User login
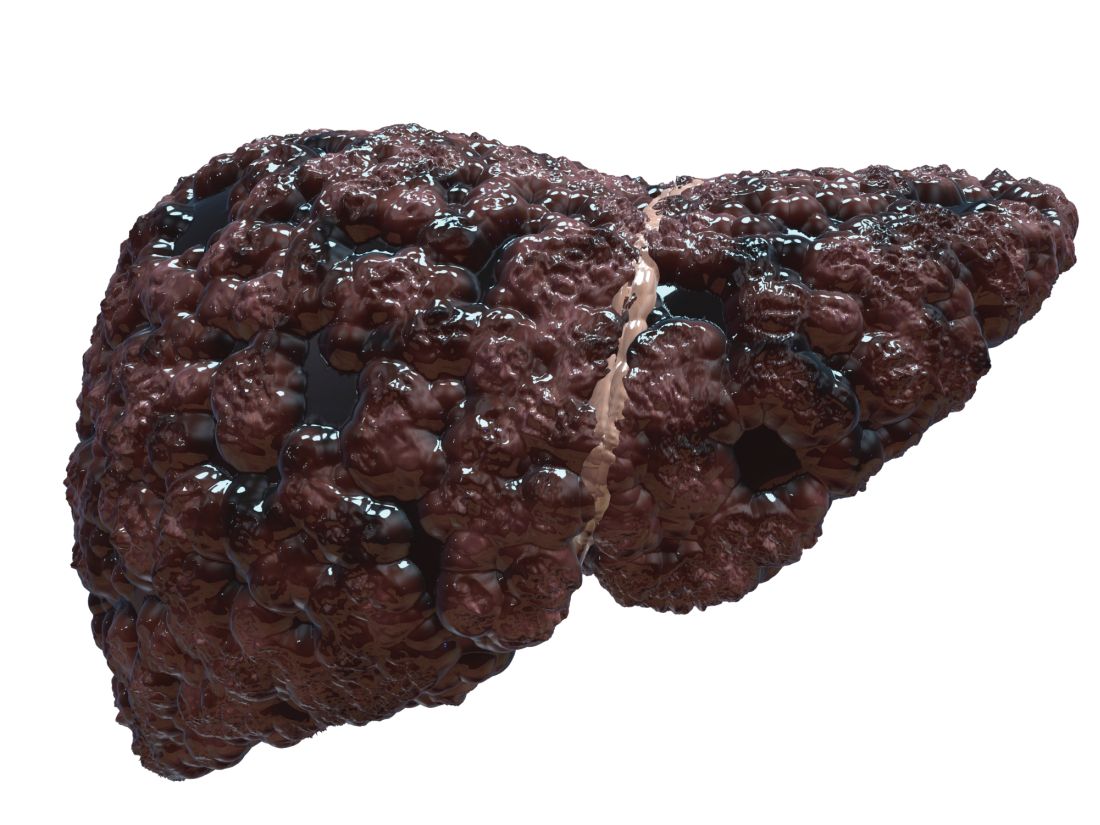
Cirrhosis study finds no link between screening, liver cancer mortality
In a case-control study of patients with cirrhosis, screening for hepatocellular carcinoma up to 4 years prior to diagnosis was not associated with lower mortality.
Similar proportions of cases and controls underwent screening with abdominal ultrasonography, serum alpha-fetoprotein (AFP) testing, or both, reported Andrew M. Moon, MD, MPH, of the University of North Carolina at Chapel Hill, and his associates. “There was also no difference in receipt of these screening tests within 1, 2, or 3 years prior to the index date,” they wrote. The report was published in Gastroenterology. The findings “[suggest] that either these screening tests or the currently available treatments [for liver cancer], or both, are suboptimal and need to be improved.”
Because cirrhosis significantly increases the risk of hepatocellular carcinoma, the American Association for the Study of Liver Diseases, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver recommend screening cirrhotic patients every 6 months with abdominal ultrasonography with or without concomitant serum AFP. But nonliver societies have not endorsed this approach, citing a lack of high-quality data. One problem is that studies have compared patients whose liver cancer was diagnosed by screening with those diagnosed after they became symptomatic, which creates a lead-time bias that inherently favors screening, Dr. Moon and his associates noted.
To help fill the evidence gap, they identified 238 patients from the Veterans Affairs health care system who had died of hepatocellular carcinoma between 2013 and 2015 and who had been diagnosed with cirrhosis at least 4 years beforehand. They compared these cases with an equal number of patients with cirrhosis who had been in VA care for a similar amount of time and had not died of hepatocellular carcinoma. Cases and controls were matched by etiology of cirrhosis, year that cirrhosis was diagnosed, race, age, sex, Model for End-Stage Liver Disease score, and VA medical center. The researchers identified screening tests by reviewing blinded medical charts.
There were no significant differences in the proportions of cases and controls who underwent screening ultrasonography (52.9% versus 54.2%, respectively), screening serum AFP (74.8% versus 73.5%), either test (81.1% versus 79.4%), or both tests (46.6% versus 48.3%) within 4 years of the index date or the matched control. The result was similar after potential confounders were controlled for and when examining shorter time frames of 1, 2, and 3 years.
It was unlikely that these results reflect delayed diagnosis of liver cancer or a lack of treatment within the VA system, the experts wrote. A total of 51.3% of cases were diagnosed with Milan criteria, which exceeds the proportion in the national Surveillance, Epidemiology, and End Results registry, they noted. None of the fatal cases underwent liver transplantation, but 66.8% received other treatments for liver cancer.
Funders included the National Institutes of Health and the Veterans Affairs Clinical Science Research & Development. The investigators reported having no conflicts of interest.
SOURCE: Moon AM et al. Gastroenterology. 2018 Jul 5. doi: 10.1053/j.gastro.2018.06.079.
In a case-control study of patients with cirrhosis, screening for hepatocellular carcinoma up to 4 years prior to diagnosis was not associated with lower mortality.
Similar proportions of cases and controls underwent screening with abdominal ultrasonography, serum alpha-fetoprotein (AFP) testing, or both, reported Andrew M. Moon, MD, MPH, of the University of North Carolina at Chapel Hill, and his associates. “There was also no difference in receipt of these screening tests within 1, 2, or 3 years prior to the index date,” they wrote. The report was published in Gastroenterology. The findings “[suggest] that either these screening tests or the currently available treatments [for liver cancer], or both, are suboptimal and need to be improved.”
Because cirrhosis significantly increases the risk of hepatocellular carcinoma, the American Association for the Study of Liver Diseases, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver recommend screening cirrhotic patients every 6 months with abdominal ultrasonography with or without concomitant serum AFP. But nonliver societies have not endorsed this approach, citing a lack of high-quality data. One problem is that studies have compared patients whose liver cancer was diagnosed by screening with those diagnosed after they became symptomatic, which creates a lead-time bias that inherently favors screening, Dr. Moon and his associates noted.
To help fill the evidence gap, they identified 238 patients from the Veterans Affairs health care system who had died of hepatocellular carcinoma between 2013 and 2015 and who had been diagnosed with cirrhosis at least 4 years beforehand. They compared these cases with an equal number of patients with cirrhosis who had been in VA care for a similar amount of time and had not died of hepatocellular carcinoma. Cases and controls were matched by etiology of cirrhosis, year that cirrhosis was diagnosed, race, age, sex, Model for End-Stage Liver Disease score, and VA medical center. The researchers identified screening tests by reviewing blinded medical charts.
