User login
Milk: Friend to bones, foe to faces?
ORLANDO – A greasy hamburger and fries and a chocolate milkshake may all earn the finger of blame when teens fret over acne. But which of these foods is the real culprit?
A growing body of data suggests it may be the milk – especially if it’s fat-free milk, according to Andrea Zaenglein, MD, who spoke at the annual meeting of the American Academy of Dermatology. Skim milk has been at the center of a long-simmering acne controversy, said Dr. Zaenglein, professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey.
The same association was seen in a subsequent study of 4,273 teen boys, published in 2008. There was a 10% increased risk for acne associated with intake of whole or 2% milk, a 17% increased risk for 1% milk, and a 19% increased risk for skim milk (J Am Acad Dermatol. 2008 May;58[5]: 787-93).
A prospective study of about 6,000 girls found similar risks associated with all types of milk: a 19% increased risk for whole milk, 17% for low-fat milk, and 19% for skim milk (Dermatol Online J. 2006 May 30;12[4]:1).
They found positive associations with total dairy and with nonfat dairy, but not with whole-fat or low-fat dairy. “The association was driven by the nonfat dairy,” Dr. Zaenglein said. “When we took nonfat [dairy] out of the total dairy, the association there was no longer significant.” They also found no significant association with body mass index, glycemic index, or glycemic load, she added.
“You have to wonder, what could this association between dairy – and skim milk in particular – be? Could dairy actually be involved in the pathogenesis of acne?” There are a number of proposed mechanisms, none of which have ever been confirmed, she said. “Could it be related to steroids? Milk is a very bioactive substance with estrogens and other hormones, but these are fat soluble and would be removed in skim milk.”
Another theory suggests that insulinlike growth factor-1, either in milk or endogenously stimulated by its consumption, may make a contribution. “People who are passionate about this have published prolifically about the activation of this pathway,” Dr. Zaenglein said, “but it remains speculative.”
She added, there are a plethora of studies showing milk’s benefits in many other areas, including the benefits exerted by milk’s medium-chain fatty acids on cardiovascular health, glycemic control, insulin regulation, and even obesity.
Finally, dairy’s importance to bone health in the United States can’t be ignored. In fact, dairy products are the most commonly recommended foods for ensuring adequate calcium intake in children, teens, and young adults.
“It’s really hard to make a firm recommendation to eliminate dairy, because, in this country, it makes up a good portion of the calcium teens need during their bone-building years, and kids are already at high risk for not meeting these requirements.”
National nutritional guidelines recommend 1,300 mg of calcium every day, which can be accomplished in three to five servings of dairy. “An 8-ounce glass of milk has 300 mg. Yogurt, cheese, and calcium-fortified juice are all highly accepted by teens. But, to get that same amount from vegetables, for example, you’d have to eat 3 cups of cooked kale. That’s a lot of kale,” Dr. Zaenglein said.
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
ORLANDO – A greasy hamburger and fries and a chocolate milkshake may all earn the finger of blame when teens fret over acne. But which of these foods is the real culprit?
A growing body of data suggests it may be the milk – especially if it’s fat-free milk, according to Andrea Zaenglein, MD, who spoke at the annual meeting of the American Academy of Dermatology. Skim milk has been at the center of a long-simmering acne controversy, said Dr. Zaenglein, professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey.
The same association was seen in a subsequent study of 4,273 teen boys, published in 2008. There was a 10% increased risk for acne associated with intake of whole or 2% milk, a 17% increased risk for 1% milk, and a 19% increased risk for skim milk (J Am Acad Dermatol. 2008 May;58[5]: 787-93).
A prospective study of about 6,000 girls found similar risks associated with all types of milk: a 19% increased risk for whole milk, 17% for low-fat milk, and 19% for skim milk (Dermatol Online J. 2006 May 30;12[4]:1).
They found positive associations with total dairy and with nonfat dairy, but not with whole-fat or low-fat dairy. “The association was driven by the nonfat dairy,” Dr. Zaenglein said. “When we took nonfat [dairy] out of the total dairy, the association there was no longer significant.” They also found no significant association with body mass index, glycemic index, or glycemic load, she added.
“You have to wonder, what could this association between dairy – and skim milk in particular – be? Could dairy actually be involved in the pathogenesis of acne?” There are a number of proposed mechanisms, none of which have ever been confirmed, she said. “Could it be related to steroids? Milk is a very bioactive substance with estrogens and other hormones, but these are fat soluble and would be removed in skim milk.”
Another theory suggests that insulinlike growth factor-1, either in milk or endogenously stimulated by its consumption, may make a contribution. “People who are passionate about this have published prolifically about the activation of this pathway,” Dr. Zaenglein said, “but it remains speculative.”
She added, there are a plethora of studies showing milk’s benefits in many other areas, including the benefits exerted by milk’s medium-chain fatty acids on cardiovascular health, glycemic control, insulin regulation, and even obesity.
Finally, dairy’s importance to bone health in the United States can’t be ignored. In fact, dairy products are the most commonly recommended foods for ensuring adequate calcium intake in children, teens, and young adults.
“It’s really hard to make a firm recommendation to eliminate dairy, because, in this country, it makes up a good portion of the calcium teens need during their bone-building years, and kids are already at high risk for not meeting these requirements.”
National nutritional guidelines recommend 1,300 mg of calcium every day, which can be accomplished in three to five servings of dairy. “An 8-ounce glass of milk has 300 mg. Yogurt, cheese, and calcium-fortified juice are all highly accepted by teens. But, to get that same amount from vegetables, for example, you’d have to eat 3 cups of cooked kale. That’s a lot of kale,” Dr. Zaenglein said.
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
ORLANDO – A greasy hamburger and fries and a chocolate milkshake may all earn the finger of blame when teens fret over acne. But which of these foods is the real culprit?
A growing body of data suggests it may be the milk – especially if it’s fat-free milk, according to Andrea Zaenglein, MD, who spoke at the annual meeting of the American Academy of Dermatology. Skim milk has been at the center of a long-simmering acne controversy, said Dr. Zaenglein, professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey.
The same association was seen in a subsequent study of 4,273 teen boys, published in 2008. There was a 10% increased risk for acne associated with intake of whole or 2% milk, a 17% increased risk for 1% milk, and a 19% increased risk for skim milk (J Am Acad Dermatol. 2008 May;58[5]: 787-93).
A prospective study of about 6,000 girls found similar risks associated with all types of milk: a 19% increased risk for whole milk, 17% for low-fat milk, and 19% for skim milk (Dermatol Online J. 2006 May 30;12[4]:1).
They found positive associations with total dairy and with nonfat dairy, but not with whole-fat or low-fat dairy. “The association was driven by the nonfat dairy,” Dr. Zaenglein said. “When we took nonfat [dairy] out of the total dairy, the association there was no longer significant.” They also found no significant association with body mass index, glycemic index, or glycemic load, she added.
“You have to wonder, what could this association between dairy – and skim milk in particular – be? Could dairy actually be involved in the pathogenesis of acne?” There are a number of proposed mechanisms, none of which have ever been confirmed, she said. “Could it be related to steroids? Milk is a very bioactive substance with estrogens and other hormones, but these are fat soluble and would be removed in skim milk.”
Another theory suggests that insulinlike growth factor-1, either in milk or endogenously stimulated by its consumption, may make a contribution. “People who are passionate about this have published prolifically about the activation of this pathway,” Dr. Zaenglein said, “but it remains speculative.”
She added, there are a plethora of studies showing milk’s benefits in many other areas, including the benefits exerted by milk’s medium-chain fatty acids on cardiovascular health, glycemic control, insulin regulation, and even obesity.
Finally, dairy’s importance to bone health in the United States can’t be ignored. In fact, dairy products are the most commonly recommended foods for ensuring adequate calcium intake in children, teens, and young adults.
“It’s really hard to make a firm recommendation to eliminate dairy, because, in this country, it makes up a good portion of the calcium teens need during their bone-building years, and kids are already at high risk for not meeting these requirements.”
National nutritional guidelines recommend 1,300 mg of calcium every day, which can be accomplished in three to five servings of dairy. “An 8-ounce glass of milk has 300 mg. Yogurt, cheese, and calcium-fortified juice are all highly accepted by teens. But, to get that same amount from vegetables, for example, you’d have to eat 3 cups of cooked kale. That’s a lot of kale,” Dr. Zaenglein said.
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
EXPERT ANALYSIS FROM AAD 17
Unavoidable, random DNA replication errors are the most common cancer drivers
Up to two-thirds of the mutations that drive human cancers may be due to DNA replication errors in normally dividing stem cells, not by inherited or environmentally induced mutations, according to a mathematical modeling study.
The proportion of replication error-driven mutations varied widely among 17 cancers analyzed, but the overall attributable risk of these errors was remarkably consistent among 69 countries included in the study, said Cristian Tomasetti, PhD, a coauthor of the paper and a biostatistician at Johns Hopkins University, Baltimore.
The findings should be a game-changer in the cancer field, Dr. Tomasetti said during a press briefing sponsored by the American Association for the Advancement of Science. Research dogma has long held that most cancers are related to lifestyle and environmental exposure, with a few primarily due to genetic factors.
“We have now determined that there is a third factor, and that it causes most of the mutations that drive cancer,” Dr. Tomasetti said. “We cannot ignore it and pretend it doesn’t exist. This is a complete paradigm shift in how we think of cancer and what causes it.”
The finding that 66% of cancer-driving mutations are based on unavoidable replication errors doesn’t challenge well-established epidemiology, said Dr. Tomasetti and his coauthor, Bert Vogelstein, MD. Rather, it fits perfectly with several key understandings of cancer: that about 40% of cases are preventable, that rapidly dividing tissues are more prone to develop cancers, and that cancer incidence rises exponentially as humans age.
“If we have as our starting point the assumption that 42% of cancers are preventable, we are completely consistent with that,” in finding that about 60% of cancers are unavoidable, Dr. Tomasetti said. “Those two numbers go perfectly together.”
The study also found that replication-error mutations (R) were most likely to drive cancers in tissues with rapid turnover, such as colorectal tissue. This makes intuitive sense, given that basal mutation rates hover at about three errors per cell replication cycle regardless of tissue type.
“The basal mutation rate in all cells is pretty even,” said Dr. Vogelstein, the Clayton Professor of Oncology and Pathology at John Hopkins University, Baltimore. “The difference is the number of stem cells. The more cells, the more divisions, and the more mistakes.”
R-mutations also contribute to age-related cancer incidence. As a person ages, more cell divisions accumulate, thus increasing the risk of a cancer-driving R-error. But these mutations also occur in children, who have rapid cell division in all their tissues. In fact, the colleagues suspect that R-errors are the main drivers of almost all pediatric cancers.
The new study bolsters the duo’s controversial 2015 work.
The theory sparked controversy among scholars and researchers. They challenged it on a number of technical fronts, from stem cell counts and division rates to charges that it didn’t adequately assess the interaction between R-mutations and environmental risks.
Some commentators, perceiving nihilism in the paper, expressed concern that clinicians and patients would get the idea that cancer prevention strategies were useless, since most cancers were simply a case of “bad luck.”
A pervading theme of these counter arguments was one familiar to any researcher: Correlation does not equal causation. The new study was an attempt to expand upon and strengthen the original findings, Dr. Tomasetti said.
“There are well-known environmental risk variations across the world, and there was a question of how our findings might change if we did this analysis in a different country. This paper is also the very first time that someone has ever looked at the proportions of mutations in each cancer type and assigned them to these factors.”
The new study employed a similar mathematical model, but comprised data from 423 cancer registries in 69 countries. The researchers examined the relationship between the lifetime risk of 17 cancers (including breast and prostate, which were not included in the 2015 study) and lifetime stem cell divisions for each tissue. The median correlation coefficient was 0.80; 89% of the countries examined had a correlation of greater than 0.70. This was “remarkably similar” to the correlation determined in the 2015 U.S.-only study.
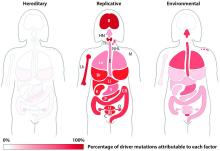
The team’s next step was to determine what fraction of cancer-driving mutations arose from R-errors, from environmental factors (E), and from hereditary factors (H). They examined these proportions in 32 different cancers in which environmental, lifestyle, and genetic factors have been thoroughly studied. Overall, 29% of the driver mutations were due to environment, 5% to heredity, and 66% to R-errors.
