User login
VRE Bacteremia Treatment With Linezolid or Daptomycin
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
Copyright © 2011 Society of Hospital Medicine
Evaluation of glycemic control following discontinuation of an intensive insulin protocol
Hyperglycemia and insulin resistance are common occurrences in critically ill patients, even those without a past medical history of diabetes.1, 2 This hyperglycemic state is associated with adverse outcomes, including severe infections, polyneuropathy, multiple‐organ failure, and death.3 Several studies have shown benefit in keeping patients' blood glucose (BG) tightly controlled.37 In a randomized controlled study, strict BG control (80‐110 mg/dL) with an insulin drip significantly reduced morbidity and mortality in critically ill patients.3 A recent meta‐analysis concluded that avoiding BG levels >150 mg/dL appeared to be crucial to reducing mortality in a mixed medical and surgical intensive care unit (ICU) population.7
The Diabetes Mellitus Insulin‐Glucose Infusion in Acute Myocardial Infarction study addressed the issue of tight glycemic control both acutely and chronically in 620 diabetic patients postmyocardial infarction. Patients were randomized to tight glycemic control (126‐180 mg/dL) followed by a transition to maintenance insulin or to standard care. This intervention demonstrated a sustained mortality reduction of 7.5% at 1 year.8 In contrast, the CREATE‐ECLA study showed a neutral mortality benefit of a short‐term (24‐hour) insulin infusion in postmyocardial infarction patients.9 These data demonstrate the need for clinicians to consider insulin requirements throughout the hospital stay and after discharge. To date, there are no published studies evaluating glycemic control following discontinuation of an intensive insulin protocol (IIP). Therefore, the current study was conducted to compare BG control during the use of an IIP and for the 5 days following intensive insulin therapy.
METHODS
Patient Population
This retrospective chart review was conducted at Methodist University Hospital (MUH), Memphis, TN. MUH is a 500‐bed, university‐affiliated tertiary referral hospital. The study was approved by the hospital institutional review board. From January 2006 to January 2007, a computer‐generated pharmacy report was used to identify all patients receiving the hospital‐approved IIP. Patients were included if they were 18 years old and received the IIP for 24 hours. Patients were excluded from the study if they met any of the following criteria: (1) complete BG measurements were not retrievable while the patient received the IIP or for the 5 days following discontinuation of the IIP, (2) the patient died while receiving the IIP, and (3) an endocrinologist was involved in the care of the patient.
IIP
The hospital‐approved IIP is a paper‐based, physician‐initiated, nurse‐managed protocol. Criteria required before initiating the IIP include (1) ICU admission, (2) 2 BG measurements >150 mg/dL, (3) administration of continuous exogenous glucose, and (4) absence of diabetic ketoacidosis. The goal range of the IIP is 80 to 150 mg/dL. Hourly BG measurements are initially required, but as control is achieved, measurements may be extended to every 2 hours and then every 4 hours. In general, the criteria used for transitioning off the IIP include stability during the last 12 hours. Patients were considered to be stable on the IIP if they had >70% of their glucose measurements within the goal range during the last 12 hours.
Data Collection
When inclusion criteria were met, patients' medical records were reviewed. Data collection included basic demographic information, concurrent medications, duration of IIP, amount of insulin administered during the last 12 hours of the IIP, insulin regimen post‐IIP, and BG measurements during the last 12 hours on the IIP and for a total of 5 days after the IIP was stopped (follow‐up period). For this study, hyperglycemia was defined as a BG value >150 mg/dL, significant hyperglycemia was defined as >200 mg/dL, and severe hyperglycemia was defined as >300 mg/dL. Hypoglycemia was defined as a BG value <60 mg/dL. The values of <60 mg/dL, >150 mg/dL, and >200 mg/dL were chosen on the basis of the criteria used in the MUH IIP and standard sliding‐scale protocols. A value of >300 mg/dL was used to better describe patients with hyperglycemia. Poor glycemic control following the IIP was defined as a >30% change in mean BG during the last 12 hours on the drip and on the first day after discontinuation of the drip.
Statistical Analysis
The primary objective of this study was to compare BG control during the last 12 hours of an IIP and for the 5 days following its discontinuation. Secondary objectives were to evaluate the incidence of hyperglycemia and hypoglycemia during the transition period and to identify patients at risk of poor glycemic control following discontinuation of the IIP. Continuous data are appropriately reported as the mean standard deviation or median (interquartile range), depending on the distribution. Continuous variables were compared with the Student t test or Wilcoxon rank sum test. Discrete variables were compared with chi‐square analysis and Bonferroni Correction where appropriate. For comparisons of BG during the IIP and on days 1 to 5 of the follow‐up period, repeated‐measures analysis of variance on ranks was conducted because of the distribution. These statistical analyses were performed with SigmaStat version 2.03 (Systat Software, Inc., Richmond, VA). A P value of less than 0.05 was considered significant. However, when the Bonferroni correction was used, a value of less than 0.01 was considered significant. Multivariable logistic regression was used to determine independent predictors of a greater than 30% change in the mean BG value between the last 12 hours of the IIP and the first day off the insulin drip. Potential independent variables included in the analysis were stability on protocol, requiring less than 20 units of insulin in the last 12 hours on the IIP, use of antibiotics, use of steroids, history of diabetes, and type of insulin to which the patient was transitioned (none, sliding scale, and scheduled and sliding scale). The model was built in a backwards, stepwise fashion with SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
A total of 171 patients received the IIP during the study period. Ninety‐seven patients did not meet inclusion criteria because they received the IIP for less than 24 hours. Of the 74 patients meeting inclusion criteria, 9 were excluded (5 had insufficient glucose data, 3 were cared for by an endocrinologist, and 1 died while receiving the IIP). Thus, 65 patients were included in the study.
Table 1 lists the baseline demographics for all patients and those with and without a history of diabetes mellitus (DM). The majority of the patients (n = 49) underwent a surgical procedure, with the most common procedure being coronary artery bypass graft (n = 38). Patients undergoing coronary artery bypass graft had the IIP included in their standard postoperative order set. The majority of patients were considered stable during the 12 hours prior to discontinuation of the IIP, including 23 patients with a history of DM. Of the 65 patients who were included in the study, 25 (38.5%) received a scheduled insulin order following discontinuation of the IIP, whereas 38 (58.5%) received some form of sliding‐scale insulin (SSI). Additionally, 2 (3%) patients did not receive any form of insulin order after stopping the IIP. Of those receiving scheduled insulin, 15 (60%) received neutral protamine Hagedorn, 5 (20%) received glargine, 5 (20%) received 70/30, and 1 (4%) received regular insulin. Of those receiving SSI only, the prescribed frequency was as follows: every 4 hours for 17 (45%), before meals and at bedtime for 15 (39%), every 6 hours for 5 (13%), and every 2 hours for 1 (3%).