There were no significant differences in the proportions of cases and controls who underwent screening ultrasonography (52.9% versus 54.2%, respectively), screening serum AFP (74.8% versus 73.5%), either test (81.1% versus 79.4%), or both tests (46.6% versus 48.3%) within 4 years of the index date or the matched control. The result was similar after potential confounders were controlled for and when examining shorter time frames of 1, 2, and 3 years.
It was unlikely that these results reflect delayed diagnosis of liver cancer or a lack of treatment within the VA system, the experts wrote. A total of 51.3% of cases were diagnosed with Milan criteria, which exceeds the proportion in the national Surveillance, Epidemiology, and End Results registry, they noted. None of the fatal cases underwent liver transplantation, but 66.8% received other treatments for liver cancer.
Funders included the National Institutes of Health and the Veterans Affairs Clinical Science Research & Development. The investigators reported having no conflicts of interest.
SOURCE: Moon AM et al. Gastroenterology. 2018 Jul 5. doi: 10.1053/j.gastro.2018.06.079.
In a case-control study of patients with cirrhosis, screening for hepatocellular carcinoma up to 4 years prior to diagnosis was not associated with lower mortality.
Similar proportions of cases and controls underwent screening with abdominal ultrasonography, serum alpha-fetoprotein (AFP) testing, or both, reported Andrew M. Moon, MD, MPH, of the University of North Carolina at Chapel Hill, and his associates. “There was also no difference in receipt of these screening tests within 1, 2, or 3 years prior to the index date,” they wrote. The report was published in Gastroenterology. The findings “[suggest] that either these screening tests or the currently available treatments [for liver cancer], or both, are suboptimal and need to be improved.”
Because cirrhosis significantly increases the risk of hepatocellular carcinoma, the American Association for the Study of Liver Diseases, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver recommend screening cirrhotic patients every 6 months with abdominal ultrasonography with or without concomitant serum AFP. But nonliver societies have not endorsed this approach, citing a lack of high-quality data. One problem is that studies have compared patients whose liver cancer was diagnosed by screening with those diagnosed after they became symptomatic, which creates a lead-time bias that inherently favors screening, Dr. Moon and his associates noted.
To help fill the evidence gap, they identified 238 patients from the Veterans Affairs health care system who had died of hepatocellular carcinoma between 2013 and 2015 and who had been diagnosed with cirrhosis at least 4 years beforehand. They compared these cases with an equal number of patients with cirrhosis who had been in VA care for a similar amount of time and had not died of hepatocellular carcinoma. Cases and controls were matched by etiology of cirrhosis, year that cirrhosis was diagnosed, race, age, sex, Model for End-Stage Liver Disease score, and VA medical center. The researchers identified screening tests by reviewing blinded medical charts.
There were no significant differences in the proportions of cases and controls who underwent screening ultrasonography (52.9% versus 54.2%, respectively), screening serum AFP (74.8% versus 73.5%), either test (81.1% versus 79.4%), or both tests (46.6% versus 48.3%) within 4 years of the index date or the matched control. The result was similar after potential confounders were controlled for and when examining shorter time frames of 1, 2, and 3 years.
It was unlikely that these results reflect delayed diagnosis of liver cancer or a lack of treatment within the VA system, the experts wrote. A total of 51.3% of cases were diagnosed with Milan criteria, which exceeds the proportion in the national Surveillance, Epidemiology, and End Results registry, they noted. None of the fatal cases underwent liver transplantation, but 66.8% received other treatments for liver cancer.
Funders included the National Institutes of Health and the Veterans Affairs Clinical Science Research & Development. The investigators reported having no conflicts of interest.
SOURCE: Moon AM et al. Gastroenterology. 2018 Jul 5. doi: 10.1053/j.gastro.2018.06.079.
FROM GASTROENTEROLOGY
Key clinical point: Among patients with cirrhosis, screening for hepatocellular carcinoma was not associated with reductions in liver cancer mortality.
Major finding: Similar proportions of cases and controls were screened by abdominal ultrasonography, serum alpha-fetoprotein, or both up to 4 years before the index date and even after researchers controlled for relevant confounders.
Study details: A matched case-control study of 476 patients from the Veterans Affairs health care system.
Disclosures: Funders included the National Institutes of Health and the Veterans Affairs Clinical Science Research & Development. The investigators reported no conflicts of interest.
Source: Moon AM et al. Gastroenterology. 2018 Jul 5. doi: 10.1053/j.gastro.2018.06.079.
Experts update diagnostic guidelines for eosinophilic esophagitis
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
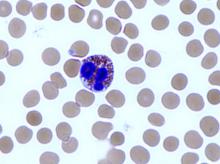
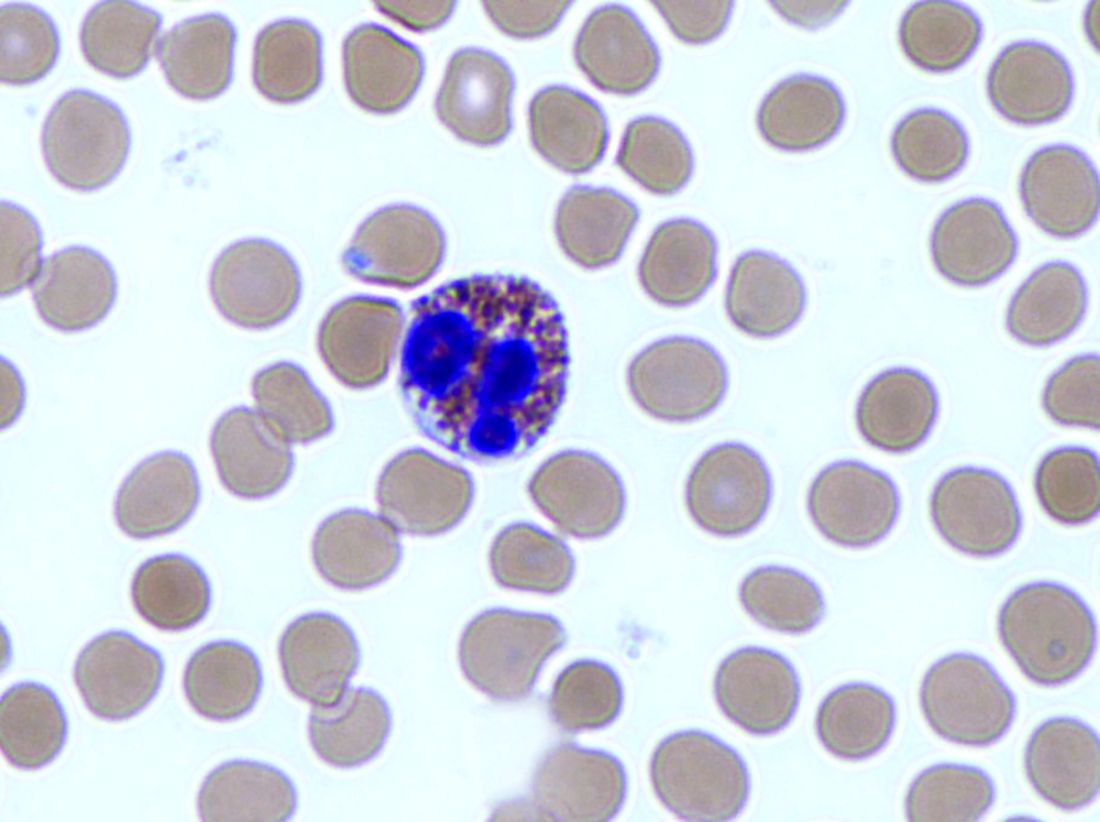
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
FROM GASTROENTEROLOGY
Key clinical point: The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor therapy.
