User login
Mepolizumab shows glucocorticoid-sparing effect in severe asthma patients
The investigational humanized monoclonal antibody mepolizumab had a significant glucocorticoid-sparing effect in patients with severe eosinophilic asthma, researchers report.
Severe asthma patients who added mepolizumab to their maintenance dose of oral glucocorticoids were 2.39 times more likely to tolerate a reduction in glucocorticoid dosage, compared with the placebo group (95% confidence interval, 1.25-4.56; P = .008), Dr. Elisabeth H. Bel and her colleagues from the University of Amsterdam’s department of respiratory medicine found.
The findings of their industry-sponsored Steroid Reduction with Mepolizumab (SIRIUS) study were presented at the annual congress of the European Respiratory Society and published simultaneously in the New England Journal of Medicine.
The phase III trial included 135 adults with severe asthma who had at least a 6-month history of glucocorticoid treatment. Eosinophilic inflammation was defined as a blood eosinophil level of 300 cells/mcL or more before the study, or 150 cells/mcL or more during the optimization phase (doi: 10.1056/NEJMoa1403291).
In the first of four phases, glucocorticoid use was reduced weekly to establish the lowest dose needed to maintain asthma control. In the induction phase, patients were randomized to receive either a 100-mg dose of mepolizumab or placebo, in addition to their optimized glucocorticoid dose. Then, in the reduction phase (weeks 4 to 20), this glucocorticoid dose was gradually reduced by 1.25-10 mg per day every 4 weeks, based on asthma control and adrenal insufficiency. Finally, in the maintenance phase (weeks 20-24), no additional modifications were made to the glucocorticoid dose, and a follow-up safety visit was scheduled. Patients used an electronic diary to record data on peak expiratory flow, asthma symptoms, and scores on the Asthma Control Questionnaire 5 (ACQ-5).
Efficacy was measured by the percentage reduction in daily oral glucocorticoid dose during the maintenance phase, compared with the optimized dose in the first phase.
The primary analysis showed that 23% of patients in the mepolizumab group had a glucocorticoid dose reduction of 90%-100%, compared with just 11% of patients in the placebo group. Additionally, 17% of mepolizumab patients saw a reduction of 70% to less than 90%, compared with 8% of placebo patients. A total of 56% of patients in the placebo group had no reduction in glucocorticoid dose, showed a lack of asthma control, or pulled out of the trial, versus 36% of patients in the mepolizumab group.
Because the use of oral glucocorticoid treatment can lead to serious adverse effects, many patients with severe eosinophilic asthma may take lower doses than is needed to adequately maintain symptom control, the investigators said in the report. The results of this study suggest that adding mepolizumab to this regimen may be a viable option to allow for use of lower glucocorticoid doses in these patients while still achieving symptom control and mitigating severe complications, they added.
Mepolizumab is not currently approved anywhere in the world.
Among potential limitations of their small study, the authors wrote, was that they "assumed a relationship between a worsening of symptoms and an increase in eosinophilic airway inflammation, which may not be valid for all patients. It is possible that if we had mandated evidence of eosinophilic inflammation in the optimization phase, a different drug effect would have been seen."
Several researchers disclosed financial relationships with industry firms, including mepolizumab developer GlaxoSmithKline, the sponsor and designer of the study.
On Twitter @mrajaraman
The investigational humanized monoclonal antibody mepolizumab had a significant glucocorticoid-sparing effect in patients with severe eosinophilic asthma, researchers report.
Severe asthma patients who added mepolizumab to their maintenance dose of oral glucocorticoids were 2.39 times more likely to tolerate a reduction in glucocorticoid dosage, compared with the placebo group (95% confidence interval, 1.25-4.56; P = .008), Dr. Elisabeth H. Bel and her colleagues from the University of Amsterdam’s department of respiratory medicine found.
The findings of their industry-sponsored Steroid Reduction with Mepolizumab (SIRIUS) study were presented at the annual congress of the European Respiratory Society and published simultaneously in the New England Journal of Medicine.
The phase III trial included 135 adults with severe asthma who had at least a 6-month history of glucocorticoid treatment. Eosinophilic inflammation was defined as a blood eosinophil level of 300 cells/mcL or more before the study, or 150 cells/mcL or more during the optimization phase (doi: 10.1056/NEJMoa1403291).
In the first of four phases, glucocorticoid use was reduced weekly to establish the lowest dose needed to maintain asthma control. In the induction phase, patients were randomized to receive either a 100-mg dose of mepolizumab or placebo, in addition to their optimized glucocorticoid dose. Then, in the reduction phase (weeks 4 to 20), this glucocorticoid dose was gradually reduced by 1.25-10 mg per day every 4 weeks, based on asthma control and adrenal insufficiency. Finally, in the maintenance phase (weeks 20-24), no additional modifications were made to the glucocorticoid dose, and a follow-up safety visit was scheduled. Patients used an electronic diary to record data on peak expiratory flow, asthma symptoms, and scores on the Asthma Control Questionnaire 5 (ACQ-5).
Efficacy was measured by the percentage reduction in daily oral glucocorticoid dose during the maintenance phase, compared with the optimized dose in the first phase.
The primary analysis showed that 23% of patients in the mepolizumab group had a glucocorticoid dose reduction of 90%-100%, compared with just 11% of patients in the placebo group. Additionally, 17% of mepolizumab patients saw a reduction of 70% to less than 90%, compared with 8% of placebo patients. A total of 56% of patients in the placebo group had no reduction in glucocorticoid dose, showed a lack of asthma control, or pulled out of the trial, versus 36% of patients in the mepolizumab group.
Because the use of oral glucocorticoid treatment can lead to serious adverse effects, many patients with severe eosinophilic asthma may take lower doses than is needed to adequately maintain symptom control, the investigators said in the report. The results of this study suggest that adding mepolizumab to this regimen may be a viable option to allow for use of lower glucocorticoid doses in these patients while still achieving symptom control and mitigating severe complications, they added.
Mepolizumab is not currently approved anywhere in the world.
Among potential limitations of their small study, the authors wrote, was that they "assumed a relationship between a worsening of symptoms and an increase in eosinophilic airway inflammation, which may not be valid for all patients. It is possible that if we had mandated evidence of eosinophilic inflammation in the optimization phase, a different drug effect would have been seen."
Several researchers disclosed financial relationships with industry firms, including mepolizumab developer GlaxoSmithKline, the sponsor and designer of the study.
On Twitter @mrajaraman
The investigational humanized monoclonal antibody mepolizumab had a significant glucocorticoid-sparing effect in patients with severe eosinophilic asthma, researchers report.
Severe asthma patients who added mepolizumab to their maintenance dose of oral glucocorticoids were 2.39 times more likely to tolerate a reduction in glucocorticoid dosage, compared with the placebo group (95% confidence interval, 1.25-4.56; P = .008), Dr. Elisabeth H. Bel and her colleagues from the University of Amsterdam’s department of respiratory medicine found.
The findings of their industry-sponsored Steroid Reduction with Mepolizumab (SIRIUS) study were presented at the annual congress of the European Respiratory Society and published simultaneously in the New England Journal of Medicine.
The phase III trial included 135 adults with severe asthma who had at least a 6-month history of glucocorticoid treatment. Eosinophilic inflammation was defined as a blood eosinophil level of 300 cells/mcL or more before the study, or 150 cells/mcL or more during the optimization phase (doi: 10.1056/NEJMoa1403291).
In the first of four phases, glucocorticoid use was reduced weekly to establish the lowest dose needed to maintain asthma control. In the induction phase, patients were randomized to receive either a 100-mg dose of mepolizumab or placebo, in addition to their optimized glucocorticoid dose. Then, in the reduction phase (weeks 4 to 20), this glucocorticoid dose was gradually reduced by 1.25-10 mg per day every 4 weeks, based on asthma control and adrenal insufficiency. Finally, in the maintenance phase (weeks 20-24), no additional modifications were made to the glucocorticoid dose, and a follow-up safety visit was scheduled. Patients used an electronic diary to record data on peak expiratory flow, asthma symptoms, and scores on the Asthma Control Questionnaire 5 (ACQ-5).
Efficacy was measured by the percentage reduction in daily oral glucocorticoid dose during the maintenance phase, compared with the optimized dose in the first phase.
The primary analysis showed that 23% of patients in the mepolizumab group had a glucocorticoid dose reduction of 90%-100%, compared with just 11% of patients in the placebo group. Additionally, 17% of mepolizumab patients saw a reduction of 70% to less than 90%, compared with 8% of placebo patients. A total of 56% of patients in the placebo group had no reduction in glucocorticoid dose, showed a lack of asthma control, or pulled out of the trial, versus 36% of patients in the mepolizumab group.
Because the use of oral glucocorticoid treatment can lead to serious adverse effects, many patients with severe eosinophilic asthma may take lower doses than is needed to adequately maintain symptom control, the investigators said in the report. The results of this study suggest that adding mepolizumab to this regimen may be a viable option to allow for use of lower glucocorticoid doses in these patients while still achieving symptom control and mitigating severe complications, they added.
Mepolizumab is not currently approved anywhere in the world.
Among potential limitations of their small study, the authors wrote, was that they "assumed a relationship between a worsening of symptoms and an increase in eosinophilic airway inflammation, which may not be valid for all patients. It is possible that if we had mandated evidence of eosinophilic inflammation in the optimization phase, a different drug effect would have been seen."
Several researchers disclosed financial relationships with industry firms, including mepolizumab developer GlaxoSmithKline, the sponsor and designer of the study.
On Twitter @mrajaraman
FROM THE ERS ANNUAL CONGRESS
Key clinical point: Adding mepolizumab can reduce the need for high-dose oral glucocorticoids.
Major finding: Severe asthma patients receiving mepolizumab in addition to their oral glucocorticoid dose were 2.39 times more likely to tolerate a reduction in glucocorticoid dosage, compared with the placebo group (95% CI, 1.25-4.56; P = .008). A total of 23% of patients in the mepolizumab group had a glucocorticoid dose reduction of 90%-100%.
