User login
Expanded policy restricts health aid to countries that promote abortion
The U.S. State Department is moving forward with an expanded policy that restricts recipients of U.S. global health assistance from performing or promoting abortions.
In January, President Trump reinstated the “Mexico City Policy,” a policy that requires foreign nongovernmental organizations (NGOs) to certify they will not perform or actively promote abortion as a method of family planning using funds from any source as a condition for receiving U.S. global family planning assistance. The policy has been revoked and reinstated by presidential administrations along party lines for the last 32 years. However, President Trump’s order expands the definition of “global health assistance” to include funding for international health programs, such as HIV/AIDS, maternal and child health, malaria, global health security, family planning, and reproductive health care.
“All foreign NGOs will have the opportunity to receive global health assistance awards if they indicate their agreement to abide by the terms of Protecting Life in Global Health Assistance by accepting the provisions in their award,” the department stated. “Given the expansive nature of the new policy, the department will undertake a thorough and comprehensive review of the effectiveness and impact of the policy’s application over the next 6 months, which could include identifying implementation issues, and any other new information affecting implementation going forward.”
Nancy Northup, president and CEO for the Center for Reproductive Rights, called President Trump’s expansion of the “global gag rule” a major assault on those who serve the world’s poorest and most vulnerable women. “This policy does not protect life,” Ms. Northup said in a statement. “It jeopardizes the lives of countless women by withholding critical information and access to the full range of reproductive health care.”
But Rep. Chris Smith (R-N.J.), a supporter of the expanded policy, said it ensures that U.S. taxpayers will no longer subsidize foreign nongovernmental organizations that perform or promote abortion on demand. “This humane policy seeks to respect and protect the precious lives of unborn girls and boys from the violence of abortion,” Rep. Smith said in a statement. “The new policy doesn’t cut global health assistance by so much as a penny.”
[email protected]
On Twitter @legal_med
The U.S. State Department is moving forward with an expanded policy that restricts recipients of U.S. global health assistance from performing or promoting abortions.
In January, President Trump reinstated the “Mexico City Policy,” a policy that requires foreign nongovernmental organizations (NGOs) to certify they will not perform or actively promote abortion as a method of family planning using funds from any source as a condition for receiving U.S. global family planning assistance. The policy has been revoked and reinstated by presidential administrations along party lines for the last 32 years. However, President Trump’s order expands the definition of “global health assistance” to include funding for international health programs, such as HIV/AIDS, maternal and child health, malaria, global health security, family planning, and reproductive health care.
“All foreign NGOs will have the opportunity to receive global health assistance awards if they indicate their agreement to abide by the terms of Protecting Life in Global Health Assistance by accepting the provisions in their award,” the department stated. “Given the expansive nature of the new policy, the department will undertake a thorough and comprehensive review of the effectiveness and impact of the policy’s application over the next 6 months, which could include identifying implementation issues, and any other new information affecting implementation going forward.”
Nancy Northup, president and CEO for the Center for Reproductive Rights, called President Trump’s expansion of the “global gag rule” a major assault on those who serve the world’s poorest and most vulnerable women. “This policy does not protect life,” Ms. Northup said in a statement. “It jeopardizes the lives of countless women by withholding critical information and access to the full range of reproductive health care.”
But Rep. Chris Smith (R-N.J.), a supporter of the expanded policy, said it ensures that U.S. taxpayers will no longer subsidize foreign nongovernmental organizations that perform or promote abortion on demand. “This humane policy seeks to respect and protect the precious lives of unborn girls and boys from the violence of abortion,” Rep. Smith said in a statement. “The new policy doesn’t cut global health assistance by so much as a penny.”
[email protected]
On Twitter @legal_med
The U.S. State Department is moving forward with an expanded policy that restricts recipients of U.S. global health assistance from performing or promoting abortions.
In January, President Trump reinstated the “Mexico City Policy,” a policy that requires foreign nongovernmental organizations (NGOs) to certify they will not perform or actively promote abortion as a method of family planning using funds from any source as a condition for receiving U.S. global family planning assistance. The policy has been revoked and reinstated by presidential administrations along party lines for the last 32 years. However, President Trump’s order expands the definition of “global health assistance” to include funding for international health programs, such as HIV/AIDS, maternal and child health, malaria, global health security, family planning, and reproductive health care.
“All foreign NGOs will have the opportunity to receive global health assistance awards if they indicate their agreement to abide by the terms of Protecting Life in Global Health Assistance by accepting the provisions in their award,” the department stated. “Given the expansive nature of the new policy, the department will undertake a thorough and comprehensive review of the effectiveness and impact of the policy’s application over the next 6 months, which could include identifying implementation issues, and any other new information affecting implementation going forward.”
Nancy Northup, president and CEO for the Center for Reproductive Rights, called President Trump’s expansion of the “global gag rule” a major assault on those who serve the world’s poorest and most vulnerable women. “This policy does not protect life,” Ms. Northup said in a statement. “It jeopardizes the lives of countless women by withholding critical information and access to the full range of reproductive health care.”
But Rep. Chris Smith (R-N.J.), a supporter of the expanded policy, said it ensures that U.S. taxpayers will no longer subsidize foreign nongovernmental organizations that perform or promote abortion on demand. “This humane policy seeks to respect and protect the precious lives of unborn girls and boys from the violence of abortion,” Rep. Smith said in a statement. “The new policy doesn’t cut global health assistance by so much as a penny.”