Major finding: Eosinophilic esophagitis and gastroesophageal reflux disease are not mutually exclusive.
Study details: Review by an international consensus panel of studies published between 1966 and 2016.
Disclosures: The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships with Adare, Allakos, Alivio, Banner, Celgene/Receptos, Enumeral, GSK, Regeneron, and Shire. He also reported receiving research funding from Adare, Celgene/Receptos, Miraca, Meritage, Nutricia, Regeneron, and Shire and educational grants from Banner and Holoclara. The majority of his coauthors disclosed relationships with numerous medical companies.
Source: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
Coagulopathy outbreak underscores danger of synthetic cannabinoids
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: There were more than 150 cases in Illinois with four deaths among patients who developed spontaneous intracranial bleeding.
Study details: A single-institution case series of 15 patients.
Disclosures: Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
Source: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Atrial fib guidelines may fall short on oral anticoagulation
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold. Anticoagulation thresholds were lower but still varied widely in a model of non–vitamin K antagonist therapy.
Study details: Markov state-transition model of 33,434 patients with nonvalvular atrial fibrillation.
Disclosures: The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
Source: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762.
AGA Guideline: Treatment of opioid-induced constipation
For patients with suspected opioid-induced constipation, start by taking a careful history of defecation and dietary patterns, stool consistency, incomplete evacuation, and “alarm symptoms,” such as bloody stools or weight loss, state new guidelines from the American Gastroenterological Association in Gastroenterology.
Clinicians also should rule out other causes of constipation, such as pelvic outlet dysfunction, mechanical obstruction, metabolic abnormalities, and comorbidities or concurrent medications, wrote Seth D. Crockett, MD, MPH, of the University of North Carolina at Chapel Hill, together with his associates. The guideline was published online Sept. 1.
Opioid therapy can lead to a range of gastrointestinal symptoms, such as constipation, gastroesophageal reflux, nausea and vomiting, bloating, and abdominal pain. Among these, constipation is by far the most common and debilitating, the guideline notes. In past studies, 40%-80% of patients who received opioids developed opioid-induced constipation (OIC), a more severe presentation that involves a combination of reduced stool frequency in addition to other symptoms, such as harder stools, new or worsening straining during defecation, and a sense of incomplete rectal evacuation.
Treating OIC should start with lifestyle interventions, such as drinking more fluids, toileting as soon as possible when feeling the urge to defecate, and adding regular moderate exercise whenever tolerable, the guideline advises. For patients on oral or parenteral therapy, consider switching to an equianalgesic dose of a less-constipating opioid, such as transdermal fentanyl or oxycodone-naloxone combination therapy.
Many patients with OIC require interventions beyond lifestyle changes or opioid switching. For these patients, the guideline advises starting with conventional laxative therapies based on their safety, low cost, and “established efficacy” in the OIC setting. Options include stool softeners (docusate sodium), osmotic laxatives (polyethylene glycol, magnesium hydroxide, magnesium citrate, and lactulose), lubricants (mineral oil), and stimulant laxatives (bisacodyl, sodium picosulfate, and senna). “Of note, there is little evidence that routine use of stimulant laxatives is harmful to the colon, despite widespread concern to the contrary,” the guideline states. Although randomized, controlled trials have not evaluated particular laxative combinations or titrations for OIC, the best evidence supports stimulant and osmotic laxative therapy, the authors note.
Before deeming any case of OIC laxative refractory, ensure that a patient receives an adequate trial of at least two classes of laxatives administered on a regular schedule, not just “as needed,” the guideline specifies. For example, a patient might receive a 2-week trial of a daily osmotic laxative plus a stimulant laxative two to three times weekly. The guideline authors suggest restricting the use of enemas to rescue therapy. They also note that consuming more fiber tends not to help patients with OIC because fiber does not affect colonic motility.
For truly laxative-refractory OIC, the guidelines recommend escalating treatment to peripherally acting mu-opioid receptor antagonists (PAMORAs). These drugs restore the function of the enteric nervous system by blocking mu-opioid receptors in the gut. Among the PAMORAs, the guideline strongly recommends the use of naldemedine or naloxegol over no treatment, based on robust data from randomized, double-blind, placebo-controlled trials. In the phase 3 COMPOSE 1, 2, and 3 trials, about 52% of patients who received naldemedine achieved at least three spontaneous bowel movements per week, compared with 35% of patients who received placebo. Additionally, in a 52-week safety and efficacy study (COMPOSE 3), naldemedine was associated with one more spontaneous bowel movement per week versus placebo and with a low absolute increase in adverse events.
The guideline bases its strong recommendation for naloxegol on moderate-quality data from three studies, including two phase 3, double-blind, randomized, placebo-controlled trials. Although at least five randomized, controlled trials have evaluated methylnaltrexone, the evidence was low quality and therefore the guideline only conditionally recommends prescribing this PAMORA over no treatment.
The guideline also makes no recommendation on the use of the intestinal secretagogue lubiprostone or the 5HT agonist prucalopride. Studies of lubiprostone were limited by possible reporting bias and showed no clear treatment benefit, the authors state. They describe a similar evidence gap for prucalopride, noting that at least one trial ended early without publication of the findings. They recommend further studying lubiprostone as well as prucalopride and other highly selective 5-HT4 agonists for treating OIC. Head-to-head trials would help guide treatment choice for patients with laxative-refractory OIC, they add. “Cost-effectiveness studies are also lacking in this field, which could inform prescribing strategy, particularly for newer, more expensive agents.”
For patients with suspected opioid-induced constipation, start by taking a careful history of defecation and dietary patterns, stool consistency, incomplete evacuation, and “alarm symptoms,” such as bloody stools or weight loss, state new guidelines from the American Gastroenterological Association in Gastroenterology.
Clinicians also should rule out other causes of constipation, such as pelvic outlet dysfunction, mechanical obstruction, metabolic abnormalities, and comorbidities or concurrent medications, wrote Seth D. Crockett, MD, MPH, of the University of North Carolina at Chapel Hill, together with his associates. The guideline was published online Sept. 1.
Opioid therapy can lead to a range of gastrointestinal symptoms, such as constipation, gastroesophageal reflux, nausea and vomiting, bloating, and abdominal pain. Among these, constipation is by far the most common and debilitating, the guideline notes. In past studies, 40%-80% of patients who received opioids developed opioid-induced constipation (OIC), a more severe presentation that involves a combination of reduced stool frequency in addition to other symptoms, such as harder stools, new or worsening straining during defecation, and a sense of incomplete rectal evacuation.
Treating OIC should start with lifestyle interventions, such as drinking more fluids, toileting as soon as possible when feeling the urge to defecate, and adding regular moderate exercise whenever tolerable, the guideline advises. For patients on oral or parenteral therapy, consider switching to an equianalgesic dose of a less-constipating opioid, such as transdermal fentanyl or oxycodone-naloxone combination therapy.
