User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
FDA panel leans toward more robust breast implant surveillance
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
Occurrence of pulmonary embolisms in hospitalized patients nearly doubled during 2004-2015
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
REPORTING FROM ACC 2019
Patient selection for acute stroke thrombectomy stirs controversy
HONOLULU – A little more than a year ago, results from the DAWN and DEFUSE 3 trials substantially broadened the time window for endovascular thrombectomy of acute ischemic stroke by selecting patients using brain imaging. Stroke clinicians are now trying to reconcile widespread, routine use of this life-changing treatment against an uncertain need to replicate the higher-end perfusion CT and analytical software imaging that these landmark trials used for patient selection. This has produced a schism in what experts advise for using endovascular thrombectomy on acute ischemic stroke patients.
“Go open the artery, people!” Michael D. Hill, MD, exhorted during a talk at the International Stroke Conference, sponsored by the American Heart Association. “Don’t get over-selective; more people will benefit than you think,” said Dr. Hill, a professor of clinical neurosciences at the University of Calgary (Alta.).
“We are over-selecting, and depriving patients,” commented Raul C. Nogueira, MD, professor of neurology at Emory University in Atlanta and a lead investigator of the DAWN trial, speaking from the audience during a discussion at the session where Dr. Hill spoke.
“The prevalence of treatable [acute ischemic stroke] patients is far higher than the prevalence of patients who are not good candidates, so you just want to exclude the ‘wipe-outs’; that’s what we do,” Dr. Hill explained. “Fortunately, endovascular therapy is very safe, and you’re not going to harm many patients. With other treatments [used routinely in medicine] some patients don’t benefit, but when you have a large effect size we use the treatment on almost everyone. The effect size from thrombectomy is so large it’s an argument to treat almost everyone, although the patients in the trials were selected by imaging.”
Dr. Hill repeatedly stressed that for most patients a non-contrast CT image is usually adequate to identify patients with salvageable brain tissue and a low risk for hemorrhage from intervention, and he endorsed also doing CT angiography to further inform the diagnosis. But he dismissed CT perfusion imaging as unnecessary. “Noncontrast CT and CT angiography are more than adequate to make treatment decisions,” he said. “The prevalence of poor collaterals is quite low, about 10%,” which means that about 90% of acute ischemic stroke patients will have more slowly progressing infarction,” making them amenable to treatment in an expanded time window and boosting the volume of salvageable tissue.
But these appeals for more liberal use of thrombectomy without the perfusion CT imaging used in DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21)and DEFUSE-3 (N Engl J Med. 2018 Feb 22;378[8]:708-18) received push back. Maarten G. Lansberg, MD, a co-investigator on the DEFUSE 3 trial, highlighted the speed and simplicity of CT perfusion imaging, and its utility in helping to better target thrombectomy to the right patients. It’s “speedy, simple, and safe,” it “excludes patients who will not benefit” from thrombectomy, and it helps when the patient’s history and noncontrast CT images are inconclusive, said Dr. Lansberg, a neurologist at Stanford (Calif.) University.
“Clinical presentation will only tell you so much.” With imaging that includes CT perfusion, “you can find out, in 5, 10 minutes, whether there is an occlusion, its location, the extent of dead tissue – that’s all really helpful,” said Marc Fisher, MD, professor of neurology at Harvard Medical School in Boston. “There is a tension now between doing treatment really fast and the concept of slow and fast evolvers. For slow evolvers, the concern about speed is irrelevant because it can take days” for their brains to have substantial damage. “For the fast evolvers, time matters, but they could also possibly be harmed; that’s why we need more data.”
A pitch for more data also came from Pooja Khatri, MD, who also spoke at the session. “There is a real tension now between personalizing the imaging and figuring out exactly the right patients against the time trade off for doing that. Some argue to keep it simple and move fast, and by doing that you’ll wash out any difference from doing more fancy stuff. Plus some places, even in developed countries, can’t afford the image-processing software” used in the DAWN and DEFUSE 3 trials. The correct approach remains unclear and has created “an area ripe for a trial,” declared Dr. Khatri, professor of neurology at director of acute stroke at the University of Cincinnati.
