User login
Physicians face hurdles in following new task force fluoride recommendations
Pediatricians may face challenges in implementing new U.S. Preventive Services Task Force recommendations that advocate the provision of oral fluoride supplementation to children in fluoride-deficient areas and fluoride varnish to all children by primary care clinicians.
The speed with which the recommendations are applied in primary care settings likely will depend on state support, training availability, and insurer cooperation.
"The updated recommendations are a very important step forward toward improving oral health in children through collaborative care," Dr. Lee Savio Beers of Children’s National Medical Center, Washington, said in an interview. However, "primary care providers will face a number of barriers in implementing these recommendations, including workflow and staffing issues, access to training, and adequate payment."
The USPSTF guidelines, published in early May 2014, recommend that primary care providers prescribe oral fluoride supplementation starting at 6 months for children whose water supply is lacking in fluoride and that they apply fluoride varnish to the primary teeth of all children starting at primary tooth eruption. The recommendations cite evidence that show fluoride varnish and oral supplements help prevent dental caries in children aged 5 years and younger, and that the treatments’ benefits outweigh the potential harms of fluorosis (Pediatrics 2014[doi:10.15425/peds.2014-0483]). The recommendations update 2004 guidelines in which only oral fluoride supplementation was recommended for children in areas with fluoride levels below 0.6 ppm in their local drinking water. That recommendation remains.
Whether the treatments will be covered by insurers will depend greatly on the state and the insurer. In nearly every state, Medicaid currently reimburses providers for the provision of fluoride varnish, said Dr. Patricia Braun, a pediatrician at Denver Health’s Eastside Neighborhood Health Center, and at the University of Colorado. She is a member of the American Academy of Pediatrics Section on Oral Health.
"From the publically insured perspective, it has already been decided that (such treatments) are important," Dr. Braun said in an interview. "The next challenge will be to get private insurers to do the same. As the task force recommendations indicate, all kids are at risk for caries, some more than others ... and all benefit from these services, including those (who) are insured by private organizations."
Payment for the recommended treatments is an issue that state agencies, professional organizations, and oral health advocates should start investigating now, Dr. Beers added.
"It will be important for pediatric primary care providers, pediatric dentists, regulatory agencies, and payers to work together in each state or region to develop an implementation plan in order to ensure the best intake," she said. "This is not something primary care providers should be expected to implement without this type of comprehensive support, including, but not limited to training and payment."
Training for pediatricians is already available in many states. Most jurisdictions have oral education programs that have been running for some time, Dr. Braun said, such as Colorado’s Cavity Free at Three and North Carolina’s Into the Mouths of Babes. Physicians also can utilize online programs such as Smiles for Life, a national oral health curriculum developed by the Society of Teachers of Family Medicine.
Dr. Beers recommends doctors visit the American Academy of Pediatrics’ website for more information about oral health training programs and resources, the Protecting All Children’s Teeth curriculum and the Bright Futures resources.
"We don’t need to reinvent the wheel," Dr. Braun said. "A lot has really been developed in the last decade, and we can now take advantage of the education" available about these services.
Other challenges physicians may face in executing the recommendations include integrating the treatments into their routine practice, said Dr. Anupama Rao Tate, DMD, of Children’s National Medical Center, dentistry (oral health) department in Washington. For instance, physicians must decide whether the treatments should be provided as part of a well visit or independently.
In addition, electronic records may or may not have a place to track the services, Dr. Tate said. Conversations with parents also are necessary to help families understand why these services are being provided by their children’s primary care provider.
"Traditionally, dentistry has been separate from medicine," Dr. Tate said. Pediatricians are "going to have to change the mindset of parents and educate (them) as to why they’re doing something (pertaining to) dental health."
Pediatricians may face challenges in implementing new U.S. Preventive Services Task Force recommendations that advocate the provision of oral fluoride supplementation to children in fluoride-deficient areas and fluoride varnish to all children by primary care clinicians.
The speed with which the recommendations are applied in primary care settings likely will depend on state support, training availability, and insurer cooperation.
"The updated recommendations are a very important step forward toward improving oral health in children through collaborative care," Dr. Lee Savio Beers of Children’s National Medical Center, Washington, said in an interview. However, "primary care providers will face a number of barriers in implementing these recommendations, including workflow and staffing issues, access to training, and adequate payment."
The USPSTF guidelines, published in early May 2014, recommend that primary care providers prescribe oral fluoride supplementation starting at 6 months for children whose water supply is lacking in fluoride and that they apply fluoride varnish to the primary teeth of all children starting at primary tooth eruption. The recommendations cite evidence that show fluoride varnish and oral supplements help prevent dental caries in children aged 5 years and younger, and that the treatments’ benefits outweigh the potential harms of fluorosis (Pediatrics 2014[doi:10.15425/peds.2014-0483]). The recommendations update 2004 guidelines in which only oral fluoride supplementation was recommended for children in areas with fluoride levels below 0.6 ppm in their local drinking water. That recommendation remains.
Whether the treatments will be covered by insurers will depend greatly on the state and the insurer. In nearly every state, Medicaid currently reimburses providers for the provision of fluoride varnish, said Dr. Patricia Braun, a pediatrician at Denver Health’s Eastside Neighborhood Health Center, and at the University of Colorado. She is a member of the American Academy of Pediatrics Section on Oral Health.
"From the publically insured perspective, it has already been decided that (such treatments) are important," Dr. Braun said in an interview. "The next challenge will be to get private insurers to do the same. As the task force recommendations indicate, all kids are at risk for caries, some more than others ... and all benefit from these services, including those (who) are insured by private organizations."
Payment for the recommended treatments is an issue that state agencies, professional organizations, and oral health advocates should start investigating now, Dr. Beers added.
"It will be important for pediatric primary care providers, pediatric dentists, regulatory agencies, and payers to work together in each state or region to develop an implementation plan in order to ensure the best intake," she said. "This is not something primary care providers should be expected to implement without this type of comprehensive support, including, but not limited to training and payment."
Training for pediatricians is already available in many states. Most jurisdictions have oral education programs that have been running for some time, Dr. Braun said, such as Colorado’s Cavity Free at Three and North Carolina’s Into the Mouths of Babes. Physicians also can utilize online programs such as Smiles for Life, a national oral health curriculum developed by the Society of Teachers of Family Medicine.
Dr. Beers recommends doctors visit the American Academy of Pediatrics’ website for more information about oral health training programs and resources, the Protecting All Children’s Teeth curriculum and the Bright Futures resources.
"We don’t need to reinvent the wheel," Dr. Braun said. "A lot has really been developed in the last decade, and we can now take advantage of the education" available about these services.
Other challenges physicians may face in executing the recommendations include integrating the treatments into their routine practice, said Dr. Anupama Rao Tate, DMD, of Children’s National Medical Center, dentistry (oral health) department in Washington. For instance, physicians must decide whether the treatments should be provided as part of a well visit or independently.
In addition, electronic records may or may not have a place to track the services, Dr. Tate said. Conversations with parents also are necessary to help families understand why these services are being provided by their children’s primary care provider.
"Traditionally, dentistry has been separate from medicine," Dr. Tate said. Pediatricians are "going to have to change the mindset of parents and educate (them) as to why they’re doing something (pertaining to) dental health."
Pediatricians may face challenges in implementing new U.S. Preventive Services Task Force recommendations that advocate the provision of oral fluoride supplementation to children in fluoride-deficient areas and fluoride varnish to all children by primary care clinicians.
The speed with which the recommendations are applied in primary care settings likely will depend on state support, training availability, and insurer cooperation.
"The updated recommendations are a very important step forward toward improving oral health in children through collaborative care," Dr. Lee Savio Beers of Children’s National Medical Center, Washington, said in an interview. However, "primary care providers will face a number of barriers in implementing these recommendations, including workflow and staffing issues, access to training, and adequate payment."
The USPSTF guidelines, published in early May 2014, recommend that primary care providers prescribe oral fluoride supplementation starting at 6 months for children whose water supply is lacking in fluoride and that they apply fluoride varnish to the primary teeth of all children starting at primary tooth eruption. The recommendations cite evidence that show fluoride varnish and oral supplements help prevent dental caries in children aged 5 years and younger, and that the treatments’ benefits outweigh the potential harms of fluorosis (Pediatrics 2014[doi:10.15425/peds.2014-0483]). The recommendations update 2004 guidelines in which only oral fluoride supplementation was recommended for children in areas with fluoride levels below 0.6 ppm in their local drinking water. That recommendation remains.
Whether the treatments will be covered by insurers will depend greatly on the state and the insurer. In nearly every state, Medicaid currently reimburses providers for the provision of fluoride varnish, said Dr. Patricia Braun, a pediatrician at Denver Health’s Eastside Neighborhood Health Center, and at the University of Colorado. She is a member of the American Academy of Pediatrics Section on Oral Health.
"From the publically insured perspective, it has already been decided that (such treatments) are important," Dr. Braun said in an interview. "The next challenge will be to get private insurers to do the same. As the task force recommendations indicate, all kids are at risk for caries, some more than others ... and all benefit from these services, including those (who) are insured by private organizations."
Payment for the recommended treatments is an issue that state agencies, professional organizations, and oral health advocates should start investigating now, Dr. Beers added.
"It will be important for pediatric primary care providers, pediatric dentists, regulatory agencies, and payers to work together in each state or region to develop an implementation plan in order to ensure the best intake," she said. "This is not something primary care providers should be expected to implement without this type of comprehensive support, including, but not limited to training and payment."
Training for pediatricians is already available in many states. Most jurisdictions have oral education programs that have been running for some time, Dr. Braun said, such as Colorado’s Cavity Free at Three and North Carolina’s Into the Mouths of Babes. Physicians also can utilize online programs such as Smiles for Life, a national oral health curriculum developed by the Society of Teachers of Family Medicine.
Dr. Beers recommends doctors visit the American Academy of Pediatrics’ website for more information about oral health training programs and resources, the Protecting All Children’s Teeth curriculum and the Bright Futures resources.
