User login
Erik Greb joined the staff of Neurology Reviews in January 2012. Since then, he has attended scientific conferences, conducted video interviews, and written about clinical research in multiple sclerosis, epilepsy, Parkinson's disease, Alzheimer's disease, stroke, and other neurologic disorders. In addition to news articles, Erik has written investigative stories about multiple sclerosis, headache, and epilepsy. He previously wrote about pharmaceutical manufacturing, drug formulation and delivery, quality assurance, and regulation for Pharmaceutical Technology.
Which patients are most likely to have a positive RNS test for myasthenia gravis?
AUSTIN, TEX. – , according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Low-frequency RNS is a common test that neurologists perform to evaluate a patient for myasthenia gravis. The effects of various clinical factors on the diagnostic yield of this test are unknown, however.
Myasthenia gravis is “mostly a clinical diagnosis,” study first author Tingting Hua, a medical student at the University of Missouri in Columbia, said in an interview. “RNS is just one of the helpful diagnostic tests for it. If we can find out in what kind of populations of patients this test is more helpful, maybe that would help cut down unnecessary tests in patients for whom it’s not necessarily helpful.”
Ms. Hua and her colleagues conducted research to assess the effects of clinical, serologic, and demographic factors on the diagnostic yield of RNS. They retrospectively analyzed patients with an established diagnosis of myasthenia gravis and at least 1 year of follow-up. The variables that the investigators examined were demographic characteristics, MGFA class, RNS study results, antibody test results, thymoma status, and treatments received.
Ms. Hua and her colleagues included 65 patients in their analysis. Thirty-one patients were female. Fifty-five patients were white, eight were black, and two were categorized as “unknown.” Of this population, 32 patients (49.2%) were in MGFA Class I, 14 (21.5%) were in MGFA Class IIa, 13 (20.0%) were in MGFA Class IIb, and the remaining 6 (9.2%) were in MGFA Classes IIIa through V. Twenty-seven patients (42%) had positive RNS studies. Twenty-one patients (32%) were seropositive for myasthenia gravis antibodies.
Eleven patients underwent RNS in an inpatient setting, and 54 were tested in an outpatient setting. Acetylcholine receptor (AChR) binding antibody titer ranged from 0.12 nmol/L to 118 nmol/L. The RNS results were significantly more likely to be positive for seropositive patients, compared with seronegative patients. Patients with MGFA Class III or higher also had higher likelihood of positive RNS results, compared with patients in lower classes. Finally, the diagnostic yield was highest for patients with MGFA Class III or higher who were tested in an inpatient setting.
The study was supported by a Missouri School of Medicine Summer Research Fellowship.
SOURCE: Hua T et al. AANEM 2019, Abstract 9.
AUSTIN, TEX. – , according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Low-frequency RNS is a common test that neurologists perform to evaluate a patient for myasthenia gravis. The effects of various clinical factors on the diagnostic yield of this test are unknown, however.
Myasthenia gravis is “mostly a clinical diagnosis,” study first author Tingting Hua, a medical student at the University of Missouri in Columbia, said in an interview. “RNS is just one of the helpful diagnostic tests for it. If we can find out in what kind of populations of patients this test is more helpful, maybe that would help cut down unnecessary tests in patients for whom it’s not necessarily helpful.”
Ms. Hua and her colleagues conducted research to assess the effects of clinical, serologic, and demographic factors on the diagnostic yield of RNS. They retrospectively analyzed patients with an established diagnosis of myasthenia gravis and at least 1 year of follow-up. The variables that the investigators examined were demographic characteristics, MGFA class, RNS study results, antibody test results, thymoma status, and treatments received.
Ms. Hua and her colleagues included 65 patients in their analysis. Thirty-one patients were female. Fifty-five patients were white, eight were black, and two were categorized as “unknown.” Of this population, 32 patients (49.2%) were in MGFA Class I, 14 (21.5%) were in MGFA Class IIa, 13 (20.0%) were in MGFA Class IIb, and the remaining 6 (9.2%) were in MGFA Classes IIIa through V. Twenty-seven patients (42%) had positive RNS studies. Twenty-one patients (32%) were seropositive for myasthenia gravis antibodies.
Eleven patients underwent RNS in an inpatient setting, and 54 were tested in an outpatient setting. Acetylcholine receptor (AChR) binding antibody titer ranged from 0.12 nmol/L to 118 nmol/L. The RNS results were significantly more likely to be positive for seropositive patients, compared with seronegative patients. Patients with MGFA Class III or higher also had higher likelihood of positive RNS results, compared with patients in lower classes. Finally, the diagnostic yield was highest for patients with MGFA Class III or higher who were tested in an inpatient setting.
The study was supported by a Missouri School of Medicine Summer Research Fellowship.
SOURCE: Hua T et al. AANEM 2019, Abstract 9.
AUSTIN, TEX. – , according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Low-frequency RNS is a common test that neurologists perform to evaluate a patient for myasthenia gravis. The effects of various clinical factors on the diagnostic yield of this test are unknown, however.
Myasthenia gravis is “mostly a clinical diagnosis,” study first author Tingting Hua, a medical student at the University of Missouri in Columbia, said in an interview. “RNS is just one of the helpful diagnostic tests for it. If we can find out in what kind of populations of patients this test is more helpful, maybe that would help cut down unnecessary tests in patients for whom it’s not necessarily helpful.”
Ms. Hua and her colleagues conducted research to assess the effects of clinical, serologic, and demographic factors on the diagnostic yield of RNS. They retrospectively analyzed patients with an established diagnosis of myasthenia gravis and at least 1 year of follow-up. The variables that the investigators examined were demographic characteristics, MGFA class, RNS study results, antibody test results, thymoma status, and treatments received.
Ms. Hua and her colleagues included 65 patients in their analysis. Thirty-one patients were female. Fifty-five patients were white, eight were black, and two were categorized as “unknown.” Of this population, 32 patients (49.2%) were in MGFA Class I, 14 (21.5%) were in MGFA Class IIa, 13 (20.0%) were in MGFA Class IIb, and the remaining 6 (9.2%) were in MGFA Classes IIIa through V. Twenty-seven patients (42%) had positive RNS studies. Twenty-one patients (32%) were seropositive for myasthenia gravis antibodies.
Eleven patients underwent RNS in an inpatient setting, and 54 were tested in an outpatient setting. Acetylcholine receptor (AChR) binding antibody titer ranged from 0.12 nmol/L to 118 nmol/L. The RNS results were significantly more likely to be positive for seropositive patients, compared with seronegative patients. Patients with MGFA Class III or higher also had higher likelihood of positive RNS results, compared with patients in lower classes. Finally, the diagnostic yield was highest for patients with MGFA Class III or higher who were tested in an inpatient setting.
The study was supported by a Missouri School of Medicine Summer Research Fellowship.
SOURCE: Hua T et al. AANEM 2019, Abstract 9.
REPORTING FROM AANEM 2019
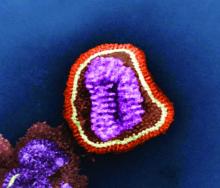
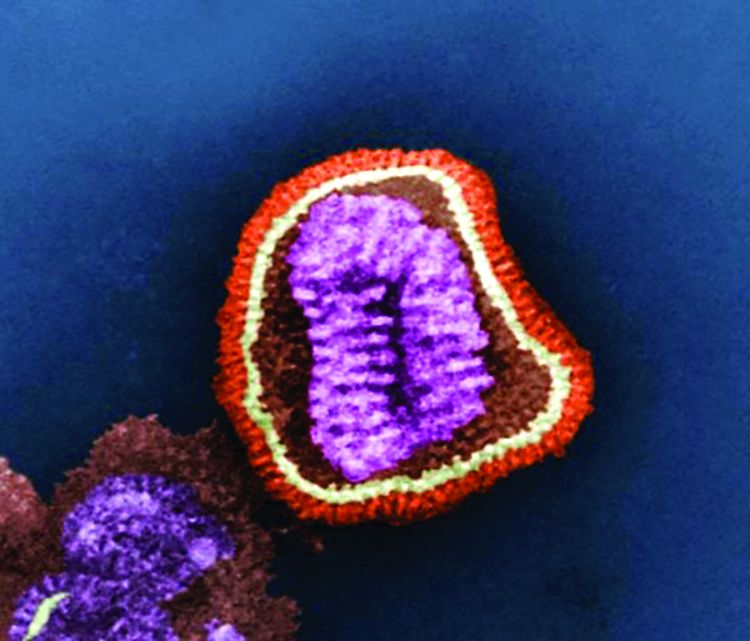
Neurologists consider flu shot safe in most patients with autoimmune neuromuscular disorders
AUSTIN, TEX. – (CIDP), according to a survey presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine. They are more conservative in recommending immunization for patients with a history of Guillain-Barré syndrome, however. Temporally associated disease relapses may be a risk factor for relapse with subsequent immunization, according to the investigators.
Influenza vaccination of patients with autoimmune neuromuscular disorders such as myasthenia gravis, CIDP, or Guillain-Barré syndrome is controversial, and no clear guideline helps clinicians to decide whether vaccination for such patients is appropriate. Tess Litchman, a medical student at Yale University, New Haven, Conn., and colleagues conducted a web-based survey of neurologists throughout the United States to examine current practices for recommending influenza vaccination for patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome.
The researchers received 184 survey responses, with the highest proportions of responses coming from California (8.8%), Connecticut (8.8%), and Texas (8.3%). On average, respondents had been in practice for 15.5 years. Their reported practice specialties were neuromuscular medicine in 50%, general neurology in 20%, mixed specialties in 20%, and other in 10%.
Across practice settings, neurologists followed 6,448 patients with myasthenia gravis, 2,310 patients with CIDP, and 1,907 patients with Guillain-Barré syndrome. Approximately 83% of respondents reported recommending influenza vaccination for all of their patients with myasthenia gravis, 59% reported recommending vaccination for all of their patients with CIDP, and 43% of respondents reported recommending vaccination for all of their patients with Guillain-Barré syndrome. About 2%, 8%, and 15% of respondents reported that they do not recommend influenza vaccination for any of their patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome, respectively.
A temporal association between disease relapse and influenza vaccination was reported in 1.5% of patients with myasthenia gravis, 3.7% of patients with CIDP, and 8.7% of patients with Guillain-Barré syndrome. Recurrent relapses occurred in 87% (26 of 30) of patients with myasthenia gravis, 92% (23 of 25) of patients with CIDP, and 74% (26 of 35) of patients with Guillain-Barré syndrome who received another influenza vaccination.
“According to existing guidelines per the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices, all patients with myasthenia gravis and CIDP should be vaccinated, and patients with Guillain-Barré syndrome who did not develop the syndrome due to a flu shot should be vaccinated,” said Richard J. Nowak, MD, director of the program in clinical and translational neuromuscular research at Yale and one of the senior investigators on the study. “This survey demonstrates that clearer guidelines and education from a professional academic neurology society is an unmet need and would be helpful to better inform the neurology community about the possible risks and benefits of immunization in myasthenia gravis, CIDP, and Guillain-Barré syndrome patients. We hope to utilize these initial results to stimulate a larger scale study, and identify whether this topic represents a knowledge gap in the community or an area in which we can improve on the best-practice standard.”
Dr. Nowak had no relevant disclosures. The study was supported by the department of neurology at Yale University; there was no external funding.
SOURCE: Litchman T et al. AANEM 2019, Abstract 16.
AUSTIN, TEX. – (CIDP), according to a survey presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine. They are more conservative in recommending immunization for patients with a history of Guillain-Barré syndrome, however. Temporally associated disease relapses may be a risk factor for relapse with subsequent immunization, according to the investigators.
Influenza vaccination of patients with autoimmune neuromuscular disorders such as myasthenia gravis, CIDP, or Guillain-Barré syndrome is controversial, and no clear guideline helps clinicians to decide whether vaccination for such patients is appropriate. Tess Litchman, a medical student at Yale University, New Haven, Conn., and colleagues conducted a web-based survey of neurologists throughout the United States to examine current practices for recommending influenza vaccination for patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome.
The researchers received 184 survey responses, with the highest proportions of responses coming from California (8.8%), Connecticut (8.8%), and Texas (8.3%). On average, respondents had been in practice for 15.5 years. Their reported practice specialties were neuromuscular medicine in 50%, general neurology in 20%, mixed specialties in 20%, and other in 10%.
Across practice settings, neurologists followed 6,448 patients with myasthenia gravis, 2,310 patients with CIDP, and 1,907 patients with Guillain-Barré syndrome. Approximately 83% of respondents reported recommending influenza vaccination for all of their patients with myasthenia gravis, 59% reported recommending vaccination for all of their patients with CIDP, and 43% of respondents reported recommending vaccination for all of their patients with Guillain-Barré syndrome. About 2%, 8%, and 15% of respondents reported that they do not recommend influenza vaccination for any of their patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome, respectively.
A temporal association between disease relapse and influenza vaccination was reported in 1.5% of patients with myasthenia gravis, 3.7% of patients with CIDP, and 8.7% of patients with Guillain-Barré syndrome. Recurrent relapses occurred in 87% (26 of 30) of patients with myasthenia gravis, 92% (23 of 25) of patients with CIDP, and 74% (26 of 35) of patients with Guillain-Barré syndrome who received another influenza vaccination.
“According to existing guidelines per the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices, all patients with myasthenia gravis and CIDP should be vaccinated, and patients with Guillain-Barré syndrome who did not develop the syndrome due to a flu shot should be vaccinated,” said Richard J. Nowak, MD, director of the program in clinical and translational neuromuscular research at Yale and one of the senior investigators on the study. “This survey demonstrates that clearer guidelines and education from a professional academic neurology society is an unmet need and would be helpful to better inform the neurology community about the possible risks and benefits of immunization in myasthenia gravis, CIDP, and Guillain-Barré syndrome patients. We hope to utilize these initial results to stimulate a larger scale study, and identify whether this topic represents a knowledge gap in the community or an area in which we can improve on the best-practice standard.”
Dr. Nowak had no relevant disclosures. The study was supported by the department of neurology at Yale University; there was no external funding.
SOURCE: Litchman T et al. AANEM 2019, Abstract 16.
