDA approved biomarker tests in rheumatology compared to all other specialties until this last couple of years where we’re starting to see this explosion of genetic testing in oncology – and we’ve been doing genetic testing,” she said.
However, there is a great deal more work to be done.
“We still have a long way to go to go to get the right drug at the right dose at the right time in the right patient in order to optimize outcomes in all of these diseases that we are responsible for as rheumatologists,” she said.
The fields of oncology and hematology have been intensely focused on precision medicine – the development of unique therapies based on specific genetic abnormalities in an individual’s tumor – and this focus is apparent in practice patterns: A recent survey of 132 medical oncologists and hematologists/oncologists showed that nearly 90% had ordered DNA sequencing, about 65% do so monthly, and 25% do so weekly.
“Those numbers are just going to continue to climb, and I think will see this in other disciplines as well,” she said.
The possibilities for improved outcomes in rheumatologic conditions using tailored treatments based on individual characteristics are practically limitless, she said, noting the heterogeneity of many rheumatologic conditions.
This is particularly true for systemic lupus erythematosus (SLE) patients, she said.
Identifying patient subsets based on organ involvement, demographics, and biomarkers, for example, could lead to personalized treatments with different doses, routes of administration, and concurrent medications, she explained.
Genetics in SLE
Dr. James highlighted the role of genetics and the value of precision medicine in the SLE setting in a large transancestral association study published in 2017. The investigators analyzed Immunochip genotype data from 27,574 SLE cases and controls and identified 58 distinct non–human leukocyte antigen (HLA) regions in Americans with European ancestry, 9 in those with African ancestry, and 16 in those with Hispanic ancestry. The investigators found that these non-HLA regions included 24 novel to SLE, and in their analysis the researchers were able to refine association signals in previously established regions, extend associations to additional ancestries, and reveal a complex multigenic effect just outside of the HLA region (Nature Commun. 2017;8:16021).
The findings led to a “cumulative hit hypothesis” for autoimmune disease, and help to clarify genetic architecture and ethnic disparities in SLE, they concluded.
“So we now have over a hundred genetic regions that have been associated with lupus, compared to healthy controls,” Dr. James said.
A frustration with genetic data such as these, however, is the challenge of “getting it into the clinic,” she noted.
“I think that looking at individual [single nuclear polymorphisms] is probably not what we’re going to be doing, but we’re seeing a lot of interest in the idea of genetic load,” she said, explaining that it may soon be possible to use genetic load information to evaluate patient risk.
A recent study at her institution looked at lupus risk from another angle: She and her colleagues recontacted family members from Oklahoma Lupus Genetics studies to look more closely at which blood relatives of SLE patients transitioned to SLE, and what factors were associated with that transition when compared with relatives who remained unaffected (Arthritis Rheumatol. 2017;69[3]:630-42).
Among the findings was a higher risk of transitioning among family members with both a positive antinuclear antibody test and a baseline Connective Tissue Disease Screening Questionnaire score indicative of connective tissue disease.
“We also found, of course, biomarkers, or blood markers, that helped us identify the individuals who were at the highest risk of transitioning, so we think a blood test might really be helpful,” she said.
That study also suggested that there may be ways to intervene in SLE patients’ relatives at increased risk for also developing lupus. For example, those who transitioned had increased levels of soluble tumor necrosis factor receptors and the interferon-driven chemokine MCP-3; a prevention trial is now underway, she noted.
Beyond genetics
Genetics are just one piece of the precision medicine puzzle, and other areas of investigation that may help to divide patients into subgroups for more precise treatment include genomics, soluble mediators, and immunophenotyping, Dr. James said.
“It may be that we need different pieces of all of these things to help guide our treatment in lupus patients,” she said.
Longitudinal clinical and blood transcriptional profiling of patients in the Dallas Pediatric SLE cohort, for example, identified a molecular classification system for SLE patients. The analysis of 972 samples from 158 SLE patients and 48 healthy controls, which were collected for up to 4 years, showed that an interferon response signature was present in 784 of the samples.
The investigators found that a plasmablast signature, which is found more in African-American patients than in other populations, best correlates with disease activity and that a neutrophil-related signature is associated with progression to active lupus nephritis (Cell. 2016;165[3]:551-65).
“This is something that will potentially be helpful [in the clinic], and we need to test this in the adult population,” Dr. James said.
The investigators also were able to stratify patients, based on individual immunoprofiling, into seven major groups based on molecular correlates. They concluded that such stratification could help improve the outcomes of clinical trials in SLE.
In another study, researchers looked at longitudinal gene expression in SLE patients by stratifying each of two independent sets of patients (a pediatric cohort and an adult cohort) into three clinically differentiated disease clusters defined by mechanisms of disease progression (Arthritis Rheumatol. Dec 2018;70[12]:2025-35).
The clusters included one showing a correlation between the percentage of neutrophils and disease activity progression, one showing a correlation between the percentage of lymphocytes and disease activity progression, and a third for which the percentage of neutrophils correlated to a lesser degree with disease activity but was functionally more heterogeneous. Patients in the two neutrophil‐driven clusters had an increased risk of developing proliferative nephritis.
The results have implications for treatment, trial design, and understanding of disease etiology, the investigators concluded.
“This may help us in the future as we think about which medicine to start patients on, and which medicines to start patients on first,” Dr. James said.
It is clear that precision medicine will play an increasingly important role in rheumatology, Dr. James said, when considering the context of other findings in recent years, such as those from studies looking at soluble mediators of inflammation associated with disease flare, as well as those that involved extensive immunophenotyping and showed widely divergent transcriptional patterns based on ancestral backgrounds. Other research, such as the BOLD (Biomarkers of Lupus Disease) study, looked at various mechanisms of disease flare.
Numerous types of personalized therapies are being considered in rheumatology, ranging from expanded regulatory T cells to chimeric antigen receptor T cell therapy to risk profiling for disease prevention, just to name a few. Going forward it will be important to perform more systems biology analyses to assemble precision medicine–related data that can inform clinical diagnosis, prognosis, and therapy selection and optimization, she said.
The future of personalized therapies in rheumatology will require more input from rheumatologists on large-scale precision medicine projects such as the National Institutes of Health’s All of Us Research Project and the Million Veteran Program, as well as other similar programs of major health systems, she noted, adding that different types of training and interaction with molecular pathologists, genetic counselors, health coaches, and other key players also are needed.
Dr. James reported having no relevant disclosures.
Advances in precision medicine present enormous opportunity for rheumatology, but optimizing its benefits requires more input from the specialty and a sharper focus on related training for rheumatologists, according to Judith A. James, MD, PhD.
Precision medicine is getting a great deal of attention and is an exciting area, but it is already widely used in the field; think treat-to-target in rheumatoid arthritis, autoantibody testing for patient stratification across various conditions, and individual monitoring and dose escalation to achieve optimal uric acid levels in gout patients, Dr. James, professor of medicine and associate vice provost of clinical and translational science at the University of Oklahoma, Oklahoma City, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“We have historically ... actually had the highest number of FDA approved biomarker tests in rheumatology compared to all other specialties until this last couple of years where we’re starting to see this explosion of genetic testing in oncology – and we’ve been doing genetic testing,” she said.
However, there is a great deal more work to be done.
“We still have a long way to go to go to get the right drug at the right dose at the right time in the right patient in order to optimize outcomes in all of these diseases that we are responsible for as rheumatologists,” she said.
The fields of oncology and hematology have been intensely focused on precision medicine – the development of unique therapies based on specific genetic abnormalities in an individual’s tumor – and this focus is apparent in practice patterns: A recent survey of 132 medical oncologists and hematologists/oncologists showed that nearly 90% had ordered DNA sequencing, about 65% do so monthly, and 25% do so weekly.
“Those numbers are just going to continue to climb, and I think will see this in other disciplines as well,” she said.
The possibilities for improved outcomes in rheumatologic conditions using tailored treatments based on individual characteristics are practically limitless, she said, noting the heterogeneity of many rheumatologic conditions.
This is particularly true for systemic lupus erythematosus (SLE) patients, she said.
Identifying patient subsets based on organ involvement, demographics, and biomarkers, for example, could lead to personalized treatments with different doses, routes of administration, and concurrent medications, she explained.
Genetics in SLE
Dr. James highlighted the role of genetics and the value of precision medicine in the SLE setting in a large transancestral association study published in 2017. The investigators analyzed Immunochip genotype data from 27,574 SLE cases and controls and identified 58 distinct non–human leukocyte antigen (HLA) regions in Americans with European ancestry, 9 in those with African ancestry, and 16 in those with Hispanic ancestry. The investigators found that these non-HLA regions included 24 novel to SLE, and in their analysis the researchers were able to refine association signals in previously established regions, extend associations to additional ancestries, and reveal a complex multigenic effect just outside of the HLA region (Nature Commun. 2017;8:16021).
The findings led to a “cumulative hit hypothesis” for autoimmune disease, and help to clarify genetic architecture and ethnic disparities in SLE, they concluded.
“So we now have over a hundred genetic regions that have been associated with lupus, compared to healthy controls,” Dr. James said.
A frustration with genetic data such as these, however, is the challenge of “getting it into the clinic,” she noted.
“I think that looking at individual [single nuclear polymorphisms] is probably not what we’re going to be doing, but we’re seeing a lot of interest in the idea of genetic load,” she said, explaining that it may soon be possible to use genetic load information to evaluate patient risk.
A recent study at her institution looked at lupus risk from another angle: She and her colleagues recontacted family members from Oklahoma Lupus Genetics studies to look more closely at which blood relatives of SLE patients transitioned to SLE, and what factors were associated with that transition when compared with relatives who remained unaffected (Arthritis Rheumatol. 2017;69[3]:630-42).
Among the findings was a higher risk of transitioning among family members with both a positive antinuclear antibody test and a baseline Connective Tissue Disease Screening Questionnaire score indicative of connective tissue disease.
“We also found, of course, biomarkers, or blood markers, that helped us identify the individuals who were at the highest risk of transitioning, so we think a blood test might really be helpful,” she said.
That study also suggested that there may be ways to intervene in SLE patients’ relatives at increased risk for also developing lupus. For example, those who transitioned had increased levels of soluble tumor necrosis factor receptors and the interferon-driven chemokine MCP-3; a prevention trial is now underway, she noted.
Beyond genetics
Genetics are just one piece of the precision medicine puzzle, and other areas of investigation that may help to divide patients into subgroups for more precise treatment include genomics, soluble mediators, and immunophenotyping, Dr. James said.
“It may be that we need different pieces of all of these things to help guide our treatment in lupus patients,” she said.
