User login
Poorest children at higher risk for PICU admissions, death
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Children who live in neighborhoods that are at the bottom of the socioeconomic ladder are at significantly greater risk for being admitted to a pediatric intensive care unit (PICU) and of dying there, a study of Medicaid data showed.
Among more than 4 million children and adolescents in 12 U.S. states, those in the most socioeconomically deprived quartile had a significantly higher risk for PICU admission and in-hospital death, compared with patients from the least-deprived areas.
Black children were also at significantly higher risk for death than children of other races, reported Hannah K. Mitchell, BMBS, MSc, from Evelina Children’s Hospital, London.“I think we need to do better work for trying to understand the mechanisms behind these disparities, ... whether they can be intervened over in a hospital setting, and to try to identify targeted interventions,” she said during a presentation at the American Thoracic Society International Conference 2022.
Medicaid data
During her residency in pediatrics at Children’s Hospital of Philadelphia, Ms. Mitchell and colleagues conducted a study to determine whether there were disparities in PICU admissions and mortality according to socioeconomic deprivation in specific neighborhoods.
They created a retrospective cohort study of Medicaid patients from birth to age 20 who were covered from 2007 through 2014 in 12 U.S. states, using ZIP codes to identify areas of social deprivation.
They restricted the analysis to children from households with annual incomes below 150% of the federal poverty line and divided the cohort into socioeconomic quartiles.
A total of nearly 4.1 million children and adolescents were included in the sample. Of this group, 274,782 were admitted to a PICU during the study period.
The median age of children admitted to a PICU was 4 years (interquartile range 0-15), and slightly more than two-thirds (68.5%) had a chronic complex condition.
In all, 43.5% were identified as White, and 32.1% were identified as Black. Ms. Mitchell noted that one of the limitations of the study was missing data on patients of Hispanic/Latinx origin.
The mortality rate among all patients admitted to a PICU was 2.5%.
In univariate logistic regression analysis, the odds ratio for PICU admission among children living in the most impoverished circumstances was 1.21 (P < .0001).
Among all patients admitted to a PICU, the OR for death for children in the most deprived quartile, compared with the least deprived was 1.12 (P = .0047).
In addition, Black children were significantly more likely than White children to be admitted to a PICU (OR, 1.14; P < .0001) and to die in hospital (OR, 1.18, P < .0001).
Ms. Mitchell said that clinicians need to move beyond describing disparities and should instead begin to focus on interventions to eliminate or reduce them.
She noted that children in poor neighborhoods may be more likely to receive care in lower-quality hospitals or may be treated differently from other children when hospitalized because of their socioeconomic status.
Poor housing, environmental injustice
A pediatric pulmonary specialist who works in a safety net hospital told this news organization that there are multiple factors that contribute to increased risk for PICU admissions and mortality in disadvantaged neighborhoods.
“The overwhelming majority of our patients are not only of low socioeconomic status on an individual level but also live in areas of great socioeconomic deprivation, and all of those social determinants of health are resulting in increased admissions to the PICU,” said Robyn T. Cohen, MD, associate professor of pediatrics at Boston University Medical Center.
“They’re living in poor housing conditions with environmental pollution and experiencing competing priorities that prevent early access to care or the ability to obtain medications. We should be doing better to prevent that from happening” said Dr. Cohen, who co-moderated the session but was not involved with the study.
The study was supported by a grant from the National Institutes of Health. Ms. Mitchell and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Race-based spirometry may lead to missed diagnoses
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ATS 2022
Age, skin cancer risks for ICI-induced bullous pemphigoid identified
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
that may result in treatment interruption or cessation.
Investigators in Boston report that among patients receiving ICIs, being aged 70 years or older and having skin cancer are both significant risk factors for bullous pemphigoid. On the plus side, ICI-induced bullous pemphigoid also appears to be a marker for improved tumor responses to therapy.
In a nested case-control study of 5,636 patients with cancer who received either a programmed death 1 inhibitor such as pembrolizumab (Keytruda) or nivolumab (Opdivo) or a cytotoxic T-lymphocyte–associated protein 4 inhibitor such as ipilimumab (Yervoy), 35 patients (0.6%) developed bullous pemphigoid. The study by Nicole R. LeBoeuf, MD, MPH, from Brigham and Women’s Hospital in Boston and colleagues was published online in JAMA Dermatology.
“What is interesting is that 0.6 is a small number, but we’re seeing bullous pemphigoid at considerably higher frequency than is expected in the general population,” Dr. LeBoeuf said in an interview.
And although bullous pemphigoid has the potential to disrupt ICI therapy, it also appears to be a marker for a favorable tumor response, the investigators found.
Their findings suggest that management of bullous pemphigoid for patients receiving ICIs should focus on early identification and management with therapies directed at the specific toxicity, Dr. LeBoeuf said.
“When you make a specific diagnosis like bullous pemphigoid, then you can treat that specific disease with very targeted therapies, such as omalizumab or dupilumab or rituximab – things that are not globally immune suppressing like steroid or other T-cell–depleting agents. Studies have shown that depleting B cells with anti-CD20 agents is not detrimental to immune checkpoint inhibitor therapy,” she said.
Dermatologic AEs common
About 40% of patients with cancer treated with ICIs experience immune-related dermatologic adverse events (AEs) that can range from mild rashes and hair and nail changes to uncommon but life-threatening complications, such as Stevens-Johnson syndrome, a form of toxic epidermal necrolysis, according to members of a European Academy of Dermatology and Venereology task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they wrote in a position statement on the management of ICI-derived dermatologic adverse events.
Dr. LeBoeuf and colleagues note that, while reported risk factors for idiopathic bullous pemphigoid include advanced age, type 2 diabetes, use of dipeptidyl peptidase-4 inhibitors, cerebrovascular disease, and neurocognitive disease, risk factors for bullous pemphigoid and other adverse dermatologic events associated with ICIs are less well known.
Study details
To identify risk factors for bullous pemphigoid in patients receiving ICI, the investigators performed a case-control study nested within a retrospective cohort study.
They evaluated records for all patients in the three Harvard-affiliated hospitals to identify patients with ICI-associated bullous pemphigoid from October 2014 through December 2020. Control persons were all patients in the Dana-Farber cancer registry who received ICIs during the study period.
The investigators chose age at ICI initiation (69 years and younger or 70 years and older), sex, ICI agents, and cancer type as potential risk factors.
They used propensity score matching based on age, cancer type, ICI agent, and number of ICI cycles to match two control persons with each case patient.
Of the 5,636 patients treated with ICIs during the study period, 35 (0.6%) developed bullous pemphigoid. The median age was 72.8 years, and 71.4% were men.
In a multivariate logistic regression model that included 2,955 patients with complete data in the cancer registry, factors significantly associated with developing bullous pemphigoid included age 70 years or older (odds ratio, 2.32; P = .01), having melanoma (OR, 3.21; P < .001), and having nonmelanoma skin cancer (OR, 8.32; P < .001).
In comparing the 35 case patients with their matched control patients, a complete or partial response at first restaging imaging was significantly associated with developing bullous pemphigoid (OR, 3.37; P = .01). In addition, there was a higher likelihood of tumor responses to ICIs among patients with bullous pemphigoid, compared with matched control patients (objective response rate, 82.9% vs. 61.4%; P = .03).
Prudent toxicity management
Ryan Sullivan, MD, who treats patients with skin cancer at Massachusetts General Hospital Cancer Center, Boston, but was not involved in the study, commented that the findings raise questions about the relationship between skin cancers and immune-related adverse events.
“It is compelling that bullous pemphigoid is a skin toxicity and is more common to happen in skin cancer patients,” he noted. “That’s a very interesting finding, and the reason that it’s interesting is that it’s harder to understand why a presumably antibody-mediated side effect would be more likely to have that cross-reactivity where the tumor started and where the toxicity happened,” he said in an interview.
He noted that the benefits of ICIs for patients with skin cancers far outweigh the risks of dermatologic adverse events such as bullous pemphigoid and that ICI-associated events require judicious management.
“This is true across the spectrum of toxicities: There are clear manifestations of toxicity that we should be more thoughtful about what’s driving them, more thoughtful about what it is, and more thoughtful about treating them, other than just pouring steroids into patients in industrial doses and hoping that everything’s going to be OK,” he said.
No funding source for the study was reported. Dr. LeBoeuf reported receiving grants from the National Institutes of Health National Cancer Institute during the conduct of the study and personal fees for serving as a consultant for several companies outside the study. Coauthor Arash Mostaghimi, MD, MPA, MPH, is associate editor of JAMA Dermatology but was not involved in study selection or evaluation for publication. Dr. Sullivan disclosed consulting for ICI makers Bristol-Myers Squibb and Merck.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Preop nivolumab plus chemo ‘a quantum leap’ in NSCLC therapy
NEW ORLEANS – For patients with resectable non–small cell lung cancer (NSCLC), further
The combination resulted in significantly longer event-free survival and a 14-fold greater chance of having a pathological complete response compared with chemotherapy alone.
Adding immunotherapy (IO) to chemotherapy in the neoadjuvant setting represents “a quantum leap in lung cancer therapy,” commented David P. Carbone, MD, PhD, director of the James Thoracic Center at Ohio State University, Columbus.
“Combining IO with surgery I think is a new standard of care and will almost certainly improve overall survival [OS] in early-stage disease, for the first time in decades, in my entire career,” he said while discussing the new data at the annual meeting of the American Association for Cancer Research.
The data come from the phase 3 CheckMate 816 study, an open-label trial involving patients with stage IB-IIIA resectable NSCLC. The study was published in the New England Journal of Medicine to coincide with the presentation.
Results from this trial were the basis of the Food and Drug Administration’s recent approval of neoadjuvant therapy with nivolumab (Opdivo) and platinum-based chemotherapy in this population, which one expert described as “a turning point in how we treat resectable NSCLC.”
“Neoadjuvant IO has multiple theoretical advantages of over adjuvant IO,” commented Dr. Carbone. “CheckMate 816 suggests that practice will prove this theory correct.”
Importance of Neoadjuvant Immunotherapy
New details of the results were presented at the meeting by Nicolas Girard, MD, from Institut Curie in Paris.
Among 358 patients in the trial, the median event-free survival (EFS) was 31.6 months for patients randomly assigned to the combination of the immune checkpoint inhibitor nivolumab and platinum-base chemotherapy, compared with 20.8 months for patients assigned to chemotherapy alone. This translated into a hazard ratio for disease recurrence, progression, or death of 0.63 (P = .005).
In addition, 24% of patients assigned to the nivolumab plus chemotherapy arm had a pathological complete response (pCR) to neoadjuvant therapy, compared with only 2.2% of those assigned to chemotherapy alone (P < .001).
Dr. Girard said the study provided important clues to the importance of neoadjuvant therapy for improving objective responses.
“Event-free survival was improved in patients with a pathological complete response, compared with those without, suggesting pCR is a surrogate endpoint for long-term outcomes in resectable non–small cell lung cancer, and this is the first time [this has been shown] in a randomized, phase 3 study,” he said.
Neoadjuvant slow to catch on
About one -fourth of all patients who are diagnosed with NSCLC have resectable disease, Dr. Girard and colleagues noted. However, 30%-55% of patients who undergo surgery with curative intent ultimately experience recurrence and die from their disease.
Neoadjuvant therapy may improve chances for complete resection and prevent or delay recurrence after surgery, but the absolute difference in 5-year recurrence-free survival and OS with neoadjuvant chemotherapy alone is only about 6%, they noted.
The new results suggest that adding neoadjuvant immunotherapy to chemotherapy will improve upon this, although so far, the OS data from this trial are immature.
In an interim analysis, the median OS rate was 83% at 2 years for patients treated with nivolumab plus chemotherapy, compared with 71% for patients treated with chemotherapy alone. The published results show a significant improvement in the two primary endpoints – EFS and pCR.
