User login
Sickle cell anemia: Stroke screening still underused
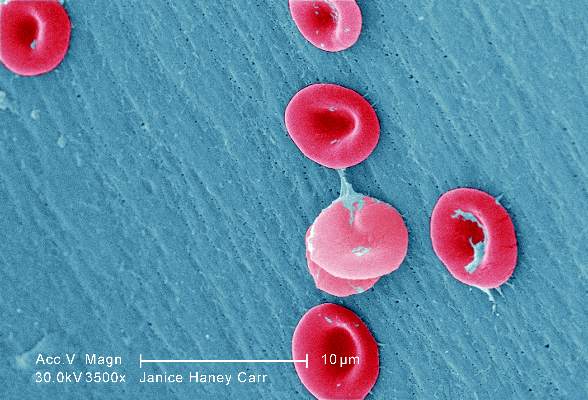
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
FROM JAMA PEDIATRICS
Key clinical point: Transcranial Doppler screening for stroke risk is still underused among children and adolescents with sickle cell anemia, despite clinical guidelines that strongly recommend annual screening.
Major finding: Screening rates increased somewhat across all six states studied, from 22% to 44%, but even the highest rates were suboptimal.
Data source: A retrospective cross-sectional analysis of administrative claims data for 4,775 pediatric patients treated in a 5-year period.
Disclosures: This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
Blood test predicts progression to active TB
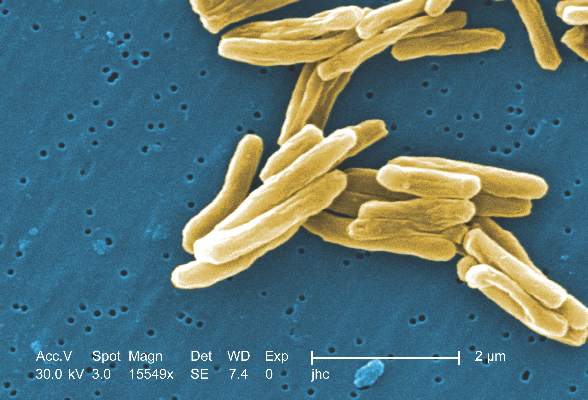
An international team of researchers has developed a blood test that identifies the 5%-10% of patients infected with latent tuberculosis who are likely to progress to active TB, up to 18 months before they show any sign of illness, according to a report published in the Lancet.
Worldwide, one-third of the apparently healthy population is infected with Mycobacterium tuberculosis, but only a fraction will develop active TB during their lifetimes. Until now there has been no way to predict which of these people will progress and become ill. Treating all latently infected people in endemic areas for the necessary 6-9 months isn’t feasible, but a test that distinguishes which cases will become active would allow targeted preventive therapy. This could potentially interrupt the global spread of TB, said Daniel E. Zak, Ph.D. of the Center for Infectious Disease Research, Seattle, and his associates.
Such a test also might be used to assess treatment response, as well as to enroll only the highest-risk carriers of M. tuberculosis in trials of new drugs and vaccines, they added.
The investigators began by analyzing gene expression in peripheral whole-blood samples from 6,363 apparently healthy adolescents participating in a South African cohort study who were followed for 2-4 years for the development of active TB. They compared RNA-sequencing data from 46 participants who developed active TB against that from 107 matched control subjects who remained healthy and identified a candidate 16-gene risk signature for TB progression. “Robust discrimination between progressors and controls based on the expression of the gene pairs in the signature was readily apparent,” the researchers said.
In this subgroup of patients, the risk signature had a 71.2% sensitivity for predicting active TB during the 6 months preceding diagnosis, a 62.9% sensitivity during the 12 months preceding diagnosis, and a 47.7% sensitivity during the 18 months preceding diagnosis. The specificity was 80.6%.
To validate their findings, the investigators adapted the risk signature to a more practical PCR platform and used it to predict the risk of active TB in the remainder of the study population. The risk signature remained comparably sensitive and specific in this analysis.
To validate their findings in an independent cohort, Dr. Zak and his associates analyzed whole-blood samples from 4,466 apparently healthy adults from South Africa and the Gambia who were participating in a study of household contacts of patients with newly diagnosed active TB. During follow-up, 43 progressors and 172 control subjects were identified at the South African study site, and 30 progressors and 129 control subjects were identified at the Gambian study site. The risk signature again reliably distinguished patients who progressed from latent to active TB from those who didn’t progress, months before any sign of illness surfaced.
“When applied to combined data from 4 studies of HIV-uninfected South African adults involving 130 prevalent TB cases and 230 controls, the signature discriminated between patients with active TB and controls with 87% sensitivity and 97% specificity,” the investigators noted.
Adapting the risk signature further to microarrays so that it could be used in other datasets, the researchers found that it readily distinguished latent from active TB infection in stored samples from more cohorts from the United Kingdom, South Africa, and Malawi. In these cases the risk signature also distinguished active TB from other pulmonary diseases and from other diseases of childhood, and did so regardless of whether the study subjects were coinfected with HIV or not. “Finally, applying the signature to data from a treatment study showed that the active TB signature gradually disappears during 6 months of therapy,” Dr. Zak and his associates wrote (Lancet 2016 March 23. doi:10.1016/S0140-6736[15]01316-1).
These latter observations suggest that the risk signature may reflect the TB bacterial load in the lung.
The study results were particularly encouraging given the marked diversity among these study populations. The participants had different age ranges, different infection or exposure status, distinct ethnic and genetic backgrounds, different local epidemiology, and different circulating strains of M. tuberculosis. “Our results … pave the way for the establishment of diagnostic methods that are scalable and inexpensive. An important first step would be to test whether the signature can predict TB in the general population, rather than the select populations included in this project,” the investigators added.
This study was funded by the Bill and Melinda Gates Foundation, the National Institutes of Health, the European Union, the South African Medical Research Council, and Aeras. Dr. Hanekom and his associates reported having no relevant financial disclosures.
The current TB epidemic is sustained by the emergence of new cases from the 2 billion people worldwide who have latent TB infection, and from the subsequent infection of their contacts. A test that identifies which people with latent infection will progress to active infection would transform TB control by allowing targeted treatment that would prevent these new cases from emerging.
Another significant finding from the work of Dr. Zak and his associates is that differences in gene expression were detected months before TB symptoms developed. This suggests that progressors have an immune response well before they are diagnosed, that their immune response differs from that of people who remain well, and that the progression from latent to active TB infection is a continuum in the battle between host and pathogen.
Dr. Michael Levin and Dr. Myrsini Kaforou are in the section for pediatric infectious diseases at Imperial College London. They reported being members of an EU-funded TB vaccine consortium and previously worked on an EU-funded study of TB biomarkers, both of which included some of Dr. Zak’s associates. Dr. Levin and Dr. Kaforou made these remarks in an editorial comment accompanying Dr. Zak’s report (Lancet. 2016 Mar 23. doi: 10.1016/S50140-6736[16]00165-3).
