User login
Sofosbuvir and ribavirin combo reduced HCV recurrence post transplant
WASHINGTON – The use of the experimental drug sofosbuvir in combination with ribavirin successfully reduced hepatitis C virus infection recurrence in 77% of posttransplant patients 4 weeks after treatment ended, based on the initial results of an ongoing large, prospective multicenter study.
HCV recurrence is the most common cause of mortality and graft loss following transplantation, and 10%-50% of those with a recurrent infection progress to cirrhosis within 5 years, Dr. Michael R. Charlton, professor of medicine at the Mayo Clinic, Rochester, Minn., said at the annual meeting of the American Association for the Study of Liver Diseases.
Sofosbuvir, manufactured by Gilead Sciences, is a nucleotide analogue inhibitor of the NS5B polymerase enzyme, which plays an important role in HCV replication. The compound is active against HCV genotypes 1 (the most common genotype in the United States), 2, 3, 4, 5, and 6.
There are no approved treatments currently in the United States to prevent posttransplant HCV recurrence.
Dr. Charlton reported results for 40 patients in an ongoing open-label interferon-free study. Their mean age was 59 years, with a range of 49-75 years; 78% were male, 85% were white, 8% were black, and 3% were Hispanic. Thirty-five patients (88%) had been previously treated, with 9 of the 40 having been previously treated with protease inhibitors. The study enrollees had a mean baseline HCV RNA of 6.55 log10 IU/mL. Sixteen patients (40%) had cirrhosis. The predominant genotype was 1a, found in 22 patients (55%); 11 had genotype 1b, 6 had genotype 3, and 1 had genotype 4.
In the study, posttransplant patients with recurrent HCV infection of any genotype were included. The transplant had to have occurred between 6 and 150 months prior to enrollment. Patients had to have an absence of rejection and were excluded if they took more than 5 mg of prednisone daily. Study participants were given up to 24 weeks of sofosbuvir in a daily dose of 400 mg and ribavirin starting at 400 mg daily. The ribavirin dose was increased up to 1,200 mg daily, depending on the patient’s hemoglobin levels.
At week 4 of the study, all 40 patients were HCV RNA negative. At the end of treatment, 39 of the patients who were still in the trial were HCV negative. Four weeks post treatment, 27 of 35 were negative.
Of the nine patients who relapsed post treatment, eight were male, five were genotype 1a, three were genotype 1b, and one was genotype 4. Eight of the nine had prior treatment. And five had bridging fibrosis or cirrhosis.
There were no episodes of rejection, and there were no interactions that required adjustment of immunosuppressive therapy.
The most common side effects were fatigue, arthralgia, headache, and diarrhea. Six patients had a serious adverse event. Two patients withdrew as a result of a serious adverse event, but the events were not related to sofosbuvir, said Dr. Charlton.
In late October, the Food and Drug Administration’s Antiviral Drugs Advisory Committee unanimously recommended the approval of sofosbuvir for two indications: in combination with pegylated interferon and ribavirin, for treatment-naive adults with genotype 1 and 4 infections and in combination with ribavirin, for adults with genotype 2 and 3 infections.
If approved, as is expected, the second indication will mark the first approval of a treatment for chronic hepatitis C with an interferon-free regimen, and it will be the first drug in its class to be approved. The FDA is expected to make a decision by Dec. 8. Sofosbuvir also is under review in the European Union, Australia, Canada, New Zealand, Switzerland, and Turkey, according to Gilead.
Dr. Charlton disclosed that he has received research support and consulting fees from a variety of companies, including AbbeVie, Biotest, Bristol Myers-Squibb, Gilead, Novartis, and Vertex.
The study was funded by Gilead Sciences.
On Twitter @aliciaault
WASHINGTON – The use of the experimental drug sofosbuvir in combination with ribavirin successfully reduced hepatitis C virus infection recurrence in 77% of posttransplant patients 4 weeks after treatment ended, based on the initial results of an ongoing large, prospective multicenter study.
HCV recurrence is the most common cause of mortality and graft loss following transplantation, and 10%-50% of those with a recurrent infection progress to cirrhosis within 5 years, Dr. Michael R. Charlton, professor of medicine at the Mayo Clinic, Rochester, Minn., said at the annual meeting of the American Association for the Study of Liver Diseases.
Sofosbuvir, manufactured by Gilead Sciences, is a nucleotide analogue inhibitor of the NS5B polymerase enzyme, which plays an important role in HCV replication. The compound is active against HCV genotypes 1 (the most common genotype in the United States), 2, 3, 4, 5, and 6.
There are no approved treatments currently in the United States to prevent posttransplant HCV recurrence.
Dr. Charlton reported results for 40 patients in an ongoing open-label interferon-free study. Their mean age was 59 years, with a range of 49-75 years; 78% were male, 85% were white, 8% were black, and 3% were Hispanic. Thirty-five patients (88%) had been previously treated, with 9 of the 40 having been previously treated with protease inhibitors. The study enrollees had a mean baseline HCV RNA of 6.55 log10 IU/mL. Sixteen patients (40%) had cirrhosis. The predominant genotype was 1a, found in 22 patients (55%); 11 had genotype 1b, 6 had genotype 3, and 1 had genotype 4.
In the study, posttransplant patients with recurrent HCV infection of any genotype were included. The transplant had to have occurred between 6 and 150 months prior to enrollment. Patients had to have an absence of rejection and were excluded if they took more than 5 mg of prednisone daily. Study participants were given up to 24 weeks of sofosbuvir in a daily dose of 400 mg and ribavirin starting at 400 mg daily. The ribavirin dose was increased up to 1,200 mg daily, depending on the patient’s hemoglobin levels.
At week 4 of the study, all 40 patients were HCV RNA negative. At the end of treatment, 39 of the patients who were still in the trial were HCV negative. Four weeks post treatment, 27 of 35 were negative.
Of the nine patients who relapsed post treatment, eight were male, five were genotype 1a, three were genotype 1b, and one was genotype 4. Eight of the nine had prior treatment. And five had bridging fibrosis or cirrhosis.
There were no episodes of rejection, and there were no interactions that required adjustment of immunosuppressive therapy.
The most common side effects were fatigue, arthralgia, headache, and diarrhea. Six patients had a serious adverse event. Two patients withdrew as a result of a serious adverse event, but the events were not related to sofosbuvir, said Dr. Charlton.
In late October, the Food and Drug Administration’s Antiviral Drugs Advisory Committee unanimously recommended the approval of sofosbuvir for two indications: in combination with pegylated interferon and ribavirin, for treatment-naive adults with genotype 1 and 4 infections and in combination with ribavirin, for adults with genotype 2 and 3 infections.
If approved, as is expected, the second indication will mark the first approval of a treatment for chronic hepatitis C with an interferon-free regimen, and it will be the first drug in its class to be approved. The FDA is expected to make a decision by Dec. 8. Sofosbuvir also is under review in the European Union, Australia, Canada, New Zealand, Switzerland, and Turkey, according to Gilead.
