User login
Lucas Franki is an associate editor for MDedge News, and has been with the company since 2014. He has a BA in English from Penn State University and is an Eagle Scout.
Inflammatory markers may start in later stages of bipolar disorder
Interleukin-6, IL-1 receptor antagonist (IL-1RA), and tumor necrosis factor–alpha (TNF-alpha) activity was associated with inflammation and neurodegeneration in patients with chronic bipolar disorder, according to Sercan Karabulut, MD, of Kepez State Hospital in Antalya, Turkey, and associates.
In a study published in the Turkish Journal of Psychiatry, the investigators collected enzyme-linked immunosorbent assays from 30 patients with early-stage bipolar disorder, 77 with chronic disease, and 30 healthy controls. Early-stage disease patients were significantly younger than chronic patients (25.3 years vs. 37.8 years). reported Dr. Karabulut and associates.
Patients with chronic bipolar disorder had significantly increased levels of all measured markers, compared with those with early-stage disease and the healthy controls. IL-6 and IL-1RA levels correlated with neuron-specific enolase and S100B, biomarkers that are associated with glial alterations and neuronal damage. TNF-alpha correlated with scores on the Clinical Global Impressions Scale and other measures.
“The present findings support in part the hypothesis that inflammation starts at later stages of [bipolar disorder], presumably as an associated effect of gliosis and neuronal loss, which appear to be particularly associated with IL-1RA and IL-6 activity,” the investigators wrote. “TNF-alpha ... might be a useful prognostic marker in patients with [bipolar disorder].”
No conflicts of interest were reported.
SOURCE: Karabulut S et al. Turk Psikiyatri Derg. 2019 Winter;30(2):75-81.
Interleukin-6, IL-1 receptor antagonist (IL-1RA), and tumor necrosis factor–alpha (TNF-alpha) activity was associated with inflammation and neurodegeneration in patients with chronic bipolar disorder, according to Sercan Karabulut, MD, of Kepez State Hospital in Antalya, Turkey, and associates.
In a study published in the Turkish Journal of Psychiatry, the investigators collected enzyme-linked immunosorbent assays from 30 patients with early-stage bipolar disorder, 77 with chronic disease, and 30 healthy controls. Early-stage disease patients were significantly younger than chronic patients (25.3 years vs. 37.8 years). reported Dr. Karabulut and associates.
Patients with chronic bipolar disorder had significantly increased levels of all measured markers, compared with those with early-stage disease and the healthy controls. IL-6 and IL-1RA levels correlated with neuron-specific enolase and S100B, biomarkers that are associated with glial alterations and neuronal damage. TNF-alpha correlated with scores on the Clinical Global Impressions Scale and other measures.
“The present findings support in part the hypothesis that inflammation starts at later stages of [bipolar disorder], presumably as an associated effect of gliosis and neuronal loss, which appear to be particularly associated with IL-1RA and IL-6 activity,” the investigators wrote. “TNF-alpha ... might be a useful prognostic marker in patients with [bipolar disorder].”
No conflicts of interest were reported.
SOURCE: Karabulut S et al. Turk Psikiyatri Derg. 2019 Winter;30(2):75-81.
Interleukin-6, IL-1 receptor antagonist (IL-1RA), and tumor necrosis factor–alpha (TNF-alpha) activity was associated with inflammation and neurodegeneration in patients with chronic bipolar disorder, according to Sercan Karabulut, MD, of Kepez State Hospital in Antalya, Turkey, and associates.
In a study published in the Turkish Journal of Psychiatry, the investigators collected enzyme-linked immunosorbent assays from 30 patients with early-stage bipolar disorder, 77 with chronic disease, and 30 healthy controls. Early-stage disease patients were significantly younger than chronic patients (25.3 years vs. 37.8 years). reported Dr. Karabulut and associates.
Patients with chronic bipolar disorder had significantly increased levels of all measured markers, compared with those with early-stage disease and the healthy controls. IL-6 and IL-1RA levels correlated with neuron-specific enolase and S100B, biomarkers that are associated with glial alterations and neuronal damage. TNF-alpha correlated with scores on the Clinical Global Impressions Scale and other measures.
“The present findings support in part the hypothesis that inflammation starts at later stages of [bipolar disorder], presumably as an associated effect of gliosis and neuronal loss, which appear to be particularly associated with IL-1RA and IL-6 activity,” the investigators wrote. “TNF-alpha ... might be a useful prognostic marker in patients with [bipolar disorder].”
No conflicts of interest were reported.
SOURCE: Karabulut S et al. Turk Psikiyatri Derg. 2019 Winter;30(2):75-81.
