User login
50 years of pediatric residency: What has changed?
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
When Eileen Ouellette, MD, graduated from Boston’s Harvard Medical School in 1962, she was one of seven women in her class of 141 students. She went on to become one of only three women in pediatric residency at Massachusetts General Hospital later that year.
Free room and board was included in the program, Dr. Ouellette recalled, but her cramped room was poorly insulated and so small that she had to kneel on the bed to open her chest of drawers. The young doctor also soon learned that the women residents made less money than their male counterparts.
Dr. Ouellette, 79, now can laugh at the memory of her tiny room and tinier paycheck. The pediatric residents of today are entering a vastly different environment, she said. For starters, the average pay for medical residents in 2017 is $54,107. Women pediatric residents today far outnumber male residents. And most residents enjoy standard-sized rooms or apartments when completing their residencies.
Technology, for instance, greatly aids pediatric residents in their education today, said Renee Jenkins, MD, a professor at Howard University in Washington and a past AAP president.
Fewer hours, more hand-offs
During Dr. Ouellette’s residency from 1962 to 1965, sleep became a luxury. Of 168 hours in a week, residents were sometimes off for only 26 of them, she said.
“That was absolutely brutal,” she said. “You could not think of anything other than sleep. That became the primary focus of your whole life.”
“It didn’t seem crazy at the time,” said Dr. Stanton, founding dean of Seton Hall University Hackensack Meridian School of Medicine, South Orange, N.J. ”You developed the kind of bond with these families that it wouldn’t occur to you to go home.”
In the 1960s, there were no explicit limits on duty hours, according to Susan White, director of external communications for the Accreditation Council of Graduate Medical Education (ACGME). A “Guide for Residency Programs in Pediatrics,” published in 1968, recommended that “time off should be taken only when the service needs of the patients are assured and that “night and weekend duty provides a valuable educational experience. ... Duty of this type every second or third night and weekend is desirable.”
The guide predates the existence of the ACGME – established in 1981 – but it originated from a committee approved by the American Academy of Pediatrics, the American Board of Pediatrics, and the Council on Medical Education of the American Medical Association, according to Ms. White. While some residency programs changed their work hours over the years, the first mandated requirements for duty hours came in 1990 when ACGME set an 80-hour work week for four specialties: internal medicine, dermatology, ophthalmology, and preventive medicine. The council also limited on-call to every third night that year. In 2003, ACGME put in place duty hour requirements for all specialties.
“The pediatric requirements currently in effect provide safeguards for the resident, guidelines for educational programs, specific competencies and medical knowledge, as well as communication skills, professionalism requirements, and standardized assessment,” Ms. White said.
Current limitations for duty hours are beneficial in terms of resident safety, but the restrictions can be a double-edged sword, Dr. Jenkins said.
A changing gender demographic
By the time Dr. Stanton graduated from Yale in 1976, about 15% of her class were women, a marked shift from just a few years earlier, she said.
“In my residency program, women made up a quarter of our group,” she recalled. “That was a big change.”
The number of women going into pediatric residency has steadily increased in the last 5 decades, now far surpassing the number of men. Of 8,933 pediatric residents from 2015 to 2016, 67% were female and 25% were male, (with 8% not reporting), according to ACGME data.
“
Pediatrics is a natural selection for women, especially for those who plan to raise families, said Antoinette Eaton, MD, a retired pediatrician who completed her residency in the late 1950s at what is now Nationwide Children’s Hospital in Columbus, Ohio. Pediatrics is a prime specialty for career and family balance, she said.
“I worked part time a lot during my career,” said Dr. Eaton, a past AAP president. “Always being responsible as a mother and to the house were very high priorities.”
Dr. Stanton agrees that pediatric practices are much more tolerant of part time work, allowing women to better juggle children and career. However, she notes that the decline of male pediatricians also can be negative for the field overall.
New focus, growing debt
The curriculum focus for pediatric residency, meanwhile, has changed significantly over the years, pediatricians say. Dr. Eaton recalls her residency being almost entirely focused on inpatient care. In fact, insurance companies often refused to pay for outpatient care in sharp contrast to today, she said.
“You had to admit the patient if you wanted insurance to pay for it,” she said. “For example, if you had a patient with cerebral palsy or special needs, I had to admit that patient for 3, 4, 5 days. It was really different than what you have today.”
As time has passed, pediatric requirements have changed to emphasize the need for balance between inpatient and outpatient care, with a focus on continuity of care in either setting, Ms. White said. Newer additions to the requirements include the competencies of professionalism, communication, and life-long learning.
“Over the years these setting have expanded to include inpatients in hospitals, clinics, emergency centers, intensive care units, and in the community, [including] schools and other settings,” she said. “The requirements have always emphasized the importance of having high-quality, board-certified faculty to provide bedside teaching and deliver lectures at conferences.”
Another marked change for pediatric residents is the accumulation of debt. After her medical education, Dr. Jenkins owed about $1,500, she recalls.
“Today, that’s a drop in the bucket,” she said. “For the most part, you stayed out of [debt] trouble. It was nothing compared to that kids have to pay now.”
In 2014, the average medical school student graduated with a median debt of $180,000, according to data from the Association of American Medical Colleges. The wide debt differences are attributed to more expensive medical education today, Dr. Jenkins said.
While debt has risen, clinical responsibilities for residents have dropped as physician extenders and advanced equipment have become commonplace.
When Dr. Ouellette was a resident in the 1960s, there were few technicians to assist and no CT scans or MRIs for imaging. Residents drew blood from and gave blood to patients themselves. They took x-rays and developed them, she said.
“We had to use our brains and figure out what was going on,” she said. “People don’t think so much now. They send x-rays or scans to someone else, rather than figuring out the answer. Medicine may not be as much fun now as it was back then.”
Dr. Eaton added that residents have more technical demands today, more regulations to follow, and more paperwork to complete than the residents of the past. However, she believes pediatrics remains a worthwhile medical path. Three of her four children became doctors, one of whom went into pediatrics.
“I’m very disturbed when people try to convince children not to go into medicine,” she said. “I think it’s still a wonderful and rewarding career.”
[email protected]
On Twitter @legal_med
*Clarification made on 4/21/17
Senate committee moves Gorsuch nomination forward
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
Judge Neil Gorsuch has moved one step closer to becoming the next U.S. Supreme Court Justice.
The U.S. Senate Committee on the Judiciary approved Judge Gorsuch’s nomination by a 11-9 vote on April 3. The vote was a strict party line vote with 11 Republicans voting in favor of Judge Gorsuch and 9 Democrats voting against him.
“He’s a mainstream judge who’s earned the universal respect of his colleagues on the bench and in the bar,” Sen. Grassley said. “He applies the law as we in Congress write it – as the judicial oath says, ‘Without respect to persons.’ And he refuses to compromise his independence. This nominee ... is a judge’s judge. He’s a picture of the kind of justice we should have on the Supreme Court.”
Conversely, Sen. Dianne Feinstein (D-Calif.) expressed opposition to Judge Gorsuch, criticizing his past rulings and calling his answers during his nomination hearing vague and ambiguous.
“As I’ve said, our job is to assess whether the nominee will protect the legal and constitutional rights of all Americans and whether the nominee will recognize the humanity and justice required when evaluating the cases before him,” Sen. Feinstein said before the vote. “Unfortunately, based on the judge’s record at the Department of Justice, his tenure on the bench, his appearance before the Senate, and his written questions for the record, I cannot support his nomination.”
The full Senate is expected to vote on Judge Gorsuch’s nomination on April 7.
[email protected]
On Twitter @legal_med
What do doctors want from health reform?
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
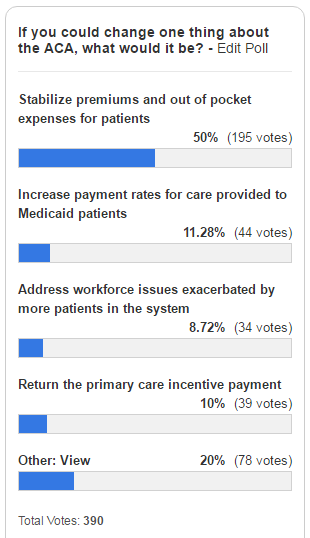
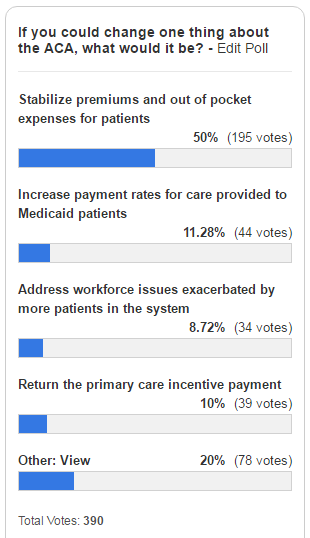
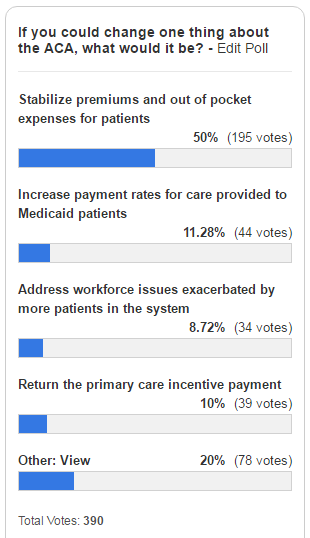
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
With the demise of Republican repeal and replace legislation, analysts say the landscape is ripe for repairs to the Affordable Care Act or for additional legislation that both political parties could support. So what do physicians want from health reform?
The first step should be stabilizing the health insurance marketplaces by strengthening and perhaps extending risk mitigation measures such as the risk adjustment, risk corridors, and reinsurance provisions of the law, said Patricia Salber, MD, an internist and health care consultant who blogs at TheDoctorWeighsIn.com. Those three ACA provisions were intended to promote insurer competition on the basis of quality and value and promote insurance market stability.