Dr. Charlton disclosed that he has received research support and consulting fees from a variety of companies, including AbbeVie, Biotest, Bristol Myers-Squibb, Gilead, Novartis, and Vertex.
The study was funded by Gilead Sciences.
On Twitter @aliciaault
WASHINGTON – The use of the experimental drug sofosbuvir in combination with ribavirin successfully reduced hepatitis C virus infection recurrence in 77% of posttransplant patients 4 weeks after treatment ended, based on the initial results of an ongoing large, prospective multicenter study.
HCV recurrence is the most common cause of mortality and graft loss following transplantation, and 10%-50% of those with a recurrent infection progress to cirrhosis within 5 years, Dr. Michael R. Charlton, professor of medicine at the Mayo Clinic, Rochester, Minn., said at the annual meeting of the American Association for the Study of Liver Diseases.
Sofosbuvir, manufactured by Gilead Sciences, is a nucleotide analogue inhibitor of the NS5B polymerase enzyme, which plays an important role in HCV replication. The compound is active against HCV genotypes 1 (the most common genotype in the United States), 2, 3, 4, 5, and 6.
There are no approved treatments currently in the United States to prevent posttransplant HCV recurrence.
Dr. Charlton reported results for 40 patients in an ongoing open-label interferon-free study. Their mean age was 59 years, with a range of 49-75 years; 78% were male, 85% were white, 8% were black, and 3% were Hispanic. Thirty-five patients (88%) had been previously treated, with 9 of the 40 having been previously treated with protease inhibitors. The study enrollees had a mean baseline HCV RNA of 6.55 log10 IU/mL. Sixteen patients (40%) had cirrhosis. The predominant genotype was 1a, found in 22 patients (55%); 11 had genotype 1b, 6 had genotype 3, and 1 had genotype 4.
In the study, posttransplant patients with recurrent HCV infection of any genotype were included. The transplant had to have occurred between 6 and 150 months prior to enrollment. Patients had to have an absence of rejection and were excluded if they took more than 5 mg of prednisone daily. Study participants were given up to 24 weeks of sofosbuvir in a daily dose of 400 mg and ribavirin starting at 400 mg daily. The ribavirin dose was increased up to 1,200 mg daily, depending on the patient’s hemoglobin levels.
At week 4 of the study, all 40 patients were HCV RNA negative. At the end of treatment, 39 of the patients who were still in the trial were HCV negative. Four weeks post treatment, 27 of 35 were negative.
Of the nine patients who relapsed post treatment, eight were male, five were genotype 1a, three were genotype 1b, and one was genotype 4. Eight of the nine had prior treatment. And five had bridging fibrosis or cirrhosis.
There were no episodes of rejection, and there were no interactions that required adjustment of immunosuppressive therapy.
The most common side effects were fatigue, arthralgia, headache, and diarrhea. Six patients had a serious adverse event. Two patients withdrew as a result of a serious adverse event, but the events were not related to sofosbuvir, said Dr. Charlton.
In late October, the Food and Drug Administration’s Antiviral Drugs Advisory Committee unanimously recommended the approval of sofosbuvir for two indications: in combination with pegylated interferon and ribavirin, for treatment-naive adults with genotype 1 and 4 infections and in combination with ribavirin, for adults with genotype 2 and 3 infections.
If approved, as is expected, the second indication will mark the first approval of a treatment for chronic hepatitis C with an interferon-free regimen, and it will be the first drug in its class to be approved. The FDA is expected to make a decision by Dec. 8. Sofosbuvir also is under review in the European Union, Australia, Canada, New Zealand, Switzerland, and Turkey, according to Gilead.
Dr. Charlton disclosed that he has received research support and consulting fees from a variety of companies, including AbbeVie, Biotest, Bristol Myers-Squibb, Gilead, Novartis, and Vertex.
The study was funded by Gilead Sciences.
On Twitter @aliciaault
FROM THE LIVER MEETING 2013
Major finding: A combination of sofosbuvir with ribavirin reduced hepatitis C recurrence in 77% of 40 posttransplant patients 4 weeks after treatment ended.
Data source: Preliminary results of a prospective, multicenter, open-label single-arm study.
Disclosures: Gilead Sciences funded the study. Dr. Charlton disclosed that he has received research support and consulting fees from a variety of companies, including AbbeVie, Biotest, Bristol Myers-Squibb, Gilead, Novartis, and Vertex.
ECHO Model Cost-effective for HCV
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
AT THE LIVER MEETING 2013
ECHO model cost-effective for HCV
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
WASHINGTON – Using the ECHO model of primary care to treat hepatitis C is cost saving in 35% of patients and very cost effective overall, according to a retrospective analysis presented by Dr. John B. Wong, at the annual meeting of the American Association for the Study of Liver Diseases.
Project ECHO (Extension for Community Healthcare Outcomes) was begun at the University of New Mexico, Albuquerque, and has been adopted by the Veterans Affairs department, among other organizations, as a means of extending primary care to those who might not otherwise have access.
"This is not about the antiviral treatment, it’s about the engagement of primary care physicians, to train them, educate them, and help them take care of patients with hepatitis C," said Dr. Wong, chief of the division of clinical decision making at Tufts Medical Center, Boston. "It’s about increasing access," he added.
Dr. Wong presented the results of a cost-effectiveness analysis he and his Tufts colleagues conducted on a study of ECHO’s effectiveness in treating HCV, published in the New England Journal of Medicine in 2011 (N. Engl. J. Med. 2011;364:2199-207).
That prospective cohort study evaluated ECHO in the HCV treatment of 261 patients at 16 community sites and 5 prisons.
Dr. Wong and his colleagues updated the data, using information from the United Network for Organ Sharing; the Surveillance, Epidemiology and End Results Program; and life tables from the Centers for Disease Control and Prevention. They also used the previously established and validated Markov cohort simulation model to compare ECHO to no antiviral therapy for each of the 261 patients.
Costs taken into account included expenses for drugs, physician visits, lab tests, adverse events, HCV disease complications, and multidisciplinary ECHO personnel (physician, pharmacist, psychiatrist, nurse manager, coordinator, and user support analyst).
Dr. Wong said that the researchers also performed an analysis of the cost of antiviral treatment if patients traveled to the academic center to receive care instead of having ECHO come to them. Travel costs included mileage, patient time, and guard costs for prisoners. The investigators used quality-of-life adjustments to account for antiviral treatment and disease-related morbidity, and discounted costs and effectiveness at 3% a year.
They calculated that ECHO led to a 63% reduction in lifetime cirrhosis when compared with no antiviral therapy. Hepatocellular carcinoma declined by 45% and liver death by 46%. There was a 4.4-year gain in life expectancy overall, and a 5.5-year gain in quality-adjusted life expectancy.
For 42% of the 261 patients, the incremental effectiveness did not outweigh the cost – and the opportunity cost – of taking an antiviral, said Dr. Wong. In another 23% of patients, the antiviral therapy extended life, but in the end, when the costs of the disease and the antivirals were added in, there was an extra cost associated with the therapy.
But in 35% of the patients, there was an extension of life – as much as 8 additional years – and a reduction in cost of treatment, as much as $40,000.