The current TB epidemic is sustained by the emergence of new cases from the 2 billion people worldwide who have latent TB infection, and from the subsequent infection of their contacts. A test that identifies which people with latent infection will progress to active infection would transform TB control by allowing targeted treatment that would prevent these new cases from emerging.
Another significant finding from the work of Dr. Zak and his associates is that differences in gene expression were detected months before TB symptoms developed. This suggests that progressors have an immune response well before they are diagnosed, that their immune response differs from that of people who remain well, and that the progression from latent to active TB infection is a continuum in the battle between host and pathogen.
Dr. Michael Levin and Dr. Myrsini Kaforou are in the section for pediatric infectious diseases at Imperial College London. They reported being members of an EU-funded TB vaccine consortium and previously worked on an EU-funded study of TB biomarkers, both of which included some of Dr. Zak’s associates. Dr. Levin and Dr. Kaforou made these remarks in an editorial comment accompanying Dr. Zak’s report (Lancet. 2016 Mar 23. doi: 10.1016/S50140-6736[16]00165-3).
The current TB epidemic is sustained by the emergence of new cases from the 2 billion people worldwide who have latent TB infection, and from the subsequent infection of their contacts. A test that identifies which people with latent infection will progress to active infection would transform TB control by allowing targeted treatment that would prevent these new cases from emerging.
Another significant finding from the work of Dr. Zak and his associates is that differences in gene expression were detected months before TB symptoms developed. This suggests that progressors have an immune response well before they are diagnosed, that their immune response differs from that of people who remain well, and that the progression from latent to active TB infection is a continuum in the battle between host and pathogen.
Dr. Michael Levin and Dr. Myrsini Kaforou are in the section for pediatric infectious diseases at Imperial College London. They reported being members of an EU-funded TB vaccine consortium and previously worked on an EU-funded study of TB biomarkers, both of which included some of Dr. Zak’s associates. Dr. Levin and Dr. Kaforou made these remarks in an editorial comment accompanying Dr. Zak’s report (Lancet. 2016 Mar 23. doi: 10.1016/S50140-6736[16]00165-3).
An international team of researchers has developed a blood test that identifies the 5%-10% of patients infected with latent tuberculosis who are likely to progress to active TB, up to 18 months before they show any sign of illness, according to a report published in the Lancet.
Worldwide, one-third of the apparently healthy population is infected with Mycobacterium tuberculosis, but only a fraction will develop active TB during their lifetimes. Until now there has been no way to predict which of these people will progress and become ill. Treating all latently infected people in endemic areas for the necessary 6-9 months isn’t feasible, but a test that distinguishes which cases will become active would allow targeted preventive therapy. This could potentially interrupt the global spread of TB, said Daniel E. Zak, Ph.D. of the Center for Infectious Disease Research, Seattle, and his associates.
Such a test also might be used to assess treatment response, as well as to enroll only the highest-risk carriers of M. tuberculosis in trials of new drugs and vaccines, they added.
The investigators began by analyzing gene expression in peripheral whole-blood samples from 6,363 apparently healthy adolescents participating in a South African cohort study who were followed for 2-4 years for the development of active TB. They compared RNA-sequencing data from 46 participants who developed active TB against that from 107 matched control subjects who remained healthy and identified a candidate 16-gene risk signature for TB progression. “Robust discrimination between progressors and controls based on the expression of the gene pairs in the signature was readily apparent,” the researchers said.
In this subgroup of patients, the risk signature had a 71.2% sensitivity for predicting active TB during the 6 months preceding diagnosis, a 62.9% sensitivity during the 12 months preceding diagnosis, and a 47.7% sensitivity during the 18 months preceding diagnosis. The specificity was 80.6%.
To validate their findings, the investigators adapted the risk signature to a more practical PCR platform and used it to predict the risk of active TB in the remainder of the study population. The risk signature remained comparably sensitive and specific in this analysis.
To validate their findings in an independent cohort, Dr. Zak and his associates analyzed whole-blood samples from 4,466 apparently healthy adults from South Africa and the Gambia who were participating in a study of household contacts of patients with newly diagnosed active TB. During follow-up, 43 progressors and 172 control subjects were identified at the South African study site, and 30 progressors and 129 control subjects were identified at the Gambian study site. The risk signature again reliably distinguished patients who progressed from latent to active TB from those who didn’t progress, months before any sign of illness surfaced.
“When applied to combined data from 4 studies of HIV-uninfected South African adults involving 130 prevalent TB cases and 230 controls, the signature discriminated between patients with active TB and controls with 87% sensitivity and 97% specificity,” the investigators noted.
Adapting the risk signature further to microarrays so that it could be used in other datasets, the researchers found that it readily distinguished latent from active TB infection in stored samples from more cohorts from the United Kingdom, South Africa, and Malawi. In these cases the risk signature also distinguished active TB from other pulmonary diseases and from other diseases of childhood, and did so regardless of whether the study subjects were coinfected with HIV or not. “Finally, applying the signature to data from a treatment study showed that the active TB signature gradually disappears during 6 months of therapy,” Dr. Zak and his associates wrote (Lancet 2016 March 23. doi:10.1016/S0140-6736[15]01316-1).
These latter observations suggest that the risk signature may reflect the TB bacterial load in the lung.
The study results were particularly encouraging given the marked diversity among these study populations. The participants had different age ranges, different infection or exposure status, distinct ethnic and genetic backgrounds, different local epidemiology, and different circulating strains of M. tuberculosis. “Our results … pave the way for the establishment of diagnostic methods that are scalable and inexpensive. An important first step would be to test whether the signature can predict TB in the general population, rather than the select populations included in this project,” the investigators added.
This study was funded by the Bill and Melinda Gates Foundation, the National Institutes of Health, the European Union, the South African Medical Research Council, and Aeras. Dr. Hanekom and his associates reported having no relevant financial disclosures.
An international team of researchers has developed a blood test that identifies the 5%-10% of patients infected with latent tuberculosis who are likely to progress to active TB, up to 18 months before they show any sign of illness, according to a report published in the Lancet.
Worldwide, one-third of the apparently healthy population is infected with Mycobacterium tuberculosis, but only a fraction will develop active TB during their lifetimes. Until now there has been no way to predict which of these people will progress and become ill. Treating all latently infected people in endemic areas for the necessary 6-9 months isn’t feasible, but a test that distinguishes which cases will become active would allow targeted preventive therapy. This could potentially interrupt the global spread of TB, said Daniel E. Zak, Ph.D. of the Center for Infectious Disease Research, Seattle, and his associates.
