User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
COVID-19 in children: Weekly cases drop to 6-month low
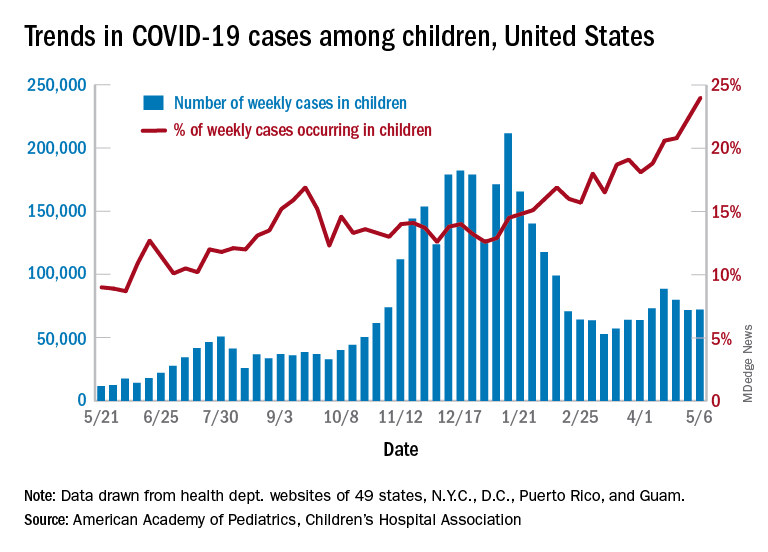
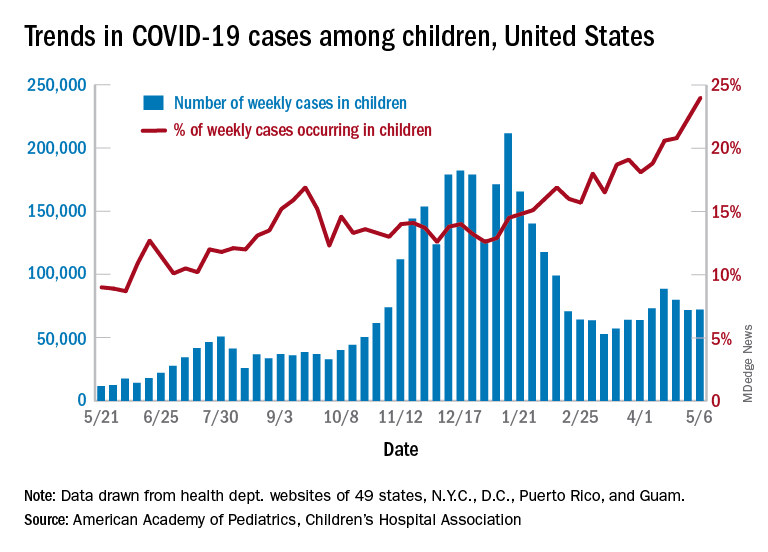
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
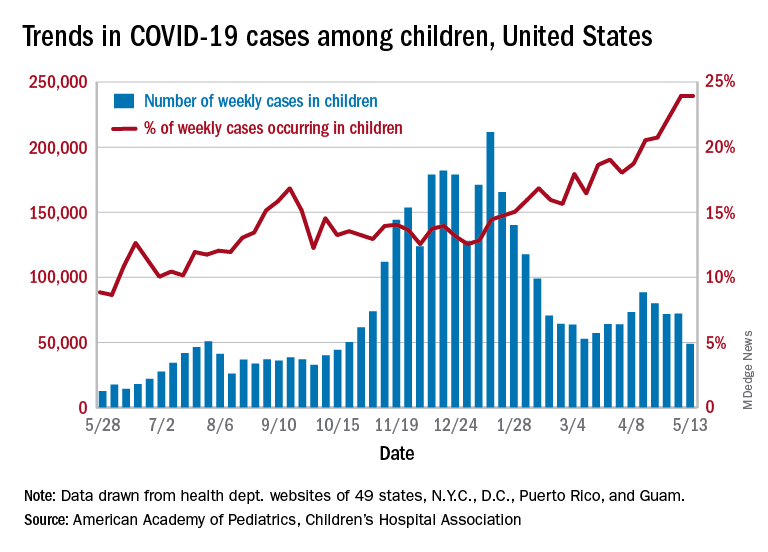
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
Canned diabetes prevention and a haunted COVID castle
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
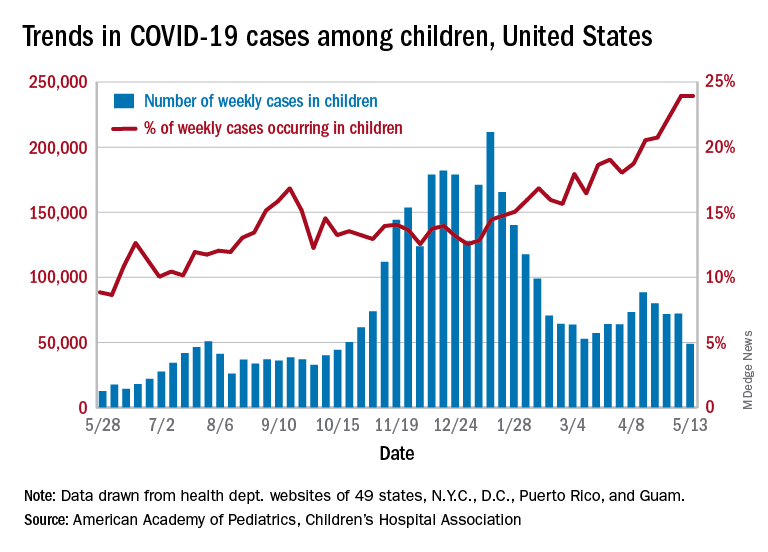
Small increase seen in new COVID-19 cases among children
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
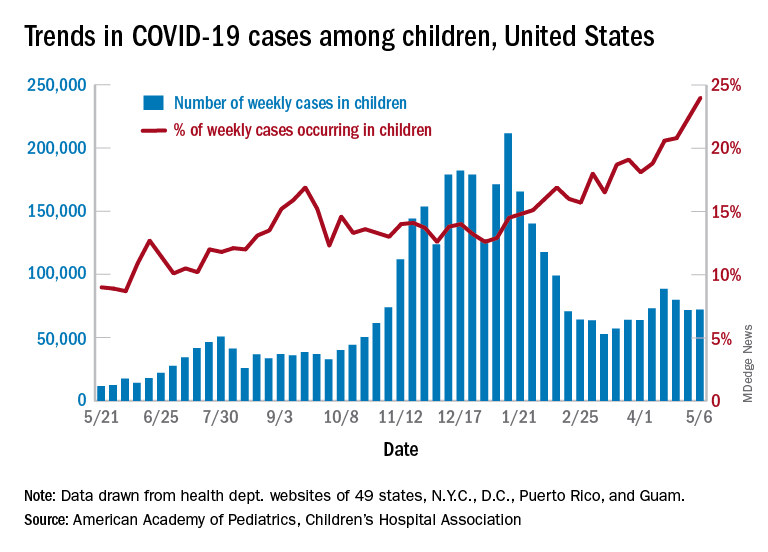
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
Possible obesity effect detected in cancer death rates

“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.