Keeping premiums at manageable levels for patients should also be addressed, said William J. Burke, DO, dean of Ohio University Heritage College of Osteopathic Medicine.
That was echoed in a poll taken by this news organization. Of 390 respondents, fully half (50%) said they would repair the ACA by stabilizing premiums and out-of-pocket costs for patients as of April 2. About 11% stated they would increase payment rates for care provided to Medicaid patients, and 10% said they would return the primary care incentive payment. About 9% of those surveyed would address workforce issues exacerbated by more patients in the system.
Improving reimbursement for Medicaid services is a necessary health reform change, agreed Diane J. Horvath-Cosper MD, an obstetrician-gynecologist and reproductive health advocacy fellow for Physicians for Reproductive Health, a reproductive rights advocacy organization.
“Reimbursement rates are so low that sometimes [physicians] have to limit the number of Medicaid patients to be able to pay staff,” Dr. Horvath said in an interview. “That’s a terrible position to put physicians in because we want to be able to see as many people who want to see us.”
Speaking of Medicaid, Dr. Salber adds that governors should be encouraged to continue expanding Medicaid to eliminate the coverage gap for the “near poor” that exists in states that did not participate in the expansion.
“Now that the [American Health Care Act] has failed, I think we will see some expansion take place organically even in states that were deeply opposed before,” she said.
“The volume of prior authorizations that all physicians face, but especially primary care physicians, is huge,” Dr. Munger said in an interview. “In many cases, we’re having to hire extra staff just to handle all of the prior authorizations. Every patient may not just have one prior authorization, but they may require two or three or four prior authorizations each month or quarterly. It really detracts from meaningful time you can spend with the patient.”
For starters, doctors should provide care to patients based on mutually agreed terms and without the interference of insurers, Dr. Orient said in an interview. In such a private medicine system, patients would pay doctors for services, and patients would then file claims with their insurer for reimbursement. Similarly, physicians should not be at the mercy of Medicare for payment, Dr. Orient said.
“Doctors can sign away their rights if they want in a Medicare participation agreement,” she said. “Doctors who do not sign the agreement to take assignment in all cases doctors should be freed of price controls and coding demands. Their patients should be allowed to file their own simple claims to Medicare with an itemized bill as they did before the 1990s law that requires physicians to submit the claims. Non-participating doctors should be exempted from MACRA [the Medicare Access and CHIP Reauthorization Act], and without the price controls, there is no need for [Recovery Audit Contractors] and other auditors.”
While contraceptive care was strengthened by the ACA, Dr. Horvath said further efforts should be made to improve coverage and level the playing field for reproductive medicine. In addition, she said that abortion should be treated a valid medical procedure, rather than parsed out, and both public and private insurers should be required to pay for the procedure, she said.
“I would love to see strengthened provisions for contraception coverage,” Dr. Horvath said. “[We need to] make sure that doesn’t get bargained away. The other thing is to expand coverage and make sure every method is covered, not just one method in each category.”
However, Robert Doherty, ACP senior vice president of governmental affairs and public policy, said the college is concerned that the current administration may fail to maintain the ACA now that its proposed repeal law has fallen through.
Without aggressively pushing ACA enrollment for younger patients and continued support for the individual mandate, more insurers may pull out of the marketplaces, and the ACA could implode, Mr. Doherty said.
“There are a number of ways that Republicans could either make things better or worse with action or inaction,” Mr. Doherty said during the press conference. “The insurance [companies] have gone to this administration with a wish list of things that will help keep them in the market. What remains to be seen is whether this administration is going to be receptive. If they don’t aggressively enforce the requirement that people buy coverage, more younger people will opt out and stay out until they get sick. That would make the problem of adverse selection even worse and could create the death cycle for insurance.”
Dr. Price consistently answered that Americans should be able to select the kinds of coverage they want. What “we believe is that individuals ought to be able to have access to the kind of coverage that they select for themselves and for their families and not what the government forces them to buy,” Dr. Price testified, echoing the message from his confirmation hearings.
He was also pressed on issues such as the individual mandate, and while noting that it is his duty to uphold the law of the land, he also remained noncommittal in answering questions about whether he would direct the agency to enforce the individual mandate. The first executive order from President Trump beginning his administration gave the agency discretion to not enforce mandates if they caused harm.
[email protected]
On Twitter @legal_med
Gregory Twachtman contributed to this report.
Gorsuch keeps cards close during nomination hearing
Throughout his marathon confirmation hearing, U.S. Supreme Court nominee Neil Gorsuch remained tight-lipped about how he might rule on major health care issues if confirmed to the country’s highest court, pledging to look at the facts of each case and rule according to the law.
The Senate Committee on the Judiciary wrapped up its nearly week-long questioning of Judge Gorsuch on March 23. Inquiries during the hearing ranged from Judge Gorsuch’s stance on abortion, to his support of religious freedom, to whether he would uphold President Trump’s controversial Executive Order on travel and immigration. Through it all, Judge Gorsuch, who presides over Denver’s 10th Circuit, kept his composure and refused to offer insight into which way he would lean when deciding such hot-button issues.
“If I were to start telling you which are my favorite [Supreme Court] precedents or which are my least favorite precedents, or if I viewed precedents in that fashion, I would be tipping my hand and suggesting to litigants that I’ve already made up my mind about their cases. That’s not a fair judge. I didn’t want that kind of judge when I was a lawyer, and I don’t want to be that kind of judge now.”
During the hearing, the case of Roe v. Wade was brought up repeatedly, and multiple senators from both parties questioned whether Judge Gorsuch would vote to overturn the right to an abortion. Sen. Lindsey Graham, (R-S.C.) discussed recent legislation he supports that would prohibit abortion if the probable postfertilization age of the fetus is 20 weeks or greater.
“We’re one of seven nations that allow wholesale, on demand, unlimited abortion at 20 weeks. I’d like to get out of that club,” Sen. Graham said during the hearing. “I’m just letting everybody know that if this legislation passes, it will be challenged before you and you will have to look at a new theory of how the state can protect the unborn ... Here’s what I think. You will read the briefs, look at the facts, and make a decision, am I fair to conclude that?”
“Senator, I can promise you no more than that, and I guarantee no less than that in every single case that comes before me,” Judge Gorsuch responded.
Sen. Dianne Feinstein (D-Calif.) queried whether Judge Gorsuch considered Roe to be “super precedent.”
“Senator, [the ruling] has been reaffirmed many times,” Judge Gorsuch responded, stressing that all Supreme Court precedent deserves respect and consideration when deciding new challenges.
The judge defended his 10th Circuit decision that found in favor of Hobby Lobby Stores after the company objected to the Affordable Care Act’s contraceptive coverage requirements based on religious grounds. In a separate case, Judge Gorsuch dissented from a ruling not to rehear a challenge by the Little Sisters of the Poor against certain contraceptive coverage provisions.
“Senator, our job there was to apply the statute as best we could understand its purpose as expressed in its text,” Judge Gorsuch said. “And I think every judge who faced that case – everyone – found it a hard case and did their level best and that’s all any judge can promise or guarantee. I respect all of my colleagues who addressed that case.”
The subject of religious freedom also was addressed during questions regarding President Trump’s Executive Order on travel and immigration and whether Judge Gorsuch would uphold the Executive Order if it came before the high court.
“President Trump promised a Muslim ban,” Sen. Patrick J. Leahy (D-Vt.) said during the hearing. “He still has on his website to this day that he’s called for a total and complete shutdown of Muslims entering the United States. And a Republican congressman recently said the best thing the president can do for his Muslim ban is to make sure he has Gorsuch on the Supreme Court.”
Judge Gorsuch called the unnamed congressman’s remark “silly,” adding that the congressman had “no idea” how Judge Gorsuch would rule in any case that comes before him. Sen. Leahy went on to ask Judge Gorsuch whether the president has the authority to block Jews from coming to the country or ban residents of Israel.
“We have a Constitution,” Judge Gorsuch replied. “And it does guarantee free exercise [of religion]. It also guarantees equal protection of the laws and a whole lot else besides, and the Supreme Court has held that due process rights extend even to undocumented persons in this country. I will apply the law faithfully and fearlessly and without regard to persons.”
A vote by the Senate Judiciary Committee is expected April 3 followed by a Senate floor vote later that week. Supreme Court justices require 60 votes for confirmation. Republicans control the Senate 52-48, so eight Democrats are needed to confirm Judge Gorsuch. Senate Minority Leader Charles E. Schumer (D-N.Y.) vowed on March 23 to oppose Judge Gorsuch and asked other Democrats to join him, setting up a potential filibuster against Judge Gorsuch’s confirmation.
[email protected]
On Twitter @legal_med
Throughout his marathon confirmation hearing, U.S. Supreme Court nominee Neil Gorsuch remained tight-lipped about how he might rule on major health care issues if confirmed to the country’s highest court, pledging to look at the facts of each case and rule according to the law.
The Senate Committee on the Judiciary wrapped up its nearly week-long questioning of Judge Gorsuch on March 23. Inquiries during the hearing ranged from Judge Gorsuch’s stance on abortion, to his support of religious freedom, to whether he would uphold President Trump’s controversial Executive Order on travel and immigration. Through it all, Judge Gorsuch, who presides over Denver’s 10th Circuit, kept his composure and refused to offer insight into which way he would lean when deciding such hot-button issues.
“If I were to start telling you which are my favorite [Supreme Court] precedents or which are my least favorite precedents, or if I viewed precedents in that fashion, I would be tipping my hand and suggesting to litigants that I’ve already made up my mind about their cases. That’s not a fair judge. I didn’t want that kind of judge when I was a lawyer, and I don’t want to be that kind of judge now.”
During the hearing, the case of Roe v. Wade was brought up repeatedly, and multiple senators from both parties questioned whether Judge Gorsuch would vote to overturn the right to an abortion. Sen. Lindsey Graham, (R-S.C.) discussed recent legislation he supports that would prohibit abortion if the probable postfertilization age of the fetus is 20 weeks or greater.