AUSTIN, TEX. – (CIDP), according to a survey presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine. They are more conservative in recommending immunization for patients with a history of Guillain-Barré syndrome, however. Temporally associated disease relapses may be a risk factor for relapse with subsequent immunization, according to the investigators.
Influenza vaccination of patients with autoimmune neuromuscular disorders such as myasthenia gravis, CIDP, or Guillain-Barré syndrome is controversial, and no clear guideline helps clinicians to decide whether vaccination for such patients is appropriate. Tess Litchman, a medical student at Yale University, New Haven, Conn., and colleagues conducted a web-based survey of neurologists throughout the United States to examine current practices for recommending influenza vaccination for patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome.
The researchers received 184 survey responses, with the highest proportions of responses coming from California (8.8%), Connecticut (8.8%), and Texas (8.3%). On average, respondents had been in practice for 15.5 years. Their reported practice specialties were neuromuscular medicine in 50%, general neurology in 20%, mixed specialties in 20%, and other in 10%.
Across practice settings, neurologists followed 6,448 patients with myasthenia gravis, 2,310 patients with CIDP, and 1,907 patients with Guillain-Barré syndrome. Approximately 83% of respondents reported recommending influenza vaccination for all of their patients with myasthenia gravis, 59% reported recommending vaccination for all of their patients with CIDP, and 43% of respondents reported recommending vaccination for all of their patients with Guillain-Barré syndrome. About 2%, 8%, and 15% of respondents reported that they do not recommend influenza vaccination for any of their patients with myasthenia gravis, CIDP, and Guillain-Barré syndrome, respectively.
A temporal association between disease relapse and influenza vaccination was reported in 1.5% of patients with myasthenia gravis, 3.7% of patients with CIDP, and 8.7% of patients with Guillain-Barré syndrome. Recurrent relapses occurred in 87% (26 of 30) of patients with myasthenia gravis, 92% (23 of 25) of patients with CIDP, and 74% (26 of 35) of patients with Guillain-Barré syndrome who received another influenza vaccination.
“According to existing guidelines per the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices, all patients with myasthenia gravis and CIDP should be vaccinated, and patients with Guillain-Barré syndrome who did not develop the syndrome due to a flu shot should be vaccinated,” said Richard J. Nowak, MD, director of the program in clinical and translational neuromuscular research at Yale and one of the senior investigators on the study. “This survey demonstrates that clearer guidelines and education from a professional academic neurology society is an unmet need and would be helpful to better inform the neurology community about the possible risks and benefits of immunization in myasthenia gravis, CIDP, and Guillain-Barré syndrome patients. We hope to utilize these initial results to stimulate a larger scale study, and identify whether this topic represents a knowledge gap in the community or an area in which we can improve on the best-practice standard.”
Dr. Nowak had no relevant disclosures. The study was supported by the department of neurology at Yale University; there was no external funding.
SOURCE: Litchman T et al. AANEM 2019, Abstract 16.
REPORTING FROM AANEM 2019
Late response to eculizumab may occur in minority of myasthenia gravis patients
AUSTIN – according to a secondary analysis presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Evidence for the sustained effectiveness of eculizumab, a terminal complement inhibitor, in adult patients with antiacetylcholine receptor antibody-positive refractory generalized myasthenia gravis was provided by the 6-month, double-blind, placebo-controlled REGAIN study and its open-label extension. James F. Howard Jr., MD, distinguished professor of neuromuscular disease at the University of North Carolina in Chapel Hill and colleagues sought to analyze response profiles in REGAIN and its open-label extension.
The findings raise the possibility that complement inhibition with eculizumab should not be abandoned rapidly. “We accept that [eculizumab] works quickly,” Dr. Howard said. “There is an impression that if you don’t respond within the first 3 months, you’re not going to respond. I think these data would suggest otherwise.”
The investigators analyzed participants’ Myasthenia Gravis–Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) scores, which had been recorded throughout REGAIN and the extension. They defined early and late responses as improvement in MG-ADL score (i.e., a decrease of three or more points) or QMG score (i.e., a decrease of five or more points) occurring at 12 weeks or earlier or after 12 weeks, respectively, after initiation of eculizumab therapy. Patients randomized to eculizumab in REGAIN initially were treated with an IV induction dose of 900 mg/week before receiving 1,200 mg every 2 weeks thereafter.
Dr. Howard and colleagues included 98 patients in their analysis. Approximately 32% of patients achieved their first response within the first week of treatment, and 15% responded at week 2. About 16% of patients had a late response.
Responses to treatment on the MG-ADL scale had occurred in 67.3% by week 12 and in 84.7% by the end of the extension. Treatment with eculizumab resulted in QMG responses in 56.1% by week 12 and 71.4% by the end of the extension. The investigators observed response over multiple consecutive assessments for the vast majority of patients.
At week 130, the least-squares mean percentage changes from baseline in MG-ADL score were −61.9% and −47.5% in early and late MG-ADL responders, respectively. The least-squares mean percentage changes from baseline in QMG score were −40.8% and −55.5% in early and late QMG responders, respectively.
The investigators observed significant baseline differences between early versus late QMG responders in mean duration of myasthenia gravis (10.46 years vs. 5.46 years) and mean QMG score (18.6 vs. 15.1).
“I can’t explain [this finding]. It may simply be due to the low numbers of patients,” Dr. Howard said. “Whether this is going to hold up in postmarketing analysis remains to be seen. I’m not convinced that that is meaningful.”
Study funding was provided by Alexion Pharmaceuticals (the developer of eculizumab), the Centers for Disease Control and Prevention, and the National Institutes of Health. Dr. Howard reported receiving research support and consulting fees or honoraria from Alexion and several other pharmaceutical companies. Several other authors reported financial relationships with Alexion and other pharmaceutical companies; two authors are employees of Alexion.
Howard J et al. AANEM 2019. Unnumbered Abstract.
AUSTIN – according to a secondary analysis presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Evidence for the sustained effectiveness of eculizumab, a terminal complement inhibitor, in adult patients with antiacetylcholine receptor antibody-positive refractory generalized myasthenia gravis was provided by the 6-month, double-blind, placebo-controlled REGAIN study and its open-label extension. James F. Howard Jr., MD, distinguished professor of neuromuscular disease at the University of North Carolina in Chapel Hill and colleagues sought to analyze response profiles in REGAIN and its open-label extension.
The findings raise the possibility that complement inhibition with eculizumab should not be abandoned rapidly. “We accept that [eculizumab] works quickly,” Dr. Howard said. “There is an impression that if you don’t respond within the first 3 months, you’re not going to respond. I think these data would suggest otherwise.”
The investigators analyzed participants’ Myasthenia Gravis–Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) scores, which had been recorded throughout REGAIN and the extension. They defined early and late responses as improvement in MG-ADL score (i.e., a decrease of three or more points) or QMG score (i.e., a decrease of five or more points) occurring at 12 weeks or earlier or after 12 weeks, respectively, after initiation of eculizumab therapy. Patients randomized to eculizumab in REGAIN initially were treated with an IV induction dose of 900 mg/week before receiving 1,200 mg every 2 weeks thereafter.
Dr. Howard and colleagues included 98 patients in their analysis. Approximately 32% of patients achieved their first response within the first week of treatment, and 15% responded at week 2. About 16% of patients had a late response.
Responses to treatment on the MG-ADL scale had occurred in 67.3% by week 12 and in 84.7% by the end of the extension. Treatment with eculizumab resulted in QMG responses in 56.1% by week 12 and 71.4% by the end of the extension. The investigators observed response over multiple consecutive assessments for the vast majority of patients.
At week 130, the least-squares mean percentage changes from baseline in MG-ADL score were −61.9% and −47.5% in early and late MG-ADL responders, respectively. The least-squares mean percentage changes from baseline in QMG score were −40.8% and −55.5% in early and late QMG responders, respectively.
The investigators observed significant baseline differences between early versus late QMG responders in mean duration of myasthenia gravis (10.46 years vs. 5.46 years) and mean QMG score (18.6 vs. 15.1).
“I can’t explain [this finding]. It may simply be due to the low numbers of patients,” Dr. Howard said. “Whether this is going to hold up in postmarketing analysis remains to be seen. I’m not convinced that that is meaningful.”
Study funding was provided by Alexion Pharmaceuticals (the developer of eculizumab), the Centers for Disease Control and Prevention, and the National Institutes of Health. Dr. Howard reported receiving research support and consulting fees or honoraria from Alexion and several other pharmaceutical companies. Several other authors reported financial relationships with Alexion and other pharmaceutical companies; two authors are employees of Alexion.
Howard J et al. AANEM 2019. Unnumbered Abstract.
AUSTIN – according to a secondary analysis presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
Evidence for the sustained effectiveness of eculizumab, a terminal complement inhibitor, in adult patients with antiacetylcholine receptor antibody-positive refractory generalized myasthenia gravis was provided by the 6-month, double-blind, placebo-controlled REGAIN study and its open-label extension. James F. Howard Jr., MD, distinguished professor of neuromuscular disease at the University of North Carolina in Chapel Hill and colleagues sought to analyze response profiles in REGAIN and its open-label extension.
The findings raise the possibility that complement inhibition with eculizumab should not be abandoned rapidly. “We accept that [eculizumab] works quickly,” Dr. Howard said. “There is an impression that if you don’t respond within the first 3 months, you’re not going to respond. I think these data would suggest otherwise.”
The investigators analyzed participants’ Myasthenia Gravis–Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) scores, which had been recorded throughout REGAIN and the extension. They defined early and late responses as improvement in MG-ADL score (i.e., a decrease of three or more points) or QMG score (i.e., a decrease of five or more points) occurring at 12 weeks or earlier or after 12 weeks, respectively, after initiation of eculizumab therapy. Patients randomized to eculizumab in REGAIN initially were treated with an IV induction dose of 900 mg/week before receiving 1,200 mg every 2 weeks thereafter.
Dr. Howard and colleagues included 98 patients in their analysis. Approximately 32% of patients achieved their first response within the first week of treatment, and 15% responded at week 2. About 16% of patients had a late response.
Responses to treatment on the MG-ADL scale had occurred in 67.3% by week 12 and in 84.7% by the end of the extension. Treatment with eculizumab resulted in QMG responses in 56.1% by week 12 and 71.4% by the end of the extension. The investigators observed response over multiple consecutive assessments for the vast majority of patients.
At week 130, the least-squares mean percentage changes from baseline in MG-ADL score were −61.9% and −47.5% in early and late MG-ADL responders, respectively. The least-squares mean percentage changes from baseline in QMG score were −40.8% and −55.5% in early and late QMG responders, respectively.
The investigators observed significant baseline differences between early versus late QMG responders in mean duration of myasthenia gravis (10.46 years vs. 5.46 years) and mean QMG score (18.6 vs. 15.1).
“I can’t explain [this finding]. It may simply be due to the low numbers of patients,” Dr. Howard said. “Whether this is going to hold up in postmarketing analysis remains to be seen. I’m not convinced that that is meaningful.”
Study funding was provided by Alexion Pharmaceuticals (the developer of eculizumab), the Centers for Disease Control and Prevention, and the National Institutes of Health. Dr. Howard reported receiving research support and consulting fees or honoraria from Alexion and several other pharmaceutical companies. Several other authors reported financial relationships with Alexion and other pharmaceutical companies; two authors are employees of Alexion.
Howard J et al. AANEM 2019. Unnumbered Abstract.
REPORTING FROM AANEM 2019
Neurologists publish consensus statement on stridor in MSA
The statement was published Oct. 1 in Neurology. In addition to reviewing the literature on the topic and providing recommendations, the authors described several areas for future research.
MSA is a rare neurodegenerative disorder that entails autonomic failure, cerebellar ataxia, and parkinsonism. Laryngeal stridor has a high positive predictive value in the diagnosis of MSA, but consensus about its definition and clinical implications had not been established previously. The Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) delle Scienze Neurologiche di Bologna (Italy) convened a consensus conference of experts in 2017 to determine diagnostic criteria for stridor in MSA, define its prognostic value, suggest treatment options, and indicate subjects for future research. The neurologists reviewed studies of any design that reported original data. They based their statements on 34 published articles, most of which were class III or IV.
The authors defined stridor in MSA as “a strained, high-pitched, harsh respiratory sound, mainly inspiratory, caused by laryngeal dysfunction leading to narrowing of the rima glottidis.” Stridor may occur exclusively during sleep or during sleep and wakefulness. It may be recognized during a clinical examination, through witness report, or through an audio recording. Neurologists may consider laryngoscopy to exclude mechanical lesions or functional vocal cord abnormalities related to other neurologic conditions, wrote the authors. Drug-induced sleep endoscopy and video polysomnography also may be considered.
Whether stridor, or certain features of stridor, affects survival in MSA is uncertain. “Stridor within 3 years of motor or autonomic symptom onset may shorten survival,” according to the statement. “However, identification of stridor onset may be difficult.” Moreover, stridor during wakefulness is considered to reflect a more advanced stage of disease, compared with stridor during sleep. Although stridor can be distressing for the patient and his or her caregivers, its influence on health-related quality of life has yet to be determined, according to the statement.
Continuous positive airway pressure (CPAP) during sleep can be a useful symptomatic treatment and should be considered a first-line therapy for stridor, wrote the authors. Tracheostomy, another effective symptomatic treatment, bypasses upper-airway obstruction at the larynx. “Persistent and severe stridor may require tracheostomy,” according to the statement. It is not certain whether CPAP improves survival in patients with MSA and stridor, and tracheostomy may improve survival. The literature contains insufficient evidence about whether minimally invasive procedures or botulinum toxin injections are effective symptomatic treatments for stridor, wrote the authors.
During their review of the literature, the authors identified what they considered to be several research gaps. The diagnosis of stridor remains challenging, and investigators should develop a questionnaire for detecting stridor, they wrote. A smartphone application also could be developed to recognize stridor automatically. “The relationship between stridor and other breathing disorders (i.e., central apneas and breathing rate abnormalities) and their respective contributions to disease prognosis and survival should be determined through a multicenter prospective study,” according to the statement. Finally, randomized controlled trials comparing CPAP and tracheostomy for various degrees of stridor could guide physicians’ choice of treatment.