“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.

“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
FROM JAMA NETWORK OPEN
Pandemic took a cut of cosmetic procedures in 2020
pandemic, according to the American Society of Plastic Surgeons.
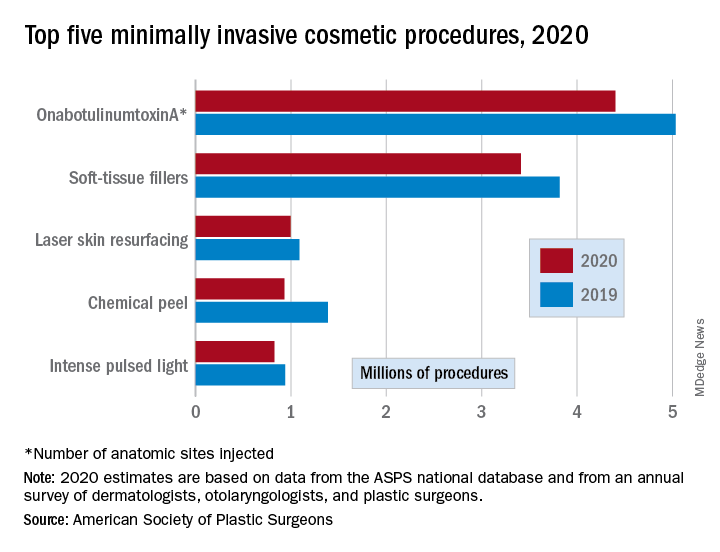
There were an estimated 15.6 million cosmetic procedures performed in 2020, compared with 18.4 million in 2019, a drop of 15.2%. Meanwhile, society members reported that they stopped performing elective surgery for an average of 8.1 weeks, which works out to 15.6% of a 52-week year, the ASPS said in its annual statistics report.
“The pandemic isn’t over, but thanks to vaccines, a new normal is starting to define itself – and some surgeons’ offices that were closed or offered only limited services within the last year are seeing higher demand,” Lynn Jeffers, MD, MBA, immediate past president of the ASPS, said in a written statement.
Minimally invasive procedures, which made up the majority of cosmetic procedures in 2020, dropped by a slightly higher 16%, compared with 14% on the surgical side. “Injectables continued to be the most sought-after treatments in 2020,” the ASPS said, with survey respondents citing “a significant uptick in demand during the coronavirus pandemic.”
OnabotuliumtoxinA injection, the most popular form of minimally invasive procedure, was down by 13% from 2019, while use of soft-tissue fillers fell by 11%. Laser skin resurfacing was third in popularity and had the smallest drop, just 8%, among the top five from 2019 to 2020, the ASPS data show.
The drop in volume for chemical peels was large enough (33%), to move it from third place in 2019 to fourth in 2020, and a slightly less than average drop of 12% moved intense pulsed-light treatments from sixth place in 2019 to fifth in 2020, switching places with laser hair removal (down 28%), the ASPS reported.
Among the surgical procedures, rhinoplasty was the most popular in 2020, as it was in 2019, after dropping by just 3%. Blepharoplasty was down by 8% from 2019, but two other common procedures, liposuction and breast augmentation, fell by 20% and 33%, respectively, the ASPS said.
pandemic, according to the American Society of Plastic Surgeons.
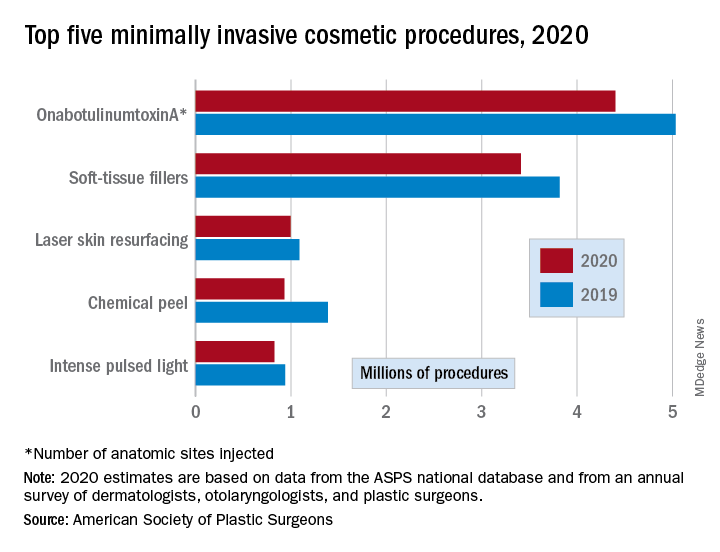
There were an estimated 15.6 million cosmetic procedures performed in 2020, compared with 18.4 million in 2019, a drop of 15.2%. Meanwhile, society members reported that they stopped performing elective surgery for an average of 8.1 weeks, which works out to 15.6% of a 52-week year, the ASPS said in its annual statistics report.
“The pandemic isn’t over, but thanks to vaccines, a new normal is starting to define itself – and some surgeons’ offices that were closed or offered only limited services within the last year are seeing higher demand,” Lynn Jeffers, MD, MBA, immediate past president of the ASPS, said in a written statement.
Minimally invasive procedures, which made up the majority of cosmetic procedures in 2020, dropped by a slightly higher 16%, compared with 14% on the surgical side. “Injectables continued to be the most sought-after treatments in 2020,” the ASPS said, with survey respondents citing “a significant uptick in demand during the coronavirus pandemic.”
OnabotuliumtoxinA injection, the most popular form of minimally invasive procedure, was down by 13% from 2019, while use of soft-tissue fillers fell by 11%. Laser skin resurfacing was third in popularity and had the smallest drop, just 8%, among the top five from 2019 to 2020, the ASPS data show.
The drop in volume for chemical peels was large enough (33%), to move it from third place in 2019 to fourth in 2020, and a slightly less than average drop of 12% moved intense pulsed-light treatments from sixth place in 2019 to fifth in 2020, switching places with laser hair removal (down 28%), the ASPS reported.
Among the surgical procedures, rhinoplasty was the most popular in 2020, as it was in 2019, after dropping by just 3%. Blepharoplasty was down by 8% from 2019, but two other common procedures, liposuction and breast augmentation, fell by 20% and 33%, respectively, the ASPS said.
pandemic, according to the American Society of Plastic Surgeons.