"We don’t need to reinvent the wheel," Dr. Braun said. "A lot has really been developed in the last decade, and we can now take advantage of the education" available about these services.
Other challenges physicians may face in executing the recommendations include integrating the treatments into their routine practice, said Dr. Anupama Rao Tate, DMD, of Children’s National Medical Center, dentistry (oral health) department in Washington. For instance, physicians must decide whether the treatments should be provided as part of a well visit or independently.
In addition, electronic records may or may not have a place to track the services, Dr. Tate said. Conversations with parents also are necessary to help families understand why these services are being provided by their children’s primary care provider.
"Traditionally, dentistry has been separate from medicine," Dr. Tate said. Pediatricians are "going to have to change the mindset of parents and educate (them) as to why they’re doing something (pertaining to) dental health."
Answering subpoenas poses legal, privacy risks for doctors
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Doctors’ first steps after lawsuit filing are vital, warn attorneys
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
25% of lawsuits against internists end in payment
Errors in diagnosis, improper procedures, and medication errors make up the top reasons that internists are sued, according to a study published online April 28 in JAMA Internal Medicine. A quarter of claims against internists result in payment, the study found.
Researchers studied 247,073 closed cases from 1985 to 2009 collected by PIAA (Physician Insurers Association of America), a trade association that represents domestic and international medical professional liability insurers. Of the closed claims, 14% were against internists. Twenty-six percent of the lawsuits against internists involved diagnostic errors, including allegations of misdiagnosing lung cancer, acute myocardial infarction, colon cancer, and breast cancer. Another 25% of claims involved no departure from the standard of care, while 11% related to improper performance of a procedure and 9% were attributed to medication errors, wrote Dr. Sandeep S. Mangalmurti, of Bassett Medical Center, Cooperstown, N.Y., and his colleagues (JAMA Intern. Med. 2014 April 28 [doi: 10.1001/jamainternmed.2014.1116]).
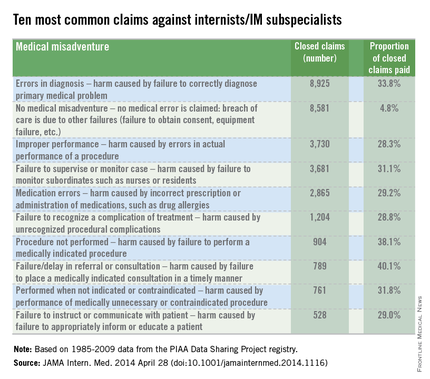
The results showed a wide variation among claims that resulted in payment against internists. For example, 40% of claims as a result of failure to refer and 38% of cases associated with failure to perform a procedure resulted in a claims payment. Cases in which no deviation from the standard of care occurred resulted in payment in 5% of suits. (In such cases, allegations such as failure to obtain consent or equipment were alleged.)
"Alleged departures from the appropriate standard of care are defined as medical misadventures," according to PIAA, the study, reported as a research letter, noted.
The findings confirm that internists are vulnerable to claims pertaining to their common practices of patient evaluation and health management, the authors noted. Insight into these claims patterns may help internists craft practice patterns and changes that will result in fewer patient injuries and fewer lawsuits, the authors said.
Errors in diagnosis, improper procedures, and medication errors make up the top reasons that internists are sued, according to a study published online April 28 in JAMA Internal Medicine. A quarter of claims against internists result in payment, the study found.
Researchers studied 247,073 closed cases from 1985 to 2009 collected by PIAA (Physician Insurers Association of America), a trade association that represents domestic and international medical professional liability insurers. Of the closed claims, 14% were against internists. Twenty-six percent of the lawsuits against internists involved diagnostic errors, including allegations of misdiagnosing lung cancer, acute myocardial infarction, colon cancer, and breast cancer. Another 25% of claims involved no departure from the standard of care, while 11% related to improper performance of a procedure and 9% were attributed to medication errors, wrote Dr. Sandeep S. Mangalmurti, of Bassett Medical Center, Cooperstown, N.Y., and his colleagues (JAMA Intern. Med. 2014 April 28 [doi: 10.1001/jamainternmed.2014.1116]).
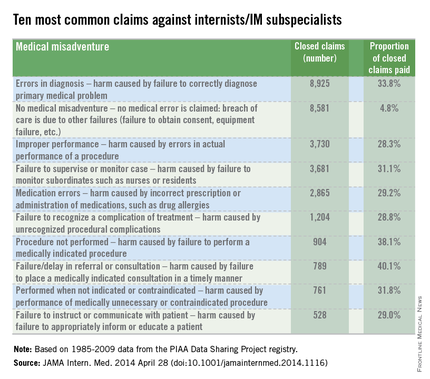
The results showed a wide variation among claims that resulted in payment against internists. For example, 40% of claims as a result of failure to refer and 38% of cases associated with failure to perform a procedure resulted in a claims payment. Cases in which no deviation from the standard of care occurred resulted in payment in 5% of suits. (In such cases, allegations such as failure to obtain consent or equipment were alleged.)
"Alleged departures from the appropriate standard of care are defined as medical misadventures," according to PIAA, the study, reported as a research letter, noted.
The findings confirm that internists are vulnerable to claims pertaining to their common practices of patient evaluation and health management, the authors noted. Insight into these claims patterns may help internists craft practice patterns and changes that will result in fewer patient injuries and fewer lawsuits, the authors said.
Errors in diagnosis, improper procedures, and medication errors make up the top reasons that internists are sued, according to a study published online April 28 in JAMA Internal Medicine. A quarter of claims against internists result in payment, the study found.
Researchers studied 247,073 closed cases from 1985 to 2009 collected by PIAA (Physician Insurers Association of America), a trade association that represents domestic and international medical professional liability insurers. Of the closed claims, 14% were against internists. Twenty-six percent of the lawsuits against internists involved diagnostic errors, including allegations of misdiagnosing lung cancer, acute myocardial infarction, colon cancer, and breast cancer. Another 25% of claims involved no departure from the standard of care, while 11% related to improper performance of a procedure and 9% were attributed to medication errors, wrote Dr. Sandeep S. Mangalmurti, of Bassett Medical Center, Cooperstown, N.Y., and his colleagues (JAMA Intern. Med. 2014 April 28 [doi: 10.1001/jamainternmed.2014.1116]).
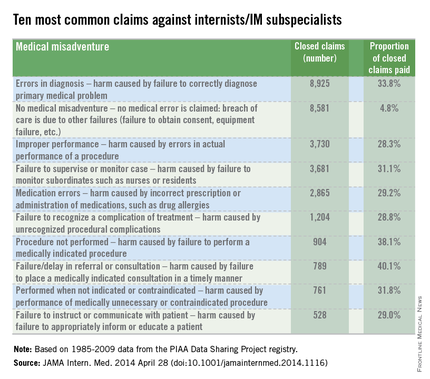
The results showed a wide variation among claims that resulted in payment against internists. For example, 40% of claims as a result of failure to refer and 38% of cases associated with failure to perform a procedure resulted in a claims payment. Cases in which no deviation from the standard of care occurred resulted in payment in 5% of suits. (In such cases, allegations such as failure to obtain consent or equipment were alleged.)
"Alleged departures from the appropriate standard of care are defined as medical misadventures," according to PIAA, the study, reported as a research letter, noted.
The findings confirm that internists are vulnerable to claims pertaining to their common practices of patient evaluation and health management, the authors noted. Insight into these claims patterns may help internists craft practice patterns and changes that will result in fewer patient injuries and fewer lawsuits, the authors said.
FROM JAMA INTERNAL MEDICINE
Teamwork, technology improve hepatitis C rural care
Communication and collaborative use of technology by physicians who serve underserved populations and by specialists can enhance patient management and treatment of hepatitis C virus infection, according to a report released May 8 by the Centers for Disease Control and Prevention.
Researchers analyzed programs in Utah and Arizona aimed at improving access to primary care providers with the capacity to manage and treat HCV infection. Both programs were modeled after the Extension for Community Healthcare Outcomes (Project ECHO) developed by the University of New Mexico’s Health Sciences Center in 2003. The initiative builds primary care providers’ capacity to treat diseases through videoconferencing and case-based learning in "teleECHO" clinics (MMWR 2014;63:393-8).
From Sept. 30, 2012, to Feb. 28, 2014, the Utah and Arizona programs trained 66 primary care clinicians, predominantly from rural settings. Ninety-three percent of the providers had no prior experience in care and treatment of HCV infection. Primary care clinicians attended weekly teleECHO sessions with specialists after an initial HCV training. Utah’s team of specialists included a hepatologist, psychiatrist, and pharmacist; Arizona’s team consisted of a hepatologist and nurse practitioner. Through videoconferencing, clinicians presented their HCV cases to specialists who provided advice and clinical mentoring.
A total of 280 unique cases of chronic HCV infection were presented in teleECHO sessions. In both states, a combined 46% of the HCV-infected patients received antiviral treatment, more than doubling the proportion of patients expected to receive treatment. Of the 46%, nearly three-quarters were treated with an interferon-based regimen and 26% were treated with a regimen containing sofosbuvir, a drug approved in December 2013.
The study’s authors concluded that Project ECHO is a model that can significantly enhance primary care provider capacity to treat HCV infection among underserved populations, including the use of newly approved medications. Collaborations with specialists will help primary care providers to incorporate new treatments for HCV infection, the investigators noted, and will be an important measure for improving access and reducing barriers to treatment.
Communication and collaborative use of technology by physicians who serve underserved populations and by specialists can enhance patient management and treatment of hepatitis C virus infection, according to a report released May 8 by the Centers for Disease Control and Prevention.
Researchers analyzed programs in Utah and Arizona aimed at improving access to primary care providers with the capacity to manage and treat HCV infection. Both programs were modeled after the Extension for Community Healthcare Outcomes (Project ECHO) developed by the University of New Mexico’s Health Sciences Center in 2003. The initiative builds primary care providers’ capacity to treat diseases through videoconferencing and case-based learning in "teleECHO" clinics (MMWR 2014;63:393-8).