Data source: A randomized, double-blind study of 135 patients with severe eosinophilic asthma.
Disclosures: Dr. Bel disclosed financial relationships with several industry firms, including mepolizumab developer GlaxoSmithKline, the sponsor and designer of the study.
Prediabetes increases cancer risk by 15%
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
Prediabetes increases cancer risk in adults by 15%, with significantly increased risk for cancer of the stomach, liver, pancreas, breast, and endometrium, in a meta-analysis published Sept. 8 in Diabetologia.
Moreover, that increase in risk for all cancer types was seen in studies that used the low-threshold cutoff for impaired fasting glucose recommended by the American Diabetes Association, suggesting that international experts should adopt the ADA’s definition.
The meta-analysis included 16 eligible studies comprising 891,426 adults aged 18 and older. The study evaluated cancer risk associated with impaired fasting glucose and impaired glucose tolerance, reported Dr. Yi Huang and associates at the Clinical Medicine Research Center, First People’s Hospital of Shunde, Foshan, China.
Participants met the inclusion criteria of elevated blood glucose at baseline, duration of 3 years’ follow-up or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Prediabetes was defined as impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both. IFG was defined as a fasting plasma glucose (FPG) range of 5.6-6.9 mmol/L if the study used American Diabetes Association guidelines (Diabetes Care 26[Suppl 1]:S5–S20), or 6.1-6.9 mmol/L if the study used international guidelines. IGT was defined as a 2-hour plasma glucose of 7.8-11.1 mmol/L during an oral glucose tolerance test.
Prediabetes was associated with a 15% increased risk of cancer overall, compared with normoglycemia. The lowered ADA threshold of 5.6 mmol/L resulted in 49% increase in risk, whereas the higher threshold was linked with an 11% increase in risk. Measured by IFG, the cancer risk was 25% higher. However, these differences in risk between prediabetes definitions did not reach statistical significance, the investigators said (Diabetologia 2014 Sept. 8 [doi:10.1007/s00125-014-3361-2]).
Additionally, a secondary analysis of site-specific cancer risk showed that prediabetes was significantly associated with an increased risk of cancer of the stomach, liver, pancreas, breast, and endometrium, but was not associated with cancer of the lung, prostate, ovary, kidney, or bladder.
Subgroup analyses showed no differences in cancer risk by sex, age, or follow-up duration, but did reveal a significantly higher relative risk for Asian (1.50) than non-Asian patients (1.12).
Dr. Huang and colleagues said the results of this study have important implications for the definition and treatment of prediabetes.
"One of the most important arguments against using the lower threshold is that it greatly increases the prevalence of IFG, but without enough data to support the clinical prognostic implications," they wrote.
These results demonstrate similar cancer risk with different definitions of prediabetes, thus providing evidence for the use of the new ADA definition, which has not yet been accepted by the World Health Organization and other international groups, they said.
"These findings support the lower threshold definition IFG proposed by the ADA, and highlight the clinical value of the early management of hyperglycemia to prevent cancer," they said.
They added that several factors – insulin resistance, genetic interferences, and chronic hyperglycemia and its related conditions, such as chronic oxidative stress – may contribute to the increased cancer risk in persons with prediabetes. Typically, lifestyle intervention is the preferred treatment in prediabetes patients, and metformin may be added to delay progression to diabetes in those who present with additional risk factors such as a body mass index of at least 35 kg/m2, dyslipidemia, hypertension, or a family history of diabetes.
Research has shown that metformin may contribute to a 30% decrease in cancer risk in diabetes patients. Future exploration should focus on the possibility of protective anticancer properties of metformin in adults with prediabetes as well, the investigators said.
The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
FROM DIABETOLOGIA
Key clinical point: Prediabetes patients may have an increased risk of cancer.
Major finding: Prediabetes was associated with a 15% increased risk of cancer overall, and was significantly associated with increased risk of cancer of the stomach/colorectum, liver, pancreas, breast, and endometrium.
Data source: A meta-analysis of 16 studies comprising 891,426 adults with elevated blood glucose at baseline, follow-up of 3 years or more with a cancer risk assessment, and adjusted relative risk reported for events associated with prediabetes.
Disclosures: The study was funded by the Health Ministry of Guangdong province, China, and the Scientific Research Funds of Foshan and Shunde. The authors reported having no conflicts of interest.
Isolated systolic hypertension linked to angina; isolated diastolic hypertension linked to AAA
Isolated high systolic blood pressure is strongly associated with risk for intracerebral hemorrhage, subarachnoid hemorrhage, and stable angina, whereas isolated high diastolic blood pressure is associated with risk for abdominal aortic aneurysm, according to findings published in the Lancet.
The observations debunk widespread assumptions that isolated systolic and diastolic blood pressures are similarly and consistently associated with cardiovascular diseases, wrote Dr. Eleni Rapsomaniki and associates of the Farr Institute of Health Informatics Research in London (Lancet 2014;383:1899-1911).
"Our data support the possibility that blood pressure functions through different underlying biological mechanisms for different diseases," the researchers wrote. These data can be considered when counseling patients.
The results "also emphasize the limitations of existing blood pressure–lowering strategies," they added. Better implementation of existing blood pressure–lowering treatments and better management of other cardiovascular risk factors as part of global risk estimation could help to mitigate excess risk.
The researchers studied 1.25 million patients, aged 30 years or older, who had no previous history of cardiovascular disease. Baseline blood pressures were recorded during primary care consultations. Patients were classified as having hypertension with a baseline blood pressure reading of 140/90 mm Hg or greater, a previous diagnosis of hypertension, or repeat prescriptions for blood pressure–lowering medications.
Isolated systolic hypertension was defined as a value of 140 mm Hg or higher with a diastolic level of lower than 90 mm Hg. Isolated diastolic hypertension was defined as systolic blood pressure of less than 140 mm Hg and a diastolic level of 90 mm Hg or higher.
Endpoints were defined as the initial presentation of any of 12 cardiovascular diseases.
The primary analysis reported associations of outcomes with a 20/10 mm Hg increase in systolic/diastolic blood pressure by age group (30-59 years, 60-79 years, and 80 years or older), and estimated risks and years of life lost associated with hypertension for the index ages of 30, 60, and 80 years. The secondary analysis reported associations of blood pressure with cardiovascular outcomes, after adjusting for smoking status, diabetes, cholesterol, body mass index, and baseline treatment with hypertension drugs.
Isolated systolic hypertension was strongly associated with intracerebral hemorrhage (hazard ratio, 1.44; 95% confidence interval, 1.32-1.58), subarachnoid hemorrhage (HR, 1.43; CI, 1.25-1.63), and stable angina (HR, 1.41; CI, 1.36-1.46).
Isolated diastolic hypertension was associated with abdominal aortic aneurysm (HR, 1.45; 95% CI, 1.34-1.56).
Peripheral arterial disease had the strongest association with pulse pressure (HR, 1.23; CI, 1.20-1.27).
The lifetime risk of total cardiovascular disease at 30 years of age was 63.3% in people with hypertension and 46·1% in those with healthy blood pressure, with stable and unstable angina as the most frequent outcomes. The mean number of cardiovascular disease–free life years lost in those with hypertension was 5 years at 30 years of age, 3.4 years at 60 years, and 1.6 years at 80 years.
The study was funded by the National Institute for Health Research, the Wellcome Trust, the Medical Research Council Prognosis Research Strategy Partnership, and numerous other sources. The researchers had no competing interests.
This study provides important new information to improve risk assessment, patient counseling, and decision making for patients with hypertension.
Factors that can improve drug compliance and treatment persistence to prescribed therapy ought to be better understood than they are at present. Within 2 years, 35% of patients who start antihypertensive drug therapy discontinue treatment. Furthermore, many patients referred for so-called treatment-resistant hypertension do not take their prescribed medication. Additionally, home blood-pressure monitoring and 24-hour ambulatory blood-pressure monitoring would identify patients susceptible to the white coat effect, improve risk stratification, and increase patient engagement.
People with secondary forms of hypertension can often be offered specific treatment and are thus important to identify, in particular those with apparently treatment-resistant disease. Finally, most patients with remaining uncontrolled hypertension can be well controlled when referred to a specialist
The clinical benefit of improved risk assessment and appropriate treatment might be substantial.
Dr. Thomas Kahan is with the Karolinska Institute in Stockholm, Sweden. He made his remarks in an editorial that accompanied the study. Dr. Kahan reported receiving research grants from Celladon, Medtronic, Pfizer, and Servier.
This study provides important new information to improve risk assessment, patient counseling, and decision making for patients with hypertension.
Factors that can improve drug compliance and treatment persistence to prescribed therapy ought to be better understood than they are at present. Within 2 years, 35% of patients who start antihypertensive drug therapy discontinue treatment. Furthermore, many patients referred for so-called treatment-resistant hypertension do not take their prescribed medication. Additionally, home blood-pressure monitoring and 24-hour ambulatory blood-pressure monitoring would identify patients susceptible to the white coat effect, improve risk stratification, and increase patient engagement.
People with secondary forms of hypertension can often be offered specific treatment and are thus important to identify, in particular those with apparently treatment-resistant disease. Finally, most patients with remaining uncontrolled hypertension can be well controlled when referred to a specialist
The clinical benefit of improved risk assessment and appropriate treatment might be substantial.
Dr. Thomas Kahan is with the Karolinska Institute in Stockholm, Sweden. He made his remarks in an editorial that accompanied the study. Dr. Kahan reported receiving research grants from Celladon, Medtronic, Pfizer, and Servier.
This study provides important new information to improve risk assessment, patient counseling, and decision making for patients with hypertension.
