User login
Supreme Court won’t hear IPAB challenge
The Supreme Court has declined to hear a case challenging the Independent Payment Advisory Board.
This leaves in place a ruling from the 9th U.S. Circuit Court of appeals, which dismissed the lawsuit Coons v. Lew, on the grounds that the plaintiffs failed to show harm from the provision of the Affordable Care Act that created the IPAB.
The 15-member panel, created under the ACA to help control health care costs, is charged with identifying cuts to Medicare when the program’s spending exceeds gross domestic product plus 1%. Current slowing growth in Medicare spending had meant that the IPAB provision has not be triggered, and so far no members have been named to the panel.
Attorneys representing the plaintiff said they remain ready to refile their case if and when the IPAB is ever activated.
“This case is not dead; we’re simply in a holding pattern,” Christina Sandefur, senior attorney at the Goldwater Institute, said in a statement.
Congress also continues to look at the IPAB. In March, Rep. Phil Roe (R-Tenn.) reintroduced legislation to repeal the panel.
The Supreme Court has declined to hear a case challenging the Independent Payment Advisory Board.
This leaves in place a ruling from the 9th U.S. Circuit Court of appeals, which dismissed the lawsuit Coons v. Lew, on the grounds that the plaintiffs failed to show harm from the provision of the Affordable Care Act that created the IPAB.
The 15-member panel, created under the ACA to help control health care costs, is charged with identifying cuts to Medicare when the program’s spending exceeds gross domestic product plus 1%. Current slowing growth in Medicare spending had meant that the IPAB provision has not be triggered, and so far no members have been named to the panel.
Attorneys representing the plaintiff said they remain ready to refile their case if and when the IPAB is ever activated.
“This case is not dead; we’re simply in a holding pattern,” Christina Sandefur, senior attorney at the Goldwater Institute, said in a statement.
Congress also continues to look at the IPAB. In March, Rep. Phil Roe (R-Tenn.) reintroduced legislation to repeal the panel.
The Supreme Court has declined to hear a case challenging the Independent Payment Advisory Board.
This leaves in place a ruling from the 9th U.S. Circuit Court of appeals, which dismissed the lawsuit Coons v. Lew, on the grounds that the plaintiffs failed to show harm from the provision of the Affordable Care Act that created the IPAB.
The 15-member panel, created under the ACA to help control health care costs, is charged with identifying cuts to Medicare when the program’s spending exceeds gross domestic product plus 1%. Current slowing growth in Medicare spending had meant that the IPAB provision has not be triggered, and so far no members have been named to the panel.
Attorneys representing the plaintiff said they remain ready to refile their case if and when the IPAB is ever activated.
“This case is not dead; we’re simply in a holding pattern,” Christina Sandefur, senior attorney at the Goldwater Institute, said in a statement.
Congress also continues to look at the IPAB. In March, Rep. Phil Roe (R-Tenn.) reintroduced legislation to repeal the panel.
Commonwealth Fund: ACA’s medical loss ratio rule saves $5 billion
The Affordable Care Act’s requirement that health insurers pay out a minimum percentage of premiums in medical claims or quality improvement generated $5 billion in savings from 2011 to 2013, according to the Commonwealth Fund.
However, insurance companies were not increasing spending on quality improvements during that period, according to a report released March 26.
Under the ACA, insurers who fail to meet minimum percentages of premiums paid as claims must rebate the difference to consumers.
In 2011, insurers paid $1.1 billion in rebates, researchers found. That figured dropped to $325 million in 2013, with the rebate total across the 3-year period being nearly $2 billion. The remaining $3 billion was generated from reductions in administrative costs without any increase in net profits during that time period.
The decline in consumer rebates reflects “greater compliance with the [medical loss ratio] rule,” the report’s authors noted, and “that insurers are spending a larger percentage of premium dollars on medical claims.”
The report noted that insurers could spend premium dollars on quality improvement to meet requirements – but in 2013, those quality improvement expenses remained at just below 1% and were relatively steady during the study period.
The Affordable Care Act’s requirement that health insurers pay out a minimum percentage of premiums in medical claims or quality improvement generated $5 billion in savings from 2011 to 2013, according to the Commonwealth Fund.
However, insurance companies were not increasing spending on quality improvements during that period, according to a report released March 26.
Under the ACA, insurers who fail to meet minimum percentages of premiums paid as claims must rebate the difference to consumers.
In 2011, insurers paid $1.1 billion in rebates, researchers found. That figured dropped to $325 million in 2013, with the rebate total across the 3-year period being nearly $2 billion. The remaining $3 billion was generated from reductions in administrative costs without any increase in net profits during that time period.
The decline in consumer rebates reflects “greater compliance with the [medical loss ratio] rule,” the report’s authors noted, and “that insurers are spending a larger percentage of premium dollars on medical claims.”
The report noted that insurers could spend premium dollars on quality improvement to meet requirements – but in 2013, those quality improvement expenses remained at just below 1% and were relatively steady during the study period.
The Affordable Care Act’s requirement that health insurers pay out a minimum percentage of premiums in medical claims or quality improvement generated $5 billion in savings from 2011 to 2013, according to the Commonwealth Fund.
However, insurance companies were not increasing spending on quality improvements during that period, according to a report released March 26.
Under the ACA, insurers who fail to meet minimum percentages of premiums paid as claims must rebate the difference to consumers.
In 2011, insurers paid $1.1 billion in rebates, researchers found. That figured dropped to $325 million in 2013, with the rebate total across the 3-year period being nearly $2 billion. The remaining $3 billion was generated from reductions in administrative costs without any increase in net profits during that time period.
The decline in consumer rebates reflects “greater compliance with the [medical loss ratio] rule,” the report’s authors noted, and “that insurers are spending a larger percentage of premium dollars on medical claims.”
The report noted that insurers could spend premium dollars on quality improvement to meet requirements – but in 2013, those quality improvement expenses remained at just below 1% and were relatively steady during the study period.
CMS: Stage 3 meaningful use by 2018
All physicians and hospitals would need to meet stage 3 meaningful use beginning in 2018, according to a recent proposal by the Centers for Medicare & Medicaid Services.
In the agency’s Stage 3 proposed rule, there would be no transition period from earlier stages for those just starting or those who were in an earlier stage. CMS said that this is “expected to be the final stage” and will incorporate elements of the previous two stages.