[email protected]
On Twitter @legal_med
Five ways the AHCA may affect women’s health
Dramatic changes could be on the horizon for women’s health care should the controversial American Health Care Act of 2017 (AHCA) become law.
In May, the House of Representatives passed the AHCA, a bill that would replace many elements of the Affordable Care Act (ACA). The legislation is now being considered by the Senate, where it’s future is uncertain.
From contraceptive coverage to maternity care to abortion services, women have much at stake under the bill, said Kandice A. Kapinos, PhD, an economist who specializes in maternal health care at the nonpartisan RAND Corporation.
Here’s a look at the primary provisions of the AHCA and how they may impact women’s health.
1. Tax credits change
Under the ACA, individuals receive tax credits based on income, which means higher subsidies for patients who are lower income, older, and who live in areas with more expensive coverage. The AHCA would calculate tax credit assistance based primarily on age, and the bill would repeal the ACA’s cost-sharing protections for low-income individuals.
“How these credits are calculated [under the AHCA] will really affect lower-income women,” Dr. Kapinos said. “They will pay more under these calculations because their credits will be lowered. The other women who will be negatively affected by those changes will be women in rural or high-cost areas where care is on average more expensive.”
2. Essential health benefits waiver
The ACA required that marketplace plans and Medicaid expansion plans cover 10 benefit categories, including maternity care, preventive services, mental health, and hospitalizations and emergency care. Under the AHCA, states could apply for a waiver to define their own essential health benefits starting in 2020, leaving states free to exclude certain benefits such as maternity care or pregnancy-related services.
In addition, the AHCA would rescind the essential health benefit requirement for Medicaid expansion programs, meaning that patients in expansion plans would not be entitled to coverage for all 10 categories.
3. Medicaid changes
To reduce federal spending, the AHCA would shift the Medicaid program from an open-ended matching system to an annual fixed amount of federal funds. To this end, states would get to choose between a per capita cap funding approach or a block grant structure. Under a block grant, states would receive a fixed amount of funding for Medicaid that would increase by a specified amount each year. Under a per capita cap, federal funding would be capped based on the number of beneficiaries, or separate caps could be applied per Medicaid coverage groups such as children, adults, seniors, and disabled individuals.
Both capped approaches would limit a state’s ability to respond to rising costs, new and costly treatments, or public health emergencies such as Zika, according to a summary of the AHCA by the Kaiser Family Foundation. Women could get the short end of the stick if states decide to limit the number of women enrollees or if they limit certain benefits, Dr. Kapinos said. For instance, states could decide to cover only lower-cost contraception services, such as birth control pills, rather than more expensive methods such as an IUD, she said. A per capita cap approach would still require states to cover family planning services, but there would no longer be an enhanced federal matching rate for family planning services provided to most beneficiaries, the Kaiser summary notes. Under the block grant option, family planning services would no longer be a mandatory benefit for nondisabled women on Medicaid.
4. Preexisting conditions
The AHCA would retain the current ban on coverage denials for preexisting conditions. However, the bill would charge patients a penalty if they did not maintain continuous insurance coverage and then tried to regain insurance. These patients could pay higher premiums for 1 year or states could obtain a waiver that allows insurers to consider an individual’s health status for 1 year, enabling them to charge higher rates for prior health conditions.
“They could charge you more if you’re pregnant and you haven’t had insurance for more than 2 months,” Ms. Kapinos said. “They could only charge you a higher amount for 1 year and they can’t deny you coverage, but effectively what happens, the woman who’s pregnant would be sent to a higher-risk pool and be charged higher premiums. That could be a big deal for women, especially lower-income women.”
5. Planned Parenthood gets defunded
Although federal law already bans federal funds from paying for most abortions, the AHCA would stop Planned Parenthood from receiving federal Medicaid funding for 1 year. The AHCA would provide additional funds to other community health centers, but the bill does not require the health centers to use the money to provide women’s health services.
An AHCA analysis by the Congressional Budget Office found that withholding Medicaid payments to Planned Parenthood for 1 year would reduce access to care for women in some low-income communities and would result in thousands of unintended pregnancies that would ultimately be financed by Medicaid.
“That means a woman who’s covered by Medicaid and would go to Planned Parenthood to say, get a Pap smear, couldn’t go there and do that because they’re not going to let Medicaid reimburse Planned Parenthood,” Ms. Kapinos said. “That has real implications for access in areas where there aren’t a lot choices to get this kind of preventive care.”
[email protected]
On Twitter @legal_med
Dramatic changes could be on the horizon for women’s health care should the controversial American Health Care Act of 2017 (AHCA) become law.
In May, the House of Representatives passed the AHCA, a bill that would replace many elements of the Affordable Care Act (ACA). The legislation is now being considered by the Senate, where it’s future is uncertain.
From contraceptive coverage to maternity care to abortion services, women have much at stake under the bill, said Kandice A. Kapinos, PhD, an economist who specializes in maternal health care at the nonpartisan RAND Corporation.
Here’s a look at the primary provisions of the AHCA and how they may impact women’s health.
1. Tax credits change
Under the ACA, individuals receive tax credits based on income, which means higher subsidies for patients who are lower income, older, and who live in areas with more expensive coverage. The AHCA would calculate tax credit assistance based primarily on age, and the bill would repeal the ACA’s cost-sharing protections for low-income individuals.
