User login
ACP warns of concierge practices neglecting the underserved population
The growth of concierge medical practices could “potentially exacerbate racial, ethnic, and socioeconomic disparities in health care,” the American College of Physicians warns in a new policy position paper.
Direct patient-contracting practices (DPCPs) also could impose “too high a cost burden on some lower-income patients,” ACP stated in the paper, published Nov. 9 in Annals of Internal Medicine.
The college said it supports physician and patient choice of practices that are “accessible, viable, and ethical,” but asserts that physicians who choose concierge practices “must ensure they are meeting their obligations to serve patients of all types, especially the poor and other vulnerable patients.”
In particular, “physicians in all types of practices should strive to take care of patients enrolled in Medicaid,” according to the policy.
ACP also is calling for more research on DPCPs, including determining the number of physicians in such practices; the factors that are leading physicians to work in DPCPs; the effects of these practices on the physician workforce; the effects on out-of-pocket costs, quality of care, and outcomes; and the effect of physicians not participating in national quality measures and programs such as interoperable electronic health records, and the associated effect on quality and outcomes (Ann Intern Med. 2015 Nov 9. doi:10.7326/M15-0366).
Tom Blue, chief strategy officer of the American Academy of Private Physicians, a group that represents physicians in direct patient-contracting practices, suggested that concierge medicine is not out of reach, even for lower-income populations.
“Most people think of them as luxury medicine, but the average price nationwide is probably now at about no higher than $135 a month and the fastest growing segment of private physician population is under $100 a month,” Mr. Blue said in an interview.
Private physicians “as a group, because of the way that their schedules work and the control that they have over them, I have found they are far more prone to reaching out to the underserved through free clinics or through what they call ‘scholarship programs’ in their own practices” where monthly membership fees are adjusted for those in need, Mr. Blue said.
The growth of concierge medical practices could “potentially exacerbate racial, ethnic, and socioeconomic disparities in health care,” the American College of Physicians warns in a new policy position paper.
Direct patient-contracting practices (DPCPs) also could impose “too high a cost burden on some lower-income patients,” ACP stated in the paper, published Nov. 9 in Annals of Internal Medicine.
The college said it supports physician and patient choice of practices that are “accessible, viable, and ethical,” but asserts that physicians who choose concierge practices “must ensure they are meeting their obligations to serve patients of all types, especially the poor and other vulnerable patients.”
In particular, “physicians in all types of practices should strive to take care of patients enrolled in Medicaid,” according to the policy.
ACP also is calling for more research on DPCPs, including determining the number of physicians in such practices; the factors that are leading physicians to work in DPCPs; the effects of these practices on the physician workforce; the effects on out-of-pocket costs, quality of care, and outcomes; and the effect of physicians not participating in national quality measures and programs such as interoperable electronic health records, and the associated effect on quality and outcomes (Ann Intern Med. 2015 Nov 9. doi:10.7326/M15-0366).
Tom Blue, chief strategy officer of the American Academy of Private Physicians, a group that represents physicians in direct patient-contracting practices, suggested that concierge medicine is not out of reach, even for lower-income populations.
“Most people think of them as luxury medicine, but the average price nationwide is probably now at about no higher than $135 a month and the fastest growing segment of private physician population is under $100 a month,” Mr. Blue said in an interview.
Private physicians “as a group, because of the way that their schedules work and the control that they have over them, I have found they are far more prone to reaching out to the underserved through free clinics or through what they call ‘scholarship programs’ in their own practices” where monthly membership fees are adjusted for those in need, Mr. Blue said.
The growth of concierge medical practices could “potentially exacerbate racial, ethnic, and socioeconomic disparities in health care,” the American College of Physicians warns in a new policy position paper.
Direct patient-contracting practices (DPCPs) also could impose “too high a cost burden on some lower-income patients,” ACP stated in the paper, published Nov. 9 in Annals of Internal Medicine.
The college said it supports physician and patient choice of practices that are “accessible, viable, and ethical,” but asserts that physicians who choose concierge practices “must ensure they are meeting their obligations to serve patients of all types, especially the poor and other vulnerable patients.”
In particular, “physicians in all types of practices should strive to take care of patients enrolled in Medicaid,” according to the policy.
ACP also is calling for more research on DPCPs, including determining the number of physicians in such practices; the factors that are leading physicians to work in DPCPs; the effects of these practices on the physician workforce; the effects on out-of-pocket costs, quality of care, and outcomes; and the effect of physicians not participating in national quality measures and programs such as interoperable electronic health records, and the associated effect on quality and outcomes (Ann Intern Med. 2015 Nov 9. doi:10.7326/M15-0366).
Tom Blue, chief strategy officer of the American Academy of Private Physicians, a group that represents physicians in direct patient-contracting practices, suggested that concierge medicine is not out of reach, even for lower-income populations.
“Most people think of them as luxury medicine, but the average price nationwide is probably now at about no higher than $135 a month and the fastest growing segment of private physician population is under $100 a month,” Mr. Blue said in an interview.
Private physicians “as a group, because of the way that their schedules work and the control that they have over them, I have found they are far more prone to reaching out to the underserved through free clinics or through what they call ‘scholarship programs’ in their own practices” where monthly membership fees are adjusted for those in need, Mr. Blue said.
FROM ANNALS OF INTERNAL MEDICINE
ACC rates hospitals’ performance on med prescribing at discharge
The American College of Cardiology is releasing hospital performance data to help patients and caregivers make informed choices about where to go for cardiac procedures.
The first element of the database, found online at FindYourHeartaHome.org, examines a hospital’s performance in prescribing appropriate medication at discharge. Participation in the performance data program is voluntary.
In its Nov. 3, announcement, the ACC noted that there are guidelines in place for appropriate medication for patients who receive an implantable cardioverter defibrillator or undergo percutaneous coronary intervention to help protect against further complications. While the guidelines are followed most of the time, there can be variations in treatment. Hospitals are rated on a four-star scale based on their performance in providing evidence-based care.
“Our hope is that by tracking and publicly reporting these measures, we can raise awareness of variation where it exists and help to ensure consistent, evidence-based care is provided across the United States,” ACC President Kim Allan Williams Sr., M.D., said in a statement. Hospitals volunteering data for public dissemination “are showing a true commitment to quality improvement and helping to ensure heart disease patients nationwide receive the best possible care.”
Participating hospitals release discharge medication data from the National Cardiovascular Data Registry’s ICD Registry and CathPCI Registry. All data are anonymous.
The American College of Cardiology is releasing hospital performance data to help patients and caregivers make informed choices about where to go for cardiac procedures.
The first element of the database, found online at FindYourHeartaHome.org, examines a hospital’s performance in prescribing appropriate medication at discharge. Participation in the performance data program is voluntary.