In an editorial accompanying the study, Christine M. Lovly, MD, PhD, from the Vanderbilt-Ingram Cancer Center at Vanderbilt University in Nashville, Tenn., commented that the results of the trial are expected to change practice.
“However, several issues remain to be addressed,” she wrote. “First, is a pathological complete response predictive of event-free survival? Can event-free survival be used as a surrogate endpoint for overall survival? Second, although not mandated for this trial, approximately 20% of the patients received postoperative therapy. Is adjuvant therapy necessary? What criteria should be used to select patients to receive adjuvant therapy?”
Dr. Lovly also pointed out that patients with tumors harboring mutations in the genes EGFR or ALK were excluded from the trial.
“Therefore, implementation of neoadjuvant therapies requires biomarker testing for patients with early-stage disease at the time of diagnosis, a considerable alteration in the routine practice of lung-cancer medicine,” she wrote.
Fears of delaying surgery
In an interview, Upal Basu Roy, PhD, MPH, executive director of research at the LUNGevity Foundation, who was not involved in the study, gave a reason why neoadjuvant therapy is not more widely prescribed for patients with resectable NSCLC.
“Clinicians are always scared, and I think patients are as well, that giving a treatment before surgery would delay surgery,” he said. “When patients are diagnosed with lung cancer and they’re told that surgery offers the potential of cure and then hear that you’re giving them a treatment before surgery and that treatment may potentially delay surgery, that is a huge source of anxiety.”
In addition, clinicians until recently were unsure about which patients were most likely to benefit from neoadjuvant therapy when the only option was chemotherapy, “but that’s changing, obviously, with the recent approval of neoadjuvant nivolumab through CheckMate 816,” he said.
CheckMate 816 details
In the CheckMate 816 study, investigators enrolled patients with newly diagnosed resectable NSCLC (stage IB-IIIA) who had good performance status and no known sensitizing EGFR mutations or ALK alterations.
After stratification by stage, programmed death–1 status, and sex, the team randomly assigned patients to receive either nivolumab 360 mg plus platinum-based chemotherapy every 3 weeks for a total of three cycles or chemotherapy alone.
At the end of neoadjuvant therapy, patients underwent radiologic restaging and surgery within 6 weeks. Patients could also receive optional adjuvant chemotherapy with or without radiotherapy.
Of the 179 patients in each arm, 176 received the assigned treatment. In all, 149 (83%) of those assigned to the combination had definitive surgery, as did 135 (75%) of those assigned to chemotherapy alone.
In addition, 35 patients (20%) of those assigned to nivolumab-chemo and 56 (32%) assigned to chemotherapy alone received adjuvant therapy.
The coprimary endpoints of EFS and pCR favored the combination, both in the overall population and across most subgroups, including patients younger than 65, men and women, Asian patients, those with stage IIIA disease, nonsquamous histology, current smokers and never-smokers, and patients with higher levels of PD–ligand 1 expression.
The rates of grade 3 or 4 treatment-related adverse events were similar between the groups, at 33.5% with the combination and 36.9% with chemotherapy alone.
Rates of adverse events leading to study discontinuation, treatment-related adverse events, and surgery-related adverse events were similar between the groups. There were two treatment-related deaths, both in the chemotherapy-alone arm.
CheckMate 816 was funded by Bristol-Myers Squibb (manufacturer of nivolumab). Girard has consulted for and has received grant support from Bristol-Myers Squibb and other companies. Dr. Carbone has consulted for Bristol-Myers Squibb and other companies. Dr. Lovly has consulted for various companies. Dr. Roy has received grants from Bristol-Myers Squibb to the LUNGevity Foundation.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – For patients with resectable non–small cell lung cancer (NSCLC), further
The combination resulted in significantly longer event-free survival and a 14-fold greater chance of having a pathological complete response compared with chemotherapy alone.
Adding immunotherapy (IO) to chemotherapy in the neoadjuvant setting represents “a quantum leap in lung cancer therapy,” commented David P. Carbone, MD, PhD, director of the James Thoracic Center at Ohio State University, Columbus.
“Combining IO with surgery I think is a new standard of care and will almost certainly improve overall survival [OS] in early-stage disease, for the first time in decades, in my entire career,” he said while discussing the new data at the annual meeting of the American Association for Cancer Research.
The data come from the phase 3 CheckMate 816 study, an open-label trial involving patients with stage IB-IIIA resectable NSCLC. The study was published in the New England Journal of Medicine to coincide with the presentation.
Results from this trial were the basis of the Food and Drug Administration’s recent approval of neoadjuvant therapy with nivolumab (Opdivo) and platinum-based chemotherapy in this population, which one expert described as “a turning point in how we treat resectable NSCLC.”
“Neoadjuvant IO has multiple theoretical advantages of over adjuvant IO,” commented Dr. Carbone. “CheckMate 816 suggests that practice will prove this theory correct.”
Importance of Neoadjuvant Immunotherapy
New details of the results were presented at the meeting by Nicolas Girard, MD, from Institut Curie in Paris.
Among 358 patients in the trial, the median event-free survival (EFS) was 31.6 months for patients randomly assigned to the combination of the immune checkpoint inhibitor nivolumab and platinum-base chemotherapy, compared with 20.8 months for patients assigned to chemotherapy alone. This translated into a hazard ratio for disease recurrence, progression, or death of 0.63 (P = .005).
In addition, 24% of patients assigned to the nivolumab plus chemotherapy arm had a pathological complete response (pCR) to neoadjuvant therapy, compared with only 2.2% of those assigned to chemotherapy alone (P < .001).
Dr. Girard said the study provided important clues to the importance of neoadjuvant therapy for improving objective responses.
“Event-free survival was improved in patients with a pathological complete response, compared with those without, suggesting pCR is a surrogate endpoint for long-term outcomes in resectable non–small cell lung cancer, and this is the first time [this has been shown] in a randomized, phase 3 study,” he said.
Neoadjuvant slow to catch on
About one -fourth of all patients who are diagnosed with NSCLC have resectable disease, Dr. Girard and colleagues noted. However, 30%-55% of patients who undergo surgery with curative intent ultimately experience recurrence and die from their disease.
Neoadjuvant therapy may improve chances for complete resection and prevent or delay recurrence after surgery, but the absolute difference in 5-year recurrence-free survival and OS with neoadjuvant chemotherapy alone is only about 6%, they noted.
The new results suggest that adding neoadjuvant immunotherapy to chemotherapy will improve upon this, although so far, the OS data from this trial are immature.
In an interim analysis, the median OS rate was 83% at 2 years for patients treated with nivolumab plus chemotherapy, compared with 71% for patients treated with chemotherapy alone. The published results show a significant improvement in the two primary endpoints – EFS and pCR.
In an editorial accompanying the study, Christine M. Lovly, MD, PhD, from the Vanderbilt-Ingram Cancer Center at Vanderbilt University in Nashville, Tenn., commented that the results of the trial are expected to change practice.
“However, several issues remain to be addressed,” she wrote. “First, is a pathological complete response predictive of event-free survival? Can event-free survival be used as a surrogate endpoint for overall survival? Second, although not mandated for this trial, approximately 20% of the patients received postoperative therapy. Is adjuvant therapy necessary? What criteria should be used to select patients to receive adjuvant therapy?”
Dr. Lovly also pointed out that patients with tumors harboring mutations in the genes EGFR or ALK were excluded from the trial.
“Therefore, implementation of neoadjuvant therapies requires biomarker testing for patients with early-stage disease at the time of diagnosis, a considerable alteration in the routine practice of lung-cancer medicine,” she wrote.
Fears of delaying surgery
In an interview, Upal Basu Roy, PhD, MPH, executive director of research at the LUNGevity Foundation, who was not involved in the study, gave a reason why neoadjuvant therapy is not more widely prescribed for patients with resectable NSCLC.
“Clinicians are always scared, and I think patients are as well, that giving a treatment before surgery would delay surgery,” he said. “When patients are diagnosed with lung cancer and they’re told that surgery offers the potential of cure and then hear that you’re giving them a treatment before surgery and that treatment may potentially delay surgery, that is a huge source of anxiety.”
In addition, clinicians until recently were unsure about which patients were most likely to benefit from neoadjuvant therapy when the only option was chemotherapy, “but that’s changing, obviously, with the recent approval of neoadjuvant nivolumab through CheckMate 816,” he said.
CheckMate 816 details
In the CheckMate 816 study, investigators enrolled patients with newly diagnosed resectable NSCLC (stage IB-IIIA) who had good performance status and no known sensitizing EGFR mutations or ALK alterations.
After stratification by stage, programmed death–1 status, and sex, the team randomly assigned patients to receive either nivolumab 360 mg plus platinum-based chemotherapy every 3 weeks for a total of three cycles or chemotherapy alone.
At the end of neoadjuvant therapy, patients underwent radiologic restaging and surgery within 6 weeks. Patients could also receive optional adjuvant chemotherapy with or without radiotherapy.
Of the 179 patients in each arm, 176 received the assigned treatment. In all, 149 (83%) of those assigned to the combination had definitive surgery, as did 135 (75%) of those assigned to chemotherapy alone.
In addition, 35 patients (20%) of those assigned to nivolumab-chemo and 56 (32%) assigned to chemotherapy alone received adjuvant therapy.
The coprimary endpoints of EFS and pCR favored the combination, both in the overall population and across most subgroups, including patients younger than 65, men and women, Asian patients, those with stage IIIA disease, nonsquamous histology, current smokers and never-smokers, and patients with higher levels of PD–ligand 1 expression.
The rates of grade 3 or 4 treatment-related adverse events were similar between the groups, at 33.5% with the combination and 36.9% with chemotherapy alone.
Rates of adverse events leading to study discontinuation, treatment-related adverse events, and surgery-related adverse events were similar between the groups. There were two treatment-related deaths, both in the chemotherapy-alone arm.
CheckMate 816 was funded by Bristol-Myers Squibb (manufacturer of nivolumab). Girard has consulted for and has received grant support from Bristol-Myers Squibb and other companies. Dr. Carbone has consulted for Bristol-Myers Squibb and other companies. Dr. Lovly has consulted for various companies. Dr. Roy has received grants from Bristol-Myers Squibb to the LUNGevity Foundation.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – For patients with resectable non–small cell lung cancer (NSCLC), further
The combination resulted in significantly longer event-free survival and a 14-fold greater chance of having a pathological complete response compared with chemotherapy alone.
Adding immunotherapy (IO) to chemotherapy in the neoadjuvant setting represents “a quantum leap in lung cancer therapy,” commented David P. Carbone, MD, PhD, director of the James Thoracic Center at Ohio State University, Columbus.
“Combining IO with surgery I think is a new standard of care and will almost certainly improve overall survival [OS] in early-stage disease, for the first time in decades, in my entire career,” he said while discussing the new data at the annual meeting of the American Association for Cancer Research.
The data come from the phase 3 CheckMate 816 study, an open-label trial involving patients with stage IB-IIIA resectable NSCLC. The study was published in the New England Journal of Medicine to coincide with the presentation.
Results from this trial were the basis of the Food and Drug Administration’s recent approval of neoadjuvant therapy with nivolumab (Opdivo) and platinum-based chemotherapy in this population, which one expert described as “a turning point in how we treat resectable NSCLC.”
“Neoadjuvant IO has multiple theoretical advantages of over adjuvant IO,” commented Dr. Carbone. “CheckMate 816 suggests that practice will prove this theory correct.”
Importance of Neoadjuvant Immunotherapy
New details of the results were presented at the meeting by Nicolas Girard, MD, from Institut Curie in Paris.
Among 358 patients in the trial, the median event-free survival (EFS) was 31.6 months for patients randomly assigned to the combination of the immune checkpoint inhibitor nivolumab and platinum-base chemotherapy, compared with 20.8 months for patients assigned to chemotherapy alone. This translated into a hazard ratio for disease recurrence, progression, or death of 0.63 (P = .005).
