User login
More than half eligible opted out of PQRS and eRx incentives in 2012
More than half of eligible providers did not participate in either the Physician Quality Reporting System or the Electronic Prescriber program in 2012, according to a comprehensive report released by the Centers for Medicare & Medicaid Services April 3.
The Physician Quality Reporting System (PQRS) was created by the Tax Relief and Health Care Act of 2006; the first reporting year was 2007. Physicians will be penalized beginning in 2015 if they do not successfully report the required quality measures.
In 2012, 64% of more than 1.2 million eligible health care providers did not participate in PQRS. The approximately 436,000 who did participate received incentives equal to 0.5% of their Medicare Part B allowable charges for the year. Participation in the program increased 36% from 2011 to 2012*, according to the CMS report.
The Electronic Prescriber (eRx) program was created by the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008, and began in 2009.
Eligible health care providers had to report for at least the first 6 months of 2013 to avoid a penalty in 2014. Prescribers also could be penalized in 2012 and 2013 if they were not deemed successful e-prescribers.
Just over half (56%) of about 779,000 eligible health care providers opted out of the eRx program in 2012, while the 345,000 who participated received a bonus payment. That represented a 22% increase in participation from 2011. About 60,000 of those who were eligible did not receive an incentive and were instead penalized. Most (75%) eligible providers were penalized because they did not participate at all. In 2012, e-prescriptions were submitted for 13 million Medicare beneficiaries.
Overall, the CMS paid $503 million in incentives through the two programs in 2012, with $167 million going to PQRS participants, and $335 million to eRx participants. The average PQRS payment was $457 and the average eRx payment was $1,474.
These totals do not include an additional 0.5% incentive payment for participation in maintenance of certification (MOC) efforts. In 2012, some 5,600 physicians received a bonus for participating in MOC. Emergency physicians led the effort, accounting for more than 3,200 of the 5,600 bonus earners. They received $1 million in incentives overall.
Emergency physicians also had the highest number of eligible providers participating in the two incentive programs – some 65% of all eligible. Other hospital-based health care providers also had high participating rates, including radiologists and nurse anesthetists.
Internists, family physicians, and cardiologists led in reporting through claims, registries, EHRs, and accountable care organizations. About 20% of eligible internists and family practice physicians participated.
The top five measures reported to the programs were on the adoption and/or use of electronic health records; tobacco screening and cessation intervention; documentation of current medications in the medical record; pneumonia vaccination for patients aged 65 years and older; and electrocardiogram for nontraumatic chest pain (emergency medicine).
On Twitter @aliciaault
*This article has been updated 4/25/2014.
More than half of eligible providers did not participate in either the Physician Quality Reporting System or the Electronic Prescriber program in 2012, according to a comprehensive report released by the Centers for Medicare & Medicaid Services April 3.
The Physician Quality Reporting System (PQRS) was created by the Tax Relief and Health Care Act of 2006; the first reporting year was 2007. Physicians will be penalized beginning in 2015 if they do not successfully report the required quality measures.
In 2012, 64% of more than 1.2 million eligible health care providers did not participate in PQRS. The approximately 436,000 who did participate received incentives equal to 0.5% of their Medicare Part B allowable charges for the year. Participation in the program increased 36% from 2011 to 2012*, according to the CMS report.
The Electronic Prescriber (eRx) program was created by the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008, and began in 2009.
Eligible health care providers had to report for at least the first 6 months of 2013 to avoid a penalty in 2014. Prescribers also could be penalized in 2012 and 2013 if they were not deemed successful e-prescribers.
Just over half (56%) of about 779,000 eligible health care providers opted out of the eRx program in 2012, while the 345,000 who participated received a bonus payment. That represented a 22% increase in participation from 2011. About 60,000 of those who were eligible did not receive an incentive and were instead penalized. Most (75%) eligible providers were penalized because they did not participate at all. In 2012, e-prescriptions were submitted for 13 million Medicare beneficiaries.
Overall, the CMS paid $503 million in incentives through the two programs in 2012, with $167 million going to PQRS participants, and $335 million to eRx participants. The average PQRS payment was $457 and the average eRx payment was $1,474.
These totals do not include an additional 0.5% incentive payment for participation in maintenance of certification (MOC) efforts. In 2012, some 5,600 physicians received a bonus for participating in MOC. Emergency physicians led the effort, accounting for more than 3,200 of the 5,600 bonus earners. They received $1 million in incentives overall.
Emergency physicians also had the highest number of eligible providers participating in the two incentive programs – some 65% of all eligible. Other hospital-based health care providers also had high participating rates, including radiologists and nurse anesthetists.
Internists, family physicians, and cardiologists led in reporting through claims, registries, EHRs, and accountable care organizations. About 20% of eligible internists and family practice physicians participated.
The top five measures reported to the programs were on the adoption and/or use of electronic health records; tobacco screening and cessation intervention; documentation of current medications in the medical record; pneumonia vaccination for patients aged 65 years and older; and electrocardiogram for nontraumatic chest pain (emergency medicine).
On Twitter @aliciaault
*This article has been updated 4/25/2014.
More than half of eligible providers did not participate in either the Physician Quality Reporting System or the Electronic Prescriber program in 2012, according to a comprehensive report released by the Centers for Medicare & Medicaid Services April 3.
The Physician Quality Reporting System (PQRS) was created by the Tax Relief and Health Care Act of 2006; the first reporting year was 2007. Physicians will be penalized beginning in 2015 if they do not successfully report the required quality measures.
In 2012, 64% of more than 1.2 million eligible health care providers did not participate in PQRS. The approximately 436,000 who did participate received incentives equal to 0.5% of their Medicare Part B allowable charges for the year. Participation in the program increased 36% from 2011 to 2012*, according to the CMS report.
The Electronic Prescriber (eRx) program was created by the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008, and began in 2009.
Eligible health care providers had to report for at least the first 6 months of 2013 to avoid a penalty in 2014. Prescribers also could be penalized in 2012 and 2013 if they were not deemed successful e-prescribers.
Just over half (56%) of about 779,000 eligible health care providers opted out of the eRx program in 2012, while the 345,000 who participated received a bonus payment. That represented a 22% increase in participation from 2011. About 60,000 of those who were eligible did not receive an incentive and were instead penalized. Most (75%) eligible providers were penalized because they did not participate at all. In 2012, e-prescriptions were submitted for 13 million Medicare beneficiaries.
Overall, the CMS paid $503 million in incentives through the two programs in 2012, with $167 million going to PQRS participants, and $335 million to eRx participants. The average PQRS payment was $457 and the average eRx payment was $1,474.
These totals do not include an additional 0.5% incentive payment for participation in maintenance of certification (MOC) efforts. In 2012, some 5,600 physicians received a bonus for participating in MOC. Emergency physicians led the effort, accounting for more than 3,200 of the 5,600 bonus earners. They received $1 million in incentives overall.
Emergency physicians also had the highest number of eligible providers participating in the two incentive programs – some 65% of all eligible. Other hospital-based health care providers also had high participating rates, including radiologists and nurse anesthetists.
Internists, family physicians, and cardiologists led in reporting through claims, registries, EHRs, and accountable care organizations. About 20% of eligible internists and family practice physicians participated.
The top five measures reported to the programs were on the adoption and/or use of electronic health records; tobacco screening and cessation intervention; documentation of current medications in the medical record; pneumonia vaccination for patients aged 65 years and older; and electrocardiogram for nontraumatic chest pain (emergency medicine).
On Twitter @aliciaault
*This article has been updated 4/25/2014.
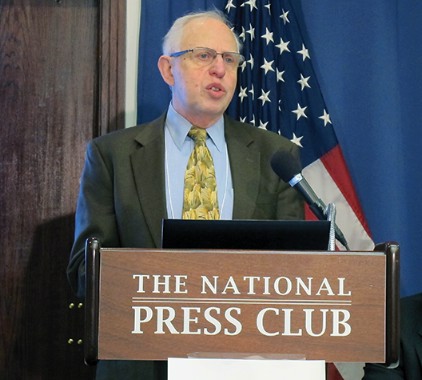
Federal agencies outline vision for regulating all health IT
Three federal agencies have issued a draft report outlining how they may approach the regulation of any and all health information technology, from billing software and radiation therapy dosing software to mobile apps and interoperability and functionality of electronic health records.
Initially, the agencies aren’t proposing any major changes to current regulation. Instead, they’re seeking more public comment on the report – both in writing and at a public meeting slated for May – before issuing any new policies or regulations, said Dr. Jeffrey E. Shuren, director of the Center for Devices and Radiological Health at the Food and Drug Administration, in a media briefing.
Overall, the approach is, "We are first asking, ‘What is the product intended to do?’ instead of, ‘What is the product’s platform?’ " said Dr. Shuren. "Also, we are asking, ‘What is the risk to patients?’ "
The FDA is one of the three main agencies charged with overseeing health information technology (IT); the others are the U.S. Department of Health & Human Services Office of the National Coordinator for Health Information Technology (ONC), and the Federal Communications Commission (FCC).
"The diverse and rapidly developing industry of health information technology requires a thoughtful, flexible approach," said HHS Secretary Kathleen Sebelius in a statement. "This proposed strategy is designed to promote innovation and provide technology to consumers and health care providers while maintaining patient safety."
Congress required the health IT report as part of the Food and Drug Administration Safety and Innovation Act (FDASIA), which became law in July 2012. It is the amalgamation of input from a 28-stakeholder workgroup that held 30 public meetings, as well as public comment on the recommendations the group issued in September.
Though not the report’s main focus, interoperability of electronic health records (EHRs) will be one focus of health IT policy going forward. The "health IT framework should promote interoperability and electronic information sharing between health IT products and across organizational boundaries," according to the report.
