User login
Cortisol levels on COVID-19 admission may be a marker of severity
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to hospital have a substantially increased risk of dying, U.K. researchers have discovered.
Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London, and colleagues studied 535 patients admitted to major London hospitals. Their article was published online June 18 in Lancet Diabetes & Endocrinology.
“Our analyses show for the first time that patients with COVID-19 mount a marked and appropriate acute cortisol stress response,” said Dr. Dhillo and colleagues.
Moreover, “high cortisol concentrations were associated with increased mortality and a reduced median survival, probably because this is a marker of the severity of illness.”
So measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” Dr. Dhillo noted in a statement from his institution.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said.
However, it’s important to note that this means – particularly in the wake of the RECOVERY trial reported last week – that “in the early part of the disease you don’t need steroids,” he said.
In contrast to SARS, no adrenal insufficiency with COVID-19
Cortisol levels when healthy and resting are 100-200 nmol/L and nearly zero when sleeping, the researchers explained.
They decided to examine cortisol levels because, although physiological stress from critical illness normally increases levels of the hormone, the prior coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), had the opposite effect and induced cortisol insufficiency in some patients.
“We would have said we’re not quite sure” what effect SARS-CoV-2 is having on cortisol levels, “so that’s why we collected the data,” Dr. Dhillo said in an interview.
The researchers studied patients admitted to three large London teaching hospitals between March 9 and April 22 with a clinical suspicion of SARS-CoV-2 infection. All patients had a standard set of blood tests, including full blood count, creatinine, C-reactive protein, D-dimer, and serum cortisol.
After exclusions, the team assessed 535 patients admitted over the study period who had baseline cortisol measured within 48 hours of admission.
Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing (88%) or a strong clinical and radiological suspicion, despite a negative test (12%).
In total, 132 (25%) individuals were not diagnosed with COVID-19.
Patients with COVID-19 were a mean age of 66.3 years, and 59.6% were men.
Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus (619 vs 519 nmol/L; P < .0001).
And by May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%; P < .0001).
Doubling of cortisol levels associated with 40% higher mortality
Multivariate analysis taking into account age, presence of comorbidities, and laboratory tests revealed that a doubling of cortisol concentrations among those with COVID-19 was associated with a significant increase in mortality, at a hazard ratio of 1.42 (P = .014).
And patients with COVID-19 whose baseline cortisol level was >744 nmol/L had a median survival of just 15 days, compared with those with a level ≤744 nmol/L, who had a median survival of 36 days (P < .0001).
The team notes that the cortisol stress responses in their patients with COVID-19 ranged up to 3,241 nmol/L, which is “a marked cortisol stress response, perhaps higher than is observed in patients undergoing major surgery.”
Of interest, there was no interaction between cortisol levels and ethnicity in their study; a subsequent analysis of the data stratified by black, Asian, and other minority ethnicities revealed no significant differences.
The team note that their results will need to be reproduced in other populations.
“Any potential role for cortisol measurement at baseline and later during an inpatient stay with COVID-19 as a prognostic biomarker, either by itself or in combination with other biomarkers, will require validation in a prospective study.”
Implications for treatment: Reserve dexamethasone for critically ill
Dr. Dhillo explained that, because their findings indicate that people initially infected with COVID-19 do mount an appropriate stress (cortisol) response, it is important that people properly understand this in the wake of the RECOVERY trial, reported last week.
The trial showed that the widely available steroid dexamethasone significantly reduced mortality among severely ill COVID-19 patients in the intensive care unit when given at a supraphysiologic dose of 6 mg.
But it would be hazardous for anyone to self-medicate with steroids at an early stage of COVID-19 because that would further increase cortisol levels and could suppress the immune system.
“For the average person on the street with COVID-19,” excess steroids will make their symptoms worse, Dr. Dhillo explained, adding this is important to emphasize because dexamethasone, and similar steroids, “are cheap and likely available on the Internet, and so misunderstanding of the RECOVERY trial could have serious implications.”
But once patients are very sick, with “inflammation in their lungs” and are in the intensive care unit, and often on ventilators – which is a very small subgroup of those with COVID-19 – it becomes a very different story, he stressed.
“RECOVERY shows clearly there seems to be a benefit once you need oxygen or are on a ventilator, and that makes sense because [dexamethasone] is going to be an anti-inflammatory,” in this instance when the “lungs are full of water.”
“But in the early days you definitely don’t need it and it could be harmful,” he reiterated.
The study is funded by the U.K. National Institute for Health Research and Medical Research Council. The authors have reported no relevant financial relationships.
This article first appeared on Medscape.com.
What’s pushing cannabis use in first-episode psychosis?
The desire to feel better is a major driver for patients with first-episode psychosis (FEP) to turn to cannabis, new research shows.
An analysis of more than 1,300 individuals from six European countries showed patients with FEP were four times more likely than their healthy peers to start smoking cannabis in order to make themselves feel better.
The results also revealed that initiating cannabis use to feel better was associated with a more than tripled risk of being a daily user.
as well as offer an opportunity for psychoeducation – particularly as the reasons for starting cannabis appear to influence frequency of use, study investigator Edoardo Spinazzola, MD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, said in an interview.
Patients who start smoking cannabis because their friends or family partakes may benefit from therapies that encourage more “assertiveness” and being “socially comfortable without the substance,” Dr. Spinazzola said, noting that it might also be beneficial to identify the specific cause of the psychological discomfort driving cannabis use, such as depression, and specifically treat that issue.
The results were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
Answering the skeptics
Previous studies suggest that cannabis use can increase risk for psychosis up to 290%, with both frequency of use and potency playing a role, the researchers noted.
However, they added that “skeptics” argue the association could be caused by individuals with psychosis using cannabis as a form of self-medication, the comorbid effect of other psychogenic drugs, or a common genetic vulnerability between cannabis use and psychosis.
The reasons for starting cannabis use remain “largely unexplored,” so the researchers examined records from the European network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) database, which includes patients with FEP and healthy individuals acting as controls from France, Italy, the Netherlands, Spain, United Kingdom, and Brazil.
The analysis included 1,347 individuals, of whom 446 had a diagnosis of nonaffective psychosis, 89 had bipolar disorder, and 58 had psychotic depression.
Reasons to start smoking cannabis and patterns of use were determined using the modified version of the Cannabis Experiences Questionnaire.
Results showed that participants who started cannabis to feel better were significantly more likely to be younger, have fewer years of education, to be black or of mixed ethnicity, to be single, or to not be living independently than those who started it because their friends or family were using it (P < .001 for all comparisons).
In addition, 68% of the patients with FEP and 85% of the healthy controls started using cannabis because friends or family were using it. In contrast, 18% of those with FEP versus 5% of controls starting using cannabis to feel better; 13% versus 10%, respectively, started using for “other reasons.”
After taking into account gender, age, ethnicity, and study site, the patients with FEP were significantly more likely than their healthy peers to have started using cannabis to feel better (relative risk ratio, 4.67; P < .001).
Starting to smoke cannabis to feel better versus any other reason was associated with an increased frequency of use in both those with and without FEP, with an RRR of 2.9 for using the drug more than once a week (P = .001) and an RRR of 3.13 for daily use (P < .001). However, the association was stronger in the healthy controls than in those with FEP, with an RRR for daily use of 4.45 versus 3.11, respectively.
The investigators also examined whether there was a link between reasons to start smoking and an individual’s polygenic risk score (PRS) for developing schizophrenia.
Multinomial regression indicated that PRS was not associated with starting cannabis to feel better or because friends were using it. However, there was an association between PRS score and starting the drug because family members were using it (RRR, 0.68; P < .05).
Complex association
Gabriella Gobbi, MD, PhD, professor in the neurobiological psychiatry unit, department of psychiatry, at McGill University, Montreal, said the data confirm “what we already know about cannabis.”
She noted that one of the “major causes” of young people starting cannabis is the social environment, while the desire to use the drug to feel better is linked to “the fact that cannabis, in a lot of cases, is used as a self-medication” in order to be calmer and as a relief from anxiety.
There is a “very complex” association between using cannabis to feel better and the self-medication seen with cigarette smoking and alcohol in patients with schizophrenia, said Dr. Gobbi, who was not involved with the research.
“When we talk about [patients using] cannabis, alcohol, and cigarettes, actually we’re talking about the same group of people,” she said.
Although “it is true they say that people look to cigarettes, tobacco, and alcohol to feel happier because they are depressed, the risk of psychosis is only for cannabis,” she added. “It is very low for alcohol and tobacco.”
As a result, Dr. Gobbi said she and her colleagues are “very worried” about the consequences for mental health of the legalization of cannabis consumption in Canada in October 2018 with the passing of the Cannabis Act.
Although there are no firm statistics yet, she has observed that since the law was passed, cannabis use has stabilized at a lower level among adolescents. “But now we have another population of people aged 34 and older that consume cannabis,” she said.
Particularly when considering the impact of higher strength cannabis on psychosis risk, Dr. Gobbi believes the increase in consumption in this age group will result in a “more elevated” risk for mental health issues.
Dr. Spinazzola and Dr. Gobbi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The desire to feel better is a major driver for patients with first-episode psychosis (FEP) to turn to cannabis, new research shows.
An analysis of more than 1,300 individuals from six European countries showed patients with FEP were four times more likely than their healthy peers to start smoking cannabis in order to make themselves feel better.
The results also revealed that initiating cannabis use to feel better was associated with a more than tripled risk of being a daily user.
as well as offer an opportunity for psychoeducation – particularly as the reasons for starting cannabis appear to influence frequency of use, study investigator Edoardo Spinazzola, MD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, said in an interview.
Patients who start smoking cannabis because their friends or family partakes may benefit from therapies that encourage more “assertiveness” and being “socially comfortable without the substance,” Dr. Spinazzola said, noting that it might also be beneficial to identify the specific cause of the psychological discomfort driving cannabis use, such as depression, and specifically treat that issue.
The results were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
Answering the skeptics
Previous studies suggest that cannabis use can increase risk for psychosis up to 290%, with both frequency of use and potency playing a role, the researchers noted.
However, they added that “skeptics” argue the association could be caused by individuals with psychosis using cannabis as a form of self-medication, the comorbid effect of other psychogenic drugs, or a common genetic vulnerability between cannabis use and psychosis.
The reasons for starting cannabis use remain “largely unexplored,” so the researchers examined records from the European network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) database, which includes patients with FEP and healthy individuals acting as controls from France, Italy, the Netherlands, Spain, United Kingdom, and Brazil.
The analysis included 1,347 individuals, of whom 446 had a diagnosis of nonaffective psychosis, 89 had bipolar disorder, and 58 had psychotic depression.
Reasons to start smoking cannabis and patterns of use were determined using the modified version of the Cannabis Experiences Questionnaire.
Results showed that participants who started cannabis to feel better were significantly more likely to be younger, have fewer years of education, to be black or of mixed ethnicity, to be single, or to not be living independently than those who started it because their friends or family were using it (P < .001 for all comparisons).
In addition, 68% of the patients with FEP and 85% of the healthy controls started using cannabis because friends or family were using it. In contrast, 18% of those with FEP versus 5% of controls starting using cannabis to feel better; 13% versus 10%, respectively, started using for “other reasons.”
After taking into account gender, age, ethnicity, and study site, the patients with FEP were significantly more likely than their healthy peers to have started using cannabis to feel better (relative risk ratio, 4.67; P < .001).
Starting to smoke cannabis to feel better versus any other reason was associated with an increased frequency of use in both those with and without FEP, with an RRR of 2.9 for using the drug more than once a week (P = .001) and an RRR of 3.13 for daily use (P < .001). However, the association was stronger in the healthy controls than in those with FEP, with an RRR for daily use of 4.45 versus 3.11, respectively.
The investigators also examined whether there was a link between reasons to start smoking and an individual’s polygenic risk score (PRS) for developing schizophrenia.
Multinomial regression indicated that PRS was not associated with starting cannabis to feel better or because friends were using it. However, there was an association between PRS score and starting the drug because family members were using it (RRR, 0.68; P < .05).
Complex association
Gabriella Gobbi, MD, PhD, professor in the neurobiological psychiatry unit, department of psychiatry, at McGill University, Montreal, said the data confirm “what we already know about cannabis.”
She noted that one of the “major causes” of young people starting cannabis is the social environment, while the desire to use the drug to feel better is linked to “the fact that cannabis, in a lot of cases, is used as a self-medication” in order to be calmer and as a relief from anxiety.
There is a “very complex” association between using cannabis to feel better and the self-medication seen with cigarette smoking and alcohol in patients with schizophrenia, said Dr. Gobbi, who was not involved with the research.
“When we talk about [patients using] cannabis, alcohol, and cigarettes, actually we’re talking about the same group of people,” she said.
Although “it is true they say that people look to cigarettes, tobacco, and alcohol to feel happier because they are depressed, the risk of psychosis is only for cannabis,” she added. “It is very low for alcohol and tobacco.”
As a result, Dr. Gobbi said she and her colleagues are “very worried” about the consequences for mental health of the legalization of cannabis consumption in Canada in October 2018 with the passing of the Cannabis Act.
Although there are no firm statistics yet, she has observed that since the law was passed, cannabis use has stabilized at a lower level among adolescents. “But now we have another population of people aged 34 and older that consume cannabis,” she said.
Particularly when considering the impact of higher strength cannabis on psychosis risk, Dr. Gobbi believes the increase in consumption in this age group will result in a “more elevated” risk for mental health issues.
Dr. Spinazzola and Dr. Gobbi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The desire to feel better is a major driver for patients with first-episode psychosis (FEP) to turn to cannabis, new research shows.
An analysis of more than 1,300 individuals from six European countries showed patients with FEP were four times more likely than their healthy peers to start smoking cannabis in order to make themselves feel better.
The results also revealed that initiating cannabis use to feel better was associated with a more than tripled risk of being a daily user.
as well as offer an opportunity for psychoeducation – particularly as the reasons for starting cannabis appear to influence frequency of use, study investigator Edoardo Spinazzola, MD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, said in an interview.
Patients who start smoking cannabis because their friends or family partakes may benefit from therapies that encourage more “assertiveness” and being “socially comfortable without the substance,” Dr. Spinazzola said, noting that it might also be beneficial to identify the specific cause of the psychological discomfort driving cannabis use, such as depression, and specifically treat that issue.
The results were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
Answering the skeptics
Previous studies suggest that cannabis use can increase risk for psychosis up to 290%, with both frequency of use and potency playing a role, the researchers noted.
However, they added that “skeptics” argue the association could be caused by individuals with psychosis using cannabis as a form of self-medication, the comorbid effect of other psychogenic drugs, or a common genetic vulnerability between cannabis use and psychosis.
The reasons for starting cannabis use remain “largely unexplored,” so the researchers examined records from the European network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI) database, which includes patients with FEP and healthy individuals acting as controls from France, Italy, the Netherlands, Spain, United Kingdom, and Brazil.
The analysis included 1,347 individuals, of whom 446 had a diagnosis of nonaffective psychosis, 89 had bipolar disorder, and 58 had psychotic depression.
Reasons to start smoking cannabis and patterns of use were determined using the modified version of the Cannabis Experiences Questionnaire.
Results showed that participants who started cannabis to feel better were significantly more likely to be younger, have fewer years of education, to be black or of mixed ethnicity, to be single, or to not be living independently than those who started it because their friends or family were using it (P < .001 for all comparisons).
In addition, 68% of the patients with FEP and 85% of the healthy controls started using cannabis because friends or family were using it. In contrast, 18% of those with FEP versus 5% of controls starting using cannabis to feel better; 13% versus 10%, respectively, started using for “other reasons.”
