User login
Teens with PID underscreened for HIV, syphilis
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
CHICAGO – Adolescents with pelvic inflammatory disease (PID) were unlikely to be screened for HIV or syphilis, and many didn’t receive an appropriate antibiotic regimen, according to a recent study reported at the annual meeting of the American Academy of Pediatrics.
Patients who were sent home rather than admitted were especially likely to miss screening, as were Hispanic patients and those with private insurance.
The Centers for Disease Control and Prevention strongly recommends that all women diagnosed with PID be tested for HIV, and that high-risk individuals also be tested for syphilis, wrote Amanda Jichlinski, MD, and her coauthors at Children’s National Health System, Washington.
The study, presented during a poster session, used data from the national Pediatric Health Information System database from 2010 to 2015. A total of 10,698 records with a diagnostic code for PID were included; patients were females aged 12-21 years seen in a pediatric emergency department.
In addition to the primary outcome of syphilis and HIV testing, the authors also looked at whether antibiotic administration for PID was in line with CDC recommendations – and it wasn’t. “Fewer than half of patients in the ED received antibiotic regimens adherent to CDC guidelines,” wrote Dr. Jichlinski and her coauthors.
Forty-six percent of patients received ceftriaxone and doxycycline, 21% received ceftriaxone and azithromycin, and 6% received ceftriaxone and metronidazole. Ceftriaxone monotherapy was given to 15% of patients. One in 10 patients with a PID diagnosis received no antibiotic at all; 2% of patients received some other regimen.
The researchers used multivariable analysis to examine separately which patient and hospital characteristics were associated with an increased likelihood of testing for both HIV and syphilis. With white, non-Hispanic adolescents used as the referent, Hispanic females with PID were less likely to receive screening for either HIV or syphilis (adjusted odds ratio, 0.8 for both; 95% confidence interval, 0.7-1.0 for both).
In contrast, black non-Hispanic females were screened more often; the aOR for HIV screening was 1.4 (95% CI, 1.2-1.6), and the aOR for syphilis screening was 1.8 (95% CI, 1.6-2.0) for this group of adolescents.
Patients were dichotomized into older (17-21 years of age; n = 4,737, 44%) and younger (12-16 years of age; n = 5,961, 56%) age groups; younger patients were slightly more likely to receive HIV (aOR, 1.2) and syphilis (aOR, 1.1) screening.
Just under a third of patients in the study were seen in a hospital with fewer than 300 beds, and these facilities were more likely to screen for HIV (aOR, 1.4) and syphilis (aOR, 1.1) than the larger hospitals.
By far the largest predictor of whether HIV and syphilis screening was done, though, was a hospital admission. Patients who were admitted (n = 4,043, 38%) were 7 times more likely to be screened for HIV and 4.6 times more likely to be screened for syphilis than those who were sent home from the emergency department.
Although the large, nationally representative study had many strengths, Dr. Jichlinski and her coauthors acknowledged that the data they were provided couldn’t account for medication that was prescribed, rather than administered in the emergency department. Also, the results may not be generalizable to adolescents treated in nonpediatric emergency departments or other facilities, such as urgent care centers.
“Adolescents with PID are underscreened for HIV and syphilis,” wrote Dr. Jichlinski and her coauthors. They called for pediatricians to receive more education about management of PID in adolescents. From a practical perspective, the investigators also suggested incorporating order sets for sexually transmitted infection testing and antibiotic administration into electronic medical records; in this way, a PID diagnosis code would trigger simplified testing and treatment choices.
Dr. Jichlinski reported no conflicts of interest. Dr. Monika Goyal, MD, senior author on the study, reported funding support by the National Institute of Child Health and Human Development. Dr. Goyal also holds an appointment at the George Washington University, Washington.
SOURCE: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine.
REPORTING FROM AAP 2017
Key clinical point:
Major finding: Hispanic females were least likely to be screened (adjusted OR, 0.8), compared with non-Hispanic white females.
Study details: Retrospective study of 10,698 adolescent patients with PID from a national database.
Disclosures: The study was funded in part by the National Institute of Child Health and Development. The authors had no relevant financial disclosures.
Source: Jichlinski A et al. AAP 2017 Abstract 5, AAP Section on Emergency Medicine
Unplanned cesareans more common with excess gestational weight gain
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
REPORTING FROM NAPCRG 2017
Key clinical point: The risk for an unplanned cesarean delivery rose with excess gestational weight gain.
Major finding: The adjusted odds ratio for unplanned cesarean was 1.61 for those with excess GWG (P = .013).
Study details: Retrospective analysis of 2,107 responses to the Infant Feeding Practices Study II (IFPSII).
Disclosures: Study data were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
Source: Francescon J. NAPCRG 2017 Abstract P495.
Length of stay shorter with admission to family medicine, not hospitalist, service
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
REPORTING FROM NAPCRG 2017
Key clinical point: Patients’ length of stay was shorter when they were cared for by family medicine doctors and not hospitalists.
Major finding: After multivariable analysis, the adjusted length of stay was 31.8% longer for patients on the hospitalist service than on the family medicine inpatient service.
Study details: A retrospective review of records from 3,125 admissions of 2,138 patients.
Disclosures: Dr. Garrison reported no conflicts of interest and no outside sources of funding.
Source: Garrison G et al. NAPCRG 2017 Abstract AE32.
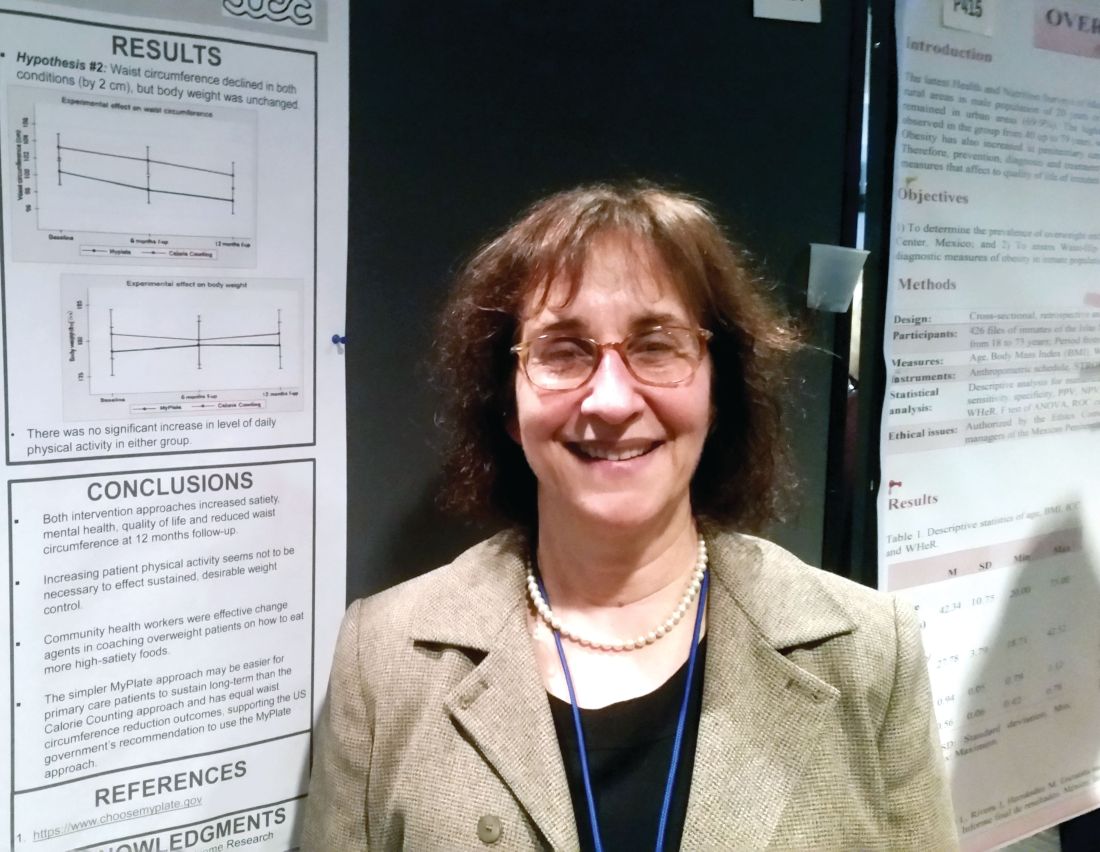
MyPlate as effective as calorie counting after 12 months
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
REPORTING FROM NAPCRG 2017
Key clinical point:
Major finding: At 12 months, both approaches reduced waist circumference by 2 cm but didn’t result in weight loss.
