User login
Stress independently predicts peptic ulcers
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
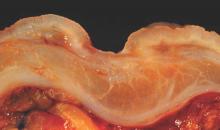
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High stress levels independently predicted peptic ulcers.
Major finding: After adjustment for other risk factors, every one-point increase on a 12-item stress questionnaire increased the odds of peptic ulcers by 12% (OR, 1.12; 95% CI, 1.01-1.23).
Data source: Prospective, population-based study of 76 patients with peptic ulcers.
Disclosures: The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
Study linked gastric phenotypes, hormone levels to obesity
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
Key clinical point: Obesity was linked to lower satiety levels, faster gastric emptying, greater fasted gastric volume, and lower levels of PYY.
Major finding: Obese individuals had larger stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of PYY after eating (P = .003), and higher postprandial levels of GLP-1 (P < .001), compared with normal-weight individuals.
Data source: Prospective study of 328 adults, expanded study of 509 adults, and nested randomized, controlled clinical trial of 24 obese adults.
Disclosures: The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
Draft FDA compounding policies draw criticism
New Food and Drug Administration draft guidance on pharmaceutical compounding drew criticism this week from the American Academy of Dermatologists, whose president said the policies could erode patients’ access to important therapies.
“Many of the more than 3,000 skin diseases that dermatologists care for use compounded pharmaceutical treatments,” AAD President Brett Coldiron said in a statement. “Many of these diseases are rare and do not have cures or FDA-approved treatments. But we’ve seen patients’ quality of life markedly improve as a result of personalized care with compounded medications.”
Published Feb. 13, the five draft FDA documents specify that “biological products” that are “mixed, diluted, or repackaged” by physicians, pharmacies, federal facilities, or outsourcing facilities must meet specific licensing requirements.
The policies “are critical to protecting the public health,” according to the FDA. But dermatologists are “most concerned about FDA’s guidance that does not allow for in-office compounding,” Dr. Coldiron said in an interview. “For example, take a patient with a rare and debilitating skin disease. Dermatologists can provide immediate relief by dispensing safe and effective compounded treatments in their office. Patients shouldn’t have to wait 1 or 2 days to get access to their medication.”
While the draft policies note that physicians would not necessarily have to license individualized mixtures of FDA-approved allergenic extracts used for subcutaneous immunotherapy, they do not similarly exclude topical compounded agents used for orphan skin diseases and other dermatologic conditions.
“Why would we take that away, particularly in an era of personalized medicine?” Dr. Coldiron said. “Dermatologists must maintain full access to in-office compounding to ensure quality patient care.”
The new proposals come in the wake of the Drug Quality and Security Act, which Congress passed in November 2013 to improve regulators’ ability to trace drugs through the pharmaceutical supply chain and to track and report adverse events related to the use of compounded medications.
Enactment of the law followed an outbreak of 751 cases of fungal meningitis among patients who received contaminated, preservative-free medroxyprogesterone acetate (MPA) steroid injections prepared by the New England Compounding Center in Framingham, Mass. A total of 64 patients died in the outbreak, and federal prosecutors later charged two NECC executives with 25 related counts of second-degree homicide. (Twelve other NECC-affiliated individuals were charged with racketeering, mail fraud, conspiracy, contempt, structuring, and violations of the Food, Drug and Cosmetic Act.
But nonsterile topical compounded medications pose substantially less risk to patients than do compounded injectables and related solutions that are meant to be sterile, Dr. Coldiron said. For example, a published review of outbreaks linked to compounding pharmacies between 2000 and 2012 implicated flush and cardioplegia solutions, as well as ophthalmic and injectable medications, but not topical agents (Am. J. Health. Syst. Pharm. 2013 Aug. 1 [doi:10.2146/ajhp130049]). Based on such data, the AAD has supported differential, risk-based regulation of pharmaceutical compounding and has maintained that any new policies on compounding should grant physicians “full access to topical compounded products, including in-office use, without overly burdensome regulatory restrictions” that could limit treatment access. The AAD also has opposed limiting access to commonly used, nonsterile topical products from traditional compounding pharmacies.
The draft FDA policies are open for public comment at www.regulations.gov for 90 days after the guidance is published in the Federal Register. The first meeting of the FDA’s reconstituted Pharmacy Compounding Advisory Committee will be held Feb. 23-24.
New Food and Drug Administration draft guidance on pharmaceutical compounding drew criticism this week from the American Academy of Dermatologists, whose president said the policies could erode patients’ access to important therapies.
“Many of the more than 3,000 skin diseases that dermatologists care for use compounded pharmaceutical treatments,” AAD President Brett Coldiron said in a statement. “Many of these diseases are rare and do not have cures or FDA-approved treatments. But we’ve seen patients’ quality of life markedly improve as a result of personalized care with compounded medications.”
Published Feb. 13, the five draft FDA documents specify that “biological products” that are “mixed, diluted, or repackaged” by physicians, pharmacies, federal facilities, or outsourcing facilities must meet specific licensing requirements.
The policies “are critical to protecting the public health,” according to the FDA. But dermatologists are “most concerned about FDA’s guidance that does not allow for in-office compounding,” Dr. Coldiron said in an interview. “For example, take a patient with a rare and debilitating skin disease. Dermatologists can provide immediate relief by dispensing safe and effective compounded treatments in their office. Patients shouldn’t have to wait 1 or 2 days to get access to their medication.”
