User login
Embolic protection cut lesions, did not aid neurocognition
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
The 5-day “window” for MRI assessment having been too long was among the study’s limitations, Dr. Kapadia said.
Claret Medical funded the study and Dr. Kapadia’s associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
The authors have demonstrated the safety of cerebral protection systems, but not their clinical benefit in terms of preventing adverse neurological outcomes. As they note, a larger study group might produce a statistical difference. Commentary on the added cost of the device would be helpful to weigh their cost effectiveness.
The authors have demonstrated the safety of cerebral protection systems, but not their clinical benefit in terms of preventing adverse neurological outcomes. As they note, a larger study group might produce a statistical difference. Commentary on the added cost of the device would be helpful to weigh their cost effectiveness.
The authors have demonstrated the safety of cerebral protection systems, but not their clinical benefit in terms of preventing adverse neurological outcomes. As they note, a larger study group might produce a statistical difference. Commentary on the added cost of the device would be helpful to weigh their cost effectiveness.
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
The 5-day “window” for MRI assessment having been too long was among the study’s limitations, Dr. Kapadia said.
Claret Medical funded the study and Dr. Kapadia’s associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
The largest randomized clinical trial to assess the safety and efficacy of cerebral embolic protection systems during transcatheter aortic valve replacement yielded puzzling and somewhat contradictory results, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
Virtually every device in this industry-sponsored study involving 363 elderly patients (mean age, 83.4 years) with severe aortic stenosis trapped particulate debris as intended, the mean volume of new lesions in the protected areas of the brain was reduced by 42%, and the number and volume of new lesions correlated with neurocognitive outcomes at 30 days.
However, the reduction in lesion volume did not achieve statistical significance, and the improvement in neurocognitive function also did not reach statistical significance.
In addition, “the sample size was clearly too low to assess clinical outcomes, and in retrospect, was also too low to evaluate follow-up MRI findings or neurocognitive outcomes.” Nevertheless, the trial “provides reassuring evidence of device safety,” said Samir R. Kapadia, MD, of the Cleveland Clinic (J Am Coll Cardiol. 2016 Nov 1. doi: 10.1016/j.jacc.2016.10.023).
In this prospective study, the investigators assessed patients at 17 medical centers in the United States and 2 in Germany. In addition to being elderly, the study patients were at high risk because of frequent comorbidities, including atrial fibrillation (31.7%) and prior stroke (5.8%).
The remaining 123 patients underwent TAVR but not MRI in a safety arm of the trial.
The protection devices were placed “without safety concerns” in most patients. The rate of major adverse events with the device was 7.3%, markedly less than the 18.3% prespecified performance goal for this outcome. Total procedure time was lengthened by only 13 minutes when the device was used, and total fluoroscopy time was increased by only 3 minutes. These findings demonstrate the overall safety of using the device, Dr. Kapadia said.
Debris including thrombus with tissue elements, artery wall particles, calcifications, valve tissue, and foreign materials was retrieved from the filters in 99% of patients.
The mean volume of new cerebral lesions in areas of the brain protected by the device was reduced by 42%, compared with that in patients who underwent TAVR without the protection device. However, this reduction was not statistically significant, so the primary efficacy endpoint of the study was not met.
Similarly, neurocognitive testing at 30 days showed that the volume of new lesions correlated with poorer outcomes. However, the difference in neurocognitive function between the intervention group and the control group did not reach statistical significance.
The 5-day “window” for MRI assessment having been too long was among the study’s limitations, Dr. Kapadia said.
Claret Medical funded the study and Dr. Kapadia’s associates reported numerous ties to industry sources. The meeting was sponsored by the Cardiovascular Research Foundation.
Cerebral protection in TAVI cuts ischemic lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Hypothermia does not provide neuroprotection during convulsive status epilepticus
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group.
Data source: An open-label, multicenter, randomized controlled trial involving 268 consecutive adults treated at 11 ICUs in France during a 4-year period.
Disclosures: This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
January 2017: Click for Credit
Here are 5 articles in the January issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Gluten-free Adherence Triples While Celiac Disease Prevalence Remains Stable
To take the posttest, go to: http://bit.ly/2h2LFDu
Expires September 6, 2017
2. Fluoxetine Appears Safer for Bone Health in At-risk Older Patients
To take the posttest, go to: http://bit.ly/2he1FTD
Expires September 15, 2017
3. High Free T4 Levels Linked to Sudden Cardiac Death
To take the posttest, go to: http://bit.ly/2gMJqUz
Expires September 16, 2017
4. Morning Sickness Linked to Lower Risk for Pregnancy Loss
To take the posttest, go to: http://bit.ly/2uaWMkH
Expires September 26, 2017
5. Anxiety, Depression May Precede Parkinson's by 25 Years
To take the posttest, go to: http://bit.ly/2gMFQtr
Expires September 27, 2017
Here are 5 articles in the January issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Gluten-free Adherence Triples While Celiac Disease Prevalence Remains Stable
To take the posttest, go to: http://bit.ly/2h2LFDu
Expires September 6, 2017
2. Fluoxetine Appears Safer for Bone Health in At-risk Older Patients
To take the posttest, go to: http://bit.ly/2he1FTD
Expires September 15, 2017
3. High Free T4 Levels Linked to Sudden Cardiac Death
To take the posttest, go to: http://bit.ly/2gMJqUz
Expires September 16, 2017
4. Morning Sickness Linked to Lower Risk for Pregnancy Loss
To take the posttest, go to: http://bit.ly/2uaWMkH
Expires September 26, 2017
5. Anxiety, Depression May Precede Parkinson's by 25 Years
To take the posttest, go to: http://bit.ly/2gMFQtr
Expires September 27, 2017
Here are 5 articles in the January issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Gluten-free Adherence Triples While Celiac Disease Prevalence Remains Stable
To take the posttest, go to: http://bit.ly/2h2LFDu
Expires September 6, 2017
2. Fluoxetine Appears Safer for Bone Health in At-risk Older Patients
To take the posttest, go to: http://bit.ly/2he1FTD
Expires September 15, 2017
3. High Free T4 Levels Linked to Sudden Cardiac Death
To take the posttest, go to: http://bit.ly/2gMJqUz
Expires September 16, 2017
4. Morning Sickness Linked to Lower Risk for Pregnancy Loss
To take the posttest, go to: http://bit.ly/2uaWMkH
Expires September 26, 2017
5. Anxiety, Depression May Precede Parkinson's by 25 Years
To take the posttest, go to: http://bit.ly/2gMFQtr
Expires September 27, 2017
Diabetes, ischemic heart disease, pain lead health spending
Diabetes, ischemic heart disease, and back and neck pain are the top three conditions accounting for the highest spending on personal health care in the United States, according to a report published online Dec. 27 in JAMA.
In addition, spending on pharmaceuticals – particularly diabetes therapies, antihypertensive drugs, and medications for hyperlipidemia – drove much of the massive increase in health care spending during the past 2 decades, said Joseph L. Dieleman, PhD, of the Institute for Health Metrics and Evaluation, University of Washington, Seattle, and his associates.
Recent increases in health care spending are well documented, but less is known about what is spent for individual conditions, in different health care settings, and in various patient age groups. To assess health care spending across these categories, the investigators collected and analyzed data for 1996 through 2013 from nationally representative surveys of households, nationally representative surveys of medical facilities, insurance claims, government budgets, and other official records.
They grouped the data into six type-of-care categories: inpatient care, ambulatory care, emergency department care, nursing facility care, dental care, and prescribed pharmaceuticals. “Spending on the six types of personal health care was then disaggregated across 155 mutually exclusive and collectively exhaustive conditions and 38 age and sex groups,” with each sex being divided into 5-year age groups, the researchers noted.
