User login
VIDEO: Do clinical approaches aid statistical violence assessments?
CHICAGO – Does clinical judgment improve or worsen an actuarial assessment of violence?
Forensic psychiatrist Brian A. Falls sought to answer the question in an inpatient study presented at the American Academy of Psychiatry and the Law’s annual meeting. His research, conducted while Dr. Falls was a fellow at the University of California Davis Medical Center in Sacramento, analyzed whether adding clinical judgment to the use of the Classification of Violence Risk (COVR) tool led to better prediction of future violence. COVR is a software program that considers up to 40 risk factors to estimate a patient’s violence risk. Dr. Fall’s study found that clinical judgment improves overall actuarial assessment of violence but does not have the same relationship with all types of violence.
In a video interview at the meeting, Dr. Falls spoke about how clinical conclusions can affect the use of COVR and why different violence categories might have yielded contrasting results. The first-of-its-kind research might help evaluators better identify individuals prone to committing violence and those at less risk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
CHICAGO – Does clinical judgment improve or worsen an actuarial assessment of violence?
Forensic psychiatrist Brian A. Falls sought to answer the question in an inpatient study presented at the American Academy of Psychiatry and the Law’s annual meeting. His research, conducted while Dr. Falls was a fellow at the University of California Davis Medical Center in Sacramento, analyzed whether adding clinical judgment to the use of the Classification of Violence Risk (COVR) tool led to better prediction of future violence. COVR is a software program that considers up to 40 risk factors to estimate a patient’s violence risk. Dr. Fall’s study found that clinical judgment improves overall actuarial assessment of violence but does not have the same relationship with all types of violence.
In a video interview at the meeting, Dr. Falls spoke about how clinical conclusions can affect the use of COVR and why different violence categories might have yielded contrasting results. The first-of-its-kind research might help evaluators better identify individuals prone to committing violence and those at less risk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
CHICAGO – Does clinical judgment improve or worsen an actuarial assessment of violence?
Forensic psychiatrist Brian A. Falls sought to answer the question in an inpatient study presented at the American Academy of Psychiatry and the Law’s annual meeting. His research, conducted while Dr. Falls was a fellow at the University of California Davis Medical Center in Sacramento, analyzed whether adding clinical judgment to the use of the Classification of Violence Risk (COVR) tool led to better prediction of future violence. COVR is a software program that considers up to 40 risk factors to estimate a patient’s violence risk. Dr. Fall’s study found that clinical judgment improves overall actuarial assessment of violence but does not have the same relationship with all types of violence.
In a video interview at the meeting, Dr. Falls spoke about how clinical conclusions can affect the use of COVR and why different violence categories might have yielded contrasting results. The first-of-its-kind research might help evaluators better identify individuals prone to committing violence and those at less risk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AT THE AAPL ANNUAL MEETING
Government recovers more than $2 billion in health fraud in 2014
The Department of Justice recouped $2.3 billion in health care fraud and false claim settlements in fiscal 2014, down from $2.6 billion last year.
The retrieval brings the government’s total False Claims Act (FCA) recoveries to $14.5 billion from 2009 to 2014, according to a November announcement by the Justice Department.
The pharmaceutical, hospital, and home health service industries accounted for a substantial part of the 2014 health fraud recoveries with physician kickbacks playing a large part in many of the alleged schemes. Health care entities that paid significant health fraud settlements and judgments in 2014 included:
• Johnson & Johnson (J&J) and its subsidiaries, Janssen Pharmaceuticals and Scios, which paid a $1.1 billion settlement to resolve FCA claims relating to the promotion of three prescription drugs for unapproved uses. The drug promotions resulted in the submission of false claims against Medicare, Medicaid, and TRICARE by physicians. The Justice Department alleged also that J&J paid kickbacks to physicians and to Omnicare, a provider of pharmaceuticals to nursing homes.
• In a separate settlement, the department recovered $116 million from Omnicare to resolve allegations of a kickback arrangement with skilled nursing facilities.
• Community Health Systems, the nation’s largest operator of acute care hospitals, paid the government $98.2 million to settle allegations that it billed Medicare, Medicaid, and TRICARE for inpatient services that should have been provided in a less costly outpatient setting.
• Halifax Hospital Medical Center paid $85 million to resolve allegations of improper financial relationships with referring physicians.
• In a trio of cases involving cardiac procedures, Boston Scientific, which purchased Guidant, paid $30 million to settle claims that Guidant sold defective heart devices to physicians who implanted them into Medicare patients. Two Kentucky hospitals King’s Daughters Medical Center and Saint Joseph Health System, paid the government a combined $55 million for allegedly billing Medicare and Medicaid for unnecessary coronary procedures that were performed on patients.
The FCA is the government’s primary civil remedy to redress false claims for government funds and property under government contracts. Most FCA actions are filed under the act’s whistle-blower, or qui tam, provisions that allow individuals to file lawsuits alleging false claims on behalf of the government. If the government prevails in the action, the whistle-blower receives up to 30% of the recovery.
The $2.3 billion in health care fraud recoveries were part of an overall $5.7 billion in settlements and judgments from civil cases involving fraud and false claims against the government in fiscal year 2014. Of the $5.7 billion recovered, nearly $3 billion involved lawsuits filed under the FCA’s qui tam provisions. During the same period, the government paid out $435 million to the whistle-blowers who filed qui tam complaints.
On Twitter @legal_med
The Department of Justice recouped $2.3 billion in health care fraud and false claim settlements in fiscal 2014, down from $2.6 billion last year.
The retrieval brings the government’s total False Claims Act (FCA) recoveries to $14.5 billion from 2009 to 2014, according to a November announcement by the Justice Department.
The pharmaceutical, hospital, and home health service industries accounted for a substantial part of the 2014 health fraud recoveries with physician kickbacks playing a large part in many of the alleged schemes. Health care entities that paid significant health fraud settlements and judgments in 2014 included:
• Johnson & Johnson (J&J) and its subsidiaries, Janssen Pharmaceuticals and Scios, which paid a $1.1 billion settlement to resolve FCA claims relating to the promotion of three prescription drugs for unapproved uses. The drug promotions resulted in the submission of false claims against Medicare, Medicaid, and TRICARE by physicians. The Justice Department alleged also that J&J paid kickbacks to physicians and to Omnicare, a provider of pharmaceuticals to nursing homes.