After taking into account gender, age, ethnicity, and study site, the patients with FEP were significantly more likely than their healthy peers to have started using cannabis to feel better (relative risk ratio, 4.67; P < .001).
Starting to smoke cannabis to feel better versus any other reason was associated with an increased frequency of use in both those with and without FEP, with an RRR of 2.9 for using the drug more than once a week (P = .001) and an RRR of 3.13 for daily use (P < .001). However, the association was stronger in the healthy controls than in those with FEP, with an RRR for daily use of 4.45 versus 3.11, respectively.
The investigators also examined whether there was a link between reasons to start smoking and an individual’s polygenic risk score (PRS) for developing schizophrenia.
Multinomial regression indicated that PRS was not associated with starting cannabis to feel better or because friends were using it. However, there was an association between PRS score and starting the drug because family members were using it (RRR, 0.68; P < .05).
Complex association
Gabriella Gobbi, MD, PhD, professor in the neurobiological psychiatry unit, department of psychiatry, at McGill University, Montreal, said the data confirm “what we already know about cannabis.”
She noted that one of the “major causes” of young people starting cannabis is the social environment, while the desire to use the drug to feel better is linked to “the fact that cannabis, in a lot of cases, is used as a self-medication” in order to be calmer and as a relief from anxiety.
There is a “very complex” association between using cannabis to feel better and the self-medication seen with cigarette smoking and alcohol in patients with schizophrenia, said Dr. Gobbi, who was not involved with the research.
“When we talk about [patients using] cannabis, alcohol, and cigarettes, actually we’re talking about the same group of people,” she said.
Although “it is true they say that people look to cigarettes, tobacco, and alcohol to feel happier because they are depressed, the risk of psychosis is only for cannabis,” she added. “It is very low for alcohol and tobacco.”
As a result, Dr. Gobbi said she and her colleagues are “very worried” about the consequences for mental health of the legalization of cannabis consumption in Canada in October 2018 with the passing of the Cannabis Act.
Although there are no firm statistics yet, she has observed that since the law was passed, cannabis use has stabilized at a lower level among adolescents. “But now we have another population of people aged 34 and older that consume cannabis,” she said.
Particularly when considering the impact of higher strength cannabis on psychosis risk, Dr. Gobbi believes the increase in consumption in this age group will result in a “more elevated” risk for mental health issues.
Dr. Spinazzola and Dr. Gobbi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM SIRS 2020
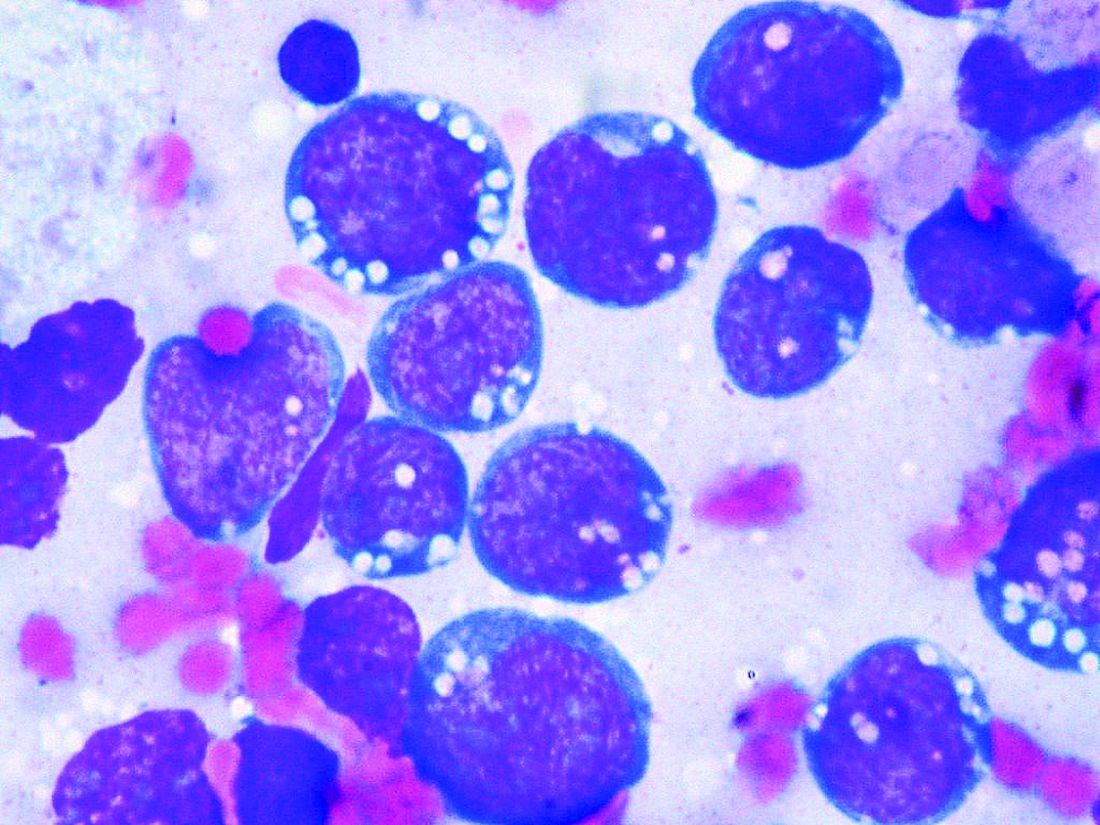
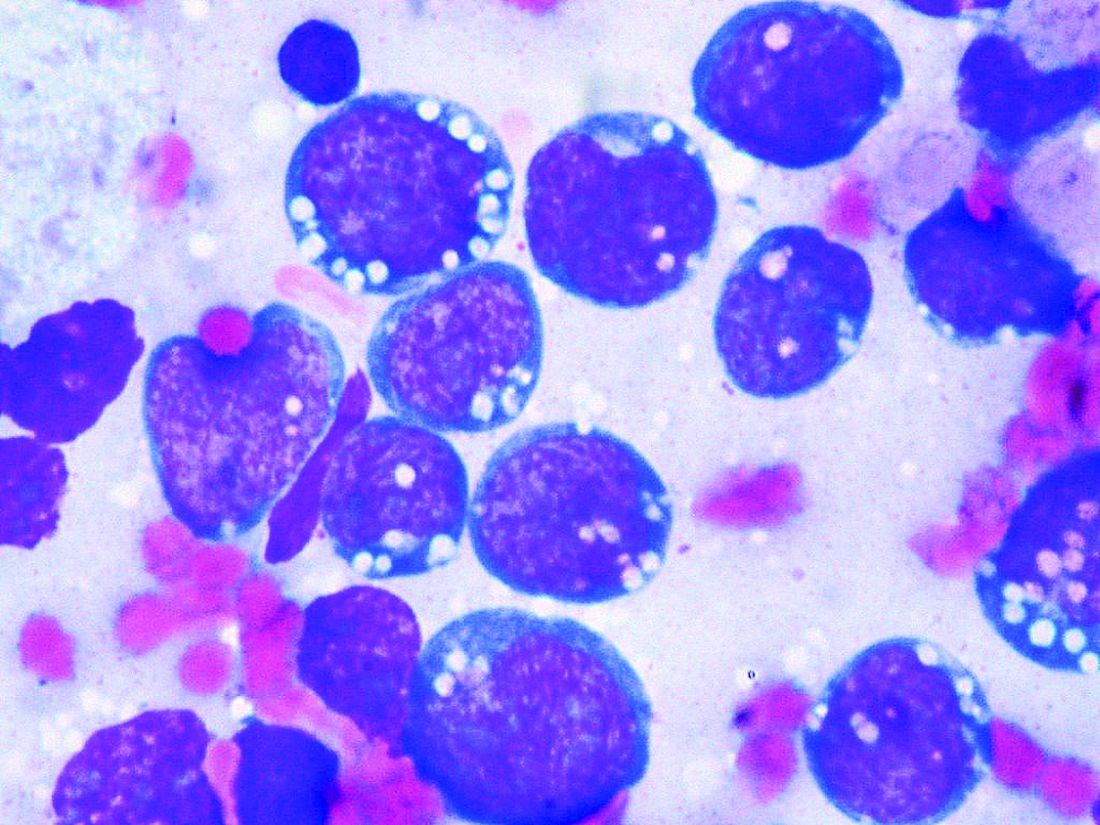
New EPOCH for adult patients with Burkitt lymphoma
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
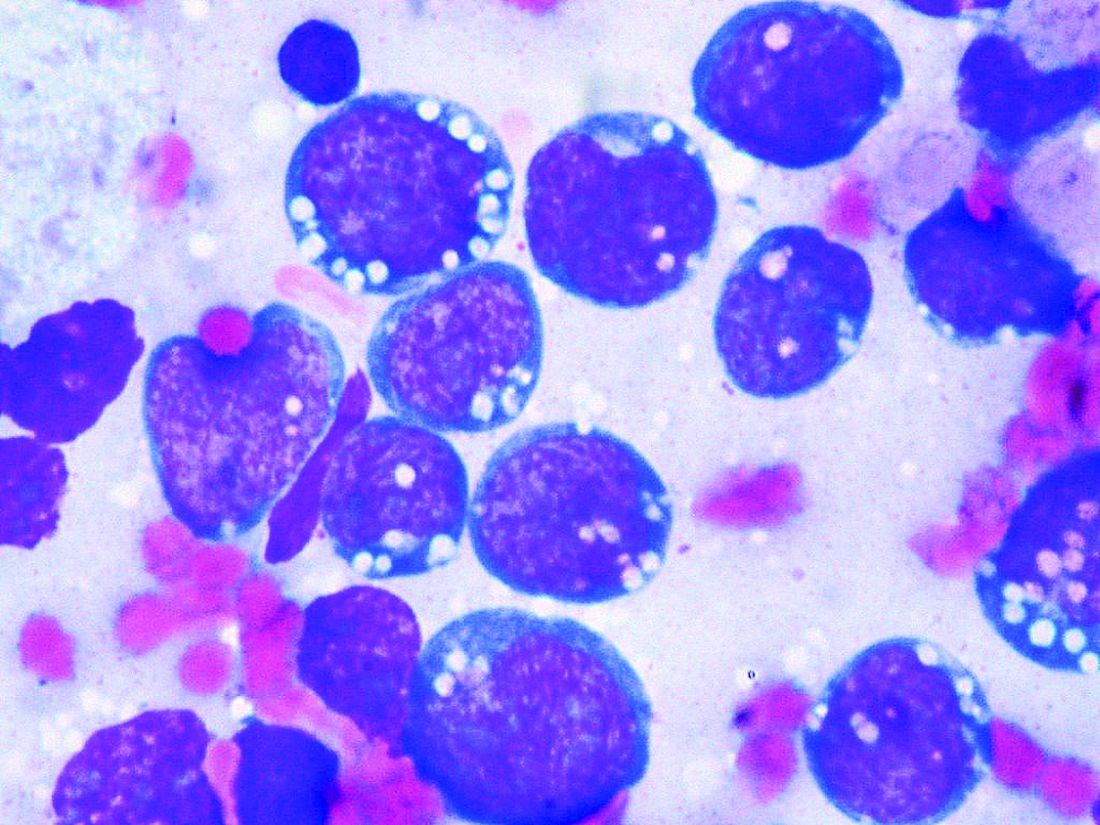
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Weekly cisplatin new standard in postop head and neck cancer
For the first time, weekly cisplatin plus radiotherapy (CDDP+RT) has been shown to be not only less toxic than dosing once every three weeks but to also achieve better outcomes in patients with postoperative squamous cell carcinoma of the head and neck (SCCHN), say Japanese researchers.
These results, from the JCOG1008 trial, suggest the weekly schedule should become the new standard of care in these patients, potentially settling what has been a “contentious” issue.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 6502), held virtually because of the coronavirus pandemic.
Lead author Naomi Kiyota, MD, PhD, medical oncology and hematology, Cancer Center, Kobe University Hospital, Japan, said the study involving more than 160 high-risk patients with SCCHN demonstrated comparable overall survival in the weekly and three-weekly CDDP+RT groups.
Moreover, it showed that the weekly schedule was associated with better relapse-free and local relapse-free survival, and, in line with previous studies, had a more favorable safety profile.
“This phase II/III study is the first to show that weekly CDDP+RT is noninferior to three-weekly CDDP+RT [and] is a new standard treatment option for these patients,” Dr. Kiyota said.
Study discussant Hisham M. Mehanna, MD, PhD, Warwickshire Head and Neck Clinic, University of Birmingham, UK, described the study as a “significant achievement” that answers “an important question that we’ve been asking for a very long time.”
He said that, despite three-weekly CDDP+RT being the standard treatment in the postoperative setting for SCCHN, there have been “lingering concerns,” as 40% of patients don’t get all three CDDP cycles “and it is toxic.”
Weekly CDDP is, on the other hand, “widely used, although the evidence for it is not as strong,” and has a number of advantages, including that it can be delivered in the outpatient setting and it may be less toxic.
Dr. Mehanna said there was “a surprise” to the current study, in that it was terminated early because it crossed the boundary for non-inferiority because weekly CDDP has better survival than the three-weekly dose; notably, however, superiority was not achieved.
Dr. Mehanna also expressed some reservations over imbalances in the treatment groups that could have meant the three-weekly cohort had an unfavorable prognosis, and said questions remain over longer-term toxicity.
‘Contentious issue’
In a highlights session, Nabil F. Saba, MD, director of the head and neck oncology program at Emory University’s Winship Cancer Institute in Atlanta, Georgia, said the dosing of CDDP in these patients has been “a contentious issue.”
One issue has been whether scheduling of CDDP or the cumulative dose achieved is the key determinant of clinical outcome, and he suggested that the superior results seen in the current study can be attributed to the high cumulative dose the investigators achieved in their patients compared with previous investigations.
For Dr. Saba, the take-home message of the trial is that weekly cisplatin “is now, finally, an accepted standard of care in the postoperative high-risk setting, which is a major change at this ASCO meeting.”
Presenting the trial, Dr. Kiyota said, in a recent study (J Clin Oncol. 2017 Dec 8. doi: 10.1200/JCO.2017.74.9457) from the Tata Memorial Hospital, weekly CDDP at 30 mg/m2 plus radiotherapy failed to achieve noninferiority to a three-weekly regimen, “albeit with fewer toxicities.”
He suggested that this could be because it was a single-center trial, two different treatment strategies were used, the majority of primary sites were in the oral cavity, and the dose was insufficient.
His team, on the other hand, undertook a randomized trial in which patients with postoperative high-risk SCCHN were recruited from 28 institutions.
The participants, who were aged 20-75 years and had ECOG performance status 0-1, all had pathological stage III/IV disease and a microscopically positive margin and/or extranodal extension.
They were randomly assigned to 100 mg/m2 CDDP once every three weeks or weekly 40 mg/m2 CDDP, plus radiotherapy at 66 Gy over 33 fractions.
For the intention-to-treat efficacy analysis, 132 patients received three-weekly CDDP+RT and 129 had weekly CDDP+RT, while the per-protocol safety analysis included 129 and 122 patients, respectively.
The median age of the patients was 61-62 years, and 110 patients in both treatment groups were male. Although there was a similar distribution of primary sites and high-risk factors in the two groups, more patients in the weekly group had pathological stage T2 disease (40) than in the three-weekly group (26).
The dose targets were met in both treatment groups. In the three-weekly group, the cumulative dose of CDDP achieved was 280 mg/m2, and, in the weekly group, it was 239 mg/m2.
The second planned interim analysis showed that, over a median follow-up of 2.2 years, 3-year overall survival was estimated at 71.6% in the weekly group versus 59.1% in the three-weekly group (hazard ratio, 0.69).