Dr. Hill has received honoraria from Merck and received research funding from Boehringer Ingelheim, Covidien, Medtronic, and Stryker. He has an ownership interest in Calgary Scientific and holds a patent on acute stroke triage methods. Dr. Nogueira has financial relationships with many companies. Dr. Lansberg and Dr. Fisher had no disclosures. Dr. Khatri has been a consultant to Lumosa and has received research funding from Cerenovus/Johnson & Johnson, Genentech, and Nervive.
HONOLULU – A little more than a year ago, results from the DAWN and DEFUSE 3 trials substantially broadened the time window for endovascular thrombectomy of acute ischemic stroke by selecting patients using brain imaging. Stroke clinicians are now trying to reconcile widespread, routine use of this life-changing treatment against an uncertain need to replicate the higher-end perfusion CT and analytical software imaging that these landmark trials used for patient selection. This has produced a schism in what experts advise for using endovascular thrombectomy on acute ischemic stroke patients.
“Go open the artery, people!” Michael D. Hill, MD, exhorted during a talk at the International Stroke Conference, sponsored by the American Heart Association. “Don’t get over-selective; more people will benefit than you think,” said Dr. Hill, a professor of clinical neurosciences at the University of Calgary (Alta.).
“We are over-selecting, and depriving patients,” commented Raul C. Nogueira, MD, professor of neurology at Emory University in Atlanta and a lead investigator of the DAWN trial, speaking from the audience during a discussion at the session where Dr. Hill spoke.
“The prevalence of treatable [acute ischemic stroke] patients is far higher than the prevalence of patients who are not good candidates, so you just want to exclude the ‘wipe-outs’; that’s what we do,” Dr. Hill explained. “Fortunately, endovascular therapy is very safe, and you’re not going to harm many patients. With other treatments [used routinely in medicine] some patients don’t benefit, but when you have a large effect size we use the treatment on almost everyone. The effect size from thrombectomy is so large it’s an argument to treat almost everyone, although the patients in the trials were selected by imaging.”
Dr. Hill repeatedly stressed that for most patients a non-contrast CT image is usually adequate to identify patients with salvageable brain tissue and a low risk for hemorrhage from intervention, and he endorsed also doing CT angiography to further inform the diagnosis. But he dismissed CT perfusion imaging as unnecessary. “Noncontrast CT and CT angiography are more than adequate to make treatment decisions,” he said. “The prevalence of poor collaterals is quite low, about 10%,” which means that about 90% of acute ischemic stroke patients will have more slowly progressing infarction,” making them amenable to treatment in an expanded time window and boosting the volume of salvageable tissue.
But these appeals for more liberal use of thrombectomy without the perfusion CT imaging used in DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21)and DEFUSE-3 (N Engl J Med. 2018 Feb 22;378[8]:708-18) received push back. Maarten G. Lansberg, MD, a co-investigator on the DEFUSE 3 trial, highlighted the speed and simplicity of CT perfusion imaging, and its utility in helping to better target thrombectomy to the right patients. It’s “speedy, simple, and safe,” it “excludes patients who will not benefit” from thrombectomy, and it helps when the patient’s history and noncontrast CT images are inconclusive, said Dr. Lansberg, a neurologist at Stanford (Calif.) University.
“Clinical presentation will only tell you so much.” With imaging that includes CT perfusion, “you can find out, in 5, 10 minutes, whether there is an occlusion, its location, the extent of dead tissue – that’s all really helpful,” said Marc Fisher, MD, professor of neurology at Harvard Medical School in Boston. “There is a tension now between doing treatment really fast and the concept of slow and fast evolvers. For slow evolvers, the concern about speed is irrelevant because it can take days” for their brains to have substantial damage. “For the fast evolvers, time matters, but they could also possibly be harmed; that’s why we need more data.”
A pitch for more data also came from Pooja Khatri, MD, who also spoke at the session. “There is a real tension now between personalizing the imaging and figuring out exactly the right patients against the time trade off for doing that. Some argue to keep it simple and move fast, and by doing that you’ll wash out any difference from doing more fancy stuff. Plus some places, even in developed countries, can’t afford the image-processing software” used in the DAWN and DEFUSE 3 trials. The correct approach remains unclear and has created “an area ripe for a trial,” declared Dr. Khatri, professor of neurology at director of acute stroke at the University of Cincinnati.
