User login
National three-digit suicide lifeline to take effect in 2022
Beginning in July 2022, Americans experiencing a mental health crisis will be able to dial 9-8-8 and be connected to the services and counselors at the National Suicide Prevention Lifeline.
The number was finalized when President Donald J. Trump signed the National Suicide Hotline Designation Act on Oct. 17. It completes what has been a multiyear effort by Republican and Democratic lawmakers to make it easier for individuals to reach out during mental health emergencies.
“When your house is on fire, you can get help by calling 9-1-1,” noted Rep. Seth Moulton (D-Mass.), a key sponsor of the legislation, in a statement. The new number “is a national step forward out of the shadows of stigma that prevent too many people from getting help and into a new era when mental health care is easy to get and normal to talk about,” said Rep. Moulton, a combat veteran who has openly discussed his struggles with PTSD.
The law requires the Department of Health & Human Services to develop a strategy to provide access to specialized services for high-risk populations such as LGBTQ youth, minorities, and people who live in rural areas.
“This law is a historic victory, as this is the first explicitly LGBTQ-inclusive bill to pass unanimously in history – and 9-8-8 will undoubtedly save countless lives,” said Sam Brinton, vice president of advocacy and government affairs for the Trevor Project, in a statement, also noting that “More than half of transgender and nonbinary youth having seriously considered it.”
Robert Gebbia, CEO of the American Foundation for Suicide Prevention, said in a statement: “This easy-to-remember number will increase public access to mental health and suicide prevention crisis resources, encourage help-seeking for individuals in need, and is a crucial entry point for establishing a continuum of crisis care.”
Mr. Gabbia called for more funding for local crisis centers to “respond to what we expect will be an increased call volume and provide effective crisis services to those in need when 9-8-8 is made available in July 2022.”
In 2017, then-Senator Orrin Hatch (R-Utah) and colleague Joe Donnelly (D-Ind.) pushed for a three-digit number for people having mental health crises. Their legislation passed in the Senate that fall and passed in the House in July 2018.
The bill directed the Federal Communications Commission to submit a report to Congress that would include a recommended number, a cost-benefit analysis comparing the three-digit code with the current hotline, and an assessment of how much it might cost service providers, states, local towns, and cities.
Mr. Trump signed that bill in 2018. The FCC unanimously approved the 9-8-8 number in July 2020.
Until the new number is active in July 2022, those in crisis should continue to call the National Suicide Lifeline at 1-800-273-TALK (8255).
A version of this article originally appeared on Medscape.com.
Beginning in July 2022, Americans experiencing a mental health crisis will be able to dial 9-8-8 and be connected to the services and counselors at the National Suicide Prevention Lifeline.
The number was finalized when President Donald J. Trump signed the National Suicide Hotline Designation Act on Oct. 17. It completes what has been a multiyear effort by Republican and Democratic lawmakers to make it easier for individuals to reach out during mental health emergencies.
“When your house is on fire, you can get help by calling 9-1-1,” noted Rep. Seth Moulton (D-Mass.), a key sponsor of the legislation, in a statement. The new number “is a national step forward out of the shadows of stigma that prevent too many people from getting help and into a new era when mental health care is easy to get and normal to talk about,” said Rep. Moulton, a combat veteran who has openly discussed his struggles with PTSD.
The law requires the Department of Health & Human Services to develop a strategy to provide access to specialized services for high-risk populations such as LGBTQ youth, minorities, and people who live in rural areas.
“This law is a historic victory, as this is the first explicitly LGBTQ-inclusive bill to pass unanimously in history – and 9-8-8 will undoubtedly save countless lives,” said Sam Brinton, vice president of advocacy and government affairs for the Trevor Project, in a statement, also noting that “More than half of transgender and nonbinary youth having seriously considered it.”
Robert Gebbia, CEO of the American Foundation for Suicide Prevention, said in a statement: “This easy-to-remember number will increase public access to mental health and suicide prevention crisis resources, encourage help-seeking for individuals in need, and is a crucial entry point for establishing a continuum of crisis care.”
Mr. Gabbia called for more funding for local crisis centers to “respond to what we expect will be an increased call volume and provide effective crisis services to those in need when 9-8-8 is made available in July 2022.”