Based on these data, the investigators came to the following conclusions:
• Twenty conditions accounted for approximately 58% of personal health care spending, which totaled an estimated $1.2 trillion in 2013.
• More resources were spent on diabetes than any other condition in 2013, at an estimated $101.4 billion. Prescribed medications accounted for nearly 60% of diabetes costs.
• The second-highest amount of health care spending was for ischemic heart disease, which accounted for $88.1 billion in 2013. Most such spending occurred in inpatient settings.
• Low-back and neck pain, comprising the third-highest level of spending, cost an estimated $87.6 billion. Approximately 60% of this spending occurred in ambulatory settings.
• Among all 155 conditions, spending for diabetes and low-back and neck pain increased the most during the 18-year study period.
• Among all six types of care, spending on pharmaceuticals and emergency care increased the most during the study period.
It is important to note that for the purposes of this study, cancer was disaggregated into 29 separate conditions, and none of them placed in the top 20 for health care spending, Dr. Dieleman and his associates noted (JAMA. 2016;316[24]:2627-46. doi: 10.1001/jama.2016.16885).
When spending was categorized by patient age groups, working-age adults accounted for the greatest amount spent in 2013, estimated at $1,070.1 billion. But that was followed closely by patients aged 65 and older, who accounted for an estimated $796.5 billion, much of which was spent on care in nursing facilities. The smallest amount of health care spending was in children over age 1 and adolescents, who accounted for an estimated $233.5 billion.
Among the other study findings:
• Spending on pharmaceutical treatment of two conditions, hypertension and hyperlipidemia, increased at more than double the rate of total health care spending. It totaled an estimated $135.7 billion in 2013.
• Other top-20 conditions included falls, depression, skin disorders such as acne and eczema, sense disorders such as vision correction and hearing loss, dental care, urinary disorders, and lower respiratory tract infection.
This work was supported by the National Institute on Aging and the Vitality Institute. Dr. Dieleman and his associates reported having no relevant financial disclosures.
Dieleman et al. have “followed” the health care money, and the trail could ultimately lead to the United States changing how it spends a staggering, almost unimaginable amount – roughly $3.2 trillion in 2015 – on health care.
At the very least, their data indicate that the United States should pay more attention to managing physical pain, controlling the costs of pharmaceuticals, and promoting lifestyle interventions that prevent or ameliorate obesity and other factors contributing to diabetes and heart disease.
Ezekiel J. Emanuel, MD, is provost of the department of medical ethics and health policy at the Perelman School of Medicine and in the department of health care management at The Wharton School, University of Pennsylvania, Philadelphia. He reported receiving speaking fees from numerous industry sources. Dr. Emanuel made these remarks in an editorial comment accompanying Dr. Dieleman’s report (JAMA 2016;316:2604-6. doi: 10.1001/jama.2016.16739).
Dieleman et al. have “followed” the health care money, and the trail could ultimately lead to the United States changing how it spends a staggering, almost unimaginable amount – roughly $3.2 trillion in 2015 – on health care.
At the very least, their data indicate that the United States should pay more attention to managing physical pain, controlling the costs of pharmaceuticals, and promoting lifestyle interventions that prevent or ameliorate obesity and other factors contributing to diabetes and heart disease.
Ezekiel J. Emanuel, MD, is provost of the department of medical ethics and health policy at the Perelman School of Medicine and in the department of health care management at The Wharton School, University of Pennsylvania, Philadelphia. He reported receiving speaking fees from numerous industry sources. Dr. Emanuel made these remarks in an editorial comment accompanying Dr. Dieleman’s report (JAMA 2016;316:2604-6. doi: 10.1001/jama.2016.16739).
Dieleman et al. have “followed” the health care money, and the trail could ultimately lead to the United States changing how it spends a staggering, almost unimaginable amount – roughly $3.2 trillion in 2015 – on health care.
At the very least, their data indicate that the United States should pay more attention to managing physical pain, controlling the costs of pharmaceuticals, and promoting lifestyle interventions that prevent or ameliorate obesity and other factors contributing to diabetes and heart disease.
Ezekiel J. Emanuel, MD, is provost of the department of medical ethics and health policy at the Perelman School of Medicine and in the department of health care management at The Wharton School, University of Pennsylvania, Philadelphia. He reported receiving speaking fees from numerous industry sources. Dr. Emanuel made these remarks in an editorial comment accompanying Dr. Dieleman’s report (JAMA 2016;316:2604-6. doi: 10.1001/jama.2016.16739).
Diabetes, ischemic heart disease, and back and neck pain are the top three conditions accounting for the highest spending on personal health care in the United States, according to a report published online Dec. 27 in JAMA.
In addition, spending on pharmaceuticals – particularly diabetes therapies, antihypertensive drugs, and medications for hyperlipidemia – drove much of the massive increase in health care spending during the past 2 decades, said Joseph L. Dieleman, PhD, of the Institute for Health Metrics and Evaluation, University of Washington, Seattle, and his associates.
Recent increases in health care spending are well documented, but less is known about what is spent for individual conditions, in different health care settings, and in various patient age groups. To assess health care spending across these categories, the investigators collected and analyzed data for 1996 through 2013 from nationally representative surveys of households, nationally representative surveys of medical facilities, insurance claims, government budgets, and other official records.
They grouped the data into six type-of-care categories: inpatient care, ambulatory care, emergency department care, nursing facility care, dental care, and prescribed pharmaceuticals. “Spending on the six types of personal health care was then disaggregated across 155 mutually exclusive and collectively exhaustive conditions and 38 age and sex groups,” with each sex being divided into 5-year age groups, the researchers noted.
Based on these data, the investigators came to the following conclusions:
• Twenty conditions accounted for approximately 58% of personal health care spending, which totaled an estimated $1.2 trillion in 2013.
• More resources were spent on diabetes than any other condition in 2013, at an estimated $101.4 billion. Prescribed medications accounted for nearly 60% of diabetes costs.
• The second-highest amount of health care spending was for ischemic heart disease, which accounted for $88.1 billion in 2013. Most such spending occurred in inpatient settings.
• Low-back and neck pain, comprising the third-highest level of spending, cost an estimated $87.6 billion. Approximately 60% of this spending occurred in ambulatory settings.
• Among all 155 conditions, spending for diabetes and low-back and neck pain increased the most during the 18-year study period.
• Among all six types of care, spending on pharmaceuticals and emergency care increased the most during the study period.
It is important to note that for the purposes of this study, cancer was disaggregated into 29 separate conditions, and none of them placed in the top 20 for health care spending, Dr. Dieleman and his associates noted (JAMA. 2016;316[24]:2627-46. doi: 10.1001/jama.2016.16885).
When spending was categorized by patient age groups, working-age adults accounted for the greatest amount spent in 2013, estimated at $1,070.1 billion. But that was followed closely by patients aged 65 and older, who accounted for an estimated $796.5 billion, much of which was spent on care in nursing facilities. The smallest amount of health care spending was in children over age 1 and adolescents, who accounted for an estimated $233.5 billion.
Among the other study findings:
• Spending on pharmaceutical treatment of two conditions, hypertension and hyperlipidemia, increased at more than double the rate of total health care spending. It totaled an estimated $135.7 billion in 2013.
• Other top-20 conditions included falls, depression, skin disorders such as acne and eczema, sense disorders such as vision correction and hearing loss, dental care, urinary disorders, and lower respiratory tract infection.
This work was supported by the National Institute on Aging and the Vitality Institute. Dr. Dieleman and his associates reported having no relevant financial disclosures.
Diabetes, ischemic heart disease, and back and neck pain are the top three conditions accounting for the highest spending on personal health care in the United States, according to a report published online Dec. 27 in JAMA.
