User login
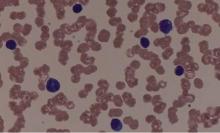
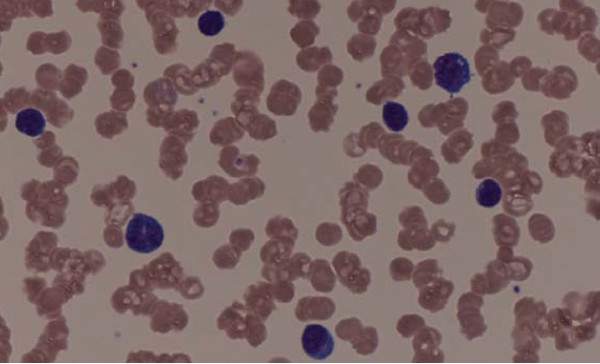
Androgen improved survival in elderly AML patients
Elderly patients with acute myeloid leukemia (AML) generally have a poor prognosis, but maintenance therapy with an androgen, norethandrolone, significantly improved survival in this population, investigators report in the Journal of Clinical Oncology.
The 5-year disease-free survival was almost double in patients who received norethandrolone (31.2% vs 16.2%), and event-free survival (EFS) and overall survival (OS) were also markedly improved.
A number of hypotheses could explain why norethandrolone improves outcomes in this population. “Because androgen supplementation was initiated when the tumoral mass was decreased, it is possible that norethandrolone decreased the proliferation of remaining blast cells and/or their genetic instability in restoring proper telomere length,” wrote Arnaud Pigneux, MD, PhD, of the Centre Hospitalier Universitaire, Bordeaux (France), and his coauthors. “In addition, as in aplastic anemia, a beneficial effect could be exerted by androgens on normal hematopoietic cells recovering after the end of the postinduction aplastic phase,” they said (J Clin Oncol. 2016 Oct 17. doi: 10.1200/JCO.2016.67.6213)
The majority of patients with AML are older than 60 years of age at the time of their diagnosis, and the prognosis is particularly poor for a number of reasons, including a greater intolerance to intensive chemotherapies and the presence of comorbidities. In addition, older patients also frequently present with unfavorable prognostic features, including multidrug resistant phenotypes or poor-risk cytogenetics.
In this study, Dr. Pigneux and his team enrolled 330 patients with AML de novo or secondary to chemotherapy or radiotherapy, who were 60 years of age or older. Induction therapy of idarubicin 8 mg/m2 on days 1 to 5, cytarabine 100 mg/m2 on days 1 to 7, and lomustine 200 mg/m2 on day 1 was administered.
Those who achieved complete or partial remission received six reinduction courses, alternating idarubicin and cytarabine, and a regimen of methotrexate and mercaptopurine. The cohort was then randomized to receive norethandrolone 10 or 20 mg/day (arm A) according to body weight, or no norethandrolone (arm B) for a 2-year maintenance therapy regimen.
Disease-free survival (DFS) was significantly improved in patients who received androgen therapy, but there was no difference between groups in patients with a high WBC count.
The 5-year DFS was 39.2% for arm A versus 15.1% in arm B for patients with a low WBC count, and 14.3% in arm A versus 20.8% in arm B for patients with a high WBC count.
From the time of inclusion, the 5-year EFS and OS were 21.5% (95% confidence interval, 15.5%-28.1%) and 26.3% (95% CI, 19.7%-33.2%), respectively, in arm A versus 12.9% (95% CI, 8.3%-18.5%) and 17.2% (95% CI, 11.9%-23.4%), respectively, in arm B.
For patients with unfavorable cytogenetics (n = 78), outcomes were better if they received norethandrolone.
The 5-year DFS for this subset was 15.79% in arm A versus 7.69% in arm B. For patients with low- or intermediate-risk cytogenetics, the 5-year DFS was 39.73% in arm A versus 19.72% in arm B.
No funding source was disclosed. Dr. Pigneux has disclosed consulting or advisory roles with Amgen, Celgene, MSD, and Novartis, and disclosed receiving funding for travel and accommodations expenses from Amgen and Pfizer. Several of the authors have disclosed relationships with industry.
Elderly patients with acute myeloid leukemia (AML) generally have a poor prognosis, but maintenance therapy with an androgen, norethandrolone, significantly improved survival in this population, investigators report in the Journal of Clinical Oncology.
The 5-year disease-free survival was almost double in patients who received norethandrolone (31.2% vs 16.2%), and event-free survival (EFS) and overall survival (OS) were also markedly improved.
A number of hypotheses could explain why norethandrolone improves outcomes in this population. “Because androgen supplementation was initiated when the tumoral mass was decreased, it is possible that norethandrolone decreased the proliferation of remaining blast cells and/or their genetic instability in restoring proper telomere length,” wrote Arnaud Pigneux, MD, PhD, of the Centre Hospitalier Universitaire, Bordeaux (France), and his coauthors. “In addition, as in aplastic anemia, a beneficial effect could be exerted by androgens on normal hematopoietic cells recovering after the end of the postinduction aplastic phase,” they said (J Clin Oncol. 2016 Oct 17. doi: 10.1200/JCO.2016.67.6213)
The majority of patients with AML are older than 60 years of age at the time of their diagnosis, and the prognosis is particularly poor for a number of reasons, including a greater intolerance to intensive chemotherapies and the presence of comorbidities. In addition, older patients also frequently present with unfavorable prognostic features, including multidrug resistant phenotypes or poor-risk cytogenetics.
In this study, Dr. Pigneux and his team enrolled 330 patients with AML de novo or secondary to chemotherapy or radiotherapy, who were 60 years of age or older. Induction therapy of idarubicin 8 mg/m2 on days 1 to 5, cytarabine 100 mg/m2 on days 1 to 7, and lomustine 200 mg/m2 on day 1 was administered.
Those who achieved complete or partial remission received six reinduction courses, alternating idarubicin and cytarabine, and a regimen of methotrexate and mercaptopurine. The cohort was then randomized to receive norethandrolone 10 or 20 mg/day (arm A) according to body weight, or no norethandrolone (arm B) for a 2-year maintenance therapy regimen.
Disease-free survival (DFS) was significantly improved in patients who received androgen therapy, but there was no difference between groups in patients with a high WBC count.
The 5-year DFS was 39.2% for arm A versus 15.1% in arm B for patients with a low WBC count, and 14.3% in arm A versus 20.8% in arm B for patients with a high WBC count.
From the time of inclusion, the 5-year EFS and OS were 21.5% (95% confidence interval, 15.5%-28.1%) and 26.3% (95% CI, 19.7%-33.2%), respectively, in arm A versus 12.9% (95% CI, 8.3%-18.5%) and 17.2% (95% CI, 11.9%-23.4%), respectively, in arm B.
For patients with unfavorable cytogenetics (n = 78), outcomes were better if they received norethandrolone.
The 5-year DFS for this subset was 15.79% in arm A versus 7.69% in arm B. For patients with low- or intermediate-risk cytogenetics, the 5-year DFS was 39.73% in arm A versus 19.72% in arm B.
No funding source was disclosed. Dr. Pigneux has disclosed consulting or advisory roles with Amgen, Celgene, MSD, and Novartis, and disclosed receiving funding for travel and accommodations expenses from Amgen and Pfizer. Several of the authors have disclosed relationships with industry.
Elderly patients with acute myeloid leukemia (AML) generally have a poor prognosis, but maintenance therapy with an androgen, norethandrolone, significantly improved survival in this population, investigators report in the Journal of Clinical Oncology.
The 5-year disease-free survival was almost double in patients who received norethandrolone (31.2% vs 16.2%), and event-free survival (EFS) and overall survival (OS) were also markedly improved.
A number of hypotheses could explain why norethandrolone improves outcomes in this population. “Because androgen supplementation was initiated when the tumoral mass was decreased, it is possible that norethandrolone decreased the proliferation of remaining blast cells and/or their genetic instability in restoring proper telomere length,” wrote Arnaud Pigneux, MD, PhD, of the Centre Hospitalier Universitaire, Bordeaux (France), and his coauthors. “In addition, as in aplastic anemia, a beneficial effect could be exerted by androgens on normal hematopoietic cells recovering after the end of the postinduction aplastic phase,” they said (J Clin Oncol. 2016 Oct 17. doi: 10.1200/JCO.2016.67.6213)
The majority of patients with AML are older than 60 years of age at the time of their diagnosis, and the prognosis is particularly poor for a number of reasons, including a greater intolerance to intensive chemotherapies and the presence of comorbidities. In addition, older patients also frequently present with unfavorable prognostic features, including multidrug resistant phenotypes or poor-risk cytogenetics.
