User login
Lucas Franki is an associate editor for MDedge News, and has been with the company since 2014. He has a BA in English from Penn State University and is an Eagle Scout.
Dr. Google, potty pot, Snoopy smells cancer
Paging Dr. Google
When something hurts, itches, or burns, to whom do you turn? Not Mom or your physician – we all turn first to Google.
Apparently, sharing symptoms with our omniscient virtual overlords is a national pastime. A recent survey found that nearly 90% of people googled their health symptoms well before going to a doctor. Maybe that’s why we keep getting targeted ads for itchy foot cream?
The survey team constructed a map that broke down the most-googled symptoms for each state. While many states’ highest search were related to cold and flu, some places had more intriguing googles.
Californians have issues with sweaty palms, and New Jerseyans are concerned about their lucid dreaming. Wisconsin seems to have an epidemic of “light-colored poop” (must be all the cheese), while South Carolina has the opposite problem – their most googled symptom is “dark green stool.”
Idaho’s biggest health concern was “symptoms of E. coli”; so, if you’re visiting the Gem State, maybe bring your own food.
Find your state here!
Smartphone skull spikes
Ever felt a little down because you’re just a regular Homo sapiens? Thanks to smartphones, you might be the next step on the evolutionary chain!
Humans have started developing external occipital protuberances – actual spikes – at the base of their skull. Spikes on your skull? How metal is that?
The spike was first observed in 1885. But there has been a rapid increase in the appearance of them, and researchers believe it’s because of smartphones.
Before you start panicking, know that the skull spike is not caused by toxic radiation from your phone. David Shahar’s team from the University of the Sunshine Coast in Australia studied thousands of x-rays. They believe that the skull spikes develop because of the constant hunched-neck position we all take as we pore over our devices for hours a day. The spike is most common in younger people – 1 in 4 people aged 18-30 years had it. This calls for a LOT more yoga.
The nose knows cancer
Just when you thought man’s best friend couldn’t get any better, they go and learn how to smell cancer.
According to a study published in the Journal of the American Osteopathic Association, researchers trained a group of beagles – noted for their superior sense of smell – to sniff out differences in blood samples from healthy patients and those with lung cancer. Snoopy and friends correctly identified the cancerous samples 97% of the time and are now learning how to identify lung, breast, and colorectal cancer using breath samples.
The researchers argued that their findings could pave the way for an over-the-counter test, similar to that used for pregnancy – but where the patient breathes into a device, and it tells them whether they’re positive for cancer or not. However, we suspect the researchers just want to give everyone a dog. There are worse ideas.
And that’s not even the only bit of olfactory-related cancer news we’ve got this week. We’re moving from lung cancer to brain tumors, as a group of researchers at Tampere University in Finland have developed an artificial nose to literally sniff out malignant tissue during surgery.
Electrosurgical resection is common during brain operations, and this process gives off smoke. The nose can detect differences in the smoke from malignant tissue and healthy tissue, allowing the surgeons to more precisely remove tumors from the brain.
No word yet as to whether the surgeons actually have to wear the nose on top of their own, but we can only hope.
Legalizing a not-so-straight flush
How many times has this happened to you? You get up early, hoping to be the first one to the sewage treatment plant so you can get the really fresh wastewater samples. But when you get there, all they have is frozen.
Or maybe you’re part of the research team that analyzed the wastewater of Tacoma, Wash., to determine marijuana usage before and after it became legal in the state. In that case, you’re used to the frozen stuff. Those scientists spent 3 years looking for THC-COOH, which is produced when the psychoactive THC in cannabis is metabolized in the human body, to determine if users were switching from the illegal to the legal market.
Turns out they did. THC-COOH in wastewater increased by 9% per quarter from December 2013 to December 2016, while sales increased by nearly 70% per quarter from Aug. 1, 2014, when legal sales went into effect, to December 2016.
“Given that wastewater represents a total population measure, these findings suggest that many established users switched very quickly from the illegal to the legal market,” team leader Dan Burgard, PhD, of the University of Puget Sound, said in a written statement. “This is the strongest statement possible regarding displacement of the illegal market.”
And the frozen samples? Over the course of the study, the investigators made 387 trips to the two sewage treatment plants. We’ll let MyNorthwest.com explain the rest: “The scientists would pick up a cooler full of frozen wastewater samples, thaw them, and analyze them using liquid chromatography and mass spectrometry.”
Mmm, frozen sewage. Who says science isn’t glamorous?
Paging Dr. Google
When something hurts, itches, or burns, to whom do you turn? Not Mom or your physician – we all turn first to Google.
Apparently, sharing symptoms with our omniscient virtual overlords is a national pastime. A recent survey found that nearly 90% of people googled their health symptoms well before going to a doctor. Maybe that’s why we keep getting targeted ads for itchy foot cream?
The survey team constructed a map that broke down the most-googled symptoms for each state. While many states’ highest search were related to cold and flu, some places had more intriguing googles.
Californians have issues with sweaty palms, and New Jerseyans are concerned about their lucid dreaming. Wisconsin seems to have an epidemic of “light-colored poop” (must be all the cheese), while South Carolina has the opposite problem – their most googled symptom is “dark green stool.”
Idaho’s biggest health concern was “symptoms of E. coli”; so, if you’re visiting the Gem State, maybe bring your own food.
Find your state here!
Smartphone skull spikes
Ever felt a little down because you’re just a regular Homo sapiens? Thanks to smartphones, you might be the next step on the evolutionary chain!
Humans have started developing external occipital protuberances – actual spikes – at the base of their skull. Spikes on your skull? How metal is that?
The spike was first observed in 1885. But there has been a rapid increase in the appearance of them, and researchers believe it’s because of smartphones.
Before you start panicking, know that the skull spike is not caused by toxic radiation from your phone. David Shahar’s team from the University of the Sunshine Coast in Australia studied thousands of x-rays. They believe that the skull spikes develop because of the constant hunched-neck position we all take as we pore over our devices for hours a day. The spike is most common in younger people – 1 in 4 people aged 18-30 years had it. This calls for a LOT more yoga.
The nose knows cancer
Just when you thought man’s best friend couldn’t get any better, they go and learn how to smell cancer.
According to a study published in the Journal of the American Osteopathic Association, researchers trained a group of beagles – noted for their superior sense of smell – to sniff out differences in blood samples from healthy patients and those with lung cancer. Snoopy and friends correctly identified the cancerous samples 97% of the time and are now learning how to identify lung, breast, and colorectal cancer using breath samples.
The researchers argued that their findings could pave the way for an over-the-counter test, similar to that used for pregnancy – but where the patient breathes into a device, and it tells them whether they’re positive for cancer or not. However, we suspect the researchers just want to give everyone a dog. There are worse ideas.
And that’s not even the only bit of olfactory-related cancer news we’ve got this week. We’re moving from lung cancer to brain tumors, as a group of researchers at Tampere University in Finland have developed an artificial nose to literally sniff out malignant tissue during surgery.
Electrosurgical resection is common during brain operations, and this process gives off smoke. The nose can detect differences in the smoke from malignant tissue and healthy tissue, allowing the surgeons to more precisely remove tumors from the brain.
No word yet as to whether the surgeons actually have to wear the nose on top of their own, but we can only hope.
Legalizing a not-so-straight flush
How many times has this happened to you? You get up early, hoping to be the first one to the sewage treatment plant so you can get the really fresh wastewater samples. But when you get there, all they have is frozen.
Or maybe you’re part of the research team that analyzed the wastewater of Tacoma, Wash., to determine marijuana usage before and after it became legal in the state. In that case, you’re used to the frozen stuff. Those scientists spent 3 years looking for THC-COOH, which is produced when the psychoactive THC in cannabis is metabolized in the human body, to determine if users were switching from the illegal to the legal market.
Turns out they did. THC-COOH in wastewater increased by 9% per quarter from December 2013 to December 2016, while sales increased by nearly 70% per quarter from Aug. 1, 2014, when legal sales went into effect, to December 2016.
“Given that wastewater represents a total population measure, these findings suggest that many established users switched very quickly from the illegal to the legal market,” team leader Dan Burgard, PhD, of the University of Puget Sound, said in a written statement. “This is the strongest statement possible regarding displacement of the illegal market.”
And the frozen samples? Over the course of the study, the investigators made 387 trips to the two sewage treatment plants. We’ll let MyNorthwest.com explain the rest: “The scientists would pick up a cooler full of frozen wastewater samples, thaw them, and analyze them using liquid chromatography and mass spectrometry.”