In addition, spending on pharmaceuticals – particularly diabetes therapies, antihypertensive drugs, and medications for hyperlipidemia – drove much of the massive increase in health care spending during the past 2 decades, said Joseph L. Dieleman, PhD, of the Institute for Health Metrics and Evaluation, University of Washington, Seattle, and his associates.
Recent increases in health care spending are well documented, but less is known about what is spent for individual conditions, in different health care settings, and in various patient age groups. To assess health care spending across these categories, the investigators collected and analyzed data for 1996 through 2013 from nationally representative surveys of households, nationally representative surveys of medical facilities, insurance claims, government budgets, and other official records.
They grouped the data into six type-of-care categories: inpatient care, ambulatory care, emergency department care, nursing facility care, dental care, and prescribed pharmaceuticals. “Spending on the six types of personal health care was then disaggregated across 155 mutually exclusive and collectively exhaustive conditions and 38 age and sex groups,” with each sex being divided into 5-year age groups, the researchers noted.
Based on these data, the investigators came to the following conclusions:
• Twenty conditions accounted for approximately 58% of personal health care spending, which totaled an estimated $1.2 trillion in 2013.
• More resources were spent on diabetes than any other condition in 2013, at an estimated $101.4 billion. Prescribed medications accounted for nearly 60% of diabetes costs.
• The second-highest amount of health care spending was for ischemic heart disease, which accounted for $88.1 billion in 2013. Most such spending occurred in inpatient settings.
• Low-back and neck pain, comprising the third-highest level of spending, cost an estimated $87.6 billion. Approximately 60% of this spending occurred in ambulatory settings.
• Among all 155 conditions, spending for diabetes and low-back and neck pain increased the most during the 18-year study period.
• Among all six types of care, spending on pharmaceuticals and emergency care increased the most during the study period.
It is important to note that for the purposes of this study, cancer was disaggregated into 29 separate conditions, and none of them placed in the top 20 for health care spending, Dr. Dieleman and his associates noted (JAMA. 2016;316[24]:2627-46. doi: 10.1001/jama.2016.16885).
When spending was categorized by patient age groups, working-age adults accounted for the greatest amount spent in 2013, estimated at $1,070.1 billion. But that was followed closely by patients aged 65 and older, who accounted for an estimated $796.5 billion, much of which was spent on care in nursing facilities. The smallest amount of health care spending was in children over age 1 and adolescents, who accounted for an estimated $233.5 billion.
Among the other study findings:
• Spending on pharmaceutical treatment of two conditions, hypertension and hyperlipidemia, increased at more than double the rate of total health care spending. It totaled an estimated $135.7 billion in 2013.
• Other top-20 conditions included falls, depression, skin disorders such as acne and eczema, sense disorders such as vision correction and hearing loss, dental care, urinary disorders, and lower respiratory tract infection.
This work was supported by the National Institute on Aging and the Vitality Institute. Dr. Dieleman and his associates reported having no relevant financial disclosures.
FROM JAMA
Key clinical point:
Major finding: More resources were spent on diabetes than any other condition in 2013, at an estimated $101.4 billion.
Data source: A comprehensive estimate of U.S. spending on personal health care, based on information collected from nationally representative surveys of households and medical facilities, government budgets, insurance claims, and official records from 1996 through 2013.
Disclosures: The National Institute on Aging and the Vitality Institute supported the work. Dr. Dieleman and his associates reported having no relevant financial disclosures.
‘Negative’ appendectomy = longer LOS, higher morbidity
Among adults, “negative” appendectomy, or appendectomy in which the surgeon discovers there is no appendicitis, is associated with a prolonged hospital stay, greater morbidity, and higher costs than is curative nonperforated appendectomy, according to a report in the American Journal of Surgery.
“Many argue that negative appendectomy is justified to decrease the risk of perforated appendicitis, as it has been accepted that an inverse relationship exists between the rates of negative appendectomy and perforated appendicitis. However, with the increasing prevalence of preoperative imaging, the rate of negative appendectomy has been decreasing, whereas the rate of perforated appendicitis has remained largely the same,” said Kyle Mock, MD, of the department of surgery, Harbor-University of California Los Angeles Medical Center, and his associates (Am J Surg. 2016;212[6]:1076-82). The study found that the prevalence of negative appendectomy decreased from 4.5% to 2.8% in California from 2005 to 2011, while the prevalence of perforated appendicitis decreased from 23.1% to 21.7%
To examine this issue, Dr. Mock and his associates analyzed information from a statewide California inpatient database, focusing on 180,958 adult appendectomy admissions during a 6-year period. Compared with nonperforated appendectomy, negative appendectomy required an additional 0.8 days in length of stay, was associated with greater morbidity, and cost approximately $1,063 more per patient. Rates of negative appendectomy also did not correlate with rates of appendiceal perforation, so negative appendectomy cannot be said to prevent what otherwise would have been a ruptured appendix.
“Consequently, negative appendectomy should no longer be thought of as a benign procedure,” the investigators said.
It is important to note that patients who undergo negative appendectomy likely have other disease processes underlying their signs and symptoms, and they likely require longer hospitalization and incur greater morbidity and costs to identify and treat these alternative disorders. In contrast, patients who undergo routine appendectomy usually are discharged home the same day, Dr. Mock and his associates added.
This researchers had no financial relationships or sources of support in the form of grants, equipment, or drugs. Dr. Mock and his associates reported having no relevant conflicts of interest.
Among adults, “negative” appendectomy, or appendectomy in which the surgeon discovers there is no appendicitis, is associated with a prolonged hospital stay, greater morbidity, and higher costs than is curative nonperforated appendectomy, according to a report in the American Journal of Surgery.
“Many argue that negative appendectomy is justified to decrease the risk of perforated appendicitis, as it has been accepted that an inverse relationship exists between the rates of negative appendectomy and perforated appendicitis. However, with the increasing prevalence of preoperative imaging, the rate of negative appendectomy has been decreasing, whereas the rate of perforated appendicitis has remained largely the same,” said Kyle Mock, MD, of the department of surgery, Harbor-University of California Los Angeles Medical Center, and his associates (Am J Surg. 2016;212[6]:1076-82). The study found that the prevalence of negative appendectomy decreased from 4.5% to 2.8% in California from 2005 to 2011, while the prevalence of perforated appendicitis decreased from 23.1% to 21.7%
To examine this issue, Dr. Mock and his associates analyzed information from a statewide California inpatient database, focusing on 180,958 adult appendectomy admissions during a 6-year period. Compared with nonperforated appendectomy, negative appendectomy required an additional 0.8 days in length of stay, was associated with greater morbidity, and cost approximately $1,063 more per patient. Rates of negative appendectomy also did not correlate with rates of appendiceal perforation, so negative appendectomy cannot be said to prevent what otherwise would have been a ruptured appendix.
“Consequently, negative appendectomy should no longer be thought of as a benign procedure,” the investigators said.
It is important to note that patients who undergo negative appendectomy likely have other disease processes underlying their signs and symptoms, and they likely require longer hospitalization and incur greater morbidity and costs to identify and treat these alternative disorders. In contrast, patients who undergo routine appendectomy usually are discharged home the same day, Dr. Mock and his associates added.
This researchers had no financial relationships or sources of support in the form of grants, equipment, or drugs. Dr. Mock and his associates reported having no relevant conflicts of interest.
Among adults, “negative” appendectomy, or appendectomy in which the surgeon discovers there is no appendicitis, is associated with a prolonged hospital stay, greater morbidity, and higher costs than is curative nonperforated appendectomy, according to a report in the American Journal of Surgery.