The three-agency framework will complement other efforts at the ONC to encourage more interoperability, Jodi G. Daniel, director of the ONC’s office of planning and policy, said during the briefing. The FDA and the ONC are looking for organizations that will be willing to test the interoperability of EHRs, Dr. Shuren added.
Overall, the agencies are recommending that health IT be separated into three categories for regulatory purposes:
• Administrative health IT, which would include billing and claims processing, practice and inventory management, and scheduling programs, which are believed to pose limited or no risk to patient safety. This category would not require any oversight beyond what’s currently in place.
• Health management health IT, which would include health information and data management; data capture and encounter documentation; electronic access to clinical results; most clinical decision support; medication management (electronic medication administration records); electronic communication and coordination (provider to patient, patient to provider, provider to provider, etc.); provider order entry; knowledge (clinical evidence) management; and, patient identification and matching. The safety risks of these types of tools are thought to be low, compared with the potential benefits.
The ONC is going to be taking a closer look at this type of health IT. To mitigate any potential risk involved with these products, the ONC will promote the use of quality management principles; identify, develop, and adopt standards and best practices; leverage conformity assessment tools; and create an environment of learning and continual improvement.
• Medical device health IT functions, which include computer-aided detection/diagnostic software, radiation treatment planning, and robotic surgical planning and control software. Both the ONC and the FCC have some involvement already in regulation of these products, such as ensuring interoperability between a device and an EHR (ONC), and use of the wireless spectrum (FCC).
The FDA currently regulates many of these products, such as electrocardiography analytical software. The report suggests that the FDA should continue that oversight, but the agency also should work to clarify its policies on the distinction between wellness and disease-related claims, medical device accessories, medical device clinical decision support software, and mobile medical apps.
The three agencies also said that they would develop a Health IT Safety Center, a public-private entity that would convene stakeholders to work on best practices and provide a forum for the exchange of ideas and information focused on patient safety.
The report "is a proposed strategy," said Dr. Shuren, adding that it is "not a final framework."
He said it’s not clear when or if any of the agencies would issue any new regulations, but that the approach would likely evolve with the public’s input.
On Twitter @aliciaault
Three federal agencies have issued a draft report outlining how they may approach the regulation of any and all health information technology, from billing software and radiation therapy dosing software to mobile apps and interoperability and functionality of electronic health records.
Initially, the agencies aren’t proposing any major changes to current regulation. Instead, they’re seeking more public comment on the report – both in writing and at a public meeting slated for May – before issuing any new policies or regulations, said Dr. Jeffrey E. Shuren, director of the Center for Devices and Radiological Health at the Food and Drug Administration, in a media briefing.
Overall, the approach is, "We are first asking, ‘What is the product intended to do?’ instead of, ‘What is the product’s platform?’ " said Dr. Shuren. "Also, we are asking, ‘What is the risk to patients?’ "
The FDA is one of the three main agencies charged with overseeing health information technology (IT); the others are the U.S. Department of Health & Human Services Office of the National Coordinator for Health Information Technology (ONC), and the Federal Communications Commission (FCC).
"The diverse and rapidly developing industry of health information technology requires a thoughtful, flexible approach," said HHS Secretary Kathleen Sebelius in a statement. "This proposed strategy is designed to promote innovation and provide technology to consumers and health care providers while maintaining patient safety."
Congress required the health IT report as part of the Food and Drug Administration Safety and Innovation Act (FDASIA), which became law in July 2012. It is the amalgamation of input from a 28-stakeholder workgroup that held 30 public meetings, as well as public comment on the recommendations the group issued in September.
Though not the report’s main focus, interoperability of electronic health records (EHRs) will be one focus of health IT policy going forward. The "health IT framework should promote interoperability and electronic information sharing between health IT products and across organizational boundaries," according to the report.
The three-agency framework will complement other efforts at the ONC to encourage more interoperability, Jodi G. Daniel, director of the ONC’s office of planning and policy, said during the briefing. The FDA and the ONC are looking for organizations that will be willing to test the interoperability of EHRs, Dr. Shuren added.
Overall, the agencies are recommending that health IT be separated into three categories for regulatory purposes:
• Administrative health IT, which would include billing and claims processing, practice and inventory management, and scheduling programs, which are believed to pose limited or no risk to patient safety. This category would not require any oversight beyond what’s currently in place.
• Health management health IT, which would include health information and data management; data capture and encounter documentation; electronic access to clinical results; most clinical decision support; medication management (electronic medication administration records); electronic communication and coordination (provider to patient, patient to provider, provider to provider, etc.); provider order entry; knowledge (clinical evidence) management; and, patient identification and matching. The safety risks of these types of tools are thought to be low, compared with the potential benefits.
The ONC is going to be taking a closer look at this type of health IT. To mitigate any potential risk involved with these products, the ONC will promote the use of quality management principles; identify, develop, and adopt standards and best practices; leverage conformity assessment tools; and create an environment of learning and continual improvement.
• Medical device health IT functions, which include computer-aided detection/diagnostic software, radiation treatment planning, and robotic surgical planning and control software. Both the ONC and the FCC have some involvement already in regulation of these products, such as ensuring interoperability between a device and an EHR (ONC), and use of the wireless spectrum (FCC).
The FDA currently regulates many of these products, such as electrocardiography analytical software. The report suggests that the FDA should continue that oversight, but the agency also should work to clarify its policies on the distinction between wellness and disease-related claims, medical device accessories, medical device clinical decision support software, and mobile medical apps.
The three agencies also said that they would develop a Health IT Safety Center, a public-private entity that would convene stakeholders to work on best practices and provide a forum for the exchange of ideas and information focused on patient safety.
The report "is a proposed strategy," said Dr. Shuren, adding that it is "not a final framework."
He said it’s not clear when or if any of the agencies would issue any new regulations, but that the approach would likely evolve with the public’s input.
On Twitter @aliciaault
Three federal agencies have issued a draft report outlining how they may approach the regulation of any and all health information technology, from billing software and radiation therapy dosing software to mobile apps and interoperability and functionality of electronic health records.
Initially, the agencies aren’t proposing any major changes to current regulation. Instead, they’re seeking more public comment on the report – both in writing and at a public meeting slated for May – before issuing any new policies or regulations, said Dr. Jeffrey E. Shuren, director of the Center for Devices and Radiological Health at the Food and Drug Administration, in a media briefing.
Overall, the approach is, "We are first asking, ‘What is the product intended to do?’ instead of, ‘What is the product’s platform?’ " said Dr. Shuren. "Also, we are asking, ‘What is the risk to patients?’ "
The FDA is one of the three main agencies charged with overseeing health information technology (IT); the others are the U.S. Department of Health & Human Services Office of the National Coordinator for Health Information Technology (ONC), and the Federal Communications Commission (FCC).
"The diverse and rapidly developing industry of health information technology requires a thoughtful, flexible approach," said HHS Secretary Kathleen Sebelius in a statement. "This proposed strategy is designed to promote innovation and provide technology to consumers and health care providers while maintaining patient safety."
Congress required the health IT report as part of the Food and Drug Administration Safety and Innovation Act (FDASIA), which became law in July 2012. It is the amalgamation of input from a 28-stakeholder workgroup that held 30 public meetings, as well as public comment on the recommendations the group issued in September.
Though not the report’s main focus, interoperability of electronic health records (EHRs) will be one focus of health IT policy going forward. The "health IT framework should promote interoperability and electronic information sharing between health IT products and across organizational boundaries," according to the report.
The three-agency framework will complement other efforts at the ONC to encourage more interoperability, Jodi G. Daniel, director of the ONC’s office of planning and policy, said during the briefing. The FDA and the ONC are looking for organizations that will be willing to test the interoperability of EHRs, Dr. Shuren added.
Overall, the agencies are recommending that health IT be separated into three categories for regulatory purposes:
• Administrative health IT, which would include billing and claims processing, practice and inventory management, and scheduling programs, which are believed to pose limited or no risk to patient safety. This category would not require any oversight beyond what’s currently in place.
• Health management health IT, which would include health information and data management; data capture and encounter documentation; electronic access to clinical results; most clinical decision support; medication management (electronic medication administration records); electronic communication and coordination (provider to patient, patient to provider, provider to provider, etc.); provider order entry; knowledge (clinical evidence) management; and, patient identification and matching. The safety risks of these types of tools are thought to be low, compared with the potential benefits.
The ONC is going to be taking a closer look at this type of health IT. To mitigate any potential risk involved with these products, the ONC will promote the use of quality management principles; identify, develop, and adopt standards and best practices; leverage conformity assessment tools; and create an environment of learning and continual improvement.
• Medical device health IT functions, which include computer-aided detection/diagnostic software, radiation treatment planning, and robotic surgical planning and control software. Both the ONC and the FCC have some involvement already in regulation of these products, such as ensuring interoperability between a device and an EHR (ONC), and use of the wireless spectrum (FCC).
The FDA currently regulates many of these products, such as electrocardiography analytical software. The report suggests that the FDA should continue that oversight, but the agency also should work to clarify its policies on the distinction between wellness and disease-related claims, medical device accessories, medical device clinical decision support software, and mobile medical apps.
The three agencies also said that they would develop a Health IT Safety Center, a public-private entity that would convene stakeholders to work on best practices and provide a forum for the exchange of ideas and information focused on patient safety.
The report "is a proposed strategy," said Dr. Shuren, adding that it is "not a final framework."
He said it’s not clear when or if any of the agencies would issue any new regulations, but that the approach would likely evolve with the public’s input.
On Twitter @aliciaault
Line up credit now for possible ICD-10 cash crunch, experts advise
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
Feds extend ACA enrollment deadline for some
Consumers who have had difficulty enrolling in a health insurance plan through healthcare.gov or through federal call centers will be given extra time to sign up beyond the March 31 open enrollment deadline, according to the Obama administration.