In this study, Dr. Pigneux and his team enrolled 330 patients with AML de novo or secondary to chemotherapy or radiotherapy, who were 60 years of age or older. Induction therapy of idarubicin 8 mg/m2 on days 1 to 5, cytarabine 100 mg/m2 on days 1 to 7, and lomustine 200 mg/m2 on day 1 was administered.
Those who achieved complete or partial remission received six reinduction courses, alternating idarubicin and cytarabine, and a regimen of methotrexate and mercaptopurine. The cohort was then randomized to receive norethandrolone 10 or 20 mg/day (arm A) according to body weight, or no norethandrolone (arm B) for a 2-year maintenance therapy regimen.
Disease-free survival (DFS) was significantly improved in patients who received androgen therapy, but there was no difference between groups in patients with a high WBC count.
The 5-year DFS was 39.2% for arm A versus 15.1% in arm B for patients with a low WBC count, and 14.3% in arm A versus 20.8% in arm B for patients with a high WBC count.
From the time of inclusion, the 5-year EFS and OS were 21.5% (95% confidence interval, 15.5%-28.1%) and 26.3% (95% CI, 19.7%-33.2%), respectively, in arm A versus 12.9% (95% CI, 8.3%-18.5%) and 17.2% (95% CI, 11.9%-23.4%), respectively, in arm B.
For patients with unfavorable cytogenetics (n = 78), outcomes were better if they received norethandrolone.
The 5-year DFS for this subset was 15.79% in arm A versus 7.69% in arm B. For patients with low- or intermediate-risk cytogenetics, the 5-year DFS was 39.73% in arm A versus 19.72% in arm B.
No funding source was disclosed. Dr. Pigneux has disclosed consulting or advisory roles with Amgen, Celgene, MSD, and Novartis, and disclosed receiving funding for travel and accommodations expenses from Amgen and Pfizer. Several of the authors have disclosed relationships with industry.
Key clinical point: Maintenance therapy with norethandrolone improved outcomes in elderly patients with acute myeloid leukemia.
Major finding: 5-year disease-free survival was 31.2% (for the norethandrolone group) vs. 16.2% and event-free survival was 21.5% and 12.9%, respectively.
Data source: Prospective, randomized, multicenter, open-label phase III study that included 330 patients with AML.
Disclosures: No funding source was disclosed. Dr. Pigneux has disclosed consulting or advisory roles with Amgen, Celgene, MSD, and Novartis, and disclosed receiving funding for travel and accommodations expenses from Amgen and Pfizer. Several of the authors have also disclosed relationships with industry.
Oral bacterium linked to poor esophageal cancer survival
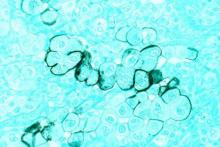
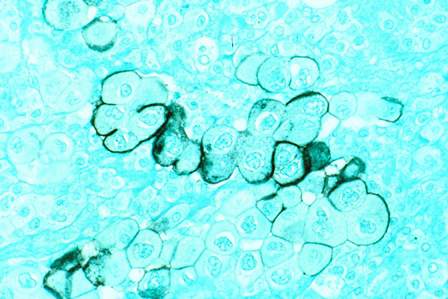
Fusobacterium nucleatum, a component of the human microbiome, appears to be associated with shorter survival in esophageal cancer, according to new findings.
F. nucleatum, generally found in the oral cavity and associated with periodontal disease, may have a potential role as a prognostic biomarker, and it might also contribute to aggressive tumor behavior via activation of chemokines, the study authors suggest (Clin Cancer Res. 2016 Oct. doi: 10.1158/1078-0432.CCR-16-1786).
They add that this is “the first study to provide the evidence for the relationship between F. nucleatum and poor prognosis in esophageal cancer.”
An assessment of F. nucleatum DNA in esophageal cancer tissues by qPCR assay showed that levels were higher in malignant tissue than in paired adjacent nontumor tissues (P = .021). The relative F. nucleatum DNA levels were also measured in samples from 325 esophageal cancer cases.
Within those samples, F. nucleatum was detected in 74 (23%) of 325 cases. F. nucleatum positivity was not associated with most clinicopathologic features including patient sex, year of surgery, preoperative performance status, smoking history, alcohol history, comorbidity, tumor location, histology, tumor size, or preoperative therapy (all P greater than .05). However, it was associated with tumor stage (P = .016), T stage (P less than .01), and N stage (P = .039).
There were a total of 112 deaths among the 325 esophageal cancer patients, with 75 specific to the disease. The median follow-up time for censored patients was 2.6 years.
Patients positive for F. nucleatum had significantly shorter cancer-specific survival (logrank P = .0039) and overall survival (logrank P = .046) as compared with those who were F. nucleatum negative. In an analysis of F. nucleatum DNA status by Cox regression analysis, patients who were positive had significantly higher cancer-specific mortality as compared with those who were negative (hazard ratio, 2.01; P = .0068). After the analysis was adjusted for clinical, pathologic, and epidemiologic features, F. nucleatum positivity was associated with significantly higher cancer-specific mortality (multivariate HR, 1.78; P = .032), and similar findings were observed for overall mortality.
Dr. Yamamura and his team had also hypothesized that F. nucleatum might contribute to aggressive tumor behavior by activation of chemokines, and they were able to confirm that the presence or absence of F. nucleatum was significantly associated with CCL20 expression status, which was identified as the most upregulated chemokine.
*This article was updated 10/26/2016.
Fusobacterium nucleatum, a component of the human microbiome, appears to be associated with shorter survival in esophageal cancer, according to new findings.
F. nucleatum, generally found in the oral cavity and associated with periodontal disease, may have a potential role as a prognostic biomarker, and it might also contribute to aggressive tumor behavior via activation of chemokines, the study authors suggest (Clin Cancer Res. 2016 Oct. doi: 10.1158/1078-0432.CCR-16-1786).
They add that this is “the first study to provide the evidence for the relationship between F. nucleatum and poor prognosis in esophageal cancer.”
An assessment of F. nucleatum DNA in esophageal cancer tissues by qPCR assay showed that levels were higher in malignant tissue than in paired adjacent nontumor tissues (P = .021). The relative F. nucleatum DNA levels were also measured in samples from 325 esophageal cancer cases.
Within those samples, F. nucleatum was detected in 74 (23%) of 325 cases. F. nucleatum positivity was not associated with most clinicopathologic features including patient sex, year of surgery, preoperative performance status, smoking history, alcohol history, comorbidity, tumor location, histology, tumor size, or preoperative therapy (all P greater than .05). However, it was associated with tumor stage (P = .016), T stage (P less than .01), and N stage (P = .039).
There were a total of 112 deaths among the 325 esophageal cancer patients, with 75 specific to the disease. The median follow-up time for censored patients was 2.6 years.
Patients positive for F. nucleatum had significantly shorter cancer-specific survival (logrank P = .0039) and overall survival (logrank P = .046) as compared with those who were F. nucleatum negative. In an analysis of F. nucleatum DNA status by Cox regression analysis, patients who were positive had significantly higher cancer-specific mortality as compared with those who were negative (hazard ratio, 2.01; P = .0068). After the analysis was adjusted for clinical, pathologic, and epidemiologic features, F. nucleatum positivity was associated with significantly higher cancer-specific mortality (multivariate HR, 1.78; P = .032), and similar findings were observed for overall mortality.
Dr. Yamamura and his team had also hypothesized that F. nucleatum might contribute to aggressive tumor behavior by activation of chemokines, and they were able to confirm that the presence or absence of F. nucleatum was significantly associated with CCL20 expression status, which was identified as the most upregulated chemokine.
*This article was updated 10/26/2016.
Fusobacterium nucleatum, a component of the human microbiome, appears to be associated with shorter survival in esophageal cancer, according to new findings.
F. nucleatum, generally found in the oral cavity and associated with periodontal disease, may have a potential role as a prognostic biomarker, and it might also contribute to aggressive tumor behavior via activation of chemokines, the study authors suggest (Clin Cancer Res. 2016 Oct. doi: 10.1158/1078-0432.CCR-16-1786).
They add that this is “the first study to provide the evidence for the relationship between F. nucleatum and poor prognosis in esophageal cancer.”