• In a separate settlement, the department recovered $116 million from Omnicare to resolve allegations of a kickback arrangement with skilled nursing facilities.
• Community Health Systems, the nation’s largest operator of acute care hospitals, paid the government $98.2 million to settle allegations that it billed Medicare, Medicaid, and TRICARE for inpatient services that should have been provided in a less costly outpatient setting.
• Halifax Hospital Medical Center paid $85 million to resolve allegations of improper financial relationships with referring physicians.
• In a trio of cases involving cardiac procedures, Boston Scientific, which purchased Guidant, paid $30 million to settle claims that Guidant sold defective heart devices to physicians who implanted them into Medicare patients. Two Kentucky hospitals King’s Daughters Medical Center and Saint Joseph Health System, paid the government a combined $55 million for allegedly billing Medicare and Medicaid for unnecessary coronary procedures that were performed on patients.
The FCA is the government’s primary civil remedy to redress false claims for government funds and property under government contracts. Most FCA actions are filed under the act’s whistle-blower, or qui tam, provisions that allow individuals to file lawsuits alleging false claims on behalf of the government. If the government prevails in the action, the whistle-blower receives up to 30% of the recovery.
The $2.3 billion in health care fraud recoveries were part of an overall $5.7 billion in settlements and judgments from civil cases involving fraud and false claims against the government in fiscal year 2014. Of the $5.7 billion recovered, nearly $3 billion involved lawsuits filed under the FCA’s qui tam provisions. During the same period, the government paid out $435 million to the whistle-blowers who filed qui tam complaints.
On Twitter @legal_med
The Department of Justice recouped $2.3 billion in health care fraud and false claim settlements in fiscal 2014, down from $2.6 billion last year.
The retrieval brings the government’s total False Claims Act (FCA) recoveries to $14.5 billion from 2009 to 2014, according to a November announcement by the Justice Department.
The pharmaceutical, hospital, and home health service industries accounted for a substantial part of the 2014 health fraud recoveries with physician kickbacks playing a large part in many of the alleged schemes. Health care entities that paid significant health fraud settlements and judgments in 2014 included:
• Johnson & Johnson (J&J) and its subsidiaries, Janssen Pharmaceuticals and Scios, which paid a $1.1 billion settlement to resolve FCA claims relating to the promotion of three prescription drugs for unapproved uses. The drug promotions resulted in the submission of false claims against Medicare, Medicaid, and TRICARE by physicians. The Justice Department alleged also that J&J paid kickbacks to physicians and to Omnicare, a provider of pharmaceuticals to nursing homes.
• In a separate settlement, the department recovered $116 million from Omnicare to resolve allegations of a kickback arrangement with skilled nursing facilities.
• Community Health Systems, the nation’s largest operator of acute care hospitals, paid the government $98.2 million to settle allegations that it billed Medicare, Medicaid, and TRICARE for inpatient services that should have been provided in a less costly outpatient setting.
• Halifax Hospital Medical Center paid $85 million to resolve allegations of improper financial relationships with referring physicians.
• In a trio of cases involving cardiac procedures, Boston Scientific, which purchased Guidant, paid $30 million to settle claims that Guidant sold defective heart devices to physicians who implanted them into Medicare patients. Two Kentucky hospitals King’s Daughters Medical Center and Saint Joseph Health System, paid the government a combined $55 million for allegedly billing Medicare and Medicaid for unnecessary coronary procedures that were performed on patients.
The FCA is the government’s primary civil remedy to redress false claims for government funds and property under government contracts. Most FCA actions are filed under the act’s whistle-blower, or qui tam, provisions that allow individuals to file lawsuits alleging false claims on behalf of the government. If the government prevails in the action, the whistle-blower receives up to 30% of the recovery.
The $2.3 billion in health care fraud recoveries were part of an overall $5.7 billion in settlements and judgments from civil cases involving fraud and false claims against the government in fiscal year 2014. Of the $5.7 billion recovered, nearly $3 billion involved lawsuits filed under the FCA’s qui tam provisions. During the same period, the government paid out $435 million to the whistle-blowers who filed qui tam complaints.
On Twitter @legal_med
Insurance commissioners publish first draft of network adequacy model law
Model legislation that aims to ensure the adequacy, accessibility, and quality of health insurers’ provider networks does not address a number of concerns voiced by physicians.
The draft legislation, released by the National Association of Insurance Commissioners (NAIC), provides that a managed care plan shall maintain a network sufficient in numbers and types of providers to ensure that all services to covered persons will be accessible without unreasonable delay. Determining adequacy includes – but is not limited to – provider-covered person ratios by specialty; geographic accessibility; waiting times for appointments; hours of operation; new health delivery options, such as telemedicine; and the volume of technological and specialty services available.
The model law applies to all forms of health insurance, including qualified health plans, health maintenance organizations, and preferred provider organizations, J.P. Weiske, chair of NAIC’s network adequacy model review (B) subgroup said in a Nov. 19 webinar hosted by the Alliance for Health Reform.
“One of the biggest decisions we made is it would apply to all forms of health insurance that’s sold,” said Mr. Weiske, who serves as legislative liaison for Wisconsin Insurance Commissioner Ted Nickel.
Once finalized, the model law could be used as a basis for legislation to reform health insurance that could be introduced in any or all state legislatures.
The model legislation arrives amid ongoing physician criticism that many plans being sold on the Affordable Care Act’s insurance exchanges have narrow networks that limit access to primary care doctors, area hospitals, and specialists.
On Nov. 17, more than 115 health care organizations, including the American Medical Association, sent a letter to NAIC calling for network adequacy for patients, greater regulatory oversight in the hands of commissioners, and increased transparency for health insurers. The AMA also passed a new policy at its Nov. 11 interim meeting that supports strengthening the monitoring and enforcement of network adequacy at the federal and state levels.