FROM THE TURKISH JOURNAL OF PSYCHIATRY
iPhone trypophobia and chicken kissin’
Please, no photos
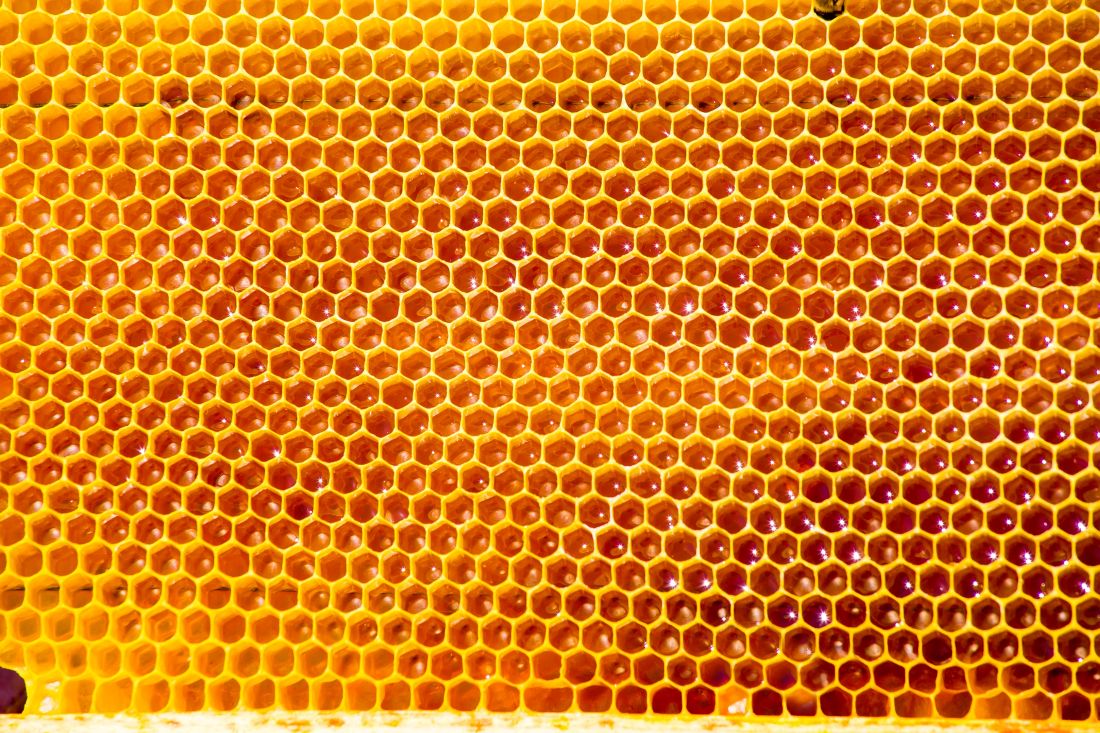
What does the new iPhone have in common with honeycombs and lotus flowers? They all strike terror and nausea in the hearts of trypophobics everywhere.
Trypophobia, in case you haven’t heard, is the fear of irregular patterns of holes or bumps clustered together. It sounds weird, until you look at photos like this and your skin starts to crawl. Now, we can add the iPhone 11 to the list of fear-inducing everyday objects. The new phone design includes three camera lenses, and it’s giving people … issues. Sure, amateur photographers are ecstatic, but social media users collectively shuddered over their keyboards when the tri-camera was revealed.
Trypophobia is not widely studied, but it’s been theorized that the revulsion is a biological instinct against things that look unsafe or diseased. Safe to say this might lead to Apple losing that core demographic – the trypophobe population. They’ll be switching to Androids en masse.
Don’t kiss your chickens after they hatch
All in all, it’s pretty easy to avoid getting salmonella. Refrigerate your food properly. Don’t eat undercooked ground meats. Oh, and don’t kiss the chickens you’ve been raising in your backyard.
Okay, that’s not the only takeaway from a Centers for Disease Control and Prevention update on the 2019 salmonella outbreak that has so far affected just over a thousand people in 49 states. Because the outbreak has been linked to the increased prevalence of backyard poultry, with 67% of patients interviewed reporting contact with chicks and/or ducklings, the CDC has issued a slew of recommendations on how to avoid salmonella.
Some of them are common sense: Don’t let small children handle livestock, and wash your hands after contact. Some are a bit bizarre: Don’t let poultry wander through your house, and don’t eat or drink where livestock roam and live (eww).
Then there’s the gem: Don’t kiss your chickens, or snuggle them and then touch your face and/or mouth.
We know baby chickens or ducks are adorable. And there’s absolutely nothing wrong with loving your livestock like a cat or dog. Just don’t, um, love your livestock.
Dept. of unintended consequences
This week’s case report is brought to you by the entomologists of Texas Medical Center in Houston.
The original problem: Large numbers of birds, such as grackles and pigeons, which may carry diseases and make a mess with their droppings, were gathering in large numbers in Texas Medical Center’s live oak trees. The campus is visited by 10 million people seeking health care each year.
The solution: Cover the trees with nets to prevent the birds from gathering.
The new problem: The lack of predatory birds has “created a haven for a flourishing population of Megalopyge opercularis, commonly referred to as asps,” according to investigators at Rice University. The asp in question happens to be one of North America’s most toxic caterpillars, and they are 7,300% more abundant in the netted trees, compared with nonnetted trees nearby.
The discussion: “I’ve been stung by a lot of things, and an asp sting definitely ranks high up there,” said Mattheau Comerford, one of the investigators. “It feels like a broken bone, and the pain lasts for hours. I was stung on the wrist, and the pain traveled up my arm, into my arm pit, and my jaw started to feel pain.”