“How these credits are calculated [under the AHCA] will really affect lower-income women,” Dr. Kapinos said. “They will pay more under these calculations because their credits will be lowered. The other women who will be negatively affected by those changes will be women in rural or high-cost areas where care is on average more expensive.”
2. Essential health benefits waiver
The ACA required that marketplace plans and Medicaid expansion plans cover 10 benefit categories, including maternity care, preventive services, mental health, and hospitalizations and emergency care. Under the AHCA, states could apply for a waiver to define their own essential health benefits starting in 2020, leaving states free to exclude certain benefits such as maternity care or pregnancy-related services.
In addition, the AHCA would rescind the essential health benefit requirement for Medicaid expansion programs, meaning that patients in expansion plans would not be entitled to coverage for all 10 categories.
3. Medicaid changes
To reduce federal spending, the AHCA would shift the Medicaid program from an open-ended matching system to an annual fixed amount of federal funds. To this end, states would get to choose between a per capita cap funding approach or a block grant structure. Under a block grant, states would receive a fixed amount of funding for Medicaid that would increase by a specified amount each year. Under a per capita cap, federal funding would be capped based on the number of beneficiaries, or separate caps could be applied per Medicaid coverage groups such as children, adults, seniors, and disabled individuals.
Both capped approaches would limit a state’s ability to respond to rising costs, new and costly treatments, or public health emergencies such as Zika, according to a summary of the AHCA by the Kaiser Family Foundation. Women could get the short end of the stick if states decide to limit the number of women enrollees or if they limit certain benefits, Dr. Kapinos said. For instance, states could decide to cover only lower-cost contraception services, such as birth control pills, rather than more expensive methods such as an IUD, she said. A per capita cap approach would still require states to cover family planning services, but there would no longer be an enhanced federal matching rate for family planning services provided to most beneficiaries, the Kaiser summary notes. Under the block grant option, family planning services would no longer be a mandatory benefit for nondisabled women on Medicaid.
4. Preexisting conditions
The AHCA would retain the current ban on coverage denials for preexisting conditions. However, the bill would charge patients a penalty if they did not maintain continuous insurance coverage and then tried to regain insurance. These patients could pay higher premiums for 1 year or states could obtain a waiver that allows insurers to consider an individual’s health status for 1 year, enabling them to charge higher rates for prior health conditions.
“They could charge you more if you’re pregnant and you haven’t had insurance for more than 2 months,” Ms. Kapinos said. “They could only charge you a higher amount for 1 year and they can’t deny you coverage, but effectively what happens, the woman who’s pregnant would be sent to a higher-risk pool and be charged higher premiums. That could be a big deal for women, especially lower-income women.”
5. Planned Parenthood gets defunded
Although federal law already bans federal funds from paying for most abortions, the AHCA would stop Planned Parenthood from receiving federal Medicaid funding for 1 year. The AHCA would provide additional funds to other community health centers, but the bill does not require the health centers to use the money to provide women’s health services.
An AHCA analysis by the Congressional Budget Office found that withholding Medicaid payments to Planned Parenthood for 1 year would reduce access to care for women in some low-income communities and would result in thousands of unintended pregnancies that would ultimately be financed by Medicaid.
“That means a woman who’s covered by Medicaid and would go to Planned Parenthood to say, get a Pap smear, couldn’t go there and do that because they’re not going to let Medicaid reimburse Planned Parenthood,” Ms. Kapinos said. “That has real implications for access in areas where there aren’t a lot choices to get this kind of preventive care.”
[email protected]
On Twitter @legal_med
Dramatic changes could be on the horizon for women’s health care should the controversial American Health Care Act of 2017 (AHCA) become law.
In May, the House of Representatives passed the AHCA, a bill that would replace many elements of the Affordable Care Act (ACA). The legislation is now being considered by the Senate, where it’s future is uncertain.
From contraceptive coverage to maternity care to abortion services, women have much at stake under the bill, said Kandice A. Kapinos, PhD, an economist who specializes in maternal health care at the nonpartisan RAND Corporation.
Here’s a look at the primary provisions of the AHCA and how they may impact women’s health.
1. Tax credits change
Under the ACA, individuals receive tax credits based on income, which means higher subsidies for patients who are lower income, older, and who live in areas with more expensive coverage. The AHCA would calculate tax credit assistance based primarily on age, and the bill would repeal the ACA’s cost-sharing protections for low-income individuals.
“How these credits are calculated [under the AHCA] will really affect lower-income women,” Dr. Kapinos said. “They will pay more under these calculations because their credits will be lowered. The other women who will be negatively affected by those changes will be women in rural or high-cost areas where care is on average more expensive.”
2. Essential health benefits waiver
The ACA required that marketplace plans and Medicaid expansion plans cover 10 benefit categories, including maternity care, preventive services, mental health, and hospitalizations and emergency care. Under the AHCA, states could apply for a waiver to define their own essential health benefits starting in 2020, leaving states free to exclude certain benefits such as maternity care or pregnancy-related services.
In addition, the AHCA would rescind the essential health benefit requirement for Medicaid expansion programs, meaning that patients in expansion plans would not be entitled to coverage for all 10 categories.
3. Medicaid changes
To reduce federal spending, the AHCA would shift the Medicaid program from an open-ended matching system to an annual fixed amount of federal funds. To this end, states would get to choose between a per capita cap funding approach or a block grant structure. Under a block grant, states would receive a fixed amount of funding for Medicaid that would increase by a specified amount each year. Under a per capita cap, federal funding would be capped based on the number of beneficiaries, or separate caps could be applied per Medicaid coverage groups such as children, adults, seniors, and disabled individuals.
