User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
People with HIV still at increased cardiovascular risk
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
CHICAGO – HIV infection remained linked with an increased risk for developing a cardiovascular disease event among U.S. patients, even in a recent era of antiretroviral therapy.
U.S. health insurance beneficiaries diagnosed with an HIV infection and likely put on antiretroviral therapy sometime during 2011-2015 had a statistically significant, 21% increased risk for the combination of MIs, coronary revascularizations, stroke, and lower-extremity peripheral artery disease (PAD) in a case-control, retrospective analysis, Robert S. Rosenson, MD, said in a poster he presented at the American Heart Association scientific sessions.
“We looked at a contemporary population of people with HIV treated with antiretroviral therapy, and we looked at stroke and lower-extremity PAD [peripheral artery disease] as well as MI, while most prior studies only looked at MIs,” noted Dr. Rosenson, a professor of medicine and director of cardiometabolic disorders at the Icahn School of Medicine at Mount Sinai Medical Center in New York.
The analysis found no significant differences in outcomes that linked with the specific type of antiretroviral therapy patients received. The most commonly used antiretroviral drug was a non–nucleoside reverse transcriptase inhibitor, taken by about 80% of the HIV-infected patients, Dr. Rosenson said. The 2011-2015 period examined in the study largely predated the more recent era, when integrase strand transfer inhibitor drugs have increasingly become the core agent for treating HIV infection.
Another key finding in the study was that a scant 19% of the people infected with HIV received statin treatment, and only 4% were on a high-intensity dosage. The 2018 guideline on cholesterol management identifies HIV infection as one of several “risk enhancers” that boost a person’s cardiovascular disease (CVD) risk and intensify their need for statin treatment (Circulation. 2018 Nov 10. doi: 10.1161/CIR.0000000000000625).
“Hopefully use of statins will increase in people with HIV, but of course we need evidence because so far the evidence does not show benefit,” he noted. In the data Dr. Rosenson reported, the HIV-infected patients who received a statin had roughly the same elevated risk for a CVD event as did HIV-infected patients who did not get a statin.
His study used data from a U.S. commercial database that combined Medicare patients with patients covered by commercial insurers. The analysis identified 82,426 people presumed recently infected by HIV based on either a hospitalization discharge with a diagnostic code for HIV or after filling at least two prescriptions for an antiretroviral drug during January 2011–June 2015. The researchers matched these cases on a 4:1 basis with 329,704 controls from the database matched by age, sex, and year for their index date. The total study cohort averaged about 45 years old, but the people infected by HIV averaged a couple of years older and also had at baseline an increased prevalence of several CVD risk factors and comorbidities. The people with HIV had a more than threefold higher rate of tobacco use, chronic kidney disease, and liver disease, and double the rate of diagnosed depression.
In a multivariate analysis that controlled for many demographic, social, and clinical variables, the results showed that the HIV-infected people had statistically significant higher rates of every individual element in the CVD composite. They had a 26% higher rate of MIs, a 17% higher rate of MIs plus coronary revascularization, a 30% higher rate of stroke, and a doubled rate of lower-extremity PAD.
SOURCE: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: U.S. insurance beneficiaries newly diagnosed with HIV had a significantly higher rate of CVD events than people without HIV.
Major finding: The adjusted rate of cardiovascular disease events was 21% higher in people infected with HIV, compared with matched, uninfected people.
Study details: A retrospective, case control study of 412,130 U.S. health insurance beneficiaries.
Disclosures: The study received partial funding from Amgen. Dr. Rosenson has received honoraria from Amgen, Akcaa, and Kowa; he has been an advisor to Amgen, Regeneron, and Sanofi; and he has received research funding from Amgen, Akcaa, AstraZeneca, and The Medicines Company.
Source: Rosenson RS et al. Circulation. 2018 Nov 6;138[suppl 1]:A14410.
Methotrexate fails to cut CVD events in a large RCT
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CIRT is an important study. Considering the results from CIRT, which used methotrexate, along with the results from CANTOS, which used canakinumab, provides helpful mechanistic observations about selective drug effects when targeting inflammation. Two additional trials that are now in progress using colchicine in a clinical setting similar to CIRT and CANTOS should give us even more insight into the relationships between inflammation and atherosclerotic cardiovascular disease and possible new approaches to treatment.
Despite these differences between the two trials, the results from CIRT clearly showed that, in the enrolled patients, the dosage of methotrexate used had no apparent impact on levels of hsCRP, IL-1B, and IL-6.
Sidney C. Smith Jr., MD, is a cardiologist and professor of medicine at the University of North Carolina at Chapel Hill. He made these comments as the designated discussant for the CIRT trial. He had no disclosures.
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
CHICAGO – Both methotrexate and canakinumab are anti-inflammatory drugs, but only canakinumab cut the incidence of cardiovascular disease events in a major clinical trial, CANTOS. A second big trial designed to parallel CANTOS tested methotrexate in roughly the same way and found it produced no cardiovascular disease benefit among high-risk patients.
The CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study) results with canakinumab and the new results with methotrexate “demonstrate that inflammation inhibition [with canakinumab] can significantly reduce cardiovascular event rates independent of lipid lowering and blood pressure reduction,” Paul M. Ridker, MD, said at the American Heart Association scientific sessions. But, “inhibition of the IL [interleukin]–1 beta to IL-6 to CRP [C-reactive protein] pathway of innate immunity appears to be important for atheroprotection,” and was something methotrexate couldn’t deliver, concluded Dr. Ridker, a professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston.
The new results he reported showed that weekly treatment with a single, oral, 15- to 20-mg dose of methotrexate not only had no effect on cardiovascular events but also had no discernible impact on serum levels of IL-1beta (IL-1B), IL-6, or high sensitivity (hs) CRP, in contrast to canakinumab, which Dr. Ridker took as evidence that this inflammatory pathway links to the pathophysiology of atherosclerotic cardiovascular disease.
CIRT (Cardiovascular Inflammation Reduction Trial) randomized 4,786 patients at 417 centers in the United States or Canada. Enrolled patients had to have a history of an MI or documented multivessel coronary disease, and also had to have type 2 diabetes, metabolic syndrome, or both. All patients were maintained on optimized dosages of a statin, aspirin, a beta-blocker, and an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. All patients also received 1 mg folate daily. Randomization assigned patients to either receive 15-20 mg methotrexate orally once a week or placebo.
CIRT stopped prematurely because of futility after a median follow-up of 2.3 years. At that time, the incidence of one of two primary endpoints, the combination of cardiovascular death, nonfatal MI, and nonfatal stroke was 3.46/100 person-years with methotrexate treatment and 3.43/100 person-years with placebo, a difference that was not statistically significant. The incidence of the second primary endpoint, which combined the first three types of events plus hospitalization for unstable angina that led to urgent coronary revascularization, occurred in 4.13/100 person-years with methotrexate and 4.31/100 person years with placebo, also a difference that was not statistically significant. Concurrently with this report, the results were published online (N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1809798).
Analysis of inflammatory markers in the blood after 8 months on treatment showed that methotrexate had no effect on levels of IL-1B, IL-6, and hsCRP. Methotrexate’s lack of an effect on these markers as well as the absence of an effect on cardiovascular disease events contrasted sharply with results that Dr. Ridker and his associates reported a little more than a year earlier in CANTOS. The study’s investigators randomized 10,061 patients with a history of an MI and an elevated serum level of hsCRP, at least 2.0 mg/L. After a median follow-up of 3.7 years, treatment with 150 mg of canakinumab injected subcutaneously once every 3 months produced a 15% relative risk reduction in the combined rate of cardiovascular death, nonfatal MI, and nonfatal stroke, compared with patients treated with placebo, a statistically significant between-group difference (N Engl J Med. 2017 Sep 21;377[12]:1119-31). Canakinumab had no impact on LDL cholesterol levels, but lowered hsCRP levels by more than a third. Dr. Ridker and his associates designed the CIRT and CANTOS trials “in parallel,” he said, and the CIRT results using methotrexate provided a “neutral control” to complement the positive results from canakinumab in CANTOS,
Given its high cost, canakinumab (Ilaris) is not an obviously practical option for treating patients similar to those enrolled in CANTOS, so other candidate agents that inhibit the IL-1B, IL-6, CRP inflammatory pathway are now under study, Dr. Ridker said in an interview. The mechanism of methotrexate’s inhibition of inflammation is unknown, but clearly does not involve this pathway; it may be mediated by adenosine, Dr. Ridker suggested. Canakinumab has Food and Drug Administration approval for treating systemic juvenile idiopathic arthritis and a handful of additional, low-prevalence diseases. Novartis, the company that markets canakinumab, made a submission to the Food and Drug Administration seeking an indication for prevention of cardiovascular disease based on the CANTOS results, and the company said in October 2018 that the FDA denied this request.
The CIRT results also showed a previously unseen signal of a possible safety issue with the tested methotrexate regimen. The incidence of non–basal cell skin cancer was 0.65/100 person-years with methotrexate, compared with 0.24/100 person-years with placebo, a statistically significant difference. Until now, no one had reported a link like this and it requires further analysis, Dr. Ridker said.
CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Siemens and AstraZeneca.
SOURCE: Ridker P et al. AHA scientific sessions, Abstract 17778.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The combined rate of CVD events was 3.46/100 person-years on methotrexate and 3.43/100 on placebo.