Factors that can improve drug compliance and treatment persistence to prescribed therapy ought to be better understood than they are at present. Within 2 years, 35% of patients who start antihypertensive drug therapy discontinue treatment. Furthermore, many patients referred for so-called treatment-resistant hypertension do not take their prescribed medication. Additionally, home blood-pressure monitoring and 24-hour ambulatory blood-pressure monitoring would identify patients susceptible to the white coat effect, improve risk stratification, and increase patient engagement.
People with secondary forms of hypertension can often be offered specific treatment and are thus important to identify, in particular those with apparently treatment-resistant disease. Finally, most patients with remaining uncontrolled hypertension can be well controlled when referred to a specialist
The clinical benefit of improved risk assessment and appropriate treatment might be substantial.
Dr. Thomas Kahan is with the Karolinska Institute in Stockholm, Sweden. He made his remarks in an editorial that accompanied the study. Dr. Kahan reported receiving research grants from Celladon, Medtronic, Pfizer, and Servier.
Isolated high systolic blood pressure is strongly associated with risk for intracerebral hemorrhage, subarachnoid hemorrhage, and stable angina, whereas isolated high diastolic blood pressure is associated with risk for abdominal aortic aneurysm, according to findings published in the Lancet.
The observations debunk widespread assumptions that isolated systolic and diastolic blood pressures are similarly and consistently associated with cardiovascular diseases, wrote Dr. Eleni Rapsomaniki and associates of the Farr Institute of Health Informatics Research in London (Lancet 2014;383:1899-1911).
"Our data support the possibility that blood pressure functions through different underlying biological mechanisms for different diseases," the researchers wrote. These data can be considered when counseling patients.
The results "also emphasize the limitations of existing blood pressure–lowering strategies," they added. Better implementation of existing blood pressure–lowering treatments and better management of other cardiovascular risk factors as part of global risk estimation could help to mitigate excess risk.
The researchers studied 1.25 million patients, aged 30 years or older, who had no previous history of cardiovascular disease. Baseline blood pressures were recorded during primary care consultations. Patients were classified as having hypertension with a baseline blood pressure reading of 140/90 mm Hg or greater, a previous diagnosis of hypertension, or repeat prescriptions for blood pressure–lowering medications.
Isolated systolic hypertension was defined as a value of 140 mm Hg or higher with a diastolic level of lower than 90 mm Hg. Isolated diastolic hypertension was defined as systolic blood pressure of less than 140 mm Hg and a diastolic level of 90 mm Hg or higher.
Endpoints were defined as the initial presentation of any of 12 cardiovascular diseases.
The primary analysis reported associations of outcomes with a 20/10 mm Hg increase in systolic/diastolic blood pressure by age group (30-59 years, 60-79 years, and 80 years or older), and estimated risks and years of life lost associated with hypertension for the index ages of 30, 60, and 80 years. The secondary analysis reported associations of blood pressure with cardiovascular outcomes, after adjusting for smoking status, diabetes, cholesterol, body mass index, and baseline treatment with hypertension drugs.
Isolated systolic hypertension was strongly associated with intracerebral hemorrhage (hazard ratio, 1.44; 95% confidence interval, 1.32-1.58), subarachnoid hemorrhage (HR, 1.43; CI, 1.25-1.63), and stable angina (HR, 1.41; CI, 1.36-1.46).
Isolated diastolic hypertension was associated with abdominal aortic aneurysm (HR, 1.45; 95% CI, 1.34-1.56).
Peripheral arterial disease had the strongest association with pulse pressure (HR, 1.23; CI, 1.20-1.27).
The lifetime risk of total cardiovascular disease at 30 years of age was 63.3% in people with hypertension and 46·1% in those with healthy blood pressure, with stable and unstable angina as the most frequent outcomes. The mean number of cardiovascular disease–free life years lost in those with hypertension was 5 years at 30 years of age, 3.4 years at 60 years, and 1.6 years at 80 years.
The study was funded by the National Institute for Health Research, the Wellcome Trust, the Medical Research Council Prognosis Research Strategy Partnership, and numerous other sources. The researchers had no competing interests.
Isolated high systolic blood pressure is strongly associated with risk for intracerebral hemorrhage, subarachnoid hemorrhage, and stable angina, whereas isolated high diastolic blood pressure is associated with risk for abdominal aortic aneurysm, according to findings published in the Lancet.
The observations debunk widespread assumptions that isolated systolic and diastolic blood pressures are similarly and consistently associated with cardiovascular diseases, wrote Dr. Eleni Rapsomaniki and associates of the Farr Institute of Health Informatics Research in London (Lancet 2014;383:1899-1911).
"Our data support the possibility that blood pressure functions through different underlying biological mechanisms for different diseases," the researchers wrote. These data can be considered when counseling patients.
The results "also emphasize the limitations of existing blood pressure–lowering strategies," they added. Better implementation of existing blood pressure–lowering treatments and better management of other cardiovascular risk factors as part of global risk estimation could help to mitigate excess risk.
The researchers studied 1.25 million patients, aged 30 years or older, who had no previous history of cardiovascular disease. Baseline blood pressures were recorded during primary care consultations. Patients were classified as having hypertension with a baseline blood pressure reading of 140/90 mm Hg or greater, a previous diagnosis of hypertension, or repeat prescriptions for blood pressure–lowering medications.
Isolated systolic hypertension was defined as a value of 140 mm Hg or higher with a diastolic level of lower than 90 mm Hg. Isolated diastolic hypertension was defined as systolic blood pressure of less than 140 mm Hg and a diastolic level of 90 mm Hg or higher.
Endpoints were defined as the initial presentation of any of 12 cardiovascular diseases.
The primary analysis reported associations of outcomes with a 20/10 mm Hg increase in systolic/diastolic blood pressure by age group (30-59 years, 60-79 years, and 80 years or older), and estimated risks and years of life lost associated with hypertension for the index ages of 30, 60, and 80 years. The secondary analysis reported associations of blood pressure with cardiovascular outcomes, after adjusting for smoking status, diabetes, cholesterol, body mass index, and baseline treatment with hypertension drugs.
Isolated systolic hypertension was strongly associated with intracerebral hemorrhage (hazard ratio, 1.44; 95% confidence interval, 1.32-1.58), subarachnoid hemorrhage (HR, 1.43; CI, 1.25-1.63), and stable angina (HR, 1.41; CI, 1.36-1.46).
Isolated diastolic hypertension was associated with abdominal aortic aneurysm (HR, 1.45; 95% CI, 1.34-1.56).
Peripheral arterial disease had the strongest association with pulse pressure (HR, 1.23; CI, 1.20-1.27).
The lifetime risk of total cardiovascular disease at 30 years of age was 63.3% in people with hypertension and 46·1% in those with healthy blood pressure, with stable and unstable angina as the most frequent outcomes. The mean number of cardiovascular disease–free life years lost in those with hypertension was 5 years at 30 years of age, 3.4 years at 60 years, and 1.6 years at 80 years.
The study was funded by the National Institute for Health Research, the Wellcome Trust, the Medical Research Council Prognosis Research Strategy Partnership, and numerous other sources. The researchers had no competing interests.
FROM THE LANCET
Key clinical point: Isolated systolic and diastolic blood pressures are associated with increased risks for different types of cardiovascular disease.
Major finding: High systolic BP was strongly associated with intracerebral hemorrhage (HR, 1.44) and stable angina (HR, 1.41). High diastolic BP was associated with abdominal aortic aneurysm (HR, 1.45).
Data source: A study of the association of blood pressure with 12 cardiovascular diseases in 1.25 million patients in the CALIBER program, 30 years of age and older with no previous diagnosis of CVD.
Disclosures: The study was largely funded by the National Institute for Health Research, the Wellcome Trust, and the Medical Research Council Prognosis Research Strategy Partnership. The researchers declared no competing interests.
Shift work associated with higher diabetes risk, especially in men
People who work on a shift schedule may be at increased risk for developing type 2 diabetes, according to a new study.
In findings published July 24 in the journal Occupational & Environmental Medicine, workers on a shift schedule were 9% more likely to develop type 2 diabetes than were those working regular office hours. This risk was highest in men and those working rotating shifts.
The link between shift work and diabetes can be attributed to a number of biological factors, including interference with circadian rhythms and poor sleep quality, which may worsen insulin resistance.
Dr. Yong Gan and his colleagues at the Huazhong University of Science and Technology in Hubei, China, analyzed 12 studies with a total of 226,652 study participants, of whom 14,595 had type 2 diabetes.
Shifts were divided into five categories: rotating shifts, irregular shifts, night shifts, mixed shifts, and evening shifts. The study found that workers on rotating shifts were at the greatest risk of developing type 2 diabetes, with a 42% increase in risk, compared with workers who never did shift work. This is likely because rotating shift work often disrupts the body’s natural sleep and eating patterns, resulting in increased stress, Dr. Gan and his associates wrote.
"In most cases, the human body was exposed to continuous stress from attempts to adjust as quickly as possible to the varying working hours, but at the same time was frustrated by the continuous shift rotation," the investigators said. "Consequently, the health effect on the rotating shift groups may be more profound and pronounced than for other shift groups."
Additionally, among shift workers, men were 37% more likely than women to develop the disease, because of repeated disruption of the circadian system in men, which may adversely affect androgen secretion and lead to a greater risk of developing diabetes, the authors wrote.
The authors cited some limitations to their analysis. Shift work was not clearly defined in many original studies used in the analysis, which may have affected the results. Also, different definitions of shift exposure and diabetes outcome across studies may have resulted in heterogeneity in the results.
In addition, "more prospective and interventional studies are needed to explore the underlying mechanism and to determine the cause and effect relationships of gender difference" that link shift work and diabetes, they wrote.
Dr. Gan and his colleagues did not disclose any conflicts of interest.
On Twitter @mrajaraman
People who work on a shift schedule may be at increased risk for developing type 2 diabetes, according to a new study.
In findings published July 24 in the journal Occupational & Environmental Medicine, workers on a shift schedule were 9% more likely to develop type 2 diabetes than were those working regular office hours. This risk was highest in men and those working rotating shifts.