As this was below the one-sided P value for noninferiority, the data and safety monitoring committee recommended terminating the trial early.
The researchers also found that the 3-year relapse-free survival was higher with weekly CDDP+RT, at 64.5%, vs 53.0% with three-weekly dosing (HR, 0.71).
Local relapse-free survival was also better with weekly dosing, at a 3-year rate of 69.6% versus 59.5% for patients in the three-weekly group (HR, 0.73).
On a planned subgroup analysis, weekly CDDP+RT was nonsignificantly superior to the three-weekly schedule on almost every measure, whether looking at patient age, ECOG performance status, and primary site.
There were also differences in the occurrence of hematologic toxicities between the two groups, with fewer patients given the weekly schedule experiencing grade 3/4 neutropenia than those on the three-weekly dosing. However, there were more cases of any grade thrombocytopenia for patients getting the weekly dosing.
The weekly CDDP+RT regimen demonstrated its lower toxicity when looking at acute nonhematologic adverse events, with fewer occurrences of any grade dysphagia, nausea, hyponatremia, renal impairment, and hearing impairment versus the three-weekly schedule.
The weekly dosing schedule was also associated with lower rates of grade 3/4 dysphagia, nausea, and infection.
The study was funded by the National Cancer Center Research and Development Fund, Japan Agency for Medical Research and Development Fund.
Dr. Kiyota reports honoraria from AstraZeneca, Bayer, Bristol-Myers Squibb Japan, Chugai Pharma, Eisai, Merck Serono, MSD, and Ono Pharmaceutical; speakers bureau fees from AstraZeneca, Bayer, Bristol-Myers Squibb Japan; Eisai, Merck Serono, MSD, and Ono Pharmaceutical; and receiving research funding from AstraZeneca (Inst), Bristol-Myers Squibb (Inst), Ono Pharmaceutical (Inst), Pfizer (Inst), and Roche (Inst). Other study authors report potential conflicts of interest. The full list can be found here.
Dr. Mehanna reports stock and other ownership interests in Warwickshire Head and Neck Clinic; honoraria from AstraZeneca; speakers bureau fess from Merck, MSD, and Sanofi Pasteur; research funding from AstraZeneca, GlaxoSmithKline (Inst), MSD (Inst), Sanofi Pasteur (Inst), and Silence Therapeutics (Inst); and travel, accommodations, and expenses from Merck, MSD, and Sanofi Pasteur.
Dr. Saba reports honoraria from Aduro Biotech, Bristol-Myers Squibb, Cue Biopharma, Genentech/Roche, GSK, Kura, Lilly, Merck, and Pfizer; a consulting or advisory role with Biontech, Bluprint, Bristol-Myers Squibb, Lilly, Merck, and Pfizer; research funding from Bristol-Myers Squibb and Exelixis; travel, accommodations, and expenses from Bluprint, Bristol-Myers Squibb, Genentech/Roche, GSK, Lilly, Merck, and Pfizer.
This article first appeared on Medscape.com.
For the first time, weekly cisplatin plus radiotherapy (CDDP+RT) has been shown to be not only less toxic than dosing once every three weeks but to also achieve better outcomes in patients with postoperative squamous cell carcinoma of the head and neck (SCCHN), say Japanese researchers.
These results, from the JCOG1008 trial, suggest the weekly schedule should become the new standard of care in these patients, potentially settling what has been a “contentious” issue.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 6502), held virtually because of the coronavirus pandemic.
Lead author Naomi Kiyota, MD, PhD, medical oncology and hematology, Cancer Center, Kobe University Hospital, Japan, said the study involving more than 160 high-risk patients with SCCHN demonstrated comparable overall survival in the weekly and three-weekly CDDP+RT groups.
Moreover, it showed that the weekly schedule was associated with better relapse-free and local relapse-free survival, and, in line with previous studies, had a more favorable safety profile.
“This phase II/III study is the first to show that weekly CDDP+RT is noninferior to three-weekly CDDP+RT [and] is a new standard treatment option for these patients,” Dr. Kiyota said.
Study discussant Hisham M. Mehanna, MD, PhD, Warwickshire Head and Neck Clinic, University of Birmingham, UK, described the study as a “significant achievement” that answers “an important question that we’ve been asking for a very long time.”
He said that, despite three-weekly CDDP+RT being the standard treatment in the postoperative setting for SCCHN, there have been “lingering concerns,” as 40% of patients don’t get all three CDDP cycles “and it is toxic.”
Weekly CDDP is, on the other hand, “widely used, although the evidence for it is not as strong,” and has a number of advantages, including that it can be delivered in the outpatient setting and it may be less toxic.
Dr. Mehanna said there was “a surprise” to the current study, in that it was terminated early because it crossed the boundary for non-inferiority because weekly CDDP has better survival than the three-weekly dose; notably, however, superiority was not achieved.
Dr. Mehanna also expressed some reservations over imbalances in the treatment groups that could have meant the three-weekly cohort had an unfavorable prognosis, and said questions remain over longer-term toxicity.
‘Contentious issue’
In a highlights session, Nabil F. Saba, MD, director of the head and neck oncology program at Emory University’s Winship Cancer Institute in Atlanta, Georgia, said the dosing of CDDP in these patients has been “a contentious issue.”
One issue has been whether scheduling of CDDP or the cumulative dose achieved is the key determinant of clinical outcome, and he suggested that the superior results seen in the current study can be attributed to the high cumulative dose the investigators achieved in their patients compared with previous investigations.
For Dr. Saba, the take-home message of the trial is that weekly cisplatin “is now, finally, an accepted standard of care in the postoperative high-risk setting, which is a major change at this ASCO meeting.”
Presenting the trial, Dr. Kiyota said, in a recent study (J Clin Oncol. 2017 Dec 8. doi: 10.1200/JCO.2017.74.9457) from the Tata Memorial Hospital, weekly CDDP at 30 mg/m2 plus radiotherapy failed to achieve noninferiority to a three-weekly regimen, “albeit with fewer toxicities.”
He suggested that this could be because it was a single-center trial, two different treatment strategies were used, the majority of primary sites were in the oral cavity, and the dose was insufficient.
His team, on the other hand, undertook a randomized trial in which patients with postoperative high-risk SCCHN were recruited from 28 institutions.
The participants, who were aged 20-75 years and had ECOG performance status 0-1, all had pathological stage III/IV disease and a microscopically positive margin and/or extranodal extension.
They were randomly assigned to 100 mg/m2 CDDP once every three weeks or weekly 40 mg/m2 CDDP, plus radiotherapy at 66 Gy over 33 fractions.
For the intention-to-treat efficacy analysis, 132 patients received three-weekly CDDP+RT and 129 had weekly CDDP+RT, while the per-protocol safety analysis included 129 and 122 patients, respectively.
The median age of the patients was 61-62 years, and 110 patients in both treatment groups were male. Although there was a similar distribution of primary sites and high-risk factors in the two groups, more patients in the weekly group had pathological stage T2 disease (40) than in the three-weekly group (26).
The dose targets were met in both treatment groups. In the three-weekly group, the cumulative dose of CDDP achieved was 280 mg/m2, and, in the weekly group, it was 239 mg/m2.
The second planned interim analysis showed that, over a median follow-up of 2.2 years, 3-year overall survival was estimated at 71.6% in the weekly group versus 59.1% in the three-weekly group (hazard ratio, 0.69).
As this was below the one-sided P value for noninferiority, the data and safety monitoring committee recommended terminating the trial early.
The researchers also found that the 3-year relapse-free survival was higher with weekly CDDP+RT, at 64.5%, vs 53.0% with three-weekly dosing (HR, 0.71).
Local relapse-free survival was also better with weekly dosing, at a 3-year rate of 69.6% versus 59.5% for patients in the three-weekly group (HR, 0.73).
On a planned subgroup analysis, weekly CDDP+RT was nonsignificantly superior to the three-weekly schedule on almost every measure, whether looking at patient age, ECOG performance status, and primary site.
There were also differences in the occurrence of hematologic toxicities between the two groups, with fewer patients given the weekly schedule experiencing grade 3/4 neutropenia than those on the three-weekly dosing. However, there were more cases of any grade thrombocytopenia for patients getting the weekly dosing.
The weekly CDDP+RT regimen demonstrated its lower toxicity when looking at acute nonhematologic adverse events, with fewer occurrences of any grade dysphagia, nausea, hyponatremia, renal impairment, and hearing impairment versus the three-weekly schedule.
The weekly dosing schedule was also associated with lower rates of grade 3/4 dysphagia, nausea, and infection.
The study was funded by the National Cancer Center Research and Development Fund, Japan Agency for Medical Research and Development Fund.
Dr. Kiyota reports honoraria from AstraZeneca, Bayer, Bristol-Myers Squibb Japan, Chugai Pharma, Eisai, Merck Serono, MSD, and Ono Pharmaceutical; speakers bureau fees from AstraZeneca, Bayer, Bristol-Myers Squibb Japan; Eisai, Merck Serono, MSD, and Ono Pharmaceutical; and receiving research funding from AstraZeneca (Inst), Bristol-Myers Squibb (Inst), Ono Pharmaceutical (Inst), Pfizer (Inst), and Roche (Inst). Other study authors report potential conflicts of interest. The full list can be found here.
Dr. Mehanna reports stock and other ownership interests in Warwickshire Head and Neck Clinic; honoraria from AstraZeneca; speakers bureau fess from Merck, MSD, and Sanofi Pasteur; research funding from AstraZeneca, GlaxoSmithKline (Inst), MSD (Inst), Sanofi Pasteur (Inst), and Silence Therapeutics (Inst); and travel, accommodations, and expenses from Merck, MSD, and Sanofi Pasteur.
Dr. Saba reports honoraria from Aduro Biotech, Bristol-Myers Squibb, Cue Biopharma, Genentech/Roche, GSK, Kura, Lilly, Merck, and Pfizer; a consulting or advisory role with Biontech, Bluprint, Bristol-Myers Squibb, Lilly, Merck, and Pfizer; research funding from Bristol-Myers Squibb and Exelixis; travel, accommodations, and expenses from Bluprint, Bristol-Myers Squibb, Genentech/Roche, GSK, Lilly, Merck, and Pfizer.
This article first appeared on Medscape.com.
For the first time, weekly cisplatin plus radiotherapy (CDDP+RT) has been shown to be not only less toxic than dosing once every three weeks but to also achieve better outcomes in patients with postoperative squamous cell carcinoma of the head and neck (SCCHN), say Japanese researchers.
These results, from the JCOG1008 trial, suggest the weekly schedule should become the new standard of care in these patients, potentially settling what has been a “contentious” issue.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 6502), held virtually because of the coronavirus pandemic.
Lead author Naomi Kiyota, MD, PhD, medical oncology and hematology, Cancer Center, Kobe University Hospital, Japan, said the study involving more than 160 high-risk patients with SCCHN demonstrated comparable overall survival in the weekly and three-weekly CDDP+RT groups.
Moreover, it showed that the weekly schedule was associated with better relapse-free and local relapse-free survival, and, in line with previous studies, had a more favorable safety profile.
“This phase II/III study is the first to show that weekly CDDP+RT is noninferior to three-weekly CDDP+RT [and] is a new standard treatment option for these patients,” Dr. Kiyota said.
Study discussant Hisham M. Mehanna, MD, PhD, Warwickshire Head and Neck Clinic, University of Birmingham, UK, described the study as a “significant achievement” that answers “an important question that we’ve been asking for a very long time.”
He said that, despite three-weekly CDDP+RT being the standard treatment in the postoperative setting for SCCHN, there have been “lingering concerns,” as 40% of patients don’t get all three CDDP cycles “and it is toxic.”
Weekly CDDP is, on the other hand, “widely used, although the evidence for it is not as strong,” and has a number of advantages, including that it can be delivered in the outpatient setting and it may be less toxic.
Dr. Mehanna said there was “a surprise” to the current study, in that it was terminated early because it crossed the boundary for non-inferiority because weekly CDDP has better survival than the three-weekly dose; notably, however, superiority was not achieved.
Dr. Mehanna also expressed some reservations over imbalances in the treatment groups that could have meant the three-weekly cohort had an unfavorable prognosis, and said questions remain over longer-term toxicity.
‘Contentious issue’
In a highlights session, Nabil F. Saba, MD, director of the head and neck oncology program at Emory University’s Winship Cancer Institute in Atlanta, Georgia, said the dosing of CDDP in these patients has been “a contentious issue.”
One issue has been whether scheduling of CDDP or the cumulative dose achieved is the key determinant of clinical outcome, and he suggested that the superior results seen in the current study can be attributed to the high cumulative dose the investigators achieved in their patients compared with previous investigations.
For Dr. Saba, the take-home message of the trial is that weekly cisplatin “is now, finally, an accepted standard of care in the postoperative high-risk setting, which is a major change at this ASCO meeting.”
Presenting the trial, Dr. Kiyota said, in a recent study (J Clin Oncol. 2017 Dec 8. doi: 10.1200/JCO.2017.74.9457) from the Tata Memorial Hospital, weekly CDDP at 30 mg/m2 plus radiotherapy failed to achieve noninferiority to a three-weekly regimen, “albeit with fewer toxicities.”
He suggested that this could be because it was a single-center trial, two different treatment strategies were used, the majority of primary sites were in the oral cavity, and the dose was insufficient.
His team, on the other hand, undertook a randomized trial in which patients with postoperative high-risk SCCHN were recruited from 28 institutions.
The participants, who were aged 20-75 years and had ECOG performance status 0-1, all had pathological stage III/IV disease and a microscopically positive margin and/or extranodal extension.
They were randomly assigned to 100 mg/m2 CDDP once every three weeks or weekly 40 mg/m2 CDDP, plus radiotherapy at 66 Gy over 33 fractions.
For the intention-to-treat efficacy analysis, 132 patients received three-weekly CDDP+RT and 129 had weekly CDDP+RT, while the per-protocol safety analysis included 129 and 122 patients, respectively.
The median age of the patients was 61-62 years, and 110 patients in both treatment groups were male. Although there was a similar distribution of primary sites and high-risk factors in the two groups, more patients in the weekly group had pathological stage T2 disease (40) than in the three-weekly group (26).
The dose targets were met in both treatment groups. In the three-weekly group, the cumulative dose of CDDP achieved was 280 mg/m2, and, in the weekly group, it was 239 mg/m2.
The second planned interim analysis showed that, over a median follow-up of 2.2 years, 3-year overall survival was estimated at 71.6% in the weekly group versus 59.1% in the three-weekly group (hazard ratio, 0.69).
As this was below the one-sided P value for noninferiority, the data and safety monitoring committee recommended terminating the trial early.
The researchers also found that the 3-year relapse-free survival was higher with weekly CDDP+RT, at 64.5%, vs 53.0% with three-weekly dosing (HR, 0.71).
Local relapse-free survival was also better with weekly dosing, at a 3-year rate of 69.6% versus 59.5% for patients in the three-weekly group (HR, 0.73).
On a planned subgroup analysis, weekly CDDP+RT was nonsignificantly superior to the three-weekly schedule on almost every measure, whether looking at patient age, ECOG performance status, and primary site.
There were also differences in the occurrence of hematologic toxicities between the two groups, with fewer patients given the weekly schedule experiencing grade 3/4 neutropenia than those on the three-weekly dosing. However, there were more cases of any grade thrombocytopenia for patients getting the weekly dosing.
The weekly CDDP+RT regimen demonstrated its lower toxicity when looking at acute nonhematologic adverse events, with fewer occurrences of any grade dysphagia, nausea, hyponatremia, renal impairment, and hearing impairment versus the three-weekly schedule.