Mmm, frozen sewage. Who says science isn’t glamorous?
Paging Dr. Google
When something hurts, itches, or burns, to whom do you turn? Not Mom or your physician – we all turn first to Google.
Apparently, sharing symptoms with our omniscient virtual overlords is a national pastime. A recent survey found that nearly 90% of people googled their health symptoms well before going to a doctor. Maybe that’s why we keep getting targeted ads for itchy foot cream?
The survey team constructed a map that broke down the most-googled symptoms for each state. While many states’ highest search were related to cold and flu, some places had more intriguing googles.
Californians have issues with sweaty palms, and New Jerseyans are concerned about their lucid dreaming. Wisconsin seems to have an epidemic of “light-colored poop” (must be all the cheese), while South Carolina has the opposite problem – their most googled symptom is “dark green stool.”
Idaho’s biggest health concern was “symptoms of E. coli”; so, if you’re visiting the Gem State, maybe bring your own food.
Find your state here!
Smartphone skull spikes
Ever felt a little down because you’re just a regular Homo sapiens? Thanks to smartphones, you might be the next step on the evolutionary chain!
Humans have started developing external occipital protuberances – actual spikes – at the base of their skull. Spikes on your skull? How metal is that?
The spike was first observed in 1885. But there has been a rapid increase in the appearance of them, and researchers believe it’s because of smartphones.
Before you start panicking, know that the skull spike is not caused by toxic radiation from your phone. David Shahar’s team from the University of the Sunshine Coast in Australia studied thousands of x-rays. They believe that the skull spikes develop because of the constant hunched-neck position we all take as we pore over our devices for hours a day. The spike is most common in younger people – 1 in 4 people aged 18-30 years had it. This calls for a LOT more yoga.
The nose knows cancer
Just when you thought man’s best friend couldn’t get any better, they go and learn how to smell cancer.
According to a study published in the Journal of the American Osteopathic Association, researchers trained a group of beagles – noted for their superior sense of smell – to sniff out differences in blood samples from healthy patients and those with lung cancer. Snoopy and friends correctly identified the cancerous samples 97% of the time and are now learning how to identify lung, breast, and colorectal cancer using breath samples.
The researchers argued that their findings could pave the way for an over-the-counter test, similar to that used for pregnancy – but where the patient breathes into a device, and it tells them whether they’re positive for cancer or not. However, we suspect the researchers just want to give everyone a dog. There are worse ideas.
And that’s not even the only bit of olfactory-related cancer news we’ve got this week. We’re moving from lung cancer to brain tumors, as a group of researchers at Tampere University in Finland have developed an artificial nose to literally sniff out malignant tissue during surgery.
Electrosurgical resection is common during brain operations, and this process gives off smoke. The nose can detect differences in the smoke from malignant tissue and healthy tissue, allowing the surgeons to more precisely remove tumors from the brain.
No word yet as to whether the surgeons actually have to wear the nose on top of their own, but we can only hope.
Legalizing a not-so-straight flush
How many times has this happened to you? You get up early, hoping to be the first one to the sewage treatment plant so you can get the really fresh wastewater samples. But when you get there, all they have is frozen.
Or maybe you’re part of the research team that analyzed the wastewater of Tacoma, Wash., to determine marijuana usage before and after it became legal in the state. In that case, you’re used to the frozen stuff. Those scientists spent 3 years looking for THC-COOH, which is produced when the psychoactive THC in cannabis is metabolized in the human body, to determine if users were switching from the illegal to the legal market.
Turns out they did. THC-COOH in wastewater increased by 9% per quarter from December 2013 to December 2016, while sales increased by nearly 70% per quarter from Aug. 1, 2014, when legal sales went into effect, to December 2016.
“Given that wastewater represents a total population measure, these findings suggest that many established users switched very quickly from the illegal to the legal market,” team leader Dan Burgard, PhD, of the University of Puget Sound, said in a written statement. “This is the strongest statement possible regarding displacement of the illegal market.”
And the frozen samples? Over the course of the study, the investigators made 387 trips to the two sewage treatment plants. We’ll let MyNorthwest.com explain the rest: “The scientists would pick up a cooler full of frozen wastewater samples, thaw them, and analyze them using liquid chromatography and mass spectrometry.”
Mmm, frozen sewage. Who says science isn’t glamorous?
Food insecurity tied to migraine in young adults
, according to Jason M. Nagata, MD, of the University of California, San Francisco, and associates.
Data were collected from a cross-sectional, nationally representative set of 14,786 young adults in the United States aged 24-32 years who participated in the 2008 National Longitudinal Study of Adolescent to Adult Health, the investigators wrote in a research letter published in JAMA Neurology.
Food insecurity was assessed by self-report through the interview question, “In the past 12 months, was there a time when (you/your household were/was) worried whether food would run out before you would get money to buy more?” Migraine was assessed by a positive answer to the interview question, “Has a doctor, nurse, or other health care professional ever told you that you have or had migraine headaches?”
In all, 1,647 study participants (11%) reported food insecurity; the prevalence of migraine in this group was 23.9%, compared with a prevalence of 13.6% in participants who did not report food insecurity. The association between food insecurity and migraine was significant both before (odds ratio, 2.00; 95% confidence interval, 1.68-2.38; P less than .001) and after adjustment (adjusted OR, .58; 95% CI, 1.30-1.95; P less than .001).
“Health care clinicians caring for persons who experience migraine should consider screening for food insecurity as a potential contributor to migraine exacerbations and provide referrals to programs such as the Supplemental Nutrition Assistance Program [formerly the Food Stamp Program] when appropriate,” the investigators concluded (JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1663).
No conflicts of interest were reported. The study was supported by grants from the University of California Global Food Initiative Fellowship, the American Academy of Pediatrics, the American Pediatric Society, and the Norman Schlossberger Research Fund from the University of California.
, according to Jason M. Nagata, MD, of the University of California, San Francisco, and associates.
Data were collected from a cross-sectional, nationally representative set of 14,786 young adults in the United States aged 24-32 years who participated in the 2008 National Longitudinal Study of Adolescent to Adult Health, the investigators wrote in a research letter published in JAMA Neurology.
Food insecurity was assessed by self-report through the interview question, “In the past 12 months, was there a time when (you/your household were/was) worried whether food would run out before you would get money to buy more?” Migraine was assessed by a positive answer to the interview question, “Has a doctor, nurse, or other health care professional ever told you that you have or had migraine headaches?”
In all, 1,647 study participants (11%) reported food insecurity; the prevalence of migraine in this group was 23.9%, compared with a prevalence of 13.6% in participants who did not report food insecurity. The association between food insecurity and migraine was significant both before (odds ratio, 2.00; 95% confidence interval, 1.68-2.38; P less than .001) and after adjustment (adjusted OR, .58; 95% CI, 1.30-1.95; P less than .001).
“Health care clinicians caring for persons who experience migraine should consider screening for food insecurity as a potential contributor to migraine exacerbations and provide referrals to programs such as the Supplemental Nutrition Assistance Program [formerly the Food Stamp Program] when appropriate,” the investigators concluded (JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1663).
No conflicts of interest were reported. The study was supported by grants from the University of California Global Food Initiative Fellowship, the American Academy of Pediatrics, the American Pediatric Society, and the Norman Schlossberger Research Fund from the University of California.
, according to Jason M. Nagata, MD, of the University of California, San Francisco, and associates.
Data were collected from a cross-sectional, nationally representative set of 14,786 young adults in the United States aged 24-32 years who participated in the 2008 National Longitudinal Study of Adolescent to Adult Health, the investigators wrote in a research letter published in JAMA Neurology.
Food insecurity was assessed by self-report through the interview question, “In the past 12 months, was there a time when (you/your household were/was) worried whether food would run out before you would get money to buy more?” Migraine was assessed by a positive answer to the interview question, “Has a doctor, nurse, or other health care professional ever told you that you have or had migraine headaches?”
In all, 1,647 study participants (11%) reported food insecurity; the prevalence of migraine in this group was 23.9%, compared with a prevalence of 13.6% in participants who did not report food insecurity. The association between food insecurity and migraine was significant both before (odds ratio, 2.00; 95% confidence interval, 1.68-2.38; P less than .001) and after adjustment (adjusted OR, .58; 95% CI, 1.30-1.95; P less than .001).