Data source: Prospective randomized comparative effectiveness trial of 261 patients.
Disclosures: Dr. Gelberg reported no conflicts of interest. The study was funded by the Patient-Centered Comparative Effectiveness Institute.
Source: Gelberg L, abstract P414.
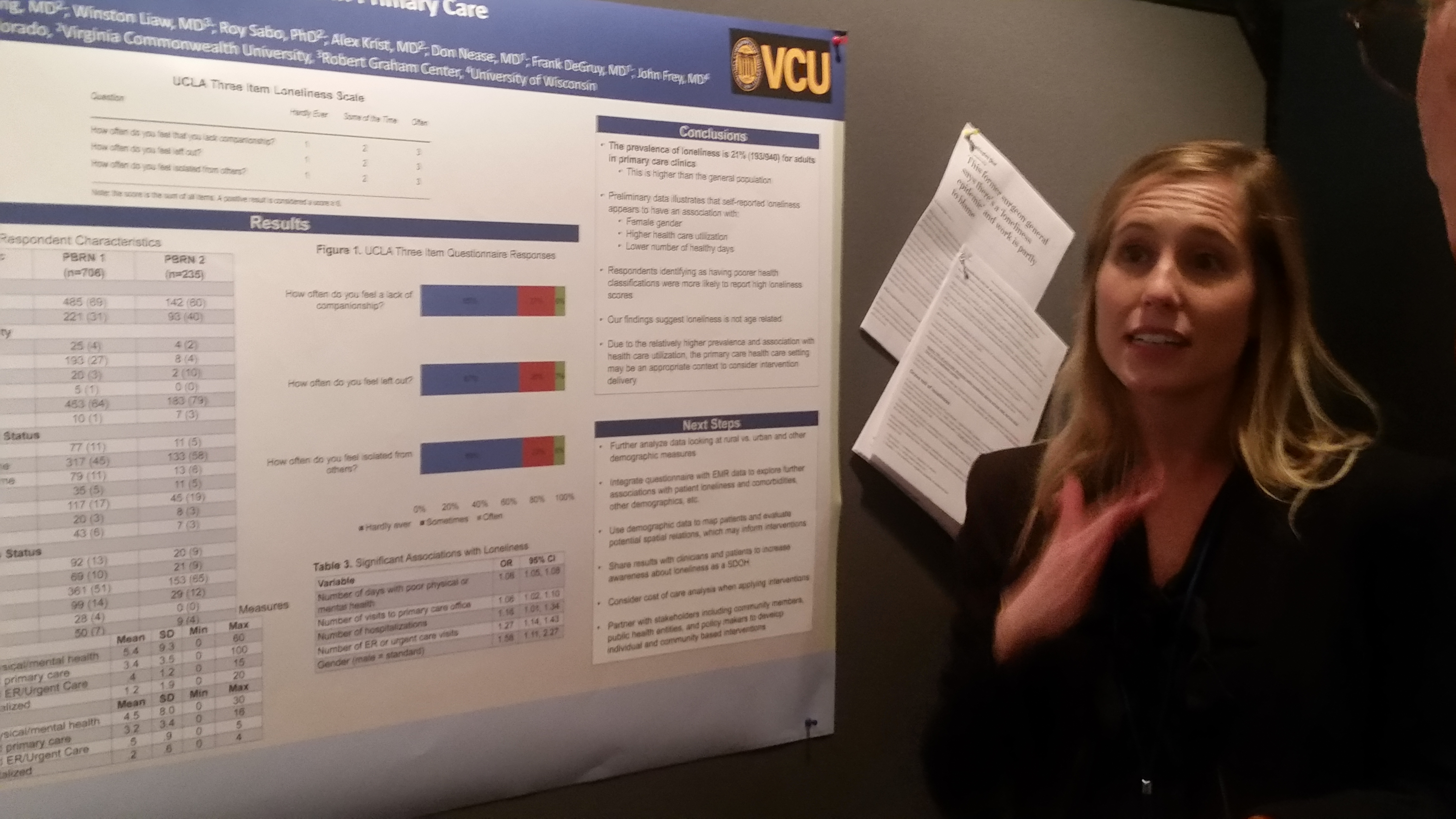
Loneliness is common, and not just in the elderly
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
REPORTING FROM NAPCRG 2017
Key clinical point: One in five adults – and more women than men – reported loneliness.
Major finding: Of 940 adults surveyed, 193 (21%) reported being lonely.
Study details: A prospective survey of 940 adults seeking care in primary care clinics.
Disclosures: Dr. Mullen reported no relevant financial conflicts of interest.
Bright Futures 4th Edition gets a clinical refresher
CHICAGO – Bracing his audience for a whirlwind tour of the many updates to the fourth edition of Bright Futures, Joseph F. Hagan Jr., MD, said that it’s still completely possible to fit Bright Futures visits into a clinic day.
“I practice primary care pediatrics,” said Dr. Hagan, a pediatrician in private practice and clinical professor of pediatrics at the University of Vermont, both in Burlington. “I said to my Bright Futures colleagues, if I didn’t think I could do this in 18 minutes, I wouldn’t ask you to do it.”
The Bright Futures framework, described by Dr. Hagan as the health prevention and disease prevention component of the medical home for children and youth, emerges in the Fourth Edition with a significant evidence-based refresher. The changes and updates are built within the existing framework and encompass surveillance and screening recommendations as well as anticipatory guidance. All content, including family handouts, has been updated, said Dr. Hagan, a coeditor of the Fourth Edition of Bright Futures. He spoke at the annual meeting of the American Academy of Pediatrics.
New clinical content
“What’s new? Maternal depression screening is new,” said Dr. Hagan, noting that the recommendation has long been under discussion. Now, supported by a 2016 United States Preventative Task Force (USPSTF) recommendation that carries a grade B level of evidence, all mothers should be screened for depression at the 1-, 2-, 4-, and 6-month Bright Futures visits.
However, he said, know your local regulations. “State mandates to do more might overrule this.” And conversely, “Just because we’re doing it universally until 6 months doesn’t mean you couldn’t selectively screen later if you have concerns.”
Safe sleep is another area with new clinical focus, he said. The new recommendation for the child to sleep in the parent’s room for “at least 6 months” draws on data from European studies showing lower mortality for children who share a room with parents during this period.
Clinicians should continue to recommend that parents not sleep with their infants in couches, chairs, or beds. As before, parents should be told not to have loose blankets, stuffed toys, or crib bumpers in their babies’ cribs. Another key message, said Dr. Hagan, is that “There is no such thing as safe ‘breast-sleeping.’ ”
Parents should be reminded not to swaddle at nap – or bedtime. The risk is that even a 2-month-old infant may be capable of wriggling over from back to front, and a swaddled infant whose hands are trapped may not be able to move to protect her airway once prone. “Swaddle for comfort, swaddle for crying, swaddle for nursing, but don’t swaddle for sleep” is the message, said Dr. Hagan.
For breast-fed babies, iron supplementation should begin at the 4-month visit. The notion is to prevent progression from iron deficiency to frank anemia, said Dr. Hagan. “We know that we screen for iron deficiency anemia … but we also know that before you’re iron deficient anemic, you’re iron deficient,” he said, and iron’s also critical to brain development. For convenience, switching from vitamin D alone to a multivitamin drop with iron at 4 months is a practical choice.