Longitudinal clinical and blood transcriptional profiling of patients in the Dallas Pediatric SLE cohort, for example, identified a molecular classification system for SLE patients. The analysis of 972 samples from 158 SLE patients and 48 healthy controls, which were collected for up to 4 years, showed that an interferon response signature was present in 784 of the samples.
The investigators found that a plasmablast signature, which is found more in African-American patients than in other populations, best correlates with disease activity and that a neutrophil-related signature is associated with progression to active lupus nephritis (Cell. 2016;165[3]:551-65).
“This is something that will potentially be helpful [in the clinic], and we need to test this in the adult population,” Dr. James said.
The investigators also were able to stratify patients, based on individual immunoprofiling, into seven major groups based on molecular correlates. They concluded that such stratification could help improve the outcomes of clinical trials in SLE.
In another study, researchers looked at longitudinal gene expression in SLE patients by stratifying each of two independent sets of patients (a pediatric cohort and an adult cohort) into three clinically differentiated disease clusters defined by mechanisms of disease progression (Arthritis Rheumatol. Dec 2018;70[12]:2025-35).
The clusters included one showing a correlation between the percentage of neutrophils and disease activity progression, one showing a correlation between the percentage of lymphocytes and disease activity progression, and a third for which the percentage of neutrophils correlated to a lesser degree with disease activity but was functionally more heterogeneous. Patients in the two neutrophil‐driven clusters had an increased risk of developing proliferative nephritis.
The results have implications for treatment, trial design, and understanding of disease etiology, the investigators concluded.
“This may help us in the future as we think about which medicine to start patients on, and which medicines to start patients on first,” Dr. James said.
It is clear that precision medicine will play an increasingly important role in rheumatology, Dr. James said, when considering the context of other findings in recent years, such as those from studies looking at soluble mediators of inflammation associated with disease flare, as well as those that involved extensive immunophenotyping and showed widely divergent transcriptional patterns based on ancestral backgrounds. Other research, such as the BOLD (Biomarkers of Lupus Disease) study, looked at various mechanisms of disease flare.
Numerous types of personalized therapies are being considered in rheumatology, ranging from expanded regulatory T cells to chimeric antigen receptor T cell therapy to risk profiling for disease prevention, just to name a few. Going forward it will be important to perform more systems biology analyses to assemble precision medicine–related data that can inform clinical diagnosis, prognosis, and therapy selection and optimization, she said.
The future of personalized therapies in rheumatology will require more input from rheumatologists on large-scale precision medicine projects such as the National Institutes of Health’s All of Us Research Project and the Million Veteran Program, as well as other similar programs of major health systems, she noted, adding that different types of training and interaction with molecular pathologists, genetic counselors, health coaches, and other key players also are needed.
Dr. James reported having no relevant disclosures.
Advances in precision medicine present enormous opportunity for rheumatology, but optimizing its benefits requires more input from the specialty and a sharper focus on related training for rheumatologists, according to Judith A. James, MD, PhD.
Precision medicine is getting a great deal of attention and is an exciting area, but it is already widely used in the field; think treat-to-target in rheumatoid arthritis, autoantibody testing for patient stratification across various conditions, and individual monitoring and dose escalation to achieve optimal uric acid levels in gout patients, Dr. James, professor of medicine and associate vice provost of clinical and translational science at the University of Oklahoma, Oklahoma City, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“We have historically ... actually had the highest number of FDA approved biomarker tests in rheumatology compared to all other specialties until this last couple of years where we’re starting to see this explosion of genetic testing in oncology – and we’ve been doing genetic testing,” she said.
However, there is a great deal more work to be done.
“We still have a long way to go to go to get the right drug at the right dose at the right time in the right patient in order to optimize outcomes in all of these diseases that we are responsible for as rheumatologists,” she said.
The fields of oncology and hematology have been intensely focused on precision medicine – the development of unique therapies based on specific genetic abnormalities in an individual’s tumor – and this focus is apparent in practice patterns: A recent survey of 132 medical oncologists and hematologists/oncologists showed that nearly 90% had ordered DNA sequencing, about 65% do so monthly, and 25% do so weekly.
“Those numbers are just going to continue to climb, and I think will see this in other disciplines as well,” she said.
The possibilities for improved outcomes in rheumatologic conditions using tailored treatments based on individual characteristics are practically limitless, she said, noting the heterogeneity of many rheumatologic conditions.
This is particularly true for systemic lupus erythematosus (SLE) patients, she said.
Identifying patient subsets based on organ involvement, demographics, and biomarkers, for example, could lead to personalized treatments with different doses, routes of administration, and concurrent medications, she explained.
Genetics in SLE
Dr. James highlighted the role of genetics and the value of precision medicine in the SLE setting in a large transancestral association study published in 2017. The investigators analyzed Immunochip genotype data from 27,574 SLE cases and controls and identified 58 distinct non–human leukocyte antigen (HLA) regions in Americans with European ancestry, 9 in those with African ancestry, and 16 in those with Hispanic ancestry. The investigators found that these non-HLA regions included 24 novel to SLE, and in their analysis the researchers were able to refine association signals in previously established regions, extend associations to additional ancestries, and reveal a complex multigenic effect just outside of the HLA region (Nature Commun. 2017;8:16021).
The findings led to a “cumulative hit hypothesis” for autoimmune disease, and help to clarify genetic architecture and ethnic disparities in SLE, they concluded.
“So we now have over a hundred genetic regions that have been associated with lupus, compared to healthy controls,” Dr. James said.
A frustration with genetic data such as these, however, is the challenge of “getting it into the clinic,” she noted.
“I think that looking at individual [single nuclear polymorphisms] is probably not what we’re going to be doing, but we’re seeing a lot of interest in the idea of genetic load,” she said, explaining that it may soon be possible to use genetic load information to evaluate patient risk.
A recent study at her institution looked at lupus risk from another angle: She and her colleagues recontacted family members from Oklahoma Lupus Genetics studies to look more closely at which blood relatives of SLE patients transitioned to SLE, and what factors were associated with that transition when compared with relatives who remained unaffected (Arthritis Rheumatol. 2017;69[3]:630-42).
Among the findings was a higher risk of transitioning among family members with both a positive antinuclear antibody test and a baseline Connective Tissue Disease Screening Questionnaire score indicative of connective tissue disease.
“We also found, of course, biomarkers, or blood markers, that helped us identify the individuals who were at the highest risk of transitioning, so we think a blood test might really be helpful,” she said.
That study also suggested that there may be ways to intervene in SLE patients’ relatives at increased risk for also developing lupus. For example, those who transitioned had increased levels of soluble tumor necrosis factor receptors and the interferon-driven chemokine MCP-3; a prevention trial is now underway, she noted.
Beyond genetics
Genetics are just one piece of the precision medicine puzzle, and other areas of investigation that may help to divide patients into subgroups for more precise treatment include genomics, soluble mediators, and immunophenotyping, Dr. James said.
“It may be that we need different pieces of all of these things to help guide our treatment in lupus patients,” she said.
Longitudinal clinical and blood transcriptional profiling of patients in the Dallas Pediatric SLE cohort, for example, identified a molecular classification system for SLE patients. The analysis of 972 samples from 158 SLE patients and 48 healthy controls, which were collected for up to 4 years, showed that an interferon response signature was present in 784 of the samples.
The investigators found that a plasmablast signature, which is found more in African-American patients than in other populations, best correlates with disease activity and that a neutrophil-related signature is associated with progression to active lupus nephritis (Cell. 2016;165[3]:551-65).
“This is something that will potentially be helpful [in the clinic], and we need to test this in the adult population,” Dr. James said.
The investigators also were able to stratify patients, based on individual immunoprofiling, into seven major groups based on molecular correlates. They concluded that such stratification could help improve the outcomes of clinical trials in SLE.
In another study, researchers looked at longitudinal gene expression in SLE patients by stratifying each of two independent sets of patients (a pediatric cohort and an adult cohort) into three clinically differentiated disease clusters defined by mechanisms of disease progression (Arthritis Rheumatol. Dec 2018;70[12]:2025-35).
The clusters included one showing a correlation between the percentage of neutrophils and disease activity progression, one showing a correlation between the percentage of lymphocytes and disease activity progression, and a third for which the percentage of neutrophils correlated to a lesser degree with disease activity but was functionally more heterogeneous. Patients in the two neutrophil‐driven clusters had an increased risk of developing proliferative nephritis.
The results have implications for treatment, trial design, and understanding of disease etiology, the investigators concluded.
“This may help us in the future as we think about which medicine to start patients on, and which medicines to start patients on first,” Dr. James said.
It is clear that precision medicine will play an increasingly important role in rheumatology, Dr. James said, when considering the context of other findings in recent years, such as those from studies looking at soluble mediators of inflammation associated with disease flare, as well as those that involved extensive immunophenotyping and showed widely divergent transcriptional patterns based on ancestral backgrounds. Other research, such as the BOLD (Biomarkers of Lupus Disease) study, looked at various mechanisms of disease flare.
Numerous types of personalized therapies are being considered in rheumatology, ranging from expanded regulatory T cells to chimeric antigen receptor T cell therapy to risk profiling for disease prevention, just to name a few. Going forward it will be important to perform more systems biology analyses to assemble precision medicine–related data that can inform clinical diagnosis, prognosis, and therapy selection and optimization, she said.
The future of personalized therapies in rheumatology will require more input from rheumatologists on large-scale precision medicine projects such as the National Institutes of Health’s All of Us Research Project and the Million Veteran Program, as well as other similar programs of major health systems, she noted, adding that different types of training and interaction with molecular pathologists, genetic counselors, health coaches, and other key players also are needed.
