User login
Real-world outcomes of caplacizumab for iTTP comparable to clinical trial results
Real-world data for caplacizumab outcomes matched those seen in randomized controlled trials (RCTs) for the treatment of immune-mediated thrombotic thrombocytopenic purpura (iTTP), according to the results of a retrospective study.
Data collected from 2018 to 2020 were assessed for 85 patients (4 of them children) receiving caplacizumab at 22 United Kingdom hospitals, according to a report published online in Blood.
Researchers Tina Dutt, PhD, from the Liverpool (England) University Hospitals NHS Foundation Trust, and her colleagues compared patient characteristics and outcomes in these real-world clinical settings to those of caplacizumab trial endpoint results and to historical outcomes in the precaplacizumab era.
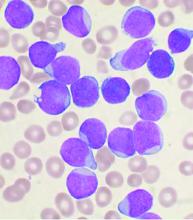
Acquired thrombotic thrombocytopenic purpura is an immune-mediated deficiency of the von Willebrand factor–cleaving protease (ADAMTS13), which allows unrestrained adhesion of von Willebrand factor multimers to platelets, leading to thrombocytopenia, hemolytic anemia, and tissue ischemia.
Standard management of iTTP has focused on the replacement of ADAMTS13 and the removal of autoantibodies using plasma exchange and immunosuppression, an approach which has reduced the mortality of acute TTP from greater than 90% to between 10% and 20%, according to the report.
Caplacizumab is a novel anti–von Willebrand factor immunoglobulin fragment that inhibits this interaction between von Willebrand factor multimers and platelets and is now added to the standard treatment regimen. The drug has been assessed in two pivotal multicenter RCTs that led to European Union and U.S. Food and Drug Administration approval.
Benefits and risk
Eighty-four of 85 patients received steroid and rituximab as well as plasma exchange along with caplacizumab treatment. All patients had ADAMTS13 activity at presentation less than 20 IU/dL, with 99% of patients (84/85) having ADAMTS13 activity less than 10 IU/dL, confirming a clinical diagnosis of acute TTP, according to the researchers.
The median time to platelet count normalization (3 days), the median duration of plasma exchange (7 days), and the median hospital stay (12 days) were all comparable with the RCT data, according to the researchers. In addition, the median duration of plasma exchange and time from beginning plasma exchange to platelet count normalization were favorable, compared with historical outcomes (P < .05).
TTP recurred in 5 of the 85 patients, all of whom had persistent ADAMTS13 activity less than 5 IU/dL.
There were 31 adverse events reported in 26 patients, 17 of these (55%) were bleeding episodes, and 5 of 31 (16%) were thrombotic events (2 unrelated to caplacizumab). The overall mortality was 6% (five patients), with no deaths attributed to caplacizumab. In four of the five deaths, caplacizumab was introduced more than 48 hours after plasma exchange initiation (range 3-21 days).
“This real-world evidence from the largest series of TTP patients receiving caplacizumab, outside of the pivotal studies, provides confirmation of the therapeutic benefits of caplacizumab and its inherent bleeding risk,” the researchers concluded.
Dr. Dutt and several of her colleagues reported receiving honoraria from Sanofi for serving on advisory boards, as well as speaker fees from Sanofi and Alexion.
Real-world data for caplacizumab outcomes matched those seen in randomized controlled trials (RCTs) for the treatment of immune-mediated thrombotic thrombocytopenic purpura (iTTP), according to the results of a retrospective study.
Data collected from 2018 to 2020 were assessed for 85 patients (4 of them children) receiving caplacizumab at 22 United Kingdom hospitals, according to a report published online in Blood.
Researchers Tina Dutt, PhD, from the Liverpool (England) University Hospitals NHS Foundation Trust, and her colleagues compared patient characteristics and outcomes in these real-world clinical settings to those of caplacizumab trial endpoint results and to historical outcomes in the precaplacizumab era.
Acquired thrombotic thrombocytopenic purpura is an immune-mediated deficiency of the von Willebrand factor–cleaving protease (ADAMTS13), which allows unrestrained adhesion of von Willebrand factor multimers to platelets, leading to thrombocytopenia, hemolytic anemia, and tissue ischemia.
Standard management of iTTP has focused on the replacement of ADAMTS13 and the removal of autoantibodies using plasma exchange and immunosuppression, an approach which has reduced the mortality of acute TTP from greater than 90% to between 10% and 20%, according to the report.
Caplacizumab is a novel anti–von Willebrand factor immunoglobulin fragment that inhibits this interaction between von Willebrand factor multimers and platelets and is now added to the standard treatment regimen. The drug has been assessed in two pivotal multicenter RCTs that led to European Union and U.S. Food and Drug Administration approval.
Benefits and risk
Eighty-four of 85 patients received steroid and rituximab as well as plasma exchange along with caplacizumab treatment. All patients had ADAMTS13 activity at presentation less than 20 IU/dL, with 99% of patients (84/85) having ADAMTS13 activity less than 10 IU/dL, confirming a clinical diagnosis of acute TTP, according to the researchers.
The median time to platelet count normalization (3 days), the median duration of plasma exchange (7 days), and the median hospital stay (12 days) were all comparable with the RCT data, according to the researchers. In addition, the median duration of plasma exchange and time from beginning plasma exchange to platelet count normalization were favorable, compared with historical outcomes (P < .05).
TTP recurred in 5 of the 85 patients, all of whom had persistent ADAMTS13 activity less than 5 IU/dL.
There were 31 adverse events reported in 26 patients, 17 of these (55%) were bleeding episodes, and 5 of 31 (16%) were thrombotic events (2 unrelated to caplacizumab). The overall mortality was 6% (five patients), with no deaths attributed to caplacizumab. In four of the five deaths, caplacizumab was introduced more than 48 hours after plasma exchange initiation (range 3-21 days).
“This real-world evidence from the largest series of TTP patients receiving caplacizumab, outside of the pivotal studies, provides confirmation of the therapeutic benefits of caplacizumab and its inherent bleeding risk,” the researchers concluded.
Dr. Dutt and several of her colleagues reported receiving honoraria from Sanofi for serving on advisory boards, as well as speaker fees from Sanofi and Alexion.
Real-world data for caplacizumab outcomes matched those seen in randomized controlled trials (RCTs) for the treatment of immune-mediated thrombotic thrombocytopenic purpura (iTTP), according to the results of a retrospective study.
Data collected from 2018 to 2020 were assessed for 85 patients (4 of them children) receiving caplacizumab at 22 United Kingdom hospitals, according to a report published online in Blood.
Researchers Tina Dutt, PhD, from the Liverpool (England) University Hospitals NHS Foundation Trust, and her colleagues compared patient characteristics and outcomes in these real-world clinical settings to those of caplacizumab trial endpoint results and to historical outcomes in the precaplacizumab era.
Acquired thrombotic thrombocytopenic purpura is an immune-mediated deficiency of the von Willebrand factor–cleaving protease (ADAMTS13), which allows unrestrained adhesion of von Willebrand factor multimers to platelets, leading to thrombocytopenia, hemolytic anemia, and tissue ischemia.
Standard management of iTTP has focused on the replacement of ADAMTS13 and the removal of autoantibodies using plasma exchange and immunosuppression, an approach which has reduced the mortality of acute TTP from greater than 90% to between 10% and 20%, according to the report.
Caplacizumab is a novel anti–von Willebrand factor immunoglobulin fragment that inhibits this interaction between von Willebrand factor multimers and platelets and is now added to the standard treatment regimen. The drug has been assessed in two pivotal multicenter RCTs that led to European Union and U.S. Food and Drug Administration approval.
Benefits and risk
Eighty-four of 85 patients received steroid and rituximab as well as plasma exchange along with caplacizumab treatment. All patients had ADAMTS13 activity at presentation less than 20 IU/dL, with 99% of patients (84/85) having ADAMTS13 activity less than 10 IU/dL, confirming a clinical diagnosis of acute TTP, according to the researchers.
The median time to platelet count normalization (3 days), the median duration of plasma exchange (7 days), and the median hospital stay (12 days) were all comparable with the RCT data, according to the researchers. In addition, the median duration of plasma exchange and time from beginning plasma exchange to platelet count normalization were favorable, compared with historical outcomes (P < .05).
TTP recurred in 5 of the 85 patients, all of whom had persistent ADAMTS13 activity less than 5 IU/dL.