Such a test also might be used to assess treatment response, as well as to enroll only the highest-risk carriers of M. tuberculosis in trials of new drugs and vaccines, they added.
The investigators began by analyzing gene expression in peripheral whole-blood samples from 6,363 apparently healthy adolescents participating in a South African cohort study who were followed for 2-4 years for the development of active TB. They compared RNA-sequencing data from 46 participants who developed active TB against that from 107 matched control subjects who remained healthy and identified a candidate 16-gene risk signature for TB progression. “Robust discrimination between progressors and controls based on the expression of the gene pairs in the signature was readily apparent,” the researchers said.
In this subgroup of patients, the risk signature had a 71.2% sensitivity for predicting active TB during the 6 months preceding diagnosis, a 62.9% sensitivity during the 12 months preceding diagnosis, and a 47.7% sensitivity during the 18 months preceding diagnosis. The specificity was 80.6%.
To validate their findings, the investigators adapted the risk signature to a more practical PCR platform and used it to predict the risk of active TB in the remainder of the study population. The risk signature remained comparably sensitive and specific in this analysis.
To validate their findings in an independent cohort, Dr. Zak and his associates analyzed whole-blood samples from 4,466 apparently healthy adults from South Africa and the Gambia who were participating in a study of household contacts of patients with newly diagnosed active TB. During follow-up, 43 progressors and 172 control subjects were identified at the South African study site, and 30 progressors and 129 control subjects were identified at the Gambian study site. The risk signature again reliably distinguished patients who progressed from latent to active TB from those who didn’t progress, months before any sign of illness surfaced.
“When applied to combined data from 4 studies of HIV-uninfected South African adults involving 130 prevalent TB cases and 230 controls, the signature discriminated between patients with active TB and controls with 87% sensitivity and 97% specificity,” the investigators noted.
Adapting the risk signature further to microarrays so that it could be used in other datasets, the researchers found that it readily distinguished latent from active TB infection in stored samples from more cohorts from the United Kingdom, South Africa, and Malawi. In these cases the risk signature also distinguished active TB from other pulmonary diseases and from other diseases of childhood, and did so regardless of whether the study subjects were coinfected with HIV or not. “Finally, applying the signature to data from a treatment study showed that the active TB signature gradually disappears during 6 months of therapy,” Dr. Zak and his associates wrote (Lancet 2016 March 23. doi:10.1016/S0140-6736[15]01316-1).
These latter observations suggest that the risk signature may reflect the TB bacterial load in the lung.
The study results were particularly encouraging given the marked diversity among these study populations. The participants had different age ranges, different infection or exposure status, distinct ethnic and genetic backgrounds, different local epidemiology, and different circulating strains of M. tuberculosis. “Our results … pave the way for the establishment of diagnostic methods that are scalable and inexpensive. An important first step would be to test whether the signature can predict TB in the general population, rather than the select populations included in this project,” the investigators added.
This study was funded by the Bill and Melinda Gates Foundation, the National Institutes of Health, the European Union, the South African Medical Research Council, and Aeras. Dr. Hanekom and his associates reported having no relevant financial disclosures.
FROM THE LANCET
Key clinical point: Researchers have developed a blood test that identifies the 5%-10% of patients infected with latent tuberculosis who will progress to active TB.
Major finding: The TB-RNA risk signature had a 71.2% sensitivity for predicting active TB during the 6 months preceding diagnosis, a 62.9% sensitivity during the 12 months preceding diagnosis, and a 47.7% sensitivity during the 18 months preceding diagnosis.
Data source: A prospective cohort study to develop (6,363 patients) and validate (4,466 patients) a method of testing whole blood for an M. tuberculosis RNA signature.
Disclosures: This study was funded by the Bill and Melinda Gates Foundation, the National Institutes of Health, the European Union, the South African Medical Research Council, and Aeras. Dr. Hanekom and his associates reported having no relevant financial disclosures.
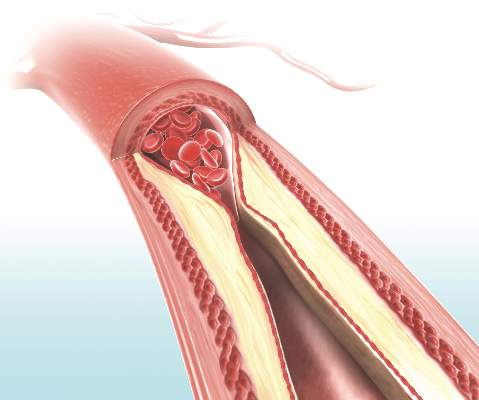
Only "Early" Estradiol Limits Atherosclerosis Progression
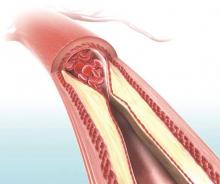
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Only "Early" Estradiol Limits Atherosclerosis Progression
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Long-term antibiotics ineffective for persistent Lyme disease
Long-term is no better than standard antibiotic therapy for persistent symptoms of Lyme disease, according to a report published online March 30 in the New England Journal of Medicine.
Randomized clinical trials have never shown convincingly that prolonged antibiotic therapy is beneficial for the many patients with Lyme disease who have persistent debilitating symptoms such as musculoskeletal pain, arthritis, arthralgia, neuralgia, sensory disturbances, dysesthesia, neuropsychological disorders, cognitive disorders, and fatigue. But some less rigorous studies have reported beneficial effects with prolonged antibiotics, and some guidelines endorse that approach, said Dr. Anneleen Berende of the Center for Infectious Diseases at Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
They performed a randomized, double-blind clinical trial, the Persistent Lyme Empiric Antibiotic Study Europe (PLEASE), in which 280 adults (mean age, 49 years) received daily 2,000-mg open-label IV ceftriaxone for 14 days and then were assigned to receive 100 mg oral doxycycline twice daily plus placebo (86 patients), combined 500 mg clarithromycin twice daily plus 200 mg hydroxychloroquine twice daily (96 patients), or two placebo capsules twice daily (98 patients) for 12 weeks. Patients were eligible for the trial if their persistent symptoms were temporally related to an erythema migrans rash or an otherwise proven case of symptomatic Lyme disease or were accompanied by Borrelia burgdorferi IgG or IgM antibodies according to immunoblot assay. They had median durations of symptoms of 2.1-2.7 years. Symptoms were assessed by self-report using the RAND SF-36 Health Status Inventory at baseline, at the end of the 14-week treatment period, and at 26, 40, and 52 weeks.