The LOTME recommendation: In this case, the rats with wings … er, we mean pigeons, seem to be the lesser of two evils. Of course, compared with poisonous caterpillars, even kissing a chicken would be the lesser of two evils.

Please, no photos
What does the new iPhone have in common with honeycombs and lotus flowers? They all strike terror and nausea in the hearts of trypophobics everywhere.
Trypophobia, in case you haven’t heard, is the fear of irregular patterns of holes or bumps clustered together. It sounds weird, until you look at photos like this and your skin starts to crawl. Now, we can add the iPhone 11 to the list of fear-inducing everyday objects. The new phone design includes three camera lenses, and it’s giving people … issues. Sure, amateur photographers are ecstatic, but social media users collectively shuddered over their keyboards when the tri-camera was revealed.
Trypophobia is not widely studied, but it’s been theorized that the revulsion is a biological instinct against things that look unsafe or diseased. Safe to say this might lead to Apple losing that core demographic – the trypophobe population. They’ll be switching to Androids en masse.
Don’t kiss your chickens after they hatch
All in all, it’s pretty easy to avoid getting salmonella. Refrigerate your food properly. Don’t eat undercooked ground meats. Oh, and don’t kiss the chickens you’ve been raising in your backyard.
Okay, that’s not the only takeaway from a Centers for Disease Control and Prevention update on the 2019 salmonella outbreak that has so far affected just over a thousand people in 49 states. Because the outbreak has been linked to the increased prevalence of backyard poultry, with 67% of patients interviewed reporting contact with chicks and/or ducklings, the CDC has issued a slew of recommendations on how to avoid salmonella.
Some of them are common sense: Don’t let small children handle livestock, and wash your hands after contact. Some are a bit bizarre: Don’t let poultry wander through your house, and don’t eat or drink where livestock roam and live (eww).
Then there’s the gem: Don’t kiss your chickens, or snuggle them and then touch your face and/or mouth.
We know baby chickens or ducks are adorable. And there’s absolutely nothing wrong with loving your livestock like a cat or dog. Just don’t, um, love your livestock.
Dept. of unintended consequences
This week’s case report is brought to you by the entomologists of Texas Medical Center in Houston.
The original problem: Large numbers of birds, such as grackles and pigeons, which may carry diseases and make a mess with their droppings, were gathering in large numbers in Texas Medical Center’s live oak trees. The campus is visited by 10 million people seeking health care each year.
The solution: Cover the trees with nets to prevent the birds from gathering.
The new problem: The lack of predatory birds has “created a haven for a flourishing population of Megalopyge opercularis, commonly referred to as asps,” according to investigators at Rice University. The asp in question happens to be one of North America’s most toxic caterpillars, and they are 7,300% more abundant in the netted trees, compared with nonnetted trees nearby.
The discussion: “I’ve been stung by a lot of things, and an asp sting definitely ranks high up there,” said Mattheau Comerford, one of the investigators. “It feels like a broken bone, and the pain lasts for hours. I was stung on the wrist, and the pain traveled up my arm, into my arm pit, and my jaw started to feel pain.”
The LOTME recommendation: In this case, the rats with wings … er, we mean pigeons, seem to be the lesser of two evils. Of course, compared with poisonous caterpillars, even kissing a chicken would be the lesser of two evils.

Please, no photos
What does the new iPhone have in common with honeycombs and lotus flowers? They all strike terror and nausea in the hearts of trypophobics everywhere.
Trypophobia, in case you haven’t heard, is the fear of irregular patterns of holes or bumps clustered together. It sounds weird, until you look at photos like this and your skin starts to crawl. Now, we can add the iPhone 11 to the list of fear-inducing everyday objects. The new phone design includes three camera lenses, and it’s giving people … issues. Sure, amateur photographers are ecstatic, but social media users collectively shuddered over their keyboards when the tri-camera was revealed.
Trypophobia is not widely studied, but it’s been theorized that the revulsion is a biological instinct against things that look unsafe or diseased. Safe to say this might lead to Apple losing that core demographic – the trypophobe population. They’ll be switching to Androids en masse.
Don’t kiss your chickens after they hatch
All in all, it’s pretty easy to avoid getting salmonella. Refrigerate your food properly. Don’t eat undercooked ground meats. Oh, and don’t kiss the chickens you’ve been raising in your backyard.
Okay, that’s not the only takeaway from a Centers for Disease Control and Prevention update on the 2019 salmonella outbreak that has so far affected just over a thousand people in 49 states. Because the outbreak has been linked to the increased prevalence of backyard poultry, with 67% of patients interviewed reporting contact with chicks and/or ducklings, the CDC has issued a slew of recommendations on how to avoid salmonella.
Some of them are common sense: Don’t let small children handle livestock, and wash your hands after contact. Some are a bit bizarre: Don’t let poultry wander through your house, and don’t eat or drink where livestock roam and live (eww).
Then there’s the gem: Don’t kiss your chickens, or snuggle them and then touch your face and/or mouth.