In 2017, then-Senator Orrin Hatch (R-Utah) and colleague Joe Donnelly (D-Ind.) pushed for a three-digit number for people having mental health crises. Their legislation passed in the Senate that fall and passed in the House in July 2018.
The bill directed the Federal Communications Commission to submit a report to Congress that would include a recommended number, a cost-benefit analysis comparing the three-digit code with the current hotline, and an assessment of how much it might cost service providers, states, local towns, and cities.
Mr. Trump signed that bill in 2018. The FCC unanimously approved the 9-8-8 number in July 2020.
Until the new number is active in July 2022, those in crisis should continue to call the National Suicide Lifeline at 1-800-273-TALK (8255).
A version of this article originally appeared on Medscape.com.
Beginning in July 2022, Americans experiencing a mental health crisis will be able to dial 9-8-8 and be connected to the services and counselors at the National Suicide Prevention Lifeline.
The number was finalized when President Donald J. Trump signed the National Suicide Hotline Designation Act on Oct. 17. It completes what has been a multiyear effort by Republican and Democratic lawmakers to make it easier for individuals to reach out during mental health emergencies.
“When your house is on fire, you can get help by calling 9-1-1,” noted Rep. Seth Moulton (D-Mass.), a key sponsor of the legislation, in a statement. The new number “is a national step forward out of the shadows of stigma that prevent too many people from getting help and into a new era when mental health care is easy to get and normal to talk about,” said Rep. Moulton, a combat veteran who has openly discussed his struggles with PTSD.
The law requires the Department of Health & Human Services to develop a strategy to provide access to specialized services for high-risk populations such as LGBTQ youth, minorities, and people who live in rural areas.
“This law is a historic victory, as this is the first explicitly LGBTQ-inclusive bill to pass unanimously in history – and 9-8-8 will undoubtedly save countless lives,” said Sam Brinton, vice president of advocacy and government affairs for the Trevor Project, in a statement, also noting that “More than half of transgender and nonbinary youth having seriously considered it.”
Robert Gebbia, CEO of the American Foundation for Suicide Prevention, said in a statement: “This easy-to-remember number will increase public access to mental health and suicide prevention crisis resources, encourage help-seeking for individuals in need, and is a crucial entry point for establishing a continuum of crisis care.”
Mr. Gabbia called for more funding for local crisis centers to “respond to what we expect will be an increased call volume and provide effective crisis services to those in need when 9-8-8 is made available in July 2022.”
In 2017, then-Senator Orrin Hatch (R-Utah) and colleague Joe Donnelly (D-Ind.) pushed for a three-digit number for people having mental health crises. Their legislation passed in the Senate that fall and passed in the House in July 2018.
The bill directed the Federal Communications Commission to submit a report to Congress that would include a recommended number, a cost-benefit analysis comparing the three-digit code with the current hotline, and an assessment of how much it might cost service providers, states, local towns, and cities.
Mr. Trump signed that bill in 2018. The FCC unanimously approved the 9-8-8 number in July 2020.
Until the new number is active in July 2022, those in crisis should continue to call the National Suicide Lifeline at 1-800-273-TALK (8255).
A version of this article originally appeared on Medscape.com.
CMS gives hospitals 14 weeks to start daily COVID, flu reports
The federal government is giving hospitals 14 weeks to comply with daily reporting requirements for COVID-19.
The Centers for Medicare & Medicaid Services will send letters on October 7 to all 6,200 hospitals that receive reimbursement from the two federal health programs informing them of how well they are doing now, said CMS Administrator Seema Verma on a press call.
Verma would not give an estimate on how many hospitals are currently not compliant. But Deborah Birx, MD, a member of the White House Coronavirus Task Force, said on the call that 86% of hospitals are currently reporting daily.
Federal officials on the call also announced that hospitals would have the option to begin reporting certain data on influenza starting October 19, but that it would become mandatory a few weeks later.
The reporting is important “to really ensure that we’re triangulating all data to understand where this epidemic is, how it’s moving through different populations, and ensuring that we’re meeting the needs of specific hospitals and communities,” Birx said.
