User login
AGA Clinical Practice Update: Expert review on atrophic gastritis
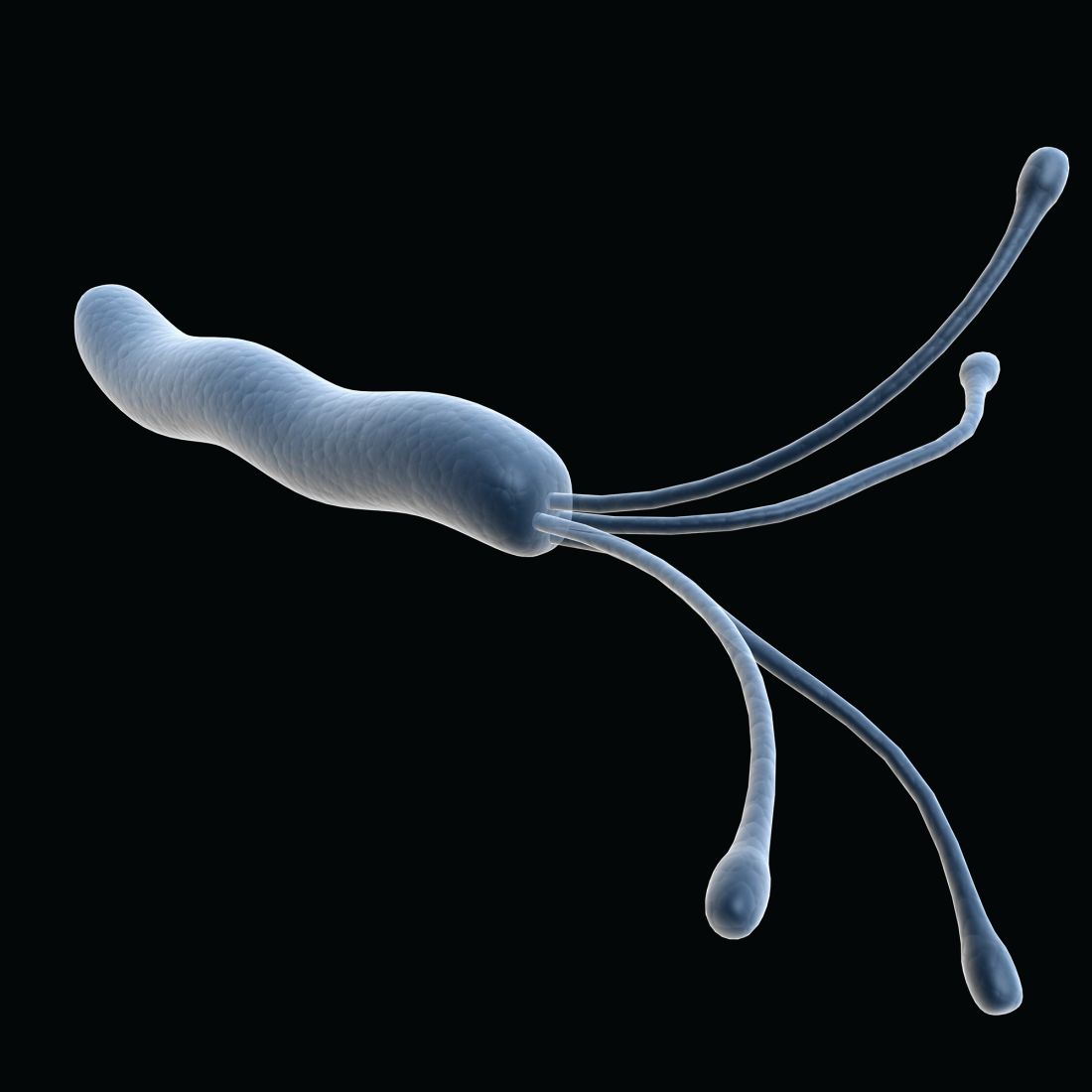
A new clinical practice update expert review for the diagnosis and management of atrophic gastritis (AG) from the American Gastroenterological Association focuses on cases linked to Helicobacter pylori infection or autoimmunity.
This update addresses a sparsity of guidelines for AG in the United States and should be seen as complementary to the AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia, according to the authors led by Shailja C. Shah, MD, MPH, of the gastroenterology section at Veterans Affairs San Diego Healthcare System and the division of gastroenterology at the University of California, San Diego.
The 2020 guidelines didn’t specifically discuss diagnosis and management of AG; however, a diagnosis of intestinal metaplasia based on gastric histopathology indicates the presence AG since metaplasia occurs in atrophic mucosa. Nevertheless, AG often goes unmentioned in histopathology reports. Such omissions are important because AG is an important stage in the potential development of gastric cancer.
AG is believed to result from genetic and environmental factors. The two primary triggers for the condition are H. pylori infection (HpAG) and autoimmunity (AIG). The condition results from chronic inflammation and replacement of normal gastric glandular structures with connective tissue or nonnative epithelium. It can proceed to other precancerous conditions, including gastric intestinal metaplasia and dysplasia. An estimated 15% of the U.S. population has AG, according to the authors, although this prevalence could be higher in populations with higher rates of H. pylori infection. AIG is rare, occurring in 0.5%-2% of the U.S. population.
Among individuals with AG, 0.1%-0.3% per year go on to develop gastric adenocarcinoma, though additional factors could heighten this risk. Furthermore, 0.4%-0.7% per year go on develop type 1 neuroendocrine tumors.
HpAG and AIG have different patterns of mucosal involvement. During diagnosis, the authors advised careful mucosal visualization with air insufflation and mucosal cleansing. High-definition white-light endoscopy is more sensitive than traditional WLE in the identification of premalignant mucosal changes.
AG diagnosis should be confirmed by histopathology. The updated Sydney protocol should be used to obtain biopsies, and serum pepsinogens can be used to identify extensive atrophy, though this testing is not generally available in the United States for clinical use. When histology results are suggestive of AIG, the presence of parietal cell antibodies and intrinsic factor antibodies can contribute to a diagnosis, although the former can be prone to false positives because of H. pylori infection, and the latter has low sensitivity.
Patients identified with AG should be tested for H. pylori and treated for infection, followed by nonserologic testing to confirm treatment success. If H. pylori is present, successful eradication may allow for reversal of AG to normal gastric mucosa; however, patients may have irreversible changes. This could leave them at elevated risk of further progression, though elimination of H. pylori does appear to blunt that risk somewhat.
Neoplastic complications from AG are rare, and the benefits of surveillance among those with AG have not been demonstrated in prospective trials. Observational trials show that severe AG is associated with greater risk of gastric adenocarcinoma, and other factors, such as comorbidities and patient values and priorities, should inform decision-making. When called for, providers should consider surveillance endoscopies every 3 years, though the authors noted that the optimal surveillance interval is unknown. Factors such as the quality of the original endoscopy, family history of gastric cancer, and a history of immigration from regions with high rates of H. pylori infection may impact decisions on surveillance intervals.
AG can lead to iron or vitamin B12 deficiency, so patients with AG, especially those with corpus-predominant AG, should be evaluated for both. AG should also be considered as a differential diagnosis in patients presenting with either deficiency.
A diagnosis of AIG should be accompanied by screening for autoimmune thyroid disease, and type 1 diabetes or Addison’s disease may also be indicated if clinical presentation is consistent.
Because AG is commonly underdiagnosed, the authors advise that gastroenterologists and pathologists should improve coordination to maximize diagnosis of the condition, and they call for comparative clinical trials to improve risk stratification algorithms and surveillance strategies.
The authors disclose no relevant conflicts of interest.
A new clinical practice update expert review for the diagnosis and management of atrophic gastritis (AG) from the American Gastroenterological Association focuses on cases linked to Helicobacter pylori infection or autoimmunity.
This update addresses a sparsity of guidelines for AG in the United States and should be seen as complementary to the AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia, according to the authors led by Shailja C. Shah, MD, MPH, of the gastroenterology section at Veterans Affairs San Diego Healthcare System and the division of gastroenterology at the University of California, San Diego.
The 2020 guidelines didn’t specifically discuss diagnosis and management of AG; however, a diagnosis of intestinal metaplasia based on gastric histopathology indicates the presence AG since metaplasia occurs in atrophic mucosa. Nevertheless, AG often goes unmentioned in histopathology reports. Such omissions are important because AG is an important stage in the potential development of gastric cancer.
AG is believed to result from genetic and environmental factors. The two primary triggers for the condition are H. pylori infection (HpAG) and autoimmunity (AIG). The condition results from chronic inflammation and replacement of normal gastric glandular structures with connective tissue or nonnative epithelium. It can proceed to other precancerous conditions, including gastric intestinal metaplasia and dysplasia. An estimated 15% of the U.S. population has AG, according to the authors, although this prevalence could be higher in populations with higher rates of H. pylori infection. AIG is rare, occurring in 0.5%-2% of the U.S. population.
Among individuals with AG, 0.1%-0.3% per year go on to develop gastric adenocarcinoma, though additional factors could heighten this risk. Furthermore, 0.4%-0.7% per year go on develop type 1 neuroendocrine tumors.
HpAG and AIG have different patterns of mucosal involvement. During diagnosis, the authors advised careful mucosal visualization with air insufflation and mucosal cleansing. High-definition white-light endoscopy is more sensitive than traditional WLE in the identification of premalignant mucosal changes.
AG diagnosis should be confirmed by histopathology. The updated Sydney protocol should be used to obtain biopsies, and serum pepsinogens can be used to identify extensive atrophy, though this testing is not generally available in the United States for clinical use. When histology results are suggestive of AIG, the presence of parietal cell antibodies and intrinsic factor antibodies can contribute to a diagnosis, although the former can be prone to false positives because of H. pylori infection, and the latter has low sensitivity.
Patients identified with AG should be tested for H. pylori and treated for infection, followed by nonserologic testing to confirm treatment success. If H. pylori is present, successful eradication may allow for reversal of AG to normal gastric mucosa; however, patients may have irreversible changes. This could leave them at elevated risk of further progression, though elimination of H. pylori does appear to blunt that risk somewhat.
Neoplastic complications from AG are rare, and the benefits of surveillance among those with AG have not been demonstrated in prospective trials. Observational trials show that severe AG is associated with greater risk of gastric adenocarcinoma, and other factors, such as comorbidities and patient values and priorities, should inform decision-making. When called for, providers should consider surveillance endoscopies every 3 years, though the authors noted that the optimal surveillance interval is unknown. Factors such as the quality of the original endoscopy, family history of gastric cancer, and a history of immigration from regions with high rates of H. pylori infection may impact decisions on surveillance intervals.
AG can lead to iron or vitamin B12 deficiency, so patients with AG, especially those with corpus-predominant AG, should be evaluated for both. AG should also be considered as a differential diagnosis in patients presenting with either deficiency.
A diagnosis of AIG should be accompanied by screening for autoimmune thyroid disease, and type 1 diabetes or Addison’s disease may also be indicated if clinical presentation is consistent.
Because AG is commonly underdiagnosed, the authors advise that gastroenterologists and pathologists should improve coordination to maximize diagnosis of the condition, and they call for comparative clinical trials to improve risk stratification algorithms and surveillance strategies.
The authors disclose no relevant conflicts of interest.
A new clinical practice update expert review for the diagnosis and management of atrophic gastritis (AG) from the American Gastroenterological Association focuses on cases linked to Helicobacter pylori infection or autoimmunity.
This update addresses a sparsity of guidelines for AG in the United States and should be seen as complementary to the AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia, according to the authors led by Shailja C. Shah, MD, MPH, of the gastroenterology section at Veterans Affairs San Diego Healthcare System and the division of gastroenterology at the University of California, San Diego.
The 2020 guidelines didn’t specifically discuss diagnosis and management of AG; however, a diagnosis of intestinal metaplasia based on gastric histopathology indicates the presence AG since metaplasia occurs in atrophic mucosa. Nevertheless, AG often goes unmentioned in histopathology reports. Such omissions are important because AG is an important stage in the potential development of gastric cancer.
AG is believed to result from genetic and environmental factors. The two primary triggers for the condition are H. pylori infection (HpAG) and autoimmunity (AIG). The condition results from chronic inflammation and replacement of normal gastric glandular structures with connective tissue or nonnative epithelium. It can proceed to other precancerous conditions, including gastric intestinal metaplasia and dysplasia. An estimated 15% of the U.S. population has AG, according to the authors, although this prevalence could be higher in populations with higher rates of H. pylori infection. AIG is rare, occurring in 0.5%-2% of the U.S. population.
Among individuals with AG, 0.1%-0.3% per year go on to develop gastric adenocarcinoma, though additional factors could heighten this risk. Furthermore, 0.4%-0.7% per year go on develop type 1 neuroendocrine tumors.
HpAG and AIG have different patterns of mucosal involvement. During diagnosis, the authors advised careful mucosal visualization with air insufflation and mucosal cleansing. High-definition white-light endoscopy is more sensitive than traditional WLE in the identification of premalignant mucosal changes.
AG diagnosis should be confirmed by histopathology. The updated Sydney protocol should be used to obtain biopsies, and serum pepsinogens can be used to identify extensive atrophy, though this testing is not generally available in the United States for clinical use. When histology results are suggestive of AIG, the presence of parietal cell antibodies and intrinsic factor antibodies can contribute to a diagnosis, although the former can be prone to false positives because of H. pylori infection, and the latter has low sensitivity.
Patients identified with AG should be tested for H. pylori and treated for infection, followed by nonserologic testing to confirm treatment success. If H. pylori is present, successful eradication may allow for reversal of AG to normal gastric mucosa; however, patients may have irreversible changes. This could leave them at elevated risk of further progression, though elimination of H. pylori does appear to blunt that risk somewhat.
Neoplastic complications from AG are rare, and the benefits of surveillance among those with AG have not been demonstrated in prospective trials. Observational trials show that severe AG is associated with greater risk of gastric adenocarcinoma, and other factors, such as comorbidities and patient values and priorities, should inform decision-making. When called for, providers should consider surveillance endoscopies every 3 years, though the authors noted that the optimal surveillance interval is unknown. Factors such as the quality of the original endoscopy, family history of gastric cancer, and a history of immigration from regions with high rates of H. pylori infection may impact decisions on surveillance intervals.