Dr. James reported having no relevant disclosures.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
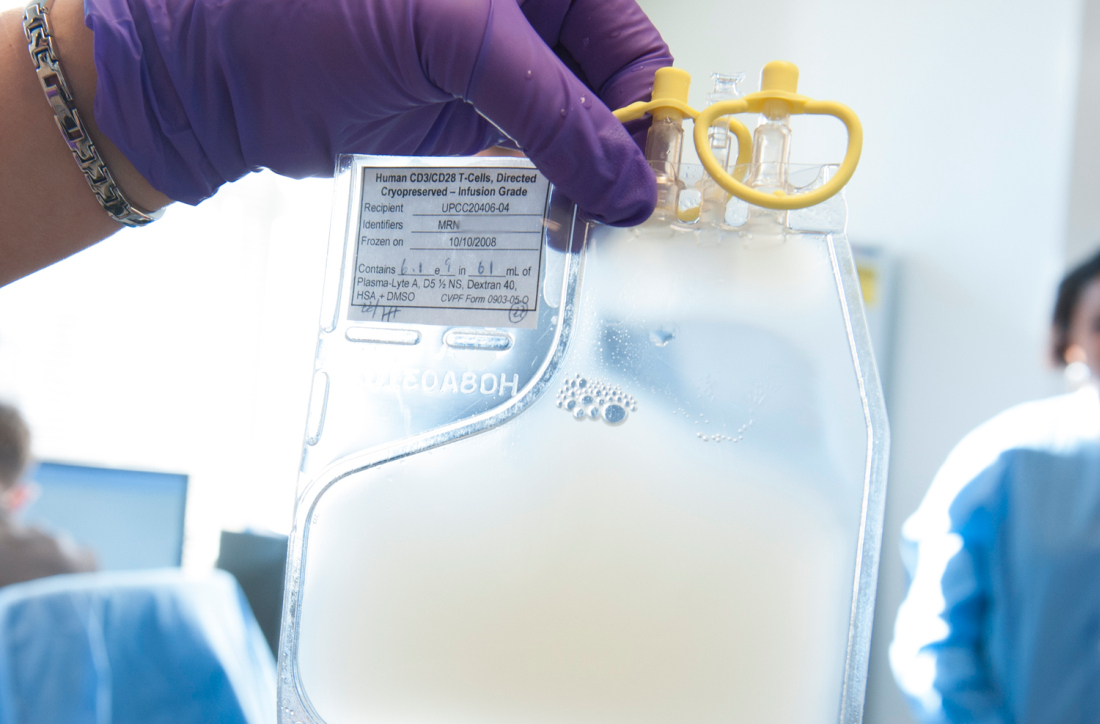
Novel bispecific CAR shows promise in B-cell malignancies
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Grade 1 cytokine release syndrome occurred in five patients, and grade 2 CRS occurred in one patient; there were no dose-limiting toxicities.
Study details: A phase 1 dose escalation study of nine patients.
Disclosures: Dr. Hossain reported having no financial disclosures.
Source: Hossain N et al. ASH 2018, Abstract 490.
Uninterrupted ibrutinib with CAR T could improve CLL outcomes
SAN DIEGO – Ibrutinib treatment continued before, during, and after infusion of the CD19-specific chimeric antigen receptor (CAR) T-cell therapy JCAR014 in patients with relapsed or refractory chronic lymphocytic leukemia (CLL) appears to improve patient responses and decrease the risk of severe cytokine release syndrome.
The findings come from a comparison of sequential cohorts from a phase 1/2 study.
At 4 weeks after infusion, the approach was highly efficacious; overall response rates by 2008 International Workshop on CLL (IWCLL) criteria were 83% in 24 patients who received the uninterrupted ibrutinib regimen along with the JCAR014 therapy – a combination of CD4 and CD8 T cells – and 65% in 19 patients from a prior cohort who did not receive continuous ibrutinib, Jordan Gauthier, MD, reported at the annual meeting of the American Society of Hematology.
Concurrent ibrutinib was generally well tolerated, with 13 of 19 patients in the ibrutinib cohort receiving treatment as planned without discontinuation. The rates of grade 1 or higher cytokine release syndrome (CRS) were statistically similar in the ibrutinib and no-ibrutinib cohorts (74% and 92%, respectively). However, the rates of severe CRS (grade 3 or higher) were, strikingly, 0% and 25%, respectively, said Dr. Gauthier, a senior fellow in the Turtle Lab at Fred Hutchinson Cancer Center, Seattle.
Neurotoxicity occurred in 32% and 42% of patients in the groups; severe neurotoxicity occurred in 26% and 29%, respectively.
In the ibrutinib cohort, one patient with grade 2 CRS developed fatal presumed cardiac arrhythmia; in the no-ibrutinib cohort, one patient died from a CAR T cell–related toxicity.
Notably, a trend toward better expansion of CD8 CAR T cells and a significantly greater expansion of CD4 CAR T cells was observed in the ibrutinib cohort, he said.
The study was designed to assess JCAR014, and based on the initial cohort findings published in 2017, established a regimen of cyclophosphamide and fludarabine (Cy/Flu) lymphodepletion followed by JCAR014 infusion at 2 x 106 CAR T cells/kg. The study was not a randomized, head-to-head comparison but the groups were similar with respect to both patient and disease characteristics, Dr. Gauthier noted.
The outcomes in the first cohort were then compared retrospectively with those from the subsequent cohort of patients who received Cy/Flu with 2 x 106 CAR T cells/kg with concurrent ibrutinib administered at 420 mg per day from at least 2 weeks prior to leukapheresis until at least 3 months after JCAR014 infusion.
The rationale for uninterrupted ibrutinib in relapsed/refractory CLL patients receiving JCAR014 included potential prevention of tumor flare, mobilization of CLL cells into the blood from the lymph nodes, improvement of CAR T-cell function, and a decrease in CAR T-cell related toxicity, he said.
The concurrent administration of ibrutinib and JCAR014 was feasible for most patients. “[It] induced high response rates and deep responses early on at 4 weeks, and it was associated with higher in vivo expansion of CD4 CAR T cells and with lower rates of severe toxicity,” Dr. Gauthier said. “The next step is to hopefully validate these findings in a prospective phase 1/2 study.”
Dr. Gauthier reported having no financial disclosures.
SOURCE: Gauthier J et al. ASH 18, Abstract 299.
SAN DIEGO – Ibrutinib treatment continued before, during, and after infusion of the CD19-specific chimeric antigen receptor (CAR) T-cell therapy JCAR014 in patients with relapsed or refractory chronic lymphocytic leukemia (CLL) appears to improve patient responses and decrease the risk of severe cytokine release syndrome.
The findings come from a comparison of sequential cohorts from a phase 1/2 study.
At 4 weeks after infusion, the approach was highly efficacious; overall response rates by 2008 International Workshop on CLL (IWCLL) criteria were 83% in 24 patients who received the uninterrupted ibrutinib regimen along with the JCAR014 therapy – a combination of CD4 and CD8 T cells – and 65% in 19 patients from a prior cohort who did not receive continuous ibrutinib, Jordan Gauthier, MD, reported at the annual meeting of the American Society of Hematology.
Concurrent ibrutinib was generally well tolerated, with 13 of 19 patients in the ibrutinib cohort receiving treatment as planned without discontinuation. The rates of grade 1 or higher cytokine release syndrome (CRS) were statistically similar in the ibrutinib and no-ibrutinib cohorts (74% and 92%, respectively). However, the rates of severe CRS (grade 3 or higher) were, strikingly, 0% and 25%, respectively, said Dr. Gauthier, a senior fellow in the Turtle Lab at Fred Hutchinson Cancer Center, Seattle.
Neurotoxicity occurred in 32% and 42% of patients in the groups; severe neurotoxicity occurred in 26% and 29%, respectively.
In the ibrutinib cohort, one patient with grade 2 CRS developed fatal presumed cardiac arrhythmia; in the no-ibrutinib cohort, one patient died from a CAR T cell–related toxicity.
Notably, a trend toward better expansion of CD8 CAR T cells and a significantly greater expansion of CD4 CAR T cells was observed in the ibrutinib cohort, he said.
The study was designed to assess JCAR014, and based on the initial cohort findings published in 2017, established a regimen of cyclophosphamide and fludarabine (Cy/Flu) lymphodepletion followed by JCAR014 infusion at 2 x 106 CAR T cells/kg. The study was not a randomized, head-to-head comparison but the groups were similar with respect to both patient and disease characteristics, Dr. Gauthier noted.
The outcomes in the first cohort were then compared retrospectively with those from the subsequent cohort of patients who received Cy/Flu with 2 x 106 CAR T cells/kg with concurrent ibrutinib administered at 420 mg per day from at least 2 weeks prior to leukapheresis until at least 3 months after JCAR014 infusion.
The rationale for uninterrupted ibrutinib in relapsed/refractory CLL patients receiving JCAR014 included potential prevention of tumor flare, mobilization of CLL cells into the blood from the lymph nodes, improvement of CAR T-cell function, and a decrease in CAR T-cell related toxicity, he said.
The concurrent administration of ibrutinib and JCAR014 was feasible for most patients. “[It] induced high response rates and deep responses early on at 4 weeks, and it was associated with higher in vivo expansion of CD4 CAR T cells and with lower rates of severe toxicity,” Dr. Gauthier said. “The next step is to hopefully validate these findings in a prospective phase 1/2 study.”
Dr. Gauthier reported having no financial disclosures.
SOURCE: Gauthier J et al. ASH 18, Abstract 299.
SAN DIEGO – Ibrutinib treatment continued before, during, and after infusion of the CD19-specific chimeric antigen receptor (CAR) T-cell therapy JCAR014 in patients with relapsed or refractory chronic lymphocytic leukemia (CLL) appears to improve patient responses and decrease the risk of severe cytokine release syndrome.
The findings come from a comparison of sequential cohorts from a phase 1/2 study.
At 4 weeks after infusion, the approach was highly efficacious; overall response rates by 2008 International Workshop on CLL (IWCLL) criteria were 83% in 24 patients who received the uninterrupted ibrutinib regimen along with the JCAR014 therapy – a combination of CD4 and CD8 T cells – and 65% in 19 patients from a prior cohort who did not receive continuous ibrutinib, Jordan Gauthier, MD, reported at the annual meeting of the American Society of Hematology.
Concurrent ibrutinib was generally well tolerated, with 13 of 19 patients in the ibrutinib cohort receiving treatment as planned without discontinuation. The rates of grade 1 or higher cytokine release syndrome (CRS) were statistically similar in the ibrutinib and no-ibrutinib cohorts (74% and 92%, respectively). However, the rates of severe CRS (grade 3 or higher) were, strikingly, 0% and 25%, respectively, said Dr. Gauthier, a senior fellow in the Turtle Lab at Fred Hutchinson Cancer Center, Seattle.
Neurotoxicity occurred in 32% and 42% of patients in the groups; severe neurotoxicity occurred in 26% and 29%, respectively.
In the ibrutinib cohort, one patient with grade 2 CRS developed fatal presumed cardiac arrhythmia; in the no-ibrutinib cohort, one patient died from a CAR T cell–related toxicity.
Notably, a trend toward better expansion of CD8 CAR T cells and a significantly greater expansion of CD4 CAR T cells was observed in the ibrutinib cohort, he said.
The study was designed to assess JCAR014, and based on the initial cohort findings published in 2017, established a regimen of cyclophosphamide and fludarabine (Cy/Flu) lymphodepletion followed by JCAR014 infusion at 2 x 106 CAR T cells/kg. The study was not a randomized, head-to-head comparison but the groups were similar with respect to both patient and disease characteristics, Dr. Gauthier noted.