That change comes along with the proposal beginning in 2017 to permanently make the attestation period a full year, with a few exceptions. A full-year attestation period was supposed to go into effect for 2015 with Stage 2, but CMS announced that it would reduce attestation to a 90-day period because of low participation.
The final year in which participants in the EHR Incentive Programs can receive bonus payments for meeting meaningful use criteria is 2017; penalties for failing to meet criteria have already begun.
The American College of Cardiology said in a statement that it is “concerned” by the proposal that even new physicians and practices will have to jump immediately to stage 3 in 2018 without a transition period.
“Implementing an EHR system in a physician or a hospital is not as simple as flipping a switch; it takes time, financial investment, careful consideration and planning, as well as education for all staff. The program must take this learning curve into consideration,” Dr. Kim Allan Williams Sr., ACC president, said in a statement.
The proposed rule also contains a number of more stringent requirements. On the patient engagement front, the proposed rule calls for 25% of patients to access their data, although it also allows for third-party providers to access a patient’s account as a means of satisfying the requirement. Patient-generated data also are highlighted, with a proposed requirement that physicians collect information via mobile devices or apps from 15% of their patients.Under the proposed Stage 3 of meaningful use, physicians and eligible hospitals must meet two of three criteria: that more than 50% of referrals or transitions of care involve the passing of information by the referring provider; that more than 40% of transitions or referrals received by a provider seeing a patient for the first time include information imported into that new provider’s EHR; or that for more than 80% of those new patients seen in transition or by referral for the first time, a clinical reconciliation be done on the information received during the health information exchange, including a review of current medications, medication allergies, and current and active diagnoses.
The proposed rule is scheduled to be published in the Federal Register on March 30; comments will be accepted at www.regulations.gov until May 29.
All physicians and hospitals would need to meet stage 3 meaningful use beginning in 2018, according to a recent proposal by the Centers for Medicare & Medicaid Services.
In the agency’s Stage 3 proposed rule, there would be no transition period from earlier stages for those just starting or those who were in an earlier stage. CMS said that this is “expected to be the final stage” and will incorporate elements of the previous two stages.
That change comes along with the proposal beginning in 2017 to permanently make the attestation period a full year, with a few exceptions. A full-year attestation period was supposed to go into effect for 2015 with Stage 2, but CMS announced that it would reduce attestation to a 90-day period because of low participation.
The final year in which participants in the EHR Incentive Programs can receive bonus payments for meeting meaningful use criteria is 2017; penalties for failing to meet criteria have already begun.
The American College of Cardiology said in a statement that it is “concerned” by the proposal that even new physicians and practices will have to jump immediately to stage 3 in 2018 without a transition period.
“Implementing an EHR system in a physician or a hospital is not as simple as flipping a switch; it takes time, financial investment, careful consideration and planning, as well as education for all staff. The program must take this learning curve into consideration,” Dr. Kim Allan Williams Sr., ACC president, said in a statement.
The proposed rule also contains a number of more stringent requirements. On the patient engagement front, the proposed rule calls for 25% of patients to access their data, although it also allows for third-party providers to access a patient’s account as a means of satisfying the requirement. Patient-generated data also are highlighted, with a proposed requirement that physicians collect information via mobile devices or apps from 15% of their patients.Under the proposed Stage 3 of meaningful use, physicians and eligible hospitals must meet two of three criteria: that more than 50% of referrals or transitions of care involve the passing of information by the referring provider; that more than 40% of transitions or referrals received by a provider seeing a patient for the first time include information imported into that new provider’s EHR; or that for more than 80% of those new patients seen in transition or by referral for the first time, a clinical reconciliation be done on the information received during the health information exchange, including a review of current medications, medication allergies, and current and active diagnoses.
The proposed rule is scheduled to be published in the Federal Register on March 30; comments will be accepted at www.regulations.gov until May 29.
All physicians and hospitals would need to meet stage 3 meaningful use beginning in 2018, according to a recent proposal by the Centers for Medicare & Medicaid Services.
In the agency’s Stage 3 proposed rule, there would be no transition period from earlier stages for those just starting or those who were in an earlier stage. CMS said that this is “expected to be the final stage” and will incorporate elements of the previous two stages.
That change comes along with the proposal beginning in 2017 to permanently make the attestation period a full year, with a few exceptions. A full-year attestation period was supposed to go into effect for 2015 with Stage 2, but CMS announced that it would reduce attestation to a 90-day period because of low participation.
The final year in which participants in the EHR Incentive Programs can receive bonus payments for meeting meaningful use criteria is 2017; penalties for failing to meet criteria have already begun.
The American College of Cardiology said in a statement that it is “concerned” by the proposal that even new physicians and practices will have to jump immediately to stage 3 in 2018 without a transition period.
“Implementing an EHR system in a physician or a hospital is not as simple as flipping a switch; it takes time, financial investment, careful consideration and planning, as well as education for all staff. The program must take this learning curve into consideration,” Dr. Kim Allan Williams Sr., ACC president, said in a statement.
The proposed rule also contains a number of more stringent requirements. On the patient engagement front, the proposed rule calls for 25% of patients to access their data, although it also allows for third-party providers to access a patient’s account as a means of satisfying the requirement. Patient-generated data also are highlighted, with a proposed requirement that physicians collect information via mobile devices or apps from 15% of their patients.Under the proposed Stage 3 of meaningful use, physicians and eligible hospitals must meet two of three criteria: that more than 50% of referrals or transitions of care involve the passing of information by the referring provider; that more than 40% of transitions or referrals received by a provider seeing a patient for the first time include information imported into that new provider’s EHR; or that for more than 80% of those new patients seen in transition or by referral for the first time, a clinical reconciliation be done on the information received during the health information exchange, including a review of current medications, medication allergies, and current and active diagnoses.
The proposed rule is scheduled to be published in the Federal Register on March 30; comments will be accepted at www.regulations.gov until May 29.
Medicare advisers: Cancer prognostic tests not ready for prime time
BALTIMORE – While prognostic tests tied to specific chemotherapy agents may offer a clear benefit in guiding treatment and improving outcomes for certain malignancies, applying the tests more broadly may not offer information that is clinically relevant.