| All Patients (n = 65) | PMH of DM (n = 36) | No PMH of DM (n = 29) | |
|---|---|---|---|
| |||
| Age, mean years SD | 62 11 | 61 10 | 64 12 |
| Male gender, n (%) | 38 (58) | 22 (61) | 16 (55.2) |
| BMI SD | 30 7.2 | 31 7 | 30 6.5 |
| Surgery, n (%) | 49 (74.2) | 27 (75) | 21 (72.4) |
| CABG, n | 38 | 22 | 16 |
| Liver transplant, n | 6 | 1 | 4 |
| Other, n | 5 | 4 | 1 |
| Last 24 hours on IIP, n (%) | |||
| Ventilator | 37 (56.9) | 22 (61.1) | 15 (51.7) |
| Antibiotics | 37 (56.9) | 20 (55.6) | 17 (58.6) |
| Vasopressors | 11 (16.9) | 5 (13.9) | 6 (20.7) |
| Hemodialysis | 8 (12.3) | 5 (13.9) | 3 (10.3) |
| Steroids | 16 (24.6) | 9 (25) | 7 (24.1) |
| Duration of IIP, mean hours SD | 72 65 | 80 78 | 62 45 |
| Insulin during last 12 hours of IIP, mean units SD | 47 37 | 51 30 | 46 45 |
| Type of insulin received following IIP, n (%) | |||
| Scheduled + sliding scale | 25 (38.5) | 19 (52.8) | 6 (20.7) |
| Sliding scale only | 38 (58.5) | 16 (44.4) | 22 (75.9) |
| None | 2 (3) | 1 (2.8) | 1 (3.4) |
| Total daily insulin following IIP, mean units SD | 28 41 | 38 49 | 17 24 |
| Patients stable on IIP | 44 (67.7) | 23 (64.8) | 21 (72.4) |
| Hospital LOS, mean days SD | 24 18 | 24 17 | 23 19 |
| Mortality, n (%) | 15 (23.1) | 5 (13.8) | 10 (34.5) |
A total of 562 glucose measurements were collected during the last 12 hours on the IIP, whereas 201 were collected during the first 12 hours immediately following the IIP. Patients demonstrated a significant increase in BG (mean standard deviation) during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP (168 50 mg/dL versus 123 26 mg/dL, P < 0.001). This corresponded to a significant decrease in the median (interquartile range) insulin administered during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP [8 (0‐18) units versus 40 (22‐65) units, P < 0.001; Figure 1]. A total of 1914 BG measurements were collected during the follow‐up period. Figure 2 shows mean BG values for all patients on the IIP compared to mean BG values for each day of the follow‐up period. There was a significant increase in mean BG measurements when the IIP was compared to each day of the follow‐up period, but there was no difference between days of the follow‐up period. Table 2 shows the proportion of patients experiencing at least 1 episode of hyperglycemia (BG > 150 mg/dL), significant hyperglycemia (BG > 200 mg/dL), severe hyperglycemia (BG > 300 mg/dL), or hypoglycemia (BG < 60 mg/dL) while receiving the IIP and during the follow‐up period. When comparing the IIP to the follow‐up period, we found a significant increase in the proportion of patients with at least 1 BG > 150 mg/dL. This was also true for patients with a BG of > 200 mg/dL.
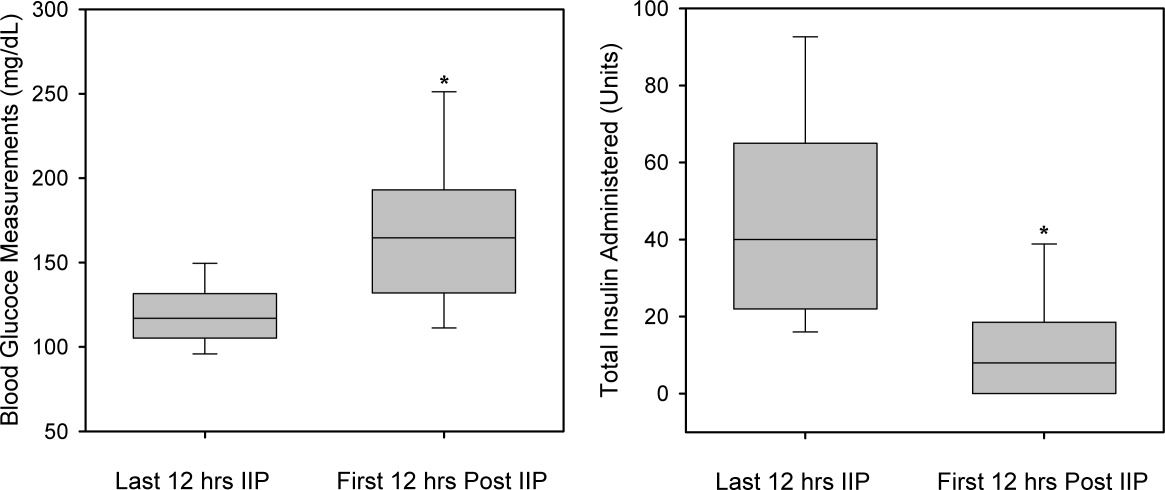
| IIP (n = 65) | Day 1 (n = 65) | Day 2 (n = 65) | Day 3 (n = 64) | Day 4 (n = 62) | Day 5 (n = 59) | |
|---|---|---|---|---|---|---|
| ||||||
| Patients with >150 mg/dL, n (%) | 33 (51) | 54 (83)* | 54 (83)* | 52 (81)* | 51 (82)* | 48 (81)* |
| Patients with >200 mg/dL, n (%) | 11 (17) | 37 (57)* | 31 (48)* | 26 (41)* | 33 (53)* | 34 (58)* |
| Patients with >300 mg/dL, n (%) | 2 (3) | 11 (17) | 7 (11) | 8 (12) | 5 (8) | 10 (17) |
| Patients with <60 mg/dL, n (%) | 6 (9) | 5 (8) | 2 (3) | 2 (3) | 2 (3) | 0 (0) |
The only independent predictor of a greater than 30% change in mean BG was the requirement for more than 20 units of insulin (>1.7 units/hour) during the last 12 hours on the IIP. The odds of a greater than 30% change was 4.62 times higher (95% confidence interval: 1.1718.17) in patients requiring more than 20 units during the last 12 hours on IIP after adjustments for stability on the protocol and past medical history of diabetes. Stability on the protocol was not identified as an independent predictor, with an adjusted odds ratio of 2.40 (95% confidence interval: 0.797.32).
DISCUSSION
This is the first study to describe glycemic control following the transition from an IIP to subcutaneous insulin. We observed that during the 5 days following discontinuation of an IIP, patients had significantly elevated mean BG values. These data are highlighted by the fact that patients received significantly less insulin during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP. Additionally, a larger than expected proportion of patients exhibited at least 1 episode of hyperglycemia during the follow‐up period. We also found that an increased insulin requirement of >1.7 units/hour during the last 12 hours of the IIP was an independent risk factor for a greater than 30% increase in mean BG on day 1 of the follow‐up period.