Dr. Hill has received honoraria from Merck and received research funding from Boehringer Ingelheim, Covidien, Medtronic, and Stryker. He has an ownership interest in Calgary Scientific and holds a patent on acute stroke triage methods. Dr. Nogueira has financial relationships with many companies. Dr. Lansberg and Dr. Fisher had no disclosures. Dr. Khatri has been a consultant to Lumosa and has received research funding from Cerenovus/Johnson & Johnson, Genentech, and Nervive.
HONOLULU – A little more than a year ago, results from the DAWN and DEFUSE 3 trials substantially broadened the time window for endovascular thrombectomy of acute ischemic stroke by selecting patients using brain imaging. Stroke clinicians are now trying to reconcile widespread, routine use of this life-changing treatment against an uncertain need to replicate the higher-end perfusion CT and analytical software imaging that these landmark trials used for patient selection. This has produced a schism in what experts advise for using endovascular thrombectomy on acute ischemic stroke patients.
“Go open the artery, people!” Michael D. Hill, MD, exhorted during a talk at the International Stroke Conference, sponsored by the American Heart Association. “Don’t get over-selective; more people will benefit than you think,” said Dr. Hill, a professor of clinical neurosciences at the University of Calgary (Alta.).
“We are over-selecting, and depriving patients,” commented Raul C. Nogueira, MD, professor of neurology at Emory University in Atlanta and a lead investigator of the DAWN trial, speaking from the audience during a discussion at the session where Dr. Hill spoke.
“The prevalence of treatable [acute ischemic stroke] patients is far higher than the prevalence of patients who are not good candidates, so you just want to exclude the ‘wipe-outs’; that’s what we do,” Dr. Hill explained. “Fortunately, endovascular therapy is very safe, and you’re not going to harm many patients. With other treatments [used routinely in medicine] some patients don’t benefit, but when you have a large effect size we use the treatment on almost everyone. The effect size from thrombectomy is so large it’s an argument to treat almost everyone, although the patients in the trials were selected by imaging.”
Dr. Hill repeatedly stressed that for most patients a non-contrast CT image is usually adequate to identify patients with salvageable brain tissue and a low risk for hemorrhage from intervention, and he endorsed also doing CT angiography to further inform the diagnosis. But he dismissed CT perfusion imaging as unnecessary. “Noncontrast CT and CT angiography are more than adequate to make treatment decisions,” he said. “The prevalence of poor collaterals is quite low, about 10%,” which means that about 90% of acute ischemic stroke patients will have more slowly progressing infarction,” making them amenable to treatment in an expanded time window and boosting the volume of salvageable tissue.
But these appeals for more liberal use of thrombectomy without the perfusion CT imaging used in DAWN (N Engl J Med. 2018 Jan 4;378[1]:11-21)and DEFUSE-3 (N Engl J Med. 2018 Feb 22;378[8]:708-18) received push back. Maarten G. Lansberg, MD, a co-investigator on the DEFUSE 3 trial, highlighted the speed and simplicity of CT perfusion imaging, and its utility in helping to better target thrombectomy to the right patients. It’s “speedy, simple, and safe,” it “excludes patients who will not benefit” from thrombectomy, and it helps when the patient’s history and noncontrast CT images are inconclusive, said Dr. Lansberg, a neurologist at Stanford (Calif.) University.
“Clinical presentation will only tell you so much.” With imaging that includes CT perfusion, “you can find out, in 5, 10 minutes, whether there is an occlusion, its location, the extent of dead tissue – that’s all really helpful,” said Marc Fisher, MD, professor of neurology at Harvard Medical School in Boston. “There is a tension now between doing treatment really fast and the concept of slow and fast evolvers. For slow evolvers, the concern about speed is irrelevant because it can take days” for their brains to have substantial damage. “For the fast evolvers, time matters, but they could also possibly be harmed; that’s why we need more data.”