New dental health recommendations bring prevention to the pediatrician’s office. “Fluoride varnish? Do it!” said Dr. Hagan. Although the USPSTF made a 2014 grade B recommendation that primary care clinicians apply fluoride varnish to primary teeth as soon as they erupt, “It’s new to the Bright Futures periodicity schedule,” he said; parents can be assured that fluoride varnish does not cause fluorosis.
The good news for clinicians, he noted. “Once it hits the periodicity schedule, now, it’s a billable service that must be paid” under Affordable Care Act regulations, said Dr. Hagan. “Don’t let your insurer say, ‘That’s part of what you’re already being paid for.’ ” He recommends avoiding the pressure to bundle this important service. Use the discrete CPT code 99188, “Application of a fluoride varnish by a physician or other qualified health care professional.”
Although Bright Futures has updated recommendations for dyslipidemia blood screening, the USPSTF found insufficient evidence to back lipid screening for those younger than 20 years of age, citing an inability to assess the balance of benefits and harms for universal, rather than risk-based, screening. However, said Dr. Hagan, the American Academy of Pediatrics (AAP), and the National Heart, Lung, and Blood Institute (NHLBI) were looking at this issue at about the same time, and they “did a really good job of showing their work,” to show that if family history alone guided screening in the pediatric population, it “just wasn’t getting done.” And AAP and NHLBI did demonstrate evidence sufficient to support this recommendation.
Accordingly, Bright Futures recommends one screening between ages 9 and 11 years and an additional screening between ages 17 and 21. These windows are designed to bracket puberty, said Dr. Hagan, because values can be skewed during that period. “It’s billable, it’s not bundle-able, and I’d recommend that you do it,” he said.
Developmental surveillance and screening
What’s new with developmental surveillance and screening? “Well, we could argue that the milestones are something to think about, because the milestones are the cornerstone of developmental surveillance,” said Dr. Hagan. “You’re in the room with the child. You’re trained, you’re experienced, you’re smart, your gestalt tells you if their development is good or bad.”
As important as surveillance is, though, he said, it is “nowhere near as important as screening.” Surveillance happens at every well-child visit, but there’s no substitute for formal developmental screening. For the Fourth Edition guidance and toolkit, gross motor milestones have been adjusted to reflect what’s really being seen as more parents adopt the Back to Sleep recommendations as well.
A standardized developmental screening tool is used at the 9-, 18-, and 30-month visits, and when parents or caregivers express concern about development. Autism-specific screening happens at 18 and 24 months.
“Remember this, if you remember nothing else: If the screening is positive, and you believe there’s a problem, you’re going to refer,” not just to the appropriate specialist but also for early intervention services, so time isn’t lost as the child is waiting for further evaluation and a formal diagnosis, said Dr. Hagan. This coordinated effort appropriately places the responsibility for early identification of developmental delays and disorders at the doorstep of the child’s medical home.
The federally-coordinated Birth to 5: Watch Me Thrive! effort has aggregated research-based screening tools, users’ guides targeted at a variety of audiences, and resources to help caregivers, said Dr. Hagan.
Four commonly-used tools to consider using during the visit are the Parents’ Evaluation of Developmental Status, the Ages and Stages Questionnaire, the Child Health and Development Interactive System, and the Survey of Wellbeing of Young Children. Of these, said Dr. Hagan, the latter is the only tool that’s in the public domain. However, he said, they are “all really good.”
Consider having parents fill out screening questionnaires in the waiting room before the visit, said Dr. Hagan. “I always tell my colleagues, ‘Have them start the visit without you, if you want to get it done in 18 minutes.’ ”
Two questionnaires per visit are available in the Bright Futures toolkit. One questionnaire asks developmental surveillance and risk assessment questions for selective screening. The second questionnaire asks prescreening questions to help with the anticipatory guidance part of the visit, he said. Having families do these ahead of time, said Dr. Hagan, “allows you to become more focused.”
Paying attention to practicalities can make all this go more smoothly, and maximize reimbursement as well. In his own practice, Dr. Hagan said, screening tools and questionnaires are integrated into the EHR system, so that appropriate paperwork prints automatically ahead of the visit.
It’s also worth reviewing billing practices to make sure that CPT code 96110 is used when administering screening with a standardized instrument and completing scoring and documentation. According to the Bright Futures periodicity schedule, this may be done at the 9-, 18-, and 30-month visits for developmental screening, as well as at 18 and 24 months for autism-specific screening.
Promoting lifelong health
Since the initial Bright Futures guidelines were published in the late 1990s, said Dr. Hagan, the focus has always been on seeing the child as part of the family, who, in turn, are part of the community, forming a framework that addresses the social components of child health. “If you’re not looking at the whole picture, you’re not promoting health,” he said. “It’s no big surprise that we now have a specific, called-out focus on promoting lifelong health.”
In the Fourth Edition, the theme of promoting lifelong health for families and communities is woven throughout, with social determinants of health being a specific visit priority. For example, questions about food insecurity have been drawn from the published literature and are included. Also, said Dr. Hagan, there’s specific anticipatory guidance content that’s clearly marked as addressing social determinants of health.
The fundamental importance of socioeconomic status as a social determinant of health was brought home by the Robert Wood Johnson Foundation’s Commission to Build a Healthier America, which demonstrated that, “Your ZIP code is more important to your health than your genetic code,” said Dr. Hagan. “So your work in health supervision is important, and you have been leaders in this effort.”
Research guides Bright Futures updates
The fourth edition of Bright Futures builds on health promotion themes to support the mental and physical health of children and adolescents, and has a robust framework of evidence underpinning the guidelines, said Dr. Hagan.
The goal is for clinicians to “use evidence to decide upon content of their own health supervision visits,” he explained.
The chapter of the Bright Futures guidelines that addresses the evidence and rationale for the guidelines has been expanded to better answer two questions, said Dr. Hagan: “What evidence grounds our recommendations?” and “What rationale did we use when evidence was insufficient or lacking?”
When possible, the editors of the guidelines used evidence-based sources such as recommendations from the USPSTF, the Centers for Disease Control Community Guide, and the Cochrane Collaboration.
There were many more evidence-based recommendations available to those working on the 4th edition than there had been when writing the previous edition, when, said Dr. Hagan, the USPSTF had exactly two recommendations for those under the age of 21 years. The current expanded number of USPSTF pediatric recommendations was due in part to the attention the AAP was able to bring regarding the need for evidence-based recommendations in pediatrics, he said.
When guidelines were not available, the editors also turned to high quality studies from peer reviewed publications. When such high quality evidence was lacking in a particular area, the guidelines make clear what rationale was used to formulate a given recommendation, and that some recommendations should be interpreted with a degree of caution.
And, said Dr. Hagan, even science-based guidelines will change as more data accumulates. “Don’t forget about peanuts!” he said. “It was really logical 15 years ago when we said don’t give peanut products until 1 year of age. And about 2 years ago, we found out that it really didn’t work.”
Although there are specific updates to clinical content, there also were changes made in broader strokes throughout the 4th edition. One of these shifts embeds social determinants of health in many visits. This adjustment acknowledges the growing body of knowledge that “strengths and protective factors make a difference, and risk factors make a difference” in pediatric outcomes.
A greater focus on lifelong physical and mental health is included under the general rubric of promoting lifelong health for families and communities. More emphasis is placed on promoting health for children and youth who have special health care needs as well.
Nuts-and-bolts changes in the updated 4th edition include updates for milestones of development and accompanying developmental surveillance questions, new clinical content and guidance for implementation that have been added based on strong evidence, and a variety of updates for adolescent screenings in particular.
The full 4th edition Bright Futures toolkit will be available for use in 2018.
Dr. Hagan was a coeditor of the Fourth Edition of Bright Futures.
*This article was updated on December 21, 2017
CHICAGO – Bracing his audience for a whirlwind tour of the many updates to the fourth edition of Bright Futures, Joseph F. Hagan Jr., MD, said that it’s still completely possible to fit Bright Futures visits into a clinic day.