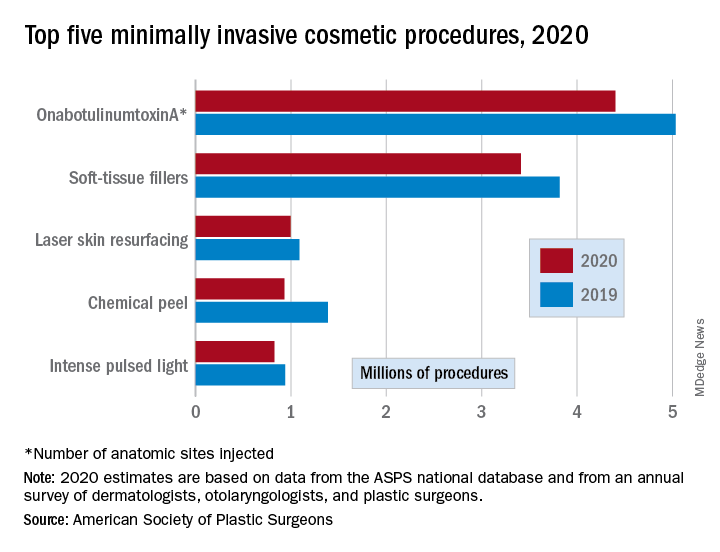
There were an estimated 15.6 million cosmetic procedures performed in 2020, compared with 18.4 million in 2019, a drop of 15.2%. Meanwhile, society members reported that they stopped performing elective surgery for an average of 8.1 weeks, which works out to 15.6% of a 52-week year, the ASPS said in its annual statistics report.
“The pandemic isn’t over, but thanks to vaccines, a new normal is starting to define itself – and some surgeons’ offices that were closed or offered only limited services within the last year are seeing higher demand,” Lynn Jeffers, MD, MBA, immediate past president of the ASPS, said in a written statement.
Minimally invasive procedures, which made up the majority of cosmetic procedures in 2020, dropped by a slightly higher 16%, compared with 14% on the surgical side. “Injectables continued to be the most sought-after treatments in 2020,” the ASPS said, with survey respondents citing “a significant uptick in demand during the coronavirus pandemic.”
OnabotuliumtoxinA injection, the most popular form of minimally invasive procedure, was down by 13% from 2019, while use of soft-tissue fillers fell by 11%. Laser skin resurfacing was third in popularity and had the smallest drop, just 8%, among the top five from 2019 to 2020, the ASPS data show.
The drop in volume for chemical peels was large enough (33%), to move it from third place in 2019 to fourth in 2020, and a slightly less than average drop of 12% moved intense pulsed-light treatments from sixth place in 2019 to fifth in 2020, switching places with laser hair removal (down 28%), the ASPS reported.
Among the surgical procedures, rhinoplasty was the most popular in 2020, as it was in 2019, after dropping by just 3%. Blepharoplasty was down by 8% from 2019, but two other common procedures, liposuction and breast augmentation, fell by 20% and 33%, respectively, the ASPS said.
Porous pill printing and prognostic poop
Printing meds per patient
What if there was a way to get exact doses of a medication, tailored specifically for each and every patient that needed it? Well, apparently it’s as easy as getting them out of a printer.
Researchers from the University of East Anglia in England may have found a new method to do just that.
Currently, medicine is “manufactured in ‘one-size-fits-all’ fashion,” said Dr. Sheng Qi, the research lead. But no patient is exactly the same, so why shouldn’t their medications be just as unique? Research on pharmaceutical 3D printing has been developing over the past 5 years, with the most common method requiring the drug to be put into “spaghetti-like filaments” before printing.
Dr. Qi and his team developed a process that bypasses the filaments, allowing them to 3D-print pills with varied porous structures that can regulate the rate of release of the drug into the body. This could be revolutionary for elderly patients and patients with complicated conditions – who often take many different drugs – to ensure more accurate doses that provide maximum benefits and minimal adverse effects.
Just as a custom-tailored suit perfectly fits the body for which it was made, the ability to tailor medication could have the same effect on a patient’s health. The only difference is what’s coming through the printer would be pills, not fabric.
It’s hip to be Pfizered
COVID-19 vaccination levels are rising, but we’ve heard a rumor that some people are still a bit reticent to participate. So how can physicians get more people to come in for a shot?
Make sure that they’re giving patients the right vaccine, for one thing. And by “right” vaccine, we mean, of course, the cool vaccine. Yes, the Internet has decided that the Pfizer vaccine is cooler than the others, according to the Atlantic.
There is, it seems, such a thing as “Pfizer superiority complex,” the article noted, while adding that, “on TikTok, hundreds of videos use a soundtrack of a woman explaining – slowly, voice full of disdain, like the rudest preschool teacher on Earth – ‘Only hot people get the Pfizer vaccine.’ ” A reporter from Slate was welcomed “to the ruling class” after sharing her upcoming Pfizer vaccination.
For the ultimate test of coolness, we surveyed the LOTME staff about the COVID-19 vaccines they had received. The results? Two Pfizers (coincidentally, the only two who knew what the hell TikTok is), one Moderna, one Johnson & Johnson, and one Godbold’s Vegetable Balsam (coincidentally, the same one who told us to get off his lawn).
And yes, we are checking on that last one.
Allergies stink!
A baby’s first bowel movement might mean more than just being the first of many diaper changes.
That particular bowel movement, called meconium, is a mixture of materials that have gone into a baby’s mouth late in the pregnancy, such as skin cells and amniotic fluid. Sounds lovely, right? The contents also include certain biochemicals and gut bacteria, and a lack of these can show an increased risk of allergies, eczema, and asthma.
Studies show that certain gut bacteria actually teach the immune system to accept compounds that are not harmful. Since allergies and other conditions are caused by a person’s immune system telling them harmless compounds are bad, it makes sense that lacking gut bacteria might show potential for developing such conditions.
Charisse Petersen, a researcher at the University of British Columbia in Vancouver, told NewScientist that parents could help decrease the development of allergies by not giving their children antibiotics that aren’t necessary and by letting kids play outside more.
Tom Marrs of King’s College London even noted that having a dog in the house is linked to a lower risk of allergies, so it might be time to get that puppy that the kids have been begging you for all through the pandemic.
Indiana Jones and the outhouse of parasites
Some archaeological finds are more impressive than others. Sometimes you find evidence of some long-lost civilization, sometimes you find a 200-year-old outhouse. That was the case with an outhouse buried near Dartmouth College that belonged to Mill Olcott, a wealthy businessman and politician who was a graduate of the college, and his family.
Now, that’s not particularly medically interesting, but the contents of the outhouse were very well preserved. That treasure trove included some fecal samples, and that’s where the story gets good, since they were preserved enough to be analyzed for parasites. Now, researchers know that parasites were very common in urban areas back in those days, when medicinal knowledge and sanitation were still deep in the dark ages, but whether or not people who lived in rural areas, wealthy or not, had them as well was a mystery.