In addition, 24% of patients assigned to the nivolumab plus chemotherapy arm had a pathological complete response (pCR) to neoadjuvant therapy, compared with only 2.2% of those assigned to chemotherapy alone (P < .001).
Dr. Girard said the study provided important clues to the importance of neoadjuvant therapy for improving objective responses.
“Event-free survival was improved in patients with a pathological complete response, compared with those without, suggesting pCR is a surrogate endpoint for long-term outcomes in resectable non–small cell lung cancer, and this is the first time [this has been shown] in a randomized, phase 3 study,” he said.
Neoadjuvant slow to catch on
About one -fourth of all patients who are diagnosed with NSCLC have resectable disease, Dr. Girard and colleagues noted. However, 30%-55% of patients who undergo surgery with curative intent ultimately experience recurrence and die from their disease.
Neoadjuvant therapy may improve chances for complete resection and prevent or delay recurrence after surgery, but the absolute difference in 5-year recurrence-free survival and OS with neoadjuvant chemotherapy alone is only about 6%, they noted.
The new results suggest that adding neoadjuvant immunotherapy to chemotherapy will improve upon this, although so far, the OS data from this trial are immature.
In an interim analysis, the median OS rate was 83% at 2 years for patients treated with nivolumab plus chemotherapy, compared with 71% for patients treated with chemotherapy alone. The published results show a significant improvement in the two primary endpoints – EFS and pCR.
In an editorial accompanying the study, Christine M. Lovly, MD, PhD, from the Vanderbilt-Ingram Cancer Center at Vanderbilt University in Nashville, Tenn., commented that the results of the trial are expected to change practice.
“However, several issues remain to be addressed,” she wrote. “First, is a pathological complete response predictive of event-free survival? Can event-free survival be used as a surrogate endpoint for overall survival? Second, although not mandated for this trial, approximately 20% of the patients received postoperative therapy. Is adjuvant therapy necessary? What criteria should be used to select patients to receive adjuvant therapy?”
Dr. Lovly also pointed out that patients with tumors harboring mutations in the genes EGFR or ALK were excluded from the trial.
“Therefore, implementation of neoadjuvant therapies requires biomarker testing for patients with early-stage disease at the time of diagnosis, a considerable alteration in the routine practice of lung-cancer medicine,” she wrote.
Fears of delaying surgery
In an interview, Upal Basu Roy, PhD, MPH, executive director of research at the LUNGevity Foundation, who was not involved in the study, gave a reason why neoadjuvant therapy is not more widely prescribed for patients with resectable NSCLC.
“Clinicians are always scared, and I think patients are as well, that giving a treatment before surgery would delay surgery,” he said. “When patients are diagnosed with lung cancer and they’re told that surgery offers the potential of cure and then hear that you’re giving them a treatment before surgery and that treatment may potentially delay surgery, that is a huge source of anxiety.”
In addition, clinicians until recently were unsure about which patients were most likely to benefit from neoadjuvant therapy when the only option was chemotherapy, “but that’s changing, obviously, with the recent approval of neoadjuvant nivolumab through CheckMate 816,” he said.
CheckMate 816 details
In the CheckMate 816 study, investigators enrolled patients with newly diagnosed resectable NSCLC (stage IB-IIIA) who had good performance status and no known sensitizing EGFR mutations or ALK alterations.
After stratification by stage, programmed death–1 status, and sex, the team randomly assigned patients to receive either nivolumab 360 mg plus platinum-based chemotherapy every 3 weeks for a total of three cycles or chemotherapy alone.
At the end of neoadjuvant therapy, patients underwent radiologic restaging and surgery within 6 weeks. Patients could also receive optional adjuvant chemotherapy with or without radiotherapy.
Of the 179 patients in each arm, 176 received the assigned treatment. In all, 149 (83%) of those assigned to the combination had definitive surgery, as did 135 (75%) of those assigned to chemotherapy alone.
In addition, 35 patients (20%) of those assigned to nivolumab-chemo and 56 (32%) assigned to chemotherapy alone received adjuvant therapy.
The coprimary endpoints of EFS and pCR favored the combination, both in the overall population and across most subgroups, including patients younger than 65, men and women, Asian patients, those with stage IIIA disease, nonsquamous histology, current smokers and never-smokers, and patients with higher levels of PD–ligand 1 expression.
The rates of grade 3 or 4 treatment-related adverse events were similar between the groups, at 33.5% with the combination and 36.9% with chemotherapy alone.
Rates of adverse events leading to study discontinuation, treatment-related adverse events, and surgery-related adverse events were similar between the groups. There were two treatment-related deaths, both in the chemotherapy-alone arm.
CheckMate 816 was funded by Bristol-Myers Squibb (manufacturer of nivolumab). Girard has consulted for and has received grant support from Bristol-Myers Squibb and other companies. Dr. Carbone has consulted for Bristol-Myers Squibb and other companies. Dr. Lovly has consulted for various companies. Dr. Roy has received grants from Bristol-Myers Squibb to the LUNGevity Foundation.
A version of this article first appeared on Medscape.com.
AT AACR 2022
Made-to-order TILs effective against metastatic melanoma
NEW ORLEANS – In just over one-third of patients with metastatic melanoma who had experienced disease progression while receiving multiple prior lines of therapy, including immunotherapy and targeted agents,
The product, called lifileucel, is custom made for each patient and utilizes tumor-infiltrating lymphocytes (TILs) extracted from tumor lesions. This approach differs from other cell-based therapies, such as chimeric antigen receptor (CAR) T cell therapy, which utilizes T cells collected from the patient’s blood.
The new results come from a phase 2 trial conducted in 66 patients with previously treated unresectable or metastatic melanoma who received a single dose of the product. The objective response rate was 36.4%.
“Lifileucel has demonstrated efficacy and durability of response for patients with metastatic melanoma and represents a viable therapeutic option warranting further investigation,” commented Jason Alan Chesney, MD, PhD, from the James Graham Brown Cancer Center, the University of Louisville (Ky.).
He presented the new data at the virtual American Association for Cancer Research (AACR) Annual Meeting 2021.
Customized cell therapy with TILs has been explored for the treatment of melanoma for more than a decade. Some researchers have reported durable response in 25% of patients.
However, “generalizing TIL therapy has been hampered by the complex and really not absolutely defined process for generating cells,” commented Philip Greenberg, MD, professor and head of the program in immunology in the Clinical Research Division of the Fred Hutchinson Cancer Center, Seattle, who was the invited discussant.
The current study demonstrates that cell generation can be performed at a centralized facility that has the required technical expertise. The patient-specific products are then disseminated to multiple centers, he said. The study also demonstrates that TILs can be successfully generated from tumor sites other than skin or lymph nodes.
“Toxicity was, however, significant, although it was generally manageable, and it did occur early, generally within the first 2 weeks,” he noted.
Patient-derived product
Lifileucel is a tailor-made immunotherapy product created from melanoma tumor tissues resected from lesions in skin, lymph nodes, liver, lung, peritoneum, musculoskeletal system, breast, or other visceral organs. The cells are shipped to a central manufacturing facility, whre the TILs are isolated, cultured, expanded, and reinvigorated. The cells are then harvested and cryopreserved. The process takes about 22 days. The cryopreserved product is then shipped back to the treating facility.
Prior to receiving the expanded and rejuvenated TILs, patients undergo myeloablative conditioning with cyclophosphamide followed by fludarabine. The TILs are then delivered in a single infusion, followed by administration of up to six doses of interleukin-2 (IL-2).
Details from clinical trial
At the meeting, Dr. Chesney reported details on the 66 patients in the trial. They had metastatic melanoma that was progressing on treatment. The mean number of prior lines of therapy was 3.3. All of the patients had received prior anti–programmed cell death protein–1 (PD-1) or programmed cell death–ligand-1 (PD-L1) agents; 53 had received a cytotoxic T lymphocyte protein 4 (CTLA-4) inhibitor; and 15 had received a BRAF/MEK inhibitor.
These patients had a mean of six baseline target and nontarget lesions, and 28 patients had liver and/or brain metastases.
Just over a third of patients (24 of 66, 36.4%) had an objective response; three patients had a complete response; and 21 had a partial response. In addition, 29 patients had stable disease, and nine experienced disease progression. Four patients had not undergone the first assessment at the time of data cutoff.
After a median follow-up of 28.1 months, the median duration of response was not reached. It ranged from 2.2 to > 35.2 months.
Since the data cutoff in April 2020, reduction of tumor burden has occurred in 50 of 62 evaluable patients. Reductions in the target lesion sum of diameters has occurred in 11 patients. In one patient, a partial response converted to a complete response 24 months after infusion, Dr. Chesney noted.
The mean number of TILs infused was 27.3 billion (27.3 x 109). Appropriate amounts of TILs were manufactured from tumor samples acquired across all sites, and reductions in target lesion sum of diameter were seen across the range of TIL total cell doses.
All patients experienced at least one adverse event of any grade; all but two experienced grade 3 or 4 adverse events. Two patients died, one as a result of intra-abdominal hemorrhage considered possibly related to TIL therapy, and one from acute respiratory failure deemed not related to TILs.
The most common grade 3 or 4 adverse events were thrombocytopenia, anemia, febrile neutropenia, neutropenia, hypophosphatemia, and lymphopenia.
“The adverse event profile was manageable and was consistent with the underlying and the known profiles of the nonmyeloblative depletion regimen and IL-2,” Dr. Chesney said.
The decreasing frequency of adverse events over time reflects the potential benefit of the one-time infusion, and no new safety risks have been identified during more than 2 years of follow-up, he added.
Remaining questions, next steps
Dr. Greenberg commented that the one of the limitations of the study is that the investigators did not characterize the TIL product.
“Studies have predicted that there’s a particular type of cell, a stemlike T cell, that’s responsible for mediating the efficacy,” he commented. He referred to research from Steven Rosenberg, MD, PhD, and colleagues at the National Cancer Institute, where TILs were first used in 2002.
Dr. Greenberg also raised the question of whether high-dose IL-2 was required post infusion, given that the patients were lymphodepleted before receiving lifileucel.
Future steps for TIL therapy, he said, should include identification of biomarkers for success or failure; strategies to enhance generation and expansion of tumor-reactive T cells; postinfusion strategies, such as using vaccines and/or checkpoint inhibitors to increase therapeutic activity; genetic modifications to enhance the function of TILs in the tumor microenvironment; and research into other tumor types that may be effectively treated with TILs.
The study was supported by Iovance Biotherapeutics. Dr. Chesney has received research funding from Iovance and other companies and has consulted for Amgen and Replimune. Dr. Greenberg has served on scientific advisory boards, has received grant/research support, and owns stock in several companies that do not include Iovance.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – In just over one-third of patients with metastatic melanoma who had experienced disease progression while receiving multiple prior lines of therapy, including immunotherapy and targeted agents,
The product, called lifileucel, is custom made for each patient and utilizes tumor-infiltrating lymphocytes (TILs) extracted from tumor lesions. This approach differs from other cell-based therapies, such as chimeric antigen receptor (CAR) T cell therapy, which utilizes T cells collected from the patient’s blood.
The new results come from a phase 2 trial conducted in 66 patients with previously treated unresectable or metastatic melanoma who received a single dose of the product. The objective response rate was 36.4%.
“Lifileucel has demonstrated efficacy and durability of response for patients with metastatic melanoma and represents a viable therapeutic option warranting further investigation,” commented Jason Alan Chesney, MD, PhD, from the James Graham Brown Cancer Center, the University of Louisville (Ky.).
He presented the new data at the virtual American Association for Cancer Research (AACR) Annual Meeting 2021.
Customized cell therapy with TILs has been explored for the treatment of melanoma for more than a decade. Some researchers have reported durable response in 25% of patients.
However, “generalizing TIL therapy has been hampered by the complex and really not absolutely defined process for generating cells,” commented Philip Greenberg, MD, professor and head of the program in immunology in the Clinical Research Division of the Fred Hutchinson Cancer Center, Seattle, who was the invited discussant.