The IRCCS funded the study. One of the authors is a section editor for Neurology, and other authors reported receiving honoraria from various companies such as Novartis, Sanofi, and UCB.
The statement was published Oct. 1 in Neurology. In addition to reviewing the literature on the topic and providing recommendations, the authors described several areas for future research.
MSA is a rare neurodegenerative disorder that entails autonomic failure, cerebellar ataxia, and parkinsonism. Laryngeal stridor has a high positive predictive value in the diagnosis of MSA, but consensus about its definition and clinical implications had not been established previously. The Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) delle Scienze Neurologiche di Bologna (Italy) convened a consensus conference of experts in 2017 to determine diagnostic criteria for stridor in MSA, define its prognostic value, suggest treatment options, and indicate subjects for future research. The neurologists reviewed studies of any design that reported original data. They based their statements on 34 published articles, most of which were class III or IV.
The authors defined stridor in MSA as “a strained, high-pitched, harsh respiratory sound, mainly inspiratory, caused by laryngeal dysfunction leading to narrowing of the rima glottidis.” Stridor may occur exclusively during sleep or during sleep and wakefulness. It may be recognized during a clinical examination, through witness report, or through an audio recording. Neurologists may consider laryngoscopy to exclude mechanical lesions or functional vocal cord abnormalities related to other neurologic conditions, wrote the authors. Drug-induced sleep endoscopy and video polysomnography also may be considered.
Whether stridor, or certain features of stridor, affects survival in MSA is uncertain. “Stridor within 3 years of motor or autonomic symptom onset may shorten survival,” according to the statement. “However, identification of stridor onset may be difficult.” Moreover, stridor during wakefulness is considered to reflect a more advanced stage of disease, compared with stridor during sleep. Although stridor can be distressing for the patient and his or her caregivers, its influence on health-related quality of life has yet to be determined, according to the statement.
Continuous positive airway pressure (CPAP) during sleep can be a useful symptomatic treatment and should be considered a first-line therapy for stridor, wrote the authors. Tracheostomy, another effective symptomatic treatment, bypasses upper-airway obstruction at the larynx. “Persistent and severe stridor may require tracheostomy,” according to the statement. It is not certain whether CPAP improves survival in patients with MSA and stridor, and tracheostomy may improve survival. The literature contains insufficient evidence about whether minimally invasive procedures or botulinum toxin injections are effective symptomatic treatments for stridor, wrote the authors.
During their review of the literature, the authors identified what they considered to be several research gaps. The diagnosis of stridor remains challenging, and investigators should develop a questionnaire for detecting stridor, they wrote. A smartphone application also could be developed to recognize stridor automatically. “The relationship between stridor and other breathing disorders (i.e., central apneas and breathing rate abnormalities) and their respective contributions to disease prognosis and survival should be determined through a multicenter prospective study,” according to the statement. Finally, randomized controlled trials comparing CPAP and tracheostomy for various degrees of stridor could guide physicians’ choice of treatment.
The IRCCS funded the study. One of the authors is a section editor for Neurology, and other authors reported receiving honoraria from various companies such as Novartis, Sanofi, and UCB.
The statement was published Oct. 1 in Neurology. In addition to reviewing the literature on the topic and providing recommendations, the authors described several areas for future research.
MSA is a rare neurodegenerative disorder that entails autonomic failure, cerebellar ataxia, and parkinsonism. Laryngeal stridor has a high positive predictive value in the diagnosis of MSA, but consensus about its definition and clinical implications had not been established previously. The Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) delle Scienze Neurologiche di Bologna (Italy) convened a consensus conference of experts in 2017 to determine diagnostic criteria for stridor in MSA, define its prognostic value, suggest treatment options, and indicate subjects for future research. The neurologists reviewed studies of any design that reported original data. They based their statements on 34 published articles, most of which were class III or IV.
The authors defined stridor in MSA as “a strained, high-pitched, harsh respiratory sound, mainly inspiratory, caused by laryngeal dysfunction leading to narrowing of the rima glottidis.” Stridor may occur exclusively during sleep or during sleep and wakefulness. It may be recognized during a clinical examination, through witness report, or through an audio recording. Neurologists may consider laryngoscopy to exclude mechanical lesions or functional vocal cord abnormalities related to other neurologic conditions, wrote the authors. Drug-induced sleep endoscopy and video polysomnography also may be considered.
Whether stridor, or certain features of stridor, affects survival in MSA is uncertain. “Stridor within 3 years of motor or autonomic symptom onset may shorten survival,” according to the statement. “However, identification of stridor onset may be difficult.” Moreover, stridor during wakefulness is considered to reflect a more advanced stage of disease, compared with stridor during sleep. Although stridor can be distressing for the patient and his or her caregivers, its influence on health-related quality of life has yet to be determined, according to the statement.
Continuous positive airway pressure (CPAP) during sleep can be a useful symptomatic treatment and should be considered a first-line therapy for stridor, wrote the authors. Tracheostomy, another effective symptomatic treatment, bypasses upper-airway obstruction at the larynx. “Persistent and severe stridor may require tracheostomy,” according to the statement. It is not certain whether CPAP improves survival in patients with MSA and stridor, and tracheostomy may improve survival. The literature contains insufficient evidence about whether minimally invasive procedures or botulinum toxin injections are effective symptomatic treatments for stridor, wrote the authors.
During their review of the literature, the authors identified what they considered to be several research gaps. The diagnosis of stridor remains challenging, and investigators should develop a questionnaire for detecting stridor, they wrote. A smartphone application also could be developed to recognize stridor automatically. “The relationship between stridor and other breathing disorders (i.e., central apneas and breathing rate abnormalities) and their respective contributions to disease prognosis and survival should be determined through a multicenter prospective study,” according to the statement. Finally, randomized controlled trials comparing CPAP and tracheostomy for various degrees of stridor could guide physicians’ choice of treatment.
The IRCCS funded the study. One of the authors is a section editor for Neurology, and other authors reported receiving honoraria from various companies such as Novartis, Sanofi, and UCB.
FROM NEUROLOGY
Accounting for sex may improve diagnosis of amnestic MCI
, according to an investigation published Oct. 9 in Neurology. Using sex-specific cut scores to define verbal memory impairment improves diagnostic accuracy and “may result in earlier detection of memory impairment in women and avoid false diagnoses in men,” wrote Erin E. Sundermann, PhD, assistant project scientist in psychiatry at the University of California, San Diego, and colleagues.
A diagnosis of aMCI generally requires a verbal memory deficit. Ample research demonstrates a female advantage on verbal memory tests, but normative data for these tests usually do not adjust for sex. Dr. Sundermann and colleagues previously showed that among men and women with aMCI and similar disease burden, women perform better on tests of verbal memory. Given these results, the investigators initiated a new study to test the hypothesis that using sex-specific norms and cut scores to identify memory impairment improves the accuracy of aMCI diagnosis, compared with non–sex-specific norms and cut scores.
An examination of ADNI data
Dr. Sundermann’s group extracted cross-sectional data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database in October 2016. They included participants without dementia for whom neuropsychologic and Alzheimer’s disease pathologic marker data were available at baseline. They excluded patients with a non-aMCI diagnosis based on typical and sex-specific criteria.
The researchers’ primary outcome was the Rey Auditory Verbal Learning Test (RAVLT). They also determined the presence or absence of the APOE e4 allele for each participant. Biomarker outcomes included the CSF ratio of hyperphosphorylated tau (p-tau) to beta-amyloid (A-beta), and cortical A-beta deposition.
Dr. Sundermann and colleagues applied the Jak/Bondi actuarial neuropsychologic diagnostic method to baseline data. This method relies on six neuropsychologic tests, including the RAVLT Learning and Delayed Recall. They subsequently derived two sets of normative data for the RAVLT outcomes in a normative sample of 1,620 patients enrolled in the Mayo Clinic Study of Aging (MCSA). The latter patients were considered normal controls at baseline and at least two follow-up visits at 15 months apart. One set of normative data was specific for age and education, and the other was specific for age, education, and sex. Dr. Sundermann’s group next applied the typical Jak/Bondi method and the sex-specific Jak/Bondi method to all ADNI participants’ data.
Biomarker analysis supported the hypothesis
The researchers included 985 participants (453 women) in their final sample. Approximately 94% of the population was white. Mean age was 72.9 years, and mean education duration was 16.3 years. Overall, women had a significantly lower mean age (71.9 years vs. 73.6 years), significantly fewer mean years of education (15.7 years vs. 16.7 years), and a significantly higher mean Mini-Mental State Examination score (28 vs. 28.1) compared with men. Compared with men’s scores, women’s scores on the RAVLT Learning (mean 42.3 vs. mean 35.6) and Delayed Recall (mean 6.2 vs. mean 4.5) were significantly higher.
When Dr. Sundermann and colleagues used typical cut scores, the frequency of aMCI diagnosis was significantly higher in men. Using sex-specific cut scores eliminated this sex difference, however. Among men, 184 (35%) were categorized as true positive, 293 (55%) as true negative, and 55 (10%) as false positive. No men were categorized as false negative. Among women, 120 (26%) were categorized as true positive, 288 (64%) as true negative, and 45 (10%) as false negative. No women were categorized as false positive.
The likelihood of cortical amyloid positivity in false negative women was 3.6 times greater than in true negative women but did not differ from that in true positive women. The likelihood of positivity for the CSF p-tau/A-beta ratio in false negative women was more than two times higher than in true negative women but did not differ from that in true positive women. The likelihood of having an APOE e4 allele in false negative women was almost fivefold higher than in true negative women but did not differ from that in true positive women.
The likelihood of cortical amyloid positivity in false positive men was less than that in true positive men (odds ratio [OR], 0.45) but did not differ from that in true negative men. The likelihood of positivity for CSF p-tau/A-beta ratio in false positive men was significantly less than in true positive men (OR, 0.47) but did not differ from that in true negative men. The likelihood of having the APOE e4 allele in false positive men was lower than that in true positive men (OR, 0.63) and higher than that in true negative men (OR, 1.50), but not significantly.
Results have implications for treatment
“If these results are confirmed, they have vital implications,” Dr. Sundermann said in a press release. “If women are inaccurately identified as having no problems with memory and thinking skills when they actually have MCI, then treatments are not being started, and they and their families are not planning ahead for their care or their financial or legal situations. And for men who are inaccurately diagnosed with MCI, they can be exposed to unneeded medications along with undue stress for them and their families.”
Among the limitations that the investigators acknowledged was the study’s cross-sectional, rather than longitudinal, design. In addition, the ADNI population that the researchers examined is a convenience sample of predominantly white and well-educated volunteers. The results therefore may not be generalizable to the broader U.S. population, wrote the authors.
Grants from the National Institutes of Health funded the study. Several of the investigators reported receiving honoraria from various pharmaceutical companies such as Mylan. One investigator sits on the editorial board for Neurology.
, according to an investigation published Oct. 9 in Neurology. Using sex-specific cut scores to define verbal memory impairment improves diagnostic accuracy and “may result in earlier detection of memory impairment in women and avoid false diagnoses in men,” wrote Erin E. Sundermann, PhD, assistant project scientist in psychiatry at the University of California, San Diego, and colleagues.
A diagnosis of aMCI generally requires a verbal memory deficit. Ample research demonstrates a female advantage on verbal memory tests, but normative data for these tests usually do not adjust for sex. Dr. Sundermann and colleagues previously showed that among men and women with aMCI and similar disease burden, women perform better on tests of verbal memory. Given these results, the investigators initiated a new study to test the hypothesis that using sex-specific norms and cut scores to identify memory impairment improves the accuracy of aMCI diagnosis, compared with non–sex-specific norms and cut scores.
An examination of ADNI data
Dr. Sundermann’s group extracted cross-sectional data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database in October 2016. They included participants without dementia for whom neuropsychologic and Alzheimer’s disease pathologic marker data were available at baseline. They excluded patients with a non-aMCI diagnosis based on typical and sex-specific criteria.
The researchers’ primary outcome was the Rey Auditory Verbal Learning Test (RAVLT). They also determined the presence or absence of the APOE e4 allele for each participant. Biomarker outcomes included the CSF ratio of hyperphosphorylated tau (p-tau) to beta-amyloid (A-beta), and cortical A-beta deposition.
Dr. Sundermann and colleagues applied the Jak/Bondi actuarial neuropsychologic diagnostic method to baseline data. This method relies on six neuropsychologic tests, including the RAVLT Learning and Delayed Recall. They subsequently derived two sets of normative data for the RAVLT outcomes in a normative sample of 1,620 patients enrolled in the Mayo Clinic Study of Aging (MCSA). The latter patients were considered normal controls at baseline and at least two follow-up visits at 15 months apart. One set of normative data was specific for age and education, and the other was specific for age, education, and sex. Dr. Sundermann’s group next applied the typical Jak/Bondi method and the sex-specific Jak/Bondi method to all ADNI participants’ data.
Biomarker analysis supported the hypothesis
The researchers included 985 participants (453 women) in their final sample. Approximately 94% of the population was white. Mean age was 72.9 years, and mean education duration was 16.3 years. Overall, women had a significantly lower mean age (71.9 years vs. 73.6 years), significantly fewer mean years of education (15.7 years vs. 16.7 years), and a significantly higher mean Mini-Mental State Examination score (28 vs. 28.1) compared with men. Compared with men’s scores, women’s scores on the RAVLT Learning (mean 42.3 vs. mean 35.6) and Delayed Recall (mean 6.2 vs. mean 4.5) were significantly higher.
When Dr. Sundermann and colleagues used typical cut scores, the frequency of aMCI diagnosis was significantly higher in men. Using sex-specific cut scores eliminated this sex difference, however. Among men, 184 (35%) were categorized as true positive, 293 (55%) as true negative, and 55 (10%) as false positive. No men were categorized as false negative. Among women, 120 (26%) were categorized as true positive, 288 (64%) as true negative, and 45 (10%) as false negative. No women were categorized as false positive.