While the draft policies note that physicians would not necessarily have to license individualized mixtures of FDA-approved allergenic extracts used for subcutaneous immunotherapy, they do not similarly exclude topical compounded agents used for orphan skin diseases and other dermatologic conditions.
“Why would we take that away, particularly in an era of personalized medicine?” Dr. Coldiron said. “Dermatologists must maintain full access to in-office compounding to ensure quality patient care.”
The new proposals come in the wake of the Drug Quality and Security Act, which Congress passed in November 2013 to improve regulators’ ability to trace drugs through the pharmaceutical supply chain and to track and report adverse events related to the use of compounded medications.
Enactment of the law followed an outbreak of 751 cases of fungal meningitis among patients who received contaminated, preservative-free medroxyprogesterone acetate (MPA) steroid injections prepared by the New England Compounding Center in Framingham, Mass. A total of 64 patients died in the outbreak, and federal prosecutors later charged two NECC executives with 25 related counts of second-degree homicide. (Twelve other NECC-affiliated individuals were charged with racketeering, mail fraud, conspiracy, contempt, structuring, and violations of the Food, Drug and Cosmetic Act.
But nonsterile topical compounded medications pose substantially less risk to patients than do compounded injectables and related solutions that are meant to be sterile, Dr. Coldiron said. For example, a published review of outbreaks linked to compounding pharmacies between 2000 and 2012 implicated flush and cardioplegia solutions, as well as ophthalmic and injectable medications, but not topical agents (Am. J. Health. Syst. Pharm. 2013 Aug. 1 [doi:10.2146/ajhp130049]). Based on such data, the AAD has supported differential, risk-based regulation of pharmaceutical compounding and has maintained that any new policies on compounding should grant physicians “full access to topical compounded products, including in-office use, without overly burdensome regulatory restrictions” that could limit treatment access. The AAD also has opposed limiting access to commonly used, nonsterile topical products from traditional compounding pharmacies.
The draft FDA policies are open for public comment at www.regulations.gov for 90 days after the guidance is published in the Federal Register. The first meeting of the FDA’s reconstituted Pharmacy Compounding Advisory Committee will be held Feb. 23-24.
New Food and Drug Administration draft guidance on pharmaceutical compounding drew criticism this week from the American Academy of Dermatologists, whose president said the policies could erode patients’ access to important therapies.
“Many of the more than 3,000 skin diseases that dermatologists care for use compounded pharmaceutical treatments,” AAD President Brett Coldiron said in a statement. “Many of these diseases are rare and do not have cures or FDA-approved treatments. But we’ve seen patients’ quality of life markedly improve as a result of personalized care with compounded medications.”
Published Feb. 13, the five draft FDA documents specify that “biological products” that are “mixed, diluted, or repackaged” by physicians, pharmacies, federal facilities, or outsourcing facilities must meet specific licensing requirements.
The policies “are critical to protecting the public health,” according to the FDA. But dermatologists are “most concerned about FDA’s guidance that does not allow for in-office compounding,” Dr. Coldiron said in an interview. “For example, take a patient with a rare and debilitating skin disease. Dermatologists can provide immediate relief by dispensing safe and effective compounded treatments in their office. Patients shouldn’t have to wait 1 or 2 days to get access to their medication.”
While the draft policies note that physicians would not necessarily have to license individualized mixtures of FDA-approved allergenic extracts used for subcutaneous immunotherapy, they do not similarly exclude topical compounded agents used for orphan skin diseases and other dermatologic conditions.
“Why would we take that away, particularly in an era of personalized medicine?” Dr. Coldiron said. “Dermatologists must maintain full access to in-office compounding to ensure quality patient care.”
The new proposals come in the wake of the Drug Quality and Security Act, which Congress passed in November 2013 to improve regulators’ ability to trace drugs through the pharmaceutical supply chain and to track and report adverse events related to the use of compounded medications.
Enactment of the law followed an outbreak of 751 cases of fungal meningitis among patients who received contaminated, preservative-free medroxyprogesterone acetate (MPA) steroid injections prepared by the New England Compounding Center in Framingham, Mass. A total of 64 patients died in the outbreak, and federal prosecutors later charged two NECC executives with 25 related counts of second-degree homicide. (Twelve other NECC-affiliated individuals were charged with racketeering, mail fraud, conspiracy, contempt, structuring, and violations of the Food, Drug and Cosmetic Act.
But nonsterile topical compounded medications pose substantially less risk to patients than do compounded injectables and related solutions that are meant to be sterile, Dr. Coldiron said. For example, a published review of outbreaks linked to compounding pharmacies between 2000 and 2012 implicated flush and cardioplegia solutions, as well as ophthalmic and injectable medications, but not topical agents (Am. J. Health. Syst. Pharm. 2013 Aug. 1 [doi:10.2146/ajhp130049]). Based on such data, the AAD has supported differential, risk-based regulation of pharmaceutical compounding and has maintained that any new policies on compounding should grant physicians “full access to topical compounded products, including in-office use, without overly burdensome regulatory restrictions” that could limit treatment access. The AAD also has opposed limiting access to commonly used, nonsterile topical products from traditional compounding pharmacies.