From Sept. 30, 2012, to Feb. 28, 2014, the Utah and Arizona programs trained 66 primary care clinicians, predominantly from rural settings. Ninety-three percent of the providers had no prior experience in care and treatment of HCV infection. Primary care clinicians attended weekly teleECHO sessions with specialists after an initial HCV training. Utah’s team of specialists included a hepatologist, psychiatrist, and pharmacist; Arizona’s team consisted of a hepatologist and nurse practitioner. Through videoconferencing, clinicians presented their HCV cases to specialists who provided advice and clinical mentoring.
A total of 280 unique cases of chronic HCV infection were presented in teleECHO sessions. In both states, a combined 46% of the HCV-infected patients received antiviral treatment, more than doubling the proportion of patients expected to receive treatment. Of the 46%, nearly three-quarters were treated with an interferon-based regimen and 26% were treated with a regimen containing sofosbuvir, a drug approved in December 2013.
The study’s authors concluded that Project ECHO is a model that can significantly enhance primary care provider capacity to treat HCV infection among underserved populations, including the use of newly approved medications. Collaborations with specialists will help primary care providers to incorporate new treatments for HCV infection, the investigators noted, and will be an important measure for improving access and reducing barriers to treatment.
Communication and collaborative use of technology by physicians who serve underserved populations and by specialists can enhance patient management and treatment of hepatitis C virus infection, according to a report released May 8 by the Centers for Disease Control and Prevention.
Researchers analyzed programs in Utah and Arizona aimed at improving access to primary care providers with the capacity to manage and treat HCV infection. Both programs were modeled after the Extension for Community Healthcare Outcomes (Project ECHO) developed by the University of New Mexico’s Health Sciences Center in 2003. The initiative builds primary care providers’ capacity to treat diseases through videoconferencing and case-based learning in "teleECHO" clinics (MMWR 2014;63:393-8).
From Sept. 30, 2012, to Feb. 28, 2014, the Utah and Arizona programs trained 66 primary care clinicians, predominantly from rural settings. Ninety-three percent of the providers had no prior experience in care and treatment of HCV infection. Primary care clinicians attended weekly teleECHO sessions with specialists after an initial HCV training. Utah’s team of specialists included a hepatologist, psychiatrist, and pharmacist; Arizona’s team consisted of a hepatologist and nurse practitioner. Through videoconferencing, clinicians presented their HCV cases to specialists who provided advice and clinical mentoring.
A total of 280 unique cases of chronic HCV infection were presented in teleECHO sessions. In both states, a combined 46% of the HCV-infected patients received antiviral treatment, more than doubling the proportion of patients expected to receive treatment. Of the 46%, nearly three-quarters were treated with an interferon-based regimen and 26% were treated with a regimen containing sofosbuvir, a drug approved in December 2013.
The study’s authors concluded that Project ECHO is a model that can significantly enhance primary care provider capacity to treat HCV infection among underserved populations, including the use of newly approved medications. Collaborations with specialists will help primary care providers to incorporate new treatments for HCV infection, the investigators noted, and will be an important measure for improving access and reducing barriers to treatment.
Federal legislation would provide doctors litigation safe harbor
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Mergers and acquisitions pose legal challenges for physician-sellers
Practice mergers with physician groups and larger health systems are becoming commonplace as more doctors trade in their shingles for fewer business burdens and more stability. But as with all transactions, selling or merging a medical practice comes with legal risks.
"There are numerous complex issues, legal and otherwise, that the seller of a medical practice needs to consider, both in preparations for the sale and during the transaction," wrote health law attorney David N. Vozza in a recent article for Kern Augustine Conroy & Schoppmann, a health care litigation firm with offices in the East Coast.
One of the most significant legal considerations pertains to the correct transfer of medical records during sales and mergers, Mr. Vozza said in an interview. To meet privacy requirements, all current patients must be advised that the practice is being transferred and they must have the opportunity to obtain their original records if they desire a new physician, he said. Records also must not be released to third parties without the patient’s express authorization. In addition, physicians run the risk of an "abandonment" lawsuit, if patient care is compromised because of the sale or merger.
"If you know a patient has a pressing care or treatment need, that can’t be delayed because you’re in the middle of a sale," Mr. Vozza said. "It can’t get lost in the shuffle of the transaction."
Another key consideration when merging practices is the assessment of liability cases, said Mathew J. Levy, a health law attorney and principal at Kern Augustine Conroy & Schoppmann and a coauthor of the risk management article. Physicians combining practices should be aware of any pending malpractice cases or audits of their potential partners.
"When merging with a larger group, you should be concerned with how they are doing internally," Mr. Levy said. "Are they under any audits or investigations? Have they been disciplined by the state licensure board? You have to make sure you’re not accountable for" their debts or malpractice issues.
Physicians should also consider the effect their merger may have on their malpractice insurance, Mr. Levy adds. Coverage for prior actions can become challenging in the event that a physician has a claims-made policy, which offers protection only while the policy is in effect. If a claims-made policy is discontinued, the doctor must obtain "tail" coverage to cover past actions. While the physician likely will have new coverage from the hospital or health system, many hospitals are self-insured and do not provide incoming physicians with prior act or so-called nose coverage.
Along with discussing tail coverage during a merger, doctors should also be wary of "anti-compete" clauses in contracts with larger hospitals and health systems. Such clauses prohibit physicians from working for a competitor and/or in close proximity to the hospital. Mr. Levy encourages physicians to include an exception to the non-compete clause in their contracts and discuss options in case the relationship fails.
"If not, you would be stuck and be prohibited from working in a nearby location and generating patients for your career," he said. "That’s a significant issue."
Antitrust requirements should also be high on physicians’ radar long before a transaction proceeds.
The Federal Trade Commission in January revised the thresholds that determine whether health care providers must notify federal antitrust authorities about pending transactions under the Hart-Scott-Rodino (HSR) Antitrust Improvements Act. The HSR Act requires companies to notify government agencies if the size of the parties at issue and the value of a transaction exceed the filing thresholds. The 2014 FTC revision raised the threshold for reporting proposed mergers and acquisitions from $70.9 million to $75.9 million.
"If notification is required and "you proceed to complete a transaction without filing the required notification, than you’re in violation of the antitrust law," said Christine White, chair of the American Health Lawyers Association’s Antitrust Practice Group and a staff attorney in the FTC’s Northeast Regional Office.
Potential antitrust violations can result in government investigations, fines, legal settlements, or other discipline. Ms. White suggests that physicians review guidance on the FTC’s website for more information about the HSR Act and other antitrust requirements, such as when it’s acceptable to share confidential information with competitors.
"Not every sale of a physician practice will raise significant antitrust concerns. In fact, the vast majority of physician practice group consolidations do not raise major antitrust concerns. But, in certain circumstances, such as if a practice group is selling to a direct competitor or a potential competitor, the antitrust concerns may merit serious consideration," she said.
Practice mergers with physician groups and larger health systems are becoming commonplace as more doctors trade in their shingles for fewer business burdens and more stability. But as with all transactions, selling or merging a medical practice comes with legal risks.
"There are numerous complex issues, legal and otherwise, that the seller of a medical practice needs to consider, both in preparations for the sale and during the transaction," wrote health law attorney David N. Vozza in a recent article for Kern Augustine Conroy & Schoppmann, a health care litigation firm with offices in the East Coast.
One of the most significant legal considerations pertains to the correct transfer of medical records during sales and mergers, Mr. Vozza said in an interview. To meet privacy requirements, all current patients must be advised that the practice is being transferred and they must have the opportunity to obtain their original records if they desire a new physician, he said. Records also must not be released to third parties without the patient’s express authorization. In addition, physicians run the risk of an "abandonment" lawsuit, if patient care is compromised because of the sale or merger.
"If you know a patient has a pressing care or treatment need, that can’t be delayed because you’re in the middle of a sale," Mr. Vozza said. "It can’t get lost in the shuffle of the transaction."
Another key consideration when merging practices is the assessment of liability cases, said Mathew J. Levy, a health law attorney and principal at Kern Augustine Conroy & Schoppmann and a coauthor of the risk management article. Physicians combining practices should be aware of any pending malpractice cases or audits of their potential partners.
"When merging with a larger group, you should be concerned with how they are doing internally," Mr. Levy said. "Are they under any audits or investigations? Have they been disciplined by the state licensure board? You have to make sure you’re not accountable for" their debts or malpractice issues.
Physicians should also consider the effect their merger may have on their malpractice insurance, Mr. Levy adds. Coverage for prior actions can become challenging in the event that a physician has a claims-made policy, which offers protection only while the policy is in effect. If a claims-made policy is discontinued, the doctor must obtain "tail" coverage to cover past actions. While the physician likely will have new coverage from the hospital or health system, many hospitals are self-insured and do not provide incoming physicians with prior act or so-called nose coverage.
Along with discussing tail coverage during a merger, doctors should also be wary of "anti-compete" clauses in contracts with larger hospitals and health systems. Such clauses prohibit physicians from working for a competitor and/or in close proximity to the hospital. Mr. Levy encourages physicians to include an exception to the non-compete clause in their contracts and discuss options in case the relationship fails.
"If not, you would be stuck and be prohibited from working in a nearby location and generating patients for your career," he said. "That’s a significant issue."
Antitrust requirements should also be high on physicians’ radar long before a transaction proceeds.
The Federal Trade Commission in January revised the thresholds that determine whether health care providers must notify federal antitrust authorities about pending transactions under the Hart-Scott-Rodino (HSR) Antitrust Improvements Act. The HSR Act requires companies to notify government agencies if the size of the parties at issue and the value of a transaction exceed the filing thresholds. The 2014 FTC revision raised the threshold for reporting proposed mergers and acquisitions from $70.9 million to $75.9 million.
"If notification is required and "you proceed to complete a transaction without filing the required notification, than you’re in violation of the antitrust law," said Christine White, chair of the American Health Lawyers Association’s Antitrust Practice Group and a staff attorney in the FTC’s Northeast Regional Office.