There were 31 adverse events reported in 26 patients, 17 of these (55%) were bleeding episodes, and 5 of 31 (16%) were thrombotic events (2 unrelated to caplacizumab). The overall mortality was 6% (five patients), with no deaths attributed to caplacizumab. In four of the five deaths, caplacizumab was introduced more than 48 hours after plasma exchange initiation (range 3-21 days).
“This real-world evidence from the largest series of TTP patients receiving caplacizumab, outside of the pivotal studies, provides confirmation of the therapeutic benefits of caplacizumab and its inherent bleeding risk,” the researchers concluded.
Dr. Dutt and several of her colleagues reported receiving honoraria from Sanofi for serving on advisory boards, as well as speaker fees from Sanofi and Alexion.
FROM BLOOD
Risk factors predict graft failure in pediatric acute leukemia patients
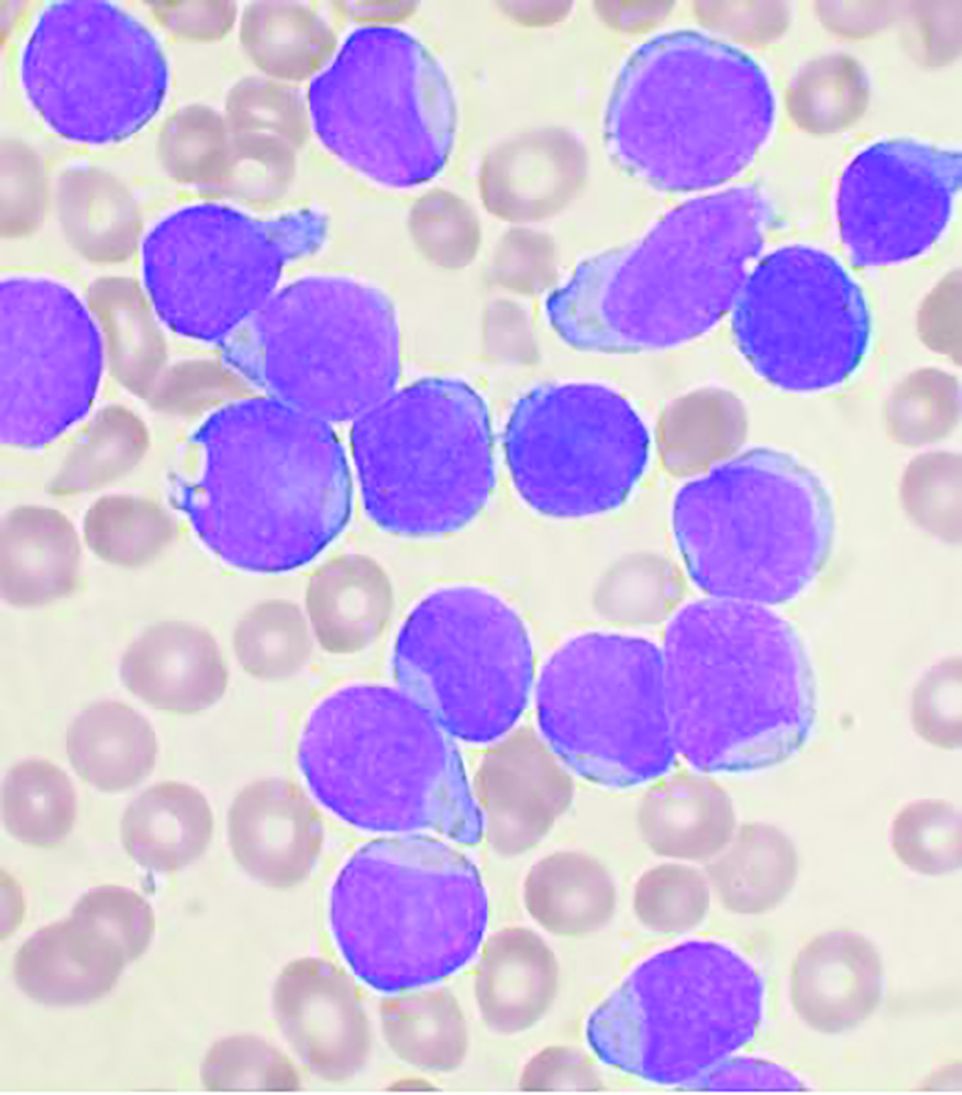
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
Researchers developed a predictive score for the risk of graft failure in patients with acute leukemia who underwent allogeneic hematopoietic stem cell transplantation (aHSCT) with ex vivo T-cell depletion. T-cell depletion is performed in an effort to prevent subsequent graft-versus-host disease (GVHD) after transplant.
The risk score was based on patient age and the T-lymphocyte population pre-aHSCT with 1 point of risk possible in each category. Patients with 1 point had a graft failure risk of 5% and 13% if they had 2 points, according to the results of the study presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Graft failure is a potentially severe complication in patients treated with aHSCT, but there are few studies analyzing risk factors when ex vivo T-cell depletion is used, Ivan López Torija of the Hospital Infantil Universitario Niño Jesús, Madrid, and colleagues noted in their presentation, which won the Best Young Poster Abstract Award at the meeting.
The researchers assessed 148 pediatric patients (64% boys) with acute leukemia who underwent allogeneic HSCT from haploidentical donors using ex vivo T-cell depletion between 2005 and 2020. About 53% of the patients were diagnosed with acute lymphoblastic leukemia, the rest with acute myeloid leukemia. The donor mean age was 40 years, and all transplant patients received toxicity reduction conditioning based on fludarabine busulfan and thiotepa.
Predictive results
Multivariate analysis showed that T-cell count (CD3+/CD8+ ≥ 350/mL: hazard ratio, 2,6; P = .01) and patient age (less than 9 years: HR; 5.0; P = .04) were associated with graft failure. A risk score was established using these results and based on patient age and T lymphocyte pre-aHSCT with 1 point each for each increased risk category. Patients with 1 point had a graft failure risk of 5% and a risk of 13% if they had 2 points.
However, in this particular population, with a mean follow up of 4 years, the overall survival rate was 60%, with no significant differences seen between patients that presented graft failure and those without graft failure.
“Patient age and pretransplant number of CD3+/CD8+ are associated with [graft failure] in pediatric patients with acute leukemia undergoing ex vivo T-cell–depleted haploidentical transplantation. These findings highlight the importance of preexisting cellular immunity in the transplant recipient and support T-cell population analysis as part of a pretransplant working program,” the researchers concluded.
The authors reported that they had no disclosures.
FROM EBMT 2021
Allo-HSCT plus monoclonal antibody treatment can improve survival in patients with r/r B-ALL
The use of allogeneic hematopoietic stem cell transplantation (allo-HSCT) can improve survival in minimal residual disease (MRD)–negative remission patients with relapsed/refractory (r/r) B-cell acute lymphoblastic leukemia (B-ALL) after the start of monoclonal antibody treatment, according to the results of a landmark analysis presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Previous studies have indicated that allo-HSCT improves the results of treatment in r/r B-ALL patients, compared with chemotherapy alone. In addition, it has been found that the monoclonal antibodies (Mab), anti-CD19-blinatumomab and anti-CD22-inotuzumab ozogamicin, induced remission in a significant proportion of such patients.
To determine if the use of allo-HSCT improves the outcome of patients in MRD-negative remission with or without Mab treatment, researchers performed a landmark analysis of 110 patients who achieved MRD-negative status after Mab treatment. The analysis examined results at 2, 4, and 6 months subsequent to the initiation of Mab treatment, according to poster presentation by Inna V. Markova, MD, and colleagues at Pavlov University, Saint Petersburg, Russian Federation.
Study details
The researchers included 110 patients who achieved MRD-negative status outside of clinical trials at a single institution in the analysis. Forty of the patients (36%) were children and 70 (64%) were adults. The median age for all patients was 23 years and the median follow up was 24 months. Fifty-seven (52%) and 53 (48%) patients received Mab for hematological relapse and persistent measurable residual disease or for molecular relapse, respectively. Therapy with Mab alone without subsequent allo-HSCT was used in 36 (31%) patients (30 received blinatumomab and 6 received inotuzumab ozogamicin). A total of 74 (69%) patients received allo-HSCT from a matched related or unrelated donor (MD-HSCT, n = 38) or haploidentical donor (Haplo-HSCT, n = 36). All patients received posttransplantation cyclophosphamide (PTCY)–based graft-versus host disease (GVHD) prophylaxis. Landmark analysis was performed at 2, 4, and 6 months after Mab therapy initiation to determine the effect of allo-HSCT on the outcome and the optimal timing of HSCT. Overall survival and disease-free survival (DFS) were used as outcomes.