AG can lead to iron or vitamin B12 deficiency, so patients with AG, especially those with corpus-predominant AG, should be evaluated for both. AG should also be considered as a differential diagnosis in patients presenting with either deficiency.
A diagnosis of AIG should be accompanied by screening for autoimmune thyroid disease, and type 1 diabetes or Addison’s disease may also be indicated if clinical presentation is consistent.
Because AG is commonly underdiagnosed, the authors advise that gastroenterologists and pathologists should improve coordination to maximize diagnosis of the condition, and they call for comparative clinical trials to improve risk stratification algorithms and surveillance strategies.
The authors disclose no relevant conflicts of interest.
FROM GASTROENTEROLOGY
The Barcelona baseline risk score may predict long-term MS course
The high-risk group had the shortest time to progression to an Expanded Disability Status Score (EDSS) of 3.0, and were also more likely to progress by MRI and quality of life measures.
The ranking is based on sex, age at the first clinically isolated syndrome, CIS topography, the number of T2 lesions, and the presence of infratentorial and spinal cord lesions, contrast-enhancing lesions, and oligoclonal bands.
“What we wanted to do is merge all of the different prognostic variables for one single patient into one single score,” said Mar Tintoré, MD, PhD, in an interview. Dr. Tintoré is a professor of neurology at Vall d’Hebron University Hospital in Barcelona and a senior consultant at the Multiple Sclerosis Centre of Catalonia (Cemcat). Dr. Tintoré presented the results of the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
The three groups had different outcomes in MRI, clinical factors, and MRI scans, and quality of life outcomes over the course of their disease. “So this is a confirmation that this classification at baseline is really meaningful,” Dr. Tintoré said in an interview.
She attributed the success of the model to its reliance on multiple factors, but it is also designed to be simple to use. “We have been trying to use it with simple factors, [information] that you always have, like age, sex, gender, number of lesions, and topography of the region. Everybody has this information at their desk.”
Proof of concept
The study validates the approach that neurologists already utilize, according to Patricia Coyle, MD, who moderated the session. “I think the prospective study is a really unique and powerful concept,” said Dr. Coyle, who is a professor of neurology, vice chair of neurology, and director of the Stony Brook (N.Y.) Comprehensive Care Center.
The new study “kind of confirmed their concept of the initial rating, judging long-term disability progression measures in subsets. They also looked at brain atrophy, they looked at gray-matter atrophy, and that also traveled with these three different groups of severity. So it kind of gives value to looking at prognostic indicators at a first attack,” said Dr. Coyle.
The results also validate the Barcelona group’s heavy emphasis on MRI, which Dr. Coyle pointed out is common practice. “If the brain MRI looks very bad, if there are a lot of spinal cord lesions, then that’s somebody we’re much more worried about.”
Once the model is confirmed in other cohorts, the researchers plan to release the model as a generally available algorithm that clinicians could use to help manage patients. Dr. Tintoré pointed out the debate over when to begin a patient on high-efficacy disease-modifying therapies. That choice depends on a lot of factors, including patient choice, safety, and comorbidities. “But knowing that your patient is at risk of having a bad prognosis is something that is helpful” in that decision-making process, she said.
Predicting time to EDSS 3.0
The researchers used the Barcelona CIS cohort to build a Weibull survival regression in order to estimate the median time to EDSS 3.0. The model produced three categories with widely divergent predicted times from CIS to EDSS 3.0: low risk, medium risk, and high risk.
In the current report, the researchers compared the model to a “360 degree” measure of measures in 1,308 patients, including clinical milestones (McDonald 2017 MS, confirmed secondary progressive MS, progression independent of relapse activity [PIRA], EDSS disability, number of T2 MRI lesions and brain atrophy, and Patient Reported Outcomes for MS [walking speed, manual dexterity, processing speed, and contrast sensitivity]).
At 30 years after CIS, the risk of reaching EDSS 3.0 was higher in the medium risk (hazard ratio, 3.0 versus low risk) and in the high risk group (HR, 8.3 versus low risk). At 10 years, the low risk group had a 40% risk of fulfilling McDonald 2017 criteria, versus 89% in the intermediate group, and 98% in the high risk group. A similar relationship was seen for SPMS (1%, 8%, 16%) and PIRA (17%, 26%, 35%).
At 10 years, the estimated accumulated T2 lesions was 7 in the low-risk group (95% CI, 5-9), 15 in the medium-risk group (95% CI, 12-17), and 21 in the high-risk group (95% CI, 15-27).
Compared with the low- and medium-risk groups, the high-risk group had lower brain parenchymal fraction and gray-matter fraction at 5 years. They also experienced higher stigma, had worse perception of upper and lower limb function as measured by Neuro QoL, and had worse cognitive performance.
Dr. Tintoré has received compensation for consulting services and speaking honoraria from Aimirall, Bayer Schering Pharma, Biogen-Idec, Genzyme, Janssen, Merck-Serono, Novartis, Roche, Sanofi-Aventis, Teva Pharmaceuticals, and Viela Bio. Dr. Coyle has no relevant disclosures.
The high-risk group had the shortest time to progression to an Expanded Disability Status Score (EDSS) of 3.0, and were also more likely to progress by MRI and quality of life measures.
The ranking is based on sex, age at the first clinically isolated syndrome, CIS topography, the number of T2 lesions, and the presence of infratentorial and spinal cord lesions, contrast-enhancing lesions, and oligoclonal bands.
“What we wanted to do is merge all of the different prognostic variables for one single patient into one single score,” said Mar Tintoré, MD, PhD, in an interview. Dr. Tintoré is a professor of neurology at Vall d’Hebron University Hospital in Barcelona and a senior consultant at the Multiple Sclerosis Centre of Catalonia (Cemcat). Dr. Tintoré presented the results of the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
The three groups had different outcomes in MRI, clinical factors, and MRI scans, and quality of life outcomes over the course of their disease. “So this is a confirmation that this classification at baseline is really meaningful,” Dr. Tintoré said in an interview.
She attributed the success of the model to its reliance on multiple factors, but it is also designed to be simple to use. “We have been trying to use it with simple factors, [information] that you always have, like age, sex, gender, number of lesions, and topography of the region. Everybody has this information at their desk.”
Proof of concept
The study validates the approach that neurologists already utilize, according to Patricia Coyle, MD, who moderated the session. “I think the prospective study is a really unique and powerful concept,” said Dr. Coyle, who is a professor of neurology, vice chair of neurology, and director of the Stony Brook (N.Y.) Comprehensive Care Center.
The new study “kind of confirmed their concept of the initial rating, judging long-term disability progression measures in subsets. They also looked at brain atrophy, they looked at gray-matter atrophy, and that also traveled with these three different groups of severity. So it kind of gives value to looking at prognostic indicators at a first attack,” said Dr. Coyle.
The results also validate the Barcelona group’s heavy emphasis on MRI, which Dr. Coyle pointed out is common practice. “If the brain MRI looks very bad, if there are a lot of spinal cord lesions, then that’s somebody we’re much more worried about.”
Once the model is confirmed in other cohorts, the researchers plan to release the model as a generally available algorithm that clinicians could use to help manage patients. Dr. Tintoré pointed out the debate over when to begin a patient on high-efficacy disease-modifying therapies. That choice depends on a lot of factors, including patient choice, safety, and comorbidities. “But knowing that your patient is at risk of having a bad prognosis is something that is helpful” in that decision-making process, she said.
Predicting time to EDSS 3.0
The researchers used the Barcelona CIS cohort to build a Weibull survival regression in order to estimate the median time to EDSS 3.0. The model produced three categories with widely divergent predicted times from CIS to EDSS 3.0: low risk, medium risk, and high risk.
In the current report, the researchers compared the model to a “360 degree” measure of measures in 1,308 patients, including clinical milestones (McDonald 2017 MS, confirmed secondary progressive MS, progression independent of relapse activity [PIRA], EDSS disability, number of T2 MRI lesions and brain atrophy, and Patient Reported Outcomes for MS [walking speed, manual dexterity, processing speed, and contrast sensitivity]).
At 30 years after CIS, the risk of reaching EDSS 3.0 was higher in the medium risk (hazard ratio, 3.0 versus low risk) and in the high risk group (HR, 8.3 versus low risk). At 10 years, the low risk group had a 40% risk of fulfilling McDonald 2017 criteria, versus 89% in the intermediate group, and 98% in the high risk group. A similar relationship was seen for SPMS (1%, 8%, 16%) and PIRA (17%, 26%, 35%).
At 10 years, the estimated accumulated T2 lesions was 7 in the low-risk group (95% CI, 5-9), 15 in the medium-risk group (95% CI, 12-17), and 21 in the high-risk group (95% CI, 15-27).
Compared with the low- and medium-risk groups, the high-risk group had lower brain parenchymal fraction and gray-matter fraction at 5 years. They also experienced higher stigma, had worse perception of upper and lower limb function as measured by Neuro QoL, and had worse cognitive performance.
Dr. Tintoré has received compensation for consulting services and speaking honoraria from Aimirall, Bayer Schering Pharma, Biogen-Idec, Genzyme, Janssen, Merck-Serono, Novartis, Roche, Sanofi-Aventis, Teva Pharmaceuticals, and Viela Bio. Dr. Coyle has no relevant disclosures.
The high-risk group had the shortest time to progression to an Expanded Disability Status Score (EDSS) of 3.0, and were also more likely to progress by MRI and quality of life measures.
The ranking is based on sex, age at the first clinically isolated syndrome, CIS topography, the number of T2 lesions, and the presence of infratentorial and spinal cord lesions, contrast-enhancing lesions, and oligoclonal bands.
“What we wanted to do is merge all of the different prognostic variables for one single patient into one single score,” said Mar Tintoré, MD, PhD, in an interview. Dr. Tintoré is a professor of neurology at Vall d’Hebron University Hospital in Barcelona and a senior consultant at the Multiple Sclerosis Centre of Catalonia (Cemcat). Dr. Tintoré presented the results of the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
The three groups had different outcomes in MRI, clinical factors, and MRI scans, and quality of life outcomes over the course of their disease. “So this is a confirmation that this classification at baseline is really meaningful,” Dr. Tintoré said in an interview.
She attributed the success of the model to its reliance on multiple factors, but it is also designed to be simple to use. “We have been trying to use it with simple factors, [information] that you always have, like age, sex, gender, number of lesions, and topography of the region. Everybody has this information at their desk.”
Proof of concept
The study validates the approach that neurologists already utilize, according to Patricia Coyle, MD, who moderated the session. “I think the prospective study is a really unique and powerful concept,” said Dr. Coyle, who is a professor of neurology, vice chair of neurology, and director of the Stony Brook (N.Y.) Comprehensive Care Center.
The new study “kind of confirmed their concept of the initial rating, judging long-term disability progression measures in subsets. They also looked at brain atrophy, they looked at gray-matter atrophy, and that also traveled with these three different groups of severity. So it kind of gives value to looking at prognostic indicators at a first attack,” said Dr. Coyle.
The results also validate the Barcelona group’s heavy emphasis on MRI, which Dr. Coyle pointed out is common practice. “If the brain MRI looks very bad, if there are a lot of spinal cord lesions, then that’s somebody we’re much more worried about.”
Once the model is confirmed in other cohorts, the researchers plan to release the model as a generally available algorithm that clinicians could use to help manage patients. Dr. Tintoré pointed out the debate over when to begin a patient on high-efficacy disease-modifying therapies. That choice depends on a lot of factors, including patient choice, safety, and comorbidities. “But knowing that your patient is at risk of having a bad prognosis is something that is helpful” in that decision-making process, she said.
Predicting time to EDSS 3.0
The researchers used the Barcelona CIS cohort to build a Weibull survival regression in order to estimate the median time to EDSS 3.0. The model produced three categories with widely divergent predicted times from CIS to EDSS 3.0: low risk, medium risk, and high risk.
In the current report, the researchers compared the model to a “360 degree” measure of measures in 1,308 patients, including clinical milestones (McDonald 2017 MS, confirmed secondary progressive MS, progression independent of relapse activity [PIRA], EDSS disability, number of T2 MRI lesions and brain atrophy, and Patient Reported Outcomes for MS [walking speed, manual dexterity, processing speed, and contrast sensitivity]).
At 30 years after CIS, the risk of reaching EDSS 3.0 was higher in the medium risk (hazard ratio, 3.0 versus low risk) and in the high risk group (HR, 8.3 versus low risk). At 10 years, the low risk group had a 40% risk of fulfilling McDonald 2017 criteria, versus 89% in the intermediate group, and 98% in the high risk group. A similar relationship was seen for SPMS (1%, 8%, 16%) and PIRA (17%, 26%, 35%).
At 10 years, the estimated accumulated T2 lesions was 7 in the low-risk group (95% CI, 5-9), 15 in the medium-risk group (95% CI, 12-17), and 21 in the high-risk group (95% CI, 15-27).
Compared with the low- and medium-risk groups, the high-risk group had lower brain parenchymal fraction and gray-matter fraction at 5 years. They also experienced higher stigma, had worse perception of upper and lower limb function as measured by Neuro QoL, and had worse cognitive performance.
Dr. Tintoré has received compensation for consulting services and speaking honoraria from Aimirall, Bayer Schering Pharma, Biogen-Idec, Genzyme, Janssen, Merck-Serono, Novartis, Roche, Sanofi-Aventis, Teva Pharmaceuticals, and Viela Bio. Dr. Coyle has no relevant disclosures.
FROM ECTRIMS 2021
In MS, baseline cortical lesions predict cognitive decline
, according to findings from a new analysis. The findings had good accuracy, and could help clinicians monitor and treat cognitive impairment as it develops, according to Stefano Ziccardi, PhD, who is a postdoctoral researcher at the University of Verona in Italy.