In its Nov. 3, announcement, the ACC noted that there are guidelines in place for appropriate medication for patients who receive an implantable cardioverter defibrillator or undergo percutaneous coronary intervention to help protect against further complications. While the guidelines are followed most of the time, there can be variations in treatment. Hospitals are rated on a four-star scale based on their performance in providing evidence-based care.
“Our hope is that by tracking and publicly reporting these measures, we can raise awareness of variation where it exists and help to ensure consistent, evidence-based care is provided across the United States,” ACC President Kim Allan Williams Sr., M.D., said in a statement. Hospitals volunteering data for public dissemination “are showing a true commitment to quality improvement and helping to ensure heart disease patients nationwide receive the best possible care.”
Participating hospitals release discharge medication data from the National Cardiovascular Data Registry’s ICD Registry and CathPCI Registry. All data are anonymous.
The American College of Cardiology is releasing hospital performance data to help patients and caregivers make informed choices about where to go for cardiac procedures.
The first element of the database, found online at FindYourHeartaHome.org, examines a hospital’s performance in prescribing appropriate medication at discharge. Participation in the performance data program is voluntary.
In its Nov. 3, announcement, the ACC noted that there are guidelines in place for appropriate medication for patients who receive an implantable cardioverter defibrillator or undergo percutaneous coronary intervention to help protect against further complications. While the guidelines are followed most of the time, there can be variations in treatment. Hospitals are rated on a four-star scale based on their performance in providing evidence-based care.
“Our hope is that by tracking and publicly reporting these measures, we can raise awareness of variation where it exists and help to ensure consistent, evidence-based care is provided across the United States,” ACC President Kim Allan Williams Sr., M.D., said in a statement. Hospitals volunteering data for public dissemination “are showing a true commitment to quality improvement and helping to ensure heart disease patients nationwide receive the best possible care.”
Participating hospitals release discharge medication data from the National Cardiovascular Data Registry’s ICD Registry and CathPCI Registry. All data are anonymous.
Cautious optimism greets Medicare’s revised two-midnight hospital rule
The Centers for Medicare and Medicaid Services finalized a proposal to add more flexibility in reimbursing hospital stays under Medicare Part A if they do not cross the two-midnight threshold, a move that was met with cautious optimism.
“Hospitals appreciate the certainty that stays of at least two midnights are inpatient, with stays of less than two midnights also considered inpatient based on physician judgment,” American Hospital Association Executive Vice President Tom Nickels said in a statement.
For hospital stays for which physicians expect the patient will need fewer than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule.
In addition, the agency does not plan to send recovery audit contractors (RACs) after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“We look forward to working with the [Quality Improvement Organizations] – which are not paid on a contingency fee basis like those bounty-hunter RACs – and to more fair auditing process,” Mr. Nickels added.
How the QIOs review claims is the part that will be closely monitored by stakeholders.
“CMS finalized the changes that were proposed, which are consistent with what the AAMC has been asking the agency to do,” the Association of American Medical Colleges said in a statement. “AAMC believes it is important that CMS monitor the QIO audits to ensure that they are working as anticipated, and that the QIOs audits do not produce the myriad of problems that the RAC audits produced.”
Even with the cautious optimism, there remains a sense that the new rule does not go far enough.
“Despite ongoing concerns with observation policy overall, we appreciate CMS’ efforts to modify the two-midnight rule to address widespread concerns and issues identified by the provider community, and SHM stands ready to help make it work,” the Society of Hospital Medicine said in a statement.
The organization called for further changes in response to CMS’ initial proposal for the increased flexibility. Those suggested changes included a revised definition of inpatient care to include all time spent in the hospital, better guidance on how audits will be conducted, more concrete guidance on short inpatient stays to minimize claims denials, and better alignment between hours spent in the hospital and the midnights crossed as part of a stay.
“SHM does not believe the two-midnight rule is the optimal policy for addressing the structural issues associated with observation status payment policy,” the organization noted. “However, we recognize this policy and the changes contained in the final rule were enacted with the goal of simplifying the inpatient admission decision, reducing the number of long hospital stays under observation status, and to strengthen deference to physician judgment.”
The Centers for Medicare and Medicaid Services finalized a proposal to add more flexibility in reimbursing hospital stays under Medicare Part A if they do not cross the two-midnight threshold, a move that was met with cautious optimism.
“Hospitals appreciate the certainty that stays of at least two midnights are inpatient, with stays of less than two midnights also considered inpatient based on physician judgment,” American Hospital Association Executive Vice President Tom Nickels said in a statement.
For hospital stays for which physicians expect the patient will need fewer than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule.
In addition, the agency does not plan to send recovery audit contractors (RACs) after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“We look forward to working with the [Quality Improvement Organizations] – which are not paid on a contingency fee basis like those bounty-hunter RACs – and to more fair auditing process,” Mr. Nickels added.
How the QIOs review claims is the part that will be closely monitored by stakeholders.
“CMS finalized the changes that were proposed, which are consistent with what the AAMC has been asking the agency to do,” the Association of American Medical Colleges said in a statement. “AAMC believes it is important that CMS monitor the QIO audits to ensure that they are working as anticipated, and that the QIOs audits do not produce the myriad of problems that the RAC audits produced.”
Even with the cautious optimism, there remains a sense that the new rule does not go far enough.
“Despite ongoing concerns with observation policy overall, we appreciate CMS’ efforts to modify the two-midnight rule to address widespread concerns and issues identified by the provider community, and SHM stands ready to help make it work,” the Society of Hospital Medicine said in a statement.
The organization called for further changes in response to CMS’ initial proposal for the increased flexibility. Those suggested changes included a revised definition of inpatient care to include all time spent in the hospital, better guidance on how audits will be conducted, more concrete guidance on short inpatient stays to minimize claims denials, and better alignment between hours spent in the hospital and the midnights crossed as part of a stay.
“SHM does not believe the two-midnight rule is the optimal policy for addressing the structural issues associated with observation status payment policy,” the organization noted. “However, we recognize this policy and the changes contained in the final rule were enacted with the goal of simplifying the inpatient admission decision, reducing the number of long hospital stays under observation status, and to strengthen deference to physician judgment.”
The Centers for Medicare and Medicaid Services finalized a proposal to add more flexibility in reimbursing hospital stays under Medicare Part A if they do not cross the two-midnight threshold, a move that was met with cautious optimism.
“Hospitals appreciate the certainty that stays of at least two midnights are inpatient, with stays of less than two midnights also considered inpatient based on physician judgment,” American Hospital Association Executive Vice President Tom Nickels said in a statement.
For hospital stays for which physicians expect the patient will need fewer than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule.
In addition, the agency does not plan to send recovery audit contractors (RACs) after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“We look forward to working with the [Quality Improvement Organizations] – which are not paid on a contingency fee basis like those bounty-hunter RACs – and to more fair auditing process,” Mr. Nickels added.
How the QIOs review claims is the part that will be closely monitored by stakeholders.
