User login
Backlog takes toll on physicians who appeal audits
After being audited by Medicare and hit with a $150,000 recoupment demand, California primary care physician Robert E. Feiss was determined to fight the findings.
Auditors had declared that Dr. Feiss was providing care to patients in their homes that did not qualify as being medically necessary. He appealed, and after 3 long years of paperwork, petitions, and hearings, the doctor was successful in overturning the decision.
“It was a scary thing, without a doubt,” said Dr. Feiss, who is in private practice in Ventura, Calif., and treats a large population of seniors in their homes. “But I felt very strongly about what I do and am committed to what I do. It’s a bittersweet victory because, aside from the incredible stress it took, there was no recovery of legal fees. There was no recovery of damages or of the time spent away from my practice.”
Dr. Feiss’s experience is not unique. He is one of thousands of health providers who decide to appeal their audits by the federal government. Win or lose, audit experts say the course of an audit appeal is often long and arduous. Along with financial uncertainty and legal expenses, physicians face substantial delays before their case can be resolved. The wait time for an appeal to be assigned to an administrative law judge is about 2 years, according to a December 2013 letter from the Office of Medicare Hearings and Appeals (OMHA). After assignment, it’s another 6 months before the case is heard.
The wait times reflect OMHA’s enormous backlog of appeals. In fiscal 2013, OMHA received 384,151 new appeals, up from 59,600 in 2011, according to July testimony before Congress by Nancy J. Griswold, OMHA chief administrative law judge. Fiscal 2014 appeals through July 1 totaled 509,124. More than 800,000 OMHA appeals were pending as of July, and the office continues to receive 1 year’s worth of appeals every 4 to 6 weeks, Judge Griswold said. In July a coalition of medical associations, including the American Medical Association, wrote a letter to OMHA urging the agency to immediately remedy the excessive surplus.
“The backlog is a huge problem,” said Jessica L. Gustafson, a Southfield, Mich., health law attorney and vice chair of the American Bar Association Health Law Section’s Physician Issues Interest Group. “One major implication of the backlog is a cash flow interruption to a physician’s practice.”
Ms. Gustafson noted that under federal law, the Centers for Medicare & Medicaid Services is prohibited from recouping an alleged overpayment during the first two stages of an appeal. However, following a reconsideration decision, the CMS is authorized to recoup an alleged overpayment and withhold future payments as an offset to the alleged overpayment. Because of the backlog, the CMS can hold onto a physician’s money for years, until a final determination is made, she said.
In Dr. Feiss’s case, the CMS withheld his Medicare payments during the appeals process, he said. He hired Ms. Gustafson, who assisted him through three rounds of appeals before the case was assigned to an administrative law judge. The process was fraught with unexpected costs, such as hiring an accountant and paying for expert witnesses, he said.
“It was a very stressful period in my life,” Dr. Feiss said in an interview. “It’s almost like having two jobs. I was trying to maintain my practice, but I was trying to compile all this information that was required by Medicare and educate myself in terms of the terminology and definitions of Medicare law to understand their vernacular.”
While the lengthy process of an audit appeal may sound off-putting, experts stress that a large portion of physician appeals are successful. In 2013, 60% of Medicare Part B claims appealed were overturned in providers’ favor, according to a September report released by the CMS. In contrast, only 11% of Medicare Part A claims were overturned on appeal. Of Part B appeals associated with overpayments, about 9% of determinations were overturned in 2013.
For physicians deciding whether to appeal an audit, key considerations include whether their argument against the recoupment is sound and if they have sufficient documentation, said Michael E. Clark, a health law attorney in Houston, speaking in an interview.
“Physicians should assess whether they have meritorious grounds for an appeal before doing so because if the Qualified Independent Contractor renders an adverse decision then they will be required to pay interest on the overpayments in addition to the amount of the overpayment,” said Mr. Clark, who is chair of the American Bar Association’s Health Law Section. “Some basic issues are whether the underlying documentation is complete and supports the claims for reimbursement that have been made and whether the coding used is appropriate.”
Physicians should also consider the number of claims at issue and the amount of payment before deciding whether to pursue the appeal, Ms. Gustafson adds.
“In many physician cases, the amount at issue may not be worth the time associated with pursuing the appeal,” she said.
On the other hand, appealing is the only way to stop a recoupment demand, said Dr. Brent Moody, a member of the American Academy of Dermatology’s Workgroup on Innovation Payment Delivery and an American Academy of Dermatology Association adviser to the American Medical Association’s Relative Value Scale Update Committee (RUC).
“If a provider thinks they’re in the right, they should appeal,” Dr. Moody said in an interview. “It’s their right to appeal. They should exercise that right if they believe the RAC audit is incorrect.”
The government meanwhile, is taking steps to reduce the appeals backlog. Earlier this year, CMS offered to pay hospitals 68% of inpatient-status claims in exchange for withdrawing their pending appeals. If hospitals accept the offer, the move would free up the system for other pending claims, Ms. Gustafson said.
Mr. Clark does not foresee the appeals bottleneck truly loosening until Congress funds additional administrative law judge positions, he said.
“There’s a well known saying that well describes this problem: ‘Justice delayed is justice denied,’ ” Mr. Clark said. “The specter of having to wait months or years before an appeal can be heard is simply inexcusable given the intrusive nature of the RAC audits, the uncertainties involved, and the impact on the ability of physicians to practice medicine without fear of financial ruin.”
On Twitter @legal_med
After being audited by Medicare and hit with a $150,000 recoupment demand, California primary care physician Robert E. Feiss was determined to fight the findings.
Auditors had declared that Dr. Feiss was providing care to patients in their homes that did not qualify as being medically necessary. He appealed, and after 3 long years of paperwork, petitions, and hearings, the doctor was successful in overturning the decision.
