User login
Nonprocedural “Time Out”
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
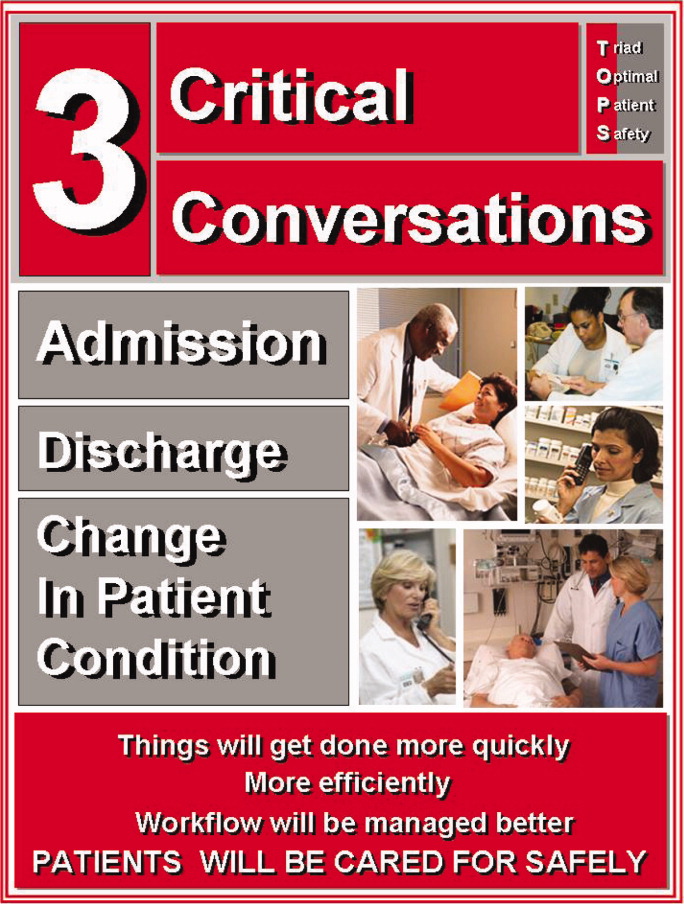
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
Communication and teamwork failures are the most frequently cited cause of adverse events.1, 2 Strategies to improve communication have focused on implementing formal teamwork training programs and/or teaching specific communication skills.36 For instance, many institutions have adopted SBAR (Situation‐Background‐Assessment‐Recommendation) as a method for providers to deliver critical clinical information in a structured format.7 SBAR focuses on the immediate and urgent event at hand and can occur between any 2 providers. The situation is a brief description of the event (eg, Hi Dr. Smith, this is Paul from 14‐Long, I'm calling about Mrs. Jones in 1427 who is in acute respiratory distress). The background describes details relevant to the situation (eg, She was admitted with a COPD exacerbation yesterday night, and, for the past couple hours, she appears in more distress. Her vital signs are). The assessment (eg, Her breath sounds are diminished and she's moving less air) and recommendation (eg, I'd like to call respiratory therapy and would like you to come assess her now) drive toward having an action defined at the end. Given the professional silos that exist in healthcare, the advent of a shared set of communication tools helps bridge existing gaps in training, experience, and teamwork between different providers.
Regulatory agencies have been heavily invested in attempts to standardize communication in healthcare settings. In 2003, the Joint Commission elevated the concerns for wrong‐site surgery by making its prevention a National Patient Safety Goal, and the following year required compliance with a Universal Protocol (UP).8 In addition to adequate preoperative identification of the patient and marking of their surgical site, the UP called for a time out (TO) just prior to the surgery or procedure. The UP states that a TO requires active communication among all members of the surgical/procedure team, consistently initiated by a designated member of the team, conducted in a fail‐safe mode, so that the planned procedure is not started if a member of the team has concerns.8 Simply, the TO provides an opportunity to clarify plans for care and discuss events anticipated during the procedure among all members of the team (eg, surgeons, anesthesiologists, nurses, technicians). This all‐important pause point ensures that each team member is on the same page.
Whereas a TO involves many high‐risk procedural settings, a significant proportion of hospital care occurs outside of procedures. Patients are often evaluated in an emergency department, admitted to a medical/surgical ward, treated without the need for a procedure, and ultimately discharged home or transferred to another healthcare facility (eg, skilled nursing or acute rehabilitation). In this paper, we introduce the concept of Critical Conversations, a form of nonprocedural time out, as a tool, intervention, and policy that promotes communication and teamwork at the most vulnerable junctures in a patient's hospitalization.
Rationale for Critical Conversations: a Case Scenario
An 82‐year‐old man with hypertension and chronic obstructive pulmonary disease (COPD) is admitted to the hospital with community‐acquired pneumonia and an exacerbation of his COPD. The admitting physician evaluates the patient in the emergency department and completes admission orders. The patient arrives on the medical/surgical unit and the unit clerk processes the orders, stimulating a cascade of downstream events for different providers.
Nurse
The nurse reviews the medication list, notices antibiotics and bronchodilators, and wonders why aren't we administering steroids for his COPD? Do any of these medications need to be given now? Is there anything the physician is worried about? What specific things should prompt me to call the physician with an update or change in condition? I'm not sure if it's safe to send the patient down for the ordered radiographic study because he still looks pretty short of breath. I hate paging the physician several times to get these questions answered because I know that person is busy as well. I also know the patient will have questions about the care plans, which I won't be able to answer. I wonder if I should finish administering evening medications for my other patients as I'm running behind schedule on my other tasks.
Respiratory therapist
At the same time, the respiratory therapist (RT) is contacted to assist with nebulizer therapy for the patient. In reviewing the order for bronchodilators, the RT silently asks, do we think he is going to need continuous nebulizers? What is our oxygen saturation goaldo we want him at 90% or above 95%? I wonder if this patient has a history of CO2 retention and if I should have a BiPAP machine at the bedside.
Physician
After completing the orders for the patient, the physician remains in the emergency department to admit a different patient with a gastrointestinal bleed. This is the fifth admission in the past few hours. The physician feels the impact of constant paging interruptions. A unit clerk pages asking for clarification about a radiographic study that was ordered. A bedside nurse pages and asks if the physician can come and speak to the family about the diagnosis and treatment plans for an earlier admission (something the nurse is not clear about, either). A second bedside nurse pages, stating a different admission is still tachycardic after 3 liters of intravenous fluids and wants to know whether the fluids should be continued. Finally, the bedside nurse pages about whether the new COPD admission can go off the floor for the ordered chest CT or remain on continuous pulse oximetry because of shortness of breath.
Our case scenario is representative of most non‐surgical admissions to a hospital. The hypothetical questions posed from different provider perspectives are also common and often remain unanswered in a timely fashion. Partly because there is no site to mark and no anesthesia to deliver, the clinical encounter escapes attention as an opportunity for error prevention. In our experience, there are specific times during a hospitalization when communication failures are most likely to compromise patient care: the time of admission, the time of discharge,9 and any time when a patient's clinical condition changes acutely. Whereas handoff communications focus on transitions between providers (eg, shift changes), these circumstances are driven by patient transitions. Indirect communications, such as phone, email, or faxes, are suboptimal forms of communication at such times.10 We believe that there should be an expectation for direct communication at these junctures, and we define these direct communications as Critical Conversations.
Description of a Critical Conversation
In the hours that follow an admission, providers (and often the patients or their family as well) invariably exchange any number of inefficient calls or pages to clarify care plans, discuss a suspected diagnosis, anticipate concerns in the first night, and/or highlight which orders should be prioritized, such as medications or diagnostic studies. A Critical Conversation at time of admission does in this circumstance exactly what a TO attempts to provide before a procedure foster communication and teamwork as a patient is about to be placed at risk for adverse events. The exchange involves discussion of the following:
Admitting diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any admitting orders
Guidelines for physician notification when a change in patient condition occurs.
At the other end of a hospitalization, with the known complications arising from a patient's discharge,11, 12 the same process is needed. Rather than having each discipline focus on an individual role or task in getting a patient safely discharged, Critical Conversations allow the entire team, including the patient,13 to ensure that concerns have been addressed. This might help clarify simple measures around follow‐up appointments, whom to call with questions after discharge, or symptoms to watch for that may warrant a repeat evaluation. Nurses anecdotally lament that they first learn about a planned discharge only when the discharge order is written in the chart or if a patient informs them. Both scenarios reflect poorly on the teamwork required to assure patients we're working together, and that key providers are on the same page with respect to discharge planning. The exchange at discharge involves discussion of these elements:
Discharge diagnosis
Follow‐up plans
Need for education/training prior to discharge
Necessary paperwork completed
Anticipated time of discharge.
Finally, where many patients are admitted to a hospital, improve, and then return home, others develop acute changes during their hospitalization. For example, the patient in our case scenario could develop respiratory failure and require transfer to the intensive care unit (ICU). Or a different patient might have an acute change in mental status, a new fever, a new abnormal vital sign (eg, tachycardia or hypoxia), or an acute change re existing abdominal painall of which may require a battery of diagnostic tests. These circumstances define the third time for a Critical Conversation: a change in clinical condition. Such situations often require a change in the care plan, a change in priorities for delivering care at that time (for the patient in need and for other patients being cared for by the same nurse and physician), a need for additional resources (eg, respiratory therapist, phlebotomist, pharmacist), and, ultimately, a well‐orchestrated team effort to make it all happen. The specific item prompting the Critical Conversation may impact the nature of the exchange, which involves discussion of these components:
Suspected diagnosis
Immediate treatment plan
Medications ordered (particularly those new to a patient to anticipate an adverse event)
Priority for completing any new orders
Guidelines for physician notification when a change in patient condition occurs.
In addition to the above checklist for each Critical Conversation, each exchange should also address two open‐ended questions: 1) what do you anticipate happening in the next 24 hours, and 2) what questions might the patient/family have?
One may ask, and we did, why not have a direct communication daily between a physician and a bedside nurse on each patient? Most physicians and nurses know the importance of direct communication, but there are also times when each is prioritizing work in competing fashions. Adopting Critical Conversations isn't meant to deter from communications that are vital to patient care; rather, it is intended to codify distinct times when a direct communication is required for patient safety.
Lessons Learned
Table 1 provides an example of a Critical Conversation using the sample case scenario. Table 2 lists the most frequent outcomes that resulted from providers engaging in Critical Conversations. These were captured from discussions with bedside nurses and internal medicine residents on our primary medical unit. Both tables highlight how these deliberate and direct communications can create a shared understanding of the patient's medical problems, can help prioritize what tasks should take place (eg, radiology study, medication administration, calling another provider), can improve communication between providers and patients, and potentially accomplish all of these goals in a more efficient manner.
| Physician: Hi Nurse X, I'm Dr. Y, and I just wrote admission orders for Mr. Z whom, I understand, you'll be admitting. He's 82 with a history of COPD and is having an exacerbation related to a community‐acquired pneumonia. He looks comfortable right now as he's received his first dose of antibiotics, a liter of IVF, and 2 nebulizer treatments with some relief of his dyspnea. The main thing he needs up on the floor right now is to have respiratory therapy evaluate him. He's apparently been intubated before for his COPD, so I'd like to have them on board early and consider placing a BiPAP machine at the bedside for the next few hours. I don't anticipate an acute worsening of his condition given his initial improvements in the ED, but you should call me with any change in his condition. I haven't met the family yet because they were not at the bedside, but please convey the plans to them as well. I'll be up later to talk to them directly. Do you have any questions for me right now? |
| Nurse: I'll call the respiratory therapist right now and we'll make sure to contact you with any changes in his respiratory status. It looks like a chest CT was ordered, but not completed yet. Would you like him to go down for it off monitor? |
| Physician: Actually, let's watch him for a few hours to make sure he's continuing to improve. I initially ordered the chest CT to exclude a pulmonary embolus, but his history, exam, and chest x‐ray seem consistent with pneumonia. Let's reassess in a few hours. |
| Nurse: Sounds good. I'll text‐message you a set of his vital signs in 3‐4 hours to give you an update on his respiratory status. |
| General Themes | Specific Examples |
|---|---|
| Clarity on plan of care | Clear understanding of action steps at critical junctures of hospitalization |
| Goals of admission discussed rather than gleaned from chart or less direct modes of communication | |
| Discharge planning more proactive with better anticipation of timing among patients and providers | |
| Expectation for shared understanding of care plans | |
| Assistance with prioritization of tasks (as well as for competing tasks) | Allows RNs to prioritize tasks for new admissions or planned discharges, to determine whether these tasks outweigh tasks for other patients, and to provide early planning when additional resources will be required |
| Allows MDs to prioritize communications to ensure critical orders receive attention, to obtain support for care plans that require multiple disciplines, and to confirm that intended care plans are implemented with shared sense of priority | |
| Ability to communicate plans to patient and family members | Improved consistency in information provided to patients at critical hospital junctures |
| Increased engagement of patients in understanding their care plans | |
| Better model for teamwork curative for patients when providers on the same page with communication | |
| More efficient and effective use of resources | Fewer pages between admitting RN and MD with time saved from paging and waiting for responses |
| Less time trying to interpret plans of care from chart and other less direct modes of communication | |
| Improved sharing and knowledge of information with less duplication of gathering from patients and among providers | |
| Improved teamwork | Fosters a culture for direct communication and opens lines for questioning and speaking up when care plans are not clear |
Making Critical Conversations Happen
Integrating Critical Conversations into practice requires both buy‐in among providers and a plan for monitoring the interactions. We recommend beginning with educational efforts (eg, at a physician or nurse staff meeting) and reinforcing them with visual cues, such as posters on the unit (Figure 1). These actions promote awareness and generate expectations that this new clinical policy is being supported by clinical and hospital leadership. Our experiences have demonstrated tremendous learning, including numerous anecdotes about the value of Critical Conversations (Table 3). Our implementation efforts also raised a number of questions that ultimately led to improved clarity in later iterations.
| Nothing is worse than meeting a patient for the first time at admission and not being able to answer the basic question of why they were admitted or what the plan is. It gives the impression that we don't talk to each other in caring for patients. [Critical Conversations] can really minimize that interaction and reassure patients, rather than make them worried about the apparent mixed messages or lack of communication and teamwork.Bedside Nurse |
| [Critical Conversations] seemed like an additional timely responsibility, and not always a part of my workflow, when sitting in the emergency department admitting patients. But, I found that the often 60 second conversations decreased the number of pages I would get for the same patientactually saving me time.Physician |
| I don't need to have direct communications for every order written. In fact, it would be inefficient for me and the doctors. On the other hand, being engaged in a Critical Conversation provides an opportunity for me to prioritize not only my tasks for the patient in need, but also in context of the other patients I'm caring for.Bedside Nurse |
| Late in the afternoon, there will often be several admissions coming to our unit simultaneously. Prioritizing what orders need to be processed or faxed is a typically blind task based on the way charts get organizedrather than someone telling me this is a priority.Unit Clerk |
| There are so many times when I'm trying to determine what the care plans are for a new admission, and simply having a quick conversation allows me to feel part of the team, and, more importantly, allows me to reinforce education and support for the patients and their family members.Bedside Nurse |
| Discharge always seems chaotic with everyone racing to fill out forms and meet their own tasks and requirements. Invariably, you get called to fix, change, or add new information to the discharge process that would have been easily averted by actually having a brief conversation with the bedside nurse or case manager. Every time I have [a Critical Conversation], I realize its importance for patient care.Physician |
Who should be involved in a Critical Conversation?
Identifying which healthcare team members should be involved in Critical Conversations is best determined by the conversation owner. That is, we found communication was most effective when the individual initiating the Critical Conversation directed others who needed to be involved. At admission, the physician writing the admission orders is best suited to make this determination; at a minimum, he or she should engage the bedside nurse but, as in the case example presented, the physician may also need to engage other services in particularly complex situations (eg, respiratory therapy, pharmacy). At time of discharge, there should be a physiciannurse Critical Conversation; however, the owner of the discharge process may determine that other conversations should occur, and this may be inclusive of or driven by a case manager or social worker. Because local culture and practices may drive specific ownership, it's key to outline a protocol for how this should occur. For instance, at admission, we asked the admitting physicians to take responsibility in contacting the bedside nurse. In other venues, this may work more effectively if the bedside nurse pages the physician once the orders are received and reviewed.
Conclusions
We introduced Critical Conversations as an innovative tool and policy that promotes communication and teamwork in a structured format and at a consistent time. Developing formal systems that decrease communication failures in high‐risk circumstances remains a focus in patient safety, evidenced by guidelines for TOs in procedural settings, handoffs in patient care (eg, sign‐out between providers),14, 15 and transitions into and from the hospital setting.16 Furthermore, there is growing evidence that such structured times for communication and teamwork, such as with briefings, can improve efficiency and reduce delays in care.17, 18 However, handoffs, which address provider transitions, and daily multidisciplinary rounds, which bring providers together regularly, are provider‐centered rather than patient‐centered. Critical Conversations focus on times when patients require direct communication about their care plans to ensure safe and high quality outcomes.
Implementation of Critical Conversations provides an opportunity to codify a professional standard for patient‐centered communication at times when it should be expected. Critical Conversations also help build a system that supports a positive safety culture and encourages teamwork and direct communication. This is particularly true at a time when rapid adoption of information technology may have the unintended and opposite effect. For instance, as our hospital moved toward an entirely electronic health record, providers were increasingly relocating from patient care units into remote offices, corner hideaways, or designated computer rooms to complete orders and documentation. Although this may reduce many related errors in these processes and potentially improve communication via shared access to an electronic record, it does allow for less direct communicationa circumstance that traditionally occurs (even informally) when providers share the same clinical work areas. This situation is aggravated where the nurses are unit‐based and other providers (eg, physicians, therapists, case managers) are service‐based.
Integrating Critical Conversations into practice comes with expected challenges, most notably around workflow (eg, adds a step, although may save steps down the line) and the expectations concomitant with any change in standard of care (possible enforcement or auditing of their occurrence). Certain cultural barriers may also play a significant role, such as the presence of hierarchies that can hinder open communication and the related ability to speak up with concerns, as related in the TO literature. Where these cultural barriers highlight historical descriptions of the doctornurse relationship and its effect on patient care,1921 Critical Conversations provide an opportunity to improve such interdisciplinary relationships by providing a shared tool for direct communication.
In summary, we described an innovative communication tool that promotes direct communication at critical junctures during a hospitalization. With the growing complexity of hospital care and greater interdependence between teams that deliver this care, Critical Conversations provide an opportunity to further address the known communication failures that contribute to medical errors.
Acknowledgements
Critical Conversations was developed during the Triad for Optimal Patient Safety (TOPS) project, an effort focused on improving unit‐based safety culture through improved teamwork and communication. We thank the Gordon and Betty Moore Foundation for their active support and funding of the TOPS project, which was a collaboration between the Schools of Medicine, Nursing, and Pharmacy at the University of California, San Francisco.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14(6):401–407.
- ,,.Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79(2):186–194.
- ,.TeamSTEPPS: assuring optimal teamwork in clinical settings.Am J Med Qual.2007;22(3):214–217.
- ,,,,,.Medical team training: applying crew resource management in the Veterans Health Administration.Jt Comm J Qual Patient Saf.2007;33(6):317–325.
- ,,,,,,,,,.A multidisciplinary teamwork training program: the Triad for Optimal Patient Safety (TOPS) Experience.J Gen Intern Med.2008;23(12):2053–2057.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13Suppl‐1:i85–90.
- ,,.SBAR: a shared mental model for improving communication between clinicians.Jt Comm J Qual Patient Saf.2006;32(3):167–175.
- The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. Available at: http://www.jointcommission.org/NR/rdonlyres/E3C600EB‐043B‐4E86‐B04E‐CA4A89AD5433/0/universal_protocol.pdf. Accessed January 24, 2010.
- ,,.The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process.J Patient Saf.2007;3:97–106.
- How do we communicate? Communication on Agile Software Projects. Available at: www.agilemodeling.com/essays/communication.htm. Accessed January 24, 2010.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- .Engaging patients at hospital discharge.J Hosp Med.2008;3(6):498–500.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141(7):533–536.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,, et al.Impact of preoperative briefings on operating room delays.Arch Surg.2008;143(11):1068–1072.
- ,,, et al.Operating room briefings: working on the same page.Jt Comm J Qual Patient Saf.2006;32(6):351–355.
- .Doctors and nurses: a troubled partnership.Ann Surg.1999;230(3):279–288.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,, et al.Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication.Arch Surg.2008;143(1):12–17.
Copyright © 2011 Society of Hospital Medicine
Faculty Development for Hospitalists
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
The growth of hospitalists nationally continues at an unprecedented pace.1 In academic medical centers, the development of hospital medicine groups either as independent divisions or as part of divisions of general internal medicine (DGIM) reflects this trend. Drivers for growth in the academic setting include housestaff work hour restrictions, increased need for oversight on teaching services, development of nonhousestaff services, surgical comanagement, and greater emphasis on efficiency, quality, and safety.26 These drivers have created tremendous opportunities for hospitalists, but the rapid growth has also created challenges to achieving traditional academic success.7, 8
While hospitalists feel the traditional academic pressures to produce new knowledge and teach, the extraordinary need to expand clinical services has resulted in a young hospitalist workforce, with most lacking fellowship training. At the same time, there are few senior mentors available. Taken together, many academic hospital medicine (AHM) programs find themselves populated by large cadres of junior faculty without the support, training, and mentoring they need to succeed in a faculty career.9 For hospital medicine groups, the risk to faculty recruitment, retention, productivity, and morale is high.
In this article, we describe the development and implementation of a multifaceted Faculty Development (FD) program whose goal was to provide our faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction.
Methods
Problem Identification
The University of California, San Francisco (UCSF) Medical Center operates nearly 800 beds across 2 hospitals (Parnassus and Mount Zion campuses). The UCSF Division of Hospital Medicine (DHM) provides care on the teaching service (90% of all ward months covered by a hospitalist faculty), a nonhousestaff medical service based at Mount Zion,4 a palliative care service,10 a medical consultation service, a neurosurgical comanagement service, a procedure service, and comanagement on advanced heart failure and cancer services. Like many AHM groups, ours has experienced explosive growth, more than doubling in faculty size in 3 years (50+ faculty by July 2010).
In addition, many of our new faculty joined the division directly after residency training whereas our early hospitalists were mostly former chief residents and/or fellowship‐trained. During a 2‐year period, our division lost several faculty to burnout from clinically heavy positions or because they felt their ultimate academic success was in doubt. During a 2008 divisional retreat, the single greatest need identified was to invest in the development of our first‐year faculty who were felt to be at greatest risk for burnout, dissatisfaction, and failing to integrate into the divisional mission. Based on this result, we set out to develop a program to meet this pressing need.
Needs Assessment
We formed a FD steering committee comprised of faculty from all ranks and career paths in our division (eg, educator, administrator, and investigator), with overrepresentation of recent hires to ascertain how best to meet their needs. Information from the division retreat provided the basis for the program and its priorities. The FD steering committee then outlined ideas that guided program development, which included:
New faculty should be required to meet regularly with assigned faculty mentors during their first year, and expectations for that relationship should be outlined for both parties
New faculty should be required to attend dedicated sessions that build their teaching skills
New faculty should receive a specially designed first year curriculum to provide learnings focused on high‐yield and relevant topics
New faculty should receive a set of goals, or scholarly expectations, for their first year that would foster a partnership between individual faculty and the division to meet those goals
The division should create new structures for FD that promote collaboration, sharing of personal and professional growth and challenges, and a culture of continuous learning
All of the activities that comprise our new FD program must be aligned with our stated mission: to provide the highest quality clinical care, education, system improvements, and research that benefit our patients and trainees by developing successful academic hospitalist faculty.
Program Goals and Objectives
Our DHM FD program established the goal to provide our new faculty with clinical, educational, leadership, and scholarly skills that would promote academic output and foster work satisfaction. From a broader divisional standpoint, the goal was simply to create new FD structures that fostered the division's commitment to the program. The primary objectives of the program were for new faculty to:
Increase their knowledge, skills, and attitudes about key academic hospitalist domains following participation in the program;
Demonstrate successful production of scholarly output, participation in a hospital committee, and participation in a quality or safety improvement initiative by the end of their first year;
Report high levels of satisfaction with the FD program and their first year on faculty.
Program Development Principles
We began by conducting a literature review to draw on the successes and lessons learned from existing FD programs, particularly in large departments, academic centers, and the hospitalist field.1115 We focused our program development on a set of FD principles, which included instructional improvement, organizational development, the development of professional academic skills, and the teaching of specific content.11 Furthermore, whereas many FD programs traditionally focus on mentoring or a longitudinal set of seminars, we believed a multifaceted approach could help shift our culture towards one that prioritized FD and generated a sense of community. We hoped this cultural shift would create an environment that increased faculty satisfaction with their work, with their colleagues, and in our division.
This context drove us to build programmatic activities that not only targeted new faculty, the initial focus of our planning efforts, but also the division more broadly. We wanted to adopt known strategies (eg, mentoring relationships, teaching methods for FD, and grand rounds) but also weave in new ones that targeted AHM and our Division. It was clear that successful programs used a variety of instructional methods, and often combined methods, to create active and engaged faculty. We similarly wanted to create venues for didactic and small‐group learning, but also opportunities for peer learning and facilitated discussions around important topics. Allowing new faculty to learn from each other, and having them observe more senior faculty do the same, would be an important and explicit programmatic element.
Program Description and Implementation
All new faculty meet with Divisional leadership (RMW/BAS), administrative staff (they receive an orientation binder that highlights frequently asked questions and provides service‐specific orientation documents), and the Director of FD (NLS). The latter introduces the DHM FD Program and provides the road map for their first year (Supporting Information). The checklist serves to orient, guide, and emphasize the various programmatic goals, expectations, and logistics. Discussion focuses on the activities targeted to new faculty followed by wider divisional offerings. New faculty activities include:
Coaching Program
Rather than having new faculty independently seek out an appropriate mentor, we explicitly paired each with a more senior hospitalist (eg, 3 years on faculty). We provided explicit goals and expectations for the faculty coach and used a similar road map to guide their role (Supporting Information). We chose to call them coaches rather than mentors because in the first year, we felt a new faculty member needed nuts and bolts support from a big sibling more than they needed formal academic mentoring. We placed the burden of organizing the coaching sessions on the faculty coach and provided them with periodic reminders and suggestions for topics to discuss over the course the year, including supporting the junior faculty's performance against their scholarly benchmarks. Finally, we also organized a peer mentoring session for new facultydesigned to create additional peer support and shared learnings, and establish the importance of these relationships moving forward.
Core Seminars
We created a 12‐hour curriculum to cover a broad range of relevant AHM topics (Table 1). The choice of topics was informed by our needs assessment, suggestions of the FD Steering Committee, and the new faculty themselves. The sessions included a few didactic presentations, but they were largely interactive in a workshop‐style format to allow new faculty to engage the content. For instance, a session on quality improvement asked new faculty to bring a project idea and then work through creating a project plan. We coupled three half‐day sessions with a divisional social activity and made every attempt to ensure new faculty were not distracted by clinical responsibilities (eg, not on a clinical service or coverage was provided).
|
| Core Seminars |
| Being an academic hospitalist: The nuts & bolts |
| Tools for the master clinician |
| Documentation pearls & practices: Clinical, billing, and medico‐legal issues |
| Preparing your first talk: From topic selection to power point presentation |
| Choosing a case and writing it up for a clinical vignette abstract submission |
| Searching for clinical answers: An interactive computer‐lab workshop |
| Introduction to quality improvement |
| Leadership 101: Self‐awareness, your Myers‐Briggs, and leading change |
| Project Management: An exercise in team building |
| Thinking about systems and creating a culture of safety |
| Lunch Seminars |
| Managing and updating your academic CV |
| What to do when a patient on your service dies? |
| Evaluating students & housestaffAnd giving feedback |
| Being an effective ward attending |
| Medical‐legal consultative work & being an expert witness |
| Getting involved in professional societies |
| Understanding the promotion tracks: Practical tips and career preparation |
| Getting involved in hospital committee work |
| Caring for sick family members & navigating the healthcare system as a physician |
| Retirement planning 101: Life after UCSF |
| Time management & creating scholarly work |
| Teaching medical students on the wards |
| Clinical resources: What do you use to find answers? |
Teaching Course
One of our faculty (BAS) delivered the Stanford Faculty Development Clinical Teaching program16 (a train the trainer model designed to teach faculty how to become more effective teachers) to all new faculty. The program consisted of 14 hours of highly interactive curricula, video review, and role plays. The course was offered after hours (4 PM or 5 PM) and with input from the new faculty to ensure availability and participation.
Feedback and Observation
Each new faculty received directed feedback about their teaching and supervision on the housestaff service following their first rotation. Feedback was based on housestaff evaluations and direct observation of the new faculty during patient care and teaching rounds. One of our faculty (BAS) observed each new faculty member during rounds, and met with them individually to provide feedback and generate a discussion about teaching style and improvement opportunities.
Scholarly Expectations
We developed a set of scholarly expectations for new faculty. These helped inform the coach‐new faculty meetings and our selection of content for the Core Seminars. We initially had concerns that these expectations could overwhelm new faculty, but those junior faculty (years 2‐4) on the FD steering committee urged this practice, wishing they had similar guidance in their first year.
From the divisional perspective, we also added a number of new structures.
Grand Rounds
We established a monthly continuing medical education (CME) credit‐granting DHM Grand Rounds that combined a 10‐minute Hospital Medicine Update with a 45‐minute didactic presentation. The updates were presented by new faculty in order to provide them with an opportunity to receive feedback on their teaching and presentation skills (eg, how to give a talk, make PowerPoint slides, etc.). Didactic presentations were given by senior DHM faculty as well as subspecialty colleagues or ones from other departments (eg, dermatology or neurology), disciplines (eg, risk management), or campuses.