The link between shift work and diabetes can be attributed to a number of biological factors, including interference with circadian rhythms and poor sleep quality, which may worsen insulin resistance.
Dr. Yong Gan and his colleagues at the Huazhong University of Science and Technology in Hubei, China, analyzed 12 studies with a total of 226,652 study participants, of whom 14,595 had type 2 diabetes.
Shifts were divided into five categories: rotating shifts, irregular shifts, night shifts, mixed shifts, and evening shifts. The study found that workers on rotating shifts were at the greatest risk of developing type 2 diabetes, with a 42% increase in risk, compared with workers who never did shift work. This is likely because rotating shift work often disrupts the body’s natural sleep and eating patterns, resulting in increased stress, Dr. Gan and his associates wrote.
"In most cases, the human body was exposed to continuous stress from attempts to adjust as quickly as possible to the varying working hours, but at the same time was frustrated by the continuous shift rotation," the investigators said. "Consequently, the health effect on the rotating shift groups may be more profound and pronounced than for other shift groups."
Additionally, among shift workers, men were 37% more likely than women to develop the disease, because of repeated disruption of the circadian system in men, which may adversely affect androgen secretion and lead to a greater risk of developing diabetes, the authors wrote.
The authors cited some limitations to their analysis. Shift work was not clearly defined in many original studies used in the analysis, which may have affected the results. Also, different definitions of shift exposure and diabetes outcome across studies may have resulted in heterogeneity in the results.
In addition, "more prospective and interventional studies are needed to explore the underlying mechanism and to determine the cause and effect relationships of gender difference" that link shift work and diabetes, they wrote.
Dr. Gan and his colleagues did not disclose any conflicts of interest.
On Twitter @mrajaraman
People who work on a shift schedule may be at increased risk for developing type 2 diabetes, according to a new study.
In findings published July 24 in the journal Occupational & Environmental Medicine, workers on a shift schedule were 9% more likely to develop type 2 diabetes than were those working regular office hours. This risk was highest in men and those working rotating shifts.
The link between shift work and diabetes can be attributed to a number of biological factors, including interference with circadian rhythms and poor sleep quality, which may worsen insulin resistance.
Dr. Yong Gan and his colleagues at the Huazhong University of Science and Technology in Hubei, China, analyzed 12 studies with a total of 226,652 study participants, of whom 14,595 had type 2 diabetes.
Shifts were divided into five categories: rotating shifts, irregular shifts, night shifts, mixed shifts, and evening shifts. The study found that workers on rotating shifts were at the greatest risk of developing type 2 diabetes, with a 42% increase in risk, compared with workers who never did shift work. This is likely because rotating shift work often disrupts the body’s natural sleep and eating patterns, resulting in increased stress, Dr. Gan and his associates wrote.
"In most cases, the human body was exposed to continuous stress from attempts to adjust as quickly as possible to the varying working hours, but at the same time was frustrated by the continuous shift rotation," the investigators said. "Consequently, the health effect on the rotating shift groups may be more profound and pronounced than for other shift groups."
Additionally, among shift workers, men were 37% more likely than women to develop the disease, because of repeated disruption of the circadian system in men, which may adversely affect androgen secretion and lead to a greater risk of developing diabetes, the authors wrote.
The authors cited some limitations to their analysis. Shift work was not clearly defined in many original studies used in the analysis, which may have affected the results. Also, different definitions of shift exposure and diabetes outcome across studies may have resulted in heterogeneity in the results.
In addition, "more prospective and interventional studies are needed to explore the underlying mechanism and to determine the cause and effect relationships of gender difference" that link shift work and diabetes, they wrote.
Dr. Gan and his colleagues did not disclose any conflicts of interest.
On Twitter @mrajaraman
FROM OCCUPATIONAL & ENVIRONMENTAL MEDICINE
Key clinical point: Workers on a shift schedule are at a higher risk of developing type 2 diabetes than those working normal office hours.
Major finding: People working on shift schedules were 9% more likely to develop diabetes.
Data source: A meta-analysis of 12 studies including 226,652 study participants in Japan, Sweden, the United States, Belgium, and China.
Disclosures: Dr. Gan and his colleagues did not disclose any conflicts of interest.
Aerobic walking beneficial in patients with mild to moderate Parkinson’s
Patients with mild to moderate Parkinson’s disease who walked regularly for 6 months at the federally recommended level and duration each week improved in several disease-related and quality of life factors, according to the results of a study published July 2 in Neurology.
"Our results suggest that patients with mild to moderate PD can safely exercise per the guidelines for the general adult population and experience benefits," Dr. Ergun Y. Uc of the department of neurology at the University of Iowa, Iowa City, and his associates wrote in their report. The Department of Health & Human Services’ guidelines for physical activity are 150 minutes per week of moderate-intensity aerobic activity for healthy adults aged 18-65 years.
The investigators observed 60 patients with Parkinson’s disease (mean age at baseline, 65 years) who were required to exercise three times per week and wear electronic heart rate and walking speed monitors. During the first 2 years of the study, 43 patients had been randomly assigned to either continuous/moderate intensity training or interval training that alternated between low and vigorous intensity, but the remaining 17 patients were assigned to continuous training because preliminary analyses indicated a higher rate of musculoskeletal adverse events in those assigned to interval training. Their exercise duration increased from 15 minutes to 45 minutes over the first 6 weeks. They had a mean walking speed of 2.9 miles/hour.
Significant improvement was observed in aerobic fitness, with a mean increase of 1.56 mL/min per kilogram in maximum oxygen uptake. "Maximal effort" was defined as meeting two of three criteria: a plateau in oxygen uptake between two or more workloads, a respiratory exchange ratio of at least 1.10, and a heart rate 85% or more of age-predicted maximal heart rate (Neurology 2014;83:1-13).
The participants also experienced a mean improvement in cognition (–2.41%), based on the change in percent increase score on the Eriksen flanker task.
Parkinsonism significantly improved by a mean of –3.37 points on the Unified Parkinson’s Disease Rating Scale, and quality of life rose significantly based on a decline of 1.62 points in mean score on the Parkinson’s Disease Quality of Life Scale.
Additionally, the patients’ mean improvement of 2.8 points in the motor UPDRS score "appears to be meaningful because it exceeded the reported mean minimal clinically important difference of 2.5 (2.3-2.7) points."
All of the mean changes in the factors that the investigators measured were adjusted simultaneously for different training methods and settings, calendar year, and change in levodopa equivalent.
The investigators acknowledged that the lack of a control group is a limitation of the study and that the results cannot prove efficacy, but provide guidance for a future phase III study.
The study was funded primarily by the Department of Veterans Affairs, Rehabilitation R&D Branch Merit Review Award, with additional support from other sources.
Patients with mild to moderate Parkinson’s disease who walked regularly for 6 months at the federally recommended level and duration each week improved in several disease-related and quality of life factors, according to the results of a study published July 2 in Neurology.
"Our results suggest that patients with mild to moderate PD can safely exercise per the guidelines for the general adult population and experience benefits," Dr. Ergun Y. Uc of the department of neurology at the University of Iowa, Iowa City, and his associates wrote in their report. The Department of Health & Human Services’ guidelines for physical activity are 150 minutes per week of moderate-intensity aerobic activity for healthy adults aged 18-65 years.
The investigators observed 60 patients with Parkinson’s disease (mean age at baseline, 65 years) who were required to exercise three times per week and wear electronic heart rate and walking speed monitors. During the first 2 years of the study, 43 patients had been randomly assigned to either continuous/moderate intensity training or interval training that alternated between low and vigorous intensity, but the remaining 17 patients were assigned to continuous training because preliminary analyses indicated a higher rate of musculoskeletal adverse events in those assigned to interval training. Their exercise duration increased from 15 minutes to 45 minutes over the first 6 weeks. They had a mean walking speed of 2.9 miles/hour.
Significant improvement was observed in aerobic fitness, with a mean increase of 1.56 mL/min per kilogram in maximum oxygen uptake. "Maximal effort" was defined as meeting two of three criteria: a plateau in oxygen uptake between two or more workloads, a respiratory exchange ratio of at least 1.10, and a heart rate 85% or more of age-predicted maximal heart rate (Neurology 2014;83:1-13).
The participants also experienced a mean improvement in cognition (–2.41%), based on the change in percent increase score on the Eriksen flanker task.
Parkinsonism significantly improved by a mean of –3.37 points on the Unified Parkinson’s Disease Rating Scale, and quality of life rose significantly based on a decline of 1.62 points in mean score on the Parkinson’s Disease Quality of Life Scale.
Additionally, the patients’ mean improvement of 2.8 points in the motor UPDRS score "appears to be meaningful because it exceeded the reported mean minimal clinically important difference of 2.5 (2.3-2.7) points."
All of the mean changes in the factors that the investigators measured were adjusted simultaneously for different training methods and settings, calendar year, and change in levodopa equivalent.
The investigators acknowledged that the lack of a control group is a limitation of the study and that the results cannot prove efficacy, but provide guidance for a future phase III study.
The study was funded primarily by the Department of Veterans Affairs, Rehabilitation R&D Branch Merit Review Award, with additional support from other sources.
Patients with mild to moderate Parkinson’s disease who walked regularly for 6 months at the federally recommended level and duration each week improved in several disease-related and quality of life factors, according to the results of a study published July 2 in Neurology.
"Our results suggest that patients with mild to moderate PD can safely exercise per the guidelines for the general adult population and experience benefits," Dr. Ergun Y. Uc of the department of neurology at the University of Iowa, Iowa City, and his associates wrote in their report. The Department of Health & Human Services’ guidelines for physical activity are 150 minutes per week of moderate-intensity aerobic activity for healthy adults aged 18-65 years.