The current study demonstrates that cell generation can be performed at a centralized facility that has the required technical expertise. The patient-specific products are then disseminated to multiple centers, he said. The study also demonstrates that TILs can be successfully generated from tumor sites other than skin or lymph nodes.
“Toxicity was, however, significant, although it was generally manageable, and it did occur early, generally within the first 2 weeks,” he noted.
Patient-derived product
Lifileucel is a tailor-made immunotherapy product created from melanoma tumor tissues resected from lesions in skin, lymph nodes, liver, lung, peritoneum, musculoskeletal system, breast, or other visceral organs. The cells are shipped to a central manufacturing facility, whre the TILs are isolated, cultured, expanded, and reinvigorated. The cells are then harvested and cryopreserved. The process takes about 22 days. The cryopreserved product is then shipped back to the treating facility.
Prior to receiving the expanded and rejuvenated TILs, patients undergo myeloablative conditioning with cyclophosphamide followed by fludarabine. The TILs are then delivered in a single infusion, followed by administration of up to six doses of interleukin-2 (IL-2).
Details from clinical trial
At the meeting, Dr. Chesney reported details on the 66 patients in the trial. They had metastatic melanoma that was progressing on treatment. The mean number of prior lines of therapy was 3.3. All of the patients had received prior anti–programmed cell death protein–1 (PD-1) or programmed cell death–ligand-1 (PD-L1) agents; 53 had received a cytotoxic T lymphocyte protein 4 (CTLA-4) inhibitor; and 15 had received a BRAF/MEK inhibitor.
These patients had a mean of six baseline target and nontarget lesions, and 28 patients had liver and/or brain metastases.
Just over a third of patients (24 of 66, 36.4%) had an objective response; three patients had a complete response; and 21 had a partial response. In addition, 29 patients had stable disease, and nine experienced disease progression. Four patients had not undergone the first assessment at the time of data cutoff.
After a median follow-up of 28.1 months, the median duration of response was not reached. It ranged from 2.2 to > 35.2 months.
Since the data cutoff in April 2020, reduction of tumor burden has occurred in 50 of 62 evaluable patients. Reductions in the target lesion sum of diameters has occurred in 11 patients. In one patient, a partial response converted to a complete response 24 months after infusion, Dr. Chesney noted.
The mean number of TILs infused was 27.3 billion (27.3 x 109). Appropriate amounts of TILs were manufactured from tumor samples acquired across all sites, and reductions in target lesion sum of diameter were seen across the range of TIL total cell doses.
All patients experienced at least one adverse event of any grade; all but two experienced grade 3 or 4 adverse events. Two patients died, one as a result of intra-abdominal hemorrhage considered possibly related to TIL therapy, and one from acute respiratory failure deemed not related to TILs.
The most common grade 3 or 4 adverse events were thrombocytopenia, anemia, febrile neutropenia, neutropenia, hypophosphatemia, and lymphopenia.
“The adverse event profile was manageable and was consistent with the underlying and the known profiles of the nonmyeloblative depletion regimen and IL-2,” Dr. Chesney said.
The decreasing frequency of adverse events over time reflects the potential benefit of the one-time infusion, and no new safety risks have been identified during more than 2 years of follow-up, he added.
Remaining questions, next steps
Dr. Greenberg commented that the one of the limitations of the study is that the investigators did not characterize the TIL product.
“Studies have predicted that there’s a particular type of cell, a stemlike T cell, that’s responsible for mediating the efficacy,” he commented. He referred to research from Steven Rosenberg, MD, PhD, and colleagues at the National Cancer Institute, where TILs were first used in 2002.
Dr. Greenberg also raised the question of whether high-dose IL-2 was required post infusion, given that the patients were lymphodepleted before receiving lifileucel.
Future steps for TIL therapy, he said, should include identification of biomarkers for success or failure; strategies to enhance generation and expansion of tumor-reactive T cells; postinfusion strategies, such as using vaccines and/or checkpoint inhibitors to increase therapeutic activity; genetic modifications to enhance the function of TILs in the tumor microenvironment; and research into other tumor types that may be effectively treated with TILs.
The study was supported by Iovance Biotherapeutics. Dr. Chesney has received research funding from Iovance and other companies and has consulted for Amgen and Replimune. Dr. Greenberg has served on scientific advisory boards, has received grant/research support, and owns stock in several companies that do not include Iovance.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – In just over one-third of patients with metastatic melanoma who had experienced disease progression while receiving multiple prior lines of therapy, including immunotherapy and targeted agents,
The product, called lifileucel, is custom made for each patient and utilizes tumor-infiltrating lymphocytes (TILs) extracted from tumor lesions. This approach differs from other cell-based therapies, such as chimeric antigen receptor (CAR) T cell therapy, which utilizes T cells collected from the patient’s blood.
The new results come from a phase 2 trial conducted in 66 patients with previously treated unresectable or metastatic melanoma who received a single dose of the product. The objective response rate was 36.4%.
“Lifileucel has demonstrated efficacy and durability of response for patients with metastatic melanoma and represents a viable therapeutic option warranting further investigation,” commented Jason Alan Chesney, MD, PhD, from the James Graham Brown Cancer Center, the University of Louisville (Ky.).
He presented the new data at the virtual American Association for Cancer Research (AACR) Annual Meeting 2021.
Customized cell therapy with TILs has been explored for the treatment of melanoma for more than a decade. Some researchers have reported durable response in 25% of patients.
However, “generalizing TIL therapy has been hampered by the complex and really not absolutely defined process for generating cells,” commented Philip Greenberg, MD, professor and head of the program in immunology in the Clinical Research Division of the Fred Hutchinson Cancer Center, Seattle, who was the invited discussant.
The current study demonstrates that cell generation can be performed at a centralized facility that has the required technical expertise. The patient-specific products are then disseminated to multiple centers, he said. The study also demonstrates that TILs can be successfully generated from tumor sites other than skin or lymph nodes.
“Toxicity was, however, significant, although it was generally manageable, and it did occur early, generally within the first 2 weeks,” he noted.
Patient-derived product
Lifileucel is a tailor-made immunotherapy product created from melanoma tumor tissues resected from lesions in skin, lymph nodes, liver, lung, peritoneum, musculoskeletal system, breast, or other visceral organs. The cells are shipped to a central manufacturing facility, whre the TILs are isolated, cultured, expanded, and reinvigorated. The cells are then harvested and cryopreserved. The process takes about 22 days. The cryopreserved product is then shipped back to the treating facility.
Prior to receiving the expanded and rejuvenated TILs, patients undergo myeloablative conditioning with cyclophosphamide followed by fludarabine. The TILs are then delivered in a single infusion, followed by administration of up to six doses of interleukin-2 (IL-2).
Details from clinical trial
At the meeting, Dr. Chesney reported details on the 66 patients in the trial. They had metastatic melanoma that was progressing on treatment. The mean number of prior lines of therapy was 3.3. All of the patients had received prior anti–programmed cell death protein–1 (PD-1) or programmed cell death–ligand-1 (PD-L1) agents; 53 had received a cytotoxic T lymphocyte protein 4 (CTLA-4) inhibitor; and 15 had received a BRAF/MEK inhibitor.
These patients had a mean of six baseline target and nontarget lesions, and 28 patients had liver and/or brain metastases.
Just over a third of patients (24 of 66, 36.4%) had an objective response; three patients had a complete response; and 21 had a partial response. In addition, 29 patients had stable disease, and nine experienced disease progression. Four patients had not undergone the first assessment at the time of data cutoff.
After a median follow-up of 28.1 months, the median duration of response was not reached. It ranged from 2.2 to > 35.2 months.
Since the data cutoff in April 2020, reduction of tumor burden has occurred in 50 of 62 evaluable patients. Reductions in the target lesion sum of diameters has occurred in 11 patients. In one patient, a partial response converted to a complete response 24 months after infusion, Dr. Chesney noted.
The mean number of TILs infused was 27.3 billion (27.3 x 109). Appropriate amounts of TILs were manufactured from tumor samples acquired across all sites, and reductions in target lesion sum of diameter were seen across the range of TIL total cell doses.
All patients experienced at least one adverse event of any grade; all but two experienced grade 3 or 4 adverse events. Two patients died, one as a result of intra-abdominal hemorrhage considered possibly related to TIL therapy, and one from acute respiratory failure deemed not related to TILs.
The most common grade 3 or 4 adverse events were thrombocytopenia, anemia, febrile neutropenia, neutropenia, hypophosphatemia, and lymphopenia.
“The adverse event profile was manageable and was consistent with the underlying and the known profiles of the nonmyeloblative depletion regimen and IL-2,” Dr. Chesney said.
The decreasing frequency of adverse events over time reflects the potential benefit of the one-time infusion, and no new safety risks have been identified during more than 2 years of follow-up, he added.
Remaining questions, next steps
Dr. Greenberg commented that the one of the limitations of the study is that the investigators did not characterize the TIL product.
“Studies have predicted that there’s a particular type of cell, a stemlike T cell, that’s responsible for mediating the efficacy,” he commented. He referred to research from Steven Rosenberg, MD, PhD, and colleagues at the National Cancer Institute, where TILs were first used in 2002.
Dr. Greenberg also raised the question of whether high-dose IL-2 was required post infusion, given that the patients were lymphodepleted before receiving lifileucel.
Future steps for TIL therapy, he said, should include identification of biomarkers for success or failure; strategies to enhance generation and expansion of tumor-reactive T cells; postinfusion strategies, such as using vaccines and/or checkpoint inhibitors to increase therapeutic activity; genetic modifications to enhance the function of TILs in the tumor microenvironment; and research into other tumor types that may be effectively treated with TILs.
The study was supported by Iovance Biotherapeutics. Dr. Chesney has received research funding from Iovance and other companies and has consulted for Amgen and Replimune. Dr. Greenberg has served on scientific advisory boards, has received grant/research support, and owns stock in several companies that do not include Iovance.
A version of this article first appeared on Medscape.com.
AT AACR 2022
‘Major advance’: Sotorasib benefit persists in KRAS+ NSCLC
NEW ORLEANS – with the first-in-class KRAS inhibitor sotorasib (Lumakras, Amgen).
The finding comes from an analysis of long-term follow-up data from the CodeBreaK100 trial, which showed a 2-year overall survival (OS) rate of 32.5% in pretreated patients with KRASG12C-mutant disease.
That rate compares favorably with historical data on NSCLC therapies, said Grace K. Dy, MD, from Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“We expect about half of that [survival rate] in patients who are treated with docetaxel,” she said in a plenary session at the annual meeting of the American Association for Cancer Research.
Sotorasib was approved by the Food and Drug Administration in May 2021 as the first drug for patients with NSCLC and KRAS mutations and was described as a “historic milestone.”
In this most recent analysis, which combined data from patients enrolled in phases 1 and 2 of the trial, the “objective response rate of 41% of patients was achieved with sotorasib, with a durable [disease] control rate of 84% and a median duration of response of 12.3 months, with no new safety signals emerging,” she said.
Nearly one-fourth of patients saw long-term benefit, as defined by progression-free survival of at least 12 months, and this long-term benefit was seen across variant allele frequencies of KRASG12C, programmed death–ligand 1 (PD-L1) tumor proportion score, and other comutations, she noted.
“KRASG12C inhibitors represent a major advance in the treatment of KRAS-mutant lung cancers and other types as well,” said invited discussant Mark M. Awad, MD, PhD, director of clinical research at the Lowe Center for Thoracic Oncology at Dana-Farber Cancer Center, Boston.
He cautioned, however, that “the therapeutic efficacy of these G12C inhibitors is currently limited by several things, including patient factors, intrinsic biology, and the emergence of complex resistance mechanisms.”
New approaches will be needed, he said, “to delay and overcome drug resistance to hopefully keep kicking cancer’s KRAS.”