The proportions of these drivers did vary widely between the cancer types, the team noted. For example, lung and esophageal cancers and melanoma were primarily driven by environmental factors (more than 60% each). However, they wrote, “even in lung adenocarcinomas, R contributes a third of the total mutations, with tobacco smoke [including secondhand smoke], diet, radiation, and occupational exposures contributing the remainder. In cancers that are less strongly associated with environmental factors, such as those of the pancreas, brain, bone, or prostate, the majority of the mutations are attributable to R.”
During the press briefing, Dr. Tomasetti and Dr. Vogelstein stressed that most of the inevitable R-errors don’t precipitate cancer – and that even if they do increase risk, that risk may not ever trip the disease process.
“Most of the time these replicative mutations do no harm,” Dr Vogelstein said. “They occur in junk DNA genes, or in areas that are unimportant with respect to cancer. That’s the good luck. Occasionally, they occur in a cancer driver gene, and that is bad luck.”
But even a dose of bad luck isn’t enough to cause cancer. Most cancers require multiple hits to develop – which makes primary prevention strategies more important than ever, Dr. Tomasetti said.
“In the case of lung cancer, for instance, three or more mutations are needed. We showed that these mutations are caused by a combination of environment and R-errors. In theory, then, all of these cancers are preventable because if we can prevent even one of the environmentally caused mutations, then that patient won’t develop cancer.”
However, he said, some cancers do appear to be entirely driven by E-errors and, thus, appear entirely unavoidable. This is an extremely difficult area for clinicians and patients to navigate, said Dr. Vogelstein, a former pediatrician.
“We hope that understanding this will offer some comfort to the literally millions of patients who develop cancer despite having lead a near-perfect life,” in terms of managing risk factors. “Cancer develops in people who haven’t smoked, who avoided the sun and wore sunscreen, who eat perfectly healthy diets and exercise regularly. This is a particularly important concept for parents of children who have cancer, who think ‘I either transmitted a bad gene or unknowingly exposed my child to an environmental agent that caused their cancer.’ They need to understand that these cancers would have occurred no matter what they did.”
Dr. Tomasetti had no disclosures. Dr. Vogelstein is on the scientific advisory boards of Morphotek, Exelixis GP, and Sysmex Inostics, and is a founder of PapGene and Personal Genome Diagnostics.
[email protected]
On Twitter @Alz_gal
Up to two-thirds of the mutations that drive human cancers may be due to DNA replication errors in normally dividing stem cells, not by inherited or environmentally induced mutations, according to a mathematical modeling study.
The proportion of replication error-driven mutations varied widely among 17 cancers analyzed, but the overall attributable risk of these errors was remarkably consistent among 69 countries included in the study, said Cristian Tomasetti, PhD, a coauthor of the paper and a biostatistician at Johns Hopkins University, Baltimore.
The findings should be a game-changer in the cancer field, Dr. Tomasetti said during a press briefing sponsored by the American Association for the Advancement of Science. Research dogma has long held that most cancers are related to lifestyle and environmental exposure, with a few primarily due to genetic factors.
“We have now determined that there is a third factor, and that it causes most of the mutations that drive cancer,” Dr. Tomasetti said. “We cannot ignore it and pretend it doesn’t exist. This is a complete paradigm shift in how we think of cancer and what causes it.”
The finding that 66% of cancer-driving mutations are based on unavoidable replication errors doesn’t challenge well-established epidemiology, said Dr. Tomasetti and his coauthor, Bert Vogelstein, MD. Rather, it fits perfectly with several key understandings of cancer: that about 40% of cases are preventable, that rapidly dividing tissues are more prone to develop cancers, and that cancer incidence rises exponentially as humans age.
“If we have as our starting point the assumption that 42% of cancers are preventable, we are completely consistent with that,” in finding that about 60% of cancers are unavoidable, Dr. Tomasetti said. “Those two numbers go perfectly together.”
The study also found that replication-error mutations (R) were most likely to drive cancers in tissues with rapid turnover, such as colorectal tissue. This makes intuitive sense, given that basal mutation rates hover at about three errors per cell replication cycle regardless of tissue type.
“The basal mutation rate in all cells is pretty even,” said Dr. Vogelstein, the Clayton Professor of Oncology and Pathology at John Hopkins University, Baltimore. “The difference is the number of stem cells. The more cells, the more divisions, and the more mistakes.”
R-mutations also contribute to age-related cancer incidence. As a person ages, more cell divisions accumulate, thus increasing the risk of a cancer-driving R-error. But these mutations also occur in children, who have rapid cell division in all their tissues. In fact, the colleagues suspect that R-errors are the main drivers of almost all pediatric cancers.
The new study bolsters the duo’s controversial 2015 work.
The theory sparked controversy among scholars and researchers. They challenged it on a number of technical fronts, from stem cell counts and division rates to charges that it didn’t adequately assess the interaction between R-mutations and environmental risks.
Some commentators, perceiving nihilism in the paper, expressed concern that clinicians and patients would get the idea that cancer prevention strategies were useless, since most cancers were simply a case of “bad luck.”
A pervading theme of these counter arguments was one familiar to any researcher: Correlation does not equal causation. The new study was an attempt to expand upon and strengthen the original findings, Dr. Tomasetti said.
“There are well-known environmental risk variations across the world, and there was a question of how our findings might change if we did this analysis in a different country. This paper is also the very first time that someone has ever looked at the proportions of mutations in each cancer type and assigned them to these factors.”
The new study employed a similar mathematical model, but comprised data from 423 cancer registries in 69 countries. The researchers examined the relationship between the lifetime risk of 17 cancers (including breast and prostate, which were not included in the 2015 study) and lifetime stem cell divisions for each tissue. The median correlation coefficient was 0.80; 89% of the countries examined had a correlation of greater than 0.70. This was “remarkably similar” to the correlation determined in the 2015 U.S.-only study.
The team’s next step was to determine what fraction of cancer-driving mutations arose from R-errors, from environmental factors (E), and from hereditary factors (H). They examined these proportions in 32 different cancers in which environmental, lifestyle, and genetic factors have been thoroughly studied. Overall, 29% of the driver mutations were due to environment, 5% to heredity, and 66% to R-errors.
The proportions of these drivers did vary widely between the cancer types, the team noted. For example, lung and esophageal cancers and melanoma were primarily driven by environmental factors (more than 60% each). However, they wrote, “even in lung adenocarcinomas, R contributes a third of the total mutations, with tobacco smoke [including secondhand smoke], diet, radiation, and occupational exposures contributing the remainder. In cancers that are less strongly associated with environmental factors, such as those of the pancreas, brain, bone, or prostate, the majority of the mutations are attributable to R.”
During the press briefing, Dr. Tomasetti and Dr. Vogelstein stressed that most of the inevitable R-errors don’t precipitate cancer – and that even if they do increase risk, that risk may not ever trip the disease process.
“Most of the time these replicative mutations do no harm,” Dr Vogelstein said. “They occur in junk DNA genes, or in areas that are unimportant with respect to cancer. That’s the good luck. Occasionally, they occur in a cancer driver gene, and that is bad luck.”
But even a dose of bad luck isn’t enough to cause cancer. Most cancers require multiple hits to develop – which makes primary prevention strategies more important than ever, Dr. Tomasetti said.
“In the case of lung cancer, for instance, three or more mutations are needed. We showed that these mutations are caused by a combination of environment and R-errors. In theory, then, all of these cancers are preventable because if we can prevent even one of the environmentally caused mutations, then that patient won’t develop cancer.”
However, he said, some cancers do appear to be entirely driven by E-errors and, thus, appear entirely unavoidable. This is an extremely difficult area for clinicians and patients to navigate, said Dr. Vogelstein, a former pediatrician.
“We hope that understanding this will offer some comfort to the literally millions of patients who develop cancer despite having lead a near-perfect life,” in terms of managing risk factors. “Cancer develops in people who haven’t smoked, who avoided the sun and wore sunscreen, who eat perfectly healthy diets and exercise regularly. This is a particularly important concept for parents of children who have cancer, who think ‘I either transmitted a bad gene or unknowingly exposed my child to an environmental agent that caused their cancer.’ They need to understand that these cancers would have occurred no matter what they did.”
Dr. Tomasetti had no disclosures. Dr. Vogelstein is on the scientific advisory boards of Morphotek, Exelixis GP, and Sysmex Inostics, and is a founder of PapGene and Personal Genome Diagnostics.
[email protected]
On Twitter @Alz_gal
Up to two-thirds of the mutations that drive human cancers may be due to DNA replication errors in normally dividing stem cells, not by inherited or environmentally induced mutations, according to a mathematical modeling study.
The proportion of replication error-driven mutations varied widely among 17 cancers analyzed, but the overall attributable risk of these errors was remarkably consistent among 69 countries included in the study, said Cristian Tomasetti, PhD, a coauthor of the paper and a biostatistician at Johns Hopkins University, Baltimore.
The findings should be a game-changer in the cancer field, Dr. Tomasetti said during a press briefing sponsored by the American Association for the Advancement of Science. Research dogma has long held that most cancers are related to lifestyle and environmental exposure, with a few primarily due to genetic factors.
“We have now determined that there is a third factor, and that it causes most of the mutations that drive cancer,” Dr. Tomasetti said. “We cannot ignore it and pretend it doesn’t exist. This is a complete paradigm shift in how we think of cancer and what causes it.”
The finding that 66% of cancer-driving mutations are based on unavoidable replication errors doesn’t challenge well-established epidemiology, said Dr. Tomasetti and his coauthor, Bert Vogelstein, MD. Rather, it fits perfectly with several key understandings of cancer: that about 40% of cases are preventable, that rapidly dividing tissues are more prone to develop cancers, and that cancer incidence rises exponentially as humans age.
“If we have as our starting point the assumption that 42% of cancers are preventable, we are completely consistent with that,” in finding that about 60% of cancers are unavoidable, Dr. Tomasetti said. “Those two numbers go perfectly together.”
The study also found that replication-error mutations (R) were most likely to drive cancers in tissues with rapid turnover, such as colorectal tissue. This makes intuitive sense, given that basal mutation rates hover at about three errors per cell replication cycle regardless of tissue type.
“The basal mutation rate in all cells is pretty even,” said Dr. Vogelstein, the Clayton Professor of Oncology and Pathology at John Hopkins University, Baltimore. “The difference is the number of stem cells. The more cells, the more divisions, and the more mistakes.”
R-mutations also contribute to age-related cancer incidence. As a person ages, more cell divisions accumulate, thus increasing the risk of a cancer-driving R-error. But these mutations also occur in children, who have rapid cell division in all their tissues. In fact, the colleagues suspect that R-errors are the main drivers of almost all pediatric cancers.
The new study bolsters the duo’s controversial 2015 work.
The theory sparked controversy among scholars and researchers. They challenged it on a number of technical fronts, from stem cell counts and division rates to charges that it didn’t adequately assess the interaction between R-mutations and environmental risks.
Some commentators, perceiving nihilism in the paper, expressed concern that clinicians and patients would get the idea that cancer prevention strategies were useless, since most cancers were simply a case of “bad luck.”
A pervading theme of these counter arguments was one familiar to any researcher: Correlation does not equal causation. The new study was an attempt to expand upon and strengthen the original findings, Dr. Tomasetti said.
“There are well-known environmental risk variations across the world, and there was a question of how our findings might change if we did this analysis in a different country. This paper is also the very first time that someone has ever looked at the proportions of mutations in each cancer type and assigned them to these factors.”
The new study employed a similar mathematical model, but comprised data from 423 cancer registries in 69 countries. The researchers examined the relationship between the lifetime risk of 17 cancers (including breast and prostate, which were not included in the 2015 study) and lifetime stem cell divisions for each tissue. The median correlation coefficient was 0.80; 89% of the countries examined had a correlation of greater than 0.70. This was “remarkably similar” to the correlation determined in the 2015 U.S.-only study.
The team’s next step was to determine what fraction of cancer-driving mutations arose from R-errors, from environmental factors (E), and from hereditary factors (H). They examined these proportions in 32 different cancers in which environmental, lifestyle, and genetic factors have been thoroughly studied. Overall, 29% of the driver mutations were due to environment, 5% to heredity, and 66% to R-errors.
The proportions of these drivers did vary widely between the cancer types, the team noted. For example, lung and esophageal cancers and melanoma were primarily driven by environmental factors (more than 60% each). However, they wrote, “even in lung adenocarcinomas, R contributes a third of the total mutations, with tobacco smoke [including secondhand smoke], diet, radiation, and occupational exposures contributing the remainder. In cancers that are less strongly associated with environmental factors, such as those of the pancreas, brain, bone, or prostate, the majority of the mutations are attributable to R.”