The draft FDA policies are open for public comment at www.regulations.gov for 90 days after the guidance is published in the Federal Register. The first meeting of the FDA’s reconstituted Pharmacy Compounding Advisory Committee will be held Feb. 23-24.
UVA damage to skin DNA continues for hours after exposure
DNA damage to skin continues for hours after UVA exposure ceases, and melanin is a key culprit in the process, based on the results of cell cultures and studies in mice.
“What is extraordinary about this study is that it implicates melanin as a potential source of oxidative stress, [which can] lead to DNA damage and ultimately accelerate skin aging and skin cancer,” said Dr. Adam Friedman, director of dermatologic research at Albert Einstein College of Medicine, New York, who was not involved in the research. “For years, melanin was thought of as only a UV radiation protectant and antioxidant. Could this be a missing element in our fight to prevent skin cancer? The emphasis has always been on preventing the fire, not necessarily putting it out.”
The findings suggest that antioxidant-rich lotions might one day help prevent damage if users apply the “quenchers” soon after sun exposure, said lead author Sanjay Premi, Ph.D. at Yale University in New Haven, Conn., and his associates. Vitamin E and ethyl sorbate are two possible candidates for such “evening after” sunscreens, the researchers said (Science 2015 Feb. 20;347:842-7). For their study, the researchers exposed mouse fibroblasts and melanocytes to UVA, the main type of cancer-causing radiation from sunlight and tanning beds. Then they measured the accumulation of cyclobutane pyrimidine dimers (CPDs), a hallmark of UV-induced DNA damage. Levels of CPDs peaked immediately after UVA exposure in skin cells from albino mice, but kept rising for at least another 3 hours in melanocytes from pigmented mice, the investigators reported. Furthermore, 2 hours after live mice were exposed to UVA, their CPD levels were three times greater than just after UVA exposure, they said. “If the same holds for human skin, this would mean that past measurements of CPDs immediately after UV exposure have underestimated the consequences of UV exposure,” the researchers concluded.
They found similar results for human melanocytes, except that CPD levels varied more, probably because of genetic differences among human skin donors, Dr. Premi and his associates wrote. Further testing of melanin fragments revealed the process by which DNA damage accumulates, even after UVA exposures ends: Reactive oxygen and nitrogen species together excited an electron that in turn damaged DNA in the same way that UV radiation did. “A consequence of these events is that melanin may be carcinogenic as well as protective against cancer,” the researchers emphasized. “This double nature would explain the apparent cancer-facilitating effects of melanin seen in mice and in human epidemiology.”
Although “it is difficult to translate cell assays and mouse models to the human system,” the findings “no doubt raise important, paradigm-shifting ideas in terms of our understanding of UV-induced DNA damage,” said Dr. Friedman. For example, studies have shown that skin cells incur DNA damage even when individuals wear sunscreen as directed, he noted. “Are these cellular changes a result of sunscreen inefficiency, or is it delayed damage due to persistent melanin radicals?” he asked. “We see patients all the time who say, ‘I used sunscreen but I still got burned.’ Granted, there are likely many confounding factors, such as amount of sunscreen applied, frequency, clothing choice, and water exposure. However, maybe we can add progressive and persistent oxidative stress to the list.”
Developing effective “evening-after” lotions to halt UVA damage after exposure will take work, Dr. Friedman added. “The reality is that many, if not most, antioxidants are highly unstable, whether they oxidize easily when exposed to air, or are photo-labile, meaning they degrade upon exposure to sunlight,” he said. One solution is to encapsulate antioxidants within liposomes, solid lipid nanoparticles, or polymeric nanoparticles, but “skin penetration is not the only issue,” he added. “These antioxidants need to actually get into the cells to be effective.”
For that reason, researchers have explored systemic administration of agents such as polypodium leucotomos, which has antioxidant and anti-inflammatory properties, Dr. Friedman noted. “The clinical data available looks at using this natural ingredient to increase minimal erythemal dose, rather then postirradiation recovery,” he said. “Could postirradiation intake be effective? Possibly.”
The research was funded by the U.S. Department of Defense, the National Institutes of Health, the University of Veterinary Medicine in Vienna, Fundação de Amparo à Pesquisa do Estado de São Paulo, and INCT–Processos Redox em Biomedicina. The investigators declared having no conflicts of interest.
DNA damage to skin continues for hours after UVA exposure ceases, and melanin is a key culprit in the process, based on the results of cell cultures and studies in mice.
“What is extraordinary about this study is that it implicates melanin as a potential source of oxidative stress, [which can] lead to DNA damage and ultimately accelerate skin aging and skin cancer,” said Dr. Adam Friedman, director of dermatologic research at Albert Einstein College of Medicine, New York, who was not involved in the research. “For years, melanin was thought of as only a UV radiation protectant and antioxidant. Could this be a missing element in our fight to prevent skin cancer? The emphasis has always been on preventing the fire, not necessarily putting it out.”