In the intention-to-treat analysis, the primary outcome measure – health-related quality of life as assessed on the physical component summary score of the RAND SF-36 at 14 weeks – did not differ significantly among the three study groups. The mean physical component summary scores were 35.0 with doxycycline, 35.6 with clarithromycin/hydroxychloroquine, and 34.8 with placebo. In addition, none of the secondary outcome measures, including mental impairment and fatigue, differed significantly among the three study groups, either at the end of treatment or at any subsequent follow-up visit.
The results of all sensitivity analyses, including the per-protocol analysis restricted to the 212 patients most adherent to the study regimen, accorded with those of the main analysis, Dr. Berende and her associates said (N Engl J Med. 2016;374[13]:1209-20).
“At the 14-week visit at the end of the treatment period, the mean SF-36 physical component summary score had improved significantly from baseline regardless of the study group assignment, but quality of life remained below that of the general population,” they noted.
Nearly three-fourths of patients reported at least one adverse event of a given type during the open-label and randomized phases combined, and approximately half reported adverse events during the randomized phase without any significant difference in rate across the groups. Patients taking doxycycline reported photosensitivity and nausea most often, and patients taking clarithromycin-hydroxychloroquine reported nausea, diarrhea, and rash most often. Fourteen patients (5.0%) discontinued the intervention because of adverse effects, and the number was similar across the three study groups.
This study was supported by the Netherlands Organization for Health Research and Development (ZonMw). Dr. Berende reported having no relevant financial disclosures; one of her associates reported inventing a patented cellular diagnostic test for Lyme disease.
This well-performed study should reduce the temptation among clinicians to prescribe prolonged courses of antibiotics for persistent Lyme symptoms “just in case” they might help.
Long-term antibiotics are not benign. Even though the adverse effects in this study were mostly minor, 68.6% of patients taking doxycycline or clarithromycin-hydroxychloroquine reported at least one adverse reaction judged to be drug related.
Dr. Michael T. Melia and Dr. Paul G. Auwaerter are at the Sherilyn and Ken Fisher Center for Environmental Infectious Diseases at Johns Hopkins University, Baltimore. Dr. Melia reported conducting studies for which his institution received funding from Merck Sharpe & Dohme, Janssen, Gilead, Bristol-Myers Squibb, and AbbVie. Dr. Auwaerter reported ties to Biomerieux and being a member of the Infectious Diseases Society of America’s panel currently updating the organization’s clinical practice guideline for Lyme disease. Dr. Melia and Dr. Auwaerter made these remarks in an editorial accompanying Dr. Berende’s report (N Engl J Med. 2016;374[13]:1277-8).
This well-performed study should reduce the temptation among clinicians to prescribe prolonged courses of antibiotics for persistent Lyme symptoms “just in case” they might help.
Long-term antibiotics are not benign. Even though the adverse effects in this study were mostly minor, 68.6% of patients taking doxycycline or clarithromycin-hydroxychloroquine reported at least one adverse reaction judged to be drug related.
Dr. Michael T. Melia and Dr. Paul G. Auwaerter are at the Sherilyn and Ken Fisher Center for Environmental Infectious Diseases at Johns Hopkins University, Baltimore. Dr. Melia reported conducting studies for which his institution received funding from Merck Sharpe & Dohme, Janssen, Gilead, Bristol-Myers Squibb, and AbbVie. Dr. Auwaerter reported ties to Biomerieux and being a member of the Infectious Diseases Society of America’s panel currently updating the organization’s clinical practice guideline for Lyme disease. Dr. Melia and Dr. Auwaerter made these remarks in an editorial accompanying Dr. Berende’s report (N Engl J Med. 2016;374[13]:1277-8).
This well-performed study should reduce the temptation among clinicians to prescribe prolonged courses of antibiotics for persistent Lyme symptoms “just in case” they might help.
Long-term antibiotics are not benign. Even though the adverse effects in this study were mostly minor, 68.6% of patients taking doxycycline or clarithromycin-hydroxychloroquine reported at least one adverse reaction judged to be drug related.
Dr. Michael T. Melia and Dr. Paul G. Auwaerter are at the Sherilyn and Ken Fisher Center for Environmental Infectious Diseases at Johns Hopkins University, Baltimore. Dr. Melia reported conducting studies for which his institution received funding from Merck Sharpe & Dohme, Janssen, Gilead, Bristol-Myers Squibb, and AbbVie. Dr. Auwaerter reported ties to Biomerieux and being a member of the Infectious Diseases Society of America’s panel currently updating the organization’s clinical practice guideline for Lyme disease. Dr. Melia and Dr. Auwaerter made these remarks in an editorial accompanying Dr. Berende’s report (N Engl J Med. 2016;374[13]:1277-8).
Long-term is no better than standard antibiotic therapy for persistent symptoms of Lyme disease, according to a report published online March 30 in the New England Journal of Medicine.
Randomized clinical trials have never shown convincingly that prolonged antibiotic therapy is beneficial for the many patients with Lyme disease who have persistent debilitating symptoms such as musculoskeletal pain, arthritis, arthralgia, neuralgia, sensory disturbances, dysesthesia, neuropsychological disorders, cognitive disorders, and fatigue. But some less rigorous studies have reported beneficial effects with prolonged antibiotics, and some guidelines endorse that approach, said Dr. Anneleen Berende of the Center for Infectious Diseases at Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
They performed a randomized, double-blind clinical trial, the Persistent Lyme Empiric Antibiotic Study Europe (PLEASE), in which 280 adults (mean age, 49 years) received daily 2,000-mg open-label IV ceftriaxone for 14 days and then were assigned to receive 100 mg oral doxycycline twice daily plus placebo (86 patients), combined 500 mg clarithromycin twice daily plus 200 mg hydroxychloroquine twice daily (96 patients), or two placebo capsules twice daily (98 patients) for 12 weeks. Patients were eligible for the trial if their persistent symptoms were temporally related to an erythema migrans rash or an otherwise proven case of symptomatic Lyme disease or were accompanied by Borrelia burgdorferi IgG or IgM antibodies according to immunoblot assay. They had median durations of symptoms of 2.1-2.7 years. Symptoms were assessed by self-report using the RAND SF-36 Health Status Inventory at baseline, at the end of the 14-week treatment period, and at 26, 40, and 52 weeks.
In the intention-to-treat analysis, the primary outcome measure – health-related quality of life as assessed on the physical component summary score of the RAND SF-36 at 14 weeks – did not differ significantly among the three study groups. The mean physical component summary scores were 35.0 with doxycycline, 35.6 with clarithromycin/hydroxychloroquine, and 34.8 with placebo. In addition, none of the secondary outcome measures, including mental impairment and fatigue, differed significantly among the three study groups, either at the end of treatment or at any subsequent follow-up visit.
The results of all sensitivity analyses, including the per-protocol analysis restricted to the 212 patients most adherent to the study regimen, accorded with those of the main analysis, Dr. Berende and her associates said (N Engl J Med. 2016;374[13]:1209-20).
