User login
Similar Outcomes From Weekend Discharge
Hospitals typically reduce staffing levels and the availability of diagnostic, laboratory, and treatment services on weekends, and patients admitted on weekends exhibit poorer in‐hospital outcomes for several medical conditions.[1, 2, 3, 4, 5, 6, 7, 8, 9] Whether or not patients discharged on weekends have worse clinical outcomes has been less well studied.[10, 11, 12] Discharge rates on Saturday and Sunday are lower than for the other 5 days of the week,[12] but bed shortages and hospital overcrowding have increased the demand for maximizing 24/7 week‐round discharge efficiency. Given that the number of patients discharged on weekends is likely to continue to increase, it is important to assess the risk of weekend discharge on outcomes monitored as performance indicators by organizations such as the Centers for Medicare and Medicaid Services, the American Medical Association Physicians Consortium for Performance Improvement, the National Quality Forum, and the Joint Commission.
Thus, we designed this study to evaluate baseline characteristics, length of stay (LOS), and postdischarge outcomes for general internal medicine (GIM) patients in teaching hospitals discharged on weekends compared to weekdays. Our objective was to determine whether postdischarge outcomes differed for patients discharged on weekends versus weekdays.
METHODS
Study Setting
The Canadian province of Alberta has a single vertically integrated healthcare system that is government‐funded and provides universal access to hospitals, emergency departments (EDs), and outpatient physician services for all 4.1 million Albertans as well as all prescription medications for the poor, socially disadvantaged, disabled, or those age 65 years and older. This study received approval from the University of Alberta Health Research Ethics Board with waiver of informed consent.
Data Sources
This study used deidentified linked data from 3 Alberta Health administrative databases that capture vital status and all hospital or ED visits and have previously been shown to have high accuracy for medical diagnoses.[13] The Alberta Health Care Insurance Plan Registry tracks date of death or emigration from the province. The Discharge Abstract Database includes the most responsible diagnosis identified by the hospital attending physician, up to 25 other diagnoses coded by nosologists in each hospital, the admission and discharge dates, and the admission category (elective or urgent/emergent) for all acute care hospitalizations. Of note, unlike US studies, the hospital databases are able to distinguish in‐hospital (eg, adverse events) versus premorbid diagnoses (eg, preexisting comorbidities). The Ambulatory Care Database captures all patient visits to EDs with coding for up to 10 conditions per encounter.
Study Cohort
We identified all adults with an acute care hospitalization on the GIM services at all 7 Alberta teaching hospitals (ie, defined as those with Royal College of Physicians and Surgeons of Canadaapproved residency training programs in internal medicine, the equivalent of the Association of American Medical Colleges certification in the United States) between October 1, 2009 and September 30, 2010 and between April 1, 2011 and December 1, 2011 (these 20 months covered most of the pre/post intervals for a recently reported quality improvement initiative at 1 of the teaching hospitals that had no significant impact on postdischarge outcomes).[14] Patients from out of the province or transferred from/to another inpatient service (eg, the intensive care unit, a different service in the same hospital [such as surgery], another acute care hospital, or rehabilitation hospital) or with lengths of stay greater than 30 days were excluded. We only included the first hospitalization for any patient in our study timeframe and thus excluded repeat discharges of the same patient.
Explanatory Variable of Interest
The independent variable of interest was calendar day of discharge, stratified according to weekday (Monday thru Friday) versus weekend (Saturday and Sunday). Only 1.4% of weekday discharges occurred on a statutory holiday, and for the purposes of this study, these discharges were also considered weekend discharges. At the 7 teaching hospitals in Alberta, nursing staffing ratios do not differ between weekend and weekday, but availability of all other members of the healthcare team does. Physician census decreases from 4 to 5 per ward to 1 to 2, and ward‐based social workers, occupational therapists, physiotherapists, and pharmacist educators are generally not available on weekends.
Outcomes
Our primary outcome of interest was the composite outcome of death or all‐cause nonelective readmission within 30 days of discharge (ie, not including in‐hospital events prior to discharge or elective readmissions after discharge for planned procedures such as chemotherapy); hereafter we refer to this as death or readmission. This is a patient‐relevant outcome that is highlighted in the Affordable Care Act and for which there are several validated risk adjustment models.[15] We chose a composite outcome to deal with the issue of competing risks; if weekend discharges were more likely to die then we could observe a spurious association between weekend discharge and reduced readmissions if we focused on only that outcome.
Other Measures
Comorbidities for each patient were identified using International Classification of Diseases, Ninth Revision and Tenth Revision codes from the Discharge Abstract Database for the index hospitalization and any hospitalizations in the 12 months prior to their index admission, a method previously validated in Alberta databases.[13] We also recorded health resource use during their index hospitalization and calculated each patient's LACE score at the time of discharge, which is an index for predicting unplanned readmission or early death postdischarge previously validated in Canadian administrative databases.[15] The LACE index includes length of hospital stay (L), acuity of admission (A, based on the admission category variable described earlier), comorbidity burden quantified using the Charlson Comorbidity Index (C), and emergency department visits in the 6 months prior to admission (E); patients with discharge LACE scores >10 (total possible score is 19) are defined as being at high risk of death/readmission within 30 days.[16] As detailed below, to deal with potential concerns that LOS may be a mediator in the causal pathway, we ran 2 sensitivity analyses, 1 in which we excluded LOS from the analyses and 1 in which we included expected LOS rather than the actual LOS. Expected LOS is a data‐driven estimate based on the most current 2 years of patient LOS information available in the Canadian Institute for Health Information discharge abstract database (
Statistical Analysis
Baseline patient characteristics between weekend and weekday discharges were compared with t tests for continuous variables and [2] tests for binary or categorical variables. Logistic regression was used for comparison of death or readmission for weekend versus weekday discharges. Multivariable models were adjusted for age, sex, hospital, and LACE scores (as a continuous variable) at time of discharge; in sensitivity analyses we adjusted for (1) LACE score without including LOS and (2) LACE score using expected LOS rather than actual LOS. In further sensitivity analyses we (1) restricted the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater and (2) included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge). Day of admission (weekend vs weekday) was also considered for the multivariable models, but was not found to be significant and thus was omitted from final models. We do not have any physician identifying variables in our dataset and thus could not investigate the potential correlation among patients discharged by the same physician. We did explore the hospital intraclass correlation coefficient, and as it was very small (0.001), we did not utilize models to account for the hierarchical nature of the data, but did include hospital as a fixed effect in the logistic models. The results were virtually identical whether we did or did not include hospital in the models. Adjusted odds ratios (aORs) are displayed with 95% confidence intervals (CI) and P values. Average LOS was calculated for weekend and weekday discharges with 95% CIs. P values for adjusted length of stay were calculated using multivariable linear regression adjusting for age, sex, day of admission, and Charlson score. All statistical analyses were done using SAS for Windows version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Patient Characteristics
Of the 7991 patients discharged during our study interval, 1146 (14.3%) were discharged on weekend or holiday days (Table 1). In contrast, 2180 of our cohort were admitted on a weekend (27.3%). The mean age of our study population was 62.1 years, 51.9% were men, mean Charlson score was 2.56, and 4591 (57.5%) had LACE scores of at least 10 at discharge.