Both capped approaches would limit a state’s ability to respond to rising costs, new and costly treatments, or public health emergencies such as Zika, according to a summary of the AHCA by the Kaiser Family Foundation. Women could get the short end of the stick if states decide to limit the number of women enrollees or if they limit certain benefits, Dr. Kapinos said. For instance, states could decide to cover only lower-cost contraception services, such as birth control pills, rather than more expensive methods such as an IUD, she said. A per capita cap approach would still require states to cover family planning services, but there would no longer be an enhanced federal matching rate for family planning services provided to most beneficiaries, the Kaiser summary notes. Under the block grant option, family planning services would no longer be a mandatory benefit for nondisabled women on Medicaid.
4. Preexisting conditions
The AHCA would retain the current ban on coverage denials for preexisting conditions. However, the bill would charge patients a penalty if they did not maintain continuous insurance coverage and then tried to regain insurance. These patients could pay higher premiums for 1 year or states could obtain a waiver that allows insurers to consider an individual’s health status for 1 year, enabling them to charge higher rates for prior health conditions.
“They could charge you more if you’re pregnant and you haven’t had insurance for more than 2 months,” Ms. Kapinos said. “They could only charge you a higher amount for 1 year and they can’t deny you coverage, but effectively what happens, the woman who’s pregnant would be sent to a higher-risk pool and be charged higher premiums. That could be a big deal for women, especially lower-income women.”
5. Planned Parenthood gets defunded
Although federal law already bans federal funds from paying for most abortions, the AHCA would stop Planned Parenthood from receiving federal Medicaid funding for 1 year. The AHCA would provide additional funds to other community health centers, but the bill does not require the health centers to use the money to provide women’s health services.
An AHCA analysis by the Congressional Budget Office found that withholding Medicaid payments to Planned Parenthood for 1 year would reduce access to care for women in some low-income communities and would result in thousands of unintended pregnancies that would ultimately be financed by Medicaid.
“That means a woman who’s covered by Medicaid and would go to Planned Parenthood to say, get a Pap smear, couldn’t go there and do that because they’re not going to let Medicaid reimburse Planned Parenthood,” Ms. Kapinos said. “That has real implications for access in areas where there aren’t a lot choices to get this kind of preventive care.”
[email protected]
On Twitter @legal_med
VIDEO: Sutureless aortic valve shows promise in IDE trial
BOSTON – A new study highlights the success, safety, and effectiveness of a new sutureless aortic valve device in patients with severe symptomatic aortic valve stenosis (AS).
The findings, reported at the annual meeting of the American Association for Thoracic Surgery, were based on a prospective, single-arm clinical trial approved under a Food and Drug Administration Investigational Device Exemption (IDE) that aimed to assess the safety and efficacy of a new bovine pericardial sutureless aortic valve in patients with severe AS undergoing aortic valve replacement with or without concomitant procedures. In this video interview, Michael Borger, MD, explains how the study was conducted and what the findings mean for future use of the sutureless aortic valve device.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – A new study highlights the success, safety, and effectiveness of a new sutureless aortic valve device in patients with severe symptomatic aortic valve stenosis (AS).
The findings, reported at the annual meeting of the American Association for Thoracic Surgery, were based on a prospective, single-arm clinical trial approved under a Food and Drug Administration Investigational Device Exemption (IDE) that aimed to assess the safety and efficacy of a new bovine pericardial sutureless aortic valve in patients with severe AS undergoing aortic valve replacement with or without concomitant procedures. In this video interview, Michael Borger, MD, explains how the study was conducted and what the findings mean for future use of the sutureless aortic valve device.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – A new study highlights the success, safety, and effectiveness of a new sutureless aortic valve device in patients with severe symptomatic aortic valve stenosis (AS).
The findings, reported at the annual meeting of the American Association for Thoracic Surgery, were based on a prospective, single-arm clinical trial approved under a Food and Drug Administration Investigational Device Exemption (IDE) that aimed to assess the safety and efficacy of a new bovine pericardial sutureless aortic valve in patients with severe AS undergoing aortic valve replacement with or without concomitant procedures. In this video interview, Michael Borger, MD, explains how the study was conducted and what the findings mean for future use of the sutureless aortic valve device.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
AT THE AATS ANNUAL MEETING
VIDEO: Incoming AATS president outlines goals
BOSTON – Strengthening member engagement is a top goal for incoming AATS President Duke E. Cameron, MD.
In this video, Dr. Cameron, of Massachusetts General Hospital, Boston, shared his objectives as the next AATS leader and the direction he envisions for the specialty over the next 100 years. Dr. Cameron also discussed his hope for new online educational efforts and the importance of physician collaboration with other health professionals.
On Twitter @legal_med
BOSTON – Strengthening member engagement is a top goal for incoming AATS President Duke E. Cameron, MD.
In this video, Dr. Cameron, of Massachusetts General Hospital, Boston, shared his objectives as the next AATS leader and the direction he envisions for the specialty over the next 100 years. Dr. Cameron also discussed his hope for new online educational efforts and the importance of physician collaboration with other health professionals.
On Twitter @legal_med
BOSTON – Strengthening member engagement is a top goal for incoming AATS President Duke E. Cameron, MD.