Potential antitrust violations can result in government investigations, fines, legal settlements, or other discipline. Ms. White suggests that physicians review guidance on the FTC’s website for more information about the HSR Act and other antitrust requirements, such as when it’s acceptable to share confidential information with competitors.
"Not every sale of a physician practice will raise significant antitrust concerns. In fact, the vast majority of physician practice group consolidations do not raise major antitrust concerns. But, in certain circumstances, such as if a practice group is selling to a direct competitor or a potential competitor, the antitrust concerns may merit serious consideration," she said.
Practice mergers with physician groups and larger health systems are becoming commonplace as more doctors trade in their shingles for fewer business burdens and more stability. But as with all transactions, selling or merging a medical practice comes with legal risks.
"There are numerous complex issues, legal and otherwise, that the seller of a medical practice needs to consider, both in preparations for the sale and during the transaction," wrote health law attorney David N. Vozza in a recent article for Kern Augustine Conroy & Schoppmann, a health care litigation firm with offices in the East Coast.
One of the most significant legal considerations pertains to the correct transfer of medical records during sales and mergers, Mr. Vozza said in an interview. To meet privacy requirements, all current patients must be advised that the practice is being transferred and they must have the opportunity to obtain their original records if they desire a new physician, he said. Records also must not be released to third parties without the patient’s express authorization. In addition, physicians run the risk of an "abandonment" lawsuit, if patient care is compromised because of the sale or merger.
"If you know a patient has a pressing care or treatment need, that can’t be delayed because you’re in the middle of a sale," Mr. Vozza said. "It can’t get lost in the shuffle of the transaction."
Another key consideration when merging practices is the assessment of liability cases, said Mathew J. Levy, a health law attorney and principal at Kern Augustine Conroy & Schoppmann and a coauthor of the risk management article. Physicians combining practices should be aware of any pending malpractice cases or audits of their potential partners.
"When merging with a larger group, you should be concerned with how they are doing internally," Mr. Levy said. "Are they under any audits or investigations? Have they been disciplined by the state licensure board? You have to make sure you’re not accountable for" their debts or malpractice issues.
Physicians should also consider the effect their merger may have on their malpractice insurance, Mr. Levy adds. Coverage for prior actions can become challenging in the event that a physician has a claims-made policy, which offers protection only while the policy is in effect. If a claims-made policy is discontinued, the doctor must obtain "tail" coverage to cover past actions. While the physician likely will have new coverage from the hospital or health system, many hospitals are self-insured and do not provide incoming physicians with prior act or so-called nose coverage.
Along with discussing tail coverage during a merger, doctors should also be wary of "anti-compete" clauses in contracts with larger hospitals and health systems. Such clauses prohibit physicians from working for a competitor and/or in close proximity to the hospital. Mr. Levy encourages physicians to include an exception to the non-compete clause in their contracts and discuss options in case the relationship fails.
"If not, you would be stuck and be prohibited from working in a nearby location and generating patients for your career," he said. "That’s a significant issue."
Antitrust requirements should also be high on physicians’ radar long before a transaction proceeds.
The Federal Trade Commission in January revised the thresholds that determine whether health care providers must notify federal antitrust authorities about pending transactions under the Hart-Scott-Rodino (HSR) Antitrust Improvements Act. The HSR Act requires companies to notify government agencies if the size of the parties at issue and the value of a transaction exceed the filing thresholds. The 2014 FTC revision raised the threshold for reporting proposed mergers and acquisitions from $70.9 million to $75.9 million.
"If notification is required and "you proceed to complete a transaction without filing the required notification, than you’re in violation of the antitrust law," said Christine White, chair of the American Health Lawyers Association’s Antitrust Practice Group and a staff attorney in the FTC’s Northeast Regional Office.
Potential antitrust violations can result in government investigations, fines, legal settlements, or other discipline. Ms. White suggests that physicians review guidance on the FTC’s website for more information about the HSR Act and other antitrust requirements, such as when it’s acceptable to share confidential information with competitors.
"Not every sale of a physician practice will raise significant antitrust concerns. In fact, the vast majority of physician practice group consolidations do not raise major antitrust concerns. But, in certain circumstances, such as if a practice group is selling to a direct competitor or a potential competitor, the antitrust concerns may merit serious consideration," she said.
States aim to repeal, raise malpractice caps
Caps on noneconomic damages in medical malpractice cases are coming under fire by courts, legislators, and trial attorneys in a number of states.
In March, the Florida Supreme Court struck down the state’s $1 million cap on noneconomic damages.
Meanwhile, a proposed ballot measure in California aims to quadruple that state’s $250,000 cap. And Missouri doctors are pushing to reinstate their state’s noneconomic damages cap after a court overturned the $350,000 limit in 2012.
"The courts have always swung back and forth in some states [on upholding caps], and that probably won’t change," said William Encinosa, Ph.D., a senior economist for the Center for Delivery, Organization and Markets at the Agency for Healthcare Research and Quality (AHRQ). "However, on the legislative side, as more states reform their Medicaid, they may be willing to pass caps to contain costs."
Close to 30 states limit award damages in medical malpractice cases; however, cap amounts and their application vary. For example, Texas caps pain and suffering at $250,000, while Nebraska has a $1.75 million limit on total damages. At least 16 state courts have upheld a noneconomic or total damages cap as constitutional, according to American Medical Association data. Judges in at least 12 states however, have overturned caps.
Florida physicians were disappointed to lose the wrongful death damages cap, said Jeff Scott, director for legal and government affairs for the Florida Medical Association. Since its enactment, the cap helped stabilize premiums in Florida and has supported the return of a number of liability insurers returning to the state, he said.
"We thought [the opinion] was fully reasoned and fully decided," Mr. Scott said in an interview. "It was unfortunate. Our Supreme Court has been on a roll of striking down good tort reform legislation and this wasn’t a very big surprise."
The Missouri Supreme Court ruled similarly in July 2012 when it threw out the state’s noneconomic damages cap. A doctor-backed bill that would restore the $350,000 limit passed the Missouri House in March. The state Senate discussed the proposed law in April, but had not reached an agreement by this article’s deadline.
California physicians also are defending the damages cap law in their state – the Medical Injury Compensation Reform Act (MICRA). The law has survived numerous legal challenges, but now faces a proposed ballot initiative that would significantly elevate the cap. California plaintiffs’ attorneys and other MICRA critics are advocating a ballot measure that would increase the noneconomic damage award to roughly $1 million. Trial attorneys filed signatures with county registrars in March to qualify the measure for the November ballot.
"The proposed ballot measure would increase costs for everyone in California," California Medical Association President Dr. Richard Thorp said in a statement. "This initiative would take money directly out of the health care delivery system and put it straight into the pockets of trial attorneys. That’s why such a broad coalition, including doctors, nurses, hospitals, community clinics, dentists, labor, local government and hundreds of others are all in opposition."
Kansas physicians, meanwhile, are applauding a new law that raises Kansas’ damages cap, but keeps it intact. The Kansas Supreme Court upheld the state’s $250,000 medical malpractice noneconomic damages limit in 2012, but the opinion warned the Legislature should raise the cap or face a likely reversal in the future, said Rachelle Colombo, director of government affairs for the Kansas Medical Society. To prevent this from happening, KMS led the creation of SB 311, a law that would gradually increase the cap to $350,000 over an 8-year span. The law was signed by Gov. Sam Brownback (R) on April 18.
"We’re thrilled," Ms. Colombo said in an interview. "It is very significant and provides stability for physicians in Kansas for decades to come. [The cap] has been the cornerstone of our positive malpractice environment. It has allowed for premiums to significantly decrease and we’ve seen physicians who have crossed over state lines to practice in Kansas."
Studies evaluating malpractice damages caps have found varying degrees of impact. A 2007 metaanalysis of more than 20 studies found nearly all rigorous, empirical studies conducted since 1990 have found that malpractice premiums are lower in the presence of damages caps (Milbank Q. 2007;85:259-86). A 2003 study by AHRQ researchers found that states with noneconomic damages caps had 12% more physicians per capita than did those without; however, states with relatively high caps were less likely to experience the same effect on physician supply.
Mr. Encinosa, a coauthor of the AHRQ study, said it’s clear that lower caps positively impact the medical malpractice environment for doctors.
"The high caps just limit the case with very large noneconomic damage verdicts," he said in an interview. "These cases are often only found among a handful of high-risk physicians, and so don’t impact a lot of physicians. The lower caps impact more physicians and thus encourage them to engage in less-defensive medicine. There are litigation savings as well as savings from reduced defensive medicine under lower caps."
Caps on noneconomic damages in medical malpractice cases are coming under fire by courts, legislators, and trial attorneys in a number of states.
In March, the Florida Supreme Court struck down the state’s $1 million cap on noneconomic damages.
Meanwhile, a proposed ballot measure in California aims to quadruple that state’s $250,000 cap. And Missouri doctors are pushing to reinstate their state’s noneconomic damages cap after a court overturned the $350,000 limit in 2012.
"The courts have always swung back and forth in some states [on upholding caps], and that probably won’t change," said William Encinosa, Ph.D., a senior economist for the Center for Delivery, Organization and Markets at the Agency for Healthcare Research and Quality (AHRQ). "However, on the legislative side, as more states reform their Medicaid, they may be willing to pass caps to contain costs."
Close to 30 states limit award damages in medical malpractice cases; however, cap amounts and their application vary. For example, Texas caps pain and suffering at $250,000, while Nebraska has a $1.75 million limit on total damages. At least 16 state courts have upheld a noneconomic or total damages cap as constitutional, according to American Medical Association data. Judges in at least 12 states however, have overturned caps.
Florida physicians were disappointed to lose the wrongful death damages cap, said Jeff Scott, director for legal and government affairs for the Florida Medical Association. Since its enactment, the cap helped stabilize premiums in Florida and has supported the return of a number of liability insurers returning to the state, he said.
"We thought [the opinion] was fully reasoned and fully decided," Mr. Scott said in an interview. "It was unfortunate. Our Supreme Court has been on a roll of striking down good tort reform legislation and this wasn’t a very big surprise."