The outcomes in the first cohort were then compared retrospectively with those from the subsequent cohort of patients who received Cy/Flu with 2 x 106 CAR T cells/kg with concurrent ibrutinib administered at 420 mg per day from at least 2 weeks prior to leukapheresis until at least 3 months after JCAR014 infusion.
The rationale for uninterrupted ibrutinib in relapsed/refractory CLL patients receiving JCAR014 included potential prevention of tumor flare, mobilization of CLL cells into the blood from the lymph nodes, improvement of CAR T-cell function, and a decrease in CAR T-cell related toxicity, he said.
The concurrent administration of ibrutinib and JCAR014 was feasible for most patients. “[It] induced high response rates and deep responses early on at 4 weeks, and it was associated with higher in vivo expansion of CD4 CAR T cells and with lower rates of severe toxicity,” Dr. Gauthier said. “The next step is to hopefully validate these findings in a prospective phase 1/2 study.”
Dr. Gauthier reported having no financial disclosures.
SOURCE: Gauthier J et al. ASH 18, Abstract 299.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Severe cytokine release syndrome occurred in 0% versus 25% of patients in the ibrutinib and no-ibrutinib cohorts, respectively.
Study details: A retrospective comparison of 43 patients in two cohorts from a phase 1/2 study.
Disclosures: Dr. Gauthier reported having no financial disclosures.
Source: Gauthier J et al. ASH 2018, Abstract 299.
Investigational gene therapy shows promise in hemophilia A
SAN DIEGO – Investigational SPK-8011 gene transfer results in safe, durable, dose-dependent Factor VIII (FVIII) expression in patients with severe or moderately severe hemophilia A, according to preliminary findings from an ongoing phase 1/2 study.
An overall reduction of 97% was seen in both the annualized bleeding rate (ABR) and annualized infusion rate (AIR) in the first 12 patients treated with SPK-8011, which is a Spark Therapeutics product that consists of a bioengineered AAV capsid expressing B domain-deleted FVIII under the control of a liver-specific promoter, principal investigator Lindsey A. George, MD, reported at the annual meeting of the American Society of Hematology.
Study subjects were men aged 18-52 years, including 11 with severe disease and 1 with moderately severe disease, who received a single infusion of either 5E11 vg/kg (2 patients), 1E12 vg/kg (3 patients), or 2E12 vg/kg (7 patients).
“All vector doses led to expression of FVIII levels adequate to prevent bleeding and allow cessation of prophylaxis,” said Dr. George, associate professor of pediatrics at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and an attending physician in the division of hematology at Children’s Hospital of Philadelphia.
In the two men in the 5E11 dose cohort, mean FVIII levels beginning 12 weeks after infusion were 13%, and neither experienced bleeding events, had elevated transaminase levels, or required steroids, she said, noting that FVIII expression remained stable for at least 66 weeks (and up to 78 weeks in one patient).
The three men in the 1E12 dose cohort had mean FVIII levels of 15% beginning at 12 weeks post infusion, and the levels were stable for at least 46 weeks.
The first patient was infused with a single dose of factor concentrate for a spontaneous joint bleed at day 159, and the second patient received multiple infusions for a traumatic bleed beginning at day 195. Both received a successful course of tapering steroids, at 12 and 7 weeks after infusion, respectively, for declining FVIII levels, Dr. George said.
The third subject had no bleeding and did not receive factor infusions or steroids, she added.
In the highest dose cohort (2E12), five of seven subjects had FVIII levels between 16% and 49%.
Steroids were required and given between 6 and 11 weeks after infusion in five of the seven patients in that cohort for either declining FVIII levels, a rise in alanine aminotransferase (ALT) above baseline, or elevated IFN-g ELISPOTs to AAV capsid. The steroids normalized ALT levels and extinguished the ELISPOT signal in all cases.
In two patients, FVIII levels showed limited stabilization, and fell to less than 6%. This was most likely due to the immune response, Dr. George explained, noting that in one of the two patients no bleeds were reported through 12 weeks of follow-up, while the other experienced four bleeds through 37 weeks of observation.
SPK-8011 was well tolerated in this study, which had cumulative follow-up of 506 weeks at the time of Dr. George’s presentation. No inhibitor formation was noted in the safety analysis and the only serious adverse event – the immune response to AAV capsid – has resolved, she said.
Data from the lowest dose cohort (5E11) are consistent with published natural history data indicating FVIII:C 12% is adequate to prevent spontaneous bleeding events, she said. However, she noted that the loss of some FVIII expression in two patients in the 2E12 dose cohort (which eventually stabilized on steroids), and the fact that five of seven subjects in this cohort required steroids, suggests a possible role for prophylactic steroid administration in patients treated with SPK-8011.
“Gene transfer for hemophilia A offers the potential for a one-time disease-altering treatment that eliminates bleed risk and could free patients from the burden of lifelong chronic therapy,” Dr. George said.
A phase 3 run-in study is planned, she added.
Spark Therapeutics sponsored the study. Dr. George reported equity ownership related to the University of Pennsylvania and consultancy for Pfizer.
SOURCE: High K et al., ASH 2018, Abstract 487.
SAN DIEGO – Investigational SPK-8011 gene transfer results in safe, durable, dose-dependent Factor VIII (FVIII) expression in patients with severe or moderately severe hemophilia A, according to preliminary findings from an ongoing phase 1/2 study.
An overall reduction of 97% was seen in both the annualized bleeding rate (ABR) and annualized infusion rate (AIR) in the first 12 patients treated with SPK-8011, which is a Spark Therapeutics product that consists of a bioengineered AAV capsid expressing B domain-deleted FVIII under the control of a liver-specific promoter, principal investigator Lindsey A. George, MD, reported at the annual meeting of the American Society of Hematology.
Study subjects were men aged 18-52 years, including 11 with severe disease and 1 with moderately severe disease, who received a single infusion of either 5E11 vg/kg (2 patients), 1E12 vg/kg (3 patients), or 2E12 vg/kg (7 patients).
“All vector doses led to expression of FVIII levels adequate to prevent bleeding and allow cessation of prophylaxis,” said Dr. George, associate professor of pediatrics at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and an attending physician in the division of hematology at Children’s Hospital of Philadelphia.
In the two men in the 5E11 dose cohort, mean FVIII levels beginning 12 weeks after infusion were 13%, and neither experienced bleeding events, had elevated transaminase levels, or required steroids, she said, noting that FVIII expression remained stable for at least 66 weeks (and up to 78 weeks in one patient).
The three men in the 1E12 dose cohort had mean FVIII levels of 15% beginning at 12 weeks post infusion, and the levels were stable for at least 46 weeks.
The first patient was infused with a single dose of factor concentrate for a spontaneous joint bleed at day 159, and the second patient received multiple infusions for a traumatic bleed beginning at day 195. Both received a successful course of tapering steroids, at 12 and 7 weeks after infusion, respectively, for declining FVIII levels, Dr. George said.
The third subject had no bleeding and did not receive factor infusions or steroids, she added.
In the highest dose cohort (2E12), five of seven subjects had FVIII levels between 16% and 49%.
Steroids were required and given between 6 and 11 weeks after infusion in five of the seven patients in that cohort for either declining FVIII levels, a rise in alanine aminotransferase (ALT) above baseline, or elevated IFN-g ELISPOTs to AAV capsid. The steroids normalized ALT levels and extinguished the ELISPOT signal in all cases.
In two patients, FVIII levels showed limited stabilization, and fell to less than 6%. This was most likely due to the immune response, Dr. George explained, noting that in one of the two patients no bleeds were reported through 12 weeks of follow-up, while the other experienced four bleeds through 37 weeks of observation.
SPK-8011 was well tolerated in this study, which had cumulative follow-up of 506 weeks at the time of Dr. George’s presentation. No inhibitor formation was noted in the safety analysis and the only serious adverse event – the immune response to AAV capsid – has resolved, she said.
Data from the lowest dose cohort (5E11) are consistent with published natural history data indicating FVIII:C 12% is adequate to prevent spontaneous bleeding events, she said. However, she noted that the loss of some FVIII expression in two patients in the 2E12 dose cohort (which eventually stabilized on steroids), and the fact that five of seven subjects in this cohort required steroids, suggests a possible role for prophylactic steroid administration in patients treated with SPK-8011.
“Gene transfer for hemophilia A offers the potential for a one-time disease-altering treatment that eliminates bleed risk and could free patients from the burden of lifelong chronic therapy,” Dr. George said.
A phase 3 run-in study is planned, she added.
Spark Therapeutics sponsored the study. Dr. George reported equity ownership related to the University of Pennsylvania and consultancy for Pfizer.
SOURCE: High K et al., ASH 2018, Abstract 487.
SAN DIEGO – Investigational SPK-8011 gene transfer results in safe, durable, dose-dependent Factor VIII (FVIII) expression in patients with severe or moderately severe hemophilia A, according to preliminary findings from an ongoing phase 1/2 study.
An overall reduction of 97% was seen in both the annualized bleeding rate (ABR) and annualized infusion rate (AIR) in the first 12 patients treated with SPK-8011, which is a Spark Therapeutics product that consists of a bioengineered AAV capsid expressing B domain-deleted FVIII under the control of a liver-specific promoter, principal investigator Lindsey A. George, MD, reported at the annual meeting of the American Society of Hematology.
Study subjects were men aged 18-52 years, including 11 with severe disease and 1 with moderately severe disease, who received a single infusion of either 5E11 vg/kg (2 patients), 1E12 vg/kg (3 patients), or 2E12 vg/kg (7 patients).
“All vector doses led to expression of FVIII levels adequate to prevent bleeding and allow cessation of prophylaxis,” said Dr. George, associate professor of pediatrics at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and an attending physician in the division of hematology at Children’s Hospital of Philadelphia.
In the two men in the 5E11 dose cohort, mean FVIII levels beginning 12 weeks after infusion were 13%, and neither experienced bleeding events, had elevated transaminase levels, or required steroids, she said, noting that FVIII expression remained stable for at least 66 weeks (and up to 78 weeks in one patient).
The three men in the 1E12 dose cohort had mean FVIII levels of 15% beginning at 12 weeks post infusion, and the levels were stable for at least 46 weeks.
The first patient was infused with a single dose of factor concentrate for a spontaneous joint bleed at day 159, and the second patient received multiple infusions for a traumatic bleed beginning at day 195. Both received a successful course of tapering steroids, at 12 and 7 weeks after infusion, respectively, for declining FVIII levels, Dr. George said.