At a media briefing where Dr. Dy presented the data prior to the oral abstract session, moderator Timothy A. Yap, MBBS, PhD, from the University of Texas MD Anderson Cancer Center, Houston, commented that the development of drug resistance is common in oncology.
“That is exactly why we’re now actively working on multiple different combinatorial approaches in the clinic. There have been pretty compelling data published from Mirati [Therapeutics] and from other companies, from Amgen, that really show the resistance mechanisms that actually come about upon monotherapy with KRASG12C inhibitors, including CDK4/6, including P13K-Akt pathways,” he said.
“The solution there really is, No. 1, we need to identify proactively the resistance mechanisms involved and driving each cancer’s resistance, and No. 2, then apply the combinatorial agent, to bring in a combination that’s a rational approach to match a patient’s molecular profile upon resistance,” he said.
Tarnished triumph
As previously reported, sotorasib was hailed as “a triumph of drug discovery” when early results of the trial were reported at the European Society of Medical Oncology annual meeting in 2020.
Sotorasib is a small-molecule, specific, and irreversible inhibitor of KRAS that interacts with a “pocket” on the gene’s surface that is present only in an inactive conformation of KRAS. The drug inhibits oncogenic signaling and tumorigenesis by preventing cycling of the oncogene into its active form.
But as Dr. Awad reported at the 2021 AACR annual meeting, the efficacy of sotorasib and other KRAS inhibitors in development has been threatened by the development of resistance caused by a wide range of genomic and histologic mechanisms.
Dr. Awad reported that among 30 patients with NSCLC or colorectal cancer bearing the KRASG12C mutation who had disease progression while being treated with the investigational inhibitor adagrasib in clinical trials, investigators found multiple on-target KRAS alterations and off-target bypass mechanisms of acquired resistance to the drug.
“Diverse mechanisms confer resistance to the KRASG12C inhibitors, including secondary KRAS mutations, MAP [mitogen-activated protein] kinase pathway alterations, acquired genomic rearrangements, and histologic transformation,” he said.
Long follow-up
The long-term data reported at the 2022 meeting by Dr. Dy and colleagues included data on 48 patients enrolled in phase 1 of the trial, which had a primary endpoint of safety and tolerability, and 126 patients enrolled in phase 2, with a primary endpoint of objective response rate by blinded independent review.
The trial was conducted in centers in the United States, Europe, Australia, Japan, and South Korea.
Nearly all patients were pretreated: 92.5% of patients had received prior platinum-based chemotherapy and 90.2% had received anti–PD-1/PD-L1 immunotherapy.
Patients received oral sotorasib 960 mg once daily and were followed with radiographic scans every 6 weeks for the first year and once every 12 weeks thereafter.
Of the 174 patients enrolled, two were not evaluable for response at 2 years because of a lack of measurable lesions at baseline.
At a median follow-up of 24.9 months, 5 patients (2.9%) had a complete response and 65 (37.8%) had a partial response, for an objective response rate of 40.7%. An additional 74 patients (43%) had stable disease, for a disease control rate of 83.7%. Of the remaining patients, 23 (13.4%) had disease progression, and 5 were either not evaluable or had missing scan data.
Median progression-free survival was 6.3 months. Median time to response was 6 weeks, and median duration of response was 12.3 months. Half of patients who had a response retained that response for at least 12 months.
Median OS was 12.5 months. The 1-year and 2-year OS rates were 50.8% and 32.5%, respectively.
Grade 3 or 4 treatment-related adverse events occurred in 21% of patients, and one patient had new-onset grade 3 hemolytic anemia 1 year after starting therapy. There were no treatment-related deaths and no treatment-related adverse events leading to discontinuation after the first year.
In exploratory analyses, the benefit of the drug was seen across tumors with varying levels of PD-L1 expression and the oncogenic STK11 comutation, and across KRASG12C variant allele frequency.
The investigators also reported that baseline circulating tumor DNA levels correlated with tumor burden, and that patients who had long-term benefits had lower baseline ctDNA. This finding is consistent with the documented role of ctDNA as a marker for poor prognosis regardless of therapy.
Dr. Dy reported receiving consulting fees from AstraZeneca, Eli Lilly, Mirati Therapeutics, and Takeda in the past 2 years. Dr. Yap disclosed receiving consulting fees from multiple companies. Dr. Awad disclosed consulting for multiple companies.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – with the first-in-class KRAS inhibitor sotorasib (Lumakras, Amgen).
The finding comes from an analysis of long-term follow-up data from the CodeBreaK100 trial, which showed a 2-year overall survival (OS) rate of 32.5% in pretreated patients with KRASG12C-mutant disease.
That rate compares favorably with historical data on NSCLC therapies, said Grace K. Dy, MD, from Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“We expect about half of that [survival rate] in patients who are treated with docetaxel,” she said in a plenary session at the annual meeting of the American Association for Cancer Research.
Sotorasib was approved by the Food and Drug Administration in May 2021 as the first drug for patients with NSCLC and KRAS mutations and was described as a “historic milestone.”
In this most recent analysis, which combined data from patients enrolled in phases 1 and 2 of the trial, the “objective response rate of 41% of patients was achieved with sotorasib, with a durable [disease] control rate of 84% and a median duration of response of 12.3 months, with no new safety signals emerging,” she said.
Nearly one-fourth of patients saw long-term benefit, as defined by progression-free survival of at least 12 months, and this long-term benefit was seen across variant allele frequencies of KRASG12C, programmed death–ligand 1 (PD-L1) tumor proportion score, and other comutations, she noted.
“KRASG12C inhibitors represent a major advance in the treatment of KRAS-mutant lung cancers and other types as well,” said invited discussant Mark M. Awad, MD, PhD, director of clinical research at the Lowe Center for Thoracic Oncology at Dana-Farber Cancer Center, Boston.
He cautioned, however, that “the therapeutic efficacy of these G12C inhibitors is currently limited by several things, including patient factors, intrinsic biology, and the emergence of complex resistance mechanisms.”
New approaches will be needed, he said, “to delay and overcome drug resistance to hopefully keep kicking cancer’s KRAS.”
At a media briefing where Dr. Dy presented the data prior to the oral abstract session, moderator Timothy A. Yap, MBBS, PhD, from the University of Texas MD Anderson Cancer Center, Houston, commented that the development of drug resistance is common in oncology.
“That is exactly why we’re now actively working on multiple different combinatorial approaches in the clinic. There have been pretty compelling data published from Mirati [Therapeutics] and from other companies, from Amgen, that really show the resistance mechanisms that actually come about upon monotherapy with KRASG12C inhibitors, including CDK4/6, including P13K-Akt pathways,” he said.
“The solution there really is, No. 1, we need to identify proactively the resistance mechanisms involved and driving each cancer’s resistance, and No. 2, then apply the combinatorial agent, to bring in a combination that’s a rational approach to match a patient’s molecular profile upon resistance,” he said.
Tarnished triumph
As previously reported, sotorasib was hailed as “a triumph of drug discovery” when early results of the trial were reported at the European Society of Medical Oncology annual meeting in 2020.
Sotorasib is a small-molecule, specific, and irreversible inhibitor of KRAS that interacts with a “pocket” on the gene’s surface that is present only in an inactive conformation of KRAS. The drug inhibits oncogenic signaling and tumorigenesis by preventing cycling of the oncogene into its active form.
But as Dr. Awad reported at the 2021 AACR annual meeting, the efficacy of sotorasib and other KRAS inhibitors in development has been threatened by the development of resistance caused by a wide range of genomic and histologic mechanisms.
Dr. Awad reported that among 30 patients with NSCLC or colorectal cancer bearing the KRASG12C mutation who had disease progression while being treated with the investigational inhibitor adagrasib in clinical trials, investigators found multiple on-target KRAS alterations and off-target bypass mechanisms of acquired resistance to the drug.
“Diverse mechanisms confer resistance to the KRASG12C inhibitors, including secondary KRAS mutations, MAP [mitogen-activated protein] kinase pathway alterations, acquired genomic rearrangements, and histologic transformation,” he said.
Long follow-up
The long-term data reported at the 2022 meeting by Dr. Dy and colleagues included data on 48 patients enrolled in phase 1 of the trial, which had a primary endpoint of safety and tolerability, and 126 patients enrolled in phase 2, with a primary endpoint of objective response rate by blinded independent review.
The trial was conducted in centers in the United States, Europe, Australia, Japan, and South Korea.
Nearly all patients were pretreated: 92.5% of patients had received prior platinum-based chemotherapy and 90.2% had received anti–PD-1/PD-L1 immunotherapy.
Patients received oral sotorasib 960 mg once daily and were followed with radiographic scans every 6 weeks for the first year and once every 12 weeks thereafter.
Of the 174 patients enrolled, two were not evaluable for response at 2 years because of a lack of measurable lesions at baseline.
At a median follow-up of 24.9 months, 5 patients (2.9%) had a complete response and 65 (37.8%) had a partial response, for an objective response rate of 40.7%. An additional 74 patients (43%) had stable disease, for a disease control rate of 83.7%. Of the remaining patients, 23 (13.4%) had disease progression, and 5 were either not evaluable or had missing scan data.
Median progression-free survival was 6.3 months. Median time to response was 6 weeks, and median duration of response was 12.3 months. Half of patients who had a response retained that response for at least 12 months.
Median OS was 12.5 months. The 1-year and 2-year OS rates were 50.8% and 32.5%, respectively.
Grade 3 or 4 treatment-related adverse events occurred in 21% of patients, and one patient had new-onset grade 3 hemolytic anemia 1 year after starting therapy. There were no treatment-related deaths and no treatment-related adverse events leading to discontinuation after the first year.
In exploratory analyses, the benefit of the drug was seen across tumors with varying levels of PD-L1 expression and the oncogenic STK11 comutation, and across KRASG12C variant allele frequency.
The investigators also reported that baseline circulating tumor DNA levels correlated with tumor burden, and that patients who had long-term benefits had lower baseline ctDNA. This finding is consistent with the documented role of ctDNA as a marker for poor prognosis regardless of therapy.
Dr. Dy reported receiving consulting fees from AstraZeneca, Eli Lilly, Mirati Therapeutics, and Takeda in the past 2 years. Dr. Yap disclosed receiving consulting fees from multiple companies. Dr. Awad disclosed consulting for multiple companies.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – with the first-in-class KRAS inhibitor sotorasib (Lumakras, Amgen).
The finding comes from an analysis of long-term follow-up data from the CodeBreaK100 trial, which showed a 2-year overall survival (OS) rate of 32.5% in pretreated patients with KRASG12C-mutant disease.
That rate compares favorably with historical data on NSCLC therapies, said Grace K. Dy, MD, from Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
“We expect about half of that [survival rate] in patients who are treated with docetaxel,” she said in a plenary session at the annual meeting of the American Association for Cancer Research.
Sotorasib was approved by the Food and Drug Administration in May 2021 as the first drug for patients with NSCLC and KRAS mutations and was described as a “historic milestone.”
In this most recent analysis, which combined data from patients enrolled in phases 1 and 2 of the trial, the “objective response rate of 41% of patients was achieved with sotorasib, with a durable [disease] control rate of 84% and a median duration of response of 12.3 months, with no new safety signals emerging,” she said.
Nearly one-fourth of patients saw long-term benefit, as defined by progression-free survival of at least 12 months, and this long-term benefit was seen across variant allele frequencies of KRASG12C, programmed death–ligand 1 (PD-L1) tumor proportion score, and other comutations, she noted.
“KRASG12C inhibitors represent a major advance in the treatment of KRAS-mutant lung cancers and other types as well,” said invited discussant Mark M. Awad, MD, PhD, director of clinical research at the Lowe Center for Thoracic Oncology at Dana-Farber Cancer Center, Boston.
He cautioned, however, that “the therapeutic efficacy of these G12C inhibitors is currently limited by several things, including patient factors, intrinsic biology, and the emergence of complex resistance mechanisms.”
