User login
Maternal methadone opioid maintenance therapy may be tied to smaller postnatal head circumference
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
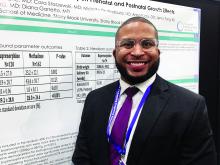
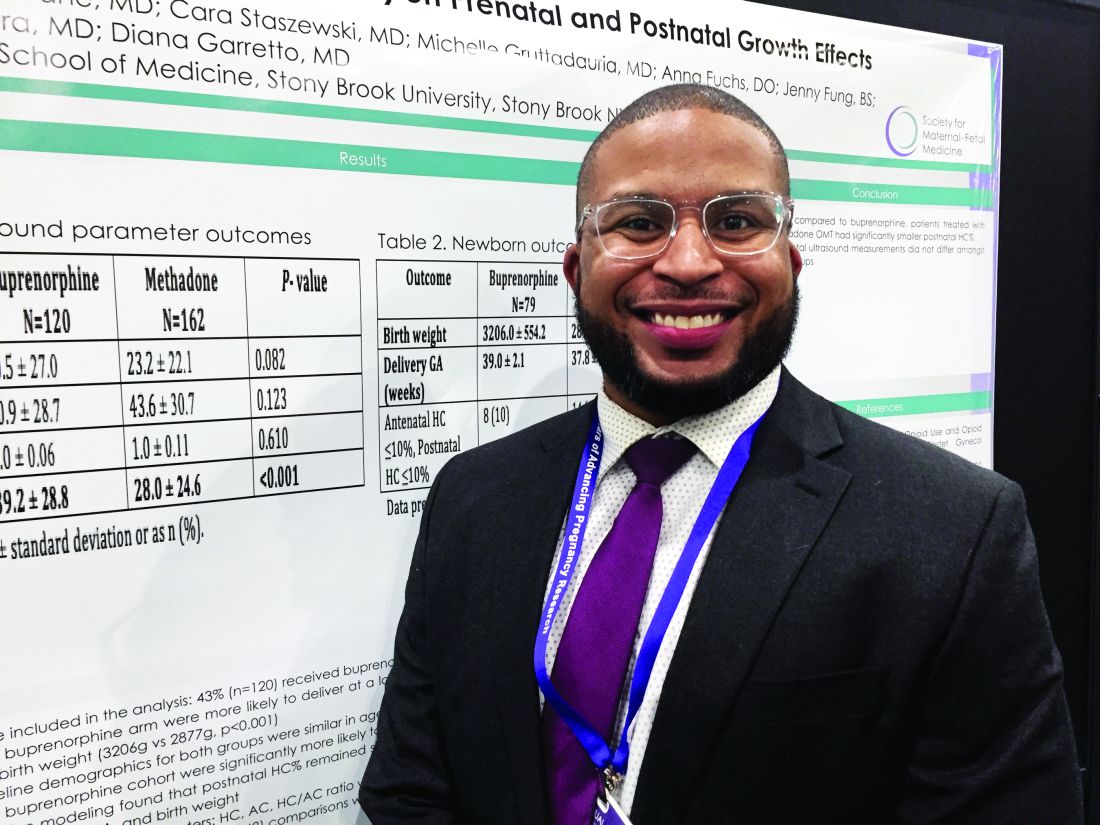
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
REPORTING FROM THE PREGNANCY MEETING
Should patients with COVID-19 avoid ibuprofen or RAAS antagonists?
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
20% of U.S. COVID-19 deaths were aged 20-64 years
*Correction, 3/20/2020: An earlier version of this story misstated the age range for COVID-19 deaths. The headline of this story was corrected to read "20% of COVID-19 deaths were aged 20-64 years" and the text was adjusted to reflect the correct age range.
A review of more than 4,000 U.S. patients who were diagnosed with novel coronavirus infection (COVID-19) shows that an unexpected 20% of deaths occurred among adults aged 20-64 years, and 20% of those hospitalized were aged 20-44 years.
The expectation has been that people over 65 are most vulnerable to COVID-19 infection, but this study indicates that, at least in the United States, a significant number of patients under 45 can land in the hospital and can even die of the disease.
To assess rates of hospitalization, admission to an ICU, and death among patients with COVID-19 by age group, the Centers for Disease Control and Prevention analyzed 4,226 COVID-19 cases in the United States that were reported between Feb. 12 and March 16.
Overall, older patients in this group were the most likely to be hospitalized, to be admitted to ICU, and to die of COVID-19. A total of 31% of the cases, 45% of hospitalizations, 53% of ICU admissions, and 80% of deaths occurred in patients aged 65 years and older. “Similar to reports from other countries, this finding suggests that the risk for serious disease and death from COVID-19 is higher in older age groups,” said the investigators. “In contrast, persons aged [19 years and younger] appear to have milder COVID-19 illness, with almost no hospitalizations or deaths reported to date in the United States in this age group.”
But compared with the under-19 group, patients aged 20-44 years appeared to be at higher risk for hospitalization and ICU admission, according to the data published March 18 in Morbidity and Mortality Weekly Report.
The researchers excluded from their analysis patients who repatriated to the United States from Wuhan, China, and from Japan, including patients repatriated from cruise ships. Data on serious underlying health conditions were not available, and many cases were missing key data, they noted.
Among 508 patients known to have been hospitalized, 9% were aged 85 years or older, 36% were aged 65-84 years, 17% were aged 55-64 years, 18% were 45-54 years, and 20% were aged 20-44 years.