The third subject had no bleeding and did not receive factor infusions or steroids, she added.
In the highest dose cohort (2E12), five of seven subjects had FVIII levels between 16% and 49%.
Steroids were required and given between 6 and 11 weeks after infusion in five of the seven patients in that cohort for either declining FVIII levels, a rise in alanine aminotransferase (ALT) above baseline, or elevated IFN-g ELISPOTs to AAV capsid. The steroids normalized ALT levels and extinguished the ELISPOT signal in all cases.
In two patients, FVIII levels showed limited stabilization, and fell to less than 6%. This was most likely due to the immune response, Dr. George explained, noting that in one of the two patients no bleeds were reported through 12 weeks of follow-up, while the other experienced four bleeds through 37 weeks of observation.
SPK-8011 was well tolerated in this study, which had cumulative follow-up of 506 weeks at the time of Dr. George’s presentation. No inhibitor formation was noted in the safety analysis and the only serious adverse event – the immune response to AAV capsid – has resolved, she said.
Data from the lowest dose cohort (5E11) are consistent with published natural history data indicating FVIII:C 12% is adequate to prevent spontaneous bleeding events, she said. However, she noted that the loss of some FVIII expression in two patients in the 2E12 dose cohort (which eventually stabilized on steroids), and the fact that five of seven subjects in this cohort required steroids, suggests a possible role for prophylactic steroid administration in patients treated with SPK-8011.
“Gene transfer for hemophilia A offers the potential for a one-time disease-altering treatment that eliminates bleed risk and could free patients from the burden of lifelong chronic therapy,” Dr. George said.
A phase 3 run-in study is planned, she added.
Spark Therapeutics sponsored the study. Dr. George reported equity ownership related to the University of Pennsylvania and consultancy for Pfizer.
SOURCE: High K et al., ASH 2018, Abstract 487.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: The overall reduction in annualized infusion rate (AIR) and annualized bleeding rate (ABR) was 97% for each.
Study details: A phase 1/2 study of 12 patients
Disclosures: Spark Therapeutics sponsored the study. Dr. George reported equity ownership related to the University of Pennsylvania and consultancy for Pfizer.
Source: High K et al. ASH 2018, Abstract 487.
Next-generation anti-BCMA CAR T shows promise for RRMM
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Objective response rate was 83% in the first 12 treated patients.
Study details: The CRB-402 phase 1 dose-escalation of 12 patients (up to 50 planned).
Disclosures: This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
Source: Shah N et al. ASH 2018, Abstract 488.
ALL chemotherapy looks effective in mixed phenotype leukemia
SAN DIEGO – The majority of pediatric patients with mixed phenotype acute leukemia (MPAL) who were treated with acute lymphoblastic leukemia (ALL)–directed chemotherapy achieved a minimum residual disease (MRD)–negative complete response by the end of consolidation, according to findings from a multicenter retrospective cohort study.
The cohort included 94 patients aged 1-21 years who met strict World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions. Most had B/myeloid phenotype (89%), and 87 patients were treated with an ALL regimen, Etan Orgel, MD, reported at the annual meeting of the American Society of Hematology.
Of those 87 patients, 81 (93%) experienced an end-of-induction (EOI) complete response. One patient died during induction and six had induction failures, defined as either disease progression before EOI (two patients) or EOI MRD of 5% or greater (three patients), said Dr. Orgel of the University of Southern California, Los Angeles, and Children’s Hospital Los Angeles.
The MRD-negative rates, defined as MRD less than 0.01%, were 70% at EOI and 86% at EOI or end of consolidation (EOC); 12 of 14 patients who were MRD positive at EOI and continued on ALL therapy achieved an EOC MRD-negative complete response, including 8 of 8 with EOI MRD of 0.01%-0.09% and 4 of 6 with EOI MRD of 1% or greater.
Event-free survival at 5 years in the 78 patients without hematopoietic stem cell transplant at first remission was 75%, and 5-year overall survival was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said. “This is very different from the approach used at many adult centers and many of the adult recommendations.”
Overall 5-year EOI event-free survival was 80% in the 59 patients who were MRD negative at EOI, and 13% in 25 patients who were MRD-positive at EOI. The corresponding overall survival rates were 91% and 84%.
Overall 5-year EOC event-free survival was 77% in 74 patients who were MRD negative at EOC and was unavailable in 3 patients who were MRD positive at EOC, although all three were salvaged. The corresponding EOC overall survival rates were 89% and “not available,” Dr. Orgel reported.
Multivariable analysis confirmed the predictive value of MRD at EOI (hazard ratio for event-free survival and overall survival, 3.77 and 3.54, respectively).
Of note, there was a possible trend toward earlier failure and a trend toward worse overall survival (HR, 4.49, P = .074) for T-lineage–containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” he said.
MRD in pediatric MPAL is rare. Recent studies of MPAL biology show areas of similarity with ALL and AML, and while this could eventually help further subcategorize or classify the disease and lead to biology-driven therapies, it is important to know how to treat the disease today, Dr. Orgel said.
The evolving consensus is that ALL therapy is adequate for most MPAL, but there is no established threshold for MRD to enable a risk-stratified MPAL approach, he added.
The current findings suggest that ALL therapy – without hematopoietic stem cell transplant – may be sufficient to treat most patients with pediatric MPAL, Dr. Orgen reported, noting that clinical trials are necessary to prospectively validate MRD thresholds at EOI and EOC and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” he said.
Dr. Orgel reported having no financial disclosures.
SOURCE: Oberley M et al. ASH 2018, Abstract 558.
SAN DIEGO – The majority of pediatric patients with mixed phenotype acute leukemia (MPAL) who were treated with acute lymphoblastic leukemia (ALL)–directed chemotherapy achieved a minimum residual disease (MRD)–negative complete response by the end of consolidation, according to findings from a multicenter retrospective cohort study.
The cohort included 94 patients aged 1-21 years who met strict World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions. Most had B/myeloid phenotype (89%), and 87 patients were treated with an ALL regimen, Etan Orgel, MD, reported at the annual meeting of the American Society of Hematology.
Of those 87 patients, 81 (93%) experienced an end-of-induction (EOI) complete response. One patient died during induction and six had induction failures, defined as either disease progression before EOI (two patients) or EOI MRD of 5% or greater (three patients), said Dr. Orgel of the University of Southern California, Los Angeles, and Children’s Hospital Los Angeles.
The MRD-negative rates, defined as MRD less than 0.01%, were 70% at EOI and 86% at EOI or end of consolidation (EOC); 12 of 14 patients who were MRD positive at EOI and continued on ALL therapy achieved an EOC MRD-negative complete response, including 8 of 8 with EOI MRD of 0.01%-0.09% and 4 of 6 with EOI MRD of 1% or greater.
Event-free survival at 5 years in the 78 patients without hematopoietic stem cell transplant at first remission was 75%, and 5-year overall survival was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said. “This is very different from the approach used at many adult centers and many of the adult recommendations.”
Overall 5-year EOI event-free survival was 80% in the 59 patients who were MRD negative at EOI, and 13% in 25 patients who were MRD-positive at EOI. The corresponding overall survival rates were 91% and 84%.
Overall 5-year EOC event-free survival was 77% in 74 patients who were MRD negative at EOC and was unavailable in 3 patients who were MRD positive at EOC, although all three were salvaged. The corresponding EOC overall survival rates were 89% and “not available,” Dr. Orgel reported.
Multivariable analysis confirmed the predictive value of MRD at EOI (hazard ratio for event-free survival and overall survival, 3.77 and 3.54, respectively).
Of note, there was a possible trend toward earlier failure and a trend toward worse overall survival (HR, 4.49, P = .074) for T-lineage–containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” he said.
MRD in pediatric MPAL is rare. Recent studies of MPAL biology show areas of similarity with ALL and AML, and while this could eventually help further subcategorize or classify the disease and lead to biology-driven therapies, it is important to know how to treat the disease today, Dr. Orgel said.
The evolving consensus is that ALL therapy is adequate for most MPAL, but there is no established threshold for MRD to enable a risk-stratified MPAL approach, he added.
The current findings suggest that ALL therapy – without hematopoietic stem cell transplant – may be sufficient to treat most patients with pediatric MPAL, Dr. Orgen reported, noting that clinical trials are necessary to prospectively validate MRD thresholds at EOI and EOC and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” he said.
Dr. Orgel reported having no financial disclosures.
SOURCE: Oberley M et al. ASH 2018, Abstract 558.
SAN DIEGO – The majority of pediatric patients with mixed phenotype acute leukemia (MPAL) who were treated with acute lymphoblastic leukemia (ALL)–directed chemotherapy achieved a minimum residual disease (MRD)–negative complete response by the end of consolidation, according to findings from a multicenter retrospective cohort study.
The cohort included 94 patients aged 1-21 years who met strict World Health Organization MPAL criteria and were treated between 2008 and 2016 at one of six U.S. institutions. Most had B/myeloid phenotype (89%), and 87 patients were treated with an ALL regimen, Etan Orgel, MD, reported at the annual meeting of the American Society of Hematology.
Of those 87 patients, 81 (93%) experienced an end-of-induction (EOI) complete response. One patient died during induction and six had induction failures, defined as either disease progression before EOI (two patients) or EOI MRD of 5% or greater (three patients), said Dr. Orgel of the University of Southern California, Los Angeles, and Children’s Hospital Los Angeles.
The MRD-negative rates, defined as MRD less than 0.01%, were 70% at EOI and 86% at EOI or end of consolidation (EOC); 12 of 14 patients who were MRD positive at EOI and continued on ALL therapy achieved an EOC MRD-negative complete response, including 8 of 8 with EOI MRD of 0.01%-0.09% and 4 of 6 with EOI MRD of 1% or greater.
Event-free survival at 5 years in the 78 patients without hematopoietic stem cell transplant at first remission was 75%, and 5-year overall survival was 89%, “thus demonstrating that, for a majority of patients, transplant in first remission may not be necessary,” Dr. Orgel said. “This is very different from the approach used at many adult centers and many of the adult recommendations.”
Overall 5-year EOI event-free survival was 80% in the 59 patients who were MRD negative at EOI, and 13% in 25 patients who were MRD-positive at EOI. The corresponding overall survival rates were 91% and 84%.
Overall 5-year EOC event-free survival was 77% in 74 patients who were MRD negative at EOC and was unavailable in 3 patients who were MRD positive at EOC, although all three were salvaged. The corresponding EOC overall survival rates were 89% and “not available,” Dr. Orgel reported.
Multivariable analysis confirmed the predictive value of MRD at EOI (hazard ratio for event-free survival and overall survival, 3.77 and 3.54, respectively).