“We’re one of seven nations that allow wholesale, on demand, unlimited abortion at 20 weeks. I’d like to get out of that club,” Sen. Graham said during the hearing. “I’m just letting everybody know that if this legislation passes, it will be challenged before you and you will have to look at a new theory of how the state can protect the unborn ... Here’s what I think. You will read the briefs, look at the facts, and make a decision, am I fair to conclude that?”
“Senator, I can promise you no more than that, and I guarantee no less than that in every single case that comes before me,” Judge Gorsuch responded.
Sen. Dianne Feinstein (D-Calif.) queried whether Judge Gorsuch considered Roe to be “super precedent.”
“Senator, [the ruling] has been reaffirmed many times,” Judge Gorsuch responded, stressing that all Supreme Court precedent deserves respect and consideration when deciding new challenges.
The judge defended his 10th Circuit decision that found in favor of Hobby Lobby Stores after the company objected to the Affordable Care Act’s contraceptive coverage requirements based on religious grounds. In a separate case, Judge Gorsuch dissented from a ruling not to rehear a challenge by the Little Sisters of the Poor against certain contraceptive coverage provisions.
“Senator, our job there was to apply the statute as best we could understand its purpose as expressed in its text,” Judge Gorsuch said. “And I think every judge who faced that case – everyone – found it a hard case and did their level best and that’s all any judge can promise or guarantee. I respect all of my colleagues who addressed that case.”
The subject of religious freedom also was addressed during questions regarding President Trump’s Executive Order on travel and immigration and whether Judge Gorsuch would uphold the Executive Order if it came before the high court.
“President Trump promised a Muslim ban,” Sen. Patrick J. Leahy (D-Vt.) said during the hearing. “He still has on his website to this day that he’s called for a total and complete shutdown of Muslims entering the United States. And a Republican congressman recently said the best thing the president can do for his Muslim ban is to make sure he has Gorsuch on the Supreme Court.”
Judge Gorsuch called the unnamed congressman’s remark “silly,” adding that the congressman had “no idea” how Judge Gorsuch would rule in any case that comes before him. Sen. Leahy went on to ask Judge Gorsuch whether the president has the authority to block Jews from coming to the country or ban residents of Israel.
“We have a Constitution,” Judge Gorsuch replied. “And it does guarantee free exercise [of religion]. It also guarantees equal protection of the laws and a whole lot else besides, and the Supreme Court has held that due process rights extend even to undocumented persons in this country. I will apply the law faithfully and fearlessly and without regard to persons.”
A vote by the Senate Judiciary Committee is expected April 3 followed by a Senate floor vote later that week. Supreme Court justices require 60 votes for confirmation. Republicans control the Senate 52-48, so eight Democrats are needed to confirm Judge Gorsuch. Senate Minority Leader Charles E. Schumer (D-N.Y.) vowed on March 23 to oppose Judge Gorsuch and asked other Democrats to join him, setting up a potential filibuster against Judge Gorsuch’s confirmation.
[email protected]
On Twitter @legal_med
Throughout his marathon confirmation hearing, U.S. Supreme Court nominee Neil Gorsuch remained tight-lipped about how he might rule on major health care issues if confirmed to the country’s highest court, pledging to look at the facts of each case and rule according to the law.
The Senate Committee on the Judiciary wrapped up its nearly week-long questioning of Judge Gorsuch on March 23. Inquiries during the hearing ranged from Judge Gorsuch’s stance on abortion, to his support of religious freedom, to whether he would uphold President Trump’s controversial Executive Order on travel and immigration. Through it all, Judge Gorsuch, who presides over Denver’s 10th Circuit, kept his composure and refused to offer insight into which way he would lean when deciding such hot-button issues.
“If I were to start telling you which are my favorite [Supreme Court] precedents or which are my least favorite precedents, or if I viewed precedents in that fashion, I would be tipping my hand and suggesting to litigants that I’ve already made up my mind about their cases. That’s not a fair judge. I didn’t want that kind of judge when I was a lawyer, and I don’t want to be that kind of judge now.”
During the hearing, the case of Roe v. Wade was brought up repeatedly, and multiple senators from both parties questioned whether Judge Gorsuch would vote to overturn the right to an abortion. Sen. Lindsey Graham, (R-S.C.) discussed recent legislation he supports that would prohibit abortion if the probable postfertilization age of the fetus is 20 weeks or greater.
“We’re one of seven nations that allow wholesale, on demand, unlimited abortion at 20 weeks. I’d like to get out of that club,” Sen. Graham said during the hearing. “I’m just letting everybody know that if this legislation passes, it will be challenged before you and you will have to look at a new theory of how the state can protect the unborn ... Here’s what I think. You will read the briefs, look at the facts, and make a decision, am I fair to conclude that?”
“Senator, I can promise you no more than that, and I guarantee no less than that in every single case that comes before me,” Judge Gorsuch responded.
Sen. Dianne Feinstein (D-Calif.) queried whether Judge Gorsuch considered Roe to be “super precedent.”
“Senator, [the ruling] has been reaffirmed many times,” Judge Gorsuch responded, stressing that all Supreme Court precedent deserves respect and consideration when deciding new challenges.
The judge defended his 10th Circuit decision that found in favor of Hobby Lobby Stores after the company objected to the Affordable Care Act’s contraceptive coverage requirements based on religious grounds. In a separate case, Judge Gorsuch dissented from a ruling not to rehear a challenge by the Little Sisters of the Poor against certain contraceptive coverage provisions.
“Senator, our job there was to apply the statute as best we could understand its purpose as expressed in its text,” Judge Gorsuch said. “And I think every judge who faced that case – everyone – found it a hard case and did their level best and that’s all any judge can promise or guarantee. I respect all of my colleagues who addressed that case.”
The subject of religious freedom also was addressed during questions regarding President Trump’s Executive Order on travel and immigration and whether Judge Gorsuch would uphold the Executive Order if it came before the high court.
“President Trump promised a Muslim ban,” Sen. Patrick J. Leahy (D-Vt.) said during the hearing. “He still has on his website to this day that he’s called for a total and complete shutdown of Muslims entering the United States. And a Republican congressman recently said the best thing the president can do for his Muslim ban is to make sure he has Gorsuch on the Supreme Court.”
Judge Gorsuch called the unnamed congressman’s remark “silly,” adding that the congressman had “no idea” how Judge Gorsuch would rule in any case that comes before him. Sen. Leahy went on to ask Judge Gorsuch whether the president has the authority to block Jews from coming to the country or ban residents of Israel.
“We have a Constitution,” Judge Gorsuch replied. “And it does guarantee free exercise [of religion]. It also guarantees equal protection of the laws and a whole lot else besides, and the Supreme Court has held that due process rights extend even to undocumented persons in this country. I will apply the law faithfully and fearlessly and without regard to persons.”
A vote by the Senate Judiciary Committee is expected April 3 followed by a Senate floor vote later that week. Supreme Court justices require 60 votes for confirmation. Republicans control the Senate 52-48, so eight Democrats are needed to confirm Judge Gorsuch. Senate Minority Leader Charles E. Schumer (D-N.Y.) vowed on March 23 to oppose Judge Gorsuch and asked other Democrats to join him, setting up a potential filibuster against Judge Gorsuch’s confirmation.
[email protected]
On Twitter @legal_med
Foreign doctors may lose U.S. jobs after visa program suspension
While much of the drama surrounding the Trump administration’s immigration policy has centered on the so-called travel ban, changes to a specialized visa program may have a bigger impact on foreign doctors in the United States and the employers who hope to hire them.
Starting April 3, U.S. Citizenship and Immigration Services (USCIS) is temporarily suspending its expedited processing of H-1B visas, a primary route used by highly skilled foreign physicians and students to practice and train in the United States.
Under the existing “premium processing” system, foreign medical graduates – usually sponsored by a U.S. institution – pay an extra $1,200 when submitting an H-1B petition to ensure a response from USCIS within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
In the meantime, many foreign medical students and physicians will lose top training spots and jobs as their H-1B applications linger in the system, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“As a practical matter, the percentages of physicians coming into the U.S. who are accepted into residencies or fellowships, those are the top of the top for medical graduates around the world,” Ms. Minear said in an interview. “Most of them who stay afterward wind up working in underserved areas of the United States. It really doesn’t make much sense as a policy matter to create obstacles to attracting those people to the United States that would prevent them from getting here, obtaining U.S. education, and then remaining in the U.S. and providing urgently needed care to populations that would otherwise go without.”
Changing rules, uncertain futures
The H-1B processing change has left Amr Marawan, MD, unsure if a job offer may fall through and if he will be able to work in the United States at all over the next year.
Dr. Marawan, a native of Cairo, Egypt, will finish his internal medicine residency at the University of Tennessee, Chattanooga, in June and had planned to pursue a cardiology fellowship under a continuation of his J-1 alien physician visa. After the 2016 election, he decided instead to take a position as assistant professor of internal medicine at Virginia Commonwealth University in Richmond.
Among his reasons: A J-1 visa requires foreign trainees to return to their home country for 2 years following the completion of their training. With that requirement, he said there would be a gap in his career progression and that he might face challenges returning to the United States.
However, if Dr. Marawan accepted the job at VCU and received approval to waive the 2-year home country requirement from the Virginia Department of Health and the U.S. Department of State, he could apply for a 3-year H-1B visa through the premium processing program.
To get the home country requirement waived, physicians must agree to be employed full time in H-1B status at a health care facility within a designated health professional shortage area, medically underserved area, or medically underserved population.
“The main reason I switched my plan was after the presidential election, there was a lot of talk about changes to visas, so I thought it might be better to take this step now and do the waiver and hopefully this will help me to be more secure while working in order to pursue my medical career,” Dr. Marawan said.
Like many foreign doctors, Dr. Marawan now faces a conundrum. His J-1 visa expires in June and his position at VCU is slated to start in July, but the premium processing program terminates in April. If forced to wait the typical 6-10 months for standard processing, he may lose the position.
“There’s no way we can finish the [state approval] before June,” he said. “And now if we wait and file the H-1B in June, it will take months to get approved. During that time, I cannot work.”