Members of the Medicare Evidence Development & Coverage Advisory Committee were asked to examine prognostic tests for three types of cancers – adenocarcinoma of the colon and rectum, breast cancer (both invasive duct and lobular cancers), and non–small cell lung cancers – in a preliminary effort to determine how Medicare should pay for the use of such tests. They found little evidence on how these tests could lead to better outcomes, despite evidence showing the tests did confirm the analytic and clinical validity of the biomarkers.
Turning to the usefulness of such tests in aiding clinical decision making by physicians and patients, data on “the downstream effects of these tests ... got very thin very quickly,” according to advisory committee member Dr. Beverly A. Guadagnolo of the department of radiation oncology at M.D. Anderson Cancer Center, Houston.
At its March 24 meeting, the committee found that only three tests – microsatellite instability tests in adenocarcinoma of the colon and rectum, and MammaPrint and Oncotype DX Breast – showed evidence of some level of utility in managing patients and improving outcomes; however, none reached an average of 3 (intermediate confidence) on the committee’s 5-point scale of evaluating the strength of the evidence. Oncotype DX Breast was the highest, with a 2.875 average vote across the eight voting members.
Dr. Mitchell Kamrava of the department of radiation oncology at the University of California, Los Angeles, also noted that physicians are doing their best to understand what the different biomarkers actually mean when it comes to treating patients, “but the data are just not quite there yet.”
For Medicare officials, the emphasis going forward will be how useful these tests will be for improving care.
“We approached various lab vendors and they are able to show us plenty of information in terms of analytic validity as well as clinical validity,” Dr. James Rollins, director of the Division of Items and Devices in CMS’ Coverage & Analysis Group, said. “Some of them feel that demonstrating clinical utility is something that they don’t need to provide commercial insurers. I don’t know why they feel that way. But as I said, as time goes on, we will be using more and more clinical utility.”
CMS currently does not have any open national coverage analysis decisions that relate to prognostic cancer tests.
Dr. Rollins said the agency is defining clinical utility as information that leads to improved health outcomes either due to increased benefit or reduction in harm.
BALTIMORE – While prognostic tests tied to specific chemotherapy agents may offer a clear benefit in guiding treatment and improving outcomes for certain malignancies, applying the tests more broadly may not offer information that is clinically relevant.
Members of the Medicare Evidence Development & Coverage Advisory Committee were asked to examine prognostic tests for three types of cancers – adenocarcinoma of the colon and rectum, breast cancer (both invasive duct and lobular cancers), and non–small cell lung cancers – in a preliminary effort to determine how Medicare should pay for the use of such tests. They found little evidence on how these tests could lead to better outcomes, despite evidence showing the tests did confirm the analytic and clinical validity of the biomarkers.
Turning to the usefulness of such tests in aiding clinical decision making by physicians and patients, data on “the downstream effects of these tests ... got very thin very quickly,” according to advisory committee member Dr. Beverly A. Guadagnolo of the department of radiation oncology at M.D. Anderson Cancer Center, Houston.
At its March 24 meeting, the committee found that only three tests – microsatellite instability tests in adenocarcinoma of the colon and rectum, and MammaPrint and Oncotype DX Breast – showed evidence of some level of utility in managing patients and improving outcomes; however, none reached an average of 3 (intermediate confidence) on the committee’s 5-point scale of evaluating the strength of the evidence. Oncotype DX Breast was the highest, with a 2.875 average vote across the eight voting members.
Dr. Mitchell Kamrava of the department of radiation oncology at the University of California, Los Angeles, also noted that physicians are doing their best to understand what the different biomarkers actually mean when it comes to treating patients, “but the data are just not quite there yet.”
For Medicare officials, the emphasis going forward will be how useful these tests will be for improving care.
“We approached various lab vendors and they are able to show us plenty of information in terms of analytic validity as well as clinical validity,” Dr. James Rollins, director of the Division of Items and Devices in CMS’ Coverage & Analysis Group, said. “Some of them feel that demonstrating clinical utility is something that they don’t need to provide commercial insurers. I don’t know why they feel that way. But as I said, as time goes on, we will be using more and more clinical utility.”
CMS currently does not have any open national coverage analysis decisions that relate to prognostic cancer tests.
Dr. Rollins said the agency is defining clinical utility as information that leads to improved health outcomes either due to increased benefit or reduction in harm.
BALTIMORE – While prognostic tests tied to specific chemotherapy agents may offer a clear benefit in guiding treatment and improving outcomes for certain malignancies, applying the tests more broadly may not offer information that is clinically relevant.
Members of the Medicare Evidence Development & Coverage Advisory Committee were asked to examine prognostic tests for three types of cancers – adenocarcinoma of the colon and rectum, breast cancer (both invasive duct and lobular cancers), and non–small cell lung cancers – in a preliminary effort to determine how Medicare should pay for the use of such tests. They found little evidence on how these tests could lead to better outcomes, despite evidence showing the tests did confirm the analytic and clinical validity of the biomarkers.
Turning to the usefulness of such tests in aiding clinical decision making by physicians and patients, data on “the downstream effects of these tests ... got very thin very quickly,” according to advisory committee member Dr. Beverly A. Guadagnolo of the department of radiation oncology at M.D. Anderson Cancer Center, Houston.
At its March 24 meeting, the committee found that only three tests – microsatellite instability tests in adenocarcinoma of the colon and rectum, and MammaPrint and Oncotype DX Breast – showed evidence of some level of utility in managing patients and improving outcomes; however, none reached an average of 3 (intermediate confidence) on the committee’s 5-point scale of evaluating the strength of the evidence. Oncotype DX Breast was the highest, with a 2.875 average vote across the eight voting members.
Dr. Mitchell Kamrava of the department of radiation oncology at the University of California, Los Angeles, also noted that physicians are doing their best to understand what the different biomarkers actually mean when it comes to treating patients, “but the data are just not quite there yet.”
For Medicare officials, the emphasis going forward will be how useful these tests will be for improving care.
“We approached various lab vendors and they are able to show us plenty of information in terms of analytic validity as well as clinical validity,” Dr. James Rollins, director of the Division of Items and Devices in CMS’ Coverage & Analysis Group, said. “Some of them feel that demonstrating clinical utility is something that they don’t need to provide commercial insurers. I don’t know why they feel that way. But as I said, as time goes on, we will be using more and more clinical utility.”
