User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Management of Lewy body dementia remains complex
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
EXPERT ANALYSIS FROM ANA 2018
Parkinson’s prevalence varies significantly from state to state
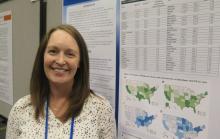
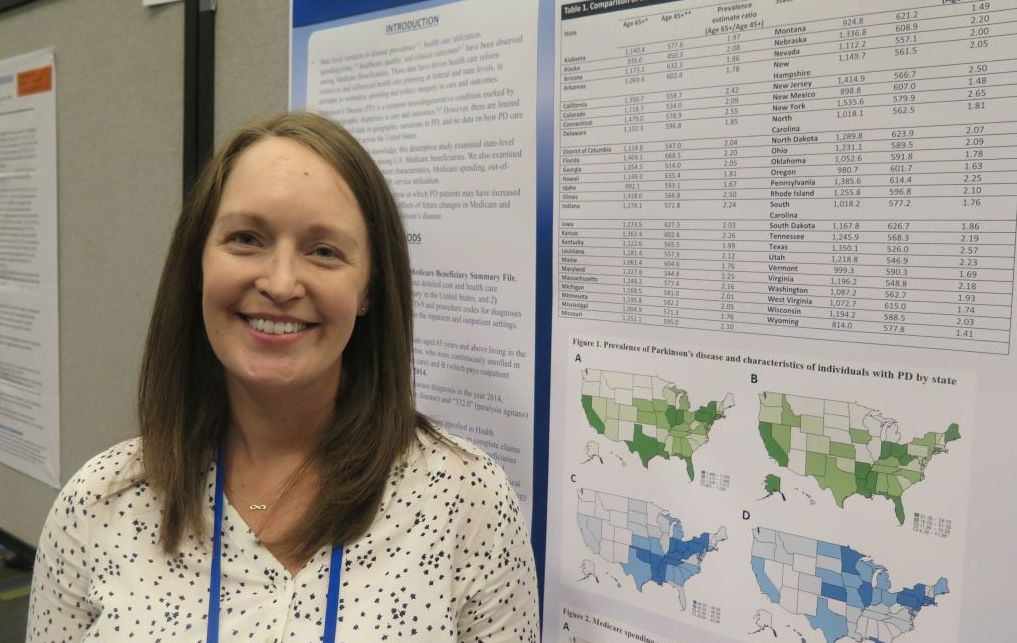
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).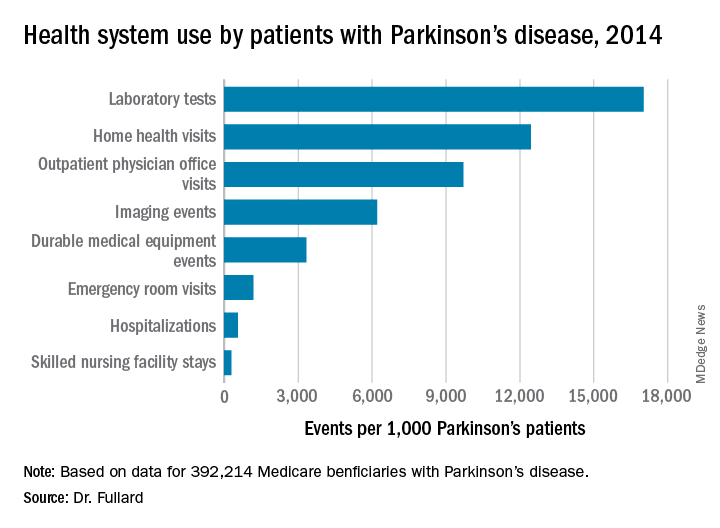
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).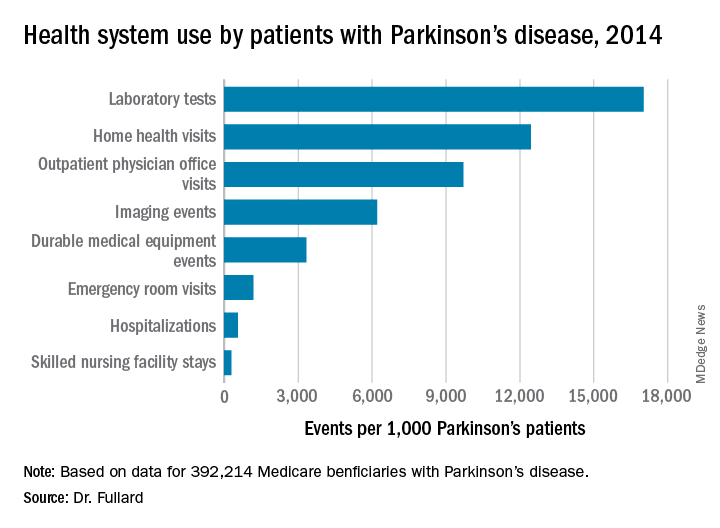
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).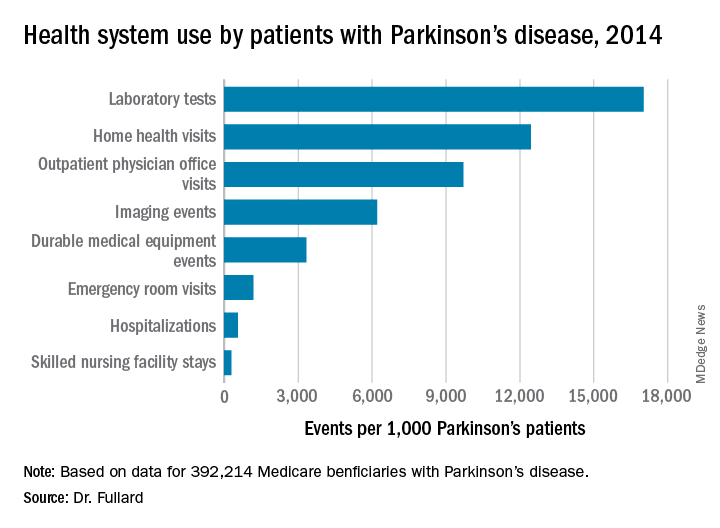
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
REPORTING FROM ANA 2018
Key clinical point:
Major finding: States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), and Connecticut (1,560/100,000), while Minnesota had the lowest prevalence (803/100,000).