“Many argue that negative appendectomy is justified to decrease the risk of perforated appendicitis, as it has been accepted that an inverse relationship exists between the rates of negative appendectomy and perforated appendicitis. However, with the increasing prevalence of preoperative imaging, the rate of negative appendectomy has been decreasing, whereas the rate of perforated appendicitis has remained largely the same,” said Kyle Mock, MD, of the department of surgery, Harbor-University of California Los Angeles Medical Center, and his associates (Am J Surg. 2016;212[6]:1076-82). The study found that the prevalence of negative appendectomy decreased from 4.5% to 2.8% in California from 2005 to 2011, while the prevalence of perforated appendicitis decreased from 23.1% to 21.7%
To examine this issue, Dr. Mock and his associates analyzed information from a statewide California inpatient database, focusing on 180,958 adult appendectomy admissions during a 6-year period. Compared with nonperforated appendectomy, negative appendectomy required an additional 0.8 days in length of stay, was associated with greater morbidity, and cost approximately $1,063 more per patient. Rates of negative appendectomy also did not correlate with rates of appendiceal perforation, so negative appendectomy cannot be said to prevent what otherwise would have been a ruptured appendix.
“Consequently, negative appendectomy should no longer be thought of as a benign procedure,” the investigators said.
It is important to note that patients who undergo negative appendectomy likely have other disease processes underlying their signs and symptoms, and they likely require longer hospitalization and incur greater morbidity and costs to identify and treat these alternative disorders. In contrast, patients who undergo routine appendectomy usually are discharged home the same day, Dr. Mock and his associates added.
This researchers had no financial relationships or sources of support in the form of grants, equipment, or drugs. Dr. Mock and his associates reported having no relevant conflicts of interest.
Key clinical point: In adults, “negative” appendectomy – appendectomy in which the surgeon discovers there is no appendicitis – is associated with longer length of stay, higher morbidity, and higher costs than curative appendectomy.
Major finding: Compared with nonperforated appendectomy, negative appendectomy required an additional 0.8 days in length of stay, was associated with greater morbidity, and cost approximately $1,063 more per patient.
Data source: An analysis of information regarding 180,958 appendectomies performed during a 6-year period and detailed in a state (California) inpatient database.
Disclosures: The researchers had no financial relationships or sources of support in the form of grants, equipment, or drugs. Dr. Mock and his associates reported having no relevant conflicts of interest.
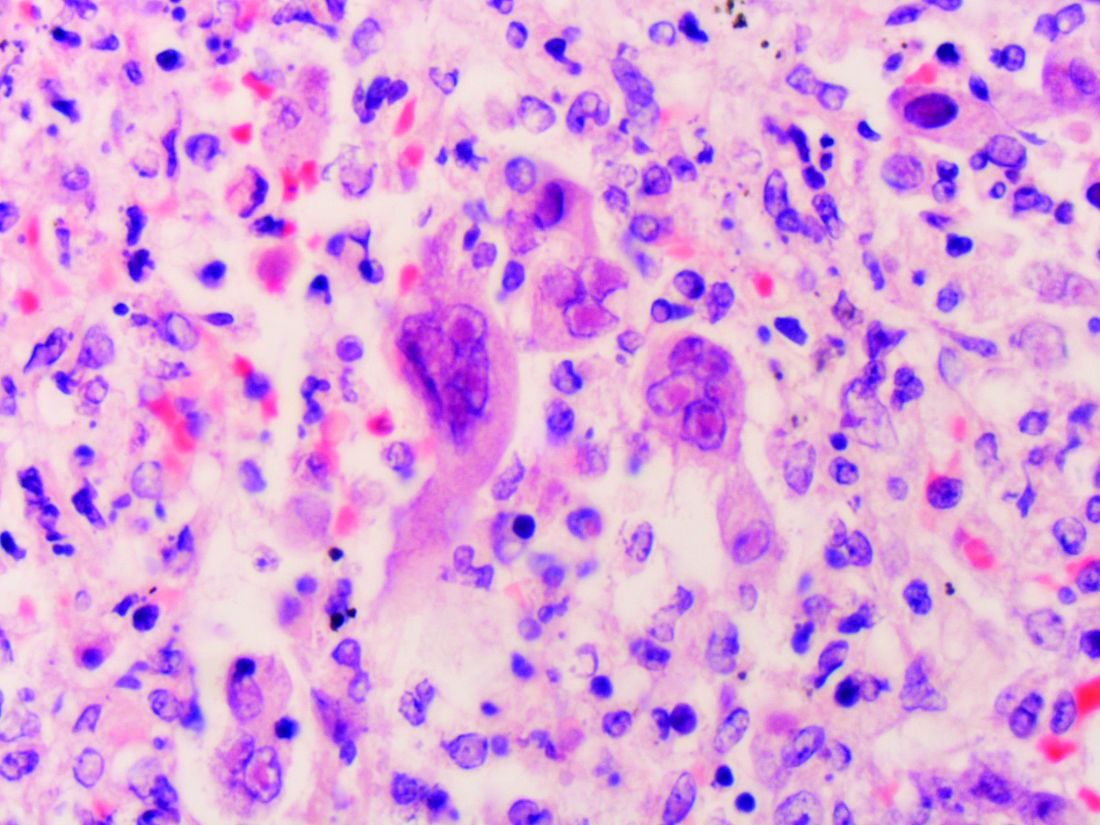
USPSTF nixes routine genital herpes screening
Asymptomatic adolescents and adults, including pregnant women, should not undergo routine serologic screening for genital herpes because the harms of this approach outweigh the benefits, according to an updated US Preventive Services Task Force (USPSTF) Recommendation Statement published online in JAMA.
The USPSTF last addressed screening for herpes simplex virus (HSV) in a 2005 Recommendation Statement, which advised against routine screening of asymptomatic patients at that time. “A small number” of clinical trials examined the issue since then, so the group commissioned a review of the literature through October 2016 to incorporate any new findings into the update, said Kirsten Bibbins-Domingo, MD, PhD, chair of the USPSTF and lead author of the update, and her associates.
Dr. Feltner and her colleagues concluded that current serologic screening tests produce a high rate of false-positive results – as much as 50% – and that those in turn lead to psychosocial harms such as distress and disruption of personal relationships, as well as increased costs and potential medical harm associated with confirmatory testing and unnecessary treatment.
Given the false-positive rates of the most widely used screening tests and the 15% prevalence of genital herpes in the general population, “screening 10,000 persons would result in approximately 1,485 true-positive and 1,445 false-positive results.” Moreover, confirmatory testing is offered only at a single research laboratory, said Dr. Bibbins-Domingo, professor of medicine at the University of California, San Francisco, and her associates on the Task Force.
Based on these findings and given the natural history and epidemiology of genital herpes, they characterized the potential benefits of routine screening as “no greater than small,” and the harms as “at least moderate” (JAMA. 2016 Dec 20;316[23]:2525-30. doi: 10.1001/jama.2016.16776).
The American Academy of Family Physicians, the American College of Obstetrics and Gynecology, and the Centers for Disease Control and Prevention also recommend against routine HSV screening of adolescents and adults, including pregnant women, the investigators noted.
The USPSTF is an independent, voluntary group that evaluates preventive health care services and is funded by the Agency for Healthcare Research and Quality by mandate of the U.S. Congress. The authors’ financial disclosures are available at www.uspreventiveservicestaskforce.org.
[email protected]
On Twitter @idpractitioner
It’s disappointing that the performance of screening tests hasn’t improved during the 10 years since the last USPSTF Recommendation Statement.
These findings should serve as a call to action for federal health agencies and their partners in industry to prioritize the development of better tests and stem the continuing epidemic of genital herpes.
Another important step would be to work vigorously to reduce the pervasive stigma of this disease, which also hinders management and control efforts. The public continues to harbor misperceptions about the severity of genital herpes and the availability of effective treatment, which adds to disproportionate stigmatization of those infected.