The investigators observed 60 patients with Parkinson’s disease (mean age at baseline, 65 years) who were required to exercise three times per week and wear electronic heart rate and walking speed monitors. During the first 2 years of the study, 43 patients had been randomly assigned to either continuous/moderate intensity training or interval training that alternated between low and vigorous intensity, but the remaining 17 patients were assigned to continuous training because preliminary analyses indicated a higher rate of musculoskeletal adverse events in those assigned to interval training. Their exercise duration increased from 15 minutes to 45 minutes over the first 6 weeks. They had a mean walking speed of 2.9 miles/hour.
Significant improvement was observed in aerobic fitness, with a mean increase of 1.56 mL/min per kilogram in maximum oxygen uptake. "Maximal effort" was defined as meeting two of three criteria: a plateau in oxygen uptake between two or more workloads, a respiratory exchange ratio of at least 1.10, and a heart rate 85% or more of age-predicted maximal heart rate (Neurology 2014;83:1-13).
The participants also experienced a mean improvement in cognition (–2.41%), based on the change in percent increase score on the Eriksen flanker task.
Parkinsonism significantly improved by a mean of –3.37 points on the Unified Parkinson’s Disease Rating Scale, and quality of life rose significantly based on a decline of 1.62 points in mean score on the Parkinson’s Disease Quality of Life Scale.
Additionally, the patients’ mean improvement of 2.8 points in the motor UPDRS score "appears to be meaningful because it exceeded the reported mean minimal clinically important difference of 2.5 (2.3-2.7) points."
All of the mean changes in the factors that the investigators measured were adjusted simultaneously for different training methods and settings, calendar year, and change in levodopa equivalent.
The investigators acknowledged that the lack of a control group is a limitation of the study and that the results cannot prove efficacy, but provide guidance for a future phase III study.
The study was funded primarily by the Department of Veterans Affairs, Rehabilitation R&D Branch Merit Review Award, with additional support from other sources.
FROM NEUROLOGY
Key clinical point: Patients with mild to moderate PD can safely exercise per the Department of Health & Human Services’ guidelines for physical activity for the general adult population.
Major finding: Parkinsonism significantly improved by a mean of –3.37 points on the Unified Parkinson’s Disease Rating Scale, and quality of life rose significantly based on a decline of 1.62 points in mean score on the Parkinson’s Disease Quality of Life Scale.
Data source: A 6-month study of aerobic exercise programs in 60 patients with Parkinson’s disease.
Disclosures: The study was funded primarily by the Department of Veterans Affairs Rehabilitation R&D Branch Merit Review Award, with additional support from other sources.
NIDA releases updated tools to help parents talk to teens about marijuana
The National Institute on Drug Abuse has released an updated set of resources to help parents "sort out marijuana myths from science based facts," according to a statement released May 20 by the National Institutes of Health.
Two updated booklets are being released in conjunction with the Substance Abuse and Mental Health Services Administration’s National Prevention Week 2014, which takes place May 18-24.
"Marijuana Facts for Teens" covers the topics of marijuana’s health consequences in teens, its effect on the developing brain, addiction risk, and updated information about its potential medical benefits. "Marijuana: Facts Parents Need to Know" contains updated guidelines for parents on how to tell if their child is using marijuana and how to discuss the topic with their children.
Both publications have been updated to include new sections on the dangers of synthetic marijuana, the effect of marijuana use on teens’ IQ, and potential therapeutic uses of the drug.
According to the 2013 Monitoring the Future survey, 45.5% of teens will have tried marijuana at least once by the time they graduate high school, and more than 6% of high school seniors report smoking daily.
For more information, visit http://teens.drugabuse.gov/.
The National Institute on Drug Abuse has released an updated set of resources to help parents "sort out marijuana myths from science based facts," according to a statement released May 20 by the National Institutes of Health.
Two updated booklets are being released in conjunction with the Substance Abuse and Mental Health Services Administration’s National Prevention Week 2014, which takes place May 18-24.
"Marijuana Facts for Teens" covers the topics of marijuana’s health consequences in teens, its effect on the developing brain, addiction risk, and updated information about its potential medical benefits. "Marijuana: Facts Parents Need to Know" contains updated guidelines for parents on how to tell if their child is using marijuana and how to discuss the topic with their children.
Both publications have been updated to include new sections on the dangers of synthetic marijuana, the effect of marijuana use on teens’ IQ, and potential therapeutic uses of the drug.
According to the 2013 Monitoring the Future survey, 45.5% of teens will have tried marijuana at least once by the time they graduate high school, and more than 6% of high school seniors report smoking daily.
For more information, visit http://teens.drugabuse.gov/.
The National Institute on Drug Abuse has released an updated set of resources to help parents "sort out marijuana myths from science based facts," according to a statement released May 20 by the National Institutes of Health.
Two updated booklets are being released in conjunction with the Substance Abuse and Mental Health Services Administration’s National Prevention Week 2014, which takes place May 18-24.
"Marijuana Facts for Teens" covers the topics of marijuana’s health consequences in teens, its effect on the developing brain, addiction risk, and updated information about its potential medical benefits. "Marijuana: Facts Parents Need to Know" contains updated guidelines for parents on how to tell if their child is using marijuana and how to discuss the topic with their children.
Both publications have been updated to include new sections on the dangers of synthetic marijuana, the effect of marijuana use on teens’ IQ, and potential therapeutic uses of the drug.
According to the 2013 Monitoring the Future survey, 45.5% of teens will have tried marijuana at least once by the time they graduate high school, and more than 6% of high school seniors report smoking daily.
For more information, visit http://teens.drugabuse.gov/.
Second U.S. case of MERS infection confirmed
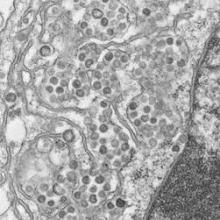
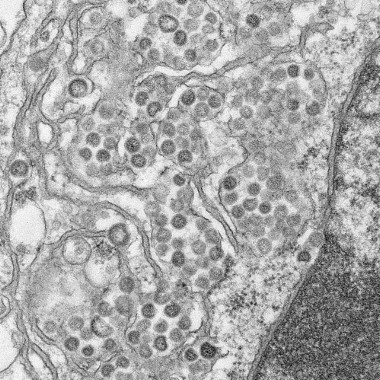
The Centers for Disease Control and Prevention has confirmed the second case of Middle East Respiratory Syndrome coronavirus (MERS-CoV) in the United States.
The patient, a health care provider working and residing in Saudi Arabia, first began to experience fever, chills, and a cough on a May 1 flight from Jeddah to Boston. The patient then traveled on two more flights – Boston to Atlanta and Atlanta to Orlando, before being admitted with symptoms to a Florida hospital on May 8.
Lab samples were tested and confirmed in Atlanta on May 11, the CDC announced in a May 12 teleconference.
The Florida patient is isolated and in stable condition, though public health officials continue to identify and reach out to the more than 500 people who may have traveled in close proximity to the infected patient.
The new case does not appear to be linked to the first U.S. case of MERS virus in Indiana, which was confirmed on May 2, officials said.
CDC director Dr. Tom Frieden said in the briefing that the MERS infection behaves similarly to the SARS virus, and that "transmission requires close contact, such as caring for someone infected when sick at home or in the hospital."
Though the health care worker is believed to have worked in a Saudi hospital treating patients with the MERS virus, information is not yet available about whether he or she had direct contact with infected patients.
The MERS virus was first reported in Saudi Arabia in 2012. CDC officials said there has been an international uptake in the number of reported cases since March of this year.
"As of May 12, a total of 538 lab-confirmed cases, including 145 deaths due to MERS, have been reported worldwide," said Dr. Anne Schuchat, director of the CDC’s National Center for Immunization and Respiratory Diseases. A vast majority of cases have occurred in Saudi Arabia, which has reported 450 cases and 118 deaths to date, she added.
Dr. Schuchat noted that despite this second importation of the virus into the United States, risk of infection remains "very low" for the general public, and the virus does not appear to spread easily in community settings. "The clusters of spread are seen most frequently on health care workers caring for MERS patients," she said.
There is no vaccine available to prevent MERS-CoV, but Dr. Schuchat emphasized the importance of practicing basic, everyday precautions such as frequent handwashing, keeping hands away from the face and mouth, staying home when sick, and avoiding contact with sick individuals.
The CDC does not recommend making changes to travel plans at this time, but does urge travelers, particularly those employed in health care settings, to seek immediate medical attention if they experience cough, fever, or respiratory illness within 14 days of travel to the Arabian peninsula.
The Centers for Disease Control and Prevention has confirmed the second case of Middle East Respiratory Syndrome coronavirus (MERS-CoV) in the United States.
The patient, a health care provider working and residing in Saudi Arabia, first began to experience fever, chills, and a cough on a May 1 flight from Jeddah to Boston. The patient then traveled on two more flights – Boston to Atlanta and Atlanta to Orlando, before being admitted with symptoms to a Florida hospital on May 8.
Lab samples were tested and confirmed in Atlanta on May 11, the CDC announced in a May 12 teleconference.
The Florida patient is isolated and in stable condition, though public health officials continue to identify and reach out to the more than 500 people who may have traveled in close proximity to the infected patient.
The new case does not appear to be linked to the first U.S. case of MERS virus in Indiana, which was confirmed on May 2, officials said.
CDC director Dr. Tom Frieden said in the briefing that the MERS infection behaves similarly to the SARS virus, and that "transmission requires close contact, such as caring for someone infected when sick at home or in the hospital."
Though the health care worker is believed to have worked in a Saudi hospital treating patients with the MERS virus, information is not yet available about whether he or she had direct contact with infected patients.
The MERS virus was first reported in Saudi Arabia in 2012. CDC officials said there has been an international uptake in the number of reported cases since March of this year.
"As of May 12, a total of 538 lab-confirmed cases, including 145 deaths due to MERS, have been reported worldwide," said Dr. Anne Schuchat, director of the CDC’s National Center for Immunization and Respiratory Diseases. A vast majority of cases have occurred in Saudi Arabia, which has reported 450 cases and 118 deaths to date, she added.