In their letter, the groups requested that NAIC tackle several critical issues within its model act, recommending that provider networks include a full range of primary, specialty, and subspecialty providers to ensure that consumers have access to all covered services; that regulators actively review and monitor all networks using appropriate quantitative standards; that appeals processes are fair, timely, and transparent; and that the use of tiered provider networks be regulated.
NAIC’s model legislation addresses such issues as provider directories, telemedicine, and the transparency of health networks. It would require that a health insurer post online a current provider directory for each of its network plans and update each directory at least monthly. It also calls on insurers to prepare an access plan prior to offering a new managed care network plan and include:
• How the use of telemedicine or other technology may be used to meet access standards.
• The health insurer’s procedures for making and authorizing referrals within and outside its network, if applicable.
• The health insurer’s process for monitoring and ensuring the sufficiency of the network to meet the health care needs of populations that enroll in managed care network plans.
But the model law does not include standards related to some prevalent concerns by doctors, such as certain appeals, rules related to tiers, and time and distance standards.
For instance, the model does not include provisions about an appeals process for providers unhappy about being excluded from a network or how close geographically a network’s providers should be to patients they are serving. In regard to tiered networks, the model act includes only a sidebar noting that “states may want to pay particular attention to network sufficiency, marketing, and disclosure issues that may arise with respect to certain health carrier network designs, such as so-called tiered networks.” NAIC may revisit the issue of tiered networks at a later date.
“The problem that we had with tiered networks is that they’re relatively new,” Mr. Weiske said during the webinar. “There’s not a lot of similarity between them, but there are some significant regulatory concerns. We decided to essentially put regulators on notice that this is something they should look at.”
Mr. Weiske noted that it made sense to include broad flexibility in the model legislation to allow state regulators to dictate the details that best fit their patient populations and health care systems.
If enacted, the proposed law could end up being very different in different states, added Dr. John J. Reilly Jr., senior medical director of population health for the University of Pittsburgh Medical Center’s health services division and chair of the university’s department of medicine.
“The draft we’ve seen is very broad,” he said during the webinar. “It does not mean the way that states implement it is going to be broad. They can be very specific in their language. For insurers or clinical systems that cross state lines, there will be the potential for having different regulations across their networks because of different implementation of this model draft by different state regulatory agencies.”
Stakeholders have until Jan. 12, 2015, to provide comments on the first draft of the model law. The draft will then move through several NAIC committees before becoming a final model and ready for state legislators to review.
On Twitter @legal_med
Model legislation that aims to ensure the adequacy, accessibility, and quality of health insurers’ provider networks does not address a number of concerns voiced by physicians.
The draft legislation, released by the National Association of Insurance Commissioners (NAIC), provides that a managed care plan shall maintain a network sufficient in numbers and types of providers to ensure that all services to covered persons will be accessible without unreasonable delay. Determining adequacy includes – but is not limited to – provider-covered person ratios by specialty; geographic accessibility; waiting times for appointments; hours of operation; new health delivery options, such as telemedicine; and the volume of technological and specialty services available.
The model law applies to all forms of health insurance, including qualified health plans, health maintenance organizations, and preferred provider organizations, J.P. Weiske, chair of NAIC’s network adequacy model review (B) subgroup said in a Nov. 19 webinar hosted by the Alliance for Health Reform.
“One of the biggest decisions we made is it would apply to all forms of health insurance that’s sold,” said Mr. Weiske, who serves as legislative liaison for Wisconsin Insurance Commissioner Ted Nickel.
Once finalized, the model law could be used as a basis for legislation to reform health insurance that could be introduced in any or all state legislatures.
The model legislation arrives amid ongoing physician criticism that many plans being sold on the Affordable Care Act’s insurance exchanges have narrow networks that limit access to primary care doctors, area hospitals, and specialists.
On Nov. 17, more than 115 health care organizations, including the American Medical Association, sent a letter to NAIC calling for network adequacy for patients, greater regulatory oversight in the hands of commissioners, and increased transparency for health insurers. The AMA also passed a new policy at its Nov. 11 interim meeting that supports strengthening the monitoring and enforcement of network adequacy at the federal and state levels.
In their letter, the groups requested that NAIC tackle several critical issues within its model act, recommending that provider networks include a full range of primary, specialty, and subspecialty providers to ensure that consumers have access to all covered services; that regulators actively review and monitor all networks using appropriate quantitative standards; that appeals processes are fair, timely, and transparent; and that the use of tiered provider networks be regulated.
NAIC’s model legislation addresses such issues as provider directories, telemedicine, and the transparency of health networks. It would require that a health insurer post online a current provider directory for each of its network plans and update each directory at least monthly. It also calls on insurers to prepare an access plan prior to offering a new managed care network plan and include:
• How the use of telemedicine or other technology may be used to meet access standards.
• The health insurer’s procedures for making and authorizing referrals within and outside its network, if applicable.
• The health insurer’s process for monitoring and ensuring the sufficiency of the network to meet the health care needs of populations that enroll in managed care network plans.
But the model law does not include standards related to some prevalent concerns by doctors, such as certain appeals, rules related to tiers, and time and distance standards.
For instance, the model does not include provisions about an appeals process for providers unhappy about being excluded from a network or how close geographically a network’s providers should be to patients they are serving. In regard to tiered networks, the model act includes only a sidebar noting that “states may want to pay particular attention to network sufficiency, marketing, and disclosure issues that may arise with respect to certain health carrier network designs, such as so-called tiered networks.” NAIC may revisit the issue of tiered networks at a later date.
“The problem that we had with tiered networks is that they’re relatively new,” Mr. Weiske said during the webinar. “There’s not a lot of similarity between them, but there are some significant regulatory concerns. We decided to essentially put regulators on notice that this is something they should look at.”
Mr. Weiske noted that it made sense to include broad flexibility in the model legislation to allow state regulators to dictate the details that best fit their patient populations and health care systems.