During the press briefing, Dr. Tomasetti and Dr. Vogelstein stressed that most of the inevitable R-errors don’t precipitate cancer – and that even if they do increase risk, that risk may not ever trip the disease process.
“Most of the time these replicative mutations do no harm,” Dr Vogelstein said. “They occur in junk DNA genes, or in areas that are unimportant with respect to cancer. That’s the good luck. Occasionally, they occur in a cancer driver gene, and that is bad luck.”
But even a dose of bad luck isn’t enough to cause cancer. Most cancers require multiple hits to develop – which makes primary prevention strategies more important than ever, Dr. Tomasetti said.
“In the case of lung cancer, for instance, three or more mutations are needed. We showed that these mutations are caused by a combination of environment and R-errors. In theory, then, all of these cancers are preventable because if we can prevent even one of the environmentally caused mutations, then that patient won’t develop cancer.”
However, he said, some cancers do appear to be entirely driven by E-errors and, thus, appear entirely unavoidable. This is an extremely difficult area for clinicians and patients to navigate, said Dr. Vogelstein, a former pediatrician.
“We hope that understanding this will offer some comfort to the literally millions of patients who develop cancer despite having lead a near-perfect life,” in terms of managing risk factors. “Cancer develops in people who haven’t smoked, who avoided the sun and wore sunscreen, who eat perfectly healthy diets and exercise regularly. This is a particularly important concept for parents of children who have cancer, who think ‘I either transmitted a bad gene or unknowingly exposed my child to an environmental agent that caused their cancer.’ They need to understand that these cancers would have occurred no matter what they did.”
Dr. Tomasetti had no disclosures. Dr. Vogelstein is on the scientific advisory boards of Morphotek, Exelixis GP, and Sysmex Inostics, and is a founder of PapGene and Personal Genome Diagnostics.
[email protected]
On Twitter @Alz_gal
Key clinical point:
Major finding: Two-thirds (66%) of cancer drivers are replication errors, 29% are environmentally induced, and 5% are hereditary.
Data source: The researchers examined cancer mutation drivers in two cohorts that spanned 69 countries.
Disclosures: Dr. Tomasetti had no disclosures. Dr. Vogelstein is on the scientific advisory boards of Morphotek, Exelixis GP, and Sysmex Inostics, and is a founder of PapGene and Personal Genome Diagnostics.
For Latinos, misperceptions and lack of medical care make preventing melanoma risky business
ORLANDO – Ignorance and exposure are teaming up to put Latinos in the bull’s-eye of skin cancer.
Many believe that they are not at risk for either melanoma or nonmelanoma skin cancers – and too often, their physicians believe the same, Maritza Perez, MD, said at the annual meeting of the American Academy of Dermatology. Because of such incorrect perceptions, Latino patients get little counseling about risky behaviors, and so their exposure to those dangers continues unabated.
“The behavior of many Hispanic patients is very risky,” said Dr. Perez, a clinical professor of dermatology, at Mount Sinai Medical Center, New York. “They don’t wear sunscreen. They don’t do skin self-exams. They use tanning beds. And because of these beliefs, they don’t educate their children about sun safety.”
A research letter published in the Journal of the American Academy of Dermatology in 2011 broke down levels of skin cancer awareness by race and ethnicity among 165 whites, Hispanics, blacks, and Asians surveyed in New York City (64[1]:198-200). Compared with whites, Hispanics were significantly less likely to have ever had a doctor perform a full body skin exam (21% vs. 61%) or to have performed a self-exam (37% vs. 54%). Significantly fewer believed that skin cancer could occur in darker skin (78% vs. 91%). Only 8% had heard of the ABCDs of early melanoma detection, compared with 27% of whites. And about half as many Hispanics said they wore sunscreen (55% vs. 96%).
Unfortunately, Dr. Perez said, doctors aren’t correcting these misperceptions. Many physicians display a similar lack of understanding. They may correctly believe that the risk for skin cancer is less among Hispanics than it is among whites overall, but fail to communicate individual risk.
What these physicians may not understand, Dr. Perez said, is that the Hispanic population comprises an incredible variety of ethnic backgrounds. The population’s centuries-long genetic mixing bowl means there is no “typical” Hispanic skin. Instead, it includes every Fitzpatrick skin type, from fair-skinned redheads to the darkest brown and black skins.
Inadequate healthcare access exerts yet another damaging force. Like other ethnic minorities, many Hispanic patients lack insurance or adequate access to medical care. Instead of seeking regular primary care that would include skin cancer screenings, they tend to rely on urgent care or emergency departments to address emergent health issues, Dr. Perez said. When primary and preventive care falls by the wayside, melanomas that could be diagnosed at a curable stage invariably progress.
“We know that the only way of curing melanoma is with a scalpel. And the only way to remove it is by treating early disease. We’re not doing that. Our melanoma patients are diagnosed at younger ages with more advanced disease with more lymph node involvement than Caucasians, so there is also more mortality. We achieve early-stage diagnosis in 91% of Caucasians, but only 74% of Hispanics.”
A 2011 paper on racial and ethnic variations in the incidence and survival of melanoma, based on national cancer registry data covering almost 70% of the U.S. population, from 1999-2006, provided more information on the differences between the white and Hispanic populations (J Am Acad Dermatol. 2011 Nov;65[5 Suppl 1]:S26-37). Compared with non-Hispanic whites, Hispanics presented with thicker tumors (more than 1 mm, 35% vs. 25%), more regional involvement (12% vs. 8%), and more distant metastasis (7% vs. 4%).
Because adult Hispanic patients lack knowledge about their melanoma risk, they aren’t improving the outlook for their children, Dr. Perez said. The Hispanic demographic in the United States is already a young one. According on 2014 data cited by the Pew Research Center, 58% of Hispanics in the United States are aged 33 years or younger; 32% are younger than 18 years.
These young people are already endangering their health with unsafe sun behavior, Dr. Perez said. A 2007 study surveyed 369 white Hispanic and white non-Hispanic high school students in Miami about sun protection behaviors and skin cancer risk. The Hispanic teens were 2.5 times more likely to have used a tanning bed in the previous year; they were also less likely to wear sunscreen and protective clothing. The Hispanic students generally believed they were less likely to get skin cancer than the Caucasian students. They were 60% less likely to have heard of a skin self-exam and 70% less likely to have been told how to do one (Arch Dermatol. 2007;143[8]:983-8).
The oil to calm these troubled waters is education, Dr. Perez said. She takes this commitment very seriously, and said a simple conversation is the first step.
“I tell all my patients, no matter what ethnicity you are or what skin type you have, you can get skin cancer and you need regular, complete skin exams. And I teach them to do this for themselves.”
A senior vice-president for the Skin Cancer Foundation, Dr. Perez is coauthor of “Understanding Melanoma: What You Need to Know,” which is now in its fifth edition.
The book, originally published in 1996, is aimed at melanoma patients and their families. It covers the four types of melanoma and their causes and risk factors. Information on melanoma diagnosis, staging, treatment options, prognosis, and hereditary and genetic factors is also included, as well as guidelines for prevention.
The updated edition contains information on the latest immunotherapy and genetically targeted treatments, including ipilimumab (Yervoy), pembrolizumab (Keytruda), nivolumab (Opdivo), vemurafenib (Zelboraf), dabrafenib (Tafinlar) and trametinib (Mekinist). The book is available for download for a nominal fee.
She has also committed to educating physicians about the issue.
“If we want to decrease the incidence of melanoma in Latinos, decrease the tumor depth at diagnosis and bring down the higher mortality, we have to first educate the doctors who are taking care of these patients and correct the message delivered to Latinos by telling them that they are as prone to skin cancer as Caucasians. We simply have to get the message across that, just like everyone else, they need protection from the sun by applying sunblocks, using sunglasses, and covering their bodies with sun-protective clothing and large-rim hats. And we have to make medical care more accessible so that these people can be diagnosed and saved. This is what we need to do now. But I don’t know how many decades it will take to turn the tables.”
Dr. Perez had no disclosures relevant to her lecture.
[email protected]
On Twitter @Alz_Gal
ORLANDO – Ignorance and exposure are teaming up to put Latinos in the bull’s-eye of skin cancer.
Many believe that they are not at risk for either melanoma or nonmelanoma skin cancers – and too often, their physicians believe the same, Maritza Perez, MD, said at the annual meeting of the American Academy of Dermatology. Because of such incorrect perceptions, Latino patients get little counseling about risky behaviors, and so their exposure to those dangers continues unabated.
“The behavior of many Hispanic patients is very risky,” said Dr. Perez, a clinical professor of dermatology, at Mount Sinai Medical Center, New York. “They don’t wear sunscreen. They don’t do skin self-exams. They use tanning beds. And because of these beliefs, they don’t educate their children about sun safety.”
A research letter published in the Journal of the American Academy of Dermatology in 2011 broke down levels of skin cancer awareness by race and ethnicity among 165 whites, Hispanics, blacks, and Asians surveyed in New York City (64[1]:198-200). Compared with whites, Hispanics were significantly less likely to have ever had a doctor perform a full body skin exam (21% vs. 61%) or to have performed a self-exam (37% vs. 54%). Significantly fewer believed that skin cancer could occur in darker skin (78% vs. 91%). Only 8% had heard of the ABCDs of early melanoma detection, compared with 27% of whites. And about half as many Hispanics said they wore sunscreen (55% vs. 96%).
Unfortunately, Dr. Perez said, doctors aren’t correcting these misperceptions. Many physicians display a similar lack of understanding. They may correctly believe that the risk for skin cancer is less among Hispanics than it is among whites overall, but fail to communicate individual risk.
What these physicians may not understand, Dr. Perez said, is that the Hispanic population comprises an incredible variety of ethnic backgrounds. The population’s centuries-long genetic mixing bowl means there is no “typical” Hispanic skin. Instead, it includes every Fitzpatrick skin type, from fair-skinned redheads to the darkest brown and black skins.
Inadequate healthcare access exerts yet another damaging force. Like other ethnic minorities, many Hispanic patients lack insurance or adequate access to medical care. Instead of seeking regular primary care that would include skin cancer screenings, they tend to rely on urgent care or emergency departments to address emergent health issues, Dr. Perez said. When primary and preventive care falls by the wayside, melanomas that could be diagnosed at a curable stage invariably progress.
“We know that the only way of curing melanoma is with a scalpel. And the only way to remove it is by treating early disease. We’re not doing that. Our melanoma patients are diagnosed at younger ages with more advanced disease with more lymph node involvement than Caucasians, so there is also more mortality. We achieve early-stage diagnosis in 91% of Caucasians, but only 74% of Hispanics.”
A 2011 paper on racial and ethnic variations in the incidence and survival of melanoma, based on national cancer registry data covering almost 70% of the U.S. population, from 1999-2006, provided more information on the differences between the white and Hispanic populations (J Am Acad Dermatol. 2011 Nov;65[5 Suppl 1]:S26-37). Compared with non-Hispanic whites, Hispanics presented with thicker tumors (more than 1 mm, 35% vs. 25%), more regional involvement (12% vs. 8%), and more distant metastasis (7% vs. 4%).
Because adult Hispanic patients lack knowledge about their melanoma risk, they aren’t improving the outlook for their children, Dr. Perez said. The Hispanic demographic in the United States is already a young one. According on 2014 data cited by the Pew Research Center, 58% of Hispanics in the United States are aged 33 years or younger; 32% are younger than 18 years.
These young people are already endangering their health with unsafe sun behavior, Dr. Perez said. A 2007 study surveyed 369 white Hispanic and white non-Hispanic high school students in Miami about sun protection behaviors and skin cancer risk. The Hispanic teens were 2.5 times more likely to have used a tanning bed in the previous year; they were also less likely to wear sunscreen and protective clothing. The Hispanic students generally believed they were less likely to get skin cancer than the Caucasian students. They were 60% less likely to have heard of a skin self-exam and 70% less likely to have been told how to do one (Arch Dermatol. 2007;143[8]:983-8).
The oil to calm these troubled waters is education, Dr. Perez said. She takes this commitment very seriously, and said a simple conversation is the first step.
“I tell all my patients, no matter what ethnicity you are or what skin type you have, you can get skin cancer and you need regular, complete skin exams. And I teach them to do this for themselves.”
A senior vice-president for the Skin Cancer Foundation, Dr. Perez is coauthor of “Understanding Melanoma: What You Need to Know,” which is now in its fifth edition.
The book, originally published in 1996, is aimed at melanoma patients and their families. It covers the four types of melanoma and their causes and risk factors. Information on melanoma diagnosis, staging, treatment options, prognosis, and hereditary and genetic factors is also included, as well as guidelines for prevention.