“I practice primary care pediatrics,” said Dr. Hagan, a pediatrician in private practice and clinical professor of pediatrics at the University of Vermont, both in Burlington. “I said to my Bright Futures colleagues, if I didn’t think I could do this in 18 minutes, I wouldn’t ask you to do it.”
The Bright Futures framework, described by Dr. Hagan as the health prevention and disease prevention component of the medical home for children and youth, emerges in the Fourth Edition with a significant evidence-based refresher. The changes and updates are built within the existing framework and encompass surveillance and screening recommendations as well as anticipatory guidance. All content, including family handouts, has been updated, said Dr. Hagan, a coeditor of the Fourth Edition of Bright Futures. He spoke at the annual meeting of the American Academy of Pediatrics.
New clinical content
“What’s new? Maternal depression screening is new,” said Dr. Hagan, noting that the recommendation has long been under discussion. Now, supported by a 2016 United States Preventative Task Force (USPSTF) recommendation that carries a grade B level of evidence, all mothers should be screened for depression at the 1-, 2-, 4-, and 6-month Bright Futures visits.
However, he said, know your local regulations. “State mandates to do more might overrule this.” And conversely, “Just because we’re doing it universally until 6 months doesn’t mean you couldn’t selectively screen later if you have concerns.”
Safe sleep is another area with new clinical focus, he said. The new recommendation for the child to sleep in the parent’s room for “at least 6 months” draws on data from European studies showing lower mortality for children who share a room with parents during this period.
Clinicians should continue to recommend that parents not sleep with their infants in couches, chairs, or beds. As before, parents should be told not to have loose blankets, stuffed toys, or crib bumpers in their babies’ cribs. Another key message, said Dr. Hagan, is that “There is no such thing as safe ‘breast-sleeping.’ ”
Parents should be reminded not to swaddle at nap – or bedtime. The risk is that even a 2-month-old infant may be capable of wriggling over from back to front, and a swaddled infant whose hands are trapped may not be able to move to protect her airway once prone. “Swaddle for comfort, swaddle for crying, swaddle for nursing, but don’t swaddle for sleep” is the message, said Dr. Hagan.
For breast-fed babies, iron supplementation should begin at the 4-month visit. The notion is to prevent progression from iron deficiency to frank anemia, said Dr. Hagan. “We know that we screen for iron deficiency anemia … but we also know that before you’re iron deficient anemic, you’re iron deficient,” he said, and iron’s also critical to brain development. For convenience, switching from vitamin D alone to a multivitamin drop with iron at 4 months is a practical choice.
New dental health recommendations bring prevention to the pediatrician’s office. “Fluoride varnish? Do it!” said Dr. Hagan. Although the USPSTF made a 2014 grade B recommendation that primary care clinicians apply fluoride varnish to primary teeth as soon as they erupt, “It’s new to the Bright Futures periodicity schedule,” he said; parents can be assured that fluoride varnish does not cause fluorosis.
The good news for clinicians, he noted. “Once it hits the periodicity schedule, now, it’s a billable service that must be paid” under Affordable Care Act regulations, said Dr. Hagan. “Don’t let your insurer say, ‘That’s part of what you’re already being paid for.’ ” He recommends avoiding the pressure to bundle this important service. Use the discrete CPT code 99188, “Application of a fluoride varnish by a physician or other qualified health care professional.”
Although Bright Futures has updated recommendations for dyslipidemia blood screening, the USPSTF found insufficient evidence to back lipid screening for those younger than 20 years of age, citing an inability to assess the balance of benefits and harms for universal, rather than risk-based, screening. However, said Dr. Hagan, the American Academy of Pediatrics (AAP), and the National Heart, Lung, and Blood Institute (NHLBI) were looking at this issue at about the same time, and they “did a really good job of showing their work,” to show that if family history alone guided screening in the pediatric population, it “just wasn’t getting done.” And AAP and NHLBI did demonstrate evidence sufficient to support this recommendation.
Accordingly, Bright Futures recommends one screening between ages 9 and 11 years and an additional screening between ages 17 and 21. These windows are designed to bracket puberty, said Dr. Hagan, because values can be skewed during that period. “It’s billable, it’s not bundle-able, and I’d recommend that you do it,” he said.
Developmental surveillance and screening
What’s new with developmental surveillance and screening? “Well, we could argue that the milestones are something to think about, because the milestones are the cornerstone of developmental surveillance,” said Dr. Hagan. “You’re in the room with the child. You’re trained, you’re experienced, you’re smart, your gestalt tells you if their development is good or bad.”
As important as surveillance is, though, he said, it is “nowhere near as important as screening.” Surveillance happens at every well-child visit, but there’s no substitute for formal developmental screening. For the Fourth Edition guidance and toolkit, gross motor milestones have been adjusted to reflect what’s really being seen as more parents adopt the Back to Sleep recommendations as well.
A standardized developmental screening tool is used at the 9-, 18-, and 30-month visits, and when parents or caregivers express concern about development. Autism-specific screening happens at 18 and 24 months.
“Remember this, if you remember nothing else: If the screening is positive, and you believe there’s a problem, you’re going to refer,” not just to the appropriate specialist but also for early intervention services, so time isn’t lost as the child is waiting for further evaluation and a formal diagnosis, said Dr. Hagan. This coordinated effort appropriately places the responsibility for early identification of developmental delays and disorders at the doorstep of the child’s medical home.
The federally-coordinated Birth to 5: Watch Me Thrive! effort has aggregated research-based screening tools, users’ guides targeted at a variety of audiences, and resources to help caregivers, said Dr. Hagan.
Four commonly-used tools to consider using during the visit are the Parents’ Evaluation of Developmental Status, the Ages and Stages Questionnaire, the Child Health and Development Interactive System, and the Survey of Wellbeing of Young Children. Of these, said Dr. Hagan, the latter is the only tool that’s in the public domain. However, he said, they are “all really good.”
Consider having parents fill out screening questionnaires in the waiting room before the visit, said Dr. Hagan. “I always tell my colleagues, ‘Have them start the visit without you, if you want to get it done in 18 minutes.’ ”
Two questionnaires per visit are available in the Bright Futures toolkit. One questionnaire asks developmental surveillance and risk assessment questions for selective screening. The second questionnaire asks prescreening questions to help with the anticipatory guidance part of the visit, he said. Having families do these ahead of time, said Dr. Hagan, “allows you to become more focused.”
Paying attention to practicalities can make all this go more smoothly, and maximize reimbursement as well. In his own practice, Dr. Hagan said, screening tools and questionnaires are integrated into the EHR system, so that appropriate paperwork prints automatically ahead of the visit.
It’s also worth reviewing billing practices to make sure that CPT code 96110 is used when administering screening with a standardized instrument and completing scoring and documentation. According to the Bright Futures periodicity schedule, this may be done at the 9-, 18-, and 30-month visits for developmental screening, as well as at 18 and 24 months for autism-specific screening.
Promoting lifelong health
Since the initial Bright Futures guidelines were published in the late 1990s, said Dr. Hagan, the focus has always been on seeing the child as part of the family, who, in turn, are part of the community, forming a framework that addresses the social components of child health. “If you’re not looking at the whole picture, you’re not promoting health,” he said. “It’s no big surprise that we now have a specific, called-out focus on promoting lifelong health.”
In the Fourth Edition, the theme of promoting lifelong health for families and communities is woven throughout, with social determinants of health being a specific visit priority. For example, questions about food insecurity have been drawn from the published literature and are included. Also, said Dr. Hagan, there’s specific anticipatory guidance content that’s clearly marked as addressing social determinants of health.
The fundamental importance of socioeconomic status as a social determinant of health was brought home by the Robert Wood Johnson Foundation’s Commission to Build a Healthier America, which demonstrated that, “Your ZIP code is more important to your health than your genetic code,” said Dr. Hagan. “So your work in health supervision is important, and you have been leaders in this effort.”