The likelihood of cortical amyloid positivity in false negative women was 3.6 times greater than in true negative women but did not differ from that in true positive women. The likelihood of positivity for the CSF p-tau/A-beta ratio in false negative women was more than two times higher than in true negative women but did not differ from that in true positive women. The likelihood of having an APOE e4 allele in false negative women was almost fivefold higher than in true negative women but did not differ from that in true positive women.
The likelihood of cortical amyloid positivity in false positive men was less than that in true positive men (odds ratio [OR], 0.45) but did not differ from that in true negative men. The likelihood of positivity for CSF p-tau/A-beta ratio in false positive men was significantly less than in true positive men (OR, 0.47) but did not differ from that in true negative men. The likelihood of having the APOE e4 allele in false positive men was lower than that in true positive men (OR, 0.63) and higher than that in true negative men (OR, 1.50), but not significantly.
Results have implications for treatment
“If these results are confirmed, they have vital implications,” Dr. Sundermann said in a press release. “If women are inaccurately identified as having no problems with memory and thinking skills when they actually have MCI, then treatments are not being started, and they and their families are not planning ahead for their care or their financial or legal situations. And for men who are inaccurately diagnosed with MCI, they can be exposed to unneeded medications along with undue stress for them and their families.”
Among the limitations that the investigators acknowledged was the study’s cross-sectional, rather than longitudinal, design. In addition, the ADNI population that the researchers examined is a convenience sample of predominantly white and well-educated volunteers. The results therefore may not be generalizable to the broader U.S. population, wrote the authors.
Grants from the National Institutes of Health funded the study. Several of the investigators reported receiving honoraria from various pharmaceutical companies such as Mylan. One investigator sits on the editorial board for Neurology.
, according to an investigation published Oct. 9 in Neurology. Using sex-specific cut scores to define verbal memory impairment improves diagnostic accuracy and “may result in earlier detection of memory impairment in women and avoid false diagnoses in men,” wrote Erin E. Sundermann, PhD, assistant project scientist in psychiatry at the University of California, San Diego, and colleagues.
A diagnosis of aMCI generally requires a verbal memory deficit. Ample research demonstrates a female advantage on verbal memory tests, but normative data for these tests usually do not adjust for sex. Dr. Sundermann and colleagues previously showed that among men and women with aMCI and similar disease burden, women perform better on tests of verbal memory. Given these results, the investigators initiated a new study to test the hypothesis that using sex-specific norms and cut scores to identify memory impairment improves the accuracy of aMCI diagnosis, compared with non–sex-specific norms and cut scores.
An examination of ADNI data
Dr. Sundermann’s group extracted cross-sectional data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database in October 2016. They included participants without dementia for whom neuropsychologic and Alzheimer’s disease pathologic marker data were available at baseline. They excluded patients with a non-aMCI diagnosis based on typical and sex-specific criteria.
The researchers’ primary outcome was the Rey Auditory Verbal Learning Test (RAVLT). They also determined the presence or absence of the APOE e4 allele for each participant. Biomarker outcomes included the CSF ratio of hyperphosphorylated tau (p-tau) to beta-amyloid (A-beta), and cortical A-beta deposition.
Dr. Sundermann and colleagues applied the Jak/Bondi actuarial neuropsychologic diagnostic method to baseline data. This method relies on six neuropsychologic tests, including the RAVLT Learning and Delayed Recall. They subsequently derived two sets of normative data for the RAVLT outcomes in a normative sample of 1,620 patients enrolled in the Mayo Clinic Study of Aging (MCSA). The latter patients were considered normal controls at baseline and at least two follow-up visits at 15 months apart. One set of normative data was specific for age and education, and the other was specific for age, education, and sex. Dr. Sundermann’s group next applied the typical Jak/Bondi method and the sex-specific Jak/Bondi method to all ADNI participants’ data.
Biomarker analysis supported the hypothesis
The researchers included 985 participants (453 women) in their final sample. Approximately 94% of the population was white. Mean age was 72.9 years, and mean education duration was 16.3 years. Overall, women had a significantly lower mean age (71.9 years vs. 73.6 years), significantly fewer mean years of education (15.7 years vs. 16.7 years), and a significantly higher mean Mini-Mental State Examination score (28 vs. 28.1) compared with men. Compared with men’s scores, women’s scores on the RAVLT Learning (mean 42.3 vs. mean 35.6) and Delayed Recall (mean 6.2 vs. mean 4.5) were significantly higher.
When Dr. Sundermann and colleagues used typical cut scores, the frequency of aMCI diagnosis was significantly higher in men. Using sex-specific cut scores eliminated this sex difference, however. Among men, 184 (35%) were categorized as true positive, 293 (55%) as true negative, and 55 (10%) as false positive. No men were categorized as false negative. Among women, 120 (26%) were categorized as true positive, 288 (64%) as true negative, and 45 (10%) as false negative. No women were categorized as false positive.
The likelihood of cortical amyloid positivity in false negative women was 3.6 times greater than in true negative women but did not differ from that in true positive women. The likelihood of positivity for the CSF p-tau/A-beta ratio in false negative women was more than two times higher than in true negative women but did not differ from that in true positive women. The likelihood of having an APOE e4 allele in false negative women was almost fivefold higher than in true negative women but did not differ from that in true positive women.
The likelihood of cortical amyloid positivity in false positive men was less than that in true positive men (odds ratio [OR], 0.45) but did not differ from that in true negative men. The likelihood of positivity for CSF p-tau/A-beta ratio in false positive men was significantly less than in true positive men (OR, 0.47) but did not differ from that in true negative men. The likelihood of having the APOE e4 allele in false positive men was lower than that in true positive men (OR, 0.63) and higher than that in true negative men (OR, 1.50), but not significantly.
Results have implications for treatment
“If these results are confirmed, they have vital implications,” Dr. Sundermann said in a press release. “If women are inaccurately identified as having no problems with memory and thinking skills when they actually have MCI, then treatments are not being started, and they and their families are not planning ahead for their care or their financial or legal situations. And for men who are inaccurately diagnosed with MCI, they can be exposed to unneeded medications along with undue stress for them and their families.”
Among the limitations that the investigators acknowledged was the study’s cross-sectional, rather than longitudinal, design. In addition, the ADNI population that the researchers examined is a convenience sample of predominantly white and well-educated volunteers. The results therefore may not be generalizable to the broader U.S. population, wrote the authors.
Grants from the National Institutes of Health funded the study. Several of the investigators reported receiving honoraria from various pharmaceutical companies such as Mylan. One investigator sits on the editorial board for Neurology.
FROM NEUROLOGY
Influenza vaccination modestly reduces risk of hospitalizations in patients with COPD
(COPD), according to data published in the Journal of Infectious Diseases.
“To the best of our knowledge, this is the first large, real-world population study to examine vaccine effectiveness in people with COPD using the test-negative design and influenza-specific study outcomes,” wrote Andrea S. Gershon, MD, of Sunnybrook Health Sciences Center in Toronto and colleagues. “These findings emphasize the need for more effective influenza vaccines for older COPD patients and other preventive strategies.”
A test-negative study design
Data suggest that 70% of COPD exacerbations are caused by infection, and influenza often is identified as the cause. Although all major COPD practice guidelines recommend seasonal influenza vaccination, the evidence indicating that vaccination reduces hospitalizations and death is limited. The inherent or corticosteroid-induced decrease in immune response to vaccination and respiratory infection among patients with COPD may reduce the effectiveness of influenza vaccination, wrote Dr. Gershon and colleagues.
The investigators used a test-negative design to evaluate how effectively influenza vaccination prevents laboratory-confirmed influenza–associated hospitalizations in community-dwelling older patients with COPD. They chose this design because it attenuates biases resulting from misclassification of infection and from differences in health care–seeking behavior between vaccinated and unvaccinated patients.
Dr. Gershon and colleagues examined health care administrative data and respiratory specimens collected from patients who had been tested for influenza during the 2010-2011 to 2015-2016 influenza seasons. Eligible patients were aged 66 years or older, had physician-diagnosed COPD, and had been tested for influenza within 3 days before and during an acute care hospitalization. The researchers determined influenza vaccination status using physician and pharmacist billing claims. They obtained demographic information through linkage with the provincial health insurance database. Multivariable logistic regression allowed Dr. Gershon and colleagues to estimate the adjusted odds ratio of influenza vaccination in people with laboratory-confirmed influenza, compared with those without.
Effectiveness did not vary by demographic factors
The investigators included 21,748 patients in their analysis. Of this population, 3,636 (16.7%) patients tested positive for influenza. Vaccinated patients were less likely than unvaccinated patients to test positive for influenza (15.3% vs. 18.6%). Vaccinated patients also were more likely to be older; live in an urban area; live in a higher income neighborhood; have had more outpatient visits with a physician in the previous year; have received a prescription for a COPD medication in the previous 6 months; have diabetes, asthma, or immunocompromising conditions; have a longer duration of COPD; and have had an outpatient COPD exacerbation in the previous year.
The overall unadjusted estimate of vaccine effectiveness against laboratory-confirmed influenza–associated hospitalizations was 21%. Multivariable adjustment yielded an effectiveness of 22%. When Dr. Gershon and colleagues corrected for misclassification of vaccination status among people with COPD, the effectiveness was estimated to be 43%. Vaccine effectiveness did not vary significantly according to influenza season, nor did it vary significantly by patient-specific factors such as age, sex, influenza subtype, codiagnosis of asthma, duration of COPD, previous outpatient COPD exacerbations, previous COPD hospitalization, previous receipt of inhaled corticosteroids, and previous pneumonia.
One limitation of the study was the possibility that COPD was misclassified because not all participants underwent pulmonary function testing. In addition, the estimates of vaccine effectiveness in the present study are specific to the outcome of influenza hospitalization and may not be generalizable to vaccine effectiveness estimates of outpatient outcomes, said the investigators. Finally, Dr. Gershon and colleagues could not identify the type of vaccine received.
“Given that a large pragmatic randomized controlled trial evaluating influenza vaccination would be unethical, this is likely the most robust estimate of vaccine effectiveness for hospitalizations in the COPD population to guide influenza vaccine recommendations for patients with COPD,” wrote Dr. Gershon and colleagues.
An Ontario Ministry of Health and Long-Term Care Health Systems Research Fund Capacity Grant and a Canadian Institutes of Health Research operating grant funded this research. One investigator received grants from the Canadian Institutes of Health Research during the study, and others received grants from pharmaceutical companies that were unrelated to this study.
SOURCE: Gershon AS et al. J Infect Dis. 2019 Sep 24. doi: 10.1093/infdis/jiz419.
(COPD), according to data published in the Journal of Infectious Diseases.
“To the best of our knowledge, this is the first large, real-world population study to examine vaccine effectiveness in people with COPD using the test-negative design and influenza-specific study outcomes,” wrote Andrea S. Gershon, MD, of Sunnybrook Health Sciences Center in Toronto and colleagues. “These findings emphasize the need for more effective influenza vaccines for older COPD patients and other preventive strategies.”
A test-negative study design
Data suggest that 70% of COPD exacerbations are caused by infection, and influenza often is identified as the cause. Although all major COPD practice guidelines recommend seasonal influenza vaccination, the evidence indicating that vaccination reduces hospitalizations and death is limited. The inherent or corticosteroid-induced decrease in immune response to vaccination and respiratory infection among patients with COPD may reduce the effectiveness of influenza vaccination, wrote Dr. Gershon and colleagues.
The investigators used a test-negative design to evaluate how effectively influenza vaccination prevents laboratory-confirmed influenza–associated hospitalizations in community-dwelling older patients with COPD. They chose this design because it attenuates biases resulting from misclassification of infection and from differences in health care–seeking behavior between vaccinated and unvaccinated patients.
Dr. Gershon and colleagues examined health care administrative data and respiratory specimens collected from patients who had been tested for influenza during the 2010-2011 to 2015-2016 influenza seasons. Eligible patients were aged 66 years or older, had physician-diagnosed COPD, and had been tested for influenza within 3 days before and during an acute care hospitalization. The researchers determined influenza vaccination status using physician and pharmacist billing claims. They obtained demographic information through linkage with the provincial health insurance database. Multivariable logistic regression allowed Dr. Gershon and colleagues to estimate the adjusted odds ratio of influenza vaccination in people with laboratory-confirmed influenza, compared with those without.
Effectiveness did not vary by demographic factors
The investigators included 21,748 patients in their analysis. Of this population, 3,636 (16.7%) patients tested positive for influenza. Vaccinated patients were less likely than unvaccinated patients to test positive for influenza (15.3% vs. 18.6%). Vaccinated patients also were more likely to be older; live in an urban area; live in a higher income neighborhood; have had more outpatient visits with a physician in the previous year; have received a prescription for a COPD medication in the previous 6 months; have diabetes, asthma, or immunocompromising conditions; have a longer duration of COPD; and have had an outpatient COPD exacerbation in the previous year.
The overall unadjusted estimate of vaccine effectiveness against laboratory-confirmed influenza–associated hospitalizations was 21%. Multivariable adjustment yielded an effectiveness of 22%. When Dr. Gershon and colleagues corrected for misclassification of vaccination status among people with COPD, the effectiveness was estimated to be 43%. Vaccine effectiveness did not vary significantly according to influenza season, nor did it vary significantly by patient-specific factors such as age, sex, influenza subtype, codiagnosis of asthma, duration of COPD, previous outpatient COPD exacerbations, previous COPD hospitalization, previous receipt of inhaled corticosteroids, and previous pneumonia.
One limitation of the study was the possibility that COPD was misclassified because not all participants underwent pulmonary function testing. In addition, the estimates of vaccine effectiveness in the present study are specific to the outcome of influenza hospitalization and may not be generalizable to vaccine effectiveness estimates of outpatient outcomes, said the investigators. Finally, Dr. Gershon and colleagues could not identify the type of vaccine received.
“Given that a large pragmatic randomized controlled trial evaluating influenza vaccination would be unethical, this is likely the most robust estimate of vaccine effectiveness for hospitalizations in the COPD population to guide influenza vaccine recommendations for patients with COPD,” wrote Dr. Gershon and colleagues.
An Ontario Ministry of Health and Long-Term Care Health Systems Research Fund Capacity Grant and a Canadian Institutes of Health Research operating grant funded this research. One investigator received grants from the Canadian Institutes of Health Research during the study, and others received grants from pharmaceutical companies that were unrelated to this study.