The incremental cost-effectiveness ratio – a formula calculated by dividing the additional cost by the additional benefit – for ECHO is $3,700, Dr. Wong said. The World Health Organization considers anything less than the per capita gross domestic product of a country to be "very cost effective," and anything less than three times that per capita number to be "cost effective," he said. He noted that the mean GDP in the United States is $50,000, putting the ECHO intervention well within the WHO’s range for very cost effective.
The gains were even greater for patients living in correctional institutions, with an incremental cost-effectiveness ratio of $1,400.
The study is limited by the fact that it is a computer simulation, and some travel data were missing, said Dr. Wong.
Additional trials are needed to confirm the results, he said.
The University of New Mexico recently started an institute to spread the ECHO model.
Dr. Wong reported no conflicts of interest.
mailto:[email protected]
On Twitter @aliciaault
AT THE LIVER MEETING 2013
Major finding: The ECHO model for treating hepatitis C is cost saving in 35% of patients and very cost effective overall.
Data source: A retrospective cost-effectiveness analysis of a prospective, 261-patient cohort study.
Disclosures: Dr. Wong reported no disclosures.
Twelve percent of boomers are HCV-positive in ED screening study
WASHINGTON – A pilot study screening for hepatitis C in the emergency department found that at least 12% of baby boomers who were previously unaware of their HCV status were positive for the virus.
Infection was confirmed in almost 9% of HCV-positive patients, lead author Dr. James W. Galbraith reported at the annual meeting of the American Association for the Study of Liver Diseases.
Dr. Galbraith, an associate professor of emergency medicine at the University of Alabama, Birmingham, reported on initial results of a screening program funded by the Centers for Disease Control and Prevention that began in September. Results are currently tabulated through Oct. 17. During that time, there were 2,363 unique ED visits by patients born in the years 1945 to 1965. Seventy-three percent (1,721) agreed to answer two questions given by a triage nurse: Have you ever been tested for HCV, and if yes, are you aware of that result? Seventy-five percent, or 1,287 patients, did not know their status and were offered testing.
Of those, 90% (1,148) accepted the antibody test. Patients were excluded from testing if they were medically or surgically unstable, had known HCV infection, or if they chose to opt out.
Antibody tests were performed on 984 of those patients, with results returned to ED physicians within 30-60 minutes. Eighty-eight percent had negative results, but 12%, or 118 patients, were HCV positive.
Researchers attempt to verify positive test results with polymerase chain reaction testing, but it is not always easy to do so, said Dr. Galbraith. Patients must be kept for a new blood draw, and many have already left the ED. Testing is also expensive, he noted.
Overall, men were significantly more likely than were women to test positive (17% compared with 8%). There was no significant difference in HCV positivity rates between whites and African Americans (11% vs. 13%). Patients without insurance or those on Medicaid or other public insurance plans were significantly more likely to be positive, with 17% in each of those groups exhibiting reactivity on the antibody assay, compared with 5% of insured patients.
When patients are determined to be HCV positive, ED physicians counsel and direct them to resources in the community, including specialists. Dr. Galbraith said that the numbers of baby boomers being found to be HCV positive are likely to overwhelm the available specialists.
By September 2014, Dr. Galbraith said, his ED is likely to screen 8,000 baby boomers. If the prevalence rate remains stable, that would mean 864 who are HCV positive and more than 600 with confirmed infection, he said.
Still, it’s important to screen, said Dr. Galbraith, adding that given the study results, "the implication is that the ED may be an important venue for HCV screening."
Two federal entities have called for increased screening. In May, the CDC urged HCV testing for all Americans born between 1945 and 1965.
The U.S. Preventive Services Task Force followed in June, recommending routine HCV screening for high risk Americans, and one-time screening for adults born between 1945 and 1965.
The study was funded by the Centers for Disease Control and Prevention. Dr. Galbraith reported no disclosures.
On Twitter @aliciaault
WASHINGTON – A pilot study screening for hepatitis C in the emergency department found that at least 12% of baby boomers who were previously unaware of their HCV status were positive for the virus.
Infection was confirmed in almost 9% of HCV-positive patients, lead author Dr. James W. Galbraith reported at the annual meeting of the American Association for the Study of Liver Diseases.
Dr. Galbraith, an associate professor of emergency medicine at the University of Alabama, Birmingham, reported on initial results of a screening program funded by the Centers for Disease Control and Prevention that began in September. Results are currently tabulated through Oct. 17. During that time, there were 2,363 unique ED visits by patients born in the years 1945 to 1965. Seventy-three percent (1,721) agreed to answer two questions given by a triage nurse: Have you ever been tested for HCV, and if yes, are you aware of that result? Seventy-five percent, or 1,287 patients, did not know their status and were offered testing.
Of those, 90% (1,148) accepted the antibody test. Patients were excluded from testing if they were medically or surgically unstable, had known HCV infection, or if they chose to opt out.
Antibody tests were performed on 984 of those patients, with results returned to ED physicians within 30-60 minutes. Eighty-eight percent had negative results, but 12%, or 118 patients, were HCV positive.
Researchers attempt to verify positive test results with polymerase chain reaction testing, but it is not always easy to do so, said Dr. Galbraith. Patients must be kept for a new blood draw, and many have already left the ED. Testing is also expensive, he noted.
Overall, men were significantly more likely than were women to test positive (17% compared with 8%). There was no significant difference in HCV positivity rates between whites and African Americans (11% vs. 13%). Patients without insurance or those on Medicaid or other public insurance plans were significantly more likely to be positive, with 17% in each of those groups exhibiting reactivity on the antibody assay, compared with 5% of insured patients.
When patients are determined to be HCV positive, ED physicians counsel and direct them to resources in the community, including specialists. Dr. Galbraith said that the numbers of baby boomers being found to be HCV positive are likely to overwhelm the available specialists.
By September 2014, Dr. Galbraith said, his ED is likely to screen 8,000 baby boomers. If the prevalence rate remains stable, that would mean 864 who are HCV positive and more than 600 with confirmed infection, he said.
Still, it’s important to screen, said Dr. Galbraith, adding that given the study results, "the implication is that the ED may be an important venue for HCV screening."
Two federal entities have called for increased screening. In May, the CDC urged HCV testing for all Americans born between 1945 and 1965.
The U.S. Preventive Services Task Force followed in June, recommending routine HCV screening for high risk Americans, and one-time screening for adults born between 1945 and 1965.
The study was funded by the Centers for Disease Control and Prevention. Dr. Galbraith reported no disclosures.
On Twitter @aliciaault
WASHINGTON – A pilot study screening for hepatitis C in the emergency department found that at least 12% of baby boomers who were previously unaware of their HCV status were positive for the virus.
Infection was confirmed in almost 9% of HCV-positive patients, lead author Dr. James W. Galbraith reported at the annual meeting of the American Association for the Study of Liver Diseases.