New approaches will be needed, he said, “to delay and overcome drug resistance to hopefully keep kicking cancer’s KRAS.”
At a media briefing where Dr. Dy presented the data prior to the oral abstract session, moderator Timothy A. Yap, MBBS, PhD, from the University of Texas MD Anderson Cancer Center, Houston, commented that the development of drug resistance is common in oncology.
“That is exactly why we’re now actively working on multiple different combinatorial approaches in the clinic. There have been pretty compelling data published from Mirati [Therapeutics] and from other companies, from Amgen, that really show the resistance mechanisms that actually come about upon monotherapy with KRASG12C inhibitors, including CDK4/6, including P13K-Akt pathways,” he said.
“The solution there really is, No. 1, we need to identify proactively the resistance mechanisms involved and driving each cancer’s resistance, and No. 2, then apply the combinatorial agent, to bring in a combination that’s a rational approach to match a patient’s molecular profile upon resistance,” he said.
Tarnished triumph
As previously reported, sotorasib was hailed as “a triumph of drug discovery” when early results of the trial were reported at the European Society of Medical Oncology annual meeting in 2020.
Sotorasib is a small-molecule, specific, and irreversible inhibitor of KRAS that interacts with a “pocket” on the gene’s surface that is present only in an inactive conformation of KRAS. The drug inhibits oncogenic signaling and tumorigenesis by preventing cycling of the oncogene into its active form.
But as Dr. Awad reported at the 2021 AACR annual meeting, the efficacy of sotorasib and other KRAS inhibitors in development has been threatened by the development of resistance caused by a wide range of genomic and histologic mechanisms.
Dr. Awad reported that among 30 patients with NSCLC or colorectal cancer bearing the KRASG12C mutation who had disease progression while being treated with the investigational inhibitor adagrasib in clinical trials, investigators found multiple on-target KRAS alterations and off-target bypass mechanisms of acquired resistance to the drug.
“Diverse mechanisms confer resistance to the KRASG12C inhibitors, including secondary KRAS mutations, MAP [mitogen-activated protein] kinase pathway alterations, acquired genomic rearrangements, and histologic transformation,” he said.
Long follow-up
The long-term data reported at the 2022 meeting by Dr. Dy and colleagues included data on 48 patients enrolled in phase 1 of the trial, which had a primary endpoint of safety and tolerability, and 126 patients enrolled in phase 2, with a primary endpoint of objective response rate by blinded independent review.
The trial was conducted in centers in the United States, Europe, Australia, Japan, and South Korea.
Nearly all patients were pretreated: 92.5% of patients had received prior platinum-based chemotherapy and 90.2% had received anti–PD-1/PD-L1 immunotherapy.
Patients received oral sotorasib 960 mg once daily and were followed with radiographic scans every 6 weeks for the first year and once every 12 weeks thereafter.
Of the 174 patients enrolled, two were not evaluable for response at 2 years because of a lack of measurable lesions at baseline.
At a median follow-up of 24.9 months, 5 patients (2.9%) had a complete response and 65 (37.8%) had a partial response, for an objective response rate of 40.7%. An additional 74 patients (43%) had stable disease, for a disease control rate of 83.7%. Of the remaining patients, 23 (13.4%) had disease progression, and 5 were either not evaluable or had missing scan data.
Median progression-free survival was 6.3 months. Median time to response was 6 weeks, and median duration of response was 12.3 months. Half of patients who had a response retained that response for at least 12 months.
Median OS was 12.5 months. The 1-year and 2-year OS rates were 50.8% and 32.5%, respectively.
Grade 3 or 4 treatment-related adverse events occurred in 21% of patients, and one patient had new-onset grade 3 hemolytic anemia 1 year after starting therapy. There were no treatment-related deaths and no treatment-related adverse events leading to discontinuation after the first year.
In exploratory analyses, the benefit of the drug was seen across tumors with varying levels of PD-L1 expression and the oncogenic STK11 comutation, and across KRASG12C variant allele frequency.
The investigators also reported that baseline circulating tumor DNA levels correlated with tumor burden, and that patients who had long-term benefits had lower baseline ctDNA. This finding is consistent with the documented role of ctDNA as a marker for poor prognosis regardless of therapy.
Dr. Dy reported receiving consulting fees from AstraZeneca, Eli Lilly, Mirati Therapeutics, and Takeda in the past 2 years. Dr. Yap disclosed receiving consulting fees from multiple companies. Dr. Awad disclosed consulting for multiple companies.
A version of this article first appeared on Medscape.com.
AT AACR 2022
Sex differences in COPD slow to be recognized, treated
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
Global melanoma incidence high and on the rise
Even by cautious calculations,
An estimated 325,000 people worldwide received a new diagnosis of cutaneous melanoma in 2020, and if present trends continue, the incidence of new cases is predicted to increase by about 50% in 2040, with melanoma deaths expected to rise by almost 70%, Melina Arnold, PhD, from the Cancer Surveillance Branch of the International Agency for Research on Cancer in Lyon, France, and colleagues reported.
“Melanoma is the most lethal form of skin cancer; this epidemiological assessment found a heavy public health and economic burden, and our projections suggest that it will remain so in the coming decades,” they wrote in a study published online in JAMA Dermatology.
In an accompanying editorial, Mavis Obeng-Kusi, MPharm and Ivo Abraham, PhD from the Center for Health Outcomes and PharmacoEconomic Research at the University of Arizona, Tucson, commented that the findings are “sobering,” but may substantially underestimate the gravity of the problem in low- and middle-income countries (LMIC).
“The study by Arnold et al. brings to the fore a public health concern that requires global attention and initiates conversations particularly related to LMIC settings, where the incidence and mortality of melanoma is thought to be minimal and for which preventive measures may be insufficient,” they wrote.
Down Under nations lead
Dr. Arnold and colleagues looked at data on age-standardized melanoma incidence and mortality rates per 100,000 person-years (PY) by country, each of 20 world regions as defined by the United Nations, and according to the UN’s four-tier Human Development Index, which stratifies countries into low-, medium-, high-, and very high–income categories.
As noted previously, the researchers estimated that there were 325,000 new melanoma cases worldwide in 2020 (174,000 cases in males and 151,000 in females). There were 57,000 estimated melanoma deaths the same year (32,000 in males and 25,000 in females.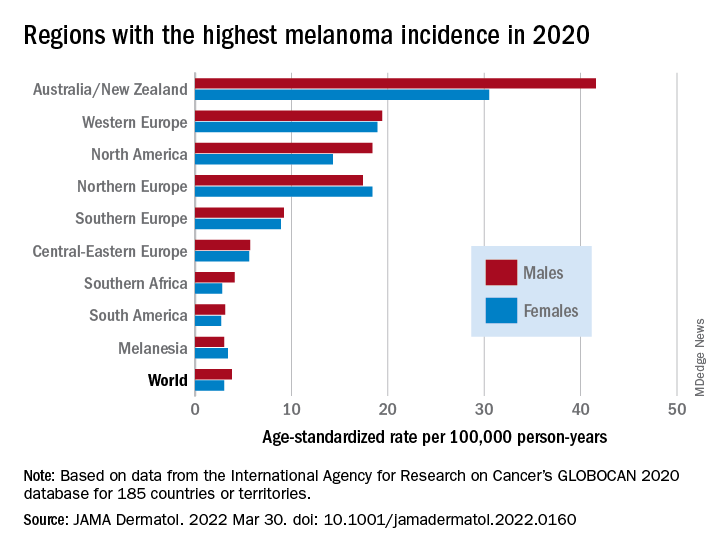
The highest incidence rates were seen in Australia and New Zealand, at 42 per 100,000 PY among males and 31 per 100,000 PY in females, followed by Western Europe with 19 per 100,000 PY in both males and females, North America with 18 and 14 cases per 100,000 PY in males and females respectively, and Northern Europe, with 17 per 100,000 PY in males, and 18 per 100,000 PY in females.
In contrast, in most African and Asian countries melanoma was rare, with rates commonly less than 1 per 100,000 PY, the investigators noted.
The melanoma mortality rate was highest in New Zealand, at 5 per 100,000 PY. Mortality rates worldwide varied less widely than incidence rates. In most other regions of the world, mortality rates were “much lower,” ranging between 0.2-1.0 per 100,000 PY, they wrote.
The authors estimated that, if 2020 rates remain stable, the global burden from melanoma in 2040 will increase to approximately 510,000 new cases and 96,000 deaths.
Public health efforts needed
In their editorial, Ms. Obeng-Kusi and Dr. Abraham pointed out that the study was hampered by the limited availability of cancer data from LMICs, leading the authors to estimate incidence and mortality rates based on proxy data, such as statistical modeling or averaged rates from neighboring countries.
They emphasized the need for going beyond the statistics: “Specific to cutaneous melanoma data, what is most important globally, knowing the exact numbers of cases and deaths or understanding the order of magnitude of the present and future epidemiology? No doubt the latter. Melanoma can be treated more easily if caught at earlier stages.”
Projections such as those provided by Dr. Arnold and colleagues could help to raise awareness of the importance of decreasing exposure to UV radiation, which accounts for three-fourths of all incident melanomas, the editorialists said.
The study was funded in part by a grant to coauthor Anna E. Cust, PhD, MPH. Dr. Cust reported receiving a fellowship from the Australian National Health and Medical Research Council outside the submitted work. Dr. Arnold had no conflicts of interested to disclose. Dr. Abraham reported financial relationships with various entities. Ms. Obeng-Kusi had no disclosures.
Even by cautious calculations,
An estimated 325,000 people worldwide received a new diagnosis of cutaneous melanoma in 2020, and if present trends continue, the incidence of new cases is predicted to increase by about 50% in 2040, with melanoma deaths expected to rise by almost 70%, Melina Arnold, PhD, from the Cancer Surveillance Branch of the International Agency for Research on Cancer in Lyon, France, and colleagues reported.
“Melanoma is the most lethal form of skin cancer; this epidemiological assessment found a heavy public health and economic burden, and our projections suggest that it will remain so in the coming decades,” they wrote in a study published online in JAMA Dermatology.
In an accompanying editorial, Mavis Obeng-Kusi, MPharm and Ivo Abraham, PhD from the Center for Health Outcomes and PharmacoEconomic Research at the University of Arizona, Tucson, commented that the findings are “sobering,” but may substantially underestimate the gravity of the problem in low- and middle-income countries (LMIC).
“The study by Arnold et al. brings to the fore a public health concern that requires global attention and initiates conversations particularly related to LMIC settings, where the incidence and mortality of melanoma is thought to be minimal and for which preventive measures may be insufficient,” they wrote.
Down Under nations lead
Dr. Arnold and colleagues looked at data on age-standardized melanoma incidence and mortality rates per 100,000 person-years (PY) by country, each of 20 world regions as defined by the United Nations, and according to the UN’s four-tier Human Development Index, which stratifies countries into low-, medium-, high-, and very high–income categories.
As noted previously, the researchers estimated that there were 325,000 new melanoma cases worldwide in 2020 (174,000 cases in males and 151,000 in females). There were 57,000 estimated melanoma deaths the same year (32,000 in males and 25,000 in females.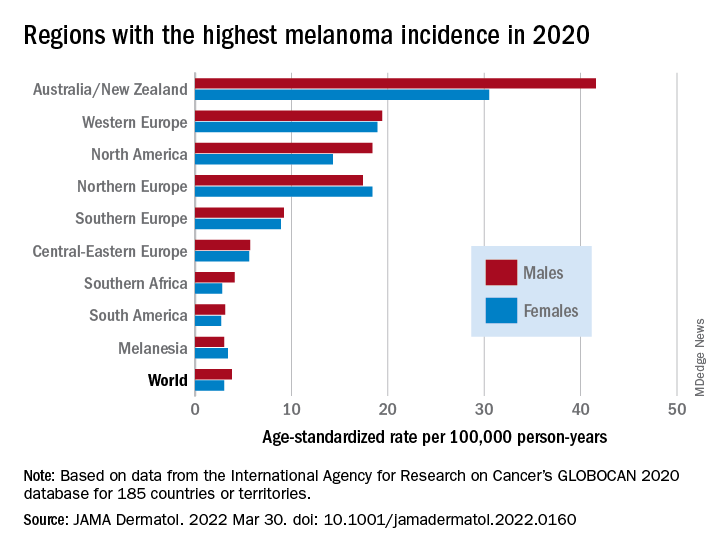
The highest incidence rates were seen in Australia and New Zealand, at 42 per 100,000 PY among males and 31 per 100,000 PY in females, followed by Western Europe with 19 per 100,000 PY in both males and females, North America with 18 and 14 cases per 100,000 PY in males and females respectively, and Northern Europe, with 17 per 100,000 PY in males, and 18 per 100,000 PY in females.