CMS currently does not have any open national coverage analysis decisions that relate to prognostic cancer tests.
Dr. Rollins said the agency is defining clinical utility as information that leads to improved health outcomes either due to increased benefit or reduction in harm.
AT A MEDCAC MEETING
Medicaid expansion brings coverage to more diabetes patients
More new diabetes patients are being diagnosed in states that have expanded their Medicaid programs under the Affordable Care Act, compared with states that chose not to expand, according to a study published online March 23 in Diabetes Care.
Dr. Harvey Kaufman, senior medical director at Quest Diagnostics, and his colleagues analyzed data from Quest Diagnostics’ corporate database of clinical laboratory services for the first 6 months of 2013 and the same period in 2014, identifying 215,398 with a new diagnosis of diabetes in 2013 and 218,890 in 2014. A total of 26,237 were enrolled in Medicaid in 2013 vs. 29,673 in 2014 – a 13% increase in overall new diagnoses of diabetes.
The increase was greater – 23% – in the 26 states and the District of Columbia that had expanded their Medicaid programs. In states that had not expanded, the increase in newly diagnosed patients was 0.4% (Diabetes Care 2015 March 23 [doi: 10.2337/dc14-2334]).
“It is likely that changes in access to health care for patients with Medicaid contributed to testing for diabetes at an earlier stage of disease,” Dr. Kaufman wrote .
Access to health care also identified patients at earlier stages of diabetes, as evidenced by diagnosis at a lower mean hemoglobin A1c level. In states with expanded Medicaid programs, mean HbA1c was 7.96 at diagnosis, compared to 8.14 in states without expanded Medicaid programs.
“These Medicaid patients with newly identified diabetes will experience better management of their diabetes than if diagnosis had been made later,” Dr.Kaufman wrote. “This could be anticipated to lead to fewer long-term complications.”
The data demonstrate the benefits of Medicaid expansion, yet nearly half of our states have chosen not to expand this benefit to their citizens. The real-world benefits and costs of Medicaid expansion merit additional research and civil debate. And perhaps, most important, their results should be used to guide health policy to address the growing burden of chronic disease.
Dr. William Herman is professor of internal medicine at the University of Michigan; Dr. William Cefalu is executive director of the Pennington Biomedical Research Center at Louisiana State University in Baton Rouge, La. Their views are taken from an editorial accompanying the study (Diabetes Care 2015 March 23 [doi: 10.2337/dc15-0348]).
The data demonstrate the benefits of Medicaid expansion, yet nearly half of our states have chosen not to expand this benefit to their citizens. The real-world benefits and costs of Medicaid expansion merit additional research and civil debate. And perhaps, most important, their results should be used to guide health policy to address the growing burden of chronic disease.
Dr. William Herman is professor of internal medicine at the University of Michigan; Dr. William Cefalu is executive director of the Pennington Biomedical Research Center at Louisiana State University in Baton Rouge, La. Their views are taken from an editorial accompanying the study (Diabetes Care 2015 March 23 [doi: 10.2337/dc15-0348]).
The data demonstrate the benefits of Medicaid expansion, yet nearly half of our states have chosen not to expand this benefit to their citizens. The real-world benefits and costs of Medicaid expansion merit additional research and civil debate. And perhaps, most important, their results should be used to guide health policy to address the growing burden of chronic disease.
Dr. William Herman is professor of internal medicine at the University of Michigan; Dr. William Cefalu is executive director of the Pennington Biomedical Research Center at Louisiana State University in Baton Rouge, La. Their views are taken from an editorial accompanying the study (Diabetes Care 2015 March 23 [doi: 10.2337/dc15-0348]).
More new diabetes patients are being diagnosed in states that have expanded their Medicaid programs under the Affordable Care Act, compared with states that chose not to expand, according to a study published online March 23 in Diabetes Care.
Dr. Harvey Kaufman, senior medical director at Quest Diagnostics, and his colleagues analyzed data from Quest Diagnostics’ corporate database of clinical laboratory services for the first 6 months of 2013 and the same period in 2014, identifying 215,398 with a new diagnosis of diabetes in 2013 and 218,890 in 2014. A total of 26,237 were enrolled in Medicaid in 2013 vs. 29,673 in 2014 – a 13% increase in overall new diagnoses of diabetes.
The increase was greater – 23% – in the 26 states and the District of Columbia that had expanded their Medicaid programs. In states that had not expanded, the increase in newly diagnosed patients was 0.4% (Diabetes Care 2015 March 23 [doi: 10.2337/dc14-2334]).
“It is likely that changes in access to health care for patients with Medicaid contributed to testing for diabetes at an earlier stage of disease,” Dr. Kaufman wrote .
Access to health care also identified patients at earlier stages of diabetes, as evidenced by diagnosis at a lower mean hemoglobin A1c level. In states with expanded Medicaid programs, mean HbA1c was 7.96 at diagnosis, compared to 8.14 in states without expanded Medicaid programs.
“These Medicaid patients with newly identified diabetes will experience better management of their diabetes than if diagnosis had been made later,” Dr.Kaufman wrote. “This could be anticipated to lead to fewer long-term complications.”
More new diabetes patients are being diagnosed in states that have expanded their Medicaid programs under the Affordable Care Act, compared with states that chose not to expand, according to a study published online March 23 in Diabetes Care.
Dr. Harvey Kaufman, senior medical director at Quest Diagnostics, and his colleagues analyzed data from Quest Diagnostics’ corporate database of clinical laboratory services for the first 6 months of 2013 and the same period in 2014, identifying 215,398 with a new diagnosis of diabetes in 2013 and 218,890 in 2014. A total of 26,237 were enrolled in Medicaid in 2013 vs. 29,673 in 2014 – a 13% increase in overall new diagnoses of diabetes.
The increase was greater – 23% – in the 26 states and the District of Columbia that had expanded their Medicaid programs. In states that had not expanded, the increase in newly diagnosed patients was 0.4% (Diabetes Care 2015 March 23 [doi: 10.2337/dc14-2334]).
“It is likely that changes in access to health care for patients with Medicaid contributed to testing for diabetes at an earlier stage of disease,” Dr. Kaufman wrote .