The findings suggest that antioxidant-rich lotions might one day help prevent damage if users apply the “quenchers” soon after sun exposure, said lead author Sanjay Premi, Ph.D. at Yale University in New Haven, Conn., and his associates. Vitamin E and ethyl sorbate are two possible candidates for such “evening after” sunscreens, the researchers said (Science 2015 Feb. 20;347:842-7). For their study, the researchers exposed mouse fibroblasts and melanocytes to UVA, the main type of cancer-causing radiation from sunlight and tanning beds. Then they measured the accumulation of cyclobutane pyrimidine dimers (CPDs), a hallmark of UV-induced DNA damage. Levels of CPDs peaked immediately after UVA exposure in skin cells from albino mice, but kept rising for at least another 3 hours in melanocytes from pigmented mice, the investigators reported. Furthermore, 2 hours after live mice were exposed to UVA, their CPD levels were three times greater than just after UVA exposure, they said. “If the same holds for human skin, this would mean that past measurements of CPDs immediately after UV exposure have underestimated the consequences of UV exposure,” the researchers concluded.
They found similar results for human melanocytes, except that CPD levels varied more, probably because of genetic differences among human skin donors, Dr. Premi and his associates wrote. Further testing of melanin fragments revealed the process by which DNA damage accumulates, even after UVA exposures ends: Reactive oxygen and nitrogen species together excited an electron that in turn damaged DNA in the same way that UV radiation did. “A consequence of these events is that melanin may be carcinogenic as well as protective against cancer,” the researchers emphasized. “This double nature would explain the apparent cancer-facilitating effects of melanin seen in mice and in human epidemiology.”
Although “it is difficult to translate cell assays and mouse models to the human system,” the findings “no doubt raise important, paradigm-shifting ideas in terms of our understanding of UV-induced DNA damage,” said Dr. Friedman. For example, studies have shown that skin cells incur DNA damage even when individuals wear sunscreen as directed, he noted. “Are these cellular changes a result of sunscreen inefficiency, or is it delayed damage due to persistent melanin radicals?” he asked. “We see patients all the time who say, ‘I used sunscreen but I still got burned.’ Granted, there are likely many confounding factors, such as amount of sunscreen applied, frequency, clothing choice, and water exposure. However, maybe we can add progressive and persistent oxidative stress to the list.”
Developing effective “evening-after” lotions to halt UVA damage after exposure will take work, Dr. Friedman added. “The reality is that many, if not most, antioxidants are highly unstable, whether they oxidize easily when exposed to air, or are photo-labile, meaning they degrade upon exposure to sunlight,” he said. One solution is to encapsulate antioxidants within liposomes, solid lipid nanoparticles, or polymeric nanoparticles, but “skin penetration is not the only issue,” he added. “These antioxidants need to actually get into the cells to be effective.”
For that reason, researchers have explored systemic administration of agents such as polypodium leucotomos, which has antioxidant and anti-inflammatory properties, Dr. Friedman noted. “The clinical data available looks at using this natural ingredient to increase minimal erythemal dose, rather then postirradiation recovery,” he said. “Could postirradiation intake be effective? Possibly.”
The research was funded by the U.S. Department of Defense, the National Institutes of Health, the University of Veterinary Medicine in Vienna, Fundação de Amparo à Pesquisa do Estado de São Paulo, and INCT–Processos Redox em Biomedicina. The investigators declared having no conflicts of interest.
DNA damage to skin continues for hours after UVA exposure ceases, and melanin is a key culprit in the process, based on the results of cell cultures and studies in mice.
“What is extraordinary about this study is that it implicates melanin as a potential source of oxidative stress, [which can] lead to DNA damage and ultimately accelerate skin aging and skin cancer,” said Dr. Adam Friedman, director of dermatologic research at Albert Einstein College of Medicine, New York, who was not involved in the research. “For years, melanin was thought of as only a UV radiation protectant and antioxidant. Could this be a missing element in our fight to prevent skin cancer? The emphasis has always been on preventing the fire, not necessarily putting it out.”
The findings suggest that antioxidant-rich lotions might one day help prevent damage if users apply the “quenchers” soon after sun exposure, said lead author Sanjay Premi, Ph.D. at Yale University in New Haven, Conn., and his associates. Vitamin E and ethyl sorbate are two possible candidates for such “evening after” sunscreens, the researchers said (Science 2015 Feb. 20;347:842-7). For their study, the researchers exposed mouse fibroblasts and melanocytes to UVA, the main type of cancer-causing radiation from sunlight and tanning beds. Then they measured the accumulation of cyclobutane pyrimidine dimers (CPDs), a hallmark of UV-induced DNA damage. Levels of CPDs peaked immediately after UVA exposure in skin cells from albino mice, but kept rising for at least another 3 hours in melanocytes from pigmented mice, the investigators reported. Furthermore, 2 hours after live mice were exposed to UVA, their CPD levels were three times greater than just after UVA exposure, they said. “If the same holds for human skin, this would mean that past measurements of CPDs immediately after UV exposure have underestimated the consequences of UV exposure,” the researchers concluded.
They found similar results for human melanocytes, except that CPD levels varied more, probably because of genetic differences among human skin donors, Dr. Premi and his associates wrote. Further testing of melanin fragments revealed the process by which DNA damage accumulates, even after UVA exposures ends: Reactive oxygen and nitrogen species together excited an electron that in turn damaged DNA in the same way that UV radiation did. “A consequence of these events is that melanin may be carcinogenic as well as protective against cancer,” the researchers emphasized. “This double nature would explain the apparent cancer-facilitating effects of melanin seen in mice and in human epidemiology.”