Dr. Galbraith, an associate professor of emergency medicine at the University of Alabama, Birmingham, reported on initial results of a screening program funded by the Centers for Disease Control and Prevention that began in September. Results are currently tabulated through Oct. 17. During that time, there were 2,363 unique ED visits by patients born in the years 1945 to 1965. Seventy-three percent (1,721) agreed to answer two questions given by a triage nurse: Have you ever been tested for HCV, and if yes, are you aware of that result? Seventy-five percent, or 1,287 patients, did not know their status and were offered testing.
Of those, 90% (1,148) accepted the antibody test. Patients were excluded from testing if they were medically or surgically unstable, had known HCV infection, or if they chose to opt out.
Antibody tests were performed on 984 of those patients, with results returned to ED physicians within 30-60 minutes. Eighty-eight percent had negative results, but 12%, or 118 patients, were HCV positive.
Researchers attempt to verify positive test results with polymerase chain reaction testing, but it is not always easy to do so, said Dr. Galbraith. Patients must be kept for a new blood draw, and many have already left the ED. Testing is also expensive, he noted.
Overall, men were significantly more likely than were women to test positive (17% compared with 8%). There was no significant difference in HCV positivity rates between whites and African Americans (11% vs. 13%). Patients without insurance or those on Medicaid or other public insurance plans were significantly more likely to be positive, with 17% in each of those groups exhibiting reactivity on the antibody assay, compared with 5% of insured patients.
When patients are determined to be HCV positive, ED physicians counsel and direct them to resources in the community, including specialists. Dr. Galbraith said that the numbers of baby boomers being found to be HCV positive are likely to overwhelm the available specialists.
By September 2014, Dr. Galbraith said, his ED is likely to screen 8,000 baby boomers. If the prevalence rate remains stable, that would mean 864 who are HCV positive and more than 600 with confirmed infection, he said.
Still, it’s important to screen, said Dr. Galbraith, adding that given the study results, "the implication is that the ED may be an important venue for HCV screening."
Two federal entities have called for increased screening. In May, the CDC urged HCV testing for all Americans born between 1945 and 1965.
The U.S. Preventive Services Task Force followed in June, recommending routine HCV screening for high risk Americans, and one-time screening for adults born between 1945 and 1965.
The study was funded by the Centers for Disease Control and Prevention. Dr. Galbraith reported no disclosures.
On Twitter @aliciaault
AT THE LIVER MEETING 2013
Major finding: Twelve percent of baby boomers were HCV-positive, and 8.7% had confirmed infection in an emergency department screening study.
Data source: Six-week results of screening of 1,721 patients born between 1945 and 1965.
Disclosures: The study was funded by the Centers for Disease Control and Prevention. Dr. Galbraith reported no disclosures.
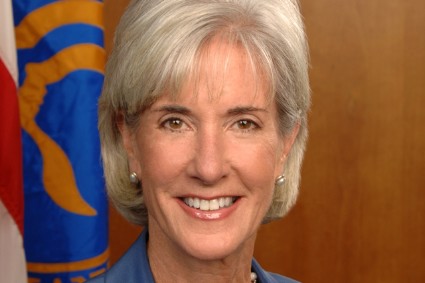
Sebelius: Hold me accountable for healthcare.gov
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
AT A HOUSE ENERGY AND COMMERCE COMMITTEE HEARING
Tavenner apologizes for healthcare.gov woes
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
Committee Chairman Dave Camp,
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
Committee Chairman Dave Camp,
Committee Chairman Dave Camp,
AT A HOUSE WAYS AND MEANS COMMITTEE HEARING
NINDS seeks comment on draft epilepsy research agenda
The National Institute of Neurological Disorders and Stroke is seeking comment on a 5-10 year plan for advancing epilepsy research.
The framework, 2014 Benchmarks for Epilepsy Research, came out of a 2-day meeting called Curing the Epilepsies 2013: Pathways Forward, which was held in April at the NINDS. The meeting was convened to discuss advances in the field since 2007, when the previous research agenda was established.
The draft framework for 2014 includes goals in four major areas:
• Understanding the causes of epilepsies and epilepsy-related conditions.
• Preventing epilepsy and its progression.
• Improving treatment options for controlling seizures and epilepsy-related conditions without side effects.
• Limiting or preventing adverse consequences of seizures and their treatment across the lifespan.
At the April meeting, researchers spoke of specific challenges in epilepsy research, prevention, and treatment. Vast amounts of data are being generated, requiring technologies to sort it all into useful information. Genomics is a growing field, with its own set of challenges. Technology is playing a role in creating new diagnostic capabilities and new avenues for research. There is a need for models that more closely reflect the etiology and clinical features of human disease. And translational studies are urgently required to bring basic science into the clinical realm.
"Embracing a culture of data sharing, collaboration, and integration across scales and approaches may best enable the epilepsy community to capitalize on these resources," according to the draft.
The draft also recognizes that much progress may come from areas that aren’t highlighted in the agenda. The NINDS is suggesting that researchers and clinicians in the epilepsy field also incorporate recommendations from a 2012 report from the Institute of Medicine, "Epilepsy Across the Spectrum: Promoting Health and Understanding." That report set priorities that focused on the public health aspects of the epilepsies, including population research, quality of care issues, and patient and clinician education.
The NINDS is accepting comments on the draft through Nov. 4. They can be submitted electronically at the institute’s website. The comments will be considered in the development of the final version of the research and benchmarking agenda.
On Twitter @aliciaault
The National Institute of Neurological Disorders and Stroke is seeking comment on a 5-10 year plan for advancing epilepsy research.
The framework, 2014 Benchmarks for Epilepsy Research, came out of a 2-day meeting called Curing the Epilepsies 2013: Pathways Forward, which was held in April at the NINDS. The meeting was convened to discuss advances in the field since 2007, when the previous research agenda was established.
The draft framework for 2014 includes goals in four major areas:
• Understanding the causes of epilepsies and epilepsy-related conditions.
• Preventing epilepsy and its progression.
• Improving treatment options for controlling seizures and epilepsy-related conditions without side effects.
• Limiting or preventing adverse consequences of seizures and their treatment across the lifespan.
At the April meeting, researchers spoke of specific challenges in epilepsy research, prevention, and treatment. Vast amounts of data are being generated, requiring technologies to sort it all into useful information. Genomics is a growing field, with its own set of challenges. Technology is playing a role in creating new diagnostic capabilities and new avenues for research. There is a need for models that more closely reflect the etiology and clinical features of human disease. And translational studies are urgently required to bring basic science into the clinical realm.
"Embracing a culture of data sharing, collaboration, and integration across scales and approaches may best enable the epilepsy community to capitalize on these resources," according to the draft.
The draft also recognizes that much progress may come from areas that aren’t highlighted in the agenda. The NINDS is suggesting that researchers and clinicians in the epilepsy field also incorporate recommendations from a 2012 report from the Institute of Medicine, "Epilepsy Across the Spectrum: Promoting Health and Understanding." That report set priorities that focused on the public health aspects of the epilepsies, including population research, quality of care issues, and patient and clinician education.
The NINDS is accepting comments on the draft through Nov. 4. They can be submitted electronically at the institute’s website. The comments will be considered in the development of the final version of the research and benchmarking agenda.