“CMS finalized the changes that were proposed, which are consistent with what the AAMC has been asking the agency to do,” the Association of American Medical Colleges said in a statement. “AAMC believes it is important that CMS monitor the QIO audits to ensure that they are working as anticipated, and that the QIOs audits do not produce the myriad of problems that the RAC audits produced.”
Even with the cautious optimism, there remains a sense that the new rule does not go far enough.
“Despite ongoing concerns with observation policy overall, we appreciate CMS’ efforts to modify the two-midnight rule to address widespread concerns and issues identified by the provider community, and SHM stands ready to help make it work,” the Society of Hospital Medicine said in a statement.
The organization called for further changes in response to CMS’ initial proposal for the increased flexibility. Those suggested changes included a revised definition of inpatient care to include all time spent in the hospital, better guidance on how audits will be conducted, more concrete guidance on short inpatient stays to minimize claims denials, and better alignment between hours spent in the hospital and the midnights crossed as part of a stay.
“SHM does not believe the two-midnight rule is the optimal policy for addressing the structural issues associated with observation status payment policy,” the organization noted. “However, we recognize this policy and the changes contained in the final rule were enacted with the goal of simplifying the inpatient admission decision, reducing the number of long hospital stays under observation status, and to strengthen deference to physician judgment.”
AMA expands med schools in education consortium
The American Medical Association has added 20 schools to its Accelerating Change in Medical Education Consortium in an effort to better prepare students for the rapid change in medical practice.
“With medicine and health care delivery in the United States changing in such new and exciting ways, we’ve asked for and are starting to receive a medical education system that keeps pace with this rate of change,” Dr. James Madara, AMA chief operating officer, said during a Nov. 4 press teleconference. “This means trying new content, giving students information they need to know but in the past haven’t been taught, [and] trying new methods,” such as better understanding whether certain content is better shared through lecture or via simulation or electronic channels.
The program launched in 2013 with 11 schools. The new schools added were culled from proposals submitted by 108 of 170 eligible academic institutions.
“We sought proposals that would significantly redesign medical education and these experts reviewed entries with that goal in mind,” said Dr. Susan Skochelak, AMA group vice president for medical education. “The advisory panel evaluated each school’s proposal based on how the project would align with or enhance the 11 founding schools’ work and the projects’ uniqueness and feasibility for implementation at other medical schools.”
Winning programs cover concepts such as care coordination in accountable care organizations, advanced simulation and telemedicine technologies, and addressing the needs of underserved and diverse communities.
The new schools entering the consortium include A. T. Still University School of Osteopathic Medicine, Mesa, Ariz.; Case Western Reserve University, Cleveland; Eastern Virgina Medical School, Norfolk; Emory University, Atlanta; Florida International University, Miami; Harvard Medical School, Boston; Morehouse School of Medicine, Atlanta; Ohio University Heritage College of Osteopathic Medicine, Cleveland campus; Robert Wood Johnson Medical School, New Brunswick, N.J.; City College of New York Sophie Davis School of Biomedical Education, New York; Thomas Jefferson University Sidney Kimmel Medical College, Philadelphia; University of Chicago; University of Connecticut, Farmington; University of Nebraska, Omaha; University of North Carolina at Chapel Hill; University of North Dakota, Grand Forks; University of Texas, Austin; University of Texas Rio Grande Valley School of Medicine, South Texas; University of Utah, Salt Lake City; and University of Washington, Seattle.
“By tripling the number of schools participating in this effort, we know that we will be able to more quickly disseminate the consortium schools’ innovative curriculum models to create the seismic shift that our medical education system needs so that our future physicians can better care for their patients,” Dr. Madara said.
The American Medical Association has added 20 schools to its Accelerating Change in Medical Education Consortium in an effort to better prepare students for the rapid change in medical practice.
“With medicine and health care delivery in the United States changing in such new and exciting ways, we’ve asked for and are starting to receive a medical education system that keeps pace with this rate of change,” Dr. James Madara, AMA chief operating officer, said during a Nov. 4 press teleconference. “This means trying new content, giving students information they need to know but in the past haven’t been taught, [and] trying new methods,” such as better understanding whether certain content is better shared through lecture or via simulation or electronic channels.
The program launched in 2013 with 11 schools. The new schools added were culled from proposals submitted by 108 of 170 eligible academic institutions.
“We sought proposals that would significantly redesign medical education and these experts reviewed entries with that goal in mind,” said Dr. Susan Skochelak, AMA group vice president for medical education. “The advisory panel evaluated each school’s proposal based on how the project would align with or enhance the 11 founding schools’ work and the projects’ uniqueness and feasibility for implementation at other medical schools.”
Winning programs cover concepts such as care coordination in accountable care organizations, advanced simulation and telemedicine technologies, and addressing the needs of underserved and diverse communities.
The new schools entering the consortium include A. T. Still University School of Osteopathic Medicine, Mesa, Ariz.; Case Western Reserve University, Cleveland; Eastern Virgina Medical School, Norfolk; Emory University, Atlanta; Florida International University, Miami; Harvard Medical School, Boston; Morehouse School of Medicine, Atlanta; Ohio University Heritage College of Osteopathic Medicine, Cleveland campus; Robert Wood Johnson Medical School, New Brunswick, N.J.; City College of New York Sophie Davis School of Biomedical Education, New York; Thomas Jefferson University Sidney Kimmel Medical College, Philadelphia; University of Chicago; University of Connecticut, Farmington; University of Nebraska, Omaha; University of North Carolina at Chapel Hill; University of North Dakota, Grand Forks; University of Texas, Austin; University of Texas Rio Grande Valley School of Medicine, South Texas; University of Utah, Salt Lake City; and University of Washington, Seattle.
“By tripling the number of schools participating in this effort, we know that we will be able to more quickly disseminate the consortium schools’ innovative curriculum models to create the seismic shift that our medical education system needs so that our future physicians can better care for their patients,” Dr. Madara said.
The American Medical Association has added 20 schools to its Accelerating Change in Medical Education Consortium in an effort to better prepare students for the rapid change in medical practice.
“With medicine and health care delivery in the United States changing in such new and exciting ways, we’ve asked for and are starting to receive a medical education system that keeps pace with this rate of change,” Dr. James Madara, AMA chief operating officer, said during a Nov. 4 press teleconference. “This means trying new content, giving students information they need to know but in the past haven’t been taught, [and] trying new methods,” such as better understanding whether certain content is better shared through lecture or via simulation or electronic channels.
The program launched in 2013 with 11 schools. The new schools added were culled from proposals submitted by 108 of 170 eligible academic institutions.
“We sought proposals that would significantly redesign medical education and these experts reviewed entries with that goal in mind,” said Dr. Susan Skochelak, AMA group vice president for medical education. “The advisory panel evaluated each school’s proposal based on how the project would align with or enhance the 11 founding schools’ work and the projects’ uniqueness and feasibility for implementation at other medical schools.”