The weekly dosing schedule was also associated with lower rates of grade 3/4 dysphagia, nausea, and infection.
The study was funded by the National Cancer Center Research and Development Fund, Japan Agency for Medical Research and Development Fund.
Dr. Kiyota reports honoraria from AstraZeneca, Bayer, Bristol-Myers Squibb Japan, Chugai Pharma, Eisai, Merck Serono, MSD, and Ono Pharmaceutical; speakers bureau fees from AstraZeneca, Bayer, Bristol-Myers Squibb Japan; Eisai, Merck Serono, MSD, and Ono Pharmaceutical; and receiving research funding from AstraZeneca (Inst), Bristol-Myers Squibb (Inst), Ono Pharmaceutical (Inst), Pfizer (Inst), and Roche (Inst). Other study authors report potential conflicts of interest. The full list can be found here.
Dr. Mehanna reports stock and other ownership interests in Warwickshire Head and Neck Clinic; honoraria from AstraZeneca; speakers bureau fess from Merck, MSD, and Sanofi Pasteur; research funding from AstraZeneca, GlaxoSmithKline (Inst), MSD (Inst), Sanofi Pasteur (Inst), and Silence Therapeutics (Inst); and travel, accommodations, and expenses from Merck, MSD, and Sanofi Pasteur.
Dr. Saba reports honoraria from Aduro Biotech, Bristol-Myers Squibb, Cue Biopharma, Genentech/Roche, GSK, Kura, Lilly, Merck, and Pfizer; a consulting or advisory role with Biontech, Bluprint, Bristol-Myers Squibb, Lilly, Merck, and Pfizer; research funding from Bristol-Myers Squibb and Exelixis; travel, accommodations, and expenses from Bluprint, Bristol-Myers Squibb, Genentech/Roche, GSK, Lilly, Merck, and Pfizer.
This article first appeared on Medscape.com.
FROM ASCO 2020
Three years of imatinib may halve death rate in GIST
, phase 3 trial data suggest.
The most recent analysis of the SSGXVIII/AIO trial shows that, in about 400 patients who underwent surgery and had a high estimated risk of recurrence, there was a 50% increase in overall survival with longer treatment at 10 years on an efficacy analysis.
Moreover, there was a 30% improvement in recurrence-free survival (RFS) with 3 years vs 1 year of imatinib, with an even greater benefit seen in patients with a common tumor mutation.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 11503), held virtually because of the coronavirus pandemic.
Lead author Peter Reichardt, MD, Helios Klinikum Berlin-Buch, Berlin, Germany, said the results show that “3 years of adjuvant imatinib is highly superior” in terms of RFS and overall survival to 1 year of treatment.
“Overall, approximately 50% of deaths can be avoided during the first 10 years of follow-up after surgery with the longer adjuvant imatinib treatment.”
Study discussant Giovanni Grignani, MD, Division of Medical Oncology, Candiolo Cancer Institute, FPO-IRCCS, Turin, Italy, said that the “burning question” in the sarcoma space is: “Can we improve overall survival by reducing the risk of relapse with a perioperative treatment?
“We would like to able to identify patients for whom the cost of toxicity is paid off by an improvement in their outcome,” he added, noting that this is not achievable “and this is why perioperative treatment is so controversial in oncology.”
Grignani said the picture is a little different for GIST, as the relapse risk is unevenly distributed, the activity of imatinib is “extraordinary,” and the drug toxicity is “certainly bearable but not negligible.”
RFS is, however, affected by the inability of imatinib to eradicate resistant clones left behind by surgery, and replication resumes once the drug is stopped.
The current study nevertheless shows that overall survival “clearly favors 3-year imatinib therapy…with an impressive median follow-up of 119 months [10 years],” commented Patrick Leavey, MD, University of Texas Southwestern Medical Center, Dallas, in a highlights session.
He added that, in GIST, what might be considered “new progress” with the findings “is clarity over the length of imatinib therapy, which ... seems to be safe.”
Reichardt began by noting that several large randomized trials over the past decade have shown that adjuvant imatinib improves both RFS and overall survival.
However, “it is unknown whether imatinib improves overall survival after extended follow-up,” in addition to which “little is known about the long-term safety” of the drug in this setting.
To offer further insights, the protocol of SSGXVIII/AIO was amended in April 2017 to allow for a third analysis to be carried out once the last patient who entered the trial has been followed up for 10 years.
More Details
Reichardt recalled that the study, which was an open-label, multicenter phase 3 trial, involved GIST patients who were randomly assigned following surgery in a 1:1 fashion to imatinib for either 12 months or 36 months.
The patients were required to have a high-risk of recurrence, defined as at least one of the following:
- Tumor size >10 cm
- Tumor mitosis count >10/50 on high-powered microscopy (HPF)
- Tumor size >5 cm and mitosis count >5/50 HPF
- Tumor rupture, either spontaneously or at surgery.
Four hundred patients were recruited between February 2004 and September 2008, and 181 patients who were randomly assigned to 12 months of imatinib and 177 to 36 months were included in the efficacy analysis.
The median age of the patients was approximately 61 years, and half were female. The treatment groups were well-balanced in terms of their baseline characteristics.
Of note, 69% of patients in the 1-year treatment group and 71% of those given imatinib for 3 years had a detectable mutation in the KIT exon 11 site. The mean mitosis count was 10/50 and 8/50, respectively.
Over a median follow-up of 119 months (9 years, 11 months), 53% of 1-year treatment patients experienced a recurrence event, and 30% died, of whom 82% died with metastatic GIST.
In the 3-year treatment group, 44% experienced a recurrence event, and 18% died, with 83% of deaths from metastatic GIST.
On intention-to-treat analysis, RFS at 10 years was significantly higher with 3 years of imatinib than with 1 year, at 53% vs 42% (hazard ratio [HR], 0.66; P = .003).
Overall survival at 10 years was also higher with longer imatinib treatment, at 79% with 3 years of therapy vs 65% with 1 year (HR, 0.55; P = .004).
The team found on subgroup analysis that RFS was significantly better with 3-year than 1-year imatinib in patients with:
- A local mitotic count >10 (HR = 0.42)
- A central mitotic count >10 (HR = 0.50)
- A KIT exon 11 tumor mutation (HR = 0.57).
On the efficacy analysis, which included patients who signed informed consent, had GIST at pathology review, and no overt metastases at study entry, the HR for RFS with 3-year vs 1-year therapy was 0.70, whereas the HR for overall survival was 0.50.
Patients treated with imatinib for 3 years had a higher rate of any new cancer during follow-up, at 17%, vs 12% for those treated with imatinib for 1 year. Prostate cancer was the most common form of the disease in both groups.
Cardiac events were, in contrast, evenly distributed between the two groups, with 5% of 3-year patients and 6% of 1-year patients experiencing an event.
The study was funded by Novartis.
Reichardt reports honoraria from Amgen, Bayer, Lilly, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, Clinigen Group, Decipher, Lilly, Novartis, Pfizer, PharmaMar, and Roche; and receiving research funding from Novartis (Inst). Other authors report potential conflicts of interest.
Grignani reports honoraria from Bayer, EISAI, Lilly, Merck Serono, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, EISAI, and PharmaMar; receiving research funding from PharmaMar (Inst); and travel, accommodations, expenses from PharmaMar and Tesaro.
Leavey reports receiving research funding from Elison Pharmaceuticals (Inst).
This article first appeared on Medscape.com.
, phase 3 trial data suggest.
The most recent analysis of the SSGXVIII/AIO trial shows that, in about 400 patients who underwent surgery and had a high estimated risk of recurrence, there was a 50% increase in overall survival with longer treatment at 10 years on an efficacy analysis.
Moreover, there was a 30% improvement in recurrence-free survival (RFS) with 3 years vs 1 year of imatinib, with an even greater benefit seen in patients with a common tumor mutation.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 11503), held virtually because of the coronavirus pandemic.
Lead author Peter Reichardt, MD, Helios Klinikum Berlin-Buch, Berlin, Germany, said the results show that “3 years of adjuvant imatinib is highly superior” in terms of RFS and overall survival to 1 year of treatment.
“Overall, approximately 50% of deaths can be avoided during the first 10 years of follow-up after surgery with the longer adjuvant imatinib treatment.”
Study discussant Giovanni Grignani, MD, Division of Medical Oncology, Candiolo Cancer Institute, FPO-IRCCS, Turin, Italy, said that the “burning question” in the sarcoma space is: “Can we improve overall survival by reducing the risk of relapse with a perioperative treatment?
“We would like to able to identify patients for whom the cost of toxicity is paid off by an improvement in their outcome,” he added, noting that this is not achievable “and this is why perioperative treatment is so controversial in oncology.”
Grignani said the picture is a little different for GIST, as the relapse risk is unevenly distributed, the activity of imatinib is “extraordinary,” and the drug toxicity is “certainly bearable but not negligible.”
RFS is, however, affected by the inability of imatinib to eradicate resistant clones left behind by surgery, and replication resumes once the drug is stopped.
The current study nevertheless shows that overall survival “clearly favors 3-year imatinib therapy…with an impressive median follow-up of 119 months [10 years],” commented Patrick Leavey, MD, University of Texas Southwestern Medical Center, Dallas, in a highlights session.
He added that, in GIST, what might be considered “new progress” with the findings “is clarity over the length of imatinib therapy, which ... seems to be safe.”
Reichardt began by noting that several large randomized trials over the past decade have shown that adjuvant imatinib improves both RFS and overall survival.
However, “it is unknown whether imatinib improves overall survival after extended follow-up,” in addition to which “little is known about the long-term safety” of the drug in this setting.
To offer further insights, the protocol of SSGXVIII/AIO was amended in April 2017 to allow for a third analysis to be carried out once the last patient who entered the trial has been followed up for 10 years.
More Details
Reichardt recalled that the study, which was an open-label, multicenter phase 3 trial, involved GIST patients who were randomly assigned following surgery in a 1:1 fashion to imatinib for either 12 months or 36 months.
The patients were required to have a high-risk of recurrence, defined as at least one of the following:
- Tumor size >10 cm
- Tumor mitosis count >10/50 on high-powered microscopy (HPF)
- Tumor size >5 cm and mitosis count >5/50 HPF
- Tumor rupture, either spontaneously or at surgery.
Four hundred patients were recruited between February 2004 and September 2008, and 181 patients who were randomly assigned to 12 months of imatinib and 177 to 36 months were included in the efficacy analysis.
The median age of the patients was approximately 61 years, and half were female. The treatment groups were well-balanced in terms of their baseline characteristics.
Of note, 69% of patients in the 1-year treatment group and 71% of those given imatinib for 3 years had a detectable mutation in the KIT exon 11 site. The mean mitosis count was 10/50 and 8/50, respectively.
Over a median follow-up of 119 months (9 years, 11 months), 53% of 1-year treatment patients experienced a recurrence event, and 30% died, of whom 82% died with metastatic GIST.
In the 3-year treatment group, 44% experienced a recurrence event, and 18% died, with 83% of deaths from metastatic GIST.
On intention-to-treat analysis, RFS at 10 years was significantly higher with 3 years of imatinib than with 1 year, at 53% vs 42% (hazard ratio [HR], 0.66; P = .003).
Overall survival at 10 years was also higher with longer imatinib treatment, at 79% with 3 years of therapy vs 65% with 1 year (HR, 0.55; P = .004).
The team found on subgroup analysis that RFS was significantly better with 3-year than 1-year imatinib in patients with:
- A local mitotic count >10 (HR = 0.42)
- A central mitotic count >10 (HR = 0.50)
- A KIT exon 11 tumor mutation (HR = 0.57).
On the efficacy analysis, which included patients who signed informed consent, had GIST at pathology review, and no overt metastases at study entry, the HR for RFS with 3-year vs 1-year therapy was 0.70, whereas the HR for overall survival was 0.50.
Patients treated with imatinib for 3 years had a higher rate of any new cancer during follow-up, at 17%, vs 12% for those treated with imatinib for 1 year. Prostate cancer was the most common form of the disease in both groups.
Cardiac events were, in contrast, evenly distributed between the two groups, with 5% of 3-year patients and 6% of 1-year patients experiencing an event.
The study was funded by Novartis.
Reichardt reports honoraria from Amgen, Bayer, Lilly, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, Clinigen Group, Decipher, Lilly, Novartis, Pfizer, PharmaMar, and Roche; and receiving research funding from Novartis (Inst). Other authors report potential conflicts of interest.
Grignani reports honoraria from Bayer, EISAI, Lilly, Merck Serono, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, EISAI, and PharmaMar; receiving research funding from PharmaMar (Inst); and travel, accommodations, expenses from PharmaMar and Tesaro.
Leavey reports receiving research funding from Elison Pharmaceuticals (Inst).
This article first appeared on Medscape.com.
, phase 3 trial data suggest.
The most recent analysis of the SSGXVIII/AIO trial shows that, in about 400 patients who underwent surgery and had a high estimated risk of recurrence, there was a 50% increase in overall survival with longer treatment at 10 years on an efficacy analysis.
Moreover, there was a 30% improvement in recurrence-free survival (RFS) with 3 years vs 1 year of imatinib, with an even greater benefit seen in patients with a common tumor mutation.
The research was presented at the 2020 annual meeting of the American Society of Clinical Oncology (abstract 11503), held virtually because of the coronavirus pandemic.
Lead author Peter Reichardt, MD, Helios Klinikum Berlin-Buch, Berlin, Germany, said the results show that “3 years of adjuvant imatinib is highly superior” in terms of RFS and overall survival to 1 year of treatment.
“Overall, approximately 50% of deaths can be avoided during the first 10 years of follow-up after surgery with the longer adjuvant imatinib treatment.”
Study discussant Giovanni Grignani, MD, Division of Medical Oncology, Candiolo Cancer Institute, FPO-IRCCS, Turin, Italy, said that the “burning question” in the sarcoma space is: “Can we improve overall survival by reducing the risk of relapse with a perioperative treatment?
“We would like to able to identify patients for whom the cost of toxicity is paid off by an improvement in their outcome,” he added, noting that this is not achievable “and this is why perioperative treatment is so controversial in oncology.”
Grignani said the picture is a little different for GIST, as the relapse risk is unevenly distributed, the activity of imatinib is “extraordinary,” and the drug toxicity is “certainly bearable but not negligible.”
RFS is, however, affected by the inability of imatinib to eradicate resistant clones left behind by surgery, and replication resumes once the drug is stopped.
The current study nevertheless shows that overall survival “clearly favors 3-year imatinib therapy…with an impressive median follow-up of 119 months [10 years],” commented Patrick Leavey, MD, University of Texas Southwestern Medical Center, Dallas, in a highlights session.
He added that, in GIST, what might be considered “new progress” with the findings “is clarity over the length of imatinib therapy, which ... seems to be safe.”
Reichardt began by noting that several large randomized trials over the past decade have shown that adjuvant imatinib improves both RFS and overall survival.
However, “it is unknown whether imatinib improves overall survival after extended follow-up,” in addition to which “little is known about the long-term safety” of the drug in this setting.
To offer further insights, the protocol of SSGXVIII/AIO was amended in April 2017 to allow for a third analysis to be carried out once the last patient who entered the trial has been followed up for 10 years.
More Details
Reichardt recalled that the study, which was an open-label, multicenter phase 3 trial, involved GIST patients who were randomly assigned following surgery in a 1:1 fashion to imatinib for either 12 months or 36 months.
The patients were required to have a high-risk of recurrence, defined as at least one of the following:
- Tumor size >10 cm
- Tumor mitosis count >10/50 on high-powered microscopy (HPF)
- Tumor size >5 cm and mitosis count >5/50 HPF
- Tumor rupture, either spontaneously or at surgery.