Among 121 patients admitted to an ICU, 7% were aged 85 years or older, 46% were aged 65-84 years, 36% were aged 45-64 years, and 12% were aged 20-44 years. Between 11% and 31% of patients with COVID-19 aged 75-84 years were admitted to an ICU.
Of 44 deaths, more than a third occurred among adults aged 85 years and older, and 46% occurred among adults aged 65-84 years, and 20% occurred among adults aged 20-64 years.
More follow-up time is needed to determine outcomes among active cases, the researchers said. These results also might overestimate the prevalence of severe disease because the initial approach to testing for COVID-19 focused on people with more severe disease. “These preliminary data also demonstrate that severe illness leading to hospitalization, including ICU admission and death, can occur in adults of any age with COVID-19,” according to the CDC.
SOURCE: CDC COVID-19 Response Team. MMWR Morb Mortal Wkly Rep. 2020 Mar 18. doi: 10.15585/mmwr.mm6912e2.
*Correction, 3/20/2020: An earlier version of this story misstated the age range for COVID-19 deaths. The headline of this story was corrected to read "20% of COVID-19 deaths were aged 20-64 years" and the text was adjusted to reflect the correct age range.
A review of more than 4,000 U.S. patients who were diagnosed with novel coronavirus infection (COVID-19) shows that an unexpected 20% of deaths occurred among adults aged 20-64 years, and 20% of those hospitalized were aged 20-44 years.
The expectation has been that people over 65 are most vulnerable to COVID-19 infection, but this study indicates that, at least in the United States, a significant number of patients under 45 can land in the hospital and can even die of the disease.
To assess rates of hospitalization, admission to an ICU, and death among patients with COVID-19 by age group, the Centers for Disease Control and Prevention analyzed 4,226 COVID-19 cases in the United States that were reported between Feb. 12 and March 16.
Overall, older patients in this group were the most likely to be hospitalized, to be admitted to ICU, and to die of COVID-19. A total of 31% of the cases, 45% of hospitalizations, 53% of ICU admissions, and 80% of deaths occurred in patients aged 65 years and older. “Similar to reports from other countries, this finding suggests that the risk for serious disease and death from COVID-19 is higher in older age groups,” said the investigators. “In contrast, persons aged [19 years and younger] appear to have milder COVID-19 illness, with almost no hospitalizations or deaths reported to date in the United States in this age group.”
But compared with the under-19 group, patients aged 20-44 years appeared to be at higher risk for hospitalization and ICU admission, according to the data published March 18 in Morbidity and Mortality Weekly Report.
The researchers excluded from their analysis patients who repatriated to the United States from Wuhan, China, and from Japan, including patients repatriated from cruise ships. Data on serious underlying health conditions were not available, and many cases were missing key data, they noted.
Among 508 patients known to have been hospitalized, 9% were aged 85 years or older, 36% were aged 65-84 years, 17% were aged 55-64 years, 18% were 45-54 years, and 20% were aged 20-44 years.
Among 121 patients admitted to an ICU, 7% were aged 85 years or older, 46% were aged 65-84 years, 36% were aged 45-64 years, and 12% were aged 20-44 years. Between 11% and 31% of patients with COVID-19 aged 75-84 years were admitted to an ICU.
Of 44 deaths, more than a third occurred among adults aged 85 years and older, and 46% occurred among adults aged 65-84 years, and 20% occurred among adults aged 20-64 years.
More follow-up time is needed to determine outcomes among active cases, the researchers said. These results also might overestimate the prevalence of severe disease because the initial approach to testing for COVID-19 focused on people with more severe disease. “These preliminary data also demonstrate that severe illness leading to hospitalization, including ICU admission and death, can occur in adults of any age with COVID-19,” according to the CDC.
SOURCE: CDC COVID-19 Response Team. MMWR Morb Mortal Wkly Rep. 2020 Mar 18. doi: 10.15585/mmwr.mm6912e2.
*Correction, 3/20/2020: An earlier version of this story misstated the age range for COVID-19 deaths. The headline of this story was corrected to read "20% of COVID-19 deaths were aged 20-64 years" and the text was adjusted to reflect the correct age range.
A review of more than 4,000 U.S. patients who were diagnosed with novel coronavirus infection (COVID-19) shows that an unexpected 20% of deaths occurred among adults aged 20-64 years, and 20% of those hospitalized were aged 20-44 years.
The expectation has been that people over 65 are most vulnerable to COVID-19 infection, but this study indicates that, at least in the United States, a significant number of patients under 45 can land in the hospital and can even die of the disease.
To assess rates of hospitalization, admission to an ICU, and death among patients with COVID-19 by age group, the Centers for Disease Control and Prevention analyzed 4,226 COVID-19 cases in the United States that were reported between Feb. 12 and March 16.
Overall, older patients in this group were the most likely to be hospitalized, to be admitted to ICU, and to die of COVID-19. A total of 31% of the cases, 45% of hospitalizations, 53% of ICU admissions, and 80% of deaths occurred in patients aged 65 years and older. “Similar to reports from other countries, this finding suggests that the risk for serious disease and death from COVID-19 is higher in older age groups,” said the investigators. “In contrast, persons aged [19 years and younger] appear to have milder COVID-19 illness, with almost no hospitalizations or deaths reported to date in the United States in this age group.”
But compared with the under-19 group, patients aged 20-44 years appeared to be at higher risk for hospitalization and ICU admission, according to the data published March 18 in Morbidity and Mortality Weekly Report.