An assessment of F. nucleatum DNA in esophageal cancer tissues by qPCR assay showed that levels were higher in malignant tissue than in paired adjacent nontumor tissues (P = .021). The relative F. nucleatum DNA levels were also measured in samples from 325 esophageal cancer cases.
Within those samples, F. nucleatum was detected in 74 (23%) of 325 cases. F. nucleatum positivity was not associated with most clinicopathologic features including patient sex, year of surgery, preoperative performance status, smoking history, alcohol history, comorbidity, tumor location, histology, tumor size, or preoperative therapy (all P greater than .05). However, it was associated with tumor stage (P = .016), T stage (P less than .01), and N stage (P = .039).
There were a total of 112 deaths among the 325 esophageal cancer patients, with 75 specific to the disease. The median follow-up time for censored patients was 2.6 years.
Patients positive for F. nucleatum had significantly shorter cancer-specific survival (logrank P = .0039) and overall survival (logrank P = .046) as compared with those who were F. nucleatum negative. In an analysis of F. nucleatum DNA status by Cox regression analysis, patients who were positive had significantly higher cancer-specific mortality as compared with those who were negative (hazard ratio, 2.01; P = .0068). After the analysis was adjusted for clinical, pathologic, and epidemiologic features, F. nucleatum positivity was associated with significantly higher cancer-specific mortality (multivariate HR, 1.78; P = .032), and similar findings were observed for overall mortality.
Dr. Yamamura and his team had also hypothesized that F. nucleatum might contribute to aggressive tumor behavior by activation of chemokines, and they were able to confirm that the presence or absence of F. nucleatum was significantly associated with CCL20 expression status, which was identified as the most upregulated chemokine.
*This article was updated 10/26/2016.
FROM CLINICAL CANCER RESEARCH
Key clinical point: F. nucleatum present in esophageal cancer tissue is associated with poorer prognosis.
Major finding: Patients positive for F. nucleatum had significantly shorter cancer-specific survival (logrank P = .0039) and OS (logrank P = .046).
Data source: Tissue samples from 325 patients with esophageal cancer.
Disclosures: This study was supported in part by the SGH Foundation. The authors have no disclosures.
R-CHOP and intensive R-HDS comparable in DLBCL
Two front-line treatment regimens for patients with high-risk diffuse large B-cell lymphomas (DLBCL) produced comparable outcomes, according to new data.
Patients who received rituximab combined with high-dose sequential chemotherapy (R-HDS) plus autologous stem-cell transplantation (ASCT) had similar results in terms of overall response rate and long-term outcomes, compared to patients treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
It was presumed that event-free survival would be improved with chemotherapy and ASCT, but that result was not observed at 3-year follow up, wrote Sergio Cortelazzo, MD, of Humanitas Gavazzeni, Bergamo, Italy, and coauthors.
“Our results indicate that CHOP chemotherapy, optimally supplemented by eight doses of rituximab, remains the standard of care also for this group of patients at higher risk for disease resistance or recurrence,” they wrote in a study published online ahead of print in the Journal of Clinical Oncology (J Clin Oncol. 2016 Oct 3. doi: 10.1200/JCO.2016.67.2980).
The benefit of R-HDS chemotherapy with ASCT as front-line therapy for this patient population is still a matter of debate. To address that issue, Dr. Cortelazzo and his colleagues conducted a phase III randomized trial in which 246 high-risk patients with a high-intermediate (56%) or high (44%) International Prognostic Index (IPI) score were assigned to receive either R-CHOP or R-HDS.
The primary efficacy endpoint was 3-year, event-free survival, and the results were analyzed on an intent-to-treat basis.
At a median follow-up of 5 years (range, 0.05-9.49), with an intent-to-treat analysis, the 3-year, event-free survival was 62% (95% CI, 54%-71%) for the R-CHOP arm, compared with 65% (95% CI, 56% to 74%) for those treated with R-HDS (P = .83; hazard ratio, 0.99; 95% CI, 0.66-1.48).
There was no difference in event-free survival even when analyzed within the IPI subgroups.
The 3-year progression free survival also did not significantly differ between groups; 65% in the R-CHOP arm (95% CI, 57% to 74%) versus 75% (95% CI, 67%-83%; P = .119) for the R-HDS arm in the whole population, as well as within IPI subgroups.
Of note, the 3-year disease-free survival was better in the R-HDS group (79% vs. 91%, respectively; P = .034), but this difference subsequently disappeared with longer follow-up.
Grade 3-4 hematologic toxicity was lower in the R-CHOP arm compared with the R-HDS arm, with at least one episode of neutropenia in 34% versus 84% of patients (P less than .001), anemia in 15% versus 71% of patients (P less than .001), and thrombocytopenia in 5% versus 86% (P less than .001).
The study was supported in part by the Associazione Italiana Lotta alla Leucemia sezione di Bergamo, the Associazione Italiana per la Ricerca sul Cancro, Ministero Istruzione, Universita e Ricerca and unrestricted grants from Roche SpA and Amgen, Italy. Dr Cortelazzo had no relevant disclosures. Several coauthors indicated relationships with industry.
Two front-line treatment regimens for patients with high-risk diffuse large B-cell lymphomas (DLBCL) produced comparable outcomes, according to new data.
Patients who received rituximab combined with high-dose sequential chemotherapy (R-HDS) plus autologous stem-cell transplantation (ASCT) had similar results in terms of overall response rate and long-term outcomes, compared to patients treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
It was presumed that event-free survival would be improved with chemotherapy and ASCT, but that result was not observed at 3-year follow up, wrote Sergio Cortelazzo, MD, of Humanitas Gavazzeni, Bergamo, Italy, and coauthors.
“Our results indicate that CHOP chemotherapy, optimally supplemented by eight doses of rituximab, remains the standard of care also for this group of patients at higher risk for disease resistance or recurrence,” they wrote in a study published online ahead of print in the Journal of Clinical Oncology (J Clin Oncol. 2016 Oct 3. doi: 10.1200/JCO.2016.67.2980).
The benefit of R-HDS chemotherapy with ASCT as front-line therapy for this patient population is still a matter of debate. To address that issue, Dr. Cortelazzo and his colleagues conducted a phase III randomized trial in which 246 high-risk patients with a high-intermediate (56%) or high (44%) International Prognostic Index (IPI) score were assigned to receive either R-CHOP or R-HDS.
The primary efficacy endpoint was 3-year, event-free survival, and the results were analyzed on an intent-to-treat basis.
At a median follow-up of 5 years (range, 0.05-9.49), with an intent-to-treat analysis, the 3-year, event-free survival was 62% (95% CI, 54%-71%) for the R-CHOP arm, compared with 65% (95% CI, 56% to 74%) for those treated with R-HDS (P = .83; hazard ratio, 0.99; 95% CI, 0.66-1.48).
There was no difference in event-free survival even when analyzed within the IPI subgroups.
The 3-year progression free survival also did not significantly differ between groups; 65% in the R-CHOP arm (95% CI, 57% to 74%) versus 75% (95% CI, 67%-83%; P = .119) for the R-HDS arm in the whole population, as well as within IPI subgroups.
Of note, the 3-year disease-free survival was better in the R-HDS group (79% vs. 91%, respectively; P = .034), but this difference subsequently disappeared with longer follow-up.
Grade 3-4 hematologic toxicity was lower in the R-CHOP arm compared with the R-HDS arm, with at least one episode of neutropenia in 34% versus 84% of patients (P less than .001), anemia in 15% versus 71% of patients (P less than .001), and thrombocytopenia in 5% versus 86% (P less than .001).
The study was supported in part by the Associazione Italiana Lotta alla Leucemia sezione di Bergamo, the Associazione Italiana per la Ricerca sul Cancro, Ministero Istruzione, Universita e Ricerca and unrestricted grants from Roche SpA and Amgen, Italy. Dr Cortelazzo had no relevant disclosures. Several coauthors indicated relationships with industry.
Two front-line treatment regimens for patients with high-risk diffuse large B-cell lymphomas (DLBCL) produced comparable outcomes, according to new data.
Patients who received rituximab combined with high-dose sequential chemotherapy (R-HDS) plus autologous stem-cell transplantation (ASCT) had similar results in terms of overall response rate and long-term outcomes, compared to patients treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
It was presumed that event-free survival would be improved with chemotherapy and ASCT, but that result was not observed at 3-year follow up, wrote Sergio Cortelazzo, MD, of Humanitas Gavazzeni, Bergamo, Italy, and coauthors.