“It was a scary thing, without a doubt,” said Dr. Feiss, who is in private practice in Ventura, Calif., and treats a large population of seniors in their homes. “But I felt very strongly about what I do and am committed to what I do. It’s a bittersweet victory because, aside from the incredible stress it took, there was no recovery of legal fees. There was no recovery of damages or of the time spent away from my practice.”
Dr. Feiss’s experience is not unique. He is one of thousands of health providers who decide to appeal their audits by the federal government. Win or lose, audit experts say the course of an audit appeal is often long and arduous. Along with financial uncertainty and legal expenses, physicians face substantial delays before their case can be resolved. The wait time for an appeal to be assigned to an administrative law judge is about 2 years, according to a December 2013 letter from the Office of Medicare Hearings and Appeals (OMHA). After assignment, it’s another 6 months before the case is heard.
The wait times reflect OMHA’s enormous backlog of appeals. In fiscal 2013, OMHA received 384,151 new appeals, up from 59,600 in 2011, according to July testimony before Congress by Nancy J. Griswold, OMHA chief administrative law judge. Fiscal 2014 appeals through July 1 totaled 509,124. More than 800,000 OMHA appeals were pending as of July, and the office continues to receive 1 year’s worth of appeals every 4 to 6 weeks, Judge Griswold said. In July a coalition of medical associations, including the American Medical Association, wrote a letter to OMHA urging the agency to immediately remedy the excessive surplus.
“The backlog is a huge problem,” said Jessica L. Gustafson, a Southfield, Mich., health law attorney and vice chair of the American Bar Association Health Law Section’s Physician Issues Interest Group. “One major implication of the backlog is a cash flow interruption to a physician’s practice.”
Ms. Gustafson noted that under federal law, the Centers for Medicare & Medicaid Services is prohibited from recouping an alleged overpayment during the first two stages of an appeal. However, following a reconsideration decision, the CMS is authorized to recoup an alleged overpayment and withhold future payments as an offset to the alleged overpayment. Because of the backlog, the CMS can hold onto a physician’s money for years, until a final determination is made, she said.
In Dr. Feiss’s case, the CMS withheld his Medicare payments during the appeals process, he said. He hired Ms. Gustafson, who assisted him through three rounds of appeals before the case was assigned to an administrative law judge. The process was fraught with unexpected costs, such as hiring an accountant and paying for expert witnesses, he said.
“It was a very stressful period in my life,” Dr. Feiss said in an interview. “It’s almost like having two jobs. I was trying to maintain my practice, but I was trying to compile all this information that was required by Medicare and educate myself in terms of the terminology and definitions of Medicare law to understand their vernacular.”
While the lengthy process of an audit appeal may sound off-putting, experts stress that a large portion of physician appeals are successful. In 2013, 60% of Medicare Part B claims appealed were overturned in providers’ favor, according to a September report released by the CMS. In contrast, only 11% of Medicare Part A claims were overturned on appeal. Of Part B appeals associated with overpayments, about 9% of determinations were overturned in 2013.
For physicians deciding whether to appeal an audit, key considerations include whether their argument against the recoupment is sound and if they have sufficient documentation, said Michael E. Clark, a health law attorney in Houston, speaking in an interview.
“Physicians should assess whether they have meritorious grounds for an appeal before doing so because if the Qualified Independent Contractor renders an adverse decision then they will be required to pay interest on the overpayments in addition to the amount of the overpayment,” said Mr. Clark, who is chair of the American Bar Association’s Health Law Section. “Some basic issues are whether the underlying documentation is complete and supports the claims for reimbursement that have been made and whether the coding used is appropriate.”
Physicians should also consider the number of claims at issue and the amount of payment before deciding whether to pursue the appeal, Ms. Gustafson adds.
“In many physician cases, the amount at issue may not be worth the time associated with pursuing the appeal,” she said.
On the other hand, appealing is the only way to stop a recoupment demand, said Dr. Brent Moody, a member of the American Academy of Dermatology’s Workgroup on Innovation Payment Delivery and an American Academy of Dermatology Association adviser to the American Medical Association’s Relative Value Scale Update Committee (RUC).
“If a provider thinks they’re in the right, they should appeal,” Dr. Moody said in an interview. “It’s their right to appeal. They should exercise that right if they believe the RAC audit is incorrect.”
The government meanwhile, is taking steps to reduce the appeals backlog. Earlier this year, CMS offered to pay hospitals 68% of inpatient-status claims in exchange for withdrawing their pending appeals. If hospitals accept the offer, the move would free up the system for other pending claims, Ms. Gustafson said.
Mr. Clark does not foresee the appeals bottleneck truly loosening until Congress funds additional administrative law judge positions, he said.
“There’s a well known saying that well describes this problem: ‘Justice delayed is justice denied,’ ” Mr. Clark said. “The specter of having to wait months or years before an appeal can be heard is simply inexcusable given the intrusive nature of the RAC audits, the uncertainties involved, and the impact on the ability of physicians to practice medicine without fear of financial ruin.”
On Twitter @legal_med
After being audited by Medicare and hit with a $150,000 recoupment demand, California primary care physician Robert E. Feiss was determined to fight the findings.
Auditors had declared that Dr. Feiss was providing care to patients in their homes that did not qualify as being medically necessary. He appealed, and after 3 long years of paperwork, petitions, and hearings, the doctor was successful in overturning the decision.
“It was a scary thing, without a doubt,” said Dr. Feiss, who is in private practice in Ventura, Calif., and treats a large population of seniors in their homes. “But I felt very strongly about what I do and am committed to what I do. It’s a bittersweet victory because, aside from the incredible stress it took, there was no recovery of legal fees. There was no recovery of damages or of the time spent away from my practice.”