The Missouri Supreme Court ruled similarly in July 2012 when it threw out the state’s noneconomic damages cap. A doctor-backed bill that would restore the $350,000 limit passed the Missouri House in March. The state Senate discussed the proposed law in April, but had not reached an agreement by this article’s deadline.
California physicians also are defending the damages cap law in their state – the Medical Injury Compensation Reform Act (MICRA). The law has survived numerous legal challenges, but now faces a proposed ballot initiative that would significantly elevate the cap. California plaintiffs’ attorneys and other MICRA critics are advocating a ballot measure that would increase the noneconomic damage award to roughly $1 million. Trial attorneys filed signatures with county registrars in March to qualify the measure for the November ballot.
"The proposed ballot measure would increase costs for everyone in California," California Medical Association President Dr. Richard Thorp said in a statement. "This initiative would take money directly out of the health care delivery system and put it straight into the pockets of trial attorneys. That’s why such a broad coalition, including doctors, nurses, hospitals, community clinics, dentists, labor, local government and hundreds of others are all in opposition."
Kansas physicians, meanwhile, are applauding a new law that raises Kansas’ damages cap, but keeps it intact. The Kansas Supreme Court upheld the state’s $250,000 medical malpractice noneconomic damages limit in 2012, but the opinion warned the Legislature should raise the cap or face a likely reversal in the future, said Rachelle Colombo, director of government affairs for the Kansas Medical Society. To prevent this from happening, KMS led the creation of SB 311, a law that would gradually increase the cap to $350,000 over an 8-year span. The law was signed by Gov. Sam Brownback (R) on April 18.
"We’re thrilled," Ms. Colombo said in an interview. "It is very significant and provides stability for physicians in Kansas for decades to come. [The cap] has been the cornerstone of our positive malpractice environment. It has allowed for premiums to significantly decrease and we’ve seen physicians who have crossed over state lines to practice in Kansas."
Studies evaluating malpractice damages caps have found varying degrees of impact. A 2007 metaanalysis of more than 20 studies found nearly all rigorous, empirical studies conducted since 1990 have found that malpractice premiums are lower in the presence of damages caps (Milbank Q. 2007;85:259-86). A 2003 study by AHRQ researchers found that states with noneconomic damages caps had 12% more physicians per capita than did those without; however, states with relatively high caps were less likely to experience the same effect on physician supply.
Mr. Encinosa, a coauthor of the AHRQ study, said it’s clear that lower caps positively impact the medical malpractice environment for doctors.
"The high caps just limit the case with very large noneconomic damage verdicts," he said in an interview. "These cases are often only found among a handful of high-risk physicians, and so don’t impact a lot of physicians. The lower caps impact more physicians and thus encourage them to engage in less-defensive medicine. There are litigation savings as well as savings from reduced defensive medicine under lower caps."
Caps on noneconomic damages in medical malpractice cases are coming under fire by courts, legislators, and trial attorneys in a number of states.
In March, the Florida Supreme Court struck down the state’s $1 million cap on noneconomic damages.
Meanwhile, a proposed ballot measure in California aims to quadruple that state’s $250,000 cap. And Missouri doctors are pushing to reinstate their state’s noneconomic damages cap after a court overturned the $350,000 limit in 2012.
"The courts have always swung back and forth in some states [on upholding caps], and that probably won’t change," said William Encinosa, Ph.D., a senior economist for the Center for Delivery, Organization and Markets at the Agency for Healthcare Research and Quality (AHRQ). "However, on the legislative side, as more states reform their Medicaid, they may be willing to pass caps to contain costs."
Close to 30 states limit award damages in medical malpractice cases; however, cap amounts and their application vary. For example, Texas caps pain and suffering at $250,000, while Nebraska has a $1.75 million limit on total damages. At least 16 state courts have upheld a noneconomic or total damages cap as constitutional, according to American Medical Association data. Judges in at least 12 states however, have overturned caps.
Florida physicians were disappointed to lose the wrongful death damages cap, said Jeff Scott, director for legal and government affairs for the Florida Medical Association. Since its enactment, the cap helped stabilize premiums in Florida and has supported the return of a number of liability insurers returning to the state, he said.
"We thought [the opinion] was fully reasoned and fully decided," Mr. Scott said in an interview. "It was unfortunate. Our Supreme Court has been on a roll of striking down good tort reform legislation and this wasn’t a very big surprise."
The Missouri Supreme Court ruled similarly in July 2012 when it threw out the state’s noneconomic damages cap. A doctor-backed bill that would restore the $350,000 limit passed the Missouri House in March. The state Senate discussed the proposed law in April, but had not reached an agreement by this article’s deadline.
California physicians also are defending the damages cap law in their state – the Medical Injury Compensation Reform Act (MICRA). The law has survived numerous legal challenges, but now faces a proposed ballot initiative that would significantly elevate the cap. California plaintiffs’ attorneys and other MICRA critics are advocating a ballot measure that would increase the noneconomic damage award to roughly $1 million. Trial attorneys filed signatures with county registrars in March to qualify the measure for the November ballot.
"The proposed ballot measure would increase costs for everyone in California," California Medical Association President Dr. Richard Thorp said in a statement. "This initiative would take money directly out of the health care delivery system and put it straight into the pockets of trial attorneys. That’s why such a broad coalition, including doctors, nurses, hospitals, community clinics, dentists, labor, local government and hundreds of others are all in opposition."
Kansas physicians, meanwhile, are applauding a new law that raises Kansas’ damages cap, but keeps it intact. The Kansas Supreme Court upheld the state’s $250,000 medical malpractice noneconomic damages limit in 2012, but the opinion warned the Legislature should raise the cap or face a likely reversal in the future, said Rachelle Colombo, director of government affairs for the Kansas Medical Society. To prevent this from happening, KMS led the creation of SB 311, a law that would gradually increase the cap to $350,000 over an 8-year span. The law was signed by Gov. Sam Brownback (R) on April 18.
"We’re thrilled," Ms. Colombo said in an interview. "It is very significant and provides stability for physicians in Kansas for decades to come. [The cap] has been the cornerstone of our positive malpractice environment. It has allowed for premiums to significantly decrease and we’ve seen physicians who have crossed over state lines to practice in Kansas."
Studies evaluating malpractice damages caps have found varying degrees of impact. A 2007 metaanalysis of more than 20 studies found nearly all rigorous, empirical studies conducted since 1990 have found that malpractice premiums are lower in the presence of damages caps (Milbank Q. 2007;85:259-86). A 2003 study by AHRQ researchers found that states with noneconomic damages caps had 12% more physicians per capita than did those without; however, states with relatively high caps were less likely to experience the same effect on physician supply.
Mr. Encinosa, a coauthor of the AHRQ study, said it’s clear that lower caps positively impact the medical malpractice environment for doctors.
"The high caps just limit the case with very large noneconomic damage verdicts," he said in an interview. "These cases are often only found among a handful of high-risk physicians, and so don’t impact a lot of physicians. The lower caps impact more physicians and thus encourage them to engage in less-defensive medicine. There are litigation savings as well as savings from reduced defensive medicine under lower caps."
Heads of the class: New clinical informatics certification opens up opportunities
A new subspecialty is drawing physicians from diverse medical backgrounds and career settings who aim to combine informatics with providing health care. More than 400 physicians recently became board certified in clinical informatics – the first class of diplomates in the freshly minted subspecialty.
Clinical informatics (CI) has "now become a subspecialty because there are so many people who believe it’s important," said Dr. William Hersh, an internist and chair of the department of medical informatics and clinical epidemiology at Oregon Health and Science University, Portland.
"More and more health care organizations and certainly, almost every large health care organization, have someone who plays the role of chief medical informatics officer. By having a subspecialty, you then give professional recognition to those physicians who play this role. It really takes expertise by someone who understands medicine and understands information systems to make sure things run smoothly."
CI is the application of informatics and information technology to the delivery of health care services. The domain includes a wide spectrum of areas including clinical documentation, order entry systems, system design, system implementation, and adoption issues. While already incorporated into many practices, CI was not a recognized subspecialty until it was approved by the American Board of Medical Specialties in 2011. The American Medical Informatics Association (AMIA) spearheaded the new subspecialty, working for more than 5 years to define and help design the discipline. Physicians who are board certified by any of the 24 American Board of Medical Specialties (ABMS) member boards can now also certify in CI through an exam offered by the American Board of Preventive Medicine. In December 2013, 455 new subspecialists across the country became certified.
One of those alumni is Dr. Hersh, who also serves as director of the AMIA’s clinical informatics board review course.
"I’m proud to be a part of the pioneer class of leaders in this field," Dr. Hersh said in a statement. "When you look at the Accreditation Council for Graduate Medical Education’s (ACGME’s) definition of the informatics discipline, the operative word is ‘transform.’ Every day, informaticians are working in their health care settings to change how we do things, to improve patient care and population health."
Having a far-reaching, positive impact on health populations has long been a primary objective of Dr. Katherine Schneider, a family physician who recently became CI certified. The Pennsylvania doctor started her medical career as the head of a community medicine program, accessing outreach initiatives and working to improve care for the uninsured. She then took on a senior vice president position at AtlantiCare, where she led the system’s strategic transformational work toward accountable care. Dr. Schneider did not hesitate when she learned of the opportunity to become board certified in CI.
"It’s the birth of a new specialty; why not get involved at the very beginning?" said Dr. Schneider, who now serves as chief medical officer for Medecision, a national provider of health care management solutions. CI "by definition, it’s in my everyday work. It’s my role to help make sure we are helping customers use this correctly, understand what our pain points are, and build the right kind of tools to solve problems of effectiveness and efficiency."
Along with bringing new information and technology terms to her current position, her CI training has enabled Dr. Schneider to expand her professional network of clinical informaticians and industry experts, she said.
"One really great benefit is that you meet other people that either do something similar to you or understand the role that you’re in," she said. "Having that peer network is going to be really nice. It’s nice to have recognition that you have expertise in a field. It’s fun to be there at the beginning and participate in the debate about what’s relevant and where it’s going to be in a few years."