Winning programs cover concepts such as care coordination in accountable care organizations, advanced simulation and telemedicine technologies, and addressing the needs of underserved and diverse communities.
The new schools entering the consortium include A. T. Still University School of Osteopathic Medicine, Mesa, Ariz.; Case Western Reserve University, Cleveland; Eastern Virgina Medical School, Norfolk; Emory University, Atlanta; Florida International University, Miami; Harvard Medical School, Boston; Morehouse School of Medicine, Atlanta; Ohio University Heritage College of Osteopathic Medicine, Cleveland campus; Robert Wood Johnson Medical School, New Brunswick, N.J.; City College of New York Sophie Davis School of Biomedical Education, New York; Thomas Jefferson University Sidney Kimmel Medical College, Philadelphia; University of Chicago; University of Connecticut, Farmington; University of Nebraska, Omaha; University of North Carolina at Chapel Hill; University of North Dakota, Grand Forks; University of Texas, Austin; University of Texas Rio Grande Valley School of Medicine, South Texas; University of Utah, Salt Lake City; and University of Washington, Seattle.
“By tripling the number of schools participating in this effort, we know that we will be able to more quickly disseminate the consortium schools’ innovative curriculum models to create the seismic shift that our medical education system needs so that our future physicians can better care for their patients,” Dr. Madara said.
Robotic surgery progress: Is resistance futile?
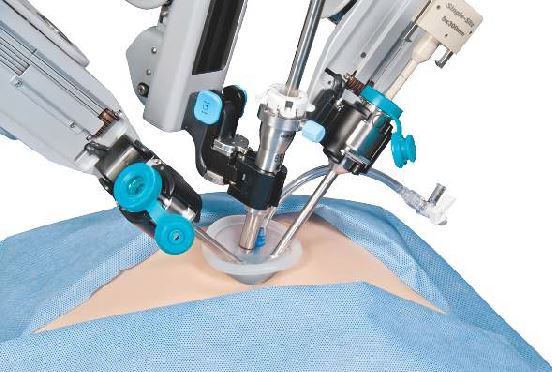
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
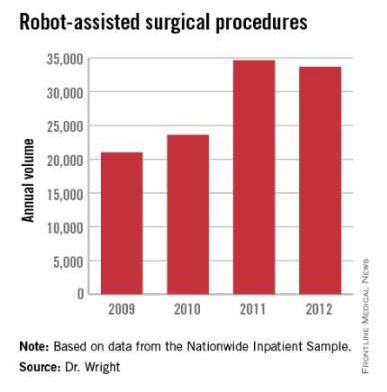
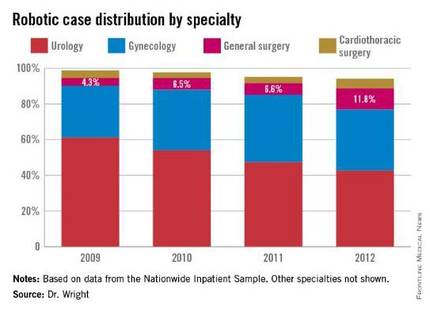
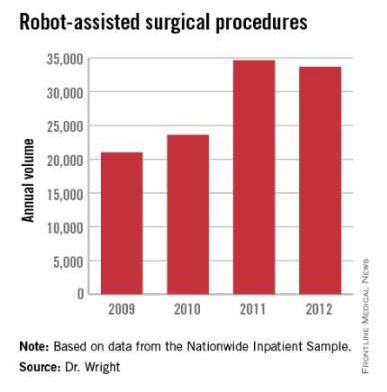
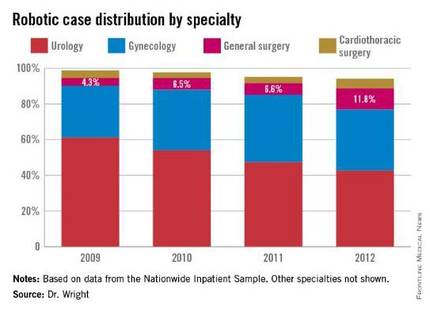
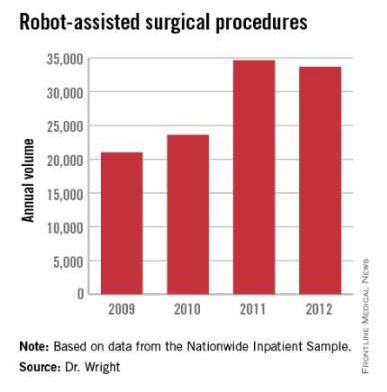
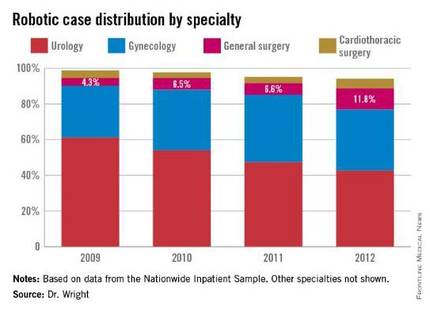
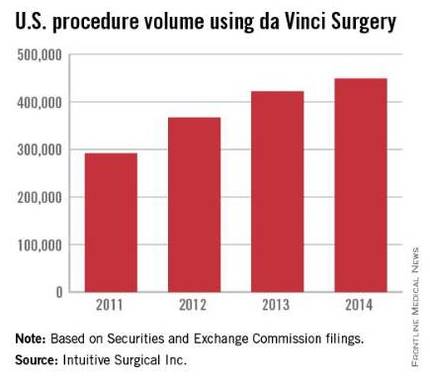
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]
Robotic surgery: Resistance is futile
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
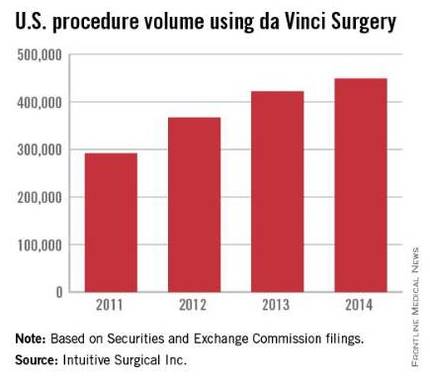
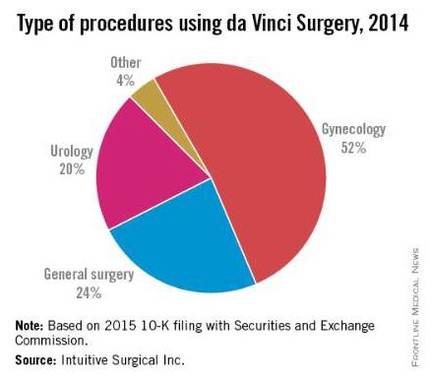
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
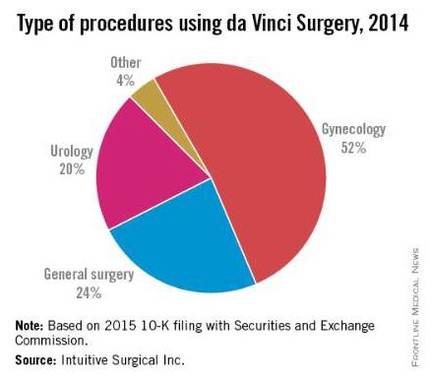
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
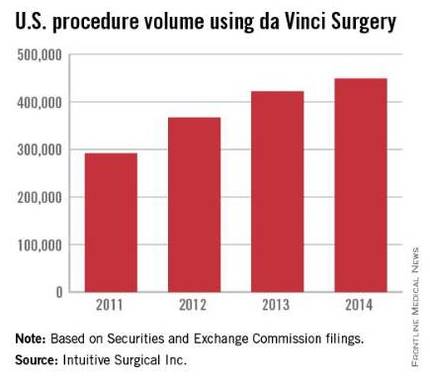
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
House curbs Medicare premium increase under budget deal
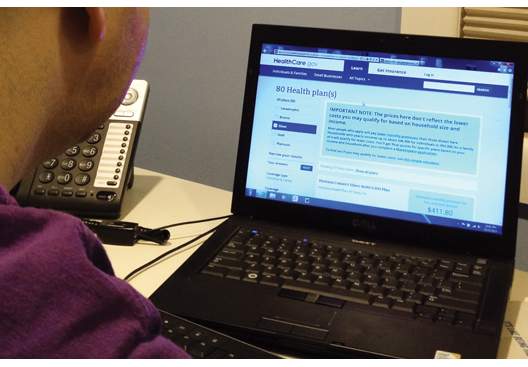
Lawmakers are seeking to limit an increase in Medicare Part B premiums as part of the budget deal negotiated between outgoing House Speaker John Boehner (R-Ohio) and the White House, and approved by the House on Oct. 28.