| Characteristic | Weekend Discharge | Weekday Discharge | P Value |
|---|---|---|---|
| |||
| No. of patients | 1,146 | 6,845 | |
| Age, y, mean (SD) | 57.97 (19.70) | 62.77 (19.37) | <0.0001 |
| Male | 601 (52.4) | 3,548 (51.8) | 0.70 |
| Top 5 most responsible diagnoses | |||
| COPD | 74 (6.5) | 507 (7.4) | |
| Pneumonia | 64 (5.6) | 326 (4.8) | |
| Heart failure | 31 (2.7) | 375 (5.5) | |
| Urinary tract infection | 39 (3.4) | 254 (3.7) | |
| Venous thromboembolism | 31 (2.7) | 259 (3.8) | |
| Charlson score, mean (SD) | 2.17 (3.29) | 2.63 (3.30) | <0.0001 |
| Comorbidities (based on index hospitalization and prior 12 months) | |||
| Hypertension | 485 (42.3) | 3,265 (47.7) | 0.00 |
| Diabetes mellitus | 326 (28.4) | 2,106 (30.8) | 0.11 |
| Fluid imbalance | 332 (29.0) | 1,969 (28.8) | 0.89 |
| COPD | 255 (22.3) | 1,790 (26.2) | 0.01 |
| Psychiatric disorder | 179 (15.6) | 1,459 (21.3) | <0.0001 |
| Pneumonia | 242 (21.1) | 1,427 (20.8) | 0.84 |
| Anemia | 167 (14.6) | 1,233 (18.0) | 0.00 |
| Trauma | 169 (14.7) | 1,209 (17.7) | 0.02 |
| Atrial fibrillation | 141 (12.3) | 1,069 (15.6) | 0.00 |
| Heart failure | 101 (8.8) | 946 (13.8) | <0.0001 |
| Drug abuse | 188 (16.4) | 966 (14.1) | 0.04 |
| Cancer | 124 (10.8) | 867 (12.7) | 0.08 |
| Renal disease | 93 (8.1) | 689 (10.1) | 0.04 |
| Dementia | 49 (4.3) | 564 (8.2) | <0.0001 |
| Mild liver disease | 99 (8.6) | 587 (8.6) | 0.94 |
| Cerebrovascular disease | 59 (5.1) | 492 (7.2) | 0.01 |
| Gastrointestinal bleed | 84 (7.3) | 496 (7.2) | 0.92 |
| Asthma | 83 (7.2) | 426 (6.2) | 0.19 |
| Stroke | 42 (3.7) | 332 (4.9) | 0.08 |
| Prior myocardial infarction | 47 (4.1) | 329 (4.8) | 0.30 |
| Arthritis | 42 (3.7) | 309 (4.5) | 0.19 |
| Peripheral vascular disease | 42 (3.7) | 259 (3.8) | 0.84 |
| Severe liver disease | 44 (3.8) | 261 (3.8) | 0.97 |
| Valve disease | 24 (2.1) | 188 (2.7) | 0.20 |
| Paralysis | 31 (2.7) | 201 (2.9) | 0.67 |
| Skin ulcer | 17 (1.5) | 137 (2.0) | 0.24 |
| Shock | 19 (1.7) | 99 (1.4) | 0.58 |
| HIV | 15 (1.3) | 109 (1.6) | 0.47 |
| Protein calorie malnutrition | 0 (0.0) | 9 (0.1) | 0.21 |
| Features of index hospitalization | |||
| Resource intensity weight, mean (SD) | 1.10 (0.82) | 1.38 (1.24) | <0.0001 |
| LACE score, mean (SD) | 9.45 (2.85) | 10.51 (3.03) | <0.0001 |
| Expected LOS, mean (SD) | 6.20 (4.08) | 7.12 (4.89) | <0.0001 |
| Acute LOS, mean (SD) | 5.64 (4.99) | 7.86 (6.13) | <0.0001 |
| Weekend admission | 244 (21.3) | 1,936 (28.3) | <0.0001 |
| Discharge disposition | <0.0001 | ||
| Transferred to another inpatient hospital | 14 (1.2) | 189 (2.8) | |
| Transferred to long‐term care facility | 36 (3.1) | 532 (7.8) | |
| Transferred to other (except hospice) | 5 (0.4) | 24 (0.4) | |
| Discharged to home setting with support services | 125 (10.9) | 1,318 (19.3) | |
| Discharged home | 926 (80.8) | 4,646 (67.9) | |
| Left against medical advice | 40 (3.5) | 136 (2.0) | |
Weekday Versus Weekend Discharge
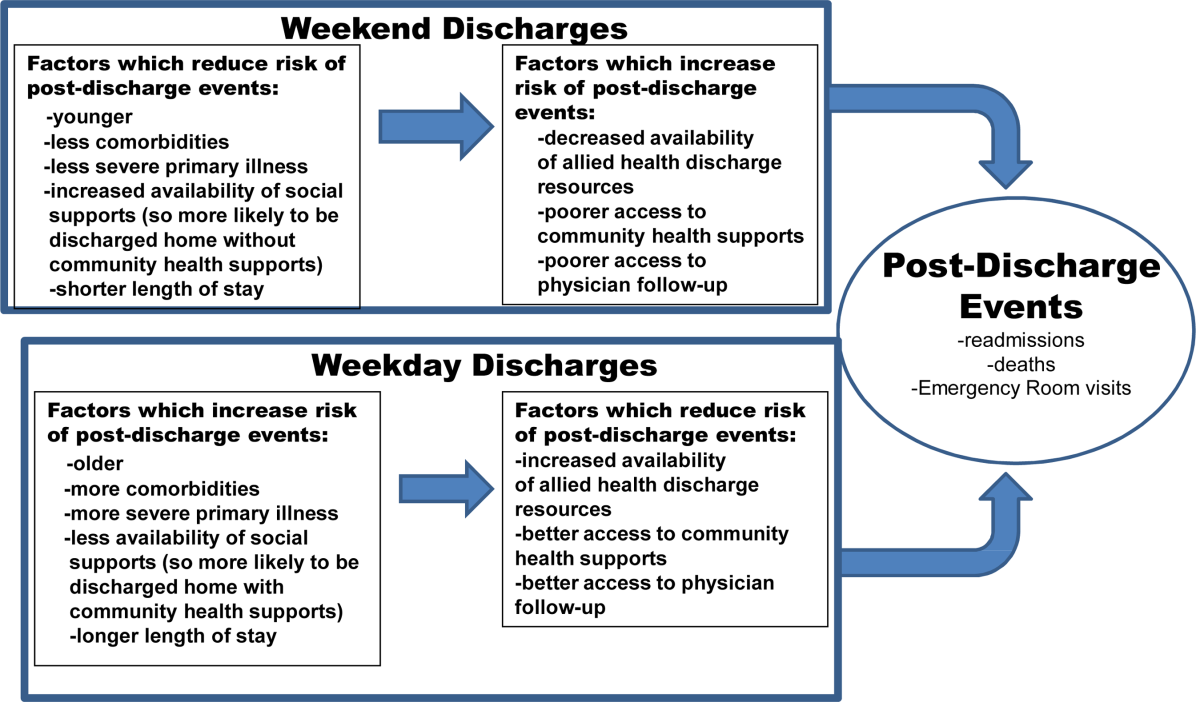
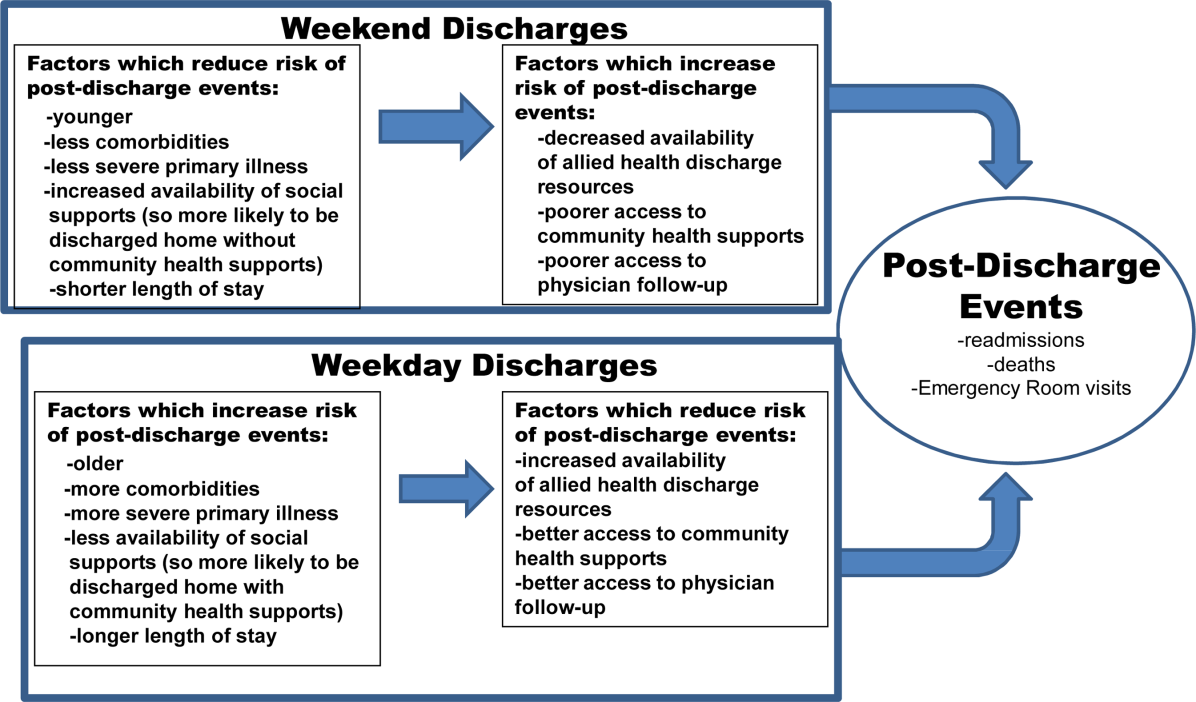
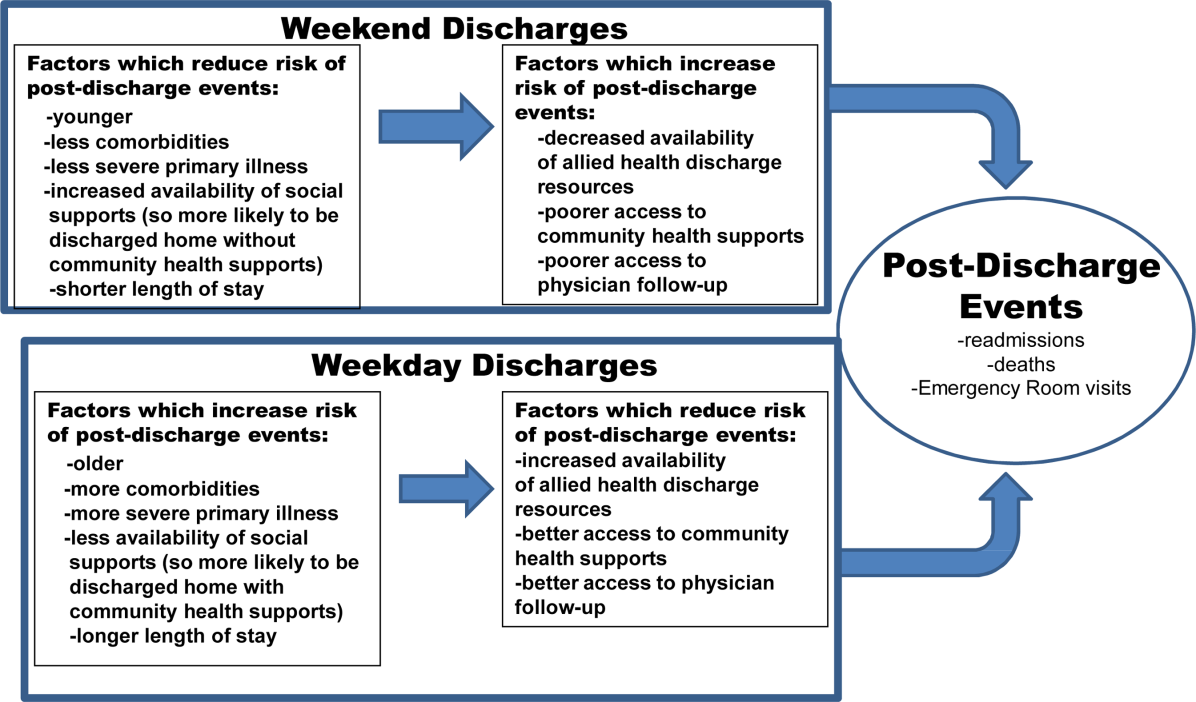
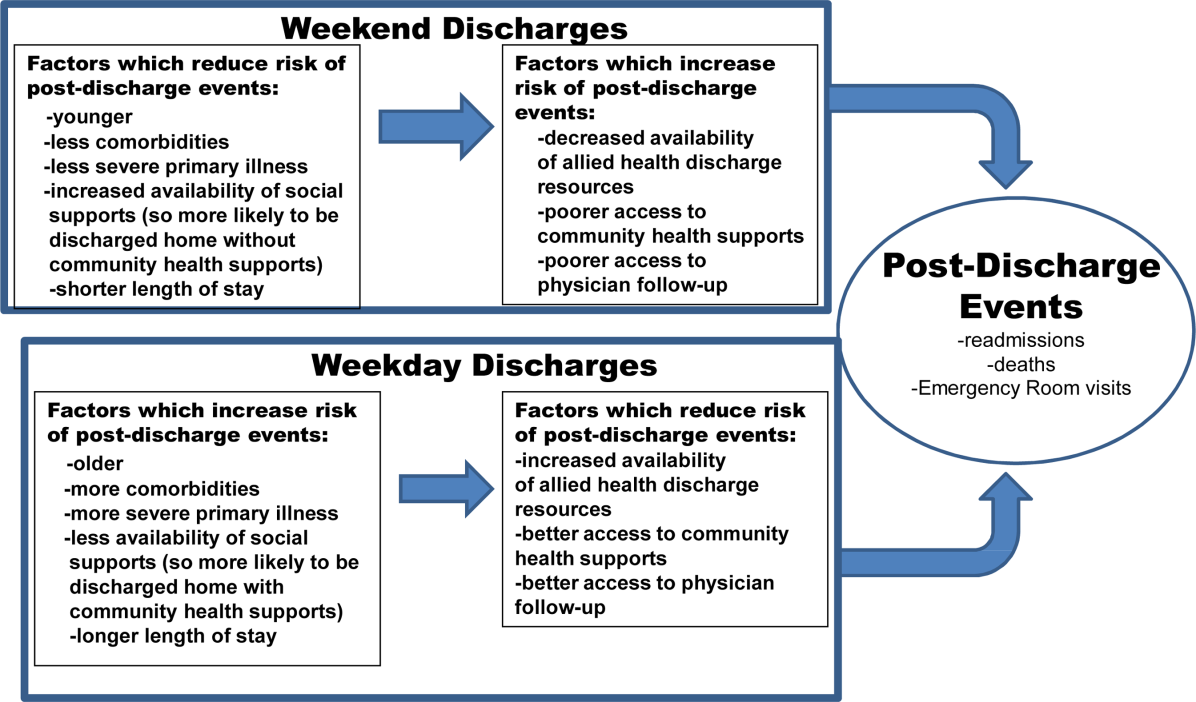
Although patients admitted on weekdays and weekends were very similar (data available upon request), patients discharged on weekends (compared to those discharged on weekdays) were younger, more likely to be discharged home without additional support, and had fewer comorbidities (Table 1, Figure 1). Patients discharged on weekends had shorter lengths of stay than those discharged on weekdays (5.6 days vs 7.9 days, P<0.0001). In adjusted linear regression analyses, this 2.3‐day difference remained statistically significant (adjusted P value <0.0001).
Patients discharged on a weekend exhibited lower unadjusted 30‐day rates of death or readmission than those discharged on a weekday (10.6% vs 13.2%), but these differences disappeared after multivariable adjustment that accounted for differences in risk profile (aOR: 0.94, 95% CI: 0.771.16 (Table 2). Results were similar in sensitivity analyses adjusting for LACE scores without LOS included (aOR: 0.88, 95% CI: 0.711.08) or adjusting for LACE scores using expected LOS rather than actual LOS (aOR: 0.90, 95% CI: 0.731.10). Restricting the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater confirmed that weekend and weekday discharges had similar outcomes in the first 30 days after discharge (aOR: 1.09, 95% CI: 0.851.41, Table 2). Similar patterns were seen when we included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge) (Table 2).
| Weekend Discharge, n/N (%) | Weekday Discharge, n/N (%) | Unadjusted P Value | aOR* (95% CI) | Adjusted P Value | |
|---|---|---|---|---|---|
| |||||