FD Lunch Seminar Series
Our division traditionally meets each Monday over the lunch hour to talk about service or academic issues. With a growing division, we believed there was an opportunity to better organize the content of these meetings. Once monthly, we dedicated a lunch session to a Faculty Development Seminar with topics that spanned a variety of interest areas, were driven by faculty suggestions, and were focused on being facilitated discussions rather than didactics. Table 1 provides examples of these seminar topics.
| Survey Statements Reporting Level of Comfort With(% responding somewhat agree or agree) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Identifying important resources within the School of Medicine | 64 | 83 |
| Identifying important resources within the Department of Medicine | 63 | 100 |
| Identifying important resources within the Division of Hospital Medicine | 90 | 100 |
| Identifying important resources within UCSF Medical Center | 72 | 67 |
| Having a system to effectively manage my email | 64 | 67 |
| Having a system to keep my CV updated | 64 | 84 |
| Using my non‐clinical time for academic success | 54 | 67 |
| Best practices for clinical/medico‐legal documentation | 54 | 67 |
| Best practices for billing documentation | 62 | 84 |
| Being an effective supervising ward attending | 90 | 84 |
| Being an effective teacher | 90 | 84 |
| Evaluating students and housestaff performance | 90 | 83 |
| Providing feedback to students and housestaff | 90 | 100 |
| Getting involved in professional societies | 27 | 100 |
| Understanding the difference between promotion pathways | 36 | 67 |
| Getting involved in hospital committee work | 54 | 84 |
| Choosing a good case for a clinical vignette submission to a regional/national meeting | 54 | 83 |
| Creating a poster for presentation at a regional/national meeting | 36 | 84 |
| Giving a lecture to students or residents | 64 | 84 |
| Developing a PowerPoint presentation for a lecture | 45 | 100 |
| Describing my personality type and how it relates to my work | 45 | 100 |
| Understanding important aspects of being a leader | 54 | 100 |
| Explaining the basic principles of quality improvement | 45 | 84 |
| Participating and contributing to a quality improvement project | 54 | 67 |
| Explaining the basic principles of patient safety | 45 | 67 |
| Understanding the factors that contribute to medical errors | 36 | 84 |
| Creating scholarly products from my work | 27 | 50 |
| Identifying what kind of mentors I need for the future | 45 | 100 |
| Category (% completed during first year) | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| Medical student teaching | 90 | 100 |
| Talk for trainees | 45 | 100 |
| Hospital committee involvement | 63 | 100 |
| Participation in a quality or safety project | 33 | 67 |
| Abstract submission | 27 | 50 |
| Identified mentor for year 2 | 63 | 83 |
Quality and Safety Lunch Seminars
In addition to our FD seminars, we also used one lunch session each month to provide updates on performance measures, ongoing quality or safety improvement initiatives, or a broader quality or safety topic. Speakers were either divisional or outside experts, depending on the topic, and organized by our director for quality and safety.
Incubator Sessions
Our director of research (AA) organized a weekly works in progress meeting, to which faculty and fellows brought ideas, grant applications, early manuscript drafts, or other potential scholarship products to obtain feedback and further group mentorship.
Divisional Retreats
We began alternating annual full‐day and mini half‐day retreats as a method to bring the division together, build camaraderie, set strategic priorities, identify divisional goals, and assess needs. These helped guide the creation of additional FD opportunities as well as our overall division's strategy to achieve our academic mission. The outcomes of these retreats led to many significant initiatives and policies, such as changes in compensation models, new scheduling processes, and decisions to spend resources on areas such as quality improvement.
Program Evaluation
Our evaluation focused on measuring the FD program's impact on our new faculty. We tracked their success in completing the stated scholarly expectations and surveyed them about their satisfaction with the programmatic activities, their first year on faculty, and their preparation for year 2. Prior to implementing the program, we surveyed the previous 2 years of new faculty to provide a comparison.
Results
Seven faculty participated in the inaugural program. We compared their scholarly output and experiences (6 faculty completed the survey; 87% response rate) with that of 11 more senior faculty who completed the comparison survey. Of note, the response rate of the comparison group was 69% (5 faculty who departed from our division during the previous 2 years were not surveyed). New faculty were surveyed at the start of the academic year with the follow‐up survey completed the following June. The more senior faculty completed the survey once at the same time as the baseline survey for the new faculty. All new faculty participated in each of the Core Seminars, the Teaching Course, the required number of Coaching sessions, and the observed teaching activity. We did not track their attendance at Divisional activities such as Grand Rounds or the Lunch Seminars.
Overall, the FD programmatic offerings were rated highly by new faculty (on a scale of 1 [lowest] to 5 [highest] for a global rating of each FD activity): Core Seminars 4.83 0.41, Coaching Program 4.5 0.84, Teaching Course 4.5 0.55, Grand Rounds 4.83 0.41, and Lunch Seminars 4.5 0.84. Table 2, which compares responses to a series of end of the year statements posed to new faculty, highlights notable differences in their level of comfort with specific skills and resource awareness. Given the small sample size, statistical significance was not calculated. Table 3 illustrates similar comparisons focused on academic output, which demonstrate that new faculty gave more talks to trainees, had greater involvement in hospital committees, more actively participated in quality and safety projects, and submitted more abstracts to regional or national meetings. New faculty also responded differently to which part of the FD program was most influential with 1 suggesting the Coaching Program, 2 the Core Seminars, 2 the entire program efforts, and 1 did not specify.
Table 4 illustrates comparison responses to a series of directed statements. New faculty all reported greater degrees of satisfaction overall, measured by the above responses, compared to previous faculty.
| Categories | Previous Faculty, % (n = 11) | New Faculty, % (n = 6) |
|---|---|---|
| ||
| Success: To what degree do you feel successful as an academic hospitalist at the end of your first year? (% responding successful or very successful) | 27 | 67 |
| Prepared: To what degree do you feel prepared for academic success moving into your second year on faculty? (% responding prepared or very prepared) | 27 | 100 |
| Part of DHM: I felt like an integral part of our division after my first year on faculty (% responding somewhat agree or agree) | 45 | 84 |
| Expectations: My first year on faculty exceeded my expectations (% responding somewhat agree or agree) | 27 | 84 |
Discussion
We implemented an FD program to foster the academic development of new faculty, and to mitigate the effects of growing clinical demands and a rapid group expansion on our academic mission. The impact of the program was measured by increased work satisfaction and academic output in first year faculty, greater self‐reported comfort in a variety of skills and knowledge of resources, and an improvement in our sense of purpose behind our academic mission. Though the program is only in its second year, we believe the model is of value for other AHM groups, and perhaps even nonacademic groups, all of whom may use such an investment in their hospitalists as a method to improve recruitment, job satisfaction, and retention.
Reviewing our program's first year suggests there were at least 3 keys to our success. First, we benefited tremendously from the time spent crafting a vision for the program and relying heavily on input from the target audience of junior faculty. Moreover, we made every effort to leverage existing resources (eg, using faculty who already taught about a given topic) and time commitments (eg, reshaping our existing Monday lunch meeting). Finally, we increasingly used our FD venues to connect and build networks with colleagues outside our division and within the hospital. This was a deliberate effort to create opportunities for individual faculty to be exposed to and collaborate with nonhospitalists for academic output.
Our research has some limitations, most notably the small sample size in evaluating the program for statistical significance, and the incomplete survey return rates. However, the results were quite consistent and the nonresponses of departed faculty would tend to bias our results toward the null. We also acknowledge the possibility of other confounding factors (eg, changes in clinical compensation models) that may have played a role, although compensation changes were relatively minor during the period studied and faculty did attribute many of the benefits in job satisfaction and skill building to the FD program itself.
Hospital medicine is an unusual field in that there is low barrier to entry and exit. Providers can change jobs without having to say goodbye to a large panel of patients, and in the continued mismatch between available positions and hospitalists, alternative positions can easily and quickly be found if they are dissatisfied.17 In the academic arena, even as hospitalists are hired to fill clinical gaps, they still have to perform under more traditional academic rules in order to be promoted and receive the support and kudos of colleagues and trainees. For both these reasons, early nurturing and socialization is critical to retention and academic success. While some opportunities for FD will be offered by national organizations,18 groups also have local responsibilities to support, mentor, and develop their junior faculty. Not only is such support crucial for the junior faculty themselves, but in our young field, the mentored very quickly become the mentors. Our decision to invest in both mentees and mentors reinforced the importance of mentorship for academic success and retention while planting the seeds for continued success and growth.1923 A recent study suggested that the environment for mentoring may be as important as the mentoring itself, a finding we did not specifically measure, but would support based our anecdotal experiences.24 This orientation toward future needs and creating the right milieu is crucial because demands for continued hospitalist growth are likely to remain.
Moving into year 2 of our FD program and reflecting on the lessons learned from year 1, we've adopted the same multifaceted approach with only minor adjustments to the curriculum, greater expansion of faculty involved in teaching and coaching, and a continued focus on building a sense of community around our academic mission. For the Core Seminars, we moved away from the 3 half‐day sessions and chose to host 2‐hour sessions every other month. This allowed for the same curriculum to be delivered but was much easier to logistically orchestrate. It also had the intended effect of bringing the new faculty together more regularly. In addition, we created dedicated sessions in preparation for our national meeting to allow faculty to bring abstract submissions for review and later, posters and oral presentations for feedback. These added sessions came partly as a suggestion from new faculty in our first year program, and seemed to further energize junior faculty around converting their projects into scholarship. Finally, we continue to further develop coaching and mentoring relationships in our division, partly a result of successful new facultycoach pairings.
In conclusion, our FD program had a noted impact on our new faculty and had a meaningful impact on our division in terms of camaraderie and cohesion, a shared commitment to an academic mission, and a mechanism for recruitment and retention. We hope our practical description for development and implementation of an FD program, including our specific tools, are useful to other groups considering such an initiative.
Acknowledgements
The authors thank Katherine Li for her invaluable assistance in coordinating the DHM FD program. They are also indebted to their faculty colleagues for their time and roles in teaching and mentoring within the program. Dr. Sehgal partly developed this program as part of a project during his California Healthcare Foundation Leadership Fellowship. Dr. Sharpe delivered the teaching workshops at UCSF after completing the Stanford Faculty Development Teaching Program.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
- ,,,.The status of Hospital Medicine Groups in the United States.J Hosp Med.2006;1(2):75–80.
- Accreditation Council for Graduate Medical Education: information related to the ACGME's effort to address resident duty hours and other relevant resource materials. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_index.asp. Accessed August 2010.
- ,,, et al.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294(9):1088–1100.
- ,,,,.Non‐housestaff medicine services in academic centers: models and challenges.J Hosp Med.2008;3(3):247–255.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136(37–38):591–596.
- 2007–08 Hospital Medicine Survey. Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Survey19(4):392–393.
- ,,, et al.Challenges and opportunities in Academic Hospital Medicine: report from the Academic Hospital Medicine Summit.J Hosp Med.2009;4(4):240–246.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1(1):5–6.
- ,.Faculty development: principles and practices.J Vet Med Educ.2006;33(3):317–324.
- ,,, et al.A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8.Med Teach.2006;28(6):497–526.
- ,.A successful approach to faculty development at an independent academic medical center.Med Teach.2008;30:e10–e14.
- ,,,.An innovative approach to supporting hospitalist physicians towards academic success.J Hosp Med.2008;3(4):314–318.
- ,,, et al.The curriculum for the Hospitalized Aging Medical Patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Stanford Faculty Development Clinical Teaching Program. Available at: http://www.stanford.edu/group/SFDP. Accessed August 2010.
- ,,, et al.Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21(10):1079–1085.
- The Academic Hospitalist Academy. Available at: http://www.sgim.org/index.cfm?pageId=815. Accessed August 2010.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296(9):1103–1115.
- ,,.Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine.Acad Med.2004;79(10 Suppl):S9–S11.
- ,,, et al.Retention of junior faculty in academic medicine at the University of California, San Diego.Acad Med.2009;84(1):37–41.
- ,,,.Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program.Acad Med.2002;77:377–384.
- ,,, et al.Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center.Acad Med.2002;77:1235–1240.
- ,,.A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.J Gen Intern Med.2010;25(1);72–78.
Copyright © 2011 Society of Hospital Medicine
Community‐Acquired Pneumonia
Pneumonia may well be called the friend of the aged. Taken off by it in an acute, short, not often painful illness, the old man escapes those cold gradations of decay so distressing of himself and to his friends.
William Osler, MD, 1898
Community‐acquired pneumonia (CAP) is commonly defined as an infection of the pulmonary parenchyma that is associated with at least some symptoms and signs of acute infection, accompanied by the presence of an acute infiltrate on chest radiograph, in a patient not hospitalized or residing in a long‐term‐care facility for 14 days prior to the onset of symptoms.1 CAP continues to be a common and serious illness, causing substantial morbidity and mortality in the adult population. There are an estimated 56 million cases a year in the United States, with greater than 1 million hospitalizations. Community‐acquired pneumonia is one of the most common admitting diagnoses among adults, and with a 30‐day mortality between 10% and 14% for patients admitted to the hospital, it is the leading cause of infectious death in the United States.2 In elderly patients, hospitalization for CAP portends a poor long‐term prognosis. In a Medicare database, the 1‐year mortality for patients with CAP was nearly 40%, compared to 29% in patients with other diagnoses.3 Community‐acquired pneumonia is a model illness in hospital medicineit is a common disease that allows for evidence‐based and cost‐effective management. In addition, many national organizations have proposed multiple quality indicators for community‐acquired pneumonia, thus providing an opportunity for institutional quality improvement. This review article outlines the assessment and management of patients admitted to the hospital with community‐acquired pneumonia.
Etiology
Although many pathogens can cause community‐acquired pneumonia, the clinical syndromes and microbiology of CAP have traditionally been characterized as either typical or atypical. The typical organisms include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, and the atypical organisms include Chlamydia spp., Mycoplasma pneumoniae, Legionella spp., and viruses. This historical distinction has recently come into question. It is now clear that the presenting symptoms, signs, and basic laboratory findings (including the chest radiograph) cannot be reliably used to predict the etiologic pathogen or to distinguish typical from atypical organisms.4 Rather, the specific causative agent of CAP depends more on the degree of patient illness. Table 1 shows what prospective studies with comprehensive diagnostic strategies determined to be the most common pathogens in patients hospitalized for CAP in ICU and non‐ICU settings.5 Streptococcus pneumoniae remains the most common cause of CAP in hospitalized patients and is the most common cause of fatal pneumonia, whereas Legionella spp. is a common cause of severe CAP, more often found in patients requiring admission to the intensive care unit. Gram‐negative bacilli can cause CAP in elderly patients and those recently treated with broad‐spectrum antibiotics or with underlying lung disease. Notably, though, despite improved diagnostic testing, only one quarter of all admitted patients with CAP have the etiologic agent defined, and therefore empiric therapy should be directed broadly at the most likely organisms.6
| Non‐ICU inpatients | ICU inpatients (severe) |
|---|---|
| S. pneumoniae | S. pneumoniae |
| M. pneumoniae | Legionella spp |
| C. pneumoniae | H. influenzae |
| H. influenzae | Gram‐negative bacilli |
| Legionella spp | S. aureus |
| Aspiration | |
| Respiratory viruses |
Clinical Presentation
Patients admitted to the hospital with CAP typically present with a brief history of respiratory complaints, including cough (greater than 90%), dyspnea (66%), sputum production (66%), and pleuritic chest pain (50%); see Table 2.7, 8 In 10%30% of patients, nonrespiratory complaints predominate, including headache, myalgias, fatigue, and gastrointestinal symptoms.6 Elderly patients, an increasing percentage of hospitalized patients, are less likely to present with typical CAP symptoms (such as cough) and more likely to have altered mental status as a presenting symptom.9
| Symptoms | Signs (exam) |
|---|---|
| Cough 90% | Fever 80% |
| Dyspnea 66% | Tachypnea 70% |
| Sputum 66% | Tachycardia 50% |
| Pleuritic chest pain 50% | Focal lung exam >90% |
On physical examination, patients with CAP usually have signs of fever (80%), tachypnea (70%), and tachycardia (50%); see Table 2. Most will have a focal lung exam (>90%) with findings ranging from crackles to bronchial breath sounds.10 No exam finding is specific for the diagnosis of pneumonia, but the absence of fever, tachycardia, and tachypnea significantly reduces the probability of CAP in patients with suspected pneumonia.10 Furthermore, similar to the clinical history, the physical examination of elderly patients with community‐acquired pneumonia is not specific or sensitive for the diagnosis of CAP. For example, up to 40% of elderly patients subsequently determined to have CAP may not have fever.11
Leukocytosis is common in patients with CAP; however, its absence does not rule out disease.12 A number of guidelines recommend laboratory evaluation of electrolytes, urea nitrogen, creatinine, liver enzymes, and bilirubin, although these are used primarily for prognostication and are not specifically useful in the diagnosis of CAP.
DIAGNOSIS
Differential Diagnosis
Given the nonspecific nature of the symptoms and signs associated with CAP, there is no single clinical feature or combination of clinical features that adequately rules in or out the diagnosis of CAP. Consequently, the differential diagnosis to be considered in patients with suspected CAP is broad. Noninfectious diseases can often present with similar clinical syndromes; these include congestive heart failure, exacerbation of chronic obstructive pulmonary disease (COPD), asthma, pulmonary embolism, and hypersensitivity pneumonitis. These diseases can often be distinguished with a thorough history and physical examination.
In addition, other upper‐ and lower‐airway infectious diseases can have similar nonspecific signs and symptoms. In particular, pneumonia must often be differentiated from acute bronchitis, which as a diagnosis accounts for up to 40% of patients evaluated for cough (versus 5% for pneumonia).10 Patients with acute bronchitis frequently do not present with high fevers or hypoxia and in general will not benefit from antibiotic therapy.13 Patients believed to have community‐acquired pneumonia might also be suffering from other pneumonia syndromes including aspiration pneumonia, postobstructive pneumonia, and pneumonia in immunocompromised patients (eg, those with HIV, on steroids, receiving chemotherapy). Determining the correct diagnosis can have implications for therapy and prognosis.
Diagnostic Studies
The diagnosis of community‐acquired pneumonia requires that a patient have both signs and symptoms consistent with pulmonary infection and evidence of a new radiographic infiltrate. Therefore, most guidelines recommend that all patients with a possible diagnosis of CAP be evaluated with chest radiography.1, 14, 15
The specific radiographic findings in community‐acquired pneumonia range from lobar consolidation to hazy focal infiltrate to diffuse bilateral interstitial opacities (see Figure 1). Although chest radiography has traditionally been considered the gold standard for the diagnosis of CAP, its exact performance characteristics are unknown, and it is clearly not 100% sensitive or 100% specific. The utility of the chest radiograph can be limited by patient body habitus, underlying lung disease, or dehydration. Computed tomography (CT) scanning, although not recommended for routine use, can identify pulmonary consolidation in up to 30% of patients with a normal or equivocal chest radiograph in whom pneumonia is suspected and can also identify complications of pneumonia including an empyema or pulmonary abscess.16

Limitations in the performance of the chest radiograph have resulted in an interest in the diagnostic performance of serologic markers of infection such as C‐reactive protein (CRP), procalcitonin, and soluble triggering receptor expressed on myeloid cells (s‐TREM).1719 Preliminary evidence suggests these inflammatory markers may ultimately prove useful in differentiating infectious from noninfectious pulmonary processes, but regular use of these new tests cannot currently be recommended.
Most expert guidelines state that 2 sets of blood cultures should be taken and analyzed prior to antibiotic administration in all patients admitted to the hospital with suspected community‐acquired pneumonia.1, 14, 15 Isolation of bacteria from blood cultures in CAP is a very specific way to identify a causative organism in order to subsequently narrow therapy and also identifies a high‐risk group of patients because bacteremia is associated with increased mortality. Obtaining blood cultures within 24 hours of admission has been associated with 10% lower odds of 30‐day mortality in patients with CAP,20 and as a result, drawing blood cultures prior to antibiotic administration is a national quality indicator for CAP.
There are, however, a number of problems with the routine acquisition of blood cultures in all patients admitted with CAP. Practically, the cultures can be difficult to obtain, can potentially delay the initiation of antibiotics, and are often contaminated, which has been shown to increase both cost and length of stay.21, 22 The yield is generally low: the true‐positive bacteremia rate for admitted patients with CAP ranges from 6% to 9%, and the culture results rarely change management or outcomes.23, 24 Given these limitations, many have argued that blood cultures should be obtained with a more targeted approach. A recent study used a Medicare database to create a decision‐support tool to help maximize the value of blood cultures in CAP.25 The predictors of a positive blood culture are shown in Table 3. Not obtaining cultures on patients who had received prior antibiotics or had no risk factors resulted in about 40% fewer overall cultures while identifying approximately 90% of bacteremias. In their guidelines, the British Thoracic Society (BTS) advocates a similar strategy, recommending blood cultures be omitted in nonsevere pneumonia and in patients without comorbidities.15, 26 Although recommendations vary for non‐severe CAP in hospitalized patients, all professional society guidelines agree that blood cultures should be obtained in critically ill patients, and if cultures are obtained, they should be drawn prior to antibiotics.1, 14, 15, 26
| Comorbidities |
| Liver disease |
| Vital signs |
| Systolic blood pressure < 90 mm Hg |
| Temperature < 35C or 40C |
| Pulse 125 beats/min |
| Laboratory and radiographic data |
| Blood urea nitrogen (BUN) 30 mg/dL |
| Sodium < 130 mmol/L |
| White blood cells < 5000/mm3 or > 20,000/mm3 |
| Prior use of antibiotics (negative predictor) |
Substantial controversy surrounds the utility of routine sputum gram stains and cultures for patients admitted to the hospital with CAP. The Infectious Disease Society of America (IDSA) and the British Thoracic Society (BTS) both recommend that all patients admitted to the hospital with community‐acquired pneumonia should have a gram stain and culture of expectorated sputum.1, 15, 26 Both organizations argue sputum collection is a simple and inexpensive procedure that can potentially identify pathogenic organisms and can affect both initial and long‐term antibiotic therapy. Most notably, they highlight gram stain specificity of greater than 80% for pneumococcal pneumonia. Conversely, the American Thoracic Society (ATS) argues that sputum gram stains and cultures generally have low sensitivity, specificity, and positive predictive value.14 Furthermore, they argue the utility of sputum testing is also limited practically; in one study 30% of patients could not produce an adequate sputum specimen and up to 30% had received prior antibiotic therapy, substantially reducing the yield.27 In another study, good‐quality sputum with a predominant morphotype could be obtained in only 14% of patients admitted with CAP.28 However, targeting sputum analysis to patients who have not received prior antibiotics and are able to produce an adequate sample improved the yield significantly.29 In addition, with increasing rates of antibiotic resistance among common community isolates (ie, S. Pneumoniae) and the increasing prevalence of infecting organisms not targeted by routine empiric therapy (methicillin‐resistant Staphylococcus Aureus [MRSA]), isolation of potential causative pathogens is increasingly important. We believe that severely ill patients with CAP (such as patients admitted to the ICU), as well as patients with identifiable risk factors for uncommon or drug‐resistant pathogens (eg, Pseudomonas aeruginosa, enteric gram‐negative rods, MRSA, etc.) should have sputum sent for gram stain and culture. Ideally, sputum obtained for gram stain and culture should be:
-
Prior to antibiotic therapy,
-
A deep‐cough, expectorated specimen,
-
A purulent specimen (>25 polymorphonucleacytes and less than 10 squamous cells per high‐powered field), and
-
Rapidly transported to the laboratory.
Subsequent gram stain and culture results should be interpreted in the specific clinical context and antibiotic choices targeted appropriately.
Alternative Diagnostic Tests
In recent years, there has been growth in additional diagnostic tests targeting specific organisms. The pneumococcal urinary antigen assay is a relatively sensitive (50%80%) and highly specific (90%) test for the detection of pneumococcal pneumonia, when compared with conventional diagnostic methods.27 The test is simple, convenient, rapid ( 15 min), and, with its high specificity, may allow for more focused antimicrobial therapy early in management. Current limitations include the possibility of false‐positive tests in patients colonized with S. pneumoniae or infected with other streptococcal species, as well as the inability to determine antibiotic sensitivity from positive tests. Updated IDSA and BTS guidelines state pneumococcal urinary antigen testing is an acceptable adjunct to other diagnostic tests, but blood and sputum analyses should still be performed.26, 27 For patients with suspected Legionella pneumonia (primarily critically ill and immunocompromised patients or in association with regional outbreaks), the urinary Legionella antigen assay is the test of choice, which detects 80%95% of community‐acquired cases of Legionnaires' disease with a specificity of 90%.27
During the winter months (typically from October to March), rapid antigen testing for influenza is generally recommended for patients with signs or symptoms consistent with influenza.27 The sensitivity of these tests is approximately 50%70%, so negative test results do not exclude the diagnosis, but results can be important epidemiologically and therapeutically (differentiating influenza A and B strains).27 Diagnostic tests targeting other common CAP pathogens, such as serologic tests for Mycoplasma pneumoniae or Chlamydia spp, should not be routinely performed. Testing for less common causative pathogens such as Mycobacterium tuberculosis should only be employed in the appropriate clinical setting.
ADMISSION DECISION
Once the diagnosis of CAP has been made, the initial site where treatment will occur, whether the hospital or the home, must be determined. The decision to hospitalize should be based on 3 factors: 1) evaluation of the safety of home treatment, 2) calculation of the Pneumonia Severity Index (PSI), and 3) clinical judgment of the physician.27 The PSI, or PORT (Pneumonia Outcomes Research Team) score, is a validated prediction rule that quantifies mortality and allows for risk stratification of patients with community‐acquired pneumonia.2 The PSI combines clinical history, physical examination, and laboratory data at the time of admission to divide patients into 5 risk classes and to estimate 30‐day mortality (Figure 2), which ranges from 0.1% of patients in risk class I to 27.0% in risk class V.2
On the basis of the estimated prognosis and in the absence of concerns about home safety or comorbidities, patients in risk classes I, II, and III should be managed at home. Many prospective trials have shown that implementation of PSI significantly increases the number of low‐risk patients managed outside the hospital, with no differences in quality of life, complications, readmissions, or short‐term mortality.30, 31 Most recently, a trial randomizing patients in risk classes II and III to treatment in the hospital or at home found no significant differences in clinical outcomes but did find that patients were more satisfied with care at home.32 Because the number of patients with CAP being treated at home is increasing, the American College of Chest Physicians recently published a consensus statement on the management of community‐acquired pneumonia in the home.33 All national guidelines for the management of community‐acquired pneumonia recommend using the PSI to help determine the initial location of treatment, with the caveat that using the prediction rule should never supersede clinical judgment in the decision about whether to admit.1, 14, 15, 26, 27 A practical decision tree for the use of the PSI is shown in Figure 3.
There are no reliable prediction rules for deciding on whether admission to the intensive care unit is necessary. Hemodynamic instability requiring resuscitation and monitoring or respiratory failure requiring ventilatory support are clear indications for ICU admission. Additional variables such as tachypnea (respiratory rate 30), altered mental status, multilobar disease, and azotemia are associated with severe CAP and should prompt consideration of ICU admission, especially when 2 or more variables coexist.14
TREATMENT
Initial Treatment
Once the admission decision is made and the initial diagnostic tests are completed (including blood and sputum cultures), patients with presumed community‐acquired pneumonia should receive necessary supportive care (O2, intravenous fluids, etc.) and prompt antimicrobial therapy. Antibiotics should be administered within 4 hours of arrival to patients with suspected CAP, as such prompt administration may be associated with shorter in‐hospital stays and decreased 30‐day mortality.34, 35 Regulatory organizations such as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the Center for Medicare Services (CMS) have made delivery of antibiotics in less than 4 hours a hospital quality measure.
Despite diagnostic testing, the specific etiologic agent causing the pneumonia of a patient remains unknown in up to 75% of those admitted to the hospital.14 Most expert guidelines therefore recommend broad‐spectrum empiric therapy targeting both the typical and the atypical organisms that commonly cause CAP (Table 1).
Recommendations for empiric antibiotics are driven by 2 key factors: antibiotic resistance by S. pneumoniae and the results of studies of CAP treatment outcomes. Historically, patients with suspected community‐acquired pneumonia were treated with penicillin with generally good outcomes. Recently, the rate of S. pneumoniae isolates resistant to penicillin has risen dramatically in the United States, ranging between 20% and 30%, with high‐level resistance (MIC 4 mg/L) as high as 5.7%.36, 37 Concurrently, the rates of resistance of S. pneumoniae to many other antibiotics commonly used to treat CAP have also risen.37 Despite increasing resistance overall, most U.S. pneumococcal isolates have low resistance to third‐generation cephalosporins and fluoroquinolones with enhanced activity against S. pneumoniae.3638 In addition, despite increasing resistance by pneumococcal isolates to penicillin, several observational studies have shown that regardless of initial therapy, resistance to penicillin as well as third‐generation cephalosporins is not associated with higher mortality or worse outcomes when controlled for other risk factors for drug resistance.39, 40 An exception to that rule is pneumococcal isolates that are very highly resistant to PCN (MIC 4 mg/dL). At least one study has shown that patients with such isolates may be at higher risk for adverse outcomes and should probably not be treated with penicillins.1, 14, 15, 41 However, nationally, fewer than 6% of pneumococcal isolates have this level of resistance.37
The rationale for empiric broad‐spectrum coverage against both typical and atypical organisms has arisen from many retrospective and observational studies that have suggested that there is clinical benefit and improved outcomes with such regimens. One large retrospective study showed that in elderly patients with CAP, fluoroquinolone monotherapy was associated with lower 30‐day mortality when compared to monotherapy with a third‐generation cephalosporin.34 Adding an extended‐spectrum macrolide (eg, azithromycin) to an extended‐spectrum ‐lactam (eg, ceftriaxone) in the treatment of patients hospitalized with nonsevere CAP also appears to be associated with improved outcomes. Adding a macrolide has resulted in shorter lengths of stay (LOS), less treatment failure, and lower mortality.34, 4244 Similarly, according to unpublished observations, adding doxycycline to a ‐lactam as initial therapy was associated with a benefit of decreased mortality.45 The presumed etiology of the benefit has been the addition of specific coverage of atypical organisms, such as Mycoplasma pneumoniae and Chlamydia pneumoniae, which are common causes of CAP (Table 1). Others have proposed that the benefit of therapy with macrolides may be derived from the inherent anti‐inflammatory properties of macrolides.46 Because research has shown a benefit of dual versus monotherapy across a spectrum of antibiotics, others have proposed the benefit is simply a result of receiving double antibiotic coverage. In particular, 2 studies found a benefit of reduced mortality from combination therapy over monotherapy in bacteremic pneumococcal pneumonia.47, 48
Yet the accumulated evidence for adding coverage of atypical organisms has been only retrospective and observational. Because of this, the recommendation to routinely add antibiotics active against atypical organisms has been questioned by some. Two recent meta‐analyses and a systematic review examined all the available data on the need for atypical coverage in the treatment of patients with community‐acquired pneumonia.4951 Surprisingly, none showed a benefit in clinical efficacy or survival in patients treated with agents active against both atypical and typical organisms when compared to regimens with only typical coverage. In subset analyses, there was a benefit to providing empiric atypical coverage in patients subsequently shown to have Legionella spp. as a causative pathogen. However, this organism was uncommon in all 3 studies. Unfortunately, most studies included in the meta‐analyses compared fluoroquinolone or macrolide monotherapy with third‐generation cephalosporin monotherapy. There have been no high‐quality randomized, controlled trials of the treatment of hospitalized patients with CAP assessing combination therapy covering both typical and atypical organisms with monotherapy targeting typical organisms alone. High‐quality trials are warranted.
