User login
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
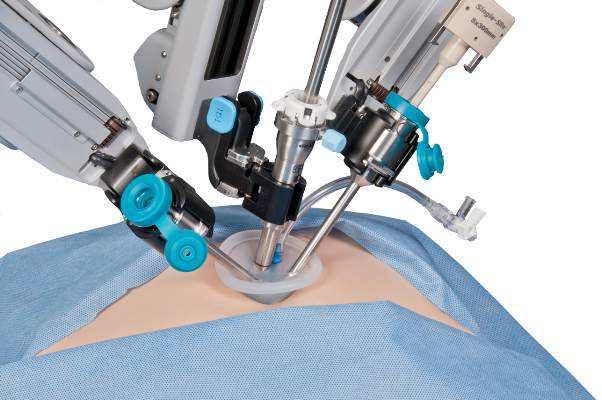
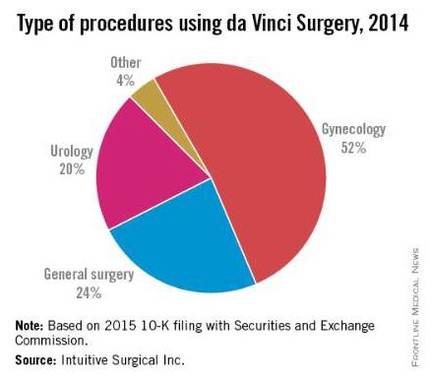
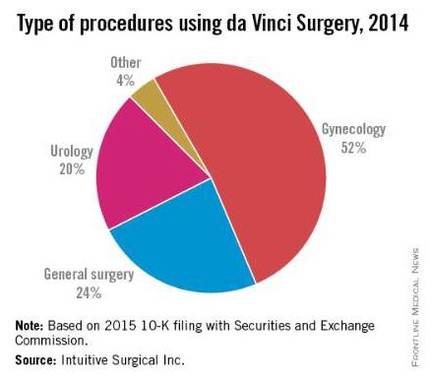
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What will help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
“I believe that that’s the case – that 10 years from now, we will be doing a lot more robotic surgery and the technology will be better and the cost will be dramatically less,” he said.
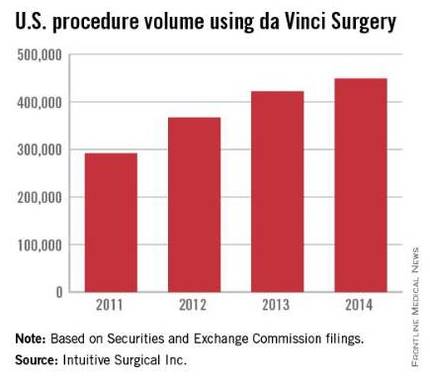
And while Dr. Pitt is looking forward, industry is promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci Surgery robot, in an Oct. 8, 2015, briefing with the press, presented data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now.
According to the company’s research, using only peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures, Andrew Yiu, Intuitive Surgical’s manager of clinical economics, said that outcomes were showing improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others.
Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculates the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci Xi Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, however, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spend in other areas of need.
“I think that cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
Ultimately, though, it comes down to cost, and Mr. Yiu stated that the company’s research is focused on costs related to the total episode of care. Yet Intuitive’s analysis does not factor capital and maintenance costs, which could have a dramatic impact on the overall cost-effectiveness equation.
First, there is a potential up-front cost of $1 to $2 million, as well as ongoing costs related to usage and maintenance, according to Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao. With the robot, “you have to get brand-new parts every single time, the new arm attachments. The only thing that is reusable is the camera itself. Everything is also an add-on to the cost and then you have the maintenance fee. It adds up on top of that,” she said in an interview.
In a study presented by Ms. Postoev and colleagues at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, she found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery.
“Most of the data that I’ve seen, and it’s frequently discussed in surgical meetings, is whether or not the difference in robotics is sufficient to justify the cost,” Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
In the education ranks, students are seeing robotics more often as well.
“Everybody is going toward robotics,” Ms. Postoev said in an interview. “It’s much easier for a new surgeon to use than laparoscopic” surgery.
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”