Access to health care also identified patients at earlier stages of diabetes, as evidenced by diagnosis at a lower mean hemoglobin A1c level. In states with expanded Medicaid programs, mean HbA1c was 7.96 at diagnosis, compared to 8.14 in states without expanded Medicaid programs.
“These Medicaid patients with newly identified diabetes will experience better management of their diabetes than if diagnosis had been made later,” Dr.Kaufman wrote. “This could be anticipated to lead to fewer long-term complications.”
FROM DIABETES CARE
Key clinical point: Health care coverage can lead to improved outcomes in diabetes patients.
Major finding: Twenty-three percent more Medicaid patients received a new diagnosis of diabetes in states that have expanded their Medicaid programs than in states that did not.
Data source: Analysis of more than 150 million clinical laboratory records in a corporate database maintained by Quest Diagnostics.
Disclosures: Dr. Kauffman is an employee of Quest Diagnostics. A coauthor reported financial ties with makers of diabetes drugs.
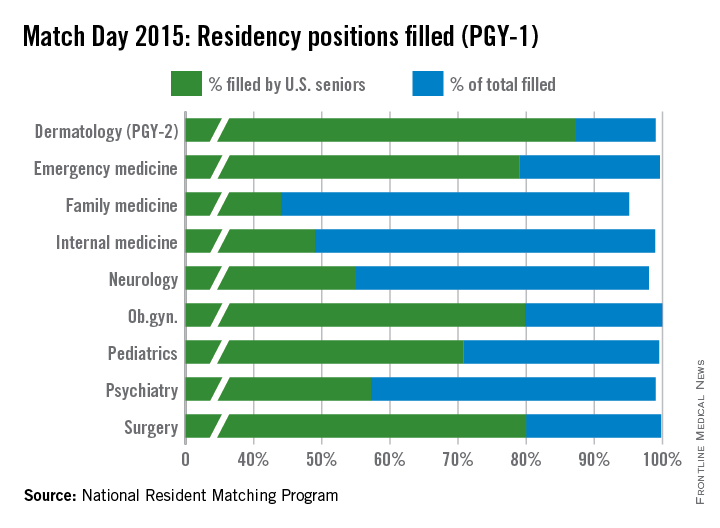
Match Day 2015: Primary care continues slow growth
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
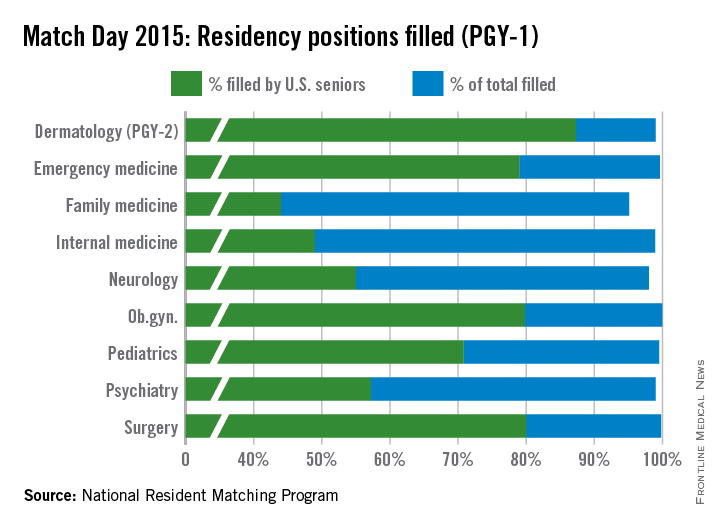
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
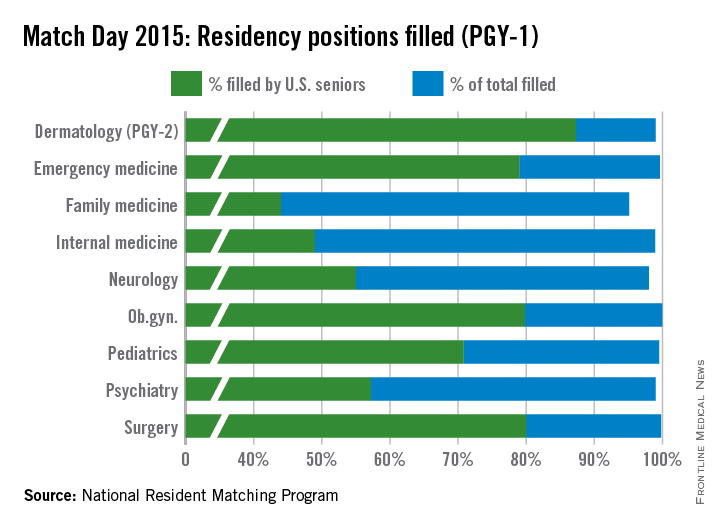
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.
Medical school seniors continue to show an increasing interest in primary care, according to the results of the 2015 Main Residency Match.
And for the third year in a row a record number of first- and second-year residency positions were offered – 30,212 positions, up from the 29,671 positions in 2014, according to the National Resident Matching Program (NRMP).
Family medicine residency programs offered a total of 3,195 positions in the 2105 match, up from 3,109 last year. Greater than 95% of those positions were filled; 44% were filled by U.S. medical school graduates, the NRMP announced March 20.
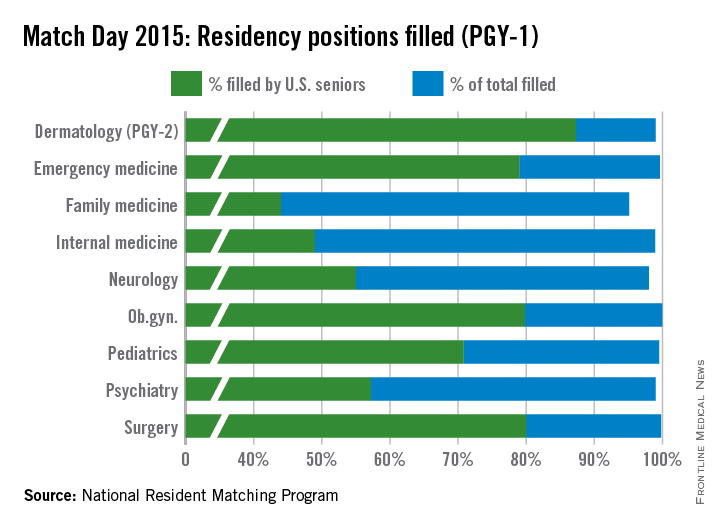
Numbers were similar in internal medicine, where residency programs offered 6,770 positions this year, up from 6,542 in 2014. Just under 99% of positions were filled, with 49% filled by U.S. medical school graduates.