Increasing evidence demonstrates that the development of hyperglycemia in the hospital setting is a marker of poor clinical outcome and mortality. In fact, hyperglycemia has been associated with prolonged hospital stay, infection, disability after discharge, and death in patients on general surgical and medical wards.1012 This makes the increase in mean BG found in our study following discontinuation of the IIP a concern.
SSI with subcutaneous short‐acting insulin has been used for inpatients as the standard of care for many years. However, evidence supporting the effectiveness of SSI alone is lacking, and it is not recommended by the American Diabetes Association.13 Queale et al.14 showed that SSI regimens when used alone were associated with suboptimal glycemic control and a 3‐fold higher risk of hyperglycemic episodes.1 Two retrospective studies have also demonstrated that SSI is less effective and widely variable in comparison with proactive preventative therapy.15, 16 In the current study, 58.5% of patients received SSI alone during the follow‐up period. As indicated in Figure 1, there was a significant increase in mean BG during this time interval. The choice of an inappropriate insulin regimen might be a contributing factor to poor glycemic control.
Because only 38.5% of patients were transitioned to scheduled insulin in our study, one possible strategy to help improve glycemic control would be to transition patients to a scheduled insulin regimen. Umpierrez et al.12 conducted a prospective, multicenter randomized trial to compare the efficacy and safety of a basal‐bolus insulin regimen with that of SSI in hospitalized type 2 diabetics. These authors found that patients treated with insulin glargine and glulisine had greater improvement in glycemic control than those treated with SSI (P < 0.01).12 Interestingly, the basal‐bolus method provides a maintenance insulin regimen that is aggressively titrated upward as well as an adjustable SSI based on insulin sensitivity. Patients in the current study may have benefited from a similar approach as many did not have their scheduled insulin adjusted despite persistent hyperglycemia.
With the increasing evidence for tight glycemic control in the ICU, a standardized transition from an intensive insulin infusion to a subcutaneous basal‐bolus regimen or other scheduled regimen is needed. To date, the current study is the first to describe this transition. Based on these data, recommendations for transitioning patients off an IIP provided by Furnary and Braithwaite17 should be considered by clinicians. In fact, one of their proposed predictors for unsuccessful transition was an insulin requirement of 2 units/hour. Indeed, the only independent risk factor for poor glycemic control identified in the current study was a requirement of >20 units (>1.7 units/hour) during the last 12 hours of the IIP. Further research is required to verify the other predictors suggested by Furnary and Braithwaite. They recommended using a standardized conversion protocol to transition patients off an IIP.
More recently, Kitabchi et al.18 recommended that a BG target of less than 180 mg/dL be maintained for the hospitalized patient.18 Although our study showed a mean BG less than 180 mg/dL during the follow‐up period, the variability in these values raises concerns for individual patients.
The current study is limited by its size and retrospective nature. As with all retrospective studies, the inability to control the implementation and discontinuation of the IIP may confound the results. However, this study demonstrates a real world experience with an IIP and illustrates the difficulties with transitioning patients to a subcutaneous regimen. BG values and administered insulin were collected only for the last 12 hours on the IIP. This duration is considered appropriate as this time period is used clinically at MUH, and previous recommendations for transitioning patients suggest using a time period of 6 to 8 hours to guide the transition insulin regimen.17 In addition, data regarding the severity of illness and new onset of infections were not collected for patients in the study. Both could affect glucose control. All patients had to be in an ICU to receive the IIP, but their location during the follow‐up period varied. Although these data were not available, control of BG is a problem that should be addressed whether the patient is in the ICU or not. Another possible limitation of the study was the identification of patients with or without a past medical history of DM. The inability to identify new‐onset or previously undiagnosed DM may have affected analyses based on this variable.
CONCLUSIONS
This study demonstrated a significant increase in mean BG following discontinuation of an IIP; this corresponded to a significant decrease in the amount of insulin administered. This increase was sustained for a period of at least 5 days. Additionally, an independent risk factor for poor glycemic control immediately following discontinuation of an IIP was an insulin requirement of >1.7 units/hour during the previous 12 hours. Further study into transitioning off an IIP is warranted.
- ,,.Stress‐induced hyperglycemia.Crit Care Clin.2001;17:107–124.
- .Alterations in carbohydrate metabolism during stress: a review of the literature.Am J Med.1995;98:75–84.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- .Effect of an intensive glucose management protocol on the mortality of critically ill adult patients.Mayo Clin Proc.2004;79(8):992–1000.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2) effects on mortality and morbidity.Eur Heart J.2005;26:651–661.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units.Diabetes.2006;55:3151–3159.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26:56–65.
- ,,, et al.Effect of glucose‐insulin‐potassium infusion on mortality in patients with acute ST‐segment elevation myocardial infarction: the CREATE‐ECLA randomized controlled trial.JAMA.2005;293(4):437–446.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30(9):2181–2186.
- ,,, et al.,for the American Diabetes Association Professional Practice Committee. Diagnosis and classification of diabetes mellitus.Diabetes Care.2006;29(suppl 1):43–48.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Management of diabetes mellitus in hospitalized patients: efficiency and effectiveness of sliding‐scale insulin therapy.Pharmacotherapy.2006;26(10):1421–1432.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14(4):313–322.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- ,,.Evidence for strict inpatient blood glucose control: time to revise glycemic goals in hospitalized patients.Metabolism.2008;57:116–120.
Hyperglycemia and insulin resistance are common occurrences in critically ill patients, even those without a past medical history of diabetes.1, 2 This hyperglycemic state is associated with adverse outcomes, including severe infections, polyneuropathy, multiple‐organ failure, and death.3 Several studies have shown benefit in keeping patients' blood glucose (BG) tightly controlled.37 In a randomized controlled study, strict BG control (80‐110 mg/dL) with an insulin drip significantly reduced morbidity and mortality in critically ill patients.3 A recent meta‐analysis concluded that avoiding BG levels >150 mg/dL appeared to be crucial to reducing mortality in a mixed medical and surgical intensive care unit (ICU) population.7
The Diabetes Mellitus Insulin‐Glucose Infusion in Acute Myocardial Infarction study addressed the issue of tight glycemic control both acutely and chronically in 620 diabetic patients postmyocardial infarction. Patients were randomized to tight glycemic control (126‐180 mg/dL) followed by a transition to maintenance insulin or to standard care. This intervention demonstrated a sustained mortality reduction of 7.5% at 1 year.8 In contrast, the CREATE‐ECLA study showed a neutral mortality benefit of a short‐term (24‐hour) insulin infusion in postmyocardial infarction patients.9 These data demonstrate the need for clinicians to consider insulin requirements throughout the hospital stay and after discharge. To date, there are no published studies evaluating glycemic control following discontinuation of an intensive insulin protocol (IIP). Therefore, the current study was conducted to compare BG control during the use of an IIP and for the 5 days following intensive insulin therapy.