Study details: An analysis of 392,214 Medicare beneficiaries who carried a diagnosis of Parkinson’s disease.
Disclosures: The study was supported by the Parkinson’s Foundation. Dr. Fullard reported having no financial disclosures.
Source: Ann Neurol. 2018;84[S22]:S89-90. Abstract S215.
Investigational gene therapy for medically refractory Parkinson’s shows promise
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
REPORTING FROM ANA 2018
Key clinical point: AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated.
Major finding: At 12 months, the researchers observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively.
Study details: A study of 15 patients in three cohorts who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions.
Disclosures: The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
Many oromandibular dystonia patients report improvement after botulinum toxin injections
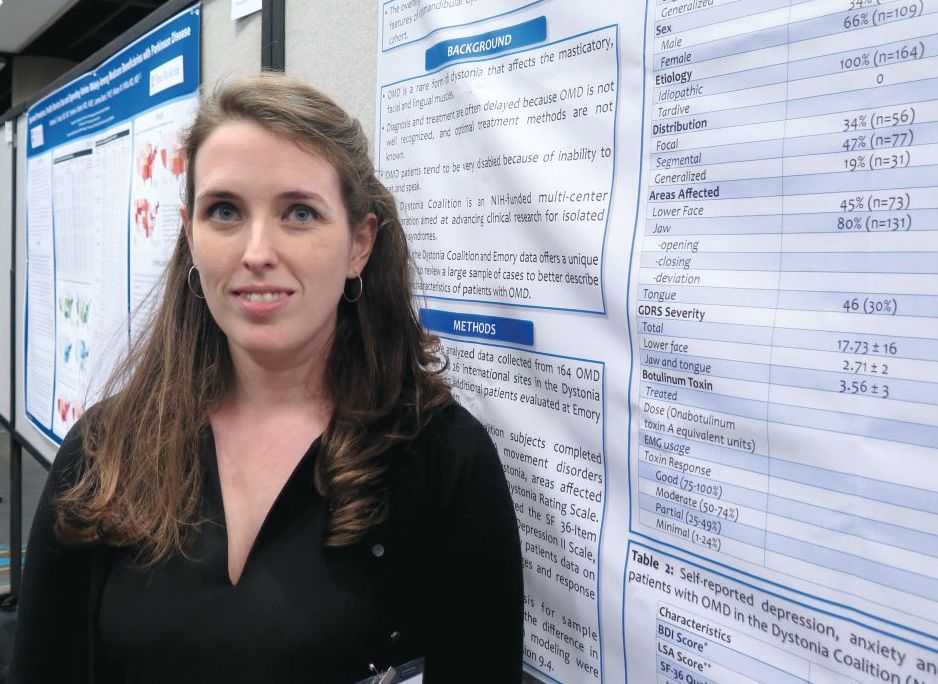
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
AT ANA 2018
Key clinical point: Oromandibular dystonia is associated with increased social anxiety and impaired quality of life.
Major finding: After receiving botulinum toxin injections, 78% of patients with oromandibular dystonia reported improvements in the range of 50%-100%.
Study details: A retrospective review of 201 patients with oromandibular dystonia.
Disclosures: The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr researchers reported having no financial disclosures.
Source: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
Higher BMI associated with greater loss of gray matter volume in MS
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
ATLANTA – Among patients with relapsing-remitting multiple sclerosis, higher body mass index, but not vitamin D status, appears to be related to greater loss of gray matter brain volume over time, results from a 5-year analysis showed.
“We had previously known that obesity is a risk factor for developing MS, and among those who already have the disease, obesity-related comorbidities are associated with increased morbidity and mortality,” lead study author Ellen M. Mowry, MD, said in an interview at the annual meeting of the American Neurological Association. “Loss of brain tissue, especially as measured by reduced volume of gray matter noted on brain MRI, is predictive of long-term disability in MS. While we await the results of confirmatory studies and randomized trials, this study adds to the growing body of evidence suggesting there may be a role for modification of lifestyle factors in mitigating longer-term MS-related disability risk.”