The match results demonstrate “stability in the number of individuals going into internal medicine,” Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians, said in an interview. “We’re impressed that there were more students in this year’s match and there were more training positions available in this year’s match as well and yet despite that, we were able to continue to fill most of the programs.”
Dr. Robert Wergin, president of the American Academy of Family Physicians expressed some concern about the number of U.S. medical school graduates matching to family medicine.
“We saw a consistent and increasing growth in U.S. medical students matching to family medicine during the implementation of health system reforms that emphasized the importance of comprehensive primary medical care,” Dr. Wergin said in a statement. “That has slowed as policy makers have pulled back from supporting primary medical care.”
Pediatric positions saw a slight increase in the total number of positions offered to 2,668 from 2,640. U.S. graduates matched to 71% of the 2,654 positions filled. The 1,889 positions filled by U.S. medical school students is up from the 1,818 slots filled in 2014, suggesting last year’s decline was just a blip in a 5-year trend that has been increasing each year in general.
The increase in primary care positions also caught the eye of NRMP President and CEO Mona Signer.
“It’s a good trend for health manpower in general that there are more primary care physicians because, obviously, if you’ve done any reading at all, you know that primary care is where a shortage is anticipated,” Ms. Signer said in an interview.
Concerns still remain regarding whether future primary care workforce needs will be met. Key obstacles include sizable medical school debt and the hassles of owning a medical practice, Dr Alguire said. “I have a feeling that unless those are addressed head on with a national strategy for improving the physician workforce in the United States, these problems will continue.”
He added that the geographic distribution of the physician workforce is problematic, too.
“If you look at the distribution of many physicians, they tend to congregate in cities and there are fewer primary care physicians in the areas of greater need in rural areas and I think we need to address that strategically rather than simply hoping that physicians will go to those areas of great need and begin to practice primary care,” Dr. Alguire said.
Dr. Wergin added that the increases need to speed “dramatically” to ensure necessary access to primary care.
SGR repeal bill reintroduced; payment mechanism not addressed
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
A bill to repeal the Medicare Sustainable Growth Rate formula was reintroduced into the House and Senate March 19.
H.R. 1470, the SGR Repeal and Medicare Provider Payment Modernization Act, is described as “nearly identical” to the bicameral, bipartisan bill that was passed in the House in April 2014, with a spokesman for the House Ways & Means Committee describing the changes as technical in nature.
The bill’s introduction comes as the latest so-called “doc fix” patch set to expire on March 31, with a physician payment cut of 21% set to go into effect on April 1. Congress previously has passed 17 patches.
In addition to repealing the SGR, the bill includes a 0.5% pay increase per year for the next 5 years; consolidates existing quality programs into a single value-based performance program; incentivizes physicians to use alternate payment models that focus on care coordination and prevention to improve quality and reduce costs; and pushes more transparency of Medicare data for both patients and providers to help them improve care.
It does not address any how to pay for SGR repeal, nor does it include any language to extend funding for the Children’s Health Insurance Program, which expires in 2015.
Dr. David Fleming, president of the American College of Physicians, said in a statement that the bill “achieves ACP’s top priorities for physician payment reform,” and “strongly urges” its passage before the current patch expires.
A March 16 letter, signed by more than 750 organizations, including national and state medical societies, was sent to House Speaker John Boehner (R-Ohio), calling for passage of last year’s SGR repeal.
Rep. Michael C. Burgess (R-Texas) cosponsored the bill in the House with Republican and Democratic leadership in the Ways and Means and Energy and Commerce Committees and the chairmen and ranking members of their health subcommittees. The Senate version of the bill was introduce by Finance Committee Chairman Orrin Hatch (R-Utah).
ACP: Avoid ECG, MPI cardiac screening in low-risk patients
Clinicians should not screen for cardiac disease in asymptomatic, low-risk adults using resting or stress electrocardiography, stress echocardiography, or stress myocardial perfusion imaging , according to new guidelines from the American College of Physicians.
“There is no evidence that cardiac screening of low-risk adults with resting or stress ECG, stress echocardiography, or stress MPI improves outcomes, but it is associated with increased costs and potential harms,” wrote the guideline’s author, Dr. Roger Chou, associate professor of medicine at Oregon Health & Science University, Portland.
The recommendation is based on a systematic literature review, recommendations from the U.S. Preventive Services Task Force, and American College of Cardiology guidelines. The new ACP clinical guideline was published March 17 in Annals of Internal Medicine (doi: 10.7326/M14-1225).
“What we are saying here is that, as physicians, we have responsibility to understand what the pretest probability is, and what the likelihood is that someone actually has disease – and if it’s low enough, then doing the screening test is going to cause a lot more false positives than true positives,” Dr. Robert Centor, regional dean of the Huntsville Medical Campus of the University of Alabama at Birmingham, explained in an interview.
“Even if it is a true positive, there is no evidence that we can find that finding that heart disease will do anything other than lead someone to do a procedure that we have no evidence will improve their outcomes,” added Dr. Centor, chair of the ACP Board of Regents.
Despite existing recommendations to the contrary, physicians are increasingly performing these tests on low-risk patients, the ACP cautioned.
For example, a Consumer Reports survey found that “39% of asymptomatic adults without high blood pressure or a high cholesterol level reported having ECG within the past 5 years, and 12% reported undergoing exercise ECG,” Dr. Chou wrote in his report on behalf of the ACP High Value Care Task Force. More than half of those patients said their physicians recommended the tests as part of their routine health care.
The rise in the use of such tests is likely the result of a combination of factors, Dr. Centor said. Those factors include money (patients see no out-of-pocket cost and thus don’t consider the cost of tests in their decision making), direct-to-consumer advertising, fear on behalf of physicians that they might miss a diagnosis, and a lack of understanding by patients on the adverse effects of screening if they are at low risk for heart disease.