“At the 14-week visit at the end of the treatment period, the mean SF-36 physical component summary score had improved significantly from baseline regardless of the study group assignment, but quality of life remained below that of the general population,” they noted.
Nearly three-fourths of patients reported at least one adverse event of a given type during the open-label and randomized phases combined, and approximately half reported adverse events during the randomized phase without any significant difference in rate across the groups. Patients taking doxycycline reported photosensitivity and nausea most often, and patients taking clarithromycin-hydroxychloroquine reported nausea, diarrhea, and rash most often. Fourteen patients (5.0%) discontinued the intervention because of adverse effects, and the number was similar across the three study groups.
This study was supported by the Netherlands Organization for Health Research and Development (ZonMw). Dr. Berende reported having no relevant financial disclosures; one of her associates reported inventing a patented cellular diagnostic test for Lyme disease.
Long-term is no better than standard antibiotic therapy for persistent symptoms of Lyme disease, according to a report published online March 30 in the New England Journal of Medicine.
Randomized clinical trials have never shown convincingly that prolonged antibiotic therapy is beneficial for the many patients with Lyme disease who have persistent debilitating symptoms such as musculoskeletal pain, arthritis, arthralgia, neuralgia, sensory disturbances, dysesthesia, neuropsychological disorders, cognitive disorders, and fatigue. But some less rigorous studies have reported beneficial effects with prolonged antibiotics, and some guidelines endorse that approach, said Dr. Anneleen Berende of the Center for Infectious Diseases at Radboud University Medical Center, Nijmegen, the Netherlands, and her associates.
They performed a randomized, double-blind clinical trial, the Persistent Lyme Empiric Antibiotic Study Europe (PLEASE), in which 280 adults (mean age, 49 years) received daily 2,000-mg open-label IV ceftriaxone for 14 days and then were assigned to receive 100 mg oral doxycycline twice daily plus placebo (86 patients), combined 500 mg clarithromycin twice daily plus 200 mg hydroxychloroquine twice daily (96 patients), or two placebo capsules twice daily (98 patients) for 12 weeks. Patients were eligible for the trial if their persistent symptoms were temporally related to an erythema migrans rash or an otherwise proven case of symptomatic Lyme disease or were accompanied by Borrelia burgdorferi IgG or IgM antibodies according to immunoblot assay. They had median durations of symptoms of 2.1-2.7 years. Symptoms were assessed by self-report using the RAND SF-36 Health Status Inventory at baseline, at the end of the 14-week treatment period, and at 26, 40, and 52 weeks.
In the intention-to-treat analysis, the primary outcome measure – health-related quality of life as assessed on the physical component summary score of the RAND SF-36 at 14 weeks – did not differ significantly among the three study groups. The mean physical component summary scores were 35.0 with doxycycline, 35.6 with clarithromycin/hydroxychloroquine, and 34.8 with placebo. In addition, none of the secondary outcome measures, including mental impairment and fatigue, differed significantly among the three study groups, either at the end of treatment or at any subsequent follow-up visit.
The results of all sensitivity analyses, including the per-protocol analysis restricted to the 212 patients most adherent to the study regimen, accorded with those of the main analysis, Dr. Berende and her associates said (N Engl J Med. 2016;374[13]:1209-20).
“At the 14-week visit at the end of the treatment period, the mean SF-36 physical component summary score had improved significantly from baseline regardless of the study group assignment, but quality of life remained below that of the general population,” they noted.
Nearly three-fourths of patients reported at least one adverse event of a given type during the open-label and randomized phases combined, and approximately half reported adverse events during the randomized phase without any significant difference in rate across the groups. Patients taking doxycycline reported photosensitivity and nausea most often, and patients taking clarithromycin-hydroxychloroquine reported nausea, diarrhea, and rash most often. Fourteen patients (5.0%) discontinued the intervention because of adverse effects, and the number was similar across the three study groups.
This study was supported by the Netherlands Organization for Health Research and Development (ZonMw). Dr. Berende reported having no relevant financial disclosures; one of her associates reported inventing a patented cellular diagnostic test for Lyme disease.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Long-term is no better than standard antibiotic therapy for persistent symptoms of Lyme disease.
Major finding: After 14 weeks of treatment, the mean physical component summary scores on the SF-36 were 35.0 with doxycycline, 35.6 with clarithromycin/hydroxychloroquine, and 34.8 with placebo.
Data source: A randomized, double-blind trial involving 280 patients in the Netherlands followed for 1 year.
Disclosures: This study was supported by the Netherlands Organization for Health Research and Development (ZonMw). Dr. Berende reported having no relevant financial disclosures; one of her associates reported inventing a patented cellular diagnostic test for Lyme disease.
Only ‘early’ estradiol limits atherosclerosis progression
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Despite the favorable effect of estrogen on atherosclerosis in early postmenopausal women in the ELITE trial, the relevance of these results to clinical coronary heart disease events remains questionable. The trial assessed only surrogate measures of coronary heart disease and was not designed or powered to assess clinical events. The occurrence of myocardial infarction and stroke involves not only atherosclerotic plaque formation but also plaque rupture and thrombosis. Any changes in these latter two phenomena would not be captured by the CIMT measurements in ELITE — a point of particular interest, given that postmenopausal hormone therapy may promote thrombosis and inflammation. A final caution is that the available clinical data in support of the timing hypothesis are suggestive but inconsistent.
Guidelines from various professional organizations currently caution against using postmenopausal hormone therapy for the purpose of preventing cardiovascular events. Although the ELITE trial results support the hypothesis that postmenopausal hormone therapy may have more favorable effects on atherosclerosis when initiated soon after menopause, extrapolation of these results to clinical events would be premature, and the present guidance remains prudent.
Dr. John F. Keaney, Jr., is at the University of Massachusetts, Worcester and is an associate editor at the New England Journal of Medicine, and Dr. Caren G. Solomon is a deputy editor at the New England Journal of Medicine. They reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (N Engl J Med. 2016 Mar 30. doi: 10.1056/NEJMe1602846).
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Hormone therapy – estradiol with or without progesterone – only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause onset, according to a report published online March 30 in the New England Journal of Medicine.
The “hormone-timing hypothesis” posits that hormone therapy’s beneficial effects on atherosclerosis depend on the timing of initiating that therapy relative to menopause. To test this hypothesis, researchers began the ELITE study (Early versus Late Intervention Trial with Estradiol) in 2002, using serial noninvasive measurements of carotid-artery intima-media thickness (CIMT) as a marker of atherosclerosis progression.
Several other studies since 2002 have reported that the timing hypothesis appears to be valid, wrote Dr. Howard N. Hodis of the Atherosclerosis Research Unit, University of Southern California, Los Angeles, and his associates.