On Twitter @aliciaault
The National Institute of Neurological Disorders and Stroke is seeking comment on a 5-10 year plan for advancing epilepsy research.
The framework, 2014 Benchmarks for Epilepsy Research, came out of a 2-day meeting called Curing the Epilepsies 2013: Pathways Forward, which was held in April at the NINDS. The meeting was convened to discuss advances in the field since 2007, when the previous research agenda was established.
The draft framework for 2014 includes goals in four major areas:
• Understanding the causes of epilepsies and epilepsy-related conditions.
• Preventing epilepsy and its progression.
• Improving treatment options for controlling seizures and epilepsy-related conditions without side effects.
• Limiting or preventing adverse consequences of seizures and their treatment across the lifespan.
At the April meeting, researchers spoke of specific challenges in epilepsy research, prevention, and treatment. Vast amounts of data are being generated, requiring technologies to sort it all into useful information. Genomics is a growing field, with its own set of challenges. Technology is playing a role in creating new diagnostic capabilities and new avenues for research. There is a need for models that more closely reflect the etiology and clinical features of human disease. And translational studies are urgently required to bring basic science into the clinical realm.
"Embracing a culture of data sharing, collaboration, and integration across scales and approaches may best enable the epilepsy community to capitalize on these resources," according to the draft.
The draft also recognizes that much progress may come from areas that aren’t highlighted in the agenda. The NINDS is suggesting that researchers and clinicians in the epilepsy field also incorporate recommendations from a 2012 report from the Institute of Medicine, "Epilepsy Across the Spectrum: Promoting Health and Understanding." That report set priorities that focused on the public health aspects of the epilepsies, including population research, quality of care issues, and patient and clinician education.
The NINDS is accepting comments on the draft through Nov. 4. They can be submitted electronically at the institute’s website. The comments will be considered in the development of the final version of the research and benchmarking agenda.
On Twitter @aliciaault
Doctors: Major responsibility for cost control not ours
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves. Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren?t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions ? both cost-control keystones advanced by the Obama administration ? were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not. When it comes to individual physicians? responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients? trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
In an accompanying editorial, Dr. Ezekiel J. Emanuel, an ethicist at the University of Pennsylvania, Philadelphia, said that, "if there were ever an ?all-hands-on-deck? moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual,"" (JAMA 2013;310:374-5).
Physicians have moved beyond denying that health care costs are a problem, he added. "Yet, they are not quite willing to accept physicians? primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
"This study by Tilburt et al. indicates that the medical profession is not there yet ? that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians, he concluded.
Dr. Emanuel had no conflicts.
Upon reading the JAMA manuscript (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278), and more specifically, this summary article with commentary, I am reminded of the story about the defendant who takes the stand in court and is asked by the prosecution, "Sir, what year did you begin to beat your wife...". The defendant, of course, has never beaten his wife, but he now faces an up-hill battle with a now-biased jury.

| |
| Dr. Mark Morasch |
If asked, for which would you be most enthusiastic when it comes to controlling health care costs ? pursuing tort-reform (amongst other choices) or accepting salary reduction ? it is quite obvious which option the majority would choose. I am quite sure, if asked a similar question, the lion?s share of any profession would answer in kind. Furthermore, given the choice between looking after a patient?s best interest or, the alternative, reducing expense, it shouldn?t be hard to predict that a high percentage of respondents would choose the former. It is all about what questions are asked and how individuals may subjectively interpret the aggregate responses. The authors of the original article conclude that U.S. physicians agree that they do have some responsibility when it comes to addressing health care costs in their practices. Physicians also agree that efforts to improve quality and efficiency of care while increasing transparency with regards to cost information should be paramount. Their responses seem measured and reasonable to me.
In his accompanying commentary, Dr. Emanuel, an ethicist, has taken a significant leap when he interprets the data through his own prism and concludes that physicians choose to "Blame others and persevere with ?business as usual?" and that we "are not willing to accept...primary responsibility and take action." This attack seems to have been prompted by a reluctance, on the part of practicing physicians, to overwhelmingly support replacement of established fee-for-service paradigms. I am sorry, Dr. Emanuel, but completely eliminating fee-for-service and replacing it with a one-size-fits-all solution is simply not tenable at this time. Yes, we all must take responsibility when it comes to controlling the significant costs of health care and it is true that we risk marginalization if we fail, as a group, to be a part of the solution. But Dr. Emanuel seems to be trying his best to offend the one group who, arguably, best understands the problem and who holds, as our most important credo, to do whatever it takes to help the population we serve. To vilify physicians won?t help fix the problem.
Dr. Mark D. Morasch is a vascular surgeon at St. Vincent Healthcare Heart and Vascular, Billings, Mon., and an associate medical editor for Vascular Specialist.
Upon reading the JAMA manuscript (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278), and more specifically, this summary article with commentary, I am reminded of the story about the defendant who takes the stand in court and is asked by the prosecution, "Sir, what year did you begin to beat your wife...". The defendant, of course, has never beaten his wife, but he now faces an up-hill battle with a now-biased jury.

| |
| Dr. Mark Morasch |
If asked, for which would you be most enthusiastic when it comes to controlling health care costs ? pursuing tort-reform (amongst other choices) or accepting salary reduction ? it is quite obvious which option the majority would choose. I am quite sure, if asked a similar question, the lion?s share of any profession would answer in kind. Furthermore, given the choice between looking after a patient?s best interest or, the alternative, reducing expense, it shouldn?t be hard to predict that a high percentage of respondents would choose the former. It is all about what questions are asked and how individuals may subjectively interpret the aggregate responses. The authors of the original article conclude that U.S. physicians agree that they do have some responsibility when it comes to addressing health care costs in their practices. Physicians also agree that efforts to improve quality and efficiency of care while increasing transparency with regards to cost information should be paramount. Their responses seem measured and reasonable to me.
In his accompanying commentary, Dr. Emanuel, an ethicist, has taken a significant leap when he interprets the data through his own prism and concludes that physicians choose to "Blame others and persevere with ?business as usual?" and that we "are not willing to accept...primary responsibility and take action." This attack seems to have been prompted by a reluctance, on the part of practicing physicians, to overwhelmingly support replacement of established fee-for-service paradigms. I am sorry, Dr. Emanuel, but completely eliminating fee-for-service and replacing it with a one-size-fits-all solution is simply not tenable at this time. Yes, we all must take responsibility when it comes to controlling the significant costs of health care and it is true that we risk marginalization if we fail, as a group, to be a part of the solution. But Dr. Emanuel seems to be trying his best to offend the one group who, arguably, best understands the problem and who holds, as our most important credo, to do whatever it takes to help the population we serve. To vilify physicians won?t help fix the problem.
Dr. Mark D. Morasch is a vascular surgeon at St. Vincent Healthcare Heart and Vascular, Billings, Mon., and an associate medical editor for Vascular Specialist.
Upon reading the JAMA manuscript (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278), and more specifically, this summary article with commentary, I am reminded of the story about the defendant who takes the stand in court and is asked by the prosecution, "Sir, what year did you begin to beat your wife...". The defendant, of course, has never beaten his wife, but he now faces an up-hill battle with a now-biased jury.