The researchers excluded from their analysis patients who repatriated to the United States from Wuhan, China, and from Japan, including patients repatriated from cruise ships. Data on serious underlying health conditions were not available, and many cases were missing key data, they noted.
Among 508 patients known to have been hospitalized, 9% were aged 85 years or older, 36% were aged 65-84 years, 17% were aged 55-64 years, 18% were 45-54 years, and 20% were aged 20-44 years.
Among 121 patients admitted to an ICU, 7% were aged 85 years or older, 46% were aged 65-84 years, 36% were aged 45-64 years, and 12% were aged 20-44 years. Between 11% and 31% of patients with COVID-19 aged 75-84 years were admitted to an ICU.
Of 44 deaths, more than a third occurred among adults aged 85 years and older, and 46% occurred among adults aged 65-84 years, and 20% occurred among adults aged 20-64 years.
More follow-up time is needed to determine outcomes among active cases, the researchers said. These results also might overestimate the prevalence of severe disease because the initial approach to testing for COVID-19 focused on people with more severe disease. “These preliminary data also demonstrate that severe illness leading to hospitalization, including ICU admission and death, can occur in adults of any age with COVID-19,” according to the CDC.
SOURCE: CDC COVID-19 Response Team. MMWR Morb Mortal Wkly Rep. 2020 Mar 18. doi: 10.15585/mmwr.mm6912e2.
Do urgent care centers use optimal medications for acute migraine?
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
FROM HEADACHE
DMT use is common in older patients with MS
WEST PALM BEACH, FLA. –
MS disease activity typically declines with age. At the same time, evidence to support the efficacy of MS drugs in older patients is limited, said Yinan Zhang, MD, a researcher at Icahn School of Medicine at Mount Sinai, New York. Clinical trials have tended to enroll younger patients and to include only patients with active disease, which is not representative of most older patients in the real world, Dr. Zhang said.
“DMTs for MS may be less efficacious in the elderly, especially in the absence of active disease, yet real-world prescribing patterns still show widespread use of DMTs in older patients,” Dr. Zhang and colleagues said. Physicians may be able to use the presence of disease activity to identify older patients who should receive therapy. “Continuing DMTs in elderly patients who have no evidence of disease activity should be questioned rather than accepted,” they said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To investigate whether age affects the efficacy of DMTs in patients with relapsing-remitting MS and how often DMTs are used in different age groups, Dr. Zhang and coinvestigators conducted a meta-analysis of group-level data from clinical trial, analyzed individual-level data from one of the trials, and reviewed survey data from two registries.
The meta-analysis included 26 clinical trials of 13 DMTs with more than 12,400 patients. Participants had an average age of about 37 years. “An age-dependent relationship of DMTs on relapse rate in RRMS [relapsing-remitting MS] cannot be established with currently published aggregate summary data,” the researchers said. “The meta-analysis was limited by the use of group-level data resulting in a narrow range of mean age.”
In an effort to overcome the limitations of group-level data, they analyzed individual-level data from approximately 1,000 patients in the CombiRx trial, which compared interferon beta-1a plus glatiramer acetate versus the agents alone. Thirty-seven of the patients were aged 55 years or older. The results suggest that each “1-year increase in baseline age was associated with a 3.2% reduction in the odds of having a relapse” during the trial, the investigators said. Change in annualized relapse rate was not significantly associated with age group, which may have resulted from “enrollment criteria selecting for patients with active disease, where DMTs are expected to show the greatest efficacy,” the researchers said.
Finally, Dr. Zhang and colleagues reviewed data on DMT use by age group from the North American Research Committee on Multiple Sclerosis (NARCOMS) and the Multiple Sclerosis Surveillance Registry (MSSR) from Veterans Affairs. In a 2018 survey of nearly 7,000 patients in the NARCOMS registry, 39.2% of patients older than 60 years were taking a DMT, including 44.5% of patients aged 61-70, 28.6% of patients aged 71-80, and 11% of patients aged 81 years and older. In comparison, about 62% of patients aged 41-50 years were taking DMT.
A 2019 survey of about 1,700 veterans in the MSSR found that 36.3% of patients older than 60 years were taking a DMT, including 41.1% of patients aged 61-70, 27.2% of patients aged 71-80, and 7.1% of patients aged 81 years and older. Among patients aged 41-50 years, more than 72% were taking a DMT. “The continued use of DMTs in the elderly may be the result of the perceived notion that disease inactivity is due to the effect of DMTs rather than the natural disease course with aging,” they said.
Dr. Zhang had no relevant disclosures. Coauthors disclosed consulting for and grant support from various pharmaceutical companies.
SOURCE: Zhang Y et al. ACTRIMS Forum 2020. Abstract P263.
WEST PALM BEACH, FLA. –
MS disease activity typically declines with age. At the same time, evidence to support the efficacy of MS drugs in older patients is limited, said Yinan Zhang, MD, a researcher at Icahn School of Medicine at Mount Sinai, New York. Clinical trials have tended to enroll younger patients and to include only patients with active disease, which is not representative of most older patients in the real world, Dr. Zhang said.
“DMTs for MS may be less efficacious in the elderly, especially in the absence of active disease, yet real-world prescribing patterns still show widespread use of DMTs in older patients,” Dr. Zhang and colleagues said. Physicians may be able to use the presence of disease activity to identify older patients who should receive therapy. “Continuing DMTs in elderly patients who have no evidence of disease activity should be questioned rather than accepted,” they said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To investigate whether age affects the efficacy of DMTs in patients with relapsing-remitting MS and how often DMTs are used in different age groups, Dr. Zhang and coinvestigators conducted a meta-analysis of group-level data from clinical trial, analyzed individual-level data from one of the trials, and reviewed survey data from two registries.