Their single-center trial involved 643 healthy postmenopausal women who had no diabetes and no evidence of cardiovascular disease at baseline, and who were randomly assigned to receive either daily oral estradiol or a matching placebo for 5 years. Women who had an intact uterus and took active estradiol also received a 4% micronized progesterone vaginal gel, while those who had an intact uterus and took placebo also received a matching placebo gel.
The participants were stratified according to the number of years they were past menopause: less than 6 years (271 women in the “early” group) or more than 10 years (372 in the “late” group).
A total of 137 women in the early group and 186 women in the late group were assigned to active estradiol, while 134 women in the early group and 186 women in the late group were assigned to placebo. As expected, serum estradiol levels were at least 3 times higher among women assigned to active treatment, compared with those assigned to placebo.
The primary outcome – the effect of hormone therapy on CIMT progression – differed by timing of the initiation of treatment. In the “early” group, the mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo.
In contrast, in the “late” group, the rates of CIMT progression were not significantly different between estradiol and placebo, the investigators wrote (N Engl J Med. 2016;374:1221-31. doi: 10.1056/NEJMoa1505241).
This beneficial effect remained significant in a sensitivity analysis restricted only to study participants who showed at least 80% adherence to their assigned treatment. The benefit also remained significant in a post-hoc analysis comparing women who took estradiol alone against those who took estradiol plus progestogen, as well as in a separate analysis comparing women who used lipid-lowering and/or hypertensive medications against those who did not.
The findings add further evidence in favor of the hormone timing hypothesis. The effect of estradiol therapy on CIMT progression was significantly modified by time since menopause (P = .007 for the interaction), the researchers wrote.
Cardiac computer tomography (CT) was used as a different method of assessing coronary atherosclerosis in a subgroup of 167 women in the early group (88 receiving estradiol and 79 receiving placebo) and 214 in the late group (101 receiving estradiol and 113 receiving placebo). The timing of estradiol treatment did not affect coronary artery calcium and other cardiac CT measures. This is consistent with previous reports that hormone therapy has no significant effect on established lesions in the coronary arteries, the researchers wrote.
The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Estradiol only limits the progression of subclinical atherosclerosis if it is initiated within 6 years of menopause, not later.
Major finding: The mean CIMT progression rate was decreased by 0.0034 mm per year with estradiol, compared with placebo, but only in women who initiated hormone therapy within 6 years of menopause onset.
Data source: A single-center randomized, double-blind, placebo-controlled trial involving 643 healthy postmenopausal women treated for 5 years.
Disclosures: The ELITE trial was funded by the National Institute on Aging. Dr. Hodis reported having no relevant financial disclosures; two of his associates reported ties to GE and TherapeuticsMD.
Endometriosis Linked to Higher CHD Risk
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Endometriosis linked to higher CHD risk
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Endometriosis is associated with a significantly increased risk of coronary heart disease.
Major finding: Women with endometriosis showed increased relative risks for MI (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73).
Data source: A secondary analysis of data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women followed for 20 years.
Disclosures: The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Crizotinib bests chemo at controlling brain metastases in advanced NSCLC
Crizotinib achieved better control of brain metastases then chemotherapy in a manufacturer-sponsored international open-label phase III randomized trial involving 343 patients with advanced non–small-cell lung cancer (NSCLC), according to a report published March 28 in the Journal of Clinical Oncology.
Even though targeted therapies have greatly improved outcomes for patients whose NSCLC is associated with oncogenic driver mutations, brain metastases remain “a significant clinical problem, resulting in considerable physical and neurocognitive morbidity as well as mortality.” In addition, as patients live longer because of these targeted treatments, the proportion who have brain metastases rises, “such that up to 50% of patients alive at 2 years with EGFR- [epidermal growth factor receptor]–mutated or ALK- [anaplastic lymphoma kinase]–rearranged lung cancer will have brain metastases,” according to Dr. Benjamin J. Solomon of the department of medical oncology, Peter MacCallum Cancer Centre, Melbourne, and his associates.
They compared the efficacy of intracranial disease control between oral crizotinib and IV pemetrexed-platinum chemotherapy in patients who had advanced nonsquamous ALK-positive NSCLC. A total of 79 of these patients (23%) had brain metastases at baseline.
At 12 weeks, a significantly higher percentage of patients achieved intracranial disease control with crizotinib (85%) than with chemotherapy (45%), and the same was true at 24 weeks (56% vs. 25%). Median progression-free survival also was longer with crizotinib, regardless of whether patients had brain metastases at baseline (9 months vs. 4 months) or did not have brain metastases at baseline (11 months vs. 7 months), Dr. Solomon and his associates said (J Clin Oncol. 2016 Mar 28. doi: 10.1200/JCO.2015.63.5888).
Similarly, the overall response rate was significantly higher with crizotinib, regardless of whether patients had brain metastases at baseline (77% vs. 28%) or did not have brain metastases at baseline (74% vs. 50%). In addition, disease progression was less frequent with crizotinib than with chemotherapy in the overall patient population (52% vs. 77%), in the subgroup of patients who had brain metastases at baseline (54% vs. 75%), and in the subgroup of patients who did not have brain metastases at baseline (52% vs. 78%).
These findings indicate that crizotinib should be the standard first-line therapy for patients who have advanced ALK-positive NSCLC, whether or not they have brain metastases, the investigators said.
Crizotinib achieved better control of brain metastases then chemotherapy in a manufacturer-sponsored international open-label phase III randomized trial involving 343 patients with advanced non–small-cell lung cancer (NSCLC), according to a report published March 28 in the Journal of Clinical Oncology.
Even though targeted therapies have greatly improved outcomes for patients whose NSCLC is associated with oncogenic driver mutations, brain metastases remain “a significant clinical problem, resulting in considerable physical and neurocognitive morbidity as well as mortality.” In addition, as patients live longer because of these targeted treatments, the proportion who have brain metastases rises, “such that up to 50% of patients alive at 2 years with EGFR- [epidermal growth factor receptor]–mutated or ALK- [anaplastic lymphoma kinase]–rearranged lung cancer will have brain metastases,” according to Dr. Benjamin J. Solomon of the department of medical oncology, Peter MacCallum Cancer Centre, Melbourne, and his associates.
They compared the efficacy of intracranial disease control between oral crizotinib and IV pemetrexed-platinum chemotherapy in patients who had advanced nonsquamous ALK-positive NSCLC. A total of 79 of these patients (23%) had brain metastases at baseline.