Of course, 200-year-old poop is 200-year-old poop, so, in a task we wouldn’t envy anyone, the samples were rehydrated and run through several sieves to isolate the ancient goodies within. When all was said and done, both tapeworm and whipworm eggs were found, a surprise considering parasitic preference for warmer environments – not something northern New England is known for. But don’t forget, parasites can be your friend, too.
We will probably never know just which member of the Olcott household the poop belonged to, but the researchers noted that it was almost certain the entire house was infected. They added that, without proper infrastructure, even wealth was unable to protect people from disease. Hmm, we can’t think of any relevance that has in today’s world. Nope, absolutely none, since our health infrastructure is literally without flaw.
Printing meds per patient
What if there was a way to get exact doses of a medication, tailored specifically for each and every patient that needed it? Well, apparently it’s as easy as getting them out of a printer.
Researchers from the University of East Anglia in England may have found a new method to do just that.
Currently, medicine is “manufactured in ‘one-size-fits-all’ fashion,” said Dr. Sheng Qi, the research lead. But no patient is exactly the same, so why shouldn’t their medications be just as unique? Research on pharmaceutical 3D printing has been developing over the past 5 years, with the most common method requiring the drug to be put into “spaghetti-like filaments” before printing.
Dr. Qi and his team developed a process that bypasses the filaments, allowing them to 3D-print pills with varied porous structures that can regulate the rate of release of the drug into the body. This could be revolutionary for elderly patients and patients with complicated conditions – who often take many different drugs – to ensure more accurate doses that provide maximum benefits and minimal adverse effects.
Just as a custom-tailored suit perfectly fits the body for which it was made, the ability to tailor medication could have the same effect on a patient’s health. The only difference is what’s coming through the printer would be pills, not fabric.
It’s hip to be Pfizered
COVID-19 vaccination levels are rising, but we’ve heard a rumor that some people are still a bit reticent to participate. So how can physicians get more people to come in for a shot?
Make sure that they’re giving patients the right vaccine, for one thing. And by “right” vaccine, we mean, of course, the cool vaccine. Yes, the Internet has decided that the Pfizer vaccine is cooler than the others, according to the Atlantic.
There is, it seems, such a thing as “Pfizer superiority complex,” the article noted, while adding that, “on TikTok, hundreds of videos use a soundtrack of a woman explaining – slowly, voice full of disdain, like the rudest preschool teacher on Earth – ‘Only hot people get the Pfizer vaccine.’ ” A reporter from Slate was welcomed “to the ruling class” after sharing her upcoming Pfizer vaccination.
For the ultimate test of coolness, we surveyed the LOTME staff about the COVID-19 vaccines they had received. The results? Two Pfizers (coincidentally, the only two who knew what the hell TikTok is), one Moderna, one Johnson & Johnson, and one Godbold’s Vegetable Balsam (coincidentally, the same one who told us to get off his lawn).
And yes, we are checking on that last one.
Allergies stink!
A baby’s first bowel movement might mean more than just being the first of many diaper changes.
That particular bowel movement, called meconium, is a mixture of materials that have gone into a baby’s mouth late in the pregnancy, such as skin cells and amniotic fluid. Sounds lovely, right? The contents also include certain biochemicals and gut bacteria, and a lack of these can show an increased risk of allergies, eczema, and asthma.
Studies show that certain gut bacteria actually teach the immune system to accept compounds that are not harmful. Since allergies and other conditions are caused by a person’s immune system telling them harmless compounds are bad, it makes sense that lacking gut bacteria might show potential for developing such conditions.
Charisse Petersen, a researcher at the University of British Columbia in Vancouver, told NewScientist that parents could help decrease the development of allergies by not giving their children antibiotics that aren’t necessary and by letting kids play outside more.
Tom Marrs of King’s College London even noted that having a dog in the house is linked to a lower risk of allergies, so it might be time to get that puppy that the kids have been begging you for all through the pandemic.
Indiana Jones and the outhouse of parasites
Some archaeological finds are more impressive than others. Sometimes you find evidence of some long-lost civilization, sometimes you find a 200-year-old outhouse. That was the case with an outhouse buried near Dartmouth College that belonged to Mill Olcott, a wealthy businessman and politician who was a graduate of the college, and his family.
Now, that’s not particularly medically interesting, but the contents of the outhouse were very well preserved. That treasure trove included some fecal samples, and that’s where the story gets good, since they were preserved enough to be analyzed for parasites. Now, researchers know that parasites were very common in urban areas back in those days, when medicinal knowledge and sanitation were still deep in the dark ages, but whether or not people who lived in rural areas, wealthy or not, had them as well was a mystery.
Of course, 200-year-old poop is 200-year-old poop, so, in a task we wouldn’t envy anyone, the samples were rehydrated and run through several sieves to isolate the ancient goodies within. When all was said and done, both tapeworm and whipworm eggs were found, a surprise considering parasitic preference for warmer environments – not something northern New England is known for. But don’t forget, parasites can be your friend, too.
We will probably never know just which member of the Olcott household the poop belonged to, but the researchers noted that it was almost certain the entire house was infected. They added that, without proper infrastructure, even wealth was unable to protect people from disease. Hmm, we can’t think of any relevance that has in today’s world. Nope, absolutely none, since our health infrastructure is literally without flaw.
Printing meds per patient
What if there was a way to get exact doses of a medication, tailored specifically for each and every patient that needed it? Well, apparently it’s as easy as getting them out of a printer.
Researchers from the University of East Anglia in England may have found a new method to do just that.
Currently, medicine is “manufactured in ‘one-size-fits-all’ fashion,” said Dr. Sheng Qi, the research lead. But no patient is exactly the same, so why shouldn’t their medications be just as unique? Research on pharmaceutical 3D printing has been developing over the past 5 years, with the most common method requiring the drug to be put into “spaghetti-like filaments” before printing.
Dr. Qi and his team developed a process that bypasses the filaments, allowing them to 3D-print pills with varied porous structures that can regulate the rate of release of the drug into the body. This could be revolutionary for elderly patients and patients with complicated conditions – who often take many different drugs – to ensure more accurate doses that provide maximum benefits and minimal adverse effects.
Just as a custom-tailored suit perfectly fits the body for which it was made, the ability to tailor medication could have the same effect on a patient’s health. The only difference is what’s coming through the printer would be pills, not fabric.
It’s hip to be Pfizered
COVID-19 vaccination levels are rising, but we’ve heard a rumor that some people are still a bit reticent to participate. So how can physicians get more people to come in for a shot?
Make sure that they’re giving patients the right vaccine, for one thing. And by “right” vaccine, we mean, of course, the cool vaccine. Yes, the Internet has decided that the Pfizer vaccine is cooler than the others, according to the Atlantic.