| Death/readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 121/1146 (10.6) | 901/6845 (13.2) | 0.01 | 0.94 (0.77‐1.16) | 0.58 |
| All 7 teaching hospitals, but only patients with LACE <10 | 37/647 (5.7) | 225/2753 (8.2) | 0.04 | 0.72 (0.50, 1.03) | 0.07 |
| All 7 teaching hospitals, but only patients with LACE 10 | 84/499 (16.8) | 676/4092 (16.5) | 0.86 | 1.09 (0.85‐1.41) | 0.49 |
| Death/readmission/ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 218/1146 (19.0) | 1445/6845 (21.1) | 0.11 | 0.98 (0.83‐1.15) | 0.79 |
| All 7 teaching hospitals, but only patients with LACE <10 | 90/647 (13.9) | 460/2753 (16.7) | 0.08 | 0.83 (0.64‐1.06) | 0.13 |
| All 7 teaching hospitals, but only patients with LACE 10 | 128/499 (25.7) | 985/4092 (24.1) | 0.44 | 1.12 (0.90‐1.39) | 0.31 |
| Death within 30 days | |||||
| All 7 teaching hospitals, all patients | 24/1146 (2.1) | 215/6845 (3.1) | 0.05 | 0.97 (0.63‐1.51) | 0.89 |
| All 7 teaching hospitals, but only patients with LACE <10 | 4/647 (0.6) | 23/2753 (0.8) | 0.58 | 0.89 (0.30, 2.62) | 0.83 |
| All 7 teaching hospitals, but only patients with LACE 10 | 20/499 (4.0) | 192/4092 (4.7) | 0.49 | 0.99 (0.61‐1.61) | 0.98 |
| Readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 105/1146 (9.2) | 751/6845 (11.0) | 0.07 | 0.94 (0.76‐1.17) | 0.59 |
| All 7 teaching hospitals, but only patients with LACE <10 | 33/647 (5.1) | 211/2753 (7.7) | 0.02 | 0.68 (0.46‐0.99) | 0.04 |
| All 7 teaching hospitals, but only patients with LACE 10 | 72/499 (14.4) | 540/4092 (13.2) | 0.44 | 1.14 (0.87‐1.49) | 0.34 |
| ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 182/1146 (15.9) | 1118/6845 (16.3) | 0.70 | 1.00 (0.84‐1.19) | 0.99 |
| All 7 teaching hospitals, but only patients with LACE <10 | 83/647 (12.8) | 412/2753 (15.0) | 0.17 | 0.84 (0.65, 1.09) | 0.20 |
| All 7 teaching hospitals, but only patients with LACE 10 | 99/499 (19.8) | 706/4092 (17.3) | 0.15 | 1.17 (0.92‐1.48) | 0.20 |
DISCUSSION
Our data suggest that patients discharged from the GIM teaching wards we studied on weekends were appropriately triaged, as they did not exhibit a higher risk of adverse events postdischarge. Although patients discharged on weekends tended to be younger and had less comorbidities than those discharged during the week, we adjusted for baseline covariates in analyses, and we did not find an association between weekend discharge and increased postdischarge events even among the subset of patients deemed to be at high risk for postdischarge adverse events (based on high LACE scores). To our knowledge, although we previously examined this issue in patients with a most‐responsible diagnosis of heart failure,[10] examining weekend versus weekday discharges in the full gamut of general medical patients admitted to teaching hospitals has not previously been examined.
In our previous study[10] of over 24,000 heart failure patients discharged over 10 years (up to June 2009, therefore no overlap with any patients in this study), we also found that patients discharged on the weekends were younger, had fewer comorbidities, and shorter lengths of stay. Although postdischarge death/readmission rates were higher for weekend discharged patients in our earlier study (21.1% vs 19.5%, adjusted hazard ratio: 1.15, 95% CI: 1.061.25), it is worth noting that this was almost entirely driven by data from nonteaching hospitals and cardiology wards. Thus, it is important to reiterate that the findings in our current study are for GIM wards in teaching hospitals and may not be generalizable to less‐structured nonteaching settings.
Although we did not study physician decision making, our results suggest that physicians are incorporating discharge day into their discharge decision making. They may be selecting younger patients with less comorbidities for weekend discharges, or they may be delaying the discharges of older patients with more comorbidities for weekday discharges. Either is not surprising given the realities of weekend inpatient care: reduced staffing and frequent cross‐coverage (of physicians, nurses, physiotherapists, pharmacists, and occupational therapists), limited support services (such as laboratory services or diagnostic imaging), and decreased availability of community services (including home care and social support services).[17] For example, in 1 large US heart failure registry, patients discharged on a weekend received less complete discharge instructions than those discharged on weekdays.[11] Given that early follow‐up postdischarge is associated with better outcomes,[18, 19] future studies should also explore whether patterns of patient follow‐up differ after weekend versus weekday discharges.