The House approved the Bipartisan Budget Act by a vote of 266-167. The Senate is expected to act on the deal shortly.
The deal means that some Medicare beneficiaries will avoid seeing their Part B premiums jump from about $105 to $160 per month. Instead, those beneficiaries who are not “held harmless” under Medicare rules – about 30% of Medicare beneficiaries – would see their premiums rise to $120 in 2016. The bulk of Medicare beneficiaries will have stable premiums at about $105 next year.
To pay for the rollback of part of the increase, the budget agreement also calls for those beneficiaries not held harmless under the law to pay an extra $3 per month starting in 2016.
But an analysis of this provision by the National Center for Policy Analysis noted that such adjustments could happen again, as they are tied to the a cost of living adjustment. This is “just another case of Congress kicking the can down the road,” NCPA officials wrote in an Oct. 28 blog post.
The budget deal included only a few other health care–related provisions. The bill would broaden the application of inflation-triggered rebates – the rebates paid by manufacturers when drug price increases outpace inflation – to generic drugs as well as brand name drugs.
Another provision codifies the definition of provider-based off-campus hospital outpatient departments that are not on the main campus and are more than 250 yards away from the main hospital campus. Providers at these off-campus locations would be reimbursed under the ambulatory surgical center prospective payment system or the Medicare physician fee schedule rather than the hospital outpatient prospective payment system.
Finally, the budget bill eliminates a requirement from the Affordable Care Act that mandates that employers with more than 200 workers automatically enroll new full-time employees into a qualifying health plan if it is offered, and automatically reenroll existing employees.
Lawmakers are seeking to limit an increase in Medicare Part B premiums as part of the budget deal negotiated between outgoing House Speaker John Boehner (R-Ohio) and the White House, and approved by the House on Oct. 28.
The House approved the Bipartisan Budget Act by a vote of 266-167. The Senate is expected to act on the deal shortly.
The deal means that some Medicare beneficiaries will avoid seeing their Part B premiums jump from about $105 to $160 per month. Instead, those beneficiaries who are not “held harmless” under Medicare rules – about 30% of Medicare beneficiaries – would see their premiums rise to $120 in 2016. The bulk of Medicare beneficiaries will have stable premiums at about $105 next year.
To pay for the rollback of part of the increase, the budget agreement also calls for those beneficiaries not held harmless under the law to pay an extra $3 per month starting in 2016.
But an analysis of this provision by the National Center for Policy Analysis noted that such adjustments could happen again, as they are tied to the a cost of living adjustment. This is “just another case of Congress kicking the can down the road,” NCPA officials wrote in an Oct. 28 blog post.
The budget deal included only a few other health care–related provisions. The bill would broaden the application of inflation-triggered rebates – the rebates paid by manufacturers when drug price increases outpace inflation – to generic drugs as well as brand name drugs.
Another provision codifies the definition of provider-based off-campus hospital outpatient departments that are not on the main campus and are more than 250 yards away from the main hospital campus. Providers at these off-campus locations would be reimbursed under the ambulatory surgical center prospective payment system or the Medicare physician fee schedule rather than the hospital outpatient prospective payment system.
Finally, the budget bill eliminates a requirement from the Affordable Care Act that mandates that employers with more than 200 workers automatically enroll new full-time employees into a qualifying health plan if it is offered, and automatically reenroll existing employees.
Lawmakers are seeking to limit an increase in Medicare Part B premiums as part of the budget deal negotiated between outgoing House Speaker John Boehner (R-Ohio) and the White House, and approved by the House on Oct. 28.
The House approved the Bipartisan Budget Act by a vote of 266-167. The Senate is expected to act on the deal shortly.
The deal means that some Medicare beneficiaries will avoid seeing their Part B premiums jump from about $105 to $160 per month. Instead, those beneficiaries who are not “held harmless” under Medicare rules – about 30% of Medicare beneficiaries – would see their premiums rise to $120 in 2016. The bulk of Medicare beneficiaries will have stable premiums at about $105 next year.
To pay for the rollback of part of the increase, the budget agreement also calls for those beneficiaries not held harmless under the law to pay an extra $3 per month starting in 2016.
But an analysis of this provision by the National Center for Policy Analysis noted that such adjustments could happen again, as they are tied to the a cost of living adjustment. This is “just another case of Congress kicking the can down the road,” NCPA officials wrote in an Oct. 28 blog post.
The budget deal included only a few other health care–related provisions. The bill would broaden the application of inflation-triggered rebates – the rebates paid by manufacturers when drug price increases outpace inflation – to generic drugs as well as brand name drugs.
Another provision codifies the definition of provider-based off-campus hospital outpatient departments that are not on the main campus and are more than 250 yards away from the main hospital campus. Providers at these off-campus locations would be reimbursed under the ambulatory surgical center prospective payment system or the Medicare physician fee schedule rather than the hospital outpatient prospective payment system.
Finally, the budget bill eliminates a requirement from the Affordable Care Act that mandates that employers with more than 200 workers automatically enroll new full-time employees into a qualifying health plan if it is offered, and automatically reenroll existing employees.