We know baby chickens or ducks are adorable. And there’s absolutely nothing wrong with loving your livestock like a cat or dog. Just don’t, um, love your livestock.
Dept. of unintended consequences
This week’s case report is brought to you by the entomologists of Texas Medical Center in Houston.
The original problem: Large numbers of birds, such as grackles and pigeons, which may carry diseases and make a mess with their droppings, were gathering in large numbers in Texas Medical Center’s live oak trees. The campus is visited by 10 million people seeking health care each year.
The solution: Cover the trees with nets to prevent the birds from gathering.
The new problem: The lack of predatory birds has “created a haven for a flourishing population of Megalopyge opercularis, commonly referred to as asps,” according to investigators at Rice University. The asp in question happens to be one of North America’s most toxic caterpillars, and they are 7,300% more abundant in the netted trees, compared with nonnetted trees nearby.
The discussion: “I’ve been stung by a lot of things, and an asp sting definitely ranks high up there,” said Mattheau Comerford, one of the investigators. “It feels like a broken bone, and the pain lasts for hours. I was stung on the wrist, and the pain traveled up my arm, into my arm pit, and my jaw started to feel pain.”
The LOTME recommendation: In this case, the rats with wings … er, we mean pigeons, seem to be the lesser of two evils. Of course, compared with poisonous caterpillars, even kissing a chicken would be the lesser of two evils.

Colorectal screening cost effective in cystic fibrosis patients
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
Help your patients understand what do expect during and how to prepare for a colonoscopy by sharing AGA’s patient education at https://www.gastro.org/practice-guidance/gi-patient-center/topic/colonoscopy.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
Help your patients understand what do expect during and how to prepare for a colonoscopy by sharing AGA’s patient education at https://www.gastro.org/practice-guidance/gi-patient-center/topic/colonoscopy.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
Help your patients understand what do expect during and how to prepare for a colonoscopy by sharing AGA’s patient education at https://www.gastro.org/practice-guidance/gi-patient-center/topic/colonoscopy.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
FROM GASTROENTEROLOGY
FDA issues warning to JUUL on illegal marketing of e-cigarettes
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
Colorectal screening cost effective in cystic fibrosis patients
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
Screening for colorectal cancer in patients with cystic fibrosis is cost effective, and should be started at a younger age and performed more often, new research suggests.
While colorectal cancer (CRC) screening traditionally begins at age 50 years in people at average risk for the disease, those at high risk usually begin undergoing colonoscopies at an earlier age. Patients with cystic fibrosis fall under the latter category, wrote Andrea Gini, of the department of public health at Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues, with an incidence of CRC up to 30 times higher than the general population, but their shorter lifespan has led to a “different trade-off between the benefits and harms of CRC screening.”
Between 2000 and 2015, the median predicted survival age for patients with cystic fibrosis increased from 33.3 years to 41.7 years; this increased survival has brought increased risk for other diseases, particularly in the GI tract, Mr. Gini and colleagues wrote in Gastroenterology. By using the Microsimulation Screening Analysis–Colon model – a joint project between Erasmus Medical Center and Memorial Sloan Kettering Cancer Center in New York – the investigators assessed the cost-effectiveness of CRC screening in patients with cystic fibrosis.
Three cohorts of 10 million patients each were simulated, with one cohort having undergone transplant, one cohort not having transplant, and one cohort of individuals without cystic fibrosis. The simulated patient age was 30 years in 2017. A total of 76 different colonoscopy-screening strategies were assessed, with each differing in screening interval (3, 5, or 10 years for colonoscopy), age to start screening (30, 35, 40, 45, or 50 years), and age to end screening (55, 60, 65, 70, or 75 years). The optimal screening strategy was determined based on a willingness-to-pay threshold of $100,000 per life-year gained, the investigators wrote.
In the absence of screening, the mortality rate for nontransplant cystic fibrosis patients was 19.1 per 1,000 people, and the rate for cystic fibrosis patients who had undergone transplant was 22.3 per 1,000 people. The standard screening strategy prevented more than 73% of CRC deaths in the general population, 66% of deaths in nontransplant cystic fibrosis patients, and 36% of deaths in cystic fibrosis patients with transplant; however, the model predicted that only 22% of individuals who received a transplant and 36% of those who did not would reach the age of 50 years.
According to the model, the optimal colonoscopy-screening strategy for nontransplant patients was one screen every 5 years, starting at 40 and screening until the age of 75. The incremental cost-effectiveness ratio (ICER) was $84,000 per life-year gained; CRC incidence was reduced by 52% and CRC mortality was reduced by 79%. For transplant patients, the best strategy was one screen every 3 years between the ages of 35 and 55, which reduced CRC mortality by 82% at an ICER of $71,000 per life-year gained.
In a separate analysis of fecal immunochemical testing, a less-demanding alternative to colonoscopy, the optimal screening strategy was an annual test between the age of 35 and 75 years for nontransplant cystic fibrosis patients, for an ICER of $47,000 per life-year gained and a CRC mortality reduction of 78%. The best strategy for transplant patients was once a year between the ages of 30 and 60, which reduced CRC mortality by 77% at an ICER of $86,000 per life-year gained. While fecal immunochemical testing may be more cost effective than colonoscopy, “specific evidence of its performance in the cystic fibrosis population is required before considering this screening modality,” the investigators noted.