Although we were able to capture all interactions with the healthcare system in a single payer system with universal access, there are some limitations to our study. First, we used administrative data, which preclude fully adjusting for severity of diagnoses or functional status, although we used proxies such as admission from/discharge to a long‐term care facility.[20, 21] Second, we did not have access to process of care measures such as diagnostic testing or prescribing data, and thus cannot determine whether quality of care or patient adherence differed by the day of the week they were discharged on, although this seems unlikely. Third, although postdischarge follow‐up may be associated with better outcomes,[18, 19] we were unable to adjust for patterns of outpatient follow‐up in this study. Fourth, we acknowledge that death or readmission soon after discharge does not necessarily mean that the quality of care during the preceding hospitalization was suboptimal or that these deaths or readmissions were even potentially preventable. Many factors influence postdischarge mortality and/or readmission, and quality of inpatient care is only one.[22, 23, 24, 25] Fifth, although some may express concern that LOS may be a mediator in the causal pathway between discharge decision and postdischarge events, and that adjusting for LOS in analyses could thus spuriously obscure a true association, it is worth pointing out that our 2 sensitivity analyses to explore this (the 1 in which we excluded LOS from the analyses and the 1 in which we included expected LOS rather than the actual LOS) revealed nearly identical point estimates and 95% CI as our main analysis. Finally, as our study is observational, we cannot definitively conclude causality, nor can we exclude an 18% excess risk for patients discharged on weekends (or a 22% lower risk either), given our 95% CI for postdischarge adverse outcomes.
CONCLUSION
We found that the proportion of patients discharged on weekends is lower than the proportion admitted on weekends. We also found that lower risk/less severely ill patients appear to be preferentially discharged on weekends, and as a result, postdischarge outcomes are similar between weekend and weekday discharges despite shorter LOS and less availability of outpatient resources for patients discharged on a weekend. The reasons why more complicated patients are not discharged on weekends deserves further study, as safely increasing weekend discharge rates would improve efficiency and safety (by reducing unnecessary exposure to in‐hospital adverse events such as falls, unnecessary urinary catheterizations, and healthcare‐acquired infections). Although hospital admission has become a 24/7 business, we believe that hospital discharge processes should strive for the same level of efficiency.
ACKNOWLEDGMENTS
Disclosures: This study is based in part on data provided by Alberta Health. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the government of Alberta. Neither the government of Alberta nor Alberta Health express any opinion in relation to this study. F.A.M. and S.R.M. are supported by salary awards from Alberta Innovates‐Health Solutions (AIHS). F.A.M. holds the Capital Health Chair in Cardiology Outcomes Research. S.R.M. holds the Endowed Chair in Patient Health Management. This project was funded by AIHS through an investigator‐initiated peer reviewed operating grant. The funding agencies did not have input into study design, data collection, interpretation of results, or write up/approval for submission. The authors report no conflicts of interest.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668.
- , , , et al. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294:803–812.
- , . Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117:175–181.
- . Do hospitals provide lower quality care on weekends? Health Serv Res. 2007;42:1589–1612.
- , , , et al. Day of admission and clinical outcomes for patients hospitalized for heart failure: findings from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE‐HF). Circ Heart Fail. 2008;1:50–57.
- , , , et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med. 2012;105:74–84.
- , , , . Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211–1215.
- , , , . Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530–539.
- , , , . Effects of weekend admission and hospital teaching status on in‐hospital mortality. Am J Med. 2004;117:151–157.
- , , , , . Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail. 2013;6:922–929.
- , , , et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158:451–458.
- , . Risk of death or readmission among people discharged from hospital on Fridays. CMAJ. 2002;166:1672–1673.
- , , , , et al.; IMECCHI Investigators. Assessing validity of ICD‐9‐CM and ICD‐10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441.
- , , , et al. Safely and effectively reducing inpatient length of stay: a controlled study of the General Internal Medicine Care Transformation Initiative. BMJ Qual Saf. 2014;23:446–456.
- , , , et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- , . Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011;26:1050–1052.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , , , , . Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185:e681–e689.
- , , , , , . Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research. Ann Intern Med. 1993;119:844–850.
- , , , . Predictions of hospital mortality rates: a comparison of data sources. Ann Intern Med. 1997;126:347–354.
- , , , et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282.
- , . Investigating early readmission as an indicator for quality of care studies. Med Care. 1991;29(4):377–394.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , . Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402.
Hospitals typically reduce staffing levels and the availability of diagnostic, laboratory, and treatment services on weekends, and patients admitted on weekends exhibit poorer in‐hospital outcomes for several medical conditions.[1, 2, 3, 4, 5, 6, 7, 8, 9] Whether or not patients discharged on weekends have worse clinical outcomes has been less well studied.[10, 11, 12] Discharge rates on Saturday and Sunday are lower than for the other 5 days of the week,[12] but bed shortages and hospital overcrowding have increased the demand for maximizing 24/7 week‐round discharge efficiency. Given that the number of patients discharged on weekends is likely to continue to increase, it is important to assess the risk of weekend discharge on outcomes monitored as performance indicators by organizations such as the Centers for Medicare and Medicaid Services, the American Medical Association Physicians Consortium for Performance Improvement, the National Quality Forum, and the Joint Commission.
Thus, we designed this study to evaluate baseline characteristics, length of stay (LOS), and postdischarge outcomes for general internal medicine (GIM) patients in teaching hospitals discharged on weekends compared to weekdays. Our objective was to determine whether postdischarge outcomes differed for patients discharged on weekends versus weekdays.
METHODS
Study Setting
The Canadian province of Alberta has a single vertically integrated healthcare system that is government‐funded and provides universal access to hospitals, emergency departments (EDs), and outpatient physician services for all 4.1 million Albertans as well as all prescription medications for the poor, socially disadvantaged, disabled, or those age 65 years and older. This study received approval from the University of Alberta Health Research Ethics Board with waiver of informed consent.
Data Sources
This study used deidentified linked data from 3 Alberta Health administrative databases that capture vital status and all hospital or ED visits and have previously been shown to have high accuracy for medical diagnoses.[13] The Alberta Health Care Insurance Plan Registry tracks date of death or emigration from the province. The Discharge Abstract Database includes the most responsible diagnosis identified by the hospital attending physician, up to 25 other diagnoses coded by nosologists in each hospital, the admission and discharge dates, and the admission category (elective or urgent/emergent) for all acute care hospitalizations. Of note, unlike US studies, the hospital databases are able to distinguish in‐hospital (eg, adverse events) versus premorbid diagnoses (eg, preexisting comorbidities). The Ambulatory Care Database captures all patient visits to EDs with coding for up to 10 conditions per encounter.
Study Cohort
We identified all adults with an acute care hospitalization on the GIM services at all 7 Alberta teaching hospitals (ie, defined as those with Royal College of Physicians and Surgeons of Canadaapproved residency training programs in internal medicine, the equivalent of the Association of American Medical Colleges certification in the United States) between October 1, 2009 and September 30, 2010 and between April 1, 2011 and December 1, 2011 (these 20 months covered most of the pre/post intervals for a recently reported quality improvement initiative at 1 of the teaching hospitals that had no significant impact on postdischarge outcomes).[14] Patients from out of the province or transferred from/to another inpatient service (eg, the intensive care unit, a different service in the same hospital [such as surgery], another acute care hospital, or rehabilitation hospital) or with lengths of stay greater than 30 days were excluded. We only included the first hospitalization for any patient in our study timeframe and thus excluded repeat discharges of the same patient.
Explanatory Variable of Interest
The independent variable of interest was calendar day of discharge, stratified according to weekday (Monday thru Friday) versus weekend (Saturday and Sunday). Only 1.4% of weekday discharges occurred on a statutory holiday, and for the purposes of this study, these discharges were also considered weekend discharges. At the 7 teaching hospitals in Alberta, nursing staffing ratios do not differ between weekend and weekday, but availability of all other members of the healthcare team does. Physician census decreases from 4 to 5 per ward to 1 to 2, and ward‐based social workers, occupational therapists, physiotherapists, and pharmacist educators are generally not available on weekends.
Outcomes
Our primary outcome of interest was the composite outcome of death or all‐cause nonelective readmission within 30 days of discharge (ie, not including in‐hospital events prior to discharge or elective readmissions after discharge for planned procedures such as chemotherapy); hereafter we refer to this as death or readmission. This is a patient‐relevant outcome that is highlighted in the Affordable Care Act and for which there are several validated risk adjustment models.[15] We chose a composite outcome to deal with the issue of competing risks; if weekend discharges were more likely to die then we could observe a spurious association between weekend discharge and reduced readmissions if we focused on only that outcome.