The updated edition contains information on the latest immunotherapy and genetically targeted treatments, including ipilimumab (Yervoy), pembrolizumab (Keytruda), nivolumab (Opdivo), vemurafenib (Zelboraf), dabrafenib (Tafinlar) and trametinib (Mekinist). The book is available for download for a nominal fee.
She has also committed to educating physicians about the issue.
“If we want to decrease the incidence of melanoma in Latinos, decrease the tumor depth at diagnosis and bring down the higher mortality, we have to first educate the doctors who are taking care of these patients and correct the message delivered to Latinos by telling them that they are as prone to skin cancer as Caucasians. We simply have to get the message across that, just like everyone else, they need protection from the sun by applying sunblocks, using sunglasses, and covering their bodies with sun-protective clothing and large-rim hats. And we have to make medical care more accessible so that these people can be diagnosed and saved. This is what we need to do now. But I don’t know how many decades it will take to turn the tables.”
Dr. Perez had no disclosures relevant to her lecture.
[email protected]
On Twitter @Alz_Gal
ORLANDO – Ignorance and exposure are teaming up to put Latinos in the bull’s-eye of skin cancer.
Many believe that they are not at risk for either melanoma or nonmelanoma skin cancers – and too often, their physicians believe the same, Maritza Perez, MD, said at the annual meeting of the American Academy of Dermatology. Because of such incorrect perceptions, Latino patients get little counseling about risky behaviors, and so their exposure to those dangers continues unabated.
“The behavior of many Hispanic patients is very risky,” said Dr. Perez, a clinical professor of dermatology, at Mount Sinai Medical Center, New York. “They don’t wear sunscreen. They don’t do skin self-exams. They use tanning beds. And because of these beliefs, they don’t educate their children about sun safety.”
A research letter published in the Journal of the American Academy of Dermatology in 2011 broke down levels of skin cancer awareness by race and ethnicity among 165 whites, Hispanics, blacks, and Asians surveyed in New York City (64[1]:198-200). Compared with whites, Hispanics were significantly less likely to have ever had a doctor perform a full body skin exam (21% vs. 61%) or to have performed a self-exam (37% vs. 54%). Significantly fewer believed that skin cancer could occur in darker skin (78% vs. 91%). Only 8% had heard of the ABCDs of early melanoma detection, compared with 27% of whites. And about half as many Hispanics said they wore sunscreen (55% vs. 96%).
Unfortunately, Dr. Perez said, doctors aren’t correcting these misperceptions. Many physicians display a similar lack of understanding. They may correctly believe that the risk for skin cancer is less among Hispanics than it is among whites overall, but fail to communicate individual risk.
What these physicians may not understand, Dr. Perez said, is that the Hispanic population comprises an incredible variety of ethnic backgrounds. The population’s centuries-long genetic mixing bowl means there is no “typical” Hispanic skin. Instead, it includes every Fitzpatrick skin type, from fair-skinned redheads to the darkest brown and black skins.
Inadequate healthcare access exerts yet another damaging force. Like other ethnic minorities, many Hispanic patients lack insurance or adequate access to medical care. Instead of seeking regular primary care that would include skin cancer screenings, they tend to rely on urgent care or emergency departments to address emergent health issues, Dr. Perez said. When primary and preventive care falls by the wayside, melanomas that could be diagnosed at a curable stage invariably progress.
“We know that the only way of curing melanoma is with a scalpel. And the only way to remove it is by treating early disease. We’re not doing that. Our melanoma patients are diagnosed at younger ages with more advanced disease with more lymph node involvement than Caucasians, so there is also more mortality. We achieve early-stage diagnosis in 91% of Caucasians, but only 74% of Hispanics.”
A 2011 paper on racial and ethnic variations in the incidence and survival of melanoma, based on national cancer registry data covering almost 70% of the U.S. population, from 1999-2006, provided more information on the differences between the white and Hispanic populations (J Am Acad Dermatol. 2011 Nov;65[5 Suppl 1]:S26-37). Compared with non-Hispanic whites, Hispanics presented with thicker tumors (more than 1 mm, 35% vs. 25%), more regional involvement (12% vs. 8%), and more distant metastasis (7% vs. 4%).
Because adult Hispanic patients lack knowledge about their melanoma risk, they aren’t improving the outlook for their children, Dr. Perez said. The Hispanic demographic in the United States is already a young one. According on 2014 data cited by the Pew Research Center, 58% of Hispanics in the United States are aged 33 years or younger; 32% are younger than 18 years.
These young people are already endangering their health with unsafe sun behavior, Dr. Perez said. A 2007 study surveyed 369 white Hispanic and white non-Hispanic high school students in Miami about sun protection behaviors and skin cancer risk. The Hispanic teens were 2.5 times more likely to have used a tanning bed in the previous year; they were also less likely to wear sunscreen and protective clothing. The Hispanic students generally believed they were less likely to get skin cancer than the Caucasian students. They were 60% less likely to have heard of a skin self-exam and 70% less likely to have been told how to do one (Arch Dermatol. 2007;143[8]:983-8).
The oil to calm these troubled waters is education, Dr. Perez said. She takes this commitment very seriously, and said a simple conversation is the first step.
“I tell all my patients, no matter what ethnicity you are or what skin type you have, you can get skin cancer and you need regular, complete skin exams. And I teach them to do this for themselves.”
A senior vice-president for the Skin Cancer Foundation, Dr. Perez is coauthor of “Understanding Melanoma: What You Need to Know,” which is now in its fifth edition.
The book, originally published in 1996, is aimed at melanoma patients and their families. It covers the four types of melanoma and their causes and risk factors. Information on melanoma diagnosis, staging, treatment options, prognosis, and hereditary and genetic factors is also included, as well as guidelines for prevention.
The updated edition contains information on the latest immunotherapy and genetically targeted treatments, including ipilimumab (Yervoy), pembrolizumab (Keytruda), nivolumab (Opdivo), vemurafenib (Zelboraf), dabrafenib (Tafinlar) and trametinib (Mekinist). The book is available for download for a nominal fee.
She has also committed to educating physicians about the issue.
“If we want to decrease the incidence of melanoma in Latinos, decrease the tumor depth at diagnosis and bring down the higher mortality, we have to first educate the doctors who are taking care of these patients and correct the message delivered to Latinos by telling them that they are as prone to skin cancer as Caucasians. We simply have to get the message across that, just like everyone else, they need protection from the sun by applying sunblocks, using sunglasses, and covering their bodies with sun-protective clothing and large-rim hats. And we have to make medical care more accessible so that these people can be diagnosed and saved. This is what we need to do now. But I don’t know how many decades it will take to turn the tables.”
Dr. Perez had no disclosures relevant to her lecture.
[email protected]
On Twitter @Alz_Gal
EXPERT ANALYSIS FROM AAD 17
Antioxidants plus sunscreens may be two-punch knockout for melasma
ORLANDO – A two-step regimen of high-potency topical antioxidants followed by a mineral-based sunscreen may help repair light-induced skin damage and protect against new damage in patients with melasma.
Recent studies suggest that the antioxidants tamp down inflammatory cytokines and damage of oxidative stress, Maria Ivonne Arellano-Mendoza, MD, said during a special focus session on Latino skin held at the annual meeting of the American Academy of Dermatology.
“Many compounds are being studied for this purpose,” said Dr. Arellano-Mendoza, head of the dermatology department of the General Hospital of Mexico, Mexico City. “One combination is vitamin C, vitamin E, ubiquinone, and grape-seed extract. This effectively prevented infrared-A radiation–induced matrix metalloproteinase-1 messenger RNA expression in human skin. This combination can be found now in some sunscreens and daily care products.”
Another effective combination seems to be a mixture of ferulic acid, tocopherol, and vitamin C, she said.
The two-step process of regularly using a topical product with antioxidants before applying a sunscreen is all there is for now, she added, because so far it’s been impossible to combine the agents in a single product.
“The challenge will be how to create a product that stays on the surface of the skin to protect it from light, while liberating the antioxidants to penetrate the skin,” she commented.
The antioxidants’ benefits, however, will be obliterated by the continued effects of some light wavelengths that aggravate melasma unless they are used in sequence with a light-scattering sunscreen.
Sunscreens are critical components of a melasma treatment regimen, Dr. Arellano-Mendoza said. “Sunscreens are a cornerstone of treatment. We clearly tell our patients that sunscreens have to be used every day, forever, and if they are not used properly, they will have no improvement.”
Patients with hyperpigmentation disorders are susceptible to longer wavelengths that aren’t covered by chemically derived sunscreens. Longer wavelengths, including infrared light and visible light, have been shown to increase expression of matrix metalloproteinase (MMP) -1 and -9, decrease expression of type 1 procollagen, and can induce macrophage infiltration. These wavelengths also increase reactive oxygen species and proinflammatory cytokines in vitro, Dr. Arellano-Mendoza noted.
Visible light can cause erythema, transient and long-lasting hyperpigmentation, thermal damage, free radical production, and premature photoaging. It also can stimulate the production of reactive oxygen species that can damage DNA.
Mineral-based, inorganic sunscreens, however – like those with titanium dioxide, zinc oxide, and iron oxide – scatter all wavelengths.
“These micronized forms of metal oxides not only scatter and reflect light, they also absorb ultraviolet radiation. The compounds aren’t new,” she said. In 1991, Dr. Elaine Kaye of Harvard University, Boston, and associates described (Arch Dermatol. 1991;127:351-5) opaque physical sunscreens that were useful blockers of visible light and found that transmittance of light can be lowered by adding iron oxide, Dr. Arellano-Mendoza pointed out.
The inorganic sunscreens have never been widely adopted because they are highly pigmented with white or, in the case of iron oxide, with red. “Not many people accepted [the iron-containing compounds] because of the redness, but now different shades are going to be hitting the market soon,” and the hope is that consumers will find them more appealing, she said.
This is good news, as the data emerging around iron oxide are intriguingly positive. A 2015 study showed that a sunscreen with iron oxides prevented melasma relapse during the summer months. Patients were randomized to the same ultraviolet filter topical sunscreen, but for one group, micronized iron oxide was added to it. After 6 months, the median melasma area severity index score was significantly better in the group using the iron oxide compound (J Am Acad Dermatol. 2015 Jan;72[1]:189-90.e1).
Support for the two-step regimen appeared in 2014, when a small study randomized 30 healthy volunteers to an SPF 30 sunscreen or the same sunscreen supplemented with an antioxidant cocktail of grape seed extract, vitamin E, ubiquinone, and vitamin C. The endpoint was MMP-1 upregulation after exposure to infrared-A light. Skin treated with the combination regimen showed significantly lower MMP-1 activation, leading the authors to conclude that the combination of topical antioxidants conferred protection against the irradiation (Photochem Photobiol. 2015 Jan-Feb;91[1]:248-50).
Those same authors published a companion article (Photodermatol Photoimmunol Photomed. 2014;30:167-74) suggesting that another antioxidant mixture (ferulic acid, tocopherol, and vitamin C) was similarly effective.
Using a combination of antioxidants is important, Dr. Arellano-Mendoza said, because different antioxidants work differently. Some (catalase, glutathione peroxidase, and superoxide dismutase) are enzymatic, catalyzing reactions that convert free radicals to oxygen and water. Others terminate free radicals by preventing the propagation of oxidative chain reactions (vitamins A and C, flavonoids, uric acid, bilirubin, albumin, and members of the thiol group). A third group consists of metal-binding proteins that sequester free iron or copper to prevent free radical production (ferritin, transferrin, lactoferrin, and ceruloplasmin).
“I think we can now consider antioxidants a part of the tools we use in treating some pigmentary disorders as melasma,” she said. “We need to choose the compounds carefully, and we definitely need more in vivo research, but the findings are very encouraging.”
Dr. Arellano-Mendoza had no relevant financial disclosures.
This article was updated 3/20/17.
[email protected]
On Twitter @Alz_Gal
ORLANDO – A two-step regimen of high-potency topical antioxidants followed by a mineral-based sunscreen may help repair light-induced skin damage and protect against new damage in patients with melasma.
Recent studies suggest that the antioxidants tamp down inflammatory cytokines and damage of oxidative stress, Maria Ivonne Arellano-Mendoza, MD, said during a special focus session on Latino skin held at the annual meeting of the American Academy of Dermatology.
“Many compounds are being studied for this purpose,” said Dr. Arellano-Mendoza, head of the dermatology department of the General Hospital of Mexico, Mexico City. “One combination is vitamin C, vitamin E, ubiquinone, and grape-seed extract. This effectively prevented infrared-A radiation–induced matrix metalloproteinase-1 messenger RNA expression in human skin. This combination can be found now in some sunscreens and daily care products.”