In an effort to determine if body mass index (BMI) or vitamin D status is associated with longer-term MRI measures of neurodegeneration, Dr. Mowry and her colleagues drew from 469 patients participating in a longitudinal MS cohort study at the University of California, San Francisco, known as EPIC. Participants had clinical evaluations, brain MRI, and blood draws annually and were followed for 5 years. The main outcomes of interest were BMI and serum 25-hydroxyvitamin D levels measured over the time period, and their relationship to brain volume.
At baseline, the mean age of patients was 42 years, 70% were female, their mean BMI was 25 kg/m2, and their mean serum vitamin D level was 27.8 ng/mL. Dr. Mowry, a neurologist at Johns Hopkins University, Baltimore, and her colleagues found that over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001). In addition, each 1-kg/m2 higher BMI over time was independently associated with greater declines in normalized brain parenchymal brain volume (–1.1 mL; P = .039). Elevated vitamin D levels, however, did not appear to be meaningfully associated with brain volumes.
Dr. Mowry acknowledged certain limitations of the study, including its nonrandomized design. “Such a trial may be warranted but I believe will be challenging to conduct,” she said. “Also, this cohort was designed to assess the association of genes with brain MRI outcomes, and so the people included were racially homogeneous – only Caucasians were included. Since MS risk is especially high among African Americans in recent years, and African Americans appear overall to have a higher risk of long-term disability, it is important to evaluate these and other prognostic factors amongst a more representative group of people with MS.”
The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
SOURCE: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
AT ANA 2018
Key clinical point: Higher body mass in MS patients appears to be related to greater brain atrophy over time.
Major finding: Over time, each 1-kg/m2 higher BMI was independently associated with reduced gray matter in multivariate models (–1.1 mL; P = .001).
Study details: An analysis of 469 patients participating in a longitudinal MS cohort study.
Disclosures: The study received funding support from the National Institutes of Health, GlaxoSmithKline, and Biogen. Dr. Mowry disclosed that she has received medication from Teva for use in a clinical trial. In addition, she has been the primary investigator for studies sponsored by Biogen and Sun Pharma, and has conducted investigator-initiated studies sponsored by Genzyme and Biogen.
Source: Ann Neurol. 2018;84[S22]:S206-7. Abstract M250.
Statins cut all-cause mortality in spinal cord injury
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
AT ANA 2018
Key clinical point:
Major finding: The mortality rate for patients on statins was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins (P less than .0052).
Study details: A retrospective review of 163 individuals with traumatic spinal cord injuries.
Disclosures: Dr. Rabadi reported having no financial disclosures.
Source: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
High ED recidivism seen in disadvantaged populations with chest pain
SAN DIEGO – After implementation of a new chest pain protocol in the emergency department, a greater proportion of patients with low-risk chest pain were discharged, yet a higher rate of ED recidivism was observed, results from a single-center study in Detroit showed.
While the precise cause of this finding is unclear, it may stem from factors affecting socioeconomically disadvantaged populations, Eric M. Blake, one of the study authors, said at the annual meeting of the American College of Emergency Physicians. “Recurrent ED visits are associated with social determinants of health, including race and economic status,” said Mr. Blake, a second-year student at Wayne State University School of Medicine, Detroit. “Socioeconomically disadvantaged patients often lack the transportation and monetary resources to follow up at an outpatient clinic. Detroit is an example of this type of a community; 83% of our population is African American, 36% of people live below the poverty line, and Detroit has an illiteracy rate of 47% in its adult population.”
He and his colleagues hypothesized that implementation of a standardized chest pain protocol in Detroit Receiving Hospital would safely reduce the number of hospital inpatient admissions and ED recidivism rates. Implemented on Nov. 1, 2012, the protocol uses the thrombolysis in myocardial infarction (TIMI) risk score, electrocardiography, and contemporary sensitivity troponin I to triage patients into low-, intermediate-, and high-risk categories. Low-risk patients were discharged and asked to follow up with a cardiologist within 48 hours. For the current study, the researchers retrospectively analyzed patients older than age 18 who presented with low-risk chest pain in the six months before the protocol was implemented and six months after.
A total of 3,613 patients were studied: 1,837 in the pre-protocol group and 1,776 in the post-protocol group. Their mean age was 47 years, 82% were African American, and 53% were male. No differences were observed between the pre- and post-protocol groups in terms of race (P = .280) or sex (P = .497). There was no statistical difference in the proportion of patients deemed at low risk in the pre- vs. post-protocol periods (P = .167). Significantly more low-risk patients were discharged in the post-protocol group, , compared with the pre-protocol group (55% vs. 44%; P less than .001), however. ED recidivism was also significantly greater in the post-protocol vs. pre-protocol group (3% vs. 1.6%; P = .0035).
“These findings may reflect an embedded racial mistrust of the medical system by certain minority groups,” Mr. Blake said. “Due to an extensive history of racism and segregation, a community like Detroit may have reservations when it comes to medical follow-up at outpatient clinics. Difficulty assessing outpatient follow-up for a variety of logistical and monetary reasons common among underprivileged communities may also be reflected in the increased recidivism rates.”