There is, it seems, such a thing as “Pfizer superiority complex,” the article noted, while adding that, “on TikTok, hundreds of videos use a soundtrack of a woman explaining – slowly, voice full of disdain, like the rudest preschool teacher on Earth – ‘Only hot people get the Pfizer vaccine.’ ” A reporter from Slate was welcomed “to the ruling class” after sharing her upcoming Pfizer vaccination.
For the ultimate test of coolness, we surveyed the LOTME staff about the COVID-19 vaccines they had received. The results? Two Pfizers (coincidentally, the only two who knew what the hell TikTok is), one Moderna, one Johnson & Johnson, and one Godbold’s Vegetable Balsam (coincidentally, the same one who told us to get off his lawn).
And yes, we are checking on that last one.
Allergies stink!
A baby’s first bowel movement might mean more than just being the first of many diaper changes.
That particular bowel movement, called meconium, is a mixture of materials that have gone into a baby’s mouth late in the pregnancy, such as skin cells and amniotic fluid. Sounds lovely, right? The contents also include certain biochemicals and gut bacteria, and a lack of these can show an increased risk of allergies, eczema, and asthma.
Studies show that certain gut bacteria actually teach the immune system to accept compounds that are not harmful. Since allergies and other conditions are caused by a person’s immune system telling them harmless compounds are bad, it makes sense that lacking gut bacteria might show potential for developing such conditions.
Charisse Petersen, a researcher at the University of British Columbia in Vancouver, told NewScientist that parents could help decrease the development of allergies by not giving their children antibiotics that aren’t necessary and by letting kids play outside more.
Tom Marrs of King’s College London even noted that having a dog in the house is linked to a lower risk of allergies, so it might be time to get that puppy that the kids have been begging you for all through the pandemic.
Indiana Jones and the outhouse of parasites
Some archaeological finds are more impressive than others. Sometimes you find evidence of some long-lost civilization, sometimes you find a 200-year-old outhouse. That was the case with an outhouse buried near Dartmouth College that belonged to Mill Olcott, a wealthy businessman and politician who was a graduate of the college, and his family.
Now, that’s not particularly medically interesting, but the contents of the outhouse were very well preserved. That treasure trove included some fecal samples, and that’s where the story gets good, since they were preserved enough to be analyzed for parasites. Now, researchers know that parasites were very common in urban areas back in those days, when medicinal knowledge and sanitation were still deep in the dark ages, but whether or not people who lived in rural areas, wealthy or not, had them as well was a mystery.
Of course, 200-year-old poop is 200-year-old poop, so, in a task we wouldn’t envy anyone, the samples were rehydrated and run through several sieves to isolate the ancient goodies within. When all was said and done, both tapeworm and whipworm eggs were found, a surprise considering parasitic preference for warmer environments – not something northern New England is known for. But don’t forget, parasites can be your friend, too.
We will probably never know just which member of the Olcott household the poop belonged to, but the researchers noted that it was almost certain the entire house was infected. They added that, without proper infrastructure, even wealth was unable to protect people from disease. Hmm, we can’t think of any relevance that has in today’s world. Nope, absolutely none, since our health infrastructure is literally without flaw.
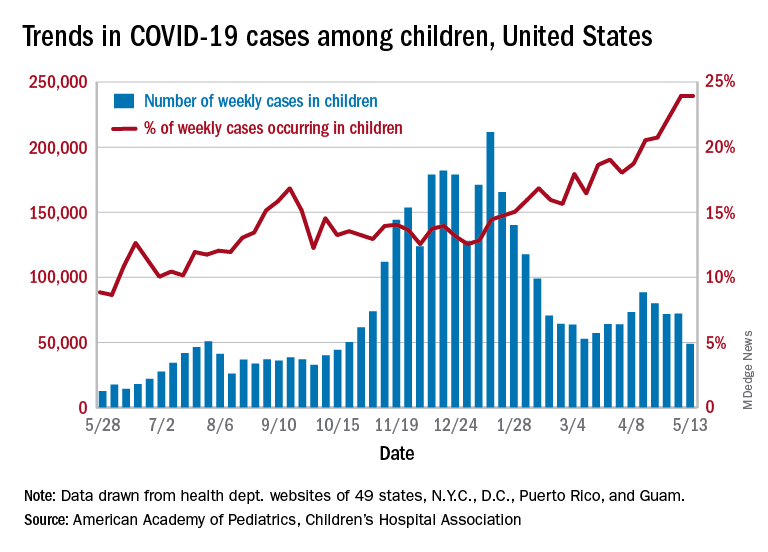
New child COVID-19 cases drop for second consecutive week
New cases of COVID-19 in children are trending downward again after dropping for a second consecutive week, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

Despite that drop, however, based on data in the weekly AAP/CHA report.
New cases totaled 71,649 for the week of April 23-29, down by 10.3% from the week before and by 19.0% over this most recent 2-week decline, but still a ways to go before reaching the low point of the year (52,695) recorded during the second week of March, the report shows.
Since the beginning of the pandemic, just over 3.78 million children have been infected by SARS-CoV-2, which is 13.8% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The overall rate of COVID-19 has reached 5,026 cases per 100,000 children, or 5% of the total pediatric population, although there is considerable variation among the states regarding age ranges used to define child cases. Most states use a range of 0-17 or 0-19 years, but Florida and Utah use a range of 0-14 years and South Carolina and Tennessee go with 0-20, the AAP and CHA noted.
There is also much variation between the states when it comes to cumulative child COVID-19 rates, with the lowest rate reported in Hawaii (1,264 per 100,000) and the highest in North Dakota (9,416 per 100,000). The lowest proportion of child cases to all cases is found in Florida (8.7%) and the highest in Vermont (22.2%), the AAP and CHA said.
The number of COVID-19–related deaths was 303 as of April 29, up by 7 from the previous week in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting mortality data by age. The proportion of child deaths to child cases remains at 0.01%, and children represent just 0.06% of all COVID-19 deaths, according to the AAP/CHA report.
New cases of COVID-19 in children are trending downward again after dropping for a second consecutive week, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

Despite that drop, however, based on data in the weekly AAP/CHA report.
New cases totaled 71,649 for the week of April 23-29, down by 10.3% from the week before and by 19.0% over this most recent 2-week decline, but still a ways to go before reaching the low point of the year (52,695) recorded during the second week of March, the report shows.
Since the beginning of the pandemic, just over 3.78 million children have been infected by SARS-CoV-2, which is 13.8% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The overall rate of COVID-19 has reached 5,026 cases per 100,000 children, or 5% of the total pediatric population, although there is considerable variation among the states regarding age ranges used to define child cases. Most states use a range of 0-17 or 0-19 years, but Florida and Utah use a range of 0-14 years and South Carolina and Tennessee go with 0-20, the AAP and CHA noted.
