User login
VIDEO: Does Childhood Abdominal Pain Portend Adult GI Problems?
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT OPINION FROM THE 2015 JAMES W. FRESTON CONFERENCE
VIDEO: Does childhood abdominal pain portend adult GI problems?
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
CHICAGO – Functional abdominal pain (FAP) is one of the most common complaints seen in pediatric and pediatric gastroenterology practices – but does that pediatric condition put patients at risk for similar problems as adults?
The worldwide prevalence of FAP in children is about 13.5%, with more than one in three children reporting weekly abdominal pain. Although that FAP often disappears over time, new research suggests that childhood FAP increases the risk for adult problems.
Indeed, roughly 30%-40% of children with FAP will go on to become adults with irritable bowel syndrome (IBS) or another functional gastrointestinal disorder (FGID), according to Miranda van Tilburg, Ph.D., of the department of gastroenterology and hepatology, University of North Carolina at Chapel Hill.
A recent prospective, longitudinal study reported that 41% of pediatric FAP patients met the symptom criteria for Rome III FGID at follow-up evaluation an average of 9.2 years after initial diagnosis. The most common FGID at follow-up was IBS (Clin Gastroenterol Hepatol. 2014 Dec;12[12]:2026-32).
Children with FAP will transition into adult care, and adult gastroenterologists need to be ready to attend to these patients and the specific issues they bring, Dr. Tilburg said at the meeting sponsored by the American Gastroenterological Association. In a video interview, Dr. van Tilburg discussed this subset of children whose FAP persists into adulthood, and what clinicians can do to care for these patients.
Dr. van Tilburg reported having no relevant conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
EXPERT OPINION FROM THE 2015 JAMES W. FRESTON CONFERENCE
Daratumumab monotherapy impresses in hard-to-treat multiple myeloma
Daratumumab monotherapy yielded impressive results in patients with heavily pretreated and refractory multiple myeloma, according to the full results of a phase I/II study published online by the New England Journal of Medicine.
Among 42 patients receiving 16 mg/kg of daratumumab in part 2 of the study, the overall response rate was 36%, including 2 complete responses, 2 very good partial responses, and 11 partial responses.
Median progression-free survival was 5.6 months. Responses deepened over time, with 65% of responders remaining progression-free at 12 months, study author Dr. Henk M. Lokhorst, of University Medical Center Utrecht, and the VU University Medical Center, Amsterdam, both in the Netherlands, and his associates reported (N Engl J Med. 2015 Aug. 26 [doi:10.1056/NEJMoa1506348]).
In 30 patients given daratumumab 8 mg/kg, the response rate was 10%, including three partial responses.
Patients in part 2 of the study were heavily pretreated with a median of four prior lines of therapy (range 2-12) and 64% were refractory to the current standard treatment of protease inhibitors (PIs) and immunomodulatory agents (IMiDs). Such patients have a poor prognosis, with an estimated median overall survival of 9 months and estimated event-free survival of 5 months at best, Dr. Lokhorst and his associates noted.
“Daratumumab showed single-agent antitumor activity in a population of patients with highly difficult-to-treat myeloma who had very few effective treatment options,” the investigators concluded. “Its target and mechanisms of action differentiate it from existing therapies.”
Daratumumab is a human monoclonal antibody that targets CD38, which is uniformly overexpressed in multiple myeloma cells.
In part 1, the dose-escalation phase of the study, no maximum-tolerated dose was identified at doses up to 24 mg/kg in 32 patients. Two dose-limiting toxicities – grade 3 anemia and grade 3 elevated aspartate aminotransferase levels – occurred at 0.1 mg/kg and 1 mg/kg, but no further events were seen with dose escalation, Dr. Lokhorst and associates reported.
The most-common adverse events in part 2 of the study – occurring in at least 25% of patients – were fatigue, allergic rhinitis, and pyrexia. Infusion-related reactions were mild and were seen in 71% of patients, typically during the first infusion.
The most-common grade 3/4 events were pneumonia (five patients) and thrombocytopenia (four patients). Neutropenia, leukopenia, anemia, and hyperglycemia occurred in two patients each. There was one grade 5 pneumonia, but investigators did not think it was related to the study drug, they wrote.
Exploratory subgroup analyses revealed that response rates were similar in patients with disease refractory to both bortezomib (Velcade) and lenalidomide (Revlimid) and the total population, but were higher in patients with two or three prior lines of therapy vs. more heavily pretreated patients (56% vs. 23%).
Data from the study were included in a Biologics License Application submitted in July 2015 to the U.S. Food and Drug Administration for daratumumab as a treatment for patients with multiple myeloma who have received at least three prior lines of therapy including both a PI and an IMiD or who are double refractory to a PI and an IMiD, according to Genmab.
Daratumumab, which has already been granted breakthrough therapy status by the FDA, is being develop by Janssen Biotech, under an exclusive license from Genmab.
On Twitter @pwendl
The single-agent activity of daratumumab, including complete responses, in this patient population is surprising and very encouraging. These results are probably due to its pleiotropic mechanisms of action against myeloma.
The introduction of monoclonal antibodies into the arsenal against myeloma is game-changing in multiple myeloma treatment. These agents have the advantage of an immune-based approach without the need for patient-specific cell manipulation. Their limited toxicity allows for easy combining with existing therapies.
Even with this enthusiasm, unanswered questions remain. How do tumors escape the effects of daratumumab? Can daratumumab, like rituximab in the treatment of lymphoma, be active in many phases of treatment, such as in induction, consolidation, and maintenance therapies? Can daratumumab resistance be predicted? As we begin to tackle the complexity of these questions, it is reassuring to know that we have yet one more treatment option that will contribute in an important way to improvement in outcomes in patients with myeloma.
These comments were excerpted from an editorial accompanying the report by Lokhorst et al. (N Engl J Med. 2015 Aug 26 [doi: 10.1056/NEJMe1509419]).
Dr. Noopur Raje is director of the multiple myeloma program at Massachusetts General Hospital, Boston. Dr. Dan L. Longo is a professor of medicine at Harvard Medical School, Boston.
The single-agent activity of daratumumab, including complete responses, in this patient population is surprising and very encouraging. These results are probably due to its pleiotropic mechanisms of action against myeloma.
The introduction of monoclonal antibodies into the arsenal against myeloma is game-changing in multiple myeloma treatment. These agents have the advantage of an immune-based approach without the need for patient-specific cell manipulation. Their limited toxicity allows for easy combining with existing therapies.
Even with this enthusiasm, unanswered questions remain. How do tumors escape the effects of daratumumab? Can daratumumab, like rituximab in the treatment of lymphoma, be active in many phases of treatment, such as in induction, consolidation, and maintenance therapies? Can daratumumab resistance be predicted? As we begin to tackle the complexity of these questions, it is reassuring to know that we have yet one more treatment option that will contribute in an important way to improvement in outcomes in patients with myeloma.
These comments were excerpted from an editorial accompanying the report by Lokhorst et al. (N Engl J Med. 2015 Aug 26 [doi: 10.1056/NEJMe1509419]).