Many patients with OIC require interventions beyond lifestyle changes or opioid switching. For these patients, the guideline advises starting with conventional laxative therapies based on their safety, low cost, and “established efficacy” in the OIC setting. Options include stool softeners (docusate sodium), osmotic laxatives (polyethylene glycol, magnesium hydroxide, magnesium citrate, and lactulose), lubricants (mineral oil), and stimulant laxatives (bisacodyl, sodium picosulfate, and senna). “Of note, there is little evidence that routine use of stimulant laxatives is harmful to the colon, despite widespread concern to the contrary,” the guideline states. Although randomized, controlled trials have not evaluated particular laxative combinations or titrations for OIC, the best evidence supports stimulant and osmotic laxative therapy, the authors note.
Before deeming any case of OIC laxative refractory, ensure that a patient receives an adequate trial of at least two classes of laxatives administered on a regular schedule, not just “as needed,” the guideline specifies. For example, a patient might receive a 2-week trial of a daily osmotic laxative plus a stimulant laxative two to three times weekly. The guideline authors suggest restricting the use of enemas to rescue therapy. They also note that consuming more fiber tends not to help patients with OIC because fiber does not affect colonic motility.
For truly laxative-refractory OIC, the guidelines recommend escalating treatment to peripherally acting mu-opioid receptor antagonists (PAMORAs). These drugs restore the function of the enteric nervous system by blocking mu-opioid receptors in the gut. Among the PAMORAs, the guideline strongly recommends the use of naldemedine or naloxegol over no treatment, based on robust data from randomized, double-blind, placebo-controlled trials. In the phase 3 COMPOSE 1, 2, and 3 trials, about 52% of patients who received naldemedine achieved at least three spontaneous bowel movements per week, compared with 35% of patients who received placebo. Additionally, in a 52-week safety and efficacy study (COMPOSE 3), naldemedine was associated with one more spontaneous bowel movement per week versus placebo and with a low absolute increase in adverse events.
The guideline bases its strong recommendation for naloxegol on moderate-quality data from three studies, including two phase 3, double-blind, randomized, placebo-controlled trials. Although at least five randomized, controlled trials have evaluated methylnaltrexone, the evidence was low quality and therefore the guideline only conditionally recommends prescribing this PAMORA over no treatment.
The guideline also makes no recommendation on the use of the intestinal secretagogue lubiprostone or the 5HT agonist prucalopride. Studies of lubiprostone were limited by possible reporting bias and showed no clear treatment benefit, the authors state. They describe a similar evidence gap for prucalopride, noting that at least one trial ended early without publication of the findings. They recommend further studying lubiprostone as well as prucalopride and other highly selective 5-HT4 agonists for treating OIC. Head-to-head trials would help guide treatment choice for patients with laxative-refractory OIC, they add. “Cost-effectiveness studies are also lacking in this field, which could inform prescribing strategy, particularly for newer, more expensive agents.”
For patients with suspected opioid-induced constipation, start by taking a careful history of defecation and dietary patterns, stool consistency, incomplete evacuation, and “alarm symptoms,” such as bloody stools or weight loss, state new guidelines from the American Gastroenterological Association in Gastroenterology.
Clinicians also should rule out other causes of constipation, such as pelvic outlet dysfunction, mechanical obstruction, metabolic abnormalities, and comorbidities or concurrent medications, wrote Seth D. Crockett, MD, MPH, of the University of North Carolina at Chapel Hill, together with his associates. The guideline was published online Sept. 1.
Opioid therapy can lead to a range of gastrointestinal symptoms, such as constipation, gastroesophageal reflux, nausea and vomiting, bloating, and abdominal pain. Among these, constipation is by far the most common and debilitating, the guideline notes. In past studies, 40%-80% of patients who received opioids developed opioid-induced constipation (OIC), a more severe presentation that involves a combination of reduced stool frequency in addition to other symptoms, such as harder stools, new or worsening straining during defecation, and a sense of incomplete rectal evacuation.
Treating OIC should start with lifestyle interventions, such as drinking more fluids, toileting as soon as possible when feeling the urge to defecate, and adding regular moderate exercise whenever tolerable, the guideline advises. For patients on oral or parenteral therapy, consider switching to an equianalgesic dose of a less-constipating opioid, such as transdermal fentanyl or oxycodone-naloxone combination therapy.
Many patients with OIC require interventions beyond lifestyle changes or opioid switching. For these patients, the guideline advises starting with conventional laxative therapies based on their safety, low cost, and “established efficacy” in the OIC setting. Options include stool softeners (docusate sodium), osmotic laxatives (polyethylene glycol, magnesium hydroxide, magnesium citrate, and lactulose), lubricants (mineral oil), and stimulant laxatives (bisacodyl, sodium picosulfate, and senna). “Of note, there is little evidence that routine use of stimulant laxatives is harmful to the colon, despite widespread concern to the contrary,” the guideline states. Although randomized, controlled trials have not evaluated particular laxative combinations or titrations for OIC, the best evidence supports stimulant and osmotic laxative therapy, the authors note.
Before deeming any case of OIC laxative refractory, ensure that a patient receives an adequate trial of at least two classes of laxatives administered on a regular schedule, not just “as needed,” the guideline specifies. For example, a patient might receive a 2-week trial of a daily osmotic laxative plus a stimulant laxative two to three times weekly. The guideline authors suggest restricting the use of enemas to rescue therapy. They also note that consuming more fiber tends not to help patients with OIC because fiber does not affect colonic motility.
For truly laxative-refractory OIC, the guidelines recommend escalating treatment to peripherally acting mu-opioid receptor antagonists (PAMORAs). These drugs restore the function of the enteric nervous system by blocking mu-opioid receptors in the gut. Among the PAMORAs, the guideline strongly recommends the use of naldemedine or naloxegol over no treatment, based on robust data from randomized, double-blind, placebo-controlled trials. In the phase 3 COMPOSE 1, 2, and 3 trials, about 52% of patients who received naldemedine achieved at least three spontaneous bowel movements per week, compared with 35% of patients who received placebo. Additionally, in a 52-week safety and efficacy study (COMPOSE 3), naldemedine was associated with one more spontaneous bowel movement per week versus placebo and with a low absolute increase in adverse events.
The guideline bases its strong recommendation for naloxegol on moderate-quality data from three studies, including two phase 3, double-blind, randomized, placebo-controlled trials. Although at least five randomized, controlled trials have evaluated methylnaltrexone, the evidence was low quality and therefore the guideline only conditionally recommends prescribing this PAMORA over no treatment.
The guideline also makes no recommendation on the use of the intestinal secretagogue lubiprostone or the 5HT agonist prucalopride. Studies of lubiprostone were limited by possible reporting bias and showed no clear treatment benefit, the authors state. They describe a similar evidence gap for prucalopride, noting that at least one trial ended early without publication of the findings. They recommend further studying lubiprostone as well as prucalopride and other highly selective 5-HT4 agonists for treating OIC. Head-to-head trials would help guide treatment choice for patients with laxative-refractory OIC, they add. “Cost-effectiveness studies are also lacking in this field, which could inform prescribing strategy, particularly for newer, more expensive agents.”
FROM GASTROENTEROLOGY
Study examines POEM learning curve
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: One hundred cases was the typical learning curve for peroral endoscopic myotomy (POEM).
Major finding: The composite rate of technical failure or adverse events was 4%. An adjusted analysis showed that the rate of this negative composite outcome fell gradually after an endoscopist had performed his or her first 100 cases.
Study details: Single-center retrospective study of 1,346 patients undergoing POEM.
Disclosures: Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest..