Despite the recent articles questioning the importance of atypical coverage, citing the substantial retrospective data and the general inability to identify causative organisms in most cases of CAP, adding a second agent with atypical coverage to a ‐lactam currently appears to be the most efficacious empiric treatment for CAP. Nearly all expert guidelines for the management of community‐acquired pneumonia recommend this empiric approach.1, 14, 27
Table 4 displays our recommendations for the treatment of community‐acquired pneumonia requiring hospitalization. Before implementation of these guidelines, hospitalists should consult with their infectious disease experts and consider local resistance patterns. In general, a typical adult patient with non‐severe CAP without additional risk factors should receive a parenteral extended‐spectrum ‐lactam plus either doxycycline or an advanced macrolide (see Table 4). Extended‐spectrum ‐lactams include cefotaxime, ceftriaxone, ampicillin‐sulbactam, and ertapenem. A respiratory fluoroquinolone as a single agent can be used for non‐ICU patients with CAP, but some agencies, including the Centers for Disease Control (CDC), discourage routine use of these agents in all patients secondary to concerns about cost and increasing gram‐negative rod fluoroquinolone resistance.52, 53
| Patient group | Empiric antibiotic therapy |
|---|---|
| |
| Inpatient, non‐ICU | ‐Lactama + either doxycycline or an advanced macrolideb |
| Severe ‐lactam allergyc | Respiratory fluoroquinoloned |
| Inpatient, ICU | |
| No risk for Pseudomonas | ‐Lactam + either an advanced macrolide or a respiratory fluoroquinolone |
| Severe ‐lactam allergy | Respiratory fluoroquinolone + clindamycin |
| Pseudomonas risk factorse | Antipseudomonal ‐lactamf + an antipseudomonal fluoroquinoloneg |
| Severe ‐lactam allergy | Aztreonam + a respiratory fluoroquinolone |
| MRSA risk factorsh | Add vancomycin to above regimens |
| From nursing home | Should be treated as nosocomial/health‐care‐associated pneumonia |
| Aspiration pneumonia | ‐Lactam or respiratory fluoroquinolone clindamycini |
Patients hospitalized with severe CAP who require ICU‐level care are at increased risk of Legionella spp. and drug‐resistant S. pneumoniae, which must be reflected in their initial antibiotic therapy.5 Patients with severe pneumonia should receive an intravenous extended‐spectrum ‐lactam plus either an intravenous macrolide or an intravenous respiratory fluoroquinolone.
All patients with severe CAP who are admitted to the intensive care unit should be routinely screened for risk factors for Pseudomonas aeruginosa. The known risk factors for pseudomonal infection are: bronchiectasis, immunosuppression including more than 10 mg/day of prednisone, malnutrition, and treatment with broad‐spectrum antibiotics in the last month.14 Those at risk for Pseudomonas aeruginosa or other resistant gram‐negative rod infection should be treated with an antipseudomonal ‐lactam plus an antipseudomonal fluoroquinolone. Many patients with severe CAP have risk factors for MRSA infection including recent prolonged hospitalization, recent use of broad‐spectrum antibiotics, and significant underlying lung disease, which should be considered in choosing initial antibiotic therapy.54 In addition, there have been reports of patients without underlying risk factors presenting with severe community‐acquired MRSA pneumonia. Many of these patients were younger and the MRSA pneumonia was associated with a necrotizing or cavitary disease requiring prolonged ICU stays.5558 In such cases or if an institution's rate of methicillin resistance in S. aureus community isolates is high (>15%20%), it may be appropriate to add initial empiric MRSA coverage for patients admitted to the ICU with CAP.55
Some patients will have unique risk factors and clinical presentations, which may require modification of these empiric recommendations. Several studies found 5%15% of cases of community‐acquired pneumonia to be aspiration pneumonia.57 Risk factors for aspiration events include, among others, dysphagia, history of stroke, altered level of consciousness, poor dentition, and tube feeding. Aspiration pneumonia traditionally was believed to be secondary to oral anaerobes, but recent research suggests gram‐positive cocci and gram‐negative rods are the predominant organisms.58 Antibiotic therapy in patients with clear aspiration pneumonia should be directed at these microbes with an extended‐spectrum ‐lactam (eg, ceftriaxone) or a respiratory fluoroquinolone (eg, levofloxacin or moxifloxacin). Anaerobic bacterial coverage can be added in patients with severe periodontal disease, alcoholism, concern for empyema, or evidence of aspiration with pulmonary abscess.58
Patients residing in long‐term care facilities are at high risk of contracting pneumonia. The microbiology of infections acquired in nursing facilities is similar to that in hospital‐acquired cases.59, 60 As a result, patients who develop pneumonia in institutional settings such as nursing homes should be treated with broad‐spectrum antibiotics, including coverage for MRSA.
Subsequent Treatment
Initial empiric antibiotic treatment should be modified based on the results of diagnostic testing. Although the specific etiologic agent is determined in only 25% of cases of CAP,35 when an organism is isolated, antibiotic coverage should be narrowed to cover that particular organism with an antibiotic with adequate lung penetration. Evidence suggests clinicians often do not adjust or narrow antibiotics based on sensitivity results, potentially breeding resistant organisms.61
Patients hospitalized with CAP usually improve quickly if they receive early, appropriate antibiotic therapy and supportive care. Excluding patients with severe CAP requiring intensive care unit admission, most patients resolve their tachycardia, tachypnea, and fever by day 2 or 3.62 Recent practice experience, evidence, and published guidelines14, 27 all indicate that patients can safely be transitioned to oral antibiotic therapy earlier in their hospital course. Table 5 outlines criteria that can be used to identify patients who have had an adequate response to parenteral therapy and can be considered for a switch to oral antibiotics. If these criteria are met, patients have less than a 1% chance of clinical deterioration necessitating admission to an ICU or transitional care unit.62 When an etiologic organism is not identified, oral therapy should reflect a spectrum of coverage to that of the initial intravenous therapy. In some cases, this may require use of more than one oral agent. We have had success, however, transitioning non‐ICU patients initially treated with intravenous ceftriaxone plus oral doxycycline, typically for 4872 hours, to oral doxycycline monotherapy at discharge.45
| Stable vital signs and clinical criteria for 24 hours |
| Temperature 37.8C (100F) |
| Heart rate 100 beats per minute |
| Respiratory rate 24 breaths per minute |
| Systolic blood pressure 90 mm Hg |
| Oxygen saturation (on room air) 90% |
| Ability to take oral medications |
There have been a limited number of high‐quality randomized trials examining the optimal duration of treatment for community‐acquired pneumonia. Most practice guidelines recommend 710 days for patients with CAP requiring hospitalization, with 14 days for documented Mycoplasma pneumoniae or Chlamydia pneumoniae. One recent randomized trial of patients with mild to severe CAP showed a short course of high‐dose levofloxacin (750 mg daily 5 days) was at least as effective as normal dosing (500 mg daily 10 days).63 Clinical experience with high‐dose levofloxacin is limited, but this regimen can be considered because it may reduce costs and exposure to antibiotics. When diagnosed, Legionella is usually treated for 1021 days, but 14 days is adequate with macrolides because of their long half‐life.27 Patients with more virulent pathogens like Staphylococcus aureus or Pseudomonas aeruginosa or other suppurative complications should be treated for at least 14 days.1, 14, 15, 27 In determining length of therapy, clinicians should use these durations of treatment as guides, and to individualize therapy, they should always consider patient age and frailty, comorbid conditions, severity of illness, and hospital course.
Failure to Respond
Although most patients hospitalized for CAP will improve rapidly and reach clinical stability in 23 days, some patients fail to respond. Some studies have estimated that failure to improve or clinical deterioration occurs in 5%10% of patients in the first 23 days.64 The common reasons for clinical decline or nonresponse to treatment, highlighted in Table 6, are:
-
Incorrect diagnosis: Illnesses such as congestive heart failure, pulmonary embolism, neoplasms, and hypersensitivity pneumonitis can mimick CAP.
-
Inadequate antibiotic selection: The etiologic agent may be resistant to empiric antibiotic selections. Examples would include methicillin‐resistant Staphylococcus aureus (MRSA) or multiresistant gram‐negative bacilli.
-
Unusual pathogen: CAP syndromes can be caused by myriad unusual organisms including Pneumocystis jirovecii, mycobacterium tuberculosis, endemic fungal infections (eg, coccidioidomycosis), and nocardiosis.
-
Complications of pneumonia: Specific complications of CAP include empyema, pulmonary abscess, extrapulmonary spread including meningitis or endocarditis, or other organ dysfunctions such as renal failure or myocardial infarction.
-
Inadequate host response: Despite appropriate antibiotic and supportive therapy, patients with CAP often fail to respond.
| Incorrect diagnosis of CAP. |
| Inadequate or inappropriate antibiotic selection for CAP. |
| Unusual pathogen causing CAP. |
| Pulmonary or extrapulmonary complication of CAP. |
| Inadequate or poor host response. |
Progressive pneumonia despite appropriate therapy and empyema were the most common causes of failure to respond in the first 72 hours in a recent study.64 Risk factors for early failure were older age (>65 years), Pneumonia Severity Index > 90, Legionella pneumonia, gram‐negative pneumonia, and initial antimicrobial therapy discordant with final culture and susceptibility results. The initial evaluation of the nonresponding patient should address these common causes and is likely to include additional imaging (CT), sampling of potential extrapulmonary infection (thoracentesis), and, in some cases, bronchoscopy.
DISCHARGE/FOLLOW‐UP PLANS
Patients hospitalized for community‐acquired pneumonia can be safely discharged when they have reached clinical stability, are able to tolerate oral medications, have no other active comorbid conditions, and have safe, close, appropriate outpatient follow‐up (see Table 7). Clinical pathways employing these discharge criteria have been found to be safe and effective in reducing the length of stay for CAP. Most important, patients should have met most if not all of the vital sign and clinical criteria noted in Table 5 in the criteria for switching to oral therapy. Patients with 2 or more abnormal vital signs (instabilities) within 24 hours prior to discharge are at high risk of readmission and mortality, but those with one or no abnormal vital signs generally have good outcomes.65 Absent other clinical factors or extenuating circumstances (persistent hypoxia, poor functional status, etc.), most patients with CAP should reach clinical stability by day 3 or 4, be considered for a switch to oral therapy, and, if stable, be discharged shortly thereafter.
| Patients should: |
|
Meet clinical criteria in Table V. |
| Be able to tolerate oral medications (no need to observe for 24 hours on oral therapy). |
| Have no evidence of active comorbid conditions (myocardial ischemia, pulmonary edema, etc.). |
| Have a normal mental status (or have returned to their baseline). |
| Have safe, appropriate outpatient follow‐up. |
When patients with CAP are discharged from the hospital, they should be counseled about the expected course of recovery. Most important, patients and families must be informed that many symptoms of CAP may persist well after hospitalization. In one study, up to 80% of patients reported persistent cough and fatigue 1 week after discharge, and up to 50% still had dyspnea and sputum production. In some, the cough can last for 46 weeks.8
All patients discharged after treatment of community‐acquired pneumonia should have follow‐up with their outpatient provider. The physician responsible for their inpatient care should communicate directly with the provider and outline the hospital course, the discharge medications, and the duration of antibiotic therapy. There is no specific time frame within which patients must be seen, but follow‐up should be dictated by patient age, comorbidities, clinical stability at discharge, and degree of illness. The American Thoracic Society guidelines do recommend patients with a substantial smoking history who are hospitalized with CAP have a follow‐up chest radiograph 46 weeks after discharge to establish a radiographic baseline and exclude the possibility of underlying malignancy.14 However, several studies have suggested that radiographic resolution may take 3 or more months in some patients, especially the elderly and those with multilobar disease.66
PREVENTION
Prevention of community‐acquired pneumonia and pneumonic syndromes has traditionally relied on vaccination with the polysaccharide pneumococcal pneumonia vaccine and the seasonal influenza vaccine. The vaccine for S. pneumoniae used in adults is composed of the 23 serotypes that cause 85%90% of the invasive pneumococcal infections in the United States. Although in randomized trials the vaccine has not consistently prevented community‐acquired pneumonia or death in elderly patients or those with comorbidities, it likely prevents invasive pneumococcal infection.67 National guidelines and the CDC recommend the pneumococcal vaccine be given to all patients older than 65 years and those with chronic medical conditions.1, 14, 15
The seasonal influenza vaccine has clearly been shown to decrease influenza‐related illness in elderly and high‐risk patient populations. As well, in a meta‐analysis and a large observational study of patients older than 65 years, vaccination against influenza prevented pneumonia, hospitalization, and death.68, 69 Vaccination of health care workers may also confer a benefit to elderly patients of reduced mortality. The CDC recommends the influenza vaccine for all patients more than 50 years old, those with comorbidities, those at high risk for influenza, and health care workers in both inpatient and outpatient settings.
Pneumococcal and influenza vaccination have traditionally been relegated to the outpatient setting. National guidelines and the CDC recommend vaccination of all eligible hospitalized patients. Vaccination is safe and effective with almost any medical illness, and both vaccines can be given simultaneously at discharge.69 Both JCAHO and CMS have defined administration of the pneumococcal and influenza vaccines to patients hospitalized with CAP as a quality measure. Using standing orders is the most effective means of ensuring vaccination.
Some evidence suggests that tobacco smokers are at increased risk of invasive pneumococcal disease or pneumonia.70 Patients hospitalized (for all illnesses, but for CAP in particular) should be counseled about smoking cessation and offered pharmacotherapy and outpatient follow‐up. And, finally, recent observational data suggests that use of acid suppressive therapy, including proton pump inhibitors and H‐2 receptor antagonists, may be associated with an increased risk of developing CAP.71 Patients using these agents who are admitted with CAP should have their indications for treatment reviewed, especially when the pneumonia has been recurrent and there is no clear indication for continued use of acid suppressive therapy, in which case they should be discontinued in the hospital.
CONCLUSIONS
Community‐acquired pneumonia remains a common cause for hospitalization of adult patients, with significant associated morbidity and mortality. Although there are multiple expert guidelines for the management of community‐acquired pneumonia, further research is urgently needed. Clinicians need improved diagnostic tests that enable an earlier and more accurate diagnosis of CAP. In addition, the etiologic agent causing CAP is rarely discovered; improved microbiologic studies might enable antibiotic therapy to be targeted to the organisms responsible. High‐quality randomized, controlled trials examining empiric antibiotic therapy in CAP are needed, especially related to the addition of agents covering atypical organisms. Last, the general management of patients hospitalized with CAP is marked by significant heterogeneity, and research and initiatives focusing on improving the quality and process of care of patients with CAP are needed.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Practice guidelines for the management of community‐acquired pneumonia.Clin Infect Dis.2000;31:347–382.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Pneumonia: still the old man's friend?Arch Intern Med.2003;163:317–323.
- ,,, et al.New and emerging etiologies for community‐acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases.Medicine.1990;69:307–316.
- .Community‐acquired pneumonia.Lancet.2003;362:1991–2001.
- ,,, et al.Processes and outcomes of care for patients with community‐acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team (PORT) cohort study.Arch Intern Med.1999;159:970–980.
- ,.Management of community‐acquired pneumonia.N Engl J Med.2002;347:2039–2045.
- ,,, et al.Measuring symptomatic and functional recovery in patients with community‐acquired pneumonia.J Gen Intern Med.1997;12:423–430.
- ,,, et al.Influence of age on symptoms at presentation with patients with community‐acquired pneumonia.Arch Intern Med.1997;157:1453–1459.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Community‐acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes.Medicine.2003;82:159–169.
- ,.Testing strategies in the initial management of patients with community‐acquired pneumonia.Ann Intern Med.2003;138:109–118.
- ,.Uncomplicated acute bronchitis.Ann Intern Med.2000;133:981–991.
- ,,, et al.American Thoracic Society: Guidelines for the management of community‐acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.British Thoracic Society guidelines for the management of community acquired pneumonia in adults.Thorax.2001;56:Suppl. 4,IV1–IV64.
- ,,,,.High‐resolution computed tomography for the diagnosis of community‐acquired pneumonia.Clin Infect Dis.1998;27:358–363.
- ,,, et al.Performance of a bedside C‐reactive protein test in the diagnosis of community‐acquired pneumonia in adults with acute cough.Am J Med.2004;116:529–535.
- ,,, et al.Effect of procalcitonin‐guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster‐randomised, single‐blinded intervention trial.Lancet.2004;363:600–607.
- ,,, et al.Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia.N Engl J Med.2004:350:451–458.
- ,,, et al.Quality of care, process, and outcomes in elderly patients with pneumonia.JAMA.1997;278:2080–2084.
- ,,,.Limited usefulness of initial blood cultures in community acquired pneumonia.Emerg Med J.2004;21:446–448.
- ,,.Contaminant blood cultures and resource utilization. The true consequences of false‐positive results.JAMA.1991;265:365–369.
- ,,, et al.The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community‐acquired pneumonia: a prospective observational study.Chest.2003;123:1142–1150.
- ,,, et al.Clinical utility of blood cultures in adult patients with community‐acquired pneumonia without defined underlying risks.Chest.1995;108:932–936.
- ,,,.Predicting bacteremia in patients with community‐acquired pneumonia.Am J Respir Crit Care Med.2004;169:342–347.
- British Thoracic Society. BTS Guidelines for the management of community acquired pneumonia in adults—2004 update. Available at: www.brit‐thoracic.org/guidelines.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Update of guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- ,,, et al.Assessment of the usefulness of sputum culture for diagnosis of community‐acquired pneumonia using the PORT predictive scoring system.Arch Intern Med.2004;164:1807–1811.
- ,,.Diagnostic value of microscopic examination of gram‐stained sputum and sputum cultures in patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2004;39(2):165–169.
- ,,, et al.Safely increasing the proportion of patients with community‐acquired pneumonia treated as outpatients: an interventional trial.Arch Intern Med.1998;158:1350–1356.
- ,,, et al.A critical pathway for treatment of community‐acquired pneumonia.JAMA.2000;283:2654–2655.
- ,,, et al.Outpatient care compared with hospitalization for community‐acquired pneumonia. A randomized control trial in low‐risk patients.Ann Intern Med.2005;142:165–172.
- ,,.Management of community‐acquired pneumonia in the home.Chest.2005;127:1752–1763.
- ,,,,.Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia.Arch Intern Med.1999;159:2562–2572.
- ,,,,.Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community‐acquired pneumonia.Arch Intern Med.2004;164:637–644.
- ,,, et al.Increasing prevalence of multidrug‐resistant Streptococcus pneumoniae in the United States.N Engl J Med.2000;343:1917–1924.
- ,,, et al.Susceptibility patterns of Streptococcus pneumoniae isolates in North America (2002–2003): contemporary in vitro activities of amoxicillin/clavulanate and 15 other antimicrobial agents.Int J Antimicrob Agents.2005;25(4):282–289.
- ,,, et al.Antimicrobial resistance among Streptococcus pneumoniae in the United States: have we begun to turn the corner on resistance to certain antimicrobial classes?Clin Infect Dis.2005;41(2):139–148.
- ,,, et al.Pneumonia acquired in the community through drug‐resistant Streptococcus pneumoniae.Am J Respir Crit Care.1999;159:1835–1842.
- ,,, et al.Drug‐resistant pneumococcal pneumonia: clinical relevance and related factors.Clin Infect Dis.2004;38:787–798.
- ,,, et al.Mortality from invasive pneumococcal pneumonia in the era of antibiotic resistance, 1995–1997.Am J Public Health.2000;90(2):223–9.
- ,,, et al.Lower mortality among patients with community‐acquired pneumonia treated with a macrolide plus a beta‐lactam agent versus a beta‐lactam alone.Eur J Clin Microbiol Infect Dis2005;24:190–195.
- ,,,.Impact of initial antibiotic choice on clinical outcomes in community‐acquired pneumonia: analysis of a hospital claims‐made database.Chest.2003;123:1503–1511.
- ,,,.Antimicrobial selection for hospitalized patients with presumed community‐acquired pneumonia: a survey of nonteaching US community hospitals.Ann Pharmacother2000;34:446–452.
- ,,,,.J Hosp Med.2006;1:7–12.
- .Anti‐inflammatory effects of macrolides—an underappreciated benefit in the treatment of community‐acquired respiratory tract infections and chronic inflammatory pulmonary conditions?J Antimicrob Chemother.2005;55:10–21.
- ,,, et al.Addition of a macrolide to a beta‐lactam based empirical antibiotic regimen is associated with lover in‐hospital mortality for patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2003;36:389–395.
- ,,, et al.Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia.Am J Respir Crit Care Med.2004;170:440–444.
- ,,,.Empiric antibiotic coverage of atypical pathogens for community‐acquired pneumonia in hospitalized adults.Cochrane Database Syst Rev.2005;2:CD004418.pub2.
- ,,.Effectiveness of β lactam antibiotics compared with antibiotics active against atypical pathogens in non‐severe community‐acquired pneumonia: meta‐analysis.Br Med J.2005;330:456.
- ,,,.Empirical atypical coverage for inpatients with community‐acquired pneumonia.Arch Intern Med.2005;165:1992–2000.
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888.
- ,,, et al.First‐generation fluoroquinolone use and subsequent emergence of multiple drug‐resistant bacteria in the intensive care unit.Crit Care Med.2005;33(2):283–289.
- ,.Etiology of community‐acquired pneumonia.Clin Chest Med.2005;26:47–55.
- .Community‐associated methicillin‐resistant Staphylococcus aureus: not only a cause of skin infections, also a new cause of pneumonia.Curr Opin Infect Dis.2005;18:123–124.
- ,,, et al.Severe community‐onset pneumonia in healthy adults caused by methicillin‐resistant Staphylococcus aureus carrying the Panton‐Valentine leukocidin genes.Clin Infect Dis.2005;40(1):100–107.
- ,,,.Fatal community‐associated methicillin‐resistant Staphylococcus aureus pneumonia in an immunocompetent young adult.Ann Emerg Med.2005;46:401–404.
- .Aspiration pneumonitis and aspiration pneumonia.N Engl J Med.2001;344:665–671.
- ,,, et al.Health care‐associated bloodstream infections in adults: a reason to change the accepted definition of community‐acquired infections.Ann Intern Med.2002;137:791–797.
- American Thoracic Society and theInfectious Diseases Society of America.Guidelines for the management of adults with hospital‐acquired, ventilator‐acquired, and healthcare‐associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Blood culture and susceptibility results and allergy history do not influence fluoroquinolone use in the treatment of community‐acquired pneumonia.Pharmacotherapy.2005;25(1):59–66.
- ,,, et al.Time to clinical stability in patients hospitalized with community‐acquired pneumonia: implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,, et al.Causes and factors associated with early failure in hospitalized patients with community‐acquired pneumonia.Arch Intern Med.2004;164:502–508.
- ,,, et al.Instability on hospital discharge and the risk of adverse outcomes in patients with pneumonia.Arch Intern Med.2002;162:1278–1284.
- ,,,.Radiographic resolution of community‐acquired bacterial pneumonia in the elderly.J Am Geriatr Soc.2004;52(2):224–229.
- ,,,.Vaccines for preventing pneumococcal infection in adults.Cochrane Database Syst Rev.2003;4:CD000422.
- ,,,,.The efficacy of influenza vaccine in elderly persons: a meta‐analysis and review of the literature.Ann Intern Med.1995;123:518–527.
- ,,, et al.Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly.N Engl J Med.2003;348:1322–1332.
- ,,,.Proportion of community‐acquired pneumonia cases attributable to tobacco smoking.Chest.1999;116:375–379.
- ,,, et al.Risk of community‐acquired pneumonia and use of gastric acid‐suppressive drugs.JAMA.2004;292:1955–1960.
Pneumonia may well be called the friend of the aged. Taken off by it in an acute, short, not often painful illness, the old man escapes those cold gradations of decay so distressing of himself and to his friends.
William Osler, MD, 1898
Community‐acquired pneumonia (CAP) is commonly defined as an infection of the pulmonary parenchyma that is associated with at least some symptoms and signs of acute infection, accompanied by the presence of an acute infiltrate on chest radiograph, in a patient not hospitalized or residing in a long‐term‐care facility for 14 days prior to the onset of symptoms.1 CAP continues to be a common and serious illness, causing substantial morbidity and mortality in the adult population. There are an estimated 56 million cases a year in the United States, with greater than 1 million hospitalizations. Community‐acquired pneumonia is one of the most common admitting diagnoses among adults, and with a 30‐day mortality between 10% and 14% for patients admitted to the hospital, it is the leading cause of infectious death in the United States.2 In elderly patients, hospitalization for CAP portends a poor long‐term prognosis. In a Medicare database, the 1‐year mortality for patients with CAP was nearly 40%, compared to 29% in patients with other diagnoses.3 Community‐acquired pneumonia is a model illness in hospital medicineit is a common disease that allows for evidence‐based and cost‐effective management. In addition, many national organizations have proposed multiple quality indicators for community‐acquired pneumonia, thus providing an opportunity for institutional quality improvement. This review article outlines the assessment and management of patients admitted to the hospital with community‐acquired pneumonia.
Etiology
Although many pathogens can cause community‐acquired pneumonia, the clinical syndromes and microbiology of CAP have traditionally been characterized as either typical or atypical. The typical organisms include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, and the atypical organisms include Chlamydia spp., Mycoplasma pneumoniae, Legionella spp., and viruses. This historical distinction has recently come into question. It is now clear that the presenting symptoms, signs, and basic laboratory findings (including the chest radiograph) cannot be reliably used to predict the etiologic pathogen or to distinguish typical from atypical organisms.4 Rather, the specific causative agent of CAP depends more on the degree of patient illness. Table 1 shows what prospective studies with comprehensive diagnostic strategies determined to be the most common pathogens in patients hospitalized for CAP in ICU and non‐ICU settings.5 Streptococcus pneumoniae remains the most common cause of CAP in hospitalized patients and is the most common cause of fatal pneumonia, whereas Legionella spp. is a common cause of severe CAP, more often found in patients requiring admission to the intensive care unit. Gram‐negative bacilli can cause CAP in elderly patients and those recently treated with broad‐spectrum antibiotics or with underlying lung disease. Notably, though, despite improved diagnostic testing, only one quarter of all admitted patients with CAP have the etiologic agent defined, and therefore empiric therapy should be directed broadly at the most likely organisms.6
| Non‐ICU inpatients | ICU inpatients (severe) |
|---|---|
| S. pneumoniae | S. pneumoniae |
| M. pneumoniae | Legionella spp |
| C. pneumoniae | H. influenzae |
| H. influenzae | Gram‐negative bacilli |
| Legionella spp | S. aureus |
| Aspiration | |
| Respiratory viruses |
Clinical Presentation
Patients admitted to the hospital with CAP typically present with a brief history of respiratory complaints, including cough (greater than 90%), dyspnea (66%), sputum production (66%), and pleuritic chest pain (50%); see Table 2.7, 8 In 10%30% of patients, nonrespiratory complaints predominate, including headache, myalgias, fatigue, and gastrointestinal symptoms.6 Elderly patients, an increasing percentage of hospitalized patients, are less likely to present with typical CAP symptoms (such as cough) and more likely to have altered mental status as a presenting symptom.9
| Symptoms | Signs (exam) |
|---|---|
| Cough 90% | Fever 80% |
| Dyspnea 66% | Tachypnea 70% |
| Sputum 66% | Tachycardia 50% |
| Pleuritic chest pain 50% | Focal lung exam >90% |
On physical examination, patients with CAP usually have signs of fever (80%), tachypnea (70%), and tachycardia (50%); see Table 2. Most will have a focal lung exam (>90%) with findings ranging from crackles to bronchial breath sounds.10 No exam finding is specific for the diagnosis of pneumonia, but the absence of fever, tachycardia, and tachypnea significantly reduces the probability of CAP in patients with suspected pneumonia.10 Furthermore, similar to the clinical history, the physical examination of elderly patients with community‐acquired pneumonia is not specific or sensitive for the diagnosis of CAP. For example, up to 40% of elderly patients subsequently determined to have CAP may not have fever.11
Leukocytosis is common in patients with CAP; however, its absence does not rule out disease.12 A number of guidelines recommend laboratory evaluation of electrolytes, urea nitrogen, creatinine, liver enzymes, and bilirubin, although these are used primarily for prognostication and are not specifically useful in the diagnosis of CAP.
DIAGNOSIS
Differential Diagnosis
Given the nonspecific nature of the symptoms and signs associated with CAP, there is no single clinical feature or combination of clinical features that adequately rules in or out the diagnosis of CAP. Consequently, the differential diagnosis to be considered in patients with suspected CAP is broad. Noninfectious diseases can often present with similar clinical syndromes; these include congestive heart failure, exacerbation of chronic obstructive pulmonary disease (COPD), asthma, pulmonary embolism, and hypersensitivity pneumonitis. These diseases can often be distinguished with a thorough history and physical examination.
In addition, other upper‐ and lower‐airway infectious diseases can have similar nonspecific signs and symptoms. In particular, pneumonia must often be differentiated from acute bronchitis, which as a diagnosis accounts for up to 40% of patients evaluated for cough (versus 5% for pneumonia).10 Patients with acute bronchitis frequently do not present with high fevers or hypoxia and in general will not benefit from antibiotic therapy.13 Patients believed to have community‐acquired pneumonia might also be suffering from other pneumonia syndromes including aspiration pneumonia, postobstructive pneumonia, and pneumonia in immunocompromised patients (eg, those with HIV, on steroids, receiving chemotherapy). Determining the correct diagnosis can have implications for therapy and prognosis.