Healthcare.gov: Premiums to jump in 8 states
Patients in eight states could be in for a big surprise when they reenroll for health insurance coverage through the federal marketplace.
The Health & Human Services department announced Oct. 26 that residents in Oklahoma, Montana, Alaska, New Mexico, South Dakota, North Carolina, Oregon, and Tennessee will see at least a 20% rise in premiums for benchmark plans. Leading the way is Oklahoma with a 35.7% increase, followed by Montana (34.5%) and Alaska (31.5%).
Open enrollment for 2016 begins on Nov. 1.
Four states will see a decline in benchmark premium rates, the largest occurring in Indiana (–12.6%), followed by Mississippi (–8.2%), Maine (–1.2%), and Ohio (–0.7%).
Across the 37 states in the federal marketplace, premiums for benchmark plan will increase on average 7.5%. In 2015, there were 8.8 million people enrolled in benchmark plans.
HHS also reported that next year, nearly 8 in 10 returning patients will be able to buy a plan with premiums less than $100 after tax credits, while 7 in 10 will be able to spend $75 or less after tax credits.
Patients in more than two-thirds of counties covered by the federal marketplace will be able to choose from three or more plans. HHS also noted that in the second open enrollment period (2015), those who switched plans within the same tier saved an average of nearly $400 on their annualized premiums after tax credits, compared with those who did not switch.
Patients in eight states could be in for a big surprise when they reenroll for health insurance coverage through the federal marketplace.
The Health & Human Services department announced Oct. 26 that residents in Oklahoma, Montana, Alaska, New Mexico, South Dakota, North Carolina, Oregon, and Tennessee will see at least a 20% rise in premiums for benchmark plans. Leading the way is Oklahoma with a 35.7% increase, followed by Montana (34.5%) and Alaska (31.5%).
Open enrollment for 2016 begins on Nov. 1.
Four states will see a decline in benchmark premium rates, the largest occurring in Indiana (–12.6%), followed by Mississippi (–8.2%), Maine (–1.2%), and Ohio (–0.7%).
Across the 37 states in the federal marketplace, premiums for benchmark plan will increase on average 7.5%. In 2015, there were 8.8 million people enrolled in benchmark plans.
HHS also reported that next year, nearly 8 in 10 returning patients will be able to buy a plan with premiums less than $100 after tax credits, while 7 in 10 will be able to spend $75 or less after tax credits.
Patients in more than two-thirds of counties covered by the federal marketplace will be able to choose from three or more plans. HHS also noted that in the second open enrollment period (2015), those who switched plans within the same tier saved an average of nearly $400 on their annualized premiums after tax credits, compared with those who did not switch.
Patients in eight states could be in for a big surprise when they reenroll for health insurance coverage through the federal marketplace.
The Health & Human Services department announced Oct. 26 that residents in Oklahoma, Montana, Alaska, New Mexico, South Dakota, North Carolina, Oregon, and Tennessee will see at least a 20% rise in premiums for benchmark plans. Leading the way is Oklahoma with a 35.7% increase, followed by Montana (34.5%) and Alaska (31.5%).
Open enrollment for 2016 begins on Nov. 1.
Four states will see a decline in benchmark premium rates, the largest occurring in Indiana (–12.6%), followed by Mississippi (–8.2%), Maine (–1.2%), and Ohio (–0.7%).
Across the 37 states in the federal marketplace, premiums for benchmark plan will increase on average 7.5%. In 2015, there were 8.8 million people enrolled in benchmark plans.
HHS also reported that next year, nearly 8 in 10 returning patients will be able to buy a plan with premiums less than $100 after tax credits, while 7 in 10 will be able to spend $75 or less after tax credits.
Patients in more than two-thirds of counties covered by the federal marketplace will be able to choose from three or more plans. HHS also noted that in the second open enrollment period (2015), those who switched plans within the same tier saved an average of nearly $400 on their annualized premiums after tax credits, compared with those who did not switch.
HIVMA, 152 others call for Turing to reverse Daraprim price increase
The HIV Medicine Association and 152 other organizations are insisting that Turing Pharmaceuticals reverse recent price increases put in place for Daraprim.
“The unjustifiable actions taken to leverage the value of an effective 70-year old medication are jeopardizing the health of individuals with a serious, life-threatening condition,” the HIVMA and others said in an Oct. 22, 2015, letter to Turing. “These individuals do not have the luxury of time to wait for promised new treatments – which also will likely be priced out of reach.”
The letter noted several physician anecdotes of courses of therapy that need to be changed as a direct result of the price change.
In August, Turing increased the price of the drug, used to treat toxoplasmosis, by more than5,000% from $13.50 per pill to $750 per pill after it acquired the exclusive rights to Daraprim from Impax Laboratories. Turing also limited the drug’s distribution.
In a letter to the company, HIVMA and others are calling on Turing to lower the price; provide price parity for inpatient and outpatient settings; offer financial support for patients with income levels at 500% of the federal poverty level, as well as transparency for patient assistance and copay assistance programs; cover the maximum out-of-pocket costs on coinsurance and copayments allowable under the Affordable Care Act; and ensure same day and direct access to the drug.
Turing announced on Sept. 24, 2015, that in response to the backlash over the price increase, it would lower the price, but it has not yet done so. On Oct. 13, 2015, the company revealed details on how it is making the product affordable to patients.
The HIV Medicine Association and 152 other organizations are insisting that Turing Pharmaceuticals reverse recent price increases put in place for Daraprim.
“The unjustifiable actions taken to leverage the value of an effective 70-year old medication are jeopardizing the health of individuals with a serious, life-threatening condition,” the HIVMA and others said in an Oct. 22, 2015, letter to Turing. “These individuals do not have the luxury of time to wait for promised new treatments – which also will likely be priced out of reach.”
The letter noted several physician anecdotes of courses of therapy that need to be changed as a direct result of the price change.
In August, Turing increased the price of the drug, used to treat toxoplasmosis, by more than5,000% from $13.50 per pill to $750 per pill after it acquired the exclusive rights to Daraprim from Impax Laboratories. Turing also limited the drug’s distribution.
In a letter to the company, HIVMA and others are calling on Turing to lower the price; provide price parity for inpatient and outpatient settings; offer financial support for patients with income levels at 500% of the federal poverty level, as well as transparency for patient assistance and copay assistance programs; cover the maximum out-of-pocket costs on coinsurance and copayments allowable under the Affordable Care Act; and ensure same day and direct access to the drug.
Turing announced on Sept. 24, 2015, that in response to the backlash over the price increase, it would lower the price, but it has not yet done so. On Oct. 13, 2015, the company revealed details on how it is making the product affordable to patients.
The HIV Medicine Association and 152 other organizations are insisting that Turing Pharmaceuticals reverse recent price increases put in place for Daraprim.