“The number of cortical lesions at MS diagnosis accurately discriminates between the presence or the absence of cognitive impairment after diagnosis of MS, and this should be considered a predictive marker of long-term cognitive impairment in these patients. Early cortical lesion evaluation should be conducted in each MS patient to anticipate the manifestation of cognitive problems to improve the monitoring of cognitive abilities, improve the diagnosis of cognitive impairment, enable prompt intervention as necessary,” said Dr. Ziccardi at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Cortical lesions are highly prevalent in MS, perhaps more so than white matter lesions, said Dr. Ziccardi. They are associated with clinical disability and lead to disease progression. “However, prognostic data about the role of early cortical lesions with reference to long-term cognitive impairment are still missing,” said Dr. Ziccardi.
That’s important because cognitive impairment is very common in MS, affecting between one-third and two-thirds of patients. It may appear early in the disease course and worsen over time, and it predicts worse clinical and neurological progression. And it presents a clinical challenge. “Clinicians struggle to predict the evolution of cognitive abilities over time,” said Dr. Ziccardi.
The findings drew praise from Iris-Katharina Penner, PhD, who comoderated the session. “I think the important point … is that the predictive value of cortical lesions is very high, because it indicates finally that we probably have a patient at risk for developing cognitive impairment in the future,” said Dr. Penner, who is a neuropsychologist and cognitive neuroscientist at Heinrich Heine University in Düsseldorf, Germany.
Clinicians often don’t pay enough attention to cognition and the complexities of MS, said Mark Gudesblatt, MD, who was asked to comment. “It’s just adding layers of complexity. We’re peeling back the onion and you realize it’s a really complicated disease. It’s not just white matter plaques, gray matter plaques, disconnection syndrome, wires cut, atrophy, ongoing inflammation, immune deficiency. All these diseases are fascinating. And we think we’re experts. But the fact is, we have much to learn,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, New York.
The researchers analyzed data from 170 patients with MS who had a disease duration of approximately 20 years. Among the study cohort 62 patients were female, and the mean duration of disease was 19.2 years. Each patient had had a 1.5 Tesla magnetic resonance imaging scan to look for cortical lesions within 3 years of diagnosis. They had also undergone periodic MRIs as well as neuropsychological exams, and underwent a neuropsychological assessment at the end of the study, which included the Brief Repeatable Battery of Neuropsychological Tests (BRB-NT) and the Stroop Test.
A total of 41% of subjects had no cortical lesions according to their first MRI; 19% had 1-2 lesions, and 40% had 3 or more. At follow-up, 50% were cognitively normal (failed no tests), 25% had mild cognitive impairment (failed one or more tests), and 25% had severe cognitive impairment (failed three or more tests).
In the overall cohort, the median number of cortical lesions at baseline was 1 (interquartile range, 5.0). Among the 50% with normal cognitive function, the median was 0 (IQR, 2.5), while for the remaining 50% with cognitive impairment, the median was 3 (IQR, 7.0).
Those with 3 or more lesions had increased odds of cognitive impairment at follow-up (odds ratio, 3.70; P < .001), with an accuracy of 65% (95% confidence interval, 58%-72%), specificity of 75% (95% CI, 65%-84%), and a sensitivity of 55% (95% CI, 44%-66%). Three or more lesions discriminated between cognitive impairment and no impairment with an area under the curve of 0.67.
Individuals with no cognitive impairment had a median 0 lesions (IQR, 2.5), those with mild cognitive impairment had a median of 2.0 (IQR, 6.0), and those with severe cognitive impairment had 4.0 (IQR, 7.25).
In a multinomial regression model, 3 or more baseline cortical lesions were associated with a greater than threefold risk of severe cognitive impairment (OR, 3.33; P = .01).
Of subjects with 0 baseline lesions, 62% were cognitively normal at follow-up. In the 1-2 lesion group, 64% were normal. In the 3 or more group, 31% were cognitively normal (P < .001). In the 0 lesion group, 26% had mild cognitive impairment and 12% had severe cognitive impairment. In the 3 or more group, 28% had mild cognitive impairment, and 41% had severe cognitive impairment.
During the Q&A session following the talk, Dr. Ziccardi was asked if the group compared cortical lesions to other MRI correlates of cognitive impairment, such as gray matter volume or white matter integrity. He responded that the group is looking into those comparisons, and recently found that neither the number nor the volume of white matter lesions improved the accuracy of the predictive models based on the number of cortical lesions. The group is also looking into the applicability of gray matter volume.
, according to findings from a new analysis. The findings had good accuracy, and could help clinicians monitor and treat cognitive impairment as it develops, according to Stefano Ziccardi, PhD, who is a postdoctoral researcher at the University of Verona in Italy.
“The number of cortical lesions at MS diagnosis accurately discriminates between the presence or the absence of cognitive impairment after diagnosis of MS, and this should be considered a predictive marker of long-term cognitive impairment in these patients. Early cortical lesion evaluation should be conducted in each MS patient to anticipate the manifestation of cognitive problems to improve the monitoring of cognitive abilities, improve the diagnosis of cognitive impairment, enable prompt intervention as necessary,” said Dr. Ziccardi at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Cortical lesions are highly prevalent in MS, perhaps more so than white matter lesions, said Dr. Ziccardi. They are associated with clinical disability and lead to disease progression. “However, prognostic data about the role of early cortical lesions with reference to long-term cognitive impairment are still missing,” said Dr. Ziccardi.
That’s important because cognitive impairment is very common in MS, affecting between one-third and two-thirds of patients. It may appear early in the disease course and worsen over time, and it predicts worse clinical and neurological progression. And it presents a clinical challenge. “Clinicians struggle to predict the evolution of cognitive abilities over time,” said Dr. Ziccardi.
The findings drew praise from Iris-Katharina Penner, PhD, who comoderated the session. “I think the important point … is that the predictive value of cortical lesions is very high, because it indicates finally that we probably have a patient at risk for developing cognitive impairment in the future,” said Dr. Penner, who is a neuropsychologist and cognitive neuroscientist at Heinrich Heine University in Düsseldorf, Germany.
Clinicians often don’t pay enough attention to cognition and the complexities of MS, said Mark Gudesblatt, MD, who was asked to comment. “It’s just adding layers of complexity. We’re peeling back the onion and you realize it’s a really complicated disease. It’s not just white matter plaques, gray matter plaques, disconnection syndrome, wires cut, atrophy, ongoing inflammation, immune deficiency. All these diseases are fascinating. And we think we’re experts. But the fact is, we have much to learn,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, New York.
The researchers analyzed data from 170 patients with MS who had a disease duration of approximately 20 years. Among the study cohort 62 patients were female, and the mean duration of disease was 19.2 years. Each patient had had a 1.5 Tesla magnetic resonance imaging scan to look for cortical lesions within 3 years of diagnosis. They had also undergone periodic MRIs as well as neuropsychological exams, and underwent a neuropsychological assessment at the end of the study, which included the Brief Repeatable Battery of Neuropsychological Tests (BRB-NT) and the Stroop Test.
A total of 41% of subjects had no cortical lesions according to their first MRI; 19% had 1-2 lesions, and 40% had 3 or more. At follow-up, 50% were cognitively normal (failed no tests), 25% had mild cognitive impairment (failed one or more tests), and 25% had severe cognitive impairment (failed three or more tests).
In the overall cohort, the median number of cortical lesions at baseline was 1 (interquartile range, 5.0). Among the 50% with normal cognitive function, the median was 0 (IQR, 2.5), while for the remaining 50% with cognitive impairment, the median was 3 (IQR, 7.0).
Those with 3 or more lesions had increased odds of cognitive impairment at follow-up (odds ratio, 3.70; P < .001), with an accuracy of 65% (95% confidence interval, 58%-72%), specificity of 75% (95% CI, 65%-84%), and a sensitivity of 55% (95% CI, 44%-66%). Three or more lesions discriminated between cognitive impairment and no impairment with an area under the curve of 0.67.
Individuals with no cognitive impairment had a median 0 lesions (IQR, 2.5), those with mild cognitive impairment had a median of 2.0 (IQR, 6.0), and those with severe cognitive impairment had 4.0 (IQR, 7.25).
In a multinomial regression model, 3 or more baseline cortical lesions were associated with a greater than threefold risk of severe cognitive impairment (OR, 3.33; P = .01).
Of subjects with 0 baseline lesions, 62% were cognitively normal at follow-up. In the 1-2 lesion group, 64% were normal. In the 3 or more group, 31% were cognitively normal (P < .001). In the 0 lesion group, 26% had mild cognitive impairment and 12% had severe cognitive impairment. In the 3 or more group, 28% had mild cognitive impairment, and 41% had severe cognitive impairment.
During the Q&A session following the talk, Dr. Ziccardi was asked if the group compared cortical lesions to other MRI correlates of cognitive impairment, such as gray matter volume or white matter integrity. He responded that the group is looking into those comparisons, and recently found that neither the number nor the volume of white matter lesions improved the accuracy of the predictive models based on the number of cortical lesions. The group is also looking into the applicability of gray matter volume.
, according to findings from a new analysis. The findings had good accuracy, and could help clinicians monitor and treat cognitive impairment as it develops, according to Stefano Ziccardi, PhD, who is a postdoctoral researcher at the University of Verona in Italy.
“The number of cortical lesions at MS diagnosis accurately discriminates between the presence or the absence of cognitive impairment after diagnosis of MS, and this should be considered a predictive marker of long-term cognitive impairment in these patients. Early cortical lesion evaluation should be conducted in each MS patient to anticipate the manifestation of cognitive problems to improve the monitoring of cognitive abilities, improve the diagnosis of cognitive impairment, enable prompt intervention as necessary,” said Dr. Ziccardi at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Cortical lesions are highly prevalent in MS, perhaps more so than white matter lesions, said Dr. Ziccardi. They are associated with clinical disability and lead to disease progression. “However, prognostic data about the role of early cortical lesions with reference to long-term cognitive impairment are still missing,” said Dr. Ziccardi.
That’s important because cognitive impairment is very common in MS, affecting between one-third and two-thirds of patients. It may appear early in the disease course and worsen over time, and it predicts worse clinical and neurological progression. And it presents a clinical challenge. “Clinicians struggle to predict the evolution of cognitive abilities over time,” said Dr. Ziccardi.
The findings drew praise from Iris-Katharina Penner, PhD, who comoderated the session. “I think the important point … is that the predictive value of cortical lesions is very high, because it indicates finally that we probably have a patient at risk for developing cognitive impairment in the future,” said Dr. Penner, who is a neuropsychologist and cognitive neuroscientist at Heinrich Heine University in Düsseldorf, Germany.
Clinicians often don’t pay enough attention to cognition and the complexities of MS, said Mark Gudesblatt, MD, who was asked to comment. “It’s just adding layers of complexity. We’re peeling back the onion and you realize it’s a really complicated disease. It’s not just white matter plaques, gray matter plaques, disconnection syndrome, wires cut, atrophy, ongoing inflammation, immune deficiency. All these diseases are fascinating. And we think we’re experts. But the fact is, we have much to learn,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, New York.
The researchers analyzed data from 170 patients with MS who had a disease duration of approximately 20 years. Among the study cohort 62 patients were female, and the mean duration of disease was 19.2 years. Each patient had had a 1.5 Tesla magnetic resonance imaging scan to look for cortical lesions within 3 years of diagnosis. They had also undergone periodic MRIs as well as neuropsychological exams, and underwent a neuropsychological assessment at the end of the study, which included the Brief Repeatable Battery of Neuropsychological Tests (BRB-NT) and the Stroop Test.
A total of 41% of subjects had no cortical lesions according to their first MRI; 19% had 1-2 lesions, and 40% had 3 or more. At follow-up, 50% were cognitively normal (failed no tests), 25% had mild cognitive impairment (failed one or more tests), and 25% had severe cognitive impairment (failed three or more tests).
In the overall cohort, the median number of cortical lesions at baseline was 1 (interquartile range, 5.0). Among the 50% with normal cognitive function, the median was 0 (IQR, 2.5), while for the remaining 50% with cognitive impairment, the median was 3 (IQR, 7.0).
Those with 3 or more lesions had increased odds of cognitive impairment at follow-up (odds ratio, 3.70; P < .001), with an accuracy of 65% (95% confidence interval, 58%-72%), specificity of 75% (95% CI, 65%-84%), and a sensitivity of 55% (95% CI, 44%-66%). Three or more lesions discriminated between cognitive impairment and no impairment with an area under the curve of 0.67.
Individuals with no cognitive impairment had a median 0 lesions (IQR, 2.5), those with mild cognitive impairment had a median of 2.0 (IQR, 6.0), and those with severe cognitive impairment had 4.0 (IQR, 7.25).
In a multinomial regression model, 3 or more baseline cortical lesions were associated with a greater than threefold risk of severe cognitive impairment (OR, 3.33; P = .01).
Of subjects with 0 baseline lesions, 62% were cognitively normal at follow-up. In the 1-2 lesion group, 64% were normal. In the 3 or more group, 31% were cognitively normal (P < .001). In the 0 lesion group, 26% had mild cognitive impairment and 12% had severe cognitive impairment. In the 3 or more group, 28% had mild cognitive impairment, and 41% had severe cognitive impairment.
During the Q&A session following the talk, Dr. Ziccardi was asked if the group compared cortical lesions to other MRI correlates of cognitive impairment, such as gray matter volume or white matter integrity. He responded that the group is looking into those comparisons, and recently found that neither the number nor the volume of white matter lesions improved the accuracy of the predictive models based on the number of cortical lesions. The group is also looking into the applicability of gray matter volume.
FROM ECTRIMS 2021
AGA Clinical Practice Update: Expert review on GI perforations
A clinical practice update expert review from the American Gastroenterological Association gives advice on management of endoscopic perforations in the gastrointestinal tract, including esophageal, gastric, duodenal and periampullary, and colon perforation.
There are various techniques for dealing with perforations, including through-the-scope clips (TTSCs), over-the-scope clips (OTSCs), self-expanding metal stents (SEMS), and endoscopic suturing. Newer methods include biological glue and esophageal vacuum therapy. These techniques have been the subject of various retrospective analyses, but few prospective studies have examined their safety and efficacy.