Diagnostic Studies
The diagnosis of community‐acquired pneumonia requires that a patient have both signs and symptoms consistent with pulmonary infection and evidence of a new radiographic infiltrate. Therefore, most guidelines recommend that all patients with a possible diagnosis of CAP be evaluated with chest radiography.1, 14, 15
The specific radiographic findings in community‐acquired pneumonia range from lobar consolidation to hazy focal infiltrate to diffuse bilateral interstitial opacities (see Figure 1). Although chest radiography has traditionally been considered the gold standard for the diagnosis of CAP, its exact performance characteristics are unknown, and it is clearly not 100% sensitive or 100% specific. The utility of the chest radiograph can be limited by patient body habitus, underlying lung disease, or dehydration. Computed tomography (CT) scanning, although not recommended for routine use, can identify pulmonary consolidation in up to 30% of patients with a normal or equivocal chest radiograph in whom pneumonia is suspected and can also identify complications of pneumonia including an empyema or pulmonary abscess.16

Limitations in the performance of the chest radiograph have resulted in an interest in the diagnostic performance of serologic markers of infection such as C‐reactive protein (CRP), procalcitonin, and soluble triggering receptor expressed on myeloid cells (s‐TREM).1719 Preliminary evidence suggests these inflammatory markers may ultimately prove useful in differentiating infectious from noninfectious pulmonary processes, but regular use of these new tests cannot currently be recommended.
Most expert guidelines state that 2 sets of blood cultures should be taken and analyzed prior to antibiotic administration in all patients admitted to the hospital with suspected community‐acquired pneumonia.1, 14, 15 Isolation of bacteria from blood cultures in CAP is a very specific way to identify a causative organism in order to subsequently narrow therapy and also identifies a high‐risk group of patients because bacteremia is associated with increased mortality. Obtaining blood cultures within 24 hours of admission has been associated with 10% lower odds of 30‐day mortality in patients with CAP,20 and as a result, drawing blood cultures prior to antibiotic administration is a national quality indicator for CAP.
There are, however, a number of problems with the routine acquisition of blood cultures in all patients admitted with CAP. Practically, the cultures can be difficult to obtain, can potentially delay the initiation of antibiotics, and are often contaminated, which has been shown to increase both cost and length of stay.21, 22 The yield is generally low: the true‐positive bacteremia rate for admitted patients with CAP ranges from 6% to 9%, and the culture results rarely change management or outcomes.23, 24 Given these limitations, many have argued that blood cultures should be obtained with a more targeted approach. A recent study used a Medicare database to create a decision‐support tool to help maximize the value of blood cultures in CAP.25 The predictors of a positive blood culture are shown in Table 3. Not obtaining cultures on patients who had received prior antibiotics or had no risk factors resulted in about 40% fewer overall cultures while identifying approximately 90% of bacteremias. In their guidelines, the British Thoracic Society (BTS) advocates a similar strategy, recommending blood cultures be omitted in nonsevere pneumonia and in patients without comorbidities.15, 26 Although recommendations vary for non‐severe CAP in hospitalized patients, all professional society guidelines agree that blood cultures should be obtained in critically ill patients, and if cultures are obtained, they should be drawn prior to antibiotics.1, 14, 15, 26
| Comorbidities |
| Liver disease |
| Vital signs |
| Systolic blood pressure < 90 mm Hg |
| Temperature < 35C or 40C |
| Pulse 125 beats/min |
| Laboratory and radiographic data |
| Blood urea nitrogen (BUN) 30 mg/dL |
| Sodium < 130 mmol/L |
| White blood cells < 5000/mm3 or > 20,000/mm3 |
| Prior use of antibiotics (negative predictor) |
Substantial controversy surrounds the utility of routine sputum gram stains and cultures for patients admitted to the hospital with CAP. The Infectious Disease Society of America (IDSA) and the British Thoracic Society (BTS) both recommend that all patients admitted to the hospital with community‐acquired pneumonia should have a gram stain and culture of expectorated sputum.1, 15, 26 Both organizations argue sputum collection is a simple and inexpensive procedure that can potentially identify pathogenic organisms and can affect both initial and long‐term antibiotic therapy. Most notably, they highlight gram stain specificity of greater than 80% for pneumococcal pneumonia. Conversely, the American Thoracic Society (ATS) argues that sputum gram stains and cultures generally have low sensitivity, specificity, and positive predictive value.14 Furthermore, they argue the utility of sputum testing is also limited practically; in one study 30% of patients could not produce an adequate sputum specimen and up to 30% had received prior antibiotic therapy, substantially reducing the yield.27 In another study, good‐quality sputum with a predominant morphotype could be obtained in only 14% of patients admitted with CAP.28 However, targeting sputum analysis to patients who have not received prior antibiotics and are able to produce an adequate sample improved the yield significantly.29 In addition, with increasing rates of antibiotic resistance among common community isolates (ie, S. Pneumoniae) and the increasing prevalence of infecting organisms not targeted by routine empiric therapy (methicillin‐resistant Staphylococcus Aureus [MRSA]), isolation of potential causative pathogens is increasingly important. We believe that severely ill patients with CAP (such as patients admitted to the ICU), as well as patients with identifiable risk factors for uncommon or drug‐resistant pathogens (eg, Pseudomonas aeruginosa, enteric gram‐negative rods, MRSA, etc.) should have sputum sent for gram stain and culture. Ideally, sputum obtained for gram stain and culture should be:
-
Prior to antibiotic therapy,
-
A deep‐cough, expectorated specimen,
-
A purulent specimen (>25 polymorphonucleacytes and less than 10 squamous cells per high‐powered field), and
-
Rapidly transported to the laboratory.
Subsequent gram stain and culture results should be interpreted in the specific clinical context and antibiotic choices targeted appropriately.
Alternative Diagnostic Tests
In recent years, there has been growth in additional diagnostic tests targeting specific organisms. The pneumococcal urinary antigen assay is a relatively sensitive (50%80%) and highly specific (90%) test for the detection of pneumococcal pneumonia, when compared with conventional diagnostic methods.27 The test is simple, convenient, rapid ( 15 min), and, with its high specificity, may allow for more focused antimicrobial therapy early in management. Current limitations include the possibility of false‐positive tests in patients colonized with S. pneumoniae or infected with other streptococcal species, as well as the inability to determine antibiotic sensitivity from positive tests. Updated IDSA and BTS guidelines state pneumococcal urinary antigen testing is an acceptable adjunct to other diagnostic tests, but blood and sputum analyses should still be performed.26, 27 For patients with suspected Legionella pneumonia (primarily critically ill and immunocompromised patients or in association with regional outbreaks), the urinary Legionella antigen assay is the test of choice, which detects 80%95% of community‐acquired cases of Legionnaires' disease with a specificity of 90%.27
During the winter months (typically from October to March), rapid antigen testing for influenza is generally recommended for patients with signs or symptoms consistent with influenza.27 The sensitivity of these tests is approximately 50%70%, so negative test results do not exclude the diagnosis, but results can be important epidemiologically and therapeutically (differentiating influenza A and B strains).27 Diagnostic tests targeting other common CAP pathogens, such as serologic tests for Mycoplasma pneumoniae or Chlamydia spp, should not be routinely performed. Testing for less common causative pathogens such as Mycobacterium tuberculosis should only be employed in the appropriate clinical setting.
ADMISSION DECISION
Once the diagnosis of CAP has been made, the initial site where treatment will occur, whether the hospital or the home, must be determined. The decision to hospitalize should be based on 3 factors: 1) evaluation of the safety of home treatment, 2) calculation of the Pneumonia Severity Index (PSI), and 3) clinical judgment of the physician.27 The PSI, or PORT (Pneumonia Outcomes Research Team) score, is a validated prediction rule that quantifies mortality and allows for risk stratification of patients with community‐acquired pneumonia.2 The PSI combines clinical history, physical examination, and laboratory data at the time of admission to divide patients into 5 risk classes and to estimate 30‐day mortality (Figure 2), which ranges from 0.1% of patients in risk class I to 27.0% in risk class V.2
On the basis of the estimated prognosis and in the absence of concerns about home safety or comorbidities, patients in risk classes I, II, and III should be managed at home. Many prospective trials have shown that implementation of PSI significantly increases the number of low‐risk patients managed outside the hospital, with no differences in quality of life, complications, readmissions, or short‐term mortality.30, 31 Most recently, a trial randomizing patients in risk classes II and III to treatment in the hospital or at home found no significant differences in clinical outcomes but did find that patients were more satisfied with care at home.32 Because the number of patients with CAP being treated at home is increasing, the American College of Chest Physicians recently published a consensus statement on the management of community‐acquired pneumonia in the home.33 All national guidelines for the management of community‐acquired pneumonia recommend using the PSI to help determine the initial location of treatment, with the caveat that using the prediction rule should never supersede clinical judgment in the decision about whether to admit.1, 14, 15, 26, 27 A practical decision tree for the use of the PSI is shown in Figure 3.
There are no reliable prediction rules for deciding on whether admission to the intensive care unit is necessary. Hemodynamic instability requiring resuscitation and monitoring or respiratory failure requiring ventilatory support are clear indications for ICU admission. Additional variables such as tachypnea (respiratory rate 30), altered mental status, multilobar disease, and azotemia are associated with severe CAP and should prompt consideration of ICU admission, especially when 2 or more variables coexist.14
TREATMENT
Initial Treatment
Once the admission decision is made and the initial diagnostic tests are completed (including blood and sputum cultures), patients with presumed community‐acquired pneumonia should receive necessary supportive care (O2, intravenous fluids, etc.) and prompt antimicrobial therapy. Antibiotics should be administered within 4 hours of arrival to patients with suspected CAP, as such prompt administration may be associated with shorter in‐hospital stays and decreased 30‐day mortality.34, 35 Regulatory organizations such as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the Center for Medicare Services (CMS) have made delivery of antibiotics in less than 4 hours a hospital quality measure.
Despite diagnostic testing, the specific etiologic agent causing the pneumonia of a patient remains unknown in up to 75% of those admitted to the hospital.14 Most expert guidelines therefore recommend broad‐spectrum empiric therapy targeting both the typical and the atypical organisms that commonly cause CAP (Table 1).
Recommendations for empiric antibiotics are driven by 2 key factors: antibiotic resistance by S. pneumoniae and the results of studies of CAP treatment outcomes. Historically, patients with suspected community‐acquired pneumonia were treated with penicillin with generally good outcomes. Recently, the rate of S. pneumoniae isolates resistant to penicillin has risen dramatically in the United States, ranging between 20% and 30%, with high‐level resistance (MIC 4 mg/L) as high as 5.7%.36, 37 Concurrently, the rates of resistance of S. pneumoniae to many other antibiotics commonly used to treat CAP have also risen.37 Despite increasing resistance overall, most U.S. pneumococcal isolates have low resistance to third‐generation cephalosporins and fluoroquinolones with enhanced activity against S. pneumoniae.3638 In addition, despite increasing resistance by pneumococcal isolates to penicillin, several observational studies have shown that regardless of initial therapy, resistance to penicillin as well as third‐generation cephalosporins is not associated with higher mortality or worse outcomes when controlled for other risk factors for drug resistance.39, 40 An exception to that rule is pneumococcal isolates that are very highly resistant to PCN (MIC 4 mg/dL). At least one study has shown that patients with such isolates may be at higher risk for adverse outcomes and should probably not be treated with penicillins.1, 14, 15, 41 However, nationally, fewer than 6% of pneumococcal isolates have this level of resistance.37
The rationale for empiric broad‐spectrum coverage against both typical and atypical organisms has arisen from many retrospective and observational studies that have suggested that there is clinical benefit and improved outcomes with such regimens. One large retrospective study showed that in elderly patients with CAP, fluoroquinolone monotherapy was associated with lower 30‐day mortality when compared to monotherapy with a third‐generation cephalosporin.34 Adding an extended‐spectrum macrolide (eg, azithromycin) to an extended‐spectrum ‐lactam (eg, ceftriaxone) in the treatment of patients hospitalized with nonsevere CAP also appears to be associated with improved outcomes. Adding a macrolide has resulted in shorter lengths of stay (LOS), less treatment failure, and lower mortality.34, 4244 Similarly, according to unpublished observations, adding doxycycline to a ‐lactam as initial therapy was associated with a benefit of decreased mortality.45 The presumed etiology of the benefit has been the addition of specific coverage of atypical organisms, such as Mycoplasma pneumoniae and Chlamydia pneumoniae, which are common causes of CAP (Table 1). Others have proposed that the benefit of therapy with macrolides may be derived from the inherent anti‐inflammatory properties of macrolides.46 Because research has shown a benefit of dual versus monotherapy across a spectrum of antibiotics, others have proposed the benefit is simply a result of receiving double antibiotic coverage. In particular, 2 studies found a benefit of reduced mortality from combination therapy over monotherapy in bacteremic pneumococcal pneumonia.47, 48
Yet the accumulated evidence for adding coverage of atypical organisms has been only retrospective and observational. Because of this, the recommendation to routinely add antibiotics active against atypical organisms has been questioned by some. Two recent meta‐analyses and a systematic review examined all the available data on the need for atypical coverage in the treatment of patients with community‐acquired pneumonia.4951 Surprisingly, none showed a benefit in clinical efficacy or survival in patients treated with agents active against both atypical and typical organisms when compared to regimens with only typical coverage. In subset analyses, there was a benefit to providing empiric atypical coverage in patients subsequently shown to have Legionella spp. as a causative pathogen. However, this organism was uncommon in all 3 studies. Unfortunately, most studies included in the meta‐analyses compared fluoroquinolone or macrolide monotherapy with third‐generation cephalosporin monotherapy. There have been no high‐quality randomized, controlled trials of the treatment of hospitalized patients with CAP assessing combination therapy covering both typical and atypical organisms with monotherapy targeting typical organisms alone. High‐quality trials are warranted.
Despite the recent articles questioning the importance of atypical coverage, citing the substantial retrospective data and the general inability to identify causative organisms in most cases of CAP, adding a second agent with atypical coverage to a ‐lactam currently appears to be the most efficacious empiric treatment for CAP. Nearly all expert guidelines for the management of community‐acquired pneumonia recommend this empiric approach.1, 14, 27
Table 4 displays our recommendations for the treatment of community‐acquired pneumonia requiring hospitalization. Before implementation of these guidelines, hospitalists should consult with their infectious disease experts and consider local resistance patterns. In general, a typical adult patient with non‐severe CAP without additional risk factors should receive a parenteral extended‐spectrum ‐lactam plus either doxycycline or an advanced macrolide (see Table 4). Extended‐spectrum ‐lactams include cefotaxime, ceftriaxone, ampicillin‐sulbactam, and ertapenem. A respiratory fluoroquinolone as a single agent can be used for non‐ICU patients with CAP, but some agencies, including the Centers for Disease Control (CDC), discourage routine use of these agents in all patients secondary to concerns about cost and increasing gram‐negative rod fluoroquinolone resistance.52, 53
| Patient group | Empiric antibiotic therapy |
|---|---|
| |
| Inpatient, non‐ICU | ‐Lactama + either doxycycline or an advanced macrolideb |
| Severe ‐lactam allergyc | Respiratory fluoroquinoloned |
| Inpatient, ICU | |
| No risk for Pseudomonas | ‐Lactam + either an advanced macrolide or a respiratory fluoroquinolone |
| Severe ‐lactam allergy | Respiratory fluoroquinolone + clindamycin |
| Pseudomonas risk factorse | Antipseudomonal ‐lactamf + an antipseudomonal fluoroquinoloneg |
| Severe ‐lactam allergy | Aztreonam + a respiratory fluoroquinolone |
| MRSA risk factorsh | Add vancomycin to above regimens |
| From nursing home | Should be treated as nosocomial/health‐care‐associated pneumonia |
| Aspiration pneumonia | ‐Lactam or respiratory fluoroquinolone clindamycini |
Patients hospitalized with severe CAP who require ICU‐level care are at increased risk of Legionella spp. and drug‐resistant S. pneumoniae, which must be reflected in their initial antibiotic therapy.5 Patients with severe pneumonia should receive an intravenous extended‐spectrum ‐lactam plus either an intravenous macrolide or an intravenous respiratory fluoroquinolone.
All patients with severe CAP who are admitted to the intensive care unit should be routinely screened for risk factors for Pseudomonas aeruginosa. The known risk factors for pseudomonal infection are: bronchiectasis, immunosuppression including more than 10 mg/day of prednisone, malnutrition, and treatment with broad‐spectrum antibiotics in the last month.14 Those at risk for Pseudomonas aeruginosa or other resistant gram‐negative rod infection should be treated with an antipseudomonal ‐lactam plus an antipseudomonal fluoroquinolone. Many patients with severe CAP have risk factors for MRSA infection including recent prolonged hospitalization, recent use of broad‐spectrum antibiotics, and significant underlying lung disease, which should be considered in choosing initial antibiotic therapy.54 In addition, there have been reports of patients without underlying risk factors presenting with severe community‐acquired MRSA pneumonia. Many of these patients were younger and the MRSA pneumonia was associated with a necrotizing or cavitary disease requiring prolonged ICU stays.5558 In such cases or if an institution's rate of methicillin resistance in S. aureus community isolates is high (>15%20%), it may be appropriate to add initial empiric MRSA coverage for patients admitted to the ICU with CAP.55
Some patients will have unique risk factors and clinical presentations, which may require modification of these empiric recommendations. Several studies found 5%15% of cases of community‐acquired pneumonia to be aspiration pneumonia.57 Risk factors for aspiration events include, among others, dysphagia, history of stroke, altered level of consciousness, poor dentition, and tube feeding. Aspiration pneumonia traditionally was believed to be secondary to oral anaerobes, but recent research suggests gram‐positive cocci and gram‐negative rods are the predominant organisms.58 Antibiotic therapy in patients with clear aspiration pneumonia should be directed at these microbes with an extended‐spectrum ‐lactam (eg, ceftriaxone) or a respiratory fluoroquinolone (eg, levofloxacin or moxifloxacin). Anaerobic bacterial coverage can be added in patients with severe periodontal disease, alcoholism, concern for empyema, or evidence of aspiration with pulmonary abscess.58
Patients residing in long‐term care facilities are at high risk of contracting pneumonia. The microbiology of infections acquired in nursing facilities is similar to that in hospital‐acquired cases.59, 60 As a result, patients who develop pneumonia in institutional settings such as nursing homes should be treated with broad‐spectrum antibiotics, including coverage for MRSA.
Subsequent Treatment
Initial empiric antibiotic treatment should be modified based on the results of diagnostic testing. Although the specific etiologic agent is determined in only 25% of cases of CAP,35 when an organism is isolated, antibiotic coverage should be narrowed to cover that particular organism with an antibiotic with adequate lung penetration. Evidence suggests clinicians often do not adjust or narrow antibiotics based on sensitivity results, potentially breeding resistant organisms.61
Patients hospitalized with CAP usually improve quickly if they receive early, appropriate antibiotic therapy and supportive care. Excluding patients with severe CAP requiring intensive care unit admission, most patients resolve their tachycardia, tachypnea, and fever by day 2 or 3.62 Recent practice experience, evidence, and published guidelines14, 27 all indicate that patients can safely be transitioned to oral antibiotic therapy earlier in their hospital course. Table 5 outlines criteria that can be used to identify patients who have had an adequate response to parenteral therapy and can be considered for a switch to oral antibiotics. If these criteria are met, patients have less than a 1% chance of clinical deterioration necessitating admission to an ICU or transitional care unit.62 When an etiologic organism is not identified, oral therapy should reflect a spectrum of coverage to that of the initial intravenous therapy. In some cases, this may require use of more than one oral agent. We have had success, however, transitioning non‐ICU patients initially treated with intravenous ceftriaxone plus oral doxycycline, typically for 4872 hours, to oral doxycycline monotherapy at discharge.45
| Stable vital signs and clinical criteria for 24 hours |
| Temperature 37.8C (100F) |
| Heart rate 100 beats per minute |
| Respiratory rate 24 breaths per minute |
| Systolic blood pressure 90 mm Hg |
| Oxygen saturation (on room air) 90% |
| Ability to take oral medications |
There have been a limited number of high‐quality randomized trials examining the optimal duration of treatment for community‐acquired pneumonia. Most practice guidelines recommend 710 days for patients with CAP requiring hospitalization, with 14 days for documented Mycoplasma pneumoniae or Chlamydia pneumoniae. One recent randomized trial of patients with mild to severe CAP showed a short course of high‐dose levofloxacin (750 mg daily 5 days) was at least as effective as normal dosing (500 mg daily 10 days).63 Clinical experience with high‐dose levofloxacin is limited, but this regimen can be considered because it may reduce costs and exposure to antibiotics. When diagnosed, Legionella is usually treated for 1021 days, but 14 days is adequate with macrolides because of their long half‐life.27 Patients with more virulent pathogens like Staphylococcus aureus or Pseudomonas aeruginosa or other suppurative complications should be treated for at least 14 days.1, 14, 15, 27 In determining length of therapy, clinicians should use these durations of treatment as guides, and to individualize therapy, they should always consider patient age and frailty, comorbid conditions, severity of illness, and hospital course.
Failure to Respond
Although most patients hospitalized for CAP will improve rapidly and reach clinical stability in 23 days, some patients fail to respond. Some studies have estimated that failure to improve or clinical deterioration occurs in 5%10% of patients in the first 23 days.64 The common reasons for clinical decline or nonresponse to treatment, highlighted in Table 6, are:
-
Incorrect diagnosis: Illnesses such as congestive heart failure, pulmonary embolism, neoplasms, and hypersensitivity pneumonitis can mimick CAP.
-
Inadequate antibiotic selection: The etiologic agent may be resistant to empiric antibiotic selections. Examples would include methicillin‐resistant Staphylococcus aureus (MRSA) or multiresistant gram‐negative bacilli.
-
Unusual pathogen: CAP syndromes can be caused by myriad unusual organisms including Pneumocystis jirovecii, mycobacterium tuberculosis, endemic fungal infections (eg, coccidioidomycosis), and nocardiosis.
-
Complications of pneumonia: Specific complications of CAP include empyema, pulmonary abscess, extrapulmonary spread including meningitis or endocarditis, or other organ dysfunctions such as renal failure or myocardial infarction.
-
Inadequate host response: Despite appropriate antibiotic and supportive therapy, patients with CAP often fail to respond.
| Incorrect diagnosis of CAP. |
| Inadequate or inappropriate antibiotic selection for CAP. |
| Unusual pathogen causing CAP. |
| Pulmonary or extrapulmonary complication of CAP. |
| Inadequate or poor host response. |
Progressive pneumonia despite appropriate therapy and empyema were the most common causes of failure to respond in the first 72 hours in a recent study.64 Risk factors for early failure were older age (>65 years), Pneumonia Severity Index > 90, Legionella pneumonia, gram‐negative pneumonia, and initial antimicrobial therapy discordant with final culture and susceptibility results. The initial evaluation of the nonresponding patient should address these common causes and is likely to include additional imaging (CT), sampling of potential extrapulmonary infection (thoracentesis), and, in some cases, bronchoscopy.
DISCHARGE/FOLLOW‐UP PLANS
Patients hospitalized for community‐acquired pneumonia can be safely discharged when they have reached clinical stability, are able to tolerate oral medications, have no other active comorbid conditions, and have safe, close, appropriate outpatient follow‐up (see Table 7). Clinical pathways employing these discharge criteria have been found to be safe and effective in reducing the length of stay for CAP. Most important, patients should have met most if not all of the vital sign and clinical criteria noted in Table 5 in the criteria for switching to oral therapy. Patients with 2 or more abnormal vital signs (instabilities) within 24 hours prior to discharge are at high risk of readmission and mortality, but those with one or no abnormal vital signs generally have good outcomes.65 Absent other clinical factors or extenuating circumstances (persistent hypoxia, poor functional status, etc.), most patients with CAP should reach clinical stability by day 3 or 4, be considered for a switch to oral therapy, and, if stable, be discharged shortly thereafter.
| Patients should: |
|
Meet clinical criteria in Table V. |
| Be able to tolerate oral medications (no need to observe for 24 hours on oral therapy). |
| Have no evidence of active comorbid conditions (myocardial ischemia, pulmonary edema, etc.). |
| Have a normal mental status (or have returned to their baseline). |
| Have safe, appropriate outpatient follow‐up. |
When patients with CAP are discharged from the hospital, they should be counseled about the expected course of recovery. Most important, patients and families must be informed that many symptoms of CAP may persist well after hospitalization. In one study, up to 80% of patients reported persistent cough and fatigue 1 week after discharge, and up to 50% still had dyspnea and sputum production. In some, the cough can last for 46 weeks.8
All patients discharged after treatment of community‐acquired pneumonia should have follow‐up with their outpatient provider. The physician responsible for their inpatient care should communicate directly with the provider and outline the hospital course, the discharge medications, and the duration of antibiotic therapy. There is no specific time frame within which patients must be seen, but follow‐up should be dictated by patient age, comorbidities, clinical stability at discharge, and degree of illness. The American Thoracic Society guidelines do recommend patients with a substantial smoking history who are hospitalized with CAP have a follow‐up chest radiograph 46 weeks after discharge to establish a radiographic baseline and exclude the possibility of underlying malignancy.14 However, several studies have suggested that radiographic resolution may take 3 or more months in some patients, especially the elderly and those with multilobar disease.66
PREVENTION
Prevention of community‐acquired pneumonia and pneumonic syndromes has traditionally relied on vaccination with the polysaccharide pneumococcal pneumonia vaccine and the seasonal influenza vaccine. The vaccine for S. pneumoniae used in adults is composed of the 23 serotypes that cause 85%90% of the invasive pneumococcal infections in the United States. Although in randomized trials the vaccine has not consistently prevented community‐acquired pneumonia or death in elderly patients or those with comorbidities, it likely prevents invasive pneumococcal infection.67 National guidelines and the CDC recommend the pneumococcal vaccine be given to all patients older than 65 years and those with chronic medical conditions.1, 14, 15
The seasonal influenza vaccine has clearly been shown to decrease influenza‐related illness in elderly and high‐risk patient populations. As well, in a meta‐analysis and a large observational study of patients older than 65 years, vaccination against influenza prevented pneumonia, hospitalization, and death.68, 69 Vaccination of health care workers may also confer a benefit to elderly patients of reduced mortality. The CDC recommends the influenza vaccine for all patients more than 50 years old, those with comorbidities, those at high risk for influenza, and health care workers in both inpatient and outpatient settings.
Pneumococcal and influenza vaccination have traditionally been relegated to the outpatient setting. National guidelines and the CDC recommend vaccination of all eligible hospitalized patients. Vaccination is safe and effective with almost any medical illness, and both vaccines can be given simultaneously at discharge.69 Both JCAHO and CMS have defined administration of the pneumococcal and influenza vaccines to patients hospitalized with CAP as a quality measure. Using standing orders is the most effective means of ensuring vaccination.
Some evidence suggests that tobacco smokers are at increased risk of invasive pneumococcal disease or pneumonia.70 Patients hospitalized (for all illnesses, but for CAP in particular) should be counseled about smoking cessation and offered pharmacotherapy and outpatient follow‐up. And, finally, recent observational data suggests that use of acid suppressive therapy, including proton pump inhibitors and H‐2 receptor antagonists, may be associated with an increased risk of developing CAP.71 Patients using these agents who are admitted with CAP should have their indications for treatment reviewed, especially when the pneumonia has been recurrent and there is no clear indication for continued use of acid suppressive therapy, in which case they should be discontinued in the hospital.
CONCLUSIONS
Community‐acquired pneumonia remains a common cause for hospitalization of adult patients, with significant associated morbidity and mortality. Although there are multiple expert guidelines for the management of community‐acquired pneumonia, further research is urgently needed. Clinicians need improved diagnostic tests that enable an earlier and more accurate diagnosis of CAP. In addition, the etiologic agent causing CAP is rarely discovered; improved microbiologic studies might enable antibiotic therapy to be targeted to the organisms responsible. High‐quality randomized, controlled trials examining empiric antibiotic therapy in CAP are needed, especially related to the addition of agents covering atypical organisms. Last, the general management of patients hospitalized with CAP is marked by significant heterogeneity, and research and initiatives focusing on improving the quality and process of care of patients with CAP are needed.
Pneumonia may well be called the friend of the aged. Taken off by it in an acute, short, not often painful illness, the old man escapes those cold gradations of decay so distressing of himself and to his friends.
William Osler, MD, 1898
Community‐acquired pneumonia (CAP) is commonly defined as an infection of the pulmonary parenchyma that is associated with at least some symptoms and signs of acute infection, accompanied by the presence of an acute infiltrate on chest radiograph, in a patient not hospitalized or residing in a long‐term‐care facility for 14 days prior to the onset of symptoms.1 CAP continues to be a common and serious illness, causing substantial morbidity and mortality in the adult population. There are an estimated 56 million cases a year in the United States, with greater than 1 million hospitalizations. Community‐acquired pneumonia is one of the most common admitting diagnoses among adults, and with a 30‐day mortality between 10% and 14% for patients admitted to the hospital, it is the leading cause of infectious death in the United States.2 In elderly patients, hospitalization for CAP portends a poor long‐term prognosis. In a Medicare database, the 1‐year mortality for patients with CAP was nearly 40%, compared to 29% in patients with other diagnoses.3 Community‐acquired pneumonia is a model illness in hospital medicineit is a common disease that allows for evidence‐based and cost‐effective management. In addition, many national organizations have proposed multiple quality indicators for community‐acquired pneumonia, thus providing an opportunity for institutional quality improvement. This review article outlines the assessment and management of patients admitted to the hospital with community‐acquired pneumonia.