Immigration attorneys have been inundated with similar stories and concerns by physicians regarding how to move forward after the H-1B premium processing suspension, said Adam Cohen, a Memphis attorney. USCIS has delayed premium processing in the past, but not to this extent, he said. [polldaddy:9710548]
This change “was dropped on us with no warning and it’s left us with less than a month to get all of these H-1B [applications] together,” he said.
While foreign physicians and students are scrambling to file their H-1B petitions before April 3, there is no guarantee that the applications will be expedited, Mr. Cohen added. It’s possible USCIS will be unable to get to every application and will simply refund the premium processing fee, he said. The applications would then be subject to standard processing.
USCIS says the suspension will help to address the accumulation of older applications, but the change will only shift the backlog, according to Washington attorney Allen Orr Jr.
USCIS spokeswoman Carolyn Gwathmey said officials cannot speculate whether they will get to every application filed before April 3.
“As noted in the agency’s announcement, we will continue to premium process form I-129 H-1B petitions if the petitioner properly filed an associated form I-907 before April 3, 2017,” Ms. Gwathmey said in an interview. “We will refund the premium processing fee if the petitioner filed the form for an H-1B petition before April 3, 2017, and we did not take adjudicative action on the case within the 15-calendar-day processing period.”
Foreign medical students face rough road
Medical students applying for residencies and fellowships may also be detoured by the premium processing ban. Students who planned to train under an H-1B visa had to wait until Match Day on March 17 to file their H-1B petitions, Ms. Minear said. There is little chance they can complete all paperwork and state approvals needed in order to submit an H-1B application before April 3.
“What this really means is that physicians effectively cannot do their residencies or fellowships in H-1B status this year because they cannot file the petitions in time for a July 1 start date,” Ms. Minear said. “Effectively, what it does is force all foreign doctors who want to do residency or fellowship in the U.S. to do their training in J-1 status.”
A large number of foreign medical students already complete their training in J-1 status; however, many residency and fellowship programs agree to sponsor students in H-1B status as an attractive recruiting incentive for top talent, Ms. Minear said. Foreign doctors often prefer the latter status because they are exempt from the 2-year requirement to return home.
Foreign medical students matching to residency programs generally have the option to apply for a J-1 visa and can still train in the United States, said Matthew Shick, JD, government relations director for the Association of American Medical Colleges. He noted that the premium processing suspension will have a greater impact on faculty, scientists, and hospital staff.
However, medical students applying for J-1 visas also may experience processing delays because of President Trump’s March 6 Executive Order on immigration. A provision in that order increases uniform screening procedures for all visa classes and nationalities, while another provision suspends the Visa Interview Waiver Program. The suspension means that certain visa applicants seeking to renew a visa must be interviewed in person by a consular officer. The Hawaii federal court that blocked much of the that Executive Order did not halt the additional screening requirements or stay the Visa Interview Waiver Program rollback. Both provisions remain in effect.
“It is reasonably foreseeable, based on the portions of the Executive Order that remain in place and based on the on-the-ground reality of State Department officials and consular officer resignations and departures, that this year it will be more challenging than in prior years for an incoming Match applicant to arrive on time at their GME program on July 1, even with the J-1 path,” Ms. Harris said.
Taskforce requests carve-out
The IMG Taskforce is urging USCIS to exempt physicians from the premium processing ban. In a March 8 letter to the agency, the task force outlined examples of how IMGs benefit the country and described how application delays could harm patient care and impair U.S. medical institutions.
“The hope is that this would encourage a review and a rethink of that shift and that upon that review, H-1B cap exempt petitions would across the board be considered for continued premium processing,” Ms. Harris said in an interview. “And/or, perhaps a greater lead time than merely 4 weeks’ notice [would be granted] so that people may be able complete their obligations.”
A group of U.S. senators also has requested that USCIS reconsider the premium processing suspension as it relates to physicians. Sen. Amy Klobuchar (D-Minn.) said that the suspension will exacerbate physician shortages, particularly in rural areas.
“The [waiver] program has helped address chronic physician shortages in rural America and other underserved areas for over two decades,” Sen. Klobuchar wrote in a March 10 letter. “We understand USCIS is facing a backlog, but USCIS has addressed this problem in the past without suspending premium processing for Conrad 30 doctors. We have every faith that USCIS can address its administrative needs without sacrificing support to this successful, time-tested program.”
Ms. Gwathmey would not comment on whether USCIS would consider an exception to the suspension for physicians. As with all affected workloads, USCIS is cognizant of processing time sensitivities for IMGs who are applying to change their status to H-1B, Ms. Gwathmey said in an interview.
“USCIS will be monitoring this workload during the coming months and will evaluate any time sensitive impacts prior to the resumption of premium processing services,” she said.
Dr. Marawan meanwhile is exhausting all efforts to keep his job offer. He is considering the option of filing an H-1B application now, before his state approval comes through, in the hopes of securing premium processing, he said. However, the option comes with a catch. Foreign doctors can file an H-1B petition without a J-1 waiver, but they can’t request a change of status from J-1 to H-1B without leaving the United States unless they have the waiver. This means if Dr. Marawan’s petition is approved by USCIS, he must go back to Egypt to apply for an H-1B visa at the U.S. Embassy in Cairo.
But with increased security delays for visa applicants and reports of foreign travelers being denied entry at U.S. airports, Dr. Marawan said he is fearful.
“Once you step out [of the United States], you never know what’s going to happen,” he said. “Sometimes visas get struck. Sometimes there’s a lot of security checks. Egypt is not included in the travel ban, but it’s always hard. There’s a lot of stories of people who are rejected getting their visas for different reasons. It’s worrisome.”
[email protected]
On Twitter @legal_med
While much of the drama surrounding the Trump administration’s immigration policy has centered on the so-called travel ban, changes to a specialized visa program may have a bigger impact on foreign doctors in the United States and the employers who hope to hire them.
Starting April 3, U.S. Citizenship and Immigration Services (USCIS) is temporarily suspending its expedited processing of H-1B visas, a primary route used by highly skilled foreign physicians and students to practice and train in the United States.
Under the existing “premium processing” system, foreign medical graduates – usually sponsored by a U.S. institution – pay an extra $1,200 when submitting an H-1B petition to ensure a response from USCIS within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
In the meantime, many foreign medical students and physicians will lose top training spots and jobs as their H-1B applications linger in the system, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“As a practical matter, the percentages of physicians coming into the U.S. who are accepted into residencies or fellowships, those are the top of the top for medical graduates around the world,” Ms. Minear said in an interview. “Most of them who stay afterward wind up working in underserved areas of the United States. It really doesn’t make much sense as a policy matter to create obstacles to attracting those people to the United States that would prevent them from getting here, obtaining U.S. education, and then remaining in the U.S. and providing urgently needed care to populations that would otherwise go without.”
Changing rules, uncertain futures
The H-1B processing change has left Amr Marawan, MD, unsure if a job offer may fall through and if he will be able to work in the United States at all over the next year.
Dr. Marawan, a native of Cairo, Egypt, will finish his internal medicine residency at the University of Tennessee, Chattanooga, in June and had planned to pursue a cardiology fellowship under a continuation of his J-1 alien physician visa. After the 2016 election, he decided instead to take a position as assistant professor of internal medicine at Virginia Commonwealth University in Richmond.
Among his reasons: A J-1 visa requires foreign trainees to return to their home country for 2 years following the completion of their training. With that requirement, he said there would be a gap in his career progression and that he might face challenges returning to the United States.
However, if Dr. Marawan accepted the job at VCU and received approval to waive the 2-year home country requirement from the Virginia Department of Health and the U.S. Department of State, he could apply for a 3-year H-1B visa through the premium processing program.
To get the home country requirement waived, physicians must agree to be employed full time in H-1B status at a health care facility within a designated health professional shortage area, medically underserved area, or medically underserved population.
“The main reason I switched my plan was after the presidential election, there was a lot of talk about changes to visas, so I thought it might be better to take this step now and do the waiver and hopefully this will help me to be more secure while working in order to pursue my medical career,” Dr. Marawan said.
Like many foreign doctors, Dr. Marawan now faces a conundrum. His J-1 visa expires in June and his position at VCU is slated to start in July, but the premium processing program terminates in April. If forced to wait the typical 6-10 months for standard processing, he may lose the position.
“There’s no way we can finish the [state approval] before June,” he said. “And now if we wait and file the H-1B in June, it will take months to get approved. During that time, I cannot work.”
Immigration attorneys have been inundated with similar stories and concerns by physicians regarding how to move forward after the H-1B premium processing suspension, said Adam Cohen, a Memphis attorney. USCIS has delayed premium processing in the past, but not to this extent, he said. [polldaddy:9710548]
This change “was dropped on us with no warning and it’s left us with less than a month to get all of these H-1B [applications] together,” he said.
While foreign physicians and students are scrambling to file their H-1B petitions before April 3, there is no guarantee that the applications will be expedited, Mr. Cohen added. It’s possible USCIS will be unable to get to every application and will simply refund the premium processing fee, he said. The applications would then be subject to standard processing.
USCIS says the suspension will help to address the accumulation of older applications, but the change will only shift the backlog, according to Washington attorney Allen Orr Jr.
USCIS spokeswoman Carolyn Gwathmey said officials cannot speculate whether they will get to every application filed before April 3.
“As noted in the agency’s announcement, we will continue to premium process form I-129 H-1B petitions if the petitioner properly filed an associated form I-907 before April 3, 2017,” Ms. Gwathmey said in an interview. “We will refund the premium processing fee if the petitioner filed the form for an H-1B petition before April 3, 2017, and we did not take adjudicative action on the case within the 15-calendar-day processing period.”
Foreign medical students face rough road
Medical students applying for residencies and fellowships may also be detoured by the premium processing ban. Students who planned to train under an H-1B visa had to wait until Match Day on March 17 to file their H-1B petitions, Ms. Minear said. There is little chance they can complete all paperwork and state approvals needed in order to submit an H-1B application before April 3.