Study details: CIRT, a multicenter, randomized trial with 4,786 high-risk patients.
Disclosures: CIRT received no commercial funding. Dr. Ridker has been a consultant to Corvidia, Inflazome, and Novartis; he has received research funding from Kowa and Novartis; and his work led to a patent held by Brigham and Women’s Hospital for inflammatory biomarkers licensed to Seimens and AstraZeneca.
Source: Ridker P et al. AHA scientific sessions, Abstract 17778.
Filgotinib shows efficacy, safety in RA phase 3 and PsA phase 2 trials
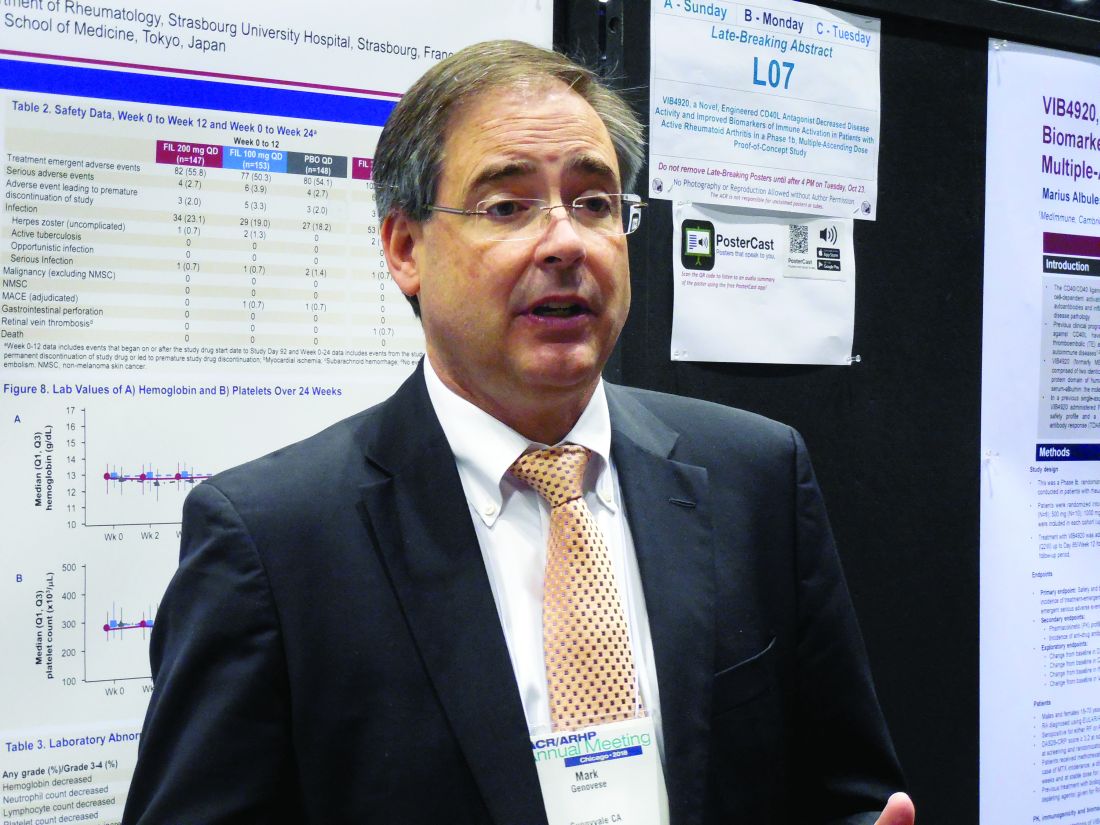
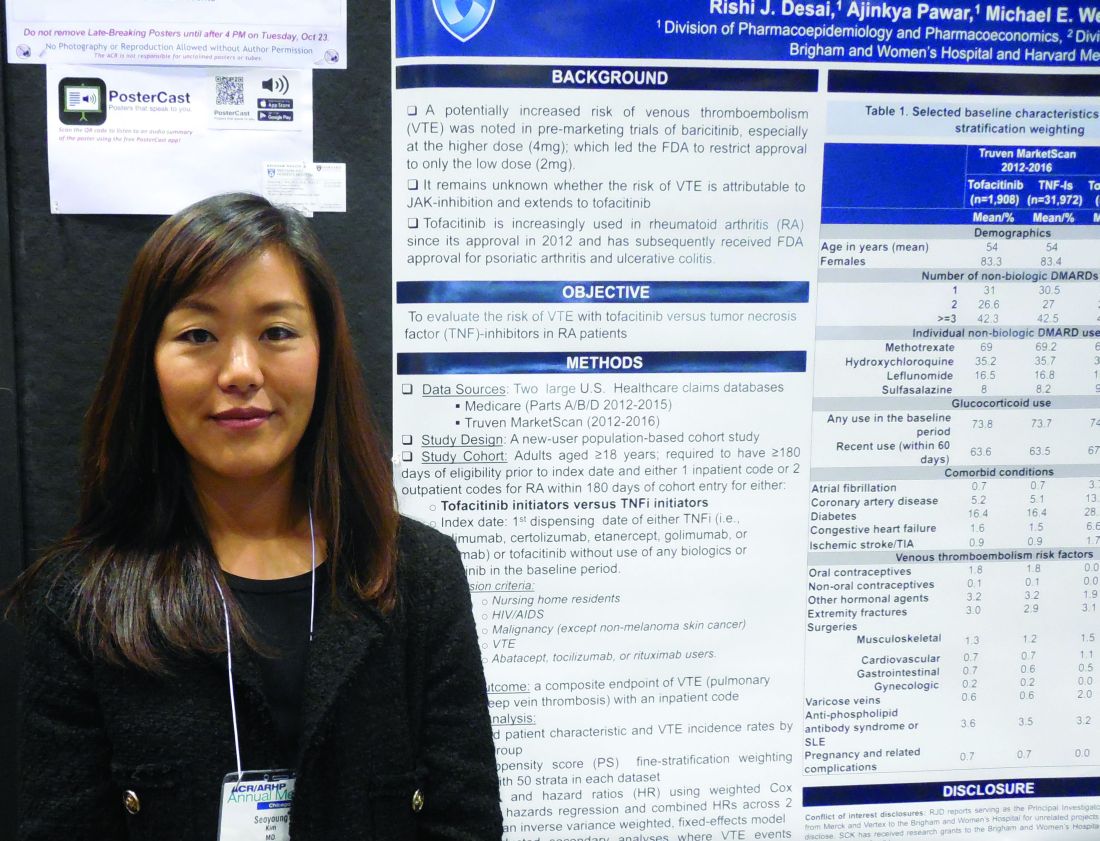
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
CHICAGO – The selective Janus kinase 1 inhibitor filgotinib showed efficacy and safety for patients with rheumatoid arthritis in a phase 3 trial, and efficacy and safety for treating patients with psoriatic arthritis in results from a phase 2 study in two separate reports at the annual meeting of the American College of Rheumatology.
In the phase 3 study, treatment with filgotinib at an oral dosage of 200 mg once daily led to a 66% incidence of American College of Rheumatology 20 (ACR20) responses after 16 weeks of treatment in 147 patients with moderately to severely active rheumatoid arthritis (RA), compared with a 31% rate among 148 patients randomized to receive placebo, a statistically significant improvement for the study’s primary efficacy endpoint, Mark C. Genovese, MD, reported in a poster at the meeting. The rate of ACR20 responses among the 153 RA patients who received 100 mg/day filgotinib was 58%, reported Dr. Genovese, professor of medicine and director of the rheumatology clinic at Stanford (Calif.) University.
After 24 weeks of daily treatment, the longest duration studied in the trial, ACR20 rates were 69%, 55%, and 35% in the 200-mg, 100-mg, and placebo patients, respectively. Dr. Genovese also reported that after 24 weeks on treatment, the rates of patients achieving low disease activity measured by their disease activity score based on 28 joints and C-reactive protein level (DAS28-CRP) were 48%, 38%, and 21%, respectively, and the percentages of patients achieving complete remission at 24 weeks based on their DAS28-CRP scores were 31%, 26%, and 12%, respectively.
“We were incredibly fortunate to see such positive results. The drug worked very well in very-challenging-to-treat patients,” Dr. Genovese said in an interview. All of the RA patients enrolled in the study had not previously responded to or were intolerant of prior treatment with at least one biologic disease-modifying antirheumatic drug (DMARD), and almost a quarter of enrolled patients had failed prior treatment with at least three different biologic DMARDs. The number of biologic DMARDs a patient had previously received showed no relationship to how well patients responded to filgotinib, he noted.
Dr. Genovese also highlighted the relatively high percentage of patients who achieved low disease activity and remission. The 48% and 31% rates, respectively, of low disease activity and remission among patients treated with the higher filgotinib dosage for 24 weeks “is fairly impressive in patients who did not previously respond to a biologic DMARD,” the researcher said. These findings are similar to data previously reported for upadacitinib, another Janus kinase (JAK) inhibitor that, like filgotinib, is selective for the JAK1 receptor, noted Dr. Genovese, who also was the lead investigator for a phase 3 study of upadacitinib in RA patients (Lancet. 2018 June 23;391[10139]:2513-24).