“Health care clinicians caring for persons who experience migraine should consider screening for food insecurity as a potential contributor to migraine exacerbations and provide referrals to programs such as the Supplemental Nutrition Assistance Program [formerly the Food Stamp Program] when appropriate,” the investigators concluded (JAMA Neurol. 2019 Jun 24. doi: 10.1001/jamaneurol.2019.1663).
No conflicts of interest were reported. The study was supported by grants from the University of California Global Food Initiative Fellowship, the American Academy of Pediatrics, the American Pediatric Society, and the Norman Schlossberger Research Fund from the University of California.
FROM JAMA NEUROLOGY
Medical cannabis laws appear no longer tied to drop in opioid overdose mortality
Correlations do not hold when analysis is expanded to 2017
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
Correlations do not hold when analysis is expanded to 2017
Correlations do not hold when analysis is expanded to 2017
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Increased awareness needed of bipolar disorder in primary care
A significant number of patients with in primary care also have unrecognized bipolar disorder, according to researchers at the University of Manchester (England).
In a systematic review and meta-analysis published in General Hospital Psychiatry, the researchers searched Medline, Embase, Cochrane, and PsycINFO for that measured the rate of unrecognized bipolar disorder in primary care.
The overall prevalence of unrecognized bipolar disorder within the patient group was 17%; however, that rate varied significantly. Depending on the study, the range was 5%-28%. A subgroup analysis showed that studies that relied on clinical interviews for patients with confirmed bipolar disorder had lower rates than studies that relied on self-reporting. However, that difference did not reach statistical significance (14% vs. 22%; P = .121).
“There is ... an imperative need to improve the recognition of bipolar disorder in patients in primary care. A lack of effective training of primary care physicians, competing clinical demands, and reduced financial incentives ... are key reasons for the unrecognition of mental health conditions in primary care,” the investigators noted.
No conflicts of interest were reported.
SOURCE: Daveney J et al. Gen Hosp Psychiatry. 2019 Mar 27. doi: 10.1016/j.genhosppsych.2019.03.006.
A significant number of patients with in primary care also have unrecognized bipolar disorder, according to researchers at the University of Manchester (England).
In a systematic review and meta-analysis published in General Hospital Psychiatry, the researchers searched Medline, Embase, Cochrane, and PsycINFO for that measured the rate of unrecognized bipolar disorder in primary care.
The overall prevalence of unrecognized bipolar disorder within the patient group was 17%; however, that rate varied significantly. Depending on the study, the range was 5%-28%. A subgroup analysis showed that studies that relied on clinical interviews for patients with confirmed bipolar disorder had lower rates than studies that relied on self-reporting. However, that difference did not reach statistical significance (14% vs. 22%; P = .121).
“There is ... an imperative need to improve the recognition of bipolar disorder in patients in primary care. A lack of effective training of primary care physicians, competing clinical demands, and reduced financial incentives ... are key reasons for the unrecognition of mental health conditions in primary care,” the investigators noted.
No conflicts of interest were reported.
SOURCE: Daveney J et al. Gen Hosp Psychiatry. 2019 Mar 27. doi: 10.1016/j.genhosppsych.2019.03.006.
A significant number of patients with in primary care also have unrecognized bipolar disorder, according to researchers at the University of Manchester (England).
In a systematic review and meta-analysis published in General Hospital Psychiatry, the researchers searched Medline, Embase, Cochrane, and PsycINFO for that measured the rate of unrecognized bipolar disorder in primary care.
The overall prevalence of unrecognized bipolar disorder within the patient group was 17%; however, that rate varied significantly. Depending on the study, the range was 5%-28%. A subgroup analysis showed that studies that relied on clinical interviews for patients with confirmed bipolar disorder had lower rates than studies that relied on self-reporting. However, that difference did not reach statistical significance (14% vs. 22%; P = .121).
“There is ... an imperative need to improve the recognition of bipolar disorder in patients in primary care. A lack of effective training of primary care physicians, competing clinical demands, and reduced financial incentives ... are key reasons for the unrecognition of mental health conditions in primary care,” the investigators noted.
No conflicts of interest were reported.
SOURCE: Daveney J et al. Gen Hosp Psychiatry. 2019 Mar 27. doi: 10.1016/j.genhosppsych.2019.03.006.
FROM GENERAL HOSPITAL PSYCHIATRY
Prophylactic rudeness, surgical barbecue, and MRI-ectomy
Stay rude, stay alive
Middle fingers up! Did you know there’s a biological theory that proposes rudeness as a mechanism for health?
The theory proposes that the single most important factor of determining human behavior is disease. Where disease flourishes, humans are meaner to strangers. This is a self-preservation tactic – strangers could carry sickness, so it’s best to steer clear. As people continue to avoid strangers (and potential new diseases), larger divides develop between language and culture.
Researchers looked at countries and cultures around the world and found that their theory held true: Locations that had less disease tended to have less diversity in language and culture, while higher disease rates coincided with more cultural diversity.
Can disease really be the sole factor for all human behavior, however? Tough to say, but in the meantime we’ll endorse never talking to strangers – just in case.
Facebook fires
If you’re a health care provider, you’ve probably had a difficult patient experience or two … or 7,000. In the olden days before the Internet, perhaps you turned to a trusted friend to vent your frustrations. Maybe you were an avid journaler, furiously sharing your problems with the page. With the advent of social media, however, you can publicly exorcise your doctor demons for your whole network to share!
In case you weren’t sure, this is a terrible idea – and now there are the data to prove it.
Participants in a recent study rated (fake) Facebook profiles of medical professionals who posted comments about their workday. Some comments were ambiguous, such as, “Started with new electronic patient charts today ... interesting experience for sure.” Other comments were blatantly frustrated, saying things like “What is it with some people?? I know I only went through 9 years of university ... but really, I know what I’m talking about ... yeesh!!!”
Unsurprisingly, the Facebook profiles with the obviously frustrated comments were rated “significantly less credible” than profiles with ambiguous comments, and they negatively affected willingness to become a patient of the fake doctor.
All this to say, when you get the urge to angrily post on Facebook about that overprotective parent in your office, perhaps turn to your diary instead.
Saying goodbye to a 12,000-lb friend
Lots of physicians have ordered MRI scans for their patients, but how many have performed an MRI-ectomy?
What? No, no, NO! We’re not talking about removing one from a patient! How would that even work? You do know that the patient goes inside the machine, right?
Okay, let’s try again.
How do you remove an MRI machine from a medical center? Verrrry carefully … with a forklift … after you’ve cut a big hole in the side of the building. That’s what they did at OSF HealthCare’s Center for Health – Glen Park in Peoria, Ill., on June 10. They had a party first, though, and someone brought one of those giant cookies, which said, “We will miss you, Open MRI,” the Pekin Daily Times reported.
Photos were taken, cookie was eaten, and tears were shed. “It’s definitely kind of bittersweet that it’s going away,” said Jamie White, manager of CT and MRI outpatient diagnostics.
On the day of the actual removal, a small crowd gathered outside to watch the experts who were brought in to extract the 6-ton machine. “I just took it off life support,” said Eddie Rivera, an engineer with ATI-Advanced Technologies, Miami, when he disconnected the electricity.
We’re tearing up a bit ourselves, actually, but there is some good news. The machine is not headed to that big imaging center in the sky just yet. Like the saying goes: Old MRIs never die, they just get hauled off to Arizona for refurbishment.
A bad case of heartburn
You would think that your day couldn’t get much worse than having to undergo emergency surgery. That’s a pretty rough time, no matter what. But for a 60-year-old man receiving a repair of an ascending aortic dissection, his doctors managed to add insult to a very serious injury: They lit a fire inside their patient.
According to a case study presented at the 2019 Euroanaesthesia Congress in Vienna, it all started with the patient’s history of chronic obstructive pulmonary disease. Bullae in the lungs caused by the disease were stuck to the sternum, and during an attempt to separate the lung from the sternum, a bulla was punctured, causing an air leak. To compensate, the surgeons boosted the proportion of oxygen to 100%.
In retrospect, what happened next almost seems predictable. A spark from the electrocautery device ignited a dry surgical pack, and with the assist of that extra oxygen, the doctors immediately had a fire on their hands, localized within their patient’s chest cavity. We believe this is what the medical community calls a “complication.”
To the surgeons’ credit, the fire was extinguished immediately, and after they presumably took a break to change into clean underwear, the rest of the operation went without incident. Though we imagine the patient was a bit confused when he woke up to the smell of barbecue.
Stay rude, stay alive
Middle fingers up! Did you know there’s a biological theory that proposes rudeness as a mechanism for health?