In contrast, in most African and Asian countries melanoma was rare, with rates commonly less than 1 per 100,000 PY, the investigators noted.
The melanoma mortality rate was highest in New Zealand, at 5 per 100,000 PY. Mortality rates worldwide varied less widely than incidence rates. In most other regions of the world, mortality rates were “much lower,” ranging between 0.2-1.0 per 100,000 PY, they wrote.
The authors estimated that, if 2020 rates remain stable, the global burden from melanoma in 2040 will increase to approximately 510,000 new cases and 96,000 deaths.
Public health efforts needed
In their editorial, Ms. Obeng-Kusi and Dr. Abraham pointed out that the study was hampered by the limited availability of cancer data from LMICs, leading the authors to estimate incidence and mortality rates based on proxy data, such as statistical modeling or averaged rates from neighboring countries.
They emphasized the need for going beyond the statistics: “Specific to cutaneous melanoma data, what is most important globally, knowing the exact numbers of cases and deaths or understanding the order of magnitude of the present and future epidemiology? No doubt the latter. Melanoma can be treated more easily if caught at earlier stages.”
Projections such as those provided by Dr. Arnold and colleagues could help to raise awareness of the importance of decreasing exposure to UV radiation, which accounts for three-fourths of all incident melanomas, the editorialists said.
The study was funded in part by a grant to coauthor Anna E. Cust, PhD, MPH. Dr. Cust reported receiving a fellowship from the Australian National Health and Medical Research Council outside the submitted work. Dr. Arnold had no conflicts of interested to disclose. Dr. Abraham reported financial relationships with various entities. Ms. Obeng-Kusi had no disclosures.
Even by cautious calculations,
An estimated 325,000 people worldwide received a new diagnosis of cutaneous melanoma in 2020, and if present trends continue, the incidence of new cases is predicted to increase by about 50% in 2040, with melanoma deaths expected to rise by almost 70%, Melina Arnold, PhD, from the Cancer Surveillance Branch of the International Agency for Research on Cancer in Lyon, France, and colleagues reported.
“Melanoma is the most lethal form of skin cancer; this epidemiological assessment found a heavy public health and economic burden, and our projections suggest that it will remain so in the coming decades,” they wrote in a study published online in JAMA Dermatology.
In an accompanying editorial, Mavis Obeng-Kusi, MPharm and Ivo Abraham, PhD from the Center for Health Outcomes and PharmacoEconomic Research at the University of Arizona, Tucson, commented that the findings are “sobering,” but may substantially underestimate the gravity of the problem in low- and middle-income countries (LMIC).
“The study by Arnold et al. brings to the fore a public health concern that requires global attention and initiates conversations particularly related to LMIC settings, where the incidence and mortality of melanoma is thought to be minimal and for which preventive measures may be insufficient,” they wrote.
Down Under nations lead
Dr. Arnold and colleagues looked at data on age-standardized melanoma incidence and mortality rates per 100,000 person-years (PY) by country, each of 20 world regions as defined by the United Nations, and according to the UN’s four-tier Human Development Index, which stratifies countries into low-, medium-, high-, and very high–income categories.
As noted previously, the researchers estimated that there were 325,000 new melanoma cases worldwide in 2020 (174,000 cases in males and 151,000 in females). There were 57,000 estimated melanoma deaths the same year (32,000 in males and 25,000 in females.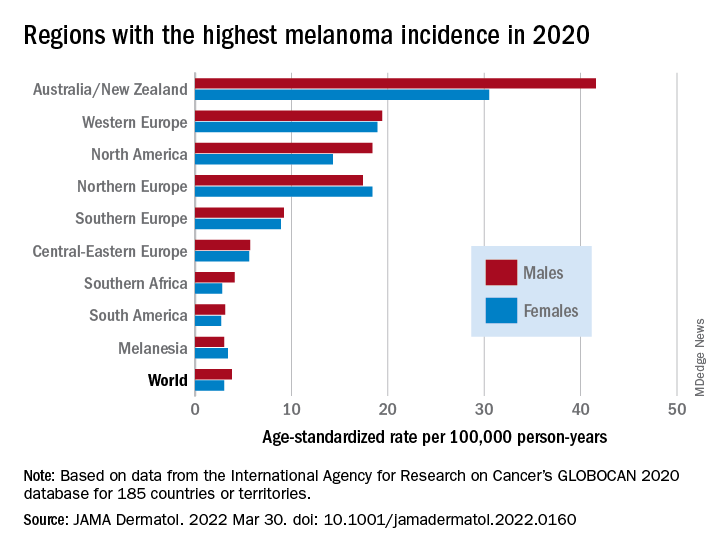
The highest incidence rates were seen in Australia and New Zealand, at 42 per 100,000 PY among males and 31 per 100,000 PY in females, followed by Western Europe with 19 per 100,000 PY in both males and females, North America with 18 and 14 cases per 100,000 PY in males and females respectively, and Northern Europe, with 17 per 100,000 PY in males, and 18 per 100,000 PY in females.
In contrast, in most African and Asian countries melanoma was rare, with rates commonly less than 1 per 100,000 PY, the investigators noted.
The melanoma mortality rate was highest in New Zealand, at 5 per 100,000 PY. Mortality rates worldwide varied less widely than incidence rates. In most other regions of the world, mortality rates were “much lower,” ranging between 0.2-1.0 per 100,000 PY, they wrote.
The authors estimated that, if 2020 rates remain stable, the global burden from melanoma in 2040 will increase to approximately 510,000 new cases and 96,000 deaths.
Public health efforts needed
In their editorial, Ms. Obeng-Kusi and Dr. Abraham pointed out that the study was hampered by the limited availability of cancer data from LMICs, leading the authors to estimate incidence and mortality rates based on proxy data, such as statistical modeling or averaged rates from neighboring countries.
They emphasized the need for going beyond the statistics: “Specific to cutaneous melanoma data, what is most important globally, knowing the exact numbers of cases and deaths or understanding the order of magnitude of the present and future epidemiology? No doubt the latter. Melanoma can be treated more easily if caught at earlier stages.”
Projections such as those provided by Dr. Arnold and colleagues could help to raise awareness of the importance of decreasing exposure to UV radiation, which accounts for three-fourths of all incident melanomas, the editorialists said.
The study was funded in part by a grant to coauthor Anna E. Cust, PhD, MPH. Dr. Cust reported receiving a fellowship from the Australian National Health and Medical Research Council outside the submitted work. Dr. Arnold had no conflicts of interested to disclose. Dr. Abraham reported financial relationships with various entities. Ms. Obeng-Kusi had no disclosures.
FROM JAMA DERMATOLOGY
Adverse skin effects of cancer immunotherapy reviewed
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Gene therapy for hemophilia A: `Truly transformative and liberating’
Significant results were seen 1 year after receiving a single intravenous infusion of valoctocogene roxaparvovec (AAV5-hFVIII-SQ), investigators from the international GENEr8-1 trial reported in the New England Journal of Medicine.
‘Truly transformative and liberating’
“If approved, this first-generation gene therapy would offer a new choice for care that could be truly transformative and liberating for eligible men with hemophilia,” writes Courtney D. Thornburg, from the Hemophilia and Thrombosis Treatment Center at Rady Children’s Hospital, San Diego, in an accompanying editorial.
Hemophilia A is an X-linked bleeding disorder caused by mutations in the gene encoding for coagulation factor VIII. Although rare, it is nevertheless the most common type, affecting about 12 per 100,000. Hemophilia B affects about 3.7 per 100,000.
The current treatment for hemophilia A is prophylactic infusions of factor VIII, often given three times per week.
With the gene therapy, such a patient could avoid at least 150 intravenous infusions of prophylactic factor in the span of a year, and have zero bleeds, Dr. Thornburg noted.
Valoctocogene roxaparvovec is an adeno-associated virus 5-based gene therapy vector that expresses a human factor VIII coding sequence, and is designed to correct the central genetic defect in hemophilia A.
Results from the phase 3 open-label trial show that it was associated with improved endogenous clotting factor production, and also a significant decrease in bleeding.
At 49-52 weeks of follow-up, 132 patients in a modified intention-to-treat analysis had a mean increase in factor VIII activity levels of 41.9 IU/dL (P < .001).
In a subgroup of 112 patients, the mean annualized factor concentrate use at 4 weeks decreased by 98.6%, and annualized rates of treated bleeding declined by 83.8% (P < .001 for both comparisons).
“Valoctocogene roxaparvovec gene transfer for severe hemophilia A provided significant increases in factor VIII activity, with reduced bleeding and factor VIII use for most participants over a period of up to 2 years,” conclude the investigators, led by Margareth C. Ozelo, MD, PhD, from the University of Campinas (Brazil).
“We are very enthusiastic about the results of this phase 3 clinical trial,” Dr. Ozelo commented to this news organization.
“It is important to recognize the clinical benefit achieved so far with treatment. During the first year, 90% of study participants had either zero treated bleeds or fewer treated bleeds post infusion than with factor VIII prophylaxis,” she said. “In addition, most of the study participants, including those from the phase 1/2 clinical trial, in the 5-year follow-up remain free of the use of additional prophylactic treatments.”
One issue that remains unanswered is how long the effects may last.
Valoctocogene roxaparvovec is a one-time infusion, she explained. “At least for now, redosing with the same AAV vector is not an option due to the immune response induced.”
“The durability of therapeutic response is one of the critical issues involving this new treatment for hemophilia. Currently, we cannot predict how long the transgene expression will last,” she added.
In the study, Dr. Ozelo and colleagues noted that “expression of the transferred gene appears to decline over time; further study is needed to address whether repeat treatment will be necessary or possible.”
Editorialist Dr. Thornburg touched on this point in an interview with this news organization.
Complete elimination of factor VIII replacement therapy is an ambitious goal, but gene therapy could obviate the need for prophylaxis in a substantial proportion of patients, she said. “Any increase of about 3%-5% in endogenous factor VIII production would eliminate the need for regular preventive treatments, either with regular factor or nonfactor replacements.
“How long that will be sustained is an open question,” she added. “With hemophilia B [factor IX deficiency] we have longer-term data showing quite good sustainability of the treatment, but I think it’s still an open question for hemophilia A.”
Dr. Thornburg also noted that further studies are needed to find similar therapies to benefit women and children with hemophilia, as well as for patients with factor VIII inhibitors, those with immunity to adenoviral vectors, and patients with hemophilia and concomitant liver disease or HIV infection.
GENEr8-1 study details and results
The trial was conducted in men 18 and older with severe congenital hemophilia A who had received prophylaxis with factor VIII concentrates for at least 1 year and were negative for factor VIII inhibitors.
The patient sample included 20 men enrolled directly, and 110 participants in a prospective noninterventional study of bleeding episodes, factor VIII infusions, and patient-reported outcomes in individuals with severe hemophilia A.
Participants received one infusion of valoctocogene roxaparvovec, at a dose of 6x1013 vector genomes per kilogram of body weight.
They remained on factor VIII prophylaxis for 4 weeks after the infusion of the gene therapy product, but after that factor VIII was used on an as-needed basis.