The filgotinib data he presented came from the FINCH 2 (Filgotinib Versus Placebo in Adults With Active Rheumatoid Arthritis Who Have an Inadequate Response to Biologic Disease-Modifying Anti-Rheumatic Drug[s] Treatment) trial, which was run at 104 sites in 15 countries, including the United States. The results also showed a “favorable safety profile and stable laboratory parameters,” Dr. Genovese reported. Results from two additional phase 3 trials in RA patients are expected in 2019, he said.
Filgotinib studied in psoriatic arthritis
The separate, phase 2 study of filgotinib in patients with psoriatic arthritis (PsA) reported during the meeting showed safety “in line with previous reports without new safety signals” in a multicenter trial with 131 patients randomized to receive oral filgotinib 200 mg daily for 16 weeks or placebo, Philip J. Mease, MD, reported in a talk at the meeting. For the primary endpoint of achievement of ACR20 response after 16 weeks, the rate was 80% of the filgotinib-treated patients and 33% of patients in the placebo group, a statistically significant difference, said Dr. Mease, a rheumatologist at Swedish Medical Center in Seattle.
EQUATOR (A Study to Assess Efficacy and Safety of Filgotinib in Active Psoriatic Arthritis) enrolled patients at sites in seven European countries who had “very active” PsA and either a history of or current plaque psoriasis. All patients had to have a history of either insufficient response to or intolerance of at least one conventional synthetic DMARD. The enrollment criteria had no specifications for prior use of an anti–tumor necrosis factor drug, and about 15% of patients had used least one of these drugs. At entry, about three-quarters of patients were on treatment with a conventional synthetic DMARD and about a quarter received treatment with a glucocorticoid.
The results showed statistically significant benefits from filgotinib, compared with placebo, for several other measures of arthritis activity, as well as measures of psoriasis, enthesitis, and pain, Dr. Mease reported. He also highlighted a “lack of meaningful changes in hemoglobin” or other laboratory measures that, along with the efficacy findings, make filgotinib “a promising first step” for patients with PsA. Dr. Mease also noted that roughly concurrently with his report, a separate group of researchers published results from a phase 2 study of filgotinib in patients with ankylosing spondylitis that also found evidence for efficacy and safety during 12 weeks of treating 116 randomized patients (Lancet. 2018 Oct 22. doi: 10.1016/S0140-6736[18]32463-2).
FINCH 2 was sponsored by Galapagos and Gilead, the two companies developing filgotinib. Dr. Genovese has had financial relationships with Galapagos and Gilead and also with AbbVie, Lilly, and Pfizer. Dr. Mease has had financial relationships with Galapagos and Gilead and a dozen other companies.
SOURCES: Genovese M et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract L06; Mease P et al. Arthritis Rheumatol. 2018;70(Suppl 10), Abstract 1821.
REPORTING FROM THE ACR ANNUAL MEETING
New VTE guidelines include over 150 recommendations
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The American Society of Hematology (ASH) has released a new set of guidelines for the prevention, diagnosis, and management of venous thromboembolism (VTE).
The new guidelines contain more than 150 individual recommendations, including sections devoted to managing VTE during pregnancy and in pediatric patients.
Guideline highlights cited by some of the writing panel include a high reliance on low-molecular-weight heparin (LMWH) as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, of the University of Pennsylvania in Philadelphia and co-chair of the guideline-writing group, said during a webcast to unveil the new guidelines.
The guidelines, released on November 27, took more than 3 years to develop, an effort that began in 2015.
Prevention
For preventing VTE in hospitalized medical patients, the guidelines recommend initial assessment of the patient’s risk for both VTE and bleeding.
Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves.
But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, of the University of Vermont in Burlington and member of the guideline writing group.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, Dr. Cushman said.
The panel also endorsed LMWH over a direct-acting oral anticoagulant (DOAC), both during hospitalization and following discharge.
The guidelines for prevention in medical patients explicitly “recommended against” using a DOAC “over other treatments” both for hospitalized medical patients and after discharge. The guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important take-away from the prevention section is a statement that combining both mechanical and medical prophylaxis is not needed for medical inpatients.
And once patients are discharged, they have no need for compression stockings or aspirin on a long plane trip if their risk for thrombosis is not elevated.
People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, of McMaster University in Hamilton, Ontario, Canada, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and that helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommend the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, Dr. Lim noted.
The guidelines also recommend using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy.
But it’s a level of care that many U.S. patients don’t currently receive and, hence, is an area ripe for growth, said Daniel M. Witt, PharmD, of the University of Utah in Salt Lake City.
The guidelines recommend against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure.
The guidelines also call for “thoughtful” use of anticoagulant reversal agents, and they advise that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, according to Dr. Cuker, lead author of a paper on the subject published in Blood.
The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated each year with heparin, argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis for medical patients, diagnosis, anticoagulation therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children.
The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published the following six articles in the journal Blood Advances that detail the guidelines and their documentation relating to VTE and:
Drs. Cushman, Lim, and Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
ARISTOPHANES: Apixaban edges other DOACS for octogenarians
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
The findings come from an analysis of insurance claims data from more than 50,000 U.S. patients – the largest observational study to date to compare these three direct-acting oral anticoagulants (DOACs) in octogenarians with nonvalvular atrial fibrillation, Steven B. Deitelzweig, MD, said at the American Heart Association scientific sessions.
“The results may help clinicians evaluate the risk-benefit ratio of the DOACs” in this population, said Dr. Deitelzweig, vice president for medical affairs at Ochsner Medical Center in New Orleans.
He noted that the results were consistent with prior reports from observational data and registries, as well as the results in a recent analysis commissioned by the Agency for Healthcare Research and Quality. “We see a consistent message that apixaban always has less risk for major bleeding, and at least comparable efficacy” when compared with other DOACs, he said in a video interview.
And for the foreseeable future, this sort of data will need to suffice for clinicians trying to decide which DOAC to use because “I know of no head-to-head trials, nor do I anticipate any head-to-head trials” that could provide a more definitive comparison of the DOACs, Dr. Deitelzweig said.
The data came from a large number of patients – about 38% of the U.S. population – which boosts the generalizability of the finding. “I think our data are useful” for helping to make treatment decisions, he concluded.
The analysis he reported came from the ARISTOPHANES (Anticoagulants for Reduction in Stroke: Observational Pooled Analysis on Health Outcomes and Experience of Patients) study, which pooled U.S. insurance claims data from several sources. For the octogenarian study, Dr. Deitelzweig and his associates used data from about 123 million U.S. residents collected between January 2012 and September 2015 by Medicare and three different commercial insurance databases. The overall level of beneficiary overlap between these four data sources was less than 0.5%.
The researchers identified patients with nonvalvular atrial fibrillation who started anticoagulant treatment with a DOAC and were at least 80 years old. This included 19,752 patients started on apixaban (Eliquis), 6,741 started on dabigatran (Pradaxa), and 27,217 started on rivaroxaban (Xarelto). A majority of the patients were at least 84 years old.
The analysis used propensity-score matching to compare similar patients and to minimize the impact of potentially confounding differences among the patients in each treatment subgroup. During a median follow-up of 7-9 months, the incidence of stroke or systemic embolism was 35% lower in the apixaban-treated patients, compared with those who received dabigatran, and 28% lower in the apixaban patients, compared with those treated with rivaroxaban, both statistically significant differences, Dr. Deitelzweig reported. The incidence of major bleeding episodes was 40% lower with apixaban than with dabigatran and 50% lower with apixaban, compared with rivaroxaban, also statistically significant differences.
When the analysis compared dabigatran with rivaroxaban it showed no statistically significant difference for the efficacy endpoint, but dabigatran produced 23% fewer major bleeds than rivaroxaban, a statistically significant difference.
These findings jibed with a recently published analysis from Dr. Deitelzweig and his associates that used data from all adults with nonvalvular atrial fibrillation started on an oral anticoagulant in an expanded ARISTOPHANES database for 2012-2015 that included more than 180 million U.S. beneficiaries. After propensity-score matching, this created subgroups of about 58,000 patients started on apixaban, nearly 27,000 started on dabigatran, and more than 83,000 started on rivaroxaban. The patients averaged about 73 years old. Again, with about 7-9 months of follow-up, very similar outcomes occurred. Patients on apixaban had significantly fewer strokes and systemic embolic events as well as significantly fewer major bleeds compared with patients treated with one of the other DOACs (Stroke. 2018 Dec;49[12]:2933-44).
The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
SOURCE: Deitelzweig SB et al. Circulation. 2018 Nov 6;138(suppl 1):A14900.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Apixaban surpassed two other direct-acting oral anticoagulants in a large, observational database.
Major finding: The adjusted stroke or systemic embolism rate with apixaban was 35% less than dabigatran and 28% less than rivaroxaban.
Study details: A retrospective analysis of observational data collected in insurance claims from 53,710 U.S. octogenarians.
Disclosures: The study was funded by Bristol-Myers Squibb and Pfizer, the companies that market apixaban (Eliquis). Dr. Deitelzweig is a consultant to and speaker on behalf of Bristol-Myers Squibb and Pfizer. He is also a consultant to or speaker on behalf of Boehringer Ingelheim, Daiichi-Sankyo, Janssen, and Portola Pharmaceuticals.
Source: Deitelzweig SB et al. Circulation. 2018 Nov 6;138[suppl 1]:A14900.