The theory proposes that the single most important factor of determining human behavior is disease. Where disease flourishes, humans are meaner to strangers. This is a self-preservation tactic – strangers could carry sickness, so it’s best to steer clear. As people continue to avoid strangers (and potential new diseases), larger divides develop between language and culture.
Researchers looked at countries and cultures around the world and found that their theory held true: Locations that had less disease tended to have less diversity in language and culture, while higher disease rates coincided with more cultural diversity.
Can disease really be the sole factor for all human behavior, however? Tough to say, but in the meantime we’ll endorse never talking to strangers – just in case.
Facebook fires
If you’re a health care provider, you’ve probably had a difficult patient experience or two … or 7,000. In the olden days before the Internet, perhaps you turned to a trusted friend to vent your frustrations. Maybe you were an avid journaler, furiously sharing your problems with the page. With the advent of social media, however, you can publicly exorcise your doctor demons for your whole network to share!
In case you weren’t sure, this is a terrible idea – and now there are the data to prove it.
Participants in a recent study rated (fake) Facebook profiles of medical professionals who posted comments about their workday. Some comments were ambiguous, such as, “Started with new electronic patient charts today ... interesting experience for sure.” Other comments were blatantly frustrated, saying things like “What is it with some people?? I know I only went through 9 years of university ... but really, I know what I’m talking about ... yeesh!!!”
Unsurprisingly, the Facebook profiles with the obviously frustrated comments were rated “significantly less credible” than profiles with ambiguous comments, and they negatively affected willingness to become a patient of the fake doctor.
All this to say, when you get the urge to angrily post on Facebook about that overprotective parent in your office, perhaps turn to your diary instead.
Saying goodbye to a 12,000-lb friend
Lots of physicians have ordered MRI scans for their patients, but how many have performed an MRI-ectomy?
What? No, no, NO! We’re not talking about removing one from a patient! How would that even work? You do know that the patient goes inside the machine, right?
Okay, let’s try again.
How do you remove an MRI machine from a medical center? Verrrry carefully … with a forklift … after you’ve cut a big hole in the side of the building. That’s what they did at OSF HealthCare’s Center for Health – Glen Park in Peoria, Ill., on June 10. They had a party first, though, and someone brought one of those giant cookies, which said, “We will miss you, Open MRI,” the Pekin Daily Times reported.
Photos were taken, cookie was eaten, and tears were shed. “It’s definitely kind of bittersweet that it’s going away,” said Jamie White, manager of CT and MRI outpatient diagnostics.
On the day of the actual removal, a small crowd gathered outside to watch the experts who were brought in to extract the 6-ton machine. “I just took it off life support,” said Eddie Rivera, an engineer with ATI-Advanced Technologies, Miami, when he disconnected the electricity.
We’re tearing up a bit ourselves, actually, but there is some good news. The machine is not headed to that big imaging center in the sky just yet. Like the saying goes: Old MRIs never die, they just get hauled off to Arizona for refurbishment.
A bad case of heartburn
You would think that your day couldn’t get much worse than having to undergo emergency surgery. That’s a pretty rough time, no matter what. But for a 60-year-old man receiving a repair of an ascending aortic dissection, his doctors managed to add insult to a very serious injury: They lit a fire inside their patient.
According to a case study presented at the 2019 Euroanaesthesia Congress in Vienna, it all started with the patient’s history of chronic obstructive pulmonary disease. Bullae in the lungs caused by the disease were stuck to the sternum, and during an attempt to separate the lung from the sternum, a bulla was punctured, causing an air leak. To compensate, the surgeons boosted the proportion of oxygen to 100%.
In retrospect, what happened next almost seems predictable. A spark from the electrocautery device ignited a dry surgical pack, and with the assist of that extra oxygen, the doctors immediately had a fire on their hands, localized within their patient’s chest cavity. We believe this is what the medical community calls a “complication.”
To the surgeons’ credit, the fire was extinguished immediately, and after they presumably took a break to change into clean underwear, the rest of the operation went without incident. Though we imagine the patient was a bit confused when he woke up to the smell of barbecue.
Stay rude, stay alive
Middle fingers up! Did you know there’s a biological theory that proposes rudeness as a mechanism for health?
The theory proposes that the single most important factor of determining human behavior is disease. Where disease flourishes, humans are meaner to strangers. This is a self-preservation tactic – strangers could carry sickness, so it’s best to steer clear. As people continue to avoid strangers (and potential new diseases), larger divides develop between language and culture.
Researchers looked at countries and cultures around the world and found that their theory held true: Locations that had less disease tended to have less diversity in language and culture, while higher disease rates coincided with more cultural diversity.
Can disease really be the sole factor for all human behavior, however? Tough to say, but in the meantime we’ll endorse never talking to strangers – just in case.
Facebook fires
If you’re a health care provider, you’ve probably had a difficult patient experience or two … or 7,000. In the olden days before the Internet, perhaps you turned to a trusted friend to vent your frustrations. Maybe you were an avid journaler, furiously sharing your problems with the page. With the advent of social media, however, you can publicly exorcise your doctor demons for your whole network to share!
In case you weren’t sure, this is a terrible idea – and now there are the data to prove it.
Participants in a recent study rated (fake) Facebook profiles of medical professionals who posted comments about their workday. Some comments were ambiguous, such as, “Started with new electronic patient charts today ... interesting experience for sure.” Other comments were blatantly frustrated, saying things like “What is it with some people?? I know I only went through 9 years of university ... but really, I know what I’m talking about ... yeesh!!!”
Unsurprisingly, the Facebook profiles with the obviously frustrated comments were rated “significantly less credible” than profiles with ambiguous comments, and they negatively affected willingness to become a patient of the fake doctor.
All this to say, when you get the urge to angrily post on Facebook about that overprotective parent in your office, perhaps turn to your diary instead.
Saying goodbye to a 12,000-lb friend
Lots of physicians have ordered MRI scans for their patients, but how many have performed an MRI-ectomy?
What? No, no, NO! We’re not talking about removing one from a patient! How would that even work? You do know that the patient goes inside the machine, right?
Okay, let’s try again.
How do you remove an MRI machine from a medical center? Verrrry carefully … with a forklift … after you’ve cut a big hole in the side of the building. That’s what they did at OSF HealthCare’s Center for Health – Glen Park in Peoria, Ill., on June 10. They had a party first, though, and someone brought one of those giant cookies, which said, “We will miss you, Open MRI,” the Pekin Daily Times reported.
Photos were taken, cookie was eaten, and tears were shed. “It’s definitely kind of bittersweet that it’s going away,” said Jamie White, manager of CT and MRI outpatient diagnostics.
On the day of the actual removal, a small crowd gathered outside to watch the experts who were brought in to extract the 6-ton machine. “I just took it off life support,” said Eddie Rivera, an engineer with ATI-Advanced Technologies, Miami, when he disconnected the electricity.
We’re tearing up a bit ourselves, actually, but there is some good news. The machine is not headed to that big imaging center in the sky just yet. Like the saying goes: Old MRIs never die, they just get hauled off to Arizona for refurbishment.
A bad case of heartburn
You would think that your day couldn’t get much worse than having to undergo emergency surgery. That’s a pretty rough time, no matter what. But for a 60-year-old man receiving a repair of an ascending aortic dissection, his doctors managed to add insult to a very serious injury: They lit a fire inside their patient.
According to a case study presented at the 2019 Euroanaesthesia Congress in Vienna, it all started with the patient’s history of chronic obstructive pulmonary disease. Bullae in the lungs caused by the disease were stuck to the sternum, and during an attempt to separate the lung from the sternum, a bulla was punctured, causing an air leak. To compensate, the surgeons boosted the proportion of oxygen to 100%.
In retrospect, what happened next almost seems predictable. A spark from the electrocautery device ignited a dry surgical pack, and with the assist of that extra oxygen, the doctors immediately had a fire on their hands, localized within their patient’s chest cavity. We believe this is what the medical community calls a “complication.”
To the surgeons’ credit, the fire was extinguished immediately, and after they presumably took a break to change into clean underwear, the rest of the operation went without incident. Though we imagine the patient was a bit confused when he woke up to the smell of barbecue.
LTC-associated suicide among older adults more common than previously thought
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
FROM JAMA NETWORK OPEN
Key clinical point: Suicide associated with long-term care may be more common than previous data have indicated.
Major finding: About 2.2% of the suicide deaths reported to the National Violent Death Reporting System occurred or were associated with long-term care.