SOURCE: Gershon AS et al. J Infect Dis. 2019 Sep 24. doi: 10.1093/infdis/jiz419.
(COPD), according to data published in the Journal of Infectious Diseases.
“To the best of our knowledge, this is the first large, real-world population study to examine vaccine effectiveness in people with COPD using the test-negative design and influenza-specific study outcomes,” wrote Andrea S. Gershon, MD, of Sunnybrook Health Sciences Center in Toronto and colleagues. “These findings emphasize the need for more effective influenza vaccines for older COPD patients and other preventive strategies.”
A test-negative study design
Data suggest that 70% of COPD exacerbations are caused by infection, and influenza often is identified as the cause. Although all major COPD practice guidelines recommend seasonal influenza vaccination, the evidence indicating that vaccination reduces hospitalizations and death is limited. The inherent or corticosteroid-induced decrease in immune response to vaccination and respiratory infection among patients with COPD may reduce the effectiveness of influenza vaccination, wrote Dr. Gershon and colleagues.
The investigators used a test-negative design to evaluate how effectively influenza vaccination prevents laboratory-confirmed influenza–associated hospitalizations in community-dwelling older patients with COPD. They chose this design because it attenuates biases resulting from misclassification of infection and from differences in health care–seeking behavior between vaccinated and unvaccinated patients.
Dr. Gershon and colleagues examined health care administrative data and respiratory specimens collected from patients who had been tested for influenza during the 2010-2011 to 2015-2016 influenza seasons. Eligible patients were aged 66 years or older, had physician-diagnosed COPD, and had been tested for influenza within 3 days before and during an acute care hospitalization. The researchers determined influenza vaccination status using physician and pharmacist billing claims. They obtained demographic information through linkage with the provincial health insurance database. Multivariable logistic regression allowed Dr. Gershon and colleagues to estimate the adjusted odds ratio of influenza vaccination in people with laboratory-confirmed influenza, compared with those without.
Effectiveness did not vary by demographic factors
The investigators included 21,748 patients in their analysis. Of this population, 3,636 (16.7%) patients tested positive for influenza. Vaccinated patients were less likely than unvaccinated patients to test positive for influenza (15.3% vs. 18.6%). Vaccinated patients also were more likely to be older; live in an urban area; live in a higher income neighborhood; have had more outpatient visits with a physician in the previous year; have received a prescription for a COPD medication in the previous 6 months; have diabetes, asthma, or immunocompromising conditions; have a longer duration of COPD; and have had an outpatient COPD exacerbation in the previous year.
The overall unadjusted estimate of vaccine effectiveness against laboratory-confirmed influenza–associated hospitalizations was 21%. Multivariable adjustment yielded an effectiveness of 22%. When Dr. Gershon and colleagues corrected for misclassification of vaccination status among people with COPD, the effectiveness was estimated to be 43%. Vaccine effectiveness did not vary significantly according to influenza season, nor did it vary significantly by patient-specific factors such as age, sex, influenza subtype, codiagnosis of asthma, duration of COPD, previous outpatient COPD exacerbations, previous COPD hospitalization, previous receipt of inhaled corticosteroids, and previous pneumonia.
One limitation of the study was the possibility that COPD was misclassified because not all participants underwent pulmonary function testing. In addition, the estimates of vaccine effectiveness in the present study are specific to the outcome of influenza hospitalization and may not be generalizable to vaccine effectiveness estimates of outpatient outcomes, said the investigators. Finally, Dr. Gershon and colleagues could not identify the type of vaccine received.
“Given that a large pragmatic randomized controlled trial evaluating influenza vaccination would be unethical, this is likely the most robust estimate of vaccine effectiveness for hospitalizations in the COPD population to guide influenza vaccine recommendations for patients with COPD,” wrote Dr. Gershon and colleagues.
An Ontario Ministry of Health and Long-Term Care Health Systems Research Fund Capacity Grant and a Canadian Institutes of Health Research operating grant funded this research. One investigator received grants from the Canadian Institutes of Health Research during the study, and others received grants from pharmaceutical companies that were unrelated to this study.
SOURCE: Gershon AS et al. J Infect Dis. 2019 Sep 24. doi: 10.1093/infdis/jiz419.
FROM JOURNAL OF INFECTIOUS DISEASES
Investigators use ARMSS score to predict future MS-related disability
STOCKHOLM – , according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. The resulting measurement is stable, not highly sensitive to age, and appropriate for research applications. “It could give a clinician an earlier indication of the potential disease course of a patient,” said Ryan Ramanujam, PhD, assistant professor of translational neuroepidemiology at Karolinska Institutet in Stockholm.
Researchers who study MS use various scores to measure disease severity, including the Expanded Disability Status Scale (EDSS) and the MS Severity Scale (MSSS). These scores cannot predict a patient’s future status, however, and they do not remain stable throughout the course of a patient’s disease. Fitting a linear model over a series of scores over time can provide a misleading impression of a patient’s disease progression. “What we need is a metric to give a holistic overview of disease course, regardless of when it’s measured in a patient’s disease progression,” said Dr. Ramanujam. Such a measurement could aid the search for genes that affect MS severity, he added.
Examining disability by patient age
Dr. Ramanujam and colleagues constructed their measure using the ARMSS score, which ranks EDSS score by age instead of by disease duration. The ARMSS score ranges from 0 to 10, and the median value is 5 for all patients at a given age. Investigators can calculate the score using a previously published global matrix of values for ARMSS and MSSS available in the R package ms.sev.
The investigators found that the ARMSS score is slightly superior to the MSSS in detecting small increases in EDSS. One benefit of the ARMSS score, compared with the MSSS, is that it allows investigators to study patients for whom time of disease onset is unknown. The ARMSS score also removes potential systematic bias that might result from a neurologist’s retrospective assignment of date of disease onset, said Dr. Ramanujam.
He and his colleagues used ARMSS to compare patients’ disease course with what is expected for that patient (i.e., an ARMSS that remains stable at 5). They extracted data for 15,831 patients participating in the Swedish MS registry, including age and EDSS score at each neurological visit. Eligible patients had serial EDSS scores for 10 years. Dr. Ramanujam and colleagues included 4,514 patients in their analysis.
Measures at 2 years correlated with those at 10 years
The researchers created what they called the ARMSS integral by calculating the ARMSS score’s change from 5 at each examination (e.g., −0.5 or 1). “The ARMSS integral can be thought of as the cumulative disability that a patient accrues over his or her disease course, relative to the average patient, who had the disease for the same ages,” said Dr. Ramanujam. At 2 years of follow-up and at 10 years of follow-up, the distribution of ARMSS integrals for the study population followed a normal pattern.
Next, the investigators sought to compare patients by standardizing their follow-up time. To do this, they calculated what they called the ARMSS-rate by dividing each patient’s ARMSS integral by the number of years of follow-up. The ARMSS-rate offers a “snapshot of disease severity and progression,” said Dr. Ramanujam. When the researchers compared ARMSS-rates at 2 years and 10 years for each patient, they found that the measure was “extremely stable over time and strongly correlated with future disability.” The correlation improved slightly when the researchers compared ARMSS-rates at 4 years and 10 years.
The investigators then categorized patients based on their ARMSS-rate at 2 years (e.g., 0 to 1, 1 to 2, 2 to 3). When they compared the values in these categories with the median ARMSS-rates for the same individuals over the subsequent 8 years, they found strong group-level correlations.
To analyze correlations on an individual level, Dr. Ramanujam and colleagues examined the ability of different metrics at the time closest to 2 years of follow-up to predict those measured at 10 years. They assigned the value 1 to the most severe quartile of outcomes and the value 0 to all other quartiles. For predictors and outcomes, the investigators examined ARMSS-rate and the integral of progression index, which they calculated using the integral of EDSS. They also included EDSS at 10 years as an outcome for progression index.
For predicting the subsequent 8 years of ARMSS-rates, ARMSS-rate at 2 years had an area under the curve (AUC) of 0.921. When the investigators performed the same analysis using a cohort of patients with MS from British Columbia, Canada, they obtained an AUC of 0.887. Progression index at 2 years had an AUC of 0.61 for predicting the most severe quartile of the next 8 years. Compared with this result, ARMSS integral up to 2 years was slightly better at predicting EDSS at 10 years, said Dr. Ramanujam. The progression index poorly predicted the most severe quartile of EDSS at 10 years.
The main limitation of the ARMSS integral and ARMSS-rate is that they are based on EDSS, he added. The EDSS gives great weight to mobility and largely does not measure cognitive disability. “Future metrics could therefore include additional data such as MRI, Symbol Digit Modalities Test, or neurofilament light levels,” said Dr. Ramanujam. “Also, self-assessment could be one area to improve in the future.”
Dr. Ramanujam had no conflicts of interest to disclose. He receives funding from the MultipleMS Project, which is part of the EU Horizon 2020 Framework.
STOCKHOLM – , according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. The resulting measurement is stable, not highly sensitive to age, and appropriate for research applications. “It could give a clinician an earlier indication of the potential disease course of a patient,” said Ryan Ramanujam, PhD, assistant professor of translational neuroepidemiology at Karolinska Institutet in Stockholm.
Researchers who study MS use various scores to measure disease severity, including the Expanded Disability Status Scale (EDSS) and the MS Severity Scale (MSSS). These scores cannot predict a patient’s future status, however, and they do not remain stable throughout the course of a patient’s disease. Fitting a linear model over a series of scores over time can provide a misleading impression of a patient’s disease progression. “What we need is a metric to give a holistic overview of disease course, regardless of when it’s measured in a patient’s disease progression,” said Dr. Ramanujam. Such a measurement could aid the search for genes that affect MS severity, he added.
Examining disability by patient age
Dr. Ramanujam and colleagues constructed their measure using the ARMSS score, which ranks EDSS score by age instead of by disease duration. The ARMSS score ranges from 0 to 10, and the median value is 5 for all patients at a given age. Investigators can calculate the score using a previously published global matrix of values for ARMSS and MSSS available in the R package ms.sev.
The investigators found that the ARMSS score is slightly superior to the MSSS in detecting small increases in EDSS. One benefit of the ARMSS score, compared with the MSSS, is that it allows investigators to study patients for whom time of disease onset is unknown. The ARMSS score also removes potential systematic bias that might result from a neurologist’s retrospective assignment of date of disease onset, said Dr. Ramanujam.
He and his colleagues used ARMSS to compare patients’ disease course with what is expected for that patient (i.e., an ARMSS that remains stable at 5). They extracted data for 15,831 patients participating in the Swedish MS registry, including age and EDSS score at each neurological visit. Eligible patients had serial EDSS scores for 10 years. Dr. Ramanujam and colleagues included 4,514 patients in their analysis.
Measures at 2 years correlated with those at 10 years
The researchers created what they called the ARMSS integral by calculating the ARMSS score’s change from 5 at each examination (e.g., −0.5 or 1). “The ARMSS integral can be thought of as the cumulative disability that a patient accrues over his or her disease course, relative to the average patient, who had the disease for the same ages,” said Dr. Ramanujam. At 2 years of follow-up and at 10 years of follow-up, the distribution of ARMSS integrals for the study population followed a normal pattern.
Next, the investigators sought to compare patients by standardizing their follow-up time. To do this, they calculated what they called the ARMSS-rate by dividing each patient’s ARMSS integral by the number of years of follow-up. The ARMSS-rate offers a “snapshot of disease severity and progression,” said Dr. Ramanujam. When the researchers compared ARMSS-rates at 2 years and 10 years for each patient, they found that the measure was “extremely stable over time and strongly correlated with future disability.” The correlation improved slightly when the researchers compared ARMSS-rates at 4 years and 10 years.
The investigators then categorized patients based on their ARMSS-rate at 2 years (e.g., 0 to 1, 1 to 2, 2 to 3). When they compared the values in these categories with the median ARMSS-rates for the same individuals over the subsequent 8 years, they found strong group-level correlations.
To analyze correlations on an individual level, Dr. Ramanujam and colleagues examined the ability of different metrics at the time closest to 2 years of follow-up to predict those measured at 10 years. They assigned the value 1 to the most severe quartile of outcomes and the value 0 to all other quartiles. For predictors and outcomes, the investigators examined ARMSS-rate and the integral of progression index, which they calculated using the integral of EDSS. They also included EDSS at 10 years as an outcome for progression index.
For predicting the subsequent 8 years of ARMSS-rates, ARMSS-rate at 2 years had an area under the curve (AUC) of 0.921. When the investigators performed the same analysis using a cohort of patients with MS from British Columbia, Canada, they obtained an AUC of 0.887. Progression index at 2 years had an AUC of 0.61 for predicting the most severe quartile of the next 8 years. Compared with this result, ARMSS integral up to 2 years was slightly better at predicting EDSS at 10 years, said Dr. Ramanujam. The progression index poorly predicted the most severe quartile of EDSS at 10 years.
The main limitation of the ARMSS integral and ARMSS-rate is that they are based on EDSS, he added. The EDSS gives great weight to mobility and largely does not measure cognitive disability. “Future metrics could therefore include additional data such as MRI, Symbol Digit Modalities Test, or neurofilament light levels,” said Dr. Ramanujam. “Also, self-assessment could be one area to improve in the future.”
Dr. Ramanujam had no conflicts of interest to disclose. He receives funding from the MultipleMS Project, which is part of the EU Horizon 2020 Framework.
STOCKHOLM – , according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. The resulting measurement is stable, not highly sensitive to age, and appropriate for research applications. “It could give a clinician an earlier indication of the potential disease course of a patient,” said Ryan Ramanujam, PhD, assistant professor of translational neuroepidemiology at Karolinska Institutet in Stockholm.
Researchers who study MS use various scores to measure disease severity, including the Expanded Disability Status Scale (EDSS) and the MS Severity Scale (MSSS). These scores cannot predict a patient’s future status, however, and they do not remain stable throughout the course of a patient’s disease. Fitting a linear model over a series of scores over time can provide a misleading impression of a patient’s disease progression. “What we need is a metric to give a holistic overview of disease course, regardless of when it’s measured in a patient’s disease progression,” said Dr. Ramanujam. Such a measurement could aid the search for genes that affect MS severity, he added.