Dr. Noopur Raje is director of the multiple myeloma program at Massachusetts General Hospital, Boston. Dr. Dan L. Longo is a professor of medicine at Harvard Medical School, Boston.
The single-agent activity of daratumumab, including complete responses, in this patient population is surprising and very encouraging. These results are probably due to its pleiotropic mechanisms of action against myeloma.
The introduction of monoclonal antibodies into the arsenal against myeloma is game-changing in multiple myeloma treatment. These agents have the advantage of an immune-based approach without the need for patient-specific cell manipulation. Their limited toxicity allows for easy combining with existing therapies.
Even with this enthusiasm, unanswered questions remain. How do tumors escape the effects of daratumumab? Can daratumumab, like rituximab in the treatment of lymphoma, be active in many phases of treatment, such as in induction, consolidation, and maintenance therapies? Can daratumumab resistance be predicted? As we begin to tackle the complexity of these questions, it is reassuring to know that we have yet one more treatment option that will contribute in an important way to improvement in outcomes in patients with myeloma.
These comments were excerpted from an editorial accompanying the report by Lokhorst et al. (N Engl J Med. 2015 Aug 26 [doi: 10.1056/NEJMe1509419]).
Dr. Noopur Raje is director of the multiple myeloma program at Massachusetts General Hospital, Boston. Dr. Dan L. Longo is a professor of medicine at Harvard Medical School, Boston.
Daratumumab monotherapy yielded impressive results in patients with heavily pretreated and refractory multiple myeloma, according to the full results of a phase I/II study published online by the New England Journal of Medicine.
Among 42 patients receiving 16 mg/kg of daratumumab in part 2 of the study, the overall response rate was 36%, including 2 complete responses, 2 very good partial responses, and 11 partial responses.
Median progression-free survival was 5.6 months. Responses deepened over time, with 65% of responders remaining progression-free at 12 months, study author Dr. Henk M. Lokhorst, of University Medical Center Utrecht, and the VU University Medical Center, Amsterdam, both in the Netherlands, and his associates reported (N Engl J Med. 2015 Aug. 26 [doi:10.1056/NEJMoa1506348]).
In 30 patients given daratumumab 8 mg/kg, the response rate was 10%, including three partial responses.
Patients in part 2 of the study were heavily pretreated with a median of four prior lines of therapy (range 2-12) and 64% were refractory to the current standard treatment of protease inhibitors (PIs) and immunomodulatory agents (IMiDs). Such patients have a poor prognosis, with an estimated median overall survival of 9 months and estimated event-free survival of 5 months at best, Dr. Lokhorst and his associates noted.
“Daratumumab showed single-agent antitumor activity in a population of patients with highly difficult-to-treat myeloma who had very few effective treatment options,” the investigators concluded. “Its target and mechanisms of action differentiate it from existing therapies.”
Daratumumab is a human monoclonal antibody that targets CD38, which is uniformly overexpressed in multiple myeloma cells.
In part 1, the dose-escalation phase of the study, no maximum-tolerated dose was identified at doses up to 24 mg/kg in 32 patients. Two dose-limiting toxicities – grade 3 anemia and grade 3 elevated aspartate aminotransferase levels – occurred at 0.1 mg/kg and 1 mg/kg, but no further events were seen with dose escalation, Dr. Lokhorst and associates reported.
The most-common adverse events in part 2 of the study – occurring in at least 25% of patients – were fatigue, allergic rhinitis, and pyrexia. Infusion-related reactions were mild and were seen in 71% of patients, typically during the first infusion.
The most-common grade 3/4 events were pneumonia (five patients) and thrombocytopenia (four patients). Neutropenia, leukopenia, anemia, and hyperglycemia occurred in two patients each. There was one grade 5 pneumonia, but investigators did not think it was related to the study drug, they wrote.
Exploratory subgroup analyses revealed that response rates were similar in patients with disease refractory to both bortezomib (Velcade) and lenalidomide (Revlimid) and the total population, but were higher in patients with two or three prior lines of therapy vs. more heavily pretreated patients (56% vs. 23%).
Data from the study were included in a Biologics License Application submitted in July 2015 to the U.S. Food and Drug Administration for daratumumab as a treatment for patients with multiple myeloma who have received at least three prior lines of therapy including both a PI and an IMiD or who are double refractory to a PI and an IMiD, according to Genmab.
Daratumumab, which has already been granted breakthrough therapy status by the FDA, is being develop by Janssen Biotech, under an exclusive license from Genmab.
On Twitter @pwendl
Daratumumab monotherapy yielded impressive results in patients with heavily pretreated and refractory multiple myeloma, according to the full results of a phase I/II study published online by the New England Journal of Medicine.
Among 42 patients receiving 16 mg/kg of daratumumab in part 2 of the study, the overall response rate was 36%, including 2 complete responses, 2 very good partial responses, and 11 partial responses.
Median progression-free survival was 5.6 months. Responses deepened over time, with 65% of responders remaining progression-free at 12 months, study author Dr. Henk M. Lokhorst, of University Medical Center Utrecht, and the VU University Medical Center, Amsterdam, both in the Netherlands, and his associates reported (N Engl J Med. 2015 Aug. 26 [doi:10.1056/NEJMoa1506348]).
In 30 patients given daratumumab 8 mg/kg, the response rate was 10%, including three partial responses.
Patients in part 2 of the study were heavily pretreated with a median of four prior lines of therapy (range 2-12) and 64% were refractory to the current standard treatment of protease inhibitors (PIs) and immunomodulatory agents (IMiDs). Such patients have a poor prognosis, with an estimated median overall survival of 9 months and estimated event-free survival of 5 months at best, Dr. Lokhorst and his associates noted.
“Daratumumab showed single-agent antitumor activity in a population of patients with highly difficult-to-treat myeloma who had very few effective treatment options,” the investigators concluded. “Its target and mechanisms of action differentiate it from existing therapies.”
Daratumumab is a human monoclonal antibody that targets CD38, which is uniformly overexpressed in multiple myeloma cells.
In part 1, the dose-escalation phase of the study, no maximum-tolerated dose was identified at doses up to 24 mg/kg in 32 patients. Two dose-limiting toxicities – grade 3 anemia and grade 3 elevated aspartate aminotransferase levels – occurred at 0.1 mg/kg and 1 mg/kg, but no further events were seen with dose escalation, Dr. Lokhorst and associates reported.
The most-common adverse events in part 2 of the study – occurring in at least 25% of patients – were fatigue, allergic rhinitis, and pyrexia. Infusion-related reactions were mild and were seen in 71% of patients, typically during the first infusion.
The most-common grade 3/4 events were pneumonia (five patients) and thrombocytopenia (four patients). Neutropenia, leukopenia, anemia, and hyperglycemia occurred in two patients each. There was one grade 5 pneumonia, but investigators did not think it was related to the study drug, they wrote.
Exploratory subgroup analyses revealed that response rates were similar in patients with disease refractory to both bortezomib (Velcade) and lenalidomide (Revlimid) and the total population, but were higher in patients with two or three prior lines of therapy vs. more heavily pretreated patients (56% vs. 23%).