“This study indicates that there is benefit to earlier CRC screening in the cystic fibrosis population and [that it] can be done at acceptable costs,” the investigators wrote. “The findings of this analysis support clinicians, researchers, and policy makers who aim to define a tailored CRC screening for individuals with cystic fibrosis in the United States.”
The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
SOURCE: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
FROM GASTROENTEROLOGY
Key clinical point: Colorectal cancer screening in patients with cystic fibrosis is cost effective and should be performed more often and at a younger age.
Major finding:
Study details: The Microsimulation Screening Analysis–Colon, involving three simulated cohorts of 10 million people.
Disclosures: The study was funded by the Cystic Fibrosis Foundation, the Cancer Intervention and Surveillance Modeling Network consortium, and Memorial Sloan Kettering Cancer Center. The investigators reported no conflicts of interest.
Source: Gini A et al. Gastroenterology. 2017 Dec 27. doi: 10.1053/j.gastro.2017.12.011.
NICE issues recommendation for dapagliflozin-insulin therapy in type 1 diabetes
The inadequately controlled by insulin alone.
In a review of clinical trials, NICE found that dapagliflozin plus insulin conferred small benefits in hemoglobin A1c, weight loss, and quality of life, compared with insulin alone. These benefits translated to a reduced risk of long-term complications over the lifetime of the patient.
In the new NICE guideline, dual treatment with dapagliflozin and insulin in adults with type 1 diabetes and a body mass index greater than 27 kg/m2 is recommended only when they are receiving insulin doses of more than 0.5 units/kg per day; have undergone an evidence-based, quality-assured education program; and are supervised by a physician specializing in endocrinology and diabetes.
Hemoglobin A1c levels should be assessed after 6 months and at regular intervals after that; if glycemic control is not improved, dapagliflozin should be stopped, as there is an increased risk of diabetic ketoacidosis.
Find the full technology appraisal guidance on the NICE website.
The inadequately controlled by insulin alone.
In a review of clinical trials, NICE found that dapagliflozin plus insulin conferred small benefits in hemoglobin A1c, weight loss, and quality of life, compared with insulin alone. These benefits translated to a reduced risk of long-term complications over the lifetime of the patient.
In the new NICE guideline, dual treatment with dapagliflozin and insulin in adults with type 1 diabetes and a body mass index greater than 27 kg/m2 is recommended only when they are receiving insulin doses of more than 0.5 units/kg per day; have undergone an evidence-based, quality-assured education program; and are supervised by a physician specializing in endocrinology and diabetes.
Hemoglobin A1c levels should be assessed after 6 months and at regular intervals after that; if glycemic control is not improved, dapagliflozin should be stopped, as there is an increased risk of diabetic ketoacidosis.
Find the full technology appraisal guidance on the NICE website.
The inadequately controlled by insulin alone.
In a review of clinical trials, NICE found that dapagliflozin plus insulin conferred small benefits in hemoglobin A1c, weight loss, and quality of life, compared with insulin alone. These benefits translated to a reduced risk of long-term complications over the lifetime of the patient.
In the new NICE guideline, dual treatment with dapagliflozin and insulin in adults with type 1 diabetes and a body mass index greater than 27 kg/m2 is recommended only when they are receiving insulin doses of more than 0.5 units/kg per day; have undergone an evidence-based, quality-assured education program; and are supervised by a physician specializing in endocrinology and diabetes.
Hemoglobin A1c levels should be assessed after 6 months and at regular intervals after that; if glycemic control is not improved, dapagliflozin should be stopped, as there is an increased risk of diabetic ketoacidosis.
Find the full technology appraisal guidance on the NICE website.
Werewolf babies, blinding fries, and the gut library
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
Decision making regarding vaccines varies among accepters, deniers, partial accepters
Parents who accepted, denied, or partially accepted participation in the Dutch National Immunization Program reached their decisions through different methods, according to Kim A.G.J. Romijnders of the National Institute for Public Health and the Environment in Bilthoven, the Netherlands, and associates.
For the study published in Vaccine, the investigators conducted a series of 12 focus groups: 3 with accepters (n = 19), 3 with deniers (n =12), and 6 with partial accepters (n =24); in the partial accepters groups, there were three groups with parents delaying vaccination and three with parents refusing some vaccinations. Three-quarters of participants were women, the average age was 39 years, and 96% had at least university education. Parents were asked about their knowledge, attitudes, deliberation, and information needs regarding childhood vaccination.
Vaccine accepters regarded the decision to vaccinate their children as self-evident, but deniers and partial accepters reported conducting extensive deliberation on the pros and cons of vaccination. Deniers and partial accepters, in general, perceived fewer risks of vaccine-preventable diseases, more risks of vaccine side effects, less social support from their environment, less trust in child welfare centers, and provided less information than accepters.
The investigators noted that This process alienated them from their child vaccine provider, with trust being lost when the provider either refused or was unable to answer questions. Partial accepters also reported a lack of social support from friends, family, and providers regarding partial vaccine acceptance.