Other Measures
Comorbidities for each patient were identified using International Classification of Diseases, Ninth Revision and Tenth Revision codes from the Discharge Abstract Database for the index hospitalization and any hospitalizations in the 12 months prior to their index admission, a method previously validated in Alberta databases.[13] We also recorded health resource use during their index hospitalization and calculated each patient's LACE score at the time of discharge, which is an index for predicting unplanned readmission or early death postdischarge previously validated in Canadian administrative databases.[15] The LACE index includes length of hospital stay (L), acuity of admission (A, based on the admission category variable described earlier), comorbidity burden quantified using the Charlson Comorbidity Index (C), and emergency department visits in the 6 months prior to admission (E); patients with discharge LACE scores >10 (total possible score is 19) are defined as being at high risk of death/readmission within 30 days.[16] As detailed below, to deal with potential concerns that LOS may be a mediator in the causal pathway, we ran 2 sensitivity analyses, 1 in which we excluded LOS from the analyses and 1 in which we included expected LOS rather than the actual LOS. Expected LOS is a data‐driven estimate based on the most current 2 years of patient LOS information available in the Canadian Institute for Health Information discharge abstract database (
Statistical Analysis
Baseline patient characteristics between weekend and weekday discharges were compared with t tests for continuous variables and [2] tests for binary or categorical variables. Logistic regression was used for comparison of death or readmission for weekend versus weekday discharges. Multivariable models were adjusted for age, sex, hospital, and LACE scores (as a continuous variable) at time of discharge; in sensitivity analyses we adjusted for (1) LACE score without including LOS and (2) LACE score using expected LOS rather than actual LOS. In further sensitivity analyses we (1) restricted the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater and (2) included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge). Day of admission (weekend vs weekday) was also considered for the multivariable models, but was not found to be significant and thus was omitted from final models. We do not have any physician identifying variables in our dataset and thus could not investigate the potential correlation among patients discharged by the same physician. We did explore the hospital intraclass correlation coefficient, and as it was very small (0.001), we did not utilize models to account for the hierarchical nature of the data, but did include hospital as a fixed effect in the logistic models. The results were virtually identical whether we did or did not include hospital in the models. Adjusted odds ratios (aORs) are displayed with 95% confidence intervals (CI) and P values. Average LOS was calculated for weekend and weekday discharges with 95% CIs. P values for adjusted length of stay were calculated using multivariable linear regression adjusting for age, sex, day of admission, and Charlson score. All statistical analyses were done using SAS for Windows version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Patient Characteristics
Of the 7991 patients discharged during our study interval, 1146 (14.3%) were discharged on weekend or holiday days (Table 1). In contrast, 2180 of our cohort were admitted on a weekend (27.3%). The mean age of our study population was 62.1 years, 51.9% were men, mean Charlson score was 2.56, and 4591 (57.5%) had LACE scores of at least 10 at discharge.
| Characteristic | Weekend Discharge | Weekday Discharge | P Value |
|---|---|---|---|
| |||
| No. of patients | 1,146 | 6,845 | |
| Age, y, mean (SD) | 57.97 (19.70) | 62.77 (19.37) | <0.0001 |
| Male | 601 (52.4) | 3,548 (51.8) | 0.70 |
| Top 5 most responsible diagnoses | |||
| COPD | 74 (6.5) | 507 (7.4) | |
| Pneumonia | 64 (5.6) | 326 (4.8) | |
| Heart failure | 31 (2.7) | 375 (5.5) | |
| Urinary tract infection | 39 (3.4) | 254 (3.7) | |
| Venous thromboembolism | 31 (2.7) | 259 (3.8) | |
| Charlson score, mean (SD) | 2.17 (3.29) | 2.63 (3.30) | <0.0001 |
| Comorbidities (based on index hospitalization and prior 12 months) | |||
| Hypertension | 485 (42.3) | 3,265 (47.7) | 0.00 |
| Diabetes mellitus | 326 (28.4) | 2,106 (30.8) | 0.11 |
| Fluid imbalance | 332 (29.0) | 1,969 (28.8) | 0.89 |
| COPD | 255 (22.3) | 1,790 (26.2) | 0.01 |
| Psychiatric disorder | 179 (15.6) | 1,459 (21.3) | <0.0001 |
| Pneumonia | 242 (21.1) | 1,427 (20.8) | 0.84 |
| Anemia | 167 (14.6) | 1,233 (18.0) | 0.00 |
| Trauma | 169 (14.7) | 1,209 (17.7) | 0.02 |
| Atrial fibrillation | 141 (12.3) | 1,069 (15.6) | 0.00 |
| Heart failure | 101 (8.8) | 946 (13.8) | <0.0001 |
| Drug abuse | 188 (16.4) | 966 (14.1) | 0.04 |
| Cancer | 124 (10.8) | 867 (12.7) | 0.08 |
| Renal disease | 93 (8.1) | 689 (10.1) | 0.04 |
| Dementia | 49 (4.3) | 564 (8.2) | <0.0001 |
| Mild liver disease | 99 (8.6) | 587 (8.6) | 0.94 |
| Cerebrovascular disease | 59 (5.1) | 492 (7.2) | 0.01 |
| Gastrointestinal bleed | 84 (7.3) | 496 (7.2) | 0.92 |
| Asthma | 83 (7.2) | 426 (6.2) | 0.19 |
| Stroke | 42 (3.7) | 332 (4.9) | 0.08 |
| Prior myocardial infarction | 47 (4.1) | 329 (4.8) | 0.30 |
| Arthritis | 42 (3.7) | 309 (4.5) | 0.19 |
| Peripheral vascular disease | 42 (3.7) | 259 (3.8) | 0.84 |
| Severe liver disease | 44 (3.8) | 261 (3.8) | 0.97 |
| Valve disease | 24 (2.1) | 188 (2.7) | 0.20 |
| Paralysis | 31 (2.7) | 201 (2.9) | 0.67 |
| Skin ulcer | 17 (1.5) | 137 (2.0) | 0.24 |
| Shock | 19 (1.7) | 99 (1.4) | 0.58 |
| HIV | 15 (1.3) | 109 (1.6) | 0.47 |
| Protein calorie malnutrition | 0 (0.0) | 9 (0.1) | 0.21 |
| Features of index hospitalization | |||
| Resource intensity weight, mean (SD) | 1.10 (0.82) | 1.38 (1.24) | <0.0001 |
| LACE score, mean (SD) | 9.45 (2.85) | 10.51 (3.03) | <0.0001 |
| Expected LOS, mean (SD) | 6.20 (4.08) | 7.12 (4.89) | <0.0001 |
| Acute LOS, mean (SD) | 5.64 (4.99) | 7.86 (6.13) | <0.0001 |
| Weekend admission | 244 (21.3) | 1,936 (28.3) | <0.0001 |
| Discharge disposition | <0.0001 | ||
| Transferred to another inpatient hospital | 14 (1.2) | 189 (2.8) | |
| Transferred to long‐term care facility | 36 (3.1) | 532 (7.8) | |
| Transferred to other (except hospice) | 5 (0.4) | 24 (0.4) | |
| Discharged to home setting with support services | 125 (10.9) | 1,318 (19.3) | |
| Discharged home | 926 (80.8) | 4,646 (67.9) | |
| Left against medical advice | 40 (3.5) | 136 (2.0) | |
Weekday Versus Weekend Discharge
Although patients admitted on weekdays and weekends were very similar (data available upon request), patients discharged on weekends (compared to those discharged on weekdays) were younger, more likely to be discharged home without additional support, and had fewer comorbidities (Table 1, Figure 1). Patients discharged on weekends had shorter lengths of stay than those discharged on weekdays (5.6 days vs 7.9 days, P<0.0001). In adjusted linear regression analyses, this 2.3‐day difference remained statistically significant (adjusted P value <0.0001).
Patients discharged on a weekend exhibited lower unadjusted 30‐day rates of death or readmission than those discharged on a weekday (10.6% vs 13.2%), but these differences disappeared after multivariable adjustment that accounted for differences in risk profile (aOR: 0.94, 95% CI: 0.771.16 (Table 2). Results were similar in sensitivity analyses adjusting for LACE scores without LOS included (aOR: 0.88, 95% CI: 0.711.08) or adjusting for LACE scores using expected LOS rather than actual LOS (aOR: 0.90, 95% CI: 0.731.10). Restricting the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater confirmed that weekend and weekday discharges had similar outcomes in the first 30 days after discharge (aOR: 1.09, 95% CI: 0.851.41, Table 2). Similar patterns were seen when we included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge) (Table 2).
| Weekend Discharge, n/N (%) | Weekday Discharge, n/N (%) | Unadjusted P Value | aOR* (95% CI) | Adjusted P Value | |
|---|---|---|---|---|---|
| |||||
| Death/readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 121/1146 (10.6) | 901/6845 (13.2) | 0.01 | 0.94 (0.77‐1.16) | 0.58 |
| All 7 teaching hospitals, but only patients with LACE <10 | 37/647 (5.7) | 225/2753 (8.2) | 0.04 | 0.72 (0.50, 1.03) | 0.07 |
| All 7 teaching hospitals, but only patients with LACE 10 | 84/499 (16.8) | 676/4092 (16.5) | 0.86 | 1.09 (0.85‐1.41) | 0.49 |
| Death/readmission/ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 218/1146 (19.0) | 1445/6845 (21.1) | 0.11 | 0.98 (0.83‐1.15) | 0.79 |
| All 7 teaching hospitals, but only patients with LACE <10 | 90/647 (13.9) | 460/2753 (16.7) | 0.08 | 0.83 (0.64‐1.06) | 0.13 |
| All 7 teaching hospitals, but only patients with LACE 10 | 128/499 (25.7) | 985/4092 (24.1) | 0.44 | 1.12 (0.90‐1.39) | 0.31 |
| Death within 30 days | |||||
| All 7 teaching hospitals, all patients | 24/1146 (2.1) | 215/6845 (3.1) | 0.05 | 0.97 (0.63‐1.51) | 0.89 |
| All 7 teaching hospitals, but only patients with LACE <10 | 4/647 (0.6) | 23/2753 (0.8) | 0.58 | 0.89 (0.30, 2.62) | 0.83 |
| All 7 teaching hospitals, but only patients with LACE 10 | 20/499 (4.0) | 192/4092 (4.7) | 0.49 | 0.99 (0.61‐1.61) | 0.98 |
| Readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 105/1146 (9.2) | 751/6845 (11.0) | 0.07 | 0.94 (0.76‐1.17) | 0.59 |
| All 7 teaching hospitals, but only patients with LACE <10 | 33/647 (5.1) | 211/2753 (7.7) | 0.02 | 0.68 (0.46‐0.99) | 0.04 |
| All 7 teaching hospitals, but only patients with LACE 10 | 72/499 (14.4) | 540/4092 (13.2) | 0.44 | 1.14 (0.87‐1.49) | 0.34 |
| ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 182/1146 (15.9) | 1118/6845 (16.3) | 0.70 | 1.00 (0.84‐1.19) | 0.99 |
| All 7 teaching hospitals, but only patients with LACE <10 | 83/647 (12.8) | 412/2753 (15.0) | 0.17 | 0.84 (0.65, 1.09) | 0.20 |
| All 7 teaching hospitals, but only patients with LACE 10 | 99/499 (19.8) | 706/4092 (17.3) | 0.15 | 1.17 (0.92‐1.48) | 0.20 |
DISCUSSION
Our data suggest that patients discharged from the GIM teaching wards we studied on weekends were appropriately triaged, as they did not exhibit a higher risk of adverse events postdischarge. Although patients discharged on weekends tended to be younger and had less comorbidities than those discharged during the week, we adjusted for baseline covariates in analyses, and we did not find an association between weekend discharge and increased postdischarge events even among the subset of patients deemed to be at high risk for postdischarge adverse events (based on high LACE scores). To our knowledge, although we previously examined this issue in patients with a most‐responsible diagnosis of heart failure,[10] examining weekend versus weekday discharges in the full gamut of general medical patients admitted to teaching hospitals has not previously been examined.