METHODS
Patient Population
This retrospective chart review was conducted at Methodist University Hospital (MUH), Memphis, TN. MUH is a 500‐bed, university‐affiliated tertiary referral hospital. The study was approved by the hospital institutional review board. From January 2006 to January 2007, a computer‐generated pharmacy report was used to identify all patients receiving the hospital‐approved IIP. Patients were included if they were 18 years old and received the IIP for 24 hours. Patients were excluded from the study if they met any of the following criteria: (1) complete BG measurements were not retrievable while the patient received the IIP or for the 5 days following discontinuation of the IIP, (2) the patient died while receiving the IIP, and (3) an endocrinologist was involved in the care of the patient.
IIP
The hospital‐approved IIP is a paper‐based, physician‐initiated, nurse‐managed protocol. Criteria required before initiating the IIP include (1) ICU admission, (2) 2 BG measurements >150 mg/dL, (3) administration of continuous exogenous glucose, and (4) absence of diabetic ketoacidosis. The goal range of the IIP is 80 to 150 mg/dL. Hourly BG measurements are initially required, but as control is achieved, measurements may be extended to every 2 hours and then every 4 hours. In general, the criteria used for transitioning off the IIP include stability during the last 12 hours. Patients were considered to be stable on the IIP if they had >70% of their glucose measurements within the goal range during the last 12 hours.
Data Collection
When inclusion criteria were met, patients' medical records were reviewed. Data collection included basic demographic information, concurrent medications, duration of IIP, amount of insulin administered during the last 12 hours of the IIP, insulin regimen post‐IIP, and BG measurements during the last 12 hours on the IIP and for a total of 5 days after the IIP was stopped (follow‐up period). For this study, hyperglycemia was defined as a BG value >150 mg/dL, significant hyperglycemia was defined as >200 mg/dL, and severe hyperglycemia was defined as >300 mg/dL. Hypoglycemia was defined as a BG value <60 mg/dL. The values of <60 mg/dL, >150 mg/dL, and >200 mg/dL were chosen on the basis of the criteria used in the MUH IIP and standard sliding‐scale protocols. A value of >300 mg/dL was used to better describe patients with hyperglycemia. Poor glycemic control following the IIP was defined as a >30% change in mean BG during the last 12 hours on the drip and on the first day after discontinuation of the drip.
Statistical Analysis
The primary objective of this study was to compare BG control during the last 12 hours of an IIP and for the 5 days following its discontinuation. Secondary objectives were to evaluate the incidence of hyperglycemia and hypoglycemia during the transition period and to identify patients at risk of poor glycemic control following discontinuation of the IIP. Continuous data are appropriately reported as the mean standard deviation or median (interquartile range), depending on the distribution. Continuous variables were compared with the Student t test or Wilcoxon rank sum test. Discrete variables were compared with chi‐square analysis and Bonferroni Correction where appropriate. For comparisons of BG during the IIP and on days 1 to 5 of the follow‐up period, repeated‐measures analysis of variance on ranks was conducted because of the distribution. These statistical analyses were performed with SigmaStat version 2.03 (Systat Software, Inc., Richmond, VA). A P value of less than 0.05 was considered significant. However, when the Bonferroni correction was used, a value of less than 0.01 was considered significant. Multivariable logistic regression was used to determine independent predictors of a greater than 30% change in the mean BG value between the last 12 hours of the IIP and the first day off the insulin drip. Potential independent variables included in the analysis were stability on protocol, requiring less than 20 units of insulin in the last 12 hours on the IIP, use of antibiotics, use of steroids, history of diabetes, and type of insulin to which the patient was transitioned (none, sliding scale, and scheduled and sliding scale). The model was built in a backwards, stepwise fashion with SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
A total of 171 patients received the IIP during the study period. Ninety‐seven patients did not meet inclusion criteria because they received the IIP for less than 24 hours. Of the 74 patients meeting inclusion criteria, 9 were excluded (5 had insufficient glucose data, 3 were cared for by an endocrinologist, and 1 died while receiving the IIP). Thus, 65 patients were included in the study.
Table 1 lists the baseline demographics for all patients and those with and without a history of diabetes mellitus (DM). The majority of the patients (n = 49) underwent a surgical procedure, with the most common procedure being coronary artery bypass graft (n = 38). Patients undergoing coronary artery bypass graft had the IIP included in their standard postoperative order set. The majority of patients were considered stable during the 12 hours prior to discontinuation of the IIP, including 23 patients with a history of DM. Of the 65 patients who were included in the study, 25 (38.5%) received a scheduled insulin order following discontinuation of the IIP, whereas 38 (58.5%) received some form of sliding‐scale insulin (SSI). Additionally, 2 (3%) patients did not receive any form of insulin order after stopping the IIP. Of those receiving scheduled insulin, 15 (60%) received neutral protamine Hagedorn, 5 (20%) received glargine, 5 (20%) received 70/30, and 1 (4%) received regular insulin. Of those receiving SSI only, the prescribed frequency was as follows: every 4 hours for 17 (45%), before meals and at bedtime for 15 (39%), every 6 hours for 5 (13%), and every 2 hours for 1 (3%).
| All Patients (n = 65) | PMH of DM (n = 36) | No PMH of DM (n = 29) | |
|---|---|---|---|
| |||
| Age, mean years SD | 62 11 | 61 10 | 64 12 |
| Male gender, n (%) | 38 (58) | 22 (61) | 16 (55.2) |
| BMI SD | 30 7.2 | 31 7 | 30 6.5 |
| Surgery, n (%) | 49 (74.2) | 27 (75) | 21 (72.4) |
| CABG, n | 38 | 22 | 16 |
| Liver transplant, n | 6 | 1 | 4 |
| Other, n | 5 | 4 | 1 |
| Last 24 hours on IIP, n (%) | |||
| Ventilator | 37 (56.9) | 22 (61.1) | 15 (51.7) |
| Antibiotics | 37 (56.9) | 20 (55.6) | 17 (58.6) |
| Vasopressors | 11 (16.9) | 5 (13.9) | 6 (20.7) |
| Hemodialysis | 8 (12.3) | 5 (13.9) | 3 (10.3) |
| Steroids | 16 (24.6) | 9 (25) | 7 (24.1) |
| Duration of IIP, mean hours SD | 72 65 | 80 78 | 62 45 |
| Insulin during last 12 hours of IIP, mean units SD | 47 37 | 51 30 | 46 45 |
| Type of insulin received following IIP, n (%) | |||
| Scheduled + sliding scale | 25 (38.5) | 19 (52.8) | 6 (20.7) |
| Sliding scale only | 38 (58.5) | 16 (44.4) | 22 (75.9) |
| None | 2 (3) | 1 (2.8) | 1 (3.4) |
| Total daily insulin following IIP, mean units SD | 28 41 | 38 49 | 17 24 |
| Patients stable on IIP | 44 (67.7) | 23 (64.8) | 21 (72.4) |
| Hospital LOS, mean days SD | 24 18 | 24 17 | 23 19 |
| Mortality, n (%) | 15 (23.1) | 5 (13.8) | 10 (34.5) |
A total of 562 glucose measurements were collected during the last 12 hours on the IIP, whereas 201 were collected during the first 12 hours immediately following the IIP. Patients demonstrated a significant increase in BG (mean standard deviation) during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP (168 50 mg/dL versus 123 26 mg/dL, P < 0.001). This corresponded to a significant decrease in the median (interquartile range) insulin administered during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP [8 (0‐18) units versus 40 (22‐65) units, P < 0.001; Figure 1]. A total of 1914 BG measurements were collected during the follow‐up period. Figure 2 shows mean BG values for all patients on the IIP compared to mean BG values for each day of the follow‐up period. There was a significant increase in mean BG measurements when the IIP was compared to each day of the follow‐up period, but there was no difference between days of the follow‐up period. Table 2 shows the proportion of patients experiencing at least 1 episode of hyperglycemia (BG > 150 mg/dL), significant hyperglycemia (BG > 200 mg/dL), severe hyperglycemia (BG > 300 mg/dL), or hypoglycemia (BG < 60 mg/dL) while receiving the IIP and during the follow‐up period. When comparing the IIP to the follow‐up period, we found a significant increase in the proportion of patients with at least 1 BG > 150 mg/dL. This was also true for patients with a BG of > 200 mg/dL.