The leeway applies only to those trying to enroll through the federal health insurance exchange, which operates in 27 states. Several other states, including Maryland, Minnesota, and Nevada, also have offered relief to consumers having trouble signing up through those states’ exchanges.
"We are experiencing a surge in demand and are making sure that we will be ready to help consumers who may be in line by the deadline to complete enrollment – either online or over the phone," said Aaron Albright, a spokesman for the Health and Human Services (HHS) department.
The agency has not yet issued guidance on how to get help finishing up the enrollment process or how long the extension would last.
For everyone else, open enrollment ends March 31.
"Like clockwork, another day, another delay," House Energy and Commerce Committee Chairman Fred Upton (R-Mich.) said in a statement. He also noted that HHS Secretary Kathleen Sebelius told the committee in December that there would be no more delays, and that "2 weeks ago an HHS official insisted that the administration did not have ‘statutory authority’ to extend the enrollment period for this year; yet here we are."
Rep. Dave Camp (R-Mich.) and Rep. Kevin Brady (R-Tex.) said in a statement that they are going to press the administration on just how many individuals have paid for their insurance coverage so far – information that HHS says it does not have.
"We have recently obtained information that suggests your most recent testimony before the Ways and Means Committee was at best evasive and perhaps misleading," they wrote in a letter to Ms. Sebelius. They note that the committee has obtained evidence that insurers are indeed submitting payment data to the Centers for Medicare and Medicaid Services.
On Twitter @aliciaault
Consumers who have had difficulty enrolling in a health insurance plan through healthcare.gov or through federal call centers will be given extra time to sign up beyond the March 31 open enrollment deadline, according to the Obama administration.
The leeway applies only to those trying to enroll through the federal health insurance exchange, which operates in 27 states. Several other states, including Maryland, Minnesota, and Nevada, also have offered relief to consumers having trouble signing up through those states’ exchanges.
"We are experiencing a surge in demand and are making sure that we will be ready to help consumers who may be in line by the deadline to complete enrollment – either online or over the phone," said Aaron Albright, a spokesman for the Health and Human Services (HHS) department.
The agency has not yet issued guidance on how to get help finishing up the enrollment process or how long the extension would last.
For everyone else, open enrollment ends March 31.
"Like clockwork, another day, another delay," House Energy and Commerce Committee Chairman Fred Upton (R-Mich.) said in a statement. He also noted that HHS Secretary Kathleen Sebelius told the committee in December that there would be no more delays, and that "2 weeks ago an HHS official insisted that the administration did not have ‘statutory authority’ to extend the enrollment period for this year; yet here we are."
Rep. Dave Camp (R-Mich.) and Rep. Kevin Brady (R-Tex.) said in a statement that they are going to press the administration on just how many individuals have paid for their insurance coverage so far – information that HHS says it does not have.
"We have recently obtained information that suggests your most recent testimony before the Ways and Means Committee was at best evasive and perhaps misleading," they wrote in a letter to Ms. Sebelius. They note that the committee has obtained evidence that insurers are indeed submitting payment data to the Centers for Medicare and Medicaid Services.
On Twitter @aliciaault
Consumers who have had difficulty enrolling in a health insurance plan through healthcare.gov or through federal call centers will be given extra time to sign up beyond the March 31 open enrollment deadline, according to the Obama administration.
The leeway applies only to those trying to enroll through the federal health insurance exchange, which operates in 27 states. Several other states, including Maryland, Minnesota, and Nevada, also have offered relief to consumers having trouble signing up through those states’ exchanges.
"We are experiencing a surge in demand and are making sure that we will be ready to help consumers who may be in line by the deadline to complete enrollment – either online or over the phone," said Aaron Albright, a spokesman for the Health and Human Services (HHS) department.
The agency has not yet issued guidance on how to get help finishing up the enrollment process or how long the extension would last.
For everyone else, open enrollment ends March 31.
"Like clockwork, another day, another delay," House Energy and Commerce Committee Chairman Fred Upton (R-Mich.) said in a statement. He also noted that HHS Secretary Kathleen Sebelius told the committee in December that there would be no more delays, and that "2 weeks ago an HHS official insisted that the administration did not have ‘statutory authority’ to extend the enrollment period for this year; yet here we are."
Rep. Dave Camp (R-Mich.) and Rep. Kevin Brady (R-Tex.) said in a statement that they are going to press the administration on just how many individuals have paid for their insurance coverage so far – information that HHS says it does not have.
"We have recently obtained information that suggests your most recent testimony before the Ways and Means Committee was at best evasive and perhaps misleading," they wrote in a letter to Ms. Sebelius. They note that the committee has obtained evidence that insurers are indeed submitting payment data to the Centers for Medicare and Medicaid Services.
On Twitter @aliciaault
Supreme Court divided on ACA contraception challenge
WASHINGTON – The Supreme Court appears divided over whether for-profit employers can be required to provide health care coverage for contraceptives if doing so goes against their religious beliefs.
The justices heard oral arguments Mar. 25 in two cases in which employers do not want to pay for coverage of specific contraception methods, including Plan B, Ella, and two intrauterine devices. The Affordable Care Act requires that preventive care services be covered at no cost to the insured; all 20 contraceptive methods approved by the Food and Drug Administration are considered preventive care services under the law.
The employers, Hobby Lobby Stores Inc. and Conestoga Wood Specialties Corp., believe that the emergency contraceptives and IUDs are abortifacient and that being required to pay for them violates their religious beliefs and their rights under the Religious Freedom Restoration Act and the Free Exercise Clause of the First Amendment.
U.S. Solicitor General Donald B. Verrilli Jr., who represented the federal government, argued that federal and state law do not regard those contraceptives as abortifacient.
"We’ve got about 2 million women who rely on the IUD as a method of birth control in this country," he told the justices. "I don’t think they think they are engaged in abortion in doing that."
Justices Sandra Sotomayor, Ruth Bader Ginsburg, and Elena Kagan closely questioned attorney Paul Clement, who represented the companies, on whether allowing such a claim might open the door to claims that other medical treatments or procedures such as vaccinations or mental health care – or even obeying wage laws or antidiscrimination laws – also violate religious freedom.
"One religious group could opt out of this and another religious group could opt out of that and everything would be piecemeal and nothing would be uniform," Justice Kagan said. She went on to say that, if the court followed the companies’ arguments, then "the entire U.S. Code" could be subject to the same types of legal claims.
Mr. Clement, a partner with Bancroft PLLC, pointed out that the federal government has already granted exceptions to the contraceptive mandate. Religious institutions and religiously affiliated organizations can use a third-party workaround so as to not directly provide contraception coverage to their employees; further, plans that existed and have not substantially changed since the ACA’s passage are not required to cover contraceptives either.
Justice Sotomayor questioned whether it is possible for a corporation to hold and exercise religious belief and how a court would decide if a corporation was sufficiently religious to be given an exception.
Several justices questioned why Hobby Lobby or Conestoga Wood didn’t just forgo providing health insurance for their workers, but Mr. Clement said that the employers believe in providing health insurance as a benefit to their employees and are required by the ACA to do so. Each would be fined by the government for not providing insurance; fines for not providing coverage for contraception are higher.
Mr. Verrilli argued that government had a compelling interest in requiring coverage of contraception because it protects the public’s health.
Justice Antonin Scalia expressed skepticism. "You can’t argue that here because the government has made a lot of exemptions," he said.
Justice Anthony Kennedy noted that the exemptions were granted merely because a government agency – the Department of Health and Human Services – had decided to do so. It shows that "the health care coverage was not that important," when weighing whether to allow some employers to opt out, Justice Kennedy said.
But Mr. Verrilli argued that the benefits were essential. If the court allowed employers to opt out of benefits required under the ACA, it "would be extinguishing statutorily guaranteed health benefits of fundamental importance to these employees, and that is something that this court has never done," he said.
The American College of Physicians agreed. In a statement issued after the oral arguments were heard, Dr. Molly Cooke, ACP president, said that allowing employers to "selectively opt out" would undermine the ACA’s protections, "leading to under-insurance, poorer health outcomes and potentially discriminatory health benefit packages based on gender, socioeconomics, health status, religion, sexual orientation, or other factors."
Outside the court after the arguments, Mr. Clement said that the two companies were "not asking for some special treatment," but to be given the same opportunity for an exception as had been given to other companies. He would not speculate on the court’s direction, but said that "the court obviously took these cases very seriously," and that he and his clients "eagerly await the court’s decision."
Charmaine Yoest, president and chief executive officer of Americans United for Life, told reporters that Hobby Lobby and Conestoga Wood should have a right to opt out of paying for emergency contraception, citing "the evidence shows that some of these drugs covered under the HHS mandate do have life-ending properties."
Americans United for Life filed a number of amicus (friend of the court) briefs in these cases on behalf of Physicians for Life, the American Association of Pro-Life Obstetricians and Gynecologists, and other groups.
On Twitter @aliciaault
WASHINGTON – The Supreme Court appears divided over whether for-profit employers can be required to provide health care coverage for contraceptives if doing so goes against their religious beliefs.
The justices heard oral arguments Mar. 25 in two cases in which employers do not want to pay for coverage of specific contraception methods, including Plan B, Ella, and two intrauterine devices. The Affordable Care Act requires that preventive care services be covered at no cost to the insured; all 20 contraceptive methods approved by the Food and Drug Administration are considered preventive care services under the law.
The employers, Hobby Lobby Stores Inc. and Conestoga Wood Specialties Corp., believe that the emergency contraceptives and IUDs are abortifacient and that being required to pay for them violates their religious beliefs and their rights under the Religious Freedom Restoration Act and the Free Exercise Clause of the First Amendment.