Dr. Feiss’s experience is not unique. He is one of thousands of health providers who decide to appeal their audits by the federal government. Win or lose, audit experts say the course of an audit appeal is often long and arduous. Along with financial uncertainty and legal expenses, physicians face substantial delays before their case can be resolved. The wait time for an appeal to be assigned to an administrative law judge is about 2 years, according to a December 2013 letter from the Office of Medicare Hearings and Appeals (OMHA). After assignment, it’s another 6 months before the case is heard.
The wait times reflect OMHA’s enormous backlog of appeals. In fiscal 2013, OMHA received 384,151 new appeals, up from 59,600 in 2011, according to July testimony before Congress by Nancy J. Griswold, OMHA chief administrative law judge. Fiscal 2014 appeals through July 1 totaled 509,124. More than 800,000 OMHA appeals were pending as of July, and the office continues to receive 1 year’s worth of appeals every 4 to 6 weeks, Judge Griswold said. In July a coalition of medical associations, including the American Medical Association, wrote a letter to OMHA urging the agency to immediately remedy the excessive surplus.
“The backlog is a huge problem,” said Jessica L. Gustafson, a Southfield, Mich., health law attorney and vice chair of the American Bar Association Health Law Section’s Physician Issues Interest Group. “One major implication of the backlog is a cash flow interruption to a physician’s practice.”
Ms. Gustafson noted that under federal law, the Centers for Medicare & Medicaid Services is prohibited from recouping an alleged overpayment during the first two stages of an appeal. However, following a reconsideration decision, the CMS is authorized to recoup an alleged overpayment and withhold future payments as an offset to the alleged overpayment. Because of the backlog, the CMS can hold onto a physician’s money for years, until a final determination is made, she said.
In Dr. Feiss’s case, the CMS withheld his Medicare payments during the appeals process, he said. He hired Ms. Gustafson, who assisted him through three rounds of appeals before the case was assigned to an administrative law judge. The process was fraught with unexpected costs, such as hiring an accountant and paying for expert witnesses, he said.
“It was a very stressful period in my life,” Dr. Feiss said in an interview. “It’s almost like having two jobs. I was trying to maintain my practice, but I was trying to compile all this information that was required by Medicare and educate myself in terms of the terminology and definitions of Medicare law to understand their vernacular.”
While the lengthy process of an audit appeal may sound off-putting, experts stress that a large portion of physician appeals are successful. In 2013, 60% of Medicare Part B claims appealed were overturned in providers’ favor, according to a September report released by the CMS. In contrast, only 11% of Medicare Part A claims were overturned on appeal. Of Part B appeals associated with overpayments, about 9% of determinations were overturned in 2013.
For physicians deciding whether to appeal an audit, key considerations include whether their argument against the recoupment is sound and if they have sufficient documentation, said Michael E. Clark, a health law attorney in Houston, speaking in an interview.
“Physicians should assess whether they have meritorious grounds for an appeal before doing so because if the Qualified Independent Contractor renders an adverse decision then they will be required to pay interest on the overpayments in addition to the amount of the overpayment,” said Mr. Clark, who is chair of the American Bar Association’s Health Law Section. “Some basic issues are whether the underlying documentation is complete and supports the claims for reimbursement that have been made and whether the coding used is appropriate.”
Physicians should also consider the number of claims at issue and the amount of payment before deciding whether to pursue the appeal, Ms. Gustafson adds.
“In many physician cases, the amount at issue may not be worth the time associated with pursuing the appeal,” she said.
On the other hand, appealing is the only way to stop a recoupment demand, said Dr. Brent Moody, a member of the American Academy of Dermatology’s Workgroup on Innovation Payment Delivery and an American Academy of Dermatology Association adviser to the American Medical Association’s Relative Value Scale Update Committee (RUC).
“If a provider thinks they’re in the right, they should appeal,” Dr. Moody said in an interview. “It’s their right to appeal. They should exercise that right if they believe the RAC audit is incorrect.”
The government meanwhile, is taking steps to reduce the appeals backlog. Earlier this year, CMS offered to pay hospitals 68% of inpatient-status claims in exchange for withdrawing their pending appeals. If hospitals accept the offer, the move would free up the system for other pending claims, Ms. Gustafson said.
Mr. Clark does not foresee the appeals bottleneck truly loosening until Congress funds additional administrative law judge positions, he said.
“There’s a well known saying that well describes this problem: ‘Justice delayed is justice denied,’ ” Mr. Clark said. “The specter of having to wait months or years before an appeal can be heard is simply inexcusable given the intrusive nature of the RAC audits, the uncertainties involved, and the impact on the ability of physicians to practice medicine without fear of financial ruin.”