Examining disability by patient age
Dr. Ramanujam and colleagues constructed their measure using the ARMSS score, which ranks EDSS score by age instead of by disease duration. The ARMSS score ranges from 0 to 10, and the median value is 5 for all patients at a given age. Investigators can calculate the score using a previously published global matrix of values for ARMSS and MSSS available in the R package ms.sev.
The investigators found that the ARMSS score is slightly superior to the MSSS in detecting small increases in EDSS. One benefit of the ARMSS score, compared with the MSSS, is that it allows investigators to study patients for whom time of disease onset is unknown. The ARMSS score also removes potential systematic bias that might result from a neurologist’s retrospective assignment of date of disease onset, said Dr. Ramanujam.
He and his colleagues used ARMSS to compare patients’ disease course with what is expected for that patient (i.e., an ARMSS that remains stable at 5). They extracted data for 15,831 patients participating in the Swedish MS registry, including age and EDSS score at each neurological visit. Eligible patients had serial EDSS scores for 10 years. Dr. Ramanujam and colleagues included 4,514 patients in their analysis.
Measures at 2 years correlated with those at 10 years
The researchers created what they called the ARMSS integral by calculating the ARMSS score’s change from 5 at each examination (e.g., −0.5 or 1). “The ARMSS integral can be thought of as the cumulative disability that a patient accrues over his or her disease course, relative to the average patient, who had the disease for the same ages,” said Dr. Ramanujam. At 2 years of follow-up and at 10 years of follow-up, the distribution of ARMSS integrals for the study population followed a normal pattern.
Next, the investigators sought to compare patients by standardizing their follow-up time. To do this, they calculated what they called the ARMSS-rate by dividing each patient’s ARMSS integral by the number of years of follow-up. The ARMSS-rate offers a “snapshot of disease severity and progression,” said Dr. Ramanujam. When the researchers compared ARMSS-rates at 2 years and 10 years for each patient, they found that the measure was “extremely stable over time and strongly correlated with future disability.” The correlation improved slightly when the researchers compared ARMSS-rates at 4 years and 10 years.
The investigators then categorized patients based on their ARMSS-rate at 2 years (e.g., 0 to 1, 1 to 2, 2 to 3). When they compared the values in these categories with the median ARMSS-rates for the same individuals over the subsequent 8 years, they found strong group-level correlations.
To analyze correlations on an individual level, Dr. Ramanujam and colleagues examined the ability of different metrics at the time closest to 2 years of follow-up to predict those measured at 10 years. They assigned the value 1 to the most severe quartile of outcomes and the value 0 to all other quartiles. For predictors and outcomes, the investigators examined ARMSS-rate and the integral of progression index, which they calculated using the integral of EDSS. They also included EDSS at 10 years as an outcome for progression index.
For predicting the subsequent 8 years of ARMSS-rates, ARMSS-rate at 2 years had an area under the curve (AUC) of 0.921. When the investigators performed the same analysis using a cohort of patients with MS from British Columbia, Canada, they obtained an AUC of 0.887. Progression index at 2 years had an AUC of 0.61 for predicting the most severe quartile of the next 8 years. Compared with this result, ARMSS integral up to 2 years was slightly better at predicting EDSS at 10 years, said Dr. Ramanujam. The progression index poorly predicted the most severe quartile of EDSS at 10 years.
The main limitation of the ARMSS integral and ARMSS-rate is that they are based on EDSS, he added. The EDSS gives great weight to mobility and largely does not measure cognitive disability. “Future metrics could therefore include additional data such as MRI, Symbol Digit Modalities Test, or neurofilament light levels,” said Dr. Ramanujam. “Also, self-assessment could be one area to improve in the future.”
Dr. Ramanujam had no conflicts of interest to disclose. He receives funding from the MultipleMS Project, which is part of the EU Horizon 2020 Framework.
REPORTING FROM ECTRIMS 2019
Continuation of natalizumab treatment reduces risk of MS relapses during pregnancy
STOCKHOLM – according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. Continuation of treatment is not associated with major fetal risks.
Pregnancy influences the choice of treatment for patients with MS. Not all therapies are compatible with pregnancy; the newer, more effective treatments in particular may pose risks in this regard. “There is a need to accumulate new data on how to manage our highly active patients with MS – in particular, patients who are treated with natalizumab,” said Doriana Landi, MD, PhD, a research fellow at the University of Rome Tor Vergata.
Data suggest that suspension of natalizumab before pregnancy is associated with significant disease worsening. In 2018, Portaccio et al. found that suspending natalizumab treatment before conception is associated with a higher risk of relapses during pregnancy (Neurology. 2018 Mar 6;90[10]:e832-9). Suspending natalizumab treatment at conception, however, reduced the risk of relapse by a factor of three. Other data have suggested that continuing natalizumab treatment until the 30th week of gestation could protect mothers and guarantee fetal safety.
Comparing two cohorts of women with MS
To investigate this question further, Dr. Landi and colleagues investigated a cohort of 29 women with MS who were receiving natalizumab and became pregnant. They compared this cohort’s outcomes with those of the cohort that Portaccio et al. had studied. The investigators categorized participants in both cohorts into three groups according to the time of their last infusion of natalizumab in relation to their last menstrual period. Group 0 had their last infusion before their last menstrual period, group 1 had their last infusion during the first trimester of pregnancy, and group 2 continued treatment after the first trimester. All women restarted natalizumab post partum and had at least 12 months of follow-up after delivery.
Dr. Landi and colleagues calculated the annualized relapse rate during pregnancy and during 12 months post partum for all groups. They also compared the outcomes of newborns between groups.
Prematurity may have influenced rate of hematologic complications
In all, the researchers analyzed 90 completed pregnancies in 86 women with MS. There were no significant demographic differences between groups. The overall population’s mean age was approximately 31 years, and its median Expanded Disability Status Scale (EDSS) score was about 2. The women gave birth to 94 newborns. Mean gestational age was 38.42 weeks, mean birth weight was 2,878.08 mg, and mean length was 48.23 cm.
Group 0 included 31 patients, group 1 included 30 patients, and group 2 included 28 patients. The median interval between the last dose of natalizumab and last menstrual period was 70 days for group 0, 21 days for group 1, and 197 days for group 2. Group 2 received a median of five natalizumab infusions during pregnancy, with a median interval of 80 days between the last prepartum dose and delivery. The median interval between last prepartum dose and the first postpartum dose was 411 days in group 0, 288 in group 1, and 103 in group 2.
Most pregnancies in group 2 were exposed to natalizumab for at least 28 weeks of gestation. Women in group 2 restarted natalizumab treatment significantly earlier, compared with women in the other groups.
Group 0 had a significantly increased ARR during and after pregnancy, compared with the other groups, and group 2 had the lowest ARR during pregnancy. The mean ARR during pregnancy was 1.06 in group 0, 0.49 in group 1, and 0.09 in group 2. The ARR decreased to 0 in pregnancies exposed to natalizumab for more than 90 days. The mean ARR post partum was 0.39 in group 0, 0.23 in group 1, and 0.10 in group 2. Women in group 0 and group 1 had a higher EDSS during pregnancy than before conception.
Newborns’ mean gestational age, birth weight, and length did not differ significantly between groups. Five newborns in group 2, three of whom were premature, had anemia. This outcome is consistent with previous findings, and prematurity may be a confounding factor, said Dr. Landi. The frequency of birth defects was higher in group 2 than in the other groups, but most of them occurred in one twin, said Dr. Landi. The investigators observed malformations in one group 0 newborn (minor), four group 1 newborns (five minor and one major), and four (two minor and four major) group 2 newborns.
In pregnancy during which natalizumab treatment is prolonged until the third trimester, treatment should be restarted after delivery within 2 weeks of the last infusion to avoid potential doubled rebound, said Dr. Landi. Future studies should examine whether extended dosing is as effective as regular dosing. A larger sample size is needed to estimate risks correctly for newborns in exposed pregnancies and counsel patients appropriately.
Dr. Landi reported receiving travel funding from Biogen, Merck Serono, Sanofi-Genzyme, and Teva; honoraria for speaking from Sanofi-Genzyme and Teva; and consultation fees from Merck Serono and Teva. She is an investigator in clinical trials being conducted for Biogen, Merck Serono, Novartis, Roche, and Teva.
SOURCE: Landi D et al. ECTRIMS 2019, Abstract 338.
STOCKHOLM – according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. Continuation of treatment is not associated with major fetal risks.
Pregnancy influences the choice of treatment for patients with MS. Not all therapies are compatible with pregnancy; the newer, more effective treatments in particular may pose risks in this regard. “There is a need to accumulate new data on how to manage our highly active patients with MS – in particular, patients who are treated with natalizumab,” said Doriana Landi, MD, PhD, a research fellow at the University of Rome Tor Vergata.
Data suggest that suspension of natalizumab before pregnancy is associated with significant disease worsening. In 2018, Portaccio et al. found that suspending natalizumab treatment before conception is associated with a higher risk of relapses during pregnancy (Neurology. 2018 Mar 6;90[10]:e832-9). Suspending natalizumab treatment at conception, however, reduced the risk of relapse by a factor of three. Other data have suggested that continuing natalizumab treatment until the 30th week of gestation could protect mothers and guarantee fetal safety.
Comparing two cohorts of women with MS
To investigate this question further, Dr. Landi and colleagues investigated a cohort of 29 women with MS who were receiving natalizumab and became pregnant. They compared this cohort’s outcomes with those of the cohort that Portaccio et al. had studied. The investigators categorized participants in both cohorts into three groups according to the time of their last infusion of natalizumab in relation to their last menstrual period. Group 0 had their last infusion before their last menstrual period, group 1 had their last infusion during the first trimester of pregnancy, and group 2 continued treatment after the first trimester. All women restarted natalizumab post partum and had at least 12 months of follow-up after delivery.
Dr. Landi and colleagues calculated the annualized relapse rate during pregnancy and during 12 months post partum for all groups. They also compared the outcomes of newborns between groups.
Prematurity may have influenced rate of hematologic complications
In all, the researchers analyzed 90 completed pregnancies in 86 women with MS. There were no significant demographic differences between groups. The overall population’s mean age was approximately 31 years, and its median Expanded Disability Status Scale (EDSS) score was about 2. The women gave birth to 94 newborns. Mean gestational age was 38.42 weeks, mean birth weight was 2,878.08 mg, and mean length was 48.23 cm.
Group 0 included 31 patients, group 1 included 30 patients, and group 2 included 28 patients. The median interval between the last dose of natalizumab and last menstrual period was 70 days for group 0, 21 days for group 1, and 197 days for group 2. Group 2 received a median of five natalizumab infusions during pregnancy, with a median interval of 80 days between the last prepartum dose and delivery. The median interval between last prepartum dose and the first postpartum dose was 411 days in group 0, 288 in group 1, and 103 in group 2.
Most pregnancies in group 2 were exposed to natalizumab for at least 28 weeks of gestation. Women in group 2 restarted natalizumab treatment significantly earlier, compared with women in the other groups.
Group 0 had a significantly increased ARR during and after pregnancy, compared with the other groups, and group 2 had the lowest ARR during pregnancy. The mean ARR during pregnancy was 1.06 in group 0, 0.49 in group 1, and 0.09 in group 2. The ARR decreased to 0 in pregnancies exposed to natalizumab for more than 90 days. The mean ARR post partum was 0.39 in group 0, 0.23 in group 1, and 0.10 in group 2. Women in group 0 and group 1 had a higher EDSS during pregnancy than before conception.
Newborns’ mean gestational age, birth weight, and length did not differ significantly between groups. Five newborns in group 2, three of whom were premature, had anemia. This outcome is consistent with previous findings, and prematurity may be a confounding factor, said Dr. Landi. The frequency of birth defects was higher in group 2 than in the other groups, but most of them occurred in one twin, said Dr. Landi. The investigators observed malformations in one group 0 newborn (minor), four group 1 newborns (five minor and one major), and four (two minor and four major) group 2 newborns.
In pregnancy during which natalizumab treatment is prolonged until the third trimester, treatment should be restarted after delivery within 2 weeks of the last infusion to avoid potential doubled rebound, said Dr. Landi. Future studies should examine whether extended dosing is as effective as regular dosing. A larger sample size is needed to estimate risks correctly for newborns in exposed pregnancies and counsel patients appropriately.
Dr. Landi reported receiving travel funding from Biogen, Merck Serono, Sanofi-Genzyme, and Teva; honoraria for speaking from Sanofi-Genzyme and Teva; and consultation fees from Merck Serono and Teva. She is an investigator in clinical trials being conducted for Biogen, Merck Serono, Novartis, Roche, and Teva.
SOURCE: Landi D et al. ECTRIMS 2019, Abstract 338.
STOCKHOLM – according to research presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis. Continuation of treatment is not associated with major fetal risks.
Pregnancy influences the choice of treatment for patients with MS. Not all therapies are compatible with pregnancy; the newer, more effective treatments in particular may pose risks in this regard. “There is a need to accumulate new data on how to manage our highly active patients with MS – in particular, patients who are treated with natalizumab,” said Doriana Landi, MD, PhD, a research fellow at the University of Rome Tor Vergata.
Data suggest that suspension of natalizumab before pregnancy is associated with significant disease worsening. In 2018, Portaccio et al. found that suspending natalizumab treatment before conception is associated with a higher risk of relapses during pregnancy (Neurology. 2018 Mar 6;90[10]:e832-9). Suspending natalizumab treatment at conception, however, reduced the risk of relapse by a factor of three. Other data have suggested that continuing natalizumab treatment until the 30th week of gestation could protect mothers and guarantee fetal safety.
Comparing two cohorts of women with MS
To investigate this question further, Dr. Landi and colleagues investigated a cohort of 29 women with MS who were receiving natalizumab and became pregnant. They compared this cohort’s outcomes with those of the cohort that Portaccio et al. had studied. The investigators categorized participants in both cohorts into three groups according to the time of their last infusion of natalizumab in relation to their last menstrual period. Group 0 had their last infusion before their last menstrual period, group 1 had their last infusion during the first trimester of pregnancy, and group 2 continued treatment after the first trimester. All women restarted natalizumab post partum and had at least 12 months of follow-up after delivery.