In our previous study[10] of over 24,000 heart failure patients discharged over 10 years (up to June 2009, therefore no overlap with any patients in this study), we also found that patients discharged on the weekends were younger, had fewer comorbidities, and shorter lengths of stay. Although postdischarge death/readmission rates were higher for weekend discharged patients in our earlier study (21.1% vs 19.5%, adjusted hazard ratio: 1.15, 95% CI: 1.061.25), it is worth noting that this was almost entirely driven by data from nonteaching hospitals and cardiology wards. Thus, it is important to reiterate that the findings in our current study are for GIM wards in teaching hospitals and may not be generalizable to less‐structured nonteaching settings.
Although we did not study physician decision making, our results suggest that physicians are incorporating discharge day into their discharge decision making. They may be selecting younger patients with less comorbidities for weekend discharges, or they may be delaying the discharges of older patients with more comorbidities for weekday discharges. Either is not surprising given the realities of weekend inpatient care: reduced staffing and frequent cross‐coverage (of physicians, nurses, physiotherapists, pharmacists, and occupational therapists), limited support services (such as laboratory services or diagnostic imaging), and decreased availability of community services (including home care and social support services).[17] For example, in 1 large US heart failure registry, patients discharged on a weekend received less complete discharge instructions than those discharged on weekdays.[11] Given that early follow‐up postdischarge is associated with better outcomes,[18, 19] future studies should also explore whether patterns of patient follow‐up differ after weekend versus weekday discharges.
Although we were able to capture all interactions with the healthcare system in a single payer system with universal access, there are some limitations to our study. First, we used administrative data, which preclude fully adjusting for severity of diagnoses or functional status, although we used proxies such as admission from/discharge to a long‐term care facility.[20, 21] Second, we did not have access to process of care measures such as diagnostic testing or prescribing data, and thus cannot determine whether quality of care or patient adherence differed by the day of the week they were discharged on, although this seems unlikely. Third, although postdischarge follow‐up may be associated with better outcomes,[18, 19] we were unable to adjust for patterns of outpatient follow‐up in this study. Fourth, we acknowledge that death or readmission soon after discharge does not necessarily mean that the quality of care during the preceding hospitalization was suboptimal or that these deaths or readmissions were even potentially preventable. Many factors influence postdischarge mortality and/or readmission, and quality of inpatient care is only one.[22, 23, 24, 25] Fifth, although some may express concern that LOS may be a mediator in the causal pathway between discharge decision and postdischarge events, and that adjusting for LOS in analyses could thus spuriously obscure a true association, it is worth pointing out that our 2 sensitivity analyses to explore this (the 1 in which we excluded LOS from the analyses and the 1 in which we included expected LOS rather than the actual LOS) revealed nearly identical point estimates and 95% CI as our main analysis. Finally, as our study is observational, we cannot definitively conclude causality, nor can we exclude an 18% excess risk for patients discharged on weekends (or a 22% lower risk either), given our 95% CI for postdischarge adverse outcomes.
CONCLUSION
We found that the proportion of patients discharged on weekends is lower than the proportion admitted on weekends. We also found that lower risk/less severely ill patients appear to be preferentially discharged on weekends, and as a result, postdischarge outcomes are similar between weekend and weekday discharges despite shorter LOS and less availability of outpatient resources for patients discharged on a weekend. The reasons why more complicated patients are not discharged on weekends deserves further study, as safely increasing weekend discharge rates would improve efficiency and safety (by reducing unnecessary exposure to in‐hospital adverse events such as falls, unnecessary urinary catheterizations, and healthcare‐acquired infections). Although hospital admission has become a 24/7 business, we believe that hospital discharge processes should strive for the same level of efficiency.
ACKNOWLEDGMENTS
Disclosures: This study is based in part on data provided by Alberta Health. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the government of Alberta. Neither the government of Alberta nor Alberta Health express any opinion in relation to this study. F.A.M. and S.R.M. are supported by salary awards from Alberta Innovates‐Health Solutions (AIHS). F.A.M. holds the Capital Health Chair in Cardiology Outcomes Research. S.R.M. holds the Endowed Chair in Patient Health Management. This project was funded by AIHS through an investigator‐initiated peer reviewed operating grant. The funding agencies did not have input into study design, data collection, interpretation of results, or write up/approval for submission. The authors report no conflicts of interest.
Hospitals typically reduce staffing levels and the availability of diagnostic, laboratory, and treatment services on weekends, and patients admitted on weekends exhibit poorer in‐hospital outcomes for several medical conditions.[1, 2, 3, 4, 5, 6, 7, 8, 9] Whether or not patients discharged on weekends have worse clinical outcomes has been less well studied.[10, 11, 12] Discharge rates on Saturday and Sunday are lower than for the other 5 days of the week,[12] but bed shortages and hospital overcrowding have increased the demand for maximizing 24/7 week‐round discharge efficiency. Given that the number of patients discharged on weekends is likely to continue to increase, it is important to assess the risk of weekend discharge on outcomes monitored as performance indicators by organizations such as the Centers for Medicare and Medicaid Services, the American Medical Association Physicians Consortium for Performance Improvement, the National Quality Forum, and the Joint Commission.
Thus, we designed this study to evaluate baseline characteristics, length of stay (LOS), and postdischarge outcomes for general internal medicine (GIM) patients in teaching hospitals discharged on weekends compared to weekdays. Our objective was to determine whether postdischarge outcomes differed for patients discharged on weekends versus weekdays.
METHODS
Study Setting
The Canadian province of Alberta has a single vertically integrated healthcare system that is government‐funded and provides universal access to hospitals, emergency departments (EDs), and outpatient physician services for all 4.1 million Albertans as well as all prescription medications for the poor, socially disadvantaged, disabled, or those age 65 years and older. This study received approval from the University of Alberta Health Research Ethics Board with waiver of informed consent.
Data Sources
This study used deidentified linked data from 3 Alberta Health administrative databases that capture vital status and all hospital or ED visits and have previously been shown to have high accuracy for medical diagnoses.[13] The Alberta Health Care Insurance Plan Registry tracks date of death or emigration from the province. The Discharge Abstract Database includes the most responsible diagnosis identified by the hospital attending physician, up to 25 other diagnoses coded by nosologists in each hospital, the admission and discharge dates, and the admission category (elective or urgent/emergent) for all acute care hospitalizations. Of note, unlike US studies, the hospital databases are able to distinguish in‐hospital (eg, adverse events) versus premorbid diagnoses (eg, preexisting comorbidities). The Ambulatory Care Database captures all patient visits to EDs with coding for up to 10 conditions per encounter.
Study Cohort
We identified all adults with an acute care hospitalization on the GIM services at all 7 Alberta teaching hospitals (ie, defined as those with Royal College of Physicians and Surgeons of Canadaapproved residency training programs in internal medicine, the equivalent of the Association of American Medical Colleges certification in the United States) between October 1, 2009 and September 30, 2010 and between April 1, 2011 and December 1, 2011 (these 20 months covered most of the pre/post intervals for a recently reported quality improvement initiative at 1 of the teaching hospitals that had no significant impact on postdischarge outcomes).[14] Patients from out of the province or transferred from/to another inpatient service (eg, the intensive care unit, a different service in the same hospital [such as surgery], another acute care hospital, or rehabilitation hospital) or with lengths of stay greater than 30 days were excluded. We only included the first hospitalization for any patient in our study timeframe and thus excluded repeat discharges of the same patient.
Explanatory Variable of Interest
The independent variable of interest was calendar day of discharge, stratified according to weekday (Monday thru Friday) versus weekend (Saturday and Sunday). Only 1.4% of weekday discharges occurred on a statutory holiday, and for the purposes of this study, these discharges were also considered weekend discharges. At the 7 teaching hospitals in Alberta, nursing staffing ratios do not differ between weekend and weekday, but availability of all other members of the healthcare team does. Physician census decreases from 4 to 5 per ward to 1 to 2, and ward‐based social workers, occupational therapists, physiotherapists, and pharmacist educators are generally not available on weekends.
Outcomes
Our primary outcome of interest was the composite outcome of death or all‐cause nonelective readmission within 30 days of discharge (ie, not including in‐hospital events prior to discharge or elective readmissions after discharge for planned procedures such as chemotherapy); hereafter we refer to this as death or readmission. This is a patient‐relevant outcome that is highlighted in the Affordable Care Act and for which there are several validated risk adjustment models.[15] We chose a composite outcome to deal with the issue of competing risks; if weekend discharges were more likely to die then we could observe a spurious association between weekend discharge and reduced readmissions if we focused on only that outcome.