Another effective combination seems to be a mixture of ferulic acid, tocopherol, and vitamin C, she said.
The two-step process of regularly using a topical product with antioxidants before applying a sunscreen is all there is for now, she added, because so far it’s been impossible to combine the agents in a single product.
“The challenge will be how to create a product that stays on the surface of the skin to protect it from light, while liberating the antioxidants to penetrate the skin,” she commented.
The antioxidants’ benefits, however, will be obliterated by the continued effects of some light wavelengths that aggravate melasma unless they are used in sequence with a light-scattering sunscreen.
Sunscreens are critical components of a melasma treatment regimen, Dr. Arellano-Mendoza said. “Sunscreens are a cornerstone of treatment. We clearly tell our patients that sunscreens have to be used every day, forever, and if they are not used properly, they will have no improvement.”
Patients with hyperpigmentation disorders are susceptible to longer wavelengths that aren’t covered by chemically derived sunscreens. Longer wavelengths, including infrared light and visible light, have been shown to increase expression of matrix metalloproteinase (MMP) -1 and -9, decrease expression of type 1 procollagen, and can induce macrophage infiltration. These wavelengths also increase reactive oxygen species and proinflammatory cytokines in vitro, Dr. Arellano-Mendoza noted.
Visible light can cause erythema, transient and long-lasting hyperpigmentation, thermal damage, free radical production, and premature photoaging. It also can stimulate the production of reactive oxygen species that can damage DNA.
Mineral-based, inorganic sunscreens, however – like those with titanium dioxide, zinc oxide, and iron oxide – scatter all wavelengths.
“These micronized forms of metal oxides not only scatter and reflect light, they also absorb ultraviolet radiation. The compounds aren’t new,” she said. In 1991, Dr. Elaine Kaye of Harvard University, Boston, and associates described (Arch Dermatol. 1991;127:351-5) opaque physical sunscreens that were useful blockers of visible light and found that transmittance of light can be lowered by adding iron oxide, Dr. Arellano-Mendoza pointed out.
The inorganic sunscreens have never been widely adopted because they are highly pigmented with white or, in the case of iron oxide, with red. “Not many people accepted [the iron-containing compounds] because of the redness, but now different shades are going to be hitting the market soon,” and the hope is that consumers will find them more appealing, she said.
This is good news, as the data emerging around iron oxide are intriguingly positive. A 2015 study showed that a sunscreen with iron oxides prevented melasma relapse during the summer months. Patients were randomized to the same ultraviolet filter topical sunscreen, but for one group, micronized iron oxide was added to it. After 6 months, the median melasma area severity index score was significantly better in the group using the iron oxide compound (J Am Acad Dermatol. 2015 Jan;72[1]:189-90.e1).
Support for the two-step regimen appeared in 2014, when a small study randomized 30 healthy volunteers to an SPF 30 sunscreen or the same sunscreen supplemented with an antioxidant cocktail of grape seed extract, vitamin E, ubiquinone, and vitamin C. The endpoint was MMP-1 upregulation after exposure to infrared-A light. Skin treated with the combination regimen showed significantly lower MMP-1 activation, leading the authors to conclude that the combination of topical antioxidants conferred protection against the irradiation (Photochem Photobiol. 2015 Jan-Feb;91[1]:248-50).
Those same authors published a companion article (Photodermatol Photoimmunol Photomed. 2014;30:167-74) suggesting that another antioxidant mixture (ferulic acid, tocopherol, and vitamin C) was similarly effective.
Using a combination of antioxidants is important, Dr. Arellano-Mendoza said, because different antioxidants work differently. Some (catalase, glutathione peroxidase, and superoxide dismutase) are enzymatic, catalyzing reactions that convert free radicals to oxygen and water. Others terminate free radicals by preventing the propagation of oxidative chain reactions (vitamins A and C, flavonoids, uric acid, bilirubin, albumin, and members of the thiol group). A third group consists of metal-binding proteins that sequester free iron or copper to prevent free radical production (ferritin, transferrin, lactoferrin, and ceruloplasmin).
“I think we can now consider antioxidants a part of the tools we use in treating some pigmentary disorders as melasma,” she said. “We need to choose the compounds carefully, and we definitely need more in vivo research, but the findings are very encouraging.”
Dr. Arellano-Mendoza had no relevant financial disclosures.
This article was updated 3/20/17.
[email protected]
On Twitter @Alz_Gal
ORLANDO – A two-step regimen of high-potency topical antioxidants followed by a mineral-based sunscreen may help repair light-induced skin damage and protect against new damage in patients with melasma.
Recent studies suggest that the antioxidants tamp down inflammatory cytokines and damage of oxidative stress, Maria Ivonne Arellano-Mendoza, MD, said during a special focus session on Latino skin held at the annual meeting of the American Academy of Dermatology.
“Many compounds are being studied for this purpose,” said Dr. Arellano-Mendoza, head of the dermatology department of the General Hospital of Mexico, Mexico City. “One combination is vitamin C, vitamin E, ubiquinone, and grape-seed extract. This effectively prevented infrared-A radiation–induced matrix metalloproteinase-1 messenger RNA expression in human skin. This combination can be found now in some sunscreens and daily care products.”
Another effective combination seems to be a mixture of ferulic acid, tocopherol, and vitamin C, she said.
The two-step process of regularly using a topical product with antioxidants before applying a sunscreen is all there is for now, she added, because so far it’s been impossible to combine the agents in a single product.
“The challenge will be how to create a product that stays on the surface of the skin to protect it from light, while liberating the antioxidants to penetrate the skin,” she commented.
The antioxidants’ benefits, however, will be obliterated by the continued effects of some light wavelengths that aggravate melasma unless they are used in sequence with a light-scattering sunscreen.
Sunscreens are critical components of a melasma treatment regimen, Dr. Arellano-Mendoza said. “Sunscreens are a cornerstone of treatment. We clearly tell our patients that sunscreens have to be used every day, forever, and if they are not used properly, they will have no improvement.”
Patients with hyperpigmentation disorders are susceptible to longer wavelengths that aren’t covered by chemically derived sunscreens. Longer wavelengths, including infrared light and visible light, have been shown to increase expression of matrix metalloproteinase (MMP) -1 and -9, decrease expression of type 1 procollagen, and can induce macrophage infiltration. These wavelengths also increase reactive oxygen species and proinflammatory cytokines in vitro, Dr. Arellano-Mendoza noted.
Visible light can cause erythema, transient and long-lasting hyperpigmentation, thermal damage, free radical production, and premature photoaging. It also can stimulate the production of reactive oxygen species that can damage DNA.
Mineral-based, inorganic sunscreens, however – like those with titanium dioxide, zinc oxide, and iron oxide – scatter all wavelengths.
“These micronized forms of metal oxides not only scatter and reflect light, they also absorb ultraviolet radiation. The compounds aren’t new,” she said. In 1991, Dr. Elaine Kaye of Harvard University, Boston, and associates described (Arch Dermatol. 1991;127:351-5) opaque physical sunscreens that were useful blockers of visible light and found that transmittance of light can be lowered by adding iron oxide, Dr. Arellano-Mendoza pointed out.
The inorganic sunscreens have never been widely adopted because they are highly pigmented with white or, in the case of iron oxide, with red. “Not many people accepted [the iron-containing compounds] because of the redness, but now different shades are going to be hitting the market soon,” and the hope is that consumers will find them more appealing, she said.
This is good news, as the data emerging around iron oxide are intriguingly positive. A 2015 study showed that a sunscreen with iron oxides prevented melasma relapse during the summer months. Patients were randomized to the same ultraviolet filter topical sunscreen, but for one group, micronized iron oxide was added to it. After 6 months, the median melasma area severity index score was significantly better in the group using the iron oxide compound (J Am Acad Dermatol. 2015 Jan;72[1]:189-90.e1).
Support for the two-step regimen appeared in 2014, when a small study randomized 30 healthy volunteers to an SPF 30 sunscreen or the same sunscreen supplemented with an antioxidant cocktail of grape seed extract, vitamin E, ubiquinone, and vitamin C. The endpoint was MMP-1 upregulation after exposure to infrared-A light. Skin treated with the combination regimen showed significantly lower MMP-1 activation, leading the authors to conclude that the combination of topical antioxidants conferred protection against the irradiation (Photochem Photobiol. 2015 Jan-Feb;91[1]:248-50).
Those same authors published a companion article (Photodermatol Photoimmunol Photomed. 2014;30:167-74) suggesting that another antioxidant mixture (ferulic acid, tocopherol, and vitamin C) was similarly effective.
Using a combination of antioxidants is important, Dr. Arellano-Mendoza said, because different antioxidants work differently. Some (catalase, glutathione peroxidase, and superoxide dismutase) are enzymatic, catalyzing reactions that convert free radicals to oxygen and water. Others terminate free radicals by preventing the propagation of oxidative chain reactions (vitamins A and C, flavonoids, uric acid, bilirubin, albumin, and members of the thiol group). A third group consists of metal-binding proteins that sequester free iron or copper to prevent free radical production (ferritin, transferrin, lactoferrin, and ceruloplasmin).
“I think we can now consider antioxidants a part of the tools we use in treating some pigmentary disorders as melasma,” she said. “We need to choose the compounds carefully, and we definitely need more in vivo research, but the findings are very encouraging.”
Dr. Arellano-Mendoza had no relevant financial disclosures.
This article was updated 3/20/17.
[email protected]
On Twitter @Alz_Gal
EXPERT ANALYSIS FROM AAD 2017
EXPERT ANALYSIS FROM AAD 2017
For optimal care, consider all acne in Latinos inflammatory
ORLANDO – Postinflammatory hyperpigmentation is a common consequence of acne in Latino skin, and aggressive medical treatments or procedures can aggravate the problem.
In fact, the hyperpigmentation that remains after acne is treated can be even more upsetting than the acne itself, according to Mercedes Florez-White, MD.
“Most of the time, the postinflammatory hyperpigmentation [PIH] has much more impact on the patient’s quality of life even than the disease itself, so you need to be very careful when treating these patients,” said Dr. Florez-White of Florida International University, Miami.
Every Fitzpatrick phototype can be observed in the Latino population, but one feature seems to link them: inflammation linked with all types of acne, even comedonal. “Even patients with very pale skin can show, at the periphery of the comedone, a little darkness signaling inflammation. The skin of a mestizo [a person of mixed Spanish/Native American ancestry] is especially prone to this,” she said at the annual meeting of the American Academy of Dermatology.
There is a paucity of research on the treatment of acne in people with skin of color, Dr. Florez-White said. Even the most recent acne treatment guidelines, published in 2016 by the AAD, acknowledge the area as a “research gap” that needs to be addressed.
In the meantime, she offered what she called “pearls of acne wisdom” gleaned from 35 years of treating Latino patients in South America and the United States.
Overview and diagnosis
Nodulocystic acne is the most common type in this population, followed by comedonal acne. Although the comedonal type is not generally considered inflammatory acne, it should be in Latino patients, given their sensitivity to skin inflammation and its outcome. “There is inflammation there from the beginning – treat it as an inflammatory disease for the best results.”
• Acne in Latino patients occurs most commonly, but not exclusively, on the lower face. “We have also seen this on the neck and chest,” she noted.
• A thorough history – including a rundown of hair and skin products the patient is using – is critical. “You never know when something you think is acne is really something else,” like an allergic reaction, she said.
Treatment
There are no AAD-generated treatment guidelines for acne in Latino patients. Dr. Florez-White manages her patients according to a treatment algorithm published by the Ibero-Latin American College of Dermatology and a paper published in the Journal of Dermatologic Treatment (2010 May;21[3]:206-11), as well as her own clinical experience.
Topical therapy
• Start topical retinoids at a lower concentration, two to three times a week, and gradually increase the dose and frequency until the desired effect is reached. Also, start benzoyl peroxide at lower doses.
• For a patient with very proinflammatory cystic acne, initiate a short course of corticosteroids to decrease inflammation – this will reduce the risk of PIH.
• Add azelaic acid in a 20% cream or 15% gel. “It’s an anti-inflammatory and antibacterial, and it really does help reduce the chance of PIH. This is used all over Latin American and Asia, but it is an off-label use in the U.S.” she said.
• For adult women, consider 5% dapsone gel, but not in combination with benzoyl peroxide.
Oral therapy
• Doxycycline is first-line treatment for moderate to severe papulopustular or nodulocystic acne. Other primary agents could be minocycline or tetracycline. Second-line antibiotic choices include erythromycin, azithromycin, and sulfamethoxazole/trimethoprim. Antibiotics should be given with benzoyl peroxide to reduce the chance of bacterial resistance.