If enacted, the proposed law could end up being very different in different states, added Dr. John J. Reilly Jr., senior medical director of population health for the University of Pittsburgh Medical Center’s health services division and chair of the university’s department of medicine.
“The draft we’ve seen is very broad,” he said during the webinar. “It does not mean the way that states implement it is going to be broad. They can be very specific in their language. For insurers or clinical systems that cross state lines, there will be the potential for having different regulations across their networks because of different implementation of this model draft by different state regulatory agencies.”
Stakeholders have until Jan. 12, 2015, to provide comments on the first draft of the model law. The draft will then move through several NAIC committees before becoming a final model and ready for state legislators to review.
On Twitter @legal_med
Model legislation that aims to ensure the adequacy, accessibility, and quality of health insurers’ provider networks does not address a number of concerns voiced by physicians.
The draft legislation, released by the National Association of Insurance Commissioners (NAIC), provides that a managed care plan shall maintain a network sufficient in numbers and types of providers to ensure that all services to covered persons will be accessible without unreasonable delay. Determining adequacy includes – but is not limited to – provider-covered person ratios by specialty; geographic accessibility; waiting times for appointments; hours of operation; new health delivery options, such as telemedicine; and the volume of technological and specialty services available.
The model law applies to all forms of health insurance, including qualified health plans, health maintenance organizations, and preferred provider organizations, J.P. Weiske, chair of NAIC’s network adequacy model review (B) subgroup said in a Nov. 19 webinar hosted by the Alliance for Health Reform.
“One of the biggest decisions we made is it would apply to all forms of health insurance that’s sold,” said Mr. Weiske, who serves as legislative liaison for Wisconsin Insurance Commissioner Ted Nickel.
Once finalized, the model law could be used as a basis for legislation to reform health insurance that could be introduced in any or all state legislatures.
The model legislation arrives amid ongoing physician criticism that many plans being sold on the Affordable Care Act’s insurance exchanges have narrow networks that limit access to primary care doctors, area hospitals, and specialists.
On Nov. 17, more than 115 health care organizations, including the American Medical Association, sent a letter to NAIC calling for network adequacy for patients, greater regulatory oversight in the hands of commissioners, and increased transparency for health insurers. The AMA also passed a new policy at its Nov. 11 interim meeting that supports strengthening the monitoring and enforcement of network adequacy at the federal and state levels.
In their letter, the groups requested that NAIC tackle several critical issues within its model act, recommending that provider networks include a full range of primary, specialty, and subspecialty providers to ensure that consumers have access to all covered services; that regulators actively review and monitor all networks using appropriate quantitative standards; that appeals processes are fair, timely, and transparent; and that the use of tiered provider networks be regulated.
NAIC’s model legislation addresses such issues as provider directories, telemedicine, and the transparency of health networks. It would require that a health insurer post online a current provider directory for each of its network plans and update each directory at least monthly. It also calls on insurers to prepare an access plan prior to offering a new managed care network plan and include:
• How the use of telemedicine or other technology may be used to meet access standards.
• The health insurer’s procedures for making and authorizing referrals within and outside its network, if applicable.
• The health insurer’s process for monitoring and ensuring the sufficiency of the network to meet the health care needs of populations that enroll in managed care network plans.
But the model law does not include standards related to some prevalent concerns by doctors, such as certain appeals, rules related to tiers, and time and distance standards.
For instance, the model does not include provisions about an appeals process for providers unhappy about being excluded from a network or how close geographically a network’s providers should be to patients they are serving. In regard to tiered networks, the model act includes only a sidebar noting that “states may want to pay particular attention to network sufficiency, marketing, and disclosure issues that may arise with respect to certain health carrier network designs, such as so-called tiered networks.” NAIC may revisit the issue of tiered networks at a later date.
“The problem that we had with tiered networks is that they’re relatively new,” Mr. Weiske said during the webinar. “There’s not a lot of similarity between them, but there are some significant regulatory concerns. We decided to essentially put regulators on notice that this is something they should look at.”
Mr. Weiske noted that it made sense to include broad flexibility in the model legislation to allow state regulators to dictate the details that best fit their patient populations and health care systems.
If enacted, the proposed law could end up being very different in different states, added Dr. John J. Reilly Jr., senior medical director of population health for the University of Pittsburgh Medical Center’s health services division and chair of the university’s department of medicine.
“The draft we’ve seen is very broad,” he said during the webinar. “It does not mean the way that states implement it is going to be broad. They can be very specific in their language. For insurers or clinical systems that cross state lines, there will be the potential for having different regulations across their networks because of different implementation of this model draft by different state regulatory agencies.”
Stakeholders have until Jan. 12, 2015, to provide comments on the first draft of the model law. The draft will then move through several NAIC committees before becoming a final model and ready for state legislators to review.
On Twitter @legal_med
Sexsomnia may gain more awareness after DSM-5 inclusion
The inclusion of a new sleep disorder in the DSM-5 might raise awareness of the underreported diagnosis and help physicians better identify the condition.
Sexsomnia can present in different forms but is generally described as engaging in sexual activity while asleep.
“Classification of sexsomnia in DSM-5 adds legitimacy to the diagnosis as it takes it out of the proposed diagnosis or research diagnosis realm and places it into a formally accepted classification manual,” said Dr. Brandon G. Moore, a psychiatry resident at Western Michigan University School of Medicine in Kalamazoo. “The classification of the diagnosis helps patients in that it opens up the topic for further discussion and education of providers so that they may more readily recognize the disorder and offer appropriate treatment.”
Sexsomnia can involve varying degrees of sexual activity while unconscious, including masturbation, fondling, groping, and intercourse. Patients often are unaware they have the condition, and signs of the disorder frequently are reported by a partner, roommate, or spouse, Dr. Moore said in an interview. The condition is not well known to many doctors, which can lead to misdiagnoses and underdiagnoses, added Dr. Kannan Ramar, an internist who practices in the division of pulmonary and critical care medicine, and the Center for Sleep Medicine at the Mayo Clinic, Rochester, Minn.