| |
| Dr. Mark Morasch |
If asked, for which would you be most enthusiastic when it comes to controlling health care costs ? pursuing tort-reform (amongst other choices) or accepting salary reduction ? it is quite obvious which option the majority would choose. I am quite sure, if asked a similar question, the lion?s share of any profession would answer in kind. Furthermore, given the choice between looking after a patient?s best interest or, the alternative, reducing expense, it shouldn?t be hard to predict that a high percentage of respondents would choose the former. It is all about what questions are asked and how individuals may subjectively interpret the aggregate responses. The authors of the original article conclude that U.S. physicians agree that they do have some responsibility when it comes to addressing health care costs in their practices. Physicians also agree that efforts to improve quality and efficiency of care while increasing transparency with regards to cost information should be paramount. Their responses seem measured and reasonable to me.
In his accompanying commentary, Dr. Emanuel, an ethicist, has taken a significant leap when he interprets the data through his own prism and concludes that physicians choose to "Blame others and persevere with ?business as usual?" and that we "are not willing to accept...primary responsibility and take action." This attack seems to have been prompted by a reluctance, on the part of practicing physicians, to overwhelmingly support replacement of established fee-for-service paradigms. I am sorry, Dr. Emanuel, but completely eliminating fee-for-service and replacing it with a one-size-fits-all solution is simply not tenable at this time. Yes, we all must take responsibility when it comes to controlling the significant costs of health care and it is true that we risk marginalization if we fail, as a group, to be a part of the solution. But Dr. Emanuel seems to be trying his best to offend the one group who, arguably, best understands the problem and who holds, as our most important credo, to do whatever it takes to help the population we serve. To vilify physicians won?t help fix the problem.
Dr. Mark D. Morasch is a vascular surgeon at St. Vincent Healthcare Heart and Vascular, Billings, Mon., and an associate medical editor for Vascular Specialist.
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves. Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren?t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions ? both cost-control keystones advanced by the Obama administration ? were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not. When it comes to individual physicians? responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients? trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
In an accompanying editorial, Dr. Ezekiel J. Emanuel, an ethicist at the University of Pennsylvania, Philadelphia, said that, "if there were ever an ?all-hands-on-deck? moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual,"" (JAMA 2013;310:374-5).
Physicians have moved beyond denying that health care costs are a problem, he added. "Yet, they are not quite willing to accept physicians? primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
"This study by Tilburt et al. indicates that the medical profession is not there yet ? that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians, he concluded.
Dr. Emanuel had no conflicts.
When it comes to reducing health costs, physicians believe burden of responsibility lies primarily with plaintiffs attorneys, followed by insurers, hospitals, drug and device makers, patients, and, lastly, themselves. Those conclusions are based on 2,438 responses from some 3,900 physicians randomly surveyed in 2012. Dr. Jon C. Tilburt of the Mayo Clinic, Rochester, Minn., and his colleagues reported their findings in JAMA.
When asked whether individual physicians should have a major responsibility in reducing health costs, 36% of respondents said yes. Sixty percent said that trial lawyers bore the major burden, with health insurers coming in a close second.
More than half said that drug and device companies, hospitals and health systems, and patients also should have major responsibility for cost containment. A total of 44% said the government had that responsibility (JAMA 2013;310:380-8 [doi:10.1001/jama.2013.8278]).
Physicians also were asked about their enthusiasm for various cost-control strategies and to examine their own role in cost containment by assessing their knowledge of prices of procedures and tests and their desire to personally curb costs in their practice. The authors asked about and analyzed potential barriers to physicians becoming more cost conscious, as well.
Doctors were very enthusiastic about improving the quality and efficiency of care, primarily through promoting continuity of care and going after fraud and abuse. Expanding access to preventive care was also warmly received. Physicians were enthusiastic about limiting access to expensive treatments that had shown little benefit, using cost-effectiveness data to choose a therapy, and promoting head-to-head trials of competing therapies.
Just over half of respondents said that cutting pay for the highest-paid specialists should be embraced.
Eliminating fee for service altogether was rejected by 70% of respondents. Ninety percent said that they weren?t enthusiastic about letting the Medicare Sustainable Growth Rate cuts take effect. Two-thirds said that bundled pay and penalties for readmissions ? both cost-control keystones advanced by the Obama administration ? were not attractive.
Not surprisingly, increasing use of electronic health records also got a strong negative response, with 29% saying they were "not enthusiastic."
When it came to their own practice, 76% said they were aware of the costs of treatments or tests they recommended, and 84% said that cost is important whether a patient pays out of pocket or not. When it comes to individual physicians? responsibility for reducing health costs, the responses were very mixed.
The survey participants largely agreed that "trying to contain costs is the responsibility of every physician" (85%) and that physicians should take a more prominent role in eliminating unnecessary tests (89%). But by almost the same percentages, physicians also said that they should be devoted to their individual patients, even if a test or therapy was expensive, and that they should not deny services to their patients because someone else might need it more.
"This apparent inconsistency may reflect inherent tensions in professional roles to serve patients individually and society as a whole," Dr. Tilburt and colleagues wrote.
Finally, physicians overwhelmingly said that fear of malpractice had substantially decreased their enjoyment of practicing medicine. The authors rated that fear as a barrier to cost-conscious practice. They also found that 43% of physicians admitted they ordered more tests when they did not know the patient as well. Half said that being more cost conscious was the right thing to do, but large numbers said that it might not make a difference or could make things worse. A total of 40% said it would not limit unreasonable patient demands, and 28% said it could erode patients? trust.
Dr. Tilburt and his colleagues pointed out that the findings should be viewed with caution in part because it could not fully reflect the opinions of all American physicians. Further, opinions could be in flux, given how much has changed since even a year ago.
They suggested that policy makers move slowly when it comes to changing payment models, and instead target areas where doctors seem to be enthusiastic, including improving quality of care and using comparative effectiveness data.
The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
In an accompanying editorial, Dr. Ezekiel J. Emanuel, an ethicist at the University of Pennsylvania, Philadelphia, said that, "if there were ever an ?all-hands-on-deck? moment in the history of health care, that moment is now. The findings of this study suggest that physician do not yet have the mentality this historical moment demands. Indeed, this survey suggests that in the face of this new and uncertain moment in the reform of the health care system, physicians are lapsing into the well-known, cautious, instinctual approaches humans adopt whenever confronted by uncertainty: Blame others and persevere with "business as usual,"" (JAMA 2013;310:374-5).
Physicians have moved beyond denying that health care costs are a problem, he added. "Yet, they are not quite willing to accept physicians? primary responsibility and take action. The study findings suggest that physicians are ambivalent; they reject transformative solutions, such as eliminating fee-for-service or bundled payments, which address the seriousness of the cost problem.
"This study by Tilburt et al. indicates that the medical profession is not there yet ? that many physicians would prefer to sit on the sidelines while other actors in the health care system do the real work of reform.
This could marginalize and demote physicians, he concluded.
Dr. Emanuel had no conflicts.