There is also much variation between the states when it comes to cumulative child COVID-19 rates, with the lowest rate reported in Hawaii (1,264 per 100,000) and the highest in North Dakota (9,416 per 100,000). The lowest proportion of child cases to all cases is found in Florida (8.7%) and the highest in Vermont (22.2%), the AAP and CHA said.
The number of COVID-19–related deaths was 303 as of April 29, up by 7 from the previous week in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting mortality data by age. The proportion of child deaths to child cases remains at 0.01%, and children represent just 0.06% of all COVID-19 deaths, according to the AAP/CHA report.
New cases of COVID-19 in children are trending downward again after dropping for a second consecutive week, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

Despite that drop, however, based on data in the weekly AAP/CHA report.
New cases totaled 71,649 for the week of April 23-29, down by 10.3% from the week before and by 19.0% over this most recent 2-week decline, but still a ways to go before reaching the low point of the year (52,695) recorded during the second week of March, the report shows.
Since the beginning of the pandemic, just over 3.78 million children have been infected by SARS-CoV-2, which is 13.8% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The overall rate of COVID-19 has reached 5,026 cases per 100,000 children, or 5% of the total pediatric population, although there is considerable variation among the states regarding age ranges used to define child cases. Most states use a range of 0-17 or 0-19 years, but Florida and Utah use a range of 0-14 years and South Carolina and Tennessee go with 0-20, the AAP and CHA noted.
There is also much variation between the states when it comes to cumulative child COVID-19 rates, with the lowest rate reported in Hawaii (1,264 per 100,000) and the highest in North Dakota (9,416 per 100,000). The lowest proportion of child cases to all cases is found in Florida (8.7%) and the highest in Vermont (22.2%), the AAP and CHA said.
The number of COVID-19–related deaths was 303 as of April 29, up by 7 from the previous week in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting mortality data by age. The proportion of child deaths to child cases remains at 0.01%, and children represent just 0.06% of all COVID-19 deaths, according to the AAP/CHA report.
Drinking your way to heart failure, and the fringe benefits of COVID-19 vaccination
Energy drink doom
Who doesn’t need some caffeine to get going in the morning and keep moving throughout the day? Whether it’s tea, coffee, or energy drinks, people can get addicted to caffeinated beverages when there are only so many hours in a day and way too much work to get done.
That’s what happened to a 21-year-old college student who powered down four 16-ounce cans of energy drink – each with double the amount of caffeine in an ordinary cup of coffee – every day for 2 years. Now, if you’ve ever overdone it with caffeine, you know there are some uncomfortable side effects, like shaking and anxiety. In this case, the student reported migraines, tremors, and heart palpitations. Instead of being able to focus better on his work, he had trouble concentrating.
Over time, after these side effects took a turn for the worse and became shortness of breath and weight loss, he visited St. Thomas’ Hospital in London, where physicians diagnosed him with both heart and renal failure.
Excessive consumption of energy drinks is known to cause issues such as high blood pressure and irregular heart beat, so if that’s your fuel of choice, it might be worth cutting down. Maybe take a morning run to get the blood pumping – in a good way – instead?
Loneliness may be hazardous to your health
Sometimes loneliness can feel like it affects your physical health, but according to a study there’s a possibility that it actually does.
Back in the 1980s, researchers from the University of Eastern Finland started monitoring almost 3,000 middle-aged men. They’ve kept up with the participants until the present day, and the results have been staggering. After an average follow-up of over 20 years, 25% of participants developed cancer and 11% died from cancer, and the increase in risk from loneliness was about 10%, regardless of age, lifestyle, and BMI.
What does that say about preventive care? The researchers think these data are cause enough to pay attention to loneliness as a health issue along with smoking and weight.
Social interactions and relationships play important roles in human mental health, of course, but this is pretty solid evidence that they play a role in physical health too. As the researchers said, “Awareness of the health effects of loneliness is constantly increasing. Therefore, it is important to examine, in more detail, the mechanisms by which loneliness causes adverse health effects.”
So, as we progress through this pandemic, maybe you should join that social group on Facebook? Who knows what kind of effect it could have on your health?
An ounce of prevention is worth 12 ounces of lager
COVID-19 vaccine refusal is now a thing, and there’s no law that says people have to be immunized against our newest, bestest buddy, SARS-CoV-2, but the folks who skip it are missing out. And no, we’re not talking about immunity against disease.
We’re talking … FREE STUFF!
Corporate America has stepped up and is now rewarding those who get the COVID-19 vaccine:
- Budweiser will give a free beer to anyone – anyone over age 21, that is – with proof of vaccination until May 16.
- Show a vaccination card at a Krispy Kreme and you can get a free glazed doughnut, every day. You don’t even need to buy anything.
- White Castle will give you a free dessert-on-a-stick just for showing proof of vaccination. No purchase is required, but the offer ends May 31.
But wait, there’s more!
Even the public sector is getting in on the giveaway action. Gov. Jim Justice announced April 26 that West Virginia will give a $100 savings bond to any resident aged 16-35 years who receives a COVID-19 vaccine. It must make sense, because the governor broke out a white board to show residents he’s done the math.
One closing thought: How cool would it be if he was named to the Supreme Court, so he could be Justice Justice?
Where no shirt has gone before
Space. The final frontier, for both humanity and for shirts. Specifically, it’s a new frontier for the Bio-Monitor smart shirt, a tank-top filled with sensors that monitor the wearer’s stats, such as heart and breathing rate, oxygen saturation, skin temperature, and blood pressure. And you thought space was just for finding a new human habitat and growing steak.
This shirt is already used by athletes to assess performance and by people with limited mobility to monitor health, so its potential impending usage by astronauts makes sense. Space is a pretty extreme environment, to put it mildly, and there’s a lot we still don’t know about how the human body reacts to it. Traditionally, astronauts hook themselves up to separate devices so their stats can be measured, a method which captures only snapshots of their bodies. By wearing the shirt constantly, the astronauts can be measured constantly, so scientists and doctors can see how the body deals with microgravity during normal activities and sleep. It also reduces stress, as there is no psychological impact of having to report in for constant health checks.
For the test, astronauts wore the shirt for 72 hours before flight and for 72 hours during flight. The shirts passed this first test with flying colors; in addition to providing accurate and more consistent stats monitoring than traditional methods, scientists on the ground determined that the astronauts recorded far less physical activity during flight than preflight, a finding in line with previous studies.
And before you question whether or not a tank top is really appropriate for space, just remember, Picard pulled it off at the end of “First Contact,” and that’s arguably the best Star Trek movie. So there’s certainly precedent.