“Awareness of this condition is not there among the medical community,” Dr. Ramar said in an interview. “More educational awareness needs to happen, and having this diagnosis listed in the DSM-5 is one right step in that direction.”
Dr. Moore recently treated a 44-year-old patient with sexsomnia referred by his neurologist. The patient originally presented for presumed restless legs syndrome but had a history of sleep-related sexual behavior. The neurologist instructed the patient and his wife to keep a sleep diary, which revealed sexual behavior by the patient during sleep, including intercourse, that had been occurring for the last 20 years, according to a case study poster by Dr. Moore presented at the American Academy of Psychiatry and the Law meeting.
Polysomnography indicated no significant sleep-disordered breathing or limb movements but did reveal episodes during non-REM sleep consistent with confusional arousal. After a diagnosis of parasomnia associated with sexual behavior, the patient was referred for psychiatric evaluation because his behavior, exacerbated by stress, was becoming increasingly aggressive and adversely affecting his marriage. The patient has since improved with the addition of paroxetine, an increase of his clonazepam dosage, as well as with psychotherapy, Dr. Moore reported.
Collecting collateral information about sleep habits from partners or roommates can help doctors pinpoint the possibility of sexsomnia, Dr. Moore said.
“Any sleepwalking disorder or history should at least raise some suspicion, but a bed partner who reports (any) physical or sexual contact that is unwanted should be explored,” he said.
Family physicians, internists, and other specialists also play a primary role in identifying sexsomnia in patients and conferring with sleep specialists.
“Knowing when to refer and/or when to call to get more information or help is needed to help manage patients with sleep disorders,” Dr. Ramar said. “Family physicians play a key role, as they are usually the first physician that a patient might see with a sleep disorder. If the treatment plan that is established for the patient does not work, then a referral to a sleep specialist is needed.”
Sexsomnia might be included as a diagnostic specifier when criteria for non-REM sleep arousal disorder, sleepwalking type, are met and accompanied by evidence of sleep-related sexual behavior.
On Twitter @legal_med
*This article was updated November 24, 2014.
The inclusion of a new sleep disorder in the DSM-5 might raise awareness of the underreported diagnosis and help physicians better identify the condition.
Sexsomnia can present in different forms but is generally described as engaging in sexual activity while asleep.
“Classification of sexsomnia in DSM-5 adds legitimacy to the diagnosis as it takes it out of the proposed diagnosis or research diagnosis realm and places it into a formally accepted classification manual,” said Dr. Brandon G. Moore, a psychiatry resident at Western Michigan University School of Medicine in Kalamazoo. “The classification of the diagnosis helps patients in that it opens up the topic for further discussion and education of providers so that they may more readily recognize the disorder and offer appropriate treatment.”
Sexsomnia can involve varying degrees of sexual activity while unconscious, including masturbation, fondling, groping, and intercourse. Patients often are unaware they have the condition, and signs of the disorder frequently are reported by a partner, roommate, or spouse, Dr. Moore said in an interview. The condition is not well known to many doctors, which can lead to misdiagnoses and underdiagnoses, added Dr. Kannan Ramar, an internist who practices in the division of pulmonary and critical care medicine, and the Center for Sleep Medicine at the Mayo Clinic, Rochester, Minn.
“Awareness of this condition is not there among the medical community,” Dr. Ramar said in an interview. “More educational awareness needs to happen, and having this diagnosis listed in the DSM-5 is one right step in that direction.”
Dr. Moore recently treated a 44-year-old patient with sexsomnia referred by his neurologist. The patient originally presented for presumed restless legs syndrome but had a history of sleep-related sexual behavior. The neurologist instructed the patient and his wife to keep a sleep diary, which revealed sexual behavior by the patient during sleep, including intercourse, that had been occurring for the last 20 years, according to a case study poster by Dr. Moore presented at the American Academy of Psychiatry and the Law meeting.
Polysomnography indicated no significant sleep-disordered breathing or limb movements but did reveal episodes during non-REM sleep consistent with confusional arousal. After a diagnosis of parasomnia associated with sexual behavior, the patient was referred for psychiatric evaluation because his behavior, exacerbated by stress, was becoming increasingly aggressive and adversely affecting his marriage. The patient has since improved with the addition of paroxetine, an increase of his clonazepam dosage, as well as with psychotherapy, Dr. Moore reported.
Collecting collateral information about sleep habits from partners or roommates can help doctors pinpoint the possibility of sexsomnia, Dr. Moore said.
“Any sleepwalking disorder or history should at least raise some suspicion, but a bed partner who reports (any) physical or sexual contact that is unwanted should be explored,” he said.
Family physicians, internists, and other specialists also play a primary role in identifying sexsomnia in patients and conferring with sleep specialists.
“Knowing when to refer and/or when to call to get more information or help is needed to help manage patients with sleep disorders,” Dr. Ramar said. “Family physicians play a key role, as they are usually the first physician that a patient might see with a sleep disorder. If the treatment plan that is established for the patient does not work, then a referral to a sleep specialist is needed.”
Sexsomnia might be included as a diagnostic specifier when criteria for non-REM sleep arousal disorder, sleepwalking type, are met and accompanied by evidence of sleep-related sexual behavior.
On Twitter @legal_med
*This article was updated November 24, 2014.
The inclusion of a new sleep disorder in the DSM-5 might raise awareness of the underreported diagnosis and help physicians better identify the condition.
Sexsomnia can present in different forms but is generally described as engaging in sexual activity while asleep.
“Classification of sexsomnia in DSM-5 adds legitimacy to the diagnosis as it takes it out of the proposed diagnosis or research diagnosis realm and places it into a formally accepted classification manual,” said Dr. Brandon G. Moore, a psychiatry resident at Western Michigan University School of Medicine in Kalamazoo. “The classification of the diagnosis helps patients in that it opens up the topic for further discussion and education of providers so that they may more readily recognize the disorder and offer appropriate treatment.”