Although “it is difficult to translate cell assays and mouse models to the human system,” the findings “no doubt raise important, paradigm-shifting ideas in terms of our understanding of UV-induced DNA damage,” said Dr. Friedman. For example, studies have shown that skin cells incur DNA damage even when individuals wear sunscreen as directed, he noted. “Are these cellular changes a result of sunscreen inefficiency, or is it delayed damage due to persistent melanin radicals?” he asked. “We see patients all the time who say, ‘I used sunscreen but I still got burned.’ Granted, there are likely many confounding factors, such as amount of sunscreen applied, frequency, clothing choice, and water exposure. However, maybe we can add progressive and persistent oxidative stress to the list.”
Developing effective “evening-after” lotions to halt UVA damage after exposure will take work, Dr. Friedman added. “The reality is that many, if not most, antioxidants are highly unstable, whether they oxidize easily when exposed to air, or are photo-labile, meaning they degrade upon exposure to sunlight,” he said. One solution is to encapsulate antioxidants within liposomes, solid lipid nanoparticles, or polymeric nanoparticles, but “skin penetration is not the only issue,” he added. “These antioxidants need to actually get into the cells to be effective.”
For that reason, researchers have explored systemic administration of agents such as polypodium leucotomos, which has antioxidant and anti-inflammatory properties, Dr. Friedman noted. “The clinical data available looks at using this natural ingredient to increase minimal erythemal dose, rather then postirradiation recovery,” he said. “Could postirradiation intake be effective? Possibly.”
The research was funded by the U.S. Department of Defense, the National Institutes of Health, the University of Veterinary Medicine in Vienna, Fundação de Amparo à Pesquisa do Estado de São Paulo, and INCT–Processos Redox em Biomedicina. The investigators declared having no conflicts of interest.
FROM SCIENCE
Key clinical point: Melanin played a key role in DNA damage to skin cells hours after UVA exposure.
Major finding: Melanocytes continued to form cyclobutane pyrimidine dimers for at least 3 hours after exposure to UVA radiation.
Data source: Histologic study of UV-exposed skin cells from mice and humans, and of in vivo mice.
Disclosures: The research was funded by the U.S. Department of Defense, the National Institutes of Health, the University of Veterinary Medicine in Vienna, Fundação de Amparo à Pesquisa do Estado de São Paulo, and INCT–Processos Redox em Biomedicina. The investigators declared having no conflicts of interest.
Brief, light exercise could cut cardiovascular deaths in elderly
Among elderly adults with limited mobility, even very short periods of light daily exercise might significantly cut 10-year risk of heart attack or coronary death, according to researchers.
Conversely, every extra half hour per day that older adults are sedentary could raise their 10-year death risk by about 1%, explained Jodi D. Fitzgerald of the University of Florida, Gainesville, and her associates (J. Am. Heart Assoc. 2015 [doi:10.1161/JAHA.114.001288]).
The cross-sectional analysis is the first to document such findings among the elderly, including those with mobility restrictions, said the researchers.
“Replacing sedentary behavior with any intensity of physical activity seems beneficial for this population,” they added. “For mobility-limited older adults, this may be achieved simply by being intentional about moving around or leaving the home more often.”
The researchers analyzed data from 1,170 adults in the Lifestyle Interventions and Independence for Elders (LIFE) study, which was carried out at eight centers in the United States. Participants were aged 70-89 years and had limited mobility, but could walk 400 meters in 15 minutes or less, the investigators said.
Using accelerometers, the researchers measured the amount of time participants were sedentary, performed light exercise such as slow walking, and engaged in moderate walking or similarly challenging activities.
After adjustment for factors such as diabetes and use of statins and antihypertensives, every extra minute of light exercise per day was associated with an estimated 0.05% drop in 10-year risk of cardiovascular death (P < .05), the investigators reported.
Every minute of sedentary behavior was linked to a 0.04% rise in 10-year death risk in patients with cardiovascular disease, and a 0.03% rise in patients without cardiovascular disease. Those findings equate to a 1% increase in 10-year death risk for every 25-30 sedentary minutes per day, the investigators said.
The National Institutes of Health and participating universities funded the study. The authors declared no conflicts of interest.
Among elderly adults with limited mobility, even very short periods of light daily exercise might significantly cut 10-year risk of heart attack or coronary death, according to researchers.
Conversely, every extra half hour per day that older adults are sedentary could raise their 10-year death risk by about 1%, explained Jodi D. Fitzgerald of the University of Florida, Gainesville, and her associates (J. Am. Heart Assoc. 2015 [doi:10.1161/JAHA.114.001288]).
The cross-sectional analysis is the first to document such findings among the elderly, including those with mobility restrictions, said the researchers.
“Replacing sedentary behavior with any intensity of physical activity seems beneficial for this population,” they added. “For mobility-limited older adults, this may be achieved simply by being intentional about moving around or leaving the home more often.”
The researchers analyzed data from 1,170 adults in the Lifestyle Interventions and Independence for Elders (LIFE) study, which was carried out at eight centers in the United States. Participants were aged 70-89 years and had limited mobility, but could walk 400 meters in 15 minutes or less, the investigators said.
Using accelerometers, the researchers measured the amount of time participants were sedentary, performed light exercise such as slow walking, and engaged in moderate walking or similarly challenging activities.