Promising results
No significant differences between the MD-HSCT, Mab alone, and Haplo-HSCT groups were observed in 2-month landmark analysis (P = .4 for OS and P =.65 for DFS). However, the 4-month landmark analysis demonstrated superior overall survival and DFS in patients after MD-HSCT, but not Haplo-HSCT, compared with Mab alone: 2-year OS was 75%, 50%, and 27,7% (P = .032) and DFS was 53.5%, 51.3%, and 16.6% (P = .02) for MD-HSCT, Mab alone and Haplo-HSCT groups, respectively. In addition, 6-month analysis showed that there was no benefit from subsequent transplantation, according to the authors, with regard to overall survival (P = .11).
“Our study demonstrated that at least MD-HSCT with PTCY platform improves survival in MRD-negative remission if performed during the first 4 months after Mab initiation. Haplo-HSCT or MD-HSCT beyond 4 months are not associated with improved outcomes in this groups of patients,” the researchers concluded.
The researchers reported they had no conflicts of interest to declare.
The use of allogeneic hematopoietic stem cell transplantation (allo-HSCT) can improve survival in minimal residual disease (MRD)–negative remission patients with relapsed/refractory (r/r) B-cell acute lymphoblastic leukemia (B-ALL) after the start of monoclonal antibody treatment, according to the results of a landmark analysis presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Previous studies have indicated that allo-HSCT improves the results of treatment in r/r B-ALL patients, compared with chemotherapy alone. In addition, it has been found that the monoclonal antibodies (Mab), anti-CD19-blinatumomab and anti-CD22-inotuzumab ozogamicin, induced remission in a significant proportion of such patients.
To determine if the use of allo-HSCT improves the outcome of patients in MRD-negative remission with or without Mab treatment, researchers performed a landmark analysis of 110 patients who achieved MRD-negative status after Mab treatment. The analysis examined results at 2, 4, and 6 months subsequent to the initiation of Mab treatment, according to poster presentation by Inna V. Markova, MD, and colleagues at Pavlov University, Saint Petersburg, Russian Federation.
Study details
The researchers included 110 patients who achieved MRD-negative status outside of clinical trials at a single institution in the analysis. Forty of the patients (36%) were children and 70 (64%) were adults. The median age for all patients was 23 years and the median follow up was 24 months. Fifty-seven (52%) and 53 (48%) patients received Mab for hematological relapse and persistent measurable residual disease or for molecular relapse, respectively. Therapy with Mab alone without subsequent allo-HSCT was used in 36 (31%) patients (30 received blinatumomab and 6 received inotuzumab ozogamicin). A total of 74 (69%) patients received allo-HSCT from a matched related or unrelated donor (MD-HSCT, n = 38) or haploidentical donor (Haplo-HSCT, n = 36). All patients received posttransplantation cyclophosphamide (PTCY)–based graft-versus host disease (GVHD) prophylaxis. Landmark analysis was performed at 2, 4, and 6 months after Mab therapy initiation to determine the effect of allo-HSCT on the outcome and the optimal timing of HSCT. Overall survival and disease-free survival (DFS) were used as outcomes.
Promising results
No significant differences between the MD-HSCT, Mab alone, and Haplo-HSCT groups were observed in 2-month landmark analysis (P = .4 for OS and P =.65 for DFS). However, the 4-month landmark analysis demonstrated superior overall survival and DFS in patients after MD-HSCT, but not Haplo-HSCT, compared with Mab alone: 2-year OS was 75%, 50%, and 27,7% (P = .032) and DFS was 53.5%, 51.3%, and 16.6% (P = .02) for MD-HSCT, Mab alone and Haplo-HSCT groups, respectively. In addition, 6-month analysis showed that there was no benefit from subsequent transplantation, according to the authors, with regard to overall survival (P = .11).
“Our study demonstrated that at least MD-HSCT with PTCY platform improves survival in MRD-negative remission if performed during the first 4 months after Mab initiation. Haplo-HSCT or MD-HSCT beyond 4 months are not associated with improved outcomes in this groups of patients,” the researchers concluded.
The researchers reported they had no conflicts of interest to declare.
The use of allogeneic hematopoietic stem cell transplantation (allo-HSCT) can improve survival in minimal residual disease (MRD)–negative remission patients with relapsed/refractory (r/r) B-cell acute lymphoblastic leukemia (B-ALL) after the start of monoclonal antibody treatment, according to the results of a landmark analysis presented at the virtual meeting of the European Society for Blood and Marrow Transplantation.
Previous studies have indicated that allo-HSCT improves the results of treatment in r/r B-ALL patients, compared with chemotherapy alone. In addition, it has been found that the monoclonal antibodies (Mab), anti-CD19-blinatumomab and anti-CD22-inotuzumab ozogamicin, induced remission in a significant proportion of such patients.
To determine if the use of allo-HSCT improves the outcome of patients in MRD-negative remission with or without Mab treatment, researchers performed a landmark analysis of 110 patients who achieved MRD-negative status after Mab treatment. The analysis examined results at 2, 4, and 6 months subsequent to the initiation of Mab treatment, according to poster presentation by Inna V. Markova, MD, and colleagues at Pavlov University, Saint Petersburg, Russian Federation.
Study details
The researchers included 110 patients who achieved MRD-negative status outside of clinical trials at a single institution in the analysis. Forty of the patients (36%) were children and 70 (64%) were adults. The median age for all patients was 23 years and the median follow up was 24 months. Fifty-seven (52%) and 53 (48%) patients received Mab for hematological relapse and persistent measurable residual disease or for molecular relapse, respectively. Therapy with Mab alone without subsequent allo-HSCT was used in 36 (31%) patients (30 received blinatumomab and 6 received inotuzumab ozogamicin). A total of 74 (69%) patients received allo-HSCT from a matched related or unrelated donor (MD-HSCT, n = 38) or haploidentical donor (Haplo-HSCT, n = 36). All patients received posttransplantation cyclophosphamide (PTCY)–based graft-versus host disease (GVHD) prophylaxis. Landmark analysis was performed at 2, 4, and 6 months after Mab therapy initiation to determine the effect of allo-HSCT on the outcome and the optimal timing of HSCT. Overall survival and disease-free survival (DFS) were used as outcomes.
Promising results
No significant differences between the MD-HSCT, Mab alone, and Haplo-HSCT groups were observed in 2-month landmark analysis (P = .4 for OS and P =.65 for DFS). However, the 4-month landmark analysis demonstrated superior overall survival and DFS in patients after MD-HSCT, but not Haplo-HSCT, compared with Mab alone: 2-year OS was 75%, 50%, and 27,7% (P = .032) and DFS was 53.5%, 51.3%, and 16.6% (P = .02) for MD-HSCT, Mab alone and Haplo-HSCT groups, respectively. In addition, 6-month analysis showed that there was no benefit from subsequent transplantation, according to the authors, with regard to overall survival (P = .11).
“Our study demonstrated that at least MD-HSCT with PTCY platform improves survival in MRD-negative remission if performed during the first 4 months after Mab initiation. Haplo-HSCT or MD-HSCT beyond 4 months are not associated with improved outcomes in this groups of patients,” the researchers concluded.
The researchers reported they had no conflicts of interest to declare.
FROM EBMT 2021
Updated recommendations released on COVID-19 and pediatric ALL
The main threat to the vast majority of children with acute lymphoblastic leukemia still remains the ALL itself, according to updated recommendations released by the Leukemia Committee of the French Society for the Fight Against Cancers and Leukemias in Children and Adolescents (SFCE).
“The situation of the current COVID-19 pandemic is continuously evolving. We thus have taken the more recent knowledge into account to update the previous recommendations from the Leukemia Committee,” Jérémie Rouger-Gaudichon, MD, of Pediatric Hemato-Immuno-Oncology Unit, Centre Hospitalier Universitaire, Caen (France), and colleagues wrote on behalf of the SFCE.
The updated recommendations are based on data collected in a real-time prospective survey among the 30 SFCE centers since April 2020. As of December 2020, 127 cases of COVID-19 were reported, most of them being enrolled in the PEDONCOVID study (NCT04433871) according to the report. Of these, eight patients required hospitalization in intensive care unit and one patient with relapsed acute lymphoblastic leukemia (ALL) died from ARDS with multiorgan failure. This confirms earlier reports that SARS-CoV-2 infection can be severe in some children with cancer and/or having hematopoietic stem cell transplant (HSCT), according to the report, which was published online in Bulletin du Cancer.