“The findings can facilitate informed decision making among parents by promoting an open dialogue at the [child welfare center], and improving the type and form of information presented. An open dialogue between parents and [child vaccine providers] may increase deliberation among parents, strengthen positive attitudes, prevent misperceptions, and resolve decisional conflict,” the investigators concluded.
The study was supported by the Dutch National Institute for Public Health and the Environment; the authors reported no conflicts of interest.
SOURCE: Romijnders KAGJ et al. Vaccine. 2019 Aug 2. doi: 10.1016/j.vaccine.2019.07.060.
Parents who accepted, denied, or partially accepted participation in the Dutch National Immunization Program reached their decisions through different methods, according to Kim A.G.J. Romijnders of the National Institute for Public Health and the Environment in Bilthoven, the Netherlands, and associates.
For the study published in Vaccine, the investigators conducted a series of 12 focus groups: 3 with accepters (n = 19), 3 with deniers (n =12), and 6 with partial accepters (n =24); in the partial accepters groups, there were three groups with parents delaying vaccination and three with parents refusing some vaccinations. Three-quarters of participants were women, the average age was 39 years, and 96% had at least university education. Parents were asked about their knowledge, attitudes, deliberation, and information needs regarding childhood vaccination.
Vaccine accepters regarded the decision to vaccinate their children as self-evident, but deniers and partial accepters reported conducting extensive deliberation on the pros and cons of vaccination. Deniers and partial accepters, in general, perceived fewer risks of vaccine-preventable diseases, more risks of vaccine side effects, less social support from their environment, less trust in child welfare centers, and provided less information than accepters.
The investigators noted that This process alienated them from their child vaccine provider, with trust being lost when the provider either refused or was unable to answer questions. Partial accepters also reported a lack of social support from friends, family, and providers regarding partial vaccine acceptance.
“The findings can facilitate informed decision making among parents by promoting an open dialogue at the [child welfare center], and improving the type and form of information presented. An open dialogue between parents and [child vaccine providers] may increase deliberation among parents, strengthen positive attitudes, prevent misperceptions, and resolve decisional conflict,” the investigators concluded.
The study was supported by the Dutch National Institute for Public Health and the Environment; the authors reported no conflicts of interest.
SOURCE: Romijnders KAGJ et al. Vaccine. 2019 Aug 2. doi: 10.1016/j.vaccine.2019.07.060.
Parents who accepted, denied, or partially accepted participation in the Dutch National Immunization Program reached their decisions through different methods, according to Kim A.G.J. Romijnders of the National Institute for Public Health and the Environment in Bilthoven, the Netherlands, and associates.
For the study published in Vaccine, the investigators conducted a series of 12 focus groups: 3 with accepters (n = 19), 3 with deniers (n =12), and 6 with partial accepters (n =24); in the partial accepters groups, there were three groups with parents delaying vaccination and three with parents refusing some vaccinations. Three-quarters of participants were women, the average age was 39 years, and 96% had at least university education. Parents were asked about their knowledge, attitudes, deliberation, and information needs regarding childhood vaccination.
Vaccine accepters regarded the decision to vaccinate their children as self-evident, but deniers and partial accepters reported conducting extensive deliberation on the pros and cons of vaccination. Deniers and partial accepters, in general, perceived fewer risks of vaccine-preventable diseases, more risks of vaccine side effects, less social support from their environment, less trust in child welfare centers, and provided less information than accepters.
The investigators noted that This process alienated them from their child vaccine provider, with trust being lost when the provider either refused or was unable to answer questions. Partial accepters also reported a lack of social support from friends, family, and providers regarding partial vaccine acceptance.
“The findings can facilitate informed decision making among parents by promoting an open dialogue at the [child welfare center], and improving the type and form of information presented. An open dialogue between parents and [child vaccine providers] may increase deliberation among parents, strengthen positive attitudes, prevent misperceptions, and resolve decisional conflict,” the investigators concluded.
The study was supported by the Dutch National Institute for Public Health and the Environment; the authors reported no conflicts of interest.
SOURCE: Romijnders KAGJ et al. Vaccine. 2019 Aug 2. doi: 10.1016/j.vaccine.2019.07.060.
FROM VACCINE
MenB vaccination coverage higher in those receiving MenB-4C
While meningococcal group B (MenB) vaccination remains suboptimal in the United States, completion was significantly higher for the MenB-4C (Bexsero) vaccine, compared with the other vaccine option, MenB-FHbp (Trumenba), according to Elizabeth Packnett of IBM Watson Health in Bethesda, Md., and associates.
In a study published in Vaccine, the investigators retrospectively analyzed 65,205 (36,118 received MenB-4C; 29,087 received MenB-FHbp) commercially insured individuals from the MarketScan Commercial Claims and Encounters Database during Jan. 1, 2015–Feb. 28, 2018, as well as 13,535 (10,153 received MenB-4C; 3,382 received MenB-FHbp) Medicaid-covered individuals from the Medicaid Multi-State Database during Jan. 1, 2015–Dec. 31, 2017.