In the expert review, published in Clinical Gastroenterology and Hepatology, authors led by Jeffrey H. Lee, MD, MPH, AGAF, of the department of gastroenterology at the University of Texas MD Anderson Cancer Center, Houston, emphasized that gastroenterologists should have a perforation protocol in place and practice procedures that will be used to address perforations. Endoscopists should also recognize their own limits and know when a patient should be sent to experienced, high-volume centers for further care.
In the event of a perforation, the entire team should be notified immediately, and carbon dioxide insufflation should be used at a low flow setting. The endoscopist should clean up luminal material to reduce the chance of peritoneal contamination, and then treat with an antibiotic regimen that counters gram-negative and anaerobic bacteria.
Esophageal perforation
Esophageal perforations most commonly occur during dilation of strictures, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD). Perforations of the mucosal flap may happen during so-called third-space endoscopy techniques like peroral endoscopic myotomy (POEM). Small perforations can be readily addressed with TTSCs. Larger perforations call for some combination of TTSCs, endoscopic suturing, fibrin glue injection, or esophageal stenting, though the latter is discouraged because of the potential for erosion.
A more concerning complication of POEM is delayed barrier failure, which can cause leaks, mediastinitis, or peritonitis. These complications have been estimated to occur in 0.2%-1.1% of cases.
In the event of an esophageal perforation, the area should be kept clean by suctioning, or by altering patient position if required. Perforations 1-2 cm in size can be closed using OTSCs. Excessive bleeding or larger tears can be addressed using a fully covered SEMS.
Leaks that occur in the ensuing days after the procedure should be closed using TTSCs, OTSCs, or endosuturing, followed by putting in a fully covered stent. Esophageal fistula should be addressed with a fully covered stent with a tight fit.
Endoscopic vacuum therapy is a newer technique to address large or persistent esophageal perforations. A review found it had a 96% success rate for esophageal perforations.
Gastric perforations
Gastric perforations often result from peptic ulcer disease or ingestion of something caustic, and it is a high risk during EMR and ESD procedures (0.4%-0.7% intraprocedural risk). The proximal gastric wall isn’t thick as in the gastric antrum, so proximal endoscopic resections require extra care. Lengthy procedures should be done under anesthesia. Ongoing gaseous insufflation during a perforation may worsen the problem because of heightened intraperitoneal pressure. OTSCs may be a better choice than TTSCs for 1-3 cm perforations, while endoloop/TTSC can be used for larger ones.
Duodenal and periampullary perforations
Duodenal and periampullary perforations occur during duodenal stricture dilation, EMR, endoscopic submucosal dissection, endoscopic ultrasound, and endoscopic retrograde cholangiopancreatography (ECRP). The thin duodenal wall makes it more susceptible to perforation than the esophagus, stomach, or colon.
Closing a duodenum perforation can be difficult. Type 1 perforations typically show sudden bleeding and lumen deflation, and often require surgical intervention. Some recent reports have suggested success with TTSCs, OTSCs, band ligation, and endoloops. Type 2 perforations are less obvious, and the endoscopist must examine the gas pattern on fluoroscopic beneath the liver or in the area of the right kidney. Retroperitoneal air following ERCP, if asymptomatic, doesn’t necessarily require intervention.
The challenges presented by the duodenum mean that, for large duodenal polyps, EMR should only be done by experienced endoscopists who are skilled at mucosal closure, and only experts should attempt ESD. Proteolytic enzymes from the pancreas can also pool in the duodenum, which can degrade muscle tissue and lead to delayed perforations. TTSC, OTSC, endosuturing, polymer gels or sheets, and TTSC combined with endoloop cinching have been used to close resection-associated perforations.
Colon perforation
Colon perforation may be caused by diverticulitis, inflammatory bowel disease, or occasionally colonic obstruction. Iatrogenic causes are more common and include endoscopic resection, hot forceps biopsy, dilation of stricture resulting from radiation or Crohn’s disease, colonic stenting, and advancement of colonoscope across angulations or into diverticula without straightening the endoscope
Large perforations are usually immediately noticeable and should be treated surgically, as should hemodynamic instability or delayed perforations with peritoneal signs.
Endoscopic closure should be attempted when the perforation site is clean, and lower rectal perforations can generally be repaired with TTSC, OTSC, or endoscopic suturing. In the cecum, or in a torturous or unclean colon, it may be difficult or dangerous to remove the colonoscope and insert an OTSC, and endoscopic suturing may not be possible, making TTSC the only procedure available for right colon perforations. The X-Tack Endoscopic HeliX Tacking System is a recently introduced, through-the-scope technology that places suture-tethered tacks into tissue surrounding the perforation and cinches it together. The system in principle can close large or irregular colonic and small bowel perforations using gastroscopes and colonoscopes, but no human studies have yet been published.
Conclusion
This update was a collaborative effort by four endoscopists who felt that it was timely to review the issue of perforations since they can be serious and challenging to manage. The evolution of endoscopic techniques over the last few years, however, has made the closure of spontaneous and iatrogenic perforations much less fear provoking, and they wished to summarize the approaches to a variety of such situations in order to guide practitioners who may encounter them.
“Although perforation is a serious event, with novel endoscopic techniques and tools, the endoscopist should no longer be paralyzed when it occurs,” the authors concluded.
Some authors reported relationships, such as consulting for or royalties from, device companies such as Medtronic and Boston Scientific. The remaining authors disclosed no conflicts.
This article was updated Oct. 25, 2021.
A clinical practice update expert review from the American Gastroenterological Association gives advice on management of endoscopic perforations in the gastrointestinal tract, including esophageal, gastric, duodenal and periampullary, and colon perforation.
There are various techniques for dealing with perforations, including through-the-scope clips (TTSCs), over-the-scope clips (OTSCs), self-expanding metal stents (SEMS), and endoscopic suturing. Newer methods include biological glue and esophageal vacuum therapy. These techniques have been the subject of various retrospective analyses, but few prospective studies have examined their safety and efficacy.
In the expert review, published in Clinical Gastroenterology and Hepatology, authors led by Jeffrey H. Lee, MD, MPH, AGAF, of the department of gastroenterology at the University of Texas MD Anderson Cancer Center, Houston, emphasized that gastroenterologists should have a perforation protocol in place and practice procedures that will be used to address perforations. Endoscopists should also recognize their own limits and know when a patient should be sent to experienced, high-volume centers for further care.
In the event of a perforation, the entire team should be notified immediately, and carbon dioxide insufflation should be used at a low flow setting. The endoscopist should clean up luminal material to reduce the chance of peritoneal contamination, and then treat with an antibiotic regimen that counters gram-negative and anaerobic bacteria.
Esophageal perforation
Esophageal perforations most commonly occur during dilation of strictures, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD). Perforations of the mucosal flap may happen during so-called third-space endoscopy techniques like peroral endoscopic myotomy (POEM). Small perforations can be readily addressed with TTSCs. Larger perforations call for some combination of TTSCs, endoscopic suturing, fibrin glue injection, or esophageal stenting, though the latter is discouraged because of the potential for erosion.
A more concerning complication of POEM is delayed barrier failure, which can cause leaks, mediastinitis, or peritonitis. These complications have been estimated to occur in 0.2%-1.1% of cases.
In the event of an esophageal perforation, the area should be kept clean by suctioning, or by altering patient position if required. Perforations 1-2 cm in size can be closed using OTSCs. Excessive bleeding or larger tears can be addressed using a fully covered SEMS.
Leaks that occur in the ensuing days after the procedure should be closed using TTSCs, OTSCs, or endosuturing, followed by putting in a fully covered stent. Esophageal fistula should be addressed with a fully covered stent with a tight fit.
Endoscopic vacuum therapy is a newer technique to address large or persistent esophageal perforations. A review found it had a 96% success rate for esophageal perforations.
Gastric perforations
Gastric perforations often result from peptic ulcer disease or ingestion of something caustic, and it is a high risk during EMR and ESD procedures (0.4%-0.7% intraprocedural risk). The proximal gastric wall isn’t thick as in the gastric antrum, so proximal endoscopic resections require extra care. Lengthy procedures should be done under anesthesia. Ongoing gaseous insufflation during a perforation may worsen the problem because of heightened intraperitoneal pressure. OTSCs may be a better choice than TTSCs for 1-3 cm perforations, while endoloop/TTSC can be used for larger ones.
Duodenal and periampullary perforations
Duodenal and periampullary perforations occur during duodenal stricture dilation, EMR, endoscopic submucosal dissection, endoscopic ultrasound, and endoscopic retrograde cholangiopancreatography (ECRP). The thin duodenal wall makes it more susceptible to perforation than the esophagus, stomach, or colon.
Closing a duodenum perforation can be difficult. Type 1 perforations typically show sudden bleeding and lumen deflation, and often require surgical intervention. Some recent reports have suggested success with TTSCs, OTSCs, band ligation, and endoloops. Type 2 perforations are less obvious, and the endoscopist must examine the gas pattern on fluoroscopic beneath the liver or in the area of the right kidney. Retroperitoneal air following ERCP, if asymptomatic, doesn’t necessarily require intervention.
The challenges presented by the duodenum mean that, for large duodenal polyps, EMR should only be done by experienced endoscopists who are skilled at mucosal closure, and only experts should attempt ESD. Proteolytic enzymes from the pancreas can also pool in the duodenum, which can degrade muscle tissue and lead to delayed perforations. TTSC, OTSC, endosuturing, polymer gels or sheets, and TTSC combined with endoloop cinching have been used to close resection-associated perforations.
Colon perforation
Colon perforation may be caused by diverticulitis, inflammatory bowel disease, or occasionally colonic obstruction. Iatrogenic causes are more common and include endoscopic resection, hot forceps biopsy, dilation of stricture resulting from radiation or Crohn’s disease, colonic stenting, and advancement of colonoscope across angulations or into diverticula without straightening the endoscope
Large perforations are usually immediately noticeable and should be treated surgically, as should hemodynamic instability or delayed perforations with peritoneal signs.
Endoscopic closure should be attempted when the perforation site is clean, and lower rectal perforations can generally be repaired with TTSC, OTSC, or endoscopic suturing. In the cecum, or in a torturous or unclean colon, it may be difficult or dangerous to remove the colonoscope and insert an OTSC, and endoscopic suturing may not be possible, making TTSC the only procedure available for right colon perforations. The X-Tack Endoscopic HeliX Tacking System is a recently introduced, through-the-scope technology that places suture-tethered tacks into tissue surrounding the perforation and cinches it together. The system in principle can close large or irregular colonic and small bowel perforations using gastroscopes and colonoscopes, but no human studies have yet been published.
Conclusion
This update was a collaborative effort by four endoscopists who felt that it was timely to review the issue of perforations since they can be serious and challenging to manage. The evolution of endoscopic techniques over the last few years, however, has made the closure of spontaneous and iatrogenic perforations much less fear provoking, and they wished to summarize the approaches to a variety of such situations in order to guide practitioners who may encounter them.
“Although perforation is a serious event, with novel endoscopic techniques and tools, the endoscopist should no longer be paralyzed when it occurs,” the authors concluded.
Some authors reported relationships, such as consulting for or royalties from, device companies such as Medtronic and Boston Scientific. The remaining authors disclosed no conflicts.
This article was updated Oct. 25, 2021.
A clinical practice update expert review from the American Gastroenterological Association gives advice on management of endoscopic perforations in the gastrointestinal tract, including esophageal, gastric, duodenal and periampullary, and colon perforation.
There are various techniques for dealing with perforations, including through-the-scope clips (TTSCs), over-the-scope clips (OTSCs), self-expanding metal stents (SEMS), and endoscopic suturing. Newer methods include biological glue and esophageal vacuum therapy. These techniques have been the subject of various retrospective analyses, but few prospective studies have examined their safety and efficacy.
In the expert review, published in Clinical Gastroenterology and Hepatology, authors led by Jeffrey H. Lee, MD, MPH, AGAF, of the department of gastroenterology at the University of Texas MD Anderson Cancer Center, Houston, emphasized that gastroenterologists should have a perforation protocol in place and practice procedures that will be used to address perforations. Endoscopists should also recognize their own limits and know when a patient should be sent to experienced, high-volume centers for further care.
In the event of a perforation, the entire team should be notified immediately, and carbon dioxide insufflation should be used at a low flow setting. The endoscopist should clean up luminal material to reduce the chance of peritoneal contamination, and then treat with an antibiotic regimen that counters gram-negative and anaerobic bacteria.
Esophageal perforation
Esophageal perforations most commonly occur during dilation of strictures, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD). Perforations of the mucosal flap may happen during so-called third-space endoscopy techniques like peroral endoscopic myotomy (POEM). Small perforations can be readily addressed with TTSCs. Larger perforations call for some combination of TTSCs, endoscopic suturing, fibrin glue injection, or esophageal stenting, though the latter is discouraged because of the potential for erosion.
A more concerning complication of POEM is delayed barrier failure, which can cause leaks, mediastinitis, or peritonitis. These complications have been estimated to occur in 0.2%-1.1% of cases.
In the event of an esophageal perforation, the area should be kept clean by suctioning, or by altering patient position if required. Perforations 1-2 cm in size can be closed using OTSCs. Excessive bleeding or larger tears can be addressed using a fully covered SEMS.
Leaks that occur in the ensuing days after the procedure should be closed using TTSCs, OTSCs, or endosuturing, followed by putting in a fully covered stent. Esophageal fistula should be addressed with a fully covered stent with a tight fit.
Endoscopic vacuum therapy is a newer technique to address large or persistent esophageal perforations. A review found it had a 96% success rate for esophageal perforations.
Gastric perforations
Gastric perforations often result from peptic ulcer disease or ingestion of something caustic, and it is a high risk during EMR and ESD procedures (0.4%-0.7% intraprocedural risk). The proximal gastric wall isn’t thick as in the gastric antrum, so proximal endoscopic resections require extra care. Lengthy procedures should be done under anesthesia. Ongoing gaseous insufflation during a perforation may worsen the problem because of heightened intraperitoneal pressure. OTSCs may be a better choice than TTSCs for 1-3 cm perforations, while endoloop/TTSC can be used for larger ones.