ASH releases new VTE guidelines
The new guidelines, released on Nov. 27, contain more than 150 individual recommendations, including sections devoted to managing venous thromboembolism (VTE) during pregnancy and in pediatric patients. Guideline highlights cited by some of the writing-panel participants included a high reliance on low-molecular-weight heparin (LMWH) agents as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
The guidelines took more than 3 years to develop, an effort that began in 2015.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, cochair of the guideline-writing group and a hematologist and thrombosis specialist at the University of Pennsylvania, Philadelphia, said during a webcast to unveil the new guidelines.
Prevention
For preventing VTE in hospitalized medical patients the guidelines recommended initial assessment of the patient’s risk for both VTE and bleeding. Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves. But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, professor and medical director of the thrombosis and hemostasis program at the University of Vermont, Burlington.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, said Dr. Cushman, a member of the writing group. The panel also endorsed LMWH over a direct-acting oral anticoagulant, both during hospitalization and following discharge. The guidelines for prevention in medical patients explicitly “recommended against” using a direct-acting oral anticoagulant “over other treatments” both for hospitalized medical patients and after discharge, and the guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important takeaway from the prevention section was a statement that combining both mechanical and medical prophylaxis was not needed for medical inpatients. And once patients are discharged, if they take a long air trip they have no need for compression stockings or aspirin if their risk for thrombosis is not elevated. People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommended the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, noted Dr. Lim, a hematologist and professor at McMaster University, Hamilton, Ont.
The guidelines also recommended using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy. But it’s a level of care that many U.S. patients don’t currently receive and hence is an area ripe for growth, said Daniel M. Witt, PharmD, professor and vice-chair of pharmacotherapy at the University of Utah, Salt Lake City.
The guidelines recommended against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure. The guidelines also called for “thoughtful” use of anticoagulant reversal agents and advised that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, said Dr. Cuker (Blood. 2012 Nov 15;120[20]:4160-7). The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated with heparin annually: argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis in medical patients, diagnosis, therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children. The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said that these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published six articles in the journal Blood Advances that detailed the guidelines and their documentation.
The articles include prophylaxis of medical patients (Blood Advances. 2018 Nov 27;2[22]:3198-225), diagnosis (Blood Advances. 2018 Nov 27;2[22]:3226-56), anticoagulation therapy (Blood Advances. 2018 Nov 27;2[22]:3257-91), pediatrics (Blood Advances. 2018 Nov 27;2[22]:3292-316), pregnancy (Blood Advances. 2018 Nov 27;2[22]:3317-59), and heparin-induced thrombocytopenia (Blood Advances. 2018 Nov 27;2[22]:3360-92).
Dr. Cushman, Dr. Lim, and Dr. Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The new guidelines, released on Nov. 27, contain more than 150 individual recommendations, including sections devoted to managing venous thromboembolism (VTE) during pregnancy and in pediatric patients. Guideline highlights cited by some of the writing-panel participants included a high reliance on low-molecular-weight heparin (LMWH) agents as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
The guidelines took more than 3 years to develop, an effort that began in 2015.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, cochair of the guideline-writing group and a hematologist and thrombosis specialist at the University of Pennsylvania, Philadelphia, said during a webcast to unveil the new guidelines.
Prevention
For preventing VTE in hospitalized medical patients the guidelines recommended initial assessment of the patient’s risk for both VTE and bleeding. Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves. But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, professor and medical director of the thrombosis and hemostasis program at the University of Vermont, Burlington.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, said Dr. Cushman, a member of the writing group. The panel also endorsed LMWH over a direct-acting oral anticoagulant, both during hospitalization and following discharge. The guidelines for prevention in medical patients explicitly “recommended against” using a direct-acting oral anticoagulant “over other treatments” both for hospitalized medical patients and after discharge, and the guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important takeaway from the prevention section was a statement that combining both mechanical and medical prophylaxis was not needed for medical inpatients. And once patients are discharged, if they take a long air trip they have no need for compression stockings or aspirin if their risk for thrombosis is not elevated. People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommended the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, noted Dr. Lim, a hematologist and professor at McMaster University, Hamilton, Ont.
The guidelines also recommended using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy. But it’s a level of care that many U.S. patients don’t currently receive and hence is an area ripe for growth, said Daniel M. Witt, PharmD, professor and vice-chair of pharmacotherapy at the University of Utah, Salt Lake City.
The guidelines recommended against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure. The guidelines also called for “thoughtful” use of anticoagulant reversal agents and advised that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, said Dr. Cuker (Blood. 2012 Nov 15;120[20]:4160-7). The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated with heparin annually: argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis in medical patients, diagnosis, therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children. The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said that these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published six articles in the journal Blood Advances that detailed the guidelines and their documentation.
The articles include prophylaxis of medical patients (Blood Advances. 2018 Nov 27;2[22]:3198-225), diagnosis (Blood Advances. 2018 Nov 27;2[22]:3226-56), anticoagulation therapy (Blood Advances. 2018 Nov 27;2[22]:3257-91), pediatrics (Blood Advances. 2018 Nov 27;2[22]:3292-316), pregnancy (Blood Advances. 2018 Nov 27;2[22]:3317-59), and heparin-induced thrombocytopenia (Blood Advances. 2018 Nov 27;2[22]:3360-92).
Dr. Cushman, Dr. Lim, and Dr. Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
The new guidelines, released on Nov. 27, contain more than 150 individual recommendations, including sections devoted to managing venous thromboembolism (VTE) during pregnancy and in pediatric patients. Guideline highlights cited by some of the writing-panel participants included a high reliance on low-molecular-weight heparin (LMWH) agents as the preferred treatment for many patients, reliance on the D-dimer test to rule out VTE in patients with a low pretest probability of disease, and reliance on the 4Ts score to identify patients with heparin-induced thrombocytopenia.
The guidelines took more than 3 years to develop, an effort that began in 2015.
An updated set of VTE guidelines were needed because clinicians now have a “greater understanding of risk factors” for VTE as well as having “more options available for treating VTE, including new medications,” Adam C. Cuker, MD, cochair of the guideline-writing group and a hematologist and thrombosis specialist at the University of Pennsylvania, Philadelphia, said during a webcast to unveil the new guidelines.
Prevention
For preventing VTE in hospitalized medical patients the guidelines recommended initial assessment of the patient’s risk for both VTE and bleeding. Patients with a high bleeding risk who need VTE prevention should preferentially receive mechanical prophylaxis, either compression stockings or pneumatic sleeves. But in patients with a high VTE risk and an “acceptable” bleeding risk, prophylaxis with an anticoagulant is preferred over mechanical measures, said Mary Cushman, MD, professor and medical director of the thrombosis and hemostasis program at the University of Vermont, Burlington.
For prevention of VTE in medical inpatients, LMWH is preferred over unfractionated heparin because of its once-daily dosing and fewer complications, said Dr. Cushman, a member of the writing group. The panel also endorsed LMWH over a direct-acting oral anticoagulant, both during hospitalization and following discharge. The guidelines for prevention in medical patients explicitly “recommended against” using a direct-acting oral anticoagulant “over other treatments” both for hospitalized medical patients and after discharge, and the guidelines further recommend against extended prophylaxis after discharge with any other anticoagulant.
Another important takeaway from the prevention section was a statement that combining both mechanical and medical prophylaxis was not needed for medical inpatients. And once patients are discharged, if they take a long air trip they have no need for compression stockings or aspirin if their risk for thrombosis is not elevated. People with a “substantially increased” thrombosis risk “may benefit” from compression stockings or treatment with LMWH, Dr. Cushman said.
Diagnosis
For diagnosis, Wendy Lim, MD, highlighted the need for first categorizing patients as having a low or high probability for VTE, a judgment that can aid the accuracy of the diagnosis and helps avoid unnecessary testing.
For patients with low pretest probability, the guidelines recommended the D-dimer test as the best first step. Further testing isn’t needed when the D-dimer is negative, noted Dr. Lim, a hematologist and professor at McMaster University, Hamilton, Ont.
The guidelines also recommended using ventilation-perfusion scintigraphy (V/Q scan) for imaging a pulmonary embolism over a CT scan, which uses more radiation. But V/Q scans are not ideal for assessing older patients or patients with lung disease, Dr. Lim cautioned.
Management
Management of VTE should occur, when feasible, through a specialized anticoagulation management service center, which can provide care that is best suited to the complexities of anticoagulation therapy. But it’s a level of care that many U.S. patients don’t currently receive and hence is an area ripe for growth, said Daniel M. Witt, PharmD, professor and vice-chair of pharmacotherapy at the University of Utah, Salt Lake City.
The guidelines recommended against bridging therapy with LMWH for most patients who need to stop warfarin when undergoing an invasive procedure. The guidelines also called for “thoughtful” use of anticoagulant reversal agents and advised that patients who survive a major bleed while on anticoagulation should often resume the anticoagulant once they are stabilized.
For patients who develop heparin-induced thrombocytopenia, the 4Ts score is the best way to make a more accurate diagnosis and boost the prospects for recovery, said Dr. Cuker (Blood. 2012 Nov 15;120[20]:4160-7). The guidelines cite several agents now available to treat this common complication, which affects about 1% of the 12 million Americans treated with heparin annually: argatroban, bivalirudin, danaparoid, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban.