The rate of vaccine completion in the MarketScan database within 15 months of initiation was 63% for MenB-4C and 52% for MenB-FHbp, and dosing schedule adherence was 62% for MenB-4C and 18% for MenB-FHbp. The median time to completion among those who finished vaccination was 68 days for MenB-4C versus 258 days for MenB-FHbp.
In the Medicaid database, the rate of vaccine completion within 15 months of initiation was 49% for MenB-4C and 31% for MenB-FHbp; dosing schedule adherence was 48% and 8%, respectively. Median time to vaccine completion was 88 days for MenB-4C versus 309 days for MenB-FHbp.
“The observations of improved completion and schedule adherence rates for MenB-4C, compared with MenB-FHbp, were consistent across both the commercial and Medicaid populations, and persisted after adjusting for individual factors in multivariable analyses, suggesting that the results were not skewed by population differences in demographic or other characteristics,” the investigators noted, adding that the significant difference in completion and schedule adherence between vaccines likely reflects the MenB-4C flexible dosing schedule.
The study was funded by GlaxoSmithKline, the maker of MenB-4C, and four coauthors reported being employed by the company. Five coauthors were employed by IBM Watson Health, which conducted the study.
SOURCE: Packnett E et al. Vaccine. 2019 Aug 20. doi: 10.1016/j.vaccine.2019.06.065.
While meningococcal group B (MenB) vaccination remains suboptimal in the United States, completion was significantly higher for the MenB-4C (Bexsero) vaccine, compared with the other vaccine option, MenB-FHbp (Trumenba), according to Elizabeth Packnett of IBM Watson Health in Bethesda, Md., and associates.
In a study published in Vaccine, the investigators retrospectively analyzed 65,205 (36,118 received MenB-4C; 29,087 received MenB-FHbp) commercially insured individuals from the MarketScan Commercial Claims and Encounters Database during Jan. 1, 2015–Feb. 28, 2018, as well as 13,535 (10,153 received MenB-4C; 3,382 received MenB-FHbp) Medicaid-covered individuals from the Medicaid Multi-State Database during Jan. 1, 2015–Dec. 31, 2017.
The rate of vaccine completion in the MarketScan database within 15 months of initiation was 63% for MenB-4C and 52% for MenB-FHbp, and dosing schedule adherence was 62% for MenB-4C and 18% for MenB-FHbp. The median time to completion among those who finished vaccination was 68 days for MenB-4C versus 258 days for MenB-FHbp.
In the Medicaid database, the rate of vaccine completion within 15 months of initiation was 49% for MenB-4C and 31% for MenB-FHbp; dosing schedule adherence was 48% and 8%, respectively. Median time to vaccine completion was 88 days for MenB-4C versus 309 days for MenB-FHbp.
“The observations of improved completion and schedule adherence rates for MenB-4C, compared with MenB-FHbp, were consistent across both the commercial and Medicaid populations, and persisted after adjusting for individual factors in multivariable analyses, suggesting that the results were not skewed by population differences in demographic or other characteristics,” the investigators noted, adding that the significant difference in completion and schedule adherence between vaccines likely reflects the MenB-4C flexible dosing schedule.
The study was funded by GlaxoSmithKline, the maker of MenB-4C, and four coauthors reported being employed by the company. Five coauthors were employed by IBM Watson Health, which conducted the study.
SOURCE: Packnett E et al. Vaccine. 2019 Aug 20. doi: 10.1016/j.vaccine.2019.06.065.
While meningococcal group B (MenB) vaccination remains suboptimal in the United States, completion was significantly higher for the MenB-4C (Bexsero) vaccine, compared with the other vaccine option, MenB-FHbp (Trumenba), according to Elizabeth Packnett of IBM Watson Health in Bethesda, Md., and associates.
In a study published in Vaccine, the investigators retrospectively analyzed 65,205 (36,118 received MenB-4C; 29,087 received MenB-FHbp) commercially insured individuals from the MarketScan Commercial Claims and Encounters Database during Jan. 1, 2015–Feb. 28, 2018, as well as 13,535 (10,153 received MenB-4C; 3,382 received MenB-FHbp) Medicaid-covered individuals from the Medicaid Multi-State Database during Jan. 1, 2015–Dec. 31, 2017.
The rate of vaccine completion in the MarketScan database within 15 months of initiation was 63% for MenB-4C and 52% for MenB-FHbp, and dosing schedule adherence was 62% for MenB-4C and 18% for MenB-FHbp. The median time to completion among those who finished vaccination was 68 days for MenB-4C versus 258 days for MenB-FHbp.
In the Medicaid database, the rate of vaccine completion within 15 months of initiation was 49% for MenB-4C and 31% for MenB-FHbp; dosing schedule adherence was 48% and 8%, respectively. Median time to vaccine completion was 88 days for MenB-4C versus 309 days for MenB-FHbp.
“The observations of improved completion and schedule adherence rates for MenB-4C, compared with MenB-FHbp, were consistent across both the commercial and Medicaid populations, and persisted after adjusting for individual factors in multivariable analyses, suggesting that the results were not skewed by population differences in demographic or other characteristics,” the investigators noted, adding that the significant difference in completion and schedule adherence between vaccines likely reflects the MenB-4C flexible dosing schedule.