Four hundred patients were recruited between February 2004 and September 2008, and 181 patients who were randomly assigned to 12 months of imatinib and 177 to 36 months were included in the efficacy analysis.
The median age of the patients was approximately 61 years, and half were female. The treatment groups were well-balanced in terms of their baseline characteristics.
Of note, 69% of patients in the 1-year treatment group and 71% of those given imatinib for 3 years had a detectable mutation in the KIT exon 11 site. The mean mitosis count was 10/50 and 8/50, respectively.
Over a median follow-up of 119 months (9 years, 11 months), 53% of 1-year treatment patients experienced a recurrence event, and 30% died, of whom 82% died with metastatic GIST.
In the 3-year treatment group, 44% experienced a recurrence event, and 18% died, with 83% of deaths from metastatic GIST.
On intention-to-treat analysis, RFS at 10 years was significantly higher with 3 years of imatinib than with 1 year, at 53% vs 42% (hazard ratio [HR], 0.66; P = .003).
Overall survival at 10 years was also higher with longer imatinib treatment, at 79% with 3 years of therapy vs 65% with 1 year (HR, 0.55; P = .004).
The team found on subgroup analysis that RFS was significantly better with 3-year than 1-year imatinib in patients with:
- A local mitotic count >10 (HR = 0.42)
- A central mitotic count >10 (HR = 0.50)
- A KIT exon 11 tumor mutation (HR = 0.57).
On the efficacy analysis, which included patients who signed informed consent, had GIST at pathology review, and no overt metastases at study entry, the HR for RFS with 3-year vs 1-year therapy was 0.70, whereas the HR for overall survival was 0.50.
Patients treated with imatinib for 3 years had a higher rate of any new cancer during follow-up, at 17%, vs 12% for those treated with imatinib for 1 year. Prostate cancer was the most common form of the disease in both groups.
Cardiac events were, in contrast, evenly distributed between the two groups, with 5% of 3-year patients and 6% of 1-year patients experiencing an event.
The study was funded by Novartis.
Reichardt reports honoraria from Amgen, Bayer, Lilly, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, Clinigen Group, Decipher, Lilly, Novartis, Pfizer, PharmaMar, and Roche; and receiving research funding from Novartis (Inst). Other authors report potential conflicts of interest.
Grignani reports honoraria from Bayer, EISAI, Lilly, Merck Serono, Novartis, Pfizer, and PharmaMar; serving in a consulting or advisory role with Bayer, EISAI, and PharmaMar; receiving research funding from PharmaMar (Inst); and travel, accommodations, expenses from PharmaMar and Tesaro.
Leavey reports receiving research funding from Elison Pharmaceuticals (Inst).
This article first appeared on Medscape.com.
FROM ASCO 2020
Updated BEACON: Doublet as good as triplet in metastatic CRC
The BEACON study tested both a doublet and a triplet of drugs for patients with previously treated BRAF V600E–mutated metastatic colorectal cancer (CRC).
New results from that trial, with an updated survival analysis, show that the doublet is sufficient and that patients can safely be treated with a combination of the BRAF inhibitor encorafenib (Braftovi, Array BioPharma) and the EGFR inhibitor monoclonal antibody cetuximab (Erbitux, Eli Lilly).
This means that the increased toxicity from the addition of the MEK inhibitor binimetinib (Mektovi, Array BioPharma) can be avoided and that good outcomes can be maintained.
The new results were presented as part of the virtual scientific program of the 2020 American Society of Clinical Oncology annual meeting.
Study discussant Michael S. Lee, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill, said he “would consider encorafenib and cetuximab now the standard of care in the second line and beyond in BRAF-mutant colorectal cancer.
“I would give the doublet rather than the triplet because of the comparable survival and better side effect profile,” he said.
“This is immediately practice changing, given the FDA approval of encorafenib and cetuximab,” commented Autumn J. McRee, MD, UNC Lineberger Comprehensive Cancer Center.
This is a “clinically relevant” trial, and it demonstrates that the “poorest prognostic group in colorectal cancer now has viable options,” she said at a Highlights of the Day session.
“We will await the results of the ANCHOR-CRC trial to see if we should be using this targeted approach in earlier lines of therapy,” she added.
New survival data
The primary analysis of BEACON CRC, presented at the 2019 World Conference on Gastrointestinal Cancer, showed that use of the triplet therapy was associated with a 48% improvement in overall survival in comparison with standard chemotherapy.
Although that was also linked to improved quality of life, questions have been raised as to whether the benefits are worth the cost, and one commentator singled the study out for harsh criticism.
Scott Kopetz, MD, PhD, from the University of Texas MD Anderson Cancer Center, Houston, presented the updated survival results from BEACON CRC, which included data from an additional 6 months of follow-up.
“We know that the V600E mutation in BRAF occurs in about 10%-15% of patients and is associated with a poor prognosis,” Dr. Kopetz commented.
“BRAF inhibitors alone are not effective,” he noted. He said preclinical models point toward an approach that targets multiple pathways, including BRAF, MEK, and EGFR.
The BEACON study had three arms, each with 205 patients, as follows:
- Encorafenib plus binimetinib plus cetuximab
- Encorafenib plus cetixumab
- A control arm of FOLFIRI plus cetuximab or irinotecan plus cetuximab.
The three arms of the trial were relatively well balanced with respect to patient characteristics, Dr. Kopetz commented. The median age of the patients ranged from 60 to 62 years, and 48%-57% of the patients were women.
Of note, between 5% and 10% of the cases were characterized by high microsatellite instability, and 34%-35% of patients had received more than one prior line of therapy.
The data now presented at ASCO represent a post hoc updated analysis that includes 6 months of additional follow-up since the primary analysis was presented, Dr. Kopetz explained.
After a median follow-up of 12.8 months, 13% of triplet therapy patients, 14% of those who received doublet therapy, and 3% of control patients were still on treatment.
The updated analysis shows that median overall survival with the doublet therapy was 9.3 months versus 5.9 months for the control group (hazard ratio, 0.61). The benefit was seen across all subgroups, including those based on the number of prior regimens.
Dr. Kopetz pointed out that overall survival was numerically superior to that seen in the primary analysis, which was 8.4 months.
The updated survival analysis for the triplet therapy indicated that the median overall survival was 9.3 months versus 5.9 months in the control arm (HR, 0.60). Again, this was consistent across subgroups.
In the primary analysis, the median overall survival with the triplet therapy was 9.0 months.
The team also compared the triplet and doublet therapies, finding that, “in contrast to what was seen in the primary analysis ... we see numerically identical median overall survival with the two arms.” The result was sustained across subgroups.
However, there were indications that there may be survival benefits with the triplet in certain patient subgroups, including those with Eastern Cooperative Oncology Group performance status 1, those in whom three or more organs are involved, those with higher baseline levels of C-reactive protein, and those with partially resected or unresected disease.
Progression-free survival was comparable between the two treatment groups, at 4.5 months with the triplet therapy and 4.3 months with the doublet, compared with just 1.5 months in the control arm.
The updated analysis also showed that the objective response rate was 27% with triplet therapy versus 20% with the doublet and 2% in the control arm. In both the doublet and triplet arms, the majority of responses were partial.
With regard to safety, Dr. Kopetz said that the updated data regarding adverse events were in general “consistent with the previously reported safety profile.”
He added it is “notable” that the triplet therapy “had slightly higher rates of GI toxicity and anemia,” which was not seen with the doublet, something that is “again associated with the known safety profile of a MEK inhibitor.”
The study was funded by Pfizer. Dr. Kopetz has stock and other ownership interests with numerous pharmaceutical companies. Other authors, as well as Dr. Lee and Dr. McRee, have also reported relevant financial relationships.
This article first appeared on Medscape.com.
The BEACON study tested both a doublet and a triplet of drugs for patients with previously treated BRAF V600E–mutated metastatic colorectal cancer (CRC).
New results from that trial, with an updated survival analysis, show that the doublet is sufficient and that patients can safely be treated with a combination of the BRAF inhibitor encorafenib (Braftovi, Array BioPharma) and the EGFR inhibitor monoclonal antibody cetuximab (Erbitux, Eli Lilly).
This means that the increased toxicity from the addition of the MEK inhibitor binimetinib (Mektovi, Array BioPharma) can be avoided and that good outcomes can be maintained.
The new results were presented as part of the virtual scientific program of the 2020 American Society of Clinical Oncology annual meeting.
Study discussant Michael S. Lee, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill, said he “would consider encorafenib and cetuximab now the standard of care in the second line and beyond in BRAF-mutant colorectal cancer.
“I would give the doublet rather than the triplet because of the comparable survival and better side effect profile,” he said.
“This is immediately practice changing, given the FDA approval of encorafenib and cetuximab,” commented Autumn J. McRee, MD, UNC Lineberger Comprehensive Cancer Center.
This is a “clinically relevant” trial, and it demonstrates that the “poorest prognostic group in colorectal cancer now has viable options,” she said at a Highlights of the Day session.
“We will await the results of the ANCHOR-CRC trial to see if we should be using this targeted approach in earlier lines of therapy,” she added.
New survival data
The primary analysis of BEACON CRC, presented at the 2019 World Conference on Gastrointestinal Cancer, showed that use of the triplet therapy was associated with a 48% improvement in overall survival in comparison with standard chemotherapy.
Although that was also linked to improved quality of life, questions have been raised as to whether the benefits are worth the cost, and one commentator singled the study out for harsh criticism.
Scott Kopetz, MD, PhD, from the University of Texas MD Anderson Cancer Center, Houston, presented the updated survival results from BEACON CRC, which included data from an additional 6 months of follow-up.
“We know that the V600E mutation in BRAF occurs in about 10%-15% of patients and is associated with a poor prognosis,” Dr. Kopetz commented.
“BRAF inhibitors alone are not effective,” he noted. He said preclinical models point toward an approach that targets multiple pathways, including BRAF, MEK, and EGFR.
The BEACON study had three arms, each with 205 patients, as follows:
- Encorafenib plus binimetinib plus cetuximab
- Encorafenib plus cetixumab
- A control arm of FOLFIRI plus cetuximab or irinotecan plus cetuximab.
The three arms of the trial were relatively well balanced with respect to patient characteristics, Dr. Kopetz commented. The median age of the patients ranged from 60 to 62 years, and 48%-57% of the patients were women.
Of note, between 5% and 10% of the cases were characterized by high microsatellite instability, and 34%-35% of patients had received more than one prior line of therapy.
The data now presented at ASCO represent a post hoc updated analysis that includes 6 months of additional follow-up since the primary analysis was presented, Dr. Kopetz explained.
After a median follow-up of 12.8 months, 13% of triplet therapy patients, 14% of those who received doublet therapy, and 3% of control patients were still on treatment.
The updated analysis shows that median overall survival with the doublet therapy was 9.3 months versus 5.9 months for the control group (hazard ratio, 0.61). The benefit was seen across all subgroups, including those based on the number of prior regimens.
Dr. Kopetz pointed out that overall survival was numerically superior to that seen in the primary analysis, which was 8.4 months.
The updated survival analysis for the triplet therapy indicated that the median overall survival was 9.3 months versus 5.9 months in the control arm (HR, 0.60). Again, this was consistent across subgroups.
In the primary analysis, the median overall survival with the triplet therapy was 9.0 months.
The team also compared the triplet and doublet therapies, finding that, “in contrast to what was seen in the primary analysis ... we see numerically identical median overall survival with the two arms.” The result was sustained across subgroups.
However, there were indications that there may be survival benefits with the triplet in certain patient subgroups, including those with Eastern Cooperative Oncology Group performance status 1, those in whom three or more organs are involved, those with higher baseline levels of C-reactive protein, and those with partially resected or unresected disease.
Progression-free survival was comparable between the two treatment groups, at 4.5 months with the triplet therapy and 4.3 months with the doublet, compared with just 1.5 months in the control arm.
The updated analysis also showed that the objective response rate was 27% with triplet therapy versus 20% with the doublet and 2% in the control arm. In both the doublet and triplet arms, the majority of responses were partial.
With regard to safety, Dr. Kopetz said that the updated data regarding adverse events were in general “consistent with the previously reported safety profile.”
He added it is “notable” that the triplet therapy “had slightly higher rates of GI toxicity and anemia,” which was not seen with the doublet, something that is “again associated with the known safety profile of a MEK inhibitor.”
The study was funded by Pfizer. Dr. Kopetz has stock and other ownership interests with numerous pharmaceutical companies. Other authors, as well as Dr. Lee and Dr. McRee, have also reported relevant financial relationships.
This article first appeared on Medscape.com.
The BEACON study tested both a doublet and a triplet of drugs for patients with previously treated BRAF V600E–mutated metastatic colorectal cancer (CRC).
New results from that trial, with an updated survival analysis, show that the doublet is sufficient and that patients can safely be treated with a combination of the BRAF inhibitor encorafenib (Braftovi, Array BioPharma) and the EGFR inhibitor monoclonal antibody cetuximab (Erbitux, Eli Lilly).
This means that the increased toxicity from the addition of the MEK inhibitor binimetinib (Mektovi, Array BioPharma) can be avoided and that good outcomes can be maintained.
The new results were presented as part of the virtual scientific program of the 2020 American Society of Clinical Oncology annual meeting.
Study discussant Michael S. Lee, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill, said he “would consider encorafenib and cetuximab now the standard of care in the second line and beyond in BRAF-mutant colorectal cancer.
“I would give the doublet rather than the triplet because of the comparable survival and better side effect profile,” he said.
“This is immediately practice changing, given the FDA approval of encorafenib and cetuximab,” commented Autumn J. McRee, MD, UNC Lineberger Comprehensive Cancer Center.
This is a “clinically relevant” trial, and it demonstrates that the “poorest prognostic group in colorectal cancer now has viable options,” she said at a Highlights of the Day session.
“We will await the results of the ANCHOR-CRC trial to see if we should be using this targeted approach in earlier lines of therapy,” she added.
New survival data
The primary analysis of BEACON CRC, presented at the 2019 World Conference on Gastrointestinal Cancer, showed that use of the triplet therapy was associated with a 48% improvement in overall survival in comparison with standard chemotherapy.
Although that was also linked to improved quality of life, questions have been raised as to whether the benefits are worth the cost, and one commentator singled the study out for harsh criticism.
Scott Kopetz, MD, PhD, from the University of Texas MD Anderson Cancer Center, Houston, presented the updated survival results from BEACON CRC, which included data from an additional 6 months of follow-up.
“We know that the V600E mutation in BRAF occurs in about 10%-15% of patients and is associated with a poor prognosis,” Dr. Kopetz commented.
“BRAF inhibitors alone are not effective,” he noted. He said preclinical models point toward an approach that targets multiple pathways, including BRAF, MEK, and EGFR.
The BEACON study had three arms, each with 205 patients, as follows:
- Encorafenib plus binimetinib plus cetuximab
- Encorafenib plus cetixumab
- A control arm of FOLFIRI plus cetuximab or irinotecan plus cetuximab.
The three arms of the trial were relatively well balanced with respect to patient characteristics, Dr. Kopetz commented. The median age of the patients ranged from 60 to 62 years, and 48%-57% of the patients were women.
Of note, between 5% and 10% of the cases were characterized by high microsatellite instability, and 34%-35% of patients had received more than one prior line of therapy.
The data now presented at ASCO represent a post hoc updated analysis that includes 6 months of additional follow-up since the primary analysis was presented, Dr. Kopetz explained.
After a median follow-up of 12.8 months, 13% of triplet therapy patients, 14% of those who received doublet therapy, and 3% of control patients were still on treatment.