ASH has a VTE website with links to detailed information for each of the guideline subcategories: prophylaxis in medical patients, diagnosis, therapy, heparin-induced thrombocytopenia, VTE in pregnancy, and VTE in children. The website indicates that additional guidelines will soon be released on managing VTE in patients with cancer, in patients with thrombophilia, and for prophylaxis in surgical patients, as well as further information on treatment. A spokesperson for ASH said that these additional documents will post sometime in 2019.
At the time of the release, the guidelines panel published six articles in the journal Blood Advances that detailed the guidelines and their documentation.
The articles include prophylaxis of medical patients (Blood Advances. 2018 Nov 27;2[22]:3198-225), diagnosis (Blood Advances. 2018 Nov 27;2[22]:3226-56), anticoagulation therapy (Blood Advances. 2018 Nov 27;2[22]:3257-91), pediatrics (Blood Advances. 2018 Nov 27;2[22]:3292-316), pregnancy (Blood Advances. 2018 Nov 27;2[22]:3317-59), and heparin-induced thrombocytopenia (Blood Advances. 2018 Nov 27;2[22]:3360-92).
Dr. Cushman, Dr. Lim, and Dr. Witt reported having no relevant disclosures. Dr. Cuker reported receiving research support from T2 Biosystems.
Glucocorticoid elimination works for 2/3 of RA patients on tocilizumab
CHICAGO – while remaining in at least low disease activity in a multicenter, randomized trial with 259 patients.
The results also showed that rheumatoid arthritis (RA) patients randomized to maintain prednisone treatment at 5 mg/day along with tocilizumab fared even better. After 24 weeks of the glucocorticoid-tapering regimen, by which time patients in the tapered arm had their prednisone dosage down to 0 mg, the average change from baseline in their disease activity score 28 with erythrocyte sedimentation rate (DAS28-ESR) was an increase of 0.538, compared with an average drop of 0.075 among untapered patients, a statistically significant difference for the study’s primary endpoint, Gerd R. Burmester, MD, said at the annual meeting of the American College of Rheumatology.
But while the results definitively showed that RA patients treated with the anti-interleukin 6 agent tocilizumab (Actemra) as their primary drug benefited from continued, additional treatment with low-dose prednisone, the results also showed that many patients could come off prednisone without immediate downside. Among the 131 randomized to a forced taper and eventual prednisone discontinuation, 85 (65%) went through this process without flaring and maintained at least low disease activity and sometimes remission, said Dr. Burmester, a professor and director of rheumatology and clinical immunology at Charité Hospital in Berlin. In contrast, 99 of 128 patients (77%) maintained on tocilizumab plus 5 mg/day of prednisone were free from any flares and had at least low disease activity after 24 weeks, a statistically significant between-group difference.
These findings “have potential to inform clinical practice and aid in conversations with patients. RA patients who achieve at least low disease activity while receiving tocilizumab and long-term glucocorticoid treatment at 5 mg/day should be considered for tapering of their glucocorticoid dosage, ideally targeting discontinuation,” Dr. Burmester said.
Addressing a comment from the audience that it’s common knowledge that patients who are well controlled on a potent immunomodulating drug like tocilizumab can often successfully wean off a glucocorticoid, Dr. Burmester insisted that it was important to show this in a randomized, blinded trial.
“When they discontinue [a glucocorticoid] patients can develop myalgias or other symptoms and we haven’t known whether that was real or psychological. In this study patients did not know whether they were being discontinued, so the psychological element was gone,” he said. The new findings confirm in a rigorous way that “we could discontinue a substantial number of patients who probably no longer need a glucocorticoid. It’s an important discussion” for clinicians to have with patients.
The SEMIRA (Steroid Elimination in RA) trial enrolled 68 patients who had already begun tocilizumab treatment and 191 patients new to the drug who had a 24-week run-in on tocilizumab, all of whom also received 5 mg prednisone daily. The trial included 46 sites in five European countries plus Russia and Tunisia. During the main 24-week phase of the study, 128 patients remained on their entry regimen of tocilizumab and prednisone, with 112 completers; 131 others went through a forced taper that culminated in no prednisone administered during the final 8 weeks, with 114 completers. Patients averaged about 54 years old, and just over three-quarters were women. Almost two-thirds of patients also received a nonbiologic disease-modifying antirheumatic drug.
A time-trend analysis of changes in DAS28-ERS showed that, while the difference in change from baseline in disease activity between the two treatment arms separated early in the taper process, the biggest uptick in DAS28-ESR in the patients coming off prednisone occurred once the final 1 mg/day dose was stopped.
The results also showed that tapering led to a statistically significant rise in the clinical disease activity index for RA, compared with that seen with not tapering, and tapering also was linked significantly with an increase in serum markers of bone turnover. The safety analysis showed no striking between-group differences in adverse events and in serious adverse events, and no patients developed confirmed adrenal insufficiency that required replacement therapy.
SOURCE: Burmester G et al. Arthritis Rheumatol. 2018;70(suppl 10): Abstract L18.
Tapering well-controlled rheumatoid arthritis patients off glucocorticoid treatment is often attempted in clinical practice, but until now no evidence base existed to justify this approach. While the results reported by Dr. Burmester from the SEMIRA study are not unexpected, it’s very helpful to see these data from a well-designed study.
What remains unclear is the generalizability of the findings: Do they only apply to patients receiving tocilizumab as their primary antirheumatic drug or does glucocorticoid tapering work the same way in RA patients on different drugs?
The results also confirm another impression that many clinicians have had but until now was unsubstantiated: Eliminating the final 1 mg of daily glucocorticoid treatment is the most difficult part of tapering patients down to complete corticosteroid withdrawal. What often happens in practice is that patients get down to the last 1 or 2 mg of daily glucocorticoid treatment but further reduction beyond that causes a flare or a manifestation of steroid-withdrawal syndrome.
The results from this study give clinicians a better context for discussing glucocorticoid tapering with patients. Even with a potent antirheumatic drug like tocilizumab, it’s hard for some patients to completely withdraw from a glucocorticoid. Even at very low dosages glucocorticoids still have a very meaningful effect on some patients.
David S. Pisetsky, MD , is a professor of medicine at Duke University in Durham, N.C. He has been a consultant to Celgene, Celltrion, GlaxoSmithKline, and Lilly, and he has received research support from Pfizer. He made these comments in an interview.
Tapering well-controlled rheumatoid arthritis patients off glucocorticoid treatment is often attempted in clinical practice, but until now no evidence base existed to justify this approach. While the results reported by Dr. Burmester from the SEMIRA study are not unexpected, it’s very helpful to see these data from a well-designed study.
What remains unclear is the generalizability of the findings: Do they only apply to patients receiving tocilizumab as their primary antirheumatic drug or does glucocorticoid tapering work the same way in RA patients on different drugs?
The results also confirm another impression that many clinicians have had but until now was unsubstantiated: Eliminating the final 1 mg of daily glucocorticoid treatment is the most difficult part of tapering patients down to complete corticosteroid withdrawal. What often happens in practice is that patients get down to the last 1 or 2 mg of daily glucocorticoid treatment but further reduction beyond that causes a flare or a manifestation of steroid-withdrawal syndrome.
The results from this study give clinicians a better context for discussing glucocorticoid tapering with patients. Even with a potent antirheumatic drug like tocilizumab, it’s hard for some patients to completely withdraw from a glucocorticoid. Even at very low dosages glucocorticoids still have a very meaningful effect on some patients.
David S. Pisetsky, MD , is a professor of medicine at Duke University in Durham, N.C. He has been a consultant to Celgene, Celltrion, GlaxoSmithKline, and Lilly, and he has received research support from Pfizer. He made these comments in an interview.
Tapering well-controlled rheumatoid arthritis patients off glucocorticoid treatment is often attempted in clinical practice, but until now no evidence base existed to justify this approach. While the results reported by Dr. Burmester from the SEMIRA study are not unexpected, it’s very helpful to see these data from a well-designed study.
What remains unclear is the generalizability of the findings: Do they only apply to patients receiving tocilizumab as their primary antirheumatic drug or does glucocorticoid tapering work the same way in RA patients on different drugs?
The results also confirm another impression that many clinicians have had but until now was unsubstantiated: Eliminating the final 1 mg of daily glucocorticoid treatment is the most difficult part of tapering patients down to complete corticosteroid withdrawal. What often happens in practice is that patients get down to the last 1 or 2 mg of daily glucocorticoid treatment but further reduction beyond that causes a flare or a manifestation of steroid-withdrawal syndrome.
The results from this study give clinicians a better context for discussing glucocorticoid tapering with patients. Even with a potent antirheumatic drug like tocilizumab, it’s hard for some patients to completely withdraw from a glucocorticoid. Even at very low dosages glucocorticoids still have a very meaningful effect on some patients.
David S. Pisetsky, MD , is a professor of medicine at Duke University in Durham, N.C. He has been a consultant to Celgene, Celltrion, GlaxoSmithKline, and Lilly, and he has received research support from Pfizer. He made these comments in an interview.
CHICAGO – while remaining in at least low disease activity in a multicenter, randomized trial with 259 patients.