Etiology
Although many pathogens can cause community‐acquired pneumonia, the clinical syndromes and microbiology of CAP have traditionally been characterized as either typical or atypical. The typical organisms include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, and the atypical organisms include Chlamydia spp., Mycoplasma pneumoniae, Legionella spp., and viruses. This historical distinction has recently come into question. It is now clear that the presenting symptoms, signs, and basic laboratory findings (including the chest radiograph) cannot be reliably used to predict the etiologic pathogen or to distinguish typical from atypical organisms.4 Rather, the specific causative agent of CAP depends more on the degree of patient illness. Table 1 shows what prospective studies with comprehensive diagnostic strategies determined to be the most common pathogens in patients hospitalized for CAP in ICU and non‐ICU settings.5 Streptococcus pneumoniae remains the most common cause of CAP in hospitalized patients and is the most common cause of fatal pneumonia, whereas Legionella spp. is a common cause of severe CAP, more often found in patients requiring admission to the intensive care unit. Gram‐negative bacilli can cause CAP in elderly patients and those recently treated with broad‐spectrum antibiotics or with underlying lung disease. Notably, though, despite improved diagnostic testing, only one quarter of all admitted patients with CAP have the etiologic agent defined, and therefore empiric therapy should be directed broadly at the most likely organisms.6
| Non‐ICU inpatients | ICU inpatients (severe) |
|---|---|
| S. pneumoniae | S. pneumoniae |
| M. pneumoniae | Legionella spp |
| C. pneumoniae | H. influenzae |
| H. influenzae | Gram‐negative bacilli |
| Legionella spp | S. aureus |
| Aspiration | |
| Respiratory viruses |
Clinical Presentation
Patients admitted to the hospital with CAP typically present with a brief history of respiratory complaints, including cough (greater than 90%), dyspnea (66%), sputum production (66%), and pleuritic chest pain (50%); see Table 2.7, 8 In 10%30% of patients, nonrespiratory complaints predominate, including headache, myalgias, fatigue, and gastrointestinal symptoms.6 Elderly patients, an increasing percentage of hospitalized patients, are less likely to present with typical CAP symptoms (such as cough) and more likely to have altered mental status as a presenting symptom.9
| Symptoms | Signs (exam) |
|---|---|
| Cough 90% | Fever 80% |
| Dyspnea 66% | Tachypnea 70% |
| Sputum 66% | Tachycardia 50% |
| Pleuritic chest pain 50% | Focal lung exam >90% |
On physical examination, patients with CAP usually have signs of fever (80%), tachypnea (70%), and tachycardia (50%); see Table 2. Most will have a focal lung exam (>90%) with findings ranging from crackles to bronchial breath sounds.10 No exam finding is specific for the diagnosis of pneumonia, but the absence of fever, tachycardia, and tachypnea significantly reduces the probability of CAP in patients with suspected pneumonia.10 Furthermore, similar to the clinical history, the physical examination of elderly patients with community‐acquired pneumonia is not specific or sensitive for the diagnosis of CAP. For example, up to 40% of elderly patients subsequently determined to have CAP may not have fever.11
Leukocytosis is common in patients with CAP; however, its absence does not rule out disease.12 A number of guidelines recommend laboratory evaluation of electrolytes, urea nitrogen, creatinine, liver enzymes, and bilirubin, although these are used primarily for prognostication and are not specifically useful in the diagnosis of CAP.
DIAGNOSIS
Differential Diagnosis
Given the nonspecific nature of the symptoms and signs associated with CAP, there is no single clinical feature or combination of clinical features that adequately rules in or out the diagnosis of CAP. Consequently, the differential diagnosis to be considered in patients with suspected CAP is broad. Noninfectious diseases can often present with similar clinical syndromes; these include congestive heart failure, exacerbation of chronic obstructive pulmonary disease (COPD), asthma, pulmonary embolism, and hypersensitivity pneumonitis. These diseases can often be distinguished with a thorough history and physical examination.
In addition, other upper‐ and lower‐airway infectious diseases can have similar nonspecific signs and symptoms. In particular, pneumonia must often be differentiated from acute bronchitis, which as a diagnosis accounts for up to 40% of patients evaluated for cough (versus 5% for pneumonia).10 Patients with acute bronchitis frequently do not present with high fevers or hypoxia and in general will not benefit from antibiotic therapy.13 Patients believed to have community‐acquired pneumonia might also be suffering from other pneumonia syndromes including aspiration pneumonia, postobstructive pneumonia, and pneumonia in immunocompromised patients (eg, those with HIV, on steroids, receiving chemotherapy). Determining the correct diagnosis can have implications for therapy and prognosis.
Diagnostic Studies
The diagnosis of community‐acquired pneumonia requires that a patient have both signs and symptoms consistent with pulmonary infection and evidence of a new radiographic infiltrate. Therefore, most guidelines recommend that all patients with a possible diagnosis of CAP be evaluated with chest radiography.1, 14, 15
The specific radiographic findings in community‐acquired pneumonia range from lobar consolidation to hazy focal infiltrate to diffuse bilateral interstitial opacities (see Figure 1). Although chest radiography has traditionally been considered the gold standard for the diagnosis of CAP, its exact performance characteristics are unknown, and it is clearly not 100% sensitive or 100% specific. The utility of the chest radiograph can be limited by patient body habitus, underlying lung disease, or dehydration. Computed tomography (CT) scanning, although not recommended for routine use, can identify pulmonary consolidation in up to 30% of patients with a normal or equivocal chest radiograph in whom pneumonia is suspected and can also identify complications of pneumonia including an empyema or pulmonary abscess.16

Limitations in the performance of the chest radiograph have resulted in an interest in the diagnostic performance of serologic markers of infection such as C‐reactive protein (CRP), procalcitonin, and soluble triggering receptor expressed on myeloid cells (s‐TREM).1719 Preliminary evidence suggests these inflammatory markers may ultimately prove useful in differentiating infectious from noninfectious pulmonary processes, but regular use of these new tests cannot currently be recommended.
Most expert guidelines state that 2 sets of blood cultures should be taken and analyzed prior to antibiotic administration in all patients admitted to the hospital with suspected community‐acquired pneumonia.1, 14, 15 Isolation of bacteria from blood cultures in CAP is a very specific way to identify a causative organism in order to subsequently narrow therapy and also identifies a high‐risk group of patients because bacteremia is associated with increased mortality. Obtaining blood cultures within 24 hours of admission has been associated with 10% lower odds of 30‐day mortality in patients with CAP,20 and as a result, drawing blood cultures prior to antibiotic administration is a national quality indicator for CAP.
There are, however, a number of problems with the routine acquisition of blood cultures in all patients admitted with CAP. Practically, the cultures can be difficult to obtain, can potentially delay the initiation of antibiotics, and are often contaminated, which has been shown to increase both cost and length of stay.21, 22 The yield is generally low: the true‐positive bacteremia rate for admitted patients with CAP ranges from 6% to 9%, and the culture results rarely change management or outcomes.23, 24 Given these limitations, many have argued that blood cultures should be obtained with a more targeted approach. A recent study used a Medicare database to create a decision‐support tool to help maximize the value of blood cultures in CAP.25 The predictors of a positive blood culture are shown in Table 3. Not obtaining cultures on patients who had received prior antibiotics or had no risk factors resulted in about 40% fewer overall cultures while identifying approximately 90% of bacteremias. In their guidelines, the British Thoracic Society (BTS) advocates a similar strategy, recommending blood cultures be omitted in nonsevere pneumonia and in patients without comorbidities.15, 26 Although recommendations vary for non‐severe CAP in hospitalized patients, all professional society guidelines agree that blood cultures should be obtained in critically ill patients, and if cultures are obtained, they should be drawn prior to antibiotics.1, 14, 15, 26
| Comorbidities |
| Liver disease |
| Vital signs |
| Systolic blood pressure < 90 mm Hg |
| Temperature < 35C or 40C |
| Pulse 125 beats/min |
| Laboratory and radiographic data |
| Blood urea nitrogen (BUN) 30 mg/dL |
| Sodium < 130 mmol/L |
| White blood cells < 5000/mm3 or > 20,000/mm3 |
| Prior use of antibiotics (negative predictor) |
Substantial controversy surrounds the utility of routine sputum gram stains and cultures for patients admitted to the hospital with CAP. The Infectious Disease Society of America (IDSA) and the British Thoracic Society (BTS) both recommend that all patients admitted to the hospital with community‐acquired pneumonia should have a gram stain and culture of expectorated sputum.1, 15, 26 Both organizations argue sputum collection is a simple and inexpensive procedure that can potentially identify pathogenic organisms and can affect both initial and long‐term antibiotic therapy. Most notably, they highlight gram stain specificity of greater than 80% for pneumococcal pneumonia. Conversely, the American Thoracic Society (ATS) argues that sputum gram stains and cultures generally have low sensitivity, specificity, and positive predictive value.14 Furthermore, they argue the utility of sputum testing is also limited practically; in one study 30% of patients could not produce an adequate sputum specimen and up to 30% had received prior antibiotic therapy, substantially reducing the yield.27 In another study, good‐quality sputum with a predominant morphotype could be obtained in only 14% of patients admitted with CAP.28 However, targeting sputum analysis to patients who have not received prior antibiotics and are able to produce an adequate sample improved the yield significantly.29 In addition, with increasing rates of antibiotic resistance among common community isolates (ie, S. Pneumoniae) and the increasing prevalence of infecting organisms not targeted by routine empiric therapy (methicillin‐resistant Staphylococcus Aureus [MRSA]), isolation of potential causative pathogens is increasingly important. We believe that severely ill patients with CAP (such as patients admitted to the ICU), as well as patients with identifiable risk factors for uncommon or drug‐resistant pathogens (eg, Pseudomonas aeruginosa, enteric gram‐negative rods, MRSA, etc.) should have sputum sent for gram stain and culture. Ideally, sputum obtained for gram stain and culture should be:
-
Prior to antibiotic therapy,
-
A deep‐cough, expectorated specimen,
-
A purulent specimen (>25 polymorphonucleacytes and less than 10 squamous cells per high‐powered field), and
-
Rapidly transported to the laboratory.
Subsequent gram stain and culture results should be interpreted in the specific clinical context and antibiotic choices targeted appropriately.
Alternative Diagnostic Tests
In recent years, there has been growth in additional diagnostic tests targeting specific organisms. The pneumococcal urinary antigen assay is a relatively sensitive (50%80%) and highly specific (90%) test for the detection of pneumococcal pneumonia, when compared with conventional diagnostic methods.27 The test is simple, convenient, rapid ( 15 min), and, with its high specificity, may allow for more focused antimicrobial therapy early in management. Current limitations include the possibility of false‐positive tests in patients colonized with S. pneumoniae or infected with other streptococcal species, as well as the inability to determine antibiotic sensitivity from positive tests. Updated IDSA and BTS guidelines state pneumococcal urinary antigen testing is an acceptable adjunct to other diagnostic tests, but blood and sputum analyses should still be performed.26, 27 For patients with suspected Legionella pneumonia (primarily critically ill and immunocompromised patients or in association with regional outbreaks), the urinary Legionella antigen assay is the test of choice, which detects 80%95% of community‐acquired cases of Legionnaires' disease with a specificity of 90%.27
During the winter months (typically from October to March), rapid antigen testing for influenza is generally recommended for patients with signs or symptoms consistent with influenza.27 The sensitivity of these tests is approximately 50%70%, so negative test results do not exclude the diagnosis, but results can be important epidemiologically and therapeutically (differentiating influenza A and B strains).27 Diagnostic tests targeting other common CAP pathogens, such as serologic tests for Mycoplasma pneumoniae or Chlamydia spp, should not be routinely performed. Testing for less common causative pathogens such as Mycobacterium tuberculosis should only be employed in the appropriate clinical setting.
ADMISSION DECISION
Once the diagnosis of CAP has been made, the initial site where treatment will occur, whether the hospital or the home, must be determined. The decision to hospitalize should be based on 3 factors: 1) evaluation of the safety of home treatment, 2) calculation of the Pneumonia Severity Index (PSI), and 3) clinical judgment of the physician.27 The PSI, or PORT (Pneumonia Outcomes Research Team) score, is a validated prediction rule that quantifies mortality and allows for risk stratification of patients with community‐acquired pneumonia.2 The PSI combines clinical history, physical examination, and laboratory data at the time of admission to divide patients into 5 risk classes and to estimate 30‐day mortality (Figure 2), which ranges from 0.1% of patients in risk class I to 27.0% in risk class V.2
On the basis of the estimated prognosis and in the absence of concerns about home safety or comorbidities, patients in risk classes I, II, and III should be managed at home. Many prospective trials have shown that implementation of PSI significantly increases the number of low‐risk patients managed outside the hospital, with no differences in quality of life, complications, readmissions, or short‐term mortality.30, 31 Most recently, a trial randomizing patients in risk classes II and III to treatment in the hospital or at home found no significant differences in clinical outcomes but did find that patients were more satisfied with care at home.32 Because the number of patients with CAP being treated at home is increasing, the American College of Chest Physicians recently published a consensus statement on the management of community‐acquired pneumonia in the home.33 All national guidelines for the management of community‐acquired pneumonia recommend using the PSI to help determine the initial location of treatment, with the caveat that using the prediction rule should never supersede clinical judgment in the decision about whether to admit.1, 14, 15, 26, 27 A practical decision tree for the use of the PSI is shown in Figure 3.
There are no reliable prediction rules for deciding on whether admission to the intensive care unit is necessary. Hemodynamic instability requiring resuscitation and monitoring or respiratory failure requiring ventilatory support are clear indications for ICU admission. Additional variables such as tachypnea (respiratory rate 30), altered mental status, multilobar disease, and azotemia are associated with severe CAP and should prompt consideration of ICU admission, especially when 2 or more variables coexist.14
TREATMENT
Initial Treatment
Once the admission decision is made and the initial diagnostic tests are completed (including blood and sputum cultures), patients with presumed community‐acquired pneumonia should receive necessary supportive care (O2, intravenous fluids, etc.) and prompt antimicrobial therapy. Antibiotics should be administered within 4 hours of arrival to patients with suspected CAP, as such prompt administration may be associated with shorter in‐hospital stays and decreased 30‐day mortality.34, 35 Regulatory organizations such as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the Center for Medicare Services (CMS) have made delivery of antibiotics in less than 4 hours a hospital quality measure.
Despite diagnostic testing, the specific etiologic agent causing the pneumonia of a patient remains unknown in up to 75% of those admitted to the hospital.14 Most expert guidelines therefore recommend broad‐spectrum empiric therapy targeting both the typical and the atypical organisms that commonly cause CAP (Table 1).
Recommendations for empiric antibiotics are driven by 2 key factors: antibiotic resistance by S. pneumoniae and the results of studies of CAP treatment outcomes. Historically, patients with suspected community‐acquired pneumonia were treated with penicillin with generally good outcomes. Recently, the rate of S. pneumoniae isolates resistant to penicillin has risen dramatically in the United States, ranging between 20% and 30%, with high‐level resistance (MIC 4 mg/L) as high as 5.7%.36, 37 Concurrently, the rates of resistance of S. pneumoniae to many other antibiotics commonly used to treat CAP have also risen.37 Despite increasing resistance overall, most U.S. pneumococcal isolates have low resistance to third‐generation cephalosporins and fluoroquinolones with enhanced activity against S. pneumoniae.3638 In addition, despite increasing resistance by pneumococcal isolates to penicillin, several observational studies have shown that regardless of initial therapy, resistance to penicillin as well as third‐generation cephalosporins is not associated with higher mortality or worse outcomes when controlled for other risk factors for drug resistance.39, 40 An exception to that rule is pneumococcal isolates that are very highly resistant to PCN (MIC 4 mg/dL). At least one study has shown that patients with such isolates may be at higher risk for adverse outcomes and should probably not be treated with penicillins.1, 14, 15, 41 However, nationally, fewer than 6% of pneumococcal isolates have this level of resistance.37
The rationale for empiric broad‐spectrum coverage against both typical and atypical organisms has arisen from many retrospective and observational studies that have suggested that there is clinical benefit and improved outcomes with such regimens. One large retrospective study showed that in elderly patients with CAP, fluoroquinolone monotherapy was associated with lower 30‐day mortality when compared to monotherapy with a third‐generation cephalosporin.34 Adding an extended‐spectrum macrolide (eg, azithromycin) to an extended‐spectrum ‐lactam (eg, ceftriaxone) in the treatment of patients hospitalized with nonsevere CAP also appears to be associated with improved outcomes. Adding a macrolide has resulted in shorter lengths of stay (LOS), less treatment failure, and lower mortality.34, 4244 Similarly, according to unpublished observations, adding doxycycline to a ‐lactam as initial therapy was associated with a benefit of decreased mortality.45 The presumed etiology of the benefit has been the addition of specific coverage of atypical organisms, such as Mycoplasma pneumoniae and Chlamydia pneumoniae, which are common causes of CAP (Table 1). Others have proposed that the benefit of therapy with macrolides may be derived from the inherent anti‐inflammatory properties of macrolides.46 Because research has shown a benefit of dual versus monotherapy across a spectrum of antibiotics, others have proposed the benefit is simply a result of receiving double antibiotic coverage. In particular, 2 studies found a benefit of reduced mortality from combination therapy over monotherapy in bacteremic pneumococcal pneumonia.47, 48
Yet the accumulated evidence for adding coverage of atypical organisms has been only retrospective and observational. Because of this, the recommendation to routinely add antibiotics active against atypical organisms has been questioned by some. Two recent meta‐analyses and a systematic review examined all the available data on the need for atypical coverage in the treatment of patients with community‐acquired pneumonia.4951 Surprisingly, none showed a benefit in clinical efficacy or survival in patients treated with agents active against both atypical and typical organisms when compared to regimens with only typical coverage. In subset analyses, there was a benefit to providing empiric atypical coverage in patients subsequently shown to have Legionella spp. as a causative pathogen. However, this organism was uncommon in all 3 studies. Unfortunately, most studies included in the meta‐analyses compared fluoroquinolone or macrolide monotherapy with third‐generation cephalosporin monotherapy. There have been no high‐quality randomized, controlled trials of the treatment of hospitalized patients with CAP assessing combination therapy covering both typical and atypical organisms with monotherapy targeting typical organisms alone. High‐quality trials are warranted.
Despite the recent articles questioning the importance of atypical coverage, citing the substantial retrospective data and the general inability to identify causative organisms in most cases of CAP, adding a second agent with atypical coverage to a ‐lactam currently appears to be the most efficacious empiric treatment for CAP. Nearly all expert guidelines for the management of community‐acquired pneumonia recommend this empiric approach.1, 14, 27
Table 4 displays our recommendations for the treatment of community‐acquired pneumonia requiring hospitalization. Before implementation of these guidelines, hospitalists should consult with their infectious disease experts and consider local resistance patterns. In general, a typical adult patient with non‐severe CAP without additional risk factors should receive a parenteral extended‐spectrum ‐lactam plus either doxycycline or an advanced macrolide (see Table 4). Extended‐spectrum ‐lactams include cefotaxime, ceftriaxone, ampicillin‐sulbactam, and ertapenem. A respiratory fluoroquinolone as a single agent can be used for non‐ICU patients with CAP, but some agencies, including the Centers for Disease Control (CDC), discourage routine use of these agents in all patients secondary to concerns about cost and increasing gram‐negative rod fluoroquinolone resistance.52, 53
| Patient group | Empiric antibiotic therapy |
|---|---|
| |
| Inpatient, non‐ICU | ‐Lactama + either doxycycline or an advanced macrolideb |
| Severe ‐lactam allergyc | Respiratory fluoroquinoloned |
| Inpatient, ICU | |
| No risk for Pseudomonas | ‐Lactam + either an advanced macrolide or a respiratory fluoroquinolone |
| Severe ‐lactam allergy | Respiratory fluoroquinolone + clindamycin |
| Pseudomonas risk factorse | Antipseudomonal ‐lactamf + an antipseudomonal fluoroquinoloneg |
| Severe ‐lactam allergy | Aztreonam + a respiratory fluoroquinolone |
| MRSA risk factorsh | Add vancomycin to above regimens |
| From nursing home | Should be treated as nosocomial/health‐care‐associated pneumonia |
| Aspiration pneumonia | ‐Lactam or respiratory fluoroquinolone clindamycini |
Patients hospitalized with severe CAP who require ICU‐level care are at increased risk of Legionella spp. and drug‐resistant S. pneumoniae, which must be reflected in their initial antibiotic therapy.5 Patients with severe pneumonia should receive an intravenous extended‐spectrum ‐lactam plus either an intravenous macrolide or an intravenous respiratory fluoroquinolone.
All patients with severe CAP who are admitted to the intensive care unit should be routinely screened for risk factors for Pseudomonas aeruginosa. The known risk factors for pseudomonal infection are: bronchiectasis, immunosuppression including more than 10 mg/day of prednisone, malnutrition, and treatment with broad‐spectrum antibiotics in the last month.14 Those at risk for Pseudomonas aeruginosa or other resistant gram‐negative rod infection should be treated with an antipseudomonal ‐lactam plus an antipseudomonal fluoroquinolone. Many patients with severe CAP have risk factors for MRSA infection including recent prolonged hospitalization, recent use of broad‐spectrum antibiotics, and significant underlying lung disease, which should be considered in choosing initial antibiotic therapy.54 In addition, there have been reports of patients without underlying risk factors presenting with severe community‐acquired MRSA pneumonia. Many of these patients were younger and the MRSA pneumonia was associated with a necrotizing or cavitary disease requiring prolonged ICU stays.5558 In such cases or if an institution's rate of methicillin resistance in S. aureus community isolates is high (>15%20%), it may be appropriate to add initial empiric MRSA coverage for patients admitted to the ICU with CAP.55
Some patients will have unique risk factors and clinical presentations, which may require modification of these empiric recommendations. Several studies found 5%15% of cases of community‐acquired pneumonia to be aspiration pneumonia.57 Risk factors for aspiration events include, among others, dysphagia, history of stroke, altered level of consciousness, poor dentition, and tube feeding. Aspiration pneumonia traditionally was believed to be secondary to oral anaerobes, but recent research suggests gram‐positive cocci and gram‐negative rods are the predominant organisms.58 Antibiotic therapy in patients with clear aspiration pneumonia should be directed at these microbes with an extended‐spectrum ‐lactam (eg, ceftriaxone) or a respiratory fluoroquinolone (eg, levofloxacin or moxifloxacin). Anaerobic bacterial coverage can be added in patients with severe periodontal disease, alcoholism, concern for empyema, or evidence of aspiration with pulmonary abscess.58
Patients residing in long‐term care facilities are at high risk of contracting pneumonia. The microbiology of infections acquired in nursing facilities is similar to that in hospital‐acquired cases.59, 60 As a result, patients who develop pneumonia in institutional settings such as nursing homes should be treated with broad‐spectrum antibiotics, including coverage for MRSA.
Subsequent Treatment
Initial empiric antibiotic treatment should be modified based on the results of diagnostic testing. Although the specific etiologic agent is determined in only 25% of cases of CAP,35 when an organism is isolated, antibiotic coverage should be narrowed to cover that particular organism with an antibiotic with adequate lung penetration. Evidence suggests clinicians often do not adjust or narrow antibiotics based on sensitivity results, potentially breeding resistant organisms.61
Patients hospitalized with CAP usually improve quickly if they receive early, appropriate antibiotic therapy and supportive care. Excluding patients with severe CAP requiring intensive care unit admission, most patients resolve their tachycardia, tachypnea, and fever by day 2 or 3.62 Recent practice experience, evidence, and published guidelines14, 27 all indicate that patients can safely be transitioned to oral antibiotic therapy earlier in their hospital course. Table 5 outlines criteria that can be used to identify patients who have had an adequate response to parenteral therapy and can be considered for a switch to oral antibiotics. If these criteria are met, patients have less than a 1% chance of clinical deterioration necessitating admission to an ICU or transitional care unit.62 When an etiologic organism is not identified, oral therapy should reflect a spectrum of coverage to that of the initial intravenous therapy. In some cases, this may require use of more than one oral agent. We have had success, however, transitioning non‐ICU patients initially treated with intravenous ceftriaxone plus oral doxycycline, typically for 4872 hours, to oral doxycycline monotherapy at discharge.45
| Stable vital signs and clinical criteria for 24 hours |
| Temperature 37.8C (100F) |
| Heart rate 100 beats per minute |
| Respiratory rate 24 breaths per minute |
| Systolic blood pressure 90 mm Hg |
| Oxygen saturation (on room air) 90% |
| Ability to take oral medications |
There have been a limited number of high‐quality randomized trials examining the optimal duration of treatment for community‐acquired pneumonia. Most practice guidelines recommend 710 days for patients with CAP requiring hospitalization, with 14 days for documented Mycoplasma pneumoniae or Chlamydia pneumoniae. One recent randomized trial of patients with mild to severe CAP showed a short course of high‐dose levofloxacin (750 mg daily 5 days) was at least as effective as normal dosing (500 mg daily 10 days).63 Clinical experience with high‐dose levofloxacin is limited, but this regimen can be considered because it may reduce costs and exposure to antibiotics. When diagnosed, Legionella is usually treated for 1021 days, but 14 days is adequate with macrolides because of their long half‐life.27 Patients with more virulent pathogens like Staphylococcus aureus or Pseudomonas aeruginosa or other suppurative complications should be treated for at least 14 days.1, 14, 15, 27 In determining length of therapy, clinicians should use these durations of treatment as guides, and to individualize therapy, they should always consider patient age and frailty, comorbid conditions, severity of illness, and hospital course.
Failure to Respond
Although most patients hospitalized for CAP will improve rapidly and reach clinical stability in 23 days, some patients fail to respond. Some studies have estimated that failure to improve or clinical deterioration occurs in 5%10% of patients in the first 23 days.64 The common reasons for clinical decline or nonresponse to treatment, highlighted in Table 6, are:
-
Incorrect diagnosis: Illnesses such as congestive heart failure, pulmonary embolism, neoplasms, and hypersensitivity pneumonitis can mimick CAP.
-
Inadequate antibiotic selection: The etiologic agent may be resistant to empiric antibiotic selections. Examples would include methicillin‐resistant Staphylococcus aureus (MRSA) or multiresistant gram‐negative bacilli.
-
Unusual pathogen: CAP syndromes can be caused by myriad unusual organisms including Pneumocystis jirovecii, mycobacterium tuberculosis, endemic fungal infections (eg, coccidioidomycosis), and nocardiosis.
-
Complications of pneumonia: Specific complications of CAP include empyema, pulmonary abscess, extrapulmonary spread including meningitis or endocarditis, or other organ dysfunctions such as renal failure or myocardial infarction.
-
Inadequate host response: Despite appropriate antibiotic and supportive therapy, patients with CAP often fail to respond.
| Incorrect diagnosis of CAP. |
| Inadequate or inappropriate antibiotic selection for CAP. |
| Unusual pathogen causing CAP. |
| Pulmonary or extrapulmonary complication of CAP. |
| Inadequate or poor host response. |
Progressive pneumonia despite appropriate therapy and empyema were the most common causes of failure to respond in the first 72 hours in a recent study.64 Risk factors for early failure were older age (>65 years), Pneumonia Severity Index > 90, Legionella pneumonia, gram‐negative pneumonia, and initial antimicrobial therapy discordant with final culture and susceptibility results. The initial evaluation of the nonresponding patient should address these common causes and is likely to include additional imaging (CT), sampling of potential extrapulmonary infection (thoracentesis), and, in some cases, bronchoscopy.
DISCHARGE/FOLLOW‐UP PLANS
Patients hospitalized for community‐acquired pneumonia can be safely discharged when they have reached clinical stability, are able to tolerate oral medications, have no other active comorbid conditions, and have safe, close, appropriate outpatient follow‐up (see Table 7). Clinical pathways employing these discharge criteria have been found to be safe and effective in reducing the length of stay for CAP. Most important, patients should have met most if not all of the vital sign and clinical criteria noted in Table 5 in the criteria for switching to oral therapy. Patients with 2 or more abnormal vital signs (instabilities) within 24 hours prior to discharge are at high risk of readmission and mortality, but those with one or no abnormal vital signs generally have good outcomes.65 Absent other clinical factors or extenuating circumstances (persistent hypoxia, poor functional status, etc.), most patients with CAP should reach clinical stability by day 3 or 4, be considered for a switch to oral therapy, and, if stable, be discharged shortly thereafter.
| Patients should: |
|
Meet clinical criteria in Table V. |
| Be able to tolerate oral medications (no need to observe for 24 hours on oral therapy). |
| Have no evidence of active comorbid conditions (myocardial ischemia, pulmonary edema, etc.). |
| Have a normal mental status (or have returned to their baseline). |
| Have safe, appropriate outpatient follow‐up. |
When patients with CAP are discharged from the hospital, they should be counseled about the expected course of recovery. Most important, patients and families must be informed that many symptoms of CAP may persist well after hospitalization. In one study, up to 80% of patients reported persistent cough and fatigue 1 week after discharge, and up to 50% still had dyspnea and sputum production. In some, the cough can last for 46 weeks.8
All patients discharged after treatment of community‐acquired pneumonia should have follow‐up with their outpatient provider. The physician responsible for their inpatient care should communicate directly with the provider and outline the hospital course, the discharge medications, and the duration of antibiotic therapy. There is no specific time frame within which patients must be seen, but follow‐up should be dictated by patient age, comorbidities, clinical stability at discharge, and degree of illness. The American Thoracic Society guidelines do recommend patients with a substantial smoking history who are hospitalized with CAP have a follow‐up chest radiograph 46 weeks after discharge to establish a radiographic baseline and exclude the possibility of underlying malignancy.14 However, several studies have suggested that radiographic resolution may take 3 or more months in some patients, especially the elderly and those with multilobar disease.66
PREVENTION
Prevention of community‐acquired pneumonia and pneumonic syndromes has traditionally relied on vaccination with the polysaccharide pneumococcal pneumonia vaccine and the seasonal influenza vaccine. The vaccine for S. pneumoniae used in adults is composed of the 23 serotypes that cause 85%90% of the invasive pneumococcal infections in the United States. Although in randomized trials the vaccine has not consistently prevented community‐acquired pneumonia or death in elderly patients or those with comorbidities, it likely prevents invasive pneumococcal infection.67 National guidelines and the CDC recommend the pneumococcal vaccine be given to all patients older than 65 years and those with chronic medical conditions.1, 14, 15
The seasonal influenza vaccine has clearly been shown to decrease influenza‐related illness in elderly and high‐risk patient populations. As well, in a meta‐analysis and a large observational study of patients older than 65 years, vaccination against influenza prevented pneumonia, hospitalization, and death.68, 69 Vaccination of health care workers may also confer a benefit to elderly patients of reduced mortality. The CDC recommends the influenza vaccine for all patients more than 50 years old, those with comorbidities, those at high risk for influenza, and health care workers in both inpatient and outpatient settings.
Pneumococcal and influenza vaccination have traditionally been relegated to the outpatient setting. National guidelines and the CDC recommend vaccination of all eligible hospitalized patients. Vaccination is safe and effective with almost any medical illness, and both vaccines can be given simultaneously at discharge.69 Both JCAHO and CMS have defined administration of the pneumococcal and influenza vaccines to patients hospitalized with CAP as a quality measure. Using standing orders is the most effective means of ensuring vaccination.