• For nonresponsive cases, use oral isotretinoin, started at half the recommended dose. Increase gradually to treatment response.
For women with hormonally mediated acne, give a trial of oral contraceptives with antiandrogen properties, or spironolactone. “I like to combine oral contraceptive pills with isotretinoin. You can give this because the absorption of isotretinoin is very superficial. You won’t have any problems with that,” she noted.
Skin care
Good skin care will help promote healing and generally increase patient compliance with medication, Dr. Florez-White said.
• A noncomedogenic broad-spectrum sunscreen should be used daily. Consider one with mineral oxides, especially iron oxide, as only these preparations scatter both visible light and infrared radiation, which both increase the risk of PIH.
• Cleanse with a synthetic detergent or lipid-free cleanser.
• Recommend daily use of a salicylic, lactic, or glycolic acid.
Camouflage is very important for some patients, especially teens. “I always recommend a noncomedogenic fluid makeup,” she said.
Procedures
• Comedo extraction is an essential part of a comprehensive acne treatment program, but hold off until after a month of retinoid treatment. Removing the lesions significantly decreases the chance of PIH.
• Very superficial chemical peels with salicylic acid alone, or in combination with mandelic acid, may improve outcome faster and decrease PIH that already exists. These can be used in conjunction with oral agents, including isotretinoin.
Dr. Florez-White had no financial disclosures.
[email protected]
On Twitter @alz_gal
ORLANDO – Postinflammatory hyperpigmentation is a common consequence of acne in Latino skin, and aggressive medical treatments or procedures can aggravate the problem.
In fact, the hyperpigmentation that remains after acne is treated can be even more upsetting than the acne itself, according to Mercedes Florez-White, MD.
“Most of the time, the postinflammatory hyperpigmentation [PIH] has much more impact on the patient’s quality of life even than the disease itself, so you need to be very careful when treating these patients,” said Dr. Florez-White of Florida International University, Miami.
Every Fitzpatrick phototype can be observed in the Latino population, but one feature seems to link them: inflammation linked with all types of acne, even comedonal. “Even patients with very pale skin can show, at the periphery of the comedone, a little darkness signaling inflammation. The skin of a mestizo [a person of mixed Spanish/Native American ancestry] is especially prone to this,” she said at the annual meeting of the American Academy of Dermatology.
There is a paucity of research on the treatment of acne in people with skin of color, Dr. Florez-White said. Even the most recent acne treatment guidelines, published in 2016 by the AAD, acknowledge the area as a “research gap” that needs to be addressed.
In the meantime, she offered what she called “pearls of acne wisdom” gleaned from 35 years of treating Latino patients in South America and the United States.
Overview and diagnosis
Nodulocystic acne is the most common type in this population, followed by comedonal acne. Although the comedonal type is not generally considered inflammatory acne, it should be in Latino patients, given their sensitivity to skin inflammation and its outcome. “There is inflammation there from the beginning – treat it as an inflammatory disease for the best results.”
• Acne in Latino patients occurs most commonly, but not exclusively, on the lower face. “We have also seen this on the neck and chest,” she noted.
• A thorough history – including a rundown of hair and skin products the patient is using – is critical. “You never know when something you think is acne is really something else,” like an allergic reaction, she said.
Treatment
There are no AAD-generated treatment guidelines for acne in Latino patients. Dr. Florez-White manages her patients according to a treatment algorithm published by the Ibero-Latin American College of Dermatology and a paper published in the Journal of Dermatologic Treatment (2010 May;21[3]:206-11), as well as her own clinical experience.
Topical therapy
• Start topical retinoids at a lower concentration, two to three times a week, and gradually increase the dose and frequency until the desired effect is reached. Also, start benzoyl peroxide at lower doses.
• For a patient with very proinflammatory cystic acne, initiate a short course of corticosteroids to decrease inflammation – this will reduce the risk of PIH.
• Add azelaic acid in a 20% cream or 15% gel. “It’s an anti-inflammatory and antibacterial, and it really does help reduce the chance of PIH. This is used all over Latin American and Asia, but it is an off-label use in the U.S.” she said.
• For adult women, consider 5% dapsone gel, but not in combination with benzoyl peroxide.
Oral therapy
• Doxycycline is first-line treatment for moderate to severe papulopustular or nodulocystic acne. Other primary agents could be minocycline or tetracycline. Second-line antibiotic choices include erythromycin, azithromycin, and sulfamethoxazole/trimethoprim. Antibiotics should be given with benzoyl peroxide to reduce the chance of bacterial resistance.
• For nonresponsive cases, use oral isotretinoin, started at half the recommended dose. Increase gradually to treatment response.
For women with hormonally mediated acne, give a trial of oral contraceptives with antiandrogen properties, or spironolactone. “I like to combine oral contraceptive pills with isotretinoin. You can give this because the absorption of isotretinoin is very superficial. You won’t have any problems with that,” she noted.
Skin care
Good skin care will help promote healing and generally increase patient compliance with medication, Dr. Florez-White said.
• A noncomedogenic broad-spectrum sunscreen should be used daily. Consider one with mineral oxides, especially iron oxide, as only these preparations scatter both visible light and infrared radiation, which both increase the risk of PIH.
• Cleanse with a synthetic detergent or lipid-free cleanser.
• Recommend daily use of a salicylic, lactic, or glycolic acid.
Camouflage is very important for some patients, especially teens. “I always recommend a noncomedogenic fluid makeup,” she said.
Procedures
• Comedo extraction is an essential part of a comprehensive acne treatment program, but hold off until after a month of retinoid treatment. Removing the lesions significantly decreases the chance of PIH.
• Very superficial chemical peels with salicylic acid alone, or in combination with mandelic acid, may improve outcome faster and decrease PIH that already exists. These can be used in conjunction with oral agents, including isotretinoin.
Dr. Florez-White had no financial disclosures.
[email protected]
On Twitter @alz_gal
ORLANDO – Postinflammatory hyperpigmentation is a common consequence of acne in Latino skin, and aggressive medical treatments or procedures can aggravate the problem.
In fact, the hyperpigmentation that remains after acne is treated can be even more upsetting than the acne itself, according to Mercedes Florez-White, MD.
“Most of the time, the postinflammatory hyperpigmentation [PIH] has much more impact on the patient’s quality of life even than the disease itself, so you need to be very careful when treating these patients,” said Dr. Florez-White of Florida International University, Miami.
Every Fitzpatrick phototype can be observed in the Latino population, but one feature seems to link them: inflammation linked with all types of acne, even comedonal. “Even patients with very pale skin can show, at the periphery of the comedone, a little darkness signaling inflammation. The skin of a mestizo [a person of mixed Spanish/Native American ancestry] is especially prone to this,” she said at the annual meeting of the American Academy of Dermatology.
There is a paucity of research on the treatment of acne in people with skin of color, Dr. Florez-White said. Even the most recent acne treatment guidelines, published in 2016 by the AAD, acknowledge the area as a “research gap” that needs to be addressed.
In the meantime, she offered what she called “pearls of acne wisdom” gleaned from 35 years of treating Latino patients in South America and the United States.
Overview and diagnosis
Nodulocystic acne is the most common type in this population, followed by comedonal acne. Although the comedonal type is not generally considered inflammatory acne, it should be in Latino patients, given their sensitivity to skin inflammation and its outcome. “There is inflammation there from the beginning – treat it as an inflammatory disease for the best results.”
• Acne in Latino patients occurs most commonly, but not exclusively, on the lower face. “We have also seen this on the neck and chest,” she noted.
• A thorough history – including a rundown of hair and skin products the patient is using – is critical. “You never know when something you think is acne is really something else,” like an allergic reaction, she said.
Treatment
There are no AAD-generated treatment guidelines for acne in Latino patients. Dr. Florez-White manages her patients according to a treatment algorithm published by the Ibero-Latin American College of Dermatology and a paper published in the Journal of Dermatologic Treatment (2010 May;21[3]:206-11), as well as her own clinical experience.
Topical therapy
• Start topical retinoids at a lower concentration, two to three times a week, and gradually increase the dose and frequency until the desired effect is reached. Also, start benzoyl peroxide at lower doses.
• For a patient with very proinflammatory cystic acne, initiate a short course of corticosteroids to decrease inflammation – this will reduce the risk of PIH.
• Add azelaic acid in a 20% cream or 15% gel. “It’s an anti-inflammatory and antibacterial, and it really does help reduce the chance of PIH. This is used all over Latin American and Asia, but it is an off-label use in the U.S.” she said.
• For adult women, consider 5% dapsone gel, but not in combination with benzoyl peroxide.
Oral therapy
• Doxycycline is first-line treatment for moderate to severe papulopustular or nodulocystic acne. Other primary agents could be minocycline or tetracycline. Second-line antibiotic choices include erythromycin, azithromycin, and sulfamethoxazole/trimethoprim. Antibiotics should be given with benzoyl peroxide to reduce the chance of bacterial resistance.
• For nonresponsive cases, use oral isotretinoin, started at half the recommended dose. Increase gradually to treatment response.
For women with hormonally mediated acne, give a trial of oral contraceptives with antiandrogen properties, or spironolactone. “I like to combine oral contraceptive pills with isotretinoin. You can give this because the absorption of isotretinoin is very superficial. You won’t have any problems with that,” she noted.
Skin care
Good skin care will help promote healing and generally increase patient compliance with medication, Dr. Florez-White said.
• A noncomedogenic broad-spectrum sunscreen should be used daily. Consider one with mineral oxides, especially iron oxide, as only these preparations scatter both visible light and infrared radiation, which both increase the risk of PIH.
• Cleanse with a synthetic detergent or lipid-free cleanser.
• Recommend daily use of a salicylic, lactic, or glycolic acid.
Camouflage is very important for some patients, especially teens. “I always recommend a noncomedogenic fluid makeup,” she said.
Procedures
• Comedo extraction is an essential part of a comprehensive acne treatment program, but hold off until after a month of retinoid treatment. Removing the lesions significantly decreases the chance of PIH.
• Very superficial chemical peels with salicylic acid alone, or in combination with mandelic acid, may improve outcome faster and decrease PIH that already exists. These can be used in conjunction with oral agents, including isotretinoin.
Dr. Florez-White had no financial disclosures.
[email protected]
On Twitter @alz_gal
EXPERT ANALYSIS FROM AAD 17
Ticagrelor improves platelet reactivity, but not clinical outcomes, in Chinese stroke patients
HOUSTON – The combination of ticagrelor and aspirin reduced the incidence of high on-treatment platelet reactivity compared with clopidogrel plus aspirin in an interim analysis of a trial of patients with minor acute ischemic stroke or high-risk transient ischemic attack, but was associated with more treatment-limiting side effects.
Significantly more patients taking the ticagrelor combination dropped out because of dyspnea and minor bleeding, Yilong Wang, MD, said at the International Stroke Conference, sponsored by the American Heart Association. Although the ticagrelor combination also prevented a few more recurrent strokes than did clopidogrel plus aspirin, the difference was not statistically significant.
Dr. Wang of Beijing Tiantan Hospital reported the results as part of an interim safety and efficacy analysis of the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial.
“Ticagrelor has been shown to be more effective in acute coronary syndromes than clopidogrel, regardless of genotype, as it is primarily metabolized by the cytochrome P3A4 enzyme,” Dr. Wang said. “In the SOCRATES Asian substudy, we saw a trend of better efficacy in reducing the risk of subsequent vascular events in the ticagrelor group. But there are limited data on the safety and efficacy of ticagrelor, compared with clopidogrel, over background aspirin in stroke patients.”
PRINCE sought to determine the safety of ticagrelor plus aspirin and their effect on platelet reactivity and clinical outcomes in Asian patients who had experienced a minor stroke or high-risk transient ischemic attack (TIA). The 90-day trial is being conducted in 26 centers in China. Its primary endpoints are P2Y12 reaction units (PRU) and the number of patients with high on-treatment platelet reactivity. Secondary outcomes were the incidence of stroke at 90 days, and a composite vascular outcome of any stroke, heart attack, or vascular death within 90 days.
The primary safety outcomes were major and minor bleeding, intracerebral hemorrhage, and total mortality. The study’s researchers hope to enroll 952 patients. The interim analysis was conducted in 476 who have completed the treatment and follow-up period.
The ticagrelor group (237) received an initial loading dose of 180 mg with 100-300 mg aspirin on day 1, followed by 180 mg ticagrelor plus 100 mg aspirin for 21 days. Thereafter, they discontinued the aspirin and continued with 180 mg ticagrelor.