The updated analysis shows that median overall survival with the doublet therapy was 9.3 months versus 5.9 months for the control group (hazard ratio, 0.61). The benefit was seen across all subgroups, including those based on the number of prior regimens.
Dr. Kopetz pointed out that overall survival was numerically superior to that seen in the primary analysis, which was 8.4 months.
The updated survival analysis for the triplet therapy indicated that the median overall survival was 9.3 months versus 5.9 months in the control arm (HR, 0.60). Again, this was consistent across subgroups.
In the primary analysis, the median overall survival with the triplet therapy was 9.0 months.
The team also compared the triplet and doublet therapies, finding that, “in contrast to what was seen in the primary analysis ... we see numerically identical median overall survival with the two arms.” The result was sustained across subgroups.
However, there were indications that there may be survival benefits with the triplet in certain patient subgroups, including those with Eastern Cooperative Oncology Group performance status 1, those in whom three or more organs are involved, those with higher baseline levels of C-reactive protein, and those with partially resected or unresected disease.
Progression-free survival was comparable between the two treatment groups, at 4.5 months with the triplet therapy and 4.3 months with the doublet, compared with just 1.5 months in the control arm.
The updated analysis also showed that the objective response rate was 27% with triplet therapy versus 20% with the doublet and 2% in the control arm. In both the doublet and triplet arms, the majority of responses were partial.
With regard to safety, Dr. Kopetz said that the updated data regarding adverse events were in general “consistent with the previously reported safety profile.”
He added it is “notable” that the triplet therapy “had slightly higher rates of GI toxicity and anemia,” which was not seen with the doublet, something that is “again associated with the known safety profile of a MEK inhibitor.”
The study was funded by Pfizer. Dr. Kopetz has stock and other ownership interests with numerous pharmaceutical companies. Other authors, as well as Dr. Lee and Dr. McRee, have also reported relevant financial relationships.
This article first appeared on Medscape.com.
FROM ASCO 2020
Need HER2-positive testing in CRC; trastuzumab deruxtecan shows benefit
Testing for HER2 in patients with colorectal cancer (CRC) should become a new standard of care, say experts discussing new results from a phase 2 trial showing benefit with trastuzumab deruxtecan (T-DXd, marketed as Enhertu, AstraZeneca/Daiichi Sankyo).
This drug is approved in the United States for use in the treatment of unresectable or metastatic HER2-positive breast cancer in patients who have already received two or more prior anti–HER2-based regimens in the metastatic setting.
Results come from a phase 2 study, dubbed DESTINY-CRC01, in patients with previously treated HER2+ advanced CRC.
The results show that, in patients with the highest degree of HER2 positivity, T-DXd was associated with an objective response rate of over 45% and a median progression-free survival (PFS) of almost 7 months.
They “demonstrate, in our opinion, the potential of T-DXd as a treatment option” for patients with advanced HER2-positive colorectal cancer that is refractory to standard therapies, said lead investigator Salvatore Siena, MD, from Niguarda Cancer Center, in Milan, Italy.
He presented the results at the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because of the coronavirus pandemic.
At the same time, results from another study, this time in gastric cancer patients, were published online in the New England Journal of Medicine.
Interstitial lung disease as adverse event
The safety profile of T-DXd seen in the colorectal trial “is consistent with what has been previously reported,” said Siena, adding that most of the adverse events were low grade. But he noted there was also a serious adverse effect – interstitial lung disease (ILD). This occurred in 6% of patients, two of whom died. This is “an important risk and requires careful monitoring and proper intervention,” he emphasized.
The ILD adverse effect in this study is “a concern…and something to consider,” commented discussant for the study Michael S. Lee, MD, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill. But he added that these are the “the best data so far for subsequent anti-HER2 therapy in colorectal cancer”.
Also, the dose of drug used in this trial was higher than that approved for breast cancer, and the incidence of ILD “begs the question of whether we should be using a lower dose in this patient population,” said Autumn J. McRee, MD, also from Lineberger, in a highlights session at the meeting.
“The question here really is whether an HER2-specific approach is superior to what we would offer to these patients in the standard of care setting,” McRee said.
She noted that the patients in DESTINY-CRC01 were “heavily pretreated…and if you think about what our options are in the refractory setting, we do have two approved treatments: regorafenib [Stivarga, Bayer] and TAS-102 [Lonsurf, Taiho Oncology].”
The current data suggest, however, that T-DXd is associated with a trend toward higher response rates and improved survival outcomes, as well as lower monthly costs.
“Without a doubt, this trial is clinically relevant,” she said, adding that it’s “important not to miss these patients.”
“They are rare…but I would argue that testing for HER2 amplification in colorectal cancer should be considered standard of care,” she said.
She added that, based on the current evidence, the trial “may be” practice changing, although it is “still to be determined how to sequence HER2 targeted therapies.”
Study details
The trial was conducted in 78 patients with previously treated unresectable and/or metastatic CRC that was HER2 expressing, RAS/BRAF wild type, and patients had to have received at least two prior regimens, including prior anti-HER2 treatment. Patients with current or suspected ILD were excluded.
Patients were divided into three cohorts based on the degree of HER2 positivity:
- HER2+ with immunohistochemistry (IHC) scoring 3+ or IHC2+/in-situ-hybridization (ISH)+ (cohort A, n = 53)
- HER2 IHC2+/ISH– (cohort B, n = 7)
- HER2 IHC1+ (cohort C, n = 18)
All patients received T-DXd at 6.4 mg/kg intravenously every 3 weeks until progression or intolerable toxicity.
Across the three cohorts, the median age was 58.5 years, and nearly half (47.4%) of patients were female. The vast majority (98.7%) of patents had ECOG performance status 0 or 1, and the primary tumor site was the left colon or rectum in 89.7%.
Siena noted that “the median number of prior lines of standard therapies was four, ranging from two to 11.” All patients had previously received irinotecan and oxaliplatin, and 20.5% had received an anti-HER2 drug.
At the data cutoff on August 9, 2019, 38.5% of patients remained on treatment. The reason for discontinuation was progressive disease in 41%, and clinical progression in 9%.
Siena reported that the overall response rate, as confirmed by independent central review, was 45.3% in cohort A, with all but one of the 24 responders having a partial response. No responses were recorded in cohorts B and C.
Stable disease was seen in 37.7% of cohort A patients, giving a disease control rate of 83%. The median duration of response was not reached.
Median PFS was 6.9 months in cohort A, and the medial overall survival was not reached.
In terms of safety, 50.9% of patients in cohort A and 48.7% patients overall experienced drug-related treatment emergent adverse events, with 22.6% and 17.9%, respectively, having serious drug-related events.
The most common treatment-emergent adverse events were nausea, anemia, reduced neutrophil count, fatigue, and decreased appetite.
There were two deaths related to the study drug, as determined by investigator assessment: one from pneumonitis and one as a result of ILD, with both occurring in cohort A.
Looking specifically at ILD, Siena said there were five events – two grade 2, one grade 3, and two grade 5 – at a median time to reported onset of 80 days. All patients received corticosteroids, as per the study protocol, and two recovered.
Study discussant Lee commented that biomarker testing, such as for HER2, “is part of our standard of care for colorectal cancer,” although studies such as the current one are providing new data to “better refine” treatment approaches.
Lee said that, overall, T-DXd had a response rate and PFS survival “that looked similar to prior data from previous single arm phase 2 studies,” with response rates generally ranging from 30% to 50%, “and this compares favorably with other standard of care options” for chemotherapy-refractory patients.
Nevertheless, there are several ongoing questions related to the treatment of HER2 amplified metastatic CRC patients, some of which are being addressed in the ongoing SWOG S1613 study.
Lee said that, for now, he would recommend that patients with HER2 amplification enroll in a clinical trial, if possible. “However, if that’s not feasible, there are a range of options to consider,” including trastuzumab plus lapatinib (Tykerb, Novartis), or trastuzumab plus pembrolizumab (Keytruda, Merck).
However, “none of these options are FDA approved so there will be issues potentially with financial toxicity and other regulatory issues,” he said.
The study was funded by Daiichi Sankyo Co, Ltd.
Siena reports stock and other ownership interests with Guardant Health and Myriad Genetics; a consulting or advisory role with Amgen, Bayer, Bristol-Myers Squibb, CheckmAb, Clovis Oncology, Daiichi Sankyo, Incyte, Merck, Novartis, Roche/Genentech, Seattle Genetics; research funding from MSD Oncology (Inst); patents, royalties, and other intellectual property from Amgen; and travel, accommodations, expenses from Amgen, Bayer, and Roche. Other coauthors report potential conflicts of interest. The full list can be found with the original article.
Lee reports: Research Funding – Amgen (Inst); Bristol-Myers Squibb (Inst); EMD Serono (Inst); Exelixis (Inst); Genentech/Roche (Inst); Pfizer (Inst); Travel, Accommodations, Expenses – Genentech/Roche.
McRee reports honoraria from Cor2Ed and Onc Live; research funding from AstraZeneca (Inst), BioMed Valley Discoveries (Inst), Boston Biomedical (Inst), Inovio Pharmaceuticals (Inst), Merck (Inst), Novartis (Inst), Rgenix (Inst), and Takeda (Inst); and travel, accommodations, expenses from Cor2Ed.
This article first appeared on Medscape.com.
Testing for HER2 in patients with colorectal cancer (CRC) should become a new standard of care, say experts discussing new results from a phase 2 trial showing benefit with trastuzumab deruxtecan (T-DXd, marketed as Enhertu, AstraZeneca/Daiichi Sankyo).
This drug is approved in the United States for use in the treatment of unresectable or metastatic HER2-positive breast cancer in patients who have already received two or more prior anti–HER2-based regimens in the metastatic setting.
Results come from a phase 2 study, dubbed DESTINY-CRC01, in patients with previously treated HER2+ advanced CRC.
The results show that, in patients with the highest degree of HER2 positivity, T-DXd was associated with an objective response rate of over 45% and a median progression-free survival (PFS) of almost 7 months.
They “demonstrate, in our opinion, the potential of T-DXd as a treatment option” for patients with advanced HER2-positive colorectal cancer that is refractory to standard therapies, said lead investigator Salvatore Siena, MD, from Niguarda Cancer Center, in Milan, Italy.
He presented the results at the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because of the coronavirus pandemic.
At the same time, results from another study, this time in gastric cancer patients, were published online in the New England Journal of Medicine.
Interstitial lung disease as adverse event
The safety profile of T-DXd seen in the colorectal trial “is consistent with what has been previously reported,” said Siena, adding that most of the adverse events were low grade. But he noted there was also a serious adverse effect – interstitial lung disease (ILD). This occurred in 6% of patients, two of whom died. This is “an important risk and requires careful monitoring and proper intervention,” he emphasized.
The ILD adverse effect in this study is “a concern…and something to consider,” commented discussant for the study Michael S. Lee, MD, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill. But he added that these are the “the best data so far for subsequent anti-HER2 therapy in colorectal cancer”.
Also, the dose of drug used in this trial was higher than that approved for breast cancer, and the incidence of ILD “begs the question of whether we should be using a lower dose in this patient population,” said Autumn J. McRee, MD, also from Lineberger, in a highlights session at the meeting.
“The question here really is whether an HER2-specific approach is superior to what we would offer to these patients in the standard of care setting,” McRee said.
She noted that the patients in DESTINY-CRC01 were “heavily pretreated…and if you think about what our options are in the refractory setting, we do have two approved treatments: regorafenib [Stivarga, Bayer] and TAS-102 [Lonsurf, Taiho Oncology].”
The current data suggest, however, that T-DXd is associated with a trend toward higher response rates and improved survival outcomes, as well as lower monthly costs.
“Without a doubt, this trial is clinically relevant,” she said, adding that it’s “important not to miss these patients.”
“They are rare…but I would argue that testing for HER2 amplification in colorectal cancer should be considered standard of care,” she said.
She added that, based on the current evidence, the trial “may be” practice changing, although it is “still to be determined how to sequence HER2 targeted therapies.”
Study details
The trial was conducted in 78 patients with previously treated unresectable and/or metastatic CRC that was HER2 expressing, RAS/BRAF wild type, and patients had to have received at least two prior regimens, including prior anti-HER2 treatment. Patients with current or suspected ILD were excluded.
Patients were divided into three cohorts based on the degree of HER2 positivity:
- HER2+ with immunohistochemistry (IHC) scoring 3+ or IHC2+/in-situ-hybridization (ISH)+ (cohort A, n = 53)
- HER2 IHC2+/ISH– (cohort B, n = 7)
- HER2 IHC1+ (cohort C, n = 18)
All patients received T-DXd at 6.4 mg/kg intravenously every 3 weeks until progression or intolerable toxicity.
Across the three cohorts, the median age was 58.5 years, and nearly half (47.4%) of patients were female. The vast majority (98.7%) of patents had ECOG performance status 0 or 1, and the primary tumor site was the left colon or rectum in 89.7%.
Siena noted that “the median number of prior lines of standard therapies was four, ranging from two to 11.” All patients had previously received irinotecan and oxaliplatin, and 20.5% had received an anti-HER2 drug.
At the data cutoff on August 9, 2019, 38.5% of patients remained on treatment. The reason for discontinuation was progressive disease in 41%, and clinical progression in 9%.
Siena reported that the overall response rate, as confirmed by independent central review, was 45.3% in cohort A, with all but one of the 24 responders having a partial response. No responses were recorded in cohorts B and C.
Stable disease was seen in 37.7% of cohort A patients, giving a disease control rate of 83%. The median duration of response was not reached.
Median PFS was 6.9 months in cohort A, and the medial overall survival was not reached.
In terms of safety, 50.9% of patients in cohort A and 48.7% patients overall experienced drug-related treatment emergent adverse events, with 22.6% and 17.9%, respectively, having serious drug-related events.
The most common treatment-emergent adverse events were nausea, anemia, reduced neutrophil count, fatigue, and decreased appetite.
There were two deaths related to the study drug, as determined by investigator assessment: one from pneumonitis and one as a result of ILD, with both occurring in cohort A.
Looking specifically at ILD, Siena said there were five events – two grade 2, one grade 3, and two grade 5 – at a median time to reported onset of 80 days. All patients received corticosteroids, as per the study protocol, and two recovered.
Study discussant Lee commented that biomarker testing, such as for HER2, “is part of our standard of care for colorectal cancer,” although studies such as the current one are providing new data to “better refine” treatment approaches.
Lee said that, overall, T-DXd had a response rate and PFS survival “that looked similar to prior data from previous single arm phase 2 studies,” with response rates generally ranging from 30% to 50%, “and this compares favorably with other standard of care options” for chemotherapy-refractory patients.
Nevertheless, there are several ongoing questions related to the treatment of HER2 amplified metastatic CRC patients, some of which are being addressed in the ongoing SWOG S1613 study.
Lee said that, for now, he would recommend that patients with HER2 amplification enroll in a clinical trial, if possible. “However, if that’s not feasible, there are a range of options to consider,” including trastuzumab plus lapatinib (Tykerb, Novartis), or trastuzumab plus pembrolizumab (Keytruda, Merck).
However, “none of these options are FDA approved so there will be issues potentially with financial toxicity and other regulatory issues,” he said.
The study was funded by Daiichi Sankyo Co, Ltd.
Siena reports stock and other ownership interests with Guardant Health and Myriad Genetics; a consulting or advisory role with Amgen, Bayer, Bristol-Myers Squibb, CheckmAb, Clovis Oncology, Daiichi Sankyo, Incyte, Merck, Novartis, Roche/Genentech, Seattle Genetics; research funding from MSD Oncology (Inst); patents, royalties, and other intellectual property from Amgen; and travel, accommodations, expenses from Amgen, Bayer, and Roche. Other coauthors report potential conflicts of interest. The full list can be found with the original article.