Some evidence suggests that tobacco smokers are at increased risk of invasive pneumococcal disease or pneumonia.70 Patients hospitalized (for all illnesses, but for CAP in particular) should be counseled about smoking cessation and offered pharmacotherapy and outpatient follow‐up. And, finally, recent observational data suggests that use of acid suppressive therapy, including proton pump inhibitors and H‐2 receptor antagonists, may be associated with an increased risk of developing CAP.71 Patients using these agents who are admitted with CAP should have their indications for treatment reviewed, especially when the pneumonia has been recurrent and there is no clear indication for continued use of acid suppressive therapy, in which case they should be discontinued in the hospital.
CONCLUSIONS
Community‐acquired pneumonia remains a common cause for hospitalization of adult patients, with significant associated morbidity and mortality. Although there are multiple expert guidelines for the management of community‐acquired pneumonia, further research is urgently needed. Clinicians need improved diagnostic tests that enable an earlier and more accurate diagnosis of CAP. In addition, the etiologic agent causing CAP is rarely discovered; improved microbiologic studies might enable antibiotic therapy to be targeted to the organisms responsible. High‐quality randomized, controlled trials examining empiric antibiotic therapy in CAP are needed, especially related to the addition of agents covering atypical organisms. Last, the general management of patients hospitalized with CAP is marked by significant heterogeneity, and research and initiatives focusing on improving the quality and process of care of patients with CAP are needed.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Practice guidelines for the management of community‐acquired pneumonia.Clin Infect Dis.2000;31:347–382.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Pneumonia: still the old man's friend?Arch Intern Med.2003;163:317–323.
- ,,, et al.New and emerging etiologies for community‐acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases.Medicine.1990;69:307–316.
- .Community‐acquired pneumonia.Lancet.2003;362:1991–2001.
- ,,, et al.Processes and outcomes of care for patients with community‐acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team (PORT) cohort study.Arch Intern Med.1999;159:970–980.
- ,.Management of community‐acquired pneumonia.N Engl J Med.2002;347:2039–2045.
- ,,, et al.Measuring symptomatic and functional recovery in patients with community‐acquired pneumonia.J Gen Intern Med.1997;12:423–430.
- ,,, et al.Influence of age on symptoms at presentation with patients with community‐acquired pneumonia.Arch Intern Med.1997;157:1453–1459.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Community‐acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes.Medicine.2003;82:159–169.
- ,.Testing strategies in the initial management of patients with community‐acquired pneumonia.Ann Intern Med.2003;138:109–118.
- ,.Uncomplicated acute bronchitis.Ann Intern Med.2000;133:981–991.
- ,,, et al.American Thoracic Society: Guidelines for the management of community‐acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.British Thoracic Society guidelines for the management of community acquired pneumonia in adults.Thorax.2001;56:Suppl. 4,IV1–IV64.
- ,,,,.High‐resolution computed tomography for the diagnosis of community‐acquired pneumonia.Clin Infect Dis.1998;27:358–363.
- ,,, et al.Performance of a bedside C‐reactive protein test in the diagnosis of community‐acquired pneumonia in adults with acute cough.Am J Med.2004;116:529–535.
- ,,, et al.Effect of procalcitonin‐guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster‐randomised, single‐blinded intervention trial.Lancet.2004;363:600–607.
- ,,, et al.Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia.N Engl J Med.2004:350:451–458.
- ,,, et al.Quality of care, process, and outcomes in elderly patients with pneumonia.JAMA.1997;278:2080–2084.
- ,,,.Limited usefulness of initial blood cultures in community acquired pneumonia.Emerg Med J.2004;21:446–448.
- ,,.Contaminant blood cultures and resource utilization. The true consequences of false‐positive results.JAMA.1991;265:365–369.
- ,,, et al.The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community‐acquired pneumonia: a prospective observational study.Chest.2003;123:1142–1150.
- ,,, et al.Clinical utility of blood cultures in adult patients with community‐acquired pneumonia without defined underlying risks.Chest.1995;108:932–936.
- ,,,.Predicting bacteremia in patients with community‐acquired pneumonia.Am J Respir Crit Care Med.2004;169:342–347.
- British Thoracic Society. BTS Guidelines for the management of community acquired pneumonia in adults—2004 update. Available at: www.brit‐thoracic.org/guidelines.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Update of guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- ,,, et al.Assessment of the usefulness of sputum culture for diagnosis of community‐acquired pneumonia using the PORT predictive scoring system.Arch Intern Med.2004;164:1807–1811.
- ,,.Diagnostic value of microscopic examination of gram‐stained sputum and sputum cultures in patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2004;39(2):165–169.
- ,,, et al.Safely increasing the proportion of patients with community‐acquired pneumonia treated as outpatients: an interventional trial.Arch Intern Med.1998;158:1350–1356.
- ,,, et al.A critical pathway for treatment of community‐acquired pneumonia.JAMA.2000;283:2654–2655.
- ,,, et al.Outpatient care compared with hospitalization for community‐acquired pneumonia. A randomized control trial in low‐risk patients.Ann Intern Med.2005;142:165–172.
- ,,.Management of community‐acquired pneumonia in the home.Chest.2005;127:1752–1763.
- ,,,,.Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia.Arch Intern Med.1999;159:2562–2572.
- ,,,,.Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community‐acquired pneumonia.Arch Intern Med.2004;164:637–644.
- ,,, et al.Increasing prevalence of multidrug‐resistant Streptococcus pneumoniae in the United States.N Engl J Med.2000;343:1917–1924.
- ,,, et al.Susceptibility patterns of Streptococcus pneumoniae isolates in North America (2002–2003): contemporary in vitro activities of amoxicillin/clavulanate and 15 other antimicrobial agents.Int J Antimicrob Agents.2005;25(4):282–289.
- ,,, et al.Antimicrobial resistance among Streptococcus pneumoniae in the United States: have we begun to turn the corner on resistance to certain antimicrobial classes?Clin Infect Dis.2005;41(2):139–148.
- ,,, et al.Pneumonia acquired in the community through drug‐resistant Streptococcus pneumoniae.Am J Respir Crit Care.1999;159:1835–1842.
- ,,, et al.Drug‐resistant pneumococcal pneumonia: clinical relevance and related factors.Clin Infect Dis.2004;38:787–798.
- ,,, et al.Mortality from invasive pneumococcal pneumonia in the era of antibiotic resistance, 1995–1997.Am J Public Health.2000;90(2):223–9.
- ,,, et al.Lower mortality among patients with community‐acquired pneumonia treated with a macrolide plus a beta‐lactam agent versus a beta‐lactam alone.Eur J Clin Microbiol Infect Dis2005;24:190–195.
- ,,,.Impact of initial antibiotic choice on clinical outcomes in community‐acquired pneumonia: analysis of a hospital claims‐made database.Chest.2003;123:1503–1511.
- ,,,.Antimicrobial selection for hospitalized patients with presumed community‐acquired pneumonia: a survey of nonteaching US community hospitals.Ann Pharmacother2000;34:446–452.
- ,,,,.J Hosp Med.2006;1:7–12.
- .Anti‐inflammatory effects of macrolides—an underappreciated benefit in the treatment of community‐acquired respiratory tract infections and chronic inflammatory pulmonary conditions?J Antimicrob Chemother.2005;55:10–21.
- ,,, et al.Addition of a macrolide to a beta‐lactam based empirical antibiotic regimen is associated with lover in‐hospital mortality for patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2003;36:389–395.
- ,,, et al.Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia.Am J Respir Crit Care Med.2004;170:440–444.
- ,,,.Empiric antibiotic coverage of atypical pathogens for community‐acquired pneumonia in hospitalized adults.Cochrane Database Syst Rev.2005;2:CD004418.pub2.
- ,,.Effectiveness of β lactam antibiotics compared with antibiotics active against atypical pathogens in non‐severe community‐acquired pneumonia: meta‐analysis.Br Med J.2005;330:456.
- ,,,.Empirical atypical coverage for inpatients with community‐acquired pneumonia.Arch Intern Med.2005;165:1992–2000.
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888.
- ,,, et al.First‐generation fluoroquinolone use and subsequent emergence of multiple drug‐resistant bacteria in the intensive care unit.Crit Care Med.2005;33(2):283–289.
- ,.Etiology of community‐acquired pneumonia.Clin Chest Med.2005;26:47–55.
- .Community‐associated methicillin‐resistant Staphylococcus aureus: not only a cause of skin infections, also a new cause of pneumonia.Curr Opin Infect Dis.2005;18:123–124.
- ,,, et al.Severe community‐onset pneumonia in healthy adults caused by methicillin‐resistant Staphylococcus aureus carrying the Panton‐Valentine leukocidin genes.Clin Infect Dis.2005;40(1):100–107.
- ,,,.Fatal community‐associated methicillin‐resistant Staphylococcus aureus pneumonia in an immunocompetent young adult.Ann Emerg Med.2005;46:401–404.
- .Aspiration pneumonitis and aspiration pneumonia.N Engl J Med.2001;344:665–671.
- ,,, et al.Health care‐associated bloodstream infections in adults: a reason to change the accepted definition of community‐acquired infections.Ann Intern Med.2002;137:791–797.
- American Thoracic Society and theInfectious Diseases Society of America.Guidelines for the management of adults with hospital‐acquired, ventilator‐acquired, and healthcare‐associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Blood culture and susceptibility results and allergy history do not influence fluoroquinolone use in the treatment of community‐acquired pneumonia.Pharmacotherapy.2005;25(1):59–66.
- ,,, et al.Time to clinical stability in patients hospitalized with community‐acquired pneumonia: implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,, et al.Causes and factors associated with early failure in hospitalized patients with community‐acquired pneumonia.Arch Intern Med.2004;164:502–508.
- ,,, et al.Instability on hospital discharge and the risk of adverse outcomes in patients with pneumonia.Arch Intern Med.2002;162:1278–1284.
- ,,,.Radiographic resolution of community‐acquired bacterial pneumonia in the elderly.J Am Geriatr Soc.2004;52(2):224–229.
- ,,,.Vaccines for preventing pneumococcal infection in adults.Cochrane Database Syst Rev.2003;4:CD000422.
- ,,,,.The efficacy of influenza vaccine in elderly persons: a meta‐analysis and review of the literature.Ann Intern Med.1995;123:518–527.
- ,,, et al.Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly.N Engl J Med.2003;348:1322–1332.
- ,,,.Proportion of community‐acquired pneumonia cases attributable to tobacco smoking.Chest.1999;116:375–379.
- ,,, et al.Risk of community‐acquired pneumonia and use of gastric acid‐suppressive drugs.JAMA.2004;292:1955–1960.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Practice guidelines for the management of community‐acquired pneumonia.Clin Infect Dis.2000;31:347–382.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Pneumonia: still the old man's friend?Arch Intern Med.2003;163:317–323.
- ,,, et al.New and emerging etiologies for community‐acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases.Medicine.1990;69:307–316.
- .Community‐acquired pneumonia.Lancet.2003;362:1991–2001.
- ,,, et al.Processes and outcomes of care for patients with community‐acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team (PORT) cohort study.Arch Intern Med.1999;159:970–980.
- ,.Management of community‐acquired pneumonia.N Engl J Med.2002;347:2039–2045.
- ,,, et al.Measuring symptomatic and functional recovery in patients with community‐acquired pneumonia.J Gen Intern Med.1997;12:423–430.
- ,,, et al.Influence of age on symptoms at presentation with patients with community‐acquired pneumonia.Arch Intern Med.1997;157:1453–1459.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Community‐acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes.Medicine.2003;82:159–169.
- ,.Testing strategies in the initial management of patients with community‐acquired pneumonia.Ann Intern Med.2003;138:109–118.
- ,.Uncomplicated acute bronchitis.Ann Intern Med.2000;133:981–991.
- ,,, et al.American Thoracic Society: Guidelines for the management of community‐acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.British Thoracic Society guidelines for the management of community acquired pneumonia in adults.Thorax.2001;56:Suppl. 4,IV1–IV64.
- ,,,,.High‐resolution computed tomography for the diagnosis of community‐acquired pneumonia.Clin Infect Dis.1998;27:358–363.
- ,,, et al.Performance of a bedside C‐reactive protein test in the diagnosis of community‐acquired pneumonia in adults with acute cough.Am J Med.2004;116:529–535.
- ,,, et al.Effect of procalcitonin‐guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster‐randomised, single‐blinded intervention trial.Lancet.2004;363:600–607.
- ,,, et al.Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia.N Engl J Med.2004:350:451–458.
- ,,, et al.Quality of care, process, and outcomes in elderly patients with pneumonia.JAMA.1997;278:2080–2084.
- ,,,.Limited usefulness of initial blood cultures in community acquired pneumonia.Emerg Med J.2004;21:446–448.
- ,,.Contaminant blood cultures and resource utilization. The true consequences of false‐positive results.JAMA.1991;265:365–369.
- ,,, et al.The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community‐acquired pneumonia: a prospective observational study.Chest.2003;123:1142–1150.
- ,,, et al.Clinical utility of blood cultures in adult patients with community‐acquired pneumonia without defined underlying risks.Chest.1995;108:932–936.
- ,,,.Predicting bacteremia in patients with community‐acquired pneumonia.Am J Respir Crit Care Med.2004;169:342–347.
- British Thoracic Society. BTS Guidelines for the management of community acquired pneumonia in adults—2004 update. Available at: www.brit‐thoracic.org/guidelines.
- ,,,,,.Guidelines from the Infectious Disease Society of America. Update of guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- ,,, et al.Assessment of the usefulness of sputum culture for diagnosis of community‐acquired pneumonia using the PORT predictive scoring system.Arch Intern Med.2004;164:1807–1811.
- ,,.Diagnostic value of microscopic examination of gram‐stained sputum and sputum cultures in patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2004;39(2):165–169.
- ,,, et al.Safely increasing the proportion of patients with community‐acquired pneumonia treated as outpatients: an interventional trial.Arch Intern Med.1998;158:1350–1356.
- ,,, et al.A critical pathway for treatment of community‐acquired pneumonia.JAMA.2000;283:2654–2655.
- ,,, et al.Outpatient care compared with hospitalization for community‐acquired pneumonia. A randomized control trial in low‐risk patients.Ann Intern Med.2005;142:165–172.
- ,,.Management of community‐acquired pneumonia in the home.Chest.2005;127:1752–1763.
- ,,,,.Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia.Arch Intern Med.1999;159:2562–2572.
- ,,,,.Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community‐acquired pneumonia.Arch Intern Med.2004;164:637–644.
- ,,, et al.Increasing prevalence of multidrug‐resistant Streptococcus pneumoniae in the United States.N Engl J Med.2000;343:1917–1924.
- ,,, et al.Susceptibility patterns of Streptococcus pneumoniae isolates in North America (2002–2003): contemporary in vitro activities of amoxicillin/clavulanate and 15 other antimicrobial agents.Int J Antimicrob Agents.2005;25(4):282–289.
- ,,, et al.Antimicrobial resistance among Streptococcus pneumoniae in the United States: have we begun to turn the corner on resistance to certain antimicrobial classes?Clin Infect Dis.2005;41(2):139–148.
- ,,, et al.Pneumonia acquired in the community through drug‐resistant Streptococcus pneumoniae.Am J Respir Crit Care.1999;159:1835–1842.
- ,,, et al.Drug‐resistant pneumococcal pneumonia: clinical relevance and related factors.Clin Infect Dis.2004;38:787–798.
- ,,, et al.Mortality from invasive pneumococcal pneumonia in the era of antibiotic resistance, 1995–1997.Am J Public Health.2000;90(2):223–9.
- ,,, et al.Lower mortality among patients with community‐acquired pneumonia treated with a macrolide plus a beta‐lactam agent versus a beta‐lactam alone.Eur J Clin Microbiol Infect Dis2005;24:190–195.
- ,,,.Impact of initial antibiotic choice on clinical outcomes in community‐acquired pneumonia: analysis of a hospital claims‐made database.Chest.2003;123:1503–1511.
- ,,,.Antimicrobial selection for hospitalized patients with presumed community‐acquired pneumonia: a survey of nonteaching US community hospitals.Ann Pharmacother2000;34:446–452.
- ,,,,.J Hosp Med.2006;1:7–12.
- .Anti‐inflammatory effects of macrolides—an underappreciated benefit in the treatment of community‐acquired respiratory tract infections and chronic inflammatory pulmonary conditions?J Antimicrob Chemother.2005;55:10–21.
- ,,, et al.Addition of a macrolide to a beta‐lactam based empirical antibiotic regimen is associated with lover in‐hospital mortality for patients with bacteremic pneumococcal pneumonia.Clin Infect Dis.2003;36:389–395.
- ,,, et al.Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia.Am J Respir Crit Care Med.2004;170:440–444.
- ,,,.Empiric antibiotic coverage of atypical pathogens for community‐acquired pneumonia in hospitalized adults.Cochrane Database Syst Rev.2005;2:CD004418.pub2.
- ,,.Effectiveness of β lactam antibiotics compared with antibiotics active against atypical pathogens in non‐severe community‐acquired pneumonia: meta‐analysis.Br Med J.2005;330:456.
- ,,,.Empirical atypical coverage for inpatients with community‐acquired pneumonia.Arch Intern Med.2005;165:1992–2000.
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888.
- ,,, et al.First‐generation fluoroquinolone use and subsequent emergence of multiple drug‐resistant bacteria in the intensive care unit.Crit Care Med.2005;33(2):283–289.
- ,.Etiology of community‐acquired pneumonia.Clin Chest Med.2005;26:47–55.
- .Community‐associated methicillin‐resistant Staphylococcus aureus: not only a cause of skin infections, also a new cause of pneumonia.Curr Opin Infect Dis.2005;18:123–124.
- ,,, et al.Severe community‐onset pneumonia in healthy adults caused by methicillin‐resistant Staphylococcus aureus carrying the Panton‐Valentine leukocidin genes.Clin Infect Dis.2005;40(1):100–107.
- ,,,.Fatal community‐associated methicillin‐resistant Staphylococcus aureus pneumonia in an immunocompetent young adult.Ann Emerg Med.2005;46:401–404.
- .Aspiration pneumonitis and aspiration pneumonia.N Engl J Med.2001;344:665–671.
- ,,, et al.Health care‐associated bloodstream infections in adults: a reason to change the accepted definition of community‐acquired infections.Ann Intern Med.2002;137:791–797.
- American Thoracic Society and theInfectious Diseases Society of America.Guidelines for the management of adults with hospital‐acquired, ventilator‐acquired, and healthcare‐associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Blood culture and susceptibility results and allergy history do not influence fluoroquinolone use in the treatment of community‐acquired pneumonia.Pharmacotherapy.2005;25(1):59–66.
- ,,, et al.Time to clinical stability in patients hospitalized with community‐acquired pneumonia: implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,, et al.Causes and factors associated with early failure in hospitalized patients with community‐acquired pneumonia.Arch Intern Med.2004;164:502–508.
- ,,, et al.Instability on hospital discharge and the risk of adverse outcomes in patients with pneumonia.Arch Intern Med.2002;162:1278–1284.
- ,,,.Radiographic resolution of community‐acquired bacterial pneumonia in the elderly.J Am Geriatr Soc.2004;52(2):224–229.
- ,,,.Vaccines for preventing pneumococcal infection in adults.Cochrane Database Syst Rev.2003;4:CD000422.
- ,,,,.The efficacy of influenza vaccine in elderly persons: a meta‐analysis and review of the literature.Ann Intern Med.1995;123:518–527.
- ,,, et al.Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly.N Engl J Med.2003;348:1322–1332.
- ,,,.Proportion of community‐acquired pneumonia cases attributable to tobacco smoking.Chest.1999;116:375–379.
- ,,, et al.Risk of community‐acquired pneumonia and use of gastric acid‐suppressive drugs.JAMA.2004;292:1955–1960.
Medical Errors, Appropriate Dress for Physicians, Blood Cultures for Pneumonia Pts, and More
Rothschild JM, Landrigan CP, Cronin JW, et al. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694-1700.
Background: Critically ill patients require complex, immediate, high-intensity care, potentially placing them at increased risk of iatrogenic injury. The frequency and nature of adverse events and errors in the modern ICU have not been clearly defined.
Methods: Harvard researchers conducted a prospective, one-year, observational study of a MICU and a CCU at a tertiary care medical center. Adverse events and medical errors were identified by a four-pronged approach: direct 24-hour observation of interns, voluntary incident reporting, a computerized adverse drug event monitoring system, and chart abstraction. Two physicians independently assessed the type, severity, and preventability of the incidents.
Results: A total of 391 patients comprising 1,490 patient-days were observed and included. Twenty percent of all patients suffered an adverse event, 45% of which were preventable and 13% of which were felt to be life-threatening. There were 223 serious errors (those that caused harm or had the potential to cause harm) observed of which 11% were life threatening. Medication adverse events and medication errors accounted for a large proportion of the incidents during the study. Slips and lapses in care were much more common than rule-based (such as using the wrong protocol) or knowledge-based mistakes.
Discussion: Since the Institute of Medicine report in 1999, there has been an increasing focus on patient safety in the inpatient setting. Based on the results of this study and others, it appears the high-intensity, fast-paced nature of critical care places patients at substantial risk for iatrogenic injury. Up to 20% of patients admitted to the ICU in this study suffered an adverse event or a medical error, which translates into 0.8 adverse events and 1.5 serious medical errors per day in a 10-bed ICU.
Because failure to carry out intended plans (usually secondary to slips and lapses on the part of healthcare providers) was the most common cause of adverse events and errors, the authors address possible solutions. They propose employing computerized-order entry, clinical pharmacists in the ICU, closed ICU staffing, “smart” intravenous pumps, and improved teamwork and communication among healthcare providers. Hospitalists often manage critically ill patients and should be aware of the high risk of medical errors and should consider implementing specific systems changes to mitigate the risk.
The Value of Obtaining Blood Cultures in Pneumonia Pts
Kennedy M, Bates DW, Wright SB, et al. Do emergency department blood cultures change practice in patients with pneumonia? Ann Emerg Med. 2005 Nov;46(5):393-400.
Background: Previous observational studies in patients hospitalized with community-acquired pneumonia (CAP) have shown obtaining blood cultures may have a mortality benefit. This practice has become expert guideline-recommended, the standard of care, as well as a quality marker in the management of CAP. Several recent studies have questioned the utility and cost-effectiveness of this practice.
Methods: Harvard researchers performed a prospective, observational, cohort study of adults admitted to an urban university medical center. Researchers identified patients who had all of the following: clinical CAP, radiographic CAP, and blood cultures at admission. Blood cultures were classified as positive, negative, or contaminated based on previously established criteria. Data were collected on antimicrobial sensitivities, empiric antibiotic choices, and antibiotic changes.
Results: In one year, 414 patients with clinical and radiographic CAP had blood cultures at the time of admission. Twenty-nine of 414 (7%) of patients had true bacteremia while 25 of 414 (6%) had contaminants. Antibiotic therapy was altered in response to blood culture results in 15 of 414 patients (3.6%), of which 11 (2.7%) had therapy narrowed and four (1.0%) had therapy broadened. Of the 11 patients with bacteremia whose therapy was not changed, culture results supported narrowing therapy in eight cases but this was not done.
Discussion: This well done prospective observational study adds to a growing body of evidence questioning the utility of routine blood cultures on all patients hospitalized with CAP. The argument traditionally has been made that blood cultures allow clinicians to narrow or broaden antibiotics based on sensitivities. Yet, empiric therapy was broadened in response to bacteremia in only a small fraction of patients (1%) and in only 11 of 19 patients was therapy appropriately narrowed based on the blood cultures. The study did not measure the impact of blood cultures on clinical outcomes, but these striking results reveal that routine blood cultures rarely alter our management of hospitalized patients with CAP.
Further, many have argued obtaining routine blood cultures in CAP can have negative consequences. Blood cultures are relatively costly and time intensive, contaminated blood cultures can lead to repeated testing and increased length of stay, and delays in obtaining blood cultures can delay antibiotic administration, another important quality marker in CAP. For now, it remains the standard of care to obtain blood cultures in these patients, but hospitalists should be aware of the limitations of this practice and consider focusing on other clinical interventions and quality measures in CAP.
A Review Study: A Dyspneic Emergency Patient
Wang CS, FitzGerald JM, Schulzer M, et al. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005 Oct 19;294:944-1956.
Background: Distinguishing CHF from non-cardiac causes of dyspnea is a major challenge for hospitalists and emergency physicians, particularly in patients with a prior history of cardiac disease. Traditionally, clinicians have relied on the history, physical examination, and basic tests (chest X-ray and electrocardiogram) to diagnose CHF, but rapid B-type natriuretic peptide (BNP) testing is now widely incorporated as well.
A previous article in the Rational Clinical Examination series (Can the clinical examination diagnose left-sided heart failure in adults? JAMA. 1997;277(21):1712-1719) found that systolic dysfunction was moderately well predicted by an abnormal apical impulse on physical examination, radiographic cardiomegaly or venous redistribution, or electrocardiographic q waves or left bundle branch block.
Methods: In this review, the authors update and extend previous findings by also assessing the utility of serum BNP testing. The authors identified articles evaluating the diagnostic accuracy of the clinical exam and laboratory testing in diagnosing CHF in patients presenting to the emergency department with undifferentiated dyspnea. The “gold standard” was a clinical diagnosis of CHF made by the treating clinicians after an appropriate diagnostic workup. Summary likelihood ratios (LRs) were calculated using meta-analytic methodology.
Results/discussion: The authors determined that several findings increase the probability of CHF. A prior history of CHF (LR 5.8, CI 4.1-8.0) or myocardial infarction (LR 3.1, 95% CI 2.0-4.9), symptoms of paroxysmal nocturnal dyspnea (LR 2.6, 95% CI 1.5-4.5) and orthopnea (LR 2.2, 95% CI 1.2-3.9) were the most predictive historical factors. On physical examination, the presence of an S3 (LR 11, 95% CI 4.9-25), jugular venous distension (5.1, 95% CI 3.2-7.9), lung rales (LR 2.8, 95% CI 1.9-4.1), and peripheral edema (2.3, 95% CI 1.5-3.7) increased the probability of CHF. In interpreting these results, it is helpful to remember that a likelihood ratio of 2 increases the post-test probability by about 15%, and an LR of 5 increases the post-test probability by about 30%. Thus, a prior history of CHF and presence of an S3 or jugular venous distension are the most useful findings. Interestingly, clinician’s gestalt was equally predictive (LR 4.4, 95% CI 1.8-10.0.)
The most useful radiographic findings were venous congestion (LR 12.0, 95% CI 6.8-21) and the presence of cardiomegaly (LR 3.3; 95% CI 2.4-4.7). The single most predictive ECG finding was atrial fibrillation (LR 3.8; 95% CI 2.7-8.8); any abnormality on ECG had an LR of 2.2 (95% CI 1.6-3.1). Serum BNP levels were not more predictive of CHF than the history or physical examination; a BNP of >250 was associated with an LR of 4.6 (95% CI 2.6-8.0).
Few findings markedly decreased the probability of CHF. Here, it is helpful to remember that an LR of 0.5 decreases the post-test probability by about 15%, and an LR of 0.2 decreases the post-test probability by about 30%. With these in mind, the absence of cardiomegaly on CXR significantly changes the post-test probability (LR 0.33; 95% CI 0.23-0.48). A serum BNP level of less than 100pg/ml strongly argues against CHF, with an LR of 0.11 (95% CI 0.07-0.16); this finding lowers the post-test probability of CHF by about 45% compared to the pre-test probability.
In summary, the most useful findings for ruling in CHF in dyspneic emergency department patients were clinical gestalt, a prior history of CHF, findings of an S3 or jugular venous distension, and radiographic findings of venous congestion or cardiomegaly. Absence of radiographic cardiomegaly and a BNP of less than 100pg/ml argue against CHF. These must be interpreted in the context of the clinical pre-test probability of CHF, as none of the findings had likelihood ratios sufficient to be diagnostic of CHF when used individually.
What Should I Wear Today?
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005 Nov; 118(11): 1279-1286.
Background: This study addresses the prototypical everyday clinical dilemma: What should I wear to work?
Methods: Patients and visitors to an outpatient Veterans Affairs internal medicine clinic in South Carolina were shown photographs of male and female physicians in four different styles of dress:
- Professional (male physician wearing white coat with tie, female physician wearing white coat with tailored skirt or trousers);
- Business (suit and tie for male, tailored trouser or skirt for female);
- Surgical (surgical scrubs for both male and female): and
- Casual (jeans and t-shirt or short skirt).
The study was randomized so that male and female respondents viewed photographs of either male or female physicians. Respondents were asked to report how strongly they felt about the importance of their physician’s appearance, and their preference for each style of dress; specifically, respondents were asked which physician was the most trustworthy, which physician they felt most comfortable with for routine examinations and emergencies, and which physician they felt most comfortable discussing psychological, sexual, and social problems with.
Results: Respondents overwhelmingly preferred professional attire for all questions: 76.3% felt most comfortable with a professionally dressed physician for all encounters, with surgical scrubs a distant second (10.2%), ahead of business dress (8.8%). Respondents were also significantly more willing to discuss psychological, sexual, and social problems with a professionally dressed physician. Even for care in an emergency situation, respondents still expressed a significant preference for professional attire over scrubs.
In a logistic regression model, patients who were older, African-American, and had less than a high school education were significantly more likely to prefer professional attire. Interestingly, female respondents who viewed photographs of female physicians placed significantly greater emphasis on physician’s attire than did male respondents.
Discussion: The study is clearly subject to caveats, chiefly that it was conducted at a single VA clinic and that only one aspect of the physician-patient encounter was addressed. Undoubtedly, patient’s preferences were influenced by the popular portrayal of physicians on TV shows. Nevertheless, given that hospitalists typically see older patients with whom they are not familiar, the initial clinical encounter may indeed by influenced by something as simple as wearing a white coat.
UA by Nephrologist Versus Hospital-Based Clinical Labs
Tsai JJ, Yeun JY, Kumar VA, Don BR. Comparison and interpretation of urinalysis performed by a nephrologist versus a hospital-based clinical laboratory. Am J Kidney Dis. 2005 Nov;46(5):820-829.
Background: Distinguishing the correct cause of acute renal failure is a frequent clinical dilemma for hospitalists, particularly diagnosing acute tubular necrosis (ATN), which is the most common cause of in-hospital acute renal failure. Although urinalysis with microscopy is the first test ordered on noting an abnormal serum creatinine, most hospitalists rely on the results generated by a laboratory technician. Anecdotally, many nephrologists have noted significant differences between urinalysis results performed by technicians and results found by nephrologists.