Duodenal and periampullary perforations
Duodenal and periampullary perforations occur during duodenal stricture dilation, EMR, endoscopic submucosal dissection, endoscopic ultrasound, and endoscopic retrograde cholangiopancreatography (ECRP). The thin duodenal wall makes it more susceptible to perforation than the esophagus, stomach, or colon.
Closing a duodenum perforation can be difficult. Type 1 perforations typically show sudden bleeding and lumen deflation, and often require surgical intervention. Some recent reports have suggested success with TTSCs, OTSCs, band ligation, and endoloops. Type 2 perforations are less obvious, and the endoscopist must examine the gas pattern on fluoroscopic beneath the liver or in the area of the right kidney. Retroperitoneal air following ERCP, if asymptomatic, doesn’t necessarily require intervention.
The challenges presented by the duodenum mean that, for large duodenal polyps, EMR should only be done by experienced endoscopists who are skilled at mucosal closure, and only experts should attempt ESD. Proteolytic enzymes from the pancreas can also pool in the duodenum, which can degrade muscle tissue and lead to delayed perforations. TTSC, OTSC, endosuturing, polymer gels or sheets, and TTSC combined with endoloop cinching have been used to close resection-associated perforations.
Colon perforation
Colon perforation may be caused by diverticulitis, inflammatory bowel disease, or occasionally colonic obstruction. Iatrogenic causes are more common and include endoscopic resection, hot forceps biopsy, dilation of stricture resulting from radiation or Crohn’s disease, colonic stenting, and advancement of colonoscope across angulations or into diverticula without straightening the endoscope
Large perforations are usually immediately noticeable and should be treated surgically, as should hemodynamic instability or delayed perforations with peritoneal signs.
Endoscopic closure should be attempted when the perforation site is clean, and lower rectal perforations can generally be repaired with TTSC, OTSC, or endoscopic suturing. In the cecum, or in a torturous or unclean colon, it may be difficult or dangerous to remove the colonoscope and insert an OTSC, and endoscopic suturing may not be possible, making TTSC the only procedure available for right colon perforations. The X-Tack Endoscopic HeliX Tacking System is a recently introduced, through-the-scope technology that places suture-tethered tacks into tissue surrounding the perforation and cinches it together. The system in principle can close large or irregular colonic and small bowel perforations using gastroscopes and colonoscopes, but no human studies have yet been published.
Conclusion
This update was a collaborative effort by four endoscopists who felt that it was timely to review the issue of perforations since they can be serious and challenging to manage. The evolution of endoscopic techniques over the last few years, however, has made the closure of spontaneous and iatrogenic perforations much less fear provoking, and they wished to summarize the approaches to a variety of such situations in order to guide practitioners who may encounter them.
“Although perforation is a serious event, with novel endoscopic techniques and tools, the endoscopist should no longer be paralyzed when it occurs,” the authors concluded.
Some authors reported relationships, such as consulting for or royalties from, device companies such as Medtronic and Boston Scientific. The remaining authors disclosed no conflicts.
This article was updated Oct. 25, 2021.
FROM THE CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Melatonin improves sleep in MS
according to a new pilot study.
The study included only 30 patients, but the findings suggest that melatonin could potentially help patients with MS who have sleep issues, according to Wan-Yu Hsu, PhD, who presented the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
There is no optimal management of sleep issues for these patients, and objective studies of sleep in patients with MS are scarce, said Dr. Hsu, who is an associate specialist in the department of neurology at the University of California, San Francisco. She worked with Riley Bove, MD, who is an associate professor of neurology at UCSF Weill Institute for Neurosciences.
“Melatonin use was associated with improvement in sleep quality and sleep disturbance in MS patients, although there was no significant change in other outcomes, like daytime sleepiness, mood, and walking ability” Dr. Hsu said in an interview.
Melatonin is inexpensive and readily available over the counter, but it’s too soon to begin recommending it to MS patients experiencing sleep problems, according to Dr. Hsu. “It’s a good start that we’re seeing some effects here with this relatively small group of people. Larger studies are needed to unravel the complex relationship between MS and sleep disturbances, as well as develop successful interventions. But for now, since melatonin is an over-the-counter, low-cost supplement, many patients are trying it already.”
Melatonin regulates the sleep-wake cycle, and previous research has shown a decrease in melatonin serum levels as a result of corticosteroid administration. Other work has suggested that the decline of melatonin secretion in MS may reflect progressive failure of the pineal gland in the pathogenesis of MS. “The cause of sleep problems can be lesions and neural damage to brain structures involved in sleep, or symptoms that indirectly disrupt sleep,” she said.
Indeed, sleep issues in MS are common and wide-ranging, according to Mark Gudesblatt, MD, who was asked to comment on the study. His group previously reported that 65% of people with MS who reported fatigue had undiagnosed obstructive sleep apnea. He also pointed out that disruption of the neural network also disrupts sleep. “That is not only sleep-disordered breathing, that’s sleep onset, REM latency, and sleep efficiency,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y.
Dr. Gudesblatt cautioned that melatonin, as a dietary supplement, is unregulated. The potency listed on the package may not be accurate and also may not be the correct dose for the patient. “It’s fraught with problems, but ultimately it’s relatively safe,” said Dr. Gudesblatt.
The study was a double-blind, placebo-controlled, crossover study. Participants had a Pittsburgh Sleep Quality Index (PSQI) score of 5 or more, or an Insomnia Severity Index (ISI) score higher than 14 at baseline. Other baseline assessments included patient-reported outcomes for sleep disturbances, sleep quality, daytime sleepiness, fatigue, walking ability, and mood. Half of the participants received melatonin for the first 2 weeks and then switched to placebo. The other half started with placebo and moved over to melatonin at the beginning of week 3.
Participants in the trial started out at 0.5 mg melatonin and were stepped up to 3.0 mg after 3 days if they didn't feel it was working, both when taking melatonin and when taking placebo. Of the 30 patients, 24 stepped up to 3.0 mg when they were receiving melatonin.*
During the second and fourth weeks, participants wore an actigraph watch to measure their physical and sleep activities, and then repeated the patient-reported outcome measures at the end of weeks 2 and 4. Melatonin improved average sleep time (6.96 vs. 6.67 hours; P = .03) as measured by the actigraph watch. Sleep efficiency was also nominally improved (84.7% vs. 83.2%), though the result was not statistically significant (P = .07). Other trends toward statistical significance included improvements in ISI (–3.5 vs. –2.4; P = .07), change in PSQI component 1 (–0.03 vs. 0.0; P = .07), and change in the NeuroQoL-Fatigue score (–4.7 vs. –2.4; P = .06).
Dr. Hsu hopes to conduct larger studies to examine how the disease-modifying therapies might affect the results of the study.
The study was funded by the National Multiple Sclerosis Society. Dr. Hsu and Dr. Gudesblatt have no relevant financial disclosures.
*This article was updated on Oct. 15.
according to a new pilot study.
The study included only 30 patients, but the findings suggest that melatonin could potentially help patients with MS who have sleep issues, according to Wan-Yu Hsu, PhD, who presented the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
There is no optimal management of sleep issues for these patients, and objective studies of sleep in patients with MS are scarce, said Dr. Hsu, who is an associate specialist in the department of neurology at the University of California, San Francisco. She worked with Riley Bove, MD, who is an associate professor of neurology at UCSF Weill Institute for Neurosciences.
“Melatonin use was associated with improvement in sleep quality and sleep disturbance in MS patients, although there was no significant change in other outcomes, like daytime sleepiness, mood, and walking ability” Dr. Hsu said in an interview.
Melatonin is inexpensive and readily available over the counter, but it’s too soon to begin recommending it to MS patients experiencing sleep problems, according to Dr. Hsu. “It’s a good start that we’re seeing some effects here with this relatively small group of people. Larger studies are needed to unravel the complex relationship between MS and sleep disturbances, as well as develop successful interventions. But for now, since melatonin is an over-the-counter, low-cost supplement, many patients are trying it already.”
Melatonin regulates the sleep-wake cycle, and previous research has shown a decrease in melatonin serum levels as a result of corticosteroid administration. Other work has suggested that the decline of melatonin secretion in MS may reflect progressive failure of the pineal gland in the pathogenesis of MS. “The cause of sleep problems can be lesions and neural damage to brain structures involved in sleep, or symptoms that indirectly disrupt sleep,” she said.
Indeed, sleep issues in MS are common and wide-ranging, according to Mark Gudesblatt, MD, who was asked to comment on the study. His group previously reported that 65% of people with MS who reported fatigue had undiagnosed obstructive sleep apnea. He also pointed out that disruption of the neural network also disrupts sleep. “That is not only sleep-disordered breathing, that’s sleep onset, REM latency, and sleep efficiency,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y.
Dr. Gudesblatt cautioned that melatonin, as a dietary supplement, is unregulated. The potency listed on the package may not be accurate and also may not be the correct dose for the patient. “It’s fraught with problems, but ultimately it’s relatively safe,” said Dr. Gudesblatt.
The study was a double-blind, placebo-controlled, crossover study. Participants had a Pittsburgh Sleep Quality Index (PSQI) score of 5 or more, or an Insomnia Severity Index (ISI) score higher than 14 at baseline. Other baseline assessments included patient-reported outcomes for sleep disturbances, sleep quality, daytime sleepiness, fatigue, walking ability, and mood. Half of the participants received melatonin for the first 2 weeks and then switched to placebo. The other half started with placebo and moved over to melatonin at the beginning of week 3.
Participants in the trial started out at 0.5 mg melatonin and were stepped up to 3.0 mg after 3 days if they didn't feel it was working, both when taking melatonin and when taking placebo. Of the 30 patients, 24 stepped up to 3.0 mg when they were receiving melatonin.*
During the second and fourth weeks, participants wore an actigraph watch to measure their physical and sleep activities, and then repeated the patient-reported outcome measures at the end of weeks 2 and 4. Melatonin improved average sleep time (6.96 vs. 6.67 hours; P = .03) as measured by the actigraph watch. Sleep efficiency was also nominally improved (84.7% vs. 83.2%), though the result was not statistically significant (P = .07). Other trends toward statistical significance included improvements in ISI (–3.5 vs. –2.4; P = .07), change in PSQI component 1 (–0.03 vs. 0.0; P = .07), and change in the NeuroQoL-Fatigue score (–4.7 vs. –2.4; P = .06).
Dr. Hsu hopes to conduct larger studies to examine how the disease-modifying therapies might affect the results of the study.
The study was funded by the National Multiple Sclerosis Society. Dr. Hsu and Dr. Gudesblatt have no relevant financial disclosures.
*This article was updated on Oct. 15.
according to a new pilot study.
The study included only 30 patients, but the findings suggest that melatonin could potentially help patients with MS who have sleep issues, according to Wan-Yu Hsu, PhD, who presented the study at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
There is no optimal management of sleep issues for these patients, and objective studies of sleep in patients with MS are scarce, said Dr. Hsu, who is an associate specialist in the department of neurology at the University of California, San Francisco. She worked with Riley Bove, MD, who is an associate professor of neurology at UCSF Weill Institute for Neurosciences.
“Melatonin use was associated with improvement in sleep quality and sleep disturbance in MS patients, although there was no significant change in other outcomes, like daytime sleepiness, mood, and walking ability” Dr. Hsu said in an interview.
Melatonin is inexpensive and readily available over the counter, but it’s too soon to begin recommending it to MS patients experiencing sleep problems, according to Dr. Hsu. “It’s a good start that we’re seeing some effects here with this relatively small group of people. Larger studies are needed to unravel the complex relationship between MS and sleep disturbances, as well as develop successful interventions. But for now, since melatonin is an over-the-counter, low-cost supplement, many patients are trying it already.”
Melatonin regulates the sleep-wake cycle, and previous research has shown a decrease in melatonin serum levels as a result of corticosteroid administration. Other work has suggested that the decline of melatonin secretion in MS may reflect progressive failure of the pineal gland in the pathogenesis of MS. “The cause of sleep problems can be lesions and neural damage to brain structures involved in sleep, or symptoms that indirectly disrupt sleep,” she said.
Indeed, sleep issues in MS are common and wide-ranging, according to Mark Gudesblatt, MD, who was asked to comment on the study. His group previously reported that 65% of people with MS who reported fatigue had undiagnosed obstructive sleep apnea. He also pointed out that disruption of the neural network also disrupts sleep. “That is not only sleep-disordered breathing, that’s sleep onset, REM latency, and sleep efficiency,” said Dr. Gudesblatt, who is medical director of the Comprehensive MS Care Center at South Shore Neurologic Associates in Patchogue, N.Y.
Dr. Gudesblatt cautioned that melatonin, as a dietary supplement, is unregulated. The potency listed on the package may not be accurate and also may not be the correct dose for the patient. “It’s fraught with problems, but ultimately it’s relatively safe,” said Dr. Gudesblatt.
The study was a double-blind, placebo-controlled, crossover study. Participants had a Pittsburgh Sleep Quality Index (PSQI) score of 5 or more, or an Insomnia Severity Index (ISI) score higher than 14 at baseline. Other baseline assessments included patient-reported outcomes for sleep disturbances, sleep quality, daytime sleepiness, fatigue, walking ability, and mood. Half of the participants received melatonin for the first 2 weeks and then switched to placebo. The other half started with placebo and moved over to melatonin at the beginning of week 3.
Participants in the trial started out at 0.5 mg melatonin and were stepped up to 3.0 mg after 3 days if they didn't feel it was working, both when taking melatonin and when taking placebo. Of the 30 patients, 24 stepped up to 3.0 mg when they were receiving melatonin.*
During the second and fourth weeks, participants wore an actigraph watch to measure their physical and sleep activities, and then repeated the patient-reported outcome measures at the end of weeks 2 and 4. Melatonin improved average sleep time (6.96 vs. 6.67 hours; P = .03) as measured by the actigraph watch. Sleep efficiency was also nominally improved (84.7% vs. 83.2%), though the result was not statistically significant (P = .07). Other trends toward statistical significance included improvements in ISI (–3.5 vs. –2.4; P = .07), change in PSQI component 1 (–0.03 vs. 0.0; P = .07), and change in the NeuroQoL-Fatigue score (–4.7 vs. –2.4; P = .06).