Research guides Bright Futures updates
The fourth edition of Bright Futures builds on health promotion themes to support the mental and physical health of children and adolescents, and has a robust framework of evidence underpinning the guidelines, said Dr. Hagan.
The goal is for clinicians to “use evidence to decide upon content of their own health supervision visits,” he explained.
The chapter of the Bright Futures guidelines that addresses the evidence and rationale for the guidelines has been expanded to better answer two questions, said Dr. Hagan: “What evidence grounds our recommendations?” and “What rationale did we use when evidence was insufficient or lacking?”
When possible, the editors of the guidelines used evidence-based sources such as recommendations from the USPSTF, the Centers for Disease Control Community Guide, and the Cochrane Collaboration.
There were many more evidence-based recommendations available to those working on the 4th edition than there had been when writing the previous edition, when, said Dr. Hagan, the USPSTF had exactly two recommendations for those under the age of 21 years. The current expanded number of USPSTF pediatric recommendations was due in part to the attention the AAP was able to bring regarding the need for evidence-based recommendations in pediatrics, he said.
When guidelines were not available, the editors also turned to high quality studies from peer reviewed publications. When such high quality evidence was lacking in a particular area, the guidelines make clear what rationale was used to formulate a given recommendation, and that some recommendations should be interpreted with a degree of caution.
And, said Dr. Hagan, even science-based guidelines will change as more data accumulates. “Don’t forget about peanuts!” he said. “It was really logical 15 years ago when we said don’t give peanut products until 1 year of age. And about 2 years ago, we found out that it really didn’t work.”
Although there are specific updates to clinical content, there also were changes made in broader strokes throughout the 4th edition. One of these shifts embeds social determinants of health in many visits. This adjustment acknowledges the growing body of knowledge that “strengths and protective factors make a difference, and risk factors make a difference” in pediatric outcomes.
A greater focus on lifelong physical and mental health is included under the general rubric of promoting lifelong health for families and communities. More emphasis is placed on promoting health for children and youth who have special health care needs as well.
Nuts-and-bolts changes in the updated 4th edition include updates for milestones of development and accompanying developmental surveillance questions, new clinical content and guidance for implementation that have been added based on strong evidence, and a variety of updates for adolescent screenings in particular.
The full 4th edition Bright Futures toolkit will be available for use in 2018.
Dr. Hagan was a coeditor of the Fourth Edition of Bright Futures.
*This article was updated on December 21, 2017
CHICAGO – Bracing his audience for a whirlwind tour of the many updates to the fourth edition of Bright Futures, Joseph F. Hagan Jr., MD, said that it’s still completely possible to fit Bright Futures visits into a clinic day.
“I practice primary care pediatrics,” said Dr. Hagan, a pediatrician in private practice and clinical professor of pediatrics at the University of Vermont, both in Burlington. “I said to my Bright Futures colleagues, if I didn’t think I could do this in 18 minutes, I wouldn’t ask you to do it.”
The Bright Futures framework, described by Dr. Hagan as the health prevention and disease prevention component of the medical home for children and youth, emerges in the Fourth Edition with a significant evidence-based refresher. The changes and updates are built within the existing framework and encompass surveillance and screening recommendations as well as anticipatory guidance. All content, including family handouts, has been updated, said Dr. Hagan, a coeditor of the Fourth Edition of Bright Futures. He spoke at the annual meeting of the American Academy of Pediatrics.
New clinical content
“What’s new? Maternal depression screening is new,” said Dr. Hagan, noting that the recommendation has long been under discussion. Now, supported by a 2016 United States Preventative Task Force (USPSTF) recommendation that carries a grade B level of evidence, all mothers should be screened for depression at the 1-, 2-, 4-, and 6-month Bright Futures visits.
However, he said, know your local regulations. “State mandates to do more might overrule this.” And conversely, “Just because we’re doing it universally until 6 months doesn’t mean you couldn’t selectively screen later if you have concerns.”
Safe sleep is another area with new clinical focus, he said. The new recommendation for the child to sleep in the parent’s room for “at least 6 months” draws on data from European studies showing lower mortality for children who share a room with parents during this period.
Clinicians should continue to recommend that parents not sleep with their infants in couches, chairs, or beds. As before, parents should be told not to have loose blankets, stuffed toys, or crib bumpers in their babies’ cribs. Another key message, said Dr. Hagan, is that “There is no such thing as safe ‘breast-sleeping.’ ”
Parents should be reminded not to swaddle at nap – or bedtime. The risk is that even a 2-month-old infant may be capable of wriggling over from back to front, and a swaddled infant whose hands are trapped may not be able to move to protect her airway once prone. “Swaddle for comfort, swaddle for crying, swaddle for nursing, but don’t swaddle for sleep” is the message, said Dr. Hagan.
For breast-fed babies, iron supplementation should begin at the 4-month visit. The notion is to prevent progression from iron deficiency to frank anemia, said Dr. Hagan. “We know that we screen for iron deficiency anemia … but we also know that before you’re iron deficient anemic, you’re iron deficient,” he said, and iron’s also critical to brain development. For convenience, switching from vitamin D alone to a multivitamin drop with iron at 4 months is a practical choice.
New dental health recommendations bring prevention to the pediatrician’s office. “Fluoride varnish? Do it!” said Dr. Hagan. Although the USPSTF made a 2014 grade B recommendation that primary care clinicians apply fluoride varnish to primary teeth as soon as they erupt, “It’s new to the Bright Futures periodicity schedule,” he said; parents can be assured that fluoride varnish does not cause fluorosis.
The good news for clinicians, he noted. “Once it hits the periodicity schedule, now, it’s a billable service that must be paid” under Affordable Care Act regulations, said Dr. Hagan. “Don’t let your insurer say, ‘That’s part of what you’re already being paid for.’ ” He recommends avoiding the pressure to bundle this important service. Use the discrete CPT code 99188, “Application of a fluoride varnish by a physician or other qualified health care professional.”
Although Bright Futures has updated recommendations for dyslipidemia blood screening, the USPSTF found insufficient evidence to back lipid screening for those younger than 20 years of age, citing an inability to assess the balance of benefits and harms for universal, rather than risk-based, screening. However, said Dr. Hagan, the American Academy of Pediatrics (AAP), and the National Heart, Lung, and Blood Institute (NHLBI) were looking at this issue at about the same time, and they “did a really good job of showing their work,” to show that if family history alone guided screening in the pediatric population, it “just wasn’t getting done.” And AAP and NHLBI did demonstrate evidence sufficient to support this recommendation.
Accordingly, Bright Futures recommends one screening between ages 9 and 11 years and an additional screening between ages 17 and 21. These windows are designed to bracket puberty, said Dr. Hagan, because values can be skewed during that period. “It’s billable, it’s not bundle-able, and I’d recommend that you do it,” he said.
Developmental surveillance and screening
What’s new with developmental surveillance and screening? “Well, we could argue that the milestones are something to think about, because the milestones are the cornerstone of developmental surveillance,” said Dr. Hagan. “You’re in the room with the child. You’re trained, you’re experienced, you’re smart, your gestalt tells you if their development is good or bad.”
As important as surveillance is, though, he said, it is “nowhere near as important as screening.” Surveillance happens at every well-child visit, but there’s no substitute for formal developmental screening. For the Fourth Edition guidance and toolkit, gross motor milestones have been adjusted to reflect what’s really being seen as more parents adopt the Back to Sleep recommendations as well.
A standardized developmental screening tool is used at the 9-, 18-, and 30-month visits, and when parents or caregivers express concern about development. Autism-specific screening happens at 18 and 24 months.
“Remember this, if you remember nothing else: If the screening is positive, and you believe there’s a problem, you’re going to refer,” not just to the appropriate specialist but also for early intervention services, so time isn’t lost as the child is waiting for further evaluation and a formal diagnosis, said Dr. Hagan. This coordinated effort appropriately places the responsibility for early identification of developmental delays and disorders at the doorstep of the child’s medical home.
The federally-coordinated Birth to 5: Watch Me Thrive! effort has aggregated research-based screening tools, users’ guides targeted at a variety of audiences, and resources to help caregivers, said Dr. Hagan.