A pitch for more data also came from Pooja Khatri, MD, who also spoke at the session. “There is a real tension now between personalizing the imaging and figuring out exactly the right patients against the time trade off for doing that. Some argue to keep it simple and move fast, and by doing that you’ll wash out any difference from doing more fancy stuff. Plus some places, even in developed countries, can’t afford the image-processing software” used in the DAWN and DEFUSE 3 trials. The correct approach remains unclear and has created “an area ripe for a trial,” declared Dr. Khatri, professor of neurology at director of acute stroke at the University of Cincinnati.
Dr. Hill has received honoraria from Merck and received research funding from Boehringer Ingelheim, Covidien, Medtronic, and Stryker. He has an ownership interest in Calgary Scientific and holds a patent on acute stroke triage methods. Dr. Nogueira has financial relationships with many companies. Dr. Lansberg and Dr. Fisher had no disclosures. Dr. Khatri has been a consultant to Lumosa and has received research funding from Cerenovus/Johnson & Johnson, Genentech, and Nervive.
REPORTING FROM ISC 2019
BP control slowed brain damage in elderly hypertensives
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
REPORTING FROM ACC 19
AUGUSTUS: Dual surpasses triple therapy when AFib patients have PCI or ACS
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
REPORTING FROM ACC 19
ACC, AHA release first cardiovascular disease primary prevention guideline
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
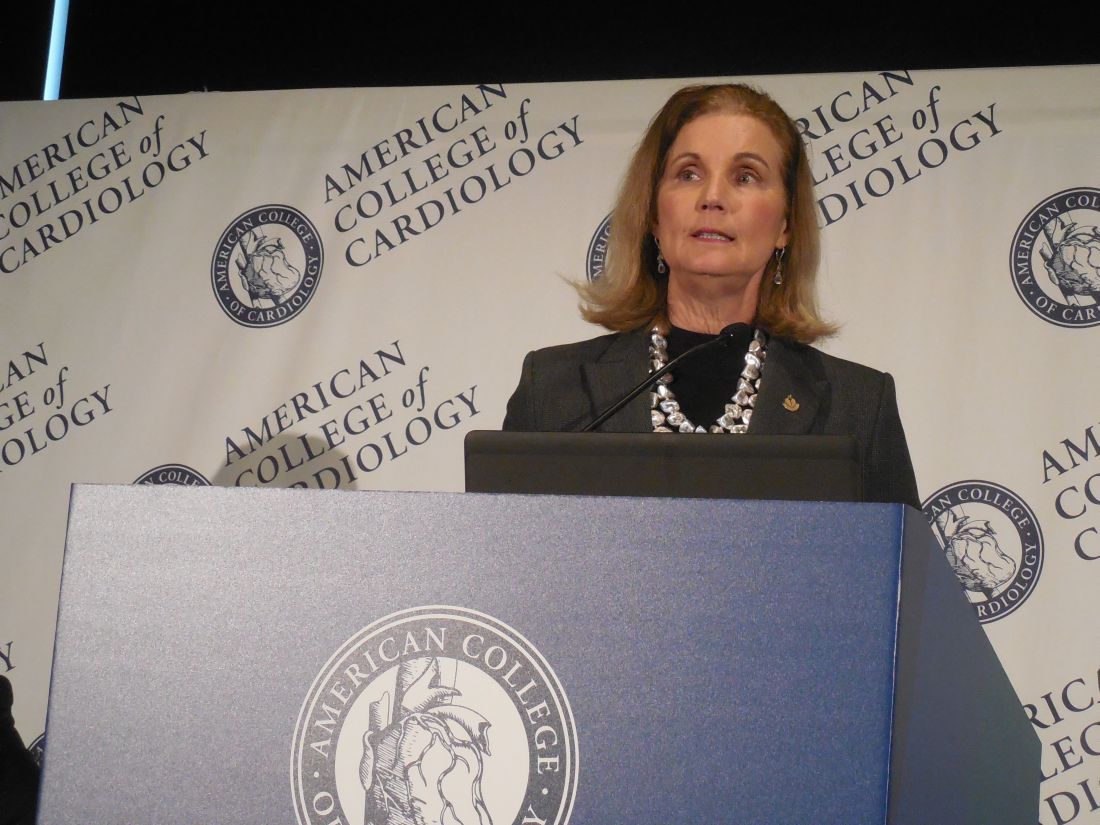
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.