On Twitter @legal_med
Calif. ballot question would drug test docs after adverse event
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med
Study: Patient Costs for Contraceptives Sharply Decreasing
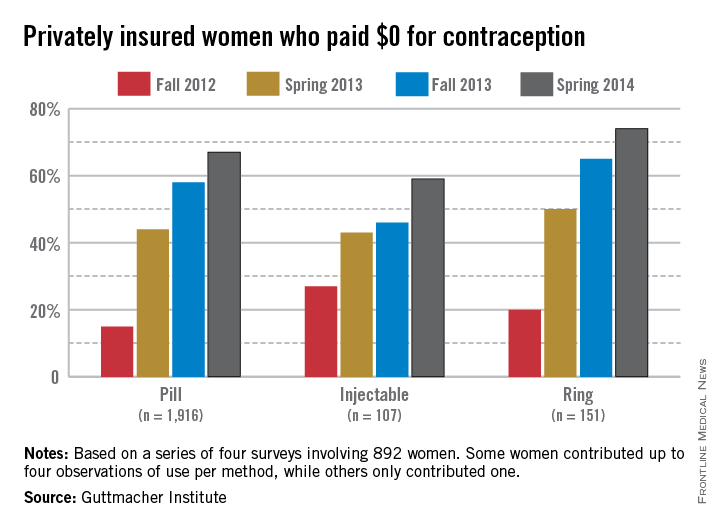
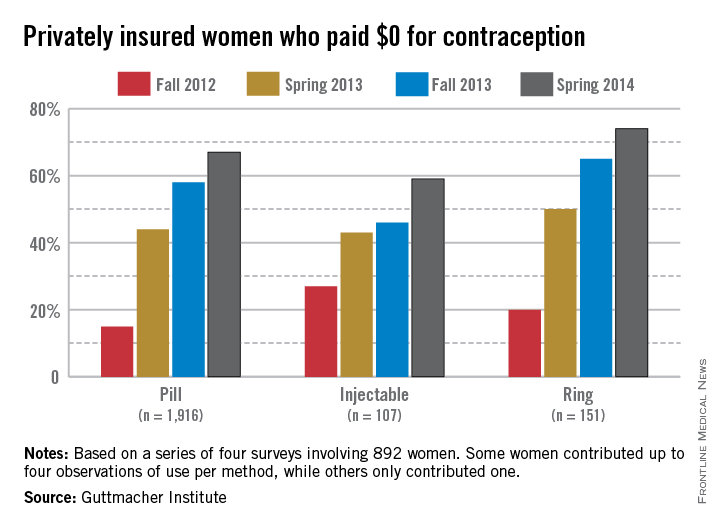
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
Study: Patient costs for contraceptives sharply decreasing
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
On Twitter @legal_med
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
On Twitter @legal_med
The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014, according to a study published online Sept. 18 in Contraception.
Investigators with the Guttmacher Institute surveyed 892 women over 3-week periods in fall 2012, spring 2013, fall 2013, and spring 2014. The women were between 18 and 39 years of age, had private insurance, and used a prescription contraceptive method during any of the four study periods. Results showed that in spring 2014, 598 of the women had paid zero out-of-pocket expenses on oral contraceptive medication, compared with 134 women in fall 2012. Guttmacher analysts credited the increase with the Affordable Care Act’s contraceptive coverage requirement, which started implementation in August 2012.
In addition, the study found the proportion of women who paid nothing out-of-pocket increased from 20% in fall 2012 to 74% in spring 2014 among those using the vaginal ring and from 27% to 59% among women using injectable contraceptives. Of 165 women with private insurance who reported using intrauterine devices in fall 2012, 45% indicated that they paid nothing for the method. The proportion increased to 62% among new users in all three subsequent waves combined. (Contraception 2014 Sept. 18 [doi:10.1016/j.contraception.2014.09.006])
The analysis shows that the ACA’s contraceptive coverage guarantee has had a substantial and rapid impact on eliminating out-of-pocket costs among privately insured women who use contraceptives, the study authors noted.
Even so, Guttmacher researchers said there are still gaps in coverage because of federal guidelines that allow insurers to charge copayments in some situations and that exempt some employer-sponsored health plans on religious grounds.
The ACA’s contraceptive coverage mandate has been the subject of hundreds of lawsuits that argue the requirement violates religious freedoms. The U.S. Supreme Court in June ruled against the mandate as it was applied to two for-profit businesses, Hobby Lobby and Conestoga Wood Specialties. The companies are protected against the mandate by the 1993 Religious Freedom Restoration Act, justices said. In response to the decision, the Centers for Medicare & Medicaid Services on Aug. 22 proposed new rules to accommodate objections to the requirement to certain for-profit entities. Comments on the proposed rules will be accepted for 60 days before a final rule is issued.
Authors of the contraception study reported no conflicts of interest. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
On Twitter @legal_med
Key clinical point: According to researchers, the ACA’s contraceptive coverage guarantee has played a role in eliminating out-of-pocket costs among privately insured women who use contraceptives.
Major finding: The number of privately insured women who paid no out-of-pocket costs for oral contraceptive pills rose from 15% in 2012 to 67% in 2014.
Data source: A survey of 892 women over four different 3-week periods from 2012 to 2014.
Disclosures: The authors have no conflicts of interest to report. The study on which this analysis was based was supported by the JPB Foundation, and additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination under a National Institutes of Health grant.
Watchdog finds security lacking at healthcare.gov, two state marketplaces
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
Survey: Many physicians plan to reduce their workload
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Judges Reveal Secrets to Successful Malpractice Trials
When it comes to the outcome of a medical malpractice jury trial, a physician’s attitude, demeanor, and presentation make all the difference, say judges who’ve presided over many such cases.
"The fact finder has to look at them and find them credible and sincere when they’re hearing their story," said Lorenzo F. Garcia, chief magistrate judge emeritus for the U.S. District Court for the District of New Mexico. "There’s truth and there’s perception, and perception can trump the truth. In litigation, being right isn’t always good enough. You can be right in a claim or right in a defense and still lose if the fact finder doesn’t believe the testimony or dislikes a person, witness, or an attorney."
Exhibiting arrogance or defensiveness when testifying can quickly sway a jury against a defendant doctor, adds Judge Garcia, who provided trial insight with several other judges at the American Conference Institute’s obstetric malpractice claims forum. When taking the stand, it helps to remain respectful at all times, refrain from acting combative, and demonstrate concern when discussing patients who were injured, he said.
Physicians should also be aware of how their attorneys are presenting themselves and interacting with legal parties. Being rude to judges, litigants, or attorneys can have a negative impact on jurors’ view of that particular side, said Sandra Mazer Moss, a retired Philadelphia Court of Common Pleas judge.