“Our results indicate that CHOP chemotherapy, optimally supplemented by eight doses of rituximab, remains the standard of care also for this group of patients at higher risk for disease resistance or recurrence,” they wrote in a study published online ahead of print in the Journal of Clinical Oncology (J Clin Oncol. 2016 Oct 3. doi: 10.1200/JCO.2016.67.2980).
The benefit of R-HDS chemotherapy with ASCT as front-line therapy for this patient population is still a matter of debate. To address that issue, Dr. Cortelazzo and his colleagues conducted a phase III randomized trial in which 246 high-risk patients with a high-intermediate (56%) or high (44%) International Prognostic Index (IPI) score were assigned to receive either R-CHOP or R-HDS.
The primary efficacy endpoint was 3-year, event-free survival, and the results were analyzed on an intent-to-treat basis.
At a median follow-up of 5 years (range, 0.05-9.49), with an intent-to-treat analysis, the 3-year, event-free survival was 62% (95% CI, 54%-71%) for the R-CHOP arm, compared with 65% (95% CI, 56% to 74%) for those treated with R-HDS (P = .83; hazard ratio, 0.99; 95% CI, 0.66-1.48).
There was no difference in event-free survival even when analyzed within the IPI subgroups.
The 3-year progression free survival also did not significantly differ between groups; 65% in the R-CHOP arm (95% CI, 57% to 74%) versus 75% (95% CI, 67%-83%; P = .119) for the R-HDS arm in the whole population, as well as within IPI subgroups.
Of note, the 3-year disease-free survival was better in the R-HDS group (79% vs. 91%, respectively; P = .034), but this difference subsequently disappeared with longer follow-up.
Grade 3-4 hematologic toxicity was lower in the R-CHOP arm compared with the R-HDS arm, with at least one episode of neutropenia in 34% versus 84% of patients (P less than .001), anemia in 15% versus 71% of patients (P less than .001), and thrombocytopenia in 5% versus 86% (P less than .001).
The study was supported in part by the Associazione Italiana Lotta alla Leucemia sezione di Bergamo, the Associazione Italiana per la Ricerca sul Cancro, Ministero Istruzione, Universita e Ricerca and unrestricted grants from Roche SpA and Amgen, Italy. Dr Cortelazzo had no relevant disclosures. Several coauthors indicated relationships with industry.
Key clinical point:
Major finding: At a median follow-up of 5 years, the 3-year event-free survival was similar for both groups: 62% versus 65% (P = .83).
Data source: A randomized phase III trial that included 246 patients with diffuse large B-cell lymphomas.
Disclosures: The study was supported in part by the Associazione Italiana Lotta alla Leucemia sezione di Bergamo, the Associazione Italiana per la Ricerca sul Cancro, Ministero Istruzione, Universita e Ricerca and unrestricted grants from Roche SpA and Amgen, Italy. Dr Cortelazzo has no disclosures. Several coauthors indicate relationships with industry.
Expert panel offers treatment recommendations in Waldenström macroglobulinemia
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
FROM BLOOD
Palifosfamide plus doxorubicin does not improve survival in sarcoma
Palifosfamide added to doxorubicin did not improve survival outcomes in patients with metastatic soft tissue sarcoma, compared with doxorubicin alone, a study showed.
The phase III randomized trial did not meet its amended primary endpoint, as there was no significant difference in progression-free survival (PFS) among patients in the two-drug regimen arm.
“This study represents one of the largest international efforts among sarcoma centers to date,” wrote Christopher W. Ryan, MD, of the Oregon Health & Science University, Knight Cancer Institute, Portland, Ore., and his coauthors (J Clin Oncol. 2016 Sept 12. doi: 10.1200/JCO.2016.67.668).
“Single-agent doxorubicin thus remains a reference standard for the treatment of metastatic soft tissue sarcoma,” they wrote.
Doxorubicin has remained the standard first-line treatment for most sarcoma patients for more than 4 decades. Palifosfamide, a tris salt of isophosphoramide mustard, has previously demonstrated broad activity against sarcoma in experimental models.
In addition, a randomized phase II trial showed improved PFS for combined doxorubicin and palifosfamide, compared with doxorubicin alone, with a hazard ratio (HR) of 0.43 (95% CI, 0.19-0.95).
Based on those promising results, Dr. Ryan and his colleagues conducted a phase III trial that evaluated the two-drug combination with doxorubicin alone as first-line treatment of metastatic soft tissue sarcoma.
The cohort included 447 patients who were randomly assigned 1:1 to receive either doxorubicin 75 mg/m2 IV on day 1 plus palifosfamide 150 mg/m2 per day IV on days 1-3, or doxorubicin plus placebo once every 21 days for up to six cycles.
The primary endpoint of the study was PFS by independent radiologic review.
There was no significant difference in PFS between the two cohorts. For the combination therapy group, the median PFS was 6.0 months, compared with 5.2 months for doxorubicin plus placebo (HR, 0.86; 95% CI, 0.68-1.08; P = .19).
Similar results were observed for median overall survival, which was also similar in the two treatment groups: 15.9 months for doxorubicin plus palifosfamide and 16.9 months for doxorubicin plus placebo (HR, 1.05; 95% CI, 0.79-1.39; P = .74).
As for toxicity, all patients had at least one treatment-emergent adverse event, with the most common of any grade being alopecia, nausea, and fatigue.
Grade 3-4 adverse events were more frequently observed in patients receiving doxorubicin plus palifosfamide (63.6%) than in the single-therapy group (50.9%; P = .0075).
“The median PFS of 5.2 months and OS [overall survival] of nearly 17 months with doxorubicin should serve as a reference in the design of future studies in the first-line treatment of metastatic soft tissue sarcoma,” Dr. Ryan and his associates said.
The study was supported by ZIOPHARM Oncology. Dr. Ryan and several of the coauthors reported multiple relationships with industry.
Palifosfamide added to doxorubicin did not improve survival outcomes in patients with metastatic soft tissue sarcoma, compared with doxorubicin alone, a study showed.
The phase III randomized trial did not meet its amended primary endpoint, as there was no significant difference in progression-free survival (PFS) among patients in the two-drug regimen arm.
“This study represents one of the largest international efforts among sarcoma centers to date,” wrote Christopher W. Ryan, MD, of the Oregon Health & Science University, Knight Cancer Institute, Portland, Ore., and his coauthors (J Clin Oncol. 2016 Sept 12. doi: 10.1200/JCO.2016.67.668).
“Single-agent doxorubicin thus remains a reference standard for the treatment of metastatic soft tissue sarcoma,” they wrote.
Doxorubicin has remained the standard first-line treatment for most sarcoma patients for more than 4 decades. Palifosfamide, a tris salt of isophosphoramide mustard, has previously demonstrated broad activity against sarcoma in experimental models.
In addition, a randomized phase II trial showed improved PFS for combined doxorubicin and palifosfamide, compared with doxorubicin alone, with a hazard ratio (HR) of 0.43 (95% CI, 0.19-0.95).
Based on those promising results, Dr. Ryan and his colleagues conducted a phase III trial that evaluated the two-drug combination with doxorubicin alone as first-line treatment of metastatic soft tissue sarcoma.
The cohort included 447 patients who were randomly assigned 1:1 to receive either doxorubicin 75 mg/m2 IV on day 1 plus palifosfamide 150 mg/m2 per day IV on days 1-3, or doxorubicin plus placebo once every 21 days for up to six cycles.
The primary endpoint of the study was PFS by independent radiologic review.
There was no significant difference in PFS between the two cohorts. For the combination therapy group, the median PFS was 6.0 months, compared with 5.2 months for doxorubicin plus placebo (HR, 0.86; 95% CI, 0.68-1.08; P = .19).
Similar results were observed for median overall survival, which was also similar in the two treatment groups: 15.9 months for doxorubicin plus palifosfamide and 16.9 months for doxorubicin plus placebo (HR, 1.05; 95% CI, 0.79-1.39; P = .74).
As for toxicity, all patients had at least one treatment-emergent adverse event, with the most common of any grade being alopecia, nausea, and fatigue.
Grade 3-4 adverse events were more frequently observed in patients receiving doxorubicin plus palifosfamide (63.6%) than in the single-therapy group (50.9%; P = .0075).