“What this really means is that physicians effectively cannot do their residencies or fellowships in H-1B status this year because they cannot file the petitions in time for a July 1 start date,” Ms. Minear said. “Effectively, what it does is force all foreign doctors who want to do residency or fellowship in the U.S. to do their training in J-1 status.”
A large number of foreign medical students already complete their training in J-1 status; however, many residency and fellowship programs agree to sponsor students in H-1B status as an attractive recruiting incentive for top talent, Ms. Minear said. Foreign doctors often prefer the latter status because they are exempt from the 2-year requirement to return home.
Foreign medical students matching to residency programs generally have the option to apply for a J-1 visa and can still train in the United States, said Matthew Shick, JD, government relations director for the Association of American Medical Colleges. He noted that the premium processing suspension will have a greater impact on faculty, scientists, and hospital staff.
However, medical students applying for J-1 visas also may experience processing delays because of President Trump’s March 6 Executive Order on immigration. A provision in that order increases uniform screening procedures for all visa classes and nationalities, while another provision suspends the Visa Interview Waiver Program. The suspension means that certain visa applicants seeking to renew a visa must be interviewed in person by a consular officer. The Hawaii federal court that blocked much of the that Executive Order did not halt the additional screening requirements or stay the Visa Interview Waiver Program rollback. Both provisions remain in effect.
“It is reasonably foreseeable, based on the portions of the Executive Order that remain in place and based on the on-the-ground reality of State Department officials and consular officer resignations and departures, that this year it will be more challenging than in prior years for an incoming Match applicant to arrive on time at their GME program on July 1, even with the J-1 path,” Ms. Harris said.
Taskforce requests carve-out
The IMG Taskforce is urging USCIS to exempt physicians from the premium processing ban. In a March 8 letter to the agency, the task force outlined examples of how IMGs benefit the country and described how application delays could harm patient care and impair U.S. medical institutions.
“The hope is that this would encourage a review and a rethink of that shift and that upon that review, H-1B cap exempt petitions would across the board be considered for continued premium processing,” Ms. Harris said in an interview. “And/or, perhaps a greater lead time than merely 4 weeks’ notice [would be granted] so that people may be able complete their obligations.”
A group of U.S. senators also has requested that USCIS reconsider the premium processing suspension as it relates to physicians. Sen. Amy Klobuchar (D-Minn.) said that the suspension will exacerbate physician shortages, particularly in rural areas.
“The [waiver] program has helped address chronic physician shortages in rural America and other underserved areas for over two decades,” Sen. Klobuchar wrote in a March 10 letter. “We understand USCIS is facing a backlog, but USCIS has addressed this problem in the past without suspending premium processing for Conrad 30 doctors. We have every faith that USCIS can address its administrative needs without sacrificing support to this successful, time-tested program.”
Ms. Gwathmey would not comment on whether USCIS would consider an exception to the suspension for physicians. As with all affected workloads, USCIS is cognizant of processing time sensitivities for IMGs who are applying to change their status to H-1B, Ms. Gwathmey said in an interview.
“USCIS will be monitoring this workload during the coming months and will evaluate any time sensitive impacts prior to the resumption of premium processing services,” she said.
Dr. Marawan meanwhile is exhausting all efforts to keep his job offer. He is considering the option of filing an H-1B application now, before his state approval comes through, in the hopes of securing premium processing, he said. However, the option comes with a catch. Foreign doctors can file an H-1B petition without a J-1 waiver, but they can’t request a change of status from J-1 to H-1B without leaving the United States unless they have the waiver. This means if Dr. Marawan’s petition is approved by USCIS, he must go back to Egypt to apply for an H-1B visa at the U.S. Embassy in Cairo.
But with increased security delays for visa applicants and reports of foreign travelers being denied entry at U.S. airports, Dr. Marawan said he is fearful.
“Once you step out [of the United States], you never know what’s going to happen,” he said. “Sometimes visas get struck. Sometimes there’s a lot of security checks. Egypt is not included in the travel ban, but it’s always hard. There’s a lot of stories of people who are rejected getting their visas for different reasons. It’s worrisome.”
[email protected]
On Twitter @legal_med
While much of the drama surrounding the Trump administration’s immigration policy has centered on the so-called travel ban, changes to a specialized visa program may have a bigger impact on foreign doctors in the United States and the employers who hope to hire them.
Starting April 3, U.S. Citizenship and Immigration Services (USCIS) is temporarily suspending its expedited processing of H-1B visas, a primary route used by highly skilled foreign physicians and students to practice and train in the United States.
Under the existing “premium processing” system, foreign medical graduates – usually sponsored by a U.S. institution – pay an extra $1,200 when submitting an H-1B petition to ensure a response from USCIS within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
In the meantime, many foreign medical students and physicians will lose top training spots and jobs as their H-1B applications linger in the system, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“As a practical matter, the percentages of physicians coming into the U.S. who are accepted into residencies or fellowships, those are the top of the top for medical graduates around the world,” Ms. Minear said in an interview. “Most of them who stay afterward wind up working in underserved areas of the United States. It really doesn’t make much sense as a policy matter to create obstacles to attracting those people to the United States that would prevent them from getting here, obtaining U.S. education, and then remaining in the U.S. and providing urgently needed care to populations that would otherwise go without.”
Changing rules, uncertain futures
The H-1B processing change has left Amr Marawan, MD, unsure if a job offer may fall through and if he will be able to work in the United States at all over the next year.
Dr. Marawan, a native of Cairo, Egypt, will finish his internal medicine residency at the University of Tennessee, Chattanooga, in June and had planned to pursue a cardiology fellowship under a continuation of his J-1 alien physician visa. After the 2016 election, he decided instead to take a position as assistant professor of internal medicine at Virginia Commonwealth University in Richmond.
Among his reasons: A J-1 visa requires foreign trainees to return to their home country for 2 years following the completion of their training. With that requirement, he said there would be a gap in his career progression and that he might face challenges returning to the United States.
However, if Dr. Marawan accepted the job at VCU and received approval to waive the 2-year home country requirement from the Virginia Department of Health and the U.S. Department of State, he could apply for a 3-year H-1B visa through the premium processing program.
To get the home country requirement waived, physicians must agree to be employed full time in H-1B status at a health care facility within a designated health professional shortage area, medically underserved area, or medically underserved population.
“The main reason I switched my plan was after the presidential election, there was a lot of talk about changes to visas, so I thought it might be better to take this step now and do the waiver and hopefully this will help me to be more secure while working in order to pursue my medical career,” Dr. Marawan said.
Like many foreign doctors, Dr. Marawan now faces a conundrum. His J-1 visa expires in June and his position at VCU is slated to start in July, but the premium processing program terminates in April. If forced to wait the typical 6-10 months for standard processing, he may lose the position.
“There’s no way we can finish the [state approval] before June,” he said. “And now if we wait and file the H-1B in June, it will take months to get approved. During that time, I cannot work.”
Immigration attorneys have been inundated with similar stories and concerns by physicians regarding how to move forward after the H-1B premium processing suspension, said Adam Cohen, a Memphis attorney. USCIS has delayed premium processing in the past, but not to this extent, he said. [polldaddy:9710548]
This change “was dropped on us with no warning and it’s left us with less than a month to get all of these H-1B [applications] together,” he said.
While foreign physicians and students are scrambling to file their H-1B petitions before April 3, there is no guarantee that the applications will be expedited, Mr. Cohen added. It’s possible USCIS will be unable to get to every application and will simply refund the premium processing fee, he said. The applications would then be subject to standard processing.
USCIS says the suspension will help to address the accumulation of older applications, but the change will only shift the backlog, according to Washington attorney Allen Orr Jr.
USCIS spokeswoman Carolyn Gwathmey said officials cannot speculate whether they will get to every application filed before April 3.
“As noted in the agency’s announcement, we will continue to premium process form I-129 H-1B petitions if the petitioner properly filed an associated form I-907 before April 3, 2017,” Ms. Gwathmey said in an interview. “We will refund the premium processing fee if the petitioner filed the form for an H-1B petition before April 3, 2017, and we did not take adjudicative action on the case within the 15-calendar-day processing period.”
Foreign medical students face rough road
Medical students applying for residencies and fellowships may also be detoured by the premium processing ban. Students who planned to train under an H-1B visa had to wait until Match Day on March 17 to file their H-1B petitions, Ms. Minear said. There is little chance they can complete all paperwork and state approvals needed in order to submit an H-1B application before April 3.
“What this really means is that physicians effectively cannot do their residencies or fellowships in H-1B status this year because they cannot file the petitions in time for a July 1 start date,” Ms. Minear said. “Effectively, what it does is force all foreign doctors who want to do residency or fellowship in the U.S. to do their training in J-1 status.”
A large number of foreign medical students already complete their training in J-1 status; however, many residency and fellowship programs agree to sponsor students in H-1B status as an attractive recruiting incentive for top talent, Ms. Minear said. Foreign doctors often prefer the latter status because they are exempt from the 2-year requirement to return home.
Foreign medical students matching to residency programs generally have the option to apply for a J-1 visa and can still train in the United States, said Matthew Shick, JD, government relations director for the Association of American Medical Colleges. He noted that the premium processing suspension will have a greater impact on faculty, scientists, and hospital staff.
However, medical students applying for J-1 visas also may experience processing delays because of President Trump’s March 6 Executive Order on immigration. A provision in that order increases uniform screening procedures for all visa classes and nationalities, while another provision suspends the Visa Interview Waiver Program. The suspension means that certain visa applicants seeking to renew a visa must be interviewed in person by a consular officer. The Hawaii federal court that blocked much of the that Executive Order did not halt the additional screening requirements or stay the Visa Interview Waiver Program rollback. Both provisions remain in effect.
“It is reasonably foreseeable, based on the portions of the Executive Order that remain in place and based on the on-the-ground reality of State Department officials and consular officer resignations and departures, that this year it will be more challenging than in prior years for an incoming Match applicant to arrive on time at their GME program on July 1, even with the J-1 path,” Ms. Harris said.