Four commonly-used tools to consider using during the visit are the Parents’ Evaluation of Developmental Status, the Ages and Stages Questionnaire, the Child Health and Development Interactive System, and the Survey of Wellbeing of Young Children. Of these, said Dr. Hagan, the latter is the only tool that’s in the public domain. However, he said, they are “all really good.”
Consider having parents fill out screening questionnaires in the waiting room before the visit, said Dr. Hagan. “I always tell my colleagues, ‘Have them start the visit without you, if you want to get it done in 18 minutes.’ ”
Two questionnaires per visit are available in the Bright Futures toolkit. One questionnaire asks developmental surveillance and risk assessment questions for selective screening. The second questionnaire asks prescreening questions to help with the anticipatory guidance part of the visit, he said. Having families do these ahead of time, said Dr. Hagan, “allows you to become more focused.”
Paying attention to practicalities can make all this go more smoothly, and maximize reimbursement as well. In his own practice, Dr. Hagan said, screening tools and questionnaires are integrated into the EHR system, so that appropriate paperwork prints automatically ahead of the visit.
It’s also worth reviewing billing practices to make sure that CPT code 96110 is used when administering screening with a standardized instrument and completing scoring and documentation. According to the Bright Futures periodicity schedule, this may be done at the 9-, 18-, and 30-month visits for developmental screening, as well as at 18 and 24 months for autism-specific screening.
Promoting lifelong health
Since the initial Bright Futures guidelines were published in the late 1990s, said Dr. Hagan, the focus has always been on seeing the child as part of the family, who, in turn, are part of the community, forming a framework that addresses the social components of child health. “If you’re not looking at the whole picture, you’re not promoting health,” he said. “It’s no big surprise that we now have a specific, called-out focus on promoting lifelong health.”
In the Fourth Edition, the theme of promoting lifelong health for families and communities is woven throughout, with social determinants of health being a specific visit priority. For example, questions about food insecurity have been drawn from the published literature and are included. Also, said Dr. Hagan, there’s specific anticipatory guidance content that’s clearly marked as addressing social determinants of health.
The fundamental importance of socioeconomic status as a social determinant of health was brought home by the Robert Wood Johnson Foundation’s Commission to Build a Healthier America, which demonstrated that, “Your ZIP code is more important to your health than your genetic code,” said Dr. Hagan. “So your work in health supervision is important, and you have been leaders in this effort.”
Research guides Bright Futures updates
The fourth edition of Bright Futures builds on health promotion themes to support the mental and physical health of children and adolescents, and has a robust framework of evidence underpinning the guidelines, said Dr. Hagan.
The goal is for clinicians to “use evidence to decide upon content of their own health supervision visits,” he explained.
The chapter of the Bright Futures guidelines that addresses the evidence and rationale for the guidelines has been expanded to better answer two questions, said Dr. Hagan: “What evidence grounds our recommendations?” and “What rationale did we use when evidence was insufficient or lacking?”
When possible, the editors of the guidelines used evidence-based sources such as recommendations from the USPSTF, the Centers for Disease Control Community Guide, and the Cochrane Collaboration.
There were many more evidence-based recommendations available to those working on the 4th edition than there had been when writing the previous edition, when, said Dr. Hagan, the USPSTF had exactly two recommendations for those under the age of 21 years. The current expanded number of USPSTF pediatric recommendations was due in part to the attention the AAP was able to bring regarding the need for evidence-based recommendations in pediatrics, he said.
When guidelines were not available, the editors also turned to high quality studies from peer reviewed publications. When such high quality evidence was lacking in a particular area, the guidelines make clear what rationale was used to formulate a given recommendation, and that some recommendations should be interpreted with a degree of caution.
And, said Dr. Hagan, even science-based guidelines will change as more data accumulates. “Don’t forget about peanuts!” he said. “It was really logical 15 years ago when we said don’t give peanut products until 1 year of age. And about 2 years ago, we found out that it really didn’t work.”
Although there are specific updates to clinical content, there also were changes made in broader strokes throughout the 4th edition. One of these shifts embeds social determinants of health in many visits. This adjustment acknowledges the growing body of knowledge that “strengths and protective factors make a difference, and risk factors make a difference” in pediatric outcomes.
A greater focus on lifelong physical and mental health is included under the general rubric of promoting lifelong health for families and communities. More emphasis is placed on promoting health for children and youth who have special health care needs as well.
Nuts-and-bolts changes in the updated 4th edition include updates for milestones of development and accompanying developmental surveillance questions, new clinical content and guidance for implementation that have been added based on strong evidence, and a variety of updates for adolescent screenings in particular.
The full 4th edition Bright Futures toolkit will be available for use in 2018.
Dr. Hagan was a coeditor of the Fourth Edition of Bright Futures.
*This article was updated on December 21, 2017
EXPERT ANALYSIS FROM AAP 2017
Survey: Safety, rather than ethics, tops concerns about uterine transplantation
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Uterine transplantation is generally seen as ethical, with acceptable risk levels for both donors and recipients, according to two parallel surveys given to women’s health physicians and to the general public.
The results, presented at the annual meeting of the American Society for Reproductive Medicine (ASRM), showed that “the majority of gynecologists surveyed find uterine transplantation to be an acceptable and ethical option for patients with uterine factor infertility,” wrote Pietro Bortoletto, MD, and his coauthors.
Similarly, about two-thirds of the general public found uterine transplantation permissible and ethical, according to responses from an age- and gender-balanced nationally representative survey.
The web-based surveys were designed to assess the personal beliefs of both the public and of physicians about the permissibility of uterine transplantation, and to evaluate respondents’ concerns about perceived risks associated with the procedure. Respondents in each survey were also asked to identify any ethical concerns they might have; recipients of both surveys received background information about uterine transplantation.
Dr. Bortoletto and his colleagues sent the survey by email to physicians who were members of ASRM and AAGL. Of the 4,216 physicians who were invited to take the survey, 447 (28.4%) completed it, though results were tallied just for the 414 respondents who were United States–based physicians.
Physician respondents, when asked whether women should be allowed to donate or receive a transplanted uterus, responded mostly in the affirmative: 20% strongly agreed and 36% agreed, while 23% were neutral. The remainder disagreed or strongly disagreed.
The possibility of complications for the recipient was identified as the top concern by about 50% of physician respondents. Next most concerning was fetal outcomes, of primary concern for about 28%, followed by complications to the donor and cost, each of which was of primary concern to 10% or fewer of the physician respondents.
The risk to donors of uterine transplantation was seen as acceptable by 73.7% of AAGL members and 71.7% of ASRM members; just over half of each group saw the risk as acceptable for the recipients and the infants, however.
Though over half of physician respondents (57.9% of AAGL members and 59.5% of ASRM members) felt that uterine transplantation should be a potential treatment option for women with absolute uterine factor infertility, fewer felt it should be covered by health insurance – 35.4% of AAGL members and 40.5% of ASRM members held this opinion.
Among the general public, over three quarters (78%) felt that women should be allowed to undergo uterine transplantation. Slightly fewer (67%) respondents to the public survey felt that uterine transplantation is ethical; those who agreed had slightly higher incomes and education levels (relative risk, 1.11 and 1.09, respectively). A similar number (66%) felt that uterine transplantation was an acceptable alternative to using a gestational carrier.
As was the case for physicians, fewer members of the general public (45%) agreed that health insurance should cover the procedure; here, women and Hispanics were more likely to agree (relative risk, 1.11 and 1.18, respectively).
The results of the survey of the general public were presented by first author Eduardo Hariton, MD, a coauthor of Dr. Bortoletto’s in the study of physician survey results. Both Dr. Hariton and Dr. Bortoletto are resident physicians in the department of obstetrics, gynecology, and reproductive biology at Brigham and Women’s Hospital, Boston.