The federal government began a new hospital reporting system in April but did not require hospitals to participate until it quietly issued guidance in mid-July informing facilities that they should no longer report to the Centers for Disease Control and Prevention (CDC).
The move perplexed many public health experts and epidemiologists, who expressed concern that asking hospitals to use a new data system during a pandemic could result in delays and lost information. The new HHS data collection site, HHS Protect, is being managed by a private contractor, not the CDC, which also raised alarms.
The final CMS rule issued in August went into effect immediately, without any chance for comment or revision. CMS said at the time that the pandemic was reason enough to skip over the normal bureaucratic process.
Hospitals were not pleased. But Verma claimed that since then CMS had been working with hospital organizations on enforcement.
“We’re going to do everything we can to facilitate reporting, including an enforcement timeline that will provide hospitals ample opportunity to come into compliance,” she said.
Hospitals that do not comply will get a notice every 3 weeks. Three weeks after the second notice, they’ll get weekly notices for a month, and a final termination notice at 14 weeks.
The Federation of American Hospitals (FAH), however, said their members were still not happy. “It is both inappropriate and frankly overkill for CMS to tie compliance with reporting to Medicare conditions of participation,” said FAH President and CEO Chip Kahn in a statement. He called the CMS proposal “sledgehammer enforcement,” and said that the continuing data request might weaken hospitals’ response to the pandemic because it would divert time and money away from patient care.
Rick Pollack, president and CEO of the American Hospital Association called the CMS rule an “overly heavy-handed approach that could jeopardize access to hospital care for all Americans.” He noted in a statement that barring hospitals from Medicare and Medicaid could harm beneficiaries and the effort to provide COVID care.
Pollack also noted that AHA has “observed errors in data processing and confusion about exactly what was being requested at the hospital, state, contractor, and federal level, and has worked diligently with the federal agencies to identify and correct those problems.”
The document that lays out U.S. Department of Health and Human Services (HHS) Protect reporting requirements were updated again on October 6 to add influenza data. The hospitals must report on total patients with laboratory-confirmed flu; previous day’s flu admissions; total ICU patients with lab-confirmed flu; total inpatients with either flu or COVID-19; and the previous day’s deaths for flu and COVID.
CDC Director Robert Redfield, MD, said on the press call that the new data will give the agency crucial hospital-level information and perhaps better estimates of the flu burden. Flu trends have been tracked using the CDC’s Influenza Hospitalization Surveillance Network (FluSurv-NET), which will not be replaced, Redfield said. But that network only tracks hospitalizations in 14 states and does not provide information in “nearly real-time,” he said.
Having the new data “will give us a true situational awareness of severe respiratory illness, provide local hospitalization trends, and help direct resources such as antiretrovirals to address potential increased impact of flu and COVID cocirculation,” Redfield said.
This article first appeared on Medscape.com.
The federal government is giving hospitals 14 weeks to comply with daily reporting requirements for COVID-19.
The Centers for Medicare & Medicaid Services will send letters on October 7 to all 6,200 hospitals that receive reimbursement from the two federal health programs informing them of how well they are doing now, said CMS Administrator Seema Verma on a press call.
Verma would not give an estimate on how many hospitals are currently not compliant. But Deborah Birx, MD, a member of the White House Coronavirus Task Force, said on the call that 86% of hospitals are currently reporting daily.
Federal officials on the call also announced that hospitals would have the option to begin reporting certain data on influenza starting October 19, but that it would become mandatory a few weeks later.
The reporting is important “to really ensure that we’re triangulating all data to understand where this epidemic is, how it’s moving through different populations, and ensuring that we’re meeting the needs of specific hospitals and communities,” Birx said.
The federal government began a new hospital reporting system in April but did not require hospitals to participate until it quietly issued guidance in mid-July informing facilities that they should no longer report to the Centers for Disease Control and Prevention (CDC).
The move perplexed many public health experts and epidemiologists, who expressed concern that asking hospitals to use a new data system during a pandemic could result in delays and lost information. The new HHS data collection site, HHS Protect, is being managed by a private contractor, not the CDC, which also raised alarms.
The final CMS rule issued in August went into effect immediately, without any chance for comment or revision. CMS said at the time that the pandemic was reason enough to skip over the normal bureaucratic process.