After adjustment for factors such as diabetes and use of statins and antihypertensives, every extra minute of light exercise per day was associated with an estimated 0.05% drop in 10-year risk of cardiovascular death (P < .05), the investigators reported.
Every minute of sedentary behavior was linked to a 0.04% rise in 10-year death risk in patients with cardiovascular disease, and a 0.03% rise in patients without cardiovascular disease. Those findings equate to a 1% increase in 10-year death risk for every 25-30 sedentary minutes per day, the investigators said.
The National Institutes of Health and participating universities funded the study. The authors declared no conflicts of interest.
Among elderly adults with limited mobility, even very short periods of light daily exercise might significantly cut 10-year risk of heart attack or coronary death, according to researchers.
Conversely, every extra half hour per day that older adults are sedentary could raise their 10-year death risk by about 1%, explained Jodi D. Fitzgerald of the University of Florida, Gainesville, and her associates (J. Am. Heart Assoc. 2015 [doi:10.1161/JAHA.114.001288]).
The cross-sectional analysis is the first to document such findings among the elderly, including those with mobility restrictions, said the researchers.
“Replacing sedentary behavior with any intensity of physical activity seems beneficial for this population,” they added. “For mobility-limited older adults, this may be achieved simply by being intentional about moving around or leaving the home more often.”
The researchers analyzed data from 1,170 adults in the Lifestyle Interventions and Independence for Elders (LIFE) study, which was carried out at eight centers in the United States. Participants were aged 70-89 years and had limited mobility, but could walk 400 meters in 15 minutes or less, the investigators said.
Using accelerometers, the researchers measured the amount of time participants were sedentary, performed light exercise such as slow walking, and engaged in moderate walking or similarly challenging activities.
After adjustment for factors such as diabetes and use of statins and antihypertensives, every extra minute of light exercise per day was associated with an estimated 0.05% drop in 10-year risk of cardiovascular death (P < .05), the investigators reported.
Every minute of sedentary behavior was linked to a 0.04% rise in 10-year death risk in patients with cardiovascular disease, and a 0.03% rise in patients without cardiovascular disease. Those findings equate to a 1% increase in 10-year death risk for every 25-30 sedentary minutes per day, the investigators said.
The National Institutes of Health and participating universities funded the study. The authors declared no conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Key clinical point: Even very short periods of light daily exercise might significantly cut 10-year risk of heart attack or coronary death in the elderly.
Major finding: Every extra minute of daily light exercise was linked to a 0.05% drop in 10-year risk of cardiovascular death (P < .05).
Data source: Cross-sectional analysis of data from 1,170 participants in the Lifestyle Interventions and Independence for Elders study.
Disclosures: The National Institutes of Health and participating universities funded the study. The authors declared no conflicts of interest.
Lower bleeding, death risk with fondaparinux after NSTEMI
Patients hospitalized with non–ST-segment myocardial infarction who received fondaparinux had significantly lower risk of suffering a major bleed or dying in the hospital, compared with those treated with low-molecular-weight heparin, investigators reported online Feb. 17 in JAMA.
The differences persisted 1 and 6 months after hospitalization, said Dr. Karolina Szummer at Karolinska University Hospital in Stockholm, and her associates. However, fondaparinux was not linked to lower rates of stroke or recurrent heart attack, compared with low-molecular-weight heparin (LMWH), the researchers said.
The European Society of Cardiology changed its NSTEMI guidelines in 2011, recommending fondaparinux as a first-choice anticoagulant for both patients treated either noninvasively or with PCI, spurring a “rapid switch” from LMWH to the indirect factor Xa inhibitor fondaparinux for treating non–ST-segment myocardial infarction (NSTEMI), said the investigators. (American Heart Association/American College of Cardiology guidelines, issued in 2012, do not favor fondaparinux over LMWH.) To study the effects of ESC’s change, they analyzed registry data from 40,616 patients hospitalized with NSTEMI between 2006 and 2010, of whom 36% of patients received fondaparinux and 64% received LMWH (JAMA 2015 Feb. 17;313:707-16).
Only 3.7% of the fondaparinux group suffered severe bleeding events or died in the hospital, compared with 5.5% of the heparin group (adjusted odds ratio, 0.67; 95% confidence interval, 0.58-0.78), the study found. Significant differences in bleeding and death rates persisted 30 days and 6 months after hospitalization, but rates of recurrent heart attack and stroke were similar between the treatment groups at all time points, the researchers said.
“This is not a randomized trial; therefore, residual confounding is very likely,” the investigators cautioned, adding that because the study used registry data, it probably underestimated bleeding events.
The work was funded by the Swedish Foundation for Strategic Research, the Swedish Heart and Lung Foundation, ALF Medicin, and the Swedish Medical Research Council. Dr. Szummer has received lecture fees from AstraZeneca. One coauthor reported financial relationships with GlaxoSmithKline, which markets fondaparinux. Other coauthors reported funding from numerous pharmaceutical companies.
Patients hospitalized with non–ST-segment myocardial infarction who received fondaparinux had significantly lower risk of suffering a major bleed or dying in the hospital, compared with those treated with low-molecular-weight heparin, investigators reported online Feb. 17 in JAMA.