“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.

“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.

“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
REPORTING FROM ACC 2019
Bempedoic acid safely dropped LDL, now seeks FDA approval
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
Key clinical point: Bempedoic acid safely lowed LDL cholesterol levels in a pivotal trial.
Major finding: In the intention-to-treat analysis, bempedoic acid cut LDL cholesterol by 18%; by 20% in an on-treatment analysis.
Study details: CLEAR Harmony, a multicenter, randomized trial with 2,230 patients.
Disclosures: CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
Sources: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
Second-generation hydrogel surpasses platinum for brain aneurysm closure
HONOLULU – A second-generation hydrogel coil that’s already approved for U.S. marketing proved superior to bare platinum wire for durably embolizing brain aneurysms in a multicenter, randomized trial with 600 patients.
For the study’s primary endpoint of recurrent intracranial aneurysm during follow-up as long as 18-24 months, the 297 patients treated with the hydrogel coil had a recurrence rate of 4%, compared with a 15% rate among patients treated with platinum wire, Bernard R. Bendok, MD, said at the International Stroke Conference sponsored by the American Heart Association. The hydrogel coil materials were also relatively easy to use – much easier than the first-generation hydrogel materials, according to Dr. Bendok – and the adverse event rate using the hydrogel coils was similar to the rate using platinum wire, the standard material for brain aneurysm embolization.
Given the similar safety and ease of use and superior efficacy, clinicians treating brain aneurysms may now increasingly use hydrogel coil. “I think these results will change practice. It’s compelling data,” Dr. Bendok predicted in an interview. “The problem with platinum is it is not conducive to healing.” When an aneurysm is “closed” by insertion of platinum wire, in reality most of the space within the aneurysm remains unfilled by metal. In contrast, animal models suggest that when hydrogel fills an aneurysm it forms a matrix for collagen deposition that further fills the aneurysm space in a wound-healing process, thereby making recurrence less likely, said Dr. Bendok, professor and chair of neurosurgery at the Mayo Clinic in Phoenix.
The HEAT (Hydrogel Endovascular Aneurysm Treatment) trial enrolled patients at 46 centers in the United States and Canada during June 2012–January 2016. Enrolled patients had a ruptured or unruptured brain aneurysm 3-14 mm in diameter, and averaged 57 years old. A blinded core laboratory reviewed brain scans to identify recurrent aneurysms. Of the 297 patients randomized to hydrogel coil treatment, 254 underwent follow-up at 3-12 months and 222 had additional follow-up at 18-24 months, the study’s prespecified time for the primary endpoint. Among 303 patients treated with platinum, 258 had follow-up after 3-12 months and 231 had follow-up at 18-24 months.
Among patients who entered the study with an unruptured aneurysm (nearly three-quarters of enrolled patients), the recurrence rate was 12% with platinum and 3% with hydrogel. Among the patients with a ruptured aneurysm, the recurrence rate was 24% with platinum and 8% with hydrogel. Adverse events occurred in 25% of those treated with platinum and 22% of those treated with hydrogel coil. Mortality during follow-up was 3% in the platinum arm and 2% in the hydrogel coil arm. The two groups also had similar outcomes as measured by the modified Rankin Scale and by quality-of-life measures.
HEAT was sponsored by MicroVention, the company that markets the tested hydrogel coil. Dr. Bendok had no personal disclosures.
SOURCE: Abi-Aad KR et al. ISC 2019, Abstract LB20.
HONOLULU – A second-generation hydrogel coil that’s already approved for U.S. marketing proved superior to bare platinum wire for durably embolizing brain aneurysms in a multicenter, randomized trial with 600 patients.