U.S. Solicitor General Donald B. Verrilli Jr., who represented the federal government, argued that federal and state law do not regard those contraceptives as abortifacient.
"We’ve got about 2 million women who rely on the IUD as a method of birth control in this country," he told the justices. "I don’t think they think they are engaged in abortion in doing that."
Justices Sandra Sotomayor, Ruth Bader Ginsburg, and Elena Kagan closely questioned attorney Paul Clement, who represented the companies, on whether allowing such a claim might open the door to claims that other medical treatments or procedures such as vaccinations or mental health care – or even obeying wage laws or antidiscrimination laws – also violate religious freedom.
"One religious group could opt out of this and another religious group could opt out of that and everything would be piecemeal and nothing would be uniform," Justice Kagan said. She went on to say that, if the court followed the companies’ arguments, then "the entire U.S. Code" could be subject to the same types of legal claims.
Mr. Clement, a partner with Bancroft PLLC, pointed out that the federal government has already granted exceptions to the contraceptive mandate. Religious institutions and religiously affiliated organizations can use a third-party workaround so as to not directly provide contraception coverage to their employees; further, plans that existed and have not substantially changed since the ACA’s passage are not required to cover contraceptives either.
Justice Sotomayor questioned whether it is possible for a corporation to hold and exercise religious belief and how a court would decide if a corporation was sufficiently religious to be given an exception.
Several justices questioned why Hobby Lobby or Conestoga Wood didn’t just forgo providing health insurance for their workers, but Mr. Clement said that the employers believe in providing health insurance as a benefit to their employees and are required by the ACA to do so. Each would be fined by the government for not providing insurance; fines for not providing coverage for contraception are higher.
Mr. Verrilli argued that government had a compelling interest in requiring coverage of contraception because it protects the public’s health.
Justice Antonin Scalia expressed skepticism. "You can’t argue that here because the government has made a lot of exemptions," he said.
Justice Anthony Kennedy noted that the exemptions were granted merely because a government agency – the Department of Health and Human Services – had decided to do so. It shows that "the health care coverage was not that important," when weighing whether to allow some employers to opt out, Justice Kennedy said.
But Mr. Verrilli argued that the benefits were essential. If the court allowed employers to opt out of benefits required under the ACA, it "would be extinguishing statutorily guaranteed health benefits of fundamental importance to these employees, and that is something that this court has never done," he said.
The American College of Physicians agreed. In a statement issued after the oral arguments were heard, Dr. Molly Cooke, ACP president, said that allowing employers to "selectively opt out" would undermine the ACA’s protections, "leading to under-insurance, poorer health outcomes and potentially discriminatory health benefit packages based on gender, socioeconomics, health status, religion, sexual orientation, or other factors."
Outside the court after the arguments, Mr. Clement said that the two companies were "not asking for some special treatment," but to be given the same opportunity for an exception as had been given to other companies. He would not speculate on the court’s direction, but said that "the court obviously took these cases very seriously," and that he and his clients "eagerly await the court’s decision."
Charmaine Yoest, president and chief executive officer of Americans United for Life, told reporters that Hobby Lobby and Conestoga Wood should have a right to opt out of paying for emergency contraception, citing "the evidence shows that some of these drugs covered under the HHS mandate do have life-ending properties."
Americans United for Life filed a number of amicus (friend of the court) briefs in these cases on behalf of Physicians for Life, the American Association of Pro-Life Obstetricians and Gynecologists, and other groups.
On Twitter @aliciaault
WASHINGTON – The Supreme Court appears divided over whether for-profit employers can be required to provide health care coverage for contraceptives if doing so goes against their religious beliefs.
The justices heard oral arguments Mar. 25 in two cases in which employers do not want to pay for coverage of specific contraception methods, including Plan B, Ella, and two intrauterine devices. The Affordable Care Act requires that preventive care services be covered at no cost to the insured; all 20 contraceptive methods approved by the Food and Drug Administration are considered preventive care services under the law.
The employers, Hobby Lobby Stores Inc. and Conestoga Wood Specialties Corp., believe that the emergency contraceptives and IUDs are abortifacient and that being required to pay for them violates their religious beliefs and their rights under the Religious Freedom Restoration Act and the Free Exercise Clause of the First Amendment.
U.S. Solicitor General Donald B. Verrilli Jr., who represented the federal government, argued that federal and state law do not regard those contraceptives as abortifacient.
"We’ve got about 2 million women who rely on the IUD as a method of birth control in this country," he told the justices. "I don’t think they think they are engaged in abortion in doing that."
Justices Sandra Sotomayor, Ruth Bader Ginsburg, and Elena Kagan closely questioned attorney Paul Clement, who represented the companies, on whether allowing such a claim might open the door to claims that other medical treatments or procedures such as vaccinations or mental health care – or even obeying wage laws or antidiscrimination laws – also violate religious freedom.
"One religious group could opt out of this and another religious group could opt out of that and everything would be piecemeal and nothing would be uniform," Justice Kagan said. She went on to say that, if the court followed the companies’ arguments, then "the entire U.S. Code" could be subject to the same types of legal claims.
Mr. Clement, a partner with Bancroft PLLC, pointed out that the federal government has already granted exceptions to the contraceptive mandate. Religious institutions and religiously affiliated organizations can use a third-party workaround so as to not directly provide contraception coverage to their employees; further, plans that existed and have not substantially changed since the ACA’s passage are not required to cover contraceptives either.
Justice Sotomayor questioned whether it is possible for a corporation to hold and exercise religious belief and how a court would decide if a corporation was sufficiently religious to be given an exception.
Several justices questioned why Hobby Lobby or Conestoga Wood didn’t just forgo providing health insurance for their workers, but Mr. Clement said that the employers believe in providing health insurance as a benefit to their employees and are required by the ACA to do so. Each would be fined by the government for not providing insurance; fines for not providing coverage for contraception are higher.
Mr. Verrilli argued that government had a compelling interest in requiring coverage of contraception because it protects the public’s health.
Justice Antonin Scalia expressed skepticism. "You can’t argue that here because the government has made a lot of exemptions," he said.
Justice Anthony Kennedy noted that the exemptions were granted merely because a government agency – the Department of Health and Human Services – had decided to do so. It shows that "the health care coverage was not that important," when weighing whether to allow some employers to opt out, Justice Kennedy said.
But Mr. Verrilli argued that the benefits were essential. If the court allowed employers to opt out of benefits required under the ACA, it "would be extinguishing statutorily guaranteed health benefits of fundamental importance to these employees, and that is something that this court has never done," he said.
The American College of Physicians agreed. In a statement issued after the oral arguments were heard, Dr. Molly Cooke, ACP president, said that allowing employers to "selectively opt out" would undermine the ACA’s protections, "leading to under-insurance, poorer health outcomes and potentially discriminatory health benefit packages based on gender, socioeconomics, health status, religion, sexual orientation, or other factors."
Outside the court after the arguments, Mr. Clement said that the two companies were "not asking for some special treatment," but to be given the same opportunity for an exception as had been given to other companies. He would not speculate on the court’s direction, but said that "the court obviously took these cases very seriously," and that he and his clients "eagerly await the court’s decision."
Charmaine Yoest, president and chief executive officer of Americans United for Life, told reporters that Hobby Lobby and Conestoga Wood should have a right to opt out of paying for emergency contraception, citing "the evidence shows that some of these drugs covered under the HHS mandate do have life-ending properties."
Americans United for Life filed a number of amicus (friend of the court) briefs in these cases on behalf of Physicians for Life, the American Association of Pro-Life Obstetricians and Gynecologists, and other groups.
On Twitter @aliciaault
AT THE SUPREME COURT
Contraception challenge could have broad impact on medicine
Should a company be required to provide employees with health insurance coverage for contraception if the owner says it is a violation of his or her religious beliefs?
That’s one issue the Supreme Court will consider when it hears oral arguments March 25 in cases filed by Hobby Lobby Stores and Conestoga Wood Specialties Corp.
Each company objects to the Affordable Care Act’s requirement that insurance plans (with some exceptions) provide coverage of family planning counseling and any Food and Drug Administration–approved contraceptive method, as well as follow-up counseling and management, all at no cost to employees.
If the court rules in favor of the companies, millions of women potentially could lose their health care coverage for contraception.
More chillingly, such a ruling could lead to interference in the physician-patient relationship. Further, if for-profit employers are allowed to deny coverage of contraception based on religion, might they eventually seek to drop coverage for vaccination, psychiatric care, transfusions, and other medical procedures from their health plans?
"It would be a dangerous precedent," Dr. Hal C. Lawrence III, executive vice president and chief executive officer of the American Congress of Obstetricians and Gynecologists (ACOG), said in a briefing with reporters.
Tom Goldstein, a partner with law firm Goldstein & Russell and the publisher of SCOTUSblog, agreed.
"The legal principle invoked by the plaintiffs has some potentially startling implications for what one might claim as a religious liberty," he said at a briefing sponsored by the Kaiser Family Foundation. A ruling in their favor could result in "more expansive, more troubling claims," including denial of coverage for other medical procedures and, potentially, discrimination based on race, ethnicity, gender, or sexual orientation – all in the name of religious freedom.
Not all insurance plans must provide contraception coverage under the ACA. Health plans that existed before 2010 and have not substantially changed since are "grandfathered" and don’t have to provide coverage. Plans offered by nonprofit religious organizations are exempt. Nonprofit, religiously affiliated employers also are accommodated. If these employers object to providing coverage on religious grounds, they must notify their insurer. The employer can elect not to pay for that benefit, but the insurer has to reimburse the worker for contraception.