Energy drink doom
Who doesn’t need some caffeine to get going in the morning and keep moving throughout the day? Whether it’s tea, coffee, or energy drinks, people can get addicted to caffeinated beverages when there are only so many hours in a day and way too much work to get done.
That’s what happened to a 21-year-old college student who powered down four 16-ounce cans of energy drink – each with double the amount of caffeine in an ordinary cup of coffee – every day for 2 years. Now, if you’ve ever overdone it with caffeine, you know there are some uncomfortable side effects, like shaking and anxiety. In this case, the student reported migraines, tremors, and heart palpitations. Instead of being able to focus better on his work, he had trouble concentrating.
Over time, after these side effects took a turn for the worse and became shortness of breath and weight loss, he visited St. Thomas’ Hospital in London, where physicians diagnosed him with both heart and renal failure.
Excessive consumption of energy drinks is known to cause issues such as high blood pressure and irregular heart beat, so if that’s your fuel of choice, it might be worth cutting down. Maybe take a morning run to get the blood pumping – in a good way – instead?
Loneliness may be hazardous to your health
Sometimes loneliness can feel like it affects your physical health, but according to a study there’s a possibility that it actually does.
Back in the 1980s, researchers from the University of Eastern Finland started monitoring almost 3,000 middle-aged men. They’ve kept up with the participants until the present day, and the results have been staggering. After an average follow-up of over 20 years, 25% of participants developed cancer and 11% died from cancer, and the increase in risk from loneliness was about 10%, regardless of age, lifestyle, and BMI.
What does that say about preventive care? The researchers think these data are cause enough to pay attention to loneliness as a health issue along with smoking and weight.
Social interactions and relationships play important roles in human mental health, of course, but this is pretty solid evidence that they play a role in physical health too. As the researchers said, “Awareness of the health effects of loneliness is constantly increasing. Therefore, it is important to examine, in more detail, the mechanisms by which loneliness causes adverse health effects.”
So, as we progress through this pandemic, maybe you should join that social group on Facebook? Who knows what kind of effect it could have on your health?
An ounce of prevention is worth 12 ounces of lager
COVID-19 vaccine refusal is now a thing, and there’s no law that says people have to be immunized against our newest, bestest buddy, SARS-CoV-2, but the folks who skip it are missing out. And no, we’re not talking about immunity against disease.
We’re talking … FREE STUFF!
Corporate America has stepped up and is now rewarding those who get the COVID-19 vaccine:
- Budweiser will give a free beer to anyone – anyone over age 21, that is – with proof of vaccination until May 16.
- Show a vaccination card at a Krispy Kreme and you can get a free glazed doughnut, every day. You don’t even need to buy anything.
- White Castle will give you a free dessert-on-a-stick just for showing proof of vaccination. No purchase is required, but the offer ends May 31.
But wait, there’s more!
Even the public sector is getting in on the giveaway action. Gov. Jim Justice announced April 26 that West Virginia will give a $100 savings bond to any resident aged 16-35 years who receives a COVID-19 vaccine. It must make sense, because the governor broke out a white board to show residents he’s done the math.
One closing thought: How cool would it be if he was named to the Supreme Court, so he could be Justice Justice?
Where no shirt has gone before
Space. The final frontier, for both humanity and for shirts. Specifically, it’s a new frontier for the Bio-Monitor smart shirt, a tank-top filled with sensors that monitor the wearer’s stats, such as heart and breathing rate, oxygen saturation, skin temperature, and blood pressure. And you thought space was just for finding a new human habitat and growing steak.
This shirt is already used by athletes to assess performance and by people with limited mobility to monitor health, so its potential impending usage by astronauts makes sense. Space is a pretty extreme environment, to put it mildly, and there’s a lot we still don’t know about how the human body reacts to it. Traditionally, astronauts hook themselves up to separate devices so their stats can be measured, a method which captures only snapshots of their bodies. By wearing the shirt constantly, the astronauts can be measured constantly, so scientists and doctors can see how the body deals with microgravity during normal activities and sleep. It also reduces stress, as there is no psychological impact of having to report in for constant health checks.
For the test, astronauts wore the shirt for 72 hours before flight and for 72 hours during flight. The shirts passed this first test with flying colors; in addition to providing accurate and more consistent stats monitoring than traditional methods, scientists on the ground determined that the astronauts recorded far less physical activity during flight than preflight, a finding in line with previous studies.
And before you question whether or not a tank top is really appropriate for space, just remember, Picard pulled it off at the end of “First Contact,” and that’s arguably the best Star Trek movie. So there’s certainly precedent.
Energy drink doom
Who doesn’t need some caffeine to get going in the morning and keep moving throughout the day? Whether it’s tea, coffee, or energy drinks, people can get addicted to caffeinated beverages when there are only so many hours in a day and way too much work to get done.
That’s what happened to a 21-year-old college student who powered down four 16-ounce cans of energy drink – each with double the amount of caffeine in an ordinary cup of coffee – every day for 2 years. Now, if you’ve ever overdone it with caffeine, you know there are some uncomfortable side effects, like shaking and anxiety. In this case, the student reported migraines, tremors, and heart palpitations. Instead of being able to focus better on his work, he had trouble concentrating.
Over time, after these side effects took a turn for the worse and became shortness of breath and weight loss, he visited St. Thomas’ Hospital in London, where physicians diagnosed him with both heart and renal failure.
Excessive consumption of energy drinks is known to cause issues such as high blood pressure and irregular heart beat, so if that’s your fuel of choice, it might be worth cutting down. Maybe take a morning run to get the blood pumping – in a good way – instead?
Loneliness may be hazardous to your health
Sometimes loneliness can feel like it affects your physical health, but according to a study there’s a possibility that it actually does.
Back in the 1980s, researchers from the University of Eastern Finland started monitoring almost 3,000 middle-aged men. They’ve kept up with the participants until the present day, and the results have been staggering. After an average follow-up of over 20 years, 25% of participants developed cancer and 11% died from cancer, and the increase in risk from loneliness was about 10%, regardless of age, lifestyle, and BMI.
What does that say about preventive care? The researchers think these data are cause enough to pay attention to loneliness as a health issue along with smoking and weight.
Social interactions and relationships play important roles in human mental health, of course, but this is pretty solid evidence that they play a role in physical health too. As the researchers said, “Awareness of the health effects of loneliness is constantly increasing. Therefore, it is important to examine, in more detail, the mechanisms by which loneliness causes adverse health effects.”
So, as we progress through this pandemic, maybe you should join that social group on Facebook? Who knows what kind of effect it could have on your health?
An ounce of prevention is worth 12 ounces of lager
COVID-19 vaccine refusal is now a thing, and there’s no law that says people have to be immunized against our newest, bestest buddy, SARS-CoV-2, but the folks who skip it are missing out. And no, we’re not talking about immunity against disease.
We’re talking … FREE STUFF!