Sexsomnia can involve varying degrees of sexual activity while unconscious, including masturbation, fondling, groping, and intercourse. Patients often are unaware they have the condition, and signs of the disorder frequently are reported by a partner, roommate, or spouse, Dr. Moore said in an interview. The condition is not well known to many doctors, which can lead to misdiagnoses and underdiagnoses, added Dr. Kannan Ramar, an internist who practices in the division of pulmonary and critical care medicine, and the Center for Sleep Medicine at the Mayo Clinic, Rochester, Minn.
“Awareness of this condition is not there among the medical community,” Dr. Ramar said in an interview. “More educational awareness needs to happen, and having this diagnosis listed in the DSM-5 is one right step in that direction.”
Dr. Moore recently treated a 44-year-old patient with sexsomnia referred by his neurologist. The patient originally presented for presumed restless legs syndrome but had a history of sleep-related sexual behavior. The neurologist instructed the patient and his wife to keep a sleep diary, which revealed sexual behavior by the patient during sleep, including intercourse, that had been occurring for the last 20 years, according to a case study poster by Dr. Moore presented at the American Academy of Psychiatry and the Law meeting.
Polysomnography indicated no significant sleep-disordered breathing or limb movements but did reveal episodes during non-REM sleep consistent with confusional arousal. After a diagnosis of parasomnia associated with sexual behavior, the patient was referred for psychiatric evaluation because his behavior, exacerbated by stress, was becoming increasingly aggressive and adversely affecting his marriage. The patient has since improved with the addition of paroxetine, an increase of his clonazepam dosage, as well as with psychotherapy, Dr. Moore reported.
Collecting collateral information about sleep habits from partners or roommates can help doctors pinpoint the possibility of sexsomnia, Dr. Moore said.
“Any sleepwalking disorder or history should at least raise some suspicion, but a bed partner who reports (any) physical or sexual contact that is unwanted should be explored,” he said.
Family physicians, internists, and other specialists also play a primary role in identifying sexsomnia in patients and conferring with sleep specialists.
“Knowing when to refer and/or when to call to get more information or help is needed to help manage patients with sleep disorders,” Dr. Ramar said. “Family physicians play a key role, as they are usually the first physician that a patient might see with a sleep disorder. If the treatment plan that is established for the patient does not work, then a referral to a sleep specialist is needed.”
Sexsomnia might be included as a diagnostic specifier when criteria for non-REM sleep arousal disorder, sleepwalking type, are met and accompanied by evidence of sleep-related sexual behavior.
On Twitter @legal_med
*This article was updated November 24, 2014.
Age, Living Arrangements Key Predictors of Pediatric Aggression
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Continue for additional results >>
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Continue for additional results >>
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Continue for additional results >>
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
AT THE AAPL ANNUAL MEETING
Age, living arrangements key predictors of pediatric aggression
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
On Twitter @legal_med
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
On Twitter @legal_med
CHICAGO – Younger children and those in foster care have a higher likelihood of aggressive behavior, reported Kacey Appel at the annual meeting of the American Academy of Psychiatry and the Law.
Ms. Appel,who is affiliated with Cincinnati Children’s Hospital Medical Center (CCHMC), and her coinvestigators evaluated 4,148 children aged 4-18 years who were admitted through the medical center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions, made between May 1, 2010 and April 31, 2014, lasted 30 days or less. The children were administered the Brief Rating of Aggression by Children and Adolescents (BRACHA) in the emergency department and later were scored twice a day using the Overt Aggression Scale (OAS), which records instances of aggression.
Investigators assessed the OAS scores, focusing on four demographic elements: age, gender, living arrangement, and history of previous hospitalizations. An OAS score of above 0 is generally considered aggressive, but Ms. Appel and her associates compared severity levels of aggression and their interplay with the four demographics.
Findings showed “no matter how you define aggression, the demographic variables remain significant,” said Ms. Appel, an epidemiology PhD candidate at the University of Cincinnati.
Results showed also that children living in foster care had a 10%-20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Only 5% of patients in the study sample were considered to live in a foster arrangement, Ms. Appel noted in an interview.
Additionally, the probability of aggression in children spiked when they were younger and decreased as they grew older, findings showed. For example, a nonfoster, female child with no previous hospitalizations had about a 60% probability of being aggressive at age 4. That probability of aggression for the same child at age 16 was about 15%. Investigators did not look at variables individually, but instead studied the four demographics together. Boys had a higher probability of being aggressive than girls.
The foster care finding is consistent with other data showing that children within such living arrangements often have a history of abuse and/or neglect, said Dr. Drew H. Barzman, director of the child and adolescent forensic psychiatry service at CCHMC and a coauthor of the study.
“Foster care kids may develop reactive attachment disorder or posttraumatic stress disorder, and these diagnoses can be associated with aggression on the inpatient unit, Dr. Barzman said in an interview.
The findings about age likely relate to younger children’s cognitive development, hormones, and mental processing, Ms. Appel added. “When kids are young, they often act out because they don’t know how to communicate what they’re frustrated about, and they can’t process what they’re frustrated about,” she said in an interview. “As they grow older, cognitively, they can more aptly process why they’re upset.”
The original intent of the research was to identify which BRACHA factors are most significant in predicting aggression. They will next study the significance of BRACHA factors based on frequency of aggression and time to aggressive incident. A primary goal of the research is to develop a web application tool for clinicians aimed at predicting more accurately which children within an inpatient population will be aggressive. The application will allow health providers to enter demographic data and BRACHA responses to determine predicted probability of aggression.
“If we can accurately predict the probability of a child being aggressive in the unit, we hope to improve safety on these inpatient units,” Ms. Appel said.
No conflicts of interest were reported.
On Twitter @legal_med
AT THE AAPL ANNUAL MEETING
Key clinical point: Younger children and foster care children have a higher likelihood of aggressive behavior.
Major finding: Children living in foster care have a 10% to 20% higher probability of being aggressive than another child with the same demographics but a different living arrangement. Also, the probability of aggression in children spikes while they are young and decreases as they grow older.