Study details: An analysis of 47,759 suicides and undetermined deaths in adults aged at least 55 years with data included in the National Violent Death Reporting System.Disclosures: The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
Source: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
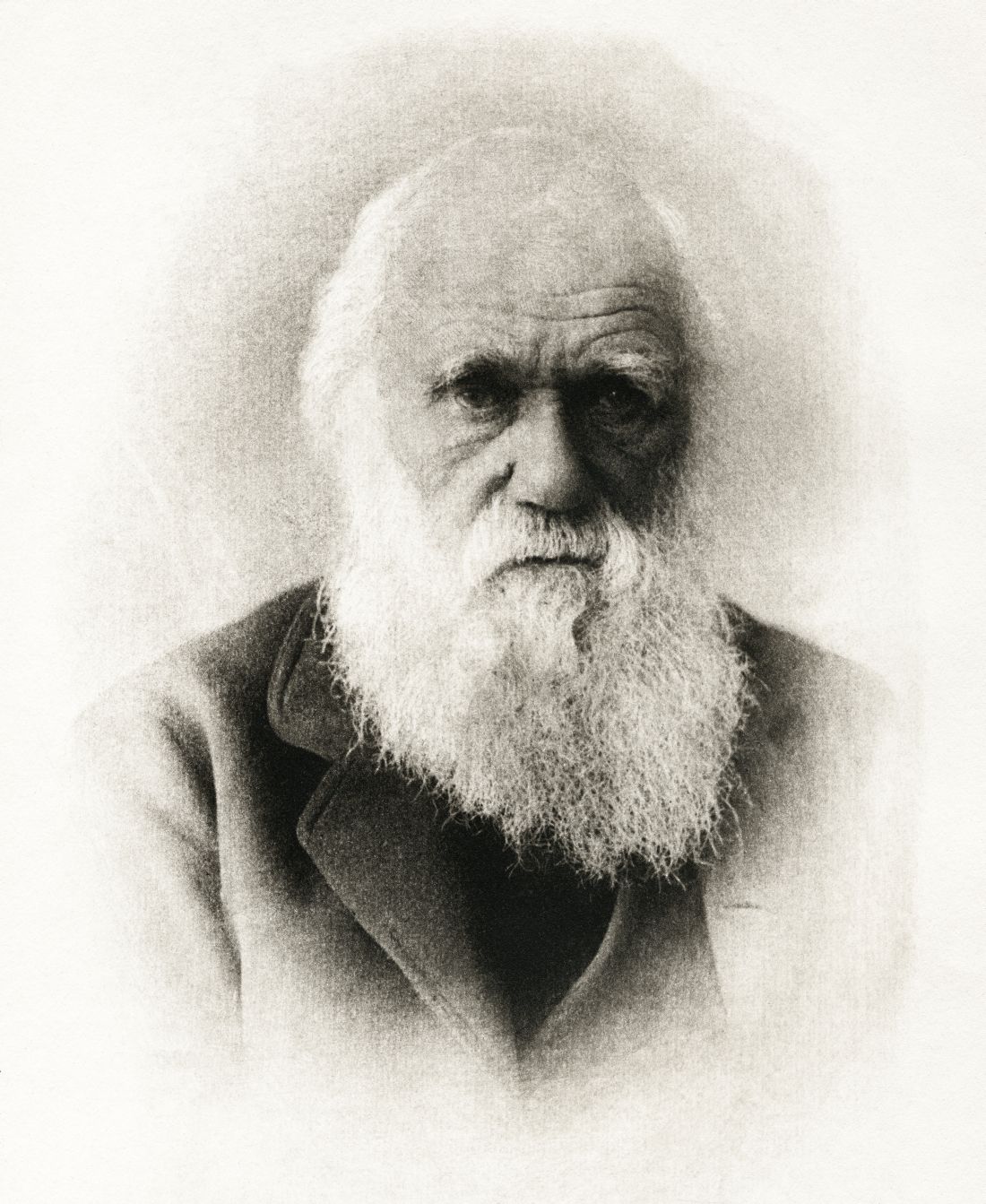
Darwin’s diet of species, umbrellas’ searing SPF, and trypophobia terror
Forks out for science
True scientists should have no limits to what they’ll do for their research. Charles Darwin proved that greatly during his life – he spent years discovering and cataloging new species.
But did you know he also chowed down on nearly every animal he found?
His taste for unusual fare began at Cambridge as a member of the “Glutton Club.” He and his fellow gluttons were dedicated to sampling “birds and beasts which were before unknown to human palate,” as reported in an article on NPR. His eating adventures only grew while on the famed Beagle voyage, where he tried puma, iguanas, armadillos, giant tortoises, and even a 20-pound rodent that he declared “the very best meat I ever tasted.”
The noble tradition of tasting your test subjects continues today. The author of the article referenced above asked scientists on social media for stories of eating what they are supposed to be studying, and the answers came pouring in.
From tasting tadpoles to nibbling on 30,000-year-old bison meat, scientists all over the world have found they can’t resist the call to just have a tiny taste.
The umbrella’s just not cutting it
Bad news for everyone who hates melanoma but also hates sunscreen: That Tommy Bahama beach umbrella isn’t doing much to shield your skin.
A team lead by researcher Hao Ou-Yang conducted a study comparing the effects of harmful UV rays on subjects who used sunscreen with subjects who only used the shade of an umbrella.
In the battle of Sun vs. Umbrella, the humble parasol had no chance. While neither sun protection method completely prevented sunburn, 78% of the umbrella-only group experienced sunburn, compared with 25% of the sunscreen wearers.
The researchers determined that umbrella shade alone is not sufficient to protect against sunburn during extended exposure to the sun (in the case of this experiment, exposure was 3.5 hours). Sunscreen, despite being smelly and sticky and gloopy, is definitely needed to protect skin from those UV rays. So, suck it up and pile on that Coppertone this summer.
Oh no, there goes Tokyo (again)
Godzilla. The king of the monsters. For 65 years, the big green guy has been the scourge (mostly) of Japan and the entire world. He arrives, he destroys, and there is very nearly nothing we can do about him.
If you’re an astute fan of the Godzilla series (and we love a good Godzilla movie at MDedge headquarters), you’ll have noticed that Godzilla is a lot bigger than he used to be. In the first movie, he stood at a relatively meager 50 meters. Nowadays, he’s scraping 120 meters, more than double his original size.
What’s going on?
In an actual study published in Science, a team at Dartmouth College in Hanover, N.H., determined that Godzilla is evolving 30 times faster than any other organism on Earth. It’s enough to make even the influenza virus jealous.
So, what is going on? Why is Godzilla evolving so quickly? The scientists assumed that Godzilla is a ceratosaurid dinosaur and ran through the usual suspects. No other dinosaur of that family got so big. Genetic drift and natural selection can’t explain it either.
The truth may be more unsettling: Our own anxiety is fueling his growth. Godzilla was born because of nuclear testing and the fear stemming from it. And the Dartmouth team even found a correlation between Godzilla’s size and American military spending from 1954 to 2019, a neat barometer of the world’s collective anxiety.
Or, you know, people just want to see a 400-foot-tall lizard destroying things. But that’s hardly worthy of a study in an elite research journal.
Hole lotta trypophobia goin’ on
We didn’t know this was even a thing, but Twitter doesn’t like pictures of woodpeckers … digging little holes in tree trunks … and then stuffing the holes with acorns.
A recent tweet of such a photo caused a minor pandemic of virality when users reacted with revulsion and panic caused by trypophobia, which is a fear of irregular patterns of small holes or bumps. You won’t find trypophobia in the DSM-5 – the term was first used in an Internet forum in 2005 – but it is a source of some debate among academics, according to Live Science.
One group says the patterns look like some poisonous animals, and that people are programmed by evolution to fear such creatures. Others suggest that the reaction is not fear but disgust, because the patterns of holes look like the lesions and pustules caused by infectious diseases such as smallpox.
We’re not scientists, so we’ll stay out of the debate on causality. But we do think we’ve uncovered the first documented case, and it goes back to the 1960s TV series “Batman.” The hero’s trusted sidekick, Robin (coincidentally, another type of bird), must have been the first person with trypophobia:
“Holy tintinnabulation!”
“Holy uncanny photographic mental processes!”
“Holy priceless collection of Etruscan snoods!”
Holy patterns of woodpecker acorns! There can be no diagnostic doubt: For Robin, it was all about the holes.

Forks out for science
True scientists should have no limits to what they’ll do for their research. Charles Darwin proved that greatly during his life – he spent years discovering and cataloging new species.