The public survey was sent to a nationally representative sample, balanced by gender and age. Of 1,444 individuals who were recruited to receive the survey, 1,337 completed it. Ninety respondents reported that they found in vitro fertilization unacceptable; these responses were excluded, Dr. Hariton said in an interview. “We wanted to get at uterine transplantation per se,” rather than assisted reproductive technology in general.
Placing the ethics of uterine transplantation in a broader context, Dr. Bortoletto said in an interview that the United States is one of just a few countries that permit gestational surrogacy, with regulations varying by state. To his knowledge, he said, Ukraine and Russia are the only other two nations that permit compensation for surrogacy. Greece and the United Kingdom permit altruistic surrogacy, while gestational surrogacy of any sort is forbidden in the European Union. Thus, in those nations, uterine transplantation will be the only option for women who wish to bear their biological children.
“I think the main takeaway is that for people who had hesitation about [uterine transplantation], it was mainly around safety,” and not ethical concerns, said Dr. Hariton. “I was a bit surprised, but also encouraged, by the degree of support.”
Neither Dr. Hariton nor Dr. Bortoletto reported any conflicts of interest. The public opinion study was funded by an Expanding the Boundaries grant.
Half of all breast cancer survivors conceived naturally within 3 months of trying
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
[email protected]
On Twitter @karioakes
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
[email protected]
On Twitter @karioakes
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
[email protected]
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: Of 36 women whose ovarian function resumed after chemotherapy, 18 (50%) conceived within 3 months of attempting conception.
Data source: A single-center prospective cohort study of women diagnosed with breast cancer who received fertility preservation consultation.
Disclosures: The study was funded by the University of California, San Francisco Clinical and Translational Science Institute.
Baylor sees first U.S. birth from uterine transplant recipient
A woman with a transplanted uterus gave birth to a live baby boy in Dallas, the first birth from a transplanted uterus in the United States. It is also the first birth resulting from uterine transplantation to be performed outside of Sweden, where a total of eight births have occurred.
“This really confirms that this is doable, that it can be replicated,” said Giuliano Testa, MD, chief of abdominal transplantation at Baylor University Medical Center, Dallas, during a press conference to discuss the birth.
With time, Dr. Testa said in an interview, he foresees uterine transplantation becoming a realistic alternative for some women. “It’s a great solution for the woman who really wants to carry her own pregnancy.”
“This is the best of academic medicine,” Dr. Testa said of the international collaboration and transparency among investigators working in the nascent field. “The communication is constant; we learn from each other ... I am very excited about what will come in the future.”
In order to protect the privacy of the patient and her family, physicians did not disclose the patient’s name, location, or the exact date of the birth. The patient also did not wish to share the infant’s gestational age at birth or birth weight, or whether the uterus had been removed after the birth. Transplanted uteri are meant to be removed after one or two pregnancies, so the recipient doesn’t have to be on lifelong immunosuppression once the desired pregnancies have been achieved.
However, during the press conference, the surgical team shared that the mother is home and doing well, and the infant is on room air and feeding well. A video of the birth shown at the press conference showed a vernix-covered baby who began crying vigorously even before his feet were delivered during the cesarean delivery.
The transplantation, pregnancy via in vitro fertilization, and subsequent birth were accomplished as part of a 10-patient clinical trial of uterine transplantation at Baylor University Medical Center. Women aged 20-35 years with absolute uterine factor infertility, such as those with congenitally absent uteri, were eligible to participate. Donors must have had one full-term delivery and may be aged 30-65 years; menopause does not render a uterus incapable of carrying a pregnancy. Donors are able to retain their ovaries.
Another study participant at Baylor is late into her pregnancy as well, Dr. Testa said.
The extensive screening process for uterus donation ensures that the team is using “a good organ from a good donor,” said Liza Johannesson, MD, PhD. In an interview, she said that the harvest is now about a 4-5 hour open procedure that takes the uterus, the cervix, and the very superior portion of the vagina, as well as the uterine arteries and veins out to the internal iliac bilaterally. The utero-ovarian veins also are harvested.
To date, the six women who have been donors in the Baylor program have not had serious complications and have returned to their previous level of function, said Dr. Johannesson, who came to Baylor from Sahlgrenska University Hospital’s successful uterine transplantation team in Gothenburg, Sweden.
Internationally, investigators have been working to reduce morbidity for women who donate their uterus. Since the vascular tree of the uterus must also be dissected and preserved during the organ harvesting procedure, operative time is longer than for a simple hysterectomy, and there’s increased risk of urinary dysfunction because of the extensive dissection, Antonio R. Gargiulo, MD, said in an interview.*
Dr. Gargiulo, medical director of the center for robotic surgery at Brigham and Women’s Hospital, Boston, said that the first few uterine harvest procedures took much longer, up to 10 hours. But, he said, the vascular harvest “is well within the capability of the best gynecologic oncology surgeons,” and newer techniques may further reduce the donor morbidity.
Using the utero-ovarian vein as the primary outflow tract is “a promising modification of this operation” that may be the “technical key to making this procedure the least morbid possible,” said Dr. Gargiulo, a reproductive endocrinologist who is involved with the development of a uterine transplantation program at the Brigham and Women’s Hospital.
Dr. Johannesson said that the Baylor team currently dissects the entire uterine vascular tree and reanastomoses what vessels they can. She pointed out that even with the best imaging techniques, it can be difficult to ascertain the best vessels until the surgery’s actually being performed.
All of the surgeons interviewed emphasized that each procedure represents an opportunity for growth in a young field with a steep learning curve. They expect ongoing technical advances, including the use of robotic surgery, to reduce operative time and lessen morbidity.
It’s worth pressing on in this field for the sake of the patients, said Dr. Testa, speaking for his transplant team. “We are all humbled by the depth of the desire of a woman to carry her own pregnancy.”
Dr. Johannesson said that she hopes that today when gynecologists talk to teenage patients who have absolute uterine infertility, they will be offering a message of hope. “When they meet young women, they should tell them that they shouldn’t stop hoping,” she said. “There is hope that they will be able to carry their own pregnancy.”
Dr. Gargiulo has been a paid consultant for Kawasaki Robotics and OmniGuide. Dr. Testa and Dr. Johannesson reported that they had no relevant conflicts of interest.
*Correction, 12/12/17: The reason for the increased risk of urinary dysfunction was misstated.
[email protected]
On Twitter @karioakes
A woman with a transplanted uterus gave birth to a live baby boy in Dallas, the first birth from a transplanted uterus in the United States. It is also the first birth resulting from uterine transplantation to be performed outside of Sweden, where a total of eight births have occurred.
“This really confirms that this is doable, that it can be replicated,” said Giuliano Testa, MD, chief of abdominal transplantation at Baylor University Medical Center, Dallas, during a press conference to discuss the birth.
With time, Dr. Testa said in an interview, he foresees uterine transplantation becoming a realistic alternative for some women. “It’s a great solution for the woman who really wants to carry her own pregnancy.”
“This is the best of academic medicine,” Dr. Testa said of the international collaboration and transparency among investigators working in the nascent field. “The communication is constant; we learn from each other ... I am very excited about what will come in the future.”
In order to protect the privacy of the patient and her family, physicians did not disclose the patient’s name, location, or the exact date of the birth. The patient also did not wish to share the infant’s gestational age at birth or birth weight, or whether the uterus had been removed after the birth. Transplanted uteri are meant to be removed after one or two pregnancies, so the recipient doesn’t have to be on lifelong immunosuppression once the desired pregnancies have been achieved.
However, during the press conference, the surgical team shared that the mother is home and doing well, and the infant is on room air and feeding well. A video of the birth shown at the press conference showed a vernix-covered baby who began crying vigorously even before his feet were delivered during the cesarean delivery.
The transplantation, pregnancy via in vitro fertilization, and subsequent birth were accomplished as part of a 10-patient clinical trial of uterine transplantation at Baylor University Medical Center. Women aged 20-35 years with absolute uterine factor infertility, such as those with congenitally absent uteri, were eligible to participate. Donors must have had one full-term delivery and may be aged 30-65 years; menopause does not render a uterus incapable of carrying a pregnancy. Donors are able to retain their ovaries.