Edward W. Hook III, MD, is in the department of microbiology at the University of Alabama at Birmingham. He reported ties to Hologic, Roche Molecular, Becton Dickinson, and Cepheid. Dr. Hook made these remarks in an editorial accompanying the USPSTF Recommendation Statement (JAMA. 2016 Dec 20;316[23]:2493-4).
It’s disappointing that the performance of screening tests hasn’t improved during the 10 years since the last USPSTF Recommendation Statement.
These findings should serve as a call to action for federal health agencies and their partners in industry to prioritize the development of better tests and stem the continuing epidemic of genital herpes.
Another important step would be to work vigorously to reduce the pervasive stigma of this disease, which also hinders management and control efforts. The public continues to harbor misperceptions about the severity of genital herpes and the availability of effective treatment, which adds to disproportionate stigmatization of those infected.
Edward W. Hook III, MD, is in the department of microbiology at the University of Alabama at Birmingham. He reported ties to Hologic, Roche Molecular, Becton Dickinson, and Cepheid. Dr. Hook made these remarks in an editorial accompanying the USPSTF Recommendation Statement (JAMA. 2016 Dec 20;316[23]:2493-4).
It’s disappointing that the performance of screening tests hasn’t improved during the 10 years since the last USPSTF Recommendation Statement.
These findings should serve as a call to action for federal health agencies and their partners in industry to prioritize the development of better tests and stem the continuing epidemic of genital herpes.
Another important step would be to work vigorously to reduce the pervasive stigma of this disease, which also hinders management and control efforts. The public continues to harbor misperceptions about the severity of genital herpes and the availability of effective treatment, which adds to disproportionate stigmatization of those infected.
Edward W. Hook III, MD, is in the department of microbiology at the University of Alabama at Birmingham. He reported ties to Hologic, Roche Molecular, Becton Dickinson, and Cepheid. Dr. Hook made these remarks in an editorial accompanying the USPSTF Recommendation Statement (JAMA. 2016 Dec 20;316[23]:2493-4).
Asymptomatic adolescents and adults, including pregnant women, should not undergo routine serologic screening for genital herpes because the harms of this approach outweigh the benefits, according to an updated US Preventive Services Task Force (USPSTF) Recommendation Statement published online in JAMA.
The USPSTF last addressed screening for herpes simplex virus (HSV) in a 2005 Recommendation Statement, which advised against routine screening of asymptomatic patients at that time. “A small number” of clinical trials examined the issue since then, so the group commissioned a review of the literature through October 2016 to incorporate any new findings into the update, said Kirsten Bibbins-Domingo, MD, PhD, chair of the USPSTF and lead author of the update, and her associates.
Dr. Feltner and her colleagues concluded that current serologic screening tests produce a high rate of false-positive results – as much as 50% – and that those in turn lead to psychosocial harms such as distress and disruption of personal relationships, as well as increased costs and potential medical harm associated with confirmatory testing and unnecessary treatment.
Given the false-positive rates of the most widely used screening tests and the 15% prevalence of genital herpes in the general population, “screening 10,000 persons would result in approximately 1,485 true-positive and 1,445 false-positive results.” Moreover, confirmatory testing is offered only at a single research laboratory, said Dr. Bibbins-Domingo, professor of medicine at the University of California, San Francisco, and her associates on the Task Force.
Based on these findings and given the natural history and epidemiology of genital herpes, they characterized the potential benefits of routine screening as “no greater than small,” and the harms as “at least moderate” (JAMA. 2016 Dec 20;316[23]:2525-30. doi: 10.1001/jama.2016.16776).
The American Academy of Family Physicians, the American College of Obstetrics and Gynecology, and the Centers for Disease Control and Prevention also recommend against routine HSV screening of adolescents and adults, including pregnant women, the investigators noted.
The USPSTF is an independent, voluntary group that evaluates preventive health care services and is funded by the Agency for Healthcare Research and Quality by mandate of the U.S. Congress. The authors’ financial disclosures are available at www.uspreventiveservicestaskforce.org.
[email protected]
On Twitter @idpractitioner
Asymptomatic adolescents and adults, including pregnant women, should not undergo routine serologic screening for genital herpes because the harms of this approach outweigh the benefits, according to an updated US Preventive Services Task Force (USPSTF) Recommendation Statement published online in JAMA.
The USPSTF last addressed screening for herpes simplex virus (HSV) in a 2005 Recommendation Statement, which advised against routine screening of asymptomatic patients at that time. “A small number” of clinical trials examined the issue since then, so the group commissioned a review of the literature through October 2016 to incorporate any new findings into the update, said Kirsten Bibbins-Domingo, MD, PhD, chair of the USPSTF and lead author of the update, and her associates.
Dr. Feltner and her colleagues concluded that current serologic screening tests produce a high rate of false-positive results – as much as 50% – and that those in turn lead to psychosocial harms such as distress and disruption of personal relationships, as well as increased costs and potential medical harm associated with confirmatory testing and unnecessary treatment.
Given the false-positive rates of the most widely used screening tests and the 15% prevalence of genital herpes in the general population, “screening 10,000 persons would result in approximately 1,485 true-positive and 1,445 false-positive results.” Moreover, confirmatory testing is offered only at a single research laboratory, said Dr. Bibbins-Domingo, professor of medicine at the University of California, San Francisco, and her associates on the Task Force.
Based on these findings and given the natural history and epidemiology of genital herpes, they characterized the potential benefits of routine screening as “no greater than small,” and the harms as “at least moderate” (JAMA. 2016 Dec 20;316[23]:2525-30. doi: 10.1001/jama.2016.16776).
The American Academy of Family Physicians, the American College of Obstetrics and Gynecology, and the Centers for Disease Control and Prevention also recommend against routine HSV screening of adolescents and adults, including pregnant women, the investigators noted.
The USPSTF is an independent, voluntary group that evaluates preventive health care services and is funded by the Agency for Healthcare Research and Quality by mandate of the U.S. Congress. The authors’ financial disclosures are available at www.uspreventiveservicestaskforce.org.
[email protected]
On Twitter @idpractitioner
FROM JAMA
Key clinical point: Asymptomatic adults and adolescents should not undergo routine serologic screening for genital herpes because the harms outweigh the benefits, according to an updated USPSTF recommendation statement.
Major finding: Given the nearly 50% false-positive rate of current screening tests, screening 10,000 members of the general population would result in approximately 1,485 true-positive and 1,445 false-positive results.
Data source: A systematic review of 17 studies involving 9,736 participants regarding the accuracy, benefits, and harms of HSV screening.
Disclosures: The USPSTF is an independent, voluntary group that evaluates preventive health care services and is funded by the Agency for Healthcare Research and Quality by mandate of the U.S. Congress. The authors’ financial disclosures are available at www.uspreventiveservicestaskforce.org.
Pritelivir beats valacyclovir at suppressing genital HSV-2 infection
A 1-month course of pritelivir reduced genital HSV-2 shedding more than valacyclovir did in a small phase II clinical trial, according to a report published online in JAMA.
Previous phase I studies suggested that oral daily pritelivir was safe and tolerable in the patient population under evaluation (healthy adults with four to nine annual genital HSV-2 recurrences). Researchers performed this randomized, double-blind, crossover trial to assess the drug’s efficacy in 91 adults (mean age 48 years) who had frequent recurrences of genital symptoms and lesions. Study participants at four U.S. clinical research centers received pritelivir or valacyclovir for 28 days, followed by a washout period, then a 28-day course of the other drug, said lead investigator Anna Wald, MD, of the University of Washington and the Fred Hutchinson Cancer Research Center, Seattle, and her associates.