He concluded that administrators and clinicians in EDs nationwide “need to better understand the needs of underprivileged patients. A reduction in resource expenditures when a patient is discharged must be balanced with the cost of a recidivism in vulnerable populations like Detroit.”
To address poor cardiac outpatient follow-up rates, he and his colleagues are conducting a prospective randomized controlled trial investigating the use of motivational interviewing techniques with these patients.
The study’s senior author was Vijaya “Arun” Kumar, MD of Wayne State University School of Medicine. Mr. Blake reported having no financial disclosures.
SOURCE: Kumar VA et al. Ann Emerg Med. 2018 Oct;72;4:S117-18. doi. 10.1016/j.annemergmed.2018.08.304.
SAN DIEGO – After implementation of a new chest pain protocol in the emergency department, a greater proportion of patients with low-risk chest pain were discharged, yet a higher rate of ED recidivism was observed, results from a single-center study in Detroit showed.
While the precise cause of this finding is unclear, it may stem from factors affecting socioeconomically disadvantaged populations, Eric M. Blake, one of the study authors, said at the annual meeting of the American College of Emergency Physicians. “Recurrent ED visits are associated with social determinants of health, including race and economic status,” said Mr. Blake, a second-year student at Wayne State University School of Medicine, Detroit. “Socioeconomically disadvantaged patients often lack the transportation and monetary resources to follow up at an outpatient clinic. Detroit is an example of this type of a community; 83% of our population is African American, 36% of people live below the poverty line, and Detroit has an illiteracy rate of 47% in its adult population.”
He and his colleagues hypothesized that implementation of a standardized chest pain protocol in Detroit Receiving Hospital would safely reduce the number of hospital inpatient admissions and ED recidivism rates. Implemented on Nov. 1, 2012, the protocol uses the thrombolysis in myocardial infarction (TIMI) risk score, electrocardiography, and contemporary sensitivity troponin I to triage patients into low-, intermediate-, and high-risk categories. Low-risk patients were discharged and asked to follow up with a cardiologist within 48 hours. For the current study, the researchers retrospectively analyzed patients older than age 18 who presented with low-risk chest pain in the six months before the protocol was implemented and six months after.
A total of 3,613 patients were studied: 1,837 in the pre-protocol group and 1,776 in the post-protocol group. Their mean age was 47 years, 82% were African American, and 53% were male. No differences were observed between the pre- and post-protocol groups in terms of race (P = .280) or sex (P = .497). There was no statistical difference in the proportion of patients deemed at low risk in the pre- vs. post-protocol periods (P = .167). Significantly more low-risk patients were discharged in the post-protocol group, , compared with the pre-protocol group (55% vs. 44%; P less than .001), however. ED recidivism was also significantly greater in the post-protocol vs. pre-protocol group (3% vs. 1.6%; P = .0035).
“These findings may reflect an embedded racial mistrust of the medical system by certain minority groups,” Mr. Blake said. “Due to an extensive history of racism and segregation, a community like Detroit may have reservations when it comes to medical follow-up at outpatient clinics. Difficulty assessing outpatient follow-up for a variety of logistical and monetary reasons common among underprivileged communities may also be reflected in the increased recidivism rates.”
He concluded that administrators and clinicians in EDs nationwide “need to better understand the needs of underprivileged patients. A reduction in resource expenditures when a patient is discharged must be balanced with the cost of a recidivism in vulnerable populations like Detroit.”
To address poor cardiac outpatient follow-up rates, he and his colleagues are conducting a prospective randomized controlled trial investigating the use of motivational interviewing techniques with these patients.
The study’s senior author was Vijaya “Arun” Kumar, MD of Wayne State University School of Medicine. Mr. Blake reported having no financial disclosures.
SOURCE: Kumar VA et al. Ann Emerg Med. 2018 Oct;72;4:S117-18. doi. 10.1016/j.annemergmed.2018.08.304.
SAN DIEGO – After implementation of a new chest pain protocol in the emergency department, a greater proportion of patients with low-risk chest pain were discharged, yet a higher rate of ED recidivism was observed, results from a single-center study in Detroit showed.
While the precise cause of this finding is unclear, it may stem from factors affecting socioeconomically disadvantaged populations, Eric M. Blake, one of the study authors, said at the annual meeting of the American College of Emergency Physicians. “Recurrent ED visits are associated with social determinants of health, including race and economic status,” said Mr. Blake, a second-year student at Wayne State University School of Medicine, Detroit. “Socioeconomically disadvantaged patients often lack the transportation and monetary resources to follow up at an outpatient clinic. Detroit is an example of this type of a community; 83% of our population is African American, 36% of people live below the poverty line, and Detroit has an illiteracy rate of 47% in its adult population.”