Recommendations
General recommendations were provided in the report, including the following:
- Test for SARS-CoV-2 (preferably by PCR or at least by immunological tests, on nasopharyngeal swab) before starting intensive induction chemotherapy or other intensive phase of treatment, for ALL patients, with or without symptoms.
- Delay systemic treatment if possible (e.g., absence of major hyperleukocytosis) in positive patients. During later phases, if patients test positive, tests should be repeated over time until negativity, especially before the beginning of an intensive course.
- Isolate any COVID-19–negative child or adolescent to allow treatment to continue (facial mask, social distancing, barrier measures, no contact with individuals suspected of COVID-19 or COVID-19–positive), in particular for patients to be allografted.
- Limit visitation to parents and potentially siblings in patients slated for HSCT and follow all necessary sanitary procedures for those visits.
The report provides a lengthy discussion of more detailed recommendations, including the following for first-line treatment of ALL:
- For patients with high-risk ALL, an individualized decision regarding transplantation and its timing should weigh the risks of transplantation in an epidemic context of COVID-19 against the risk linked to ALL.
- Minimizing hospital visits by the use of home blood tests and partial use of telemedicine may be considered.
- A physical examination should be performed regularly to avoid any delay in the diagnosis of treatment complications or relapse and preventative measures for SARS-CoV-2 should be applied in the home.
Patients with relapsed ALL may be at more risk from the effects of COVID-19 disease, according to the others, so for ALL patients receiving second-line or more treatment the recommendations include the following:
- Testing must be performed before starting a chemotherapy block, and postponing chemotherapy in case of positive test should be discussed in accordance with each specific situation and benefits/risks ratio regarding the leukemia.
- First-relapse patients should follow the INTREALL treatment protocol as much as possible and those who reach appropriate complete remission should be considered promptly for allogeneic transplantation, despite the pandemic.
- Second relapse and refractory relapses require testing and negative results for inclusion in phase I-II trials being conducted by most if not all academic or industrial promoters.
- The indication for treatment with CAR-T cells must be weighed with the center that would perform the procedure to determine the feasibility of performing all necessary procedures including apheresis and manufacturing.
In the case of a SARS-CoV-2 infection diagnosis during the treatment of ALL, discussions should occur with regard to stopping and/or postponing all chemotherapies, according to the severity of the ALL, the stage of treatment and the severity of clinical and/or radiological signs. In addition, any specific anti-COVID-19 treatment must be discussed with the infectious diseases team, according to the report.
“Fortunately, SARS-CoV-2 infection appears nevertheless to be mild in most children with cancer/ALL. Thus, the main threat to the vast majority of children with ALL still remains the ALL itself. Long-term data including well-matched case-control studies will tell if treatment delays/modifications due to COVID-19 have impacted the outcome if children with ALL,” the authors stated. However, “despite extremely rapid advances obtained in less than one year, our knowledge of SARS-CoV-2 and its complications is still incomplete,” they concluded, adding that the recommendations will likely need to be updated within another few months.
The authors reported that they had no conflicts of interest.
The main threat to the vast majority of children with acute lymphoblastic leukemia still remains the ALL itself, according to updated recommendations released by the Leukemia Committee of the French Society for the Fight Against Cancers and Leukemias in Children and Adolescents (SFCE).
“The situation of the current COVID-19 pandemic is continuously evolving. We thus have taken the more recent knowledge into account to update the previous recommendations from the Leukemia Committee,” Jérémie Rouger-Gaudichon, MD, of Pediatric Hemato-Immuno-Oncology Unit, Centre Hospitalier Universitaire, Caen (France), and colleagues wrote on behalf of the SFCE.
The updated recommendations are based on data collected in a real-time prospective survey among the 30 SFCE centers since April 2020. As of December 2020, 127 cases of COVID-19 were reported, most of them being enrolled in the PEDONCOVID study (NCT04433871) according to the report. Of these, eight patients required hospitalization in intensive care unit and one patient with relapsed acute lymphoblastic leukemia (ALL) died from ARDS with multiorgan failure. This confirms earlier reports that SARS-CoV-2 infection can be severe in some children with cancer and/or having hematopoietic stem cell transplant (HSCT), according to the report, which was published online in Bulletin du Cancer.
Recommendations
General recommendations were provided in the report, including the following:
- Test for SARS-CoV-2 (preferably by PCR or at least by immunological tests, on nasopharyngeal swab) before starting intensive induction chemotherapy or other intensive phase of treatment, for ALL patients, with or without symptoms.
- Delay systemic treatment if possible (e.g., absence of major hyperleukocytosis) in positive patients. During later phases, if patients test positive, tests should be repeated over time until negativity, especially before the beginning of an intensive course.
- Isolate any COVID-19–negative child or adolescent to allow treatment to continue (facial mask, social distancing, barrier measures, no contact with individuals suspected of COVID-19 or COVID-19–positive), in particular for patients to be allografted.
- Limit visitation to parents and potentially siblings in patients slated for HSCT and follow all necessary sanitary procedures for those visits.
The report provides a lengthy discussion of more detailed recommendations, including the following for first-line treatment of ALL:
- For patients with high-risk ALL, an individualized decision regarding transplantation and its timing should weigh the risks of transplantation in an epidemic context of COVID-19 against the risk linked to ALL.
- Minimizing hospital visits by the use of home blood tests and partial use of telemedicine may be considered.
- A physical examination should be performed regularly to avoid any delay in the diagnosis of treatment complications or relapse and preventative measures for SARS-CoV-2 should be applied in the home.
Patients with relapsed ALL may be at more risk from the effects of COVID-19 disease, according to the others, so for ALL patients receiving second-line or more treatment the recommendations include the following:
- Testing must be performed before starting a chemotherapy block, and postponing chemotherapy in case of positive test should be discussed in accordance with each specific situation and benefits/risks ratio regarding the leukemia.
- First-relapse patients should follow the INTREALL treatment protocol as much as possible and those who reach appropriate complete remission should be considered promptly for allogeneic transplantation, despite the pandemic.
- Second relapse and refractory relapses require testing and negative results for inclusion in phase I-II trials being conducted by most if not all academic or industrial promoters.
- The indication for treatment with CAR-T cells must be weighed with the center that would perform the procedure to determine the feasibility of performing all necessary procedures including apheresis and manufacturing.
In the case of a SARS-CoV-2 infection diagnosis during the treatment of ALL, discussions should occur with regard to stopping and/or postponing all chemotherapies, according to the severity of the ALL, the stage of treatment and the severity of clinical and/or radiological signs. In addition, any specific anti-COVID-19 treatment must be discussed with the infectious diseases team, according to the report.
“Fortunately, SARS-CoV-2 infection appears nevertheless to be mild in most children with cancer/ALL. Thus, the main threat to the vast majority of children with ALL still remains the ALL itself. Long-term data including well-matched case-control studies will tell if treatment delays/modifications due to COVID-19 have impacted the outcome if children with ALL,” the authors stated. However, “despite extremely rapid advances obtained in less than one year, our knowledge of SARS-CoV-2 and its complications is still incomplete,” they concluded, adding that the recommendations will likely need to be updated within another few months.
The authors reported that they had no conflicts of interest.
The main threat to the vast majority of children with acute lymphoblastic leukemia still remains the ALL itself, according to updated recommendations released by the Leukemia Committee of the French Society for the Fight Against Cancers and Leukemias in Children and Adolescents (SFCE).
“The situation of the current COVID-19 pandemic is continuously evolving. We thus have taken the more recent knowledge into account to update the previous recommendations from the Leukemia Committee,” Jérémie Rouger-Gaudichon, MD, of Pediatric Hemato-Immuno-Oncology Unit, Centre Hospitalier Universitaire, Caen (France), and colleagues wrote on behalf of the SFCE.
The updated recommendations are based on data collected in a real-time prospective survey among the 30 SFCE centers since April 2020. As of December 2020, 127 cases of COVID-19 were reported, most of them being enrolled in the PEDONCOVID study (NCT04433871) according to the report. Of these, eight patients required hospitalization in intensive care unit and one patient with relapsed acute lymphoblastic leukemia (ALL) died from ARDS with multiorgan failure. This confirms earlier reports that SARS-CoV-2 infection can be severe in some children with cancer and/or having hematopoietic stem cell transplant (HSCT), according to the report, which was published online in Bulletin du Cancer.