Corporate America has stepped up and is now rewarding those who get the COVID-19 vaccine:
- Budweiser will give a free beer to anyone – anyone over age 21, that is – with proof of vaccination until May 16.
- Show a vaccination card at a Krispy Kreme and you can get a free glazed doughnut, every day. You don’t even need to buy anything.
- White Castle will give you a free dessert-on-a-stick just for showing proof of vaccination. No purchase is required, but the offer ends May 31.
But wait, there’s more!
Even the public sector is getting in on the giveaway action. Gov. Jim Justice announced April 26 that West Virginia will give a $100 savings bond to any resident aged 16-35 years who receives a COVID-19 vaccine. It must make sense, because the governor broke out a white board to show residents he’s done the math.
One closing thought: How cool would it be if he was named to the Supreme Court, so he could be Justice Justice?
Where no shirt has gone before
Space. The final frontier, for both humanity and for shirts. Specifically, it’s a new frontier for the Bio-Monitor smart shirt, a tank-top filled with sensors that monitor the wearer’s stats, such as heart and breathing rate, oxygen saturation, skin temperature, and blood pressure. And you thought space was just for finding a new human habitat and growing steak.
This shirt is already used by athletes to assess performance and by people with limited mobility to monitor health, so its potential impending usage by astronauts makes sense. Space is a pretty extreme environment, to put it mildly, and there’s a lot we still don’t know about how the human body reacts to it. Traditionally, astronauts hook themselves up to separate devices so their stats can be measured, a method which captures only snapshots of their bodies. By wearing the shirt constantly, the astronauts can be measured constantly, so scientists and doctors can see how the body deals with microgravity during normal activities and sleep. It also reduces stress, as there is no psychological impact of having to report in for constant health checks.
For the test, astronauts wore the shirt for 72 hours before flight and for 72 hours during flight. The shirts passed this first test with flying colors; in addition to providing accurate and more consistent stats monitoring than traditional methods, scientists on the ground determined that the astronauts recorded far less physical activity during flight than preflight, a finding in line with previous studies.
And before you question whether or not a tank top is really appropriate for space, just remember, Picard pulled it off at the end of “First Contact,” and that’s arguably the best Star Trek movie. So there’s certainly precedent.
Trend reversed: New cases of COVID-19 decline in children
New cases of COVID-19 dropped among children for just the second time in the past 6 weeks, but that was not enough to reverse the trend in children’s share of the weekly total, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

of all COVID-19 cases reported for the week, surpassing the pandemic-high 20.6% seen just a week earlier, the AAP/CHA report shows.
The total number of cases in children is now over 3.7 million – that’s 13.7% of cases in all ages – since the start of the pandemic, and the cumulative rate of infection has reached 4,931 per 100,000 children, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Cases of more severe illness in children continue to trend lower. The cumulative number of hospitalizations in children (15,187) is only 2.0% of the total of almost 760,000 in the 25 jurisdictions (24 states and New York City) that report such data, and deaths in children now number 296, which is just 0.06% of all COVID-19–related mortality in 43 states, New York City, Puerto Rico, and Guam, the AAP and CHA said in their report.
Among those 46 jurisdictions, Texas has reported the most deaths (51) in children, followed by Arizona (29) and New York City (23), while 9 states and the District of Columbia have reported no deaths so far. Children represent the highest proportion of deaths (0.19%) in Colorado, but Guam, with 2 child deaths among its total of 136, has by far the highest rate at 1.47%, the AAP/CHA data show.
Data from the 25 reporting jurisdictions show that children make up the largest share of hospitalizations (3.1%) in Colorado and Minnesota, while New York City (1.9%), Georgia (1.3%), and Rhode Island (1.3%) have the highest hospitalization rates among children diagnosed with SARS-CoV-2 infection, the two groups reported.
New cases of COVID-19 dropped among children for just the second time in the past 6 weeks, but that was not enough to reverse the trend in children’s share of the weekly total, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

of all COVID-19 cases reported for the week, surpassing the pandemic-high 20.6% seen just a week earlier, the AAP/CHA report shows.
The total number of cases in children is now over 3.7 million – that’s 13.7% of cases in all ages – since the start of the pandemic, and the cumulative rate of infection has reached 4,931 per 100,000 children, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Cases of more severe illness in children continue to trend lower. The cumulative number of hospitalizations in children (15,187) is only 2.0% of the total of almost 760,000 in the 25 jurisdictions (24 states and New York City) that report such data, and deaths in children now number 296, which is just 0.06% of all COVID-19–related mortality in 43 states, New York City, Puerto Rico, and Guam, the AAP and CHA said in their report.
Among those 46 jurisdictions, Texas has reported the most deaths (51) in children, followed by Arizona (29) and New York City (23), while 9 states and the District of Columbia have reported no deaths so far. Children represent the highest proportion of deaths (0.19%) in Colorado, but Guam, with 2 child deaths among its total of 136, has by far the highest rate at 1.47%, the AAP/CHA data show.
Data from the 25 reporting jurisdictions show that children make up the largest share of hospitalizations (3.1%) in Colorado and Minnesota, while New York City (1.9%), Georgia (1.3%), and Rhode Island (1.3%) have the highest hospitalization rates among children diagnosed with SARS-CoV-2 infection, the two groups reported.
New cases of COVID-19 dropped among children for just the second time in the past 6 weeks, but that was not enough to reverse the trend in children’s share of the weekly total, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.

of all COVID-19 cases reported for the week, surpassing the pandemic-high 20.6% seen just a week earlier, the AAP/CHA report shows.
The total number of cases in children is now over 3.7 million – that’s 13.7% of cases in all ages – since the start of the pandemic, and the cumulative rate of infection has reached 4,931 per 100,000 children, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Cases of more severe illness in children continue to trend lower. The cumulative number of hospitalizations in children (15,187) is only 2.0% of the total of almost 760,000 in the 25 jurisdictions (24 states and New York City) that report such data, and deaths in children now number 296, which is just 0.06% of all COVID-19–related mortality in 43 states, New York City, Puerto Rico, and Guam, the AAP and CHA said in their report.
Among those 46 jurisdictions, Texas has reported the most deaths (51) in children, followed by Arizona (29) and New York City (23), while 9 states and the District of Columbia have reported no deaths so far. Children represent the highest proportion of deaths (0.19%) in Colorado, but Guam, with 2 child deaths among its total of 136, has by far the highest rate at 1.47%, the AAP/CHA data show.
Data from the 25 reporting jurisdictions show that children make up the largest share of hospitalizations (3.1%) in Colorado and Minnesota, while New York City (1.9%), Georgia (1.3%), and Rhode Island (1.3%) have the highest hospitalization rates among children diagnosed with SARS-CoV-2 infection, the two groups reported.
Helpful giant rodents and our old friend, the hookworm
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.