A total of 134 patients received an infusion and were included in the safety analysis. Two patients who were HIV positive were excluded from the modified intention-to-treat efficacy analysis.
As noted above, the trial met its primary efficacy endpoint of change from baseline in factor VIII activity 49-52 weeks after infusion, and the secondary endpoints of change from baseline to after week 4 in annualized use of factor VIII concentrate and the annualized number of treated bleeding episodes.
The most common adverse event was an elevation in alanine aminotransferase levels, the investigators noted.
These elevations in ALT levels, which have also been seen with gene therapy for hemophilia B, occurred in 85.8% of patients and could be safely managed with immunosuppressants, the authors commented.
Other common adverse events were headache, nausea, and elevations in aspartate aminotransferase levels, each occurring in slightly more than one third of patients.
“Overall, the risk-benefit profile appears favorable,” the team commented.
The study was supported by BioMarin Pharmaceutical. Dr. Ozelo disclosed grant support from the company. Dr. Thornburg disclosed serving as a consultant to BioMarin and others.
A version of this article first appeared on Medscape.com.
Significant results were seen 1 year after receiving a single intravenous infusion of valoctocogene roxaparvovec (AAV5-hFVIII-SQ), investigators from the international GENEr8-1 trial reported in the New England Journal of Medicine.
‘Truly transformative and liberating’
“If approved, this first-generation gene therapy would offer a new choice for care that could be truly transformative and liberating for eligible men with hemophilia,” writes Courtney D. Thornburg, from the Hemophilia and Thrombosis Treatment Center at Rady Children’s Hospital, San Diego, in an accompanying editorial.
Hemophilia A is an X-linked bleeding disorder caused by mutations in the gene encoding for coagulation factor VIII. Although rare, it is nevertheless the most common type, affecting about 12 per 100,000. Hemophilia B affects about 3.7 per 100,000.
The current treatment for hemophilia A is prophylactic infusions of factor VIII, often given three times per week.
With the gene therapy, such a patient could avoid at least 150 intravenous infusions of prophylactic factor in the span of a year, and have zero bleeds, Dr. Thornburg noted.
Valoctocogene roxaparvovec is an adeno-associated virus 5-based gene therapy vector that expresses a human factor VIII coding sequence, and is designed to correct the central genetic defect in hemophilia A.
Results from the phase 3 open-label trial show that it was associated with improved endogenous clotting factor production, and also a significant decrease in bleeding.
At 49-52 weeks of follow-up, 132 patients in a modified intention-to-treat analysis had a mean increase in factor VIII activity levels of 41.9 IU/dL (P < .001).
In a subgroup of 112 patients, the mean annualized factor concentrate use at 4 weeks decreased by 98.6%, and annualized rates of treated bleeding declined by 83.8% (P < .001 for both comparisons).
“Valoctocogene roxaparvovec gene transfer for severe hemophilia A provided significant increases in factor VIII activity, with reduced bleeding and factor VIII use for most participants over a period of up to 2 years,” conclude the investigators, led by Margareth C. Ozelo, MD, PhD, from the University of Campinas (Brazil).
“We are very enthusiastic about the results of this phase 3 clinical trial,” Dr. Ozelo commented to this news organization.
“It is important to recognize the clinical benefit achieved so far with treatment. During the first year, 90% of study participants had either zero treated bleeds or fewer treated bleeds post infusion than with factor VIII prophylaxis,” she said. “In addition, most of the study participants, including those from the phase 1/2 clinical trial, in the 5-year follow-up remain free of the use of additional prophylactic treatments.”
One issue that remains unanswered is how long the effects may last.
Valoctocogene roxaparvovec is a one-time infusion, she explained. “At least for now, redosing with the same AAV vector is not an option due to the immune response induced.”
“The durability of therapeutic response is one of the critical issues involving this new treatment for hemophilia. Currently, we cannot predict how long the transgene expression will last,” she added.
In the study, Dr. Ozelo and colleagues noted that “expression of the transferred gene appears to decline over time; further study is needed to address whether repeat treatment will be necessary or possible.”
Editorialist Dr. Thornburg touched on this point in an interview with this news organization.
Complete elimination of factor VIII replacement therapy is an ambitious goal, but gene therapy could obviate the need for prophylaxis in a substantial proportion of patients, she said. “Any increase of about 3%-5% in endogenous factor VIII production would eliminate the need for regular preventive treatments, either with regular factor or nonfactor replacements.
“How long that will be sustained is an open question,” she added. “With hemophilia B [factor IX deficiency] we have longer-term data showing quite good sustainability of the treatment, but I think it’s still an open question for hemophilia A.”
Dr. Thornburg also noted that further studies are needed to find similar therapies to benefit women and children with hemophilia, as well as for patients with factor VIII inhibitors, those with immunity to adenoviral vectors, and patients with hemophilia and concomitant liver disease or HIV infection.
GENEr8-1 study details and results
The trial was conducted in men 18 and older with severe congenital hemophilia A who had received prophylaxis with factor VIII concentrates for at least 1 year and were negative for factor VIII inhibitors.
The patient sample included 20 men enrolled directly, and 110 participants in a prospective noninterventional study of bleeding episodes, factor VIII infusions, and patient-reported outcomes in individuals with severe hemophilia A.
Participants received one infusion of valoctocogene roxaparvovec, at a dose of 6x1013 vector genomes per kilogram of body weight.
They remained on factor VIII prophylaxis for 4 weeks after the infusion of the gene therapy product, but after that factor VIII was used on an as-needed basis.
A total of 134 patients received an infusion and were included in the safety analysis. Two patients who were HIV positive were excluded from the modified intention-to-treat efficacy analysis.
As noted above, the trial met its primary efficacy endpoint of change from baseline in factor VIII activity 49-52 weeks after infusion, and the secondary endpoints of change from baseline to after week 4 in annualized use of factor VIII concentrate and the annualized number of treated bleeding episodes.
The most common adverse event was an elevation in alanine aminotransferase levels, the investigators noted.
These elevations in ALT levels, which have also been seen with gene therapy for hemophilia B, occurred in 85.8% of patients and could be safely managed with immunosuppressants, the authors commented.
Other common adverse events were headache, nausea, and elevations in aspartate aminotransferase levels, each occurring in slightly more than one third of patients.
“Overall, the risk-benefit profile appears favorable,” the team commented.
The study was supported by BioMarin Pharmaceutical. Dr. Ozelo disclosed grant support from the company. Dr. Thornburg disclosed serving as a consultant to BioMarin and others.
A version of this article first appeared on Medscape.com.
Significant results were seen 1 year after receiving a single intravenous infusion of valoctocogene roxaparvovec (AAV5-hFVIII-SQ), investigators from the international GENEr8-1 trial reported in the New England Journal of Medicine.
‘Truly transformative and liberating’
“If approved, this first-generation gene therapy would offer a new choice for care that could be truly transformative and liberating for eligible men with hemophilia,” writes Courtney D. Thornburg, from the Hemophilia and Thrombosis Treatment Center at Rady Children’s Hospital, San Diego, in an accompanying editorial.
Hemophilia A is an X-linked bleeding disorder caused by mutations in the gene encoding for coagulation factor VIII. Although rare, it is nevertheless the most common type, affecting about 12 per 100,000. Hemophilia B affects about 3.7 per 100,000.
The current treatment for hemophilia A is prophylactic infusions of factor VIII, often given three times per week.
With the gene therapy, such a patient could avoid at least 150 intravenous infusions of prophylactic factor in the span of a year, and have zero bleeds, Dr. Thornburg noted.
Valoctocogene roxaparvovec is an adeno-associated virus 5-based gene therapy vector that expresses a human factor VIII coding sequence, and is designed to correct the central genetic defect in hemophilia A.
Results from the phase 3 open-label trial show that it was associated with improved endogenous clotting factor production, and also a significant decrease in bleeding.
At 49-52 weeks of follow-up, 132 patients in a modified intention-to-treat analysis had a mean increase in factor VIII activity levels of 41.9 IU/dL (P < .001).
In a subgroup of 112 patients, the mean annualized factor concentrate use at 4 weeks decreased by 98.6%, and annualized rates of treated bleeding declined by 83.8% (P < .001 for both comparisons).
“Valoctocogene roxaparvovec gene transfer for severe hemophilia A provided significant increases in factor VIII activity, with reduced bleeding and factor VIII use for most participants over a period of up to 2 years,” conclude the investigators, led by Margareth C. Ozelo, MD, PhD, from the University of Campinas (Brazil).
“We are very enthusiastic about the results of this phase 3 clinical trial,” Dr. Ozelo commented to this news organization.
“It is important to recognize the clinical benefit achieved so far with treatment. During the first year, 90% of study participants had either zero treated bleeds or fewer treated bleeds post infusion than with factor VIII prophylaxis,” she said. “In addition, most of the study participants, including those from the phase 1/2 clinical trial, in the 5-year follow-up remain free of the use of additional prophylactic treatments.”
One issue that remains unanswered is how long the effects may last.
Valoctocogene roxaparvovec is a one-time infusion, she explained. “At least for now, redosing with the same AAV vector is not an option due to the immune response induced.”
“The durability of therapeutic response is one of the critical issues involving this new treatment for hemophilia. Currently, we cannot predict how long the transgene expression will last,” she added.
In the study, Dr. Ozelo and colleagues noted that “expression of the transferred gene appears to decline over time; further study is needed to address whether repeat treatment will be necessary or possible.”
Editorialist Dr. Thornburg touched on this point in an interview with this news organization.
Complete elimination of factor VIII replacement therapy is an ambitious goal, but gene therapy could obviate the need for prophylaxis in a substantial proportion of patients, she said. “Any increase of about 3%-5% in endogenous factor VIII production would eliminate the need for regular preventive treatments, either with regular factor or nonfactor replacements.
“How long that will be sustained is an open question,” she added. “With hemophilia B [factor IX deficiency] we have longer-term data showing quite good sustainability of the treatment, but I think it’s still an open question for hemophilia A.”
Dr. Thornburg also noted that further studies are needed to find similar therapies to benefit women and children with hemophilia, as well as for patients with factor VIII inhibitors, those with immunity to adenoviral vectors, and patients with hemophilia and concomitant liver disease or HIV infection.
GENEr8-1 study details and results
The trial was conducted in men 18 and older with severe congenital hemophilia A who had received prophylaxis with factor VIII concentrates for at least 1 year and were negative for factor VIII inhibitors.
The patient sample included 20 men enrolled directly, and 110 participants in a prospective noninterventional study of bleeding episodes, factor VIII infusions, and patient-reported outcomes in individuals with severe hemophilia A.
Participants received one infusion of valoctocogene roxaparvovec, at a dose of 6x1013 vector genomes per kilogram of body weight.
They remained on factor VIII prophylaxis for 4 weeks after the infusion of the gene therapy product, but after that factor VIII was used on an as-needed basis.
A total of 134 patients received an infusion and were included in the safety analysis. Two patients who were HIV positive were excluded from the modified intention-to-treat efficacy analysis.
As noted above, the trial met its primary efficacy endpoint of change from baseline in factor VIII activity 49-52 weeks after infusion, and the secondary endpoints of change from baseline to after week 4 in annualized use of factor VIII concentrate and the annualized number of treated bleeding episodes.
The most common adverse event was an elevation in alanine aminotransferase levels, the investigators noted.
These elevations in ALT levels, which have also been seen with gene therapy for hemophilia B, occurred in 85.8% of patients and could be safely managed with immunosuppressants, the authors commented.
Other common adverse events were headache, nausea, and elevations in aspartate aminotransferase levels, each occurring in slightly more than one third of patients.
“Overall, the risk-benefit profile appears favorable,” the team commented.
The study was supported by BioMarin Pharmaceutical. Dr. Ozelo disclosed grant support from the company. Dr. Thornburg disclosed serving as a consultant to BioMarin and others.
A version of this article first appeared on Medscape.com.
FROM NEW ENGLAND JOURNAL OF MEDICINE