Recommendations
General recommendations were provided in the report, including the following:
- Test for SARS-CoV-2 (preferably by PCR or at least by immunological tests, on nasopharyngeal swab) before starting intensive induction chemotherapy or other intensive phase of treatment, for ALL patients, with or without symptoms.
- Delay systemic treatment if possible (e.g., absence of major hyperleukocytosis) in positive patients. During later phases, if patients test positive, tests should be repeated over time until negativity, especially before the beginning of an intensive course.
- Isolate any COVID-19–negative child or adolescent to allow treatment to continue (facial mask, social distancing, barrier measures, no contact with individuals suspected of COVID-19 or COVID-19–positive), in particular for patients to be allografted.
- Limit visitation to parents and potentially siblings in patients slated for HSCT and follow all necessary sanitary procedures for those visits.
The report provides a lengthy discussion of more detailed recommendations, including the following for first-line treatment of ALL:
- For patients with high-risk ALL, an individualized decision regarding transplantation and its timing should weigh the risks of transplantation in an epidemic context of COVID-19 against the risk linked to ALL.
- Minimizing hospital visits by the use of home blood tests and partial use of telemedicine may be considered.
- A physical examination should be performed regularly to avoid any delay in the diagnosis of treatment complications or relapse and preventative measures for SARS-CoV-2 should be applied in the home.
Patients with relapsed ALL may be at more risk from the effects of COVID-19 disease, according to the others, so for ALL patients receiving second-line or more treatment the recommendations include the following:
- Testing must be performed before starting a chemotherapy block, and postponing chemotherapy in case of positive test should be discussed in accordance with each specific situation and benefits/risks ratio regarding the leukemia.
- First-relapse patients should follow the INTREALL treatment protocol as much as possible and those who reach appropriate complete remission should be considered promptly for allogeneic transplantation, despite the pandemic.
- Second relapse and refractory relapses require testing and negative results for inclusion in phase I-II trials being conducted by most if not all academic or industrial promoters.
- The indication for treatment with CAR-T cells must be weighed with the center that would perform the procedure to determine the feasibility of performing all necessary procedures including apheresis and manufacturing.
In the case of a SARS-CoV-2 infection diagnosis during the treatment of ALL, discussions should occur with regard to stopping and/or postponing all chemotherapies, according to the severity of the ALL, the stage of treatment and the severity of clinical and/or radiological signs. In addition, any specific anti-COVID-19 treatment must be discussed with the infectious diseases team, according to the report.
“Fortunately, SARS-CoV-2 infection appears nevertheless to be mild in most children with cancer/ALL. Thus, the main threat to the vast majority of children with ALL still remains the ALL itself. Long-term data including well-matched case-control studies will tell if treatment delays/modifications due to COVID-19 have impacted the outcome if children with ALL,” the authors stated. However, “despite extremely rapid advances obtained in less than one year, our knowledge of SARS-CoV-2 and its complications is still incomplete,” they concluded, adding that the recommendations will likely need to be updated within another few months.
The authors reported that they had no conflicts of interest.
FROM BULLETIN DU CANCER
High-dose chemo no better than standard dose for B-cell lymphoma
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
FROM THE LANCET HEMATOLOGY
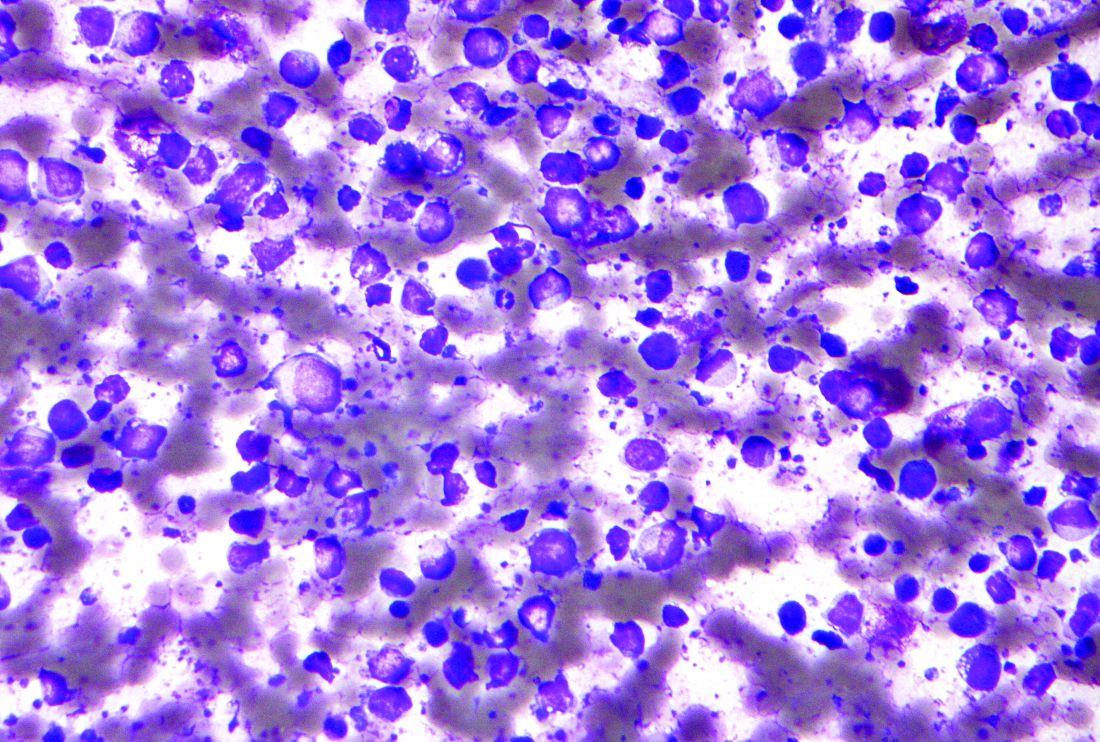
New inhibitor shows promise in previously failed B-cell malignancies
who discontinued prior Bruton’s tyrosine kinase (BTK)–inhibitor treatment due to resistance or intolerance, according to the results of the BRUIN trial, a phase 1/2 study.
Pirtobrutinib (formerly known as LOXO-305) is an oral-dose, highly selective, reversible BTK inhibitor, which might address a growing, unmet need for alternative therapies in BTK-inhibitor treatment failure patients, according to Anthony R. Mato, MD, of Memorial Sloan Kettering Cancer Center, New York, and colleagues. Their report was published in The Lancet.
The study included 109 women (34%) and 214 men (66%), with a median age of 68 years, who were treated with pirtobrutinib. Of these, 203 patients were assigned to pirtobrutinib (25-300 mg once per day) in the phase 1 portion of the study, and 120 patients were assigned to pirtobrutinib (200 mg once per day) in phase 2.
Promising outcomes
Pirtobrutinib, showed promising efficacy and tolerable safety in patients with CLL or small lymphocytic lymphoma, mantle cell lymphoma, and Waldenström macroglobulinemia who were previously treated with a BTK inhibitor. In 121 efficacy-evaluable patients with CLL or SLL treated with a previous covalent BTK inhibitor, the overall response rate with pirtobrutinib was 62% (95% confidence interval, 53-71). The ORR was similar in CLL patients with previous covalent BTK inhibitor resistance (67%), covalent BTK inhibitor intolerance (52%), BTK C481-mutant (71%), and BTK wild-type (66%) disease.
In 52 efficacy-evaluable patients with mantle cell lymphoma (MCL) previously treated with covalent BTK inhibitors, the ORR was 52% (95% CI, 38-66). Of 117 patients with CLL, SLL, or MCL who responded, all but 8 remain progression free to date, the authors stated.
In 19 efficacy-evaluable patients with Waldenström macroglobulinemia, the ORR was 68%. Among eight patients with follicular lymphoma who were efficacy evaluable, responses were observed in four (50%) patients, and six (75%) of eight efficacy evaluable patients with Richter’s transformation identified before enrollment responded to treatment, the authors stated.
No dose-limiting toxicities were observed and the maximum tolerated dose was not reached, according to the researchers. The recommended phase 2 dose was 200 mg daily. The adverse events, which occurred in at least 10% of 323 patients, were fatigue (20%), diarrhea (17%), and contusion (13%). The most common grade 3 or higher adverse event was neutropenia (10%). Five patients (1%) discontinued treatment because of a treatment-related adverse event.