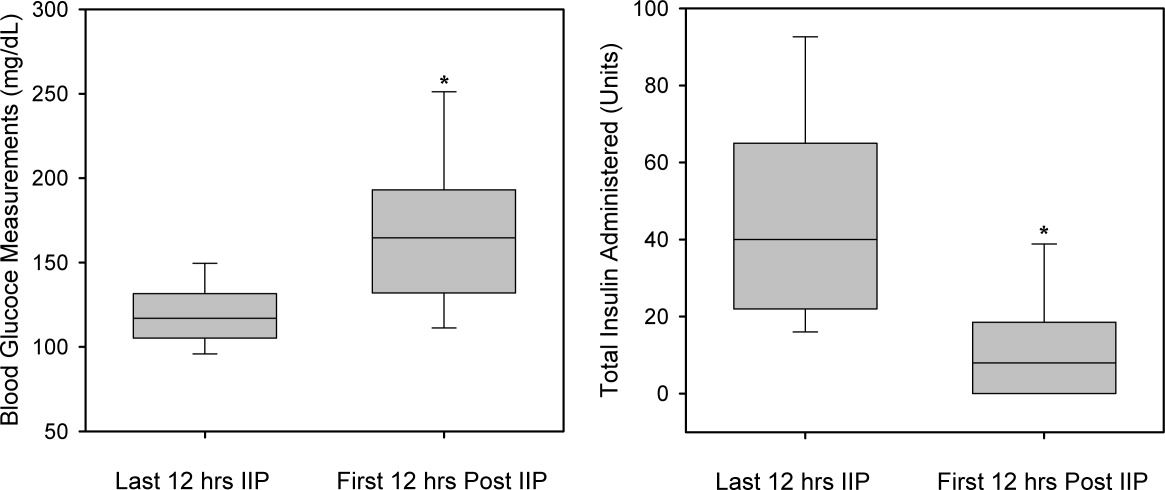
| IIP (n = 65) | Day 1 (n = 65) | Day 2 (n = 65) | Day 3 (n = 64) | Day 4 (n = 62) | Day 5 (n = 59) | |
|---|---|---|---|---|---|---|
| ||||||
| Patients with >150 mg/dL, n (%) | 33 (51) | 54 (83)* | 54 (83)* | 52 (81)* | 51 (82)* | 48 (81)* |
| Patients with >200 mg/dL, n (%) | 11 (17) | 37 (57)* | 31 (48)* | 26 (41)* | 33 (53)* | 34 (58)* |
| Patients with >300 mg/dL, n (%) | 2 (3) | 11 (17) | 7 (11) | 8 (12) | 5 (8) | 10 (17) |
| Patients with <60 mg/dL, n (%) | 6 (9) | 5 (8) | 2 (3) | 2 (3) | 2 (3) | 0 (0) |
The only independent predictor of a greater than 30% change in mean BG was the requirement for more than 20 units of insulin (>1.7 units/hour) during the last 12 hours on the IIP. The odds of a greater than 30% change was 4.62 times higher (95% confidence interval: 1.1718.17) in patients requiring more than 20 units during the last 12 hours on IIP after adjustments for stability on the protocol and past medical history of diabetes. Stability on the protocol was not identified as an independent predictor, with an adjusted odds ratio of 2.40 (95% confidence interval: 0.797.32).
DISCUSSION
This is the first study to describe glycemic control following the transition from an IIP to subcutaneous insulin. We observed that during the 5 days following discontinuation of an IIP, patients had significantly elevated mean BG values. These data are highlighted by the fact that patients received significantly less insulin during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP. Additionally, a larger than expected proportion of patients exhibited at least 1 episode of hyperglycemia during the follow‐up period. We also found that an increased insulin requirement of >1.7 units/hour during the last 12 hours of the IIP was an independent risk factor for a greater than 30% increase in mean BG on day 1 of the follow‐up period.
Increasing evidence demonstrates that the development of hyperglycemia in the hospital setting is a marker of poor clinical outcome and mortality. In fact, hyperglycemia has been associated with prolonged hospital stay, infection, disability after discharge, and death in patients on general surgical and medical wards.1012 This makes the increase in mean BG found in our study following discontinuation of the IIP a concern.
SSI with subcutaneous short‐acting insulin has been used for inpatients as the standard of care for many years. However, evidence supporting the effectiveness of SSI alone is lacking, and it is not recommended by the American Diabetes Association.13 Queale et al.14 showed that SSI regimens when used alone were associated with suboptimal glycemic control and a 3‐fold higher risk of hyperglycemic episodes.1 Two retrospective studies have also demonstrated that SSI is less effective and widely variable in comparison with proactive preventative therapy.15, 16 In the current study, 58.5% of patients received SSI alone during the follow‐up period. As indicated in Figure 1, there was a significant increase in mean BG during this time interval. The choice of an inappropriate insulin regimen might be a contributing factor to poor glycemic control.
Because only 38.5% of patients were transitioned to scheduled insulin in our study, one possible strategy to help improve glycemic control would be to transition patients to a scheduled insulin regimen. Umpierrez et al.12 conducted a prospective, multicenter randomized trial to compare the efficacy and safety of a basal‐bolus insulin regimen with that of SSI in hospitalized type 2 diabetics. These authors found that patients treated with insulin glargine and glulisine had greater improvement in glycemic control than those treated with SSI (P < 0.01).12 Interestingly, the basal‐bolus method provides a maintenance insulin regimen that is aggressively titrated upward as well as an adjustable SSI based on insulin sensitivity. Patients in the current study may have benefited from a similar approach as many did not have their scheduled insulin adjusted despite persistent hyperglycemia.