At 12 weeks, a significantly higher percentage of patients achieved intracranial disease control with crizotinib (85%) than with chemotherapy (45%), and the same was true at 24 weeks (56% vs. 25%). Median progression-free survival also was longer with crizotinib, regardless of whether patients had brain metastases at baseline (9 months vs. 4 months) or did not have brain metastases at baseline (11 months vs. 7 months), Dr. Solomon and his associates said (J Clin Oncol. 2016 Mar 28. doi: 10.1200/JCO.2015.63.5888).
Similarly, the overall response rate was significantly higher with crizotinib, regardless of whether patients had brain metastases at baseline (77% vs. 28%) or did not have brain metastases at baseline (74% vs. 50%). In addition, disease progression was less frequent with crizotinib than with chemotherapy in the overall patient population (52% vs. 77%), in the subgroup of patients who had brain metastases at baseline (54% vs. 75%), and in the subgroup of patients who did not have brain metastases at baseline (52% vs. 78%).
These findings indicate that crizotinib should be the standard first-line therapy for patients who have advanced ALK-positive NSCLC, whether or not they have brain metastases, the investigators said.
Crizotinib achieved better control of brain metastases then chemotherapy in a manufacturer-sponsored international open-label phase III randomized trial involving 343 patients with advanced non–small-cell lung cancer (NSCLC), according to a report published March 28 in the Journal of Clinical Oncology.
Even though targeted therapies have greatly improved outcomes for patients whose NSCLC is associated with oncogenic driver mutations, brain metastases remain “a significant clinical problem, resulting in considerable physical and neurocognitive morbidity as well as mortality.” In addition, as patients live longer because of these targeted treatments, the proportion who have brain metastases rises, “such that up to 50% of patients alive at 2 years with EGFR- [epidermal growth factor receptor]–mutated or ALK- [anaplastic lymphoma kinase]–rearranged lung cancer will have brain metastases,” according to Dr. Benjamin J. Solomon of the department of medical oncology, Peter MacCallum Cancer Centre, Melbourne, and his associates.
They compared the efficacy of intracranial disease control between oral crizotinib and IV pemetrexed-platinum chemotherapy in patients who had advanced nonsquamous ALK-positive NSCLC. A total of 79 of these patients (23%) had brain metastases at baseline.
At 12 weeks, a significantly higher percentage of patients achieved intracranial disease control with crizotinib (85%) than with chemotherapy (45%), and the same was true at 24 weeks (56% vs. 25%). Median progression-free survival also was longer with crizotinib, regardless of whether patients had brain metastases at baseline (9 months vs. 4 months) or did not have brain metastases at baseline (11 months vs. 7 months), Dr. Solomon and his associates said (J Clin Oncol. 2016 Mar 28. doi: 10.1200/JCO.2015.63.5888).
Similarly, the overall response rate was significantly higher with crizotinib, regardless of whether patients had brain metastases at baseline (77% vs. 28%) or did not have brain metastases at baseline (74% vs. 50%). In addition, disease progression was less frequent with crizotinib than with chemotherapy in the overall patient population (52% vs. 77%), in the subgroup of patients who had brain metastases at baseline (54% vs. 75%), and in the subgroup of patients who did not have brain metastases at baseline (52% vs. 78%).
These findings indicate that crizotinib should be the standard first-line therapy for patients who have advanced ALK-positive NSCLC, whether or not they have brain metastases, the investigators said.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Crizotinib achieved better control of brain metastases than chemotherapy in advanced NSCLC.
Major finding: A significantly higher percentage of study participants achieved intracranial disease control with crizotinib (85%) than with chemotherapy (45%) at 12 weeks and at 24 weeks (56% vs. 25%).
Data source: An ongoing international open-label phase III randomized trial involving 343 patients.
Disclosures: This study was supported by Pfizer. Dr. Solomon reported ties to Pfizer and other industry sources; his associates also reported ties to numerous industry sources.
Hormonal Birth Control Doesn’t Induce VTE Recurrence
Hormonal contraceptives don’t appear to increase the risk of recurrence of venous thromboembolism among women taking anticoagulants, according to a report published in Blood.
Clinicians are often reluctant to prescribe hormonal contraceptives for women who develop venous thromboembolism (VTE) because the drugs are known to raise the risk of VTE and are considered to be contraindicated in either active or previous VTE. But effective contraception is necessary for women of childbearing age who are taking anticoagulants, because these drugs cross the placenta and could cause fetal bleeding and other adverse events, wrote Dr. Ida Martinelli of the A. Bianchi Bonomi Hemophilia and Thrombosis Center, Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico, Milan, and her associates (Blood 2016;127[11]:1417-25).
Adding further to the confusion, World Health Organization guidelines state that estrogen-containing contraceptives confer “an unacceptable health risk” during anticoagulant therapy for VTE, but the International Society on Thrombosis and Haemostasis recommends that women diagnosed with VTE continue oral contraceptive and estrogen-replacement hormonal therapy until they discontinue anticoagulant therapy “because any prothrombotic effect of hormonal therapy is likely to be suppressed by therapeutic-intensity anticoagulation,” the investigators noted.
In the current study, the investigators performed a secondary analysis of data accrued in two large trials evaluating rivaroxaban versus enoxaparin plus vitamin K antagonists, which involved 1,888 women younger than age 60 (mean age, 41 years) who were being treated for acute deep vein thrombosis or acute pulmonary embolism. A total of 402 of these women used hormonal therapy during the 4-year studies.
There were 7 VTE recurrences during hormonal contraceptive use and 38 without hormonal contraceptive use. The incidence densities were 3.7% per year with hormonal therapy and 4.7% per year without it, for a hazard ratio of 0.56.
This indicates that hormonal contraceptive use did not make a clinically important difference in the rate of VTE recurrence. Moreover, these findings were consistent regardless of whether the contraceptives contained estrogen (incidence density, 3.7% per year) or progestin only (incidence density, 3.8% per year), and remained consistent in sensitivity analyses.
“These results challenge the WHO guidelines and instead support the International Society on Thrombosis and Haemostasis recommendations,” the investigators wrote.
“Our finding of similar risks of recurrent VTE for women who did or did not receive hormonal therapy, whether progestin-only or estrogen-containing therapy, supports a treatment selection that incorporates patient preference, including the choice of estrogen-containing contraception,” they added.
The study was funded in part by Bayer Healthcare Pharmaceuticals, which also provided editorial assistance. Dr. Martinelli reported having no relevant financial disclosures; her associates reported ties to numerous industry sources.
Martinelli et al. provide reassurance that women taking anticoagulants for VTE may safely use estrogen- or progestin-containing hormonal therapy, although it is important to note that their conclusions are based on only seven events (four with estrogen-containing and three with progestin-containing drugs).
Another important finding was that excessive uterine bleeding was more than twice as common among women taking rivaroxaban as among those taking enoxaparin plus vitamin K antagonists. Patients should be informed of this when they initiate anticoagulation.