For other recently certified physicians, the subspecialty is a door to countless professional paths.
"I became certified to update my skill set and expand my career options," said Dr. Gretchen Purcell Jackson, of the department of pediatric surgery at Vanderbilt University Medical Center, Nashville, Tenn. "I found the quality improvement and project management part of the certification really useful."
In her current practice, Dr. Jackson’s CI training aids in a range of projects, such as helping with a grant she received to study information needs and information management practices of pregnant women and their caregivers.
"The project management aspect of my CI training has been very useful in helping me organize a large clinical study," said Dr. Jackson, who has a PhD in medical information sciences from Stanford (Calif.) University. In addition, "I have recently been asked to help oversee a project that involves coordinating the efforts and technologies from Vanderbilt health information systems, a corporate partner, a non-profit research foundation, and a large funded research project. I use every aspect of my CI training to guide this project. It requires leadership, project management, quality improvement, and clinical and technological expertise."
Meanwhile, Dr. Peter Killoran, a Texas anesthesiologist, is using his CI training to help track patient outcomes and evaluate data for the University of Texas Health Science Center at Houston, School of Biomedical Informatics. Dr. Killoran’s work includes improving health care quality and safety through health information technology and biomedical informatics.
"Quality improvement is a big part of the curriculum for this specialty," said Dr. Killoran, an assistant professor of anesthesiology at the UTHealth Medical School. "That’s because increasingly, medicine is focusing on improving outcomes and the rational use of heath care resources, and all of that comes down to the data."
As the field of CI continues to grow, health providers are needed to participate in the subspecialty and add their voices, said Dr. Genevieve Melton-Meaux, of the department of surgery at the University of Minnesota, Minneapolis, and a faculty fellow for the university’s Institute for Health Informatics. She was recently CI certified.
"The electronic health record and health information technology are the ‘nervous system’ of clinical care," she said. "There are important opportunities to improve the design, implementation, optimization, and use of these technologies and their resultant data, which will ultimately help to improve the efficiency and safety of health care, as well as improve the process of clinical discovery."

|
| Dr. Blake Lesselroth |
The American Board of Medical Specialties' decision to recognize clinical informatics as a board-certified subspecialty heralds an important professional opportunity for hospitalists. Many hospitalists are already an ideal fit to serve as champions in this movement; they boast strong project management skills, possess an understanding of health-systems management, and occupy a central role within their community of practice. Also, medical facilities tend to rely upon hospitalists to implement health information technologies (HIT).
Hospitalists should expect an increased demand for their expertise as regulatory mandates accelerate HIT adoption. However, for their specialty to evolve, hospitalists should consider how formal training in informatics could reinforce their value - especially in a changing health care landscape. First, hospitalists cross-trained in informatics are better positioned to lead system design, apply evidence-based practices to deployments, and promote a constructive culture of innovation. Second, while hospitalists have long been associated with quality improvement research, they will need formal training to effectively guide in the selection, validation, and piloting of performance measures. Finally, membership in the informatics community can increase access to new ideas and products in knowledge systems, computerized decision support, and mobile technologies.
In summary, informatics certification represents one promising path to fostering professional development, guiding HIT development, and enriching a portfolio of scholarship.
Dr. Blake J. Lesselroth is a hospitalist and informatician at Portland (Ore.) Veterans Affairs Medical Center, and teaches medical informatics at Oregon Health Sciences University.

|
| Dr. Blake Lesselroth |
The American Board of Medical Specialties' decision to recognize clinical informatics as a board-certified subspecialty heralds an important professional opportunity for hospitalists. Many hospitalists are already an ideal fit to serve as champions in this movement; they boast strong project management skills, possess an understanding of health-systems management, and occupy a central role within their community of practice. Also, medical facilities tend to rely upon hospitalists to implement health information technologies (HIT).
Hospitalists should expect an increased demand for their expertise as regulatory mandates accelerate HIT adoption. However, for their specialty to evolve, hospitalists should consider how formal training in informatics could reinforce their value - especially in a changing health care landscape. First, hospitalists cross-trained in informatics are better positioned to lead system design, apply evidence-based practices to deployments, and promote a constructive culture of innovation. Second, while hospitalists have long been associated with quality improvement research, they will need formal training to effectively guide in the selection, validation, and piloting of performance measures. Finally, membership in the informatics community can increase access to new ideas and products in knowledge systems, computerized decision support, and mobile technologies.
In summary, informatics certification represents one promising path to fostering professional development, guiding HIT development, and enriching a portfolio of scholarship.
Dr. Blake J. Lesselroth is a hospitalist and informatician at Portland (Ore.) Veterans Affairs Medical Center, and teaches medical informatics at Oregon Health Sciences University.

|
| Dr. Blake Lesselroth |
The American Board of Medical Specialties' decision to recognize clinical informatics as a board-certified subspecialty heralds an important professional opportunity for hospitalists. Many hospitalists are already an ideal fit to serve as champions in this movement; they boast strong project management skills, possess an understanding of health-systems management, and occupy a central role within their community of practice. Also, medical facilities tend to rely upon hospitalists to implement health information technologies (HIT).
Hospitalists should expect an increased demand for their expertise as regulatory mandates accelerate HIT adoption. However, for their specialty to evolve, hospitalists should consider how formal training in informatics could reinforce their value - especially in a changing health care landscape. First, hospitalists cross-trained in informatics are better positioned to lead system design, apply evidence-based practices to deployments, and promote a constructive culture of innovation. Second, while hospitalists have long been associated with quality improvement research, they will need formal training to effectively guide in the selection, validation, and piloting of performance measures. Finally, membership in the informatics community can increase access to new ideas and products in knowledge systems, computerized decision support, and mobile technologies.
In summary, informatics certification represents one promising path to fostering professional development, guiding HIT development, and enriching a portfolio of scholarship.
Dr. Blake J. Lesselroth is a hospitalist and informatician at Portland (Ore.) Veterans Affairs Medical Center, and teaches medical informatics at Oregon Health Sciences University.
A new subspecialty is drawing physicians from diverse medical backgrounds and career settings who aim to combine informatics with providing health care. More than 400 physicians recently became board certified in clinical informatics – the first class of diplomates in the freshly minted subspecialty.
Clinical informatics (CI) has "now become a subspecialty because there are so many people who believe it’s important," said Dr. William Hersh, an internist and chair of the department of medical informatics and clinical epidemiology at Oregon Health and Science University, Portland.
"More and more health care organizations and certainly, almost every large health care organization, have someone who plays the role of chief medical informatics officer. By having a subspecialty, you then give professional recognition to those physicians who play this role. It really takes expertise by someone who understands medicine and understands information systems to make sure things run smoothly."
CI is the application of informatics and information technology to the delivery of health care services. The domain includes a wide spectrum of areas including clinical documentation, order entry systems, system design, system implementation, and adoption issues. While already incorporated into many practices, CI was not a recognized subspecialty until it was approved by the American Board of Medical Specialties in 2011. The American Medical Informatics Association (AMIA) spearheaded the new subspecialty, working for more than 5 years to define and help design the discipline. Physicians who are board certified by any of the 24 American Board of Medical Specialties (ABMS) member boards can now also certify in CI through an exam offered by the American Board of Preventive Medicine. In December 2013, 455 new subspecialists across the country became certified.
One of those alumni is Dr. Hersh, who also serves as director of the AMIA’s clinical informatics board review course.
"I’m proud to be a part of the pioneer class of leaders in this field," Dr. Hersh said in a statement. "When you look at the Accreditation Council for Graduate Medical Education’s (ACGME’s) definition of the informatics discipline, the operative word is ‘transform.’ Every day, informaticians are working in their health care settings to change how we do things, to improve patient care and population health."
Having a far-reaching, positive impact on health populations has long been a primary objective of Dr. Katherine Schneider, a family physician who recently became CI certified. The Pennsylvania doctor started her medical career as the head of a community medicine program, accessing outreach initiatives and working to improve care for the uninsured. She then took on a senior vice president position at AtlantiCare, where she led the system’s strategic transformational work toward accountable care. Dr. Schneider did not hesitate when she learned of the opportunity to become board certified in CI.
"It’s the birth of a new specialty; why not get involved at the very beginning?" said Dr. Schneider, who now serves as chief medical officer for Medecision, a national provider of health care management solutions. CI "by definition, it’s in my everyday work. It’s my role to help make sure we are helping customers use this correctly, understand what our pain points are, and build the right kind of tools to solve problems of effectiveness and efficiency."
Along with bringing new information and technology terms to her current position, her CI training has enabled Dr. Schneider to expand her professional network of clinical informaticians and industry experts, she said.
"One really great benefit is that you meet other people that either do something similar to you or understand the role that you’re in," she said. "Having that peer network is going to be really nice. It’s nice to have recognition that you have expertise in a field. It’s fun to be there at the beginning and participate in the debate about what’s relevant and where it’s going to be in a few years."
For other recently certified physicians, the subspecialty is a door to countless professional paths.
"I became certified to update my skill set and expand my career options," said Dr. Gretchen Purcell Jackson, of the department of pediatric surgery at Vanderbilt University Medical Center, Nashville, Tenn. "I found the quality improvement and project management part of the certification really useful."
In her current practice, Dr. Jackson’s CI training aids in a range of projects, such as helping with a grant she received to study information needs and information management practices of pregnant women and their caregivers.
"The project management aspect of my CI training has been very useful in helping me organize a large clinical study," said Dr. Jackson, who has a PhD in medical information sciences from Stanford (Calif.) University. In addition, "I have recently been asked to help oversee a project that involves coordinating the efforts and technologies from Vanderbilt health information systems, a corporate partner, a non-profit research foundation, and a large funded research project. I use every aspect of my CI training to guide this project. It requires leadership, project management, quality improvement, and clinical and technological expertise."
Meanwhile, Dr. Peter Killoran, a Texas anesthesiologist, is using his CI training to help track patient outcomes and evaluate data for the University of Texas Health Science Center at Houston, School of Biomedical Informatics. Dr. Killoran’s work includes improving health care quality and safety through health information technology and biomedical informatics.