Doctors have a critical role in helping court participants understand the medicine surrounding a case, notes Judge Mazer Moss, who also spoke at the ACI conference. This includes properly preparing attorneys to speak about medical events and ensuring jurors clearly understand medical facts.
Health providers "can help explain procedures so that attorneys can understand and relay the information," she noted. "When you put a witness on the stand, they have to [clearly] explain how the procedure was done. It would help if the doctor had physical aids, PowerPoint [slides], or models."
However, Judge Garcia stresses that physicians and their attorneys shouldn’t overly rely on technology during a trial. He has presided over medical malpractice cases in which electronic equipment failed and caused long delays, he said. In some cases, the technology problems prevented plaintiffs or defendants from effectively presenting their arguments.
"To start a trial in such a fashion and see that jurors are not happy and that time is going by; there’s a valuable lesson" there, he said. "Make sure you practice and try the technology ahead of time. [Technology] can be exceedingly effective, or it can be a disaster if it doesn’t work well."
Another contributor to a successful malpractice case is the ability to tell a powerful story, Judge Garcia said. In his experience, litigants who choose a central theme and weave that idea throughout the trial are most effective. For example, the defense may open the trial by emphasizing that the case is about a patient’s bad luck, not bad medicine, and coming back to that point throughout the proceedings.
"Quite frankly, that’s what jurors like to hear," he said. "They want to hear a story, so part of the preparation is trying to find the most important [piece] of the litigation and developing a story that can be a recurring theme. The development of a theme is one of the most significant tasks parties can engage in, and it assists in the presentation of the claim or the defense."
Can your appearance look affect the outcome of a malpractice suit? Take our Quick Poll on the Hospitalist News homepage.
When it comes to the outcome of a medical malpractice jury trial, a physician’s attitude, demeanor, and presentation make all the difference, say judges who’ve presided over many such cases.
"The fact finder has to look at them and find them credible and sincere when they’re hearing their story," said Lorenzo F. Garcia, chief magistrate judge emeritus for the U.S. District Court for the District of New Mexico. "There’s truth and there’s perception, and perception can trump the truth. In litigation, being right isn’t always good enough. You can be right in a claim or right in a defense and still lose if the fact finder doesn’t believe the testimony or dislikes a person, witness, or an attorney."
Exhibiting arrogance or defensiveness when testifying can quickly sway a jury against a defendant doctor, adds Judge Garcia, who provided trial insight with several other judges at the American Conference Institute’s obstetric malpractice claims forum. When taking the stand, it helps to remain respectful at all times, refrain from acting combative, and demonstrate concern when discussing patients who were injured, he said.
Physicians should also be aware of how their attorneys are presenting themselves and interacting with legal parties. Being rude to judges, litigants, or attorneys can have a negative impact on jurors’ view of that particular side, said Sandra Mazer Moss, a retired Philadelphia Court of Common Pleas judge.
Doctors have a critical role in helping court participants understand the medicine surrounding a case, notes Judge Mazer Moss, who also spoke at the ACI conference. This includes properly preparing attorneys to speak about medical events and ensuring jurors clearly understand medical facts.
Health providers "can help explain procedures so that attorneys can understand and relay the information," she noted. "When you put a witness on the stand, they have to [clearly] explain how the procedure was done. It would help if the doctor had physical aids, PowerPoint [slides], or models."
However, Judge Garcia stresses that physicians and their attorneys shouldn’t overly rely on technology during a trial. He has presided over medical malpractice cases in which electronic equipment failed and caused long delays, he said. In some cases, the technology problems prevented plaintiffs or defendants from effectively presenting their arguments.
"To start a trial in such a fashion and see that jurors are not happy and that time is going by; there’s a valuable lesson" there, he said. "Make sure you practice and try the technology ahead of time. [Technology] can be exceedingly effective, or it can be a disaster if it doesn’t work well."
Another contributor to a successful malpractice case is the ability to tell a powerful story, Judge Garcia said. In his experience, litigants who choose a central theme and weave that idea throughout the trial are most effective. For example, the defense may open the trial by emphasizing that the case is about a patient’s bad luck, not bad medicine, and coming back to that point throughout the proceedings.
"Quite frankly, that’s what jurors like to hear," he said. "They want to hear a story, so part of the preparation is trying to find the most important [piece] of the litigation and developing a story that can be a recurring theme. The development of a theme is one of the most significant tasks parties can engage in, and it assists in the presentation of the claim or the defense."
Can your appearance look affect the outcome of a malpractice suit? Take our Quick Poll on the Hospitalist News homepage.
When it comes to the outcome of a medical malpractice jury trial, a physician’s attitude, demeanor, and presentation make all the difference, say judges who’ve presided over many such cases.
"The fact finder has to look at them and find them credible and sincere when they’re hearing their story," said Lorenzo F. Garcia, chief magistrate judge emeritus for the U.S. District Court for the District of New Mexico. "There’s truth and there’s perception, and perception can trump the truth. In litigation, being right isn’t always good enough. You can be right in a claim or right in a defense and still lose if the fact finder doesn’t believe the testimony or dislikes a person, witness, or an attorney."
Exhibiting arrogance or defensiveness when testifying can quickly sway a jury against a defendant doctor, adds Judge Garcia, who provided trial insight with several other judges at the American Conference Institute’s obstetric malpractice claims forum. When taking the stand, it helps to remain respectful at all times, refrain from acting combative, and demonstrate concern when discussing patients who were injured, he said.
Physicians should also be aware of how their attorneys are presenting themselves and interacting with legal parties. Being rude to judges, litigants, or attorneys can have a negative impact on jurors’ view of that particular side, said Sandra Mazer Moss, a retired Philadelphia Court of Common Pleas judge.