Dr. Sam Schulman is in the division of hematology and thromboembolism at McMaster University, Hamilton, Ont. He reported receiving honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, and Daiichi. These comments are adapted from an accompanying editorial (Blood 2016;127[11]:1378-9).
Martinelli et al. provide reassurance that women taking anticoagulants for VTE may safely use estrogen- or progestin-containing hormonal therapy, although it is important to note that their conclusions are based on only seven events (four with estrogen-containing and three with progestin-containing drugs).
Another important finding was that excessive uterine bleeding was more than twice as common among women taking rivaroxaban as among those taking enoxaparin plus vitamin K antagonists. Patients should be informed of this when they initiate anticoagulation.
Dr. Sam Schulman is in the division of hematology and thromboembolism at McMaster University, Hamilton, Ont. He reported receiving honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, and Daiichi. These comments are adapted from an accompanying editorial (Blood 2016;127[11]:1378-9).
Martinelli et al. provide reassurance that women taking anticoagulants for VTE may safely use estrogen- or progestin-containing hormonal therapy, although it is important to note that their conclusions are based on only seven events (four with estrogen-containing and three with progestin-containing drugs).
Another important finding was that excessive uterine bleeding was more than twice as common among women taking rivaroxaban as among those taking enoxaparin plus vitamin K antagonists. Patients should be informed of this when they initiate anticoagulation.
Dr. Sam Schulman is in the division of hematology and thromboembolism at McMaster University, Hamilton, Ont. He reported receiving honoraria from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, and Daiichi. These comments are adapted from an accompanying editorial (Blood 2016;127[11]:1378-9).
Hormonal contraceptives don’t appear to increase the risk of recurrence of venous thromboembolism among women taking anticoagulants, according to a report published in Blood.
Clinicians are often reluctant to prescribe hormonal contraceptives for women who develop venous thromboembolism (VTE) because the drugs are known to raise the risk of VTE and are considered to be contraindicated in either active or previous VTE. But effective contraception is necessary for women of childbearing age who are taking anticoagulants, because these drugs cross the placenta and could cause fetal bleeding and other adverse events, wrote Dr. Ida Martinelli of the A. Bianchi Bonomi Hemophilia and Thrombosis Center, Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico, Milan, and her associates (Blood 2016;127[11]:1417-25).
Adding further to the confusion, World Health Organization guidelines state that estrogen-containing contraceptives confer “an unacceptable health risk” during anticoagulant therapy for VTE, but the International Society on Thrombosis and Haemostasis recommends that women diagnosed with VTE continue oral contraceptive and estrogen-replacement hormonal therapy until they discontinue anticoagulant therapy “because any prothrombotic effect of hormonal therapy is likely to be suppressed by therapeutic-intensity anticoagulation,” the investigators noted.
In the current study, the investigators performed a secondary analysis of data accrued in two large trials evaluating rivaroxaban versus enoxaparin plus vitamin K antagonists, which involved 1,888 women younger than age 60 (mean age, 41 years) who were being treated for acute deep vein thrombosis or acute pulmonary embolism. A total of 402 of these women used hormonal therapy during the 4-year studies.
There were 7 VTE recurrences during hormonal contraceptive use and 38 without hormonal contraceptive use. The incidence densities were 3.7% per year with hormonal therapy and 4.7% per year without it, for a hazard ratio of 0.56.
This indicates that hormonal contraceptive use did not make a clinically important difference in the rate of VTE recurrence. Moreover, these findings were consistent regardless of whether the contraceptives contained estrogen (incidence density, 3.7% per year) or progestin only (incidence density, 3.8% per year), and remained consistent in sensitivity analyses.
“These results challenge the WHO guidelines and instead support the International Society on Thrombosis and Haemostasis recommendations,” the investigators wrote.
“Our finding of similar risks of recurrent VTE for women who did or did not receive hormonal therapy, whether progestin-only or estrogen-containing therapy, supports a treatment selection that incorporates patient preference, including the choice of estrogen-containing contraception,” they added.
The study was funded in part by Bayer Healthcare Pharmaceuticals, which also provided editorial assistance. Dr. Martinelli reported having no relevant financial disclosures; her associates reported ties to numerous industry sources.
Hormonal contraceptives don’t appear to increase the risk of recurrence of venous thromboembolism among women taking anticoagulants, according to a report published in Blood.
Clinicians are often reluctant to prescribe hormonal contraceptives for women who develop venous thromboembolism (VTE) because the drugs are known to raise the risk of VTE and are considered to be contraindicated in either active or previous VTE. But effective contraception is necessary for women of childbearing age who are taking anticoagulants, because these drugs cross the placenta and could cause fetal bleeding and other adverse events, wrote Dr. Ida Martinelli of the A. Bianchi Bonomi Hemophilia and Thrombosis Center, Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico, Milan, and her associates (Blood 2016;127[11]:1417-25).
Adding further to the confusion, World Health Organization guidelines state that estrogen-containing contraceptives confer “an unacceptable health risk” during anticoagulant therapy for VTE, but the International Society on Thrombosis and Haemostasis recommends that women diagnosed with VTE continue oral contraceptive and estrogen-replacement hormonal therapy until they discontinue anticoagulant therapy “because any prothrombotic effect of hormonal therapy is likely to be suppressed by therapeutic-intensity anticoagulation,” the investigators noted.
In the current study, the investigators performed a secondary analysis of data accrued in two large trials evaluating rivaroxaban versus enoxaparin plus vitamin K antagonists, which involved 1,888 women younger than age 60 (mean age, 41 years) who were being treated for acute deep vein thrombosis or acute pulmonary embolism. A total of 402 of these women used hormonal therapy during the 4-year studies.
There were 7 VTE recurrences during hormonal contraceptive use and 38 without hormonal contraceptive use. The incidence densities were 3.7% per year with hormonal therapy and 4.7% per year without it, for a hazard ratio of 0.56.
This indicates that hormonal contraceptive use did not make a clinically important difference in the rate of VTE recurrence. Moreover, these findings were consistent regardless of whether the contraceptives contained estrogen (incidence density, 3.7% per year) or progestin only (incidence density, 3.8% per year), and remained consistent in sensitivity analyses.
“These results challenge the WHO guidelines and instead support the International Society on Thrombosis and Haemostasis recommendations,” the investigators wrote.
“Our finding of similar risks of recurrent VTE for women who did or did not receive hormonal therapy, whether progestin-only or estrogen-containing therapy, supports a treatment selection that incorporates patient preference, including the choice of estrogen-containing contraception,” they added.
The study was funded in part by Bayer Healthcare Pharmaceuticals, which also provided editorial assistance. Dr. Martinelli reported having no relevant financial disclosures; her associates reported ties to numerous industry sources.
FROM BLOOD