In this video, Dr. Cameron, of Massachusetts General Hospital, Boston, shared his objectives as the next AATS leader and the direction he envisions for the specialty over the next 100 years. Dr. Cameron also discussed his hope for new online educational efforts and the importance of physician collaboration with other health professionals.
On Twitter @legal_med
AT THE AATS ANNUAL MEETING
Executive order aims to reform specialized visa program
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
VIDEO: Surgery use declines for non–small cell lung cancer
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
AT THE AATS ANNUAL MEETING
Parents rate telepediatric experience as better than office visits
Three-quarters of parents who have used telemedicine services for their children say the experience was better than an in-person office visit, according to a new study.
The analysis, released April 23, 2017, by Nemours Children’s Health System operating in five states, surveyed 500 child caregivers between February 15 and 20 about their awareness and usage of telemedicine services for their children aged 17 years and younger (mean age 10 years). Of caregivers surveyed, 15% had tried telemedicine services for their children, while another 61% reported they plan to use telemedicine in the next year for their children’s medical care, according to the study. Eight percent of caregivers did not plan to use telemedicine, and 31% of those surveyed were unsure.
Of child caregivers who have used telemedicine, 75% of reported their telemedicine experience was better than an in-person visit, according to the survey. Convenience, after-hours accessibility, and immediacy were the top three reasons caregivers sought an online visit for their child. Compared with a similar survey conducted by Nemours in 2014, parents’ use of telemedicine for their children has grown by 125% and awareness of the practice has increased by 88%, the study found.
The overall takeaway is that parents are using telemedicine because of its ease and accessibility and they’re having satisfactory experiences with the technology, said Shayan Vyas, MD, a pediatrician based in Nemours’ Orlando location and director of telemedicine for Nemours Children’s Hospital.
“Parents are citing telemedicine because of convenience and that’s true for other industries that have gone mobile,” Dr. Vyas said in an interview. “We no longer hail a cab at the intersection, we use our smartphones. We now use Amazon and other companies to order diapers and other everyday items. ... More and more, patients are driving telemedicine more than the systems or the providers.”
Caregivers surveyed said they are most willing to use telehealth services for cold and flu (58%), pink eye (51%), and rashes (48%) as well as well-child visits (41%). However, parents and caregivers were hesitant to use telemedicine for chronic conditions and reported they would likely never consider telehealth services for diabetes (53%), asthma (43%), ear pain (37%), and ADHD (36%).
The findings are expected because there are limitations for providers when it comes to treating some conditions and chronic diseases with telemedicine, Dr. Vyas said. He also stressed that telemedicine should not be used to replace the medical home for children.
“We’re working really hard to ensure there’s great pediatric care online and that the medical home stays intact,” he said. “We don’t want telemedicine to become the wild wild west of retail clinics where children are getting care from providers they don’t know or who are not in touch with their primary care world.”
Nemours has incorporated telemedicine throughout its health system with direct-to-consumer care for acute, chronic, and postsurgical appointments. The telehealth program, called Nemours CareConnect, is a 24/7, on-demand pediatric service that provides access to Nemours pediatricians through smartphones, tablets, or computers. In addition, Nemours CareConnect is used to bring pediatric specialists into affiliated community hospitals.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Dr. Vyas said. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way health care is delivered.”
[email protected]
On Twitter @legal_med
Three-quarters of parents who have used telemedicine services for their children say the experience was better than an in-person office visit, according to a new study.
The analysis, released April 23, 2017, by Nemours Children’s Health System operating in five states, surveyed 500 child caregivers between February 15 and 20 about their awareness and usage of telemedicine services for their children aged 17 years and younger (mean age 10 years). Of caregivers surveyed, 15% had tried telemedicine services for their children, while another 61% reported they plan to use telemedicine in the next year for their children’s medical care, according to the study. Eight percent of caregivers did not plan to use telemedicine, and 31% of those surveyed were unsure.
Of child caregivers who have used telemedicine, 75% of reported their telemedicine experience was better than an in-person visit, according to the survey. Convenience, after-hours accessibility, and immediacy were the top three reasons caregivers sought an online visit for their child. Compared with a similar survey conducted by Nemours in 2014, parents’ use of telemedicine for their children has grown by 125% and awareness of the practice has increased by 88%, the study found.
The overall takeaway is that parents are using telemedicine because of its ease and accessibility and they’re having satisfactory experiences with the technology, said Shayan Vyas, MD, a pediatrician based in Nemours’ Orlando location and director of telemedicine for Nemours Children’s Hospital.
“Parents are citing telemedicine because of convenience and that’s true for other industries that have gone mobile,” Dr. Vyas said in an interview. “We no longer hail a cab at the intersection, we use our smartphones. We now use Amazon and other companies to order diapers and other everyday items. ... More and more, patients are driving telemedicine more than the systems or the providers.”
Caregivers surveyed said they are most willing to use telehealth services for cold and flu (58%), pink eye (51%), and rashes (48%) as well as well-child visits (41%). However, parents and caregivers were hesitant to use telemedicine for chronic conditions and reported they would likely never consider telehealth services for diabetes (53%), asthma (43%), ear pain (37%), and ADHD (36%).
The findings are expected because there are limitations for providers when it comes to treating some conditions and chronic diseases with telemedicine, Dr. Vyas said. He also stressed that telemedicine should not be used to replace the medical home for children.