Dr. Chou identified a number of potential harms related to unnecessary screenings, including sudden death or hospitalization during stress tests; adverse events from pharmacologics used to induce stress; radiation exposure from myocardial perfusion imaging; false positive results that, in turn, lead to anxiety by the patient and additional unnecessary tests and treatments; disease labeling; and downstream harms from follow-up testing and interventions.
“To be most effective, efforts to reduce the use of imaging should be multifocal and should address clinician behavior, patient expectations, direct-to-consumer screening programs, and financial incentives,” Dr. Chou explained.
In low-risk patients, physicians instead should “focus on treating modifiable risk factors (such as smoking, diabetes, hypertension, hyperlipidemia, and overweight) and encouraging healthy levels of exercise,” according to the guideline.
Clinicians should not screen for cardiac disease in asymptomatic, low-risk adults using resting or stress electrocardiography, stress echocardiography, or stress myocardial perfusion imaging , according to new guidelines from the American College of Physicians.
“There is no evidence that cardiac screening of low-risk adults with resting or stress ECG, stress echocardiography, or stress MPI improves outcomes, but it is associated with increased costs and potential harms,” wrote the guideline’s author, Dr. Roger Chou, associate professor of medicine at Oregon Health & Science University, Portland.
The recommendation is based on a systematic literature review, recommendations from the U.S. Preventive Services Task Force, and American College of Cardiology guidelines. The new ACP clinical guideline was published March 17 in Annals of Internal Medicine (doi: 10.7326/M14-1225).
“What we are saying here is that, as physicians, we have responsibility to understand what the pretest probability is, and what the likelihood is that someone actually has disease – and if it’s low enough, then doing the screening test is going to cause a lot more false positives than true positives,” Dr. Robert Centor, regional dean of the Huntsville Medical Campus of the University of Alabama at Birmingham, explained in an interview.
“Even if it is a true positive, there is no evidence that we can find that finding that heart disease will do anything other than lead someone to do a procedure that we have no evidence will improve their outcomes,” added Dr. Centor, chair of the ACP Board of Regents.
Despite existing recommendations to the contrary, physicians are increasingly performing these tests on low-risk patients, the ACP cautioned.
For example, a Consumer Reports survey found that “39% of asymptomatic adults without high blood pressure or a high cholesterol level reported having ECG within the past 5 years, and 12% reported undergoing exercise ECG,” Dr. Chou wrote in his report on behalf of the ACP High Value Care Task Force. More than half of those patients said their physicians recommended the tests as part of their routine health care.
The rise in the use of such tests is likely the result of a combination of factors, Dr. Centor said. Those factors include money (patients see no out-of-pocket cost and thus don’t consider the cost of tests in their decision making), direct-to-consumer advertising, fear on behalf of physicians that they might miss a diagnosis, and a lack of understanding by patients on the adverse effects of screening if they are at low risk for heart disease.
Dr. Chou identified a number of potential harms related to unnecessary screenings, including sudden death or hospitalization during stress tests; adverse events from pharmacologics used to induce stress; radiation exposure from myocardial perfusion imaging; false positive results that, in turn, lead to anxiety by the patient and additional unnecessary tests and treatments; disease labeling; and downstream harms from follow-up testing and interventions.
“To be most effective, efforts to reduce the use of imaging should be multifocal and should address clinician behavior, patient expectations, direct-to-consumer screening programs, and financial incentives,” Dr. Chou explained.
In low-risk patients, physicians instead should “focus on treating modifiable risk factors (such as smoking, diabetes, hypertension, hyperlipidemia, and overweight) and encouraging healthy levels of exercise,” according to the guideline.
Clinicians should not screen for cardiac disease in asymptomatic, low-risk adults using resting or stress electrocardiography, stress echocardiography, or stress myocardial perfusion imaging , according to new guidelines from the American College of Physicians.
“There is no evidence that cardiac screening of low-risk adults with resting or stress ECG, stress echocardiography, or stress MPI improves outcomes, but it is associated with increased costs and potential harms,” wrote the guideline’s author, Dr. Roger Chou, associate professor of medicine at Oregon Health & Science University, Portland.
The recommendation is based on a systematic literature review, recommendations from the U.S. Preventive Services Task Force, and American College of Cardiology guidelines. The new ACP clinical guideline was published March 17 in Annals of Internal Medicine (doi: 10.7326/M14-1225).
“What we are saying here is that, as physicians, we have responsibility to understand what the pretest probability is, and what the likelihood is that someone actually has disease – and if it’s low enough, then doing the screening test is going to cause a lot more false positives than true positives,” Dr. Robert Centor, regional dean of the Huntsville Medical Campus of the University of Alabama at Birmingham, explained in an interview.
“Even if it is a true positive, there is no evidence that we can find that finding that heart disease will do anything other than lead someone to do a procedure that we have no evidence will improve their outcomes,” added Dr. Centor, chair of the ACP Board of Regents.
Despite existing recommendations to the contrary, physicians are increasingly performing these tests on low-risk patients, the ACP cautioned.
For example, a Consumer Reports survey found that “39% of asymptomatic adults without high blood pressure or a high cholesterol level reported having ECG within the past 5 years, and 12% reported undergoing exercise ECG,” Dr. Chou wrote in his report on behalf of the ACP High Value Care Task Force. More than half of those patients said their physicians recommended the tests as part of their routine health care.
The rise in the use of such tests is likely the result of a combination of factors, Dr. Centor said. Those factors include money (patients see no out-of-pocket cost and thus don’t consider the cost of tests in their decision making), direct-to-consumer advertising, fear on behalf of physicians that they might miss a diagnosis, and a lack of understanding by patients on the adverse effects of screening if they are at low risk for heart disease.
Dr. Chou identified a number of potential harms related to unnecessary screenings, including sudden death or hospitalization during stress tests; adverse events from pharmacologics used to induce stress; radiation exposure from myocardial perfusion imaging; false positive results that, in turn, lead to anxiety by the patient and additional unnecessary tests and treatments; disease labeling; and downstream harms from follow-up testing and interventions.
“To be most effective, efforts to reduce the use of imaging should be multifocal and should address clinician behavior, patient expectations, direct-to-consumer screening programs, and financial incentives,” Dr. Chou explained.