Data from the study were included in a Biologics License Application submitted in July 2015 to the U.S. Food and Drug Administration for daratumumab as a treatment for patients with multiple myeloma who have received at least three prior lines of therapy including both a PI and an IMiD or who are double refractory to a PI and an IMiD, according to Genmab.
Daratumumab, which has already been granted breakthrough therapy status by the FDA, is being develop by Janssen Biotech, under an exclusive license from Genmab.
On Twitter @pwendl
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Daratumumab monotherapy has encouraging efficacy and a favorable safety profile in heavily pretreated and refractory multiple myeloma.
Major finding: The overall response rate was 36% with daratumumab 16 mg/kg.
Data source: Open-label phase I/II study in 104 patients with relapsed or refractory multiple myeloma.
Disclosures: The study was funded by Janssen Biotech and Genmab. Dr. Lokhorst reported grant support and personal fees from Genmab and Janssen and personal fees from Amgen. Several coauthors also reported fees from Janssen and/or Genmab. Dr. Raje reported personal fees from Celgene and Millennium/Takeda and grant support from Eli Lilly and AstraZeneca. Dr. Longo disclosed being employed as deputy editor at the New England Journal of Medicine.
Recurrence score assay driving chemo decisions in unexpected ways
Adoption of the 21-gene recurrence score (RS) assay does not appear to have decreased chemotherapy use overall among Medicare beneficiaries diagnosed with breast cancer, investigators reported online in JAMA Oncology. However, use of the assay was associated with decreased chemotherapy use in high-risk patients and increased chemotherapy use in low-risk patients in the retrospective study.
“Contrary to our hypothesis, we did not observe a change in chemotherapy use in the overall study population after the adoption of the RS assay between 2005 and 2009 or a general association between receipt of chemotherapy and use of the assay in multivariable analyses or HRR [hospital referral region]–level analyses,” Dr. Michaela Dinan of the Duke Clinical Research Institute and her associates wrote (JAMA Oncol. doi: 10.1001/jamaoncol.2015.2722).
There was, however, an interaction between use of the Oncotype DX recurrence score (RS) assay and National Comprehensive Cancer Network (NCCN) risk category.
RS use was associated with lower chemotherapy use in women with high-risk disease (odds ratio, 0.34; 99% confidence interval, 0.20-0.57) and higher chemotherapy use in those with low-risk disease (OR, 4.46; 99% CI, 3.15-6.31).
NCCN guidelines recommend considering chemotherapy in estrogen receptor (ER)-positive, node-negative breast cancer for all but the smallest tumors.
The 21-gene Oncotype DX assay was one of the first gene expression profile tests to reach the market, and studies have suggested its use could save money by guiding allocation of chemotherapy to patients most likely to benefit.
An earlier multicenter NCCN database analysis reported an association between the progressive rise in RS testing and an overall decline in adjuvant chemotherapy in hormone-receptive breast cancers diagnosed between 2006 and 2008.
The current study took a wider look at use of the RS assay and chemotherapy using a nationally representative sample of 44,044 women, aged 65 years and older, diagnosed with early-stage, ER-positive breast cancer between 2005 and 2009 in the SEER (Surveillance, Epidemiology, and End Results) database linked with Medicare claims. Of these, 24% had low-risk, 51.3% intermediate-risk, and 24.6% high-risk disease based on NCCN criteria. Roughly a quarter were node positive.
Use of the RS assay was higher among patients 70 years or younger, patients with fewer comorbid conditions, and patients with T1c tumors, node-negative disease, and intermediate-risk disease, Dr. Dinan and associates reported.
In all, 14.3% of patients overall and 26.5% of patients 70 years or younger received chemotherapy within 12 months of diagnosis, “which supports a significant influence of age on chemotherapy use,” they said.
“Our data suggest that use of the RS assay may have decreased chemotherapy use in general practice among younger patients with high-risk disease in whom receipt of chemotherapy would have otherwise been likely but that it was associated with greater chemotherapy use in patients with low-risk disease. The impact of the RS assay on chemotherapy use is likely population dependent and is influenced by the population’s pretest likelihood of undergoing chemotherapy,” they concluded.
The authors acknowledge that the study had limitations as only RS assays paid for by Medicare were analyzed, HER2 status was unavailable, and patients in the SEER registry are more likely to be nonwhite and live in high-poverty and urban areas, which may affect generalizability.
The study was sponsored by a grant from the Agency for Healthcare Research and Quality. The authors reported having no conflicts of interests. Dr. Kurian and Dr. Friese reported receiving funding from a National Cancer Institute grant to the University of Michigan.
On Twitter @pwendl
The study by Dinan et al. adds a valuable population-based lens to our knowledge of RS adoption and chemotherapy use because prior utilization studies have been more limited in scope. However, many crucial details are missing from this bird’s-eye view.
Most critical are: (1) the exclusion of women younger than 65 years, who make up the majority of breast cancer patients; (2) the lack of RS assay results, which markedly limits evaluation of its impact on chemotherapy decision making; and (3) the absence of patient and physician perspectives, without which we cannot fully understand how use of the RS assay informs treatment choices. Only 14% of patients in this study received chemotherapy, compared with 40%-50% in studies with wider age ranges; this substantial difference in systemic therapy use suggests that the RS assay use patterns observed here may not generalize to younger women.
Getting “under the hood” of such complex medical decision making requires supplementing registry data not only with genomic test results but also with measures of the patient and physician experience. We still do not know why and under what circumstances physicians choose to order an RS assay; to what extent physicians’ treatment recommendations follow RS assay results; and what role, if any, patients play in the choice to order an RS assay and in subsequent chemotherapy decisions. Ultimately, we cannot assess the effects of RS assay use on breast cancer treatment without a deeper understanding of patients’ and physicians’ perspectives.
These comments were excerpted from an editorial accompanying the report by Dr. Dinan and her associates (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2719).
Dr. Allison Kurian is an assistant professor of medicine (oncology) and of health research and policy at Stanford (Calif.) University Medical Center. Christopher Friese, Ph.D., R.N., is an assistant professor at the School of Nursing, University of Michigan, Ann Arbor.
The study by Dinan et al. adds a valuable population-based lens to our knowledge of RS adoption and chemotherapy use because prior utilization studies have been more limited in scope. However, many crucial details are missing from this bird’s-eye view.
Most critical are: (1) the exclusion of women younger than 65 years, who make up the majority of breast cancer patients; (2) the lack of RS assay results, which markedly limits evaluation of its impact on chemotherapy decision making; and (3) the absence of patient and physician perspectives, without which we cannot fully understand how use of the RS assay informs treatment choices. Only 14% of patients in this study received chemotherapy, compared with 40%-50% in studies with wider age ranges; this substantial difference in systemic therapy use suggests that the RS assay use patterns observed here may not generalize to younger women.