For the study’s primary endpoint of recurrent intracranial aneurysm during follow-up as long as 18-24 months, the 297 patients treated with the hydrogel coil had a recurrence rate of 4%, compared with a 15% rate among patients treated with platinum wire, Bernard R. Bendok, MD, said at the International Stroke Conference sponsored by the American Heart Association. The hydrogel coil materials were also relatively easy to use – much easier than the first-generation hydrogel materials, according to Dr. Bendok – and the adverse event rate using the hydrogel coils was similar to the rate using platinum wire, the standard material for brain aneurysm embolization.
Given the similar safety and ease of use and superior efficacy, clinicians treating brain aneurysms may now increasingly use hydrogel coil. “I think these results will change practice. It’s compelling data,” Dr. Bendok predicted in an interview. “The problem with platinum is it is not conducive to healing.” When an aneurysm is “closed” by insertion of platinum wire, in reality most of the space within the aneurysm remains unfilled by metal. In contrast, animal models suggest that when hydrogel fills an aneurysm it forms a matrix for collagen deposition that further fills the aneurysm space in a wound-healing process, thereby making recurrence less likely, said Dr. Bendok, professor and chair of neurosurgery at the Mayo Clinic in Phoenix.
The HEAT (Hydrogel Endovascular Aneurysm Treatment) trial enrolled patients at 46 centers in the United States and Canada during June 2012–January 2016. Enrolled patients had a ruptured or unruptured brain aneurysm 3-14 mm in diameter, and averaged 57 years old. A blinded core laboratory reviewed brain scans to identify recurrent aneurysms. Of the 297 patients randomized to hydrogel coil treatment, 254 underwent follow-up at 3-12 months and 222 had additional follow-up at 18-24 months, the study’s prespecified time for the primary endpoint. Among 303 patients treated with platinum, 258 had follow-up after 3-12 months and 231 had follow-up at 18-24 months.
Among patients who entered the study with an unruptured aneurysm (nearly three-quarters of enrolled patients), the recurrence rate was 12% with platinum and 3% with hydrogel. Among the patients with a ruptured aneurysm, the recurrence rate was 24% with platinum and 8% with hydrogel. Adverse events occurred in 25% of those treated with platinum and 22% of those treated with hydrogel coil. Mortality during follow-up was 3% in the platinum arm and 2% in the hydrogel coil arm. The two groups also had similar outcomes as measured by the modified Rankin Scale and by quality-of-life measures.
HEAT was sponsored by MicroVention, the company that markets the tested hydrogel coil. Dr. Bendok had no personal disclosures.
SOURCE: Abi-Aad KR et al. ISC 2019, Abstract LB20.
HONOLULU – A second-generation hydrogel coil that’s already approved for U.S. marketing proved superior to bare platinum wire for durably embolizing brain aneurysms in a multicenter, randomized trial with 600 patients.
For the study’s primary endpoint of recurrent intracranial aneurysm during follow-up as long as 18-24 months, the 297 patients treated with the hydrogel coil had a recurrence rate of 4%, compared with a 15% rate among patients treated with platinum wire, Bernard R. Bendok, MD, said at the International Stroke Conference sponsored by the American Heart Association. The hydrogel coil materials were also relatively easy to use – much easier than the first-generation hydrogel materials, according to Dr. Bendok – and the adverse event rate using the hydrogel coils was similar to the rate using platinum wire, the standard material for brain aneurysm embolization.
Given the similar safety and ease of use and superior efficacy, clinicians treating brain aneurysms may now increasingly use hydrogel coil. “I think these results will change practice. It’s compelling data,” Dr. Bendok predicted in an interview. “The problem with platinum is it is not conducive to healing.” When an aneurysm is “closed” by insertion of platinum wire, in reality most of the space within the aneurysm remains unfilled by metal. In contrast, animal models suggest that when hydrogel fills an aneurysm it forms a matrix for collagen deposition that further fills the aneurysm space in a wound-healing process, thereby making recurrence less likely, said Dr. Bendok, professor and chair of neurosurgery at the Mayo Clinic in Phoenix.