Dr. Hsu hopes to conduct larger studies to examine how the disease-modifying therapies might affect the results of the study.
The study was funded by the National Multiple Sclerosis Society. Dr. Hsu and Dr. Gudesblatt have no relevant financial disclosures.
*This article was updated on Oct. 15.
FROM ECTRIMS 2021
In Crohn’s disease, no decline in stomas despite increasing use of anti-TNF
Despite increasing use of anti–tumor necrosis factor (TNF) medications in recent years and a lower rate of proctectomy, there has been no decline in stoma incidence among Crohn’s disease (CD) patients, according to a new retrospective analysis of a Swedish population database.
The overall 5-year stoma incidence was 2.5%, and there was no significant difference between calendar periods, wrote Åsa H Everhov, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues. Their report is in Inflammatory Bowel Diseases. Previous population studies looking at temporal trends have found mixed results with respect to stoma formation. However, many previous studies analyzed cohorts from referral centers that included patients with more severe disease. Others had small sample sizes.
“This is somewhat surprising as the rate of overall surgery for Crohn’s has decreased with the advent of biologic therapies,” said Miguel Regueiro, MD, who was asked to comment on the study. He is chair of the Digestive Disease and Surgery Institute, and professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Dr. Regueiro pointed out that the rate of stoma creation was quite low, and characteristics of the disease may explain the lack of a trend. For example, anorectal disease, especially when accompanied by fistula and strictures, is often medication refractory. “Although the study could not delineate this, it is my clinical practice experience that some patients present with destructive anorectal disease early, and that despite medications the ‘damage is too far gone’ to reverse,” said Dr. Regueiro. Also, the anorectum does not allow for an anastomosis since there is no region to connect to that isn’t damaged, he added.
The findings shouldn’t affect patient management or counseling, according to Stephen Hanauer, MD, professor of medicine at Northwestern University, Chicago, who was not involved in the study. “The indications for surgery in Crohn’s disease have not changed with the advent of newer therapies. Complications such as strictures and abscesses are still treated with similar surgeries. It is hopeful that the future course after surgery can be modified by effective biologic therapies,” he said.
The study authors noted that the findings are consistent with previous studies suggesting that the rate of abdominal surgery had begun to decline before anti-TNF drugs were introduced. The Swedish National Patient Register used in the current work includes only inpatient data before 2001, preventing a broader analysis prior to 1999, when infliximab gained approval in Sweden. But the researchers looked at time from first surgery to stoma, and found a decline in stoma formation between 1994 and 1997. A similar analysis found no decrease in the 2000s.
The researchers pointed out that anti-TNF inhibitor use would be expected to reduce the rate of stomas by inducing remission, although temporary stomas may be created to relieve symptoms while waiting for the medication to take effect. But anti-TNF agents could also encourage patients and physicians to postpone surgery. The delay could raise the chance of surgical complications, which in turn could lead to creation of a temporary stoma. Permanent stomas are typically created in cases of severe perianal CD.
The study could come as a disappointment to some patients and physicians, according to the authors. “The more active and early use of anti-TNF (therapeutics), in combination with the decreasing incidence of abdominal surgery in general for CD, has raised hopes of decreased incidence of stoma formation, but this was not observed in the present study,” the authors wrote.
But the news wasn’t all bad. The study found a lower cumulative stoma incidence than had previous studies, and the incidence of permanent stoma was just 0.8% at 5 years, “which should be reassuring for patients,” according to the authors.
CD patients often fear that a stoma will become necessary, but a stoma can be quite beneficial, allowing patients to regain some control over their lives. That can lead to more work participation and social activity. Qualitative studies showed that both patients and clinicians described outcomes of stoma placement as exceeding expectations, with a key factor being support from other inflammatory bowel disease patients with stomas. The authors encouraged clinicians to discuss the possibility of a stoma early on in the treatment process, and to avoid referring to it as a “last resort.”
The study also suggests that patients with anal and anorectal Crohn’s disease should receive biologics early, and a multidisciplinary approach involving both the gastroenterologist and surgeon is important. And patients should be counseled on the impact of disease on diet and psychological health, according to Dr. Regueiro.
The new study analyzed data between 2003 and 2014, from 18,815 Crohn’s disease patients who had not undergone previous surgery. The median age was 39 years, 53% were women, and 12% were pediatric patients.
After a median follow-up of 9.6 years, 9.5% of patients had perianal disease. Overall, 36% of patients had been treated with immunomodulators, and 17% with anti-TNF agents; 3.5% had stoma surgery, and just 0.05% underwent proctectomy.
Among those who had a stoma placed, the median age at diagnosis was 47 years, and 53% were men. In all, 12.6% had perianal disease at diagnosis, and 24.5% had perianal disease by the end of follow-up; 43% had received immunomodulators, and 26% anti-TNF agents. Among stomas, 64% were ileostomies, and 44% were temporary, with 88% of removals performed within 2 years of surgery.
The calendar periods of CD onset (2003-2006, 2007-2010, and 2011-2014) had similar rates of cumulative stoma placement (log rank test, P = .61). Overall, the 1-year cumulative incidence of stoma was 1.3%, the 3-year incidence was 1.9%, and the 5-year incidence was 2.5%.
The cumulative incidence of ever-use of anti-TNF agents increased with each successive calendar period (P < .001), but there was no significant difference in cumulative stoma incidence (P = .07).
One limitation of the study is the lack of detailed patient characteristics, and another is the short follow-up for patients diagnosed during 2011-2014. Another is that the results may not be generalizable to a U.S. population.
The study authors have received funding and consulted for various pharmaceutical companies. Dr. Regueiro has received grants from and has consulted or been on a scientific advisory board for Abbvie, UCB, and Janssen. Dr. Hanauer has no relevant financial disclosures.
This article was updated Oct. 13, 2021.
Despite increasing use of anti–tumor necrosis factor (TNF) medications in recent years and a lower rate of proctectomy, there has been no decline in stoma incidence among Crohn’s disease (CD) patients, according to a new retrospective analysis of a Swedish population database.
The overall 5-year stoma incidence was 2.5%, and there was no significant difference between calendar periods, wrote Åsa H Everhov, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues. Their report is in Inflammatory Bowel Diseases. Previous population studies looking at temporal trends have found mixed results with respect to stoma formation. However, many previous studies analyzed cohorts from referral centers that included patients with more severe disease. Others had small sample sizes.
“This is somewhat surprising as the rate of overall surgery for Crohn’s has decreased with the advent of biologic therapies,” said Miguel Regueiro, MD, who was asked to comment on the study. He is chair of the Digestive Disease and Surgery Institute, and professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Dr. Regueiro pointed out that the rate of stoma creation was quite low, and characteristics of the disease may explain the lack of a trend. For example, anorectal disease, especially when accompanied by fistula and strictures, is often medication refractory. “Although the study could not delineate this, it is my clinical practice experience that some patients present with destructive anorectal disease early, and that despite medications the ‘damage is too far gone’ to reverse,” said Dr. Regueiro. Also, the anorectum does not allow for an anastomosis since there is no region to connect to that isn’t damaged, he added.
The findings shouldn’t affect patient management or counseling, according to Stephen Hanauer, MD, professor of medicine at Northwestern University, Chicago, who was not involved in the study. “The indications for surgery in Crohn’s disease have not changed with the advent of newer therapies. Complications such as strictures and abscesses are still treated with similar surgeries. It is hopeful that the future course after surgery can be modified by effective biologic therapies,” he said.
The study authors noted that the findings are consistent with previous studies suggesting that the rate of abdominal surgery had begun to decline before anti-TNF drugs were introduced. The Swedish National Patient Register used in the current work includes only inpatient data before 2001, preventing a broader analysis prior to 1999, when infliximab gained approval in Sweden. But the researchers looked at time from first surgery to stoma, and found a decline in stoma formation between 1994 and 1997. A similar analysis found no decrease in the 2000s.
The researchers pointed out that anti-TNF inhibitor use would be expected to reduce the rate of stomas by inducing remission, although temporary stomas may be created to relieve symptoms while waiting for the medication to take effect. But anti-TNF agents could also encourage patients and physicians to postpone surgery. The delay could raise the chance of surgical complications, which in turn could lead to creation of a temporary stoma. Permanent stomas are typically created in cases of severe perianal CD.
The study could come as a disappointment to some patients and physicians, according to the authors. “The more active and early use of anti-TNF (therapeutics), in combination with the decreasing incidence of abdominal surgery in general for CD, has raised hopes of decreased incidence of stoma formation, but this was not observed in the present study,” the authors wrote.
But the news wasn’t all bad. The study found a lower cumulative stoma incidence than had previous studies, and the incidence of permanent stoma was just 0.8% at 5 years, “which should be reassuring for patients,” according to the authors.
CD patients often fear that a stoma will become necessary, but a stoma can be quite beneficial, allowing patients to regain some control over their lives. That can lead to more work participation and social activity. Qualitative studies showed that both patients and clinicians described outcomes of stoma placement as exceeding expectations, with a key factor being support from other inflammatory bowel disease patients with stomas. The authors encouraged clinicians to discuss the possibility of a stoma early on in the treatment process, and to avoid referring to it as a “last resort.”
The study also suggests that patients with anal and anorectal Crohn’s disease should receive biologics early, and a multidisciplinary approach involving both the gastroenterologist and surgeon is important. And patients should be counseled on the impact of disease on diet and psychological health, according to Dr. Regueiro.
The new study analyzed data between 2003 and 2014, from 18,815 Crohn’s disease patients who had not undergone previous surgery. The median age was 39 years, 53% were women, and 12% were pediatric patients.
After a median follow-up of 9.6 years, 9.5% of patients had perianal disease. Overall, 36% of patients had been treated with immunomodulators, and 17% with anti-TNF agents; 3.5% had stoma surgery, and just 0.05% underwent proctectomy.
Among those who had a stoma placed, the median age at diagnosis was 47 years, and 53% were men. In all, 12.6% had perianal disease at diagnosis, and 24.5% had perianal disease by the end of follow-up; 43% had received immunomodulators, and 26% anti-TNF agents. Among stomas, 64% were ileostomies, and 44% were temporary, with 88% of removals performed within 2 years of surgery.
The calendar periods of CD onset (2003-2006, 2007-2010, and 2011-2014) had similar rates of cumulative stoma placement (log rank test, P = .61). Overall, the 1-year cumulative incidence of stoma was 1.3%, the 3-year incidence was 1.9%, and the 5-year incidence was 2.5%.
The cumulative incidence of ever-use of anti-TNF agents increased with each successive calendar period (P < .001), but there was no significant difference in cumulative stoma incidence (P = .07).
One limitation of the study is the lack of detailed patient characteristics, and another is the short follow-up for patients diagnosed during 2011-2014. Another is that the results may not be generalizable to a U.S. population.
The study authors have received funding and consulted for various pharmaceutical companies. Dr. Regueiro has received grants from and has consulted or been on a scientific advisory board for Abbvie, UCB, and Janssen. Dr. Hanauer has no relevant financial disclosures.
This article was updated Oct. 13, 2021.
Despite increasing use of anti–tumor necrosis factor (TNF) medications in recent years and a lower rate of proctectomy, there has been no decline in stoma incidence among Crohn’s disease (CD) patients, according to a new retrospective analysis of a Swedish population database.
The overall 5-year stoma incidence was 2.5%, and there was no significant difference between calendar periods, wrote Åsa H Everhov, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues. Their report is in Inflammatory Bowel Diseases. Previous population studies looking at temporal trends have found mixed results with respect to stoma formation. However, many previous studies analyzed cohorts from referral centers that included patients with more severe disease. Others had small sample sizes.
“This is somewhat surprising as the rate of overall surgery for Crohn’s has decreased with the advent of biologic therapies,” said Miguel Regueiro, MD, who was asked to comment on the study. He is chair of the Digestive Disease and Surgery Institute, and professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Dr. Regueiro pointed out that the rate of stoma creation was quite low, and characteristics of the disease may explain the lack of a trend. For example, anorectal disease, especially when accompanied by fistula and strictures, is often medication refractory. “Although the study could not delineate this, it is my clinical practice experience that some patients present with destructive anorectal disease early, and that despite medications the ‘damage is too far gone’ to reverse,” said Dr. Regueiro. Also, the anorectum does not allow for an anastomosis since there is no region to connect to that isn’t damaged, he added.
The findings shouldn’t affect patient management or counseling, according to Stephen Hanauer, MD, professor of medicine at Northwestern University, Chicago, who was not involved in the study. “The indications for surgery in Crohn’s disease have not changed with the advent of newer therapies. Complications such as strictures and abscesses are still treated with similar surgeries. It is hopeful that the future course after surgery can be modified by effective biologic therapies,” he said.
The study authors noted that the findings are consistent with previous studies suggesting that the rate of abdominal surgery had begun to decline before anti-TNF drugs were introduced. The Swedish National Patient Register used in the current work includes only inpatient data before 2001, preventing a broader analysis prior to 1999, when infliximab gained approval in Sweden. But the researchers looked at time from first surgery to stoma, and found a decline in stoma formation between 1994 and 1997. A similar analysis found no decrease in the 2000s.
The researchers pointed out that anti-TNF inhibitor use would be expected to reduce the rate of stomas by inducing remission, although temporary stomas may be created to relieve symptoms while waiting for the medication to take effect. But anti-TNF agents could also encourage patients and physicians to postpone surgery. The delay could raise the chance of surgical complications, which in turn could lead to creation of a temporary stoma. Permanent stomas are typically created in cases of severe perianal CD.
The study could come as a disappointment to some patients and physicians, according to the authors. “The more active and early use of anti-TNF (therapeutics), in combination with the decreasing incidence of abdominal surgery in general for CD, has raised hopes of decreased incidence of stoma formation, but this was not observed in the present study,” the authors wrote.
But the news wasn’t all bad. The study found a lower cumulative stoma incidence than had previous studies, and the incidence of permanent stoma was just 0.8% at 5 years, “which should be reassuring for patients,” according to the authors.