Other Measures
Comorbidities for each patient were identified using International Classification of Diseases, Ninth Revision and Tenth Revision codes from the Discharge Abstract Database for the index hospitalization and any hospitalizations in the 12 months prior to their index admission, a method previously validated in Alberta databases.[13] We also recorded health resource use during their index hospitalization and calculated each patient's LACE score at the time of discharge, which is an index for predicting unplanned readmission or early death postdischarge previously validated in Canadian administrative databases.[15] The LACE index includes length of hospital stay (L), acuity of admission (A, based on the admission category variable described earlier), comorbidity burden quantified using the Charlson Comorbidity Index (C), and emergency department visits in the 6 months prior to admission (E); patients with discharge LACE scores >10 (total possible score is 19) are defined as being at high risk of death/readmission within 30 days.[16] As detailed below, to deal with potential concerns that LOS may be a mediator in the causal pathway, we ran 2 sensitivity analyses, 1 in which we excluded LOS from the analyses and 1 in which we included expected LOS rather than the actual LOS. Expected LOS is a data‐driven estimate based on the most current 2 years of patient LOS information available in the Canadian Institute for Health Information discharge abstract database (
Statistical Analysis
Baseline patient characteristics between weekend and weekday discharges were compared with t tests for continuous variables and [2] tests for binary or categorical variables. Logistic regression was used for comparison of death or readmission for weekend versus weekday discharges. Multivariable models were adjusted for age, sex, hospital, and LACE scores (as a continuous variable) at time of discharge; in sensitivity analyses we adjusted for (1) LACE score without including LOS and (2) LACE score using expected LOS rather than actual LOS. In further sensitivity analyses we (1) restricted the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater and (2) included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge). Day of admission (weekend vs weekday) was also considered for the multivariable models, but was not found to be significant and thus was omitted from final models. We do not have any physician identifying variables in our dataset and thus could not investigate the potential correlation among patients discharged by the same physician. We did explore the hospital intraclass correlation coefficient, and as it was very small (0.001), we did not utilize models to account for the hierarchical nature of the data, but did include hospital as a fixed effect in the logistic models. The results were virtually identical whether we did or did not include hospital in the models. Adjusted odds ratios (aORs) are displayed with 95% confidence intervals (CI) and P values. Average LOS was calculated for weekend and weekday discharges with 95% CIs. P values for adjusted length of stay were calculated using multivariable linear regression adjusting for age, sex, day of admission, and Charlson score. All statistical analyses were done using SAS for Windows version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Patient Characteristics
Of the 7991 patients discharged during our study interval, 1146 (14.3%) were discharged on weekend or holiday days (Table 1). In contrast, 2180 of our cohort were admitted on a weekend (27.3%). The mean age of our study population was 62.1 years, 51.9% were men, mean Charlson score was 2.56, and 4591 (57.5%) had LACE scores of at least 10 at discharge.
| Characteristic | Weekend Discharge | Weekday Discharge | P Value |
|---|---|---|---|
| |||
| No. of patients | 1,146 | 6,845 | |
| Age, y, mean (SD) | 57.97 (19.70) | 62.77 (19.37) | <0.0001 |
| Male | 601 (52.4) | 3,548 (51.8) | 0.70 |
| Top 5 most responsible diagnoses | |||
| COPD | 74 (6.5) | 507 (7.4) | |
| Pneumonia | 64 (5.6) | 326 (4.8) | |
| Heart failure | 31 (2.7) | 375 (5.5) | |
| Urinary tract infection | 39 (3.4) | 254 (3.7) | |
| Venous thromboembolism | 31 (2.7) | 259 (3.8) | |
| Charlson score, mean (SD) | 2.17 (3.29) | 2.63 (3.30) | <0.0001 |
| Comorbidities (based on index hospitalization and prior 12 months) | |||
| Hypertension | 485 (42.3) | 3,265 (47.7) | 0.00 |
| Diabetes mellitus | 326 (28.4) | 2,106 (30.8) | 0.11 |
| Fluid imbalance | 332 (29.0) | 1,969 (28.8) | 0.89 |
| COPD | 255 (22.3) | 1,790 (26.2) | 0.01 |
| Psychiatric disorder | 179 (15.6) | 1,459 (21.3) | <0.0001 |
| Pneumonia | 242 (21.1) | 1,427 (20.8) | 0.84 |
| Anemia | 167 (14.6) | 1,233 (18.0) | 0.00 |
| Trauma | 169 (14.7) | 1,209 (17.7) | 0.02 |
| Atrial fibrillation | 141 (12.3) | 1,069 (15.6) | 0.00 |
| Heart failure | 101 (8.8) | 946 (13.8) | <0.0001 |
| Drug abuse | 188 (16.4) | 966 (14.1) | 0.04 |
| Cancer | 124 (10.8) | 867 (12.7) | 0.08 |
| Renal disease | 93 (8.1) | 689 (10.1) | 0.04 |
| Dementia | 49 (4.3) | 564 (8.2) | <0.0001 |
| Mild liver disease | 99 (8.6) | 587 (8.6) | 0.94 |
| Cerebrovascular disease | 59 (5.1) | 492 (7.2) | 0.01 |
| Gastrointestinal bleed | 84 (7.3) | 496 (7.2) | 0.92 |
| Asthma | 83 (7.2) | 426 (6.2) | 0.19 |
| Stroke | 42 (3.7) | 332 (4.9) | 0.08 |
| Prior myocardial infarction | 47 (4.1) | 329 (4.8) | 0.30 |
| Arthritis | 42 (3.7) | 309 (4.5) | 0.19 |
| Peripheral vascular disease | 42 (3.7) | 259 (3.8) | 0.84 |
| Severe liver disease | 44 (3.8) | 261 (3.8) | 0.97 |
| Valve disease | 24 (2.1) | 188 (2.7) | 0.20 |
| Paralysis | 31 (2.7) | 201 (2.9) | 0.67 |
| Skin ulcer | 17 (1.5) | 137 (2.0) | 0.24 |
| Shock | 19 (1.7) | 99 (1.4) | 0.58 |
| HIV | 15 (1.3) | 109 (1.6) | 0.47 |
| Protein calorie malnutrition | 0 (0.0) | 9 (0.1) | 0.21 |
| Features of index hospitalization | |||
| Resource intensity weight, mean (SD) | 1.10 (0.82) | 1.38 (1.24) | <0.0001 |
| LACE score, mean (SD) | 9.45 (2.85) | 10.51 (3.03) | <0.0001 |
| Expected LOS, mean (SD) | 6.20 (4.08) | 7.12 (4.89) | <0.0001 |
| Acute LOS, mean (SD) | 5.64 (4.99) | 7.86 (6.13) | <0.0001 |
| Weekend admission | 244 (21.3) | 1,936 (28.3) | <0.0001 |
| Discharge disposition | <0.0001 | ||
| Transferred to another inpatient hospital | 14 (1.2) | 189 (2.8) | |
| Transferred to long‐term care facility | 36 (3.1) | 532 (7.8) | |
| Transferred to other (except hospice) | 5 (0.4) | 24 (0.4) | |
| Discharged to home setting with support services | 125 (10.9) | 1,318 (19.3) | |
| Discharged home | 926 (80.8) | 4,646 (67.9) | |
| Left against medical advice | 40 (3.5) | 136 (2.0) | |
Weekday Versus Weekend Discharge
Although patients admitted on weekdays and weekends were very similar (data available upon request), patients discharged on weekends (compared to those discharged on weekdays) were younger, more likely to be discharged home without additional support, and had fewer comorbidities (Table 1, Figure 1). Patients discharged on weekends had shorter lengths of stay than those discharged on weekdays (5.6 days vs 7.9 days, P<0.0001). In adjusted linear regression analyses, this 2.3‐day difference remained statistically significant (adjusted P value <0.0001).
Patients discharged on a weekend exhibited lower unadjusted 30‐day rates of death or readmission than those discharged on a weekday (10.6% vs 13.2%), but these differences disappeared after multivariable adjustment that accounted for differences in risk profile (aOR: 0.94, 95% CI: 0.771.16 (Table 2). Results were similar in sensitivity analyses adjusting for LACE scores without LOS included (aOR: 0.88, 95% CI: 0.711.08) or adjusting for LACE scores using expected LOS rather than actual LOS (aOR: 0.90, 95% CI: 0.731.10). Restricting the analysis to only those patients deemed to be at high risk for events due to LACE scores of 10 or greater confirmed that weekend and weekday discharges had similar outcomes in the first 30 days after discharge (aOR: 1.09, 95% CI: 0.851.41, Table 2). Similar patterns were seen when we included ED visits as part of the composite endpoint (ie, death, unplanned readmission, or unplanned ED visit within 30 days of discharge) (Table 2).