Dr. Landi and colleagues calculated the annualized relapse rate during pregnancy and during 12 months post partum for all groups. They also compared the outcomes of newborns between groups.
Prematurity may have influenced rate of hematologic complications
In all, the researchers analyzed 90 completed pregnancies in 86 women with MS. There were no significant demographic differences between groups. The overall population’s mean age was approximately 31 years, and its median Expanded Disability Status Scale (EDSS) score was about 2. The women gave birth to 94 newborns. Mean gestational age was 38.42 weeks, mean birth weight was 2,878.08 mg, and mean length was 48.23 cm.
Group 0 included 31 patients, group 1 included 30 patients, and group 2 included 28 patients. The median interval between the last dose of natalizumab and last menstrual period was 70 days for group 0, 21 days for group 1, and 197 days for group 2. Group 2 received a median of five natalizumab infusions during pregnancy, with a median interval of 80 days between the last prepartum dose and delivery. The median interval between last prepartum dose and the first postpartum dose was 411 days in group 0, 288 in group 1, and 103 in group 2.
Most pregnancies in group 2 were exposed to natalizumab for at least 28 weeks of gestation. Women in group 2 restarted natalizumab treatment significantly earlier, compared with women in the other groups.
Group 0 had a significantly increased ARR during and after pregnancy, compared with the other groups, and group 2 had the lowest ARR during pregnancy. The mean ARR during pregnancy was 1.06 in group 0, 0.49 in group 1, and 0.09 in group 2. The ARR decreased to 0 in pregnancies exposed to natalizumab for more than 90 days. The mean ARR post partum was 0.39 in group 0, 0.23 in group 1, and 0.10 in group 2. Women in group 0 and group 1 had a higher EDSS during pregnancy than before conception.
Newborns’ mean gestational age, birth weight, and length did not differ significantly between groups. Five newborns in group 2, three of whom were premature, had anemia. This outcome is consistent with previous findings, and prematurity may be a confounding factor, said Dr. Landi. The frequency of birth defects was higher in group 2 than in the other groups, but most of them occurred in one twin, said Dr. Landi. The investigators observed malformations in one group 0 newborn (minor), four group 1 newborns (five minor and one major), and four (two minor and four major) group 2 newborns.
In pregnancy during which natalizumab treatment is prolonged until the third trimester, treatment should be restarted after delivery within 2 weeks of the last infusion to avoid potential doubled rebound, said Dr. Landi. Future studies should examine whether extended dosing is as effective as regular dosing. A larger sample size is needed to estimate risks correctly for newborns in exposed pregnancies and counsel patients appropriately.
Dr. Landi reported receiving travel funding from Biogen, Merck Serono, Sanofi-Genzyme, and Teva; honoraria for speaking from Sanofi-Genzyme and Teva; and consultation fees from Merck Serono and Teva. She is an investigator in clinical trials being conducted for Biogen, Merck Serono, Novartis, Roche, and Teva.
SOURCE: Landi D et al. ECTRIMS 2019, Abstract 338.
REPORTING FROM ECTRIMS 2019
Many institutions exceed recommended radiation doses during lung cancer screening
according to a study published in JAMA Internal Medicine.
Various institutional characteristics, such as allowing any radiologist to establish CT scan protocols, are associated with a greater likelihood of using higher radiation doses. “Dose optimization practices may benefit from being tailored to specific practice types, as well as different organizational structures, to have a higher likelihood of meeting dose guidelines,” wrote Joshua Demb, PhD, MPH, a cancer epidemiologist at the University of California, San Diego, and colleagues.
Lung cancer screening benefits patients when low-dose CT is used, but not when high-dose CT is used, because radiation from higher doses may cause as many cancers as are detected by screening. The Centers for Medicare & Medicaid Services require institutions to use low-dose techniques and participate in a dose registry to be reimbursed for lung cancer screening. The American College of Radiology recommends that lung cancer screening scans have a volume CT dose index (CTDIvol) of 3 mGy or lower and an effective dose (ED) of 1 millisieverts (mSv) or lower.
A prospective study of registry data
Dr. Demb and colleagues conducted a study to describe CT radiation doses for lung cancer screening in current practice and to identify the factors that explain variation in doses between institutions. They prospectively collected lung cancer screening examination dose metrics from 2016 to 2017 at U.S. institutions participating in the University of California, San Francisco, International Dose Registry. Eligible institutions performed a minimum of 24 lung cancer screening scans during the study period. At baseline, the investigators surveyed institutions about their characteristics (for example, how they perform and oversee CT). Dr. Demb and colleagues estimated mixed-effects linear and logistic regression models using forward variable selection. They conducted their analysis between 2018 and 2019.
The researchers chose four outcome measures. The first was mean CTDIvol, reflecting the average radiation dose per slice. The second was mean ED, reflecting the total dose received and estimated future cancer risk. The third was the proportion of CT scans using radiation doses above ACR benchmarks. The fourth was the proportion of CT scans using radiation doses above the 75th percentile of registry doses (CTDIvol greater than 2.7 mGy and ED greater than 1.4 mSv).
Institutional characteristics associated with radiation dose
Dr. Demb and colleagues collected data from 72 institutions about 12,529 patients undergoing CT scans for lung cancer screening. Approximately 58% of patients were men, and the patients’ median age was 65 years. The mean CTDIvol, adjusted for patient size, was 2.4 mGy. The mean ED for lung cancer screening, adjusted for chest diameter, was 1.2 mSv.
A total of 15 institutions (21%) had a median adjusted CTDIvol value higher than the ACR guideline, and 47 (65%) had a median adjusted ED higher than the ACR guideline. Approximately 18% of CT scans had a CTDIvol higher than guidelines, and 50% had an ED higher than ACR guidelines.
Institutions that permitted any radiologist to establish CT protocols had 44% higher mean CTDIvol and 27% higher mean ED, compared with institutions that restricted who could establish protocols. Institutions that permitted any radiologist to establish protocols also had higher odds of conducting examinations that exceeded ACR CTDIvol guidelines (odds ratio, 12.0) and of being in the 75th percentile of the registry CTDIvol (OR, 19.0) or ED (OR, 8.5) values.
In contrast, having lead radiologists establish CT protocols resulted in lower odds of using doses that exceeded ACR ED guidelines (OR, 0.01). Employing external, rather than internal, medical physicists was associated with increased odds of exceeding ACR CTDIvol guidelines (OR, 6.1). Having medical physicists establish protocols was associated with decreased odds of exceeding the 75th percentile of the registry CTDIvol (OR, 0.09) values. Institutions that updated protocols as needed, rather than annually, had 27% higher mean CTDIvol.
“Although we cannot establish causality in this observational study, our results suggest that considering these factors (for example, allowing only lead radiologists to establish protocols) could have a meaningful impact on dose, and could be important areas to develop interventions to optimize doses of CT protocols” the investigators wrote.
The Patient Centered Outcomes Research Institute and the National Institutes of Health supported this research. The authors reported no conflicts of interest.
SOURCE: Demb J et al. JAMA Intern Med. 2019 Sep 23. doi: 10.1001/jamainternmed.2019.3893.
according to a study published in JAMA Internal Medicine.
Various institutional characteristics, such as allowing any radiologist to establish CT scan protocols, are associated with a greater likelihood of using higher radiation doses. “Dose optimization practices may benefit from being tailored to specific practice types, as well as different organizational structures, to have a higher likelihood of meeting dose guidelines,” wrote Joshua Demb, PhD, MPH, a cancer epidemiologist at the University of California, San Diego, and colleagues.
Lung cancer screening benefits patients when low-dose CT is used, but not when high-dose CT is used, because radiation from higher doses may cause as many cancers as are detected by screening. The Centers for Medicare & Medicaid Services require institutions to use low-dose techniques and participate in a dose registry to be reimbursed for lung cancer screening. The American College of Radiology recommends that lung cancer screening scans have a volume CT dose index (CTDIvol) of 3 mGy or lower and an effective dose (ED) of 1 millisieverts (mSv) or lower.
A prospective study of registry data
Dr. Demb and colleagues conducted a study to describe CT radiation doses for lung cancer screening in current practice and to identify the factors that explain variation in doses between institutions. They prospectively collected lung cancer screening examination dose metrics from 2016 to 2017 at U.S. institutions participating in the University of California, San Francisco, International Dose Registry. Eligible institutions performed a minimum of 24 lung cancer screening scans during the study period. At baseline, the investigators surveyed institutions about their characteristics (for example, how they perform and oversee CT). Dr. Demb and colleagues estimated mixed-effects linear and logistic regression models using forward variable selection. They conducted their analysis between 2018 and 2019.
The researchers chose four outcome measures. The first was mean CTDIvol, reflecting the average radiation dose per slice. The second was mean ED, reflecting the total dose received and estimated future cancer risk. The third was the proportion of CT scans using radiation doses above ACR benchmarks. The fourth was the proportion of CT scans using radiation doses above the 75th percentile of registry doses (CTDIvol greater than 2.7 mGy and ED greater than 1.4 mSv).
Institutional characteristics associated with radiation dose
Dr. Demb and colleagues collected data from 72 institutions about 12,529 patients undergoing CT scans for lung cancer screening. Approximately 58% of patients were men, and the patients’ median age was 65 years. The mean CTDIvol, adjusted for patient size, was 2.4 mGy. The mean ED for lung cancer screening, adjusted for chest diameter, was 1.2 mSv.
A total of 15 institutions (21%) had a median adjusted CTDIvol value higher than the ACR guideline, and 47 (65%) had a median adjusted ED higher than the ACR guideline. Approximately 18% of CT scans had a CTDIvol higher than guidelines, and 50% had an ED higher than ACR guidelines.
Institutions that permitted any radiologist to establish CT protocols had 44% higher mean CTDIvol and 27% higher mean ED, compared with institutions that restricted who could establish protocols. Institutions that permitted any radiologist to establish protocols also had higher odds of conducting examinations that exceeded ACR CTDIvol guidelines (odds ratio, 12.0) and of being in the 75th percentile of the registry CTDIvol (OR, 19.0) or ED (OR, 8.5) values.
In contrast, having lead radiologists establish CT protocols resulted in lower odds of using doses that exceeded ACR ED guidelines (OR, 0.01). Employing external, rather than internal, medical physicists was associated with increased odds of exceeding ACR CTDIvol guidelines (OR, 6.1). Having medical physicists establish protocols was associated with decreased odds of exceeding the 75th percentile of the registry CTDIvol (OR, 0.09) values. Institutions that updated protocols as needed, rather than annually, had 27% higher mean CTDIvol.
“Although we cannot establish causality in this observational study, our results suggest that considering these factors (for example, allowing only lead radiologists to establish protocols) could have a meaningful impact on dose, and could be important areas to develop interventions to optimize doses of CT protocols” the investigators wrote.
The Patient Centered Outcomes Research Institute and the National Institutes of Health supported this research. The authors reported no conflicts of interest.
SOURCE: Demb J et al. JAMA Intern Med. 2019 Sep 23. doi: 10.1001/jamainternmed.2019.3893.
according to a study published in JAMA Internal Medicine.
Various institutional characteristics, such as allowing any radiologist to establish CT scan protocols, are associated with a greater likelihood of using higher radiation doses. “Dose optimization practices may benefit from being tailored to specific practice types, as well as different organizational structures, to have a higher likelihood of meeting dose guidelines,” wrote Joshua Demb, PhD, MPH, a cancer epidemiologist at the University of California, San Diego, and colleagues.
Lung cancer screening benefits patients when low-dose CT is used, but not when high-dose CT is used, because radiation from higher doses may cause as many cancers as are detected by screening. The Centers for Medicare & Medicaid Services require institutions to use low-dose techniques and participate in a dose registry to be reimbursed for lung cancer screening. The American College of Radiology recommends that lung cancer screening scans have a volume CT dose index (CTDIvol) of 3 mGy or lower and an effective dose (ED) of 1 millisieverts (mSv) or lower.
A prospective study of registry data
Dr. Demb and colleagues conducted a study to describe CT radiation doses for lung cancer screening in current practice and to identify the factors that explain variation in doses between institutions. They prospectively collected lung cancer screening examination dose metrics from 2016 to 2017 at U.S. institutions participating in the University of California, San Francisco, International Dose Registry. Eligible institutions performed a minimum of 24 lung cancer screening scans during the study period. At baseline, the investigators surveyed institutions about their characteristics (for example, how they perform and oversee CT). Dr. Demb and colleagues estimated mixed-effects linear and logistic regression models using forward variable selection. They conducted their analysis between 2018 and 2019.
The researchers chose four outcome measures. The first was mean CTDIvol, reflecting the average radiation dose per slice. The second was mean ED, reflecting the total dose received and estimated future cancer risk. The third was the proportion of CT scans using radiation doses above ACR benchmarks. The fourth was the proportion of CT scans using radiation doses above the 75th percentile of registry doses (CTDIvol greater than 2.7 mGy and ED greater than 1.4 mSv).
Institutional characteristics associated with radiation dose
Dr. Demb and colleagues collected data from 72 institutions about 12,529 patients undergoing CT scans for lung cancer screening. Approximately 58% of patients were men, and the patients’ median age was 65 years. The mean CTDIvol, adjusted for patient size, was 2.4 mGy. The mean ED for lung cancer screening, adjusted for chest diameter, was 1.2 mSv.
A total of 15 institutions (21%) had a median adjusted CTDIvol value higher than the ACR guideline, and 47 (65%) had a median adjusted ED higher than the ACR guideline. Approximately 18% of CT scans had a CTDIvol higher than guidelines, and 50% had an ED higher than ACR guidelines.
Institutions that permitted any radiologist to establish CT protocols had 44% higher mean CTDIvol and 27% higher mean ED, compared with institutions that restricted who could establish protocols. Institutions that permitted any radiologist to establish protocols also had higher odds of conducting examinations that exceeded ACR CTDIvol guidelines (odds ratio, 12.0) and of being in the 75th percentile of the registry CTDIvol (OR, 19.0) or ED (OR, 8.5) values.