CD patients often fear that a stoma will become necessary, but a stoma can be quite beneficial, allowing patients to regain some control over their lives. That can lead to more work participation and social activity. Qualitative studies showed that both patients and clinicians described outcomes of stoma placement as exceeding expectations, with a key factor being support from other inflammatory bowel disease patients with stomas. The authors encouraged clinicians to discuss the possibility of a stoma early on in the treatment process, and to avoid referring to it as a “last resort.”
The study also suggests that patients with anal and anorectal Crohn’s disease should receive biologics early, and a multidisciplinary approach involving both the gastroenterologist and surgeon is important. And patients should be counseled on the impact of disease on diet and psychological health, according to Dr. Regueiro.
The new study analyzed data between 2003 and 2014, from 18,815 Crohn’s disease patients who had not undergone previous surgery. The median age was 39 years, 53% were women, and 12% were pediatric patients.
After a median follow-up of 9.6 years, 9.5% of patients had perianal disease. Overall, 36% of patients had been treated with immunomodulators, and 17% with anti-TNF agents; 3.5% had stoma surgery, and just 0.05% underwent proctectomy.
Among those who had a stoma placed, the median age at diagnosis was 47 years, and 53% were men. In all, 12.6% had perianal disease at diagnosis, and 24.5% had perianal disease by the end of follow-up; 43% had received immunomodulators, and 26% anti-TNF agents. Among stomas, 64% were ileostomies, and 44% were temporary, with 88% of removals performed within 2 years of surgery.
The calendar periods of CD onset (2003-2006, 2007-2010, and 2011-2014) had similar rates of cumulative stoma placement (log rank test, P = .61). Overall, the 1-year cumulative incidence of stoma was 1.3%, the 3-year incidence was 1.9%, and the 5-year incidence was 2.5%.
The cumulative incidence of ever-use of anti-TNF agents increased with each successive calendar period (P < .001), but there was no significant difference in cumulative stoma incidence (P = .07).
One limitation of the study is the lack of detailed patient characteristics, and another is the short follow-up for patients diagnosed during 2011-2014. Another is that the results may not be generalizable to a U.S. population.
The study authors have received funding and consulted for various pharmaceutical companies. Dr. Regueiro has received grants from and has consulted or been on a scientific advisory board for Abbvie, UCB, and Janssen. Dr. Hanauer has no relevant financial disclosures.
This article was updated Oct. 13, 2021.
FROM INFLAMMATORY BOWEL DISEASES
Statins tied to diabetes progression
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE
MRE plus FIB-4 beats FAST for detecting NASH-related fibrosis
A combination of magnetic resonance elastography and blood levels of fibrosis-4 index (MEFIB) outperformed FibroScan-AST (FAST) in determining the presence of significant fibrosis among patients with nonalcoholic fatty liver disease (NAFLD), according to a new prospective cohort analysis.
Liver fibrosis is the most important prognostic factor for NAFLD, but the invasiveness, propensity for sampling error, and interoperator variability of biopsy have prompted efforts to develop alternatives. FAST, which uses vibration-controlled transient elastography (VCTE), controlled attenuation parameter (CAP), and aspartate aminotransferase levels, and MEFIB have been developed as candidates, but they had not been directly compared in screening. The findings suggest that MEFIB may be a better tool for identifying NAFLD patients at heightened risk of nonalcoholic steatohepatitis (NASH), as well as which patients could be candidates for pharmacotherapy interventions and clinical trials.
Although there are no drugs currently approved for high-risk NAFLD patients, many clinical trials are underway. Patients with stage 2 or higher fibrosis are candidates for clinical trials, but many trials experience a high screening failure rate. A noninvasive method that can identify clinical trial candidates while avoiding liver biopsy would be a welcome addition, Nobuharu Tamaki, MD, PhD, of the NAFLD Research Center, division of gastroenterology and hepatology, department of medicine, at the University of California, San Diego, and colleagues explained in Hepatology.
“We suspect that these are the patients; if there is going to be a drug approved, it will be for this patient population. So it’s important for prognosis, but it’s also important potentially for future treatment with new drugs,” said Zobair Younossi, MD, who was asked to comment on the study.
The researchers examined a cohort of 234 consecutive adults at UCSD and 314 consecutive adults at Yokohama (Japan) City University who underwent liver biopsy, magnetic resonance elastography (MRE), VCTE, and CAP assessment.
Significant fibrosis was found in 29.5% of the UCSD cohort and 66.2% of the Yokohama cohort.* MEFIB had a higher area under the receiver operating characteristic curve than FAST in the UCSD cohort (0.860 vs. 0.757; P = .005) and the Yokohama cohort (0.899 vs. 0.724; P < .001).
When the researchers employed MEFIB as a rule-in criteria (MRE value ≥3.3 kPa and FIB-4 ≥1.6), MEFIB had a positive predictive value of 91.2% in the UCSD cohort and 96.0% in the Yokohama cohort, versus 74.2% and 89.2% for FAST (≥0.67), respectively. Rule-out criteria included MRE less than 3.3 kPa and Fib-4 less than1.6 for MEFIB, as well as FAST of 0.35 or less; with those parameters, negative predictive value for significant fibrosis was 92.8% in the UCSD group and 85.6% in the Yokohama group for MEFIB, and 88.3% and 57.8% for FAST, respectively.
Most existing noninvasive tests do a pretty good job of excluding advanced fibrosis, but they don’t perform as well at identifying those with cirrhosis, according to Dr. Younossi. He added that MEFIB isn’t suitable for general population screening, but rather for case finding, in which it can be used to identify patients who are likely to have high risk for fibrosis. “Nevertheless, it seems like the combination of FIB-4 and MRE has very good performance for identifying and excluding NAFLD patients with moderate to advance fibrosis, at least in the two cohorts that were looked at,” said Dr. Younossi.
However, Dr. Younossi noted some potential limitations to the study. Both cohorts were from referral centers, making it likely that the included patients have higher prevalences of fibrosis than a typical practice patient population, making it important to validate the findings in a real-world setting. The approach also relies on magnetic resonance technology, which is costly and may not be readily available. “We need to potentially find other, simpler noninvasive test combinations that are easier to do than MRE,” said Dr. Younossi.
Several authors disclosed ties with numerous pharmaceutical and device companies, including Pfizer, AstraZeneca, and Siemens. Dr. Younossi has no relevant financial disclosures.
Correction, 1/18/22: An earlier version of this article misstated the percentage of each cohort that had significant fibrosis.
A combination of magnetic resonance elastography and blood levels of fibrosis-4 index (MEFIB) outperformed FibroScan-AST (FAST) in determining the presence of significant fibrosis among patients with nonalcoholic fatty liver disease (NAFLD), according to a new prospective cohort analysis.
Liver fibrosis is the most important prognostic factor for NAFLD, but the invasiveness, propensity for sampling error, and interoperator variability of biopsy have prompted efforts to develop alternatives. FAST, which uses vibration-controlled transient elastography (VCTE), controlled attenuation parameter (CAP), and aspartate aminotransferase levels, and MEFIB have been developed as candidates, but they had not been directly compared in screening. The findings suggest that MEFIB may be a better tool for identifying NAFLD patients at heightened risk of nonalcoholic steatohepatitis (NASH), as well as which patients could be candidates for pharmacotherapy interventions and clinical trials.
Although there are no drugs currently approved for high-risk NAFLD patients, many clinical trials are underway. Patients with stage 2 or higher fibrosis are candidates for clinical trials, but many trials experience a high screening failure rate. A noninvasive method that can identify clinical trial candidates while avoiding liver biopsy would be a welcome addition, Nobuharu Tamaki, MD, PhD, of the NAFLD Research Center, division of gastroenterology and hepatology, department of medicine, at the University of California, San Diego, and colleagues explained in Hepatology.
“We suspect that these are the patients; if there is going to be a drug approved, it will be for this patient population. So it’s important for prognosis, but it’s also important potentially for future treatment with new drugs,” said Zobair Younossi, MD, who was asked to comment on the study.
The researchers examined a cohort of 234 consecutive adults at UCSD and 314 consecutive adults at Yokohama (Japan) City University who underwent liver biopsy, magnetic resonance elastography (MRE), VCTE, and CAP assessment.
Significant fibrosis was found in 29.5% of the UCSD cohort and 66.2% of the Yokohama cohort.* MEFIB had a higher area under the receiver operating characteristic curve than FAST in the UCSD cohort (0.860 vs. 0.757; P = .005) and the Yokohama cohort (0.899 vs. 0.724; P < .001).
When the researchers employed MEFIB as a rule-in criteria (MRE value ≥3.3 kPa and FIB-4 ≥1.6), MEFIB had a positive predictive value of 91.2% in the UCSD cohort and 96.0% in the Yokohama cohort, versus 74.2% and 89.2% for FAST (≥0.67), respectively. Rule-out criteria included MRE less than 3.3 kPa and Fib-4 less than1.6 for MEFIB, as well as FAST of 0.35 or less; with those parameters, negative predictive value for significant fibrosis was 92.8% in the UCSD group and 85.6% in the Yokohama group for MEFIB, and 88.3% and 57.8% for FAST, respectively.
Most existing noninvasive tests do a pretty good job of excluding advanced fibrosis, but they don’t perform as well at identifying those with cirrhosis, according to Dr. Younossi. He added that MEFIB isn’t suitable for general population screening, but rather for case finding, in which it can be used to identify patients who are likely to have high risk for fibrosis. “Nevertheless, it seems like the combination of FIB-4 and MRE has very good performance for identifying and excluding NAFLD patients with moderate to advance fibrosis, at least in the two cohorts that were looked at,” said Dr. Younossi.
However, Dr. Younossi noted some potential limitations to the study. Both cohorts were from referral centers, making it likely that the included patients have higher prevalences of fibrosis than a typical practice patient population, making it important to validate the findings in a real-world setting. The approach also relies on magnetic resonance technology, which is costly and may not be readily available. “We need to potentially find other, simpler noninvasive test combinations that are easier to do than MRE,” said Dr. Younossi.
Several authors disclosed ties with numerous pharmaceutical and device companies, including Pfizer, AstraZeneca, and Siemens. Dr. Younossi has no relevant financial disclosures.
Correction, 1/18/22: An earlier version of this article misstated the percentage of each cohort that had significant fibrosis.
A combination of magnetic resonance elastography and blood levels of fibrosis-4 index (MEFIB) outperformed FibroScan-AST (FAST) in determining the presence of significant fibrosis among patients with nonalcoholic fatty liver disease (NAFLD), according to a new prospective cohort analysis.
Liver fibrosis is the most important prognostic factor for NAFLD, but the invasiveness, propensity for sampling error, and interoperator variability of biopsy have prompted efforts to develop alternatives. FAST, which uses vibration-controlled transient elastography (VCTE), controlled attenuation parameter (CAP), and aspartate aminotransferase levels, and MEFIB have been developed as candidates, but they had not been directly compared in screening. The findings suggest that MEFIB may be a better tool for identifying NAFLD patients at heightened risk of nonalcoholic steatohepatitis (NASH), as well as which patients could be candidates for pharmacotherapy interventions and clinical trials.
Although there are no drugs currently approved for high-risk NAFLD patients, many clinical trials are underway. Patients with stage 2 or higher fibrosis are candidates for clinical trials, but many trials experience a high screening failure rate. A noninvasive method that can identify clinical trial candidates while avoiding liver biopsy would be a welcome addition, Nobuharu Tamaki, MD, PhD, of the NAFLD Research Center, division of gastroenterology and hepatology, department of medicine, at the University of California, San Diego, and colleagues explained in Hepatology.
“We suspect that these are the patients; if there is going to be a drug approved, it will be for this patient population. So it’s important for prognosis, but it’s also important potentially for future treatment with new drugs,” said Zobair Younossi, MD, who was asked to comment on the study.
The researchers examined a cohort of 234 consecutive adults at UCSD and 314 consecutive adults at Yokohama (Japan) City University who underwent liver biopsy, magnetic resonance elastography (MRE), VCTE, and CAP assessment.
Significant fibrosis was found in 29.5% of the UCSD cohort and 66.2% of the Yokohama cohort.* MEFIB had a higher area under the receiver operating characteristic curve than FAST in the UCSD cohort (0.860 vs. 0.757; P = .005) and the Yokohama cohort (0.899 vs. 0.724; P < .001).
When the researchers employed MEFIB as a rule-in criteria (MRE value ≥3.3 kPa and FIB-4 ≥1.6), MEFIB had a positive predictive value of 91.2% in the UCSD cohort and 96.0% in the Yokohama cohort, versus 74.2% and 89.2% for FAST (≥0.67), respectively. Rule-out criteria included MRE less than 3.3 kPa and Fib-4 less than1.6 for MEFIB, as well as FAST of 0.35 or less; with those parameters, negative predictive value for significant fibrosis was 92.8% in the UCSD group and 85.6% in the Yokohama group for MEFIB, and 88.3% and 57.8% for FAST, respectively.
Most existing noninvasive tests do a pretty good job of excluding advanced fibrosis, but they don’t perform as well at identifying those with cirrhosis, according to Dr. Younossi. He added that MEFIB isn’t suitable for general population screening, but rather for case finding, in which it can be used to identify patients who are likely to have high risk for fibrosis. “Nevertheless, it seems like the combination of FIB-4 and MRE has very good performance for identifying and excluding NAFLD patients with moderate to advance fibrosis, at least in the two cohorts that were looked at,” said Dr. Younossi.
However, Dr. Younossi noted some potential limitations to the study. Both cohorts were from referral centers, making it likely that the included patients have higher prevalences of fibrosis than a typical practice patient population, making it important to validate the findings in a real-world setting. The approach also relies on magnetic resonance technology, which is costly and may not be readily available. “We need to potentially find other, simpler noninvasive test combinations that are easier to do than MRE,” said Dr. Younossi.
Several authors disclosed ties with numerous pharmaceutical and device companies, including Pfizer, AstraZeneca, and Siemens. Dr. Younossi has no relevant financial disclosures.
Correction, 1/18/22: An earlier version of this article misstated the percentage of each cohort that had significant fibrosis.