“The unjustifiable actions taken to leverage the value of an effective 70-year old medication are jeopardizing the health of individuals with a serious, life-threatening condition,” the HIVMA and others said in an Oct. 22, 2015, letter to Turing. “These individuals do not have the luxury of time to wait for promised new treatments – which also will likely be priced out of reach.”
The letter noted several physician anecdotes of courses of therapy that need to be changed as a direct result of the price change.
In August, Turing increased the price of the drug, used to treat toxoplasmosis, by more than5,000% from $13.50 per pill to $750 per pill after it acquired the exclusive rights to Daraprim from Impax Laboratories. Turing also limited the drug’s distribution.
In a letter to the company, HIVMA and others are calling on Turing to lower the price; provide price parity for inpatient and outpatient settings; offer financial support for patients with income levels at 500% of the federal poverty level, as well as transparency for patient assistance and copay assistance programs; cover the maximum out-of-pocket costs on coinsurance and copayments allowable under the Affordable Care Act; and ensure same day and direct access to the drug.
Turing announced on Sept. 24, 2015, that in response to the backlash over the price increase, it would lower the price, but it has not yet done so. On Oct. 13, 2015, the company revealed details on how it is making the product affordable to patients.
AAP urges greater action in protecting children from tobacco and nicotine
The American Academy of Pediatrics is urging more action to protect children from the harms of tobacco and nicotine in clinical and public policy statements published online in Pediatrics.
In the clinical policy statement, AAP offers a series of recommendations for pediatricians and other health care providers to guide the identification of potential issues, as well as how they can be treated upon discovery (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3108]).
“There is no safe level of tobacco smoke exposure, and teenagers and children must be protected from its harmful effects,” Dr. Karen M. Wilson, section head of pediatric medicine at Children’s Hospital, Aurora, Colo., and chair of the AAP Section on Tobacco Control said in a Oct. 23 telebriefing prior to the release of the statements. “If current trends continue, 5.6 million of today’s youth will die prematurely from tobacco and smoking,” she said.
The AAP recommends an inquiry about tobacco use and tobacco smoke as part of health supervision visits, as well as visits for diseases that may be caused or exacerbated by tobacco smoke exposure. Parents should be asked who is smoking around a child and where, and children and adolescents should be asked about cigarettes and other kinds of tobacco and nicotine products (i.e., e-cigarettes) they have may have tried or are actively using.
The recommendations are backed by a technical report that provides the evidence base to support AAP’s clinical and policy statements, also published online in Pediatrics (2015 Oct. 26 [doi: 10.1542/peds.2015-3110]).
Furthermore, guidance of tobacco prevention should be given, including messages that experimenting with tobacco use is not safe.
“Messages should start as early as children are developmentally ready to understand them, usually approximately 5 years of age,” AAP said in the statement. Messages that may resonate more with adolescents include the effect of tobacco use on appearance, breath, and sports performance; lack of benefit for weight loss; how much money they would have to spend to continue their tobacco addiction; and how the tobacco industry deceives them, AAP said.
“Adolescents are particularly susceptible to nicotine,” Dr. Wilson noted. “Even low levels of exposure to nicotine and tobacco can worsen asthma or negatively impact IQ scores in young children,” she said.
Adolescents should be offered tobacco dependence treatment if they want to stop, although the use of pharmacotherapy is not as strong a recommendation.
“Research on pharmacotherapy of moderate to severe adolescent tobacco dependence is limited by short courses of treatment, high rates of nonadherence, and high rates of relapse after discontinuation of therapy,” the statement notes, adding that adolescents can be offered pharmacotherapy “appropriate to the severity of his or her tobacco dependence and his or her readiness to change as part of a tobacco dependence treatment plan.”
Patients and parents/caregivers should be given information on quiting resources such as 1-800-QUIT-NOW or the texting service SmokefreeTXT. However, one recommendation to avoid is the use of electronic nicotine delivery systems as a treatment for tobacco dependence.
The statement also notes there is an “increased risk of suicidal ideation and suicide both among continuing smokers and among those being treated for tobacco dependence” and the potential for neuropsychiatric symptoms with tobacco dependence treatment should be considered.
Finally, if tobacco exposure cannot be eliminated, guidance should be given to help reduce a child’s exposure to tobacco smoke.
AAP also released a policy statement on e-cigarettes in general and broader tobacco use. (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3222]).
“We are particularly alarmed and concerned about electronic cigarettes because we believe they have the potential to addict a new generation of youths to nicotine,” Dr. Wilson said. “We know that youths who may not have been smoking combustible cigarettes, but who start with electronic cigarettes are then more likely to go on and smoke combustible tobacco, which concerns us that they may continue on because we know that people who start to use nicotine and smoke cigarettes before the age of 21 [years] are far more likely to become adult chronic smokers.”
The AAP policy statement on electronic nicotine delivery systems (ENDS) recommends active screening for ENDS use in particular that echo many of the overall tobacco screening and treatment recommendations. The organization also lent support to a number of public policy initiatives, including banning sale of e-cigarettes to those under 21 years; FDA oversight and regulation; banning of flavored liquid nicotine and advertising that can be viewed by youths; and packaging restrictions to prevent accidental ingestion by children.
More broadly, in the public policy statement, AAP is calling for FDA to regulate all tobacco products and to make sure the agency is adequately funded for regulatory activity; stricter advertising guidelines; higher prices to discourage initiation by youth; and wider smoking bans, including in multiunit housing (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3109]).
The American Academy of Pediatrics is urging more action to protect children from the harms of tobacco and nicotine in clinical and public policy statements published online in Pediatrics.
In the clinical policy statement, AAP offers a series of recommendations for pediatricians and other health care providers to guide the identification of potential issues, as well as how they can be treated upon discovery (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3108]).
“There is no safe level of tobacco smoke exposure, and teenagers and children must be protected from its harmful effects,” Dr. Karen M. Wilson, section head of pediatric medicine at Children’s Hospital, Aurora, Colo., and chair of the AAP Section on Tobacco Control said in a Oct. 23 telebriefing prior to the release of the statements. “If current trends continue, 5.6 million of today’s youth will die prematurely from tobacco and smoking,” she said.
The AAP recommends an inquiry about tobacco use and tobacco smoke as part of health supervision visits, as well as visits for diseases that may be caused or exacerbated by tobacco smoke exposure. Parents should be asked who is smoking around a child and where, and children and adolescents should be asked about cigarettes and other kinds of tobacco and nicotine products (i.e., e-cigarettes) they have may have tried or are actively using.
The recommendations are backed by a technical report that provides the evidence base to support AAP’s clinical and policy statements, also published online in Pediatrics (2015 Oct. 26 [doi: 10.1542/peds.2015-3110]).
Furthermore, guidance of tobacco prevention should be given, including messages that experimenting with tobacco use is not safe.