Methods: This study enrolled 26 patients hospitalized with acute renal failure on whom nephrology consultation was obtained. Urinalysis was performed both by laboratory personnel and a nephrologist (nephrologist A) who was blinded to the patient’s clinical information. Both sets of urinalysis results were independently used by nephrologist A and a second nephrologist (nephrologist B) to arrive at a clinical diagnosis for the patient, without having access to any other clinical information. These diagnoses were compared to the final diagnosis determined by the consulting nephrology service, who themselves did not have access to the diagnosis of either nephrologist A or B.
Results: The influence of having a nephrologist perform and interpret the urinalysis was striking. Nephrologist A was able to correctly diagnose 92.3% of cases based solely on his interpretation of the urinalysis. However, when given only the laboratory report of the urinalysis, both nephrologists were unable to diagnose most cases (23.1% for nephrologist A and 19.2% for nephrologist B). The major difference appeared to be in nephrologist A’s ability to find renal tubular epithelial (RTE) cells and RTE casts, which are pathognomonic of ATN. RTE cells and granular casts were frequently misinterpreted as squamous epithelial cells by laboratory personnel. This was particularly important as 81% of patients in the study had ATN as the primary cause of renal failure. Acanthocytes (dysmorphic red blood cells) were also missed by laboratory personnel in all six patients who were subsequently diagnosed with glomerulonephritis; nephrologist A correctly noted acanthocytes in five of these patients, and arrived at the correct diagnosis in all six patients.
Discussion: Microscopic evaluation of urine sediment has become a lost art among physicians, especially since passage of the Clinical Laboratory Improvement Amendments (CLIA) in 1988, which mandated that only CLIA-certified personnel could perform most laboratory tests. While it is probably unrealistic to call for training in microscopic urinalysis for all physicians, hospitalists in particular would benefit from such training, and at the very least should be mindful that laboratory urinalysis results may miss subtle findings that can be invaluable in diagnosing acute renal failure. This study points out the need for greater oversight and training of laboratory personnel, and serves as a reminder to clinicians that laboratory results should not be considered the gold standard. TH
Rothschild JM, Landrigan CP, Cronin JW, et al. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694-1700.
Background: Critically ill patients require complex, immediate, high-intensity care, potentially placing them at increased risk of iatrogenic injury. The frequency and nature of adverse events and errors in the modern ICU have not been clearly defined.
Methods: Harvard researchers conducted a prospective, one-year, observational study of a MICU and a CCU at a tertiary care medical center. Adverse events and medical errors were identified by a four-pronged approach: direct 24-hour observation of interns, voluntary incident reporting, a computerized adverse drug event monitoring system, and chart abstraction. Two physicians independently assessed the type, severity, and preventability of the incidents.
Results: A total of 391 patients comprising 1,490 patient-days were observed and included. Twenty percent of all patients suffered an adverse event, 45% of which were preventable and 13% of which were felt to be life-threatening. There were 223 serious errors (those that caused harm or had the potential to cause harm) observed of which 11% were life threatening. Medication adverse events and medication errors accounted for a large proportion of the incidents during the study. Slips and lapses in care were much more common than rule-based (such as using the wrong protocol) or knowledge-based mistakes.
Discussion: Since the Institute of Medicine report in 1999, there has been an increasing focus on patient safety in the inpatient setting. Based on the results of this study and others, it appears the high-intensity, fast-paced nature of critical care places patients at substantial risk for iatrogenic injury. Up to 20% of patients admitted to the ICU in this study suffered an adverse event or a medical error, which translates into 0.8 adverse events and 1.5 serious medical errors per day in a 10-bed ICU.
Because failure to carry out intended plans (usually secondary to slips and lapses on the part of healthcare providers) was the most common cause of adverse events and errors, the authors address possible solutions. They propose employing computerized-order entry, clinical pharmacists in the ICU, closed ICU staffing, “smart” intravenous pumps, and improved teamwork and communication among healthcare providers. Hospitalists often manage critically ill patients and should be aware of the high risk of medical errors and should consider implementing specific systems changes to mitigate the risk.
The Value of Obtaining Blood Cultures in Pneumonia Pts
Kennedy M, Bates DW, Wright SB, et al. Do emergency department blood cultures change practice in patients with pneumonia? Ann Emerg Med. 2005 Nov;46(5):393-400.
Background: Previous observational studies in patients hospitalized with community-acquired pneumonia (CAP) have shown obtaining blood cultures may have a mortality benefit. This practice has become expert guideline-recommended, the standard of care, as well as a quality marker in the management of CAP. Several recent studies have questioned the utility and cost-effectiveness of this practice.
Methods: Harvard researchers performed a prospective, observational, cohort study of adults admitted to an urban university medical center. Researchers identified patients who had all of the following: clinical CAP, radiographic CAP, and blood cultures at admission. Blood cultures were classified as positive, negative, or contaminated based on previously established criteria. Data were collected on antimicrobial sensitivities, empiric antibiotic choices, and antibiotic changes.
Results: In one year, 414 patients with clinical and radiographic CAP had blood cultures at the time of admission. Twenty-nine of 414 (7%) of patients had true bacteremia while 25 of 414 (6%) had contaminants. Antibiotic therapy was altered in response to blood culture results in 15 of 414 patients (3.6%), of which 11 (2.7%) had therapy narrowed and four (1.0%) had therapy broadened. Of the 11 patients with bacteremia whose therapy was not changed, culture results supported narrowing therapy in eight cases but this was not done.
Discussion: This well done prospective observational study adds to a growing body of evidence questioning the utility of routine blood cultures on all patients hospitalized with CAP. The argument traditionally has been made that blood cultures allow clinicians to narrow or broaden antibiotics based on sensitivities. Yet, empiric therapy was broadened in response to bacteremia in only a small fraction of patients (1%) and in only 11 of 19 patients was therapy appropriately narrowed based on the blood cultures. The study did not measure the impact of blood cultures on clinical outcomes, but these striking results reveal that routine blood cultures rarely alter our management of hospitalized patients with CAP.
Further, many have argued obtaining routine blood cultures in CAP can have negative consequences. Blood cultures are relatively costly and time intensive, contaminated blood cultures can lead to repeated testing and increased length of stay, and delays in obtaining blood cultures can delay antibiotic administration, another important quality marker in CAP. For now, it remains the standard of care to obtain blood cultures in these patients, but hospitalists should be aware of the limitations of this practice and consider focusing on other clinical interventions and quality measures in CAP.
A Review Study: A Dyspneic Emergency Patient
Wang CS, FitzGerald JM, Schulzer M, et al. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005 Oct 19;294:944-1956.
Background: Distinguishing CHF from non-cardiac causes of dyspnea is a major challenge for hospitalists and emergency physicians, particularly in patients with a prior history of cardiac disease. Traditionally, clinicians have relied on the history, physical examination, and basic tests (chest X-ray and electrocardiogram) to diagnose CHF, but rapid B-type natriuretic peptide (BNP) testing is now widely incorporated as well.
A previous article in the Rational Clinical Examination series (Can the clinical examination diagnose left-sided heart failure in adults? JAMA. 1997;277(21):1712-1719) found that systolic dysfunction was moderately well predicted by an abnormal apical impulse on physical examination, radiographic cardiomegaly or venous redistribution, or electrocardiographic q waves or left bundle branch block.
Methods: In this review, the authors update and extend previous findings by also assessing the utility of serum BNP testing. The authors identified articles evaluating the diagnostic accuracy of the clinical exam and laboratory testing in diagnosing CHF in patients presenting to the emergency department with undifferentiated dyspnea. The “gold standard” was a clinical diagnosis of CHF made by the treating clinicians after an appropriate diagnostic workup. Summary likelihood ratios (LRs) were calculated using meta-analytic methodology.
Results/discussion: The authors determined that several findings increase the probability of CHF. A prior history of CHF (LR 5.8, CI 4.1-8.0) or myocardial infarction (LR 3.1, 95% CI 2.0-4.9), symptoms of paroxysmal nocturnal dyspnea (LR 2.6, 95% CI 1.5-4.5) and orthopnea (LR 2.2, 95% CI 1.2-3.9) were the most predictive historical factors. On physical examination, the presence of an S3 (LR 11, 95% CI 4.9-25), jugular venous distension (5.1, 95% CI 3.2-7.9), lung rales (LR 2.8, 95% CI 1.9-4.1), and peripheral edema (2.3, 95% CI 1.5-3.7) increased the probability of CHF. In interpreting these results, it is helpful to remember that a likelihood ratio of 2 increases the post-test probability by about 15%, and an LR of 5 increases the post-test probability by about 30%. Thus, a prior history of CHF and presence of an S3 or jugular venous distension are the most useful findings. Interestingly, clinician’s gestalt was equally predictive (LR 4.4, 95% CI 1.8-10.0.)
The most useful radiographic findings were venous congestion (LR 12.0, 95% CI 6.8-21) and the presence of cardiomegaly (LR 3.3; 95% CI 2.4-4.7). The single most predictive ECG finding was atrial fibrillation (LR 3.8; 95% CI 2.7-8.8); any abnormality on ECG had an LR of 2.2 (95% CI 1.6-3.1). Serum BNP levels were not more predictive of CHF than the history or physical examination; a BNP of >250 was associated with an LR of 4.6 (95% CI 2.6-8.0).
Few findings markedly decreased the probability of CHF. Here, it is helpful to remember that an LR of 0.5 decreases the post-test probability by about 15%, and an LR of 0.2 decreases the post-test probability by about 30%. With these in mind, the absence of cardiomegaly on CXR significantly changes the post-test probability (LR 0.33; 95% CI 0.23-0.48). A serum BNP level of less than 100pg/ml strongly argues against CHF, with an LR of 0.11 (95% CI 0.07-0.16); this finding lowers the post-test probability of CHF by about 45% compared to the pre-test probability.
In summary, the most useful findings for ruling in CHF in dyspneic emergency department patients were clinical gestalt, a prior history of CHF, findings of an S3 or jugular venous distension, and radiographic findings of venous congestion or cardiomegaly. Absence of radiographic cardiomegaly and a BNP of less than 100pg/ml argue against CHF. These must be interpreted in the context of the clinical pre-test probability of CHF, as none of the findings had likelihood ratios sufficient to be diagnostic of CHF when used individually.
What Should I Wear Today?
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005 Nov; 118(11): 1279-1286.
Background: This study addresses the prototypical everyday clinical dilemma: What should I wear to work?
Methods: Patients and visitors to an outpatient Veterans Affairs internal medicine clinic in South Carolina were shown photographs of male and female physicians in four different styles of dress:
- Professional (male physician wearing white coat with tie, female physician wearing white coat with tailored skirt or trousers);
- Business (suit and tie for male, tailored trouser or skirt for female);
- Surgical (surgical scrubs for both male and female): and
- Casual (jeans and t-shirt or short skirt).
The study was randomized so that male and female respondents viewed photographs of either male or female physicians. Respondents were asked to report how strongly they felt about the importance of their physician’s appearance, and their preference for each style of dress; specifically, respondents were asked which physician was the most trustworthy, which physician they felt most comfortable with for routine examinations and emergencies, and which physician they felt most comfortable discussing psychological, sexual, and social problems with.
Results: Respondents overwhelmingly preferred professional attire for all questions: 76.3% felt most comfortable with a professionally dressed physician for all encounters, with surgical scrubs a distant second (10.2%), ahead of business dress (8.8%). Respondents were also significantly more willing to discuss psychological, sexual, and social problems with a professionally dressed physician. Even for care in an emergency situation, respondents still expressed a significant preference for professional attire over scrubs.
In a logistic regression model, patients who were older, African-American, and had less than a high school education were significantly more likely to prefer professional attire. Interestingly, female respondents who viewed photographs of female physicians placed significantly greater emphasis on physician’s attire than did male respondents.
Discussion: The study is clearly subject to caveats, chiefly that it was conducted at a single VA clinic and that only one aspect of the physician-patient encounter was addressed. Undoubtedly, patient’s preferences were influenced by the popular portrayal of physicians on TV shows. Nevertheless, given that hospitalists typically see older patients with whom they are not familiar, the initial clinical encounter may indeed by influenced by something as simple as wearing a white coat.
UA by Nephrologist Versus Hospital-Based Clinical Labs
Tsai JJ, Yeun JY, Kumar VA, Don BR. Comparison and interpretation of urinalysis performed by a nephrologist versus a hospital-based clinical laboratory. Am J Kidney Dis. 2005 Nov;46(5):820-829.
Background: Distinguishing the correct cause of acute renal failure is a frequent clinical dilemma for hospitalists, particularly diagnosing acute tubular necrosis (ATN), which is the most common cause of in-hospital acute renal failure. Although urinalysis with microscopy is the first test ordered on noting an abnormal serum creatinine, most hospitalists rely on the results generated by a laboratory technician. Anecdotally, many nephrologists have noted significant differences between urinalysis results performed by technicians and results found by nephrologists.
Methods: This study enrolled 26 patients hospitalized with acute renal failure on whom nephrology consultation was obtained. Urinalysis was performed both by laboratory personnel and a nephrologist (nephrologist A) who was blinded to the patient’s clinical information. Both sets of urinalysis results were independently used by nephrologist A and a second nephrologist (nephrologist B) to arrive at a clinical diagnosis for the patient, without having access to any other clinical information. These diagnoses were compared to the final diagnosis determined by the consulting nephrology service, who themselves did not have access to the diagnosis of either nephrologist A or B.
Results: The influence of having a nephrologist perform and interpret the urinalysis was striking. Nephrologist A was able to correctly diagnose 92.3% of cases based solely on his interpretation of the urinalysis. However, when given only the laboratory report of the urinalysis, both nephrologists were unable to diagnose most cases (23.1% for nephrologist A and 19.2% for nephrologist B). The major difference appeared to be in nephrologist A’s ability to find renal tubular epithelial (RTE) cells and RTE casts, which are pathognomonic of ATN. RTE cells and granular casts were frequently misinterpreted as squamous epithelial cells by laboratory personnel. This was particularly important as 81% of patients in the study had ATN as the primary cause of renal failure. Acanthocytes (dysmorphic red blood cells) were also missed by laboratory personnel in all six patients who were subsequently diagnosed with glomerulonephritis; nephrologist A correctly noted acanthocytes in five of these patients, and arrived at the correct diagnosis in all six patients.
Discussion: Microscopic evaluation of urine sediment has become a lost art among physicians, especially since passage of the Clinical Laboratory Improvement Amendments (CLIA) in 1988, which mandated that only CLIA-certified personnel could perform most laboratory tests. While it is probably unrealistic to call for training in microscopic urinalysis for all physicians, hospitalists in particular would benefit from such training, and at the very least should be mindful that laboratory urinalysis results may miss subtle findings that can be invaluable in diagnosing acute renal failure. This study points out the need for greater oversight and training of laboratory personnel, and serves as a reminder to clinicians that laboratory results should not be considered the gold standard. TH
Rothschild JM, Landrigan CP, Cronin JW, et al. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694-1700.
Background: Critically ill patients require complex, immediate, high-intensity care, potentially placing them at increased risk of iatrogenic injury. The frequency and nature of adverse events and errors in the modern ICU have not been clearly defined.
Methods: Harvard researchers conducted a prospective, one-year, observational study of a MICU and a CCU at a tertiary care medical center. Adverse events and medical errors were identified by a four-pronged approach: direct 24-hour observation of interns, voluntary incident reporting, a computerized adverse drug event monitoring system, and chart abstraction. Two physicians independently assessed the type, severity, and preventability of the incidents.
Results: A total of 391 patients comprising 1,490 patient-days were observed and included. Twenty percent of all patients suffered an adverse event, 45% of which were preventable and 13% of which were felt to be life-threatening. There were 223 serious errors (those that caused harm or had the potential to cause harm) observed of which 11% were life threatening. Medication adverse events and medication errors accounted for a large proportion of the incidents during the study. Slips and lapses in care were much more common than rule-based (such as using the wrong protocol) or knowledge-based mistakes.
Discussion: Since the Institute of Medicine report in 1999, there has been an increasing focus on patient safety in the inpatient setting. Based on the results of this study and others, it appears the high-intensity, fast-paced nature of critical care places patients at substantial risk for iatrogenic injury. Up to 20% of patients admitted to the ICU in this study suffered an adverse event or a medical error, which translates into 0.8 adverse events and 1.5 serious medical errors per day in a 10-bed ICU.
Because failure to carry out intended plans (usually secondary to slips and lapses on the part of healthcare providers) was the most common cause of adverse events and errors, the authors address possible solutions. They propose employing computerized-order entry, clinical pharmacists in the ICU, closed ICU staffing, “smart” intravenous pumps, and improved teamwork and communication among healthcare providers. Hospitalists often manage critically ill patients and should be aware of the high risk of medical errors and should consider implementing specific systems changes to mitigate the risk.
The Value of Obtaining Blood Cultures in Pneumonia Pts
Kennedy M, Bates DW, Wright SB, et al. Do emergency department blood cultures change practice in patients with pneumonia? Ann Emerg Med. 2005 Nov;46(5):393-400.
Background: Previous observational studies in patients hospitalized with community-acquired pneumonia (CAP) have shown obtaining blood cultures may have a mortality benefit. This practice has become expert guideline-recommended, the standard of care, as well as a quality marker in the management of CAP. Several recent studies have questioned the utility and cost-effectiveness of this practice.
Methods: Harvard researchers performed a prospective, observational, cohort study of adults admitted to an urban university medical center. Researchers identified patients who had all of the following: clinical CAP, radiographic CAP, and blood cultures at admission. Blood cultures were classified as positive, negative, or contaminated based on previously established criteria. Data were collected on antimicrobial sensitivities, empiric antibiotic choices, and antibiotic changes.
Results: In one year, 414 patients with clinical and radiographic CAP had blood cultures at the time of admission. Twenty-nine of 414 (7%) of patients had true bacteremia while 25 of 414 (6%) had contaminants. Antibiotic therapy was altered in response to blood culture results in 15 of 414 patients (3.6%), of which 11 (2.7%) had therapy narrowed and four (1.0%) had therapy broadened. Of the 11 patients with bacteremia whose therapy was not changed, culture results supported narrowing therapy in eight cases but this was not done.
Discussion: This well done prospective observational study adds to a growing body of evidence questioning the utility of routine blood cultures on all patients hospitalized with CAP. The argument traditionally has been made that blood cultures allow clinicians to narrow or broaden antibiotics based on sensitivities. Yet, empiric therapy was broadened in response to bacteremia in only a small fraction of patients (1%) and in only 11 of 19 patients was therapy appropriately narrowed based on the blood cultures. The study did not measure the impact of blood cultures on clinical outcomes, but these striking results reveal that routine blood cultures rarely alter our management of hospitalized patients with CAP.
Further, many have argued obtaining routine blood cultures in CAP can have negative consequences. Blood cultures are relatively costly and time intensive, contaminated blood cultures can lead to repeated testing and increased length of stay, and delays in obtaining blood cultures can delay antibiotic administration, another important quality marker in CAP. For now, it remains the standard of care to obtain blood cultures in these patients, but hospitalists should be aware of the limitations of this practice and consider focusing on other clinical interventions and quality measures in CAP.
A Review Study: A Dyspneic Emergency Patient
Wang CS, FitzGerald JM, Schulzer M, et al. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005 Oct 19;294:944-1956.
Background: Distinguishing CHF from non-cardiac causes of dyspnea is a major challenge for hospitalists and emergency physicians, particularly in patients with a prior history of cardiac disease. Traditionally, clinicians have relied on the history, physical examination, and basic tests (chest X-ray and electrocardiogram) to diagnose CHF, but rapid B-type natriuretic peptide (BNP) testing is now widely incorporated as well.
A previous article in the Rational Clinical Examination series (Can the clinical examination diagnose left-sided heart failure in adults? JAMA. 1997;277(21):1712-1719) found that systolic dysfunction was moderately well predicted by an abnormal apical impulse on physical examination, radiographic cardiomegaly or venous redistribution, or electrocardiographic q waves or left bundle branch block.
Methods: In this review, the authors update and extend previous findings by also assessing the utility of serum BNP testing. The authors identified articles evaluating the diagnostic accuracy of the clinical exam and laboratory testing in diagnosing CHF in patients presenting to the emergency department with undifferentiated dyspnea. The “gold standard” was a clinical diagnosis of CHF made by the treating clinicians after an appropriate diagnostic workup. Summary likelihood ratios (LRs) were calculated using meta-analytic methodology.
Results/discussion: The authors determined that several findings increase the probability of CHF. A prior history of CHF (LR 5.8, CI 4.1-8.0) or myocardial infarction (LR 3.1, 95% CI 2.0-4.9), symptoms of paroxysmal nocturnal dyspnea (LR 2.6, 95% CI 1.5-4.5) and orthopnea (LR 2.2, 95% CI 1.2-3.9) were the most predictive historical factors. On physical examination, the presence of an S3 (LR 11, 95% CI 4.9-25), jugular venous distension (5.1, 95% CI 3.2-7.9), lung rales (LR 2.8, 95% CI 1.9-4.1), and peripheral edema (2.3, 95% CI 1.5-3.7) increased the probability of CHF. In interpreting these results, it is helpful to remember that a likelihood ratio of 2 increases the post-test probability by about 15%, and an LR of 5 increases the post-test probability by about 30%. Thus, a prior history of CHF and presence of an S3 or jugular venous distension are the most useful findings. Interestingly, clinician’s gestalt was equally predictive (LR 4.4, 95% CI 1.8-10.0.)
The most useful radiographic findings were venous congestion (LR 12.0, 95% CI 6.8-21) and the presence of cardiomegaly (LR 3.3; 95% CI 2.4-4.7). The single most predictive ECG finding was atrial fibrillation (LR 3.8; 95% CI 2.7-8.8); any abnormality on ECG had an LR of 2.2 (95% CI 1.6-3.1). Serum BNP levels were not more predictive of CHF than the history or physical examination; a BNP of >250 was associated with an LR of 4.6 (95% CI 2.6-8.0).
Few findings markedly decreased the probability of CHF. Here, it is helpful to remember that an LR of 0.5 decreases the post-test probability by about 15%, and an LR of 0.2 decreases the post-test probability by about 30%. With these in mind, the absence of cardiomegaly on CXR significantly changes the post-test probability (LR 0.33; 95% CI 0.23-0.48). A serum BNP level of less than 100pg/ml strongly argues against CHF, with an LR of 0.11 (95% CI 0.07-0.16); this finding lowers the post-test probability of CHF by about 45% compared to the pre-test probability.
In summary, the most useful findings for ruling in CHF in dyspneic emergency department patients were clinical gestalt, a prior history of CHF, findings of an S3 or jugular venous distension, and radiographic findings of venous congestion or cardiomegaly. Absence of radiographic cardiomegaly and a BNP of less than 100pg/ml argue against CHF. These must be interpreted in the context of the clinical pre-test probability of CHF, as none of the findings had likelihood ratios sufficient to be diagnostic of CHF when used individually.
What Should I Wear Today?
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005 Nov; 118(11): 1279-1286.
Background: This study addresses the prototypical everyday clinical dilemma: What should I wear to work?
Methods: Patients and visitors to an outpatient Veterans Affairs internal medicine clinic in South Carolina were shown photographs of male and female physicians in four different styles of dress:
- Professional (male physician wearing white coat with tie, female physician wearing white coat with tailored skirt or trousers);
- Business (suit and tie for male, tailored trouser or skirt for female);
- Surgical (surgical scrubs for both male and female): and
- Casual (jeans and t-shirt or short skirt).
The study was randomized so that male and female respondents viewed photographs of either male or female physicians. Respondents were asked to report how strongly they felt about the importance of their physician’s appearance, and their preference for each style of dress; specifically, respondents were asked which physician was the most trustworthy, which physician they felt most comfortable with for routine examinations and emergencies, and which physician they felt most comfortable discussing psychological, sexual, and social problems with.
Results: Respondents overwhelmingly preferred professional attire for all questions: 76.3% felt most comfortable with a professionally dressed physician for all encounters, with surgical scrubs a distant second (10.2%), ahead of business dress (8.8%). Respondents were also significantly more willing to discuss psychological, sexual, and social problems with a professionally dressed physician. Even for care in an emergency situation, respondents still expressed a significant preference for professional attire over scrubs.
In a logistic regression model, patients who were older, African-American, and had less than a high school education were significantly more likely to prefer professional attire. Interestingly, female respondents who viewed photographs of female physicians placed significantly greater emphasis on physician’s attire than did male respondents.
Discussion: The study is clearly subject to caveats, chiefly that it was conducted at a single VA clinic and that only one aspect of the physician-patient encounter was addressed. Undoubtedly, patient’s preferences were influenced by the popular portrayal of physicians on TV shows. Nevertheless, given that hospitalists typically see older patients with whom they are not familiar, the initial clinical encounter may indeed by influenced by something as simple as wearing a white coat.
UA by Nephrologist Versus Hospital-Based Clinical Labs
Tsai JJ, Yeun JY, Kumar VA, Don BR. Comparison and interpretation of urinalysis performed by a nephrologist versus a hospital-based clinical laboratory. Am J Kidney Dis. 2005 Nov;46(5):820-829.
Background: Distinguishing the correct cause of acute renal failure is a frequent clinical dilemma for hospitalists, particularly diagnosing acute tubular necrosis (ATN), which is the most common cause of in-hospital acute renal failure. Although urinalysis with microscopy is the first test ordered on noting an abnormal serum creatinine, most hospitalists rely on the results generated by a laboratory technician. Anecdotally, many nephrologists have noted significant differences between urinalysis results performed by technicians and results found by nephrologists.
Methods: This study enrolled 26 patients hospitalized with acute renal failure on whom nephrology consultation was obtained. Urinalysis was performed both by laboratory personnel and a nephrologist (nephrologist A) who was blinded to the patient’s clinical information. Both sets of urinalysis results were independently used by nephrologist A and a second nephrologist (nephrologist B) to arrive at a clinical diagnosis for the patient, without having access to any other clinical information. These diagnoses were compared to the final diagnosis determined by the consulting nephrology service, who themselves did not have access to the diagnosis of either nephrologist A or B.
Results: The influence of having a nephrologist perform and interpret the urinalysis was striking. Nephrologist A was able to correctly diagnose 92.3% of cases based solely on his interpretation of the urinalysis. However, when given only the laboratory report of the urinalysis, both nephrologists were unable to diagnose most cases (23.1% for nephrologist A and 19.2% for nephrologist B). The major difference appeared to be in nephrologist A’s ability to find renal tubular epithelial (RTE) cells and RTE casts, which are pathognomonic of ATN. RTE cells and granular casts were frequently misinterpreted as squamous epithelial cells by laboratory personnel. This was particularly important as 81% of patients in the study had ATN as the primary cause of renal failure. Acanthocytes (dysmorphic red blood cells) were also missed by laboratory personnel in all six patients who were subsequently diagnosed with glomerulonephritis; nephrologist A correctly noted acanthocytes in five of these patients, and arrived at the correct diagnosis in all six patients.
Discussion: Microscopic evaluation of urine sediment has become a lost art among physicians, especially since passage of the Clinical Laboratory Improvement Amendments (CLIA) in 1988, which mandated that only CLIA-certified personnel could perform most laboratory tests. While it is probably unrealistic to call for training in microscopic urinalysis for all physicians, hospitalists in particular would benefit from such training, and at the very least should be mindful that laboratory urinalysis results may miss subtle findings that can be invaluable in diagnosing acute renal failure. This study points out the need for greater oversight and training of laboratory personnel, and serves as a reminder to clinicians that laboratory results should not be considered the gold standard. TH
Postdischarge Test Results, Acute Renal Failure, Diagnosing PE
Roy PM, Colombet I, Durieux P, et al. Systemic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ.2005;331:259.
Background: Despite technological advances, the diagnosis of pulmonary embolism remains challenging. A large number of diagnostic tests and strategies have been evaluated and yet the test characteristics of each and their practical use remain unclear.
Methods: Pierre-Marie Roy, MD and colleagues carried out a systematic review and meta-analysis to define the likelihood ratios (LRs) for different diagnostic modalities for pulmonary embolism and provide a simple, evidence-based diagnostic algorithm.
The authors performed a literature search from 1990-2003 identifying all articles that evaluated tests or strategies aimed at diagnosing pulmonary embolism. They only selected papers which were prospective, in which participants were recruited consecutively, and which pulmonary angiography was the reference standard for strategies to confirm pulmonary embolism and clinical follow-up or angiography were used for exclusion strategies.
Results: Forty-eight articles (11,004 patients) met the inclusion criteria and examined ventilation/perfusion (V/Q) lung scanning, computed tomography (CT) angiography, leg vein ultrasound (U/S), echocardiography, magnetic resonance (MR) angiography, and the D-dimer test. For the studies done to evaluate tests to confirm the diagnosis of pulmonary embolism, pooled positive likelihood ratios (+LRs) were calculated and were:
For the studies evaluating tests to exclude the diagnosis of pulmonary embolism, pooled negative likelihood ratios (-LR) were calculated and were:
Discussion: With the pooled positive and negative LRs, Roy and colleagues created a diagnostic algorithm, based on initial pretest probabilities, to help “rule in” and “rule out” the diagnosis of pulmonary embolism. Consistent with prior studies, a calculated post-test probability of >85% confirmed the diagnosis while a post-test probability <5% excluded PE.
In patients with a low or moderate pretest probability, pulmonary embolism is adequately excluded in patients with either 1) negative D-dimers or 2) a normal V/Q scan or 3) a negative CT angiogram in combination with a normal venous ultrasound. In patients with moderate or high pre-test probability, pulmonary embolism is confirmed by either 1) a high-probability V/Q scan or 2) a positive CT angiogram or 3) a positive venous ultrasound. Low-probability V/Q scanning, CT angiogram alone, and MR angiography have higher negative likelihood ratios and can only exclude PE in patients with low pre-test probability.
Many hospitalists are using CT angiography as their sole diagnostic test for pulmonary embolism. Based on the systematic review and meta-analysis by Roy and colleagues, we should proceed with caution as, in some patient populations, a positive or negative “spiral CT” does not adequately confirm or exclude the diagnosis of pulmonary embolism. For those that employ V/Q scanning, MR angiography, or D-dimers, the study also helps define how best to use these tests.
Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest. 2005;128:489.
Background: In recent years, peripherally inserted central catheters (PICCs) have become more popular, initially for long-term outpatient intravenous therapy but also for inpatient venous access. Traditionally, it was assumed that PICC lines have a lower rate of catheter-related bloodstream infection than conventional central venous catheters (CVCs) placed in the internal jugular, subclavian, or femoral veins.