Data source: A study of 4,148 children aged 4-18 who were admitted through Cincinnati Children’s Hospital Medical Center’s emergency department to the College Hill Campus, a pediatric residential treatment facility. The admissions were made between May 1, 2010 to April 31, 2014 and lasted 30 days or less.
Disclosures: No conflicts of interest reported.
Attorney: Be prepared for next round of HIPAA audits
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
Court: Patients can sue over HIPAA breaches
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
Patients can sue doctors for negligence after alleged patient privacy breaches, the Connecticut Supreme Court has ruled in a decision that could have nationwide implications.
The state’s highest court concluded that HIPAA does not preempt claims for emotional distress or negligence under state law. The ruling, published Nov. 11, sets precedence in Connecticut and is likely to encourage plaintiffs to raise similar claims in other states, according to Michael J. Kline, a New Jersey attorney who specializes in corporate and securities law.
“It’s a momentous case, and I think it’s serious for physician practices,” said Mr. Kline. “It can set the stage for plaintiffs’ attorneys within given states to [pursue] class actions for emotional distress or invasion of privacy on the grounds there was negligence” in connection to HIPAA violations.
The decision stems from a lawsuit filed by Emily Byrne v. Avery Center for Obstetrics and Gynecology P.C. in Westport, Conn. Ms. Byrne claimed that in 2004, she instructed the health center not to release her medical records to an ex-boyfriend. In 2005, the medical center was served with a subpoena by the former boyfriend requesting the plaintiff’s medical records for a paternity proceeding. The defendant did not alert Ms. Byrne about the subpoena and mailed a copy of her medical file to the probate court, according to court records.
Ms. Byrne later sued the health care center, claiming she suffered harassment and extortion threats from her ex-boyfriend because the medical records were exposed. The complaint alleged the health center engaged in negligent infliction of emotional distress and acted negligently by failing to use proper and reasonable care in protecting her medical file, including disclosing it without authorization in violation of HIPAA.
A trial court agreed with the medical practice’s contention that HIPAA precludes individual liability claims pertaining to confidentiality of medical information. The court cited well-established case law that HIPAA does not create a private right of action and requires alleged privacy violations to be raised through administrative channels. But the Connecticut Supreme Court overturned the decision, ruling that HIPAA does not preempt such negligence lawsuits.
“If Connecticut’s common law recognizes claims arising from a health care provider’s alleged breach of its duty of confidentiality in the course of complying with a subpoena, HIPAA and its implementing regulations do not preempt such claims,” judges said in their opinion. “We further conclude that, to the extent it has become the common practice for Connecticut health care providers to follow the procedures required under HIPAA in rendering services to their patients, HIPAA and its implementing regulations may be utilized to inform the standard of care applicable to such claims arising from allegations of negligence in the disclosure of patients’ medical records pursuant to a subpoena.”
The court went on to say that “the availability of such private rights of action in state courts ... do not preclude, conflict with, or complicate health care providers’ compliance with HIPAA.”
Similar decisions have been made by other courts, but the Connecticut ruling is the first state Supreme Court to issue such a ruling, Mr. Kline said.
For example, in Harmon v. Maury County, the U.S. District Court for the Middle District of Tennessee found that negligence claims founded on violation of HIPAA were not precluded because federal provisions do not completely preempt state law and expressly preserve state laws that aren’t at odds with its terms. The 2005 Tennessee case resulted from a privacy violation claim by a patient against a pharmacy manager. In another pharmacy-patient complaint, Fanean v. Rite Aid Corp. of Delaware Inc., the Superior Court of Delaware concluded that negligence claims could not be premised on a HIPAA violation, but that a common law negligence claim could be predicated upon Occupational Safety and Health Administration requirements. The 2009 opinion noted that HIPAA may act as a “guidepost” to determine the standard of care in common-law negligence claims.
The similar assertions by Connecticut judges that HIPAA does not preempt state rights and can also be used as a standard for what constitutes negligence or improper care of records is concerning for health providers, Mr. Kline said in an interview. Doctors now have to worry that inadvertent HIPAA violations may yield not only a complaint with the Office for Civil Rights, but a potential malpractice suit, as well.
“I would not be surprised if a case like this or even this case is appealed to the Supreme Court of the United States,” Mr. Kline said. “It is still a question of federal law, and what does the federal preemption mean?”
On Twitter @legal_med
PODCAST: Program restores competency of defendants
CHICAGO– A competency restoration program in the District of Columbia is helping defendants with mental illness become fit to stand trial, while saving the district money. The program could serve as a model for other jurisdictions that want to improve the competency of unfit defendants, Dr. Nicole R. Johnson, director of outpatient forensic service at the district’s Department of Behavioral Health said in an interview.
The District of Columbia’s Outpatient Competency Restoration Program (OCRP) started in 2009 and receives court-ordered referrals for individuals to participate in the program. The program works to restore defendants’ competency through question and answer sessions, games, and educational lessons, among other methods, Dr. Johnson reported at the American Academy of Psychiatry and the Law meeting. Some participants have mental illness and about a third have cognitive or neurologic limitations, she said. The majority of those referred receive mental health services from separate district agencies. If such needs are being not being met, OCRP administrators refer them to a clinic for treatment.
Of 170 individuals enrolled in the OCRP from 2009 to 2013, 54 were deemed competent to stand trial after completion, said Dr. Johnson, who oversees the program.
In an interview at the meeting, Dr. Johnson discussed how much money the program has saved the district and whether other jurisdictions can feasibly start similar programs.
On Twitter @legal_med
CHICAGO– A competency restoration program in the District of Columbia is helping defendants with mental illness become fit to stand trial, while saving the district money. The program could serve as a model for other jurisdictions that want to improve the competency of unfit defendants, Dr. Nicole R. Johnson, director of outpatient forensic service at the district’s Department of Behavioral Health said in an interview.