“Messages should start as early as children are developmentally ready to understand them, usually approximately 5 years of age,” AAP said in the statement. Messages that may resonate more with adolescents include the effect of tobacco use on appearance, breath, and sports performance; lack of benefit for weight loss; how much money they would have to spend to continue their tobacco addiction; and how the tobacco industry deceives them, AAP said.
“Adolescents are particularly susceptible to nicotine,” Dr. Wilson noted. “Even low levels of exposure to nicotine and tobacco can worsen asthma or negatively impact IQ scores in young children,” she said.
Adolescents should be offered tobacco dependence treatment if they want to stop, although the use of pharmacotherapy is not as strong a recommendation.
“Research on pharmacotherapy of moderate to severe adolescent tobacco dependence is limited by short courses of treatment, high rates of nonadherence, and high rates of relapse after discontinuation of therapy,” the statement notes, adding that adolescents can be offered pharmacotherapy “appropriate to the severity of his or her tobacco dependence and his or her readiness to change as part of a tobacco dependence treatment plan.”
Patients and parents/caregivers should be given information on quiting resources such as 1-800-QUIT-NOW or the texting service SmokefreeTXT. However, one recommendation to avoid is the use of electronic nicotine delivery systems as a treatment for tobacco dependence.
The statement also notes there is an “increased risk of suicidal ideation and suicide both among continuing smokers and among those being treated for tobacco dependence” and the potential for neuropsychiatric symptoms with tobacco dependence treatment should be considered.
Finally, if tobacco exposure cannot be eliminated, guidance should be given to help reduce a child’s exposure to tobacco smoke.
AAP also released a policy statement on e-cigarettes in general and broader tobacco use. (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3222]).
“We are particularly alarmed and concerned about electronic cigarettes because we believe they have the potential to addict a new generation of youths to nicotine,” Dr. Wilson said. “We know that youths who may not have been smoking combustible cigarettes, but who start with electronic cigarettes are then more likely to go on and smoke combustible tobacco, which concerns us that they may continue on because we know that people who start to use nicotine and smoke cigarettes before the age of 21 [years] are far more likely to become adult chronic smokers.”
The AAP policy statement on electronic nicotine delivery systems (ENDS) recommends active screening for ENDS use in particular that echo many of the overall tobacco screening and treatment recommendations. The organization also lent support to a number of public policy initiatives, including banning sale of e-cigarettes to those under 21 years; FDA oversight and regulation; banning of flavored liquid nicotine and advertising that can be viewed by youths; and packaging restrictions to prevent accidental ingestion by children.
More broadly, in the public policy statement, AAP is calling for FDA to regulate all tobacco products and to make sure the agency is adequately funded for regulatory activity; stricter advertising guidelines; higher prices to discourage initiation by youth; and wider smoking bans, including in multiunit housing (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3109]).
The American Academy of Pediatrics is urging more action to protect children from the harms of tobacco and nicotine in clinical and public policy statements published online in Pediatrics.
In the clinical policy statement, AAP offers a series of recommendations for pediatricians and other health care providers to guide the identification of potential issues, as well as how they can be treated upon discovery (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3108]).
“There is no safe level of tobacco smoke exposure, and teenagers and children must be protected from its harmful effects,” Dr. Karen M. Wilson, section head of pediatric medicine at Children’s Hospital, Aurora, Colo., and chair of the AAP Section on Tobacco Control said in a Oct. 23 telebriefing prior to the release of the statements. “If current trends continue, 5.6 million of today’s youth will die prematurely from tobacco and smoking,” she said.
The AAP recommends an inquiry about tobacco use and tobacco smoke as part of health supervision visits, as well as visits for diseases that may be caused or exacerbated by tobacco smoke exposure. Parents should be asked who is smoking around a child and where, and children and adolescents should be asked about cigarettes and other kinds of tobacco and nicotine products (i.e., e-cigarettes) they have may have tried or are actively using.
The recommendations are backed by a technical report that provides the evidence base to support AAP’s clinical and policy statements, also published online in Pediatrics (2015 Oct. 26 [doi: 10.1542/peds.2015-3110]).
Furthermore, guidance of tobacco prevention should be given, including messages that experimenting with tobacco use is not safe.
“Messages should start as early as children are developmentally ready to understand them, usually approximately 5 years of age,” AAP said in the statement. Messages that may resonate more with adolescents include the effect of tobacco use on appearance, breath, and sports performance; lack of benefit for weight loss; how much money they would have to spend to continue their tobacco addiction; and how the tobacco industry deceives them, AAP said.
“Adolescents are particularly susceptible to nicotine,” Dr. Wilson noted. “Even low levels of exposure to nicotine and tobacco can worsen asthma or negatively impact IQ scores in young children,” she said.
Adolescents should be offered tobacco dependence treatment if they want to stop, although the use of pharmacotherapy is not as strong a recommendation.
“Research on pharmacotherapy of moderate to severe adolescent tobacco dependence is limited by short courses of treatment, high rates of nonadherence, and high rates of relapse after discontinuation of therapy,” the statement notes, adding that adolescents can be offered pharmacotherapy “appropriate to the severity of his or her tobacco dependence and his or her readiness to change as part of a tobacco dependence treatment plan.”
Patients and parents/caregivers should be given information on quiting resources such as 1-800-QUIT-NOW or the texting service SmokefreeTXT. However, one recommendation to avoid is the use of electronic nicotine delivery systems as a treatment for tobacco dependence.
The statement also notes there is an “increased risk of suicidal ideation and suicide both among continuing smokers and among those being treated for tobacco dependence” and the potential for neuropsychiatric symptoms with tobacco dependence treatment should be considered.
Finally, if tobacco exposure cannot be eliminated, guidance should be given to help reduce a child’s exposure to tobacco smoke.
AAP also released a policy statement on e-cigarettes in general and broader tobacco use. (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3222]).
“We are particularly alarmed and concerned about electronic cigarettes because we believe they have the potential to addict a new generation of youths to nicotine,” Dr. Wilson said. “We know that youths who may not have been smoking combustible cigarettes, but who start with electronic cigarettes are then more likely to go on and smoke combustible tobacco, which concerns us that they may continue on because we know that people who start to use nicotine and smoke cigarettes before the age of 21 [years] are far more likely to become adult chronic smokers.”
The AAP policy statement on electronic nicotine delivery systems (ENDS) recommends active screening for ENDS use in particular that echo many of the overall tobacco screening and treatment recommendations. The organization also lent support to a number of public policy initiatives, including banning sale of e-cigarettes to those under 21 years; FDA oversight and regulation; banning of flavored liquid nicotine and advertising that can be viewed by youths; and packaging restrictions to prevent accidental ingestion by children.
More broadly, in the public policy statement, AAP is calling for FDA to regulate all tobacco products and to make sure the agency is adequately funded for regulatory activity; stricter advertising guidelines; higher prices to discourage initiation by youth; and wider smoking bans, including in multiunit housing (Pediatrics. 2015 Oct. 26 [doi: 10.1542/peds.2015-3109]).