The primary endpoint – the number of swabs that tested positive for HSV-2 relative to the total number of swabs collected – was 2.4% during pritelivir treatment and 5.3% during valacyclovir treatment, a significant difference (relative risk, 0.42). Genital lesions were reported on 1.9% of days during pritelivir treatment, compared with 3.9% of days during valacyclovir treatment (RR, 0.40). In addition, the frequency of subclinical shedding also was significantly lower with pritelivir (1.8% vs. 4.1%), while the percentage of episodes resolving within 24 hours was significantly higher (87% vs. 69%).
The rate and severity of adverse events were similar between the two study groups. There were no serious adverse events or deaths. Compared with valacyclovir, pritelivir was associated with more statistically significant but clinically irrelevant changes in lymphocyte counts and creatinine levels. One patient in each study group developed mild allergic reactions thought to be possibly related to treatment, which resolved upon discontinuation of the study drugs.
AiCuris, maker of pritelivir, supported the study. Dr. Wald reported ties to AiCuris, Amgen, GlaxoSmithKline, Merck, Gilead, Vical, Genocea, and Admedus; her associates reported ties to numerous industry sources.
[email protected]
On Twitter @idpractitioner
A 1-month course of pritelivir reduced genital HSV-2 shedding more than valacyclovir did in a small phase II clinical trial, according to a report published online in JAMA.
Previous phase I studies suggested that oral daily pritelivir was safe and tolerable in the patient population under evaluation (healthy adults with four to nine annual genital HSV-2 recurrences). Researchers performed this randomized, double-blind, crossover trial to assess the drug’s efficacy in 91 adults (mean age 48 years) who had frequent recurrences of genital symptoms and lesions. Study participants at four U.S. clinical research centers received pritelivir or valacyclovir for 28 days, followed by a washout period, then a 28-day course of the other drug, said lead investigator Anna Wald, MD, of the University of Washington and the Fred Hutchinson Cancer Research Center, Seattle, and her associates.
The primary endpoint – the number of swabs that tested positive for HSV-2 relative to the total number of swabs collected – was 2.4% during pritelivir treatment and 5.3% during valacyclovir treatment, a significant difference (relative risk, 0.42). Genital lesions were reported on 1.9% of days during pritelivir treatment, compared with 3.9% of days during valacyclovir treatment (RR, 0.40). In addition, the frequency of subclinical shedding also was significantly lower with pritelivir (1.8% vs. 4.1%), while the percentage of episodes resolving within 24 hours was significantly higher (87% vs. 69%).
The rate and severity of adverse events were similar between the two study groups. There were no serious adverse events or deaths. Compared with valacyclovir, pritelivir was associated with more statistically significant but clinically irrelevant changes in lymphocyte counts and creatinine levels. One patient in each study group developed mild allergic reactions thought to be possibly related to treatment, which resolved upon discontinuation of the study drugs.
AiCuris, maker of pritelivir, supported the study. Dr. Wald reported ties to AiCuris, Amgen, GlaxoSmithKline, Merck, Gilead, Vical, Genocea, and Admedus; her associates reported ties to numerous industry sources.
[email protected]
On Twitter @idpractitioner
A 1-month course of pritelivir reduced genital HSV-2 shedding more than valacyclovir did in a small phase II clinical trial, according to a report published online in JAMA.
Previous phase I studies suggested that oral daily pritelivir was safe and tolerable in the patient population under evaluation (healthy adults with four to nine annual genital HSV-2 recurrences). Researchers performed this randomized, double-blind, crossover trial to assess the drug’s efficacy in 91 adults (mean age 48 years) who had frequent recurrences of genital symptoms and lesions. Study participants at four U.S. clinical research centers received pritelivir or valacyclovir for 28 days, followed by a washout period, then a 28-day course of the other drug, said lead investigator Anna Wald, MD, of the University of Washington and the Fred Hutchinson Cancer Research Center, Seattle, and her associates.
The primary endpoint – the number of swabs that tested positive for HSV-2 relative to the total number of swabs collected – was 2.4% during pritelivir treatment and 5.3% during valacyclovir treatment, a significant difference (relative risk, 0.42). Genital lesions were reported on 1.9% of days during pritelivir treatment, compared with 3.9% of days during valacyclovir treatment (RR, 0.40). In addition, the frequency of subclinical shedding also was significantly lower with pritelivir (1.8% vs. 4.1%), while the percentage of episodes resolving within 24 hours was significantly higher (87% vs. 69%).
The rate and severity of adverse events were similar between the two study groups. There were no serious adverse events or deaths. Compared with valacyclovir, pritelivir was associated with more statistically significant but clinically irrelevant changes in lymphocyte counts and creatinine levels. One patient in each study group developed mild allergic reactions thought to be possibly related to treatment, which resolved upon discontinuation of the study drugs.
AiCuris, maker of pritelivir, supported the study. Dr. Wald reported ties to AiCuris, Amgen, GlaxoSmithKline, Merck, Gilead, Vical, Genocea, and Admedus; her associates reported ties to numerous industry sources.
[email protected]
On Twitter @idpractitioner
Key clinical point:
Major finding: Among genital swabs, 2.4% tested positive for HSV-2 during pritelivir treatment and 5.3% did during valacyclovir treatment (relative risk, 0.42).
Data source: A randomized, double-blind, crossover trial involving 91 adults with frequently recurring genital HSV-2.
Disclosures: AiCuris, maker of pritelivir, supported the study. Dr. Wald reported ties to AiCuris, Amgen, GlaxoSmithKline, Merck, Gilead, Vical, Genocea, and Admedus; her associates reported ties to numerous industry sources.
Latest CDC data: Opioid deaths still rising
Opioid-related deaths continue to rise in the United States, with a 16% increase between 2014 and 2015 driven largely by overdoses of illegally manufactured fentanyl and heroin, according to a report released Dec. 16 by the Centers for Disease Control and Prevention.
CDC investigators analyzed drug-related mortality for 2010 through 2015 in a national statistics database for all 50 states and the District of Columbia, as well as drug-related deaths by subcategories of drugs in 28 states for 2014 through 2015. They found that the rapidly evolving opioid epidemic has not only continued but worsened in many ways, across all demographics and geographical regions of the country, said Rose A. Rudd, MSPH, of the CDC’s National Center for Injury Prevention and Control in Atlanta, and her associates (MMWR. 2016 Dec 16;65:1-8).
• Mortality from drug overdoses rose significantly over the 5-year study period, from 12.3 per 100,000 in 2010 to 16.3 per 100,000 in 2015. It rose in 30 states and in the District of Columbia, stayed stable in 19 states, and initially decreased but then rose again in 2 states (Florida and South Carolina).
• During the last year for which data are complete (2015), deaths from drug overdoses rose by approximately 12%, “signifying a continuing trend since 1999.”
• Sixty-three percent of the 52,404 deaths from drug overdoses in 2015 involved an opioid.
• The age-adjusted opioid-related death rate rose by 16% during the last year, from 9.0 per 100,000 in 2014 to 10.4 per 100,000 in 2015.
• These significant increases were driven by a rise in deaths from synthetic opioids other than methadone – chiefly illicitly manufactured fentanyl and heroin, which rose by 72.2% and 20.6%, respectively.
• In contrast, death rates tied to natural or semisynthetic opioids increased by only 2.6%, while those tied to methadone decreased by 9.1%.
Dr. Rudd and her associates cited several limitations. One is that some drug overdose death certificates did not identify specific drugs. Another is that heroin and morphine are metabolized similarly, which means that some heroin deaths might have been misclassified. Also, it could be problematic to generalize the findings, because the “state-specific analyses of opioid deaths are restricted to 28 states.”
“The ongoing epidemic of opioid deaths requires intense attention and action,” Dr. Rudd and her associates wrote. “Intensifying efforts to distribute naloxone (an antidote to reverse an opioid overdose), enhancing access to treatment ... and implementing harm reduction services are urgently needed.”
The study was conducted by the CDC.