Source: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Even modest alcohol use may worsen NAFLD
Patients with nonalcoholic fatty liver disease who consumed modest quantities of alcohol had significantly less improvement in steatosis and significantly lower odds of resolution of nonalcoholic steatohepatitis, compared with nondrinkers, according to the results of a longitudinal cohort study published in the Clinical Gastroenterology and Hepatology.
Modest drinkers also had significantly less improvement in their AST levels, compared with nondrinkers, said Veeral Ajmera, MD, of the University of California, San Diego, and his associates. “Importantly, our results suggest that cessation of alcohol use may mitigate these changes,” they wrote. Clinicians should consider the spectrum of nonalcoholic fatty liver disease (NAFLD), and especially nonalcoholic steatohepatitis (NASH), when making recommendations about alcohol use. “More advanced NAFLD severity may warrant counseling against [even] modest alcohol use.”
More than one in three adults in the United States has NAFLD and about two-thirds drink alcohol, almost always in moderation, the researchers noted. Modest alcohol use has been linked to decreased cardiovascular risk, which is particularly relevant because patients with NAFLD tend to have risk factors for cardiovascular disease. Results from at least two cross-sectional studies also suggest modest drinkers with NAFLD have less severe histology, including less NASH and fibrosis. However, modest drinkers tend to be more physically active, with lower body mass indices, higher physical activity levels, and less obesity, which are potential confounders. To better understand the effects of modest alcohol consumption on NAFLD, the researchers studied adults with NAFLD who participated in studies conducted by the multicenter NASH Clinical Research Network.
The 285 participants were typically aged in their late 40s, female, white, and obese, with an average body mass index of 34.7 kg/m2. In all, 168 participants (59%) reported consuming up to two drinks per day, while 41% abstained from alcohol use. During an average of 47 months between biopsies (standard deviation, 26 months), nondrinkers averaged a 0.49 reduction in steatosis grade, significantly more than that of modest drinkers (reduction, 0.30; P = .04). Nondrinkers also had a greater decrease in mean AST level (7 U/L), compared with drinkers (2 U/L; P = .04).
A total of 64% of patients were classified as having definite NASH, 19% had NAFLD without NASH, and 17% had borderline NASH. At baseline, 23% of patients did not have fibrosis, 32% had stage 1 fibrosis, 21% had stage 2, 21% had stage 3, and 3% had stage 4. Modest drinkers were more likely to be white and were less likely to be diagnosed with definitive NASH at baseline. After controlling for these potential confounders, modest drinkers had significantly lower odds of NASH resolution, compared with nondrinkers (adjusted odds ratio, 0.32; 95% confidence interval, 0.11-0.92; P = .04).
“[The] presence of NASH has consistently been shown to predict increased risk for fibrosis progression, and therefore, our finding of less NASH resolution among consistent modest drinkers is clinically relevant,” the investigators wrote. “Although we were unable to assess the association between modest alcohol consumption and cardiovascular risk, we did not see any significant changes in measured metabolic risk factors with known associations with cardiovascular disease including low-density lipoprotein and high-density lipoprotein cholesterol and insulin resistance.”
Funders of the study included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Sciences, the Advanced/Transplant Hepatology Fellowship, the American Association for the Study of Liver Diseases Foundation, and the Intramural Research Program of the National Institutes of Health.
SOURCE: Ajmera V et al. Clin Gastroenterol Hepatol. 2018 Mar 14. doi: 10.1016/j.cgh.2018.01.026.
Patients with nonalcoholic fatty liver disease who consumed modest quantities of alcohol had significantly less improvement in steatosis and significantly lower odds of resolution of nonalcoholic steatohepatitis, compared with nondrinkers, according to the results of a longitudinal cohort study published in the Clinical Gastroenterology and Hepatology.
Modest drinkers also had significantly less improvement in their AST levels, compared with nondrinkers, said Veeral Ajmera, MD, of the University of California, San Diego, and his associates. “Importantly, our results suggest that cessation of alcohol use may mitigate these changes,” they wrote. Clinicians should consider the spectrum of nonalcoholic fatty liver disease (NAFLD), and especially nonalcoholic steatohepatitis (NASH), when making recommendations about alcohol use. “More advanced NAFLD severity may warrant counseling against [even] modest alcohol use.”
More than one in three adults in the United States has NAFLD and about two-thirds drink alcohol, almost always in moderation, the researchers noted. Modest alcohol use has been linked to decreased cardiovascular risk, which is particularly relevant because patients with NAFLD tend to have risk factors for cardiovascular disease. Results from at least two cross-sectional studies also suggest modest drinkers with NAFLD have less severe histology, including less NASH and fibrosis. However, modest drinkers tend to be more physically active, with lower body mass indices, higher physical activity levels, and less obesity, which are potential confounders. To better understand the effects of modest alcohol consumption on NAFLD, the researchers studied adults with NAFLD who participated in studies conducted by the multicenter NASH Clinical Research Network.
The 285 participants were typically aged in their late 40s, female, white, and obese, with an average body mass index of 34.7 kg/m2. In all, 168 participants (59%) reported consuming up to two drinks per day, while 41% abstained from alcohol use. During an average of 47 months between biopsies (standard deviation, 26 months), nondrinkers averaged a 0.49 reduction in steatosis grade, significantly more than that of modest drinkers (reduction, 0.30; P = .04). Nondrinkers also had a greater decrease in mean AST level (7 U/L), compared with drinkers (2 U/L; P = .04).
A total of 64% of patients were classified as having definite NASH, 19% had NAFLD without NASH, and 17% had borderline NASH. At baseline, 23% of patients did not have fibrosis, 32% had stage 1 fibrosis, 21% had stage 2, 21% had stage 3, and 3% had stage 4. Modest drinkers were more likely to be white and were less likely to be diagnosed with definitive NASH at baseline. After controlling for these potential confounders, modest drinkers had significantly lower odds of NASH resolution, compared with nondrinkers (adjusted odds ratio, 0.32; 95% confidence interval, 0.11-0.92; P = .04).
“[The] presence of NASH has consistently been shown to predict increased risk for fibrosis progression, and therefore, our finding of less NASH resolution among consistent modest drinkers is clinically relevant,” the investigators wrote. “Although we were unable to assess the association between modest alcohol consumption and cardiovascular risk, we did not see any significant changes in measured metabolic risk factors with known associations with cardiovascular disease including low-density lipoprotein and high-density lipoprotein cholesterol and insulin resistance.”
Funders of the study included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Sciences, the Advanced/Transplant Hepatology Fellowship, the American Association for the Study of Liver Diseases Foundation, and the Intramural Research Program of the National Institutes of Health.
SOURCE: Ajmera V et al. Clin Gastroenterol Hepatol. 2018 Mar 14. doi: 10.1016/j.cgh.2018.01.026.
Patients with nonalcoholic fatty liver disease who consumed modest quantities of alcohol had significantly less improvement in steatosis and significantly lower odds of resolution of nonalcoholic steatohepatitis, compared with nondrinkers, according to the results of a longitudinal cohort study published in the Clinical Gastroenterology and Hepatology.
Modest drinkers also had significantly less improvement in their AST levels, compared with nondrinkers, said Veeral Ajmera, MD, of the University of California, San Diego, and his associates. “Importantly, our results suggest that cessation of alcohol use may mitigate these changes,” they wrote. Clinicians should consider the spectrum of nonalcoholic fatty liver disease (NAFLD), and especially nonalcoholic steatohepatitis (NASH), when making recommendations about alcohol use. “More advanced NAFLD severity may warrant counseling against [even] modest alcohol use.”