“The median PFS of 5.2 months and OS [overall survival] of nearly 17 months with doxorubicin should serve as a reference in the design of future studies in the first-line treatment of metastatic soft tissue sarcoma,” Dr. Ryan and his associates said.
The study was supported by ZIOPHARM Oncology. Dr. Ryan and several of the coauthors reported multiple relationships with industry.
Palifosfamide added to doxorubicin did not improve survival outcomes in patients with metastatic soft tissue sarcoma, compared with doxorubicin alone, a study showed.
The phase III randomized trial did not meet its amended primary endpoint, as there was no significant difference in progression-free survival (PFS) among patients in the two-drug regimen arm.
“This study represents one of the largest international efforts among sarcoma centers to date,” wrote Christopher W. Ryan, MD, of the Oregon Health & Science University, Knight Cancer Institute, Portland, Ore., and his coauthors (J Clin Oncol. 2016 Sept 12. doi: 10.1200/JCO.2016.67.668).
“Single-agent doxorubicin thus remains a reference standard for the treatment of metastatic soft tissue sarcoma,” they wrote.
Doxorubicin has remained the standard first-line treatment for most sarcoma patients for more than 4 decades. Palifosfamide, a tris salt of isophosphoramide mustard, has previously demonstrated broad activity against sarcoma in experimental models.
In addition, a randomized phase II trial showed improved PFS for combined doxorubicin and palifosfamide, compared with doxorubicin alone, with a hazard ratio (HR) of 0.43 (95% CI, 0.19-0.95).
Based on those promising results, Dr. Ryan and his colleagues conducted a phase III trial that evaluated the two-drug combination with doxorubicin alone as first-line treatment of metastatic soft tissue sarcoma.
The cohort included 447 patients who were randomly assigned 1:1 to receive either doxorubicin 75 mg/m2 IV on day 1 plus palifosfamide 150 mg/m2 per day IV on days 1-3, or doxorubicin plus placebo once every 21 days for up to six cycles.
The primary endpoint of the study was PFS by independent radiologic review.
There was no significant difference in PFS between the two cohorts. For the combination therapy group, the median PFS was 6.0 months, compared with 5.2 months for doxorubicin plus placebo (HR, 0.86; 95% CI, 0.68-1.08; P = .19).
Similar results were observed for median overall survival, which was also similar in the two treatment groups: 15.9 months for doxorubicin plus palifosfamide and 16.9 months for doxorubicin plus placebo (HR, 1.05; 95% CI, 0.79-1.39; P = .74).
As for toxicity, all patients had at least one treatment-emergent adverse event, with the most common of any grade being alopecia, nausea, and fatigue.
Grade 3-4 adverse events were more frequently observed in patients receiving doxorubicin plus palifosfamide (63.6%) than in the single-therapy group (50.9%; P = .0075).
“The median PFS of 5.2 months and OS [overall survival] of nearly 17 months with doxorubicin should serve as a reference in the design of future studies in the first-line treatment of metastatic soft tissue sarcoma,” Dr. Ryan and his associates said.
The study was supported by ZIOPHARM Oncology. Dr. Ryan and several of the coauthors reported multiple relationships with industry.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Palifosfamide combined with doxorubicin did not improve survival in metastatic soft tissue sarcoma.
Major finding: The median progression-free survival was 6.0 months for palifosfamide/doxorubicin vs. 5.2 months for doxorubicin plus placebo (HR, 0.86; 95% CI, 0.68-1.08; P = 0.19).
Data source: A phase III randomized trial that included 447 patients with metastatic soft tissue sarcoma.
Disclosures: The study was supported by ZIOPHARM Oncology. Dr. Ryan and several of his coauthors reported multiple relationships with industry.
‘Meaningful’ antitumor activity with lenalidomide monotherapy in ATL
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Lenalidomide demonstrated clinical activity with acceptable toxicity in recurrent or relapsed ATL.
Major finding: The overall response rate was 42%, and this included four complete responses and one unconfirmed complete response.
Data source: Multicenter phase II trial comprising 26 patients with relapsed or recurrent ATL.
Disclosures: Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Neoadjuvant therapy improves survival in pancreatic cancer
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Neoadjuvant therapy improves outcomes in pancreatic cancer.
Major finding: Neoadjuvant therapy was associated with improved survival compared with surgery alone, with a median survival of 26 months vs. 21 months.
Data source: Retrospective database study that included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma.
Disclosures: No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Subclinical hypothyroidism: Treat or not?
The benefits of treating subclinical hypothyroidism with low-dose levothyroxine may outweigh the harms of delaying treatment until the condition has become symptomatic, requiring higher doses, according to one of the authors of a “Beyond the Guidelines” assessment of this controversy.
Last year, the U.S. Preventive Services Task Force issued guidelines and updated its 2004 recommendations, which essentially stated that there is no evidence to support treating subclinical hypothyroidism. In their own guidelines, the American Association of Clinical Endocrinologists and American Thyroid Association have instead advocated aggressive case-finding and recommend screening individuals who may be a high risk. These societies also argue that subclinical hypothyroidism can have an adverse effect on cardiovascular outcomes and therefore it merits case-findings.
In the June 6, 2016 issue of the Annals of Internal Medicine (doi: 10.7326/M16-0857), experts from Beth Israel Deaconess Medical Center in Boston offered differing perspectives on the issue, as to whether or not subclinical hypothyroidism should be treated.
They gave their viewpoints in the context of a case study:
Mrs. C is a 60-year-old woman who has experienced mild symptoms such as fatigue and constipation for about 10 years, and has a family history of “thyroid problems.” In 2012, her TSH level was slightly elevated (5.8 uIU/L), and in 2013, she reported fatigue, although her TSH level was similar (5.9 uIU/L) to the year before.
Her free thyroxine (T4) was normal (0.93 ng/dL), and given the stability of her TSH level, treatment was not initiated. Recently, she reported weight gain, intermittent constipation, and persistent fatigue. Currently she is being treated for hyperlipidemia with atorvastatin 10 mg daily as well as for cervical radiculitis. Two of her three sisters receive thyroid medication, and recently, her blood pressure was 136/79 mm Hg with a heart rate of 77 beats per minute. Her weight had increased by 9 pounds, to 156 pounds (body mass index, 29.6 kg/m2). Her thyroid examination was normal, and her TSH measurement was 6.5 uIU/ML and free T4 was 1 ng/dL.
Should she begin thyroid replacement therapy?
Dr. Pamela Hartzband noted that there is an “evidence base suggesting that patients like Ms. C may benefit with respect to both morbidity and mortality,” given her family history and elevated cholesterol levels. TSH is a sensitive indicator of primary hypothyroidism, and given that the patient’s levels have gradually increased, this is significant and suggests early thyroid failure. That said, in “reviewing the evidence for benefit of treatment, there are not only conflicting data but also conflicting interpretation[s] of the same data by different experts,” according to Dr. Hartzband.
However, subclinical hypothyroidism has been associated with a greater risk for both cardiovascular morbidity and mortality in some but not all prospective population-based studies.
Symptom relief is the primary goal for patients, and Mrs. C has described symptoms that are suggestive of hypothyroidism including fatigue, constipation, scalp hair loss, and weight gain and elevated TSH. There is a “paucity of evidence” demonstrating improvement with treatment of subclinical hypothyroidism. And while harms associated with treatment can also be a concern, there is remarkably limited evidence for harms related to the treatment of subclinical hypothyroidism, noted Dr. Hartzband of the division of endocrinology and metabolism and medical director of the Thyroid Biopsy Clinic at Beth Israel Deaconess Medical Center, Boston.
There is, however, speculation that patients might develop hyperthyroidism from being given excessive doses of levothyroxine, but this can be avoided by initiating treatment of subclinical hypothyroidism with low-dose levothyroxine (25-50 mcg).
Overall, when weighing the benefits and harms of treatment in this case, Dr. Hartzband would consider offering Ms. C a trial of levothyroxine. The reasoning is that based on family history, she is at increased risk for thyroid disease and was appropriately tested by measuring TSH. In addition, levothyroxine could lower her cholesterol levels and risk for heart disease, and she might be able to reduce or even discontinue her statin therapy.
“I believe that for Ms. C the potential for benefit outweighs potential risk,” wrote Dr. Hartzband. “If she does not feel better and if cholesterol is not improved, then levothyroxine could be stopped until her TSH rises further.”
Dr. Carol K. Bates of the division of general medicine and primary care at Beth Israel Deaconess Medical Center, Boston, leaned more toward holding back on treatment. For one thing, since there is a diurnal variation in TSH, the patient’s TSH values might have been normal if measured in the afternoon instead of the morning.