Dr. Schuchat noted that despite this second importation of the virus into the United States, risk of infection remains "very low" for the general public, and the virus does not appear to spread easily in community settings. "The clusters of spread are seen most frequently on health care workers caring for MERS patients," she said.
There is no vaccine available to prevent MERS-CoV, but Dr. Schuchat emphasized the importance of practicing basic, everyday precautions such as frequent handwashing, keeping hands away from the face and mouth, staying home when sick, and avoiding contact with sick individuals.
The CDC does not recommend making changes to travel plans at this time, but does urge travelers, particularly those employed in health care settings, to seek immediate medical attention if they experience cough, fever, or respiratory illness within 14 days of travel to the Arabian peninsula.
The Centers for Disease Control and Prevention has confirmed the second case of Middle East Respiratory Syndrome coronavirus (MERS-CoV) in the United States.
The patient, a health care provider working and residing in Saudi Arabia, first began to experience fever, chills, and a cough on a May 1 flight from Jeddah to Boston. The patient then traveled on two more flights – Boston to Atlanta and Atlanta to Orlando, before being admitted with symptoms to a Florida hospital on May 8.
Lab samples were tested and confirmed in Atlanta on May 11, the CDC announced in a May 12 teleconference.
The Florida patient is isolated and in stable condition, though public health officials continue to identify and reach out to the more than 500 people who may have traveled in close proximity to the infected patient.
The new case does not appear to be linked to the first U.S. case of MERS virus in Indiana, which was confirmed on May 2, officials said.
CDC director Dr. Tom Frieden said in the briefing that the MERS infection behaves similarly to the SARS virus, and that "transmission requires close contact, such as caring for someone infected when sick at home or in the hospital."
Though the health care worker is believed to have worked in a Saudi hospital treating patients with the MERS virus, information is not yet available about whether he or she had direct contact with infected patients.
The MERS virus was first reported in Saudi Arabia in 2012. CDC officials said there has been an international uptake in the number of reported cases since March of this year.
"As of May 12, a total of 538 lab-confirmed cases, including 145 deaths due to MERS, have been reported worldwide," said Dr. Anne Schuchat, director of the CDC’s National Center for Immunization and Respiratory Diseases. A vast majority of cases have occurred in Saudi Arabia, which has reported 450 cases and 118 deaths to date, she added.
Dr. Schuchat noted that despite this second importation of the virus into the United States, risk of infection remains "very low" for the general public, and the virus does not appear to spread easily in community settings. "The clusters of spread are seen most frequently on health care workers caring for MERS patients," she said.
There is no vaccine available to prevent MERS-CoV, but Dr. Schuchat emphasized the importance of practicing basic, everyday precautions such as frequent handwashing, keeping hands away from the face and mouth, staying home when sick, and avoiding contact with sick individuals.
The CDC does not recommend making changes to travel plans at this time, but does urge travelers, particularly those employed in health care settings, to seek immediate medical attention if they experience cough, fever, or respiratory illness within 14 days of travel to the Arabian peninsula.
FROM A CDC TELECONFERENCE
IM paliperidone improved time to relapse in incarcerated schizophrenia patients
Monthly intramuscular injections of paliperidone were significantly more effective than oral antipsychotics in maintaining patients with schizophrenia who were recently released from jail, according to a paper presented May 3 at the annual meeting of the American Psychiatric Association.
The PRIDE (Paliperidone Palmitate Research in Demonstrating Effectiveness) study "is the first prospective, randomized clinical trial to study schizophrenia treatments within the context of many ‘real world’ issues faced by patients in their daily lives, including some of the most challenging circumstances – recent incarceration or substance use," Dr. Mark Lerman, a PRIDE principal investigator, said in an interview. "Until now, no studies have been conducted comparing the effectiveness of psychopharmacologic treatments in individuals with schizophrenia following release from jail."
The PRIDE trial looked at time to treatment failure in 444 schizophrenia patients over 15 months – 226 were treated with IM paliperidone (Invega Sustenna) and 218 were treated with one of seven oral antipsychotics (aripiprazole, haloperidol, olanzapine, paliperidone, perphenazine, quetiapine, or risperidone). Time to treatment failure was defined as arrest/incarceration; psychiatric hospitalization; suicide; treatment discontinuation or supplementation due to inadequate efficacy, safety, or tolerability; or increased psychiatric services to prevent hospitalization.
All participants were adults diagnosed with schizophrenia who had been taken into custody by the criminal justice system at least twice in the previous 2 years, with at least one custody resulting in incarceration, said Dr. Lerman, medical director at the Center for Psychiatric Research at Alexian Brothers Behavioral Health Hospital in Hoffman Estates, Ill. All participants were released from their most recent custody within 90 days of screening for the trial.
IM paliperidone was associated with a significantly longer time to treatment failure than oral antipsychotics, with a median time of 416 days vs. 226 days (P = .011).
The most common treatment-emergent adverse events were injection-site pain (18.6% in patients on IM paliperidone vs. 0% on oral antipsychotics), insomnia (16.8% vs. 11.5%), weight gain (11.9% vs. 6.0%), akathisia (11.1% vs 6.9%), and anxiety (10.6% vs 7.3%).
Dr. Lerman stressed the importance of including "real world" adverse consequences in the study of schizophrenia, since mental illness patients represent a substantial proportion of the incarcerated population.
"When severely mentally ill individuals, including those with schizophrenia, are released from correctional facilities, many of them return to environments with limited support and without consistent medication or follow-up services," Dr. Lerman said. "This lack of continuous care when reentering the community can result in a ‘revolving door’ of relapse, rearrest, incarceration, and hospitalization.
"Lack of access to consistent community care may lead some individuals to cycle through jails dozens or even hundreds of times," Dr. Lerman said. "In addition to the impact on patients, these factors have created an increasingly large and costly problem for the U.S. health care system."
Dr. Lerman’s institution received funding from Janssen Pharmaceuticals. The study was sponsored by Janssen, which manufactures paliperidone.
On Twitter @mrajaraman
Monthly intramuscular injections of paliperidone were significantly more effective than oral antipsychotics in maintaining patients with schizophrenia who were recently released from jail, according to a paper presented May 3 at the annual meeting of the American Psychiatric Association.
The PRIDE (Paliperidone Palmitate Research in Demonstrating Effectiveness) study "is the first prospective, randomized clinical trial to study schizophrenia treatments within the context of many ‘real world’ issues faced by patients in their daily lives, including some of the most challenging circumstances – recent incarceration or substance use," Dr. Mark Lerman, a PRIDE principal investigator, said in an interview. "Until now, no studies have been conducted comparing the effectiveness of psychopharmacologic treatments in individuals with schizophrenia following release from jail."
The PRIDE trial looked at time to treatment failure in 444 schizophrenia patients over 15 months – 226 were treated with IM paliperidone (Invega Sustenna) and 218 were treated with one of seven oral antipsychotics (aripiprazole, haloperidol, olanzapine, paliperidone, perphenazine, quetiapine, or risperidone). Time to treatment failure was defined as arrest/incarceration; psychiatric hospitalization; suicide; treatment discontinuation or supplementation due to inadequate efficacy, safety, or tolerability; or increased psychiatric services to prevent hospitalization.
All participants were adults diagnosed with schizophrenia who had been taken into custody by the criminal justice system at least twice in the previous 2 years, with at least one custody resulting in incarceration, said Dr. Lerman, medical director at the Center for Psychiatric Research at Alexian Brothers Behavioral Health Hospital in Hoffman Estates, Ill. All participants were released from their most recent custody within 90 days of screening for the trial.
IM paliperidone was associated with a significantly longer time to treatment failure than oral antipsychotics, with a median time of 416 days vs. 226 days (P = .011).
The most common treatment-emergent adverse events were injection-site pain (18.6% in patients on IM paliperidone vs. 0% on oral antipsychotics), insomnia (16.8% vs. 11.5%), weight gain (11.9% vs. 6.0%), akathisia (11.1% vs 6.9%), and anxiety (10.6% vs 7.3%).
Dr. Lerman stressed the importance of including "real world" adverse consequences in the study of schizophrenia, since mental illness patients represent a substantial proportion of the incarcerated population.
"When severely mentally ill individuals, including those with schizophrenia, are released from correctional facilities, many of them return to environments with limited support and without consistent medication or follow-up services," Dr. Lerman said. "This lack of continuous care when reentering the community can result in a ‘revolving door’ of relapse, rearrest, incarceration, and hospitalization.
"Lack of access to consistent community care may lead some individuals to cycle through jails dozens or even hundreds of times," Dr. Lerman said. "In addition to the impact on patients, these factors have created an increasingly large and costly problem for the U.S. health care system."
Dr. Lerman’s institution received funding from Janssen Pharmaceuticals. The study was sponsored by Janssen, which manufactures paliperidone.
On Twitter @mrajaraman
Monthly intramuscular injections of paliperidone were significantly more effective than oral antipsychotics in maintaining patients with schizophrenia who were recently released from jail, according to a paper presented May 3 at the annual meeting of the American Psychiatric Association.
The PRIDE (Paliperidone Palmitate Research in Demonstrating Effectiveness) study "is the first prospective, randomized clinical trial to study schizophrenia treatments within the context of many ‘real world’ issues faced by patients in their daily lives, including some of the most challenging circumstances – recent incarceration or substance use," Dr. Mark Lerman, a PRIDE principal investigator, said in an interview. "Until now, no studies have been conducted comparing the effectiveness of psychopharmacologic treatments in individuals with schizophrenia following release from jail."
The PRIDE trial looked at time to treatment failure in 444 schizophrenia patients over 15 months – 226 were treated with IM paliperidone (Invega Sustenna) and 218 were treated with one of seven oral antipsychotics (aripiprazole, haloperidol, olanzapine, paliperidone, perphenazine, quetiapine, or risperidone). Time to treatment failure was defined as arrest/incarceration; psychiatric hospitalization; suicide; treatment discontinuation or supplementation due to inadequate efficacy, safety, or tolerability; or increased psychiatric services to prevent hospitalization.