More than one in three adults in the United States has NAFLD and about two-thirds drink alcohol, almost always in moderation, the researchers noted. Modest alcohol use has been linked to decreased cardiovascular risk, which is particularly relevant because patients with NAFLD tend to have risk factors for cardiovascular disease. Results from at least two cross-sectional studies also suggest modest drinkers with NAFLD have less severe histology, including less NASH and fibrosis. However, modest drinkers tend to be more physically active, with lower body mass indices, higher physical activity levels, and less obesity, which are potential confounders. To better understand the effects of modest alcohol consumption on NAFLD, the researchers studied adults with NAFLD who participated in studies conducted by the multicenter NASH Clinical Research Network.
The 285 participants were typically aged in their late 40s, female, white, and obese, with an average body mass index of 34.7 kg/m2. In all, 168 participants (59%) reported consuming up to two drinks per day, while 41% abstained from alcohol use. During an average of 47 months between biopsies (standard deviation, 26 months), nondrinkers averaged a 0.49 reduction in steatosis grade, significantly more than that of modest drinkers (reduction, 0.30; P = .04). Nondrinkers also had a greater decrease in mean AST level (7 U/L), compared with drinkers (2 U/L; P = .04).
A total of 64% of patients were classified as having definite NASH, 19% had NAFLD without NASH, and 17% had borderline NASH. At baseline, 23% of patients did not have fibrosis, 32% had stage 1 fibrosis, 21% had stage 2, 21% had stage 3, and 3% had stage 4. Modest drinkers were more likely to be white and were less likely to be diagnosed with definitive NASH at baseline. After controlling for these potential confounders, modest drinkers had significantly lower odds of NASH resolution, compared with nondrinkers (adjusted odds ratio, 0.32; 95% confidence interval, 0.11-0.92; P = .04).
“[The] presence of NASH has consistently been shown to predict increased risk for fibrosis progression, and therefore, our finding of less NASH resolution among consistent modest drinkers is clinically relevant,” the investigators wrote. “Although we were unable to assess the association between modest alcohol consumption and cardiovascular risk, we did not see any significant changes in measured metabolic risk factors with known associations with cardiovascular disease including low-density lipoprotein and high-density lipoprotein cholesterol and insulin resistance.”
Funders of the study included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Sciences, the Advanced/Transplant Hepatology Fellowship, the American Association for the Study of Liver Diseases Foundation, and the Intramural Research Program of the National Institutes of Health.
SOURCE: Ajmera V et al. Clin Gastroenterol Hepatol. 2018 Mar 14. doi: 10.1016/j.cgh.2018.01.026.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Consider counseling patients with more advanced nonalcoholic fatty liver disease to avoid alcohol.
Major finding: Compared with nondrinkers, patients who reported modest alcohol use had significantly less improvement in steatosis and significantly lower odds of resolution of nonalcoholic steatohepatitis (P = .04 for both comparisons).
Study details: A longitudinal cohort study of 285 adults with nonalcoholic fatty liver disease with paired biopsy specimens obtained an average of 4 years apart.
Disclosures: Funders of the study included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Sciences, the Advanced/Transplant Hepatology Fellowship, the American Association for the Study of Liver Diseases Foundation, and the Intramural Research Program of the National Institutes of Health.
Source: Ajmera V et al. Clin Gastroenterol Hepatol. 2018 Mar 14. doi: 10.1016/j.cgh.2018.01.026.
Pancreatic surveillance identified resectable cancers
Long-term pancreatic surveillance of high-risk patients identified cancers while they were still resectable, and 85% of such patients remained alive 3 years after diagnosis, researchers reported.
“Among individuals undergoing pancreatic surveillance, specific detectable lesions with worrisome features predicted neoplastic progression. The short-term outcomes of patients with screening-detected PDACs [pancreatic ductal adenocarcinomas] improved,” wrote Marcia Irene Canto, MD, MHS, of the Johns Hopkins University, Baltimore, together with her associates in the September issue of Gastroenterology.
The lifetime risk of PDAC is about 1.5%, the researchers noted. Consequently, the U.S. Preventive Services Task Force does not recommend pancreatic surveillance at a population level. However, pancreatic screening is being evaluated for individuals who are at significantly elevated risk of PDAC, including those with at least two first-degree relatives with PDAC or who have germline mutations in BRCA1, BRCA2, PALB2, PRSS1 (hereditary pancreatitis), CDKN2A, MLH1, MSH2, MSH6, PMS2 (Lynch syndrome), or STK11 (Peutz-Jeghers syndrome).
For the study, Dr. Canto and her associates analyzed data from 354 such high-risk individuals enrolled in the CAPS (Cancer of the Pancreas Screening) cohort studies, which were conducted at tertiary care academic centers during 1998-2014. All participants underwent endoscopic ultrasound at baseline, followed by surveillance with endoscopic ultrasound, magnetic resonance imaging, computed tomography, or some combination of these modalities. Patients who developed pancreatic cancer or high-grade dysplasia were offered surgery.
In all, 68 patients (19%) developed pancreatic lesions with worrisome features, such as solid masses, multiple cysts, mural nodules, thickened or enhancing walls, cysts exceeding 3 cm in size or that grew more than 4 mm annually, a greater than 5-mm dilation of the main pancreatic duct, or an abrupt change in duct caliber. The lesions developed over a median of 13.1 months (interquartile range, 0.2-52 months).
A total of 7% of patients had neoplastic progression, including 14 cases of PDAC and 10 cases of high-grade dysplasia. Median times from baseline to detection of PDAC were 4.8 years overall (IQR, 1.6-6.9 years), 1.7 years (IQR, 0.5-4.4 years) among patients aged at least 60 years at baseline, and 5.2 years among younger patients (IQR, 0.4-8 years). Patients developed PDAC at a median of 67 years old.
Among 10 PDACs detected by surveillance, 9 were resectable. Three patients subsequently died of PDAC, while one patient died of complications of gastric cancer surgery. However, 85% of patients survived for at least 3 years after surgical resection of PDAC. The remaining four cases of PDAC were detected outside surveillance or after patients stopped surveillance.
The 10 cases of high-grade dysplasia consisted of intraductal papillary mucinous neoplasm with high-grade dysplasia or high-grade pancreatic intraepithelial neoplasia. Patients whose PDAC or high-grade dysplasia was detected by surveillance survived a median of 5.3 years, while patients whose surveillance was late or stopped and who subsequently developed neoplasia survived a median of only 1.4 years after diagnosis (P less than .0001).
Funders included the Pancreatic Cancer Action Network, Lustgarten Foundation for Pancreatic Cancer Research, the John and Peter Hooven Memorial Endowment, Hugh and Rachel Victor, and ChiRhoClin. Dr. Canto had no disclosures. Three coinvestigators disclosed royalties for licensing of PALB2 as a pancreatic cancer susceptibility gene.
SOURCE: Canto MI et al. Gastroenterology. 2018 May 24. doi: 10.1053/j.gastro.2018.05.035
Long-term pancreatic surveillance of high-risk patients identified cancers while they were still resectable, and 85% of such patients remained alive 3 years after diagnosis, researchers reported.