Hospitals were not pleased. But Verma claimed that since then CMS had been working with hospital organizations on enforcement.
“We’re going to do everything we can to facilitate reporting, including an enforcement timeline that will provide hospitals ample opportunity to come into compliance,” she said.
Hospitals that do not comply will get a notice every 3 weeks. Three weeks after the second notice, they’ll get weekly notices for a month, and a final termination notice at 14 weeks.
The Federation of American Hospitals (FAH), however, said their members were still not happy. “It is both inappropriate and frankly overkill for CMS to tie compliance with reporting to Medicare conditions of participation,” said FAH President and CEO Chip Kahn in a statement. He called the CMS proposal “sledgehammer enforcement,” and said that the continuing data request might weaken hospitals’ response to the pandemic because it would divert time and money away from patient care.
Rick Pollack, president and CEO of the American Hospital Association called the CMS rule an “overly heavy-handed approach that could jeopardize access to hospital care for all Americans.” He noted in a statement that barring hospitals from Medicare and Medicaid could harm beneficiaries and the effort to provide COVID care.
Pollack also noted that AHA has “observed errors in data processing and confusion about exactly what was being requested at the hospital, state, contractor, and federal level, and has worked diligently with the federal agencies to identify and correct those problems.”
The document that lays out U.S. Department of Health and Human Services (HHS) Protect reporting requirements were updated again on October 6 to add influenza data. The hospitals must report on total patients with laboratory-confirmed flu; previous day’s flu admissions; total ICU patients with lab-confirmed flu; total inpatients with either flu or COVID-19; and the previous day’s deaths for flu and COVID.
CDC Director Robert Redfield, MD, said on the press call that the new data will give the agency crucial hospital-level information and perhaps better estimates of the flu burden. Flu trends have been tracked using the CDC’s Influenza Hospitalization Surveillance Network (FluSurv-NET), which will not be replaced, Redfield said. But that network only tracks hospitalizations in 14 states and does not provide information in “nearly real-time,” he said.
Having the new data “will give us a true situational awareness of severe respiratory illness, provide local hospitalization trends, and help direct resources such as antiretrovirals to address potential increased impact of flu and COVID cocirculation,” Redfield said.
This article first appeared on Medscape.com.
The federal government is giving hospitals 14 weeks to comply with daily reporting requirements for COVID-19.
The Centers for Medicare & Medicaid Services will send letters on October 7 to all 6,200 hospitals that receive reimbursement from the two federal health programs informing them of how well they are doing now, said CMS Administrator Seema Verma on a press call.
Verma would not give an estimate on how many hospitals are currently not compliant. But Deborah Birx, MD, a member of the White House Coronavirus Task Force, said on the call that 86% of hospitals are currently reporting daily.
Federal officials on the call also announced that hospitals would have the option to begin reporting certain data on influenza starting October 19, but that it would become mandatory a few weeks later.
The reporting is important “to really ensure that we’re triangulating all data to understand where this epidemic is, how it’s moving through different populations, and ensuring that we’re meeting the needs of specific hospitals and communities,” Birx said.
The federal government began a new hospital reporting system in April but did not require hospitals to participate until it quietly issued guidance in mid-July informing facilities that they should no longer report to the Centers for Disease Control and Prevention (CDC).
The move perplexed many public health experts and epidemiologists, who expressed concern that asking hospitals to use a new data system during a pandemic could result in delays and lost information. The new HHS data collection site, HHS Protect, is being managed by a private contractor, not the CDC, which also raised alarms.
The final CMS rule issued in August went into effect immediately, without any chance for comment or revision. CMS said at the time that the pandemic was reason enough to skip over the normal bureaucratic process.
Hospitals were not pleased. But Verma claimed that since then CMS had been working with hospital organizations on enforcement.
“We’re going to do everything we can to facilitate reporting, including an enforcement timeline that will provide hospitals ample opportunity to come into compliance,” she said.
Hospitals that do not comply will get a notice every 3 weeks. Three weeks after the second notice, they’ll get weekly notices for a month, and a final termination notice at 14 weeks.