The HEAT (Hydrogel Endovascular Aneurysm Treatment) trial enrolled patients at 46 centers in the United States and Canada during June 2012–January 2016. Enrolled patients had a ruptured or unruptured brain aneurysm 3-14 mm in diameter, and averaged 57 years old. A blinded core laboratory reviewed brain scans to identify recurrent aneurysms. Of the 297 patients randomized to hydrogel coil treatment, 254 underwent follow-up at 3-12 months and 222 had additional follow-up at 18-24 months, the study’s prespecified time for the primary endpoint. Among 303 patients treated with platinum, 258 had follow-up after 3-12 months and 231 had follow-up at 18-24 months.
Among patients who entered the study with an unruptured aneurysm (nearly three-quarters of enrolled patients), the recurrence rate was 12% with platinum and 3% with hydrogel. Among the patients with a ruptured aneurysm, the recurrence rate was 24% with platinum and 8% with hydrogel. Adverse events occurred in 25% of those treated with platinum and 22% of those treated with hydrogel coil. Mortality during follow-up was 3% in the platinum arm and 2% in the hydrogel coil arm. The two groups also had similar outcomes as measured by the modified Rankin Scale and by quality-of-life measures.
HEAT was sponsored by MicroVention, the company that markets the tested hydrogel coil. Dr. Bendok had no personal disclosures.
SOURCE: Abi-Aad KR et al. ISC 2019, Abstract LB20.
REPORTING FROM ISC 2019
MI, strokes spike during 30 days after cancer diagnosis
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
HONOLULU – During the first month after a new cancer diagnosis, patients face a substantially elevated risk for an arterial thromboembolic event – an MI or stroke – consistent with the well-described increased risk newly diagnosed cancer patients face from venous thromboembolism, based on findings from a prospective study of more than 4,000 people.
In the new study, 836 patients newly diagnosed with cancer had a 480% increased rate of a fatal or nonfatal MI or stroke during the 30 days following their diagnosis, compared with 3,339 matched people without cancer and after adjustment for baseline differences in demographics and cardiovascular risk factors, Babak B. Navi, MD, said while presenting a poster at the International Stroke Conference sponsored by the American Heart Association.
An additional analysis that focused on 210 of the 836 patients with incident cancer who had any of seven of the cancers known to pose the highest venous thromboembolism risk (lymphoma; gynecologic cancer; or cancer of the pancreas, stomach, lung, bladder, or testes) showed an 1,750% greater rate of incident MI or stroke during the first 30 days after diagnosis, compared with matched people without cancer, reported Dr. Navi, chief of the stroke and hospital neurology at Weill Cornell Medicine, New York.
In contrast, during both the period 1-3 months after the cancer diagnosis and more than 3 months after, the rate of MI or stroke among recently diagnosed cancer patients was not significantly different from the rate in comparator individuals, although the data showed modest trends toward more arterial thromboembolic events after a month, and the lack of statistically significant differences may have been a power issue, Dr. Navi suggested.
The reasons for this acutely increased risk for arterial thromboembolic events, as well as the early spike in venous thromboembolic events, are not completely clear, but they likely result from factors released by tumors, effects from the drugs that patients receive for cancer treatment, stress, and interruption of antithrombotic treatment. Dr. Navi fingered cancer-induced hypercoagulability as likely the biggest culprit. It may now be reasonable to test the idea of treating newly diagnosed cancer patients with agents that could reduce their risk for MI or stroke, such as aspirin or a statin, he said in an interview.
The new analysis used data collected in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study, which during 2003-2007 enrolled more than 30,000 U.S. residents who were at least 45 years old. Dr. Navi and his associates used data collected from all REGARDS participants who developed incident cancer and had continuous Medicare coverage for at least 1 year before entering REGARDS, excluding those with cancer before enrollment. They used the Medicare records to identify the cancer diagnoses, and matched each of these people with four similar but cancer-free people enrolled in the study. Follow-up continued through September 2015. The average age of this REGARDS subgroup at enrollment was 72 years old, and nearly half were women. The incident cancers included 640 patients with a solid tumor, 71 with hematologic cancers, 13 with brain tumors, and 112 with an unknown primary cancer site.
Dr. Navi and his associates designed this study to validate previously reported findings of increased arterial thromboembolic events in newly diagnosed cancer patients from studies of insurance claims databases. Although the increased risk for venous thromboembolism in cancer patients is already well established, documenting a similar risk for arterial events is important because they are “generally more impactful for patients than venous thromboembolism,” Dr. Navi said.