In contrast, having lead radiologists establish CT protocols resulted in lower odds of using doses that exceeded ACR ED guidelines (OR, 0.01). Employing external, rather than internal, medical physicists was associated with increased odds of exceeding ACR CTDIvol guidelines (OR, 6.1). Having medical physicists establish protocols was associated with decreased odds of exceeding the 75th percentile of the registry CTDIvol (OR, 0.09) values. Institutions that updated protocols as needed, rather than annually, had 27% higher mean CTDIvol.
“Although we cannot establish causality in this observational study, our results suggest that considering these factors (for example, allowing only lead radiologists to establish protocols) could have a meaningful impact on dose, and could be important areas to develop interventions to optimize doses of CT protocols” the investigators wrote.
The Patient Centered Outcomes Research Institute and the National Institutes of Health supported this research. The authors reported no conflicts of interest.
SOURCE: Demb J et al. JAMA Intern Med. 2019 Sep 23. doi: 10.1001/jamainternmed.2019.3893.
FROM JAMA INTERNAL MEDICINE
Key clinical point: A significant proportion of institutions exceed guideline-recommended dose levels for CT screening for lung cancer.
Major finding: About 21% of institutions have median volume CT dose index above American College of Radiology guidelines, and 65% have median effective dose above ACR guidelines.
Study details: A prospective study of data for 12,529 patients undergoing screening at 72 institutions.
Disclosures: The Patient Centered Outcomes Research Institute and the National Institutes of Health supported this research. The authors reported no conflicts of interest.
Source: Demb J et al. JAMA Intern Med. 2019 Sep 23. doi: 10.1001/jamainternmed.2019.3893.
Ofatumumab has superior efficacy in relapsing-remitting MS, compared with teriflunomide
STOCKHOLM – (MS), according to research presented at the annual congress of the European Committee for Treatment and Research in MS. Ofatumumab also reduces the risk of 3-month and 6-month confirmed disability worsening, compared with teriflunomide. The former therapy has a favorable safety profile, and the investigators did not observe any unexpected safety findings.
Ofatumumab is a fully human anti-CD20 monoclonal antibody that Novartis is developing as a monthly 20-mg subcutaneous infusion. “Targeting CD20-bearing B-cells has been shown to be an effective therapeutic against MS,” said Stephen Hauser, MD, professor of neurology at the University of California, San Francisco. “CD20 targeting is very effective at nearly complete depletion of B-cells in the blood, but [performs] only partial depletion in lymph nodes. This may explain, in part, its safety profile.”
Two concurrent phase 3 trials
Dr. Hauser and colleagues conducted two contemporaneous phase 3 trials, ASCLEPIOS I and ASCLEPIOS II, to compare the efficacy and safety of ofatumumab with those of teriflunomide. The two multicenter trials were double blinded and had a parallel-group design. Eligible patients were between ages 18 and 55 years; had an Expanded Disability Status Scale (EDSS) score of 0 to 5.5; and had had one or more relapse in the previous year, two or more relapses in the previous 2 years, or a positive gadolinium-enhancing MRI scan during the year before randomization. Patients with progressive MS, neuromyelitis optica, or progressive multifocal leukoencephalopathy were excluded.
The investigators randomized patients in equal groups to receive 20-mg subcutaneous injections of ofatumumab every 4 weeks (plus a daily oral placebo) or 14 mg/day of teriflunomide orally (plus placebo subcutaneous injections). Participants randomized to ofatumumab underwent an initial loading regimen of 20-mg subcutaneous doses on days 1, 7, and 14. The trials had flexible durations: The number of events determined the length of the studies, which could last for as long as 30 months. At study completion, participants were enrolled into an ongoing, open-label extension study.
The primary endpoint of both trials was the annualized relapse rate (ARR). Among the secondary endpoints were 3- and 6-month confirmed disability worsening, 6-month confirmed disability improvement, MRI-related outcomes, and serum neurofilament light chain (NfL) levels.
Ofatumumab improved clinical and imaging outcomes
In all, 927 patients were randomized in ASCLEPIOS I (462 to teriflunomide and 465 to ofatumumab), and 955 patients were randomized in ASCLEPIOS II (474 to teriflunomide and 481 to ofatumumab). The study completion rate was approximately 85% in ASCLEPIOS I and approximately 82% in ASCLEPIOS II. The two studies had similar populations, and the two treatment arms in each trial were well balanced. Overall, mean age was approximately 38 years, 68% of patients were female, mean disease duration was approximately 8 years, and mean EDSS score was about 3.
Compared with teriflunomide, ofatumumab reduced the ARR by 50.5% in ASCLEPIOS I and by 58.5% in ASCLEPIOS II. Ofatumumab reduced the risk of 3-month confirmed disability worsening by 34.4%, compared with teriflunomide, and reduced the risk of 6-month confirmed disability worsening by 32.5%, compared with teriflunomide. All of these differences were statistically significant. Ofatumumab tended to increase the likelihood of confirmed disability improvement, compared with teriflunomide, but the result was not statistically significant.
Ofatumumab was superior to teriflunomide on imaging and laboratory measures, as well. Compared with teriflunomide, ofatumumab significantly reduced gadolinium-enhancing T1 lesions by 97.5% in ASCLEPIOS I and by 93.8% in ASCLEPIOS II. In addition, ofatumumab significantly reduced new or enlarging T2 lesions by 82.0% in ASCLEPIOS I and by 84.5% in ASCLEPIOS II. At month 24, ofatumumab reduced serum NfL levels by 23% in ASCLEPIOS I and by 24% in ASCLEPIOS II, compared with teriflunomide.
In both studies, adverse events and serious adverse events were well balanced between treatment groups. The ofatumumab groups had a slight increase in injection-related reactions, compared with the teriflunomide groups. Most systemic injection reactions were mild to moderate.
Novartis Pharma funded the research. Dr. Hauser has received travel reimbursement from F. Hoffmann-La Roche and Novartis for meetings and presentations related to anti-CD20 therapies.
STOCKHOLM – (MS), according to research presented at the annual congress of the European Committee for Treatment and Research in MS. Ofatumumab also reduces the risk of 3-month and 6-month confirmed disability worsening, compared with teriflunomide. The former therapy has a favorable safety profile, and the investigators did not observe any unexpected safety findings.
Ofatumumab is a fully human anti-CD20 monoclonal antibody that Novartis is developing as a monthly 20-mg subcutaneous infusion. “Targeting CD20-bearing B-cells has been shown to be an effective therapeutic against MS,” said Stephen Hauser, MD, professor of neurology at the University of California, San Francisco. “CD20 targeting is very effective at nearly complete depletion of B-cells in the blood, but [performs] only partial depletion in lymph nodes. This may explain, in part, its safety profile.”
Two concurrent phase 3 trials
Dr. Hauser and colleagues conducted two contemporaneous phase 3 trials, ASCLEPIOS I and ASCLEPIOS II, to compare the efficacy and safety of ofatumumab with those of teriflunomide. The two multicenter trials were double blinded and had a parallel-group design. Eligible patients were between ages 18 and 55 years; had an Expanded Disability Status Scale (EDSS) score of 0 to 5.5; and had had one or more relapse in the previous year, two or more relapses in the previous 2 years, or a positive gadolinium-enhancing MRI scan during the year before randomization. Patients with progressive MS, neuromyelitis optica, or progressive multifocal leukoencephalopathy were excluded.
The investigators randomized patients in equal groups to receive 20-mg subcutaneous injections of ofatumumab every 4 weeks (plus a daily oral placebo) or 14 mg/day of teriflunomide orally (plus placebo subcutaneous injections). Participants randomized to ofatumumab underwent an initial loading regimen of 20-mg subcutaneous doses on days 1, 7, and 14. The trials had flexible durations: The number of events determined the length of the studies, which could last for as long as 30 months. At study completion, participants were enrolled into an ongoing, open-label extension study.
The primary endpoint of both trials was the annualized relapse rate (ARR). Among the secondary endpoints were 3- and 6-month confirmed disability worsening, 6-month confirmed disability improvement, MRI-related outcomes, and serum neurofilament light chain (NfL) levels.
Ofatumumab improved clinical and imaging outcomes
In all, 927 patients were randomized in ASCLEPIOS I (462 to teriflunomide and 465 to ofatumumab), and 955 patients were randomized in ASCLEPIOS II (474 to teriflunomide and 481 to ofatumumab). The study completion rate was approximately 85% in ASCLEPIOS I and approximately 82% in ASCLEPIOS II. The two studies had similar populations, and the two treatment arms in each trial were well balanced. Overall, mean age was approximately 38 years, 68% of patients were female, mean disease duration was approximately 8 years, and mean EDSS score was about 3.
Compared with teriflunomide, ofatumumab reduced the ARR by 50.5% in ASCLEPIOS I and by 58.5% in ASCLEPIOS II. Ofatumumab reduced the risk of 3-month confirmed disability worsening by 34.4%, compared with teriflunomide, and reduced the risk of 6-month confirmed disability worsening by 32.5%, compared with teriflunomide. All of these differences were statistically significant. Ofatumumab tended to increase the likelihood of confirmed disability improvement, compared with teriflunomide, but the result was not statistically significant.
Ofatumumab was superior to teriflunomide on imaging and laboratory measures, as well. Compared with teriflunomide, ofatumumab significantly reduced gadolinium-enhancing T1 lesions by 97.5% in ASCLEPIOS I and by 93.8% in ASCLEPIOS II. In addition, ofatumumab significantly reduced new or enlarging T2 lesions by 82.0% in ASCLEPIOS I and by 84.5% in ASCLEPIOS II. At month 24, ofatumumab reduced serum NfL levels by 23% in ASCLEPIOS I and by 24% in ASCLEPIOS II, compared with teriflunomide.
In both studies, adverse events and serious adverse events were well balanced between treatment groups. The ofatumumab groups had a slight increase in injection-related reactions, compared with the teriflunomide groups. Most systemic injection reactions were mild to moderate.
Novartis Pharma funded the research. Dr. Hauser has received travel reimbursement from F. Hoffmann-La Roche and Novartis for meetings and presentations related to anti-CD20 therapies.
STOCKHOLM – (MS), according to research presented at the annual congress of the European Committee for Treatment and Research in MS. Ofatumumab also reduces the risk of 3-month and 6-month confirmed disability worsening, compared with teriflunomide. The former therapy has a favorable safety profile, and the investigators did not observe any unexpected safety findings.
Ofatumumab is a fully human anti-CD20 monoclonal antibody that Novartis is developing as a monthly 20-mg subcutaneous infusion. “Targeting CD20-bearing B-cells has been shown to be an effective therapeutic against MS,” said Stephen Hauser, MD, professor of neurology at the University of California, San Francisco. “CD20 targeting is very effective at nearly complete depletion of B-cells in the blood, but [performs] only partial depletion in lymph nodes. This may explain, in part, its safety profile.”
Two concurrent phase 3 trials
Dr. Hauser and colleagues conducted two contemporaneous phase 3 trials, ASCLEPIOS I and ASCLEPIOS II, to compare the efficacy and safety of ofatumumab with those of teriflunomide. The two multicenter trials were double blinded and had a parallel-group design. Eligible patients were between ages 18 and 55 years; had an Expanded Disability Status Scale (EDSS) score of 0 to 5.5; and had had one or more relapse in the previous year, two or more relapses in the previous 2 years, or a positive gadolinium-enhancing MRI scan during the year before randomization. Patients with progressive MS, neuromyelitis optica, or progressive multifocal leukoencephalopathy were excluded.
The investigators randomized patients in equal groups to receive 20-mg subcutaneous injections of ofatumumab every 4 weeks (plus a daily oral placebo) or 14 mg/day of teriflunomide orally (plus placebo subcutaneous injections). Participants randomized to ofatumumab underwent an initial loading regimen of 20-mg subcutaneous doses on days 1, 7, and 14. The trials had flexible durations: The number of events determined the length of the studies, which could last for as long as 30 months. At study completion, participants were enrolled into an ongoing, open-label extension study.
The primary endpoint of both trials was the annualized relapse rate (ARR). Among the secondary endpoints were 3- and 6-month confirmed disability worsening, 6-month confirmed disability improvement, MRI-related outcomes, and serum neurofilament light chain (NfL) levels.
Ofatumumab improved clinical and imaging outcomes
In all, 927 patients were randomized in ASCLEPIOS I (462 to teriflunomide and 465 to ofatumumab), and 955 patients were randomized in ASCLEPIOS II (474 to teriflunomide and 481 to ofatumumab). The study completion rate was approximately 85% in ASCLEPIOS I and approximately 82% in ASCLEPIOS II. The two studies had similar populations, and the two treatment arms in each trial were well balanced. Overall, mean age was approximately 38 years, 68% of patients were female, mean disease duration was approximately 8 years, and mean EDSS score was about 3.
Compared with teriflunomide, ofatumumab reduced the ARR by 50.5% in ASCLEPIOS I and by 58.5% in ASCLEPIOS II. Ofatumumab reduced the risk of 3-month confirmed disability worsening by 34.4%, compared with teriflunomide, and reduced the risk of 6-month confirmed disability worsening by 32.5%, compared with teriflunomide. All of these differences were statistically significant. Ofatumumab tended to increase the likelihood of confirmed disability improvement, compared with teriflunomide, but the result was not statistically significant.
Ofatumumab was superior to teriflunomide on imaging and laboratory measures, as well. Compared with teriflunomide, ofatumumab significantly reduced gadolinium-enhancing T1 lesions by 97.5% in ASCLEPIOS I and by 93.8% in ASCLEPIOS II. In addition, ofatumumab significantly reduced new or enlarging T2 lesions by 82.0% in ASCLEPIOS I and by 84.5% in ASCLEPIOS II. At month 24, ofatumumab reduced serum NfL levels by 23% in ASCLEPIOS I and by 24% in ASCLEPIOS II, compared with teriflunomide.
In both studies, adverse events and serious adverse events were well balanced between treatment groups. The ofatumumab groups had a slight increase in injection-related reactions, compared with the teriflunomide groups. Most systemic injection reactions were mild to moderate.
Novartis Pharma funded the research. Dr. Hauser has received travel reimbursement from F. Hoffmann-La Roche and Novartis for meetings and presentations related to anti-CD20 therapies.
REPORTING FROM ECTRIMS 2019