There are no exemptions for plans offered by secular employers, which face a $100 per day per enrollee penalty if they do not provide coverage. Hobby Lobby could face fines of up to $475 million a year, and Conestoga could be looking at $35 million a year in penalties, according to Laurie Sobel, a senior policy analyst with the Kaiser Family Foundation.
The contraception requirement has triggered at least 93 lawsuits. Some object to providing any contraception coverage, while others focus in on emergency contraception. The Hobby Lobby and Conestoga cases are the first to make it to the Supreme Court.
Religious objections
The family that owns Hobby Lobby, a chain with 500 stores and 13,000 employees, says it objects to covering Plan B, Ella, or IUDs because doing so violates its religious beliefs and First Amendment rights.
The Hahn family, which owns the 950-employee Conestoga Wood Specialties, says that it objects to covering Plan B or Ella for the same reasons.
Both object to covering family planning counseling as well.
The companies argue that the Religious Freedom Restoration Act of 1993 gives them the right to deny coverage. The task before their attorneys is to convince Supreme Court justices that a corporation can have religious beliefs and that expressing those beliefs is covered by the First Amendment.
Their arguments are supported by 59 amicus (friend of the court) briefs filed by religious groups and related parties.
The court has not upheld anything like that before, according to Marci A. Hamilton, the Paul R. Verkuil Chair in Public Law at the Benjamin N. Cardozo School of Law at Yeshiva University in New York. Religious beliefs are usually strictly protected, but religious conduct, which has the potential to harm people, can be governed, Ms. Hamilton said at the Kaiser briefing.
Contraception and public health
The government is arguing that it has a compelling interest to require contraception coverage and family planning because it helps prevent unintended pregnancy and thus improves the health of women and children.
This argument is supported in 23 amicus briefs filed by groups including physician organizations such as ACOG, the American Academy of Pediatrics, the Association of Reproductive Health Professionals, the California Medical Association, the Massachusetts Medical Society, and the Society for Maternal-Fetal Medicine, among others.
"The value of family planning, including contraception, has been clearly demonstrated for decades," said Dr. Lawrence of ACOG. It gives women the ability to prevent unintended pregnancy and to time and space pregnancies, and it helps to reduce fetal and maternal morbidity and mortality, he said.
Dr. Lawrence noted that Hobby Lobby and Conestoga were characterizing emergency contraception as abortion methods. "The best scientific evidence shows that emergency contraception works by inhibiting ovulation," he said. "This is contraception, not abortion."
Doctor-patient relationship
If the court upholds the companies’ objection to counseling, that also could open the door to a wide range of restrictions on what physicians can talk to their patients about.
"Your employer would be telling your doctor what you can and can’t talk about," said Adam Sonfield, a senior public policy associate with the Guttmacher Institute. "That would be a clear violation of the rights of the patient ... and could even be considered malpractice."
Dr. Lawrence said that "to not be able to educate patients about their bodies is anathema to women’s health care."
Decisions about a woman’s needs and her health should be between her and her doctor and "should not include input from a woman’s boss," he added.
That sentiment was echoed by ACOG and other medical groups in their brief. They said that "important, private medical decisions should be made by a patient in consultation with her health care provider. There is no role for a woman’s employer in these decisions."
Predictions on ruling?
The Supreme Court could make its ruling any time between March 25 and the end of its current term in late June. Legal experts at the Kaiser Family Foundation and National Health Law Program said they did not expect a ruling in favor of the plaintiffs, Hobby Lobby and Conestoga Wood.
Should the court support the companies’ arguments, however, many state laws require contraceptive equity, said Susan Berke Fogel, director of Reproductive Health at the National Health Law Program.
Mr. Sonfeld of the Guttmacher Institute also noted that 28 states require employers to cover the full range of FDA-approved contraceptives.
On Twitter @aliciaault
Should a company be required to provide employees with health insurance coverage for contraception if the owner says it is a violation of his or her religious beliefs?
That’s one issue the Supreme Court will consider when it hears oral arguments March 25 in cases filed by Hobby Lobby Stores and Conestoga Wood Specialties Corp.
Each company objects to the Affordable Care Act’s requirement that insurance plans (with some exceptions) provide coverage of family planning counseling and any Food and Drug Administration–approved contraceptive method, as well as follow-up counseling and management, all at no cost to employees.
If the court rules in favor of the companies, millions of women potentially could lose their health care coverage for contraception.
More chillingly, such a ruling could lead to interference in the physician-patient relationship. Further, if for-profit employers are allowed to deny coverage of contraception based on religion, might they eventually seek to drop coverage for vaccination, psychiatric care, transfusions, and other medical procedures from their health plans?
"It would be a dangerous precedent," Dr. Hal C. Lawrence III, executive vice president and chief executive officer of the American Congress of Obstetricians and Gynecologists (ACOG), said in a briefing with reporters.
Tom Goldstein, a partner with law firm Goldstein & Russell and the publisher of SCOTUSblog, agreed.
"The legal principle invoked by the plaintiffs has some potentially startling implications for what one might claim as a religious liberty," he said at a briefing sponsored by the Kaiser Family Foundation. A ruling in their favor could result in "more expansive, more troubling claims," including denial of coverage for other medical procedures and, potentially, discrimination based on race, ethnicity, gender, or sexual orientation – all in the name of religious freedom.
Not all insurance plans must provide contraception coverage under the ACA. Health plans that existed before 2010 and have not substantially changed since are "grandfathered" and don’t have to provide coverage. Plans offered by nonprofit religious organizations are exempt. Nonprofit, religiously affiliated employers also are accommodated. If these employers object to providing coverage on religious grounds, they must notify their insurer. The employer can elect not to pay for that benefit, but the insurer has to reimburse the worker for contraception.
There are no exemptions for plans offered by secular employers, which face a $100 per day per enrollee penalty if they do not provide coverage. Hobby Lobby could face fines of up to $475 million a year, and Conestoga could be looking at $35 million a year in penalties, according to Laurie Sobel, a senior policy analyst with the Kaiser Family Foundation.
The contraception requirement has triggered at least 93 lawsuits. Some object to providing any contraception coverage, while others focus in on emergency contraception. The Hobby Lobby and Conestoga cases are the first to make it to the Supreme Court.
Religious objections
The family that owns Hobby Lobby, a chain with 500 stores and 13,000 employees, says it objects to covering Plan B, Ella, or IUDs because doing so violates its religious beliefs and First Amendment rights.
The Hahn family, which owns the 950-employee Conestoga Wood Specialties, says that it objects to covering Plan B or Ella for the same reasons.
Both object to covering family planning counseling as well.
The companies argue that the Religious Freedom Restoration Act of 1993 gives them the right to deny coverage. The task before their attorneys is to convince Supreme Court justices that a corporation can have religious beliefs and that expressing those beliefs is covered by the First Amendment.
Their arguments are supported by 59 amicus (friend of the court) briefs filed by religious groups and related parties.
The court has not upheld anything like that before, according to Marci A. Hamilton, the Paul R. Verkuil Chair in Public Law at the Benjamin N. Cardozo School of Law at Yeshiva University in New York. Religious beliefs are usually strictly protected, but religious conduct, which has the potential to harm people, can be governed, Ms. Hamilton said at the Kaiser briefing.
Contraception and public health
The government is arguing that it has a compelling interest to require contraception coverage and family planning because it helps prevent unintended pregnancy and thus improves the health of women and children.
This argument is supported in 23 amicus briefs filed by groups including physician organizations such as ACOG, the American Academy of Pediatrics, the Association of Reproductive Health Professionals, the California Medical Association, the Massachusetts Medical Society, and the Society for Maternal-Fetal Medicine, among others.
"The value of family planning, including contraception, has been clearly demonstrated for decades," said Dr. Lawrence of ACOG. It gives women the ability to prevent unintended pregnancy and to time and space pregnancies, and it helps to reduce fetal and maternal morbidity and mortality, he said.
Dr. Lawrence noted that Hobby Lobby and Conestoga were characterizing emergency contraception as abortion methods. "The best scientific evidence shows that emergency contraception works by inhibiting ovulation," he said. "This is contraception, not abortion."
Doctor-patient relationship
If the court upholds the companies’ objection to counseling, that also could open the door to a wide range of restrictions on what physicians can talk to their patients about.
"Your employer would be telling your doctor what you can and can’t talk about," said Adam Sonfield, a senior public policy associate with the Guttmacher Institute. "That would be a clear violation of the rights of the patient ... and could even be considered malpractice."
Dr. Lawrence said that "to not be able to educate patients about their bodies is anathema to women’s health care."
Decisions about a woman’s needs and her health should be between her and her doctor and "should not include input from a woman’s boss," he added.
That sentiment was echoed by ACOG and other medical groups in their brief. They said that "important, private medical decisions should be made by a patient in consultation with her health care provider. There is no role for a woman’s employer in these decisions."
Predictions on ruling?
The Supreme Court could make its ruling any time between March 25 and the end of its current term in late June. Legal experts at the Kaiser Family Foundation and National Health Law Program said they did not expect a ruling in favor of the plaintiffs, Hobby Lobby and Conestoga Wood.
Should the court support the companies’ arguments, however, many state laws require contraceptive equity, said Susan Berke Fogel, director of Reproductive Health at the National Health Law Program.
Mr. Sonfeld of the Guttmacher Institute also noted that 28 states require employers to cover the full range of FDA-approved contraceptives.
On Twitter @aliciaault
Should a company be required to provide employees with health insurance coverage for contraception if the owner says it is a violation of his or her religious beliefs?
That’s one issue the Supreme Court will consider when it hears oral arguments March 25 in cases filed by Hobby Lobby Stores and Conestoga Wood Specialties Corp.