The study was funded by GlaxoSmithKline, the maker of MenB-4C, and four coauthors reported being employed by the company. Five coauthors were employed by IBM Watson Health, which conducted the study.
SOURCE: Packnett E et al. Vaccine. 2019 Aug 20. doi: 10.1016/j.vaccine.2019.06.065.
FROM VACCINE
Zoledronic acid reduces symptomatic periodontal disease in patients with osteoporosis
according to Akira Taguchi, DDS, PhD, of the department of oral and maxillofacial radiology at Matsumoto Dental University, Nagano, Japan, and associates.
In a study published in Menopause, the investigators retrospectively analyzed 542 men and women with osteoporosis who participated in the randomized ZONE (Zoledronate Treatment in Efficacy to Osteoporosis) trial. Patients received either zoledronic acid (n = 258) or placebo (n = 284) once yearly for 2 years by IV infusion; mean age was 74 years in both groups. Patients were instructed to maintain good oral health at baseline and every 3 months afterward. Participants with signs or symptoms involving the oral cavity at the follow-up approximately every 3 months were referred to dentists for examination of oral disease.
Oral adverse events were significantly more common in the placebo group, compared with the zoledronic acid group (20% vs. 14%; P = .04); incidence of symptomatic periodontal disease also was significantly more common in those receiving placebo (12% vs. 5%; P = .002). While loss of teeth was more common in the control group than in those receiving zoledronic acid (11% vs. 7%), the difference was not significant.
“Because zoledronic acid can prevent symptomatic periodontal disease when combined with good oral hygiene management, it is possible that the procedures performed in this study could eventually suppress the development of [osteonecrosis of the jaw],” the investigators concluded.
The study was funded by Asahi-Kasei Pharma. The investigators reported employment or receiving consulting fees from numerous pharmaceutical companies.
SOURCE: Taguchi A et al. Menopause. 2019 Aug 19. doi: 10.1097/GME.0000000000001393.
according to Akira Taguchi, DDS, PhD, of the department of oral and maxillofacial radiology at Matsumoto Dental University, Nagano, Japan, and associates.
In a study published in Menopause, the investigators retrospectively analyzed 542 men and women with osteoporosis who participated in the randomized ZONE (Zoledronate Treatment in Efficacy to Osteoporosis) trial. Patients received either zoledronic acid (n = 258) or placebo (n = 284) once yearly for 2 years by IV infusion; mean age was 74 years in both groups. Patients were instructed to maintain good oral health at baseline and every 3 months afterward. Participants with signs or symptoms involving the oral cavity at the follow-up approximately every 3 months were referred to dentists for examination of oral disease.
Oral adverse events were significantly more common in the placebo group, compared with the zoledronic acid group (20% vs. 14%; P = .04); incidence of symptomatic periodontal disease also was significantly more common in those receiving placebo (12% vs. 5%; P = .002). While loss of teeth was more common in the control group than in those receiving zoledronic acid (11% vs. 7%), the difference was not significant.
“Because zoledronic acid can prevent symptomatic periodontal disease when combined with good oral hygiene management, it is possible that the procedures performed in this study could eventually suppress the development of [osteonecrosis of the jaw],” the investigators concluded.
The study was funded by Asahi-Kasei Pharma. The investigators reported employment or receiving consulting fees from numerous pharmaceutical companies.
SOURCE: Taguchi A et al. Menopause. 2019 Aug 19. doi: 10.1097/GME.0000000000001393.
according to Akira Taguchi, DDS, PhD, of the department of oral and maxillofacial radiology at Matsumoto Dental University, Nagano, Japan, and associates.
In a study published in Menopause, the investigators retrospectively analyzed 542 men and women with osteoporosis who participated in the randomized ZONE (Zoledronate Treatment in Efficacy to Osteoporosis) trial. Patients received either zoledronic acid (n = 258) or placebo (n = 284) once yearly for 2 years by IV infusion; mean age was 74 years in both groups. Patients were instructed to maintain good oral health at baseline and every 3 months afterward. Participants with signs or symptoms involving the oral cavity at the follow-up approximately every 3 months were referred to dentists for examination of oral disease.
Oral adverse events were significantly more common in the placebo group, compared with the zoledronic acid group (20% vs. 14%; P = .04); incidence of symptomatic periodontal disease also was significantly more common in those receiving placebo (12% vs. 5%; P = .002). While loss of teeth was more common in the control group than in those receiving zoledronic acid (11% vs. 7%), the difference was not significant.
“Because zoledronic acid can prevent symptomatic periodontal disease when combined with good oral hygiene management, it is possible that the procedures performed in this study could eventually suppress the development of [osteonecrosis of the jaw],” the investigators concluded.
The study was funded by Asahi-Kasei Pharma. The investigators reported employment or receiving consulting fees from numerous pharmaceutical companies.
SOURCE: Taguchi A et al. Menopause. 2019 Aug 19. doi: 10.1097/GME.0000000000001393.
FROM MENOPAUSE