The meta-analysis included 26 clinical trials of 13 DMTs with more than 12,400 patients. Participants had an average age of about 37 years. “An age-dependent relationship of DMTs on relapse rate in RRMS [relapsing-remitting MS] cannot be established with currently published aggregate summary data,” the researchers said. “The meta-analysis was limited by the use of group-level data resulting in a narrow range of mean age.”
In an effort to overcome the limitations of group-level data, they analyzed individual-level data from approximately 1,000 patients in the CombiRx trial, which compared interferon beta-1a plus glatiramer acetate versus the agents alone. Thirty-seven of the patients were aged 55 years or older. The results suggest that each “1-year increase in baseline age was associated with a 3.2% reduction in the odds of having a relapse” during the trial, the investigators said. Change in annualized relapse rate was not significantly associated with age group, which may have resulted from “enrollment criteria selecting for patients with active disease, where DMTs are expected to show the greatest efficacy,” the researchers said.
Finally, Dr. Zhang and colleagues reviewed data on DMT use by age group from the North American Research Committee on Multiple Sclerosis (NARCOMS) and the Multiple Sclerosis Surveillance Registry (MSSR) from Veterans Affairs. In a 2018 survey of nearly 7,000 patients in the NARCOMS registry, 39.2% of patients older than 60 years were taking a DMT, including 44.5% of patients aged 61-70, 28.6% of patients aged 71-80, and 11% of patients aged 81 years and older. In comparison, about 62% of patients aged 41-50 years were taking DMT.
A 2019 survey of about 1,700 veterans in the MSSR found that 36.3% of patients older than 60 years were taking a DMT, including 41.1% of patients aged 61-70, 27.2% of patients aged 71-80, and 7.1% of patients aged 81 years and older. Among patients aged 41-50 years, more than 72% were taking a DMT. “The continued use of DMTs in the elderly may be the result of the perceived notion that disease inactivity is due to the effect of DMTs rather than the natural disease course with aging,” they said.
Dr. Zhang had no relevant disclosures. Coauthors disclosed consulting for and grant support from various pharmaceutical companies.
SOURCE: Zhang Y et al. ACTRIMS Forum 2020. Abstract P263.
WEST PALM BEACH, FLA. –
MS disease activity typically declines with age. At the same time, evidence to support the efficacy of MS drugs in older patients is limited, said Yinan Zhang, MD, a researcher at Icahn School of Medicine at Mount Sinai, New York. Clinical trials have tended to enroll younger patients and to include only patients with active disease, which is not representative of most older patients in the real world, Dr. Zhang said.
“DMTs for MS may be less efficacious in the elderly, especially in the absence of active disease, yet real-world prescribing patterns still show widespread use of DMTs in older patients,” Dr. Zhang and colleagues said. Physicians may be able to use the presence of disease activity to identify older patients who should receive therapy. “Continuing DMTs in elderly patients who have no evidence of disease activity should be questioned rather than accepted,” they said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To investigate whether age affects the efficacy of DMTs in patients with relapsing-remitting MS and how often DMTs are used in different age groups, Dr. Zhang and coinvestigators conducted a meta-analysis of group-level data from clinical trial, analyzed individual-level data from one of the trials, and reviewed survey data from two registries.
The meta-analysis included 26 clinical trials of 13 DMTs with more than 12,400 patients. Participants had an average age of about 37 years. “An age-dependent relationship of DMTs on relapse rate in RRMS [relapsing-remitting MS] cannot be established with currently published aggregate summary data,” the researchers said. “The meta-analysis was limited by the use of group-level data resulting in a narrow range of mean age.”
In an effort to overcome the limitations of group-level data, they analyzed individual-level data from approximately 1,000 patients in the CombiRx trial, which compared interferon beta-1a plus glatiramer acetate versus the agents alone. Thirty-seven of the patients were aged 55 years or older. The results suggest that each “1-year increase in baseline age was associated with a 3.2% reduction in the odds of having a relapse” during the trial, the investigators said. Change in annualized relapse rate was not significantly associated with age group, which may have resulted from “enrollment criteria selecting for patients with active disease, where DMTs are expected to show the greatest efficacy,” the researchers said.
Finally, Dr. Zhang and colleagues reviewed data on DMT use by age group from the North American Research Committee on Multiple Sclerosis (NARCOMS) and the Multiple Sclerosis Surveillance Registry (MSSR) from Veterans Affairs. In a 2018 survey of nearly 7,000 patients in the NARCOMS registry, 39.2% of patients older than 60 years were taking a DMT, including 44.5% of patients aged 61-70, 28.6% of patients aged 71-80, and 11% of patients aged 81 years and older. In comparison, about 62% of patients aged 41-50 years were taking DMT.
A 2019 survey of about 1,700 veterans in the MSSR found that 36.3% of patients older than 60 years were taking a DMT, including 41.1% of patients aged 61-70, 27.2% of patients aged 71-80, and 7.1% of patients aged 81 years and older. Among patients aged 41-50 years, more than 72% were taking a DMT. “The continued use of DMTs in the elderly may be the result of the perceived notion that disease inactivity is due to the effect of DMTs rather than the natural disease course with aging,” they said.