Of note, there was a possible trend toward earlier failure and a trend toward worse overall survival (HR, 4.49, P = .074) for T-lineage–containing MPAL.
“That indicates that this might be a group that needs careful scrutiny of which form of ALL therapy they receive,” he said.
MRD in pediatric MPAL is rare. Recent studies of MPAL biology show areas of similarity with ALL and AML, and while this could eventually help further subcategorize or classify the disease and lead to biology-driven therapies, it is important to know how to treat the disease today, Dr. Orgel said.
The evolving consensus is that ALL therapy is adequate for most MPAL, but there is no established threshold for MRD to enable a risk-stratified MPAL approach, he added.
The current findings suggest that ALL therapy – without hematopoietic stem cell transplant – may be sufficient to treat most patients with pediatric MPAL, Dr. Orgen reported, noting that clinical trials are necessary to prospectively validate MRD thresholds at EOI and EOC and to establish the threshold for favorable survival.
“Future research should explore either intensification of therapy or different therapies for patients with persistent MRD,” he said.
Dr. Orgel reported having no financial disclosures.
SOURCE: Oberley M et al. ASH 2018, Abstract 558.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: MRD-negative rates were 70% at end of induction and 86% at end of induction or consolidation.
Study details: A retrospective cohort study of 87 pediatric MPAL patients.
Disclosures: Dr. Orgel reported having no financial disclosures.
Source: Oberley M et al. ASH 2018, Abstract 558.
GO-8: Early promise for novel FVIII variant in hemophilia A
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: A single infusion of the factor VIII variant resulted in activity levels of about 6%, compared with 1% or less at baseline.
Study details: The findings were from the first four patients in a phase 1/2 dose-escalation study.
Disclosures: Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
Source: Chowdary P et al. ASH 2018, Abstract 489.
Data underscore the importance of lifestyle interventions in breast cancer patients
SAN ANTONIO – Data continue to underscore the benefits of lifestyle interventions in women with breast cancer, but questions remain about their effects on recurrence, according to Jennifer Ligibel, MD.
Findings from the EBBA-II trial as presented at the San Antonio Breast Cancer Symposium, for example, showed that exercise improves cardiorespiratory fitness in women with early breast cancer, and findings from the SUCCESS C study showed that breast cancer patients who completed a weight-loss intervention showed some improvements, compared with those who did not, said Dr. Ligibel of Dana-Farber Cancer Institute in Boston, who was the discussant for those and other lifestyle-intervention studies at the symposium.
SUCCESS C failed to show an overall reduction in breast cancer recurrence or survival, but weight loss among intervention-group participants was modest, and more than half of the participants dropped out of the study, so it’s hard to make any firm conclusions, she said.
Overall, the findings – in the context of what is already known about lifestyle interventions among women with breast cancer – provide “yet another reason to tell women that it’s important to exercise during treatment,” she said.

In this video interview, Dr. Ligibel discussed the studies and the implications of the findings, and also mentioned an ongoing study for which she is an investigator. In that study – the Breast Cancer Weight Loss study (BWEL) – adherence among the approximately 1,700 women enrolled has been high. “So we’re hoping that this study in a few years will give us a bit more information about the power of weight loss to potentially reduce recurrence.”
For now, the available data show that there are “lots of concrete benefits” associated with improving lifestyle in women with breast cancer, she said, noting that she tells all of her patients to live as healthy a lifestyle as possible, and especially to exercise.
SAN ANTONIO – Data continue to underscore the benefits of lifestyle interventions in women with breast cancer, but questions remain about their effects on recurrence, according to Jennifer Ligibel, MD.
Findings from the EBBA-II trial as presented at the San Antonio Breast Cancer Symposium, for example, showed that exercise improves cardiorespiratory fitness in women with early breast cancer, and findings from the SUCCESS C study showed that breast cancer patients who completed a weight-loss intervention showed some improvements, compared with those who did not, said Dr. Ligibel of Dana-Farber Cancer Institute in Boston, who was the discussant for those and other lifestyle-intervention studies at the symposium.
SUCCESS C failed to show an overall reduction in breast cancer recurrence or survival, but weight loss among intervention-group participants was modest, and more than half of the participants dropped out of the study, so it’s hard to make any firm conclusions, she said.
Overall, the findings – in the context of what is already known about lifestyle interventions among women with breast cancer – provide “yet another reason to tell women that it’s important to exercise during treatment,” she said.

In this video interview, Dr. Ligibel discussed the studies and the implications of the findings, and also mentioned an ongoing study for which she is an investigator. In that study – the Breast Cancer Weight Loss study (BWEL) – adherence among the approximately 1,700 women enrolled has been high. “So we’re hoping that this study in a few years will give us a bit more information about the power of weight loss to potentially reduce recurrence.”
For now, the available data show that there are “lots of concrete benefits” associated with improving lifestyle in women with breast cancer, she said, noting that she tells all of her patients to live as healthy a lifestyle as possible, and especially to exercise.
SAN ANTONIO – Data continue to underscore the benefits of lifestyle interventions in women with breast cancer, but questions remain about their effects on recurrence, according to Jennifer Ligibel, MD.
Findings from the EBBA-II trial as presented at the San Antonio Breast Cancer Symposium, for example, showed that exercise improves cardiorespiratory fitness in women with early breast cancer, and findings from the SUCCESS C study showed that breast cancer patients who completed a weight-loss intervention showed some improvements, compared with those who did not, said Dr. Ligibel of Dana-Farber Cancer Institute in Boston, who was the discussant for those and other lifestyle-intervention studies at the symposium.
SUCCESS C failed to show an overall reduction in breast cancer recurrence or survival, but weight loss among intervention-group participants was modest, and more than half of the participants dropped out of the study, so it’s hard to make any firm conclusions, she said.
Overall, the findings – in the context of what is already known about lifestyle interventions among women with breast cancer – provide “yet another reason to tell women that it’s important to exercise during treatment,” she said.

In this video interview, Dr. Ligibel discussed the studies and the implications of the findings, and also mentioned an ongoing study for which she is an investigator. In that study – the Breast Cancer Weight Loss study (BWEL) – adherence among the approximately 1,700 women enrolled has been high. “So we’re hoping that this study in a few years will give us a bit more information about the power of weight loss to potentially reduce recurrence.”
For now, the available data show that there are “lots of concrete benefits” associated with improving lifestyle in women with breast cancer, she said, noting that she tells all of her patients to live as healthy a lifestyle as possible, and especially to exercise.
REPORTING FROM SABCS 2018
Rheumatologist prescribing rates predict chronic opioid use in RA patients
CHICAGO – A physician’s baseline opioid prescribing rate strongly predicts future chronic opioid use in rheumatoid arthritis patients, an analysis of data from the Consortium of Rheumatology Researchers of North America (Corrona) Rheumatoid Arthritis Registry suggests.
The baseline 12-month opioid prescribing rate of 148 physicians in the initial cohort varied widely from 0% to 70% (median, 27%), and among 9,337 patients in the registry beyond the baseline 12 months, physician opioid prescribing rates during the baseline period were significantly associated with risk for chronic opioid use, Yvonne C. Lee, MD, reported at the annual meeting of the American College of Rheumatology. She and her colleagues defined chronic opioid use as any opioid use during at least two consecutive study visits.
“It is important to understand the relative contributions of patient vs. physician characteristics on chronic opioid use,” said Dr. Lee of Northwestern University, Chicago. She that the goals of the current study were to identify the extent to which rheumatologists in the United States varied in baseline opioid prescribing rates and to determine the implications of baseline prescribing rates with respect to future chronic opioid use.
Compared with the lowest quartile of baseline opioid prescribing (rate of 18% or less), the second, third, and fourth quartiles of prescribing were associated with increasing odds of chronic opioid use (odds ratios of 1.16, 1.89, and 2.01 for the quartiles, respectively) during the study period, she said.
The researchers saw similar relationships when they used a stricter definition of opioid use and when they extended the cutoff between the baseline and study periods to 18 months. The relationships persisted after adjusting for numerous patient characteristics, such as age, sex, race, insurance status, RA duration, and treatments used, she said.
Subgroup analyses were also conducted to examine heterogeneity across clinical characteristics, including Clinical Disease Activity Index score (10 or less vs. greater than 10), pain intensity (scores of 40 or less, greater than 40 to 60, and greater than 60 out of 100), and use vs. nonuse of antidepressant medication. The relationships between physician baseline prescribing and chronic opioid use were similar across subgroups, she noted.
The findings help to characterize the role of rheumatologists’ prescribing rates in the ongoing opioid crisis even though the conclusions that can be reached are limited by the fact that some patients may receive opioid prescriptions from physicians outside the registry, by a lack of data on specific opioid types and doses, and by a lack of detailed information about physician characteristics, Dr. Lee said.
Physicians were included in the analysis only if they had contributed at least 10 RA patients to the registry within their first year of participation, and patients were included if they were patients of those physicians, if they had at least 12 months of follow-up data available, and if they were not prevalent opioid users at study entry.
A long-term goal is to target interventions to appropriate subgroups, she said, noting that 21%-29% of patients who are prescribed opioids for chronic pain misuse them, and more than 33,000 Americans die of opioid overdoses each year.
“Implications [of the findings] are that, in addition to targeting patients, we may also really want to consider interventions that target high-intensity prescribers. This may be useful for helping to decrease chronic opioid use in patients,” she concluded.
Dr. Lee has an investigator-initiated grant from Pfizer and owns stock in Express Scripts.
SOURCE: Lee Y et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1917
CHICAGO – A physician’s baseline opioid prescribing rate strongly predicts future chronic opioid use in rheumatoid arthritis patients, an analysis of data from the Consortium of Rheumatology Researchers of North America (Corrona) Rheumatoid Arthritis Registry suggests.
The baseline 12-month opioid prescribing rate of 148 physicians in the initial cohort varied widely from 0% to 70% (median, 27%), and among 9,337 patients in the registry beyond the baseline 12 months, physician opioid prescribing rates during the baseline period were significantly associated with risk for chronic opioid use, Yvonne C. Lee, MD, reported at the annual meeting of the American College of Rheumatology. She and her colleagues defined chronic opioid use as any opioid use during at least two consecutive study visits.
“It is important to understand the relative contributions of patient vs. physician characteristics on chronic opioid use,” said Dr. Lee of Northwestern University, Chicago. She that the goals of the current study were to identify the extent to which rheumatologists in the United States varied in baseline opioid prescribing rates and to determine the implications of baseline prescribing rates with respect to future chronic opioid use.