“We’re working really hard to ensure there’s great pediatric care online and that the medical home stays intact,” he said. “We don’t want telemedicine to become the wild wild west of retail clinics where children are getting care from providers they don’t know or who are not in touch with their primary care world.”
Nemours has incorporated telemedicine throughout its health system with direct-to-consumer care for acute, chronic, and postsurgical appointments. The telehealth program, called Nemours CareConnect, is a 24/7, on-demand pediatric service that provides access to Nemours pediatricians through smartphones, tablets, or computers. In addition, Nemours CareConnect is used to bring pediatric specialists into affiliated community hospitals.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Dr. Vyas said. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way health care is delivered.”
[email protected]
On Twitter @legal_med
Three-quarters of parents who have used telemedicine services for their children say the experience was better than an in-person office visit, according to a new study.
The analysis, released April 23, 2017, by Nemours Children’s Health System operating in five states, surveyed 500 child caregivers between February 15 and 20 about their awareness and usage of telemedicine services for their children aged 17 years and younger (mean age 10 years). Of caregivers surveyed, 15% had tried telemedicine services for their children, while another 61% reported they plan to use telemedicine in the next year for their children’s medical care, according to the study. Eight percent of caregivers did not plan to use telemedicine, and 31% of those surveyed were unsure.
Of child caregivers who have used telemedicine, 75% of reported their telemedicine experience was better than an in-person visit, according to the survey. Convenience, after-hours accessibility, and immediacy were the top three reasons caregivers sought an online visit for their child. Compared with a similar survey conducted by Nemours in 2014, parents’ use of telemedicine for their children has grown by 125% and awareness of the practice has increased by 88%, the study found.
The overall takeaway is that parents are using telemedicine because of its ease and accessibility and they’re having satisfactory experiences with the technology, said Shayan Vyas, MD, a pediatrician based in Nemours’ Orlando location and director of telemedicine for Nemours Children’s Hospital.
“Parents are citing telemedicine because of convenience and that’s true for other industries that have gone mobile,” Dr. Vyas said in an interview. “We no longer hail a cab at the intersection, we use our smartphones. We now use Amazon and other companies to order diapers and other everyday items. ... More and more, patients are driving telemedicine more than the systems or the providers.”
Caregivers surveyed said they are most willing to use telehealth services for cold and flu (58%), pink eye (51%), and rashes (48%) as well as well-child visits (41%). However, parents and caregivers were hesitant to use telemedicine for chronic conditions and reported they would likely never consider telehealth services for diabetes (53%), asthma (43%), ear pain (37%), and ADHD (36%).
The findings are expected because there are limitations for providers when it comes to treating some conditions and chronic diseases with telemedicine, Dr. Vyas said. He also stressed that telemedicine should not be used to replace the medical home for children.
“We’re working really hard to ensure there’s great pediatric care online and that the medical home stays intact,” he said. “We don’t want telemedicine to become the wild wild west of retail clinics where children are getting care from providers they don’t know or who are not in touch with their primary care world.”
Nemours has incorporated telemedicine throughout its health system with direct-to-consumer care for acute, chronic, and postsurgical appointments. The telehealth program, called Nemours CareConnect, is a 24/7, on-demand pediatric service that provides access to Nemours pediatricians through smartphones, tablets, or computers. In addition, Nemours CareConnect is used to bring pediatric specialists into affiliated community hospitals.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Dr. Vyas said. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way health care is delivered.”
[email protected]
On Twitter @legal_med
States consider abortion ‘reversal’ bills
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Malpractice: Paid claims down, but average payment up
The rate of paid legal claims against physicians dropped by more than half between 1992 and 2014, but the average claim payment amount rose, according to an analysis of the National Practitioner Data Bank.
Adam C. Schaffer, MD, of Brigham and Women’s Hospital, Boston, and his colleagues examined paid claims from the National Practitioner Data Bank from Jan. 1, 1992, to Dec. 31, 2014, accounting for specialty. Dollar amounts were inflation-adjusted to 2014 dollars using the Consumer Price Index.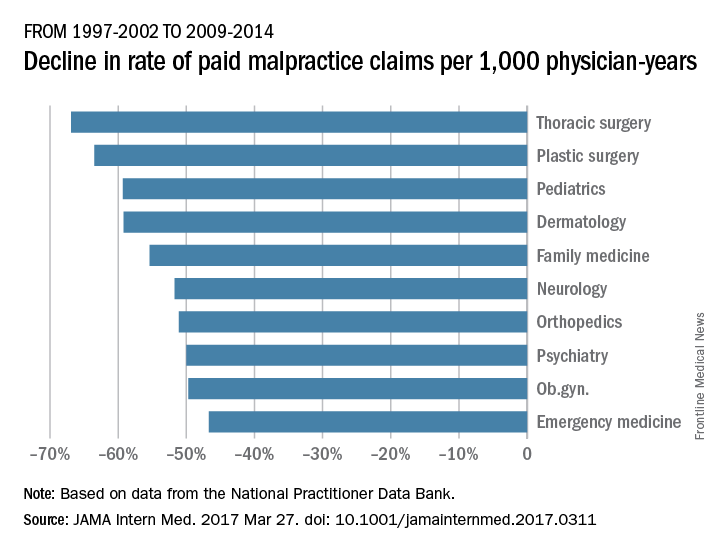
From 1992-1996 to 2009-2014, the rate of paid claims decreased by 56%, ranging from a 76% decrease in pediatrics to a 14% rate decrease in cardiology. The mean payment increased by 23% from $286,751 to $353,473 between 1992-1996 and 2009-2014. The increases ranged from $17,431 in general practice to $138,708 in pathology (JAMA Intern Med. 2017 Mar 27. doi: 10.1001/jamainternmed.2017.0311).