But did you know he also chowed down on nearly every animal he found?
His taste for unusual fare began at Cambridge as a member of the “Glutton Club.” He and his fellow gluttons were dedicated to sampling “birds and beasts which were before unknown to human palate,” as reported in an article on NPR. His eating adventures only grew while on the famed Beagle voyage, where he tried puma, iguanas, armadillos, giant tortoises, and even a 20-pound rodent that he declared “the very best meat I ever tasted.”
The noble tradition of tasting your test subjects continues today. The author of the article referenced above asked scientists on social media for stories of eating what they are supposed to be studying, and the answers came pouring in.
From tasting tadpoles to nibbling on 30,000-year-old bison meat, scientists all over the world have found they can’t resist the call to just have a tiny taste.
The umbrella’s just not cutting it
Bad news for everyone who hates melanoma but also hates sunscreen: That Tommy Bahama beach umbrella isn’t doing much to shield your skin.
A team lead by researcher Hao Ou-Yang conducted a study comparing the effects of harmful UV rays on subjects who used sunscreen with subjects who only used the shade of an umbrella.
In the battle of Sun vs. Umbrella, the humble parasol had no chance. While neither sun protection method completely prevented sunburn, 78% of the umbrella-only group experienced sunburn, compared with 25% of the sunscreen wearers.
The researchers determined that umbrella shade alone is not sufficient to protect against sunburn during extended exposure to the sun (in the case of this experiment, exposure was 3.5 hours). Sunscreen, despite being smelly and sticky and gloopy, is definitely needed to protect skin from those UV rays. So, suck it up and pile on that Coppertone this summer.
Oh no, there goes Tokyo (again)
Godzilla. The king of the monsters. For 65 years, the big green guy has been the scourge (mostly) of Japan and the entire world. He arrives, he destroys, and there is very nearly nothing we can do about him.
If you’re an astute fan of the Godzilla series (and we love a good Godzilla movie at MDedge headquarters), you’ll have noticed that Godzilla is a lot bigger than he used to be. In the first movie, he stood at a relatively meager 50 meters. Nowadays, he’s scraping 120 meters, more than double his original size.
What’s going on?
In an actual study published in Science, a team at Dartmouth College in Hanover, N.H., determined that Godzilla is evolving 30 times faster than any other organism on Earth. It’s enough to make even the influenza virus jealous.
So, what is going on? Why is Godzilla evolving so quickly? The scientists assumed that Godzilla is a ceratosaurid dinosaur and ran through the usual suspects. No other dinosaur of that family got so big. Genetic drift and natural selection can’t explain it either.
The truth may be more unsettling: Our own anxiety is fueling his growth. Godzilla was born because of nuclear testing and the fear stemming from it. And the Dartmouth team even found a correlation between Godzilla’s size and American military spending from 1954 to 2019, a neat barometer of the world’s collective anxiety.
Or, you know, people just want to see a 400-foot-tall lizard destroying things. But that’s hardly worthy of a study in an elite research journal.
Hole lotta trypophobia goin’ on
We didn’t know this was even a thing, but Twitter doesn’t like pictures of woodpeckers … digging little holes in tree trunks … and then stuffing the holes with acorns.
A recent tweet of such a photo caused a minor pandemic of virality when users reacted with revulsion and panic caused by trypophobia, which is a fear of irregular patterns of small holes or bumps. You won’t find trypophobia in the DSM-5 – the term was first used in an Internet forum in 2005 – but it is a source of some debate among academics, according to Live Science.
One group says the patterns look like some poisonous animals, and that people are programmed by evolution to fear such creatures. Others suggest that the reaction is not fear but disgust, because the patterns of holes look like the lesions and pustules caused by infectious diseases such as smallpox.
We’re not scientists, so we’ll stay out of the debate on causality. But we do think we’ve uncovered the first documented case, and it goes back to the 1960s TV series “Batman.” The hero’s trusted sidekick, Robin (coincidentally, another type of bird), must have been the first person with trypophobia:
“Holy tintinnabulation!”
“Holy uncanny photographic mental processes!”
“Holy priceless collection of Etruscan snoods!”
Holy patterns of woodpecker acorns! There can be no diagnostic doubt: For Robin, it was all about the holes.

Forks out for science
True scientists should have no limits to what they’ll do for their research. Charles Darwin proved that greatly during his life – he spent years discovering and cataloging new species.
But did you know he also chowed down on nearly every animal he found?
His taste for unusual fare began at Cambridge as a member of the “Glutton Club.” He and his fellow gluttons were dedicated to sampling “birds and beasts which were before unknown to human palate,” as reported in an article on NPR. His eating adventures only grew while on the famed Beagle voyage, where he tried puma, iguanas, armadillos, giant tortoises, and even a 20-pound rodent that he declared “the very best meat I ever tasted.”
The noble tradition of tasting your test subjects continues today. The author of the article referenced above asked scientists on social media for stories of eating what they are supposed to be studying, and the answers came pouring in.
From tasting tadpoles to nibbling on 30,000-year-old bison meat, scientists all over the world have found they can’t resist the call to just have a tiny taste.
The umbrella’s just not cutting it
Bad news for everyone who hates melanoma but also hates sunscreen: That Tommy Bahama beach umbrella isn’t doing much to shield your skin.
A team lead by researcher Hao Ou-Yang conducted a study comparing the effects of harmful UV rays on subjects who used sunscreen with subjects who only used the shade of an umbrella.
In the battle of Sun vs. Umbrella, the humble parasol had no chance. While neither sun protection method completely prevented sunburn, 78% of the umbrella-only group experienced sunburn, compared with 25% of the sunscreen wearers.
The researchers determined that umbrella shade alone is not sufficient to protect against sunburn during extended exposure to the sun (in the case of this experiment, exposure was 3.5 hours). Sunscreen, despite being smelly and sticky and gloopy, is definitely needed to protect skin from those UV rays. So, suck it up and pile on that Coppertone this summer.
Oh no, there goes Tokyo (again)
Godzilla. The king of the monsters. For 65 years, the big green guy has been the scourge (mostly) of Japan and the entire world. He arrives, he destroys, and there is very nearly nothing we can do about him.
If you’re an astute fan of the Godzilla series (and we love a good Godzilla movie at MDedge headquarters), you’ll have noticed that Godzilla is a lot bigger than he used to be. In the first movie, he stood at a relatively meager 50 meters. Nowadays, he’s scraping 120 meters, more than double his original size.
What’s going on?
In an actual study published in Science, a team at Dartmouth College in Hanover, N.H., determined that Godzilla is evolving 30 times faster than any other organism on Earth. It’s enough to make even the influenza virus jealous.
So, what is going on? Why is Godzilla evolving so quickly? The scientists assumed that Godzilla is a ceratosaurid dinosaur and ran through the usual suspects. No other dinosaur of that family got so big. Genetic drift and natural selection can’t explain it either.
The truth may be more unsettling: Our own anxiety is fueling his growth. Godzilla was born because of nuclear testing and the fear stemming from it. And the Dartmouth team even found a correlation between Godzilla’s size and American military spending from 1954 to 2019, a neat barometer of the world’s collective anxiety.
Or, you know, people just want to see a 400-foot-tall lizard destroying things. But that’s hardly worthy of a study in an elite research journal.
Hole lotta trypophobia goin’ on
We didn’t know this was even a thing, but Twitter doesn’t like pictures of woodpeckers … digging little holes in tree trunks … and then stuffing the holes with acorns.
A recent tweet of such a photo caused a minor pandemic of virality when users reacted with revulsion and panic caused by trypophobia, which is a fear of irregular patterns of small holes or bumps. You won’t find trypophobia in the DSM-5 – the term was first used in an Internet forum in 2005 – but it is a source of some debate among academics, according to Live Science.
One group says the patterns look like some poisonous animals, and that people are programmed by evolution to fear such creatures. Others suggest that the reaction is not fear but disgust, because the patterns of holes look like the lesions and pustules caused by infectious diseases such as smallpox.
We’re not scientists, so we’ll stay out of the debate on causality. But we do think we’ve uncovered the first documented case, and it goes back to the 1960s TV series “Batman.” The hero’s trusted sidekick, Robin (coincidentally, another type of bird), must have been the first person with trypophobia:
“Holy tintinnabulation!”
“Holy uncanny photographic mental processes!”
“Holy priceless collection of Etruscan snoods!”
Holy patterns of woodpecker acorns! There can be no diagnostic doubt: For Robin, it was all about the holes.