The District of Columbia’s Outpatient Competency Restoration Program (OCRP) started in 2009 and receives court-ordered referrals for individuals to participate in the program. The program works to restore defendants’ competency through question and answer sessions, games, and educational lessons, among other methods, Dr. Johnson reported at the American Academy of Psychiatry and the Law meeting. Some participants have mental illness and about a third have cognitive or neurologic limitations, she said. The majority of those referred receive mental health services from separate district agencies. If such needs are being not being met, OCRP administrators refer them to a clinic for treatment.
Of 170 individuals enrolled in the OCRP from 2009 to 2013, 54 were deemed competent to stand trial after completion, said Dr. Johnson, who oversees the program.
In an interview at the meeting, Dr. Johnson discussed how much money the program has saved the district and whether other jurisdictions can feasibly start similar programs.
On Twitter @legal_med
CHICAGO– A competency restoration program in the District of Columbia is helping defendants with mental illness become fit to stand trial, while saving the district money. The program could serve as a model for other jurisdictions that want to improve the competency of unfit defendants, Dr. Nicole R. Johnson, director of outpatient forensic service at the district’s Department of Behavioral Health said in an interview.
The District of Columbia’s Outpatient Competency Restoration Program (OCRP) started in 2009 and receives court-ordered referrals for individuals to participate in the program. The program works to restore defendants’ competency through question and answer sessions, games, and educational lessons, among other methods, Dr. Johnson reported at the American Academy of Psychiatry and the Law meeting. Some participants have mental illness and about a third have cognitive or neurologic limitations, she said. The majority of those referred receive mental health services from separate district agencies. If such needs are being not being met, OCRP administrators refer them to a clinic for treatment.
Of 170 individuals enrolled in the OCRP from 2009 to 2013, 54 were deemed competent to stand trial after completion, said Dr. Johnson, who oversees the program.
In an interview at the meeting, Dr. Johnson discussed how much money the program has saved the district and whether other jurisdictions can feasibly start similar programs.
On Twitter @legal_med
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PSYCHIATRY AND THE LAW
Inpatient handoff program reduced errors
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
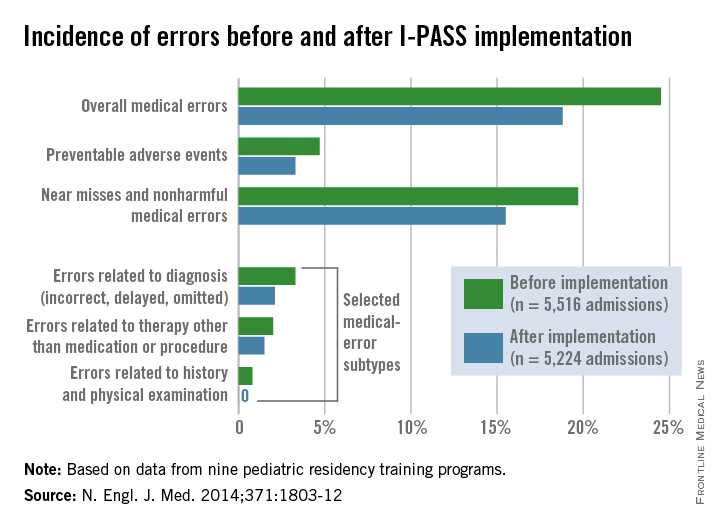
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
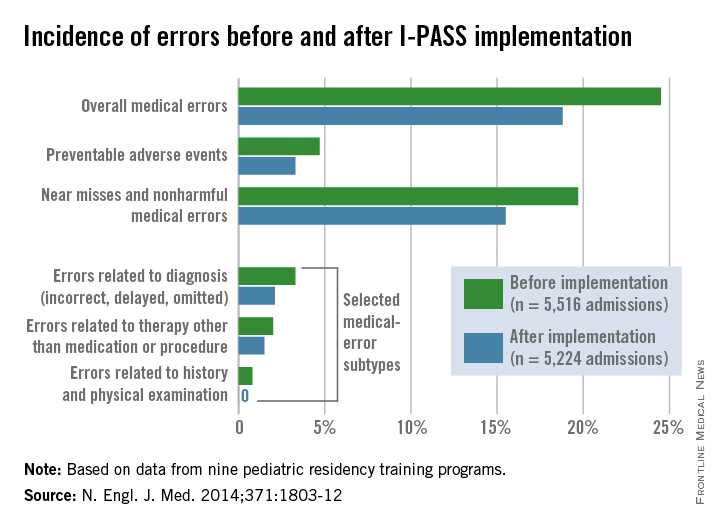
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
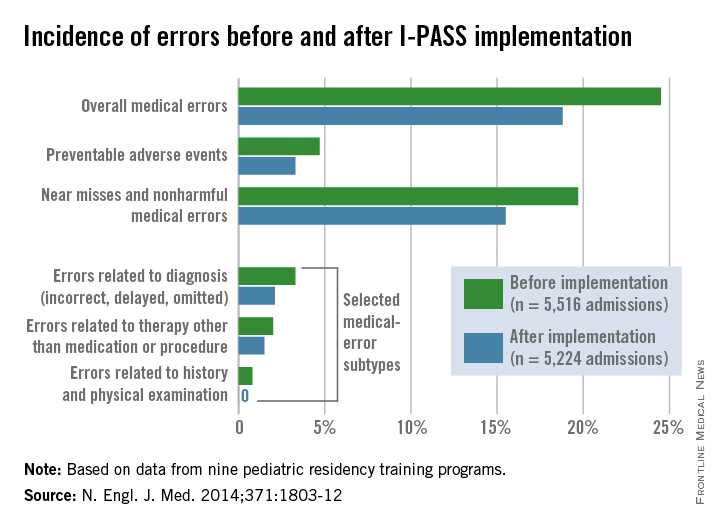
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Key clinical point: Medical errors and adverse events can be reduced through handoff programs that integrate oral and written tools.
Major finding: The rate of medical errors decreased by 23% and adverse events fell by 30% after implementation of the I-PASS Handoff Bundle.
Data source: A prospective study in nine hospitals that measured rates of medical errors, preventable adverse events, miscommunications, and workflow.
Disclosures: The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.