He and his colleagues hypothesized that implementation of a standardized chest pain protocol in Detroit Receiving Hospital would safely reduce the number of hospital inpatient admissions and ED recidivism rates. Implemented on Nov. 1, 2012, the protocol uses the thrombolysis in myocardial infarction (TIMI) risk score, electrocardiography, and contemporary sensitivity troponin I to triage patients into low-, intermediate-, and high-risk categories. Low-risk patients were discharged and asked to follow up with a cardiologist within 48 hours. For the current study, the researchers retrospectively analyzed patients older than age 18 who presented with low-risk chest pain in the six months before the protocol was implemented and six months after.
A total of 3,613 patients were studied: 1,837 in the pre-protocol group and 1,776 in the post-protocol group. Their mean age was 47 years, 82% were African American, and 53% were male. No differences were observed between the pre- and post-protocol groups in terms of race (P = .280) or sex (P = .497). There was no statistical difference in the proportion of patients deemed at low risk in the pre- vs. post-protocol periods (P = .167). Significantly more low-risk patients were discharged in the post-protocol group, , compared with the pre-protocol group (55% vs. 44%; P less than .001), however. ED recidivism was also significantly greater in the post-protocol vs. pre-protocol group (3% vs. 1.6%; P = .0035).
“These findings may reflect an embedded racial mistrust of the medical system by certain minority groups,” Mr. Blake said. “Due to an extensive history of racism and segregation, a community like Detroit may have reservations when it comes to medical follow-up at outpatient clinics. Difficulty assessing outpatient follow-up for a variety of logistical and monetary reasons common among underprivileged communities may also be reflected in the increased recidivism rates.”
He concluded that administrators and clinicians in EDs nationwide “need to better understand the needs of underprivileged patients. A reduction in resource expenditures when a patient is discharged must be balanced with the cost of a recidivism in vulnerable populations like Detroit.”
To address poor cardiac outpatient follow-up rates, he and his colleagues are conducting a prospective randomized controlled trial investigating the use of motivational interviewing techniques with these patients.
The study’s senior author was Vijaya “Arun” Kumar, MD of Wayne State University School of Medicine. Mr. Blake reported having no financial disclosures.
SOURCE: Kumar VA et al. Ann Emerg Med. 2018 Oct;72;4:S117-18. doi. 10.1016/j.annemergmed.2018.08.304.
AT ACEP18
Key clinical point:
Major finding: Following implementation of a new chest pain protocol, significantly more low-risk patients were discharged (55% vs. 44%; P less than .001).
Study details: A retrospective analysis of 3,613 adults who presented with low-risk chest pain.
Disclosures: The researchers reported having no financial disclosures.
Source: Kumar VA et al. Ann Emerg Med. 2018 Oct;72;4:S117-18. doi. 10.1016/j.annemergmed.2018.08.304.
Transition to high-sensitivity troponin T assay helped boost ED discharge rates
SAN DIEGO – After transitioning to using the high-sensitivity troponin T assay for patients over the age of 35 years who presented to the ED with chest pain or tightness, an increased number of patients were discharged, yet no impact was observed on the time to admission and/or observation, according to a study conducted at two Philadelphia-based hospitals.
“Biomarkers have been a cornerstone of evaluating patients who present with chest pain,” Frederick T. Randolph, MD, said at the annual meeting of the American College of Emergency Physicians. “Recently in the United States, fifth-generation or high-sensitivity troponin [assays] have been approved for use. Our institution made the plan to transition to utilization of high-sensitivity troponins. At that time, we were aware of European studies that they were able to discharge a higher percentage of patients from the ED. There have been no prior studies of the clinical impact of transition to high-sensitivity troponin [assays] in the U.S.”
Dr. Randolph, director of the Chest Pain Center at Thomas Jefferson University, Philadelphia, and his colleagues performed a before and after study assessing all patients over age 35 years who presented to two hospitals with chest pain or tightness and who received a troponin assay draw in the ED. They conducted two town halls, in-services with cardiology and emergency medicine, and distributed a slide set to all providers. “There was no guidance as to who to order the troponin on,” said Dr. Randolph, who is also vice chief of emergency medicine at the university. “Essentially, the recommendation was, ‘Keep using troponins the same way you’ve been using troponins for years.’ The education was centered on how frequently we were going to order repeat troponins and how to interpret those results.”
The researchers used a 0- and 2-hour sampling strategy (unless the first value was less than 6 ng/L) and used a cut-point of 19 ng/L to define “ruled out” and a cut-point of 53 ng/L to define “consistent with acute myocardial infarction.” Indeterminate values were repeated every 2 hours. Dr. Randolph and his associates collected data for 1 year prior to transition to high-sensitivity troponins in 4,295 patients, and 2 months post transition in 769 patients. The primary outcome was discharge rate from the ED. Secondary outcome was time from presentation to admission/observation decision.
There were no statistically significant differences between the pre- and posttransition groups in the percentage of those aged 36-64 years (74% vs. 76%, respectively) or in the percentage of those who were nonwhite (61% vs. 59%). The only statistically significant difference was a higher percentage of females in the preimplementation group (49% vs. 46%; P = .02).