“Among individuals undergoing pancreatic surveillance, specific detectable lesions with worrisome features predicted neoplastic progression. The short-term outcomes of patients with screening-detected PDACs [pancreatic ductal adenocarcinomas] improved,” wrote Marcia Irene Canto, MD, MHS, of the Johns Hopkins University, Baltimore, together with her associates in the September issue of Gastroenterology.
The lifetime risk of PDAC is about 1.5%, the researchers noted. Consequently, the U.S. Preventive Services Task Force does not recommend pancreatic surveillance at a population level. However, pancreatic screening is being evaluated for individuals who are at significantly elevated risk of PDAC, including those with at least two first-degree relatives with PDAC or who have germline mutations in BRCA1, BRCA2, PALB2, PRSS1 (hereditary pancreatitis), CDKN2A, MLH1, MSH2, MSH6, PMS2 (Lynch syndrome), or STK11 (Peutz-Jeghers syndrome).
For the study, Dr. Canto and her associates analyzed data from 354 such high-risk individuals enrolled in the CAPS (Cancer of the Pancreas Screening) cohort studies, which were conducted at tertiary care academic centers during 1998-2014. All participants underwent endoscopic ultrasound at baseline, followed by surveillance with endoscopic ultrasound, magnetic resonance imaging, computed tomography, or some combination of these modalities. Patients who developed pancreatic cancer or high-grade dysplasia were offered surgery.
In all, 68 patients (19%) developed pancreatic lesions with worrisome features, such as solid masses, multiple cysts, mural nodules, thickened or enhancing walls, cysts exceeding 3 cm in size or that grew more than 4 mm annually, a greater than 5-mm dilation of the main pancreatic duct, or an abrupt change in duct caliber. The lesions developed over a median of 13.1 months (interquartile range, 0.2-52 months).
A total of 7% of patients had neoplastic progression, including 14 cases of PDAC and 10 cases of high-grade dysplasia. Median times from baseline to detection of PDAC were 4.8 years overall (IQR, 1.6-6.9 years), 1.7 years (IQR, 0.5-4.4 years) among patients aged at least 60 years at baseline, and 5.2 years among younger patients (IQR, 0.4-8 years). Patients developed PDAC at a median of 67 years old.
Among 10 PDACs detected by surveillance, 9 were resectable. Three patients subsequently died of PDAC, while one patient died of complications of gastric cancer surgery. However, 85% of patients survived for at least 3 years after surgical resection of PDAC. The remaining four cases of PDAC were detected outside surveillance or after patients stopped surveillance.
The 10 cases of high-grade dysplasia consisted of intraductal papillary mucinous neoplasm with high-grade dysplasia or high-grade pancreatic intraepithelial neoplasia. Patients whose PDAC or high-grade dysplasia was detected by surveillance survived a median of 5.3 years, while patients whose surveillance was late or stopped and who subsequently developed neoplasia survived a median of only 1.4 years after diagnosis (P less than .0001).
Funders included the Pancreatic Cancer Action Network, Lustgarten Foundation for Pancreatic Cancer Research, the John and Peter Hooven Memorial Endowment, Hugh and Rachel Victor, and ChiRhoClin. Dr. Canto had no disclosures. Three coinvestigators disclosed royalties for licensing of PALB2 as a pancreatic cancer susceptibility gene.
SOURCE: Canto MI et al. Gastroenterology. 2018 May 24. doi: 10.1053/j.gastro.2018.05.035
Long-term pancreatic surveillance of high-risk patients identified cancers while they were still resectable, and 85% of such patients remained alive 3 years after diagnosis, researchers reported.
“Among individuals undergoing pancreatic surveillance, specific detectable lesions with worrisome features predicted neoplastic progression. The short-term outcomes of patients with screening-detected PDACs [pancreatic ductal adenocarcinomas] improved,” wrote Marcia Irene Canto, MD, MHS, of the Johns Hopkins University, Baltimore, together with her associates in the September issue of Gastroenterology.
The lifetime risk of PDAC is about 1.5%, the researchers noted. Consequently, the U.S. Preventive Services Task Force does not recommend pancreatic surveillance at a population level. However, pancreatic screening is being evaluated for individuals who are at significantly elevated risk of PDAC, including those with at least two first-degree relatives with PDAC or who have germline mutations in BRCA1, BRCA2, PALB2, PRSS1 (hereditary pancreatitis), CDKN2A, MLH1, MSH2, MSH6, PMS2 (Lynch syndrome), or STK11 (Peutz-Jeghers syndrome).
For the study, Dr. Canto and her associates analyzed data from 354 such high-risk individuals enrolled in the CAPS (Cancer of the Pancreas Screening) cohort studies, which were conducted at tertiary care academic centers during 1998-2014. All participants underwent endoscopic ultrasound at baseline, followed by surveillance with endoscopic ultrasound, magnetic resonance imaging, computed tomography, or some combination of these modalities. Patients who developed pancreatic cancer or high-grade dysplasia were offered surgery.
In all, 68 patients (19%) developed pancreatic lesions with worrisome features, such as solid masses, multiple cysts, mural nodules, thickened or enhancing walls, cysts exceeding 3 cm in size or that grew more than 4 mm annually, a greater than 5-mm dilation of the main pancreatic duct, or an abrupt change in duct caliber. The lesions developed over a median of 13.1 months (interquartile range, 0.2-52 months).
A total of 7% of patients had neoplastic progression, including 14 cases of PDAC and 10 cases of high-grade dysplasia. Median times from baseline to detection of PDAC were 4.8 years overall (IQR, 1.6-6.9 years), 1.7 years (IQR, 0.5-4.4 years) among patients aged at least 60 years at baseline, and 5.2 years among younger patients (IQR, 0.4-8 years). Patients developed PDAC at a median of 67 years old.
Among 10 PDACs detected by surveillance, 9 were resectable. Three patients subsequently died of PDAC, while one patient died of complications of gastric cancer surgery. However, 85% of patients survived for at least 3 years after surgical resection of PDAC. The remaining four cases of PDAC were detected outside surveillance or after patients stopped surveillance.
The 10 cases of high-grade dysplasia consisted of intraductal papillary mucinous neoplasm with high-grade dysplasia or high-grade pancreatic intraepithelial neoplasia. Patients whose PDAC or high-grade dysplasia was detected by surveillance survived a median of 5.3 years, while patients whose surveillance was late or stopped and who subsequently developed neoplasia survived a median of only 1.4 years after diagnosis (P less than .0001).
Funders included the Pancreatic Cancer Action Network, Lustgarten Foundation for Pancreatic Cancer Research, the John and Peter Hooven Memorial Endowment, Hugh and Rachel Victor, and ChiRhoClin. Dr. Canto had no disclosures. Three coinvestigators disclosed royalties for licensing of PALB2 as a pancreatic cancer susceptibility gene.
SOURCE: Canto MI et al. Gastroenterology. 2018 May 24. doi: 10.1053/j.gastro.2018.05.035
FROM GASTROENTEROLOGY
Key clinical point: Pancreatic surveillance of high-risk individuals identified neoplasias when they were still resectable.
Major finding: Nine of ten tumors detected by surveillance were resectable, and 85% of patients remained alive 3 years after surgery, versus 25% of patients who were diagnosed after stopping or delaying surveillance (P less than .001).
Study details: Prospective cohort study of 354 high-risk individuals with 16 years of follow-up.
Disclosures: Funders included the Pancreatic Cancer Action Network, Lustgarten Foundation for Pancreatic Cancer Research, the John and Peter Hooven Memorial Endowment, Hugh and Rachel Victor, and ChiRhoClin. Dr. Canto had no disclosures. Three coinvestigators disclosed royalties for licensing of PALB2 as a pancreatic cancer susceptibility gene.