As far as the risk of heart disease, where much of the treatment debate is focused, she pointed out that while there is an association between congestive heart failure, coronary artery disease, and subclinical hypothyroidism, Mrs. C only has a mildly increased TSH.
There have also been arguments that treating subclinical hypothyroidism could lower cholesterol levels. Ms. C started on a statin in 2003 when her TSH was 3.5 and thus euthyroid. Any efforts to lower cholesterol might be done by adjusting her statin dose rather than adding levothyroxine.
Both over- and undertreatment with thyroid hormone replacement are common, she pointed out, and overtreatment has been associated with an increased risk for hip and major osteoporotic fracture, as well as increasing the risk for atrial fibrillation. She also noted that there is harm in medicalizing a normal condition, as the upper range of TSH is arbitrarily set based upon population data.
In the case of Mrs. C, Dr. Bates would explain that there is no risk for heart disease given the degree of thyroid dysfunction and, especially, that her goal of weight loss and symptom relief likely won’t happen.
If she did wish to be treated, Dr. Bates would also start her on a low dose. “If she were to embark on treatment, I would suggest monitoring her weight and symptoms,” she wrote. “While many authorities would recommend treatment at a calculated full replacement dose, my experience suggests that this risks overtreatment, and I would recommend starting at 25 to 50 mcg.”
The benefits of treating subclinical hypothyroidism with low-dose levothyroxine may outweigh the harms of delaying treatment until the condition has become symptomatic, requiring higher doses, according to one of the authors of a “Beyond the Guidelines” assessment of this controversy.
Last year, the U.S. Preventive Services Task Force issued guidelines and updated its 2004 recommendations, which essentially stated that there is no evidence to support treating subclinical hypothyroidism. In their own guidelines, the American Association of Clinical Endocrinologists and American Thyroid Association have instead advocated aggressive case-finding and recommend screening individuals who may be a high risk. These societies also argue that subclinical hypothyroidism can have an adverse effect on cardiovascular outcomes and therefore it merits case-findings.
In the June 6, 2016 issue of the Annals of Internal Medicine (doi: 10.7326/M16-0857), experts from Beth Israel Deaconess Medical Center in Boston offered differing perspectives on the issue, as to whether or not subclinical hypothyroidism should be treated.
They gave their viewpoints in the context of a case study:
Mrs. C is a 60-year-old woman who has experienced mild symptoms such as fatigue and constipation for about 10 years, and has a family history of “thyroid problems.” In 2012, her TSH level was slightly elevated (5.8 uIU/L), and in 2013, she reported fatigue, although her TSH level was similar (5.9 uIU/L) to the year before.
Her free thyroxine (T4) was normal (0.93 ng/dL), and given the stability of her TSH level, treatment was not initiated. Recently, she reported weight gain, intermittent constipation, and persistent fatigue. Currently she is being treated for hyperlipidemia with atorvastatin 10 mg daily as well as for cervical radiculitis. Two of her three sisters receive thyroid medication, and recently, her blood pressure was 136/79 mm Hg with a heart rate of 77 beats per minute. Her weight had increased by 9 pounds, to 156 pounds (body mass index, 29.6 kg/m2). Her thyroid examination was normal, and her TSH measurement was 6.5 uIU/ML and free T4 was 1 ng/dL.
Should she begin thyroid replacement therapy?
Dr. Pamela Hartzband noted that there is an “evidence base suggesting that patients like Ms. C may benefit with respect to both morbidity and mortality,” given her family history and elevated cholesterol levels. TSH is a sensitive indicator of primary hypothyroidism, and given that the patient’s levels have gradually increased, this is significant and suggests early thyroid failure. That said, in “reviewing the evidence for benefit of treatment, there are not only conflicting data but also conflicting interpretation[s] of the same data by different experts,” according to Dr. Hartzband.
However, subclinical hypothyroidism has been associated with a greater risk for both cardiovascular morbidity and mortality in some but not all prospective population-based studies.
Symptom relief is the primary goal for patients, and Mrs. C has described symptoms that are suggestive of hypothyroidism including fatigue, constipation, scalp hair loss, and weight gain and elevated TSH. There is a “paucity of evidence” demonstrating improvement with treatment of subclinical hypothyroidism. And while harms associated with treatment can also be a concern, there is remarkably limited evidence for harms related to the treatment of subclinical hypothyroidism, noted Dr. Hartzband of the division of endocrinology and metabolism and medical director of the Thyroid Biopsy Clinic at Beth Israel Deaconess Medical Center, Boston.
There is, however, speculation that patients might develop hyperthyroidism from being given excessive doses of levothyroxine, but this can be avoided by initiating treatment of subclinical hypothyroidism with low-dose levothyroxine (25-50 mcg).
Overall, when weighing the benefits and harms of treatment in this case, Dr. Hartzband would consider offering Ms. C a trial of levothyroxine. The reasoning is that based on family history, she is at increased risk for thyroid disease and was appropriately tested by measuring TSH. In addition, levothyroxine could lower her cholesterol levels and risk for heart disease, and she might be able to reduce or even discontinue her statin therapy.
“I believe that for Ms. C the potential for benefit outweighs potential risk,” wrote Dr. Hartzband. “If she does not feel better and if cholesterol is not improved, then levothyroxine could be stopped until her TSH rises further.”
Dr. Carol K. Bates of the division of general medicine and primary care at Beth Israel Deaconess Medical Center, Boston, leaned more toward holding back on treatment. For one thing, since there is a diurnal variation in TSH, the patient’s TSH values might have been normal if measured in the afternoon instead of the morning.
As far as the risk of heart disease, where much of the treatment debate is focused, she pointed out that while there is an association between congestive heart failure, coronary artery disease, and subclinical hypothyroidism, Mrs. C only has a mildly increased TSH.
There have also been arguments that treating subclinical hypothyroidism could lower cholesterol levels. Ms. C started on a statin in 2003 when her TSH was 3.5 and thus euthyroid. Any efforts to lower cholesterol might be done by adjusting her statin dose rather than adding levothyroxine.
Both over- and undertreatment with thyroid hormone replacement are common, she pointed out, and overtreatment has been associated with an increased risk for hip and major osteoporotic fracture, as well as increasing the risk for atrial fibrillation. She also noted that there is harm in medicalizing a normal condition, as the upper range of TSH is arbitrarily set based upon population data.
In the case of Mrs. C, Dr. Bates would explain that there is no risk for heart disease given the degree of thyroid dysfunction and, especially, that her goal of weight loss and symptom relief likely won’t happen.
If she did wish to be treated, Dr. Bates would also start her on a low dose. “If she were to embark on treatment, I would suggest monitoring her weight and symptoms,” she wrote. “While many authorities would recommend treatment at a calculated full replacement dose, my experience suggests that this risks overtreatment, and I would recommend starting at 25 to 50 mcg.”
The benefits of treating subclinical hypothyroidism with low-dose levothyroxine may outweigh the harms of delaying treatment until the condition has become symptomatic, requiring higher doses, according to one of the authors of a “Beyond the Guidelines” assessment of this controversy.
Last year, the U.S. Preventive Services Task Force issued guidelines and updated its 2004 recommendations, which essentially stated that there is no evidence to support treating subclinical hypothyroidism. In their own guidelines, the American Association of Clinical Endocrinologists and American Thyroid Association have instead advocated aggressive case-finding and recommend screening individuals who may be a high risk. These societies also argue that subclinical hypothyroidism can have an adverse effect on cardiovascular outcomes and therefore it merits case-findings.
In the June 6, 2016 issue of the Annals of Internal Medicine (doi: 10.7326/M16-0857), experts from Beth Israel Deaconess Medical Center in Boston offered differing perspectives on the issue, as to whether or not subclinical hypothyroidism should be treated.
They gave their viewpoints in the context of a case study:
Mrs. C is a 60-year-old woman who has experienced mild symptoms such as fatigue and constipation for about 10 years, and has a family history of “thyroid problems.” In 2012, her TSH level was slightly elevated (5.8 uIU/L), and in 2013, she reported fatigue, although her TSH level was similar (5.9 uIU/L) to the year before.