FDA approves Keytruda for metastatic HNSCC
The Food and Drug Administration has approved pembrolizumab (Keytruda) for the first-line treatment of patients with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).
FDA approval was based on results of the randomized, multicenter, three-arm, open‑label, active‑controlled KEYNOTE-048 trial. The 882 patients in the trial had metastatic HNSCC, and they received either single-agent pembrolizumab; pembrolizumab, carboplatin or cisplatin, and platinum and fluorouracil; or cetuximab, carboplatin or cisplatin, and platinum and fluorouracil.
Patients who received pembrolizumab plus chemotherapy had a mean overall survival of 13.0 months, compared with 10.7 months in the cetuximab plus chemotherapy group (hazard ratio, 0.77; 95% CI, 0.63-0.93; P = .0067).
In the patient subgroups that received single-agent pembrolizumab, overall survival was 12.3 months in patients with a Combined Positive Score of at least 1, compared with 10.3 months for the cetuximab plus chemotherapy group (HR, 0.78; 95% CI, 0.64-0.96; P = .0171). In patients with a Combined Positive Score of at least 20, overall survival was 14.9 months in the pembrolizumab-only group and 10.7 months in the cetuximab plus chemotherapy group (HR, 0.61; 95% CI, 0.45-0.83; P = .0015).
The most common adverse events in patients who received single-agent pembrolizumab were fatigue, constipation, and rash. In patients who received pembrolizumab plus chemotherapy, the most common adverse events were nausea, fatigue, constipation, vomiting, mucosal inflammation, diarrhea, decreased appetite, stomatitis, and cough.
Pembrolizumab is approved for use in combination with platinum and fluorouracil for all patients and as a single agent for patients whose tumors express programmed death–ligand 1, the FDA said.
The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.
Find the full press release on the FDA website.
The Food and Drug Administration has approved pembrolizumab (Keytruda) for the first-line treatment of patients with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).
FDA approval was based on results of the randomized, multicenter, three-arm, open‑label, active‑controlled KEYNOTE-048 trial. The 882 patients in the trial had metastatic HNSCC, and they received either single-agent pembrolizumab; pembrolizumab, carboplatin or cisplatin, and platinum and fluorouracil; or cetuximab, carboplatin or cisplatin, and platinum and fluorouracil.
Patients who received pembrolizumab plus chemotherapy had a mean overall survival of 13.0 months, compared with 10.7 months in the cetuximab plus chemotherapy group (hazard ratio, 0.77; 95% CI, 0.63-0.93; P = .0067).
In the patient subgroups that received single-agent pembrolizumab, overall survival was 12.3 months in patients with a Combined Positive Score of at least 1, compared with 10.3 months for the cetuximab plus chemotherapy group (HR, 0.78; 95% CI, 0.64-0.96; P = .0171). In patients with a Combined Positive Score of at least 20, overall survival was 14.9 months in the pembrolizumab-only group and 10.7 months in the cetuximab plus chemotherapy group (HR, 0.61; 95% CI, 0.45-0.83; P = .0015).
The most common adverse events in patients who received single-agent pembrolizumab were fatigue, constipation, and rash. In patients who received pembrolizumab plus chemotherapy, the most common adverse events were nausea, fatigue, constipation, vomiting, mucosal inflammation, diarrhea, decreased appetite, stomatitis, and cough.
Pembrolizumab is approved for use in combination with platinum and fluorouracil for all patients and as a single agent for patients whose tumors express programmed death–ligand 1, the FDA said.
The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.
Find the full press release on the FDA website.
The Food and Drug Administration has approved pembrolizumab (Keytruda) for the first-line treatment of patients with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).
FDA approval was based on results of the randomized, multicenter, three-arm, open‑label, active‑controlled KEYNOTE-048 trial. The 882 patients in the trial had metastatic HNSCC, and they received either single-agent pembrolizumab; pembrolizumab, carboplatin or cisplatin, and platinum and fluorouracil; or cetuximab, carboplatin or cisplatin, and platinum and fluorouracil.
Patients who received pembrolizumab plus chemotherapy had a mean overall survival of 13.0 months, compared with 10.7 months in the cetuximab plus chemotherapy group (hazard ratio, 0.77; 95% CI, 0.63-0.93; P = .0067).
In the patient subgroups that received single-agent pembrolizumab, overall survival was 12.3 months in patients with a Combined Positive Score of at least 1, compared with 10.3 months for the cetuximab plus chemotherapy group (HR, 0.78; 95% CI, 0.64-0.96; P = .0171). In patients with a Combined Positive Score of at least 20, overall survival was 14.9 months in the pembrolizumab-only group and 10.7 months in the cetuximab plus chemotherapy group (HR, 0.61; 95% CI, 0.45-0.83; P = .0015).
The most common adverse events in patients who received single-agent pembrolizumab were fatigue, constipation, and rash. In patients who received pembrolizumab plus chemotherapy, the most common adverse events were nausea, fatigue, constipation, vomiting, mucosal inflammation, diarrhea, decreased appetite, stomatitis, and cough.
Pembrolizumab is approved for use in combination with platinum and fluorouracil for all patients and as a single agent for patients whose tumors express programmed death–ligand 1, the FDA said.
The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.
Find the full press release on the FDA website.
FDA approves Polivy for DLBCL
The Food and Drug Administration has granted accelerated approval to Polivy (polatuzumab vedotin-piiq), in conjunction with bendamustine and a rituximab product, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have undergone at least two prior therapies.
The FDA approval is based on results of an open-label, multicenter clinical trial of 80 patients with DLBCL who had undergone at least one prior regimen. Patients received either Polivy plus bendamustine and rituximab or only bendamustine and rituximab for six 21-day cycles. At the completion of therapy, 40% of patients who received Polivy in conjunction with bendamustine and rituximab achieved a complete response, compared with 18% of patients who received only bendamustine and rituximab; total response was 63% in those who received Polivy and 25% in those who did not.
The most common adverse events included neutropenia, thrombocytopenia, anemia, peripheral neuropathy, fatigue, diarrhea, pyrexia, decreased appetite, and pneumonia. Serious adverse events occurred in 64% of patients, most commonly from infection; the most common cause for treatment discontinuation was cytopenia.
The recommended dose of Polivy is 1.8 mg/kg as an intravenous infusion over 90 minutes every 21 days for six cycles in combination with bendamustine and a rituximab product, the FDA said. Subsequent infusions may be administered over 30 minutes if the previous infusion is tolerated.
Find the full press release on the FDA website.
The Food and Drug Administration has granted accelerated approval to Polivy (polatuzumab vedotin-piiq), in conjunction with bendamustine and a rituximab product, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have undergone at least two prior therapies.
The FDA approval is based on results of an open-label, multicenter clinical trial of 80 patients with DLBCL who had undergone at least one prior regimen. Patients received either Polivy plus bendamustine and rituximab or only bendamustine and rituximab for six 21-day cycles. At the completion of therapy, 40% of patients who received Polivy in conjunction with bendamustine and rituximab achieved a complete response, compared with 18% of patients who received only bendamustine and rituximab; total response was 63% in those who received Polivy and 25% in those who did not.
The most common adverse events included neutropenia, thrombocytopenia, anemia, peripheral neuropathy, fatigue, diarrhea, pyrexia, decreased appetite, and pneumonia. Serious adverse events occurred in 64% of patients, most commonly from infection; the most common cause for treatment discontinuation was cytopenia.
The recommended dose of Polivy is 1.8 mg/kg as an intravenous infusion over 90 minutes every 21 days for six cycles in combination with bendamustine and a rituximab product, the FDA said. Subsequent infusions may be administered over 30 minutes if the previous infusion is tolerated.
Find the full press release on the FDA website.
The Food and Drug Administration has granted accelerated approval to Polivy (polatuzumab vedotin-piiq), in conjunction with bendamustine and a rituximab product, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have undergone at least two prior therapies.
The FDA approval is based on results of an open-label, multicenter clinical trial of 80 patients with DLBCL who had undergone at least one prior regimen. Patients received either Polivy plus bendamustine and rituximab or only bendamustine and rituximab for six 21-day cycles. At the completion of therapy, 40% of patients who received Polivy in conjunction with bendamustine and rituximab achieved a complete response, compared with 18% of patients who received only bendamustine and rituximab; total response was 63% in those who received Polivy and 25% in those who did not.