FROM HEPATOLOGY
Lifestyle interventions improve resistant hypertension
A 4-month, structured diet and exercise intervention lowered blood pressure in adults with resistant blood pressure, according to results from a randomized, clinical trial. The program also led to improvements in baroreflex sensitivity, heart rate variability, and flow-mediated dilation, compared with individuals who received only a single education session.
The intervention included instruction from a nutritionist on how to follow the Dietary Approaches to Stop Hypertension (DASH) diet, as well as restricting calories and sodium to less than 2,300 mg/day. It included weekly, 45-minute group counseling sessions, run by a clinical psychiatrist, focusing on eating behaviors. The exercise component included 30- to 45-minute sessions at 70%-85% of initial heart rate reserve, carried out three times per week at a cardiac rehabilitation facility.
“While some individuals can make the lifestyle changes on their own, a structured program of supervised exercise and dietary modification conducted by a multidisciplinary team of physicians, psychologists, nutritionists, and physical therapists/exercise physiologists found in cardiac rehabilitation programs throughout the country is likely to be more effective. There are many cardiac rehabilitation programs throughout the country that are accessible to most patients,” said lead author James Blumenthal, PhD, the J.P. Gibbons Professor in Psychiatry and Behavioral Sciences at Duke University, Durham, N.C.
The study, called Treating Resistant Hypertension Using Lifestyle Modification to Promote Health (TRIUMPH), was published in Circulation. It is one of few that have examined lifestyle interventions in resistant hypertension, defined as systolic blood pressure ≥ 130 mm Hg or diastolic blood pressure ≥ 80 mm Hg after adherence to three or more optimally-dosed antihypertensive medications of three different classes, including one diuretic.
“This is a nice study [that] emphasizes what we often forget: Lifestyle factors, especially salt intake, are important drivers of resistant hypertension. Our own studies have shown that this is predominantly a salt retaining state, and one would expect dietary salt restriction to be particularly effective in this group of patients and that is what this study showed,” said Bryan Williams, MD, who was asked to comment on the study. Dr. Williams is chair of medicine at University College London.
The results should also be reassuring to some who worried that exercise might lead to worsened blood pressure. “This study showed that in patients with resistant hypertension, though not out of control blood pressures, exercise was not only safe, but effective in lowering their blood pressure,” said Deepak L. Bhatt, MD, MPH, who was asked to comment. He is executive director of interventional cardiovascular programs at Brigham and Women’s Hospital, and professor of medicine at Harvard Medical School, both in Boston.
The new research isn’t unique. In August, researchers in Portugal and Brazil showed that a 12-week exercise-only intervention reduced 24-hour and daytime ambulatory systolic and diastolic blood pressure. The two studies communicate the same message. “Lifestyle changes can work for resistant hypertension. So, two independent, modest-sized studies with essentially the same, positive, actionable conclusion,” said Dr. Bhatt, adding that the next step should be a larger, multicenter trial.
In the new study, 90 patients were assigned to the diet and exercise intervention and 50 to the control group. They had a mean age of 63 years, and 48% were women. Participants attended 94% of DASH diet classes and 89% of exercise sessions, and both groups had excellent adherence to medications.
The treatment group had a greater reduction in clinic systolic BP (–12.5 versus –7.1 mm Hg; P = .005) and diastolic BP (–5.9 versus –3.7 mm Hg; P = .034), as well as 24-hour ambulatory systolic BP (–7.0 versus –0.3 mm Hg; P = .001). The treatment group also had more improvement in resting baroreflex sensitivity (2.3 versus –1.1 ms/mm Hg; P = .003), high-frequency heart rate variability (0.4 versus –0.2 ln ms2; P = .025, and flow-mediated dilation (0.3% versus –1.4%, P = .022). The two groups had similar outcomes with respect to pulse wave velocity and left ventricular mass.
“Results of the TRIUMPH study suggest that policymakers should consider resistant hypertension as a new indication for cardiac rehabilitation with appropriate coverage by governmental agencies and private insurers,” Dr. Blumenthal said.
“This is an important new, evidence-based intervention for resistant hypertension. It is safe and relatively inexpensive. It should now be something physicians routinely offer these patients. Hopefully in the future, insurers will cover cardiac rehabilitation for patients with resistant hypertension,” Dr. Bhatt said.
The study also pointed towards an effective approach for patients who may be unable to sustain lifestyle changes. “Of course, not every patient will be able to maintain a healthy diet and an exercise program on their own, thus a cardiac rehabilitation program can be an excellent way to increase the likelihood of successful lifestyle modification,” Dr. Bhatt said.
TRIUMPH was sponsored by grants from the National Heart, Lung, and Blood Institute. None of the authors had disclosures to report. Dr. Bhatt disclosed having financial relationships with more than 40 pharmaceutical companies. Dr. Williams reported having no relevant financial disclosures.
A 4-month, structured diet and exercise intervention lowered blood pressure in adults with resistant blood pressure, according to results from a randomized, clinical trial. The program also led to improvements in baroreflex sensitivity, heart rate variability, and flow-mediated dilation, compared with individuals who received only a single education session.
The intervention included instruction from a nutritionist on how to follow the Dietary Approaches to Stop Hypertension (DASH) diet, as well as restricting calories and sodium to less than 2,300 mg/day. It included weekly, 45-minute group counseling sessions, run by a clinical psychiatrist, focusing on eating behaviors. The exercise component included 30- to 45-minute sessions at 70%-85% of initial heart rate reserve, carried out three times per week at a cardiac rehabilitation facility.
“While some individuals can make the lifestyle changes on their own, a structured program of supervised exercise and dietary modification conducted by a multidisciplinary team of physicians, psychologists, nutritionists, and physical therapists/exercise physiologists found in cardiac rehabilitation programs throughout the country is likely to be more effective. There are many cardiac rehabilitation programs throughout the country that are accessible to most patients,” said lead author James Blumenthal, PhD, the J.P. Gibbons Professor in Psychiatry and Behavioral Sciences at Duke University, Durham, N.C.
The study, called Treating Resistant Hypertension Using Lifestyle Modification to Promote Health (TRIUMPH), was published in Circulation. It is one of few that have examined lifestyle interventions in resistant hypertension, defined as systolic blood pressure ≥ 130 mm Hg or diastolic blood pressure ≥ 80 mm Hg after adherence to three or more optimally-dosed antihypertensive medications of three different classes, including one diuretic.
“This is a nice study [that] emphasizes what we often forget: Lifestyle factors, especially salt intake, are important drivers of resistant hypertension. Our own studies have shown that this is predominantly a salt retaining state, and one would expect dietary salt restriction to be particularly effective in this group of patients and that is what this study showed,” said Bryan Williams, MD, who was asked to comment on the study. Dr. Williams is chair of medicine at University College London.
The results should also be reassuring to some who worried that exercise might lead to worsened blood pressure. “This study showed that in patients with resistant hypertension, though not out of control blood pressures, exercise was not only safe, but effective in lowering their blood pressure,” said Deepak L. Bhatt, MD, MPH, who was asked to comment. He is executive director of interventional cardiovascular programs at Brigham and Women’s Hospital, and professor of medicine at Harvard Medical School, both in Boston.
The new research isn’t unique. In August, researchers in Portugal and Brazil showed that a 12-week exercise-only intervention reduced 24-hour and daytime ambulatory systolic and diastolic blood pressure. The two studies communicate the same message. “Lifestyle changes can work for resistant hypertension. So, two independent, modest-sized studies with essentially the same, positive, actionable conclusion,” said Dr. Bhatt, adding that the next step should be a larger, multicenter trial.
In the new study, 90 patients were assigned to the diet and exercise intervention and 50 to the control group. They had a mean age of 63 years, and 48% were women. Participants attended 94% of DASH diet classes and 89% of exercise sessions, and both groups had excellent adherence to medications.
The treatment group had a greater reduction in clinic systolic BP (–12.5 versus –7.1 mm Hg; P = .005) and diastolic BP (–5.9 versus –3.7 mm Hg; P = .034), as well as 24-hour ambulatory systolic BP (–7.0 versus –0.3 mm Hg; P = .001). The treatment group also had more improvement in resting baroreflex sensitivity (2.3 versus –1.1 ms/mm Hg; P = .003), high-frequency heart rate variability (0.4 versus –0.2 ln ms2; P = .025, and flow-mediated dilation (0.3% versus –1.4%, P = .022). The two groups had similar outcomes with respect to pulse wave velocity and left ventricular mass.
“Results of the TRIUMPH study suggest that policymakers should consider resistant hypertension as a new indication for cardiac rehabilitation with appropriate coverage by governmental agencies and private insurers,” Dr. Blumenthal said.
“This is an important new, evidence-based intervention for resistant hypertension. It is safe and relatively inexpensive. It should now be something physicians routinely offer these patients. Hopefully in the future, insurers will cover cardiac rehabilitation for patients with resistant hypertension,” Dr. Bhatt said.
The study also pointed towards an effective approach for patients who may be unable to sustain lifestyle changes. “Of course, not every patient will be able to maintain a healthy diet and an exercise program on their own, thus a cardiac rehabilitation program can be an excellent way to increase the likelihood of successful lifestyle modification,” Dr. Bhatt said.
TRIUMPH was sponsored by grants from the National Heart, Lung, and Blood Institute. None of the authors had disclosures to report. Dr. Bhatt disclosed having financial relationships with more than 40 pharmaceutical companies. Dr. Williams reported having no relevant financial disclosures.
A 4-month, structured diet and exercise intervention lowered blood pressure in adults with resistant blood pressure, according to results from a randomized, clinical trial. The program also led to improvements in baroreflex sensitivity, heart rate variability, and flow-mediated dilation, compared with individuals who received only a single education session.
The intervention included instruction from a nutritionist on how to follow the Dietary Approaches to Stop Hypertension (DASH) diet, as well as restricting calories and sodium to less than 2,300 mg/day. It included weekly, 45-minute group counseling sessions, run by a clinical psychiatrist, focusing on eating behaviors. The exercise component included 30- to 45-minute sessions at 70%-85% of initial heart rate reserve, carried out three times per week at a cardiac rehabilitation facility.
“While some individuals can make the lifestyle changes on their own, a structured program of supervised exercise and dietary modification conducted by a multidisciplinary team of physicians, psychologists, nutritionists, and physical therapists/exercise physiologists found in cardiac rehabilitation programs throughout the country is likely to be more effective. There are many cardiac rehabilitation programs throughout the country that are accessible to most patients,” said lead author James Blumenthal, PhD, the J.P. Gibbons Professor in Psychiatry and Behavioral Sciences at Duke University, Durham, N.C.
The study, called Treating Resistant Hypertension Using Lifestyle Modification to Promote Health (TRIUMPH), was published in Circulation. It is one of few that have examined lifestyle interventions in resistant hypertension, defined as systolic blood pressure ≥ 130 mm Hg or diastolic blood pressure ≥ 80 mm Hg after adherence to three or more optimally-dosed antihypertensive medications of three different classes, including one diuretic.
“This is a nice study [that] emphasizes what we often forget: Lifestyle factors, especially salt intake, are important drivers of resistant hypertension. Our own studies have shown that this is predominantly a salt retaining state, and one would expect dietary salt restriction to be particularly effective in this group of patients and that is what this study showed,” said Bryan Williams, MD, who was asked to comment on the study. Dr. Williams is chair of medicine at University College London.
The results should also be reassuring to some who worried that exercise might lead to worsened blood pressure. “This study showed that in patients with resistant hypertension, though not out of control blood pressures, exercise was not only safe, but effective in lowering their blood pressure,” said Deepak L. Bhatt, MD, MPH, who was asked to comment. He is executive director of interventional cardiovascular programs at Brigham and Women’s Hospital, and professor of medicine at Harvard Medical School, both in Boston.
The new research isn’t unique. In August, researchers in Portugal and Brazil showed that a 12-week exercise-only intervention reduced 24-hour and daytime ambulatory systolic and diastolic blood pressure. The two studies communicate the same message. “Lifestyle changes can work for resistant hypertension. So, two independent, modest-sized studies with essentially the same, positive, actionable conclusion,” said Dr. Bhatt, adding that the next step should be a larger, multicenter trial.
In the new study, 90 patients were assigned to the diet and exercise intervention and 50 to the control group. They had a mean age of 63 years, and 48% were women. Participants attended 94% of DASH diet classes and 89% of exercise sessions, and both groups had excellent adherence to medications.
The treatment group had a greater reduction in clinic systolic BP (–12.5 versus –7.1 mm Hg; P = .005) and diastolic BP (–5.9 versus –3.7 mm Hg; P = .034), as well as 24-hour ambulatory systolic BP (–7.0 versus –0.3 mm Hg; P = .001). The treatment group also had more improvement in resting baroreflex sensitivity (2.3 versus –1.1 ms/mm Hg; P = .003), high-frequency heart rate variability (0.4 versus –0.2 ln ms2; P = .025, and flow-mediated dilation (0.3% versus –1.4%, P = .022). The two groups had similar outcomes with respect to pulse wave velocity and left ventricular mass.
“Results of the TRIUMPH study suggest that policymakers should consider resistant hypertension as a new indication for cardiac rehabilitation with appropriate coverage by governmental agencies and private insurers,” Dr. Blumenthal said.
“This is an important new, evidence-based intervention for resistant hypertension. It is safe and relatively inexpensive. It should now be something physicians routinely offer these patients. Hopefully in the future, insurers will cover cardiac rehabilitation for patients with resistant hypertension,” Dr. Bhatt said.
The study also pointed towards an effective approach for patients who may be unable to sustain lifestyle changes. “Of course, not every patient will be able to maintain a healthy diet and an exercise program on their own, thus a cardiac rehabilitation program can be an excellent way to increase the likelihood of successful lifestyle modification,” Dr. Bhatt said.
TRIUMPH was sponsored by grants from the National Heart, Lung, and Blood Institute. None of the authors had disclosures to report. Dr. Bhatt disclosed having financial relationships with more than 40 pharmaceutical companies. Dr. Williams reported having no relevant financial disclosures.
FROM CIRCULATION
Gastric cancer: Family history–based H. pylori strategy would be cost effective
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
FROM GASTROENTEROLOGY