Getting “under the hood” of such complex medical decision making requires supplementing registry data not only with genomic test results but also with measures of the patient and physician experience. We still do not know why and under what circumstances physicians choose to order an RS assay; to what extent physicians’ treatment recommendations follow RS assay results; and what role, if any, patients play in the choice to order an RS assay and in subsequent chemotherapy decisions. Ultimately, we cannot assess the effects of RS assay use on breast cancer treatment without a deeper understanding of patients’ and physicians’ perspectives.
These comments were excerpted from an editorial accompanying the report by Dr. Dinan and her associates (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2719).
Dr. Allison Kurian is an assistant professor of medicine (oncology) and of health research and policy at Stanford (Calif.) University Medical Center. Christopher Friese, Ph.D., R.N., is an assistant professor at the School of Nursing, University of Michigan, Ann Arbor.
The study by Dinan et al. adds a valuable population-based lens to our knowledge of RS adoption and chemotherapy use because prior utilization studies have been more limited in scope. However, many crucial details are missing from this bird’s-eye view.
Most critical are: (1) the exclusion of women younger than 65 years, who make up the majority of breast cancer patients; (2) the lack of RS assay results, which markedly limits evaluation of its impact on chemotherapy decision making; and (3) the absence of patient and physician perspectives, without which we cannot fully understand how use of the RS assay informs treatment choices. Only 14% of patients in this study received chemotherapy, compared with 40%-50% in studies with wider age ranges; this substantial difference in systemic therapy use suggests that the RS assay use patterns observed here may not generalize to younger women.
Getting “under the hood” of such complex medical decision making requires supplementing registry data not only with genomic test results but also with measures of the patient and physician experience. We still do not know why and under what circumstances physicians choose to order an RS assay; to what extent physicians’ treatment recommendations follow RS assay results; and what role, if any, patients play in the choice to order an RS assay and in subsequent chemotherapy decisions. Ultimately, we cannot assess the effects of RS assay use on breast cancer treatment without a deeper understanding of patients’ and physicians’ perspectives.
These comments were excerpted from an editorial accompanying the report by Dr. Dinan and her associates (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2719).
Dr. Allison Kurian is an assistant professor of medicine (oncology) and of health research and policy at Stanford (Calif.) University Medical Center. Christopher Friese, Ph.D., R.N., is an assistant professor at the School of Nursing, University of Michigan, Ann Arbor.
Adoption of the 21-gene recurrence score (RS) assay does not appear to have decreased chemotherapy use overall among Medicare beneficiaries diagnosed with breast cancer, investigators reported online in JAMA Oncology. However, use of the assay was associated with decreased chemotherapy use in high-risk patients and increased chemotherapy use in low-risk patients in the retrospective study.
“Contrary to our hypothesis, we did not observe a change in chemotherapy use in the overall study population after the adoption of the RS assay between 2005 and 2009 or a general association between receipt of chemotherapy and use of the assay in multivariable analyses or HRR [hospital referral region]–level analyses,” Dr. Michaela Dinan of the Duke Clinical Research Institute and her associates wrote (JAMA Oncol. doi: 10.1001/jamaoncol.2015.2722).
There was, however, an interaction between use of the Oncotype DX recurrence score (RS) assay and National Comprehensive Cancer Network (NCCN) risk category.
RS use was associated with lower chemotherapy use in women with high-risk disease (odds ratio, 0.34; 99% confidence interval, 0.20-0.57) and higher chemotherapy use in those with low-risk disease (OR, 4.46; 99% CI, 3.15-6.31).
NCCN guidelines recommend considering chemotherapy in estrogen receptor (ER)-positive, node-negative breast cancer for all but the smallest tumors.
The 21-gene Oncotype DX assay was one of the first gene expression profile tests to reach the market, and studies have suggested its use could save money by guiding allocation of chemotherapy to patients most likely to benefit.
An earlier multicenter NCCN database analysis reported an association between the progressive rise in RS testing and an overall decline in adjuvant chemotherapy in hormone-receptive breast cancers diagnosed between 2006 and 2008.
The current study took a wider look at use of the RS assay and chemotherapy using a nationally representative sample of 44,044 women, aged 65 years and older, diagnosed with early-stage, ER-positive breast cancer between 2005 and 2009 in the SEER (Surveillance, Epidemiology, and End Results) database linked with Medicare claims. Of these, 24% had low-risk, 51.3% intermediate-risk, and 24.6% high-risk disease based on NCCN criteria. Roughly a quarter were node positive.
Use of the RS assay was higher among patients 70 years or younger, patients with fewer comorbid conditions, and patients with T1c tumors, node-negative disease, and intermediate-risk disease, Dr. Dinan and associates reported.
In all, 14.3% of patients overall and 26.5% of patients 70 years or younger received chemotherapy within 12 months of diagnosis, “which supports a significant influence of age on chemotherapy use,” they said.
“Our data suggest that use of the RS assay may have decreased chemotherapy use in general practice among younger patients with high-risk disease in whom receipt of chemotherapy would have otherwise been likely but that it was associated with greater chemotherapy use in patients with low-risk disease. The impact of the RS assay on chemotherapy use is likely population dependent and is influenced by the population’s pretest likelihood of undergoing chemotherapy,” they concluded.
The authors acknowledge that the study had limitations as only RS assays paid for by Medicare were analyzed, HER2 status was unavailable, and patients in the SEER registry are more likely to be nonwhite and live in high-poverty and urban areas, which may affect generalizability.
The study was sponsored by a grant from the Agency for Healthcare Research and Quality. The authors reported having no conflicts of interests. Dr. Kurian and Dr. Friese reported receiving funding from a National Cancer Institute grant to the University of Michigan.
On Twitter @pwendl
Adoption of the 21-gene recurrence score (RS) assay does not appear to have decreased chemotherapy use overall among Medicare beneficiaries diagnosed with breast cancer, investigators reported online in JAMA Oncology. However, use of the assay was associated with decreased chemotherapy use in high-risk patients and increased chemotherapy use in low-risk patients in the retrospective study.
“Contrary to our hypothesis, we did not observe a change in chemotherapy use in the overall study population after the adoption of the RS assay between 2005 and 2009 or a general association between receipt of chemotherapy and use of the assay in multivariable analyses or HRR [hospital referral region]–level analyses,” Dr. Michaela Dinan of the Duke Clinical Research Institute and her associates wrote (JAMA Oncol. doi: 10.1001/jamaoncol.2015.2722).
There was, however, an interaction between use of the Oncotype DX recurrence score (RS) assay and National Comprehensive Cancer Network (NCCN) risk category.
RS use was associated with lower chemotherapy use in women with high-risk disease (odds ratio, 0.34; 99% confidence interval, 0.20-0.57) and higher chemotherapy use in those with low-risk disease (OR, 4.46; 99% CI, 3.15-6.31).
NCCN guidelines recommend considering chemotherapy in estrogen receptor (ER)-positive, node-negative breast cancer for all but the smallest tumors.
The 21-gene Oncotype DX assay was one of the first gene expression profile tests to reach the market, and studies have suggested its use could save money by guiding allocation of chemotherapy to patients most likely to benefit.
An earlier multicenter NCCN database analysis reported an association between the progressive rise in RS testing and an overall decline in adjuvant chemotherapy in hormone-receptive breast cancers diagnosed between 2006 and 2008.