The clopidogrel group (239) received a 300-mg clopidogrel loading dose plus 100-300 mg aspirin on day 1, followed by 75 mg clopidogrel and 100 mg aspirin daily for 21 days. Thereafter they discontinued the aspirin and took 75 mg clopidogrel daily.
Patients were a median of 60 years old. Most (75%) were male. The median blood pressure was 152/90; 60% were hypertensive. About a quarter had diabetes. The qualifying stroke was a TIA in 22%; the rest had a minor ischemic stroke. The median National Institutes of Health Stroke Scale score was 2.
Platelet function was measured at baseline and 2 hours after the initial loading dose, and then again at 24 hours, and at 7, 21, and 90 days.
The baseline PRU was about 250 in each group. Two hours after the loading dose, it dropped significantly more among those taking ticagrelor than in those on clopidogrel (45.7 vs. 222.32). It remained significantly lower at every time point. At 90 days, the PRU favored ticagrelor (69 vs. 175).
Ticagrelor was also associated with significantly less high on-treatment platelet reactivity at every time point. The final separation at 90 days significantly favored ticagrelor (13% vs. 30%).
Clinical endpoints numerically favored ticagrelor, although none of the findings were statistically significant. Any stroke occurred in 4.6% of the ticagrelor group and 7.5% of the clopidogrel group. The rate of ischemic stroke was 4.2% and 6.7%, respectively.
There were three deaths: two in the ticagrelor and one in the clopidogrel group, and three major bleeds in each group. There was no significant difference in minor bleeding or intracerebral hemorrhage. However, ticagrelor was associated with significantly more incidents of minimal bleeding (17% vs. 7%). This difference drove the final, statistically significant doubling of bleeding risk associated with ticagrelor (hazard ratio, 2.26).
There were 49 adverse events leading to dropouts. Most of these were due to bleeding, which was significantly higher in those taking ticagrelor (12 vs. 5 events). Dyspnea was the next-leading cause of study dropout (5 vs. 1 case). The remainder of the dropouts were due to study noncompliance and patient decisions.
The study will continue, Dr. Wang noted.
PRINCE is being sponsored by the Chinese government. Dr. Wang had no financial disclosures. AstraZeneca is providing the study drug at no charge, and is not otherwise involved in the trial.
[email protected]
On Twitter @alz_gal
HOUSTON – The combination of ticagrelor and aspirin reduced the incidence of high on-treatment platelet reactivity compared with clopidogrel plus aspirin in an interim analysis of a trial of patients with minor acute ischemic stroke or high-risk transient ischemic attack, but was associated with more treatment-limiting side effects.
Significantly more patients taking the ticagrelor combination dropped out because of dyspnea and minor bleeding, Yilong Wang, MD, said at the International Stroke Conference, sponsored by the American Heart Association. Although the ticagrelor combination also prevented a few more recurrent strokes than did clopidogrel plus aspirin, the difference was not statistically significant.
Dr. Wang of Beijing Tiantan Hospital reported the results as part of an interim safety and efficacy analysis of the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial.
“Ticagrelor has been shown to be more effective in acute coronary syndromes than clopidogrel, regardless of genotype, as it is primarily metabolized by the cytochrome P3A4 enzyme,” Dr. Wang said. “In the SOCRATES Asian substudy, we saw a trend of better efficacy in reducing the risk of subsequent vascular events in the ticagrelor group. But there are limited data on the safety and efficacy of ticagrelor, compared with clopidogrel, over background aspirin in stroke patients.”
PRINCE sought to determine the safety of ticagrelor plus aspirin and their effect on platelet reactivity and clinical outcomes in Asian patients who had experienced a minor stroke or high-risk transient ischemic attack (TIA). The 90-day trial is being conducted in 26 centers in China. Its primary endpoints are P2Y12 reaction units (PRU) and the number of patients with high on-treatment platelet reactivity. Secondary outcomes were the incidence of stroke at 90 days, and a composite vascular outcome of any stroke, heart attack, or vascular death within 90 days.
The primary safety outcomes were major and minor bleeding, intracerebral hemorrhage, and total mortality. The study’s researchers hope to enroll 952 patients. The interim analysis was conducted in 476 who have completed the treatment and follow-up period.
The ticagrelor group (237) received an initial loading dose of 180 mg with 100-300 mg aspirin on day 1, followed by 180 mg ticagrelor plus 100 mg aspirin for 21 days. Thereafter, they discontinued the aspirin and continued with 180 mg ticagrelor.
The clopidogrel group (239) received a 300-mg clopidogrel loading dose plus 100-300 mg aspirin on day 1, followed by 75 mg clopidogrel and 100 mg aspirin daily for 21 days. Thereafter they discontinued the aspirin and took 75 mg clopidogrel daily.
Patients were a median of 60 years old. Most (75%) were male. The median blood pressure was 152/90; 60% were hypertensive. About a quarter had diabetes. The qualifying stroke was a TIA in 22%; the rest had a minor ischemic stroke. The median National Institutes of Health Stroke Scale score was 2.
Platelet function was measured at baseline and 2 hours after the initial loading dose, and then again at 24 hours, and at 7, 21, and 90 days.
The baseline PRU was about 250 in each group. Two hours after the loading dose, it dropped significantly more among those taking ticagrelor than in those on clopidogrel (45.7 vs. 222.32). It remained significantly lower at every time point. At 90 days, the PRU favored ticagrelor (69 vs. 175).
Ticagrelor was also associated with significantly less high on-treatment platelet reactivity at every time point. The final separation at 90 days significantly favored ticagrelor (13% vs. 30%).
Clinical endpoints numerically favored ticagrelor, although none of the findings were statistically significant. Any stroke occurred in 4.6% of the ticagrelor group and 7.5% of the clopidogrel group. The rate of ischemic stroke was 4.2% and 6.7%, respectively.
There were three deaths: two in the ticagrelor and one in the clopidogrel group, and three major bleeds in each group. There was no significant difference in minor bleeding or intracerebral hemorrhage. However, ticagrelor was associated with significantly more incidents of minimal bleeding (17% vs. 7%). This difference drove the final, statistically significant doubling of bleeding risk associated with ticagrelor (hazard ratio, 2.26).
There were 49 adverse events leading to dropouts. Most of these were due to bleeding, which was significantly higher in those taking ticagrelor (12 vs. 5 events). Dyspnea was the next-leading cause of study dropout (5 vs. 1 case). The remainder of the dropouts were due to study noncompliance and patient decisions.
The study will continue, Dr. Wang noted.
PRINCE is being sponsored by the Chinese government. Dr. Wang had no financial disclosures. AstraZeneca is providing the study drug at no charge, and is not otherwise involved in the trial.
[email protected]
On Twitter @alz_gal
HOUSTON – The combination of ticagrelor and aspirin reduced the incidence of high on-treatment platelet reactivity compared with clopidogrel plus aspirin in an interim analysis of a trial of patients with minor acute ischemic stroke or high-risk transient ischemic attack, but was associated with more treatment-limiting side effects.
Significantly more patients taking the ticagrelor combination dropped out because of dyspnea and minor bleeding, Yilong Wang, MD, said at the International Stroke Conference, sponsored by the American Heart Association. Although the ticagrelor combination also prevented a few more recurrent strokes than did clopidogrel plus aspirin, the difference was not statistically significant.
Dr. Wang of Beijing Tiantan Hospital reported the results as part of an interim safety and efficacy analysis of the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial.
“Ticagrelor has been shown to be more effective in acute coronary syndromes than clopidogrel, regardless of genotype, as it is primarily metabolized by the cytochrome P3A4 enzyme,” Dr. Wang said. “In the SOCRATES Asian substudy, we saw a trend of better efficacy in reducing the risk of subsequent vascular events in the ticagrelor group. But there are limited data on the safety and efficacy of ticagrelor, compared with clopidogrel, over background aspirin in stroke patients.”
PRINCE sought to determine the safety of ticagrelor plus aspirin and their effect on platelet reactivity and clinical outcomes in Asian patients who had experienced a minor stroke or high-risk transient ischemic attack (TIA). The 90-day trial is being conducted in 26 centers in China. Its primary endpoints are P2Y12 reaction units (PRU) and the number of patients with high on-treatment platelet reactivity. Secondary outcomes were the incidence of stroke at 90 days, and a composite vascular outcome of any stroke, heart attack, or vascular death within 90 days.
The primary safety outcomes were major and minor bleeding, intracerebral hemorrhage, and total mortality. The study’s researchers hope to enroll 952 patients. The interim analysis was conducted in 476 who have completed the treatment and follow-up period.
The ticagrelor group (237) received an initial loading dose of 180 mg with 100-300 mg aspirin on day 1, followed by 180 mg ticagrelor plus 100 mg aspirin for 21 days. Thereafter, they discontinued the aspirin and continued with 180 mg ticagrelor.
The clopidogrel group (239) received a 300-mg clopidogrel loading dose plus 100-300 mg aspirin on day 1, followed by 75 mg clopidogrel and 100 mg aspirin daily for 21 days. Thereafter they discontinued the aspirin and took 75 mg clopidogrel daily.
Patients were a median of 60 years old. Most (75%) were male. The median blood pressure was 152/90; 60% were hypertensive. About a quarter had diabetes. The qualifying stroke was a TIA in 22%; the rest had a minor ischemic stroke. The median National Institutes of Health Stroke Scale score was 2.
Platelet function was measured at baseline and 2 hours after the initial loading dose, and then again at 24 hours, and at 7, 21, and 90 days.
The baseline PRU was about 250 in each group. Two hours after the loading dose, it dropped significantly more among those taking ticagrelor than in those on clopidogrel (45.7 vs. 222.32). It remained significantly lower at every time point. At 90 days, the PRU favored ticagrelor (69 vs. 175).
Ticagrelor was also associated with significantly less high on-treatment platelet reactivity at every time point. The final separation at 90 days significantly favored ticagrelor (13% vs. 30%).
Clinical endpoints numerically favored ticagrelor, although none of the findings were statistically significant. Any stroke occurred in 4.6% of the ticagrelor group and 7.5% of the clopidogrel group. The rate of ischemic stroke was 4.2% and 6.7%, respectively.
There were three deaths: two in the ticagrelor and one in the clopidogrel group, and three major bleeds in each group. There was no significant difference in minor bleeding or intracerebral hemorrhage. However, ticagrelor was associated with significantly more incidents of minimal bleeding (17% vs. 7%). This difference drove the final, statistically significant doubling of bleeding risk associated with ticagrelor (hazard ratio, 2.26).
There were 49 adverse events leading to dropouts. Most of these were due to bleeding, which was significantly higher in those taking ticagrelor (12 vs. 5 events). Dyspnea was the next-leading cause of study dropout (5 vs. 1 case). The remainder of the dropouts were due to study noncompliance and patient decisions.
The study will continue, Dr. Wang noted.
PRINCE is being sponsored by the Chinese government. Dr. Wang had no financial disclosures. AstraZeneca is providing the study drug at no charge, and is not otherwise involved in the trial.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: At 90 days, P2Y12 reaction units favored ticagrelor (69 vs. 175).
Data source: The interim analysis of the PRINCE trial comprised 476 patients with minor acute ischemic stroke or high-risk transient ischemic attack.
Disclosures: PRINCE is being sponsored by the Chinese government. Dr. Wang had no financial disclosures. AstraZeneca is providing the study drug at no charge, and is not otherwise involved in the trial.
VIDEO: Despite promises of abstinence, isotretinoin-exposed pregnancies still occur
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT AAD 17
VIDEO: Gold nanoparticles target laser acne therapy
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
[email protected]
On Twitter @Alz_Gal
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
[email protected]
On Twitter @Alz_Gal
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
[email protected]
On Twitter @Alz_Gal
AT AAD 17
For bullous pemphigoid, doxycycline noninferior to prednisolone, but safer
ORLANDO – A 6-week course of doxycycline is an effective alternative to prednisolone for initial treatment of bullous pemphigoid in elderly patients, who may be particularly vulnerable to the potentially serious side effects of steroids.
While not as effective or quick-acting as prednisolone, doxycycline effected a cure in 74% of elderly patients who received it for 6 weeks in the Bullous Pemphigoid Steroids and Tetracyclines (BLISTER) Trial. More importantly, however, patients who took the antibiotic experienced half as many serious adverse events as those who took prednisolone (18% vs. 36%), Karen Harman, MD, said at the annual meeting of the American Academy of Dermatology.
The trial results will be published in the March 6 issue of The Lancet, she added.