The results also showed that rheumatoid arthritis (RA) patients randomized to maintain prednisone treatment at 5 mg/day along with tocilizumab fared even better. After 24 weeks of the glucocorticoid-tapering regimen, by which time patients in the tapered arm had their prednisone dosage down to 0 mg, the average change from baseline in their disease activity score 28 with erythrocyte sedimentation rate (DAS28-ESR) was an increase of 0.538, compared with an average drop of 0.075 among untapered patients, a statistically significant difference for the study’s primary endpoint, Gerd R. Burmester, MD, said at the annual meeting of the American College of Rheumatology.
But while the results definitively showed that RA patients treated with the anti-interleukin 6 agent tocilizumab (Actemra) as their primary drug benefited from continued, additional treatment with low-dose prednisone, the results also showed that many patients could come off prednisone without immediate downside. Among the 131 randomized to a forced taper and eventual prednisone discontinuation, 85 (65%) went through this process without flaring and maintained at least low disease activity and sometimes remission, said Dr. Burmester, a professor and director of rheumatology and clinical immunology at Charité Hospital in Berlin. In contrast, 99 of 128 patients (77%) maintained on tocilizumab plus 5 mg/day of prednisone were free from any flares and had at least low disease activity after 24 weeks, a statistically significant between-group difference.
These findings “have potential to inform clinical practice and aid in conversations with patients. RA patients who achieve at least low disease activity while receiving tocilizumab and long-term glucocorticoid treatment at 5 mg/day should be considered for tapering of their glucocorticoid dosage, ideally targeting discontinuation,” Dr. Burmester said.
Addressing a comment from the audience that it’s common knowledge that patients who are well controlled on a potent immunomodulating drug like tocilizumab can often successfully wean off a glucocorticoid, Dr. Burmester insisted that it was important to show this in a randomized, blinded trial.
“When they discontinue [a glucocorticoid] patients can develop myalgias or other symptoms and we haven’t known whether that was real or psychological. In this study patients did not know whether they were being discontinued, so the psychological element was gone,” he said. The new findings confirm in a rigorous way that “we could discontinue a substantial number of patients who probably no longer need a glucocorticoid. It’s an important discussion” for clinicians to have with patients.
The SEMIRA (Steroid Elimination in RA) trial enrolled 68 patients who had already begun tocilizumab treatment and 191 patients new to the drug who had a 24-week run-in on tocilizumab, all of whom also received 5 mg prednisone daily. The trial included 46 sites in five European countries plus Russia and Tunisia. During the main 24-week phase of the study, 128 patients remained on their entry regimen of tocilizumab and prednisone, with 112 completers; 131 others went through a forced taper that culminated in no prednisone administered during the final 8 weeks, with 114 completers. Patients averaged about 54 years old, and just over three-quarters were women. Almost two-thirds of patients also received a nonbiologic disease-modifying antirheumatic drug.
A time-trend analysis of changes in DAS28-ERS showed that, while the difference in change from baseline in disease activity between the two treatment arms separated early in the taper process, the biggest uptick in DAS28-ESR in the patients coming off prednisone occurred once the final 1 mg/day dose was stopped.
The results also showed that tapering led to a statistically significant rise in the clinical disease activity index for RA, compared with that seen with not tapering, and tapering also was linked significantly with an increase in serum markers of bone turnover. The safety analysis showed no striking between-group differences in adverse events and in serious adverse events, and no patients developed confirmed adrenal insufficiency that required replacement therapy.
SOURCE: Burmester G et al. Arthritis Rheumatol. 2018;70(suppl 10): Abstract L18.
CHICAGO – while remaining in at least low disease activity in a multicenter, randomized trial with 259 patients.
The results also showed that rheumatoid arthritis (RA) patients randomized to maintain prednisone treatment at 5 mg/day along with tocilizumab fared even better. After 24 weeks of the glucocorticoid-tapering regimen, by which time patients in the tapered arm had their prednisone dosage down to 0 mg, the average change from baseline in their disease activity score 28 with erythrocyte sedimentation rate (DAS28-ESR) was an increase of 0.538, compared with an average drop of 0.075 among untapered patients, a statistically significant difference for the study’s primary endpoint, Gerd R. Burmester, MD, said at the annual meeting of the American College of Rheumatology.
But while the results definitively showed that RA patients treated with the anti-interleukin 6 agent tocilizumab (Actemra) as their primary drug benefited from continued, additional treatment with low-dose prednisone, the results also showed that many patients could come off prednisone without immediate downside. Among the 131 randomized to a forced taper and eventual prednisone discontinuation, 85 (65%) went through this process without flaring and maintained at least low disease activity and sometimes remission, said Dr. Burmester, a professor and director of rheumatology and clinical immunology at Charité Hospital in Berlin. In contrast, 99 of 128 patients (77%) maintained on tocilizumab plus 5 mg/day of prednisone were free from any flares and had at least low disease activity after 24 weeks, a statistically significant between-group difference.
These findings “have potential to inform clinical practice and aid in conversations with patients. RA patients who achieve at least low disease activity while receiving tocilizumab and long-term glucocorticoid treatment at 5 mg/day should be considered for tapering of their glucocorticoid dosage, ideally targeting discontinuation,” Dr. Burmester said.
Addressing a comment from the audience that it’s common knowledge that patients who are well controlled on a potent immunomodulating drug like tocilizumab can often successfully wean off a glucocorticoid, Dr. Burmester insisted that it was important to show this in a randomized, blinded trial.
“When they discontinue [a glucocorticoid] patients can develop myalgias or other symptoms and we haven’t known whether that was real or psychological. In this study patients did not know whether they were being discontinued, so the psychological element was gone,” he said. The new findings confirm in a rigorous way that “we could discontinue a substantial number of patients who probably no longer need a glucocorticoid. It’s an important discussion” for clinicians to have with patients.
The SEMIRA (Steroid Elimination in RA) trial enrolled 68 patients who had already begun tocilizumab treatment and 191 patients new to the drug who had a 24-week run-in on tocilizumab, all of whom also received 5 mg prednisone daily. The trial included 46 sites in five European countries plus Russia and Tunisia. During the main 24-week phase of the study, 128 patients remained on their entry regimen of tocilizumab and prednisone, with 112 completers; 131 others went through a forced taper that culminated in no prednisone administered during the final 8 weeks, with 114 completers. Patients averaged about 54 years old, and just over three-quarters were women. Almost two-thirds of patients also received a nonbiologic disease-modifying antirheumatic drug.
A time-trend analysis of changes in DAS28-ERS showed that, while the difference in change from baseline in disease activity between the two treatment arms separated early in the taper process, the biggest uptick in DAS28-ESR in the patients coming off prednisone occurred once the final 1 mg/day dose was stopped.
The results also showed that tapering led to a statistically significant rise in the clinical disease activity index for RA, compared with that seen with not tapering, and tapering also was linked significantly with an increase in serum markers of bone turnover. The safety analysis showed no striking between-group differences in adverse events and in serious adverse events, and no patients developed confirmed adrenal insufficiency that required replacement therapy.
SOURCE: Burmester G et al. Arthritis Rheumatol. 2018;70(suppl 10): Abstract L18.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Many rheumatoid arthritis patients with low disease activity on tocilizumab plus a glucocorticoid can taper off the corticosteroid without flaring.
Major finding: In RA patients with low disease activity on tocilizumab plus prednisone, 65% came off the glucocorticoid without flaring or relapse.
Study details: SEMIRA, a multicenter, randomized study with 259 rheumatoid arthritis patients.
Disclosures: SEMIRA was funded by Hoffmann-La Roche. Dr. Burmester has been a consultant to and speaker on behalf of Roche and Sanofi-Genzyme.
Source: Burmester G et al. Arthritis Rheumatol. 2018;70(suppl 10): Abstract L18.
Nerve growth factor antibody cuts OA pain with low AEs
CHICAGO – The nerve growth factor antibody tanezumab met its primary efficacy endpoints for improving pain and physical function in patients with knee or hip OA while also showing a low incidence of the drug’s most concerning adverse effect in the first results from a phase 3 study of a drug in this new class.
The placebo-controlled, multicenter study enrolled 696 U.S. OA patients with moderate to severe knee or hip pain and showed that two subcutaneous injections of the humanized antibody tanezumab spaced 8 weeks apart led to statistically significant improvements relative to placebo for pain, physical function, and patient global assessment of OA, Thomas J. Schnitzer, MD, said at the annual meeting of the American College of Rheumatology.
The primary efficacy measurements occurred 8 weeks following the second subcutaneous injection. The study included two active treatment arms, and all the efficacy measures responses showed consistent, “modest” improvements in the patients who received a 2.5 mg injection followed by a 5 mg injection, compared with those who received two 2.5 mg injections.
For the safety analysis the researchers followed patients out to 24 weeks after they received their final injection. The main adverse event of interest was rapidly progressive OA (RPOA), which occurred in five patients who received two 2.5-mg dosages and in one patient who received the 2.5 mg followed by 5 mg regimen; no RPOA occurred among placebo patients. The 1.3% incidence of RPOA among all 494 patients who received tanezumab “aligned with expectations based on the risk mitigation procedures used,” said Dr. Schnitzer, a rheumatologist and professor of medicine, anesthesiology, and physical medicine and rehabilitation at Northwestern University, Chicago. No patient developed primary osteonecrosis.
Two patients who developed RPOA then underwent total joint replacement. The overall rate of total joint replacement was 4 among placebo patients, all involving knees, and 24 among patients treated with tanezumab, including 12 knee replacements and 12 hip replacements. Blinded adjudication determined that 26 of the total 28 joint replacements resulted from “normal” OA progression.