In all, the researchers were able to discharge 45.2% of all patients during the pretransition period, compared with 58.7% of patients in the posttransition period, for an absolute increase of 13% (P less than .001). There was no difference between the two groups in time to decision to admit or to observe (a mean of 199.1 vs. 192.2 minutes, respectively; P = .96). “Areas of future study would be to evaluate those patients who were discharged and monitor them for any changes in outcomes, to see if there is any increase in morbidity or complications,” said Dr. Randolph. “An additional research curiosity would be the downstream consequences on cost or revenue to the institution given the increased number of admissions and the decreased use of diagnostic testing such as coronary computed tomography angiography and stress testing.”
Dr. Randolph disclosed that some of the study authors have participated in multiple biomarker studies over the years. He reported having no financial disclosures.
Source: Randolph FT et al. Ann Emerg Med. 2018 Oct;72;4:S2-3. doi. 10.1016/j.annemergmed.2018.08.009.
SAN DIEGO – After transitioning to using the high-sensitivity troponin T assay for patients over the age of 35 years who presented to the ED with chest pain or tightness, an increased number of patients were discharged, yet no impact was observed on the time to admission and/or observation, according to a study conducted at two Philadelphia-based hospitals.
“Biomarkers have been a cornerstone of evaluating patients who present with chest pain,” Frederick T. Randolph, MD, said at the annual meeting of the American College of Emergency Physicians. “Recently in the United States, fifth-generation or high-sensitivity troponin [assays] have been approved for use. Our institution made the plan to transition to utilization of high-sensitivity troponins. At that time, we were aware of European studies that they were able to discharge a higher percentage of patients from the ED. There have been no prior studies of the clinical impact of transition to high-sensitivity troponin [assays] in the U.S.”
Dr. Randolph, director of the Chest Pain Center at Thomas Jefferson University, Philadelphia, and his colleagues performed a before and after study assessing all patients over age 35 years who presented to two hospitals with chest pain or tightness and who received a troponin assay draw in the ED. They conducted two town halls, in-services with cardiology and emergency medicine, and distributed a slide set to all providers. “There was no guidance as to who to order the troponin on,” said Dr. Randolph, who is also vice chief of emergency medicine at the university. “Essentially, the recommendation was, ‘Keep using troponins the same way you’ve been using troponins for years.’ The education was centered on how frequently we were going to order repeat troponins and how to interpret those results.”
The researchers used a 0- and 2-hour sampling strategy (unless the first value was less than 6 ng/L) and used a cut-point of 19 ng/L to define “ruled out” and a cut-point of 53 ng/L to define “consistent with acute myocardial infarction.” Indeterminate values were repeated every 2 hours. Dr. Randolph and his associates collected data for 1 year prior to transition to high-sensitivity troponins in 4,295 patients, and 2 months post transition in 769 patients. The primary outcome was discharge rate from the ED. Secondary outcome was time from presentation to admission/observation decision.
There were no statistically significant differences between the pre- and posttransition groups in the percentage of those aged 36-64 years (74% vs. 76%, respectively) or in the percentage of those who were nonwhite (61% vs. 59%). The only statistically significant difference was a higher percentage of females in the preimplementation group (49% vs. 46%; P = .02).
In all, the researchers were able to discharge 45.2% of all patients during the pretransition period, compared with 58.7% of patients in the posttransition period, for an absolute increase of 13% (P less than .001). There was no difference between the two groups in time to decision to admit or to observe (a mean of 199.1 vs. 192.2 minutes, respectively; P = .96). “Areas of future study would be to evaluate those patients who were discharged and monitor them for any changes in outcomes, to see if there is any increase in morbidity or complications,” said Dr. Randolph. “An additional research curiosity would be the downstream consequences on cost or revenue to the institution given the increased number of admissions and the decreased use of diagnostic testing such as coronary computed tomography angiography and stress testing.”
Dr. Randolph disclosed that some of the study authors have participated in multiple biomarker studies over the years. He reported having no financial disclosures.
Source: Randolph FT et al. Ann Emerg Med. 2018 Oct;72;4:S2-3. doi. 10.1016/j.annemergmed.2018.08.009.
SAN DIEGO – After transitioning to using the high-sensitivity troponin T assay for patients over the age of 35 years who presented to the ED with chest pain or tightness, an increased number of patients were discharged, yet no impact was observed on the time to admission and/or observation, according to a study conducted at two Philadelphia-based hospitals.
“Biomarkers have been a cornerstone of evaluating patients who present with chest pain,” Frederick T. Randolph, MD, said at the annual meeting of the American College of Emergency Physicians. “Recently in the United States, fifth-generation or high-sensitivity troponin [assays] have been approved for use. Our institution made the plan to transition to utilization of high-sensitivity troponins. At that time, we were aware of European studies that they were able to discharge a higher percentage of patients from the ED. There have been no prior studies of the clinical impact of transition to high-sensitivity troponin [assays] in the U.S.”
Dr. Randolph, director of the Chest Pain Center at Thomas Jefferson University, Philadelphia, and his colleagues performed a before and after study assessing all patients over age 35 years who presented to two hospitals with chest pain or tightness and who received a troponin assay draw in the ED. They conducted two town halls, in-services with cardiology and emergency medicine, and distributed a slide set to all providers. “There was no guidance as to who to order the troponin on,” said Dr. Randolph, who is also vice chief of emergency medicine at the university. “Essentially, the recommendation was, ‘Keep using troponins the same way you’ve been using troponins for years.’ The education was centered on how frequently we were going to order repeat troponins and how to interpret those results.”