Lee reports: Research Funding – Amgen (Inst); Bristol-Myers Squibb (Inst); EMD Serono (Inst); Exelixis (Inst); Genentech/Roche (Inst); Pfizer (Inst); Travel, Accommodations, Expenses – Genentech/Roche.
McRee reports honoraria from Cor2Ed and Onc Live; research funding from AstraZeneca (Inst), BioMed Valley Discoveries (Inst), Boston Biomedical (Inst), Inovio Pharmaceuticals (Inst), Merck (Inst), Novartis (Inst), Rgenix (Inst), and Takeda (Inst); and travel, accommodations, expenses from Cor2Ed.
This article first appeared on Medscape.com.
Testing for HER2 in patients with colorectal cancer (CRC) should become a new standard of care, say experts discussing new results from a phase 2 trial showing benefit with trastuzumab deruxtecan (T-DXd, marketed as Enhertu, AstraZeneca/Daiichi Sankyo).
This drug is approved in the United States for use in the treatment of unresectable or metastatic HER2-positive breast cancer in patients who have already received two or more prior anti–HER2-based regimens in the metastatic setting.
Results come from a phase 2 study, dubbed DESTINY-CRC01, in patients with previously treated HER2+ advanced CRC.
The results show that, in patients with the highest degree of HER2 positivity, T-DXd was associated with an objective response rate of over 45% and a median progression-free survival (PFS) of almost 7 months.
They “demonstrate, in our opinion, the potential of T-DXd as a treatment option” for patients with advanced HER2-positive colorectal cancer that is refractory to standard therapies, said lead investigator Salvatore Siena, MD, from Niguarda Cancer Center, in Milan, Italy.
He presented the results at the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because of the coronavirus pandemic.
At the same time, results from another study, this time in gastric cancer patients, were published online in the New England Journal of Medicine.
Interstitial lung disease as adverse event
The safety profile of T-DXd seen in the colorectal trial “is consistent with what has been previously reported,” said Siena, adding that most of the adverse events were low grade. But he noted there was also a serious adverse effect – interstitial lung disease (ILD). This occurred in 6% of patients, two of whom died. This is “an important risk and requires careful monitoring and proper intervention,” he emphasized.
The ILD adverse effect in this study is “a concern…and something to consider,” commented discussant for the study Michael S. Lee, MD, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill. But he added that these are the “the best data so far for subsequent anti-HER2 therapy in colorectal cancer”.
Also, the dose of drug used in this trial was higher than that approved for breast cancer, and the incidence of ILD “begs the question of whether we should be using a lower dose in this patient population,” said Autumn J. McRee, MD, also from Lineberger, in a highlights session at the meeting.
“The question here really is whether an HER2-specific approach is superior to what we would offer to these patients in the standard of care setting,” McRee said.
She noted that the patients in DESTINY-CRC01 were “heavily pretreated…and if you think about what our options are in the refractory setting, we do have two approved treatments: regorafenib [Stivarga, Bayer] and TAS-102 [Lonsurf, Taiho Oncology].”
The current data suggest, however, that T-DXd is associated with a trend toward higher response rates and improved survival outcomes, as well as lower monthly costs.
“Without a doubt, this trial is clinically relevant,” she said, adding that it’s “important not to miss these patients.”
“They are rare…but I would argue that testing for HER2 amplification in colorectal cancer should be considered standard of care,” she said.
She added that, based on the current evidence, the trial “may be” practice changing, although it is “still to be determined how to sequence HER2 targeted therapies.”
Study details
The trial was conducted in 78 patients with previously treated unresectable and/or metastatic CRC that was HER2 expressing, RAS/BRAF wild type, and patients had to have received at least two prior regimens, including prior anti-HER2 treatment. Patients with current or suspected ILD were excluded.
Patients were divided into three cohorts based on the degree of HER2 positivity:
- HER2+ with immunohistochemistry (IHC) scoring 3+ or IHC2+/in-situ-hybridization (ISH)+ (cohort A, n = 53)
- HER2 IHC2+/ISH– (cohort B, n = 7)
- HER2 IHC1+ (cohort C, n = 18)
All patients received T-DXd at 6.4 mg/kg intravenously every 3 weeks until progression or intolerable toxicity.
Across the three cohorts, the median age was 58.5 years, and nearly half (47.4%) of patients were female. The vast majority (98.7%) of patents had ECOG performance status 0 or 1, and the primary tumor site was the left colon or rectum in 89.7%.
Siena noted that “the median number of prior lines of standard therapies was four, ranging from two to 11.” All patients had previously received irinotecan and oxaliplatin, and 20.5% had received an anti-HER2 drug.
At the data cutoff on August 9, 2019, 38.5% of patients remained on treatment. The reason for discontinuation was progressive disease in 41%, and clinical progression in 9%.
Siena reported that the overall response rate, as confirmed by independent central review, was 45.3% in cohort A, with all but one of the 24 responders having a partial response. No responses were recorded in cohorts B and C.
Stable disease was seen in 37.7% of cohort A patients, giving a disease control rate of 83%. The median duration of response was not reached.
Median PFS was 6.9 months in cohort A, and the medial overall survival was not reached.
In terms of safety, 50.9% of patients in cohort A and 48.7% patients overall experienced drug-related treatment emergent adverse events, with 22.6% and 17.9%, respectively, having serious drug-related events.
The most common treatment-emergent adverse events were nausea, anemia, reduced neutrophil count, fatigue, and decreased appetite.
There were two deaths related to the study drug, as determined by investigator assessment: one from pneumonitis and one as a result of ILD, with both occurring in cohort A.
Looking specifically at ILD, Siena said there were five events – two grade 2, one grade 3, and two grade 5 – at a median time to reported onset of 80 days. All patients received corticosteroids, as per the study protocol, and two recovered.
Study discussant Lee commented that biomarker testing, such as for HER2, “is part of our standard of care for colorectal cancer,” although studies such as the current one are providing new data to “better refine” treatment approaches.
Lee said that, overall, T-DXd had a response rate and PFS survival “that looked similar to prior data from previous single arm phase 2 studies,” with response rates generally ranging from 30% to 50%, “and this compares favorably with other standard of care options” for chemotherapy-refractory patients.
Nevertheless, there are several ongoing questions related to the treatment of HER2 amplified metastatic CRC patients, some of which are being addressed in the ongoing SWOG S1613 study.
Lee said that, for now, he would recommend that patients with HER2 amplification enroll in a clinical trial, if possible. “However, if that’s not feasible, there are a range of options to consider,” including trastuzumab plus lapatinib (Tykerb, Novartis), or trastuzumab plus pembrolizumab (Keytruda, Merck).
However, “none of these options are FDA approved so there will be issues potentially with financial toxicity and other regulatory issues,” he said.
The study was funded by Daiichi Sankyo Co, Ltd.
Siena reports stock and other ownership interests with Guardant Health and Myriad Genetics; a consulting or advisory role with Amgen, Bayer, Bristol-Myers Squibb, CheckmAb, Clovis Oncology, Daiichi Sankyo, Incyte, Merck, Novartis, Roche/Genentech, Seattle Genetics; research funding from MSD Oncology (Inst); patents, royalties, and other intellectual property from Amgen; and travel, accommodations, expenses from Amgen, Bayer, and Roche. Other coauthors report potential conflicts of interest. The full list can be found with the original article.
Lee reports: Research Funding – Amgen (Inst); Bristol-Myers Squibb (Inst); EMD Serono (Inst); Exelixis (Inst); Genentech/Roche (Inst); Pfizer (Inst); Travel, Accommodations, Expenses – Genentech/Roche.
McRee reports honoraria from Cor2Ed and Onc Live; research funding from AstraZeneca (Inst), BioMed Valley Discoveries (Inst), Boston Biomedical (Inst), Inovio Pharmaceuticals (Inst), Merck (Inst), Novartis (Inst), Rgenix (Inst), and Takeda (Inst); and travel, accommodations, expenses from Cor2Ed.
This article first appeared on Medscape.com.
FROM ASCO 2020
New OS data with olaparib support ‘new era’ for ovarian cancer
Women with platinum-sensitive relapsed ovarian cancer and a BRCA mutation could see their survival extended by over a year by maintenance therapy with the PARP inhibitor olaparib (Lynparza, AstraZeneca).
The new overall survival (OS) data come from the SOLO2 study and were described as “a significant advance” in a cancer “that has a historically poor prognosis” by Richard Schilsky, MD, senior vice president and chief medical officer of the American Society of Clinical Oncology.
The results were highlighted at a presscast prior to being presented during the virtual scientific program of the 2020 ASCO annual meeting (abstract 6002).
The SOLO2 study randomly assigned almost 300 women with relapsed BRCA-related ovarian cancer that was responding to platinum-based chemotherapy to maintenance therapy with either olaparib or placebo.
Earlier results from this study showed that olaparib was associated with an investigator-assessed progression-free survival (PFS) of 19.1 months, versus just 5.5 months with placebo, as previously reported by Medscape Medical News.
New data from this trial, presented by Andrés Poveda, MD, Initia Oncology, Hospital Quironsalud, in Valencia, Spain, show that olaparib improved median OS by 12.9 months compared to placebo (51.7 months with olaparib vs. 38.8 months with placebo; hazard ratio, 0.74; P = .054).
At 5 years’ follow-up, 42.1% of women taking olaparib were alive, versus 33.2% taking placebo.
In an ASCO press release, Poveda described the improvement in median OS with olaparib as “impressive” and that it offers a “substantial benefit to our patients.
“This study helps usher in a new era of personalized medicine for women with this difficult-to-treat cancer,” he added.
Poveda told reporters that this study is “the first randomized phase 3 trial to provide overall survival data for maintenance PARP inhibitors.
“The finding that 22% of patient in the olaparib group received the study treatment for more than 5 years is unprecedented in the setting of relapsed ovarian cancer,” he added.
The new OS data were welcomed by Konstantin Zakashansky, MD, director of gynecologic oncology at Mount Sinai West, New York, who was not involved in the study.
“PARP inhibitor trials have revolutionized therapy for ovarian cancer in the front line, as well as in the recurrent setting, [with] all of the recently presented trials showing significant improvement in progression free survival,” he said.
“Overall survival data, however, which is considered the most clinically relevant endpoint in oncology trials and remains the ‘gold standard’ because of its relevance and objectivity, have been limited,” he continued.
Zakashansky recalled that when the earlier PFS data from SOLO2 were presented, “questions were raised regarding the clinical uncertainty of the benefit associated with olaparib maintenance, primarily whether the PFS benefit...would translate to a long-term overall survival benefit.”
For him, the current results “answer that question” and offer the “largest improvement in overall survival of any recurrent ovarian cancer patient trial reported to date.”
Schilsky added that the new data confirm that olaparib “should be the standard maintenance therapy for patients with BRCA-related relapsed ovarian cancer responding to platinum-based chemotherapy.”
The drug is already approved for this indication, but the new data showing a significant survival benefit are “comforting” and “good news,” he said.
Adverse events with olaparib
Treatment-emergent adverse events seen in the study were “consistent with the known tolerability profile of olaparib,” Poveda commented.
The most common events of any grade were nausea, fatigue/asthenia, and anemia. The most common event of grade ≥3 was anemia.
Adverse events leading to dose interruptions occurred in 50% of patients who received olaparib and 19% of patients who took placebo. Adverse events leading to dose reductions occurred in 28% and 3%, respectively.
Treatment discontinuation because of adverse events was reported in 17% of patients given olaparib and 3% of those in the placebo arm.
The study was funded by AstraZeneca and Merck Sharp & Dohme. Poveda reports a consulting or advisory role with AstraZeneca, Clovis Oncology, PharmaMar, Roche, and Tesaro and receiving expenses from PharmaMar. Many coauthors also report relationships with pharmaceutical companies.
This article first appeared on Medscape.com.
Women with platinum-sensitive relapsed ovarian cancer and a BRCA mutation could see their survival extended by over a year by maintenance therapy with the PARP inhibitor olaparib (Lynparza, AstraZeneca).
The new overall survival (OS) data come from the SOLO2 study and were described as “a significant advance” in a cancer “that has a historically poor prognosis” by Richard Schilsky, MD, senior vice president and chief medical officer of the American Society of Clinical Oncology.
The results were highlighted at a presscast prior to being presented during the virtual scientific program of the 2020 ASCO annual meeting (abstract 6002).
The SOLO2 study randomly assigned almost 300 women with relapsed BRCA-related ovarian cancer that was responding to platinum-based chemotherapy to maintenance therapy with either olaparib or placebo.
Earlier results from this study showed that olaparib was associated with an investigator-assessed progression-free survival (PFS) of 19.1 months, versus just 5.5 months with placebo, as previously reported by Medscape Medical News.
New data from this trial, presented by Andrés Poveda, MD, Initia Oncology, Hospital Quironsalud, in Valencia, Spain, show that olaparib improved median OS by 12.9 months compared to placebo (51.7 months with olaparib vs. 38.8 months with placebo; hazard ratio, 0.74; P = .054).
At 5 years’ follow-up, 42.1% of women taking olaparib were alive, versus 33.2% taking placebo.
In an ASCO press release, Poveda described the improvement in median OS with olaparib as “impressive” and that it offers a “substantial benefit to our patients.
“This study helps usher in a new era of personalized medicine for women with this difficult-to-treat cancer,” he added.
Poveda told reporters that this study is “the first randomized phase 3 trial to provide overall survival data for maintenance PARP inhibitors.
“The finding that 22% of patient in the olaparib group received the study treatment for more than 5 years is unprecedented in the setting of relapsed ovarian cancer,” he added.
The new OS data were welcomed by Konstantin Zakashansky, MD, director of gynecologic oncology at Mount Sinai West, New York, who was not involved in the study.
“PARP inhibitor trials have revolutionized therapy for ovarian cancer in the front line, as well as in the recurrent setting, [with] all of the recently presented trials showing significant improvement in progression free survival,” he said.
“Overall survival data, however, which is considered the most clinically relevant endpoint in oncology trials and remains the ‘gold standard’ because of its relevance and objectivity, have been limited,” he continued.
Zakashansky recalled that when the earlier PFS data from SOLO2 were presented, “questions were raised regarding the clinical uncertainty of the benefit associated with olaparib maintenance, primarily whether the PFS benefit...would translate to a long-term overall survival benefit.”
For him, the current results “answer that question” and offer the “largest improvement in overall survival of any recurrent ovarian cancer patient trial reported to date.”
Schilsky added that the new data confirm that olaparib “should be the standard maintenance therapy for patients with BRCA-related relapsed ovarian cancer responding to platinum-based chemotherapy.”
The drug is already approved for this indication, but the new data showing a significant survival benefit are “comforting” and “good news,” he said.
Adverse events with olaparib
Treatment-emergent adverse events seen in the study were “consistent with the known tolerability profile of olaparib,” Poveda commented.
The most common events of any grade were nausea, fatigue/asthenia, and anemia. The most common event of grade ≥3 was anemia.
Adverse events leading to dose interruptions occurred in 50% of patients who received olaparib and 19% of patients who took placebo. Adverse events leading to dose reductions occurred in 28% and 3%, respectively.
Treatment discontinuation because of adverse events was reported in 17% of patients given olaparib and 3% of those in the placebo arm.
The study was funded by AstraZeneca and Merck Sharp & Dohme. Poveda reports a consulting or advisory role with AstraZeneca, Clovis Oncology, PharmaMar, Roche, and Tesaro and receiving expenses from PharmaMar. Many coauthors also report relationships with pharmaceutical companies.
This article first appeared on Medscape.com.