The most common adverse events included neutropenia, thrombocytopenia, anemia, peripheral neuropathy, fatigue, diarrhea, pyrexia, decreased appetite, and pneumonia. Serious adverse events occurred in 64% of patients, most commonly from infection; the most common cause for treatment discontinuation was cytopenia.
The recommended dose of Polivy is 1.8 mg/kg as an intravenous infusion over 90 minutes every 21 days for six cycles in combination with bendamustine and a rituximab product, the FDA said. Subsequent infusions may be administered over 30 minutes if the previous infusion is tolerated.
Find the full press release on the FDA website.
AMA announces final eight recipients of Reimagining Residency initiative
led by medical schools, residency programs, and health systems.
“After establishing a framework for creating the medical schools of the future, the AMA is now supporting innovation projects that will better align residency training with the evolving needs of patients and communities, as well as the workforce needs of the current and future health care system,” AMA CEO and Executive Vice President James L. Madara, MD, stated in a press release.
The projects include curricular innovations to address workforce shortages and address social determinants of health. Other projects will be developed within the framework of innovations and concepts developed and implemented in medical schools over the past 6 years by the AMA’s consortium. These projects include implementing competency-based programs and incorporating Health Systems Science into residency training.
The projects were chosen through a competitive grant process by an advisory panel made up of leading experts in medical education, and selection was based on how well each program met the goals of the initiative: improving the transition from medical school to residency, ensuring readiness for practice through modifications of residency curricula, and optimizing the learning environment to support well-being.
Each of the following projects will receive $1.8 million over 5 years:
- California Oregon Medical Partnership to Address Disparities in Rural Education and Health – Oregon Health & Science University, Portland, and the University of California, Davis
- Fully Integrated Readiness for Service Training: Enhancing the Continuum from Medical School to Residency to Practice – University of North Carolina at Chapel Hill
- NYU Transition to Residency Advantage – New York University
- Promotion in Place: Enhancing Trainee Well-Being and Patient Care Through Time-Variable Graduate Medical Education – Partners HealthCare System, Massachusetts General Hospital, and Brigham and Women’s Hospital, Boston
- Reimagining Residency: Ensuring Readiness for Practice Through Growing Interprofessional Partnerships to Advance Care and Education – Maine Medical Center, Portland
- Residency Training to Effectively Address Social Determinants of Health: Applying a Curricular Framework Across Four Primary Care Specialties – Montefiore Health System, New York
- The Graduate Medical Training “Laboratory”: An Innovative Program to Generate, Implement, and Evaluate Interventions to Improve Resident Burnout and Clinical Skill – Johns Hopkins University, Baltimore; Stanford (Calif.) University; and the University of Alabama at Birmingham
- The GOL2D Project (Goals of Life and Learning Delineated): Collaboration Across Academic Health Systems to Better Align GME with Learner, Patient, and Societal Needs – Vanderbilt University, Nashville, Tenn., and the University of Mississippi, Jackson
An additional three programs will receive a smaller $50,000 planning grant to expedite further exploration and development.
“As the health care landscape and technology rapidly evolve, the AMA will continue working with its community of innovation to drive the future of medicine by supporting significant redesign in physician training. Our goal is to ensure physicians are prepared to adapt, grow, and thrive at every stage of their training and career. Better prepared physicians will deliver more effective and equitable health care,” said Dr. Madara.
led by medical schools, residency programs, and health systems.
“After establishing a framework for creating the medical schools of the future, the AMA is now supporting innovation projects that will better align residency training with the evolving needs of patients and communities, as well as the workforce needs of the current and future health care system,” AMA CEO and Executive Vice President James L. Madara, MD, stated in a press release.
The projects include curricular innovations to address workforce shortages and address social determinants of health. Other projects will be developed within the framework of innovations and concepts developed and implemented in medical schools over the past 6 years by the AMA’s consortium. These projects include implementing competency-based programs and incorporating Health Systems Science into residency training.
The projects were chosen through a competitive grant process by an advisory panel made up of leading experts in medical education, and selection was based on how well each program met the goals of the initiative: improving the transition from medical school to residency, ensuring readiness for practice through modifications of residency curricula, and optimizing the learning environment to support well-being.
Each of the following projects will receive $1.8 million over 5 years:
- California Oregon Medical Partnership to Address Disparities in Rural Education and Health – Oregon Health & Science University, Portland, and the University of California, Davis
- Fully Integrated Readiness for Service Training: Enhancing the Continuum from Medical School to Residency to Practice – University of North Carolina at Chapel Hill
- NYU Transition to Residency Advantage – New York University
- Promotion in Place: Enhancing Trainee Well-Being and Patient Care Through Time-Variable Graduate Medical Education – Partners HealthCare System, Massachusetts General Hospital, and Brigham and Women’s Hospital, Boston
- Reimagining Residency: Ensuring Readiness for Practice Through Growing Interprofessional Partnerships to Advance Care and Education – Maine Medical Center, Portland
- Residency Training to Effectively Address Social Determinants of Health: Applying a Curricular Framework Across Four Primary Care Specialties – Montefiore Health System, New York
- The Graduate Medical Training “Laboratory”: An Innovative Program to Generate, Implement, and Evaluate Interventions to Improve Resident Burnout and Clinical Skill – Johns Hopkins University, Baltimore; Stanford (Calif.) University; and the University of Alabama at Birmingham
- The GOL2D Project (Goals of Life and Learning Delineated): Collaboration Across Academic Health Systems to Better Align GME with Learner, Patient, and Societal Needs – Vanderbilt University, Nashville, Tenn., and the University of Mississippi, Jackson
An additional three programs will receive a smaller $50,000 planning grant to expedite further exploration and development.
“As the health care landscape and technology rapidly evolve, the AMA will continue working with its community of innovation to drive the future of medicine by supporting significant redesign in physician training. Our goal is to ensure physicians are prepared to adapt, grow, and thrive at every stage of their training and career. Better prepared physicians will deliver more effective and equitable health care,” said Dr. Madara.
led by medical schools, residency programs, and health systems.
“After establishing a framework for creating the medical schools of the future, the AMA is now supporting innovation projects that will better align residency training with the evolving needs of patients and communities, as well as the workforce needs of the current and future health care system,” AMA CEO and Executive Vice President James L. Madara, MD, stated in a press release.
The projects include curricular innovations to address workforce shortages and address social determinants of health. Other projects will be developed within the framework of innovations and concepts developed and implemented in medical schools over the past 6 years by the AMA’s consortium. These projects include implementing competency-based programs and incorporating Health Systems Science into residency training.
The projects were chosen through a competitive grant process by an advisory panel made up of leading experts in medical education, and selection was based on how well each program met the goals of the initiative: improving the transition from medical school to residency, ensuring readiness for practice through modifications of residency curricula, and optimizing the learning environment to support well-being.
Each of the following projects will receive $1.8 million over 5 years:
- California Oregon Medical Partnership to Address Disparities in Rural Education and Health – Oregon Health & Science University, Portland, and the University of California, Davis
- Fully Integrated Readiness for Service Training: Enhancing the Continuum from Medical School to Residency to Practice – University of North Carolina at Chapel Hill
- NYU Transition to Residency Advantage – New York University
- Promotion in Place: Enhancing Trainee Well-Being and Patient Care Through Time-Variable Graduate Medical Education – Partners HealthCare System, Massachusetts General Hospital, and Brigham and Women’s Hospital, Boston
- Reimagining Residency: Ensuring Readiness for Practice Through Growing Interprofessional Partnerships to Advance Care and Education – Maine Medical Center, Portland
- Residency Training to Effectively Address Social Determinants of Health: Applying a Curricular Framework Across Four Primary Care Specialties – Montefiore Health System, New York
- The Graduate Medical Training “Laboratory”: An Innovative Program to Generate, Implement, and Evaluate Interventions to Improve Resident Burnout and Clinical Skill – Johns Hopkins University, Baltimore; Stanford (Calif.) University; and the University of Alabama at Birmingham
- The GOL2D Project (Goals of Life and Learning Delineated): Collaboration Across Academic Health Systems to Better Align GME with Learner, Patient, and Societal Needs – Vanderbilt University, Nashville, Tenn., and the University of Mississippi, Jackson
An additional three programs will receive a smaller $50,000 planning grant to expedite further exploration and development.
“As the health care landscape and technology rapidly evolve, the AMA will continue working with its community of innovation to drive the future of medicine by supporting significant redesign in physician training. Our goal is to ensure physicians are prepared to adapt, grow, and thrive at every stage of their training and career. Better prepared physicians will deliver more effective and equitable health care,” said Dr. Madara.