Major finding: Sixty percent of responding physicians believe that trial attorneys bear major responsibility for reducing health costs.
Data source: A random survey of 3,900 physicians.
Disclosures: The study was funded by the Greenwall Foundation and the Mayo Clinic. The authors reported having no financial conflicts.
Contractors blame CMS for healthcare.gov woes
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
FROM A HOUSE ENERGY AND COMMERCE COMMITTEE HEARING
Experts call for broad sharing of clinical trial data
Clinical trial data should be shared as broadly as possible to help spur scientific innovation and answer questions of importance to public health.
"The question is not whether, but how, these data should be broadly shared," wrote Michelle M. Mello and her colleagues from Harvard University, Boston, the Pharmaceutical Research and Manufacturers of America, and several consulting companies, in an article published online Oct. 21 in the New England Journal of Medicine.
At a minimum, data-sharing should be available for trials of all approved prescription drugs, devices, and biologics in any country that has adequate intellectual property protection. A system has to ensure responsible use of data, protect privacy of research participants, and treat "all qualified data requesters and trial sponsors evenhandedly," requiring both generators and requesters to work according to the same rigorous scientific principles (N. Engl. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMhle1309073]).
The demand for more data from and about clinical trials – including protocol designs, results summaries, and more recently, raw input data – has grown over the past 15 years. Some medical journals have pushed for disclosure of more data upon request. The Food and Drug Administration increasingly has been requiring disclosure, and pharmaceutical manufacturers in the United States and Europe have made commitments to making more information public. Beginning in March 2014, the European Medicines Agency will require disclosure of some raw data, individual case report forms, and other data.
The authors envision at least four potential models for sharing data. With purely open access, everything would be available for download for free. This is the riskiest model, they said, since it would provide the least accountability.
Another model: The data generator would keep the data but answer very specific requests. A third model would have the clinical trial sponsor review data requests and decide whether and how to release the data.
In the last model, an independent review board would determine whether the data should be released. The board would collect the data from the sponsor and issue it to the requester, on a limited, need-to-know basis.
This model would likely best balance all of the competing needs, according to the authors. The independent board promises "to ensure accountability on the part of data generators and users and allow trial sponsors a voice while precluding them from denying access to data for reasons the public would not consider legitimate," they wrote.
An independent board also would help protect research participants and make sure that the playing field is level among all stakeholders, they added.
The authors noted many benefits to allowing wider access to patient-level data, such as independent analyses of safety and effectiveness, new lines of inquiry that could expose product flaws or trial design flaws, and the potential to answer questions that might affect public health but that weren’t explored in the original study.
The biggest downside is that individual participants’ privacy could be compromised, according to the authors. The risk of exposure "raises critical questions about how to ensure that participants understand the potential ramifications of data sharing," they wrote.
Mandatory disclosure could also discourage investment in research and development if manufacturers believe that the data could be used by competitors. Wider data-sharing could also lead to second-guessing of approvals by regulatory agencies.
Clinical trial data-sharing received attention from the World Medical Association in its most recent update of the Declaration of Helsinki, published online Oct. 19 in JAMA (doi: 10.1001/jama.2013.281053). Three general principles addressed data sharing:
• Number 9: It is the duty of physicians who are involved in medical research to protect the life, health, dignity, integrity, right to self-determination, privacy, and confidentiality of personal information of research subjects. The responsibility for the protection of research subjects must always rest with the physician or other health care professionals and never with the research subjects, even though they have given consent.
• Number 24. Every precaution must be taken to protect the privacy of research subjects and the confidentiality of their personal information.
• Number 32. For medical research using identifiable human material or data, such as research on material or data contained in biobanks or similar repositories, physicians must seek informed consent for its collection, storage and/or reuse. There may be exceptional situations where consent would be impossible or impracticable to obtain for such research. In such situations the research may be done only after consideration and approval of a research ethics committee.
Several of the authors of the paper published in the New England Journal of Medicine disclosed that they work for consulting companies that receive fees from various manufacturers and from academic medical centers. The working group was convened through the Multi-Regional Clinical Trials Center at Harvard University, which receives funds from pharmaceutical companies and not-for-profit entities.
On Twitter @aliciaault
Contrary to industry fears, we argue that access to full – though appropriately deidentified – data sets from clinical trials will benefit the research-based biopharmaceutical industry. We predict that it will help to increase the efficiency of drug development, improve cost-effectiveness, improve comparative-effectiveness analysis, and reduce duplication of effort among trial sponsors.
A managed-release environment that allows sharing of patient-level data while ensuring patient privacy would create a level playing field for all stakeholders. What is sometimes labeled as "free riding" may ultimately pay dividends for innovative companies and for public health. It is ironic that the organizations that most resist wider access to data are the ones that stand to benefit so much from greater transparency.
Dr. Hans-Georg Eichler, Frank Petavy, Dr. Francesco Pignatti, and Dr. Guido Rasi are all with the European Medicines Agency in London. Their remarks are taken from an accompanying editorial(N. Eng. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMp1310771]).
Contrary to industry fears, we argue that access to full – though appropriately deidentified – data sets from clinical trials will benefit the research-based biopharmaceutical industry. We predict that it will help to increase the efficiency of drug development, improve cost-effectiveness, improve comparative-effectiveness analysis, and reduce duplication of effort among trial sponsors.
A managed-release environment that allows sharing of patient-level data while ensuring patient privacy would create a level playing field for all stakeholders. What is sometimes labeled as "free riding" may ultimately pay dividends for innovative companies and for public health. It is ironic that the organizations that most resist wider access to data are the ones that stand to benefit so much from greater transparency.
Dr. Hans-Georg Eichler, Frank Petavy, Dr. Francesco Pignatti, and Dr. Guido Rasi are all with the European Medicines Agency in London. Their remarks are taken from an accompanying editorial(N. Eng. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMp1310771]).
Contrary to industry fears, we argue that access to full – though appropriately deidentified – data sets from clinical trials will benefit the research-based biopharmaceutical industry. We predict that it will help to increase the efficiency of drug development, improve cost-effectiveness, improve comparative-effectiveness analysis, and reduce duplication of effort among trial sponsors.
A managed-release environment that allows sharing of patient-level data while ensuring patient privacy would create a level playing field for all stakeholders. What is sometimes labeled as "free riding" may ultimately pay dividends for innovative companies and for public health. It is ironic that the organizations that most resist wider access to data are the ones that stand to benefit so much from greater transparency.
Dr. Hans-Georg Eichler, Frank Petavy, Dr. Francesco Pignatti, and Dr. Guido Rasi are all with the European Medicines Agency in London. Their remarks are taken from an accompanying editorial(N. Eng. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMp1310771]).
Clinical trial data should be shared as broadly as possible to help spur scientific innovation and answer questions of importance to public health.
"The question is not whether, but how, these data should be broadly shared," wrote Michelle M. Mello and her colleagues from Harvard University, Boston, the Pharmaceutical Research and Manufacturers of America, and several consulting companies, in an article published online Oct. 21 in the New England Journal of Medicine.