BLISTER randomized 253 elderly patients with bullous pemphigoid to an initial, 6-week course of either 200 mg doxycycline/day or 0.5 mg/kg prednisolone/day. After the induction period, treatment could be adjusted as needed.
The primary efficacy outcome was blister count at 6 weeks; patients with fewer than three blisters were considered treatment successes. The primary safety outcome was the proportion who experienced an adverse event of at least grade 3 (severe, life-threatening, or fatal) related to the study medication.
The study was conducted at 54 centers in the United Kingdom and Germany, said Dr. Harman, who was also a primary investigator on the trial. It was a pragmatic noninferiority trial.
“We knew from the beginning that doxycycline would not be as effective as prednisolone. We estimated that we would see a 25% reduced efficacy, but we were prepared to accept that if we could also see an improvement in safety of at least 20%.”
Patients were a mean of age of 78 years, although about a quarter were 85 years or older. They scored a mean of 70 points on the 0-100 point Karnofsky scale of functional independence, with 100 being completely functionally independent.
A score of 70 means the patient is capable of self-care but cannot engage in normal activity or work because of disease. About 10% were unable to care for themselves and 42% unable to work.
Over the year-long trial, 33 patients dropped out. The most frequent reason for withdrawal was death – not an unexpected occurrence in such an elderly and infirm group, Dr. Harman noted. There was no significant difference in deaths between the treatment arms. Another 39 withdrew consent during the study. Adverse events caused three patients to drop out (two in the doxycycline group and one in the prednisolone group). One patient taking doxycycline was unable to tolerate the study medication and dropped out.
At 6 weeks, treatment succeeded in 74% of the doxycycline group and in 91% of the prednisolone group. This was an adjusted absolute treatment difference of 18% – well within the 25% margin of noninferiority.
Baseline disease severity didn’t interact with either of the drugs’ effectiveness. Prednisolone was more effective in every severity class. Among those with mild disease, the success rates were 76% with doxycycline and 97% with prednisolone. Among those with moderate disease, success rates were 78% and 97%. Among those with severe disease, both drugs were slightly less effective, with success rates of 65% and 75%.
Adverse events of grade 3 or greater occurred in significantly fewer patients taking doxycycline (18.5% vs. 36.6%), an adjusted difference of 19%. This was close to the 20% gain in safety the investigators hoped for.
Adverse events were common, however, with 82% of patients on doxycycline and 64% on prednisolone experiencing at least one mild-moderate event. Most of these in the doxycycline group were gastrointestinal, Dr. Harman noted.
About twice as many patients taking prednisolone had an event with a maximum of grade 3 (22% vs. 11%). The proportion with a maximum event of grade 4 was 4% in each group. Eleven in the prednisolone group and three in the doxycycline group died (9.7% vs. 2.5%).
The trial had several secondary efficacy outcomes.
Doxycycline had a slower onset of action, as evidenced by the significant difference in high blister count at week 6 (26% vs. 8.7%). At 6 weeks, 20.5% of the doxycycline group and 4% of the prednisolone group experienced treatment failure and chose to switch to the other treatment arm. Adherence was also worse in the doxycycline group, with 19% missing more than 3 consecutive days of treatment vs. 5% in the prednisolone group.
The trial also included a quality of life measure for the entire 52 weeks. Through week 26, this favored prednisolone, again reflecting the slower disease control of doxycycline. Thereafter, quality of life was similar between the two groups.
The trial was run in collaboration with the Nottingham Clinical Trials Unit, the UK Dermatology Clinical Trials Network, and the Medical Research Council Clinical Trials Unit. Dr. Harman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
ORLANDO – A 6-week course of doxycycline is an effective alternative to prednisolone for initial treatment of bullous pemphigoid in elderly patients, who may be particularly vulnerable to the potentially serious side effects of steroids.
While not as effective or quick-acting as prednisolone, doxycycline effected a cure in 74% of elderly patients who received it for 6 weeks in the Bullous Pemphigoid Steroids and Tetracyclines (BLISTER) Trial. More importantly, however, patients who took the antibiotic experienced half as many serious adverse events as those who took prednisolone (18% vs. 36%), Karen Harman, MD, said at the annual meeting of the American Academy of Dermatology.
The trial results will be published in the March 6 issue of The Lancet, she added.
BLISTER randomized 253 elderly patients with bullous pemphigoid to an initial, 6-week course of either 200 mg doxycycline/day or 0.5 mg/kg prednisolone/day. After the induction period, treatment could be adjusted as needed.
The primary efficacy outcome was blister count at 6 weeks; patients with fewer than three blisters were considered treatment successes. The primary safety outcome was the proportion who experienced an adverse event of at least grade 3 (severe, life-threatening, or fatal) related to the study medication.
The study was conducted at 54 centers in the United Kingdom and Germany, said Dr. Harman, who was also a primary investigator on the trial. It was a pragmatic noninferiority trial.
“We knew from the beginning that doxycycline would not be as effective as prednisolone. We estimated that we would see a 25% reduced efficacy, but we were prepared to accept that if we could also see an improvement in safety of at least 20%.”
Patients were a mean of age of 78 years, although about a quarter were 85 years or older. They scored a mean of 70 points on the 0-100 point Karnofsky scale of functional independence, with 100 being completely functionally independent.
A score of 70 means the patient is capable of self-care but cannot engage in normal activity or work because of disease. About 10% were unable to care for themselves and 42% unable to work.
Over the year-long trial, 33 patients dropped out. The most frequent reason for withdrawal was death – not an unexpected occurrence in such an elderly and infirm group, Dr. Harman noted. There was no significant difference in deaths between the treatment arms. Another 39 withdrew consent during the study. Adverse events caused three patients to drop out (two in the doxycycline group and one in the prednisolone group). One patient taking doxycycline was unable to tolerate the study medication and dropped out.
At 6 weeks, treatment succeeded in 74% of the doxycycline group and in 91% of the prednisolone group. This was an adjusted absolute treatment difference of 18% – well within the 25% margin of noninferiority.
Baseline disease severity didn’t interact with either of the drugs’ effectiveness. Prednisolone was more effective in every severity class. Among those with mild disease, the success rates were 76% with doxycycline and 97% with prednisolone. Among those with moderate disease, success rates were 78% and 97%. Among those with severe disease, both drugs were slightly less effective, with success rates of 65% and 75%.
Adverse events of grade 3 or greater occurred in significantly fewer patients taking doxycycline (18.5% vs. 36.6%), an adjusted difference of 19%. This was close to the 20% gain in safety the investigators hoped for.
Adverse events were common, however, with 82% of patients on doxycycline and 64% on prednisolone experiencing at least one mild-moderate event. Most of these in the doxycycline group were gastrointestinal, Dr. Harman noted.
About twice as many patients taking prednisolone had an event with a maximum of grade 3 (22% vs. 11%). The proportion with a maximum event of grade 4 was 4% in each group. Eleven in the prednisolone group and three in the doxycycline group died (9.7% vs. 2.5%).
The trial had several secondary efficacy outcomes.
Doxycycline had a slower onset of action, as evidenced by the significant difference in high blister count at week 6 (26% vs. 8.7%). At 6 weeks, 20.5% of the doxycycline group and 4% of the prednisolone group experienced treatment failure and chose to switch to the other treatment arm. Adherence was also worse in the doxycycline group, with 19% missing more than 3 consecutive days of treatment vs. 5% in the prednisolone group.
The trial also included a quality of life measure for the entire 52 weeks. Through week 26, this favored prednisolone, again reflecting the slower disease control of doxycycline. Thereafter, quality of life was similar between the two groups.
The trial was run in collaboration with the Nottingham Clinical Trials Unit, the UK Dermatology Clinical Trials Network, and the Medical Research Council Clinical Trials Unit. Dr. Harman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
ORLANDO – A 6-week course of doxycycline is an effective alternative to prednisolone for initial treatment of bullous pemphigoid in elderly patients, who may be particularly vulnerable to the potentially serious side effects of steroids.
While not as effective or quick-acting as prednisolone, doxycycline effected a cure in 74% of elderly patients who received it for 6 weeks in the Bullous Pemphigoid Steroids and Tetracyclines (BLISTER) Trial. More importantly, however, patients who took the antibiotic experienced half as many serious adverse events as those who took prednisolone (18% vs. 36%), Karen Harman, MD, said at the annual meeting of the American Academy of Dermatology.
The trial results will be published in the March 6 issue of The Lancet, she added.
BLISTER randomized 253 elderly patients with bullous pemphigoid to an initial, 6-week course of either 200 mg doxycycline/day or 0.5 mg/kg prednisolone/day. After the induction period, treatment could be adjusted as needed.
The primary efficacy outcome was blister count at 6 weeks; patients with fewer than three blisters were considered treatment successes. The primary safety outcome was the proportion who experienced an adverse event of at least grade 3 (severe, life-threatening, or fatal) related to the study medication.
The study was conducted at 54 centers in the United Kingdom and Germany, said Dr. Harman, who was also a primary investigator on the trial. It was a pragmatic noninferiority trial.
“We knew from the beginning that doxycycline would not be as effective as prednisolone. We estimated that we would see a 25% reduced efficacy, but we were prepared to accept that if we could also see an improvement in safety of at least 20%.”
Patients were a mean of age of 78 years, although about a quarter were 85 years or older. They scored a mean of 70 points on the 0-100 point Karnofsky scale of functional independence, with 100 being completely functionally independent.
A score of 70 means the patient is capable of self-care but cannot engage in normal activity or work because of disease. About 10% were unable to care for themselves and 42% unable to work.
Over the year-long trial, 33 patients dropped out. The most frequent reason for withdrawal was death – not an unexpected occurrence in such an elderly and infirm group, Dr. Harman noted. There was no significant difference in deaths between the treatment arms. Another 39 withdrew consent during the study. Adverse events caused three patients to drop out (two in the doxycycline group and one in the prednisolone group). One patient taking doxycycline was unable to tolerate the study medication and dropped out.
At 6 weeks, treatment succeeded in 74% of the doxycycline group and in 91% of the prednisolone group. This was an adjusted absolute treatment difference of 18% – well within the 25% margin of noninferiority.
Baseline disease severity didn’t interact with either of the drugs’ effectiveness. Prednisolone was more effective in every severity class. Among those with mild disease, the success rates were 76% with doxycycline and 97% with prednisolone. Among those with moderate disease, success rates were 78% and 97%. Among those with severe disease, both drugs were slightly less effective, with success rates of 65% and 75%.
Adverse events of grade 3 or greater occurred in significantly fewer patients taking doxycycline (18.5% vs. 36.6%), an adjusted difference of 19%. This was close to the 20% gain in safety the investigators hoped for.
Adverse events were common, however, with 82% of patients on doxycycline and 64% on prednisolone experiencing at least one mild-moderate event. Most of these in the doxycycline group were gastrointestinal, Dr. Harman noted.
About twice as many patients taking prednisolone had an event with a maximum of grade 3 (22% vs. 11%). The proportion with a maximum event of grade 4 was 4% in each group. Eleven in the prednisolone group and three in the doxycycline group died (9.7% vs. 2.5%).
The trial had several secondary efficacy outcomes.
Doxycycline had a slower onset of action, as evidenced by the significant difference in high blister count at week 6 (26% vs. 8.7%). At 6 weeks, 20.5% of the doxycycline group and 4% of the prednisolone group experienced treatment failure and chose to switch to the other treatment arm. Adherence was also worse in the doxycycline group, with 19% missing more than 3 consecutive days of treatment vs. 5% in the prednisolone group.
The trial also included a quality of life measure for the entire 52 weeks. Through week 26, this favored prednisolone, again reflecting the slower disease control of doxycycline. Thereafter, quality of life was similar between the two groups.
The trial was run in collaboration with the Nottingham Clinical Trials Unit, the UK Dermatology Clinical Trials Network, and the Medical Research Council Clinical Trials Unit. Dr. Harman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
Key clinical point:
Major finding: At 6 weeks, treatment succeeded in 74% of the doxycycline group and 91% of the prednisolone group; severe adverse events occurred in 18% and 36%, respectively.
Data source: The BLISTER trial randomized 253 patients.
Disclosures: The trial was run in collaboration with the Nottingham Clinical Trials Unit, the UK Dermatology Clinical Trials Network, and the Medical Research Council Clinical Trials Unit. Dr. Harman had no financial disclosures.
Large, intermittent vitamin D doses may increase fracture, fall risk in elderly
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
[email protected]
On Twitter @Alz_Gal
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
[email protected]
On Twitter @Alz_Gal
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
[email protected]
On Twitter @Alz_Gal