Each company objects to the Affordable Care Act’s requirement that insurance plans (with some exceptions) provide coverage of family planning counseling and any Food and Drug Administration–approved contraceptive method, as well as follow-up counseling and management, all at no cost to employees.
If the court rules in favor of the companies, millions of women potentially could lose their health care coverage for contraception.
More chillingly, such a ruling could lead to interference in the physician-patient relationship. Further, if for-profit employers are allowed to deny coverage of contraception based on religion, might they eventually seek to drop coverage for vaccination, psychiatric care, transfusions, and other medical procedures from their health plans?
"It would be a dangerous precedent," Dr. Hal C. Lawrence III, executive vice president and chief executive officer of the American Congress of Obstetricians and Gynecologists (ACOG), said in a briefing with reporters.
Tom Goldstein, a partner with law firm Goldstein & Russell and the publisher of SCOTUSblog, agreed.
"The legal principle invoked by the plaintiffs has some potentially startling implications for what one might claim as a religious liberty," he said at a briefing sponsored by the Kaiser Family Foundation. A ruling in their favor could result in "more expansive, more troubling claims," including denial of coverage for other medical procedures and, potentially, discrimination based on race, ethnicity, gender, or sexual orientation – all in the name of religious freedom.
Not all insurance plans must provide contraception coverage under the ACA. Health plans that existed before 2010 and have not substantially changed since are "grandfathered" and don’t have to provide coverage. Plans offered by nonprofit religious organizations are exempt. Nonprofit, religiously affiliated employers also are accommodated. If these employers object to providing coverage on religious grounds, they must notify their insurer. The employer can elect not to pay for that benefit, but the insurer has to reimburse the worker for contraception.
There are no exemptions for plans offered by secular employers, which face a $100 per day per enrollee penalty if they do not provide coverage. Hobby Lobby could face fines of up to $475 million a year, and Conestoga could be looking at $35 million a year in penalties, according to Laurie Sobel, a senior policy analyst with the Kaiser Family Foundation.
The contraception requirement has triggered at least 93 lawsuits. Some object to providing any contraception coverage, while others focus in on emergency contraception. The Hobby Lobby and Conestoga cases are the first to make it to the Supreme Court.
Religious objections
The family that owns Hobby Lobby, a chain with 500 stores and 13,000 employees, says it objects to covering Plan B, Ella, or IUDs because doing so violates its religious beliefs and First Amendment rights.
The Hahn family, which owns the 950-employee Conestoga Wood Specialties, says that it objects to covering Plan B or Ella for the same reasons.
Both object to covering family planning counseling as well.
The companies argue that the Religious Freedom Restoration Act of 1993 gives them the right to deny coverage. The task before their attorneys is to convince Supreme Court justices that a corporation can have religious beliefs and that expressing those beliefs is covered by the First Amendment.
Their arguments are supported by 59 amicus (friend of the court) briefs filed by religious groups and related parties.
The court has not upheld anything like that before, according to Marci A. Hamilton, the Paul R. Verkuil Chair in Public Law at the Benjamin N. Cardozo School of Law at Yeshiva University in New York. Religious beliefs are usually strictly protected, but religious conduct, which has the potential to harm people, can be governed, Ms. Hamilton said at the Kaiser briefing.
Contraception and public health
The government is arguing that it has a compelling interest to require contraception coverage and family planning because it helps prevent unintended pregnancy and thus improves the health of women and children.
This argument is supported in 23 amicus briefs filed by groups including physician organizations such as ACOG, the American Academy of Pediatrics, the Association of Reproductive Health Professionals, the California Medical Association, the Massachusetts Medical Society, and the Society for Maternal-Fetal Medicine, among others.
"The value of family planning, including contraception, has been clearly demonstrated for decades," said Dr. Lawrence of ACOG. It gives women the ability to prevent unintended pregnancy and to time and space pregnancies, and it helps to reduce fetal and maternal morbidity and mortality, he said.
Dr. Lawrence noted that Hobby Lobby and Conestoga were characterizing emergency contraception as abortion methods. "The best scientific evidence shows that emergency contraception works by inhibiting ovulation," he said. "This is contraception, not abortion."
Doctor-patient relationship
If the court upholds the companies’ objection to counseling, that also could open the door to a wide range of restrictions on what physicians can talk to their patients about.
"Your employer would be telling your doctor what you can and can’t talk about," said Adam Sonfield, a senior public policy associate with the Guttmacher Institute. "That would be a clear violation of the rights of the patient ... and could even be considered malpractice."
Dr. Lawrence said that "to not be able to educate patients about their bodies is anathema to women’s health care."
Decisions about a woman’s needs and her health should be between her and her doctor and "should not include input from a woman’s boss," he added.
That sentiment was echoed by ACOG and other medical groups in their brief. They said that "important, private medical decisions should be made by a patient in consultation with her health care provider. There is no role for a woman’s employer in these decisions."
Predictions on ruling?
The Supreme Court could make its ruling any time between March 25 and the end of its current term in late June. Legal experts at the Kaiser Family Foundation and National Health Law Program said they did not expect a ruling in favor of the plaintiffs, Hobby Lobby and Conestoga Wood.
Should the court support the companies’ arguments, however, many state laws require contraceptive equity, said Susan Berke Fogel, director of Reproductive Health at the National Health Law Program.
Mr. Sonfeld of the Guttmacher Institute also noted that 28 states require employers to cover the full range of FDA-approved contraceptives.
On Twitter @aliciaault
FDA approves omalizumab for chronic idiopathic urticaria
The Food and Drug Administration has approved omalizumab (Xolair) for chronic idiopathic urticaria in people 12 years of age and older who remain symptomatic despite treatment with H1-antihistamine therapy.
Omalizumab was first approved in 2003 for moderate to severe asthma. In 2007, the FDA required the drug to be administered in a doctor’s office only, to monitor for potentially severe anaphylaxis; a boxed warning was added at that time.
According to the drug’s developer, Genentech, omalizumab is the first biologic and the first medicine approved for chronic idiopathic urticaria since nonsedating H1-antihistamines.
The approval was based on the results from two studies, ASTERIA I and ASTERIA II5, which were presented in November 2013 at the annual congress of the European Academy of Dermatology and Venereology.
According to Genentech, about 1.5 million Americans develop chronic idiopathic urticaria at some point, with women twice as likely as men to get the condition.
Chronic idiopathic urticaria "can be a frustrating condition for patients," said Mike Tringale, senior vice president at the Asthma and Allergy Foundation of America in a statement issued by Genentech. "This new use for Xolair gives hope to appropriate patients who can go for months or even years without getting satisfactory itch and hive reduction."
Omalizumab was jointly developed by Genentech and Novartis Pharma, and is copromoted in the United States with Novartis.
[email protected] On Twitter @aliciaault
The Food and Drug Administration has approved omalizumab (Xolair) for chronic idiopathic urticaria in people 12 years of age and older who remain symptomatic despite treatment with H1-antihistamine therapy.
Omalizumab was first approved in 2003 for moderate to severe asthma. In 2007, the FDA required the drug to be administered in a doctor’s office only, to monitor for potentially severe anaphylaxis; a boxed warning was added at that time.
According to the drug’s developer, Genentech, omalizumab is the first biologic and the first medicine approved for chronic idiopathic urticaria since nonsedating H1-antihistamines.
The approval was based on the results from two studies, ASTERIA I and ASTERIA II5, which were presented in November 2013 at the annual congress of the European Academy of Dermatology and Venereology.
According to Genentech, about 1.5 million Americans develop chronic idiopathic urticaria at some point, with women twice as likely as men to get the condition.
Chronic idiopathic urticaria "can be a frustrating condition for patients," said Mike Tringale, senior vice president at the Asthma and Allergy Foundation of America in a statement issued by Genentech. "This new use for Xolair gives hope to appropriate patients who can go for months or even years without getting satisfactory itch and hive reduction."
Omalizumab was jointly developed by Genentech and Novartis Pharma, and is copromoted in the United States with Novartis.
[email protected] On Twitter @aliciaault
The Food and Drug Administration has approved omalizumab (Xolair) for chronic idiopathic urticaria in people 12 years of age and older who remain symptomatic despite treatment with H1-antihistamine therapy.
Omalizumab was first approved in 2003 for moderate to severe asthma. In 2007, the FDA required the drug to be administered in a doctor’s office only, to monitor for potentially severe anaphylaxis; a boxed warning was added at that time.
According to the drug’s developer, Genentech, omalizumab is the first biologic and the first medicine approved for chronic idiopathic urticaria since nonsedating H1-antihistamines.
The approval was based on the results from two studies, ASTERIA I and ASTERIA II5, which were presented in November 2013 at the annual congress of the European Academy of Dermatology and Venereology.
According to Genentech, about 1.5 million Americans develop chronic idiopathic urticaria at some point, with women twice as likely as men to get the condition.
Chronic idiopathic urticaria "can be a frustrating condition for patients," said Mike Tringale, senior vice president at the Asthma and Allergy Foundation of America in a statement issued by Genentech. "This new use for Xolair gives hope to appropriate patients who can go for months or even years without getting satisfactory itch and hive reduction."
Omalizumab was jointly developed by Genentech and Novartis Pharma, and is copromoted in the United States with Novartis.
[email protected] On Twitter @aliciaault
Doctors may not get paid for care if patients don’t pay their ACA premiums
Will you get paid for the care you provide to patients who have gained insurance coverage through the Affordable Care Act’s health insurance claims? You’ll soon find out.
Under the health reform law, patients must pay their first month’s premium to be considered enrolled; they then have 90 days to pay the next premium.
If the patient doesn’t pay his or her premiums for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate his or her policy. The physician is left to collect whatever is owed for all outstanding claims from the patient.