Compared with the lowest quartile of baseline opioid prescribing (rate of 18% or less), the second, third, and fourth quartiles of prescribing were associated with increasing odds of chronic opioid use (odds ratios of 1.16, 1.89, and 2.01 for the quartiles, respectively) during the study period, she said.
The researchers saw similar relationships when they used a stricter definition of opioid use and when they extended the cutoff between the baseline and study periods to 18 months. The relationships persisted after adjusting for numerous patient characteristics, such as age, sex, race, insurance status, RA duration, and treatments used, she said.
Subgroup analyses were also conducted to examine heterogeneity across clinical characteristics, including Clinical Disease Activity Index score (10 or less vs. greater than 10), pain intensity (scores of 40 or less, greater than 40 to 60, and greater than 60 out of 100), and use vs. nonuse of antidepressant medication. The relationships between physician baseline prescribing and chronic opioid use were similar across subgroups, she noted.
The findings help to characterize the role of rheumatologists’ prescribing rates in the ongoing opioid crisis even though the conclusions that can be reached are limited by the fact that some patients may receive opioid prescriptions from physicians outside the registry, by a lack of data on specific opioid types and doses, and by a lack of detailed information about physician characteristics, Dr. Lee said.
Physicians were included in the analysis only if they had contributed at least 10 RA patients to the registry within their first year of participation, and patients were included if they were patients of those physicians, if they had at least 12 months of follow-up data available, and if they were not prevalent opioid users at study entry.
A long-term goal is to target interventions to appropriate subgroups, she said, noting that 21%-29% of patients who are prescribed opioids for chronic pain misuse them, and more than 33,000 Americans die of opioid overdoses each year.
“Implications [of the findings] are that, in addition to targeting patients, we may also really want to consider interventions that target high-intensity prescribers. This may be useful for helping to decrease chronic opioid use in patients,” she concluded.
Dr. Lee has an investigator-initiated grant from Pfizer and owns stock in Express Scripts.
SOURCE: Lee Y et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1917
CHICAGO – A physician’s baseline opioid prescribing rate strongly predicts future chronic opioid use in rheumatoid arthritis patients, an analysis of data from the Consortium of Rheumatology Researchers of North America (Corrona) Rheumatoid Arthritis Registry suggests.
The baseline 12-month opioid prescribing rate of 148 physicians in the initial cohort varied widely from 0% to 70% (median, 27%), and among 9,337 patients in the registry beyond the baseline 12 months, physician opioid prescribing rates during the baseline period were significantly associated with risk for chronic opioid use, Yvonne C. Lee, MD, reported at the annual meeting of the American College of Rheumatology. She and her colleagues defined chronic opioid use as any opioid use during at least two consecutive study visits.
“It is important to understand the relative contributions of patient vs. physician characteristics on chronic opioid use,” said Dr. Lee of Northwestern University, Chicago. She that the goals of the current study were to identify the extent to which rheumatologists in the United States varied in baseline opioid prescribing rates and to determine the implications of baseline prescribing rates with respect to future chronic opioid use.
Compared with the lowest quartile of baseline opioid prescribing (rate of 18% or less), the second, third, and fourth quartiles of prescribing were associated with increasing odds of chronic opioid use (odds ratios of 1.16, 1.89, and 2.01 for the quartiles, respectively) during the study period, she said.
The researchers saw similar relationships when they used a stricter definition of opioid use and when they extended the cutoff between the baseline and study periods to 18 months. The relationships persisted after adjusting for numerous patient characteristics, such as age, sex, race, insurance status, RA duration, and treatments used, she said.
Subgroup analyses were also conducted to examine heterogeneity across clinical characteristics, including Clinical Disease Activity Index score (10 or less vs. greater than 10), pain intensity (scores of 40 or less, greater than 40 to 60, and greater than 60 out of 100), and use vs. nonuse of antidepressant medication. The relationships between physician baseline prescribing and chronic opioid use were similar across subgroups, she noted.
The findings help to characterize the role of rheumatologists’ prescribing rates in the ongoing opioid crisis even though the conclusions that can be reached are limited by the fact that some patients may receive opioid prescriptions from physicians outside the registry, by a lack of data on specific opioid types and doses, and by a lack of detailed information about physician characteristics, Dr. Lee said.
Physicians were included in the analysis only if they had contributed at least 10 RA patients to the registry within their first year of participation, and patients were included if they were patients of those physicians, if they had at least 12 months of follow-up data available, and if they were not prevalent opioid users at study entry.
A long-term goal is to target interventions to appropriate subgroups, she said, noting that 21%-29% of patients who are prescribed opioids for chronic pain misuse them, and more than 33,000 Americans die of opioid overdoses each year.
“Implications [of the findings] are that, in addition to targeting patients, we may also really want to consider interventions that target high-intensity prescribers. This may be useful for helping to decrease chronic opioid use in patients,” she concluded.
Dr. Lee has an investigator-initiated grant from Pfizer and owns stock in Express Scripts.
SOURCE: Lee Y et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1917
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point:
Major finding: The odds of chronic opioid use increased with rising baseline prescribing rates (odds ratios, 1.16, 1.89, and 2.01 for 2nd, 3rd, and 4th quartiles vs. 1st quartile of prescribing, respectively).
Study details: An analysis of data from 148 physicians and 9,337 Corrona RA Registry patients.
Disclosures: Dr. Lee has an investigator-initiated grant from Pfizer and owns stock in Express Scripts.
Source: Lee Y et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1917
“FAST” indices help to identify fibromyalgia in routine rheumatology care
CHICAGO – Fibromyalgia assessment screening tool (FAST) indices derived from the Multidimensional Health Assessment Questionnaire (MDHAQ) provide a simple and effective method for identifying fibromyalgia in routine care, according to findings from a series of more than 500 patients.
The indices are as accurate as the existing – and more complex – diagnostic criteria for fibromyalgia, Juan Schmukler, MD, reported at the annual meeting of the American College of Rheumatology.
For example, three FAST indices developed in the course of the study had better performance versus existing diagnostic criteria than did certain individual MDHAQ scales alone (area under the curve range, 0.924-0.937 vs. 0.829-0.889, respectively), said Dr. Schmukler, who conducted the research as a medical student at Rush Medical College, Chicago, and is now a rheumatology fellow at Mount Sinai Hospital in Chicago.
The findings are notable, because the two-page MDHAQ and a summary index (the RAPID3) derived from three of the MDHAQ scales are already used routinely in clinical care for diagnosing rheumatic diseases, and the new indices could easily – and with minimal work flow disruption – also be incorporated for each patient at each visit.
“Fibromyalgia is common in the general population and it is believed to be more common in patients with other rheumatic diagnoses,” Dr. Schmukler said. “Fibromyalgia may be easily recognized in many cases, but it can also be very subtle, particularly in patients who have other rheumatic diseases.”
ACR fibromyalgia classification criteria published in 1990 were based on tender point examination and non-ACR diagnostic criteria as revised in 2011 are based entirely on patient self-report.
A one-page fibromyalgia criteria questionnaire is available and is useful in clinical trials and other research, but is “rarely, if ever” used in routine care, he said, explaining that the questionnaire contains two domains: a symptom severity score (0-12 scale) and a widespread pain index (0-19 scale).
The MDHAQ/RAPID3 is informative in RA, and has also been shown to be “useful in all rheumatic diseases in which it has been studied,” and at least three prior reports have suggested that the MDHAQ may also provide clues to the presence of fibromyalgia, Dr. Schmukler said.
“And we know from prior reports that patients with fibromyalgia reported the highest RAPID3 scores, compared to other rheumatic disease,” he added, explaining that the goal of the present study was to develop FAST cumulative indices based on the routine MDHAQ scales and using the 2011 diagnostic criteria as a reference standard.
All patients with all diagnoses seen at the Rush Medical College rheumatology clinic in Chicago complete the MDHAQ at all visits in routine care, and between April and July 2017, the fibromyalgia criteria questionnaire was also administered in 502 consecutive patients.
Of those patients, 131 met the 2011 fibromyalgia diagnostic criteria.
MDHAQ scores were analyzed for agreement with the fibromyalgia criteria questionnaire according to receiver operator characteristic curves for AUC and were compiled into three different FAST indices that included various combinations of either three or four of the MDHAQ measures that had the best agreement with the diagnostic criteria questionnaire as identified by the highest AUC values. Those were the 60-symptom checklist (AUC, 0.889), painful joint count (AUC, 0.870), fatigue visual analog scale (VAS; AUC, 0.860), and pain VAS (AUC, 0.829), Dr. Schmukler said.
Proposed cut points that reflected the optimal trade-off between specificity and sensitivity for each of the scales were scores of 6 or greater for the pain VAS and fatigue VAS, and scores of 16 or greater for the symptom checklist and painful joint count measure.
In addition to the better performance of each FAST index versus the 2011 criteria, their performance was also better than that of the RAPID3 versus the 2011 criteria (AUC, 0.848), which many clinicians use in practice without using the full MDHAQ for patient assessment, he said.
Further, the “very easily calculated” FAST indices performed as well as a “very difficult to calculate” polysymptomatic distress continuous scale derived from the fibromyalgia questionnaire to assess the degree of fibromyalgia symptoms, which had an AUC of 0.929 versus the 2011 criteria. The latter index requires complex mathematical calculations for scale conversion and thus is impractical in clinical practice, he noted.
The FAST indices also performed comparably with physician diagnoses as indicated in patient charts and with diagnoses based on tender point count as shown in prior studies.
The FAST index with the greatest sensitivity (85.5% at a cut point of 2 or greater on a scale of 1-3) was the FAST3-P, which includes pain VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater. The FAST index with the greatest specificity (90.3% at a cut point of score of 3 or greater on a scale of 1-4) was the FAST4 index, which includes a pain VAS score of 6 or greater, fatigue VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater.
Although the findings are limited by the lack of a gold standard for fibromyalgia diagnosis, changing diagnostic criteria, and a need for physician input for a fibromyalgia diagnosis, the study provides useful real-world data and supports findings from some prior studies with respect to the benefit of using these tools in routine practice.
With minimal extra physician time – if the MDHAQ is completed by patients at the time of registration – this approach can be used in all rheumatology patients to help identify fibromyalgia, he concluded.
Dr. Schmukler reported having no disclosures. One of his coauthors at Rush, Ted Pincus, MD, receives royalties and license fees for the copyright and trademark for the MDHAQ and RAPID3, all of which go to support clinical research.
SOURCE: Schmukler J et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 839.
CHICAGO – Fibromyalgia assessment screening tool (FAST) indices derived from the Multidimensional Health Assessment Questionnaire (MDHAQ) provide a simple and effective method for identifying fibromyalgia in routine care, according to findings from a series of more than 500 patients.