The current study took a wider look at use of the RS assay and chemotherapy using a nationally representative sample of 44,044 women, aged 65 years and older, diagnosed with early-stage, ER-positive breast cancer between 2005 and 2009 in the SEER (Surveillance, Epidemiology, and End Results) database linked with Medicare claims. Of these, 24% had low-risk, 51.3% intermediate-risk, and 24.6% high-risk disease based on NCCN criteria. Roughly a quarter were node positive.
Use of the RS assay was higher among patients 70 years or younger, patients with fewer comorbid conditions, and patients with T1c tumors, node-negative disease, and intermediate-risk disease, Dr. Dinan and associates reported.
In all, 14.3% of patients overall and 26.5% of patients 70 years or younger received chemotherapy within 12 months of diagnosis, “which supports a significant influence of age on chemotherapy use,” they said.
“Our data suggest that use of the RS assay may have decreased chemotherapy use in general practice among younger patients with high-risk disease in whom receipt of chemotherapy would have otherwise been likely but that it was associated with greater chemotherapy use in patients with low-risk disease. The impact of the RS assay on chemotherapy use is likely population dependent and is influenced by the population’s pretest likelihood of undergoing chemotherapy,” they concluded.
The authors acknowledge that the study had limitations as only RS assays paid for by Medicare were analyzed, HER2 status was unavailable, and patients in the SEER registry are more likely to be nonwhite and live in high-poverty and urban areas, which may affect generalizability.
The study was sponsored by a grant from the Agency for Healthcare Research and Quality. The authors reported having no conflicts of interests. Dr. Kurian and Dr. Friese reported receiving funding from a National Cancer Institute grant to the University of Michigan.
On Twitter @pwendl
FROM JAMA ONCOLOGY
Key clinical point: Use of the 21-gene recurrence score was associated with relatively lower chemotherapy use in women with high-risk disease and relatively higher chemotherapy use in patients with low-risk disease.
Major finding: RS use was associated with lower chemotherapy use in women with high-risk disease (OR, 0.34; 99% CI, 0.20-0.57) and higher chemotherapy use in those with low-risk disease (OR, 4.46; 99% CI, 3.15-6.31).
Data source: Retrospective cohort study in 44,044 Medicare beneficiaries with early-stage, ER-positive breast cancer.
Disclosures: The study was sponsored by a grant from the Agency for Healthcare Research and Quality. The authors reported having no conflicts of interests. Dr. Kurian and Dr. Friese reported receiving funding from a National Cancer Institute grant to the University of Michigan.
Burning the midnight oil does not impact surgical outcomes
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The risks of adverse outcomes of elective daytime surgical procedures were similar whether or not the attending physician had provided medical care the previous night.
Major finding: The primary composite endpoint was similar between the postmidnight and control groups (22.2% vs. 22.4%; P = .66).
Data source: Population-based, retrospective, matched cohort study in 38,978 patients.
Disclosures: Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
Scoring tool points to postop ventilator dependence
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A preoperative risk score can help identify patients at highest risk for postoperative ventilator dependence.
Major finding: A risk score greater than 3 identified the top 20%-30% of patients experiencing 60%-70% of postop ventilator dependence events.
Data source: Retrospective analysis of 7,473 elective general and vascular surgical patients.
Disclosures: The authors reported having no financial disclosures.
More octogenarians muscling through emergent surgeries
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
OR-focused effort cuts catheter use, surgical UTIs
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: An OR-focused multidisciplinary effort decreased catheter use in the operating room and catheter-associated UTIs.
Major finding: Catheter utilization in short cases declined 9% and surgical CAUTI by 89%.
Data source: Observational analysis of 2,809 surgical catheters placed.
Disclosures: The authors reported having no financial disclosures.
Experts call for greater scrutiny of egg donation practices
Fertility clinics are quick to tout their success rates to attract patients, but are they doing enough to disclose potential conflicts of interest and risks to oocyte donors?
A new report calls for professional societies to develop guidelines specifically addressing conflicts of interest in oocyte donation and to adopt tougher reporting and advertising standards (J Law Med Ethics. 2015 Jun;43[2]:410-24.).
While at least some measure of professional guidance addresses the potential conflicts that can arise at all four phases of oocyte donation – recruitment, screening and informed consent, ovarian stimulation, and follow-up – there is “a fracture between this guidance and actual practice,” the authors argued.
Some clinics and agencies may be minimizing risks in recruitment ads and websites, incentivizing repeated donations, or overstimulating donors for the benefit of recipients and clinic success rates.
One low-cost step to better inform a woman’s choice to donate would be to make complication rates publicly available along with the federally regulated annual success rates reported by the Centers for Disease Control and Prevention, said Aaron Levine, Ph.D., one of the report authors and an associate professor of public policy at the Georgia Institute of Technology in Atlanta.
“Sure, the clinics can complain it will require a little more paperwork and so on, but they should be tracking this already and if they’re not, a little nudge to track it better would be beneficial, in my view,” Dr. Levine said.
In 2010,Dr. Levine helped spark national debate after reporting that egg-donor payments rose $2,350 for every 100-point increase in SAT scores. The practice is not illegal and reflects, in part, the shortage of donors of certain ethnicities; however, the American Society for Reproductive Medicine (ASRM) egg donor compensation guidelines recommend payment not vary based on donor traits.
A separate systematic analysis of agency and clinic websites found that 34% of sites explicitly mentioned paying more for particular traits, 41% accepted donors under the ASRM recommended age minimum of 21, and many failed to present short-term (56%), long-term (92%), or psychological/emotional (77%) risks (Fertil Steril. 2012 Oct;98[4]: 995-1000).
A simple, cost-free solution may be to publish the names of programs that fail to follow ASRM/Society for Assisted Reproductive Technology (SART) guidelines, said study author Dr. Robert Klitzman, professor of psychiatry at Columbia University, New York, and director of the university’s master program in bioethics.
“There are carrots and sticks,” he said. “You can name-and-shame or you can praise those who are doing it.”
While fertility clinics tended to observe the guidelines, the analysis found that egg donor agencies or brokers were far more likely to advertise high payments, observed Dr. James Toner of the Atlanta Center for Reproductive Medicine.
“The profession cannot control what agencies offer their donors, nor prohibit private citizens from trying to find their own donors and offering exorbitant amounts,” said Dr. Toner, who is president of SART. “The true source of these guideline violations sits outside the profession.”
Dr. Klitzman argued that longitudinal follow-up is costly, but necessary to better understand the emotional and medical risks associated with egg donation. There is little interest from industry and the egg donors themselves may not want to think about creating a child for money. But, they may also look back in regret if they are childless at age 40 and have biological children they’re not in touch with, he said.
“Of course, if you go after 18- to 20-year-olds, their eggs are going to be better quality, but they’re probably going to think of these issues less,” he added.
Several studies have also shown that sperm donor–conceived offspring often want to know who their biological parent is, partly, for genetic and medical reasons to understand disease risk, Dr. Klitzman noted. In September 2014, the ASRM Ethics Committee updated its report on the interests, obligations, and rights in gamete donation and recommended that, “at minimum, gamete donors and recipients should be encouraged to provide appropriate medical updates.”