Methods: One academic medical center prospectively studied the rate of catheter-related bloodstream infection in PICC lines used exclusively in hospitalized patients as part of two trials assessing efficacy of different skin antiseptics. PICC-related bloodstream infection was confirmed when organisms isolated from positive blood cultures matched (by DNA subtyping) organisms isolated from culturing the PICC line at the time of removal. The authors also performed a systematic review of the literature to provide overall estimates of PICC-related bloodstream infection in hospitalized patients.
Results: A total of 115 patients received 251 PICC lines during the study period and the mean duration of catheterization was 11.3 days. More than 40% of the patients were in the intensive care unit (ICU) and most had risk factors for the development of bloodstream infection, including urinary catheterization, mechanical ventilation, prior antibiotic use, and low albumin. Six cases (2.4%) of PICC-related bloodstream infection were confirmed, four with coagulase-negative staphylococcus, one with S. aureus, and one with Klebsiella pneumoniae, a rate of 2.1 per 1,000 catheter-days. In their systematic review, the authors identified 14 studies evaluating the rate of PICC-related bloodstream infection in hospitalized patients; the pooled rate was 1.9 per 1,000 catheter-days.
Discussion: In a small but methodologically sound prospective study and systematic review, Safdar and Maki found a surprisingly high rate of PICC-related bloodstream infection in hospitalized patients. Their calculated rate of 2.1 cases per 1,000 catheter-days is five times the rate seen in PICCs used exclusively in outpatients (0.4 per 1,000 catheter-days). More strikingly, 2.1 cases per 1,000 catheter-days is similar to the rate of catheter-related bloodstream infection in conventional central venous catheters placed in the subclavian or internal jugular veins (two to five per 1,000 catheter-days). Unfortunately, the study didn’t assess the rate of mechanical complications associated with PICC lines or correlate the risk of infection with duration of catheterization.
Hospitalists should be aware that PICC lines likely have the same infection risk as subclavian and internal jugular lines in hospitalized patients and a much higher rate of infection than PICC lines in outpatients. The higher-than-expected rates are likely related to the increased prevalence of risk factors for bloodstream infection in hospitalized patients. Thus, the decision to use PICC lines in hospitalized patients should be made based on factors other than presumed lower infection risk.
Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients. A multinational, multicenter study. JAMA. 2005;294:813.
Background: Acute renal failure in critically ill patients is believed common and is associated with a high mortality. The exact prevalence and the calculated risk of death have not been clearly defined across populations.
Methods: A multinational group of investigators conducted a massive prospective observational study of ICU patients who developed renal failure after ICU admission. The study encompassed 54 hospitals in 23 countries with a total of 29,269 admissions over the 14-month study period. Note, acute renal failure was defined as either oliguria (urine output <200cc/12 hours) or BUN >84mg/dL.
Results: Of all ICU patients studied, 5.7% developed acute renal failure after admission and 4.7% of patients received renal replacement therapy (most often continuous replacement). The most common contributing factor to the development of acute renal failure was septic shock (48%), followed by major surgery (34%) and cardiogenic shock (26%). Up to 19% of the cases of acute renal failure were estimated to be drug-related. The in-hospital mortality for critically ill patients with acute renal failure was 60%, which was substantially higher than the mortality estimated by other physiologic scoring systems (45% mortality according to SAPS II). Of those who survived to hospital discharge, only 14% required ongoing hemodialysis.
Discussion: This large, multinational, multicenter prospective observational study helps better define the prevalence and characteristic of acute renal failure that develops in critically ill patients. Overall, acute renal failure in the ICU setting is relatively uncommon, is most often caused by septic shock, and typically does require renal replacement therapy. There was a surprisingly high rate of acute renal failure thought to be secondary to medication or drug effect (19%).
The mortality in patients who develop renal failure in the ICU is high but, surprisingly, if patients survive, they are unlikely to need long-term hemodialysis. The study is limited in that it was not randomized and outcomes associated with particular interventions could not be determined. Yet, the data adds to our understanding of acute renal failure in the ICU and knowledge of the prevalence and expected outcomes could potentially help with prognosis and end-of-life discussions in the intensive care unit.
Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143:121.
Background: Adequate communication between hospitalists and outpatient providers is essential to patient safety as well as patient and physician satisfaction. It is estimated that more than half of all preventable adverse events occurring soon after hospital discharge have been related to poor communication among providers. With increasing pressure to limit inpatient length of stay, patients are often discharged with numerous laboratory or radiologic test results pending.
Methods: Roy and colleagues at a tertiary care academic medical center prospectively determined the prevalence and characteristics of tests pending at discharge and assessed physician awareness as well as satisfaction. All patients discharged from two hospitalist services over four months in 2004 were followed. Researchers identified all pending test results for these patients and all abnormal tests were reviewed by study physicians and judged to be “potentially actionable” or not (if it could change the management of the patient by requiring a new treatment or diagnostic test, change in a treatment, scheduling of an earlier follow-up, etc).
Results: Of the 2,644 patients discharged, 1,095 (41%) had laboratory or radiographic tests pending. Approximately 43% of all pending tests were abnormal and ~10% of the pending tests were judged by physician-reviewers to be potentially actionable. Examples include a TSH that returned as <0.01 mU/mL after discharge in a patient with new atrial fibrillation, or a urine culture that grew an organism resistant to the antibiotics given at discharge. Of note, outpatient physicians were unaware of two-thirds of the “potentially actionable” results. Finally, when surveyed, the majority of inpatient physicians were concerned about appropriate follow-up of tests and dissatisfied with the system used.
Discussion: Roy and his coauthors attempted to quantify the prevalence of potentially actionable laboratory tests available after discharge and published rather striking findings. Up to half of all patients have some tests pending at discharge and up to 10% of these require some physician action. More frighteningly, outpatient MDs are generally unaware of these tests creating a huge gap in patient safety in the transition back to outpatient care.
How can we do this better? SHM and the Society for General Internal Medicine have convened a Continuity of Care Task Force and found poor communication with outpatient providers was a common and potentially dangerous problem. They outlined the best practices for the discharge of patients to ensure safety as well as maximize patient and physician satisfaction. Their recommendations are available on the SHM Web site. All hospitalists and institutions should be aware of the potential for missed results and put systems in place, electronic and otherwise, to create an appropriate safety net for our discharged patients.
Sharma R, Loomis W, Brown RB. Impact of mandatory inpatient infectious disease consultation on outpatient parenteral antibiotic therapy. Am J Med Sci. 2005;330(2):60.
Background: As the pressure to limit healthcare costs by reducing inpatient length of stay has increased, the use of outpatient parenteral antibiotic therapy has grown. When employed appropriately, home intravenous antibiotic therapy has consistently resulted in cost savings without compromising patient outcomes. As with other healthcare advances, there is some fear that outpatient parenteral antibiotic treatment will be overused or misused, limiting the cost savings or putting patients at risk.
Methods: A single academic medical center instituted mandatory infectious disease consultation on all patients referred to discharge coordinators with plans for outpatient IV antibiotic treatment. The infectious disease consultants helped to determine the need for outpatient parenteral therapy and antibiotic choice. All patients were followed for 30 days.
Results: Over the one-year study period, 44 cases received mandatory infectious disease consultation. Thirty-nine (89%) of these had some change in antibiotic regimen after the consultation. Seventeen patients (39%) were switched to oral antibiotics, 13 (30%) had a change in infectious disease antibiotic, and 5 (11%) had a change in antibiotic dose.
Skin and skin structure and intra-abdominal infections were the most common diagnoses for which antibiotics were changed; a typical change was from intravenous piperacillin/tazobactam to an oral fluoroquinolone plus oral anaerobic coverage. At 30-day follow-up, 98% of patients finished their courses without relapse or complication. The overall costs savings was $27,500 or $1,550 per patient consulted upon.
Discussion: Although from a small, nonrandomized, single-institution study, the results are impressive. Mandatory infectious disease consultation prior to discharge for patients scheduled to received outpatient parenteral antibiotic therapy resulted in substantial cost savings, and streamlined and more appropriate antibiotic regimens without any adverse impact on outcomes. Hospitalists should take two things away from this study: 1) consider consulting infection disease specialists on all patients who might be candidates for home IV antibiotics and 2) be aware that many skin and skin tissue and intra-abdominal infections can often be treated with oral therapy. TH
Roy PM, Colombet I, Durieux P, et al. Systemic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ.2005;331:259.
Background: Despite technological advances, the diagnosis of pulmonary embolism remains challenging. A large number of diagnostic tests and strategies have been evaluated and yet the test characteristics of each and their practical use remain unclear.
Methods: Pierre-Marie Roy, MD and colleagues carried out a systematic review and meta-analysis to define the likelihood ratios (LRs) for different diagnostic modalities for pulmonary embolism and provide a simple, evidence-based diagnostic algorithm.
The authors performed a literature search from 1990-2003 identifying all articles that evaluated tests or strategies aimed at diagnosing pulmonary embolism. They only selected papers which were prospective, in which participants were recruited consecutively, and which pulmonary angiography was the reference standard for strategies to confirm pulmonary embolism and clinical follow-up or angiography were used for exclusion strategies.
Results: Forty-eight articles (11,004 patients) met the inclusion criteria and examined ventilation/perfusion (V/Q) lung scanning, computed tomography (CT) angiography, leg vein ultrasound (U/S), echocardiography, magnetic resonance (MR) angiography, and the D-dimer test. For the studies done to evaluate tests to confirm the diagnosis of pulmonary embolism, pooled positive likelihood ratios (+LRs) were calculated and were:
For the studies evaluating tests to exclude the diagnosis of pulmonary embolism, pooled negative likelihood ratios (-LR) were calculated and were:
Discussion: With the pooled positive and negative LRs, Roy and colleagues created a diagnostic algorithm, based on initial pretest probabilities, to help “rule in” and “rule out” the diagnosis of pulmonary embolism. Consistent with prior studies, a calculated post-test probability of >85% confirmed the diagnosis while a post-test probability <5% excluded PE.
In patients with a low or moderate pretest probability, pulmonary embolism is adequately excluded in patients with either 1) negative D-dimers or 2) a normal V/Q scan or 3) a negative CT angiogram in combination with a normal venous ultrasound. In patients with moderate or high pre-test probability, pulmonary embolism is confirmed by either 1) a high-probability V/Q scan or 2) a positive CT angiogram or 3) a positive venous ultrasound. Low-probability V/Q scanning, CT angiogram alone, and MR angiography have higher negative likelihood ratios and can only exclude PE in patients with low pre-test probability.
Many hospitalists are using CT angiography as their sole diagnostic test for pulmonary embolism. Based on the systematic review and meta-analysis by Roy and colleagues, we should proceed with caution as, in some patient populations, a positive or negative “spiral CT” does not adequately confirm or exclude the diagnosis of pulmonary embolism. For those that employ V/Q scanning, MR angiography, or D-dimers, the study also helps define how best to use these tests.
Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest. 2005;128:489.
Background: In recent years, peripherally inserted central catheters (PICCs) have become more popular, initially for long-term outpatient intravenous therapy but also for inpatient venous access. Traditionally, it was assumed that PICC lines have a lower rate of catheter-related bloodstream infection than conventional central venous catheters (CVCs) placed in the internal jugular, subclavian, or femoral veins.
Methods: One academic medical center prospectively studied the rate of catheter-related bloodstream infection in PICC lines used exclusively in hospitalized patients as part of two trials assessing efficacy of different skin antiseptics. PICC-related bloodstream infection was confirmed when organisms isolated from positive blood cultures matched (by DNA subtyping) organisms isolated from culturing the PICC line at the time of removal. The authors also performed a systematic review of the literature to provide overall estimates of PICC-related bloodstream infection in hospitalized patients.
Results: A total of 115 patients received 251 PICC lines during the study period and the mean duration of catheterization was 11.3 days. More than 40% of the patients were in the intensive care unit (ICU) and most had risk factors for the development of bloodstream infection, including urinary catheterization, mechanical ventilation, prior antibiotic use, and low albumin. Six cases (2.4%) of PICC-related bloodstream infection were confirmed, four with coagulase-negative staphylococcus, one with S. aureus, and one with Klebsiella pneumoniae, a rate of 2.1 per 1,000 catheter-days. In their systematic review, the authors identified 14 studies evaluating the rate of PICC-related bloodstream infection in hospitalized patients; the pooled rate was 1.9 per 1,000 catheter-days.
Discussion: In a small but methodologically sound prospective study and systematic review, Safdar and Maki found a surprisingly high rate of PICC-related bloodstream infection in hospitalized patients. Their calculated rate of 2.1 cases per 1,000 catheter-days is five times the rate seen in PICCs used exclusively in outpatients (0.4 per 1,000 catheter-days). More strikingly, 2.1 cases per 1,000 catheter-days is similar to the rate of catheter-related bloodstream infection in conventional central venous catheters placed in the subclavian or internal jugular veins (two to five per 1,000 catheter-days). Unfortunately, the study didn’t assess the rate of mechanical complications associated with PICC lines or correlate the risk of infection with duration of catheterization.
Hospitalists should be aware that PICC lines likely have the same infection risk as subclavian and internal jugular lines in hospitalized patients and a much higher rate of infection than PICC lines in outpatients. The higher-than-expected rates are likely related to the increased prevalence of risk factors for bloodstream infection in hospitalized patients. Thus, the decision to use PICC lines in hospitalized patients should be made based on factors other than presumed lower infection risk.
Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients. A multinational, multicenter study. JAMA. 2005;294:813.
Background: Acute renal failure in critically ill patients is believed common and is associated with a high mortality. The exact prevalence and the calculated risk of death have not been clearly defined across populations.
Methods: A multinational group of investigators conducted a massive prospective observational study of ICU patients who developed renal failure after ICU admission. The study encompassed 54 hospitals in 23 countries with a total of 29,269 admissions over the 14-month study period. Note, acute renal failure was defined as either oliguria (urine output <200cc/12 hours) or BUN >84mg/dL.
Results: Of all ICU patients studied, 5.7% developed acute renal failure after admission and 4.7% of patients received renal replacement therapy (most often continuous replacement). The most common contributing factor to the development of acute renal failure was septic shock (48%), followed by major surgery (34%) and cardiogenic shock (26%). Up to 19% of the cases of acute renal failure were estimated to be drug-related. The in-hospital mortality for critically ill patients with acute renal failure was 60%, which was substantially higher than the mortality estimated by other physiologic scoring systems (45% mortality according to SAPS II). Of those who survived to hospital discharge, only 14% required ongoing hemodialysis.
Discussion: This large, multinational, multicenter prospective observational study helps better define the prevalence and characteristic of acute renal failure that develops in critically ill patients. Overall, acute renal failure in the ICU setting is relatively uncommon, is most often caused by septic shock, and typically does require renal replacement therapy. There was a surprisingly high rate of acute renal failure thought to be secondary to medication or drug effect (19%).
The mortality in patients who develop renal failure in the ICU is high but, surprisingly, if patients survive, they are unlikely to need long-term hemodialysis. The study is limited in that it was not randomized and outcomes associated with particular interventions could not be determined. Yet, the data adds to our understanding of acute renal failure in the ICU and knowledge of the prevalence and expected outcomes could potentially help with prognosis and end-of-life discussions in the intensive care unit.
Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143:121.
Background: Adequate communication between hospitalists and outpatient providers is essential to patient safety as well as patient and physician satisfaction. It is estimated that more than half of all preventable adverse events occurring soon after hospital discharge have been related to poor communication among providers. With increasing pressure to limit inpatient length of stay, patients are often discharged with numerous laboratory or radiologic test results pending.
Methods: Roy and colleagues at a tertiary care academic medical center prospectively determined the prevalence and characteristics of tests pending at discharge and assessed physician awareness as well as satisfaction. All patients discharged from two hospitalist services over four months in 2004 were followed. Researchers identified all pending test results for these patients and all abnormal tests were reviewed by study physicians and judged to be “potentially actionable” or not (if it could change the management of the patient by requiring a new treatment or diagnostic test, change in a treatment, scheduling of an earlier follow-up, etc).
Results: Of the 2,644 patients discharged, 1,095 (41%) had laboratory or radiographic tests pending. Approximately 43% of all pending tests were abnormal and ~10% of the pending tests were judged by physician-reviewers to be potentially actionable. Examples include a TSH that returned as <0.01 mU/mL after discharge in a patient with new atrial fibrillation, or a urine culture that grew an organism resistant to the antibiotics given at discharge. Of note, outpatient physicians were unaware of two-thirds of the “potentially actionable” results. Finally, when surveyed, the majority of inpatient physicians were concerned about appropriate follow-up of tests and dissatisfied with the system used.
Discussion: Roy and his coauthors attempted to quantify the prevalence of potentially actionable laboratory tests available after discharge and published rather striking findings. Up to half of all patients have some tests pending at discharge and up to 10% of these require some physician action. More frighteningly, outpatient MDs are generally unaware of these tests creating a huge gap in patient safety in the transition back to outpatient care.
How can we do this better? SHM and the Society for General Internal Medicine have convened a Continuity of Care Task Force and found poor communication with outpatient providers was a common and potentially dangerous problem. They outlined the best practices for the discharge of patients to ensure safety as well as maximize patient and physician satisfaction. Their recommendations are available on the SHM Web site. All hospitalists and institutions should be aware of the potential for missed results and put systems in place, electronic and otherwise, to create an appropriate safety net for our discharged patients.
Sharma R, Loomis W, Brown RB. Impact of mandatory inpatient infectious disease consultation on outpatient parenteral antibiotic therapy. Am J Med Sci. 2005;330(2):60.
Background: As the pressure to limit healthcare costs by reducing inpatient length of stay has increased, the use of outpatient parenteral antibiotic therapy has grown. When employed appropriately, home intravenous antibiotic therapy has consistently resulted in cost savings without compromising patient outcomes. As with other healthcare advances, there is some fear that outpatient parenteral antibiotic treatment will be overused or misused, limiting the cost savings or putting patients at risk.
Methods: A single academic medical center instituted mandatory infectious disease consultation on all patients referred to discharge coordinators with plans for outpatient IV antibiotic treatment. The infectious disease consultants helped to determine the need for outpatient parenteral therapy and antibiotic choice. All patients were followed for 30 days.
Results: Over the one-year study period, 44 cases received mandatory infectious disease consultation. Thirty-nine (89%) of these had some change in antibiotic regimen after the consultation. Seventeen patients (39%) were switched to oral antibiotics, 13 (30%) had a change in infectious disease antibiotic, and 5 (11%) had a change in antibiotic dose.
Skin and skin structure and intra-abdominal infections were the most common diagnoses for which antibiotics were changed; a typical change was from intravenous piperacillin/tazobactam to an oral fluoroquinolone plus oral anaerobic coverage. At 30-day follow-up, 98% of patients finished their courses without relapse or complication. The overall costs savings was $27,500 or $1,550 per patient consulted upon.
Discussion: Although from a small, nonrandomized, single-institution study, the results are impressive. Mandatory infectious disease consultation prior to discharge for patients scheduled to received outpatient parenteral antibiotic therapy resulted in substantial cost savings, and streamlined and more appropriate antibiotic regimens without any adverse impact on outcomes. Hospitalists should take two things away from this study: 1) consider consulting infection disease specialists on all patients who might be candidates for home IV antibiotics and 2) be aware that many skin and skin tissue and intra-abdominal infections can often be treated with oral therapy. TH
Roy PM, Colombet I, Durieux P, et al. Systemic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ.2005;331:259.
Background: Despite technological advances, the diagnosis of pulmonary embolism remains challenging. A large number of diagnostic tests and strategies have been evaluated and yet the test characteristics of each and their practical use remain unclear.
Methods: Pierre-Marie Roy, MD and colleagues carried out a systematic review and meta-analysis to define the likelihood ratios (LRs) for different diagnostic modalities for pulmonary embolism and provide a simple, evidence-based diagnostic algorithm.
The authors performed a literature search from 1990-2003 identifying all articles that evaluated tests or strategies aimed at diagnosing pulmonary embolism. They only selected papers which were prospective, in which participants were recruited consecutively, and which pulmonary angiography was the reference standard for strategies to confirm pulmonary embolism and clinical follow-up or angiography were used for exclusion strategies.
Results: Forty-eight articles (11,004 patients) met the inclusion criteria and examined ventilation/perfusion (V/Q) lung scanning, computed tomography (CT) angiography, leg vein ultrasound (U/S), echocardiography, magnetic resonance (MR) angiography, and the D-dimer test. For the studies done to evaluate tests to confirm the diagnosis of pulmonary embolism, pooled positive likelihood ratios (+LRs) were calculated and were:
For the studies evaluating tests to exclude the diagnosis of pulmonary embolism, pooled negative likelihood ratios (-LR) were calculated and were:
Discussion: With the pooled positive and negative LRs, Roy and colleagues created a diagnostic algorithm, based on initial pretest probabilities, to help “rule in” and “rule out” the diagnosis of pulmonary embolism. Consistent with prior studies, a calculated post-test probability of >85% confirmed the diagnosis while a post-test probability <5% excluded PE.
In patients with a low or moderate pretest probability, pulmonary embolism is adequately excluded in patients with either 1) negative D-dimers or 2) a normal V/Q scan or 3) a negative CT angiogram in combination with a normal venous ultrasound. In patients with moderate or high pre-test probability, pulmonary embolism is confirmed by either 1) a high-probability V/Q scan or 2) a positive CT angiogram or 3) a positive venous ultrasound. Low-probability V/Q scanning, CT angiogram alone, and MR angiography have higher negative likelihood ratios and can only exclude PE in patients with low pre-test probability.
Many hospitalists are using CT angiography as their sole diagnostic test for pulmonary embolism. Based on the systematic review and meta-analysis by Roy and colleagues, we should proceed with caution as, in some patient populations, a positive or negative “spiral CT” does not adequately confirm or exclude the diagnosis of pulmonary embolism. For those that employ V/Q scanning, MR angiography, or D-dimers, the study also helps define how best to use these tests.
Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest. 2005;128:489.
Background: In recent years, peripherally inserted central catheters (PICCs) have become more popular, initially for long-term outpatient intravenous therapy but also for inpatient venous access. Traditionally, it was assumed that PICC lines have a lower rate of catheter-related bloodstream infection than conventional central venous catheters (CVCs) placed in the internal jugular, subclavian, or femoral veins.
Methods: One academic medical center prospectively studied the rate of catheter-related bloodstream infection in PICC lines used exclusively in hospitalized patients as part of two trials assessing efficacy of different skin antiseptics. PICC-related bloodstream infection was confirmed when organisms isolated from positive blood cultures matched (by DNA subtyping) organisms isolated from culturing the PICC line at the time of removal. The authors also performed a systematic review of the literature to provide overall estimates of PICC-related bloodstream infection in hospitalized patients.
Results: A total of 115 patients received 251 PICC lines during the study period and the mean duration of catheterization was 11.3 days. More than 40% of the patients were in the intensive care unit (ICU) and most had risk factors for the development of bloodstream infection, including urinary catheterization, mechanical ventilation, prior antibiotic use, and low albumin. Six cases (2.4%) of PICC-related bloodstream infection were confirmed, four with coagulase-negative staphylococcus, one with S. aureus, and one with Klebsiella pneumoniae, a rate of 2.1 per 1,000 catheter-days. In their systematic review, the authors identified 14 studies evaluating the rate of PICC-related bloodstream infection in hospitalized patients; the pooled rate was 1.9 per 1,000 catheter-days.
Discussion: In a small but methodologically sound prospective study and systematic review, Safdar and Maki found a surprisingly high rate of PICC-related bloodstream infection in hospitalized patients. Their calculated rate of 2.1 cases per 1,000 catheter-days is five times the rate seen in PICCs used exclusively in outpatients (0.4 per 1,000 catheter-days). More strikingly, 2.1 cases per 1,000 catheter-days is similar to the rate of catheter-related bloodstream infection in conventional central venous catheters placed in the subclavian or internal jugular veins (two to five per 1,000 catheter-days). Unfortunately, the study didn’t assess the rate of mechanical complications associated with PICC lines or correlate the risk of infection with duration of catheterization.
Hospitalists should be aware that PICC lines likely have the same infection risk as subclavian and internal jugular lines in hospitalized patients and a much higher rate of infection than PICC lines in outpatients. The higher-than-expected rates are likely related to the increased prevalence of risk factors for bloodstream infection in hospitalized patients. Thus, the decision to use PICC lines in hospitalized patients should be made based on factors other than presumed lower infection risk.
Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients. A multinational, multicenter study. JAMA. 2005;294:813.
Background: Acute renal failure in critically ill patients is believed common and is associated with a high mortality. The exact prevalence and the calculated risk of death have not been clearly defined across populations.
Methods: A multinational group of investigators conducted a massive prospective observational study of ICU patients who developed renal failure after ICU admission. The study encompassed 54 hospitals in 23 countries with a total of 29,269 admissions over the 14-month study period. Note, acute renal failure was defined as either oliguria (urine output <200cc/12 hours) or BUN >84mg/dL.
Results: Of all ICU patients studied, 5.7% developed acute renal failure after admission and 4.7% of patients received renal replacement therapy (most often continuous replacement). The most common contributing factor to the development of acute renal failure was septic shock (48%), followed by major surgery (34%) and cardiogenic shock (26%). Up to 19% of the cases of acute renal failure were estimated to be drug-related. The in-hospital mortality for critically ill patients with acute renal failure was 60%, which was substantially higher than the mortality estimated by other physiologic scoring systems (45% mortality according to SAPS II). Of those who survived to hospital discharge, only 14% required ongoing hemodialysis.
Discussion: This large, multinational, multicenter prospective observational study helps better define the prevalence and characteristic of acute renal failure that develops in critically ill patients. Overall, acute renal failure in the ICU setting is relatively uncommon, is most often caused by septic shock, and typically does require renal replacement therapy. There was a surprisingly high rate of acute renal failure thought to be secondary to medication or drug effect (19%).
The mortality in patients who develop renal failure in the ICU is high but, surprisingly, if patients survive, they are unlikely to need long-term hemodialysis. The study is limited in that it was not randomized and outcomes associated with particular interventions could not be determined. Yet, the data adds to our understanding of acute renal failure in the ICU and knowledge of the prevalence and expected outcomes could potentially help with prognosis and end-of-life discussions in the intensive care unit.
Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143:121.
Background: Adequate communication between hospitalists and outpatient providers is essential to patient safety as well as patient and physician satisfaction. It is estimated that more than half of all preventable adverse events occurring soon after hospital discharge have been related to poor communication among providers. With increasing pressure to limit inpatient length of stay, patients are often discharged with numerous laboratory or radiologic test results pending.
Methods: Roy and colleagues at a tertiary care academic medical center prospectively determined the prevalence and characteristics of tests pending at discharge and assessed physician awareness as well as satisfaction. All patients discharged from two hospitalist services over four months in 2004 were followed. Researchers identified all pending test results for these patients and all abnormal tests were reviewed by study physicians and judged to be “potentially actionable” or not (if it could change the management of the patient by requiring a new treatment or diagnostic test, change in a treatment, scheduling of an earlier follow-up, etc).
Results: Of the 2,644 patients discharged, 1,095 (41%) had laboratory or radiographic tests pending. Approximately 43% of all pending tests were abnormal and ~10% of the pending tests were judged by physician-reviewers to be potentially actionable. Examples include a TSH that returned as <0.01 mU/mL after discharge in a patient with new atrial fibrillation, or a urine culture that grew an organism resistant to the antibiotics given at discharge. Of note, outpatient physicians were unaware of two-thirds of the “potentially actionable” results. Finally, when surveyed, the majority of inpatient physicians were concerned about appropriate follow-up of tests and dissatisfied with the system used.
Discussion: Roy and his coauthors attempted to quantify the prevalence of potentially actionable laboratory tests available after discharge and published rather striking findings. Up to half of all patients have some tests pending at discharge and up to 10% of these require some physician action. More frighteningly, outpatient MDs are generally unaware of these tests creating a huge gap in patient safety in the transition back to outpatient care.
How can we do this better? SHM and the Society for General Internal Medicine have convened a Continuity of Care Task Force and found poor communication with outpatient providers was a common and potentially dangerous problem. They outlined the best practices for the discharge of patients to ensure safety as well as maximize patient and physician satisfaction. Their recommendations are available on the SHM Web site. All hospitalists and institutions should be aware of the potential for missed results and put systems in place, electronic and otherwise, to create an appropriate safety net for our discharged patients.
Sharma R, Loomis W, Brown RB. Impact of mandatory inpatient infectious disease consultation on outpatient parenteral antibiotic therapy. Am J Med Sci. 2005;330(2):60.
Background: As the pressure to limit healthcare costs by reducing inpatient length of stay has increased, the use of outpatient parenteral antibiotic therapy has grown. When employed appropriately, home intravenous antibiotic therapy has consistently resulted in cost savings without compromising patient outcomes. As with other healthcare advances, there is some fear that outpatient parenteral antibiotic treatment will be overused or misused, limiting the cost savings or putting patients at risk.
Methods: A single academic medical center instituted mandatory infectious disease consultation on all patients referred to discharge coordinators with plans for outpatient IV antibiotic treatment. The infectious disease consultants helped to determine the need for outpatient parenteral therapy and antibiotic choice. All patients were followed for 30 days.
Results: Over the one-year study period, 44 cases received mandatory infectious disease consultation. Thirty-nine (89%) of these had some change in antibiotic regimen after the consultation. Seventeen patients (39%) were switched to oral antibiotics, 13 (30%) had a change in infectious disease antibiotic, and 5 (11%) had a change in antibiotic dose.
Skin and skin structure and intra-abdominal infections were the most common diagnoses for which antibiotics were changed; a typical change was from intravenous piperacillin/tazobactam to an oral fluoroquinolone plus oral anaerobic coverage. At 30-day follow-up, 98% of patients finished their courses without relapse or complication. The overall costs savings was $27,500 or $1,550 per patient consulted upon.
Discussion: Although from a small, nonrandomized, single-institution study, the results are impressive. Mandatory infectious disease consultation prior to discharge for patients scheduled to received outpatient parenteral antibiotic therapy resulted in substantial cost savings, and streamlined and more appropriate antibiotic regimens without any adverse impact on outcomes. Hospitalists should take two things away from this study: 1) consider consulting infection disease specialists on all patients who might be candidates for home IV antibiotics and 2) be aware that many skin and skin tissue and intra-abdominal infections can often be treated with oral therapy. TH
Listen to the Eye
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.