In low-risk patients, physicians instead should “focus on treating modifiable risk factors (such as smoking, diabetes, hypertension, hyperlipidemia, and overweight) and encouraging healthy levels of exercise,” according to the guideline.
FROM ANNALS OF INTERNAL MEDICINE
House Dems endorse ACA special enrollment period for pregnancy
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
Medicare at 50: Is the end near for SGR?
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )
The Sustainable Growth Rate formula. Few aspects of Medicare have been more problematic for physicians.
Designed to control Medicare costs, Congress has spent more since 2003 to delay SGR cuts than it would cost to fund current repeal legislation.
Passed as part of the Balanced Budget Act of 1997, the SGR was designed to make sure Medicare expenditures did not grow faster than the Gross Domestic Product based on four factors: estimated change in physician fees, estimated number of Medicare fee-for-service beneficiaries, estimated 10-year average change in GDP, and estimated changes in expenditures due to law or regulation.
It was not, however, designed to keep up with the Baby Boom. Because it does not adjust for the influx of boomers, it guarantees to produce pay cuts just as demand for physician services grows.
The next pay cut – 21% this time – is slated for April 1.
For doctors, the constant specter of lower payments simply makes it hard to do business.
“Each year, when there is supposedly a cut, it is a consideration for practices that they have to create some contingency thinking, ‘if this were actually to take place, how will I continue to maintain my practice?’ ” Dr. Robert Juhasz, president of the American Osteopathic Association, said in an interview. “If they have a high Medicare population that they take care of, and certainly if there was that kind of a cut, they could not sustain that and would have to make changes.”
Dr. Blase Polite, chair of the American Society of Clinical Oncology Government Relations Committee, agreed. “Ever since the flawed formula was put in place, it has created yearly uncertainty. In recent years, we have had it to the point where the SGR cuts went into effect and then we had to do things like hold bills for a month or 2 months to resubmit them when the SGR would get patched. It became an absolute nightmare from a small business operating standpoint.”
But the tyranny of the SGR may have outgrown itself. In January, the U.S. Department of Health & Human Services announced a major expansion of its efforts to base physicians’ Medicare pay on value instead of volume, calling for half of all Medicare payments to be out of the fee-for-service system by 2018.
“This is the first time in the history of the program that explicit goals for alternative payment models and value-based payment models have been set for Medicare,” HHS Secretary Sylvia Burwell said in an editorial Jan. 26 in the New England Journal of Medicine (doi:10.1056/NEJMp1500445).
The goal is “to move away from the old way of doing things, which amounted to, ‘the more you do, the more you get paid,’ by linking nearly all pay to quality and value in some way to see that we are spending smarter,” Ms. Burwell said in a blog post on the HHS website.
As part of that effort, the department aims to have 30% of Medicare payments tied to quality or value through alternative payment models by the end of 2016.
Further, real efforts to repeal the SGR took hold in the last Congress, with strong support to pass legislation among lawmakers of both parties in the House and in the Senate. H.R. 4015, SGR Repeal and Medicare Provider Payment Modernization Act of 2014, passed the House but was not taken up by the Senate.
“We were cautiously optimistic that this 17th year of trying to repeal the SGR might have been the successful one,” Dr. Patrick T. O’Gara, president of the American College of Cardiology, said in an interview. He said that the sticking point seemed to be that “there was no politically viable way to pay for it.”
Dr. David A. Fleming, president of the American College of Physicians, noted in a statement that finding the money had hung up what otherwise was huge progress: a bill that members of the House and Senate, Republicans and Democrats had put together, and that ultimately passed the House.
Renewed efforts at repeal are underway in the current Congress. The House Energy and Commerce Committee’s Health Subcommittee held 2 days of hearings in January, hearing from doctors and health economists on how to cover the $140 billion cost of SGR repeal. Although experts presented their thoughts on where the health care sector could come up with the money, Rep. Fred Upton (R-Mich.), chairman of the full committee, recently suggested that the funding might come from outside the health care sector, such as from his proposal to legalize Internet poker.
But with time running short, some believe that another SGR patch is in the cards and that repeal will come attached to a broader piece of legislation at the end of the year.
“I don’t think there is any way it gets fixed by the March deadline because the payment offsets are just far too complicated. I think that it has to wait to be incorporated, my guess, in a larger bill,” ASCO’s Dr. Polite said. “That’s how I would do it. You want to include it in a much bigger package of tax reforms, perhaps other entitlement reforms where there’s a lot of pluses and minuses of money flow and the $140 billion for SGR is easy to take care of in that.”
He also cautioned that if it is not taken care of this year, it could be at least another 2 years before the window for repeal is opened.
“There is some talk about it getting delayed 18 months,” Dr. Polite said. “I hope that doesn’t happen because if you kick this can down the road 18 months, you basically put us in the 2016 election cycle and nobody’s coming up with $140 billion during that time. Eighteen months basically means we will see you after the 2016 presidential election. And it would be a shame.”
SGR: A patchwork of fixes
Congress has passed 17 different bills to prevent across-the-board Medicare pay cuts due to the SGR, ranging from 3.3% (2005) to 27.4% (2012). Nearly all have been paid for by some kind of offset. Here’s the sordid history:
• 2003 Consolidated Appropriations Act (4.9%)
• 2004 Medicare Prescription Drug, Improvements, and Modernization Act (4.5%)
• 2005 Medicare Prescription Drug, Improvements, and Modernization Act (3.3%)
• 2006 Deficit Reduction Act of 2005 (4.4%)
• 2007 Tax Relief and Health Care Act (5%)
• 2008 Medicare, Medicaid and SCHIP Extension Act (about 10.%)
• 2009 Medicare Improvements for Patients and Providers Act (16%)
• 2010 DOD Appropriations Act plus two Temporary Extension Acts (21%)
• 2010 Preservation of Access to Care for Medicare Beneficiaries Act (21.2%)
• 2010 Physician Payment and Therapy Relief Act (23% )
• 2011 Medicare and Medicaid Extenders Act (25%)
• 2012 Temporary Payroll Tax Cut Continuation Act (27.4%)
• 2012 Middle Class Tax Relief and Job Creation Act (27.4%)
• 2013 American Tax Payer Relief Act (26.5%)
• 2014 Pathway for SGR Reform Act (20.1%)
• 2014 Protecting Access To Medicare Act (24% )