Source: Canto MI et al. Gastroenterology. 2018 May 24. doi: 10.1053/j.gastro.2018.05.035.
Avatrombopag cut procedure-related transfusions in patients with thrombocytopenia, chronic liver disease
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Thrombocytopenia in cirrhosis is frequent and multifactorial and includes sequestration in the spleen, reduced liver-derived thrombopoietin, bone marrow toxicity, and autoimmunity towards platelets. Severe thrombocytopenia (less than 50/nL) is rare in cirrhotic patients, but when it occurs may prevent required procedures from being performed or require platelet transfusions, which are associated with significant risks.
Previous attempts to increase platelets in cirrhotic patients with thrombopoietin agonists were halted because of increased frequency of portal vein thrombosis and hepatic decompensation.
Now avatrombopag has been specifically licensed with a 5-day regimen to increase platelets prior to elective interventions in severely thrombocytopenic (less than 50/nL) patients with chronic liver disease with a seemingly better safety profile than earlier treatments and good efficacy. The patient groups studied in the licensing trial had slightly milder but not significantly different liver disease, compared with those in the eltrombopag studies. The key difference was a pretreatment requirement of a portal vein flow of more than 10 cm/sec prior to enrollment, which likely reduced the risk of portal vein thrombosis. It is important that providers ready to use avatrombopag are aware of this.
Importantly, no data are currently available for patients with a Model for End-Stage Liver Disease score greater than 24, and very limited data are available for patients with Child B and Child C cirrhosis.
Given this limitation, careful judgment will be needed; a pretreatment portal vein flow may be advisable, though not a label requirement.
An observational study, NCT03554759, in patients with chronic liver disease and thrombocytopenia is ongoing and will further confirm the likely safety of avatrombopag.
Hans L. Tillmann, MD, is a clinical associate professor, East Carolina University, Greenville, and staff physician, Greenville (N.C.) VA Health Care Center. He has no relevant conflicts of interest.
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
Once-daily treatment with the oral second-generation thrombopoietin agonist avatrombopag (Doptelet) significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures, according to the results of two international, randomized, double-blind, phase III, placebo-controlled trials reported in the September issue of Gastroenterology.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia, versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group, versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
These results led the Food and Drug Administration to approve avatrombopag in May 2018 under its priority review process. The novel therapy “may be a safe and effective alternative to platelet transfusions” that could simplify the clinical management of patients with chronic liver disease and thrombocytopenia, Norah Terrault, MD, MPH, and her associates wrote in Gastroenterology.
The ADAPT-1 study included 231 patients, while ADAPT-2 included 204 patients. In each trial, patients were randomized on a 2:1 basis to receive oral avatrombopag or placebo once daily for 5 consecutive days. Patients in the intervention arms received 60 mg avatrombopag if their baseline platelet count was less than 40 x 109 per liter, and 40 mg if their baseline platelet count was 40-50 x 109 per liter. Procedures were scheduled for 10-13 days after treatment initiation.
“Platelet counts increased by [treatment] day 4, peaked at days 10-13, and then returned to baseline levels by day 35,” the researchers reported. Among ADAPT-1 patients with low baseline counts, 69% of avatrombopag recipients reached a prespecified target of at least 50 x 109 platelets per liter on their procedure day, versus 4% of placebo recipients (P less than .0001). Corresponding proportions in ADAPT-2 were 67% and 7%, respectively (P less than .0001). Among patients with higher baseline counts, 88% and 20% achieved the target, respectively, in ADAPT-1 (P less than .0001), as did 93% versus 39%, respectively, in ADAPT-2 (P less than .0001).
Avatrombopag and placebo produced similar rates of treatment-emergent adverse events. These most often consisted of abdominal pain, dyspepsia, nausea, pyrexia, dizziness, and headache. Only three avatrombopag patients developed platelet counts above 200 x 109 per liter, and they all remained asymptomatic, the investigators said.
Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, Bristol-Myers Squibb, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
SOURCE: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
FROM GASTROENTEROLOGY
Key clinical point: Once-daily treatment with oral avatrombopag significantly reduced the need for platelet transfusion and rescue therapy for up to 7 days after patients with chronic liver disease and thrombocytopenia underwent scheduled procedures.
Major finding: In the ADAPT-1 trial, 66% of patients in the 60-mg arm met this primary endpoint, as did 88% of patients who received 40 mg for less severe thrombocytopenia versus 23% and 38% of the placebo arms, respectively (P less than .001 for each comparison). In the ADAPT-2 trial, 69% of the 60-mg group met the primary endpoint, as did 88% of the 40-mg group versus 35% and 33% of the respective placebo groups (P less than .001 for each comparison).
Study details: ADAPT-1 and ADAPT-2, international, randomized, double-blind, placebo-controlled, phase III trials.
Disclosures: Dova Pharmaceuticals makes avatrombopag and funded medical writing support. Dr. Terrault and three coinvestigators disclosed ties to AbbVie, Allergan, BMS, Eisai, Gilead, Merck, and other pharmaceutical companies. One coinvestigator is chief medical officer of Dova, helped analyze the data and write the manuscript, and gave final approval of the submitted version.
Source: Terrault N et al. Gastroenterology. 2018 May 17. doi: 10.1053/j.gastro.2018.05.025.
Simulation could help guide MM treatment
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.
A simulation could help personalize therapy for multiple myeloma (MM), according to researchers.
With the help of gene expression signatures, a simulated treatment learning model identified which MM patients would have the greatest progression-free survival (PFS) benefit from treatment with bortezomib or lenalidomide.
Joske Ubels, of University Medical Center Utrecht in the Netherlands, and her colleagues described this research in Nature Communications.
“The key idea of simulated treatment learning is that a patient’s treatment benefit can be estimated by comparing [his or her] survival to a set of genetically similar patients [who] received the comparator treatment,” the researchers noted.
For this study, the team applied a simulated treatment learning model called GESTURE to two MM gene expression datasets. One set included patients who received bortezomib (and other therapies). The other included patients who received lenalidomide (and other therapies).
For the bortezomib dataset, the researchers combined data from three randomized, phase 3 trials of 910 MM patients (total therapy 2, total therapy 3, and HOVON-65/GMMG-HD4).
The model suggested that, in 19.8% of these patients, bortezomib would produce a two-fold greater PFS benefit than in the patient population as a whole.
For the lenalidomide dataset, the researchers obtained data on 662 MM patients in the CoMMpass trial.
The model suggested that, in 31.1% of these patients, lenalidomide would produce a three-fold greater PFS benefit than that observed in the patient population as a whole.
Based on these results, the researchers concluded that GESTURE “can derive clinically actionable gene expression signatures that enable a more personalized approach to treatment.”
The method requires a large dataset but could be useful for trials that have missed their primary endpoint, according to the researchers.
The team’s next step is to see if GESTURE makes useful treatment predictions for other cancers. The code needed to train and validate the model is available at github.com/jubels/GESTURE.
The Van Herk Fellowship provided support for this research. The lenalidomide dataset was created as part of the Multiple Myeloma Research Foundation Personalized Medicine Initiative.
Dr. Ubels and one co-investigator are employees of SkylineDx. Another co-investigator served on the company’s advisory board. All other study authors reported having no relevant conflicts of interest.