Taskforce requests carve-out
The IMG Taskforce is urging USCIS to exempt physicians from the premium processing ban. In a March 8 letter to the agency, the task force outlined examples of how IMGs benefit the country and described how application delays could harm patient care and impair U.S. medical institutions.
“The hope is that this would encourage a review and a rethink of that shift and that upon that review, H-1B cap exempt petitions would across the board be considered for continued premium processing,” Ms. Harris said in an interview. “And/or, perhaps a greater lead time than merely 4 weeks’ notice [would be granted] so that people may be able complete their obligations.”
A group of U.S. senators also has requested that USCIS reconsider the premium processing suspension as it relates to physicians. Sen. Amy Klobuchar (D-Minn.) said that the suspension will exacerbate physician shortages, particularly in rural areas.
“The [waiver] program has helped address chronic physician shortages in rural America and other underserved areas for over two decades,” Sen. Klobuchar wrote in a March 10 letter. “We understand USCIS is facing a backlog, but USCIS has addressed this problem in the past without suspending premium processing for Conrad 30 doctors. We have every faith that USCIS can address its administrative needs without sacrificing support to this successful, time-tested program.”
Ms. Gwathmey would not comment on whether USCIS would consider an exception to the suspension for physicians. As with all affected workloads, USCIS is cognizant of processing time sensitivities for IMGs who are applying to change their status to H-1B, Ms. Gwathmey said in an interview.
“USCIS will be monitoring this workload during the coming months and will evaluate any time sensitive impacts prior to the resumption of premium processing services,” she said.
Dr. Marawan meanwhile is exhausting all efforts to keep his job offer. He is considering the option of filing an H-1B application now, before his state approval comes through, in the hopes of securing premium processing, he said. However, the option comes with a catch. Foreign doctors can file an H-1B petition without a J-1 waiver, but they can’t request a change of status from J-1 to H-1B without leaving the United States unless they have the waiver. This means if Dr. Marawan’s petition is approved by USCIS, he must go back to Egypt to apply for an H-1B visa at the U.S. Embassy in Cairo.
But with increased security delays for visa applicants and reports of foreign travelers being denied entry at U.S. airports, Dr. Marawan said he is fearful.
“Once you step out [of the United States], you never know what’s going to happen,” he said. “Sometimes visas get struck. Sometimes there’s a lot of security checks. Egypt is not included in the travel ban, but it’s always hard. There’s a lot of stories of people who are rejected getting their visas for different reasons. It’s worrisome.”
[email protected]
On Twitter @legal_med
New Trump travel order could disrupt meetings, trainees
President’s Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and impede assemblies of the world’s top medical experts.
The executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The new executive measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban that has been blocked by federal courts.
The new order clarifies that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition.
The revised travel ban could disrupt the exchange of medical knowledge by barring foreign experts from traveling to medical and scientific conferences in the United States, and leaves the status of medical trainees from those countries in limbo, according to American Medical Association President Andrew W. Gurman, MD.
“Hundreds of physicians from six countries are subject to the revised executive order and have applied to U.S. training programs and requested visa sponsorship,” he said in a statement. “The new executive order leaves them in limbo and without an explicit waiver, these foreign physicians will be unable to provide care in the U.S. when training programs begin on July 1.”
The leadership of Digestive Disease Week® (DDW) believes that the recent executive order banning travel of foreign nationals and refugees from seven countries to the U.S. will stifle discussion among members of the scientific community. Presentations and meetings that occur during DDW allow physicians and scientists from around the world to learn about and discuss cutting-edge scientific research and create partnerships that often lead to innovations in identifying, screening, and treating digestive disorders, as well as improving patient care.
The new order is already being challenged in court. On March 7, the state of Hawaii filed a lawsuit seeking to block the order, saying that it subjects a portion of Hawaii’s population to “discrimination and second-class treatment.”
When the original ban took effect, thousands of academics from around the world, including physicians, researchers, and professors, vowed to boycott U.S.-based conferences. A Google Docs petition started shortly after the ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said.
A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9.
The new executive order excludes Iraq this time around and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
President’s Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and impede assemblies of the world’s top medical experts.
The executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The new executive measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban that has been blocked by federal courts.
The new order clarifies that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition.
The revised travel ban could disrupt the exchange of medical knowledge by barring foreign experts from traveling to medical and scientific conferences in the United States, and leaves the status of medical trainees from those countries in limbo, according to American Medical Association President Andrew W. Gurman, MD.
“Hundreds of physicians from six countries are subject to the revised executive order and have applied to U.S. training programs and requested visa sponsorship,” he said in a statement. “The new executive order leaves them in limbo and without an explicit waiver, these foreign physicians will be unable to provide care in the U.S. when training programs begin on July 1.”
The leadership of Digestive Disease Week® (DDW) believes that the recent executive order banning travel of foreign nationals and refugees from seven countries to the U.S. will stifle discussion among members of the scientific community. Presentations and meetings that occur during DDW allow physicians and scientists from around the world to learn about and discuss cutting-edge scientific research and create partnerships that often lead to innovations in identifying, screening, and treating digestive disorders, as well as improving patient care.
The new order is already being challenged in court. On March 7, the state of Hawaii filed a lawsuit seeking to block the order, saying that it subjects a portion of Hawaii’s population to “discrimination and second-class treatment.”
When the original ban took effect, thousands of academics from around the world, including physicians, researchers, and professors, vowed to boycott U.S.-based conferences. A Google Docs petition started shortly after the ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said.
A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9.
The new executive order excludes Iraq this time around and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
President’s Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and impede assemblies of the world’s top medical experts.
The executive order, signed March 6, bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from the affected countries from entering the U.S. for 120 days. The new executive measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban that has been blocked by federal courts.
The new order clarifies that citizens of the six countries who are legal permanent U.S. residents or who have current visas to enter the country are exempt from the travel prohibition.
The revised travel ban could disrupt the exchange of medical knowledge by barring foreign experts from traveling to medical and scientific conferences in the United States, and leaves the status of medical trainees from those countries in limbo, according to American Medical Association President Andrew W. Gurman, MD.
“Hundreds of physicians from six countries are subject to the revised executive order and have applied to U.S. training programs and requested visa sponsorship,” he said in a statement. “The new executive order leaves them in limbo and without an explicit waiver, these foreign physicians will be unable to provide care in the U.S. when training programs begin on July 1.”
The leadership of Digestive Disease Week® (DDW) believes that the recent executive order banning travel of foreign nationals and refugees from seven countries to the U.S. will stifle discussion among members of the scientific community. Presentations and meetings that occur during DDW allow physicians and scientists from around the world to learn about and discuss cutting-edge scientific research and create partnerships that often lead to innovations in identifying, screening, and treating digestive disorders, as well as improving patient care.
The new order is already being challenged in court. On March 7, the state of Hawaii filed a lawsuit seeking to block the order, saying that it subjects a portion of Hawaii’s population to “discrimination and second-class treatment.”
When the original ban took effect, thousands of academics from around the world, including physicians, researchers, and professors, vowed to boycott U.S.-based conferences. A Google Docs petition started shortly after the ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said.
A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9.
The new executive order excludes Iraq this time around and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
Senate confirms Verma as CMS administrator
The Senate confirmed Seema Verma as administrator of the Centers for Medicare & Medicaid Services on March 13 by a largely party line vote of 55-43.
Ms. Verma’s confirmation comes as Republicans begin their efforts to repeal and replace the Affordable Care Act. During the March 13 debate, Senate Finance Committee Chairman Orrin Hatch (R-Utah) reiterated his support for Ms. Verma, saying she will be a needed leader during the transition from the ACA.
Senate Finance Committee Ranking Member Ron Wyden (D-Ore.) continued to criticize Ms. Verma during the debate, stressing that she has presented no clear vision of her plans as the next CMS administrator.
“Ms. Verma gave the Finance Committee and the public virtually nothing to go by in terms of how she’d approach this job,” Sen. Wyden said during floor debate. “If confirmed, she’d be one of the top officials to implement Trumpcare, a bill that would raid Medicaid, slash Medicare, and kick millions of Americans off their health care... So I’m unable to support this nomination.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
During her confirmation hearing, senators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard, a company that had financial interests in the health programs she designed. But Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for Hewlett Packard. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
The Association for Community Affiliated Plans (ACAP) pledged to work with Ms. Verma as the Trump administration works toward changing how Medicaid is financed and administered. ACAP represents nonprofit safety net health plans in 28 states that serve patients enrolled in Medicaid, Medicare, the Children’s Health Insurance Program, marketplaces, and other publicly supported health programs.
“Flexibility is one of the great things about the Medicaid program today – this very flexibility is what has allowed the changes Ms. Verma helped to effect in Indiana,” ACAP CEO Margaret A. Murray said in a statement. “We look forward to working with Ms. Verma on pathways to refine the program while maintaining its guarantee of coverage for all eligible individuals, improving transparency and actuarial soundness in rate-setting, and assuring access to needed care and services.”
[email protected]
On Twitter @legal_med
The Senate confirmed Seema Verma as administrator of the Centers for Medicare & Medicaid Services on March 13 by a largely party line vote of 55-43.
Ms. Verma’s confirmation comes as Republicans begin their efforts to repeal and replace the Affordable Care Act. During the March 13 debate, Senate Finance Committee Chairman Orrin Hatch (R-Utah) reiterated his support for Ms. Verma, saying she will be a needed leader during the transition from the ACA.
Senate Finance Committee Ranking Member Ron Wyden (D-Ore.) continued to criticize Ms. Verma during the debate, stressing that she has presented no clear vision of her plans as the next CMS administrator.