REGARDS has received no commercial funding. Dr. Navi reported no disclosures.
SOURCE: Navi BB et al. Stroke. 2019 Feb;50(Suppl_1): Abstract WMP53.
REPORTING FROM ISC 2019
Higher blood pressure after thrombectomy links with bad stroke outcomes
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
HONOLULU – Acute ischemic stroke patients who underwent endovascular thrombectomy and then had a peak systolic blood pressure of greater than 158 mm Hg during the next 24 hours had worse 90-day outcomes than did patients whose peak systolic pressure remained at or below 158 mm Hg in a prospective, multicenter, observational study with 485 patients.
The results hint that maintaining a lower systolic blood pressure after thrombectomy in acute ischemic stroke patients may improve outcomes, but because the current study was observational, the hypothesis that patients benefit when treatment keeps their systolic pressure at or below 158 mm Hg must undergo testing in a prospective, randomized trial, Eva A. Mistry, MBBS, said at the International Stroke Conference, sponsored by the American Heart Association.
The finding from this study that 158 mm Hg provided the best dichotomous division between systolic blood pressures linked with good or bad outcomes is a first step toward trying to devise a more systematic and evidence-based approach to blood pressure management in acute ischemic stroke patients following endovascular thrombectomy, said Dr. Mistry, a neurologist at Vanderbilt University in Nashville, Tenn.
Neither Vanderbilt nor any of the other 11 major U.S. stroke centers that participated in the current study currently have an established protocol for blood pressure management after thrombectomy, Dr. Mistry said in an interview.
“We usually treat to reduce blood pressure, but we don’t have a [broadly agreed on] threshold” to trigger treatment. “It depends on a collective decision” by the various medical specialists who care for an individual acute stroke patient. In addition, no consensus yet exists for the best treatment strategy for blood pressure lowering in acute ischemic stroke patients. Intravenous nicardipine is often the top choice because it is fast-acting and easy to administer and control as an intravenous agent. Those same properties make the beta blocker labetalol a frequently used second drug, she said.
The BEST (Blood Pressure After Endovascular Stroke Therapy) study ran at 12 U.S. centers and enrolled 485 patients who underwent endovascular thrombectomy to treat an acute ischemic stroke. The patients averaged 69 years old, and 48% also underwent thrombolytic treatment. The study’s primary outcome was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after their stroke, an outcome reached by 39% of all patients in the study.
Statistical analysis of the collected data showed that a peak systolic blood pressure of 158 mm Hg reached during the 24 hours following thrombectomy best divided patients with good 90-day outcomes from those with worse outcomes. Patients with a postthrombectomy peak systolic pressure above 158 mm Hg had a 2.2-fold increased rate of having a modified Rankin Scale score of 3 or higher after 90 days, a statistically significant relationship, Dr. Mistry reported. However, in an analysis that also adjusted for age, baseline stroke severity, glucose level, time to reperfusion, ASPECTS score, history of hypertension, and recanalization status, the elevated risk for a bad outcome linked with higher systolic pressure dropped to 39% greater than that for patients with systolic pressures that did not rise above 158 mm Hg, a difference that was not statistically significant. This suggests that these adjustments were unable to account for all confounders and further highlighted the need for a prospective, randomized trial to test the value of controlling blood pressure following thrombectomy, Dr. Mistry said. The unadjusted results confirmed a prior report from Dr. Mistry and her associates that found a link between higher blood pressure after stroke thrombectomy and worse outcomes (J Am Heart Assoc. 2017 May 18. doi: 10.1161/JAHA.117.006167).
The analysis also showed that patients who were successfully recanalized by thrombectomy, achieving a thrombolysis in cerebral infarction (TICI) score of 2b or 3, had lower peak systolic blood pressures than did patients who failed to get this level of restored cerebral blood flow from thrombectomy.
BEST received no commercial funding. Dr. Mistry had no disclosures.
SOURCE: Mistry EA et al. Stroke. 2019 Feb;50(Suppl_1): Abstract 94.
REPORTING FROM ISC 2019