With the increasing evidence for tight glycemic control in the ICU, a standardized transition from an intensive insulin infusion to a subcutaneous basal‐bolus regimen or other scheduled regimen is needed. To date, the current study is the first to describe this transition. Based on these data, recommendations for transitioning patients off an IIP provided by Furnary and Braithwaite17 should be considered by clinicians. In fact, one of their proposed predictors for unsuccessful transition was an insulin requirement of 2 units/hour. Indeed, the only independent risk factor for poor glycemic control identified in the current study was a requirement of >20 units (>1.7 units/hour) during the last 12 hours of the IIP. Further research is required to verify the other predictors suggested by Furnary and Braithwaite. They recommended using a standardized conversion protocol to transition patients off an IIP.
More recently, Kitabchi et al.18 recommended that a BG target of less than 180 mg/dL be maintained for the hospitalized patient.18 Although our study showed a mean BG less than 180 mg/dL during the follow‐up period, the variability in these values raises concerns for individual patients.
The current study is limited by its size and retrospective nature. As with all retrospective studies, the inability to control the implementation and discontinuation of the IIP may confound the results. However, this study demonstrates a real world experience with an IIP and illustrates the difficulties with transitioning patients to a subcutaneous regimen. BG values and administered insulin were collected only for the last 12 hours on the IIP. This duration is considered appropriate as this time period is used clinically at MUH, and previous recommendations for transitioning patients suggest using a time period of 6 to 8 hours to guide the transition insulin regimen.17 In addition, data regarding the severity of illness and new onset of infections were not collected for patients in the study. Both could affect glucose control. All patients had to be in an ICU to receive the IIP, but their location during the follow‐up period varied. Although these data were not available, control of BG is a problem that should be addressed whether the patient is in the ICU or not. Another possible limitation of the study was the identification of patients with or without a past medical history of DM. The inability to identify new‐onset or previously undiagnosed DM may have affected analyses based on this variable.
CONCLUSIONS
This study demonstrated a significant increase in mean BG following discontinuation of an IIP; this corresponded to a significant decrease in the amount of insulin administered. This increase was sustained for a period of at least 5 days. Additionally, an independent risk factor for poor glycemic control immediately following discontinuation of an IIP was an insulin requirement of >1.7 units/hour during the previous 12 hours. Further study into transitioning off an IIP is warranted.
Hyperglycemia and insulin resistance are common occurrences in critically ill patients, even those without a past medical history of diabetes.1, 2 This hyperglycemic state is associated with adverse outcomes, including severe infections, polyneuropathy, multiple‐organ failure, and death.3 Several studies have shown benefit in keeping patients' blood glucose (BG) tightly controlled.37 In a randomized controlled study, strict BG control (80‐110 mg/dL) with an insulin drip significantly reduced morbidity and mortality in critically ill patients.3 A recent meta‐analysis concluded that avoiding BG levels >150 mg/dL appeared to be crucial to reducing mortality in a mixed medical and surgical intensive care unit (ICU) population.7
The Diabetes Mellitus Insulin‐Glucose Infusion in Acute Myocardial Infarction study addressed the issue of tight glycemic control both acutely and chronically in 620 diabetic patients postmyocardial infarction. Patients were randomized to tight glycemic control (126‐180 mg/dL) followed by a transition to maintenance insulin or to standard care. This intervention demonstrated a sustained mortality reduction of 7.5% at 1 year.8 In contrast, the CREATE‐ECLA study showed a neutral mortality benefit of a short‐term (24‐hour) insulin infusion in postmyocardial infarction patients.9 These data demonstrate the need for clinicians to consider insulin requirements throughout the hospital stay and after discharge. To date, there are no published studies evaluating glycemic control following discontinuation of an intensive insulin protocol (IIP). Therefore, the current study was conducted to compare BG control during the use of an IIP and for the 5 days following intensive insulin therapy.
METHODS
Patient Population
This retrospective chart review was conducted at Methodist University Hospital (MUH), Memphis, TN. MUH is a 500‐bed, university‐affiliated tertiary referral hospital. The study was approved by the hospital institutional review board. From January 2006 to January 2007, a computer‐generated pharmacy report was used to identify all patients receiving the hospital‐approved IIP. Patients were included if they were 18 years old and received the IIP for 24 hours. Patients were excluded from the study if they met any of the following criteria: (1) complete BG measurements were not retrievable while the patient received the IIP or for the 5 days following discontinuation of the IIP, (2) the patient died while receiving the IIP, and (3) an endocrinologist was involved in the care of the patient.
IIP
The hospital‐approved IIP is a paper‐based, physician‐initiated, nurse‐managed protocol. Criteria required before initiating the IIP include (1) ICU admission, (2) 2 BG measurements >150 mg/dL, (3) administration of continuous exogenous glucose, and (4) absence of diabetic ketoacidosis. The goal range of the IIP is 80 to 150 mg/dL. Hourly BG measurements are initially required, but as control is achieved, measurements may be extended to every 2 hours and then every 4 hours. In general, the criteria used for transitioning off the IIP include stability during the last 12 hours. Patients were considered to be stable on the IIP if they had >70% of their glucose measurements within the goal range during the last 12 hours.
Data Collection
When inclusion criteria were met, patients' medical records were reviewed. Data collection included basic demographic information, concurrent medications, duration of IIP, amount of insulin administered during the last 12 hours of the IIP, insulin regimen post‐IIP, and BG measurements during the last 12 hours on the IIP and for a total of 5 days after the IIP was stopped (follow‐up period). For this study, hyperglycemia was defined as a BG value >150 mg/dL, significant hyperglycemia was defined as >200 mg/dL, and severe hyperglycemia was defined as >300 mg/dL. Hypoglycemia was defined as a BG value <60 mg/dL. The values of <60 mg/dL, >150 mg/dL, and >200 mg/dL were chosen on the basis of the criteria used in the MUH IIP and standard sliding‐scale protocols. A value of >300 mg/dL was used to better describe patients with hyperglycemia. Poor glycemic control following the IIP was defined as a >30% change in mean BG during the last 12 hours on the drip and on the first day after discontinuation of the drip.
Statistical Analysis
The primary objective of this study was to compare BG control during the last 12 hours of an IIP and for the 5 days following its discontinuation. Secondary objectives were to evaluate the incidence of hyperglycemia and hypoglycemia during the transition period and to identify patients at risk of poor glycemic control following discontinuation of the IIP. Continuous data are appropriately reported as the mean standard deviation or median (interquartile range), depending on the distribution. Continuous variables were compared with the Student t test or Wilcoxon rank sum test. Discrete variables were compared with chi‐square analysis and Bonferroni Correction where appropriate. For comparisons of BG during the IIP and on days 1 to 5 of the follow‐up period, repeated‐measures analysis of variance on ranks was conducted because of the distribution. These statistical analyses were performed with SigmaStat version 2.03 (Systat Software, Inc., Richmond, VA). A P value of less than 0.05 was considered significant. However, when the Bonferroni correction was used, a value of less than 0.01 was considered significant. Multivariable logistic regression was used to determine independent predictors of a greater than 30% change in the mean BG value between the last 12 hours of the IIP and the first day off the insulin drip. Potential independent variables included in the analysis were stability on protocol, requiring less than 20 units of insulin in the last 12 hours on the IIP, use of antibiotics, use of steroids, history of diabetes, and type of insulin to which the patient was transitioned (none, sliding scale, and scheduled and sliding scale). The model was built in a backwards, stepwise fashion with SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
A total of 171 patients received the IIP during the study period. Ninety‐seven patients did not meet inclusion criteria because they received the IIP for less than 24 hours. Of the 74 patients meeting inclusion criteria, 9 were excluded (5 had insufficient glucose data, 3 were cared for by an endocrinologist, and 1 died while receiving the IIP). Thus, 65 patients were included in the study.