“Ms. Verma gave the Finance Committee and the public virtually nothing to go by in terms of how she’d approach this job,” Sen. Wyden said during floor debate. “If confirmed, she’d be one of the top officials to implement Trumpcare, a bill that would raid Medicaid, slash Medicare, and kick millions of Americans off their health care... So I’m unable to support this nomination.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
During her confirmation hearing, senators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard, a company that had financial interests in the health programs she designed. But Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for Hewlett Packard. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
The Association for Community Affiliated Plans (ACAP) pledged to work with Ms. Verma as the Trump administration works toward changing how Medicaid is financed and administered. ACAP represents nonprofit safety net health plans in 28 states that serve patients enrolled in Medicaid, Medicare, the Children’s Health Insurance Program, marketplaces, and other publicly supported health programs.
“Flexibility is one of the great things about the Medicaid program today – this very flexibility is what has allowed the changes Ms. Verma helped to effect in Indiana,” ACAP CEO Margaret A. Murray said in a statement. “We look forward to working with Ms. Verma on pathways to refine the program while maintaining its guarantee of coverage for all eligible individuals, improving transparency and actuarial soundness in rate-setting, and assuring access to needed care and services.”
[email protected]
On Twitter @legal_med
The Senate confirmed Seema Verma as administrator of the Centers for Medicare & Medicaid Services on March 13 by a largely party line vote of 55-43.
Ms. Verma’s confirmation comes as Republicans begin their efforts to repeal and replace the Affordable Care Act. During the March 13 debate, Senate Finance Committee Chairman Orrin Hatch (R-Utah) reiterated his support for Ms. Verma, saying she will be a needed leader during the transition from the ACA.
Senate Finance Committee Ranking Member Ron Wyden (D-Ore.) continued to criticize Ms. Verma during the debate, stressing that she has presented no clear vision of her plans as the next CMS administrator.
“Ms. Verma gave the Finance Committee and the public virtually nothing to go by in terms of how she’d approach this job,” Sen. Wyden said during floor debate. “If confirmed, she’d be one of the top officials to implement Trumpcare, a bill that would raid Medicaid, slash Medicare, and kick millions of Americans off their health care... So I’m unable to support this nomination.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
During her confirmation hearing, senators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard, a company that had financial interests in the health programs she designed. But Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for Hewlett Packard. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
The Association for Community Affiliated Plans (ACAP) pledged to work with Ms. Verma as the Trump administration works toward changing how Medicaid is financed and administered. ACAP represents nonprofit safety net health plans in 28 states that serve patients enrolled in Medicaid, Medicare, the Children’s Health Insurance Program, marketplaces, and other publicly supported health programs.
“Flexibility is one of the great things about the Medicaid program today – this very flexibility is what has allowed the changes Ms. Verma helped to effect in Indiana,” ACAP CEO Margaret A. Murray said in a statement. “We look forward to working with Ms. Verma on pathways to refine the program while maintaining its guarantee of coverage for all eligible individuals, improving transparency and actuarial soundness in rate-setting, and assuring access to needed care and services.”
[email protected]
On Twitter @legal_med
Federal judge blocks Anthem-Cigna merger
A federal district court judge has blocked health insurer Anthem from acquiring Cigna, ruling the megamerger would violate antitrust laws and stifle competition.
The decision came weeks after another U.S. district court judge barred a merger between health insurance giants Aetna and Humana.
The U.S. Department of Justice praised the latest ruling, calling the decision a victory for patients.
“This merger would have stifled competition, harming consumers by increasing health insurance prices and slowing innovation aimed at lowering the costs of health care,” Acting Assistant Attorney General Brent Snyder said in a statement.
Anthem intends to appeal the decision, said Joseph R. Swedish, Anthem’s chair, president, and chief executive officer. “Anthem is significantly disappointed by the decision, as combining Anthem and Cigna would positively impact the health and well-being of millions of Americans – saving them more than $2 billion in medical costs annually,” Mr. Swedish said in a statement. “If not overturned, the consequences of the decision are far reaching and will hurt American consumers by limiting their access to high-quality affordable care, slowing the industry’s shift to value-based care and improved outcomes for patients, and restricting innovation, which is critical to meeting the evolving needs of health care consumers.”
In a statement, a Cigna official said the company intends to carefully review the opinion and evaluate its options in accordance with the merger agreement.
“Cigna remains focused on helping to improve health care by delivering value to our customers and clients and expanding our business around the world,” the statement said.
The DOJ, 11 states, and the District of Columbia sued Anthem and Cigna in July over their proposed $54 billion consolidation in what would have been the largest merger in history.
The DOJ argued the merger would substantially harm competition and negatively impact the entire insurance industry if allowed to proceed. The consolidation would enhance Anthem’s power to profit at the expense of consumers and the doctors and hospitals who provide their medical care, DOJ attorneys said in their complaint.
Anthem and Cigna argued the proposed acquisition was “procompetitive,” and that the merger would result in efficiencies that would directly benefit consumers via greater access to affordable health care. The benefits of the merger outweigh any alleged anticompetitive effects, according to Anthem.
A trial before Judge Amy Berman Jackson of the U.S. District Court for the District of Columbia ran from November through January.
Judge Berman’s opinion is temporarily under seal to allow parties to review for confidentiality.
The ruling is the second victory for the DOJ in as many weeks. In a Jan. 23 decision, Judge John D. Bates of the U.S. District Court for the District of Columbia denied Aetna’s $37 billion plan to purchase Humana, following a month-long trial that began in early December. Judge Bates ruled the consolidation would violate antitrust laws and reduce competition.
Aetna and Humana did not respond to requests for comment.
On Twitter @legal_med
Michael E. Nelson, MD, FCCP, comments: Any business owner who has been required to absorb yearly double-digit increases in employee health insurance costs cannot help but wonder where Mr. Swedish learned his “new math.” His second statement is even more incogitable – since when were insurers known for expanding access to health care.
Michael E. Nelson, MD, FCCP, comments: Any business owner who has been required to absorb yearly double-digit increases in employee health insurance costs cannot help but wonder where Mr. Swedish learned his “new math.” His second statement is even more incogitable – since when were insurers known for expanding access to health care.
Michael E. Nelson, MD, FCCP, comments: Any business owner who has been required to absorb yearly double-digit increases in employee health insurance costs cannot help but wonder where Mr. Swedish learned his “new math.” His second statement is even more incogitable – since when were insurers known for expanding access to health care.
A federal district court judge has blocked health insurer Anthem from acquiring Cigna, ruling the megamerger would violate antitrust laws and stifle competition.
The decision came weeks after another U.S. district court judge barred a merger between health insurance giants Aetna and Humana.
The U.S. Department of Justice praised the latest ruling, calling the decision a victory for patients.
“This merger would have stifled competition, harming consumers by increasing health insurance prices and slowing innovation aimed at lowering the costs of health care,” Acting Assistant Attorney General Brent Snyder said in a statement.
Anthem intends to appeal the decision, said Joseph R. Swedish, Anthem’s chair, president, and chief executive officer. “Anthem is significantly disappointed by the decision, as combining Anthem and Cigna would positively impact the health and well-being of millions of Americans – saving them more than $2 billion in medical costs annually,” Mr. Swedish said in a statement. “If not overturned, the consequences of the decision are far reaching and will hurt American consumers by limiting their access to high-quality affordable care, slowing the industry’s shift to value-based care and improved outcomes for patients, and restricting innovation, which is critical to meeting the evolving needs of health care consumers.”
In a statement, a Cigna official said the company intends to carefully review the opinion and evaluate its options in accordance with the merger agreement.
“Cigna remains focused on helping to improve health care by delivering value to our customers and clients and expanding our business around the world,” the statement said.
The DOJ, 11 states, and the District of Columbia sued Anthem and Cigna in July over their proposed $54 billion consolidation in what would have been the largest merger in history.
The DOJ argued the merger would substantially harm competition and negatively impact the entire insurance industry if allowed to proceed. The consolidation would enhance Anthem’s power to profit at the expense of consumers and the doctors and hospitals who provide their medical care, DOJ attorneys said in their complaint.
Anthem and Cigna argued the proposed acquisition was “procompetitive,” and that the merger would result in efficiencies that would directly benefit consumers via greater access to affordable health care. The benefits of the merger outweigh any alleged anticompetitive effects, according to Anthem.
A trial before Judge Amy Berman Jackson of the U.S. District Court for the District of Columbia ran from November through January.
Judge Berman’s opinion is temporarily under seal to allow parties to review for confidentiality.
The ruling is the second victory for the DOJ in as many weeks. In a Jan. 23 decision, Judge John D. Bates of the U.S. District Court for the District of Columbia denied Aetna’s $37 billion plan to purchase Humana, following a month-long trial that began in early December. Judge Bates ruled the consolidation would violate antitrust laws and reduce competition.
Aetna and Humana did not respond to requests for comment.
On Twitter @legal_med
A federal district court judge has blocked health insurer Anthem from acquiring Cigna, ruling the megamerger would violate antitrust laws and stifle competition.
The decision came weeks after another U.S. district court judge barred a merger between health insurance giants Aetna and Humana.
The U.S. Department of Justice praised the latest ruling, calling the decision a victory for patients.
“This merger would have stifled competition, harming consumers by increasing health insurance prices and slowing innovation aimed at lowering the costs of health care,” Acting Assistant Attorney General Brent Snyder said in a statement.
Anthem intends to appeal the decision, said Joseph R. Swedish, Anthem’s chair, president, and chief executive officer. “Anthem is significantly disappointed by the decision, as combining Anthem and Cigna would positively impact the health and well-being of millions of Americans – saving them more than $2 billion in medical costs annually,” Mr. Swedish said in a statement. “If not overturned, the consequences of the decision are far reaching and will hurt American consumers by limiting their access to high-quality affordable care, slowing the industry’s shift to value-based care and improved outcomes for patients, and restricting innovation, which is critical to meeting the evolving needs of health care consumers.”
In a statement, a Cigna official said the company intends to carefully review the opinion and evaluate its options in accordance with the merger agreement.
“Cigna remains focused on helping to improve health care by delivering value to our customers and clients and expanding our business around the world,” the statement said.
The DOJ, 11 states, and the District of Columbia sued Anthem and Cigna in July over their proposed $54 billion consolidation in what would have been the largest merger in history.