Dr. Zhang had no relevant disclosures. Coauthors disclosed consulting for and grant support from various pharmaceutical companies.
SOURCE: Zhang Y et al. ACTRIMS Forum 2020. Abstract P263.
REPORTING FROM ACTRIMS FORUM 2020
Hyperlipidemia occurs earlier in patients with MS
WEST PALM BEACH, FLA. – Onset of hyperlipidemia tends to occur earlier in patients with multiple sclerosis (MS), compared with matched controls, according to new research. Among females and African Americans, the effect of MS on age of hyperlipidemia onset may be especially pronounced, said Diane Krill, PhD, professor of biological sciences at Point Park University, Pittsburgh, and colleagues.
Many patients with MS have hyperlipidemia, and adverse lipid profiles correlate with physical and cognitive impairment in this population. “There is evidence of endothelial dysfunction and inflammation in both MS and hyperlipidemia, but the timing of onset of hyperlipidemia is not known,” the researchers said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To assess whether patients with MS have hyperlipidemia diagnosed at an earlier age, relative to matched controls, Dr. Krill and colleagues analyzed data from the Cleveland Clinic health system. They included in their analyses patients with at least two hyperlipidemia diagnoses and at least five encounters with a primary care physician. They matched each patient with MS to four patients without MS using variables such as birth year, sex, race, and year of first encounter. In all, the study included 669 patients with MS and 2,676 controls. The investigators examined age of hyperlipidemia onset using multivariable Cox proportional hazard models that adjusted for sex, race, smoking, and body mass index.
Patients with MS had a 20% increased risk for earlier onset of hyperlipidemia, relative to matched controls. The effect was greater among females (hazard ratio, 1.22) and African Americans (HR, 1.42). Patients with MS have earlier onset of hyperlipidemia “irrespective of the relationship with age of MS onset,” Dr. Krill and colleagues noted. “Additional research is warranted to further characterize the temporal relationships between MS and hyperlipidemia, as well as considerations for timing of disease-modifying therapies.”
The researchers had no relevant disclosures.
SOURCE: Krill D et al. ACTRIMS Forum 2020, Abstract P085.
WEST PALM BEACH, FLA. – Onset of hyperlipidemia tends to occur earlier in patients with multiple sclerosis (MS), compared with matched controls, according to new research. Among females and African Americans, the effect of MS on age of hyperlipidemia onset may be especially pronounced, said Diane Krill, PhD, professor of biological sciences at Point Park University, Pittsburgh, and colleagues.
Many patients with MS have hyperlipidemia, and adverse lipid profiles correlate with physical and cognitive impairment in this population. “There is evidence of endothelial dysfunction and inflammation in both MS and hyperlipidemia, but the timing of onset of hyperlipidemia is not known,” the researchers said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To assess whether patients with MS have hyperlipidemia diagnosed at an earlier age, relative to matched controls, Dr. Krill and colleagues analyzed data from the Cleveland Clinic health system. They included in their analyses patients with at least two hyperlipidemia diagnoses and at least five encounters with a primary care physician. They matched each patient with MS to four patients without MS using variables such as birth year, sex, race, and year of first encounter. In all, the study included 669 patients with MS and 2,676 controls. The investigators examined age of hyperlipidemia onset using multivariable Cox proportional hazard models that adjusted for sex, race, smoking, and body mass index.
Patients with MS had a 20% increased risk for earlier onset of hyperlipidemia, relative to matched controls. The effect was greater among females (hazard ratio, 1.22) and African Americans (HR, 1.42). Patients with MS have earlier onset of hyperlipidemia “irrespective of the relationship with age of MS onset,” Dr. Krill and colleagues noted. “Additional research is warranted to further characterize the temporal relationships between MS and hyperlipidemia, as well as considerations for timing of disease-modifying therapies.”
The researchers had no relevant disclosures.
SOURCE: Krill D et al. ACTRIMS Forum 2020, Abstract P085.
WEST PALM BEACH, FLA. – Onset of hyperlipidemia tends to occur earlier in patients with multiple sclerosis (MS), compared with matched controls, according to new research. Among females and African Americans, the effect of MS on age of hyperlipidemia onset may be especially pronounced, said Diane Krill, PhD, professor of biological sciences at Point Park University, Pittsburgh, and colleagues.
Many patients with MS have hyperlipidemia, and adverse lipid profiles correlate with physical and cognitive impairment in this population. “There is evidence of endothelial dysfunction and inflammation in both MS and hyperlipidemia, but the timing of onset of hyperlipidemia is not known,” the researchers said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
To assess whether patients with MS have hyperlipidemia diagnosed at an earlier age, relative to matched controls, Dr. Krill and colleagues analyzed data from the Cleveland Clinic health system. They included in their analyses patients with at least two hyperlipidemia diagnoses and at least five encounters with a primary care physician. They matched each patient with MS to four patients without MS using variables such as birth year, sex, race, and year of first encounter. In all, the study included 669 patients with MS and 2,676 controls. The investigators examined age of hyperlipidemia onset using multivariable Cox proportional hazard models that adjusted for sex, race, smoking, and body mass index.
Patients with MS had a 20% increased risk for earlier onset of hyperlipidemia, relative to matched controls. The effect was greater among females (hazard ratio, 1.22) and African Americans (HR, 1.42). Patients with MS have earlier onset of hyperlipidemia “irrespective of the relationship with age of MS onset,” Dr. Krill and colleagues noted. “Additional research is warranted to further characterize the temporal relationships between MS and hyperlipidemia, as well as considerations for timing of disease-modifying therapies.”