All participants were adults diagnosed with schizophrenia who had been taken into custody by the criminal justice system at least twice in the previous 2 years, with at least one custody resulting in incarceration, said Dr. Lerman, medical director at the Center for Psychiatric Research at Alexian Brothers Behavioral Health Hospital in Hoffman Estates, Ill. All participants were released from their most recent custody within 90 days of screening for the trial.
IM paliperidone was associated with a significantly longer time to treatment failure than oral antipsychotics, with a median time of 416 days vs. 226 days (P = .011).
The most common treatment-emergent adverse events were injection-site pain (18.6% in patients on IM paliperidone vs. 0% on oral antipsychotics), insomnia (16.8% vs. 11.5%), weight gain (11.9% vs. 6.0%), akathisia (11.1% vs 6.9%), and anxiety (10.6% vs 7.3%).
Dr. Lerman stressed the importance of including "real world" adverse consequences in the study of schizophrenia, since mental illness patients represent a substantial proportion of the incarcerated population.
"When severely mentally ill individuals, including those with schizophrenia, are released from correctional facilities, many of them return to environments with limited support and without consistent medication or follow-up services," Dr. Lerman said. "This lack of continuous care when reentering the community can result in a ‘revolving door’ of relapse, rearrest, incarceration, and hospitalization.
"Lack of access to consistent community care may lead some individuals to cycle through jails dozens or even hundreds of times," Dr. Lerman said. "In addition to the impact on patients, these factors have created an increasingly large and costly problem for the U.S. health care system."
Dr. Lerman’s institution received funding from Janssen Pharmaceuticals. The study was sponsored by Janssen, which manufactures paliperidone.
On Twitter @mrajaraman
FROM THE APA ANNUAL MEETING
Key clinical point: Monthly intramuscular injection of antipsychotic medication may be a better treatment option for recently incarcerated schizophrenia patients.
Major finding: Patients treated with IM paliperidone experienced a median 416 days until treatment failure vs. a median of 226 days for those treated with oral antipsychotic medications.
Data source: The PRIDE study, a 15-month, randomized, open-label, multicenter study of 444 schizophrenia patients with a history of incarceration.
Disclosures: Dr. Lerman’s institution received funding from Janssen Pharmaceuticals. The study was sponsored by Janssen, which manufactures paliperidone.
Minimal residual disease associated with overall survival in leukemia
Eradication of minimal residual disease was associated with longer progression-free and overall survival in chronic lymphocytic leukemia patients on first-line chemoimmunotherapy, according to a study published in the journal Blood.
Dr. Paolo Strati and his associates studied 237 chronic lymphocytic leukemia (CLL) patients who were undergoing first-line treatment with fludarabine, cyclophosphamide, and rituximab (FCR). Bone-marrow minimal residual disease (MRD) was measured by flow cytometry in samples after the third course of treatment and 2 months after the last course. Results were categorized as either positive (greater than .01%) or negative (less than .01%), and assessment was performed on individuals who achieved complete or partial remission.
Results showed that 75% of participants received more than three courses of treatment with FCR and 25% received one to three courses. Complete remission was achieved in 65% of patients, complete remission with incomplete marrow recovery was achieved in 7%, nodular partial remission in 12%, and partial remission in 13%, reported Dr. Strati of the University of Texas MD Anderson Cancer Center, Houston, and his associates (Blood 2014 Apr. 4 [doi:10.1182/blood-2013-11-538116]).
At final assessment, 70 patients were MRD negative. MRD-negative status was achieved in 62 patients who had also achieved complete remission, 3 patients in complete remission with incomplete marrow recovery, and 5 patients in partial remission.
A multivariable analysis showed that progression-free survival was associated with MRD-negative status (hazard ratio, 0.1; 95% confidence interval, 0.01-0.8; P = .03), as was overall survival (HR, 0.6; 95% CI, 0.4-0.9; P = .02).
The improved outcomes in CLL patients on first-line chemoimmunotherapy treatment may indicate MRD-negative remission as a viable endpoint, the investigators wrote, though screening for MRD in blood versus bone marrow still needs to be studied. Early MRD eradication may be a desirable goal, prompting consideration of early discontinuation of treatment, they said.
The investigators did not disclose any conflicts of interest.
Eradication of minimal residual disease was associated with longer progression-free and overall survival in chronic lymphocytic leukemia patients on first-line chemoimmunotherapy, according to a study published in the journal Blood.
Dr. Paolo Strati and his associates studied 237 chronic lymphocytic leukemia (CLL) patients who were undergoing first-line treatment with fludarabine, cyclophosphamide, and rituximab (FCR). Bone-marrow minimal residual disease (MRD) was measured by flow cytometry in samples after the third course of treatment and 2 months after the last course. Results were categorized as either positive (greater than .01%) or negative (less than .01%), and assessment was performed on individuals who achieved complete or partial remission.
Results showed that 75% of participants received more than three courses of treatment with FCR and 25% received one to three courses. Complete remission was achieved in 65% of patients, complete remission with incomplete marrow recovery was achieved in 7%, nodular partial remission in 12%, and partial remission in 13%, reported Dr. Strati of the University of Texas MD Anderson Cancer Center, Houston, and his associates (Blood 2014 Apr. 4 [doi:10.1182/blood-2013-11-538116]).
At final assessment, 70 patients were MRD negative. MRD-negative status was achieved in 62 patients who had also achieved complete remission, 3 patients in complete remission with incomplete marrow recovery, and 5 patients in partial remission.
A multivariable analysis showed that progression-free survival was associated with MRD-negative status (hazard ratio, 0.1; 95% confidence interval, 0.01-0.8; P = .03), as was overall survival (HR, 0.6; 95% CI, 0.4-0.9; P = .02).
The improved outcomes in CLL patients on first-line chemoimmunotherapy treatment may indicate MRD-negative remission as a viable endpoint, the investigators wrote, though screening for MRD in blood versus bone marrow still needs to be studied. Early MRD eradication may be a desirable goal, prompting consideration of early discontinuation of treatment, they said.
The investigators did not disclose any conflicts of interest.
Eradication of minimal residual disease was associated with longer progression-free and overall survival in chronic lymphocytic leukemia patients on first-line chemoimmunotherapy, according to a study published in the journal Blood.
Dr. Paolo Strati and his associates studied 237 chronic lymphocytic leukemia (CLL) patients who were undergoing first-line treatment with fludarabine, cyclophosphamide, and rituximab (FCR). Bone-marrow minimal residual disease (MRD) was measured by flow cytometry in samples after the third course of treatment and 2 months after the last course. Results were categorized as either positive (greater than .01%) or negative (less than .01%), and assessment was performed on individuals who achieved complete or partial remission.
Results showed that 75% of participants received more than three courses of treatment with FCR and 25% received one to three courses. Complete remission was achieved in 65% of patients, complete remission with incomplete marrow recovery was achieved in 7%, nodular partial remission in 12%, and partial remission in 13%, reported Dr. Strati of the University of Texas MD Anderson Cancer Center, Houston, and his associates (Blood 2014 Apr. 4 [doi:10.1182/blood-2013-11-538116]).
At final assessment, 70 patients were MRD negative. MRD-negative status was achieved in 62 patients who had also achieved complete remission, 3 patients in complete remission with incomplete marrow recovery, and 5 patients in partial remission.
A multivariable analysis showed that progression-free survival was associated with MRD-negative status (hazard ratio, 0.1; 95% confidence interval, 0.01-0.8; P = .03), as was overall survival (HR, 0.6; 95% CI, 0.4-0.9; P = .02).
The improved outcomes in CLL patients on first-line chemoimmunotherapy treatment may indicate MRD-negative remission as a viable endpoint, the investigators wrote, though screening for MRD in blood versus bone marrow still needs to be studied. Early MRD eradication may be a desirable goal, prompting consideration of early discontinuation of treatment, they said.
The investigators did not disclose any conflicts of interest.
FROM BLOOD
Major finding: MRD-negative status was independently associated with significantly longer progression-free survival and overall survival (P = 0.03 and 0.02, respectively).
Data source: A multivariable analysis of 237 CLL patients who received first-line treatment with fludarabine, cyclophosphamide, and rituximab.
Disclosures: The investigators did not disclose any conflicts of interest.
Clinical definition of epilepsy broadened by new criteria
The International League Against Epilepsy has revised its definition of epilepsy to include additional criteria for clinical diagnosis, according to a report from the organization published April 14.
The existing definition of the disease requires that a patient have two unprovoked seizures more than 24 hours apart, wrote Dr. Robert S. Fisher of the department of neurology and neurological sciences at Stanford (Calif.) University. The new proposed definition expands upon this to include two additional criteria: one unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; and diagnosis of an epilepsy syndrome (Epilepsia 2014;55:475-82).
The changes to the definition are the result of attempts by an International League Against Epilepsy (ILAE) task force to account for clinical situations that may not be covered by the "two unprovoked seizures" requirement under the ILAE’s existing definition of epilepsy, originally published in 2005 (Epilepsia 2005;46:470-2).
Dr. Fisher and his colleagues differentiated between provoked and unprovoked seizures in the report, but emphasized that risk of seizure recurrence should also be considered when diagnosing epilepsy, rather than provocative factors alone.
"Epilepsy exists in a patient who has had a seizure and whose brain ... demonstrates a pathologic and enduring tendency to have recurrent seizures," they said. "This tendency can be imagined as a pathologic lowering of the seizure threshold, when compared to persons without the condition."
Under the previous definition, recurrent reflex seizures, such as those caused by sensitivity to light, would not be considered epilepsy because they are provoked. But the new "operational" definition would classify such a patient with epilepsy. In such a situation, "even though the seizures are provoked, the tendency to respond repeatedly to such stimuli with seizures meets the conceptual definition of epilepsy, in that reflex epilepsies are associated with an enduring abnormal predisposition to have such seizures," the authors said.