In this “first-in-human trial of pirtobrutinib, we showed promising efficacy and safety in patients with B-cell malignancies, including CLL or SLL, MCL, Waldenström macroglobulinemia, and follicular lymphoma. Activity was observed in heavily pretreated patients, including patients with resistance and intolerance to previous covalent BTK inhibitor treatment. Global randomized phase 3 studies in CLL or SLL, and MCL are planned,” the researchers concluded.
Birth of a third generation?
“The pirtobrutinib study, by opening the way for a third generation of BTK inhibitors, could improve such a personalized molecular approach in the treatment of B-cell malignancies,” according to accompanying editorial comment by Jean-Marie Michot, MD, and Vincent Ribrag, MD, both of the Institut de Cancérologie Gustave Roussy, Villejuif, France.
They discussed how BTK inhibitors have been a considerable therapeutic advance in the treatment of NHL-B and CLL and how the three currently approved BTK inhibitors, namely ibrutinib, acalabrutinib, and zanubrutinib, are all covalent and irreversible inhibitors at the protein – the C481 binding site. “Ibrutinib was the first approved drug. The second-generation inhibitors, acalabrutinib and zanubrutinib, were designed to be more BTK selective,” they added. However, the covalency and irreversibility of the drugs, considered therapeutic strengths, have resulted in induced resistance mutations occurring at the covalent binding, rendering the drugs inactive. “Two advantages of this new drug class are highlighted. First, the selectivity of the drug on BTK appears to be increased,” they wrote. “Second, this class does not bind BTK to the C481 residue, and the efficacy of the drug is therefore not affected by mutations in the BTK binding site.”
Several of the study authors reported receiving grants and personal fees from Loxo Oncology (a wholly owned subsidiary of Eli Lilly), which sponsored the study, as well as financial relationships with other pharmaceutical and biotechnology companies.
Dr. Michot and Dr. Ribrag reported that they had no disclosures relevant to the discussion.
who discontinued prior Bruton’s tyrosine kinase (BTK)–inhibitor treatment due to resistance or intolerance, according to the results of the BRUIN trial, a phase 1/2 study.
Pirtobrutinib (formerly known as LOXO-305) is an oral-dose, highly selective, reversible BTK inhibitor, which might address a growing, unmet need for alternative therapies in BTK-inhibitor treatment failure patients, according to Anthony R. Mato, MD, of Memorial Sloan Kettering Cancer Center, New York, and colleagues. Their report was published in The Lancet.
The study included 109 women (34%) and 214 men (66%), with a median age of 68 years, who were treated with pirtobrutinib. Of these, 203 patients were assigned to pirtobrutinib (25-300 mg once per day) in the phase 1 portion of the study, and 120 patients were assigned to pirtobrutinib (200 mg once per day) in phase 2.
Promising outcomes
Pirtobrutinib, showed promising efficacy and tolerable safety in patients with CLL or small lymphocytic lymphoma, mantle cell lymphoma, and Waldenström macroglobulinemia who were previously treated with a BTK inhibitor. In 121 efficacy-evaluable patients with CLL or SLL treated with a previous covalent BTK inhibitor, the overall response rate with pirtobrutinib was 62% (95% confidence interval, 53-71). The ORR was similar in CLL patients with previous covalent BTK inhibitor resistance (67%), covalent BTK inhibitor intolerance (52%), BTK C481-mutant (71%), and BTK wild-type (66%) disease.
In 52 efficacy-evaluable patients with mantle cell lymphoma (MCL) previously treated with covalent BTK inhibitors, the ORR was 52% (95% CI, 38-66). Of 117 patients with CLL, SLL, or MCL who responded, all but 8 remain progression free to date, the authors stated.
In 19 efficacy-evaluable patients with Waldenström macroglobulinemia, the ORR was 68%. Among eight patients with follicular lymphoma who were efficacy evaluable, responses were observed in four (50%) patients, and six (75%) of eight efficacy evaluable patients with Richter’s transformation identified before enrollment responded to treatment, the authors stated.
No dose-limiting toxicities were observed and the maximum tolerated dose was not reached, according to the researchers. The recommended phase 2 dose was 200 mg daily. The adverse events, which occurred in at least 10% of 323 patients, were fatigue (20%), diarrhea (17%), and contusion (13%). The most common grade 3 or higher adverse event was neutropenia (10%). Five patients (1%) discontinued treatment because of a treatment-related adverse event.
In this “first-in-human trial of pirtobrutinib, we showed promising efficacy and safety in patients with B-cell malignancies, including CLL or SLL, MCL, Waldenström macroglobulinemia, and follicular lymphoma. Activity was observed in heavily pretreated patients, including patients with resistance and intolerance to previous covalent BTK inhibitor treatment. Global randomized phase 3 studies in CLL or SLL, and MCL are planned,” the researchers concluded.
Birth of a third generation?
“The pirtobrutinib study, by opening the way for a third generation of BTK inhibitors, could improve such a personalized molecular approach in the treatment of B-cell malignancies,” according to accompanying editorial comment by Jean-Marie Michot, MD, and Vincent Ribrag, MD, both of the Institut de Cancérologie Gustave Roussy, Villejuif, France.
They discussed how BTK inhibitors have been a considerable therapeutic advance in the treatment of NHL-B and CLL and how the three currently approved BTK inhibitors, namely ibrutinib, acalabrutinib, and zanubrutinib, are all covalent and irreversible inhibitors at the protein – the C481 binding site. “Ibrutinib was the first approved drug. The second-generation inhibitors, acalabrutinib and zanubrutinib, were designed to be more BTK selective,” they added. However, the covalency and irreversibility of the drugs, considered therapeutic strengths, have resulted in induced resistance mutations occurring at the covalent binding, rendering the drugs inactive. “Two advantages of this new drug class are highlighted. First, the selectivity of the drug on BTK appears to be increased,” they wrote. “Second, this class does not bind BTK to the C481 residue, and the efficacy of the drug is therefore not affected by mutations in the BTK binding site.”
Several of the study authors reported receiving grants and personal fees from Loxo Oncology (a wholly owned subsidiary of Eli Lilly), which sponsored the study, as well as financial relationships with other pharmaceutical and biotechnology companies.
Dr. Michot and Dr. Ribrag reported that they had no disclosures relevant to the discussion.
who discontinued prior Bruton’s tyrosine kinase (BTK)–inhibitor treatment due to resistance or intolerance, according to the results of the BRUIN trial, a phase 1/2 study.
Pirtobrutinib (formerly known as LOXO-305) is an oral-dose, highly selective, reversible BTK inhibitor, which might address a growing, unmet need for alternative therapies in BTK-inhibitor treatment failure patients, according to Anthony R. Mato, MD, of Memorial Sloan Kettering Cancer Center, New York, and colleagues. Their report was published in The Lancet.
The study included 109 women (34%) and 214 men (66%), with a median age of 68 years, who were treated with pirtobrutinib. Of these, 203 patients were assigned to pirtobrutinib (25-300 mg once per day) in the phase 1 portion of the study, and 120 patients were assigned to pirtobrutinib (200 mg once per day) in phase 2.
Promising outcomes
Pirtobrutinib, showed promising efficacy and tolerable safety in patients with CLL or small lymphocytic lymphoma, mantle cell lymphoma, and Waldenström macroglobulinemia who were previously treated with a BTK inhibitor. In 121 efficacy-evaluable patients with CLL or SLL treated with a previous covalent BTK inhibitor, the overall response rate with pirtobrutinib was 62% (95% confidence interval, 53-71). The ORR was similar in CLL patients with previous covalent BTK inhibitor resistance (67%), covalent BTK inhibitor intolerance (52%), BTK C481-mutant (71%), and BTK wild-type (66%) disease.
In 52 efficacy-evaluable patients with mantle cell lymphoma (MCL) previously treated with covalent BTK inhibitors, the ORR was 52% (95% CI, 38-66). Of 117 patients with CLL, SLL, or MCL who responded, all but 8 remain progression free to date, the authors stated.
In 19 efficacy-evaluable patients with Waldenström macroglobulinemia, the ORR was 68%. Among eight patients with follicular lymphoma who were efficacy evaluable, responses were observed in four (50%) patients, and six (75%) of eight efficacy evaluable patients with Richter’s transformation identified before enrollment responded to treatment, the authors stated.