Table 1 lists the baseline demographics for all patients and those with and without a history of diabetes mellitus (DM). The majority of the patients (n = 49) underwent a surgical procedure, with the most common procedure being coronary artery bypass graft (n = 38). Patients undergoing coronary artery bypass graft had the IIP included in their standard postoperative order set. The majority of patients were considered stable during the 12 hours prior to discontinuation of the IIP, including 23 patients with a history of DM. Of the 65 patients who were included in the study, 25 (38.5%) received a scheduled insulin order following discontinuation of the IIP, whereas 38 (58.5%) received some form of sliding‐scale insulin (SSI). Additionally, 2 (3%) patients did not receive any form of insulin order after stopping the IIP. Of those receiving scheduled insulin, 15 (60%) received neutral protamine Hagedorn, 5 (20%) received glargine, 5 (20%) received 70/30, and 1 (4%) received regular insulin. Of those receiving SSI only, the prescribed frequency was as follows: every 4 hours for 17 (45%), before meals and at bedtime for 15 (39%), every 6 hours for 5 (13%), and every 2 hours for 1 (3%).
| All Patients (n = 65) | PMH of DM (n = 36) | No PMH of DM (n = 29) | |
|---|---|---|---|
| |||
| Age, mean years SD | 62 11 | 61 10 | 64 12 |
| Male gender, n (%) | 38 (58) | 22 (61) | 16 (55.2) |
| BMI SD | 30 7.2 | 31 7 | 30 6.5 |
| Surgery, n (%) | 49 (74.2) | 27 (75) | 21 (72.4) |
| CABG, n | 38 | 22 | 16 |
| Liver transplant, n | 6 | 1 | 4 |
| Other, n | 5 | 4 | 1 |
| Last 24 hours on IIP, n (%) | |||
| Ventilator | 37 (56.9) | 22 (61.1) | 15 (51.7) |
| Antibiotics | 37 (56.9) | 20 (55.6) | 17 (58.6) |
| Vasopressors | 11 (16.9) | 5 (13.9) | 6 (20.7) |
| Hemodialysis | 8 (12.3) | 5 (13.9) | 3 (10.3) |
| Steroids | 16 (24.6) | 9 (25) | 7 (24.1) |
| Duration of IIP, mean hours SD | 72 65 | 80 78 | 62 45 |
| Insulin during last 12 hours of IIP, mean units SD | 47 37 | 51 30 | 46 45 |
| Type of insulin received following IIP, n (%) | |||
| Scheduled + sliding scale | 25 (38.5) | 19 (52.8) | 6 (20.7) |
| Sliding scale only | 38 (58.5) | 16 (44.4) | 22 (75.9) |
| None | 2 (3) | 1 (2.8) | 1 (3.4) |
| Total daily insulin following IIP, mean units SD | 28 41 | 38 49 | 17 24 |
| Patients stable on IIP | 44 (67.7) | 23 (64.8) | 21 (72.4) |
| Hospital LOS, mean days SD | 24 18 | 24 17 | 23 19 |
| Mortality, n (%) | 15 (23.1) | 5 (13.8) | 10 (34.5) |
A total of 562 glucose measurements were collected during the last 12 hours on the IIP, whereas 201 were collected during the first 12 hours immediately following the IIP. Patients demonstrated a significant increase in BG (mean standard deviation) during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP (168 50 mg/dL versus 123 26 mg/dL, P < 0.001). This corresponded to a significant decrease in the median (interquartile range) insulin administered during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP [8 (0‐18) units versus 40 (22‐65) units, P < 0.001; Figure 1]. A total of 1914 BG measurements were collected during the follow‐up period. Figure 2 shows mean BG values for all patients on the IIP compared to mean BG values for each day of the follow‐up period. There was a significant increase in mean BG measurements when the IIP was compared to each day of the follow‐up period, but there was no difference between days of the follow‐up period. Table 2 shows the proportion of patients experiencing at least 1 episode of hyperglycemia (BG > 150 mg/dL), significant hyperglycemia (BG > 200 mg/dL), severe hyperglycemia (BG > 300 mg/dL), or hypoglycemia (BG < 60 mg/dL) while receiving the IIP and during the follow‐up period. When comparing the IIP to the follow‐up period, we found a significant increase in the proportion of patients with at least 1 BG > 150 mg/dL. This was also true for patients with a BG of > 200 mg/dL.
| IIP (n = 65) | Day 1 (n = 65) | Day 2 (n = 65) | Day 3 (n = 64) | Day 4 (n = 62) | Day 5 (n = 59) | |
|---|---|---|---|---|---|---|
| ||||||
| Patients with >150 mg/dL, n (%) | 33 (51) | 54 (83)* | 54 (83)* | 52 (81)* | 51 (82)* | 48 (81)* |
| Patients with >200 mg/dL, n (%) | 11 (17) | 37 (57)* | 31 (48)* | 26 (41)* | 33 (53)* | 34 (58)* |
| Patients with >300 mg/dL, n (%) | 2 (3) | 11 (17) | 7 (11) | 8 (12) | 5 (8) | 10 (17) |
| Patients with <60 mg/dL, n (%) | 6 (9) | 5 (8) | 2 (3) | 2 (3) | 2 (3) | 0 (0) |
The only independent predictor of a greater than 30% change in mean BG was the requirement for more than 20 units of insulin (>1.7 units/hour) during the last 12 hours on the IIP. The odds of a greater than 30% change was 4.62 times higher (95% confidence interval: 1.1718.17) in patients requiring more than 20 units during the last 12 hours on IIP after adjustments for stability on the protocol and past medical history of diabetes. Stability on the protocol was not identified as an independent predictor, with an adjusted odds ratio of 2.40 (95% confidence interval: 0.797.32).
DISCUSSION
This is the first study to describe glycemic control following the transition from an IIP to subcutaneous insulin. We observed that during the 5 days following discontinuation of an IIP, patients had significantly elevated mean BG values. These data are highlighted by the fact that patients received significantly less insulin during the first 12 hours of the follow‐up period versus the last 12 hours of the IIP. Additionally, a larger than expected proportion of patients exhibited at least 1 episode of hyperglycemia during the follow‐up period. We also found that an increased insulin requirement of >1.7 units/hour during the last 12 hours of the IIP was an independent risk factor for a greater than 30% increase in mean BG on day 1 of the follow‐up period.