Opioid-related deaths continue to rise in the United States, with a 16% increase between 2014 and 2015 driven largely by overdoses of illegally manufactured fentanyl and heroin, according to a report released Dec. 16 by the Centers for Disease Control and Prevention.
CDC investigators analyzed drug-related mortality for 2010 through 2015 in a national statistics database for all 50 states and the District of Columbia, as well as drug-related deaths by subcategories of drugs in 28 states for 2014 through 2015. They found that the rapidly evolving opioid epidemic has not only continued but worsened in many ways, across all demographics and geographical regions of the country, said Rose A. Rudd, MSPH, of the CDC’s National Center for Injury Prevention and Control in Atlanta, and her associates (MMWR. 2016 Dec 16;65:1-8).
• Mortality from drug overdoses rose significantly over the 5-year study period, from 12.3 per 100,000 in 2010 to 16.3 per 100,000 in 2015. It rose in 30 states and in the District of Columbia, stayed stable in 19 states, and initially decreased but then rose again in 2 states (Florida and South Carolina).
• During the last year for which data are complete (2015), deaths from drug overdoses rose by approximately 12%, “signifying a continuing trend since 1999.”
• Sixty-three percent of the 52,404 deaths from drug overdoses in 2015 involved an opioid.
• The age-adjusted opioid-related death rate rose by 16% during the last year, from 9.0 per 100,000 in 2014 to 10.4 per 100,000 in 2015.
• These significant increases were driven by a rise in deaths from synthetic opioids other than methadone – chiefly illicitly manufactured fentanyl and heroin, which rose by 72.2% and 20.6%, respectively.
• In contrast, death rates tied to natural or semisynthetic opioids increased by only 2.6%, while those tied to methadone decreased by 9.1%.
Dr. Rudd and her associates cited several limitations. One is that some drug overdose death certificates did not identify specific drugs. Another is that heroin and morphine are metabolized similarly, which means that some heroin deaths might have been misclassified. Also, it could be problematic to generalize the findings, because the “state-specific analyses of opioid deaths are restricted to 28 states.”
“The ongoing epidemic of opioid deaths requires intense attention and action,” Dr. Rudd and her associates wrote. “Intensifying efforts to distribute naloxone (an antidote to reverse an opioid overdose), enhancing access to treatment ... and implementing harm reduction services are urgently needed.”
The study was conducted by the CDC.
Opioid-related deaths continue to rise in the United States, with a 16% increase between 2014 and 2015 driven largely by overdoses of illegally manufactured fentanyl and heroin, according to a report released Dec. 16 by the Centers for Disease Control and Prevention.
CDC investigators analyzed drug-related mortality for 2010 through 2015 in a national statistics database for all 50 states and the District of Columbia, as well as drug-related deaths by subcategories of drugs in 28 states for 2014 through 2015. They found that the rapidly evolving opioid epidemic has not only continued but worsened in many ways, across all demographics and geographical regions of the country, said Rose A. Rudd, MSPH, of the CDC’s National Center for Injury Prevention and Control in Atlanta, and her associates (MMWR. 2016 Dec 16;65:1-8).
• Mortality from drug overdoses rose significantly over the 5-year study period, from 12.3 per 100,000 in 2010 to 16.3 per 100,000 in 2015. It rose in 30 states and in the District of Columbia, stayed stable in 19 states, and initially decreased but then rose again in 2 states (Florida and South Carolina).
• During the last year for which data are complete (2015), deaths from drug overdoses rose by approximately 12%, “signifying a continuing trend since 1999.”
• Sixty-three percent of the 52,404 deaths from drug overdoses in 2015 involved an opioid.
• The age-adjusted opioid-related death rate rose by 16% during the last year, from 9.0 per 100,000 in 2014 to 10.4 per 100,000 in 2015.
• These significant increases were driven by a rise in deaths from synthetic opioids other than methadone – chiefly illicitly manufactured fentanyl and heroin, which rose by 72.2% and 20.6%, respectively.
• In contrast, death rates tied to natural or semisynthetic opioids increased by only 2.6%, while those tied to methadone decreased by 9.1%.
Dr. Rudd and her associates cited several limitations. One is that some drug overdose death certificates did not identify specific drugs. Another is that heroin and morphine are metabolized similarly, which means that some heroin deaths might have been misclassified. Also, it could be problematic to generalize the findings, because the “state-specific analyses of opioid deaths are restricted to 28 states.”
“The ongoing epidemic of opioid deaths requires intense attention and action,” Dr. Rudd and her associates wrote. “Intensifying efforts to distribute naloxone (an antidote to reverse an opioid overdose), enhancing access to treatment ... and implementing harm reduction services are urgently needed.”
The study was conducted by the CDC.
FROM MMWR
Key clinical point: The most recent Centers for Disease Control and Prevention data show that opioid-related deaths continue to rise, with a 16% increase from 2014 to 2015, which was driven largely by overdoses of illegally manufactured fentanyl and heroin.
Major finding: Sixty-three percent of the 52,404 deaths from drug overdoses in 2015 involved opioid overdoses.
Data source: Analysis of drug-related mortality data from 2010 to 2015 in the National Vital Statistics System for all 50 states and the District of Columbia, plus an analysis of drug-related deaths by subcategories of drugs in 28 states from 2014 to 2015.
Disclosures: The study was conducted by the CDC.
Oral pomalidomide effective against Kaposi’s sarcoma
Oral pomalidomide, a derivative of thalidomide with immunomodulatory, antiangiogenic, and antiproliferative properties, proved to be well tolerated and effective against Kaposi’s sarcoma (KS) in a small phase I/II study, investigators reported in the Journal of Clinical Oncology.
There is a substantial need for oral therapies for KS, which often recurs and requires treatment, at least intermittently, for years. Existing treatments are cytotoxic agents, such as anthracyclines that are poorly tolerated and unsuitable for long-term use, said Mark N. Polizzotto, MD, of the National Cancer Institute, Bethesda, Md., and his associates.
They examined the tolerability and efficacy of pomalidomide against KS in a single-center, open-label trial involving 21 men and 1 transgender woman who had at least five evaluable cutaneous lesions. Fifteen of these participants had HIV infection. All of the patients were heavily pretreated with antiretrovirals and other agents, including thalidomide or lenalidomide, and most (17) had advanced KS with tumor-associated edema. The study participants received 5-mg oral pomalidomide once daily for 21 days in 28-day cycles for up to 12 cycles.
Sixteen patients showed an objective tumor response (overall response rate, 73%), including four who achieved a complete response (ORR, 18%). All 7 of the participants who didn’t have HIV showed an objective tumor response (ORR, 100%), as did 9 of the 15 HIV-infected participants (ORR, 60%). Three more participants, including one who was nonadeherent and lost to follow-up, achieved a partial tumor response.
Tumor responses included a decrease in the number of lesions and a decrease in the number of nodular lesions, as well as complete flattening of lesions, resolution of edema, and improvement in appearance. “The latter is particularly important because visible KS is a major source of stigma,” Dr. Polizzotto and his associates said (J Clin Oncol. 2016 Oct 3;34[34]:4125-32).
Two patients reported substantial subjective improvement in foot pain and appearance; one said he was pleased to be able to resume wearing closed shoes, the investigators noted. Treatment response generally was rapid, often commencing before the first follow-up at 4 weeks.
Pomalidomide was generally well tolerated. Adverse effects were frequent but mild and self-limiting, and they included neutropenia, constipation, anemia, fatigue, and rash. No patients required hospitalization, and there were no thromboembolic events. Three study participants developed malignancies after treatment: an Epstein-Barr-virus–associated Hodgkin lymphoma 1 year after the trial, a primary effusion lymphoma 15 months after, and a squamous-cell skin carcinoma. These probably reflect the patients’ underlying immunodeficiency, but the possibility that pomalidomide could contribute to malignancies in this high-risk population should be carefully explored in future studies, the investigators said.