At a minimum, data-sharing should be available for trials of all approved prescription drugs, devices, and biologics in any country that has adequate intellectual property protection. A system has to ensure responsible use of data, protect privacy of research participants, and treat "all qualified data requesters and trial sponsors evenhandedly," requiring both generators and requesters to work according to the same rigorous scientific principles (N. Engl. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMhle1309073]).
The demand for more data from and about clinical trials – including protocol designs, results summaries, and more recently, raw input data – has grown over the past 15 years. Some medical journals have pushed for disclosure of more data upon request. The Food and Drug Administration increasingly has been requiring disclosure, and pharmaceutical manufacturers in the United States and Europe have made commitments to making more information public. Beginning in March 2014, the European Medicines Agency will require disclosure of some raw data, individual case report forms, and other data.
The authors envision at least four potential models for sharing data. With purely open access, everything would be available for download for free. This is the riskiest model, they said, since it would provide the least accountability.
Another model: The data generator would keep the data but answer very specific requests. A third model would have the clinical trial sponsor review data requests and decide whether and how to release the data.
In the last model, an independent review board would determine whether the data should be released. The board would collect the data from the sponsor and issue it to the requester, on a limited, need-to-know basis.
This model would likely best balance all of the competing needs, according to the authors. The independent board promises "to ensure accountability on the part of data generators and users and allow trial sponsors a voice while precluding them from denying access to data for reasons the public would not consider legitimate," they wrote.
An independent board also would help protect research participants and make sure that the playing field is level among all stakeholders, they added.
The authors noted many benefits to allowing wider access to patient-level data, such as independent analyses of safety and effectiveness, new lines of inquiry that could expose product flaws or trial design flaws, and the potential to answer questions that might affect public health but that weren’t explored in the original study.
The biggest downside is that individual participants’ privacy could be compromised, according to the authors. The risk of exposure "raises critical questions about how to ensure that participants understand the potential ramifications of data sharing," they wrote.
Mandatory disclosure could also discourage investment in research and development if manufacturers believe that the data could be used by competitors. Wider data-sharing could also lead to second-guessing of approvals by regulatory agencies.
Clinical trial data-sharing received attention from the World Medical Association in its most recent update of the Declaration of Helsinki, published online Oct. 19 in JAMA (doi: 10.1001/jama.2013.281053). Three general principles addressed data sharing:
• Number 9: It is the duty of physicians who are involved in medical research to protect the life, health, dignity, integrity, right to self-determination, privacy, and confidentiality of personal information of research subjects. The responsibility for the protection of research subjects must always rest with the physician or other health care professionals and never with the research subjects, even though they have given consent.
• Number 24. Every precaution must be taken to protect the privacy of research subjects and the confidentiality of their personal information.
• Number 32. For medical research using identifiable human material or data, such as research on material or data contained in biobanks or similar repositories, physicians must seek informed consent for its collection, storage and/or reuse. There may be exceptional situations where consent would be impossible or impracticable to obtain for such research. In such situations the research may be done only after consideration and approval of a research ethics committee.
Several of the authors of the paper published in the New England Journal of Medicine disclosed that they work for consulting companies that receive fees from various manufacturers and from academic medical centers. The working group was convened through the Multi-Regional Clinical Trials Center at Harvard University, which receives funds from pharmaceutical companies and not-for-profit entities.
On Twitter @aliciaault
Clinical trial data should be shared as broadly as possible to help spur scientific innovation and answer questions of importance to public health.
"The question is not whether, but how, these data should be broadly shared," wrote Michelle M. Mello and her colleagues from Harvard University, Boston, the Pharmaceutical Research and Manufacturers of America, and several consulting companies, in an article published online Oct. 21 in the New England Journal of Medicine.
At a minimum, data-sharing should be available for trials of all approved prescription drugs, devices, and biologics in any country that has adequate intellectual property protection. A system has to ensure responsible use of data, protect privacy of research participants, and treat "all qualified data requesters and trial sponsors evenhandedly," requiring both generators and requesters to work according to the same rigorous scientific principles (N. Engl. J. Med. 2013 Oct. 21 [doi: 10.1056/NEJMhle1309073]).
The demand for more data from and about clinical trials – including protocol designs, results summaries, and more recently, raw input data – has grown over the past 15 years. Some medical journals have pushed for disclosure of more data upon request. The Food and Drug Administration increasingly has been requiring disclosure, and pharmaceutical manufacturers in the United States and Europe have made commitments to making more information public. Beginning in March 2014, the European Medicines Agency will require disclosure of some raw data, individual case report forms, and other data.
The authors envision at least four potential models for sharing data. With purely open access, everything would be available for download for free. This is the riskiest model, they said, since it would provide the least accountability.
Another model: The data generator would keep the data but answer very specific requests. A third model would have the clinical trial sponsor review data requests and decide whether and how to release the data.
In the last model, an independent review board would determine whether the data should be released. The board would collect the data from the sponsor and issue it to the requester, on a limited, need-to-know basis.
This model would likely best balance all of the competing needs, according to the authors. The independent board promises "to ensure accountability on the part of data generators and users and allow trial sponsors a voice while precluding them from denying access to data for reasons the public would not consider legitimate," they wrote.
An independent board also would help protect research participants and make sure that the playing field is level among all stakeholders, they added.
The authors noted many benefits to allowing wider access to patient-level data, such as independent analyses of safety and effectiveness, new lines of inquiry that could expose product flaws or trial design flaws, and the potential to answer questions that might affect public health but that weren’t explored in the original study.
The biggest downside is that individual participants’ privacy could be compromised, according to the authors. The risk of exposure "raises critical questions about how to ensure that participants understand the potential ramifications of data sharing," they wrote.
Mandatory disclosure could also discourage investment in research and development if manufacturers believe that the data could be used by competitors. Wider data-sharing could also lead to second-guessing of approvals by regulatory agencies.
Clinical trial data-sharing received attention from the World Medical Association in its most recent update of the Declaration of Helsinki, published online Oct. 19 in JAMA (doi: 10.1001/jama.2013.281053). Three general principles addressed data sharing:
• Number 9: It is the duty of physicians who are involved in medical research to protect the life, health, dignity, integrity, right to self-determination, privacy, and confidentiality of personal information of research subjects. The responsibility for the protection of research subjects must always rest with the physician or other health care professionals and never with the research subjects, even though they have given consent.
• Number 24. Every precaution must be taken to protect the privacy of research subjects and the confidentiality of their personal information.
• Number 32. For medical research using identifiable human material or data, such as research on material or data contained in biobanks or similar repositories, physicians must seek informed consent for its collection, storage and/or reuse. There may be exceptional situations where consent would be impossible or impracticable to obtain for such research. In such situations the research may be done only after consideration and approval of a research ethics committee.
Several of the authors of the paper published in the New England Journal of Medicine disclosed that they work for consulting companies that receive fees from various manufacturers and from academic medical centers. The working group was convened through the Multi-Regional Clinical Trials Center at Harvard University, which receives funds from pharmaceutical companies and not-for-profit entities.
On Twitter @aliciaault
FROM THE NEW ENGLAND JOURNAL OF MEDICINE