The differences persisted 1 and 6 months after hospitalization, said Dr. Karolina Szummer at Karolinska University Hospital in Stockholm, and her associates. However, fondaparinux was not linked to lower rates of stroke or recurrent heart attack, compared with low-molecular-weight heparin (LMWH), the researchers said.
The European Society of Cardiology changed its NSTEMI guidelines in 2011, recommending fondaparinux as a first-choice anticoagulant for both patients treated either noninvasively or with PCI, spurring a “rapid switch” from LMWH to the indirect factor Xa inhibitor fondaparinux for treating non–ST-segment myocardial infarction (NSTEMI), said the investigators. (American Heart Association/American College of Cardiology guidelines, issued in 2012, do not favor fondaparinux over LMWH.) To study the effects of ESC’s change, they analyzed registry data from 40,616 patients hospitalized with NSTEMI between 2006 and 2010, of whom 36% of patients received fondaparinux and 64% received LMWH (JAMA 2015 Feb. 17;313:707-16).
Only 3.7% of the fondaparinux group suffered severe bleeding events or died in the hospital, compared with 5.5% of the heparin group (adjusted odds ratio, 0.67; 95% confidence interval, 0.58-0.78), the study found. Significant differences in bleeding and death rates persisted 30 days and 6 months after hospitalization, but rates of recurrent heart attack and stroke were similar between the treatment groups at all time points, the researchers said.
“This is not a randomized trial; therefore, residual confounding is very likely,” the investigators cautioned, adding that because the study used registry data, it probably underestimated bleeding events.
The work was funded by the Swedish Foundation for Strategic Research, the Swedish Heart and Lung Foundation, ALF Medicin, and the Swedish Medical Research Council. Dr. Szummer has received lecture fees from AstraZeneca. One coauthor reported financial relationships with GlaxoSmithKline, which markets fondaparinux. Other coauthors reported funding from numerous pharmaceutical companies.
Patients hospitalized with non–ST-segment myocardial infarction who received fondaparinux had significantly lower risk of suffering a major bleed or dying in the hospital, compared with those treated with low-molecular-weight heparin, investigators reported online Feb. 17 in JAMA.
The differences persisted 1 and 6 months after hospitalization, said Dr. Karolina Szummer at Karolinska University Hospital in Stockholm, and her associates. However, fondaparinux was not linked to lower rates of stroke or recurrent heart attack, compared with low-molecular-weight heparin (LMWH), the researchers said.
The European Society of Cardiology changed its NSTEMI guidelines in 2011, recommending fondaparinux as a first-choice anticoagulant for both patients treated either noninvasively or with PCI, spurring a “rapid switch” from LMWH to the indirect factor Xa inhibitor fondaparinux for treating non–ST-segment myocardial infarction (NSTEMI), said the investigators. (American Heart Association/American College of Cardiology guidelines, issued in 2012, do not favor fondaparinux over LMWH.) To study the effects of ESC’s change, they analyzed registry data from 40,616 patients hospitalized with NSTEMI between 2006 and 2010, of whom 36% of patients received fondaparinux and 64% received LMWH (JAMA 2015 Feb. 17;313:707-16).
Only 3.7% of the fondaparinux group suffered severe bleeding events or died in the hospital, compared with 5.5% of the heparin group (adjusted odds ratio, 0.67; 95% confidence interval, 0.58-0.78), the study found. Significant differences in bleeding and death rates persisted 30 days and 6 months after hospitalization, but rates of recurrent heart attack and stroke were similar between the treatment groups at all time points, the researchers said.
“This is not a randomized trial; therefore, residual confounding is very likely,” the investigators cautioned, adding that because the study used registry data, it probably underestimated bleeding events.
The work was funded by the Swedish Foundation for Strategic Research, the Swedish Heart and Lung Foundation, ALF Medicin, and the Swedish Medical Research Council. Dr. Szummer has received lecture fees from AstraZeneca. One coauthor reported financial relationships with GlaxoSmithKline, which markets fondaparinux. Other coauthors reported funding from numerous pharmaceutical companies.
Key clinical point: Fondaparinux might lower the risk of severe bleeding and death compared with LMWH in patients with NSTEMI.
Major finding: 3.7% of the fondaparinux group had severe bleeding or died in the hospital compared with 5.5% of the LMWH group (adjusted OR, 0.67).
Data source: Prospective multicenter observational cohort study of 40,616 patients with NSTEMI.
Disclosures: The study was funded by the Swedish Foundation for Strategic Research, the Swedish Heart and Lung Foundation, ALF Medicin, and the Swedish Medical Research Council. Dr. Szummer reported received lecture fees from AstraZeneca. One coauthor reported financial relationships with GlaxoSmithKline, which markets fondaparinux. Other coauthors reported funding from numerous pharmaceutical companies.
Short-Term Hormone Replacement Therapy Upped Ovarian Cancer Risk
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
Short-term hormone replacement therapy upped ovarian cancer risk
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
The findings support adding ovarian cancer to the list of adverse effects associated with hormone therapy use. However, compared with cardiovascular diseases and breast cancer, ovarian cancer is far less common, suggesting that overall risk assessment of hormone therapy will not be strongly affected by these results.
The present study did not evaluate dose, and median year of diagnosis was 2001 — slightly before the widespread change in use patterns occurred with publication of the Women’s Health Initiative findings.