The DOJ argued the merger would substantially harm competition and negatively impact the entire insurance industry if allowed to proceed. The consolidation would enhance Anthem’s power to profit at the expense of consumers and the doctors and hospitals who provide their medical care, DOJ attorneys said in their complaint.
Anthem and Cigna argued the proposed acquisition was “procompetitive,” and that the merger would result in efficiencies that would directly benefit consumers via greater access to affordable health care. The benefits of the merger outweigh any alleged anticompetitive effects, according to Anthem.
A trial before Judge Amy Berman Jackson of the U.S. District Court for the District of Columbia ran from November through January.
Judge Berman’s opinion is temporarily under seal to allow parties to review for confidentiality.
The ruling is the second victory for the DOJ in as many weeks. In a Jan. 23 decision, Judge John D. Bates of the U.S. District Court for the District of Columbia denied Aetna’s $37 billion plan to purchase Humana, following a month-long trial that began in early December. Judge Bates ruled the consolidation would violate antitrust laws and reduce competition.
Aetna and Humana did not respond to requests for comment.
On Twitter @legal_med
Trump travel policy may affect medical meetings
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
Malpractice bill would impose $250,000 damages cap
New legislation approved by the House Judiciary Committee could mean legal relief for health providers in the form of capped damages and a tighter time frame for lawsuits.
The House Judiciary Committee passed the Protecting Access to Care Act of 2017 (H.R. 1215) on Feb. 28 by a vote of 18-17. The bill, modeled after California’s Medical Injury Compensation Reform Act (MICRA), would limit noneconomic damages in medical malpractice cases to $250,000, restrict contingency fees charged by attorneys, and enforce a 3-year statute of limitations for liability lawsuits from the date of alleged injury. The bill also includes a “fair share” rule in which defendants are liable only for the damages in direct proportion to their percentage of responsibility.
The bill is the first significant medical professional liability reform legislation to be approved by the committee since 2011, said Brian K. Atchinson, president and CEO of PIAA, a national trade association for medical liability insurers.
“Unlike previous federal bills, the bill is focused solely on health care professionals and entities, includes detailed flexibility for states for all its reforms, and is linked with the expenditure of federal dollars to address states’ rights concerns,” Mr. Atchinson said in a statement. “H.R. 1215 will help ensure fair and timely compensation to injured patients, improve access to patient care, and promote affordable and accessible medical liability insurance coverage.”
The proposed statute would apply to any patient who receives medical care provided via a federal program, such as Medicare or Medicaid, or via a subsidy or tax benefit, such as coverage purchased under the Affordable Care Act or a future* replacement. Medical care paid by employer health plans would fall under the legislation’s umbrella since insurance premiums receive federal tax exemptions. The bill would not preempt state medical malpractice laws that impose damage caps, whether higher or lower than $250,000, nor would the legislation affect the availability of economic damages, according to bill language.
As part of the H.R. 1215, courts could limit how much attorneys receive from a patient’s ultimate award. Specifically, courts would have the power to restrict payments from a plaintiff’s damage recovery to an attorney who claims a financial stake in the outcome by virtue of a contingent fee.
“The Protecting Access to Care Act will help keep the rising costs of health care from being passed along to the American people,” Rep. Goodlatte said in a statement. “The Congressional Budget Office estimates that the reforms contained in the bill would lower health care costs by tens of billions of dollars.”
Public Citizen, a consumer rights group, criticized the legislation as misleading to consumers and harmful to patients.
“Proposals to shield providers from liability are nothing but a giveaway to industry,” Lisa Gilbert, director of Public Citizen’s Congress Watch, said in a statement. “Members supporting this bill would further harm those who are suffering from doctors’ mistakes and abandon the GOP’s supposedly unwavering commitment to state’s rights.”
“There are so many moving parts to this bill, I think the likelihood of its being passed as is is low,” said Dr. Segal, founder of Medical Justice, a company that works to deter frivolous medical malpractice lawsuits. “The biggest challenge will be whether the Republicans have to get eight Democratic senators to join the bill. To make it more palatable, something will need to give. Such provisions on tort reform are likely to be the first items offered for sacrifice.”
[email protected]
On Twitter @legal_med
New legislation approved by the House Judiciary Committee could mean legal relief for health providers in the form of capped damages and a tighter time frame for lawsuits.
The House Judiciary Committee passed the Protecting Access to Care Act of 2017 (H.R. 1215) on Feb. 28 by a vote of 18-17. The bill, modeled after California’s Medical Injury Compensation Reform Act (MICRA), would limit noneconomic damages in medical malpractice cases to $250,000, restrict contingency fees charged by attorneys, and enforce a 3-year statute of limitations for liability lawsuits from the date of alleged injury. The bill also includes a “fair share” rule in which defendants are liable only for the damages in direct proportion to their percentage of responsibility.
The bill is the first significant medical professional liability reform legislation to be approved by the committee since 2011, said Brian K. Atchinson, president and CEO of PIAA, a national trade association for medical liability insurers.
“Unlike previous federal bills, the bill is focused solely on health care professionals and entities, includes detailed flexibility for states for all its reforms, and is linked with the expenditure of federal dollars to address states’ rights concerns,” Mr. Atchinson said in a statement. “H.R. 1215 will help ensure fair and timely compensation to injured patients, improve access to patient care, and promote affordable and accessible medical liability insurance coverage.”
The proposed statute would apply to any patient who receives medical care provided via a federal program, such as Medicare or Medicaid, or via a subsidy or tax benefit, such as coverage purchased under the Affordable Care Act or a future* replacement. Medical care paid by employer health plans would fall under the legislation’s umbrella since insurance premiums receive federal tax exemptions. The bill would not preempt state medical malpractice laws that impose damage caps, whether higher or lower than $250,000, nor would the legislation affect the availability of economic damages, according to bill language.
As part of the H.R. 1215, courts could limit how much attorneys receive from a patient’s ultimate award. Specifically, courts would have the power to restrict payments from a plaintiff’s damage recovery to an attorney who claims a financial stake in the outcome by virtue of a contingent fee.
“The Protecting Access to Care Act will help keep the rising costs of health care from being passed along to the American people,” Rep. Goodlatte said in a statement. “The Congressional Budget Office estimates that the reforms contained in the bill would lower health care costs by tens of billions of dollars.”
Public Citizen, a consumer rights group, criticized the legislation as misleading to consumers and harmful to patients.
“Proposals to shield providers from liability are nothing but a giveaway to industry,” Lisa Gilbert, director of Public Citizen’s Congress Watch, said in a statement. “Members supporting this bill would further harm those who are suffering from doctors’ mistakes and abandon the GOP’s supposedly unwavering commitment to state’s rights.”
“There are so many moving parts to this bill, I think the likelihood of its being passed as is is low,” said Dr. Segal, founder of Medical Justice, a company that works to deter frivolous medical malpractice lawsuits. “The biggest challenge will be whether the Republicans have to get eight Democratic senators to join the bill. To make it more palatable, something will need to give. Such provisions on tort reform are likely to be the first items offered for sacrifice.”
[email protected]
On Twitter @legal_med
New legislation approved by the House Judiciary Committee could mean legal relief for health providers in the form of capped damages and a tighter time frame for lawsuits.
The House Judiciary Committee passed the Protecting Access to Care Act of 2017 (H.R. 1215) on Feb. 28 by a vote of 18-17. The bill, modeled after California’s Medical Injury Compensation Reform Act (MICRA), would limit noneconomic damages in medical malpractice cases to $250,000, restrict contingency fees charged by attorneys, and enforce a 3-year statute of limitations for liability lawsuits from the date of alleged injury. The bill also includes a “fair share” rule in which defendants are liable only for the damages in direct proportion to their percentage of responsibility.
The bill is the first significant medical professional liability reform legislation to be approved by the committee since 2011, said Brian K. Atchinson, president and CEO of PIAA, a national trade association for medical liability insurers.
“Unlike previous federal bills, the bill is focused solely on health care professionals and entities, includes detailed flexibility for states for all its reforms, and is linked with the expenditure of federal dollars to address states’ rights concerns,” Mr. Atchinson said in a statement. “H.R. 1215 will help ensure fair and timely compensation to injured patients, improve access to patient care, and promote affordable and accessible medical liability insurance coverage.”
The proposed statute would apply to any patient who receives medical care provided via a federal program, such as Medicare or Medicaid, or via a subsidy or tax benefit, such as coverage purchased under the Affordable Care Act or a future* replacement. Medical care paid by employer health plans would fall under the legislation’s umbrella since insurance premiums receive federal tax exemptions. The bill would not preempt state medical malpractice laws that impose damage caps, whether higher or lower than $250,000, nor would the legislation affect the availability of economic damages, according to bill language.
As part of the H.R. 1215, courts could limit how much attorneys receive from a patient’s ultimate award. Specifically, courts would have the power to restrict payments from a plaintiff’s damage recovery to an attorney who claims a financial stake in the outcome by virtue of a contingent fee.
“The Protecting Access to Care Act will help keep the rising costs of health care from being passed along to the American people,” Rep. Goodlatte said in a statement. “The Congressional Budget Office estimates that the reforms contained in the bill would lower health care costs by tens of billions of dollars.”
Public Citizen, a consumer rights group, criticized the legislation as misleading to consumers and harmful to patients.
“Proposals to shield providers from liability are nothing but a giveaway to industry,” Lisa Gilbert, director of Public Citizen’s Congress Watch, said in a statement. “Members supporting this bill would further harm those who are suffering from doctors’ mistakes and abandon the GOP’s supposedly unwavering commitment to state’s rights.”
“There are so many moving parts to this bill, I think the likelihood of its being passed as is is low,” said Dr. Segal, founder of Medical Justice, a company that works to deter frivolous medical malpractice lawsuits. “The biggest challenge will be whether the Republicans have to get eight Democratic senators to join the bill. To make it more palatable, something will need to give. Such provisions on tort reform are likely to be the first items offered for sacrifice.”
[email protected]
On Twitter @legal_med