The rates of all adverse events, serious adverse events, and adverse events leading to treatment discontinuation were low and similar in the three treatment arms.
Earlier clinical studies of tanezumab had signaled a problem with RPOA (Arthritis Rheumatol. 2016 Feb;68[2]:382-91), which led the Food and Drug Administration to order a temporary halt to clinical testing of all nerve growth factor antagonists in 2010 that the agency then lifted in 2015 (Clin Exp Rheumatol. 2017 Sept-Oct;35[suppl 107]:85-7). In 2017, the FDA gave clinical development of tanezumab “fast-track” status. The results that Dr. Schnitzer reported represent the first outcomes from several phase 3 studies that the companies developing tanezumab are now running and that collectively include about 7,000 total patients, according to a written statement from the developing companies. The companies released an initial statement about the current results in July 2018.
The study reported by Dr. Schnitzer enrolled patients with OA of the knee or hip at several U.S. sites. For the primary endpoint of mean change from baseline in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score, the results at 16 weeks were –2.6 units in the placebo patients and –3.4 units among patients who received the higher dosage. For the primary outcome of mean change in WOMAC physical function score, the results were –2.6 in the placebo arm and –3.5 in patients on the higher dosage. For the primary outcome of change in patient’s global assessment of their OA, the results were –0.65 in the placebo patients and –0.90 in those on the highest dosage. All three between-group differences were statistically significant.
A key secondary outcome was the percentage of patients having at least a 50% reduction in their WOMAC pain score, which occurred in 38% of the placebo patients and in 57% on the higher tanezumab dosage, a statistically significant difference, Dr. Schnitzer reported. A final efficacy finding was the percentage of patients who had a 50% or greater pain reduction at week 16 who did not have a pain response at week 8, a parameter that could reflect incremental benefit from the larger, second tanezumab dose. This outcome occurred in 19% of placebo patients and in 22% of patients who received two 2.5-mg doses of tanezumab; among those who received a 5-mg dose after the first 2.5-mg dose, the rate was 33%.
The study was sponsored by Eli Lilly and Pfizer, the companies jointly developing tanezumab. Dr. Schnitzer has been a consultant to and has received research support from Eli Lilly and Pfizer. He has also been a consultant to AbbVie, Aptinyx, Genzyme, Regeneron, and Vertex Pharmaceuticals, and has received research support from Grünenthal and Radius Health.
SOURCE: Schnitzer TJ et al. Arthritis Rheumatol. 2018;70(Suppl 10) Abstract L20.
CHICAGO – The nerve growth factor antibody tanezumab met its primary efficacy endpoints for improving pain and physical function in patients with knee or hip OA while also showing a low incidence of the drug’s most concerning adverse effect in the first results from a phase 3 study of a drug in this new class.
The placebo-controlled, multicenter study enrolled 696 U.S. OA patients with moderate to severe knee or hip pain and showed that two subcutaneous injections of the humanized antibody tanezumab spaced 8 weeks apart led to statistically significant improvements relative to placebo for pain, physical function, and patient global assessment of OA, Thomas J. Schnitzer, MD, said at the annual meeting of the American College of Rheumatology.
The primary efficacy measurements occurred 8 weeks following the second subcutaneous injection. The study included two active treatment arms, and all the efficacy measures responses showed consistent, “modest” improvements in the patients who received a 2.5 mg injection followed by a 5 mg injection, compared with those who received two 2.5 mg injections.
For the safety analysis the researchers followed patients out to 24 weeks after they received their final injection. The main adverse event of interest was rapidly progressive OA (RPOA), which occurred in five patients who received two 2.5-mg dosages and in one patient who received the 2.5 mg followed by 5 mg regimen; no RPOA occurred among placebo patients. The 1.3% incidence of RPOA among all 494 patients who received tanezumab “aligned with expectations based on the risk mitigation procedures used,” said Dr. Schnitzer, a rheumatologist and professor of medicine, anesthesiology, and physical medicine and rehabilitation at Northwestern University, Chicago. No patient developed primary osteonecrosis.
Two patients who developed RPOA then underwent total joint replacement. The overall rate of total joint replacement was 4 among placebo patients, all involving knees, and 24 among patients treated with tanezumab, including 12 knee replacements and 12 hip replacements. Blinded adjudication determined that 26 of the total 28 joint replacements resulted from “normal” OA progression.
The rates of all adverse events, serious adverse events, and adverse events leading to treatment discontinuation were low and similar in the three treatment arms.
Earlier clinical studies of tanezumab had signaled a problem with RPOA (Arthritis Rheumatol. 2016 Feb;68[2]:382-91), which led the Food and Drug Administration to order a temporary halt to clinical testing of all nerve growth factor antagonists in 2010 that the agency then lifted in 2015 (Clin Exp Rheumatol. 2017 Sept-Oct;35[suppl 107]:85-7). In 2017, the FDA gave clinical development of tanezumab “fast-track” status. The results that Dr. Schnitzer reported represent the first outcomes from several phase 3 studies that the companies developing tanezumab are now running and that collectively include about 7,000 total patients, according to a written statement from the developing companies. The companies released an initial statement about the current results in July 2018.
The study reported by Dr. Schnitzer enrolled patients with OA of the knee or hip at several U.S. sites. For the primary endpoint of mean change from baseline in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score, the results at 16 weeks were –2.6 units in the placebo patients and –3.4 units among patients who received the higher dosage. For the primary outcome of mean change in WOMAC physical function score, the results were –2.6 in the placebo arm and –3.5 in patients on the higher dosage. For the primary outcome of change in patient’s global assessment of their OA, the results were –0.65 in the placebo patients and –0.90 in those on the highest dosage. All three between-group differences were statistically significant.
A key secondary outcome was the percentage of patients having at least a 50% reduction in their WOMAC pain score, which occurred in 38% of the placebo patients and in 57% on the higher tanezumab dosage, a statistically significant difference, Dr. Schnitzer reported. A final efficacy finding was the percentage of patients who had a 50% or greater pain reduction at week 16 who did not have a pain response at week 8, a parameter that could reflect incremental benefit from the larger, second tanezumab dose. This outcome occurred in 19% of placebo patients and in 22% of patients who received two 2.5-mg doses of tanezumab; among those who received a 5-mg dose after the first 2.5-mg dose, the rate was 33%.
The study was sponsored by Eli Lilly and Pfizer, the companies jointly developing tanezumab. Dr. Schnitzer has been a consultant to and has received research support from Eli Lilly and Pfizer. He has also been a consultant to AbbVie, Aptinyx, Genzyme, Regeneron, and Vertex Pharmaceuticals, and has received research support from Grünenthal and Radius Health.
SOURCE: Schnitzer TJ et al. Arthritis Rheumatol. 2018;70(Suppl 10) Abstract L20.
CHICAGO – The nerve growth factor antibody tanezumab met its primary efficacy endpoints for improving pain and physical function in patients with knee or hip OA while also showing a low incidence of the drug’s most concerning adverse effect in the first results from a phase 3 study of a drug in this new class.
The placebo-controlled, multicenter study enrolled 696 U.S. OA patients with moderate to severe knee or hip pain and showed that two subcutaneous injections of the humanized antibody tanezumab spaced 8 weeks apart led to statistically significant improvements relative to placebo for pain, physical function, and patient global assessment of OA, Thomas J. Schnitzer, MD, said at the annual meeting of the American College of Rheumatology.
The primary efficacy measurements occurred 8 weeks following the second subcutaneous injection. The study included two active treatment arms, and all the efficacy measures responses showed consistent, “modest” improvements in the patients who received a 2.5 mg injection followed by a 5 mg injection, compared with those who received two 2.5 mg injections.
For the safety analysis the researchers followed patients out to 24 weeks after they received their final injection. The main adverse event of interest was rapidly progressive OA (RPOA), which occurred in five patients who received two 2.5-mg dosages and in one patient who received the 2.5 mg followed by 5 mg regimen; no RPOA occurred among placebo patients. The 1.3% incidence of RPOA among all 494 patients who received tanezumab “aligned with expectations based on the risk mitigation procedures used,” said Dr. Schnitzer, a rheumatologist and professor of medicine, anesthesiology, and physical medicine and rehabilitation at Northwestern University, Chicago. No patient developed primary osteonecrosis.
Two patients who developed RPOA then underwent total joint replacement. The overall rate of total joint replacement was 4 among placebo patients, all involving knees, and 24 among patients treated with tanezumab, including 12 knee replacements and 12 hip replacements. Blinded adjudication determined that 26 of the total 28 joint replacements resulted from “normal” OA progression.
The rates of all adverse events, serious adverse events, and adverse events leading to treatment discontinuation were low and similar in the three treatment arms.
Earlier clinical studies of tanezumab had signaled a problem with RPOA (Arthritis Rheumatol. 2016 Feb;68[2]:382-91), which led the Food and Drug Administration to order a temporary halt to clinical testing of all nerve growth factor antagonists in 2010 that the agency then lifted in 2015 (Clin Exp Rheumatol. 2017 Sept-Oct;35[suppl 107]:85-7). In 2017, the FDA gave clinical development of tanezumab “fast-track” status. The results that Dr. Schnitzer reported represent the first outcomes from several phase 3 studies that the companies developing tanezumab are now running and that collectively include about 7,000 total patients, according to a written statement from the developing companies. The companies released an initial statement about the current results in July 2018.