Dr. Levine acknowledged that ethical issues aren’t new to the infertility field, but said renewed attention is called for because of the increasingly high stakes involved in maintaining an adequate egg supply, increasing evidence of limited compliance with self-regulatory guidelines, and legal challenges to professional self-regulation.
In February 2015, the U.S. District Court for the Northern District of California granted in part the plaintiff’s motion for class certification in Kamakahi v. ASRM, a case filed in 2010 alleging that ASRM and SART engaged in price fixing by capping “appropriate” compensation in guidelines at $5,000, or $10,000 with justification.
The suit also names all SART-member fertility clinics and all egg agencies that agreed to abide by the ASRM-SART guidelines maximum price from April 12, 2007 to the present.
Also, in January 2015, the U.S. Tax Court ruled in favor of the Internal Revenue Service that $20,000 paid to a California woman for donating her eggs was compensation, not damages, and therefore taxable income.
The Kamakahi v. ASRM case is ongoing, but is already prompting some agencies to drop out of the ASRM, according to Andrew Vorzimer, a Woodland Hills, Calif., fertility lawyer. Mr. Vorzimer used to own Egg Donation Inc., but said he sold the Encino, Calif., infertility center in part because he could no longer compete with agencies who ignored the ASRM guidelines and were willing to offer six-figure payments for highly sought after donors. He continues to provide legal counsel to Egg Donation Inc.
“Most agencies ignore these guidelines anyway, so I think the likely result is, No. 1, that ASRM may simply withdraw all their guidelines and stay out of this entirely because they just don’t need the headache or liability, and you’re going to see the cost of egg donation skyrocket because the $10,000 dollar cap is going to go out the window,” Mr. Vorzimer said.
The IRS tax decision will also add upward pressure on egg prices because women are “going to want a larger amount to offset their tax liability,” he said.
Dr. Toner said that if the antitrust argument prevails in the courts, “...then I think the profession would stop providing guidance about reimbursement.”
Compensation, however, would be unlikely to take off. Even with the $10,000 cap in place, the going rate for eggs in Atlanta is about $6,000 per cycle. Few recipients, who ultimately pay the bill, would seek fertility treatment if the cost of eggs suddenly jumped from $6,000 to $30,000, he said. This downward pressure on the market is already being seen in states without insurance treatment mandates, whereas the “utilization of fertilization services is double or triple in states with coverage mandates,” Dr. Toner said.
Online ads may not include all the necessary information needed by donors, but “where the rubber hits the road” is in the clinic, he said, adding: “The profession has done a laudable job when it comes to egg donors. They are fully informed, treated as patients and fairly compensated for their time and effort.”
The new report from Dr. Levine and his colleagues discusses various possible oversight models, but ultimately balks at recommending federal or state laws or regulations. The authors conclude that improved self-regulation is the “most appropriate first step,” given the absence of compelling evidence of harm to donors associated with potential conflicts and feasibility concerns associated with other oversight models.
“Everyone is clamoring for more regulation,” said Dr. Mark V. Sauer, a member of ASRM’s Ethics Committee and director of Columbia’s Center for Women’s Reproductive Care. But he contended that the practice of reproductive medicine is probably already the most regulated form of medicine in the country. Moreover, the ASRM, not unlike the American Medical Association, is “not a policing professional society. They’re not a regulatory society,” he said.
Dr. Sauer declined to comment on the Kamakahi case, but said compensation rates in the highly competitive market of New York City have settled over the last 5 years at about $8,000 – the amount Columbia pays per cycle.
Fertility clinics are quick to tout their success rates to attract patients, but are they doing enough to disclose potential conflicts of interest and risks to oocyte donors?
A new report calls for professional societies to develop guidelines specifically addressing conflicts of interest in oocyte donation and to adopt tougher reporting and advertising standards (J Law Med Ethics. 2015 Jun;43[2]:410-24.).
While at least some measure of professional guidance addresses the potential conflicts that can arise at all four phases of oocyte donation – recruitment, screening and informed consent, ovarian stimulation, and follow-up – there is “a fracture between this guidance and actual practice,” the authors argued.
Some clinics and agencies may be minimizing risks in recruitment ads and websites, incentivizing repeated donations, or overstimulating donors for the benefit of recipients and clinic success rates.
One low-cost step to better inform a woman’s choice to donate would be to make complication rates publicly available along with the federally regulated annual success rates reported by the Centers for Disease Control and Prevention, said Aaron Levine, Ph.D., one of the report authors and an associate professor of public policy at the Georgia Institute of Technology in Atlanta.
“Sure, the clinics can complain it will require a little more paperwork and so on, but they should be tracking this already and if they’re not, a little nudge to track it better would be beneficial, in my view,” Dr. Levine said.
In 2010,Dr. Levine helped spark national debate after reporting that egg-donor payments rose $2,350 for every 100-point increase in SAT scores. The practice is not illegal and reflects, in part, the shortage of donors of certain ethnicities; however, the American Society for Reproductive Medicine (ASRM) egg donor compensation guidelines recommend payment not vary based on donor traits.
A separate systematic analysis of agency and clinic websites found that 34% of sites explicitly mentioned paying more for particular traits, 41% accepted donors under the ASRM recommended age minimum of 21, and many failed to present short-term (56%), long-term (92%), or psychological/emotional (77%) risks (Fertil Steril. 2012 Oct;98[4]: 995-1000).
A simple, cost-free solution may be to publish the names of programs that fail to follow ASRM/Society for Assisted Reproductive Technology (SART) guidelines, said study author Dr. Robert Klitzman, professor of psychiatry at Columbia University, New York, and director of the university’s master program in bioethics.
“There are carrots and sticks,” he said. “You can name-and-shame or you can praise those who are doing it.”
While fertility clinics tended to observe the guidelines, the analysis found that egg donor agencies or brokers were far more likely to advertise high payments, observed Dr. James Toner of the Atlanta Center for Reproductive Medicine.
“The profession cannot control what agencies offer their donors, nor prohibit private citizens from trying to find their own donors and offering exorbitant amounts,” said Dr. Toner, who is president of SART. “The true source of these guideline violations sits outside the profession.”
Dr. Klitzman argued that longitudinal follow-up is costly, but necessary to better understand the emotional and medical risks associated with egg donation. There is little interest from industry and the egg donors themselves may not want to think about creating a child for money. But, they may also look back in regret if they are childless at age 40 and have biological children they’re not in touch with, he said.
“Of course, if you go after 18- to 20-year-olds, their eggs are going to be better quality, but they’re probably going to think of these issues less,” he added.
Several studies have also shown that sperm donor–conceived offspring often want to know who their biological parent is, partly, for genetic and medical reasons to understand disease risk, Dr. Klitzman noted. In September 2014, the ASRM Ethics Committee updated its report on the interests, obligations, and rights in gamete donation and recommended that, “at minimum, gamete donors and recipients should be encouraged to provide appropriate medical updates.”