The most common allegation was diagnostic error, followed by surgical error and medication or treatment error. The proportion of paid claims attributable to diagnostic error varied widely and was highest in pathology and radiology. Plastic surgery had the highest percentage of paid claims related to surgical errors. Specialties with the highest percentage of paid claims related to medication/treatment errors were psychiatry, general practice, and pulmonology.
While prior data have shown the overall trend of declining paid malpractice claims and increasing average payments, this study is the first to examine such trends by medical specialty, said Dr. Schaffer.
“We think it is important to try to understand the reasons for the variation among specialties in characteristics of paid malpractice claims, as understanding the reasons for this variation may provide insights about how we can provide the safest care possible,” he said in an interview.
Dr. Schaffer said that he hopes the findings make physicians more aware of the malpractice landscape and aid their future practice decisions.
“Medical malpractice is an issue that concerns many physicians, and physicians’ perceptions of their liability risk can influence the decisions they make in caring for their patients,” he said. “By performing an analysis of a national database of paid medical malpractice claims broken down by specialty, we hope to provide physicians with data that give them an accurate picture of the medical malpractice environment in which they are practicing.”
[email protected]
On Twitter @legal_med
The rate of paid legal claims against physicians dropped by more than half between 1992 and 2014, but the average claim payment amount rose, according to an analysis of the National Practitioner Data Bank.
Adam C. Schaffer, MD, of Brigham and Women’s Hospital, Boston, and his colleagues examined paid claims from the National Practitioner Data Bank from Jan. 1, 1992, to Dec. 31, 2014, accounting for specialty. Dollar amounts were inflation-adjusted to 2014 dollars using the Consumer Price Index.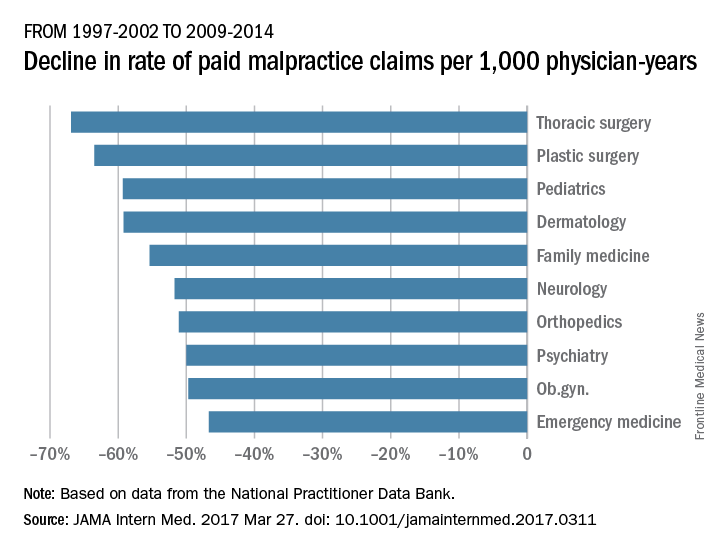
From 1992-1996 to 2009-2014, the rate of paid claims decreased by 56%, ranging from a 76% decrease in pediatrics to a 14% rate decrease in cardiology. The mean payment increased by 23% from $286,751 to $353,473 between 1992-1996 and 2009-2014. The increases ranged from $17,431 in general practice to $138,708 in pathology (JAMA Intern Med. 2017 Mar 27. doi: 10.1001/jamainternmed.2017.0311).
The most common allegation was diagnostic error, followed by surgical error and medication or treatment error. The proportion of paid claims attributable to diagnostic error varied widely and was highest in pathology and radiology. Plastic surgery had the highest percentage of paid claims related to surgical errors. Specialties with the highest percentage of paid claims related to medication/treatment errors were psychiatry, general practice, and pulmonology.
While prior data have shown the overall trend of declining paid malpractice claims and increasing average payments, this study is the first to examine such trends by medical specialty, said Dr. Schaffer.
“We think it is important to try to understand the reasons for the variation among specialties in characteristics of paid malpractice claims, as understanding the reasons for this variation may provide insights about how we can provide the safest care possible,” he said in an interview.
Dr. Schaffer said that he hopes the findings make physicians more aware of the malpractice landscape and aid their future practice decisions.
“Medical malpractice is an issue that concerns many physicians, and physicians’ perceptions of their liability risk can influence the decisions they make in caring for their patients,” he said. “By performing an analysis of a national database of paid medical malpractice claims broken down by specialty, we hope to provide physicians with data that give them an accurate picture of the medical malpractice environment in which they are practicing.”
[email protected]
On Twitter @legal_med
The rate of paid legal claims against physicians dropped by more than half between 1992 and 2014, but the average claim payment amount rose, according to an analysis of the National Practitioner Data Bank.