In contrast, a seizure following a "transient factor" such as a concussion in an otherwise normal brain would not meet the epilepsy criteria. A brain tumor or stroke, however, may meet the criteria for an epilepsy diagnosis depending on recurrence risk.
"Etiology should not be confused with provocative factors, as some etiologies will produce an enduring tendency to have seizures," the authors noted.
The task force acknowledged in the report that recurrence risks are unknown in most cases, but that in the absence of this knowledge, an epilepsy diagnosis may be made when the second unprovoked seizure occurs.
"On the other hand, if information is available to indicate that risk for a second seizure exceeds that which is usually considered to be epilepsy (about 60%), then epilepsy can be considered to be present," they added.
In addition to broadening the criteria for an epilepsy diagnosis, the new operational definition also clarifies that if a patient presents with evidence of an epilepsy syndrome, then epilepsy can indeed be considered present, regardless of the risk of subsequent seizures.
The new definition also allows for an individual’s epilepsy to be considered "resolved" if the person either had an age-dependent epilepsy syndrome but is now past the applicable age or has remained free of seizures for 10 years without the use of seizure medications for the last 5 years.
Dr. Fisher and his colleagues said the new ILAE definition of epilepsy seeks to bring "greater clarity and clinical relevance to the diagnostic process," but acknowledged that specialized skills in assessing recurrence risk and interpreting potential epileptogenicity of MRI results is vital to the process and may not always be available in primary care settings.
"When in doubt, practitioners should consider referring a patient to a specialized epilepsy center with experience in diagnosis," the task force said.
Although the new definition may improve clinical outcomes by encouraging doctors to consider recurrence risk after a single seizure, studies about seizure recurrence risk are limited and most diagnoses will still need to be made using the "two unprovoked seizures" rule, the authors said.
However, as more information about recurrence risks becomes available over time, "application of the epilepsy definitions will become more precise and more useful," they added.
In an online survey, the task force is seeking public comments on the proposed new definition, particularly in instances such as recurrence risk or when seizures might be considered "resolved" where an expert consensus was reached in lieu of lack of data.
Dr. Fisher and his associates reported receiving support and/or serving as consultants for numerous companies involved in epilepsy therapeutics.
The International League Against Epilepsy has revised its definition of epilepsy to include additional criteria for clinical diagnosis, according to a report from the organization published April 14.
The existing definition of the disease requires that a patient have two unprovoked seizures more than 24 hours apart, wrote Dr. Robert S. Fisher of the department of neurology and neurological sciences at Stanford (Calif.) University. The new proposed definition expands upon this to include two additional criteria: one unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; and diagnosis of an epilepsy syndrome (Epilepsia 2014;55:475-82).
The changes to the definition are the result of attempts by an International League Against Epilepsy (ILAE) task force to account for clinical situations that may not be covered by the "two unprovoked seizures" requirement under the ILAE’s existing definition of epilepsy, originally published in 2005 (Epilepsia 2005;46:470-2).
Dr. Fisher and his colleagues differentiated between provoked and unprovoked seizures in the report, but emphasized that risk of seizure recurrence should also be considered when diagnosing epilepsy, rather than provocative factors alone.
"Epilepsy exists in a patient who has had a seizure and whose brain ... demonstrates a pathologic and enduring tendency to have recurrent seizures," they said. "This tendency can be imagined as a pathologic lowering of the seizure threshold, when compared to persons without the condition."
Under the previous definition, recurrent reflex seizures, such as those caused by sensitivity to light, would not be considered epilepsy because they are provoked. But the new "operational" definition would classify such a patient with epilepsy. In such a situation, "even though the seizures are provoked, the tendency to respond repeatedly to such stimuli with seizures meets the conceptual definition of epilepsy, in that reflex epilepsies are associated with an enduring abnormal predisposition to have such seizures," the authors said.
In contrast, a seizure following a "transient factor" such as a concussion in an otherwise normal brain would not meet the epilepsy criteria. A brain tumor or stroke, however, may meet the criteria for an epilepsy diagnosis depending on recurrence risk.
"Etiology should not be confused with provocative factors, as some etiologies will produce an enduring tendency to have seizures," the authors noted.
The task force acknowledged in the report that recurrence risks are unknown in most cases, but that in the absence of this knowledge, an epilepsy diagnosis may be made when the second unprovoked seizure occurs.
"On the other hand, if information is available to indicate that risk for a second seizure exceeds that which is usually considered to be epilepsy (about 60%), then epilepsy can be considered to be present," they added.
In addition to broadening the criteria for an epilepsy diagnosis, the new operational definition also clarifies that if a patient presents with evidence of an epilepsy syndrome, then epilepsy can indeed be considered present, regardless of the risk of subsequent seizures.
The new definition also allows for an individual’s epilepsy to be considered "resolved" if the person either had an age-dependent epilepsy syndrome but is now past the applicable age or has remained free of seizures for 10 years without the use of seizure medications for the last 5 years.
Dr. Fisher and his colleagues said the new ILAE definition of epilepsy seeks to bring "greater clarity and clinical relevance to the diagnostic process," but acknowledged that specialized skills in assessing recurrence risk and interpreting potential epileptogenicity of MRI results is vital to the process and may not always be available in primary care settings.
"When in doubt, practitioners should consider referring a patient to a specialized epilepsy center with experience in diagnosis," the task force said.
Although the new definition may improve clinical outcomes by encouraging doctors to consider recurrence risk after a single seizure, studies about seizure recurrence risk are limited and most diagnoses will still need to be made using the "two unprovoked seizures" rule, the authors said.
However, as more information about recurrence risks becomes available over time, "application of the epilepsy definitions will become more precise and more useful," they added.
In an online survey, the task force is seeking public comments on the proposed new definition, particularly in instances such as recurrence risk or when seizures might be considered "resolved" where an expert consensus was reached in lieu of lack of data.
Dr. Fisher and his associates reported receiving support and/or serving as consultants for numerous companies involved in epilepsy therapeutics.
The International League Against Epilepsy has revised its definition of epilepsy to include additional criteria for clinical diagnosis, according to a report from the organization published April 14.
The existing definition of the disease requires that a patient have two unprovoked seizures more than 24 hours apart, wrote Dr. Robert S. Fisher of the department of neurology and neurological sciences at Stanford (Calif.) University. The new proposed definition expands upon this to include two additional criteria: one unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; and diagnosis of an epilepsy syndrome (Epilepsia 2014;55:475-82).
The changes to the definition are the result of attempts by an International League Against Epilepsy (ILAE) task force to account for clinical situations that may not be covered by the "two unprovoked seizures" requirement under the ILAE’s existing definition of epilepsy, originally published in 2005 (Epilepsia 2005;46:470-2).
Dr. Fisher and his colleagues differentiated between provoked and unprovoked seizures in the report, but emphasized that risk of seizure recurrence should also be considered when diagnosing epilepsy, rather than provocative factors alone.
"Epilepsy exists in a patient who has had a seizure and whose brain ... demonstrates a pathologic and enduring tendency to have recurrent seizures," they said. "This tendency can be imagined as a pathologic lowering of the seizure threshold, when compared to persons without the condition."
Under the previous definition, recurrent reflex seizures, such as those caused by sensitivity to light, would not be considered epilepsy because they are provoked. But the new "operational" definition would classify such a patient with epilepsy. In such a situation, "even though the seizures are provoked, the tendency to respond repeatedly to such stimuli with seizures meets the conceptual definition of epilepsy, in that reflex epilepsies are associated with an enduring abnormal predisposition to have such seizures," the authors said.
In contrast, a seizure following a "transient factor" such as a concussion in an otherwise normal brain would not meet the epilepsy criteria. A brain tumor or stroke, however, may meet the criteria for an epilepsy diagnosis depending on recurrence risk.
"Etiology should not be confused with provocative factors, as some etiologies will produce an enduring tendency to have seizures," the authors noted.
The task force acknowledged in the report that recurrence risks are unknown in most cases, but that in the absence of this knowledge, an epilepsy diagnosis may be made when the second unprovoked seizure occurs.
"On the other hand, if information is available to indicate that risk for a second seizure exceeds that which is usually considered to be epilepsy (about 60%), then epilepsy can be considered to be present," they added.
In addition to broadening the criteria for an epilepsy diagnosis, the new operational definition also clarifies that if a patient presents with evidence of an epilepsy syndrome, then epilepsy can indeed be considered present, regardless of the risk of subsequent seizures.
The new definition also allows for an individual’s epilepsy to be considered "resolved" if the person either had an age-dependent epilepsy syndrome but is now past the applicable age or has remained free of seizures for 10 years without the use of seizure medications for the last 5 years.
Dr. Fisher and his colleagues said the new ILAE definition of epilepsy seeks to bring "greater clarity and clinical relevance to the diagnostic process," but acknowledged that specialized skills in assessing recurrence risk and interpreting potential epileptogenicity of MRI results is vital to the process and may not always be available in primary care settings.
"When in doubt, practitioners should consider referring a patient to a specialized epilepsy center with experience in diagnosis," the task force said.
Although the new definition may improve clinical outcomes by encouraging doctors to consider recurrence risk after a single seizure, studies about seizure recurrence risk are limited and most diagnoses will still need to be made using the "two unprovoked seizures" rule, the authors said.
However, as more information about recurrence risks becomes available over time, "application of the epilepsy definitions will become more precise and more useful," they added.
In an online survey, the task force is seeking public comments on the proposed new definition, particularly in instances such as recurrence risk or when seizures might be considered "resolved" where an expert consensus was reached in lieu of lack of data.
Dr. Fisher and his associates reported receiving support and/or serving as consultants for numerous companies involved in epilepsy therapeutics.
FROM EPILEPSIA