The researchers used a 0- and 2-hour sampling strategy (unless the first value was less than 6 ng/L) and used a cut-point of 19 ng/L to define “ruled out” and a cut-point of 53 ng/L to define “consistent with acute myocardial infarction.” Indeterminate values were repeated every 2 hours. Dr. Randolph and his associates collected data for 1 year prior to transition to high-sensitivity troponins in 4,295 patients, and 2 months post transition in 769 patients. The primary outcome was discharge rate from the ED. Secondary outcome was time from presentation to admission/observation decision.
There were no statistically significant differences between the pre- and posttransition groups in the percentage of those aged 36-64 years (74% vs. 76%, respectively) or in the percentage of those who were nonwhite (61% vs. 59%). The only statistically significant difference was a higher percentage of females in the preimplementation group (49% vs. 46%; P = .02).
In all, the researchers were able to discharge 45.2% of all patients during the pretransition period, compared with 58.7% of patients in the posttransition period, for an absolute increase of 13% (P less than .001). There was no difference between the two groups in time to decision to admit or to observe (a mean of 199.1 vs. 192.2 minutes, respectively; P = .96). “Areas of future study would be to evaluate those patients who were discharged and monitor them for any changes in outcomes, to see if there is any increase in morbidity or complications,” said Dr. Randolph. “An additional research curiosity would be the downstream consequences on cost or revenue to the institution given the increased number of admissions and the decreased use of diagnostic testing such as coronary computed tomography angiography and stress testing.”
Dr. Randolph disclosed that some of the study authors have participated in multiple biomarker studies over the years. He reported having no financial disclosures.
Source: Randolph FT et al. Ann Emerg Med. 2018 Oct;72;4:S2-3. doi. 10.1016/j.annemergmed.2018.08.009.
AT ACEP18
Key clinical point: .
Major finding: After conversion to using the high-sensitivity troponin T assay, the ED discharge rate increased to 58.7%, from 45.2% (P less than 0.001).
Study details: A before and after study of 5,064 patients aged 35 and older who presented to the ED with chest pain or tightness.
Disclosures: Dr. Randolph disclosed that some of the study authors have participated in multiple biomarker studies over the years. He reported having no financial disclosures.
Source: Randolph FT et al. Ann Emerg Med. 2018 Oct;72;4:S2-3. doi: 10.1016/j.annemergmed.2018.08.009.
Stroke risk in elderly following AMI extends to 12 weeks
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
AT ANA 2018
Key clinical point: .
Major finding: The risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6).
Study details: An analysis of 46,182 Medicare beneficiaries who were hospitalized for acute MI and 80,466 who were hospitalized for ischemic stroke.
Disclosures: Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
About 20% of penalties from EMTALA violations linked to psychiatric emergencies
SAN DIEGO – Between 2002 and April 2018, about one in five civil monetary penalty payments linked to Emergency Medical Treatment and Labor Act (EMTALA) violations involved psychiatric emergencies, an analysis of national data found.
“Penalties were twice as high for psychiatric cases as for nonpsychiatric cases, with failure to stabilize being more common,” Sophie Terp, MD, MPH, said at the annual meeting of the American College of Emergency Physicians. “Recent large penalties suggest the need to improve care for psychiatric emergencies.”
In an effort to characterize U.S. Office of Inspector General (OIG) penalties resulting from EMTALA violations involving psychiatric emergencies, Dr. Terp, of the department of emergency medicine at the University of Southern California, Los Angeles, and her colleagues reviewed all OIG penalties between 2002 and April 2018. Characteristics of penalties involving psychiatric emergencies were described and compared with other penalties.
Of the 229 civil monetary penalties levied during the study period, 44 (19%) were related to psychiatric emergencies and the average fine was $85,488, which was significantly higher than the average fine of $32,042 for nonpsychiatric-related civil monetary penalties (P = .004). The three largest penalties during the study period were all related to psychiatric emergencies, including one for $360,000 in 2012, one for $1,295,000 in 2017, and one for $200,000 in 2018.
“Settlements have been particularly high in recent years,” Dr. Terp said. By comparison, the largest civil monetary penalty for a nonpsychiatric case was $170,000.
Failure to provide a medical screening exam was the most common reason for civil monetary settlements in both psychiatric and nonpsychiatric cases (84% vs. 74%; P = .147), but “failure to stabilize” occurred in a significantly greater proportion of psychiatric versus nonpsychiatric cases (68% vs. 51%; P = .041). About one-third of all psychiatric cases occurred in Centers for Medicare & Medicaid Services Region 4, “which is a region known to have a very high rate of EMTALA enforcement overall,” Dr. Terp said. “About half of those cases occurred in Florida, and another 20% occurred in South Carolina. About 20% occurred in CMS Region 6, and about half of those were in Texas. But the overall proportions of psychiatric versus nonpsychiatric cases that distributed over the CMS regions did not significantly differ.”
Dr. Terp reported having no financial disclosures.