Dr. Levine acknowledged that ethical issues aren’t new to the infertility field, but said renewed attention is called for because of the increasingly high stakes involved in maintaining an adequate egg supply, increasing evidence of limited compliance with self-regulatory guidelines, and legal challenges to professional self-regulation.
In February 2015, the U.S. District Court for the Northern District of California granted in part the plaintiff’s motion for class certification in Kamakahi v. ASRM, a case filed in 2010 alleging that ASRM and SART engaged in price fixing by capping “appropriate” compensation in guidelines at $5,000, or $10,000 with justification.
The suit also names all SART-member fertility clinics and all egg agencies that agreed to abide by the ASRM-SART guidelines maximum price from April 12, 2007 to the present.
Also, in January 2015, the U.S. Tax Court ruled in favor of the Internal Revenue Service that $20,000 paid to a California woman for donating her eggs was compensation, not damages, and therefore taxable income.
The Kamakahi v. ASRM case is ongoing, but is already prompting some agencies to drop out of the ASRM, according to Andrew Vorzimer, a Woodland Hills, Calif., fertility lawyer. Mr. Vorzimer used to own Egg Donation Inc., but said he sold the Encino, Calif., infertility center in part because he could no longer compete with agencies who ignored the ASRM guidelines and were willing to offer six-figure payments for highly sought after donors. He continues to provide legal counsel to Egg Donation Inc.
“Most agencies ignore these guidelines anyway, so I think the likely result is, No. 1, that ASRM may simply withdraw all their guidelines and stay out of this entirely because they just don’t need the headache or liability, and you’re going to see the cost of egg donation skyrocket because the $10,000 dollar cap is going to go out the window,” Mr. Vorzimer said.
The IRS tax decision will also add upward pressure on egg prices because women are “going to want a larger amount to offset their tax liability,” he said.
Dr. Toner said that if the antitrust argument prevails in the courts, “...then I think the profession would stop providing guidance about reimbursement.”
Compensation, however, would be unlikely to take off. Even with the $10,000 cap in place, the going rate for eggs in Atlanta is about $6,000 per cycle. Few recipients, who ultimately pay the bill, would seek fertility treatment if the cost of eggs suddenly jumped from $6,000 to $30,000, he said. This downward pressure on the market is already being seen in states without insurance treatment mandates, whereas the “utilization of fertilization services is double or triple in states with coverage mandates,” Dr. Toner said.
Online ads may not include all the necessary information needed by donors, but “where the rubber hits the road” is in the clinic, he said, adding: “The profession has done a laudable job when it comes to egg donors. They are fully informed, treated as patients and fairly compensated for their time and effort.”
The new report from Dr. Levine and his colleagues discusses various possible oversight models, but ultimately balks at recommending federal or state laws or regulations. The authors conclude that improved self-regulation is the “most appropriate first step,” given the absence of compelling evidence of harm to donors associated with potential conflicts and feasibility concerns associated with other oversight models.
“Everyone is clamoring for more regulation,” said Dr. Mark V. Sauer, a member of ASRM’s Ethics Committee and director of Columbia’s Center for Women’s Reproductive Care. But he contended that the practice of reproductive medicine is probably already the most regulated form of medicine in the country. Moreover, the ASRM, not unlike the American Medical Association, is “not a policing professional society. They’re not a regulatory society,” he said.
Dr. Sauer declined to comment on the Kamakahi case, but said compensation rates in the highly competitive market of New York City have settled over the last 5 years at about $8,000 – the amount Columbia pays per cycle.
Fertility clinics are quick to tout their success rates to attract patients, but are they doing enough to disclose potential conflicts of interest and risks to oocyte donors?
A new report calls for professional societies to develop guidelines specifically addressing conflicts of interest in oocyte donation and to adopt tougher reporting and advertising standards (J Law Med Ethics. 2015 Jun;43[2]:410-24.).
While at least some measure of professional guidance addresses the potential conflicts that can arise at all four phases of oocyte donation – recruitment, screening and informed consent, ovarian stimulation, and follow-up – there is “a fracture between this guidance and actual practice,” the authors argued.
Some clinics and agencies may be minimizing risks in recruitment ads and websites, incentivizing repeated donations, or overstimulating donors for the benefit of recipients and clinic success rates.
One low-cost step to better inform a woman’s choice to donate would be to make complication rates publicly available along with the federally regulated annual success rates reported by the Centers for Disease Control and Prevention, said Aaron Levine, Ph.D., one of the report authors and an associate professor of public policy at the Georgia Institute of Technology in Atlanta.
“Sure, the clinics can complain it will require a little more paperwork and so on, but they should be tracking this already and if they’re not, a little nudge to track it better would be beneficial, in my view,” Dr. Levine said.
In 2010,Dr. Levine helped spark national debate after reporting that egg-donor payments rose $2,350 for every 100-point increase in SAT scores. The practice is not illegal and reflects, in part, the shortage of donors of certain ethnicities; however, the American Society for Reproductive Medicine (ASRM) egg donor compensation guidelines recommend payment not vary based on donor traits.
A separate systematic analysis of agency and clinic websites found that 34% of sites explicitly mentioned paying more for particular traits, 41% accepted donors under the ASRM recommended age minimum of 21, and many failed to present short-term (56%), long-term (92%), or psychological/emotional (77%) risks (Fertil Steril. 2012 Oct;98[4]: 995-1000).
A simple, cost-free solution may be to publish the names of programs that fail to follow ASRM/Society for Assisted Reproductive Technology (SART) guidelines, said study author Dr. Robert Klitzman, professor of psychiatry at Columbia University, New York, and director of the university’s master program in bioethics.
“There are carrots and sticks,” he said. “You can name-and-shame or you can praise those who are doing it.”
While fertility clinics tended to observe the guidelines, the analysis found that egg donor agencies or brokers were far more likely to advertise high payments, observed Dr. James Toner of the Atlanta Center for Reproductive Medicine.
“The profession cannot control what agencies offer their donors, nor prohibit private citizens from trying to find their own donors and offering exorbitant amounts,” said Dr. Toner, who is president of SART. “The true source of these guideline violations sits outside the profession.”
Dr. Klitzman argued that longitudinal follow-up is costly, but necessary to better understand the emotional and medical risks associated with egg donation. There is little interest from industry and the egg donors themselves may not want to think about creating a child for money. But, they may also look back in regret if they are childless at age 40 and have biological children they’re not in touch with, he said.
“Of course, if you go after 18- to 20-year-olds, their eggs are going to be better quality, but they’re probably going to think of these issues less,” he added.
Several studies have also shown that sperm donor–conceived offspring often want to know who their biological parent is, partly, for genetic and medical reasons to understand disease risk, Dr. Klitzman noted. In September 2014, the ASRM Ethics Committee updated its report on the interests, obligations, and rights in gamete donation and recommended that, “at minimum, gamete donors and recipients should be encouraged to provide appropriate medical updates.”