The researchers had no relevant disclosures.
SOURCE: Krill D et al. ACTRIMS Forum 2020, Abstract P085.
REPORTING FROM ACTRIMS FORUM 2020
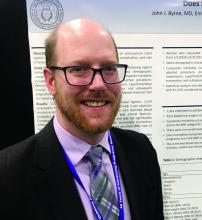
High BMI does not complicate postpartum tubal ligation
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
GRAPEVINE, TEXAS – Higher body mass index is not associated with increased morbidity in women undergoing postpartum tubal ligation, according to a study of more than 1,000 patients.
John J. Byrne, MD, said at the Pregnancy Meeting. Dr. Byrne is affiliated with the department of obstetrics and gynecology at University of Texas Southwestern Medical Center in Dallas.
Physicians may recommend contraception within 6 weeks of delivery, but many patients do not attend postpartum visits. “One option for women who have completed childbearing is bilateral midsegment salpingectomy via minilaparotomy,” Dr. Byrne said at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine. “Offering this procedure immediately after delivery makes it available to women who face obstacles to follow-up care.”
The procedure entails the risk of anesthetic complications, bowel injury, and vascular injury. Subsequent pregnancy or ectopic pregnancy also may occur. Some centers will not perform the procedure if a patient’s size affects the surgeon’s ability to feel the relevant anatomy, Dr. Byrne said. “Although operative complications are presumed to be higher among obese women,” prior studies have not examined whether BMI affects rates of procedure completion, complication, or subsequent pregnancy, the researchers said.
To study this question, Dr. Byrne and colleagues examined data from women who requested postpartum sterilization following vaginal delivery at their center in 2018. The center uses the Parkland tubal ligation technique. The researchers assessed complication rates using a composite measure that included surgical complications (that is, blood transfusion, aborted procedure, or extension of incision), anesthetic complications, readmission, superficial or deep wound infection, venous thromboembolism, ileus or small bowel obstruction, incomplete transection, and subsequent pregnancy. The investigators used statistical tests to assess the relationship between BMI and morbidity.
In all, 1,014 patients underwent a postpartum tubal ligation; 17% had undergone prior abdominal surgery. The researchers classified patients’ BMI as normal (7% of the population), overweight (28%), class I obesity (38%), class II obesity (18%), or class III obesity (9%). A composite morbidity event occurred in 2%, and the proportion of patients with a complication did not significantly differ across BMI categories. No morbid events occurred in patients with normal BMI, which indicates “minimal risk” in this population, Dr. Byrne said. One incomplete transection occurred in a patient with class I obesity, and one subsequent pregnancy occurred in a patient with class II obesity. Estimated blood loss ranged from 9 mL in patients with normal BMI to 13 mL in patients with class III obesity, and length of surgery ranged from 32 minutes to 40 minutes. Neither difference is clinically significant, Dr. Byrne said.
“For the woman who desires permanent contraception, BMI should not impede her access to the procedure,” he noted.
The researchers had no relevant disclosures.
SOURCE: Byrne JJ et al. Am J Obstet Gynecol. 2020 Jan;222(1):S290, Abstract 442.
REPORTING FROM THE PREGNANCY MEETING
Rotavirus vaccination is not a risk factor for type 1 diabetes
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
FROM JAMA PEDIATRICS
Key clinical point: Rotavirus vaccination is not associated with the incidence of type 1 diabetes and can be safely administered to infants.
Major finding: Compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for developing type 1 diabetes for children fully exposed to the vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to it, the aHR was 1.50 (95% CI, 0.81-2.77).
Study details: A retrospective cohort study of 386,937 children using data from the Vaccine Safety Datalink.
Disclosures: The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
Source: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
ERAS protocol for cesarean delivery reduces opioid usage
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
GRAPEVINE, TEX. – An enhanced recovery after surgery (ERAS) pathway for cesarean delivery decreased postoperative opioid usage by 62% in one health care organization, researchers reported at the Pregnancy Meeting. The protocol incorporates a stepwise approach to pain control with no scheduled postoperative opioids.
Abington Jefferson Health, which includes two hospitals in Pennsylvania, implemented an ERAS pathway for all cesarean deliveries in October 2018. Kathryn Ruymann, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Ruymann is an obstetrics and gynecology resident at Abington Jefferson Health.
Prior to the ERAS protocol, 99%-100% of patients took an opioid during the postoperative period. “With ERAS, 26% of patients never took an opioid during the postop period,” Dr. Ruymann and her associates reported. “Pain scores decreased with ERAS for postoperative days 1-3 and remained unchanged on day 4.”
One in 300 opioid-naive patients who receives opioids after cesarean delivery becomes a persistent user, one study has shown (Am J Obstet Gynecol. 2016 Sep; 215(3):353.e1-18). “ERAS pathways integrate evidence-based interventions before, during, and after surgery to optimize outcomes, specifically to decrease postoperative opioid use,” the researchers said.
While other surgical fields have adopted ERAS pathways, more research is needed in obstetrics, said Dr. Ruymann. More than 4,500 women deliver at Abington Jefferson Health each year, and about a third undergo cesarean deliveries.