"Quality improvement is a big part of the curriculum for this specialty," said Dr. Killoran, an assistant professor of anesthesiology at the UTHealth Medical School. "That’s because increasingly, medicine is focusing on improving outcomes and the rational use of heath care resources, and all of that comes down to the data."
As the field of CI continues to grow, health providers are needed to participate in the subspecialty and add their voices, said Dr. Genevieve Melton-Meaux, of the department of surgery at the University of Minnesota, Minneapolis, and a faculty fellow for the university’s Institute for Health Informatics. She was recently CI certified.
"The electronic health record and health information technology are the ‘nervous system’ of clinical care," she said. "There are important opportunities to improve the design, implementation, optimization, and use of these technologies and their resultant data, which will ultimately help to improve the efficiency and safety of health care, as well as improve the process of clinical discovery."
A new subspecialty is drawing physicians from diverse medical backgrounds and career settings who aim to combine informatics with providing health care. More than 400 physicians recently became board certified in clinical informatics – the first class of diplomates in the freshly minted subspecialty.
Clinical informatics (CI) has "now become a subspecialty because there are so many people who believe it’s important," said Dr. William Hersh, an internist and chair of the department of medical informatics and clinical epidemiology at Oregon Health and Science University, Portland.
"More and more health care organizations and certainly, almost every large health care organization, have someone who plays the role of chief medical informatics officer. By having a subspecialty, you then give professional recognition to those physicians who play this role. It really takes expertise by someone who understands medicine and understands information systems to make sure things run smoothly."
CI is the application of informatics and information technology to the delivery of health care services. The domain includes a wide spectrum of areas including clinical documentation, order entry systems, system design, system implementation, and adoption issues. While already incorporated into many practices, CI was not a recognized subspecialty until it was approved by the American Board of Medical Specialties in 2011. The American Medical Informatics Association (AMIA) spearheaded the new subspecialty, working for more than 5 years to define and help design the discipline. Physicians who are board certified by any of the 24 American Board of Medical Specialties (ABMS) member boards can now also certify in CI through an exam offered by the American Board of Preventive Medicine. In December 2013, 455 new subspecialists across the country became certified.
One of those alumni is Dr. Hersh, who also serves as director of the AMIA’s clinical informatics board review course.
"I’m proud to be a part of the pioneer class of leaders in this field," Dr. Hersh said in a statement. "When you look at the Accreditation Council for Graduate Medical Education’s (ACGME’s) definition of the informatics discipline, the operative word is ‘transform.’ Every day, informaticians are working in their health care settings to change how we do things, to improve patient care and population health."
Having a far-reaching, positive impact on health populations has long been a primary objective of Dr. Katherine Schneider, a family physician who recently became CI certified. The Pennsylvania doctor started her medical career as the head of a community medicine program, accessing outreach initiatives and working to improve care for the uninsured. She then took on a senior vice president position at AtlantiCare, where she led the system’s strategic transformational work toward accountable care. Dr. Schneider did not hesitate when she learned of the opportunity to become board certified in CI.
"It’s the birth of a new specialty; why not get involved at the very beginning?" said Dr. Schneider, who now serves as chief medical officer for Medecision, a national provider of health care management solutions. CI "by definition, it’s in my everyday work. It’s my role to help make sure we are helping customers use this correctly, understand what our pain points are, and build the right kind of tools to solve problems of effectiveness and efficiency."
Along with bringing new information and technology terms to her current position, her CI training has enabled Dr. Schneider to expand her professional network of clinical informaticians and industry experts, she said.
"One really great benefit is that you meet other people that either do something similar to you or understand the role that you’re in," she said. "Having that peer network is going to be really nice. It’s nice to have recognition that you have expertise in a field. It’s fun to be there at the beginning and participate in the debate about what’s relevant and where it’s going to be in a few years."
For other recently certified physicians, the subspecialty is a door to countless professional paths.
"I became certified to update my skill set and expand my career options," said Dr. Gretchen Purcell Jackson, of the department of pediatric surgery at Vanderbilt University Medical Center, Nashville, Tenn. "I found the quality improvement and project management part of the certification really useful."
In her current practice, Dr. Jackson’s CI training aids in a range of projects, such as helping with a grant she received to study information needs and information management practices of pregnant women and their caregivers.
"The project management aspect of my CI training has been very useful in helping me organize a large clinical study," said Dr. Jackson, who has a PhD in medical information sciences from Stanford (Calif.) University. In addition, "I have recently been asked to help oversee a project that involves coordinating the efforts and technologies from Vanderbilt health information systems, a corporate partner, a non-profit research foundation, and a large funded research project. I use every aspect of my CI training to guide this project. It requires leadership, project management, quality improvement, and clinical and technological expertise."
Meanwhile, Dr. Peter Killoran, a Texas anesthesiologist, is using his CI training to help track patient outcomes and evaluate data for the University of Texas Health Science Center at Houston, School of Biomedical Informatics. Dr. Killoran’s work includes improving health care quality and safety through health information technology and biomedical informatics.
"Quality improvement is a big part of the curriculum for this specialty," said Dr. Killoran, an assistant professor of anesthesiology at the UTHealth Medical School. "That’s because increasingly, medicine is focusing on improving outcomes and the rational use of heath care resources, and all of that comes down to the data."
As the field of CI continues to grow, health providers are needed to participate in the subspecialty and add their voices, said Dr. Genevieve Melton-Meaux, of the department of surgery at the University of Minnesota, Minneapolis, and a faculty fellow for the university’s Institute for Health Informatics. She was recently CI certified.
"The electronic health record and health information technology are the ‘nervous system’ of clinical care," she said. "There are important opportunities to improve the design, implementation, optimization, and use of these technologies and their resultant data, which will ultimately help to improve the efficiency and safety of health care, as well as improve the process of clinical discovery."
Legal climate for ob.gyns. results in delayed retirements, no insurance
Seventy-one-year-old obstetrician-gynecologist Josefina Domingo has practiced in the small New York town of Lowville for 40 years. While she loves her patients, she has often considered retiring and even attempted it – twice. But each time, the lack of ob.gyn. successors drew her back to her patients.
"Through the years, it’s been very tough to get someone to stay here permanently," she said. "This is a very small county. Malpractice insurance is very high. Besides difficulty in recruiting, [getting] recruits to stay [has been] difficult. Even in a small town, lawsuits are here to stay."
Similar scenarios are playing out in small and large cities across the country as the legal climate for ob.gyns. continues to worsen. Medical liability premiums for ob.gyns. remain the highest of all specialties, with enormous settlements and multimillion dollar jury verdicts the norm in some areas.
According to a 2012 survey of 9,000 practicing ob.gyns. by the American Congress of Obstetricians and Gynecologists, 77% of ob.gyns. have had at least one professional liability claim during their career, with an average of 2.6 claims per ob.gyn. The 2012 survey showed that more than half of ob.gyns. made changes to their practice as a result of the high cost or availability of liability insurance. Of those physicians, 15% increased the number of cesarean deliveries, 13.5% stopped performing vaginal birth after cesarean delivery, 8% decreased the total number of deliveries, and 5% stopped practicing obstetrics altogether.
"Ob.gyns. continue to significantly limit their services and change how and where they practice due to the unreasonably high risk of litigation in our profession," ACOG immediate past president James T. Breeden said in a statement. "As millions more women begin to access health care under the Affordable Care Act, it is imperative that Congress pass meaningful medical liability reform."
In Dr. Domingo’s case, high malpractice premiums and the area’s rural environment have long contributed to recruiting challenges for Lowville and its surrounding areas, she said in an interview. Dr. Domingo moved to Lowville in 1974 after being recruited by a local private practice ob.gyn. When he retired, she spent 3 years as the only ob-gyn in the county.
"For 3 years, I was by myself," said Dr. Domingo. "It was terrible. There were no other obstetricians I could relate to. If I had to [perform] a C-section, I had to get a surgeon to help. There was no one to brainstorm with."
As time passed, other ob.gyns. came and went, each spending just a few years in Lowville. When Dr. Domingo attempted to retire for a second time in 2003, one other ob.gyn. in the county remained. A year later, an administrator at the local hospital asked if she would return. She is now employed by Lewis County General Hospital.
"They couldn’t recruit anybody [else]," she said. "I was supposed to come back and stay for 2 years. It’s been 9 years and I’m still here."
Smaller towns are not the only areas struggling to retain ob.gyns. because of poor legal climates. Philadelphia, for instance, has only two remaining private practice ob.gyns. and six hospital maternity units. Rampant lawsuits and exorbitant insurance premiums have forced most physicians to abandon their practices, said Dr. Owen Montgomery, chair of the obstetrics and gynecology department at Drexel University, Philadelphia. The only maternity programs remaining are located at teaching institutions or hospitals.
"Philadelphia is the epicenter of the medical liability crisis," Dr. Montgomery said in an interview. "Private practice is now gone. Ninety-nine percent of all practicing ob.gyns. in Philadelphia are now employed by one of the six remaining maternity programs.
Additionally, insurers that once operated in the city have dropped all ob.gyns. from their policies. Practicing ob.gyns. or their employers must now be self-insured. This means creating your own company and developing reserves for rainy days, Dr. Montgomery said. It also means confronting significant risks if large legal awards are ever levied.
"There’s very real concern on the part of the university that a $40 million judgment against the hospital could impact university management ... research or endowments," he said.
Physicians and legal experts say in order to mitigate the bleak legal landscape for ob.gyns, stronger tort reforms are needed at the state and federal levels. One such initiative under evaluation is the Saving Lives, Saving Costs Act (H.R. 4106), a medical malpractice safe harbor bill recently proposed to Congress. The house bill would create a system to reduce lawsuits against Medicare and Medicaid providers and allow doctors to request that state suits be moved to federal court. Under the act, professional associations would develop clinical practice guidelines that could protect physicians who are sued. Doctor defendants could argue they followed proper practice standards, which would suspend the legal proceedings while a medical review panel investigated the case. The bill in March was referred to the Subcommittee on the Constitution and Civil Justice for review.