Women with platinum-sensitive relapsed ovarian cancer and a BRCA mutation could see their survival extended by over a year by maintenance therapy with the PARP inhibitor olaparib (Lynparza, AstraZeneca).
The new overall survival (OS) data come from the SOLO2 study and were described as “a significant advance” in a cancer “that has a historically poor prognosis” by Richard Schilsky, MD, senior vice president and chief medical officer of the American Society of Clinical Oncology.
The results were highlighted at a presscast prior to being presented during the virtual scientific program of the 2020 ASCO annual meeting (abstract 6002).
The SOLO2 study randomly assigned almost 300 women with relapsed BRCA-related ovarian cancer that was responding to platinum-based chemotherapy to maintenance therapy with either olaparib or placebo.
Earlier results from this study showed that olaparib was associated with an investigator-assessed progression-free survival (PFS) of 19.1 months, versus just 5.5 months with placebo, as previously reported by Medscape Medical News.
New data from this trial, presented by Andrés Poveda, MD, Initia Oncology, Hospital Quironsalud, in Valencia, Spain, show that olaparib improved median OS by 12.9 months compared to placebo (51.7 months with olaparib vs. 38.8 months with placebo; hazard ratio, 0.74; P = .054).
At 5 years’ follow-up, 42.1% of women taking olaparib were alive, versus 33.2% taking placebo.
In an ASCO press release, Poveda described the improvement in median OS with olaparib as “impressive” and that it offers a “substantial benefit to our patients.
“This study helps usher in a new era of personalized medicine for women with this difficult-to-treat cancer,” he added.
Poveda told reporters that this study is “the first randomized phase 3 trial to provide overall survival data for maintenance PARP inhibitors.
“The finding that 22% of patient in the olaparib group received the study treatment for more than 5 years is unprecedented in the setting of relapsed ovarian cancer,” he added.
The new OS data were welcomed by Konstantin Zakashansky, MD, director of gynecologic oncology at Mount Sinai West, New York, who was not involved in the study.
“PARP inhibitor trials have revolutionized therapy for ovarian cancer in the front line, as well as in the recurrent setting, [with] all of the recently presented trials showing significant improvement in progression free survival,” he said.
“Overall survival data, however, which is considered the most clinically relevant endpoint in oncology trials and remains the ‘gold standard’ because of its relevance and objectivity, have been limited,” he continued.
Zakashansky recalled that when the earlier PFS data from SOLO2 were presented, “questions were raised regarding the clinical uncertainty of the benefit associated with olaparib maintenance, primarily whether the PFS benefit...would translate to a long-term overall survival benefit.”
For him, the current results “answer that question” and offer the “largest improvement in overall survival of any recurrent ovarian cancer patient trial reported to date.”
Schilsky added that the new data confirm that olaparib “should be the standard maintenance therapy for patients with BRCA-related relapsed ovarian cancer responding to platinum-based chemotherapy.”
The drug is already approved for this indication, but the new data showing a significant survival benefit are “comforting” and “good news,” he said.
Adverse events with olaparib
Treatment-emergent adverse events seen in the study were “consistent with the known tolerability profile of olaparib,” Poveda commented.
The most common events of any grade were nausea, fatigue/asthenia, and anemia. The most common event of grade ≥3 was anemia.
Adverse events leading to dose interruptions occurred in 50% of patients who received olaparib and 19% of patients who took placebo. Adverse events leading to dose reductions occurred in 28% and 3%, respectively.
Treatment discontinuation because of adverse events was reported in 17% of patients given olaparib and 3% of those in the placebo arm.
The study was funded by AstraZeneca and Merck Sharp & Dohme. Poveda reports a consulting or advisory role with AstraZeneca, Clovis Oncology, PharmaMar, Roche, and Tesaro and receiving expenses from PharmaMar. Many coauthors also report relationships with pharmaceutical companies.
This article first appeared on Medscape.com.
FROM ASCO 2020
COVID-19: Experts hasten to head off mental health crisis
The COVID-19 pandemic is already affecting mental health at a population level, with increased anxiety, feelings of isolation, and concerns about access to mental health care.
Two U.K. surveys were conducted to inform research priorities for mental health research and in an effort to head off a mental health crisis. The U.K. charity MQ conducted a “stakeholder” survey of 2,198 individuals who had a lived experience of mental illness, while Ipsos MORI conducted a poll of 1,099 members of the public.
The online surveys were conducted in late March, the same week the U.K.’s nationwide lockdown measures were announced. Respondents were asked about their biggest mental health and well-being concerns and coping strategies as they relate to the COVID-19 pandemic.
Results showed that across the two surveys, respondents’ primary concern was anxiety, which was cited in 750 responses.
In addition, respondents were worried about being social isolated, becoming mentally unwell, and having a lack of access to mental health services, as well as the impact of the pandemic on personal relationships.
The findings were used by a panel of experts to inform a position paper published in the Lancet Psychiatry. The paper outlines a proposed government response to curb the long-term “profound” and “pervasive” impact of the pandemic on mental health.
‘Unprecedented response’ needed
“Governments must find evidence-based ways to boost the resilience of our societies and ... to treat those with mental ill health remotely to come out of this pandemic in good mental health,” coauthor of the paper Emily A. Holmes, PhD, of the department of psychology at Uppsala (Sweden) University, said in a press release.
“Frontline medical staff and vulnerable groups such as the elderly and those with serious mental health conditions must be prioritized for rapid mental health support,” she added.
The position paper authors call for “moment-to-moment” monitoring of anxiety, depression, self-harm, and suicide, as well as using digital technology and rapid deployment of evidence-based programs and treatments.
Patients will need to be accessible via computer, cell phone, and other remote technologies in order to receive treatment during physical isolation. However, they noted that there is no “one-size-fits-all” approach, and novel approaches custom tailored to particular populations, including frontline health care workers, are necessary.
“To make a real difference we will need to harness the tools of our digital age, finding smart new ways to measure the mental health of individuals remotely, finding creative ways to boost resilience, and finding ways to treat people in their homes. This effort must be considered central to our global response to the pandemic,” coauthor Ed Bullmore, PhD, of the department of psychiatry at the University of Cambridge (England), said in a statement.
Dr. Bullmore added that it will take “unprecedented research response if we are to limit the negative consequences of this pandemic on the mental health of our society now and in the future.”
Most vulnerable will bear the brunt
During a webinar held to discuss the paper, Matthew Hotopf, PhD, of the Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, cautioned that society’s most vulnerable citizens will bear the brunt of the pandemic’s mental health consequences.
“These individuals often have unstable housing, unstable work, and are disadvantaged in terms of their physical health and their mental health,” with a “very significant gap” in life expectancy versus the rest of the population, he said. The COVID-19 pandemic will widen the gap between “the haves and the have nots.”
“People with established and significant mental disorders are one version of the ‘have nots’ but actually it applies to a lot of people,” said Dr. Hotopf, noting that his experience of lockdown is “very different” from that of someone “living in overcrowded, unstable accommodation, with kids running around and maybe a partner who has problems with anger control.”
The authors of the position paper noted that the COVID-19 pandemic highlights several important research priorities that need to be addressed in the coming weeks and months. These include:
- Understanding the effect of COVID-19 on risk of anxiety, depression, and other outcomes, such as self-harm and suicide
- Understanding how to create physical and social supports to ensure mental health in a climate of physical distancing
- Determining the mental health consequences of social isolation for vulnerable groups, and how can these be mitigated under pandemic conditions
- Understanding the mental health impact of media reporting of COVID-19 in traditional and social media
- Determining the best methods for promoting successful adherence to behavioral advice about COVID-19 while enabling mental well-being and minimizing distress
Another area highlighted by the experts is the potential for neuropsychiatric sequelae in individuals infected with COVID-19. They called for “experimental medicine studies to validate clinical biomarkers and repurpose new treatments for the potentially neurotoxic effects of the virus.”
The authors/investigators disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic is already affecting mental health at a population level, with increased anxiety, feelings of isolation, and concerns about access to mental health care.
Two U.K. surveys were conducted to inform research priorities for mental health research and in an effort to head off a mental health crisis. The U.K. charity MQ conducted a “stakeholder” survey of 2,198 individuals who had a lived experience of mental illness, while Ipsos MORI conducted a poll of 1,099 members of the public.
The online surveys were conducted in late March, the same week the U.K.’s nationwide lockdown measures were announced. Respondents were asked about their biggest mental health and well-being concerns and coping strategies as they relate to the COVID-19 pandemic.
Results showed that across the two surveys, respondents’ primary concern was anxiety, which was cited in 750 responses.
In addition, respondents were worried about being social isolated, becoming mentally unwell, and having a lack of access to mental health services, as well as the impact of the pandemic on personal relationships.
The findings were used by a panel of experts to inform a position paper published in the Lancet Psychiatry. The paper outlines a proposed government response to curb the long-term “profound” and “pervasive” impact of the pandemic on mental health.
‘Unprecedented response’ needed
“Governments must find evidence-based ways to boost the resilience of our societies and ... to treat those with mental ill health remotely to come out of this pandemic in good mental health,” coauthor of the paper Emily A. Holmes, PhD, of the department of psychology at Uppsala (Sweden) University, said in a press release.
“Frontline medical staff and vulnerable groups such as the elderly and those with serious mental health conditions must be prioritized for rapid mental health support,” she added.
The position paper authors call for “moment-to-moment” monitoring of anxiety, depression, self-harm, and suicide, as well as using digital technology and rapid deployment of evidence-based programs and treatments.
Patients will need to be accessible via computer, cell phone, and other remote technologies in order to receive treatment during physical isolation. However, they noted that there is no “one-size-fits-all” approach, and novel approaches custom tailored to particular populations, including frontline health care workers, are necessary.
“To make a real difference we will need to harness the tools of our digital age, finding smart new ways to measure the mental health of individuals remotely, finding creative ways to boost resilience, and finding ways to treat people in their homes. This effort must be considered central to our global response to the pandemic,” coauthor Ed Bullmore, PhD, of the department of psychiatry at the University of Cambridge (England), said in a statement.
Dr. Bullmore added that it will take “unprecedented research response if we are to limit the negative consequences of this pandemic on the mental health of our society now and in the future.”
Most vulnerable will bear the brunt
During a webinar held to discuss the paper, Matthew Hotopf, PhD, of the Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, cautioned that society’s most vulnerable citizens will bear the brunt of the pandemic’s mental health consequences.
“These individuals often have unstable housing, unstable work, and are disadvantaged in terms of their physical health and their mental health,” with a “very significant gap” in life expectancy versus the rest of the population, he said. The COVID-19 pandemic will widen the gap between “the haves and the have nots.”
“People with established and significant mental disorders are one version of the ‘have nots’ but actually it applies to a lot of people,” said Dr. Hotopf, noting that his experience of lockdown is “very different” from that of someone “living in overcrowded, unstable accommodation, with kids running around and maybe a partner who has problems with anger control.”
The authors of the position paper noted that the COVID-19 pandemic highlights several important research priorities that need to be addressed in the coming weeks and months. These include:
- Understanding the effect of COVID-19 on risk of anxiety, depression, and other outcomes, such as self-harm and suicide
- Understanding how to create physical and social supports to ensure mental health in a climate of physical distancing
- Determining the mental health consequences of social isolation for vulnerable groups, and how can these be mitigated under pandemic conditions
- Understanding the mental health impact of media reporting of COVID-19 in traditional and social media
- Determining the best methods for promoting successful adherence to behavioral advice about COVID-19 while enabling mental well-being and minimizing distress
Another area highlighted by the experts is the potential for neuropsychiatric sequelae in individuals infected with COVID-19. They called for “experimental medicine studies to validate clinical biomarkers and repurpose new treatments for the potentially neurotoxic effects of the virus.”
The authors/investigators disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic is already affecting mental health at a population level, with increased anxiety, feelings of isolation, and concerns about access to mental health care.
Two U.K. surveys were conducted to inform research priorities for mental health research and in an effort to head off a mental health crisis. The U.K. charity MQ conducted a “stakeholder” survey of 2,198 individuals who had a lived experience of mental illness, while Ipsos MORI conducted a poll of 1,099 members of the public.
The online surveys were conducted in late March, the same week the U.K.’s nationwide lockdown measures were announced. Respondents were asked about their biggest mental health and well-being concerns and coping strategies as they relate to the COVID-19 pandemic.
Results showed that across the two surveys, respondents’ primary concern was anxiety, which was cited in 750 responses.
In addition, respondents were worried about being social isolated, becoming mentally unwell, and having a lack of access to mental health services, as well as the impact of the pandemic on personal relationships.
The findings were used by a panel of experts to inform a position paper published in the Lancet Psychiatry. The paper outlines a proposed government response to curb the long-term “profound” and “pervasive” impact of the pandemic on mental health.
‘Unprecedented response’ needed
“Governments must find evidence-based ways to boost the resilience of our societies and ... to treat those with mental ill health remotely to come out of this pandemic in good mental health,” coauthor of the paper Emily A. Holmes, PhD, of the department of psychology at Uppsala (Sweden) University, said in a press release.
“Frontline medical staff and vulnerable groups such as the elderly and those with serious mental health conditions must be prioritized for rapid mental health support,” she added.
The position paper authors call for “moment-to-moment” monitoring of anxiety, depression, self-harm, and suicide, as well as using digital technology and rapid deployment of evidence-based programs and treatments.
Patients will need to be accessible via computer, cell phone, and other remote technologies in order to receive treatment during physical isolation. However, they noted that there is no “one-size-fits-all” approach, and novel approaches custom tailored to particular populations, including frontline health care workers, are necessary.
“To make a real difference we will need to harness the tools of our digital age, finding smart new ways to measure the mental health of individuals remotely, finding creative ways to boost resilience, and finding ways to treat people in their homes. This effort must be considered central to our global response to the pandemic,” coauthor Ed Bullmore, PhD, of the department of psychiatry at the University of Cambridge (England), said in a statement.
Dr. Bullmore added that it will take “unprecedented research response if we are to limit the negative consequences of this pandemic on the mental health of our society now and in the future.”
Most vulnerable will bear the brunt
During a webinar held to discuss the paper, Matthew Hotopf, PhD, of the Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, cautioned that society’s most vulnerable citizens will bear the brunt of the pandemic’s mental health consequences.
“These individuals often have unstable housing, unstable work, and are disadvantaged in terms of their physical health and their mental health,” with a “very significant gap” in life expectancy versus the rest of the population, he said. The COVID-19 pandemic will widen the gap between “the haves and the have nots.”
“People with established and significant mental disorders are one version of the ‘have nots’ but actually it applies to a lot of people,” said Dr. Hotopf, noting that his experience of lockdown is “very different” from that of someone “living in overcrowded, unstable accommodation, with kids running around and maybe a partner who has problems with anger control.”
The authors of the position paper noted that the COVID-19 pandemic highlights several important research priorities that need to be addressed in the coming weeks and months. These include:
- Understanding the effect of COVID-19 on risk of anxiety, depression, and other outcomes, such as self-harm and suicide
- Understanding how to create physical and social supports to ensure mental health in a climate of physical distancing
- Determining the mental health consequences of social isolation for vulnerable groups, and how can these be mitigated under pandemic conditions
- Understanding the mental health impact of media reporting of COVID-19 in traditional and social media
- Determining the best methods for promoting successful adherence to behavioral advice about COVID-19 while enabling mental well-being and minimizing distress
Another area highlighted by the experts is the potential for neuropsychiatric sequelae in individuals infected with COVID-19. They called for “experimental medicine studies to validate clinical biomarkers and repurpose new treatments for the potentially neurotoxic effects of the virus.”
The authors/investigators disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Obesity link to severe COVID-19, especially in patients aged under 60
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.