The organization’s ERAS pathway incorporates preoperative education, fasting guidelines, and intraoperative analgesia, nausea prophylaxis, and antimicrobial therapy. Under the new protocol, postoperative analgesia includes scheduled administration of nonopioid medications, including celecoxib and acetaminophen. In addition, patients may take 5-10 mg of oxycodone orally every 4 hours as needed, and hydromorphone 0.4 mg IV as needed may be used for refractory pain. In addition, patients should resume eating as soon as tolerated and be out of bed within 4 hours after surgery, according to the protocol. Postoperative management of pruritus and instructions on how to wean off opioids at home are among the other elements of the enhanced recovery plan.
To examine postoperative opioid usage before and after implementation of the ERAS pathway, the investigators conducted a retrospective cohort study of 316 women who underwent cesarean delivery 3 months before the start of the ERAS pathway and 267 who underwent cesarean delivery 3 months after. The researchers used an application developed in Qlik Sense, a data analytics platform, to calculate opioid usage.
Mean postoperative opioid use decreased by 62%. The reduction in opioid use remained 8 months after starting the ERAS pathway.
“An ERAS pathway for [cesarean delivery] decreases postoperative opioid usage by integrating a multimodal stepwise approach to pain control and recovery,” the researchers said. “Standardized order sets and departmentwide education were crucial in the success of ERAS. Additional research is needed to evaluate the impact of unique components of ERAS in order to optimize this pathway.”
The researchers had no disclosures.
SOURCE: Ruymann K et al. Am J Obstet Gynecol. 2020 Jan;222(1):S212, Abstract 315.
REPORTING FROM THE PREGNANCY MEETING
Depression in MS predicted worsening of neurologic function
WEST PALM BEACH, FLA. – Among patients with relapsing-remitting multiple sclerosis (MS), depression increases the likelihood of having worse neurologic function one year later, according to a study presented at ACTRIMS Forum 2020. Patients’ subjective descriptions of disease activity did not significantly change during that time, which “suggests that depression is not merely a reactive phenomenon, but rather an independent contributor to clinical worsening in the long term,” said Jenny Feng, MD, a neuroimmunology fellow at the Mellen Center for MS Treatment and Research at the Cleveland Clinic.
The researchers hypothesize that depression’s influence on psychomotor function may contribute to clinical worsening in MS.
More than half of patients with MS have depression, and there is a higher prevalence of depression in relapsing-remitting MS than in progressive disease. “Depression is associated with systemic inflammation,” Dr. Feng said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We know that depressed individuals tend to have slower walking speeds, slower processing speeds, and worse quality of life measures.” But neurologists do not know whether patients feel depressed because the disease is getting worse, or whether depression is an independent contributing factor to MS, Dr. Feng said.
To examine whether depression affects neurologic performance and disease activity in patients with MS, Dr. Feng and colleagues analyzed real-world data from about 2,400 patients in MS PATHS (Multiple Sclerosis Partners Advancing Technology and Health Solutions), a network of centers in the United States and Europe. The researchers assessed the longitudinal relationship between depression, measures of neurologic function, and MRI metrics.
The researchers included patients with relapsing-remitting MS who had clinical and imaging data available at baseline and about 1 year later. Patients completed tests of manual dexterity, walking speed, and processing speed that are based on the Multiple Sclerosis Functional Composite. A worsening of 20% on any measure is considered clinically significant.
Patients had a mean age of about 45 years and mean disease duration of about 14 years. Patients with a T score greater than 45 on the Neuro-QoL depression questionnaire were classified as having depression, and approximately half of the population had depression. Patients with depression were more likely to have an employment status of disabled and to receive infusion medications.
The investigators used propensity score analysis to adjust for baseline differences between patients with and without depression and evaluated the effect of depression on year 1 outcome measures using logistic regression for categorical variables and linear regression for continuous variables.
“After propensity weighting for baseline covariates including neuroperformance scores, individuals with depression continued to worsen,” Dr. Feng said. Patients with depression were more likely to have a 20% worsening in at least one measure of neurologic performance at year 1 (odds ratio, 1.31). “There was a trend for increased odds of interval relapses, increased T2 lesion burden, and contrast-enhancing lesions at year 1” in patients with depression, but the results were not statistically significant. “Despite worsening neuroperformance at year 1 in individuals with baseline depression, their [patient-reported outcomes] at year 1 were not significantly worse.”
The researcher lacked information about the date of depression onset and medication compliance, Dr. Feng said. In addition, propensity weighting does not account for potential bias due to missing data.
The findings support the existing practice of actively screening for and treating depression in patients with MS, Dr. Feng said.
Dr. Feng had no disclosures. Coauthors have consulted for and received research support from pharmaceutical companies. MS PATHS is supported by Biogen.
SOURCE: Feng JJ et al. ACTRIMS Forum 2020. Abstract P226.
WEST PALM BEACH, FLA. – Among patients with relapsing-remitting multiple sclerosis (MS), depression increases the likelihood of having worse neurologic function one year later, according to a study presented at ACTRIMS Forum 2020. Patients’ subjective descriptions of disease activity did not significantly change during that time, which “suggests that depression is not merely a reactive phenomenon, but rather an independent contributor to clinical worsening in the long term,” said Jenny Feng, MD, a neuroimmunology fellow at the Mellen Center for MS Treatment and Research at the Cleveland Clinic.
The researchers hypothesize that depression’s influence on psychomotor function may contribute to clinical worsening in MS.
More than half of patients with MS have depression, and there is a higher prevalence of depression in relapsing-remitting MS than in progressive disease. “Depression is associated with systemic inflammation,” Dr. Feng said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We know that depressed individuals tend to have slower walking speeds, slower processing speeds, and worse quality of life measures.” But neurologists do not know whether patients feel depressed because the disease is getting worse, or whether depression is an independent contributing factor to MS, Dr. Feng said.