Adam C. Schaffer, MD, of Brigham and Women’s Hospital, Boston, and his colleagues examined paid claims from the National Practitioner Data Bank from Jan. 1, 1992, to Dec. 31, 2014, accounting for specialty. Dollar amounts were inflation-adjusted to 2014 dollars using the Consumer Price Index.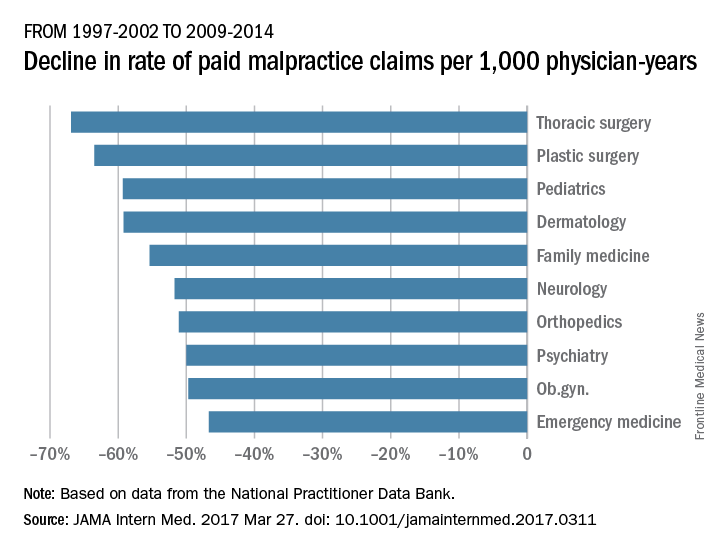
From 1992-1996 to 2009-2014, the rate of paid claims decreased by 56%, ranging from a 76% decrease in pediatrics to a 14% rate decrease in cardiology. The mean payment increased by 23% from $286,751 to $353,473 between 1992-1996 and 2009-2014. The increases ranged from $17,431 in general practice to $138,708 in pathology (JAMA Intern Med. 2017 Mar 27. doi: 10.1001/jamainternmed.2017.0311).
The most common allegation was diagnostic error, followed by surgical error and medication or treatment error. The proportion of paid claims attributable to diagnostic error varied widely and was highest in pathology and radiology. Plastic surgery had the highest percentage of paid claims related to surgical errors. Specialties with the highest percentage of paid claims related to medication/treatment errors were psychiatry, general practice, and pulmonology.
While prior data have shown the overall trend of declining paid malpractice claims and increasing average payments, this study is the first to examine such trends by medical specialty, said Dr. Schaffer.
“We think it is important to try to understand the reasons for the variation among specialties in characteristics of paid malpractice claims, as understanding the reasons for this variation may provide insights about how we can provide the safest care possible,” he said in an interview.
Dr. Schaffer said that he hopes the findings make physicians more aware of the malpractice landscape and aid their future practice decisions.
“Medical malpractice is an issue that concerns many physicians, and physicians’ perceptions of their liability risk can influence the decisions they make in caring for their patients,” he said. “By performing an analysis of a national database of paid medical malpractice claims broken down by specialty, we hope to provide physicians with data that give them an accurate picture of the medical malpractice environment in which they are practicing.”
[email protected]
On Twitter @legal_med
FROM JAMA INTERNAL MEDICINE
Trump overturns Title X family planning rule
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med
President Donald Trump has signed a resolution that could strip public funding from U.S. clinics that provide abortions, including Planned Parenthood.
The April 13 action overturns a rule imposed by the Obama administration regarding how states can distribute Title X funds, money that assists low-income patients in accessing family planning and preventive health services. The Obama administration’s rule had reinforced existing law that states cannot withhold Title X funding from medical providers for reasons other than poor performance or noncompliance. In recent years, states have begun restricting participation by certain types of providers in the Title X program, such as those that provide abortions.
“Our federal system was set up to allow states to address the unique needs of their own populations when possible, especially [when it] comes to programs as important and sensitive as family planning,” Mr. Spicer said. “With the bill signing, the president has restored respect to states’ rights on this particular issue.”
The Planned Parenthood Federation of America condemned President Trump’s measure, calling it an effort to undermine women’s health and overturn a rule that reinforced protections for millions of patients who rely on Title X for health care.
“Four million people depend on the Title X family planning program, and by signing this bill, President Trump disregards their health and well-being,” Dawn Laguens, executive vice president of the Planned Parenthood Federation of America said in a statement. “We should build on the tremendous progress made in this country with expanded access to birth control, instead of enacting policies that take us backward. Too many women still face barriers to health care, especially young women, women of color, those who live in rural areas, and women with low incomes.”
Since 2011, 13 states have restricted participation in the Title X program based on reasons other than the providers’ ability to provide the services, according to a summary of the 2016 rule. For example, Texas in 2011 reduced its contribution to family planning services, and also restructured Title X funds using a tiered approach. The combination of these actions decreased the Title X provider network in Texas from 48 to 36 providers and reduced the number of patients served from 259,606 in 2011 to 166,538 in 2015.
By statute, Title X funds cannot be used for abortions. Title X provides family planning and related reproductive health services such as testing and counseling for sexually transmitted diseases, contraceptive methods including method-specific counseling, breast and cervical cancer screening, and pregnancy tests and counseling.
The Susan B. Anthony List, an antiabortion organization, praised President Trump’s resolution and said it’s another step toward defunding Planned Parenthood and keeping taxpayer dollars away from abortion businesses.
“Prioritizing funding away from Planned Parenthood to comprehensive health care alternatives is a winning issue,” Susan B. Anthony List president, Marjorie Dannenfelser, said in a statement. “We expect to see Congress continue its efforts to redirect additional taxpayer funding away from Planned Parenthood through pro-life health care reform after the spring recess.”
[email protected]
On Twitter @legal_med