It is still not clear whether the current recommendation to use hormone therapy for the shortest duration possible is appropriate for women who are concerned about an increased risk of ovarian cancer. The current report underlines the importance and limitations of observational data for rare and long-term outcomes, especially for the complex associations between regimen, dose, duration, route of administration, and timing of hormone therapy use with ovarian, breast, and endometrial cancers.
Dr. Nicolas Wentzensen and Dr. Britton Trabert are investigators with the division of cancer epidemiology & genetics at the National Cancer Institute, Bethesda, Md. These comments are taken from their accompanying editorial (Lancet 2015 Feb. 13 [doi:10.1016/ S0140-6736(14)62458-2]). They had no competing interests.
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
Current, short-term use of hormone replacement therapy led to a 43% increase in risk of serous and endometrioid ovarian cancers, according to a large meta-analysis reported online in the Lancet.
Risk fell after women stopped hormone replacement therapy (HRT), but “remained appreciable” for the next few years, wrote the Collaborative Group on Epidemiological Studies of Ovarian Cancer. And long-term users had an estimated 25% increase in ovarian cancer risk, even a full decade after stopping HRT (relative risk, 1.25; 95% confidence interval, 1.07 to 1.46; P = .005), the group reported.
The findings “strongly suggest a causal relationship – i.e., that among otherwise similar women, use of hormone therapy increases the probability of developing the two most common types of ovarian cancer,” the group wrote (Lancet 2015 Feb. 13 [doi: 10.1016/ S0140-6736(14)61687-1]).
Guidelines on HRT from the United States and Europe do not mention ovarian cancer, and those from the United Kingdom describe only risk with long-term use. The findings are “directly relevant to medical advice, personal choices, and the current efforts to revise ... guidelines,” the investigators wrote.
The meta-analysis included 52 observational cohort studies, 17 of which were prospective. In all, 12,110 postmenopausal women in the prospective studies developed ovarian cancer, and 55% had used HRT. Women who had been on HRT for less than 5 years were 1.43 times more likely to develop ovarian cancer than were nonusers (RR, 1.43; 95% CI, 1.29 to 1.46; P < .0001). Thus, HRT might cause one extra case of ovarian cancer per 1,000 users, and one extra death from ovarian cancer per 1,700 users, the group wrote.
Risk of ovarian cancer was similar regardless of age and type of HRT use, the investigators said.
The Medical Research Council and Cancer Research UK funded the analysis. The authors declared no relevant financial conflicts of interest.
Key clinical point: Hormone replacement therapy (HRT) was linked to an increased risk of ovarian cancer.
Major finding: Current use of HRT for less than 5 years was associated with a 43% increase in ovarian cancer risk (P < .0001).
Data source: Meta-analysis of data from 17 prospective studies.
Disclosures: The Medical Research Council and Cancer Research UK funded the study. The authors declared no relevant financial conflicts of interest.
Childhood Atopic Dermatitis Linked to Central Obesity, High BP
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Childhood atopic dermatitis linked to central obesity, high BP
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Pediatric atopic dermatitis was linked with key features of metabolic syndrome, including central obesity and high blood pressure, in a multicenter prospective case-control study.
Given the findings, clinicians should routinely measure body mass index and waist circumference in children with atopic dermatitis (AD), said Dr. Jonathan I. Silverberg of Northwestern University, Chicago, and his associates. “In addition, blood pressure should be assessed in children with moderate to severe AD, even those who are a healthy weight with moderate disease and who are not receiving systemic therapy.”
Past studies have linked AD with risk factors for metabolic syndrome, such as chronic inflammation and sleep and mental health problems. To further explore the link between AD and metabolic disease, Dr. Silverberg and his associates studied 132 children with active, moderate to severe AD and 143 healthy controls matched by sex and race/ethnicity (JAMA Dermatol. 2015;151;144-152).
Compared with controls, children with AD were significantly more likely to have BMI in at least the 97th percentile for age and sex (odds ratio, 2.64, P = .02), waist circumference in at least the 85th percentile (OR, 3.92, P = .005), and waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02). Atopic dermatitis was linked with systolic blood pressure in at least the 90th percentile (OR, 2.06, P = .03), even after the researchers accounted for age, sex, race, use of cyclosporine or prednisone, BMI, and waist circumference. Those results conflict with a study in Japanese adults linking AD with low blood pressure, and indicate that more studies are need to confirm and characterize the association between blood pressure and AD, they said.
Dr. Silverberg and his associates did not record blood lipid levels, so they could not determine whether children met criteria for metabolic syndrome. They also measured blood pressure with a single reading, and the controls were significantly older than were the children with AD (P = .03).
The International Psoriasis Council supported the study. The authors reported having no relevant conflicts of interest.
Key clinical point: Childhood atopic dermatitis was associated with central obesity and high systolic blood pressure.
Major finding: Pediatric AD was linked with waist circumference in at least the 85th percentile (OR, 3.92, P = .005), waist-to-height ratio of a least 0.5 (OR, 2.22; P = .02), and systolic blood pressure in at least the 90th percentile for age, sex, and height (OR, 2.06, P = .03).
Data source: Case-control study of 132 children with moderate to severe active AD and 143 healthy controls.
Disclosures: The International Psoriasis Council supported the study. The authors declared no conflicts of interest.