Doctors have a critical role in helping court participants understand the medicine surrounding a case, notes Judge Mazer Moss, who also spoke at the ACI conference. This includes properly preparing attorneys to speak about medical events and ensuring jurors clearly understand medical facts.
Health providers "can help explain procedures so that attorneys can understand and relay the information," she noted. "When you put a witness on the stand, they have to [clearly] explain how the procedure was done. It would help if the doctor had physical aids, PowerPoint [slides], or models."
However, Judge Garcia stresses that physicians and their attorneys shouldn’t overly rely on technology during a trial. He has presided over medical malpractice cases in which electronic equipment failed and caused long delays, he said. In some cases, the technology problems prevented plaintiffs or defendants from effectively presenting their arguments.
"To start a trial in such a fashion and see that jurors are not happy and that time is going by; there’s a valuable lesson" there, he said. "Make sure you practice and try the technology ahead of time. [Technology] can be exceedingly effective, or it can be a disaster if it doesn’t work well."
Another contributor to a successful malpractice case is the ability to tell a powerful story, Judge Garcia said. In his experience, litigants who choose a central theme and weave that idea throughout the trial are most effective. For example, the defense may open the trial by emphasizing that the case is about a patient’s bad luck, not bad medicine, and coming back to that point throughout the proceedings.
"Quite frankly, that’s what jurors like to hear," he said. "They want to hear a story, so part of the preparation is trying to find the most important [piece] of the litigation and developing a story that can be a recurring theme. The development of a theme is one of the most significant tasks parties can engage in, and it assists in the presentation of the claim or the defense."
Can your appearance look affect the outcome of a malpractice suit? Take our Quick Poll on the Hospitalist News homepage.
Open Payments may help drive malpractice claims; review period closes Sept. 11
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
Federation finalizes telemedicine compact for legislative review
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
Teamwork heart of new pediatric ACO
Health Network by Cincinnati Children’s is putting a new spin on an old idea – capitation – and using it to better serve high-risk pediatric patients in southern Ohio.
The recently launched community-based network (HNCC) of physicians, health providers, and social service providers focuses on specialized case management for low-income children. Nonphysician members at the accountable care organization include nurses, social workers, mental and behavioral health care specialists, and community health workers.
"We can make those staff available to anyone that our physicians or providers see as somebody who needs some sort of help, whether it’s medical or social," Dr. Colleen Kraft, HNCC medical director, said in an interview. "The real success of the network is in the connection and relationship with families to get them to resources that help their child and prevent high-cost care."
HNCC, which started in July 2013, serves Medicaid families in eight Ohio counties and has nearly 35,000 members, 150 of whom are enrolled in high-risk case management. The network contracts with two Ohio Medicaid insurers, Paramount and Molina Healthcare – also called managed care organizations (MCOs) – to provide case management for complex patients. Any practice that accepts Paramount or Molina has access to the network’s services, whether it is a Cincinnati Children’s hospital practice, a private practice, or a federally qualified health center.
The network receives a global, capitated fee for each child in the MCO plan to spend on medical management. While a capitated payment model is nothing new, the way in which the network uses the dollars is unique, Dr. Kraft said. Traditionally, MCOs provide capitated payments to physicians for face-to-face patient care. HNCC concentrates its funds on medical management. Paramount and Molina Healthcare contract separately with physicians for payments.
"The biggest difference with this model is we are not responsible for physician payment," Dr. Kraft said. "We’ve contracted for those medical management dollars, and we’re doing our own care management for these families and building of [care] teams. There’s a lot of interaction between our vulnerable families and our care managers, and we’re able to help them navigate the health care system."
The network’s relationship with primary care providers plays a central role in the system’s success. It’s no secret that doctors are often frustrated with Medicaid’s low payments and the red tape and hassles the system brings, Dr. Kraft said. For physicians, network advantages include more feedback about cases, broader coverage of treatments, and the potential for bonuses.
HCNN uses part of its funding to provide bonuses for physician practices that see a high number of Medicaid patients. The network provides $2 per member, per month in incentive payments for all health network patients in a practice, well over what Medicaid pays, Dr. Kraft said. In addition, physician administrators and case managers regularly contact and discuss cases with physicians, said Dr. Camille Graham, HCNN’s executive community physician liaison and a Cincinnati-based pediatrician in private practice. “From the outset, the network was determined to partner with primary care physicians in a meaningful way,” she said. “With most insurance companies, the primary care physician doesn’t receive any feedback about case management other than: The case was closed, there was no response, or we’re continuing (management). With the network, there’s more of a dialogue about what’s working and what’s not working with this family.”*
HCNN has the ability to pay for services that traditionally would not be covered by Medicaid, Dr. Kraft said. Administrators conduct utilization management reviews for referrals in which they evaluate the need of items such as durable medical equipment and high-cost testing. In a recent case, family members requested an additional gastrostomy tube for their child in case the current tube became unattached. Medicaid would not pay for a second tube, although it would have paid for an emergency department visit if the original tube were to detach, she said. In another case, Medicaid refused to pay for an out-of-network provider to administer an approved medication to a pregnant teenager.
"We can pay for an extra G-tube and save an ED visit for that family," Dr. Kraft said. "We can pay for an out-of-network nurse to give a high-cost medication to a high-risk teenager to prevent a premature delivery. Because we take full risk for the patient, we have the freedom to make decisions that make sense rather than follow strict Medicaid guidelines."
In the event that a requested treatment or test cannot be authorized, administrators search for other services that can support or assist the patient, said Dr. Melodie Blacklidge, HNCC associate medical director. Dr. Blacklidge is charged with evaluating physicians’ requests for tests and procedures that don’t easily fit within Medicaid guidelines.