The Centers for Medicare and Medicaid Services (CMS) clarified the grace period policy in a letter to insurers last year.
The first ripples could come in April. Patients who started and paid for coverage in January, but who did not pay in February or March, might get dropped from coverage. That could leave physicians scrambling to cover the unreimbursed care.
Physicians’ organizations including the American Medical Association, the American College of Physicians, and the American Academy of Family Physicians have been working to reverse this provision of the Affordable Care Act, to no avail so far.
In a March 5 letter to the CMS, dozens of organizations and state medical societies urged the agency to require insurers to tell physicians whether patients had up-to-date coverage during the verification of eligibility. As the law and current regulations are written, insurers can notify physicians on their own timeline whether a patient’s coverage has lapsed.
The organizations also asked the CMS to "require issuers to assume full financial responsibility if an issuer provides inaccurate eligibility information during the last 60 days of the grace period."
"Managing risk is typically a role for insurers, but the grace period rule transfers two-thirds of that risk from the insurers to physicians and health care providers," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
She added that the AMA is now offering some resources to help physicians manage the "potential negative impact" from having unwittingly given uncompensated care.
Among the resources is a sample letter for patients that explains the 90-day grace period and the importance of paying premiums on a timely basis and in full. The AMA also provides a step-by-step outline suggesting how to collect from patients whose coverage has lapsed.
It is unclear how many individuals have paid for coverage under the Affordable Care Act. The Health and Human Services department said on March 17 that 5 million Americans have signed up for coverage through the state and federal exchanges since Oct. 1. But the department continues to say that it does not know how many have paid their premiums.
On Twitter @aliciaault
Will you get paid for the care you provide to patients who have gained insurance coverage through the Affordable Care Act’s health insurance claims? You’ll soon find out.
Under the health reform law, patients must pay their first month’s premium to be considered enrolled; they then have 90 days to pay the next premium.
If the patient doesn’t pay his or her premiums for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate his or her policy. The physician is left to collect whatever is owed for all outstanding claims from the patient.
The Centers for Medicare and Medicaid Services (CMS) clarified the grace period policy in a letter to insurers last year.
The first ripples could come in April. Patients who started and paid for coverage in January, but who did not pay in February or March, might get dropped from coverage. That could leave physicians scrambling to cover the unreimbursed care.
Physicians’ organizations including the American Medical Association, the American College of Physicians, and the American Academy of Family Physicians have been working to reverse this provision of the Affordable Care Act, to no avail so far.
In a March 5 letter to the CMS, dozens of organizations and state medical societies urged the agency to require insurers to tell physicians whether patients had up-to-date coverage during the verification of eligibility. As the law and current regulations are written, insurers can notify physicians on their own timeline whether a patient’s coverage has lapsed.
The organizations also asked the CMS to "require issuers to assume full financial responsibility if an issuer provides inaccurate eligibility information during the last 60 days of the grace period."
"Managing risk is typically a role for insurers, but the grace period rule transfers two-thirds of that risk from the insurers to physicians and health care providers," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
She added that the AMA is now offering some resources to help physicians manage the "potential negative impact" from having unwittingly given uncompensated care.
Among the resources is a sample letter for patients that explains the 90-day grace period and the importance of paying premiums on a timely basis and in full. The AMA also provides a step-by-step outline suggesting how to collect from patients whose coverage has lapsed.
It is unclear how many individuals have paid for coverage under the Affordable Care Act. The Health and Human Services department said on March 17 that 5 million Americans have signed up for coverage through the state and federal exchanges since Oct. 1. But the department continues to say that it does not know how many have paid their premiums.
On Twitter @aliciaault
Will you get paid for the care you provide to patients who have gained insurance coverage through the Affordable Care Act’s health insurance claims? You’ll soon find out.
Under the health reform law, patients must pay their first month’s premium to be considered enrolled; they then have 90 days to pay the next premium.
If the patient doesn’t pay his or her premiums for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate his or her policy. The physician is left to collect whatever is owed for all outstanding claims from the patient.
The Centers for Medicare and Medicaid Services (CMS) clarified the grace period policy in a letter to insurers last year.
The first ripples could come in April. Patients who started and paid for coverage in January, but who did not pay in February or March, might get dropped from coverage. That could leave physicians scrambling to cover the unreimbursed care.
Physicians’ organizations including the American Medical Association, the American College of Physicians, and the American Academy of Family Physicians have been working to reverse this provision of the Affordable Care Act, to no avail so far.
In a March 5 letter to the CMS, dozens of organizations and state medical societies urged the agency to require insurers to tell physicians whether patients had up-to-date coverage during the verification of eligibility. As the law and current regulations are written, insurers can notify physicians on their own timeline whether a patient’s coverage has lapsed.
The organizations also asked the CMS to "require issuers to assume full financial responsibility if an issuer provides inaccurate eligibility information during the last 60 days of the grace period."
"Managing risk is typically a role for insurers, but the grace period rule transfers two-thirds of that risk from the insurers to physicians and health care providers," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
She added that the AMA is now offering some resources to help physicians manage the "potential negative impact" from having unwittingly given uncompensated care.
Among the resources is a sample letter for patients that explains the 90-day grace period and the importance of paying premiums on a timely basis and in full. The AMA also provides a step-by-step outline suggesting how to collect from patients whose coverage has lapsed.
It is unclear how many individuals have paid for coverage under the Affordable Care Act. The Health and Human Services department said on March 17 that 5 million Americans have signed up for coverage through the state and federal exchanges since Oct. 1. But the department continues to say that it does not know how many have paid their premiums.
On Twitter @aliciaault
Autoimmune patients report mixed results with new ACA coverage
WASHINGTON – Almost half of patients with autoimmune disorders report that they face higher costs with their new Affordable Care Act coverage while just under half report they are better off than before the law went into effect.
Those are the top-line results of a non–random-sample survey of about 400 autoimmune patients released by the American Autoimmune Related Diseases Association (AARDA) on March 18.
Among all respondents, 26% said that they had to buy a new insurance plan when the health insurance marketplaces began this year; 62% did not. Overall, 42% said that their premiums had increased, but that number includes some people who were previously uninsured, and thus, were not paying premiums at all, said Stephanie Hales, a lawyer in Washington, who represents the association.
A third of respondents reported that their deductibles for either medical services or prescription drugs had increased, while 40% said their deductible had not changed. More than a third (36%) of respondents said that coverage of the services that were important to them had decreased. The ACA requires insurance companies to provide a comprehensive set of benefits.
More than half said their coverage had stayed the same or was better.
In terms of prescription drug coverage, almost 40% of patients said they were paying more.
Most survey participants (66%) also said that they were able to keep their specialist, and almost half said that they had the same accessibility. But 33% said they had experienced access issues.
The survey shows "that the ACA has helped many people so far, but that continued improvements are needed to ensure that the ACA is implemented in a way that meets the needs of patients with serious and chronic conditions, including autoimmune diseases," said Ms. Hales.
The survey was conducted to help determine how to address concerns and complaints that the various autoimmune associations have heard from patients since the enrollment period for the ACA started in October, AARDA president Virginia T. Ladd said in an interview.
The association plans to survey members again a few months after enrollment closes on March 31, to gauge the impact on access to specialists and to medications.
The small survey of about 400 patients was not random; respondents were solicited through the organizations’ websites, and most of the data were collected in January and February.
On Twitter @aliciaault
WASHINGTON – Almost half of patients with autoimmune disorders report that they face higher costs with their new Affordable Care Act coverage while just under half report they are better off than before the law went into effect.
Those are the top-line results of a non–random-sample survey of about 400 autoimmune patients released by the American Autoimmune Related Diseases Association (AARDA) on March 18.
Among all respondents, 26% said that they had to buy a new insurance plan when the health insurance marketplaces began this year; 62% did not. Overall, 42% said that their premiums had increased, but that number includes some people who were previously uninsured, and thus, were not paying premiums at all, said Stephanie Hales, a lawyer in Washington, who represents the association.
A third of respondents reported that their deductibles for either medical services or prescription drugs had increased, while 40% said their deductible had not changed. More than a third (36%) of respondents said that coverage of the services that were important to them had decreased. The ACA requires insurance companies to provide a comprehensive set of benefits.
More than half said their coverage had stayed the same or was better.
In terms of prescription drug coverage, almost 40% of patients said they were paying more.
Most survey participants (66%) also said that they were able to keep their specialist, and almost half said that they had the same accessibility. But 33% said they had experienced access issues.
The survey shows "that the ACA has helped many people so far, but that continued improvements are needed to ensure that the ACA is implemented in a way that meets the needs of patients with serious and chronic conditions, including autoimmune diseases," said Ms. Hales.
The survey was conducted to help determine how to address concerns and complaints that the various autoimmune associations have heard from patients since the enrollment period for the ACA started in October, AARDA president Virginia T. Ladd said in an interview.
The association plans to survey members again a few months after enrollment closes on March 31, to gauge the impact on access to specialists and to medications.
The small survey of about 400 patients was not random; respondents were solicited through the organizations’ websites, and most of the data were collected in January and February.
On Twitter @aliciaault
WASHINGTON – Almost half of patients with autoimmune disorders report that they face higher costs with their new Affordable Care Act coverage while just under half report they are better off than before the law went into effect.
Those are the top-line results of a non–random-sample survey of about 400 autoimmune patients released by the American Autoimmune Related Diseases Association (AARDA) on March 18.
Among all respondents, 26% said that they had to buy a new insurance plan when the health insurance marketplaces began this year; 62% did not. Overall, 42% said that their premiums had increased, but that number includes some people who were previously uninsured, and thus, were not paying premiums at all, said Stephanie Hales, a lawyer in Washington, who represents the association.