No dose-limiting toxicities were observed and the maximum tolerated dose was not reached, according to the researchers. The recommended phase 2 dose was 200 mg daily. The adverse events, which occurred in at least 10% of 323 patients, were fatigue (20%), diarrhea (17%), and contusion (13%). The most common grade 3 or higher adverse event was neutropenia (10%). Five patients (1%) discontinued treatment because of a treatment-related adverse event.
In this “first-in-human trial of pirtobrutinib, we showed promising efficacy and safety in patients with B-cell malignancies, including CLL or SLL, MCL, Waldenström macroglobulinemia, and follicular lymphoma. Activity was observed in heavily pretreated patients, including patients with resistance and intolerance to previous covalent BTK inhibitor treatment. Global randomized phase 3 studies in CLL or SLL, and MCL are planned,” the researchers concluded.
Birth of a third generation?
“The pirtobrutinib study, by opening the way for a third generation of BTK inhibitors, could improve such a personalized molecular approach in the treatment of B-cell malignancies,” according to accompanying editorial comment by Jean-Marie Michot, MD, and Vincent Ribrag, MD, both of the Institut de Cancérologie Gustave Roussy, Villejuif, France.
They discussed how BTK inhibitors have been a considerable therapeutic advance in the treatment of NHL-B and CLL and how the three currently approved BTK inhibitors, namely ibrutinib, acalabrutinib, and zanubrutinib, are all covalent and irreversible inhibitors at the protein – the C481 binding site. “Ibrutinib was the first approved drug. The second-generation inhibitors, acalabrutinib and zanubrutinib, were designed to be more BTK selective,” they added. However, the covalency and irreversibility of the drugs, considered therapeutic strengths, have resulted in induced resistance mutations occurring at the covalent binding, rendering the drugs inactive. “Two advantages of this new drug class are highlighted. First, the selectivity of the drug on BTK appears to be increased,” they wrote. “Second, this class does not bind BTK to the C481 residue, and the efficacy of the drug is therefore not affected by mutations in the BTK binding site.”
Several of the study authors reported receiving grants and personal fees from Loxo Oncology (a wholly owned subsidiary of Eli Lilly), which sponsored the study, as well as financial relationships with other pharmaceutical and biotechnology companies.
Dr. Michot and Dr. Ribrag reported that they had no disclosures relevant to the discussion.
FROM THE LANCET
Prognostic gene signature identifies high- vs. low-risk DLBCL patients
according to the results of a database analysis.
A total of 33 genes formed the signature that could be transformed into a risk score, according to a study by Santosh Khanal, a senior bioinformatics scientist at Children’s Mercy Kansas City (Mo.), and colleagues published in Cancer Genetics.
Their study used gene expression and clinical parameters from the Lymphoma/Leukemia Molecular Profiling Project from 233 patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) therapy to identify genes whose expression was associated with overall survival (OS). They refined the information to develop prognostic gene signature that could be used to calculate risk scores for each individual and predict OS.
Significant separation
The researchers initially found 61 genes individually associated with OS that had a nonadjusted P ≤ .001 using the univariate Cox regression model. The 61 genes were then assessed using multivariate Cox analysis to identify a minimal set of genes that could predict OS, resulting in a minimal set of 33 genes that were used to develop a survival risk score for each individual.
The OS of the high-risk group was significantly reduced, compared with the low-risk group (hazard ratio, 0.046; P < .0001). Upon stratification of individuals by risk score into quartiles, patients in the lowest quartile risk score had a 100% probability of survival, while individuals in the highest quartile had a 9.2% OS by year 5.
In order to validate their results, the researchers calculated risk scores using their prognostic gene set in three additional published DLBCL studies. For all three studies, individuals with low risk score had significantly better OS, “indicating the robustness of the gene signature for multiple external datasets,” according to the researchers.
The top biological pathways and processes that were significantly overrepresented in the 33-gene set were the thioester biosynthetic process (P = .00005), cellular response to hormone stimulus (P = .002), G protein–coupled receptor ligand binding (P = .003), and myeloid cell activation involved in immune responses (P = 0.006).
“As new therapies for lymphoma become available, including new immunotherapies and personalized medicine approaches such as [chimeric antigen receptor] T cells, it will be important to identify candidate individuals that are at high risk and may benefit from experimental therapeutic approaches compared with individuals who will have lower risk of death with current therapies,” the researchers concluded.
The authors reported that they had no competing interests.
according to the results of a database analysis.
A total of 33 genes formed the signature that could be transformed into a risk score, according to a study by Santosh Khanal, a senior bioinformatics scientist at Children’s Mercy Kansas City (Mo.), and colleagues published in Cancer Genetics.
Their study used gene expression and clinical parameters from the Lymphoma/Leukemia Molecular Profiling Project from 233 patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) therapy to identify genes whose expression was associated with overall survival (OS). They refined the information to develop prognostic gene signature that could be used to calculate risk scores for each individual and predict OS.
Significant separation
The researchers initially found 61 genes individually associated with OS that had a nonadjusted P ≤ .001 using the univariate Cox regression model. The 61 genes were then assessed using multivariate Cox analysis to identify a minimal set of genes that could predict OS, resulting in a minimal set of 33 genes that were used to develop a survival risk score for each individual.
The OS of the high-risk group was significantly reduced, compared with the low-risk group (hazard ratio, 0.046; P < .0001). Upon stratification of individuals by risk score into quartiles, patients in the lowest quartile risk score had a 100% probability of survival, while individuals in the highest quartile had a 9.2% OS by year 5.
In order to validate their results, the researchers calculated risk scores using their prognostic gene set in three additional published DLBCL studies. For all three studies, individuals with low risk score had significantly better OS, “indicating the robustness of the gene signature for multiple external datasets,” according to the researchers.
The top biological pathways and processes that were significantly overrepresented in the 33-gene set were the thioester biosynthetic process (P = .00005), cellular response to hormone stimulus (P = .002), G protein–coupled receptor ligand binding (P = .003), and myeloid cell activation involved in immune responses (P = 0.006).
“As new therapies for lymphoma become available, including new immunotherapies and personalized medicine approaches such as [chimeric antigen receptor] T cells, it will be important to identify candidate individuals that are at high risk and may benefit from experimental therapeutic approaches compared with individuals who will have lower risk of death with current therapies,” the researchers concluded.
The authors reported that they had no competing interests.
according to the results of a database analysis.
A total of 33 genes formed the signature that could be transformed into a risk score, according to a study by Santosh Khanal, a senior bioinformatics scientist at Children’s Mercy Kansas City (Mo.), and colleagues published in Cancer Genetics.
Their study used gene expression and clinical parameters from the Lymphoma/Leukemia Molecular Profiling Project from 233 patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) therapy to identify genes whose expression was associated with overall survival (OS). They refined the information to develop prognostic gene signature that could be used to calculate risk scores for each individual and predict OS.
Significant separation
The researchers initially found 61 genes individually associated with OS that had a nonadjusted P ≤ .001 using the univariate Cox regression model. The 61 genes were then assessed using multivariate Cox analysis to identify a minimal set of genes that could predict OS, resulting in a minimal set of 33 genes that were used to develop a survival risk score for each individual.
The OS of the high-risk group was significantly reduced, compared with the low-risk group (hazard ratio, 0.046; P < .0001). Upon stratification of individuals by risk score into quartiles, patients in the lowest quartile risk score had a 100% probability of survival, while individuals in the highest quartile had a 9.2% OS by year 5.
In order to validate their results, the researchers calculated risk scores using their prognostic gene set in three additional published DLBCL studies. For all three studies, individuals with low risk score had significantly better OS, “indicating the robustness of the gene signature for multiple external datasets,” according to the researchers.
The top biological pathways and processes that were significantly overrepresented in the 33-gene set were the thioester biosynthetic process (P = .00005), cellular response to hormone stimulus (P = .002), G protein–coupled receptor ligand binding (P = .003), and myeloid cell activation involved in immune responses (P = 0.006).
“As new therapies for lymphoma become available, including new immunotherapies and personalized medicine approaches such as [chimeric antigen receptor] T cells, it will be important to identify candidate individuals that are at high risk and may benefit from experimental therapeutic approaches compared with individuals who will have lower risk of death with current therapies,” the researchers concluded.
The authors reported that they had no competing interests.