Her free thyroxine (T4) was normal (0.93 ng/dL), and given the stability of her TSH level, treatment was not initiated. Recently, she reported weight gain, intermittent constipation, and persistent fatigue. Currently she is being treated for hyperlipidemia with atorvastatin 10 mg daily as well as for cervical radiculitis. Two of her three sisters receive thyroid medication, and recently, her blood pressure was 136/79 mm Hg with a heart rate of 77 beats per minute. Her weight had increased by 9 pounds, to 156 pounds (body mass index, 29.6 kg/m2). Her thyroid examination was normal, and her TSH measurement was 6.5 uIU/ML and free T4 was 1 ng/dL.
Should she begin thyroid replacement therapy?
Dr. Pamela Hartzband noted that there is an “evidence base suggesting that patients like Ms. C may benefit with respect to both morbidity and mortality,” given her family history and elevated cholesterol levels. TSH is a sensitive indicator of primary hypothyroidism, and given that the patient’s levels have gradually increased, this is significant and suggests early thyroid failure. That said, in “reviewing the evidence for benefit of treatment, there are not only conflicting data but also conflicting interpretation[s] of the same data by different experts,” according to Dr. Hartzband.
However, subclinical hypothyroidism has been associated with a greater risk for both cardiovascular morbidity and mortality in some but not all prospective population-based studies.
Symptom relief is the primary goal for patients, and Mrs. C has described symptoms that are suggestive of hypothyroidism including fatigue, constipation, scalp hair loss, and weight gain and elevated TSH. There is a “paucity of evidence” demonstrating improvement with treatment of subclinical hypothyroidism. And while harms associated with treatment can also be a concern, there is remarkably limited evidence for harms related to the treatment of subclinical hypothyroidism, noted Dr. Hartzband of the division of endocrinology and metabolism and medical director of the Thyroid Biopsy Clinic at Beth Israel Deaconess Medical Center, Boston.
There is, however, speculation that patients might develop hyperthyroidism from being given excessive doses of levothyroxine, but this can be avoided by initiating treatment of subclinical hypothyroidism with low-dose levothyroxine (25-50 mcg).
Overall, when weighing the benefits and harms of treatment in this case, Dr. Hartzband would consider offering Ms. C a trial of levothyroxine. The reasoning is that based on family history, she is at increased risk for thyroid disease and was appropriately tested by measuring TSH. In addition, levothyroxine could lower her cholesterol levels and risk for heart disease, and she might be able to reduce or even discontinue her statin therapy.
“I believe that for Ms. C the potential for benefit outweighs potential risk,” wrote Dr. Hartzband. “If she does not feel better and if cholesterol is not improved, then levothyroxine could be stopped until her TSH rises further.”
Dr. Carol K. Bates of the division of general medicine and primary care at Beth Israel Deaconess Medical Center, Boston, leaned more toward holding back on treatment. For one thing, since there is a diurnal variation in TSH, the patient’s TSH values might have been normal if measured in the afternoon instead of the morning.
As far as the risk of heart disease, where much of the treatment debate is focused, she pointed out that while there is an association between congestive heart failure, coronary artery disease, and subclinical hypothyroidism, Mrs. C only has a mildly increased TSH.
There have also been arguments that treating subclinical hypothyroidism could lower cholesterol levels. Ms. C started on a statin in 2003 when her TSH was 3.5 and thus euthyroid. Any efforts to lower cholesterol might be done by adjusting her statin dose rather than adding levothyroxine.
Both over- and undertreatment with thyroid hormone replacement are common, she pointed out, and overtreatment has been associated with an increased risk for hip and major osteoporotic fracture, as well as increasing the risk for atrial fibrillation. She also noted that there is harm in medicalizing a normal condition, as the upper range of TSH is arbitrarily set based upon population data.
In the case of Mrs. C, Dr. Bates would explain that there is no risk for heart disease given the degree of thyroid dysfunction and, especially, that her goal of weight loss and symptom relief likely won’t happen.
If she did wish to be treated, Dr. Bates would also start her on a low dose. “If she were to embark on treatment, I would suggest monitoring her weight and symptoms,” she wrote. “While many authorities would recommend treatment at a calculated full replacement dose, my experience suggests that this risks overtreatment, and I would recommend starting at 25 to 50 mcg.”
FROM THE ANNALS OF INTERNAL MEDICINE
New interventions improve symptoms of GERD
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Treatment failure reduced in Barrett’s esophagus with endoscopic mucosal resection
The use of endoscopic mucosal resection (EMR) before radiofrequency ablation significantly reduced the risk for treatment failure among patients with Barrett’s esophagus–associated intramucosal adenocarcinoma (IMC) and dysplasia, according to new data published in the American Journal of Surgical Pathology.
Complete eradication of IMC/dysplasia on the first follow-up endoscopy after treatment was achieved in 86% of patients, while durable eradication, defined as a complete recurrence that persisted until the last follow-up, was achieved in 78% of patients. However, there was significant variation between the different study sites (P = .03) and outcomes were significantly impacted by the baseline extent of IMC and the use of EMR prior to radiofrequency ablation (RFA) therapy.
In addition, almost a quarter of all patients developed treatment-related strictures, usually in the setting of multiple EMRs, and recurrence occurred as a malignant stricture in one patient.
Radiofrequency ablation used with or without EMR, is a safe, effective, and durable treatment option for the treatment of dysplasia associated with Barrett’s esophagus. However, studies that have assessed the predictors of treatment failure in Barrett’s esophagus-associated intramucosal adenocarcinoma (IMC) are limited.
In this study, Dr. Agoston T. Agoston of the department of pathology at Brigham and Women’s Hospital, Boston, and his colleagues investigated the rate of Barrett’s esophagus–associated IMC eradication when using RFA, with or without EMR, in a multicenter setting. In addition, they attempted to identify clinical and pathologic predictors of treatment failure.
“We anticipate that these data will have significant implications for a personalized treatment approach to patients with BE [Barrett’s esophagus]–associated IMC,” wrote the authors.
They conducted a retrospective review of medical records from four tertiary care academic medical centers, and identified 78 patients who underwent RFA with or without EMR as the primary treatment for biopsy-proven IMC.
Some notable baseline differences were observed in patient characteristics at the different study sites, including baseline Barrett’s esophagus segment length (P = .06), baseline nodularity (P = .08), and percentage of tissue involved by IMC at pretreatment endoscopy and biopsy (P = .01).
Over a mean follow-up time of 26.4 months (range, 2-116 months), 86% of patients achieved complete eradication and 78% durable eradication of IMC/dysplasia.
Within the cohort, 11 patients failed to achieve complete eradication, and of the 67 patients who initially did, 6 patients (9.0%) had a subsequent recurrence of neoplasia (3.91 recurrences per 100 patient-years). This extrapolated to an overall rate of 22% for treatment failure (17/78 patients). Of the 17 patients who failed the treatment, 3 subsequently underwent esophagectomy, 1 received palliative measures in the setting of advanced neurological disease, and 1 patient is currently undergoing a repeat ablation procedure with curative intent.
Dr. Agoston and his team also identified 2 clinicopathologic factors that were significantly associated with treatment failure, and both remained significant on univariate and multivariate analysis. The first was that the use of EMR prior to RFA was associated with a significantly reduced risk for treatment failure (hazard ratio, 0.15; 95% confidence interval, 0.05-0.48; P = .001), and the second was that the extent of IMC involving at least 50% of the columnar metaplastic area was associated with a significantly increased risk for treatment failure (HR, 4.24; 95% CI, 1.53-11.7; P = .005).
They also observed similar results when the analysis of extent of IMC as a predictor was restricted to a subset of 43 cases in which the diagnosis of IMC was made on EMR specimens only (HR, 10.8; 95% CI, 2.30-50.8; P = .003).
“In conclusion, we have identified endoscopic and pathologic factors associated with treatment success in patients with BE-associated IMC treated with RFA with or without EMR,” they wrote. “Utilization of these predictors can help in identifying patients with a high probability of success and also those patients with a higher risk for treatment failure for whom a more aggressive initial approach may be justified” (Am J Surg Pathol. 2015 Dec 5. doi: 10.1097/PAS.0000000000000566).
Dr. Rothstein and Dr. Abrams have received research support previously from Barrx/ Covidien and C2 Therapeutics/Covidien, respectively. None of the other authors reported significant conflicts of interest.
The use of endoscopic mucosal resection (EMR) before radiofrequency ablation significantly reduced the risk for treatment failure among patients with Barrett’s esophagus–associated intramucosal adenocarcinoma (IMC) and dysplasia, according to new data published in the American Journal of Surgical Pathology.