The indices are as accurate as the existing – and more complex – diagnostic criteria for fibromyalgia, Juan Schmukler, MD, reported at the annual meeting of the American College of Rheumatology.
For example, three FAST indices developed in the course of the study had better performance versus existing diagnostic criteria than did certain individual MDHAQ scales alone (area under the curve range, 0.924-0.937 vs. 0.829-0.889, respectively), said Dr. Schmukler, who conducted the research as a medical student at Rush Medical College, Chicago, and is now a rheumatology fellow at Mount Sinai Hospital in Chicago.
The findings are notable, because the two-page MDHAQ and a summary index (the RAPID3) derived from three of the MDHAQ scales are already used routinely in clinical care for diagnosing rheumatic diseases, and the new indices could easily – and with minimal work flow disruption – also be incorporated for each patient at each visit.
“Fibromyalgia is common in the general population and it is believed to be more common in patients with other rheumatic diagnoses,” Dr. Schmukler said. “Fibromyalgia may be easily recognized in many cases, but it can also be very subtle, particularly in patients who have other rheumatic diseases.”
ACR fibromyalgia classification criteria published in 1990 were based on tender point examination and non-ACR diagnostic criteria as revised in 2011 are based entirely on patient self-report.
A one-page fibromyalgia criteria questionnaire is available and is useful in clinical trials and other research, but is “rarely, if ever” used in routine care, he said, explaining that the questionnaire contains two domains: a symptom severity score (0-12 scale) and a widespread pain index (0-19 scale).
The MDHAQ/RAPID3 is informative in RA, and has also been shown to be “useful in all rheumatic diseases in which it has been studied,” and at least three prior reports have suggested that the MDHAQ may also provide clues to the presence of fibromyalgia, Dr. Schmukler said.
“And we know from prior reports that patients with fibromyalgia reported the highest RAPID3 scores, compared to other rheumatic disease,” he added, explaining that the goal of the present study was to develop FAST cumulative indices based on the routine MDHAQ scales and using the 2011 diagnostic criteria as a reference standard.
All patients with all diagnoses seen at the Rush Medical College rheumatology clinic in Chicago complete the MDHAQ at all visits in routine care, and between April and July 2017, the fibromyalgia criteria questionnaire was also administered in 502 consecutive patients.
Of those patients, 131 met the 2011 fibromyalgia diagnostic criteria.
MDHAQ scores were analyzed for agreement with the fibromyalgia criteria questionnaire according to receiver operator characteristic curves for AUC and were compiled into three different FAST indices that included various combinations of either three or four of the MDHAQ measures that had the best agreement with the diagnostic criteria questionnaire as identified by the highest AUC values. Those were the 60-symptom checklist (AUC, 0.889), painful joint count (AUC, 0.870), fatigue visual analog scale (VAS; AUC, 0.860), and pain VAS (AUC, 0.829), Dr. Schmukler said.
Proposed cut points that reflected the optimal trade-off between specificity and sensitivity for each of the scales were scores of 6 or greater for the pain VAS and fatigue VAS, and scores of 16 or greater for the symptom checklist and painful joint count measure.
In addition to the better performance of each FAST index versus the 2011 criteria, their performance was also better than that of the RAPID3 versus the 2011 criteria (AUC, 0.848), which many clinicians use in practice without using the full MDHAQ for patient assessment, he said.
Further, the “very easily calculated” FAST indices performed as well as a “very difficult to calculate” polysymptomatic distress continuous scale derived from the fibromyalgia questionnaire to assess the degree of fibromyalgia symptoms, which had an AUC of 0.929 versus the 2011 criteria. The latter index requires complex mathematical calculations for scale conversion and thus is impractical in clinical practice, he noted.
The FAST indices also performed comparably with physician diagnoses as indicated in patient charts and with diagnoses based on tender point count as shown in prior studies.
The FAST index with the greatest sensitivity (85.5% at a cut point of 2 or greater on a scale of 1-3) was the FAST3-P, which includes pain VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater. The FAST index with the greatest specificity (90.3% at a cut point of score of 3 or greater on a scale of 1-4) was the FAST4 index, which includes a pain VAS score of 6 or greater, fatigue VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater.
Although the findings are limited by the lack of a gold standard for fibromyalgia diagnosis, changing diagnostic criteria, and a need for physician input for a fibromyalgia diagnosis, the study provides useful real-world data and supports findings from some prior studies with respect to the benefit of using these tools in routine practice.
With minimal extra physician time – if the MDHAQ is completed by patients at the time of registration – this approach can be used in all rheumatology patients to help identify fibromyalgia, he concluded.
Dr. Schmukler reported having no disclosures. One of his coauthors at Rush, Ted Pincus, MD, receives royalties and license fees for the copyright and trademark for the MDHAQ and RAPID3, all of which go to support clinical research.
SOURCE: Schmukler J et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 839.
CHICAGO – Fibromyalgia assessment screening tool (FAST) indices derived from the Multidimensional Health Assessment Questionnaire (MDHAQ) provide a simple and effective method for identifying fibromyalgia in routine care, according to findings from a series of more than 500 patients.
The indices are as accurate as the existing – and more complex – diagnostic criteria for fibromyalgia, Juan Schmukler, MD, reported at the annual meeting of the American College of Rheumatology.
For example, three FAST indices developed in the course of the study had better performance versus existing diagnostic criteria than did certain individual MDHAQ scales alone (area under the curve range, 0.924-0.937 vs. 0.829-0.889, respectively), said Dr. Schmukler, who conducted the research as a medical student at Rush Medical College, Chicago, and is now a rheumatology fellow at Mount Sinai Hospital in Chicago.
The findings are notable, because the two-page MDHAQ and a summary index (the RAPID3) derived from three of the MDHAQ scales are already used routinely in clinical care for diagnosing rheumatic diseases, and the new indices could easily – and with minimal work flow disruption – also be incorporated for each patient at each visit.
“Fibromyalgia is common in the general population and it is believed to be more common in patients with other rheumatic diagnoses,” Dr. Schmukler said. “Fibromyalgia may be easily recognized in many cases, but it can also be very subtle, particularly in patients who have other rheumatic diseases.”
ACR fibromyalgia classification criteria published in 1990 were based on tender point examination and non-ACR diagnostic criteria as revised in 2011 are based entirely on patient self-report.
A one-page fibromyalgia criteria questionnaire is available and is useful in clinical trials and other research, but is “rarely, if ever” used in routine care, he said, explaining that the questionnaire contains two domains: a symptom severity score (0-12 scale) and a widespread pain index (0-19 scale).
The MDHAQ/RAPID3 is informative in RA, and has also been shown to be “useful in all rheumatic diseases in which it has been studied,” and at least three prior reports have suggested that the MDHAQ may also provide clues to the presence of fibromyalgia, Dr. Schmukler said.
“And we know from prior reports that patients with fibromyalgia reported the highest RAPID3 scores, compared to other rheumatic disease,” he added, explaining that the goal of the present study was to develop FAST cumulative indices based on the routine MDHAQ scales and using the 2011 diagnostic criteria as a reference standard.
All patients with all diagnoses seen at the Rush Medical College rheumatology clinic in Chicago complete the MDHAQ at all visits in routine care, and between April and July 2017, the fibromyalgia criteria questionnaire was also administered in 502 consecutive patients.
Of those patients, 131 met the 2011 fibromyalgia diagnostic criteria.
MDHAQ scores were analyzed for agreement with the fibromyalgia criteria questionnaire according to receiver operator characteristic curves for AUC and were compiled into three different FAST indices that included various combinations of either three or four of the MDHAQ measures that had the best agreement with the diagnostic criteria questionnaire as identified by the highest AUC values. Those were the 60-symptom checklist (AUC, 0.889), painful joint count (AUC, 0.870), fatigue visual analog scale (VAS; AUC, 0.860), and pain VAS (AUC, 0.829), Dr. Schmukler said.
Proposed cut points that reflected the optimal trade-off between specificity and sensitivity for each of the scales were scores of 6 or greater for the pain VAS and fatigue VAS, and scores of 16 or greater for the symptom checklist and painful joint count measure.
In addition to the better performance of each FAST index versus the 2011 criteria, their performance was also better than that of the RAPID3 versus the 2011 criteria (AUC, 0.848), which many clinicians use in practice without using the full MDHAQ for patient assessment, he said.
Further, the “very easily calculated” FAST indices performed as well as a “very difficult to calculate” polysymptomatic distress continuous scale derived from the fibromyalgia questionnaire to assess the degree of fibromyalgia symptoms, which had an AUC of 0.929 versus the 2011 criteria. The latter index requires complex mathematical calculations for scale conversion and thus is impractical in clinical practice, he noted.
The FAST indices also performed comparably with physician diagnoses as indicated in patient charts and with diagnoses based on tender point count as shown in prior studies.
The FAST index with the greatest sensitivity (85.5% at a cut point of 2 or greater on a scale of 1-3) was the FAST3-P, which includes pain VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater. The FAST index with the greatest specificity (90.3% at a cut point of score of 3 or greater on a scale of 1-4) was the FAST4 index, which includes a pain VAS score of 6 or greater, fatigue VAS score of 6 or greater, symptom checklist score of 16 or greater, and painful joint count of 16 or greater.
Although the findings are limited by the lack of a gold standard for fibromyalgia diagnosis, changing diagnostic criteria, and a need for physician input for a fibromyalgia diagnosis, the study provides useful real-world data and supports findings from some prior studies with respect to the benefit of using these tools in routine practice.
With minimal extra physician time – if the MDHAQ is completed by patients at the time of registration – this approach can be used in all rheumatology patients to help identify fibromyalgia, he concluded.
Dr. Schmukler reported having no disclosures. One of his coauthors at Rush, Ted Pincus, MD, receives royalties and license fees for the copyright and trademark for the MDHAQ and RAPID3, all of which go to support clinical research.
SOURCE: Schmukler J et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 839.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point:
Major finding: Each fibromyalgia assessment screening tool index had better performance versus 2011 diagnostic criteria (area under the curve, 0.924-0.937) than did individual scales alone (AUCs, 0.829-0.889) and the RAPID3 summary index (AUC, 0.848).
Study details: An assessment of fibromyalgia assessment screening tool indices developed in a series of 502 patients.
Disclosures: Dr. Schmukler reported having no disclosures. One of his coauthors at Rush, Ted Pincus, MD, receives royalties and license fees for the copyright and trademark for the Multidimensional Health Assessment Questionnaire and RAPID3, all of which go to support clinical research.
Source: Schmukler J et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 839.