“In resource-rich regions, pomalidomide may be of particular use in HIV-uninfected patients, in patients who have received substantial cumulative doses of anthracyclines, and in patients with less extensive but symptomatic disease for whom avoidance of cytotoxic chemotherapy would be beneficial. In resource-limited regions, there is an urgent need for effective and tolerable oral agents; with appropriate safeguards and monitoring, pomalidomide could address this,” Dr. Polizzotto and his associates wrote.
“Confirmatory studies of pomalidomide, alone and in combination with cytotoxic chemotherapy, are planned, including in sub-Saharan Africa,” they added.
Oral pomalidomide, a derivative of thalidomide with immunomodulatory, antiangiogenic, and antiproliferative properties, proved to be well tolerated and effective against Kaposi’s sarcoma (KS) in a small phase I/II study, investigators reported in the Journal of Clinical Oncology.
There is a substantial need for oral therapies for KS, which often recurs and requires treatment, at least intermittently, for years. Existing treatments are cytotoxic agents, such as anthracyclines that are poorly tolerated and unsuitable for long-term use, said Mark N. Polizzotto, MD, of the National Cancer Institute, Bethesda, Md., and his associates.
They examined the tolerability and efficacy of pomalidomide against KS in a single-center, open-label trial involving 21 men and 1 transgender woman who had at least five evaluable cutaneous lesions. Fifteen of these participants had HIV infection. All of the patients were heavily pretreated with antiretrovirals and other agents, including thalidomide or lenalidomide, and most (17) had advanced KS with tumor-associated edema. The study participants received 5-mg oral pomalidomide once daily for 21 days in 28-day cycles for up to 12 cycles.
Sixteen patients showed an objective tumor response (overall response rate, 73%), including four who achieved a complete response (ORR, 18%). All 7 of the participants who didn’t have HIV showed an objective tumor response (ORR, 100%), as did 9 of the 15 HIV-infected participants (ORR, 60%). Three more participants, including one who was nonadeherent and lost to follow-up, achieved a partial tumor response.
Tumor responses included a decrease in the number of lesions and a decrease in the number of nodular lesions, as well as complete flattening of lesions, resolution of edema, and improvement in appearance. “The latter is particularly important because visible KS is a major source of stigma,” Dr. Polizzotto and his associates said (J Clin Oncol. 2016 Oct 3;34[34]:4125-32).
Two patients reported substantial subjective improvement in foot pain and appearance; one said he was pleased to be able to resume wearing closed shoes, the investigators noted. Treatment response generally was rapid, often commencing before the first follow-up at 4 weeks.
Pomalidomide was generally well tolerated. Adverse effects were frequent but mild and self-limiting, and they included neutropenia, constipation, anemia, fatigue, and rash. No patients required hospitalization, and there were no thromboembolic events. Three study participants developed malignancies after treatment: an Epstein-Barr-virus–associated Hodgkin lymphoma 1 year after the trial, a primary effusion lymphoma 15 months after, and a squamous-cell skin carcinoma. These probably reflect the patients’ underlying immunodeficiency, but the possibility that pomalidomide could contribute to malignancies in this high-risk population should be carefully explored in future studies, the investigators said.
“In resource-rich regions, pomalidomide may be of particular use in HIV-uninfected patients, in patients who have received substantial cumulative doses of anthracyclines, and in patients with less extensive but symptomatic disease for whom avoidance of cytotoxic chemotherapy would be beneficial. In resource-limited regions, there is an urgent need for effective and tolerable oral agents; with appropriate safeguards and monitoring, pomalidomide could address this,” Dr. Polizzotto and his associates wrote.
“Confirmatory studies of pomalidomide, alone and in combination with cytotoxic chemotherapy, are planned, including in sub-Saharan Africa,” they added.
Oral pomalidomide, a derivative of thalidomide with immunomodulatory, antiangiogenic, and antiproliferative properties, proved to be well tolerated and effective against Kaposi’s sarcoma (KS) in a small phase I/II study, investigators reported in the Journal of Clinical Oncology.
There is a substantial need for oral therapies for KS, which often recurs and requires treatment, at least intermittently, for years. Existing treatments are cytotoxic agents, such as anthracyclines that are poorly tolerated and unsuitable for long-term use, said Mark N. Polizzotto, MD, of the National Cancer Institute, Bethesda, Md., and his associates.
They examined the tolerability and efficacy of pomalidomide against KS in a single-center, open-label trial involving 21 men and 1 transgender woman who had at least five evaluable cutaneous lesions. Fifteen of these participants had HIV infection. All of the patients were heavily pretreated with antiretrovirals and other agents, including thalidomide or lenalidomide, and most (17) had advanced KS with tumor-associated edema. The study participants received 5-mg oral pomalidomide once daily for 21 days in 28-day cycles for up to 12 cycles.
Sixteen patients showed an objective tumor response (overall response rate, 73%), including four who achieved a complete response (ORR, 18%). All 7 of the participants who didn’t have HIV showed an objective tumor response (ORR, 100%), as did 9 of the 15 HIV-infected participants (ORR, 60%). Three more participants, including one who was nonadeherent and lost to follow-up, achieved a partial tumor response.
Tumor responses included a decrease in the number of lesions and a decrease in the number of nodular lesions, as well as complete flattening of lesions, resolution of edema, and improvement in appearance. “The latter is particularly important because visible KS is a major source of stigma,” Dr. Polizzotto and his associates said (J Clin Oncol. 2016 Oct 3;34[34]:4125-32).
Two patients reported substantial subjective improvement in foot pain and appearance; one said he was pleased to be able to resume wearing closed shoes, the investigators noted. Treatment response generally was rapid, often commencing before the first follow-up at 4 weeks.
Pomalidomide was generally well tolerated. Adverse effects were frequent but mild and self-limiting, and they included neutropenia, constipation, anemia, fatigue, and rash. No patients required hospitalization, and there were no thromboembolic events. Three study participants developed malignancies after treatment: an Epstein-Barr-virus–associated Hodgkin lymphoma 1 year after the trial, a primary effusion lymphoma 15 months after, and a squamous-cell skin carcinoma. These probably reflect the patients’ underlying immunodeficiency, but the possibility that pomalidomide could contribute to malignancies in this high-risk population should be carefully explored in future studies, the investigators said.
“In resource-rich regions, pomalidomide may be of particular use in HIV-uninfected patients, in patients who have received substantial cumulative doses of anthracyclines, and in patients with less extensive but symptomatic disease for whom avoidance of cytotoxic chemotherapy would be beneficial. In resource-limited regions, there is an urgent need for effective and tolerable oral agents; with appropriate safeguards and monitoring, pomalidomide could address this,” Dr. Polizzotto and his associates wrote.
“Confirmatory studies of pomalidomide, alone and in combination with cytotoxic chemotherapy, are planned, including in sub-Saharan Africa,” they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Oral pomalidomide, a derivative of thalidomide with immunomodulatory, antiangiogenic, and antiproliferative properties, proved to be well tolerated and effective against Kaposi’s sarcoma in a small phase I/II study.
Major finding: All 7 of the participants who didn’t have HIV showed an objective tumor response with pomalidomide (ORR, 100%), as did 9 of the 15 HIV-infected participants (ORR, 60%).
Data source: A single-center open-label phase I/II study involving 22 adults with KS, including 15 who had HIV infection.
Disclosures: This study was supported by the National Institutes of Health, the National Cancer Institute, Celgene, and the National Institute of Allergy and Infectious Diseases. Dr. Polizzotto and some of his associates reported that their institutions received research funding from Celgene; one of his associates also reported ties to Ovid, Trek, PTC, Avila, Semorex, and Sorrento.