SOURCE: Terp S et al. ACEP18, Abstract 46.
SAN DIEGO – Between 2002 and April 2018, about one in five civil monetary penalty payments linked to Emergency Medical Treatment and Labor Act (EMTALA) violations involved psychiatric emergencies, an analysis of national data found.
“Penalties were twice as high for psychiatric cases as for nonpsychiatric cases, with failure to stabilize being more common,” Sophie Terp, MD, MPH, said at the annual meeting of the American College of Emergency Physicians. “Recent large penalties suggest the need to improve care for psychiatric emergencies.”
In an effort to characterize U.S. Office of Inspector General (OIG) penalties resulting from EMTALA violations involving psychiatric emergencies, Dr. Terp, of the department of emergency medicine at the University of Southern California, Los Angeles, and her colleagues reviewed all OIG penalties between 2002 and April 2018. Characteristics of penalties involving psychiatric emergencies were described and compared with other penalties.
Of the 229 civil monetary penalties levied during the study period, 44 (19%) were related to psychiatric emergencies and the average fine was $85,488, which was significantly higher than the average fine of $32,042 for nonpsychiatric-related civil monetary penalties (P = .004). The three largest penalties during the study period were all related to psychiatric emergencies, including one for $360,000 in 2012, one for $1,295,000 in 2017, and one for $200,000 in 2018.
“Settlements have been particularly high in recent years,” Dr. Terp said. By comparison, the largest civil monetary penalty for a nonpsychiatric case was $170,000.
Failure to provide a medical screening exam was the most common reason for civil monetary settlements in both psychiatric and nonpsychiatric cases (84% vs. 74%; P = .147), but “failure to stabilize” occurred in a significantly greater proportion of psychiatric versus nonpsychiatric cases (68% vs. 51%; P = .041). About one-third of all psychiatric cases occurred in Centers for Medicare & Medicaid Services Region 4, “which is a region known to have a very high rate of EMTALA enforcement overall,” Dr. Terp said. “About half of those cases occurred in Florida, and another 20% occurred in South Carolina. About 20% occurred in CMS Region 6, and about half of those were in Texas. But the overall proportions of psychiatric versus nonpsychiatric cases that distributed over the CMS regions did not significantly differ.”
Dr. Terp reported having no financial disclosures.
SOURCE: Terp S et al. ACEP18, Abstract 46.
SAN DIEGO – Between 2002 and April 2018, about one in five civil monetary penalty payments linked to Emergency Medical Treatment and Labor Act (EMTALA) violations involved psychiatric emergencies, an analysis of national data found.
“Penalties were twice as high for psychiatric cases as for nonpsychiatric cases, with failure to stabilize being more common,” Sophie Terp, MD, MPH, said at the annual meeting of the American College of Emergency Physicians. “Recent large penalties suggest the need to improve care for psychiatric emergencies.”
In an effort to characterize U.S. Office of Inspector General (OIG) penalties resulting from EMTALA violations involving psychiatric emergencies, Dr. Terp, of the department of emergency medicine at the University of Southern California, Los Angeles, and her colleagues reviewed all OIG penalties between 2002 and April 2018. Characteristics of penalties involving psychiatric emergencies were described and compared with other penalties.
Of the 229 civil monetary penalties levied during the study period, 44 (19%) were related to psychiatric emergencies and the average fine was $85,488, which was significantly higher than the average fine of $32,042 for nonpsychiatric-related civil monetary penalties (P = .004). The three largest penalties during the study period were all related to psychiatric emergencies, including one for $360,000 in 2012, one for $1,295,000 in 2017, and one for $200,000 in 2018.
“Settlements have been particularly high in recent years,” Dr. Terp said. By comparison, the largest civil monetary penalty for a nonpsychiatric case was $170,000.
Failure to provide a medical screening exam was the most common reason for civil monetary settlements in both psychiatric and nonpsychiatric cases (84% vs. 74%; P = .147), but “failure to stabilize” occurred in a significantly greater proportion of psychiatric versus nonpsychiatric cases (68% vs. 51%; P = .041). About one-third of all psychiatric cases occurred in Centers for Medicare & Medicaid Services Region 4, “which is a region known to have a very high rate of EMTALA enforcement overall,” Dr. Terp said. “About half of those cases occurred in Florida, and another 20% occurred in South Carolina. About 20% occurred in CMS Region 6, and about half of those were in Texas. But the overall proportions of psychiatric versus nonpsychiatric cases that distributed over the CMS regions did not significantly differ.”
Dr. Terp reported having no financial disclosures.
SOURCE: Terp S et al. ACEP18, Abstract 46.
REPORTING FROM ACEP18
Key clinical point: Nearly one in five settlements related to Emergency Medical Treatment and Labor Act violations involved psychiatric emergencies.
Major finding: Of the civil monetary penalties levied during the study period, 19% were related to psychiatric emergencies and the average fine was $85,488.
Study details: An analysis of 229 civil monetary penalties levied by the Office of Inspector General related to violations of EMTALA between 2002 and April 2018.
Disclosures: Dr. Terp reported having no financial disclosures.
Source: Terp S et al. ACEP18, Abstract 46.