"The bipartisan Saving Lives, Saving Costs Act is a practical way to bring down the skyrocketing cost of health care, and to make the system work better for patients that people from both parties can get behind," Dr. Ami Bera (D-Calif.) said in a statement. "As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that."
Dr. Montgomery believes in order for positive change to occur for the ob.gyn.–practice climate, the issue must become more than just a problem between "doctors and lawyers."
"Access to care and quality of care have to become issues for citizens, not just physicians," he said.
Seventy-one-year-old obstetrician-gynecologist Josefina Domingo has practiced in the small New York town of Lowville for 40 years. While she loves her patients, she has often considered retiring and even attempted it – twice. But each time, the lack of ob.gyn. successors drew her back to her patients.
"Through the years, it’s been very tough to get someone to stay here permanently," she said. "This is a very small county. Malpractice insurance is very high. Besides difficulty in recruiting, [getting] recruits to stay [has been] difficult. Even in a small town, lawsuits are here to stay."
Similar scenarios are playing out in small and large cities across the country as the legal climate for ob.gyns. continues to worsen. Medical liability premiums for ob.gyns. remain the highest of all specialties, with enormous settlements and multimillion dollar jury verdicts the norm in some areas.
According to a 2012 survey of 9,000 practicing ob.gyns. by the American Congress of Obstetricians and Gynecologists, 77% of ob.gyns. have had at least one professional liability claim during their career, with an average of 2.6 claims per ob.gyn. The 2012 survey showed that more than half of ob.gyns. made changes to their practice as a result of the high cost or availability of liability insurance. Of those physicians, 15% increased the number of cesarean deliveries, 13.5% stopped performing vaginal birth after cesarean delivery, 8% decreased the total number of deliveries, and 5% stopped practicing obstetrics altogether.
"Ob.gyns. continue to significantly limit their services and change how and where they practice due to the unreasonably high risk of litigation in our profession," ACOG immediate past president James T. Breeden said in a statement. "As millions more women begin to access health care under the Affordable Care Act, it is imperative that Congress pass meaningful medical liability reform."
In Dr. Domingo’s case, high malpractice premiums and the area’s rural environment have long contributed to recruiting challenges for Lowville and its surrounding areas, she said in an interview. Dr. Domingo moved to Lowville in 1974 after being recruited by a local private practice ob.gyn. When he retired, she spent 3 years as the only ob-gyn in the county.
"For 3 years, I was by myself," said Dr. Domingo. "It was terrible. There were no other obstetricians I could relate to. If I had to [perform] a C-section, I had to get a surgeon to help. There was no one to brainstorm with."
As time passed, other ob.gyns. came and went, each spending just a few years in Lowville. When Dr. Domingo attempted to retire for a second time in 2003, one other ob.gyn. in the county remained. A year later, an administrator at the local hospital asked if she would return. She is now employed by Lewis County General Hospital.
"They couldn’t recruit anybody [else]," she said. "I was supposed to come back and stay for 2 years. It’s been 9 years and I’m still here."
Smaller towns are not the only areas struggling to retain ob.gyns. because of poor legal climates. Philadelphia, for instance, has only two remaining private practice ob.gyns. and six hospital maternity units. Rampant lawsuits and exorbitant insurance premiums have forced most physicians to abandon their practices, said Dr. Owen Montgomery, chair of the obstetrics and gynecology department at Drexel University, Philadelphia. The only maternity programs remaining are located at teaching institutions or hospitals.
"Philadelphia is the epicenter of the medical liability crisis," Dr. Montgomery said in an interview. "Private practice is now gone. Ninety-nine percent of all practicing ob.gyns. in Philadelphia are now employed by one of the six remaining maternity programs.
Additionally, insurers that once operated in the city have dropped all ob.gyns. from their policies. Practicing ob.gyns. or their employers must now be self-insured. This means creating your own company and developing reserves for rainy days, Dr. Montgomery said. It also means confronting significant risks if large legal awards are ever levied.
"There’s very real concern on the part of the university that a $40 million judgment against the hospital could impact university management ... research or endowments," he said.
Physicians and legal experts say in order to mitigate the bleak legal landscape for ob.gyns, stronger tort reforms are needed at the state and federal levels. One such initiative under evaluation is the Saving Lives, Saving Costs Act (H.R. 4106), a medical malpractice safe harbor bill recently proposed to Congress. The house bill would create a system to reduce lawsuits against Medicare and Medicaid providers and allow doctors to request that state suits be moved to federal court. Under the act, professional associations would develop clinical practice guidelines that could protect physicians who are sued. Doctor defendants could argue they followed proper practice standards, which would suspend the legal proceedings while a medical review panel investigated the case. The bill in March was referred to the Subcommittee on the Constitution and Civil Justice for review.
"The bipartisan Saving Lives, Saving Costs Act is a practical way to bring down the skyrocketing cost of health care, and to make the system work better for patients that people from both parties can get behind," Dr. Ami Bera (D-Calif.) said in a statement. "As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that."
Dr. Montgomery believes in order for positive change to occur for the ob.gyn.–practice climate, the issue must become more than just a problem between "doctors and lawyers."
"Access to care and quality of care have to become issues for citizens, not just physicians," he said.
Seventy-one-year-old obstetrician-gynecologist Josefina Domingo has practiced in the small New York town of Lowville for 40 years. While she loves her patients, she has often considered retiring and even attempted it – twice. But each time, the lack of ob.gyn. successors drew her back to her patients.
"Through the years, it’s been very tough to get someone to stay here permanently," she said. "This is a very small county. Malpractice insurance is very high. Besides difficulty in recruiting, [getting] recruits to stay [has been] difficult. Even in a small town, lawsuits are here to stay."
Similar scenarios are playing out in small and large cities across the country as the legal climate for ob.gyns. continues to worsen. Medical liability premiums for ob.gyns. remain the highest of all specialties, with enormous settlements and multimillion dollar jury verdicts the norm in some areas.
According to a 2012 survey of 9,000 practicing ob.gyns. by the American Congress of Obstetricians and Gynecologists, 77% of ob.gyns. have had at least one professional liability claim during their career, with an average of 2.6 claims per ob.gyn. The 2012 survey showed that more than half of ob.gyns. made changes to their practice as a result of the high cost or availability of liability insurance. Of those physicians, 15% increased the number of cesarean deliveries, 13.5% stopped performing vaginal birth after cesarean delivery, 8% decreased the total number of deliveries, and 5% stopped practicing obstetrics altogether.
"Ob.gyns. continue to significantly limit their services and change how and where they practice due to the unreasonably high risk of litigation in our profession," ACOG immediate past president James T. Breeden said in a statement. "As millions more women begin to access health care under the Affordable Care Act, it is imperative that Congress pass meaningful medical liability reform."
In Dr. Domingo’s case, high malpractice premiums and the area’s rural environment have long contributed to recruiting challenges for Lowville and its surrounding areas, she said in an interview. Dr. Domingo moved to Lowville in 1974 after being recruited by a local private practice ob.gyn. When he retired, she spent 3 years as the only ob-gyn in the county.
"For 3 years, I was by myself," said Dr. Domingo. "It was terrible. There were no other obstetricians I could relate to. If I had to [perform] a C-section, I had to get a surgeon to help. There was no one to brainstorm with."
As time passed, other ob.gyns. came and went, each spending just a few years in Lowville. When Dr. Domingo attempted to retire for a second time in 2003, one other ob.gyn. in the county remained. A year later, an administrator at the local hospital asked if she would return. She is now employed by Lewis County General Hospital.
"They couldn’t recruit anybody [else]," she said. "I was supposed to come back and stay for 2 years. It’s been 9 years and I’m still here."
Smaller towns are not the only areas struggling to retain ob.gyns. because of poor legal climates. Philadelphia, for instance, has only two remaining private practice ob.gyns. and six hospital maternity units. Rampant lawsuits and exorbitant insurance premiums have forced most physicians to abandon their practices, said Dr. Owen Montgomery, chair of the obstetrics and gynecology department at Drexel University, Philadelphia. The only maternity programs remaining are located at teaching institutions or hospitals.
"Philadelphia is the epicenter of the medical liability crisis," Dr. Montgomery said in an interview. "Private practice is now gone. Ninety-nine percent of all practicing ob.gyns. in Philadelphia are now employed by one of the six remaining maternity programs.
Additionally, insurers that once operated in the city have dropped all ob.gyns. from their policies. Practicing ob.gyns. or their employers must now be self-insured. This means creating your own company and developing reserves for rainy days, Dr. Montgomery said. It also means confronting significant risks if large legal awards are ever levied.
"There’s very real concern on the part of the university that a $40 million judgment against the hospital could impact university management ... research or endowments," he said.
Physicians and legal experts say in order to mitigate the bleak legal landscape for ob.gyns, stronger tort reforms are needed at the state and federal levels. One such initiative under evaluation is the Saving Lives, Saving Costs Act (H.R. 4106), a medical malpractice safe harbor bill recently proposed to Congress. The house bill would create a system to reduce lawsuits against Medicare and Medicaid providers and allow doctors to request that state suits be moved to federal court. Under the act, professional associations would develop clinical practice guidelines that could protect physicians who are sued. Doctor defendants could argue they followed proper practice standards, which would suspend the legal proceedings while a medical review panel investigated the case. The bill in March was referred to the Subcommittee on the Constitution and Civil Justice for review.
"The bipartisan Saving Lives, Saving Costs Act is a practical way to bring down the skyrocketing cost of health care, and to make the system work better for patients that people from both parties can get behind," Dr. Ami Bera (D-Calif.) said in a statement. "As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that."
Dr. Montgomery believes in order for positive change to occur for the ob.gyn.–practice climate, the issue must become more than just a problem between "doctors and lawyers."
"Access to care and quality of care have to become issues for citizens, not just physicians," he said.


