Increasing evidence demonstrates that the development of hyperglycemia in the hospital setting is a marker of poor clinical outcome and mortality. In fact, hyperglycemia has been associated with prolonged hospital stay, infection, disability after discharge, and death in patients on general surgical and medical wards.1012 This makes the increase in mean BG found in our study following discontinuation of the IIP a concern.
SSI with subcutaneous short‐acting insulin has been used for inpatients as the standard of care for many years. However, evidence supporting the effectiveness of SSI alone is lacking, and it is not recommended by the American Diabetes Association.13 Queale et al.14 showed that SSI regimens when used alone were associated with suboptimal glycemic control and a 3‐fold higher risk of hyperglycemic episodes.1 Two retrospective studies have also demonstrated that SSI is less effective and widely variable in comparison with proactive preventative therapy.15, 16 In the current study, 58.5% of patients received SSI alone during the follow‐up period. As indicated in Figure 1, there was a significant increase in mean BG during this time interval. The choice of an inappropriate insulin regimen might be a contributing factor to poor glycemic control.
Because only 38.5% of patients were transitioned to scheduled insulin in our study, one possible strategy to help improve glycemic control would be to transition patients to a scheduled insulin regimen. Umpierrez et al.12 conducted a prospective, multicenter randomized trial to compare the efficacy and safety of a basal‐bolus insulin regimen with that of SSI in hospitalized type 2 diabetics. These authors found that patients treated with insulin glargine and glulisine had greater improvement in glycemic control than those treated with SSI (P < 0.01).12 Interestingly, the basal‐bolus method provides a maintenance insulin regimen that is aggressively titrated upward as well as an adjustable SSI based on insulin sensitivity. Patients in the current study may have benefited from a similar approach as many did not have their scheduled insulin adjusted despite persistent hyperglycemia.
With the increasing evidence for tight glycemic control in the ICU, a standardized transition from an intensive insulin infusion to a subcutaneous basal‐bolus regimen or other scheduled regimen is needed. To date, the current study is the first to describe this transition. Based on these data, recommendations for transitioning patients off an IIP provided by Furnary and Braithwaite17 should be considered by clinicians. In fact, one of their proposed predictors for unsuccessful transition was an insulin requirement of 2 units/hour. Indeed, the only independent risk factor for poor glycemic control identified in the current study was a requirement of >20 units (>1.7 units/hour) during the last 12 hours of the IIP. Further research is required to verify the other predictors suggested by Furnary and Braithwaite. They recommended using a standardized conversion protocol to transition patients off an IIP.
More recently, Kitabchi et al.18 recommended that a BG target of less than 180 mg/dL be maintained for the hospitalized patient.18 Although our study showed a mean BG less than 180 mg/dL during the follow‐up period, the variability in these values raises concerns for individual patients.
The current study is limited by its size and retrospective nature. As with all retrospective studies, the inability to control the implementation and discontinuation of the IIP may confound the results. However, this study demonstrates a real world experience with an IIP and illustrates the difficulties with transitioning patients to a subcutaneous regimen. BG values and administered insulin were collected only for the last 12 hours on the IIP. This duration is considered appropriate as this time period is used clinically at MUH, and previous recommendations for transitioning patients suggest using a time period of 6 to 8 hours to guide the transition insulin regimen.17 In addition, data regarding the severity of illness and new onset of infections were not collected for patients in the study. Both could affect glucose control. All patients had to be in an ICU to receive the IIP, but their location during the follow‐up period varied. Although these data were not available, control of BG is a problem that should be addressed whether the patient is in the ICU or not. Another possible limitation of the study was the identification of patients with or without a past medical history of DM. The inability to identify new‐onset or previously undiagnosed DM may have affected analyses based on this variable.
CONCLUSIONS
This study demonstrated a significant increase in mean BG following discontinuation of an IIP; this corresponded to a significant decrease in the amount of insulin administered. This increase was sustained for a period of at least 5 days. Additionally, an independent risk factor for poor glycemic control immediately following discontinuation of an IIP was an insulin requirement of >1.7 units/hour during the previous 12 hours. Further study into transitioning off an IIP is warranted.
- ,,.Stress‐induced hyperglycemia.Crit Care Clin.2001;17:107–124.
- .Alterations in carbohydrate metabolism during stress: a review of the literature.Am J Med.1995;98:75–84.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- .Effect of an intensive glucose management protocol on the mortality of critically ill adult patients.Mayo Clin Proc.2004;79(8):992–1000.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2) effects on mortality and morbidity.Eur Heart J.2005;26:651–661.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units.Diabetes.2006;55:3151–3159.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26:56–65.
- ,,, et al.Effect of glucose‐insulin‐potassium infusion on mortality in patients with acute ST‐segment elevation myocardial infarction: the CREATE‐ECLA randomized controlled trial.JAMA.2005;293(4):437–446.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30(9):2181–2186.
- ,,, et al.,for the American Diabetes Association Professional Practice Committee. Diagnosis and classification of diabetes mellitus.Diabetes Care.2006;29(suppl 1):43–48.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Management of diabetes mellitus in hospitalized patients: efficiency and effectiveness of sliding‐scale insulin therapy.Pharmacotherapy.2006;26(10):1421–1432.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14(4):313–322.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- ,,.Evidence for strict inpatient blood glucose control: time to revise glycemic goals in hospitalized patients.Metabolism.2008;57:116–120.
- ,,.Stress‐induced hyperglycemia.Crit Care Clin.2001;17:107–124.
- .Alterations in carbohydrate metabolism during stress: a review of the literature.Am J Med.1995;98:75–84.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- .Effect of an intensive glucose management protocol on the mortality of critically ill adult patients.Mayo Clin Proc.2004;79(8):992–1000.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2) effects on mortality and morbidity.Eur Heart J.2005;26:651–661.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units.Diabetes.2006;55:3151–3159.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26:56–65.
- ,,, et al.Effect of glucose‐insulin‐potassium infusion on mortality in patients with acute ST‐segment elevation myocardial infarction: the CREATE‐ECLA randomized controlled trial.JAMA.2005;293(4):437–446.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30(9):2181–2186.
- ,,, et al.,for the American Diabetes Association Professional Practice Committee. Diagnosis and classification of diabetes mellitus.Diabetes Care.2006;29(suppl 1):43–48.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157(5):545–552.
- ,,,,.Management of diabetes mellitus in hospitalized patients: efficiency and effectiveness of sliding‐scale insulin therapy.Pharmacotherapy.2006;26(10):1421–1432.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14(4):313–322.
- ,.Effects of outcome on in‐hospital transition from intravenous insulin infusion to subcutaneous therapy.Am J Cardiol.2006;98:557–564.
- ,,.Evidence for strict inpatient blood glucose control: time to revise glycemic goals in hospitalized patients.Metabolism.2008;57:116–120.
Copyright © 2009 Society of Hospital Medicine