Dr. Levine acknowledged that ethical issues aren’t new to the infertility field, but said renewed attention is called for because of the increasingly high stakes involved in maintaining an adequate egg supply, increasing evidence of limited compliance with self-regulatory guidelines, and legal challenges to professional self-regulation.
In February 2015, the U.S. District Court for the Northern District of California granted in part the plaintiff’s motion for class certification in Kamakahi v. ASRM, a case filed in 2010 alleging that ASRM and SART engaged in price fixing by capping “appropriate” compensation in guidelines at $5,000, or $10,000 with justification.
The suit also names all SART-member fertility clinics and all egg agencies that agreed to abide by the ASRM-SART guidelines maximum price from April 12, 2007 to the present.
Also, in January 2015, the U.S. Tax Court ruled in favor of the Internal Revenue Service that $20,000 paid to a California woman for donating her eggs was compensation, not damages, and therefore taxable income.
The Kamakahi v. ASRM case is ongoing, but is already prompting some agencies to drop out of the ASRM, according to Andrew Vorzimer, a Woodland Hills, Calif., fertility lawyer. Mr. Vorzimer used to own Egg Donation Inc., but said he sold the Encino, Calif., infertility center in part because he could no longer compete with agencies who ignored the ASRM guidelines and were willing to offer six-figure payments for highly sought after donors. He continues to provide legal counsel to Egg Donation Inc.
“Most agencies ignore these guidelines anyway, so I think the likely result is, No. 1, that ASRM may simply withdraw all their guidelines and stay out of this entirely because they just don’t need the headache or liability, and you’re going to see the cost of egg donation skyrocket because the $10,000 dollar cap is going to go out the window,” Mr. Vorzimer said.
The IRS tax decision will also add upward pressure on egg prices because women are “going to want a larger amount to offset their tax liability,” he said.
Dr. Toner said that if the antitrust argument prevails in the courts, “...then I think the profession would stop providing guidance about reimbursement.”
Compensation, however, would be unlikely to take off. Even with the $10,000 cap in place, the going rate for eggs in Atlanta is about $6,000 per cycle. Few recipients, who ultimately pay the bill, would seek fertility treatment if the cost of eggs suddenly jumped from $6,000 to $30,000, he said. This downward pressure on the market is already being seen in states without insurance treatment mandates, whereas the “utilization of fertilization services is double or triple in states with coverage mandates,” Dr. Toner said.
Online ads may not include all the necessary information needed by donors, but “where the rubber hits the road” is in the clinic, he said, adding: “The profession has done a laudable job when it comes to egg donors. They are fully informed, treated as patients and fairly compensated for their time and effort.”
The new report from Dr. Levine and his colleagues discusses various possible oversight models, but ultimately balks at recommending federal or state laws or regulations. The authors conclude that improved self-regulation is the “most appropriate first step,” given the absence of compelling evidence of harm to donors associated with potential conflicts and feasibility concerns associated with other oversight models.
“Everyone is clamoring for more regulation,” said Dr. Mark V. Sauer, a member of ASRM’s Ethics Committee and director of Columbia’s Center for Women’s Reproductive Care. But he contended that the practice of reproductive medicine is probably already the most regulated form of medicine in the country. Moreover, the ASRM, not unlike the American Medical Association, is “not a policing professional society. They’re not a regulatory society,” he said.
Dr. Sauer declined to comment on the Kamakahi case, but said compensation rates in the highly competitive market of New York City have settled over the last 5 years at about $8,000 – the amount Columbia pays per cycle.
Modifiable risk factors foretell colonic anastomotic leak
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
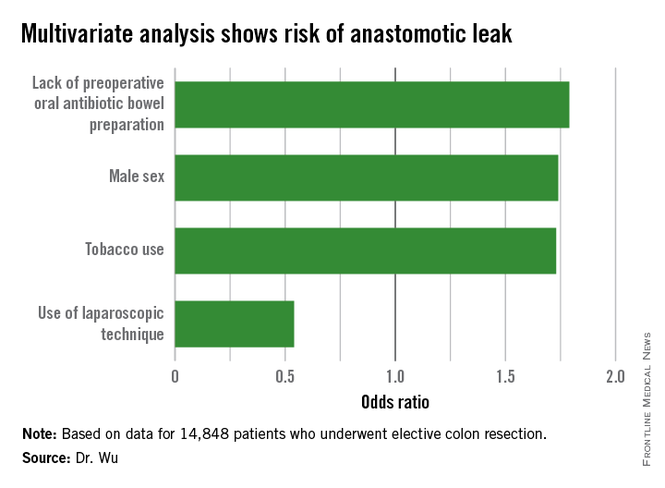
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
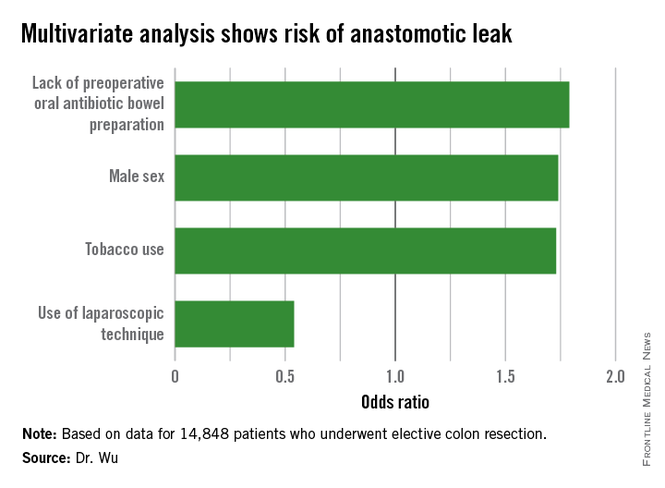
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
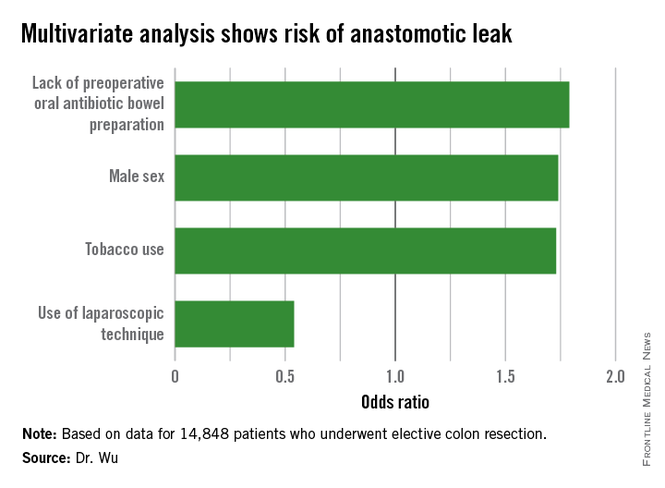
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Altering specific patient and operative factors can modify the risk of anastomotic leakage after colectomy.
Major finding: Male sex (OR, 1.74), tobacco use (OR, 1.73), and lack of an oral antibiotic bowel preparation (OR, 1.79) predicted anastomotic leak.
Data source: A retrospective study of 14,848 elective colectomies.
Disclosures: The authors reported having no relevant financial disclosures.