"If we have to deny a physician’s request for a service, we try our very best to communicate with that physician before we deny it," Dr. Blacklidge said in an interview. "I think that physician-to-physician communication goes a long way in building acceptance of the network and [demonstrating] that we’re really in this together."
HCNN now has 1 year of data to develop a baseline for cost and utilization measures for emergency department visits and inpatient visits per 1,000 members, among other statistics. Network leaders plan to determine a baseline for Healthcare Effectiveness Data and Information Set, a tool developed by the National Committee for Quality Assurance to measure care and service performance.
When considering a model such as that used by HCNN, it pays to first determine current problems in caring for at-risk patients, then to evaluate how an ACO might help, Dr. Kraft said. Questions to ask include: How can an ACO help reduce some of the hassles in treating at-risk children? How can care coordinators better communicate with doctors? How will funding be determined and distributed?
Dr. Graham stresses that a Medicaid network should be an adjunct to a practice and a team that physicians can quickly activate for the most complex children.
"Providers want streamlined patient-centered service, accurate and timely attribution data and statistics, medical authorizations based on evidence, and payment that compensates physicians for quality and access," she said. "Our health network strives to deliver all of these measures."
On Twitter @legal_med
*This story was updated on September 9, 2014.
Health Network by Cincinnati Children’s is putting a new spin on an old idea – capitation – and using it to better serve high-risk pediatric patients in southern Ohio.
The recently launched community-based network (HNCC) of physicians, health providers, and social service providers focuses on specialized case management for low-income children. Nonphysician members at the accountable care organization include nurses, social workers, mental and behavioral health care specialists, and community health workers.
"We can make those staff available to anyone that our physicians or providers see as somebody who needs some sort of help, whether it’s medical or social," Dr. Colleen Kraft, HNCC medical director, said in an interview. "The real success of the network is in the connection and relationship with families to get them to resources that help their child and prevent high-cost care."
HNCC, which started in July 2013, serves Medicaid families in eight Ohio counties and has nearly 35,000 members, 150 of whom are enrolled in high-risk case management. The network contracts with two Ohio Medicaid insurers, Paramount and Molina Healthcare – also called managed care organizations (MCOs) – to provide case management for complex patients. Any practice that accepts Paramount or Molina has access to the network’s services, whether it is a Cincinnati Children’s hospital practice, a private practice, or a federally qualified health center.
The network receives a global, capitated fee for each child in the MCO plan to spend on medical management. While a capitated payment model is nothing new, the way in which the network uses the dollars is unique, Dr. Kraft said. Traditionally, MCOs provide capitated payments to physicians for face-to-face patient care. HNCC concentrates its funds on medical management. Paramount and Molina Healthcare contract separately with physicians for payments.
"The biggest difference with this model is we are not responsible for physician payment," Dr. Kraft said. "We’ve contracted for those medical management dollars, and we’re doing our own care management for these families and building of [care] teams. There’s a lot of interaction between our vulnerable families and our care managers, and we’re able to help them navigate the health care system."
The network’s relationship with primary care providers plays a central role in the system’s success. It’s no secret that doctors are often frustrated with Medicaid’s low payments and the red tape and hassles the system brings, Dr. Kraft said. For physicians, network advantages include more feedback about cases, broader coverage of treatments, and the potential for bonuses.
HCNN uses part of its funding to provide bonuses for physician practices that see a high number of Medicaid patients. The network provides $2 per member, per month in incentive payments for all health network patients in a practice, well over what Medicaid pays, Dr. Kraft said. In addition, physician administrators and case managers regularly contact and discuss cases with physicians, said Dr. Camille Graham, HCNN’s executive community physician liaison and a Cincinnati-based pediatrician in private practice. “From the outset, the network was determined to partner with primary care physicians in a meaningful way,” she said. “With most insurance companies, the primary care physician doesn’t receive any feedback about case management other than: The case was closed, there was no response, or we’re continuing (management). With the network, there’s more of a dialogue about what’s working and what’s not working with this family.”*
HCNN has the ability to pay for services that traditionally would not be covered by Medicaid, Dr. Kraft said. Administrators conduct utilization management reviews for referrals in which they evaluate the need of items such as durable medical equipment and high-cost testing. In a recent case, family members requested an additional gastrostomy tube for their child in case the current tube became unattached. Medicaid would not pay for a second tube, although it would have paid for an emergency department visit if the original tube were to detach, she said. In another case, Medicaid refused to pay for an out-of-network provider to administer an approved medication to a pregnant teenager.
"We can pay for an extra G-tube and save an ED visit for that family," Dr. Kraft said. "We can pay for an out-of-network nurse to give a high-cost medication to a high-risk teenager to prevent a premature delivery. Because we take full risk for the patient, we have the freedom to make decisions that make sense rather than follow strict Medicaid guidelines."
In the event that a requested treatment or test cannot be authorized, administrators search for other services that can support or assist the patient, said Dr. Melodie Blacklidge, HNCC associate medical director. Dr. Blacklidge is charged with evaluating physicians’ requests for tests and procedures that don’t easily fit within Medicaid guidelines.
"If we have to deny a physician’s request for a service, we try our very best to communicate with that physician before we deny it," Dr. Blacklidge said in an interview. "I think that physician-to-physician communication goes a long way in building acceptance of the network and [demonstrating] that we’re really in this together."
HCNN now has 1 year of data to develop a baseline for cost and utilization measures for emergency department visits and inpatient visits per 1,000 members, among other statistics. Network leaders plan to determine a baseline for Healthcare Effectiveness Data and Information Set, a tool developed by the National Committee for Quality Assurance to measure care and service performance.