A third of respondents reported that their deductibles for either medical services or prescription drugs had increased, while 40% said their deductible had not changed. More than a third (36%) of respondents said that coverage of the services that were important to them had decreased. The ACA requires insurance companies to provide a comprehensive set of benefits.
More than half said their coverage had stayed the same or was better.
In terms of prescription drug coverage, almost 40% of patients said they were paying more.
Most survey participants (66%) also said that they were able to keep their specialist, and almost half said that they had the same accessibility. But 33% said they had experienced access issues.
The survey shows "that the ACA has helped many people so far, but that continued improvements are needed to ensure that the ACA is implemented in a way that meets the needs of patients with serious and chronic conditions, including autoimmune diseases," said Ms. Hales.
The survey was conducted to help determine how to address concerns and complaints that the various autoimmune associations have heard from patients since the enrollment period for the ACA started in October, AARDA president Virginia T. Ladd said in an interview.
The association plans to survey members again a few months after enrollment closes on March 31, to gauge the impact on access to specialists and to medications.
The small survey of about 400 patients was not random; respondents were solicited through the organizations’ websites, and most of the data were collected in January and February.
On Twitter @aliciaault
Autoimmune disease coalition seeks to increase physician knowledge
WASHINGTON – Some 64% of family physicians are "uncomfortable" or "stressed" when diagnosing autoimmune disease, and almost three-quarters said they have not been given adequate training in diagnosing and treating the conditions, according to a small survey.
The survey of 130 family physicians was conducted by the American Autoimmune Related Diseases Association (AARDA) last fall. The association has queried physicians each year since the mid-1990s on a variety of issues relating to the care and treatment of patients with any one of the 100 or so diseases that fall into the autoimmune category.
The AARDA, along with the National Coalition of Autoimmune Patient Groups, is pushing for more comprehensive autoimmune disorder centers where patients can receive focused and coordinated care from specialists who are more intimately involved with the diseases.
The autoimmune facilities would be modeled on comprehensive cancer centers.
Now, patients struggle to find specialists who can accurately diagnose and treat their conditions. "There’s no such thing as the autoimmunologist," said Stanley Finger, Ph.D., the AARDA’s vice chairman of the board, at a briefing.
Patients responding to AARDA surveys report that it takes 4-5 years to get an accurate diagnosis, and that they see an average of five physicians before they get that diagnosis. At least half of patients are labeled chronic complainers and told that their symptoms are figments of their imagination, Dr. Finger said.
But 75% say they would seek care at a specialized center if it existed.
Improving diagnosis also requires increasing physician awareness and education. In the AARDA’s most recent survey, almost 60% of family physicians said that they had only one or two lectures on autoimmune disease in medical school, said Dr. Finger, who is also president of Environmental Consulting and Investigations in Bluffton, S.C.
"It doesn’t give a lot of time for these physicians to become experts," Dr. Finger said. "Because of that, they don’t feel very good about the training they have received."
The AARDA plans to develop a syllabus for medical schools and a continuing education program to help fill physicians’ knowledge gaps.
The group also surveys about 1,000 members of the general public every 5-7 years to gauge awareness of how patients are interacting with physicians. In 1992, only 5% could name an autoimmune disease. That has increased, but only to 15%. In the first survey, 93% of the public thought AIDS was an autoimmune disease. Now, just 21% have that belief.
Borrowing another page from the cancer model, the AARDA and the coalition are seeking to establish an autoimmune disease registry that would be similar to the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. The SEER program compiles data about cancer incidence, mortality, and cost. It is widely used by researchers, patients, physicians, and public health agencies.
The autoimmune registry is still a work in progress. There is a huge absence of data in the autoimmune field – for example, no one knows with certainty just how many Americans have any of the various conditions, said Aaron H. Abend, the AARDA’s informatics director.
The registry would aggregate data already being compiled by various individual autoimmune associations. But the effort is in its infancy. The groups still need to agree on governance, data protocols, and other issues, Mr. Abend said. However, the registry will use software that is the standard for registries operated by the National Institutes of Health.
[email protected]
On Twitter @aliciaault
WASHINGTON – Some 64% of family physicians are "uncomfortable" or "stressed" when diagnosing autoimmune disease, and almost three-quarters said they have not been given adequate training in diagnosing and treating the conditions, according to a small survey.
The survey of 130 family physicians was conducted by the American Autoimmune Related Diseases Association (AARDA) last fall. The association has queried physicians each year since the mid-1990s on a variety of issues relating to the care and treatment of patients with any one of the 100 or so diseases that fall into the autoimmune category.
The AARDA, along with the National Coalition of Autoimmune Patient Groups, is pushing for more comprehensive autoimmune disorder centers where patients can receive focused and coordinated care from specialists who are more intimately involved with the diseases.
The autoimmune facilities would be modeled on comprehensive cancer centers.
Now, patients struggle to find specialists who can accurately diagnose and treat their conditions. "There’s no such thing as the autoimmunologist," said Stanley Finger, Ph.D., the AARDA’s vice chairman of the board, at a briefing.
Patients responding to AARDA surveys report that it takes 4-5 years to get an accurate diagnosis, and that they see an average of five physicians before they get that diagnosis. At least half of patients are labeled chronic complainers and told that their symptoms are figments of their imagination, Dr. Finger said.
But 75% say they would seek care at a specialized center if it existed.
Improving diagnosis also requires increasing physician awareness and education. In the AARDA’s most recent survey, almost 60% of family physicians said that they had only one or two lectures on autoimmune disease in medical school, said Dr. Finger, who is also president of Environmental Consulting and Investigations in Bluffton, S.C.
"It doesn’t give a lot of time for these physicians to become experts," Dr. Finger said. "Because of that, they don’t feel very good about the training they have received."
The AARDA plans to develop a syllabus for medical schools and a continuing education program to help fill physicians’ knowledge gaps.
The group also surveys about 1,000 members of the general public every 5-7 years to gauge awareness of how patients are interacting with physicians. In 1992, only 5% could name an autoimmune disease. That has increased, but only to 15%. In the first survey, 93% of the public thought AIDS was an autoimmune disease. Now, just 21% have that belief.
Borrowing another page from the cancer model, the AARDA and the coalition are seeking to establish an autoimmune disease registry that would be similar to the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. The SEER program compiles data about cancer incidence, mortality, and cost. It is widely used by researchers, patients, physicians, and public health agencies.
The autoimmune registry is still a work in progress. There is a huge absence of data in the autoimmune field – for example, no one knows with certainty just how many Americans have any of the various conditions, said Aaron H. Abend, the AARDA’s informatics director.
The registry would aggregate data already being compiled by various individual autoimmune associations. But the effort is in its infancy. The groups still need to agree on governance, data protocols, and other issues, Mr. Abend said. However, the registry will use software that is the standard for registries operated by the National Institutes of Health.
[email protected]
On Twitter @aliciaault
WASHINGTON – Some 64% of family physicians are "uncomfortable" or "stressed" when diagnosing autoimmune disease, and almost three-quarters said they have not been given adequate training in diagnosing and treating the conditions, according to a small survey.
The survey of 130 family physicians was conducted by the American Autoimmune Related Diseases Association (AARDA) last fall. The association has queried physicians each year since the mid-1990s on a variety of issues relating to the care and treatment of patients with any one of the 100 or so diseases that fall into the autoimmune category.
The AARDA, along with the National Coalition of Autoimmune Patient Groups, is pushing for more comprehensive autoimmune disorder centers where patients can receive focused and coordinated care from specialists who are more intimately involved with the diseases.
The autoimmune facilities would be modeled on comprehensive cancer centers.
Now, patients struggle to find specialists who can accurately diagnose and treat their conditions. "There’s no such thing as the autoimmunologist," said Stanley Finger, Ph.D., the AARDA’s vice chairman of the board, at a briefing.
Patients responding to AARDA surveys report that it takes 4-5 years to get an accurate diagnosis, and that they see an average of five physicians before they get that diagnosis. At least half of patients are labeled chronic complainers and told that their symptoms are figments of their imagination, Dr. Finger said.
But 75% say they would seek care at a specialized center if it existed.
Improving diagnosis also requires increasing physician awareness and education. In the AARDA’s most recent survey, almost 60% of family physicians said that they had only one or two lectures on autoimmune disease in medical school, said Dr. Finger, who is also president of Environmental Consulting and Investigations in Bluffton, S.C.
"It doesn’t give a lot of time for these physicians to become experts," Dr. Finger said. "Because of that, they don’t feel very good about the training they have received."
The AARDA plans to develop a syllabus for medical schools and a continuing education program to help fill physicians’ knowledge gaps.
The group also surveys about 1,000 members of the general public every 5-7 years to gauge awareness of how patients are interacting with physicians. In 1992, only 5% could name an autoimmune disease. That has increased, but only to 15%. In the first survey, 93% of the public thought AIDS was an autoimmune disease. Now, just 21% have that belief.
Borrowing another page from the cancer model, the AARDA and the coalition are seeking to establish an autoimmune disease registry that would be similar to the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. The SEER program compiles data about cancer incidence, mortality, and cost. It is widely used by researchers, patients, physicians, and public health agencies.
The autoimmune registry is still a work in progress. There is a huge absence of data in the autoimmune field – for example, no one knows with certainty just how many Americans have any of the various conditions, said Aaron H. Abend, the AARDA’s informatics director.
The registry would aggregate data already being compiled by various individual autoimmune associations. But the effort is in its infancy. The groups still need to agree on governance, data protocols, and other issues, Mr. Abend said. However, the registry will use software that is the standard for registries operated by the National Institutes of Health.
[email protected]
On Twitter @aliciaault
FROM A MEDIA BRIEFING BY THE AMERICAN AUTOIMMUNE RELATED DISEASES ASSOCIATION