To examine whether depression affects neurologic performance and disease activity in patients with MS, Dr. Feng and colleagues analyzed real-world data from about 2,400 patients in MS PATHS (Multiple Sclerosis Partners Advancing Technology and Health Solutions), a network of centers in the United States and Europe. The researchers assessed the longitudinal relationship between depression, measures of neurologic function, and MRI metrics.
The researchers included patients with relapsing-remitting MS who had clinical and imaging data available at baseline and about 1 year later. Patients completed tests of manual dexterity, walking speed, and processing speed that are based on the Multiple Sclerosis Functional Composite. A worsening of 20% on any measure is considered clinically significant.
Patients had a mean age of about 45 years and mean disease duration of about 14 years. Patients with a T score greater than 45 on the Neuro-QoL depression questionnaire were classified as having depression, and approximately half of the population had depression. Patients with depression were more likely to have an employment status of disabled and to receive infusion medications.
The investigators used propensity score analysis to adjust for baseline differences between patients with and without depression and evaluated the effect of depression on year 1 outcome measures using logistic regression for categorical variables and linear regression for continuous variables.
“After propensity weighting for baseline covariates including neuroperformance scores, individuals with depression continued to worsen,” Dr. Feng said. Patients with depression were more likely to have a 20% worsening in at least one measure of neurologic performance at year 1 (odds ratio, 1.31). “There was a trend for increased odds of interval relapses, increased T2 lesion burden, and contrast-enhancing lesions at year 1” in patients with depression, but the results were not statistically significant. “Despite worsening neuroperformance at year 1 in individuals with baseline depression, their [patient-reported outcomes] at year 1 were not significantly worse.”
The researcher lacked information about the date of depression onset and medication compliance, Dr. Feng said. In addition, propensity weighting does not account for potential bias due to missing data.
The findings support the existing practice of actively screening for and treating depression in patients with MS, Dr. Feng said.
Dr. Feng had no disclosures. Coauthors have consulted for and received research support from pharmaceutical companies. MS PATHS is supported by Biogen.
SOURCE: Feng JJ et al. ACTRIMS Forum 2020. Abstract P226.
WEST PALM BEACH, FLA. – Among patients with relapsing-remitting multiple sclerosis (MS), depression increases the likelihood of having worse neurologic function one year later, according to a study presented at ACTRIMS Forum 2020. Patients’ subjective descriptions of disease activity did not significantly change during that time, which “suggests that depression is not merely a reactive phenomenon, but rather an independent contributor to clinical worsening in the long term,” said Jenny Feng, MD, a neuroimmunology fellow at the Mellen Center for MS Treatment and Research at the Cleveland Clinic.
The researchers hypothesize that depression’s influence on psychomotor function may contribute to clinical worsening in MS.
More than half of patients with MS have depression, and there is a higher prevalence of depression in relapsing-remitting MS than in progressive disease. “Depression is associated with systemic inflammation,” Dr. Feng said at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We know that depressed individuals tend to have slower walking speeds, slower processing speeds, and worse quality of life measures.” But neurologists do not know whether patients feel depressed because the disease is getting worse, or whether depression is an independent contributing factor to MS, Dr. Feng said.
To examine whether depression affects neurologic performance and disease activity in patients with MS, Dr. Feng and colleagues analyzed real-world data from about 2,400 patients in MS PATHS (Multiple Sclerosis Partners Advancing Technology and Health Solutions), a network of centers in the United States and Europe. The researchers assessed the longitudinal relationship between depression, measures of neurologic function, and MRI metrics.
The researchers included patients with relapsing-remitting MS who had clinical and imaging data available at baseline and about 1 year later. Patients completed tests of manual dexterity, walking speed, and processing speed that are based on the Multiple Sclerosis Functional Composite. A worsening of 20% on any measure is considered clinically significant.
Patients had a mean age of about 45 years and mean disease duration of about 14 years. Patients with a T score greater than 45 on the Neuro-QoL depression questionnaire were classified as having depression, and approximately half of the population had depression. Patients with depression were more likely to have an employment status of disabled and to receive infusion medications.
The investigators used propensity score analysis to adjust for baseline differences between patients with and without depression and evaluated the effect of depression on year 1 outcome measures using logistic regression for categorical variables and linear regression for continuous variables.
“After propensity weighting for baseline covariates including neuroperformance scores, individuals with depression continued to worsen,” Dr. Feng said. Patients with depression were more likely to have a 20% worsening in at least one measure of neurologic performance at year 1 (odds ratio, 1.31). “There was a trend for increased odds of interval relapses, increased T2 lesion burden, and contrast-enhancing lesions at year 1” in patients with depression, but the results were not statistically significant. “Despite worsening neuroperformance at year 1 in individuals with baseline depression, their [patient-reported outcomes] at year 1 were not significantly worse.”
The researcher lacked information about the date of depression onset and medication compliance, Dr. Feng said. In addition, propensity weighting does not account for potential bias due to missing data.
The findings support the existing practice of actively screening for and treating depression in patients with MS, Dr. Feng said.
Dr. Feng had no disclosures. Coauthors have consulted for and received research support from pharmaceutical companies. MS PATHS is supported by Biogen.
SOURCE: Feng JJ et al. ACTRIMS Forum 2020. Abstract P226.
REPORTING FROM ACTRIMS Forum 2020