Complete eradication of IMC/dysplasia on the first follow-up endoscopy after treatment was achieved in 86% of patients, while durable eradication, defined as a complete recurrence that persisted until the last follow-up, was achieved in 78% of patients. However, there was significant variation between the different study sites (P = .03) and outcomes were significantly impacted by the baseline extent of IMC and the use of EMR prior to radiofrequency ablation (RFA) therapy.
In addition, almost a quarter of all patients developed treatment-related strictures, usually in the setting of multiple EMRs, and recurrence occurred as a malignant stricture in one patient.
Radiofrequency ablation used with or without EMR, is a safe, effective, and durable treatment option for the treatment of dysplasia associated with Barrett’s esophagus. However, studies that have assessed the predictors of treatment failure in Barrett’s esophagus-associated intramucosal adenocarcinoma (IMC) are limited.
In this study, Dr. Agoston T. Agoston of the department of pathology at Brigham and Women’s Hospital, Boston, and his colleagues investigated the rate of Barrett’s esophagus–associated IMC eradication when using RFA, with or without EMR, in a multicenter setting. In addition, they attempted to identify clinical and pathologic predictors of treatment failure.
“We anticipate that these data will have significant implications for a personalized treatment approach to patients with BE [Barrett’s esophagus]–associated IMC,” wrote the authors.
They conducted a retrospective review of medical records from four tertiary care academic medical centers, and identified 78 patients who underwent RFA with or without EMR as the primary treatment for biopsy-proven IMC.
Some notable baseline differences were observed in patient characteristics at the different study sites, including baseline Barrett’s esophagus segment length (P = .06), baseline nodularity (P = .08), and percentage of tissue involved by IMC at pretreatment endoscopy and biopsy (P = .01).
Over a mean follow-up time of 26.4 months (range, 2-116 months), 86% of patients achieved complete eradication and 78% durable eradication of IMC/dysplasia.
Within the cohort, 11 patients failed to achieve complete eradication, and of the 67 patients who initially did, 6 patients (9.0%) had a subsequent recurrence of neoplasia (3.91 recurrences per 100 patient-years). This extrapolated to an overall rate of 22% for treatment failure (17/78 patients). Of the 17 patients who failed the treatment, 3 subsequently underwent esophagectomy, 1 received palliative measures in the setting of advanced neurological disease, and 1 patient is currently undergoing a repeat ablation procedure with curative intent.
Dr. Agoston and his team also identified 2 clinicopathologic factors that were significantly associated with treatment failure, and both remained significant on univariate and multivariate analysis. The first was that the use of EMR prior to RFA was associated with a significantly reduced risk for treatment failure (hazard ratio, 0.15; 95% confidence interval, 0.05-0.48; P = .001), and the second was that the extent of IMC involving at least 50% of the columnar metaplastic area was associated with a significantly increased risk for treatment failure (HR, 4.24; 95% CI, 1.53-11.7; P = .005).
They also observed similar results when the analysis of extent of IMC as a predictor was restricted to a subset of 43 cases in which the diagnosis of IMC was made on EMR specimens only (HR, 10.8; 95% CI, 2.30-50.8; P = .003).
“In conclusion, we have identified endoscopic and pathologic factors associated with treatment success in patients with BE-associated IMC treated with RFA with or without EMR,” they wrote. “Utilization of these predictors can help in identifying patients with a high probability of success and also those patients with a higher risk for treatment failure for whom a more aggressive initial approach may be justified” (Am J Surg Pathol. 2015 Dec 5. doi: 10.1097/PAS.0000000000000566).
Dr. Rothstein and Dr. Abrams have received research support previously from Barrx/ Covidien and C2 Therapeutics/Covidien, respectively. None of the other authors reported significant conflicts of interest.
The use of endoscopic mucosal resection (EMR) before radiofrequency ablation significantly reduced the risk for treatment failure among patients with Barrett’s esophagus–associated intramucosal adenocarcinoma (IMC) and dysplasia, according to new data published in the American Journal of Surgical Pathology.
Complete eradication of IMC/dysplasia on the first follow-up endoscopy after treatment was achieved in 86% of patients, while durable eradication, defined as a complete recurrence that persisted until the last follow-up, was achieved in 78% of patients. However, there was significant variation between the different study sites (P = .03) and outcomes were significantly impacted by the baseline extent of IMC and the use of EMR prior to radiofrequency ablation (RFA) therapy.
In addition, almost a quarter of all patients developed treatment-related strictures, usually in the setting of multiple EMRs, and recurrence occurred as a malignant stricture in one patient.
Radiofrequency ablation used with or without EMR, is a safe, effective, and durable treatment option for the treatment of dysplasia associated with Barrett’s esophagus. However, studies that have assessed the predictors of treatment failure in Barrett’s esophagus-associated intramucosal adenocarcinoma (IMC) are limited.
In this study, Dr. Agoston T. Agoston of the department of pathology at Brigham and Women’s Hospital, Boston, and his colleagues investigated the rate of Barrett’s esophagus–associated IMC eradication when using RFA, with or without EMR, in a multicenter setting. In addition, they attempted to identify clinical and pathologic predictors of treatment failure.
“We anticipate that these data will have significant implications for a personalized treatment approach to patients with BE [Barrett’s esophagus]–associated IMC,” wrote the authors.
They conducted a retrospective review of medical records from four tertiary care academic medical centers, and identified 78 patients who underwent RFA with or without EMR as the primary treatment for biopsy-proven IMC.
Some notable baseline differences were observed in patient characteristics at the different study sites, including baseline Barrett’s esophagus segment length (P = .06), baseline nodularity (P = .08), and percentage of tissue involved by IMC at pretreatment endoscopy and biopsy (P = .01).
Over a mean follow-up time of 26.4 months (range, 2-116 months), 86% of patients achieved complete eradication and 78% durable eradication of IMC/dysplasia.
Within the cohort, 11 patients failed to achieve complete eradication, and of the 67 patients who initially did, 6 patients (9.0%) had a subsequent recurrence of neoplasia (3.91 recurrences per 100 patient-years). This extrapolated to an overall rate of 22% for treatment failure (17/78 patients). Of the 17 patients who failed the treatment, 3 subsequently underwent esophagectomy, 1 received palliative measures in the setting of advanced neurological disease, and 1 patient is currently undergoing a repeat ablation procedure with curative intent.
Dr. Agoston and his team also identified 2 clinicopathologic factors that were significantly associated with treatment failure, and both remained significant on univariate and multivariate analysis. The first was that the use of EMR prior to RFA was associated with a significantly reduced risk for treatment failure (hazard ratio, 0.15; 95% confidence interval, 0.05-0.48; P = .001), and the second was that the extent of IMC involving at least 50% of the columnar metaplastic area was associated with a significantly increased risk for treatment failure (HR, 4.24; 95% CI, 1.53-11.7; P = .005).
They also observed similar results when the analysis of extent of IMC as a predictor was restricted to a subset of 43 cases in which the diagnosis of IMC was made on EMR specimens only (HR, 10.8; 95% CI, 2.30-50.8; P = .003).
“In conclusion, we have identified endoscopic and pathologic factors associated with treatment success in patients with BE-associated IMC treated with RFA with or without EMR,” they wrote. “Utilization of these predictors can help in identifying patients with a high probability of success and also those patients with a higher risk for treatment failure for whom a more aggressive initial approach may be justified” (Am J Surg Pathol. 2015 Dec 5. doi: 10.1097/PAS.0000000000000566).
Dr. Rothstein and Dr. Abrams have received research support previously from Barrx/ Covidien and C2 Therapeutics/Covidien, respectively. None of the other authors reported significant conflicts of interest.
FROM THE AMERICAN JOURNAL OF SURGICAL PATHOLOGY
Key clinical point: The use of EMR before radiofrequency ablation significantly reduced the risk for treatment failure for IMC associated with Barrett’s esophagus.
Major finding: The overall rate of complete and durable IMC eradication in Barrett’s esophagus was 86% and 78%, respectively, during a mean follow-up of about 2 years, but was significantly impacted by the baseline extent of IMC and the use of EMR.
Data source: A retrospective review of data from four tertiary care academic medical centers that included 78 patients and was conducted to determine the rate of IMC eradication when using RFA and EMR.
Disclosures: Dr. Rothstein and Dr. Abrams have received research support previously from Barrx/ Covidien and C2 Therapeutics/Covidien, respectively. None of the other authors reported significant conflicts of interest.