Another study participant at Baylor is late into her pregnancy as well, Dr. Testa said.
The extensive screening process for uterus donation ensures that the team is using “a good organ from a good donor,” said Liza Johannesson, MD, PhD. In an interview, she said that the harvest is now about a 4-5 hour open procedure that takes the uterus, the cervix, and the very superior portion of the vagina, as well as the uterine arteries and veins out to the internal iliac bilaterally. The utero-ovarian veins also are harvested.
To date, the six women who have been donors in the Baylor program have not had serious complications and have returned to their previous level of function, said Dr. Johannesson, who came to Baylor from Sahlgrenska University Hospital’s successful uterine transplantation team in Gothenburg, Sweden.
Internationally, investigators have been working to reduce morbidity for women who donate their uterus. Since the vascular tree of the uterus must also be dissected and preserved during the organ harvesting procedure, operative time is longer than for a simple hysterectomy, and there’s increased risk of urinary dysfunction because of the extensive dissection, Antonio R. Gargiulo, MD, said in an interview.*
Dr. Gargiulo, medical director of the center for robotic surgery at Brigham and Women’s Hospital, Boston, said that the first few uterine harvest procedures took much longer, up to 10 hours. But, he said, the vascular harvest “is well within the capability of the best gynecologic oncology surgeons,” and newer techniques may further reduce the donor morbidity.
Using the utero-ovarian vein as the primary outflow tract is “a promising modification of this operation” that may be the “technical key to making this procedure the least morbid possible,” said Dr. Gargiulo, a reproductive endocrinologist who is involved with the development of a uterine transplantation program at the Brigham and Women’s Hospital.
Dr. Johannesson said that the Baylor team currently dissects the entire uterine vascular tree and reanastomoses what vessels they can. She pointed out that even with the best imaging techniques, it can be difficult to ascertain the best vessels until the surgery’s actually being performed.
All of the surgeons interviewed emphasized that each procedure represents an opportunity for growth in a young field with a steep learning curve. They expect ongoing technical advances, including the use of robotic surgery, to reduce operative time and lessen morbidity.
It’s worth pressing on in this field for the sake of the patients, said Dr. Testa, speaking for his transplant team. “We are all humbled by the depth of the desire of a woman to carry her own pregnancy.”
Dr. Johannesson said that she hopes that today when gynecologists talk to teenage patients who have absolute uterine infertility, they will be offering a message of hope. “When they meet young women, they should tell them that they shouldn’t stop hoping,” she said. “There is hope that they will be able to carry their own pregnancy.”
Dr. Gargiulo has been a paid consultant for Kawasaki Robotics and OmniGuide. Dr. Testa and Dr. Johannesson reported that they had no relevant conflicts of interest.
*Correction, 12/12/17: The reason for the increased risk of urinary dysfunction was misstated.
[email protected]
On Twitter @karioakes
A woman with a transplanted uterus gave birth to a live baby boy in Dallas, the first birth from a transplanted uterus in the United States. It is also the first birth resulting from uterine transplantation to be performed outside of Sweden, where a total of eight births have occurred.
“This really confirms that this is doable, that it can be replicated,” said Giuliano Testa, MD, chief of abdominal transplantation at Baylor University Medical Center, Dallas, during a press conference to discuss the birth.
With time, Dr. Testa said in an interview, he foresees uterine transplantation becoming a realistic alternative for some women. “It’s a great solution for the woman who really wants to carry her own pregnancy.”
“This is the best of academic medicine,” Dr. Testa said of the international collaboration and transparency among investigators working in the nascent field. “The communication is constant; we learn from each other ... I am very excited about what will come in the future.”
In order to protect the privacy of the patient and her family, physicians did not disclose the patient’s name, location, or the exact date of the birth. The patient also did not wish to share the infant’s gestational age at birth or birth weight, or whether the uterus had been removed after the birth. Transplanted uteri are meant to be removed after one or two pregnancies, so the recipient doesn’t have to be on lifelong immunosuppression once the desired pregnancies have been achieved.
However, during the press conference, the surgical team shared that the mother is home and doing well, and the infant is on room air and feeding well. A video of the birth shown at the press conference showed a vernix-covered baby who began crying vigorously even before his feet were delivered during the cesarean delivery.
The transplantation, pregnancy via in vitro fertilization, and subsequent birth were accomplished as part of a 10-patient clinical trial of uterine transplantation at Baylor University Medical Center. Women aged 20-35 years with absolute uterine factor infertility, such as those with congenitally absent uteri, were eligible to participate. Donors must have had one full-term delivery and may be aged 30-65 years; menopause does not render a uterus incapable of carrying a pregnancy. Donors are able to retain their ovaries.
Another study participant at Baylor is late into her pregnancy as well, Dr. Testa said.
The extensive screening process for uterus donation ensures that the team is using “a good organ from a good donor,” said Liza Johannesson, MD, PhD. In an interview, she said that the harvest is now about a 4-5 hour open procedure that takes the uterus, the cervix, and the very superior portion of the vagina, as well as the uterine arteries and veins out to the internal iliac bilaterally. The utero-ovarian veins also are harvested.
To date, the six women who have been donors in the Baylor program have not had serious complications and have returned to their previous level of function, said Dr. Johannesson, who came to Baylor from Sahlgrenska University Hospital’s successful uterine transplantation team in Gothenburg, Sweden.
Internationally, investigators have been working to reduce morbidity for women who donate their uterus. Since the vascular tree of the uterus must also be dissected and preserved during the organ harvesting procedure, operative time is longer than for a simple hysterectomy, and there’s increased risk of urinary dysfunction because of the extensive dissection, Antonio R. Gargiulo, MD, said in an interview.*
Dr. Gargiulo, medical director of the center for robotic surgery at Brigham and Women’s Hospital, Boston, said that the first few uterine harvest procedures took much longer, up to 10 hours. But, he said, the vascular harvest “is well within the capability of the best gynecologic oncology surgeons,” and newer techniques may further reduce the donor morbidity.
Using the utero-ovarian vein as the primary outflow tract is “a promising modification of this operation” that may be the “technical key to making this procedure the least morbid possible,” said Dr. Gargiulo, a reproductive endocrinologist who is involved with the development of a uterine transplantation program at the Brigham and Women’s Hospital.
Dr. Johannesson said that the Baylor team currently dissects the entire uterine vascular tree and reanastomoses what vessels they can. She pointed out that even with the best imaging techniques, it can be difficult to ascertain the best vessels until the surgery’s actually being performed.
All of the surgeons interviewed emphasized that each procedure represents an opportunity for growth in a young field with a steep learning curve. They expect ongoing technical advances, including the use of robotic surgery, to reduce operative time and lessen morbidity.
It’s worth pressing on in this field for the sake of the patients, said Dr. Testa, speaking for his transplant team. “We are all humbled by the depth of the desire of a woman to carry her own pregnancy.”
Dr. Johannesson said that she hopes that today when gynecologists talk to teenage patients who have absolute uterine infertility, they will be offering a message of hope. “When they meet young women, they should tell them that they shouldn’t stop hoping,” she said. “There is hope that they will be able to carry their own pregnancy.”
Dr. Gargiulo has been a paid consultant for Kawasaki Robotics and OmniGuide. Dr. Testa and Dr. Johannesson reported that they had no relevant conflicts of interest.
*Correction, 12/12/17: The reason for the increased risk of urinary dysfunction was misstated.
[email protected]
On Twitter @karioakes
E-health app helps weight loss, QOL for African American breast cancer survivors
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
[email protected]
On Twitter @karioakes
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
[email protected]
On Twitter @karioakes
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: Participants lost a mean 4.79 pounds from baseline (mean 2.14%, P less than .001).
Data source: Subanalysis from study of 61 African American survivors of early stage breast cancer, with BMI of 25 or higher.
Disclosures: Dr. Ferrante reported no conflicts of interest.