The study reported by Dr. Schnitzer enrolled patients with OA of the knee or hip at several U.S. sites. For the primary endpoint of mean change from baseline in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score, the results at 16 weeks were –2.6 units in the placebo patients and –3.4 units among patients who received the higher dosage. For the primary outcome of mean change in WOMAC physical function score, the results were –2.6 in the placebo arm and –3.5 in patients on the higher dosage. For the primary outcome of change in patient’s global assessment of their OA, the results were –0.65 in the placebo patients and –0.90 in those on the highest dosage. All three between-group differences were statistically significant.
A key secondary outcome was the percentage of patients having at least a 50% reduction in their WOMAC pain score, which occurred in 38% of the placebo patients and in 57% on the higher tanezumab dosage, a statistically significant difference, Dr. Schnitzer reported. A final efficacy finding was the percentage of patients who had a 50% or greater pain reduction at week 16 who did not have a pain response at week 8, a parameter that could reflect incremental benefit from the larger, second tanezumab dose. This outcome occurred in 19% of placebo patients and in 22% of patients who received two 2.5-mg doses of tanezumab; among those who received a 5-mg dose after the first 2.5-mg dose, the rate was 33%.
The study was sponsored by Eli Lilly and Pfizer, the companies jointly developing tanezumab. Dr. Schnitzer has been a consultant to and has received research support from Eli Lilly and Pfizer. He has also been a consultant to AbbVie, Aptinyx, Genzyme, Regeneron, and Vertex Pharmaceuticals, and has received research support from Grünenthal and Radius Health.
SOURCE: Schnitzer TJ et al. Arthritis Rheumatol. 2018;70(Suppl 10) Abstract L20.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point:
Major finding: The Western Ontario and McMaster Universities Osteoarthritis Index pain score fell by an average –3.4 points with maximum tanezumab treatment and by –2.6 points with placebo.
Study details: A multicenter, randomized study with 696 patients with moderate to severe OA of the knee or hip and moderate to severe pain.
Disclosures: The study was sponsored by Eli Lilly and Pfizer, the companies jointly developing tanezumab. Dr. Schnitzer has been a consultant to and has received research support from Eli Lilly and Pfizer. He has also been a consultant to AbbVie, Aptinyx, Genzyme, Regeneron, and Vertex Pharmaceuticals, and has received research support from Grünenthal and Radius Health.
Source: Schnitzer TJ et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract L20.
Tofacitinib and TNF inhibitors show similar VTE rates
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
CHICAGO – Rheumatoid arthritis patients treated with tofacitinib did not have a significantly increased incidence of hospitalization for venous thromboembolism, compared with patients treated with a tumor necrosis factor (TNF) inhibitor, in a study of more than 50,000 U.S. patients culled from a pair of health insurance databases.
The Janus kinase inhibitor class of agents, including tofacitinib (Xeljanz), has acquired a reputation for causing an excess of venous thromboembolic events (VTE) (Drug Saf. 2018 Jul;41[7]:645-53). To assess this in a real-world setting Seoyoung C. Kim, MD, and her associates took data from Medicare patients during 2012-2015 and from Truven MarketScan for commercially insured patients during 2012-2016 and derived a database of 16,091 RA patients on newly begun treatment with a TNF inhibitor and 995 newly begun on tofacitinib in the Medicare data, and 32,164 RA patients newly started on a TNF inhibitor and 1,910 on tofacitinib in the Truven database. The analysis excluded patients with a history of VTE.
Using propensity score–adjusted matching of patients in the two treatment arms in both of these databases, and using a VTE event – either a pulmonary embolism or deep-vein thrombosis that resulted in hospitalization – as the primary endpoint, the results showed statistically nonsignificant excesses of VTE in the patients treated with tofacitinib, compared with a TNF inhibitor, Dr. Kim reported in a poster she presented at the annual meeting of the American College of Rheumatology.
In the adjusted comparison, the Medicare data showed a nonsignificant 12% higher VTE rate in the tofacitinib-treated patients, while the Truven data showed a nonsignificant 55% higher rate of VTE during tofacitinib treatment. When the data were pooled, the result was a 33% higher rate of VTE while on tofacitinib treatment, which was not statistically significant.
Dr. Kim cautioned that the low rate of VTE events, especially among the patients on tofacitinib, limited the precision of the results. The combined data included 2,905 patients on tofacitinib treatment who had 15 VTE events, a rate of 0.77 events/100 person-years of follow-up. This compared with a rate of 0.52/100 person-years among patients on a TNF inhibitor. Thus, in both treatment groups the absolute VTE rate was low.
The most reliable finding from the analysis is that it “rules out a large increase in the risk for VTE events with tofacitinib,” said Dr. Kim, a rheumatologist at Brigham and Women’s Hospital in Boston.
The researchers also ran an analysis that included not only VTE events that resulted in hospitalization but also VTE events managed on an outpatient basis. Dr. Kim did not report the specific numbers involved in this calculation, but she reported that, when her group included both types of VTE events, the patients treated with tofacitinib had a nonsignificant 12% lower rate of events, compared with patients treated with a TNF inhibitor.
Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
SOURCE: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Rheumatoid arthritis patients treated with tofacitinib showed no excess incidence of venous thromboembolism, compared with patients on a tumor necrosis factor inhibitor.
Major finding: Propensity score–adjusted rates of VTE were 33% higher with tofacitinib, compared with TNF inhibition, which was not a statistically significant difference.
Study details: Review of 51,160 rheumatoid arthritis patients from U.S. health insurance databases.
Disclosures: Dr. Kim has received research support from Bristol-Myers Squibb, Pfizer, and Roche.
Source: Desai RJ et al. Arthritis Rheumatol. 2018;70(suppl 10), Abstract L09.
CAC scores in type 1 diabetes no higher than general population
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
CHICAGO – Roughly 70% of some 1,200 adult patients with type 1 diabetes screened for coronary artery calcium had a score of zero, about the same prevalence as in the general, U.S. adult population, suggesting the unexpected conclusion that a majority of middle-aged patients with type 1 diabetes do not have an elevated risk for coronary artery disease, in contrast to patients with type 2 diabetes.
Among 1,205 asymptomatic people with type 1 diabetes who underwent coronary artery calcium (CAC) measurement and were followed for an average of about 11 years, 71% had a CAC score of zero at baseline followed by a cardiovascular disease event rate of 5.6 events/1,000 patient years of follow-up, a “very low” event rate that made these patients no more likely to have an event than any adult of similar age and sex in the general U.S. population, Matthew J. Budoff, MD, said at the American Heart Association scientific sessions.
In prior reports, about half of patients with type 2 diabetes had a CAC score of zero, noted Dr. Budoff, professor of medicine and a specialist in cardiac CT imaging and preventive cardiology at the University of California, Los Angeles. In a general adult population that’s about 45 years old roughly three-quarters would have a CAC score of zero, he noted.
Until now, little has been known about CAC scores in asymptomatic, middle-aged adults with type 1 diabetes. The findings reported by Dr. Budoff raise questions about the 2018 revision of the cholesterol guideline from the American College of Cardiology and American Heart Association, released during the meeting (J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003), which lumps type 1 and type 2 diabetes together as a special high-risk category for cholesterol management.
The guideline should instead “advocate for more therapy with a CAC score of more than 100 and less therapy with a CAC score of zero in patients with type 1 diabetes,” Dr. Budoff suggested. “A statin for someone with a CAC score of zero probably won’t result in event reduction. The 70% of patients with type 1 diabetes who have a CAC score of zero potentially may not benefit from a statin,” he said in a video interview.
Dr. Budoff and his associates used CAC scores and outcomes data collected on 1,205 asymptomatic people with type 1 diabetes enrolled in the EDIC (Epidemiology of Diabetes Interventions and Complications) trial who underwent CAC scoring as part of the study protocol when they averaged 43 years of age. Follow-up tracked the incidence of cardiovascular disease events in 1,156 of these patients for an average of about 11 years. During follow-up, 105 patients had a cardiovascular disease event, an overall rate of 8.5 events/1,000 patient years of follow-up.
The results also confirmed the prognostic power of the CAC score in these patients. Compared with the very low event rate among those with a zero score, patients with a score of 1-100 had 71% more events, patients with a CAC score of 101-300 had a 5.4-fold higher event rate as those with no coronary calcium, and patients with a CAC score of greater than 300 had a 6.9-fold higher event rate than those with no coronary calcium, Dr. Budoff reported.
Coronary calcium deposits, a direct reflection of atheroma load, can change over time, but somewhat slowly. A CAC score of zero is very reliable for predicting a very low rate of cardiovascular disease events over the subsequent 5 years, and in many people it can reliably predict for as long as 10 years, Dr. Budoff said. Beyond that, follow-up CAC scoring is necessary to check for changes in coronary status, “especially in patients with type 1 diabetes,”
SOURCE: Budoff M et al. Abstract 13133.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: .
Major finding: Seventy-one percent of patients with type 1 diabetes had a coronary artery calcium score of zero.
Study details: Review of data collected from 1,205 patients in the EDIC trial.
Disclosures: The EDIC trial had no commercial funding. Dr. Budoff has received research funding from General Electric.
Source: Budoff M et al. AHA 2018, Abstract 13133.