When considering a model such as that used by HCNN, it pays to first determine current problems in caring for at-risk patients, then to evaluate how an ACO might help, Dr. Kraft said. Questions to ask include: How can an ACO help reduce some of the hassles in treating at-risk children? How can care coordinators better communicate with doctors? How will funding be determined and distributed?
Dr. Graham stresses that a Medicaid network should be an adjunct to a practice and a team that physicians can quickly activate for the most complex children.
"Providers want streamlined patient-centered service, accurate and timely attribution data and statistics, medical authorizations based on evidence, and payment that compensates physicians for quality and access," she said. "Our health network strives to deliver all of these measures."
On Twitter @legal_med
*This story was updated on September 9, 2014.
Health Network by Cincinnati Children’s is putting a new spin on an old idea – capitation – and using it to better serve high-risk pediatric patients in southern Ohio.
The recently launched community-based network (HNCC) of physicians, health providers, and social service providers focuses on specialized case management for low-income children. Nonphysician members at the accountable care organization include nurses, social workers, mental and behavioral health care specialists, and community health workers.
"We can make those staff available to anyone that our physicians or providers see as somebody who needs some sort of help, whether it’s medical or social," Dr. Colleen Kraft, HNCC medical director, said in an interview. "The real success of the network is in the connection and relationship with families to get them to resources that help their child and prevent high-cost care."
HNCC, which started in July 2013, serves Medicaid families in eight Ohio counties and has nearly 35,000 members, 150 of whom are enrolled in high-risk case management. The network contracts with two Ohio Medicaid insurers, Paramount and Molina Healthcare – also called managed care organizations (MCOs) – to provide case management for complex patients. Any practice that accepts Paramount or Molina has access to the network’s services, whether it is a Cincinnati Children’s hospital practice, a private practice, or a federally qualified health center.
The network receives a global, capitated fee for each child in the MCO plan to spend on medical management. While a capitated payment model is nothing new, the way in which the network uses the dollars is unique, Dr. Kraft said. Traditionally, MCOs provide capitated payments to physicians for face-to-face patient care. HNCC concentrates its funds on medical management. Paramount and Molina Healthcare contract separately with physicians for payments.
"The biggest difference with this model is we are not responsible for physician payment," Dr. Kraft said. "We’ve contracted for those medical management dollars, and we’re doing our own care management for these families and building of [care] teams. There’s a lot of interaction between our vulnerable families and our care managers, and we’re able to help them navigate the health care system."
The network’s relationship with primary care providers plays a central role in the system’s success. It’s no secret that doctors are often frustrated with Medicaid’s low payments and the red tape and hassles the system brings, Dr. Kraft said. For physicians, network advantages include more feedback about cases, broader coverage of treatments, and the potential for bonuses.
HCNN uses part of its funding to provide bonuses for physician practices that see a high number of Medicaid patients. The network provides $2 per member, per month in incentive payments for all health network patients in a practice, well over what Medicaid pays, Dr. Kraft said. In addition, physician administrators and case managers regularly contact and discuss cases with physicians, said Dr. Camille Graham, HCNN’s executive community physician liaison and a Cincinnati-based pediatrician in private practice. “From the outset, the network was determined to partner with primary care physicians in a meaningful way,” she said. “With most insurance companies, the primary care physician doesn’t receive any feedback about case management other than: The case was closed, there was no response, or we’re continuing (management). With the network, there’s more of a dialogue about what’s working and what’s not working with this family.”*
HCNN has the ability to pay for services that traditionally would not be covered by Medicaid, Dr. Kraft said. Administrators conduct utilization management reviews for referrals in which they evaluate the need of items such as durable medical equipment and high-cost testing. In a recent case, family members requested an additional gastrostomy tube for their child in case the current tube became unattached. Medicaid would not pay for a second tube, although it would have paid for an emergency department visit if the original tube were to detach, she said. In another case, Medicaid refused to pay for an out-of-network provider to administer an approved medication to a pregnant teenager.
"We can pay for an extra G-tube and save an ED visit for that family," Dr. Kraft said. "We can pay for an out-of-network nurse to give a high-cost medication to a high-risk teenager to prevent a premature delivery. Because we take full risk for the patient, we have the freedom to make decisions that make sense rather than follow strict Medicaid guidelines."
In the event that a requested treatment or test cannot be authorized, administrators search for other services that can support or assist the patient, said Dr. Melodie Blacklidge, HNCC associate medical director. Dr. Blacklidge is charged with evaluating physicians’ requests for tests and procedures that don’t easily fit within Medicaid guidelines.
"If we have to deny a physician’s request for a service, we try our very best to communicate with that physician before we deny it," Dr. Blacklidge said in an interview. "I think that physician-to-physician communication goes a long way in building acceptance of the network and [demonstrating] that we’re really in this together."
HCNN now has 1 year of data to develop a baseline for cost and utilization measures for emergency department visits and inpatient visits per 1,000 members, among other statistics. Network leaders plan to determine a baseline for Healthcare Effectiveness Data and Information Set, a tool developed by the National Committee for Quality Assurance to measure care and service performance.
When considering a model such as that used by HCNN, it pays to first determine current problems in caring for at-risk patients, then to evaluate how an ACO might help, Dr. Kraft said. Questions to ask include: How can an ACO help reduce some of the hassles in treating at-risk children? How can care coordinators better communicate with doctors? How will funding be determined and distributed?
Dr. Graham stresses that a Medicaid network should be an adjunct to a practice and a team that physicians can quickly activate for the most complex children.
"Providers want streamlined patient-centered service, accurate and timely attribution data and statistics, medical authorizations based on evidence, and payment that compensates physicians for quality and access," she said. "Our health network strives to deliver all of these measures."
On Twitter @legal_med
*This story was updated on September 9, 2014.