| Weekend Discharge, n/N (%) | Weekday Discharge, n/N (%) | Unadjusted P Value | aOR* (95% CI) | Adjusted P Value | |
|---|---|---|---|---|---|
| |||||
| Death/readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 121/1146 (10.6) | 901/6845 (13.2) | 0.01 | 0.94 (0.77‐1.16) | 0.58 |
| All 7 teaching hospitals, but only patients with LACE <10 | 37/647 (5.7) | 225/2753 (8.2) | 0.04 | 0.72 (0.50, 1.03) | 0.07 |
| All 7 teaching hospitals, but only patients with LACE 10 | 84/499 (16.8) | 676/4092 (16.5) | 0.86 | 1.09 (0.85‐1.41) | 0.49 |
| Death/readmission/ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 218/1146 (19.0) | 1445/6845 (21.1) | 0.11 | 0.98 (0.83‐1.15) | 0.79 |
| All 7 teaching hospitals, but only patients with LACE <10 | 90/647 (13.9) | 460/2753 (16.7) | 0.08 | 0.83 (0.64‐1.06) | 0.13 |
| All 7 teaching hospitals, but only patients with LACE 10 | 128/499 (25.7) | 985/4092 (24.1) | 0.44 | 1.12 (0.90‐1.39) | 0.31 |
| Death within 30 days | |||||
| All 7 teaching hospitals, all patients | 24/1146 (2.1) | 215/6845 (3.1) | 0.05 | 0.97 (0.63‐1.51) | 0.89 |
| All 7 teaching hospitals, but only patients with LACE <10 | 4/647 (0.6) | 23/2753 (0.8) | 0.58 | 0.89 (0.30, 2.62) | 0.83 |
| All 7 teaching hospitals, but only patients with LACE 10 | 20/499 (4.0) | 192/4092 (4.7) | 0.49 | 0.99 (0.61‐1.61) | 0.98 |
| Readmission within 30 days | |||||
| All 7 teaching hospitals, all patients | 105/1146 (9.2) | 751/6845 (11.0) | 0.07 | 0.94 (0.76‐1.17) | 0.59 |
| All 7 teaching hospitals, but only patients with LACE <10 | 33/647 (5.1) | 211/2753 (7.7) | 0.02 | 0.68 (0.46‐0.99) | 0.04 |
| All 7 teaching hospitals, but only patients with LACE 10 | 72/499 (14.4) | 540/4092 (13.2) | 0.44 | 1.14 (0.87‐1.49) | 0.34 |
| ED visit within 30 days | |||||
| All 7 teaching hospitals, all patients | 182/1146 (15.9) | 1118/6845 (16.3) | 0.70 | 1.00 (0.84‐1.19) | 0.99 |
| All 7 teaching hospitals, but only patients with LACE <10 | 83/647 (12.8) | 412/2753 (15.0) | 0.17 | 0.84 (0.65, 1.09) | 0.20 |
| All 7 teaching hospitals, but only patients with LACE 10 | 99/499 (19.8) | 706/4092 (17.3) | 0.15 | 1.17 (0.92‐1.48) | 0.20 |
DISCUSSION
Our data suggest that patients discharged from the GIM teaching wards we studied on weekends were appropriately triaged, as they did not exhibit a higher risk of adverse events postdischarge. Although patients discharged on weekends tended to be younger and had less comorbidities than those discharged during the week, we adjusted for baseline covariates in analyses, and we did not find an association between weekend discharge and increased postdischarge events even among the subset of patients deemed to be at high risk for postdischarge adverse events (based on high LACE scores). To our knowledge, although we previously examined this issue in patients with a most‐responsible diagnosis of heart failure,[10] examining weekend versus weekday discharges in the full gamut of general medical patients admitted to teaching hospitals has not previously been examined.
In our previous study[10] of over 24,000 heart failure patients discharged over 10 years (up to June 2009, therefore no overlap with any patients in this study), we also found that patients discharged on the weekends were younger, had fewer comorbidities, and shorter lengths of stay. Although postdischarge death/readmission rates were higher for weekend discharged patients in our earlier study (21.1% vs 19.5%, adjusted hazard ratio: 1.15, 95% CI: 1.061.25), it is worth noting that this was almost entirely driven by data from nonteaching hospitals and cardiology wards. Thus, it is important to reiterate that the findings in our current study are for GIM wards in teaching hospitals and may not be generalizable to less‐structured nonteaching settings.
Although we did not study physician decision making, our results suggest that physicians are incorporating discharge day into their discharge decision making. They may be selecting younger patients with less comorbidities for weekend discharges, or they may be delaying the discharges of older patients with more comorbidities for weekday discharges. Either is not surprising given the realities of weekend inpatient care: reduced staffing and frequent cross‐coverage (of physicians, nurses, physiotherapists, pharmacists, and occupational therapists), limited support services (such as laboratory services or diagnostic imaging), and decreased availability of community services (including home care and social support services).[17] For example, in 1 large US heart failure registry, patients discharged on a weekend received less complete discharge instructions than those discharged on weekdays.[11] Given that early follow‐up postdischarge is associated with better outcomes,[18, 19] future studies should also explore whether patterns of patient follow‐up differ after weekend versus weekday discharges.
Although we were able to capture all interactions with the healthcare system in a single payer system with universal access, there are some limitations to our study. First, we used administrative data, which preclude fully adjusting for severity of diagnoses or functional status, although we used proxies such as admission from/discharge to a long‐term care facility.[20, 21] Second, we did not have access to process of care measures such as diagnostic testing or prescribing data, and thus cannot determine whether quality of care or patient adherence differed by the day of the week they were discharged on, although this seems unlikely. Third, although postdischarge follow‐up may be associated with better outcomes,[18, 19] we were unable to adjust for patterns of outpatient follow‐up in this study. Fourth, we acknowledge that death or readmission soon after discharge does not necessarily mean that the quality of care during the preceding hospitalization was suboptimal or that these deaths or readmissions were even potentially preventable. Many factors influence postdischarge mortality and/or readmission, and quality of inpatient care is only one.[22, 23, 24, 25] Fifth, although some may express concern that LOS may be a mediator in the causal pathway between discharge decision and postdischarge events, and that adjusting for LOS in analyses could thus spuriously obscure a true association, it is worth pointing out that our 2 sensitivity analyses to explore this (the 1 in which we excluded LOS from the analyses and the 1 in which we included expected LOS rather than the actual LOS) revealed nearly identical point estimates and 95% CI as our main analysis. Finally, as our study is observational, we cannot definitively conclude causality, nor can we exclude an 18% excess risk for patients discharged on weekends (or a 22% lower risk either), given our 95% CI for postdischarge adverse outcomes.
CONCLUSION
We found that the proportion of patients discharged on weekends is lower than the proportion admitted on weekends. We also found that lower risk/less severely ill patients appear to be preferentially discharged on weekends, and as a result, postdischarge outcomes are similar between weekend and weekday discharges despite shorter LOS and less availability of outpatient resources for patients discharged on a weekend. The reasons why more complicated patients are not discharged on weekends deserves further study, as safely increasing weekend discharge rates would improve efficiency and safety (by reducing unnecessary exposure to in‐hospital adverse events such as falls, unnecessary urinary catheterizations, and healthcare‐acquired infections). Although hospital admission has become a 24/7 business, we believe that hospital discharge processes should strive for the same level of efficiency.
ACKNOWLEDGMENTS
Disclosures: This study is based in part on data provided by Alberta Health. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the government of Alberta. Neither the government of Alberta nor Alberta Health express any opinion in relation to this study. F.A.M. and S.R.M. are supported by salary awards from Alberta Innovates‐Health Solutions (AIHS). F.A.M. holds the Capital Health Chair in Cardiology Outcomes Research. S.R.M. holds the Endowed Chair in Patient Health Management. This project was funded by AIHS through an investigator‐initiated peer reviewed operating grant. The funding agencies did not have input into study design, data collection, interpretation of results, or write up/approval for submission. The authors report no conflicts of interest.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668.
- , , , et al. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294:803–812.
- , . Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117:175–181.
- . Do hospitals provide lower quality care on weekends? Health Serv Res. 2007;42:1589–1612.
- , , , et al. Day of admission and clinical outcomes for patients hospitalized for heart failure: findings from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE‐HF). Circ Heart Fail. 2008;1:50–57.
- , , , et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med. 2012;105:74–84.
- , , , . Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211–1215.
- , , , . Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530–539.
- , , , . Effects of weekend admission and hospital teaching status on in‐hospital mortality. Am J Med. 2004;117:151–157.
- , , , , . Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail. 2013;6:922–929.
- , , , et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158:451–458.
- , . Risk of death or readmission among people discharged from hospital on Fridays. CMAJ. 2002;166:1672–1673.
- , , , , et al.; IMECCHI Investigators. Assessing validity of ICD‐9‐CM and ICD‐10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441.
- , , , et al. Safely and effectively reducing inpatient length of stay: a controlled study of the General Internal Medicine Care Transformation Initiative. BMJ Qual Saf. 2014;23:446–456.
- , , , et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- , . Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011;26:1050–1052.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , , , , . Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185:e681–e689.
- , , , , , . Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research. Ann Intern Med. 1993;119:844–850.
- , , , . Predictions of hospital mortality rates: a comparison of data sources. Ann Intern Med. 1997;126:347–354.
- , , , et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282.
- , . Investigating early readmission as an indicator for quality of care studies. Med Care. 1991;29(4):377–394.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , . Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668.
- , , , et al. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294:803–812.
- , . Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117:175–181.
- . Do hospitals provide lower quality care on weekends? Health Serv Res. 2007;42:1589–1612.
- , , , et al. Day of admission and clinical outcomes for patients hospitalized for heart failure: findings from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE‐HF). Circ Heart Fail. 2008;1:50–57.
- , , , et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med. 2012;105:74–84.
- , , , . Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211–1215.
- , , , . Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40:530–539.
- , , , . Effects of weekend admission and hospital teaching status on in‐hospital mortality. Am J Med. 2004;117:151–157.
- , , , , . Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail. 2013;6:922–929.
- , , , et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158:451–458.
- , . Risk of death or readmission among people discharged from hospital on Fridays. CMAJ. 2002;166:1672–1673.
- , , , , et al.; IMECCHI Investigators. Assessing validity of ICD‐9‐CM and ICD‐10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441.
- , , , et al. Safely and effectively reducing inpatient length of stay: a controlled study of the General Internal Medicine Care Transformation Initiative. BMJ Qual Saf. 2014;23:446–456.
- , , , et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- , . Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011;26:1050–1052.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , , , , . Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185:e681–e689.
- , , , , , . Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research. Ann Intern Med. 1993;119:844–850.
- , , , . Predictions of hospital mortality rates: a comparison of data sources. Ann Intern Med. 1997;126:347–354.
- , , , et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282.
- , . Investigating early readmission as an indicator for quality of care studies. Med Care. 1991;29(4):377–394.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , . Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402.
© 2014 Society of Hospital Medicine