FROM CANCER GENETICS
CLL, MBL had lower response rates to flu vaccination, compared with healthy adults
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
FROM VACCINE
Immunoabsorption shows promise as an adjunct treatment for high-risk acquired hemophilia
Despite the high mortality rate for acquired hemophilia and the availability of suggested drug treatments, there are no randomized, controlled studies to inform doctors of the best therapies for their patients.
Immunoabsorption therapy (IA) is one such treatment that has been proposed as valid because of its ability to remove factor VIII clotting inhibitors from the bloodstream, but the data on its effectiveness are limited, according to Michael Esteves Pereira, of the Bern (Switzerland) University Hospital and the University of Bern, and colleagues.
In order to help answer the question of the benefits of IA for treating acquired hemophilia, the researchers performed a retrospective study assessing observational data as well as a systemic review and meta-analysis of published literature. They found evidence that the therapy was effective, but suggest that more confirmatory studies are needed, according to their report published online in Transfusion Medicine Reviews.
Data from the authors’ institution were available for 12 patients with acquired hemophilia treated since 2002. The median age was 76 years and four patients were women. The bleeding phenotype was extensive bruising and/or muscle hematomas in nine patients, gastrointestinal bleeding in two patients, and extensive bleeding after tooth extraction in one patient. Their data were added to the 10 published studies included in the literature review, resulting in a total of 118 patients.
Promising results
The author’s single institution analysis showed that IA treatment stopped bleeding in nine patients, while three patients did not respond. At 3 months, the median factor VIII increased to 80 IU/dL (considered complete remission) and the median inhibitor titer decreased to 0.15 BU/mL.
The pooled proportion of the meta-analysis patients treated with IA who achieved factor VIII recovery defined as complete remission was 86% (95% confidence interval, 76%-94%). The pooled proportion of patients with a reduction of the inhibitor titer was 95% (95% CI, 83%-100%), while the pooled mortality was 7% (95% CI, 0%-18%). Sensitivity analyses did not reveal any significant differences in retrospective studies or in studies using different absorbing agents.
In addition, there were few reported side effects, most of which were considered mild, according to the researchers. These included nausea and vomiting, paresthesia, and mild hypotension. The authors did suggest that, as a central venous catheter is often used, patients were exposed to an added risk of bleeding and infection.
“At our institution, IA is considered on a case-by-case base rather than a strict cutoff level. Strong arguments are life-threatening bleeding complications, inhibitor titers 20 BU/mL or greater, or failed immunosuppressive treatment with corticosteroids and cyclophosphamide using an established dose regimen,” the researchers stated.
“Even though firm evidence is still lacking and the actual ‘added value’ of IA cannot be adequately assessed, we believe that IA might be a beneficial adjunctive treatment modality in some patients with acquired hemophilia. It was associated with a complete remission in the majority of patients, most of whom are at high risk of bleeding,” the researchers added.
The authors reported that they had no relevant disclosures.
Despite the high mortality rate for acquired hemophilia and the availability of suggested drug treatments, there are no randomized, controlled studies to inform doctors of the best therapies for their patients.
Immunoabsorption therapy (IA) is one such treatment that has been proposed as valid because of its ability to remove factor VIII clotting inhibitors from the bloodstream, but the data on its effectiveness are limited, according to Michael Esteves Pereira, of the Bern (Switzerland) University Hospital and the University of Bern, and colleagues.
In order to help answer the question of the benefits of IA for treating acquired hemophilia, the researchers performed a retrospective study assessing observational data as well as a systemic review and meta-analysis of published literature. They found evidence that the therapy was effective, but suggest that more confirmatory studies are needed, according to their report published online in Transfusion Medicine Reviews.
Data from the authors’ institution were available for 12 patients with acquired hemophilia treated since 2002. The median age was 76 years and four patients were women. The bleeding phenotype was extensive bruising and/or muscle hematomas in nine patients, gastrointestinal bleeding in two patients, and extensive bleeding after tooth extraction in one patient. Their data were added to the 10 published studies included in the literature review, resulting in a total of 118 patients.
Promising results
The author’s single institution analysis showed that IA treatment stopped bleeding in nine patients, while three patients did not respond. At 3 months, the median factor VIII increased to 80 IU/dL (considered complete remission) and the median inhibitor titer decreased to 0.15 BU/mL.
The pooled proportion of the meta-analysis patients treated with IA who achieved factor VIII recovery defined as complete remission was 86% (95% confidence interval, 76%-94%). The pooled proportion of patients with a reduction of the inhibitor titer was 95% (95% CI, 83%-100%), while the pooled mortality was 7% (95% CI, 0%-18%). Sensitivity analyses did not reveal any significant differences in retrospective studies or in studies using different absorbing agents.
In addition, there were few reported side effects, most of which were considered mild, according to the researchers. These included nausea and vomiting, paresthesia, and mild hypotension. The authors did suggest that, as a central venous catheter is often used, patients were exposed to an added risk of bleeding and infection.
“At our institution, IA is considered on a case-by-case base rather than a strict cutoff level. Strong arguments are life-threatening bleeding complications, inhibitor titers 20 BU/mL or greater, or failed immunosuppressive treatment with corticosteroids and cyclophosphamide using an established dose regimen,” the researchers stated.
“Even though firm evidence is still lacking and the actual ‘added value’ of IA cannot be adequately assessed, we believe that IA might be a beneficial adjunctive treatment modality in some patients with acquired hemophilia. It was associated with a complete remission in the majority of patients, most of whom are at high risk of bleeding,” the researchers added.
The authors reported that they had no relevant disclosures.
Despite the high mortality rate for acquired hemophilia and the availability of suggested drug treatments, there are no randomized, controlled studies to inform doctors of the best therapies for their patients.
Immunoabsorption therapy (IA) is one such treatment that has been proposed as valid because of its ability to remove factor VIII clotting inhibitors from the bloodstream, but the data on its effectiveness are limited, according to Michael Esteves Pereira, of the Bern (Switzerland) University Hospital and the University of Bern, and colleagues.
In order to help answer the question of the benefits of IA for treating acquired hemophilia, the researchers performed a retrospective study assessing observational data as well as a systemic review and meta-analysis of published literature. They found evidence that the therapy was effective, but suggest that more confirmatory studies are needed, according to their report published online in Transfusion Medicine Reviews.
Data from the authors’ institution were available for 12 patients with acquired hemophilia treated since 2002. The median age was 76 years and four patients were women. The bleeding phenotype was extensive bruising and/or muscle hematomas in nine patients, gastrointestinal bleeding in two patients, and extensive bleeding after tooth extraction in one patient. Their data were added to the 10 published studies included in the literature review, resulting in a total of 118 patients.
Promising results
The author’s single institution analysis showed that IA treatment stopped bleeding in nine patients, while three patients did not respond. At 3 months, the median factor VIII increased to 80 IU/dL (considered complete remission) and the median inhibitor titer decreased to 0.15 BU/mL.
The pooled proportion of the meta-analysis patients treated with IA who achieved factor VIII recovery defined as complete remission was 86% (95% confidence interval, 76%-94%). The pooled proportion of patients with a reduction of the inhibitor titer was 95% (95% CI, 83%-100%), while the pooled mortality was 7% (95% CI, 0%-18%). Sensitivity analyses did not reveal any significant differences in retrospective studies or in studies using different absorbing agents.
In addition, there were few reported side effects, most of which were considered mild, according to the researchers. These included nausea and vomiting, paresthesia, and mild hypotension. The authors did suggest that, as a central venous catheter is often used, patients were exposed to an added risk of bleeding and infection.
“At our institution, IA is considered on a case-by-case base rather than a strict cutoff level. Strong arguments are life-threatening bleeding complications, inhibitor titers 20 BU/mL or greater, or failed immunosuppressive treatment with corticosteroids and cyclophosphamide using an established dose regimen,” the researchers stated.
“Even though firm evidence is still lacking and the actual ‘added value’ of IA cannot be adequately assessed, we believe that IA might be a beneficial adjunctive treatment modality in some patients with acquired hemophilia. It was associated with a complete remission in the majority of patients, most of whom are at high risk of bleeding,” the researchers added.
The authors reported that they had no relevant disclosures.
FROM TRANSFUSION MEDICINE REVIEWS
Ceftolozane-tazobactam found effective in critically ill patients with Pseudomonas aeruginosa infections
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
FROM THE INTERNATIONAL JOURNAL OF ANTIMICROBIAL AGENTS