The Federation of American Hospitals (FAH), however, said their members were still not happy. “It is both inappropriate and frankly overkill for CMS to tie compliance with reporting to Medicare conditions of participation,” said FAH President and CEO Chip Kahn in a statement. He called the CMS proposal “sledgehammer enforcement,” and said that the continuing data request might weaken hospitals’ response to the pandemic because it would divert time and money away from patient care.
Rick Pollack, president and CEO of the American Hospital Association called the CMS rule an “overly heavy-handed approach that could jeopardize access to hospital care for all Americans.” He noted in a statement that barring hospitals from Medicare and Medicaid could harm beneficiaries and the effort to provide COVID care.
Pollack also noted that AHA has “observed errors in data processing and confusion about exactly what was being requested at the hospital, state, contractor, and federal level, and has worked diligently with the federal agencies to identify and correct those problems.”
The document that lays out U.S. Department of Health and Human Services (HHS) Protect reporting requirements were updated again on October 6 to add influenza data. The hospitals must report on total patients with laboratory-confirmed flu; previous day’s flu admissions; total ICU patients with lab-confirmed flu; total inpatients with either flu or COVID-19; and the previous day’s deaths for flu and COVID.
CDC Director Robert Redfield, MD, said on the press call that the new data will give the agency crucial hospital-level information and perhaps better estimates of the flu burden. Flu trends have been tracked using the CDC’s Influenza Hospitalization Surveillance Network (FluSurv-NET), which will not be replaced, Redfield said. But that network only tracks hospitalizations in 14 states and does not provide information in “nearly real-time,” he said.
Having the new data “will give us a true situational awareness of severe respiratory illness, provide local hospitalization trends, and help direct resources such as antiretrovirals to address potential increased impact of flu and COVID cocirculation,” Redfield said.
This article first appeared on Medscape.com.
‘Overwhelming evidence’ FDA’s opioid approval process is shoddy
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
Despite the ongoing epidemic of misuse, overuse, and diversion of opioids, the Food and Drug Administration has set a low bar for approval of these medications over the past 20 years, new research suggests.
The study results also show that the FDA did not require manufacturers to collect safety data on tolerance, withdrawal, overdose, misuse, and diversion in any rigorous fashion.
In addition, during the study period, 17 of the 39 new drug applications (NDAs) (only one was an innovator product, known as a new molecular entity) for chronic pain were approved with an “enriched enrollment randomized withdrawal” (EERW) trial design. Such a design, in this case, allowed manufacturers to exclude 32%-43% of the initially enrolled patients from the double-blind treatment phase.
“The question for regulators, policy makers, and others is: How did we get to a point where these approvals took place based on trials that were by design unlikely to yield some of the most important information about safety and efficacy that patients and clinicians would care about?” study investigator G. Caleb Alexander, MD, Johns Hopkins University, Baltimore, said in an interview.
The study was published online Sept. 29 in the Annals of Internal Medicine.
‘Cooking the books’
Little is known about the evidence required by the FDA for new approvals of opioid analgesics.
To characterize the quality of safety and efficacy data in NDAs for opioid analgesics approved by the FDA between 1997 and 2018, the investigators conducted the cross-sectional analysis using data from ClinicalTrials.gov, FDA reviews, and peer-reviewed publications regarding phase 3 pivotal trials.
The investigators examined the key characteristics of each NDA, including the number, size, and duration of pivotal trials, trial control groups, use of EERW, and systematically measured safety outcomes.
Results showed that most of the 48 NDAs evaluated were for new dosage forms (52.1%) or new formulations (18.8%). Only one (2.1%) was for a new molecular entity.
Of 39 NDAs approved for the treatment of chronic pain, only 21 products were supported by at least one pivotal trial. The mean duration of these 28 trials was 84 days, and they enrolled a median of 299 patients.
Results showed that, for 17 of the 39 opioids approved for chronic pain, pivotal trials had an EERW design. For the latest period – 2012-2018 – trials of all eight of the approved opioids used the EERW method.
This EERW design allows the manufacturer to assess efficacy “among a subset of patients most likely to respond and least likely to have adverse effects, reducing generalizability to real-world settings,” the investigators noted.
They called on the FDA to stop relying on this type of trial to assess opioid efficacy.
In an August 2020 article, Andrew Kolodny, MD, pointed out the pitfalls of the EERW approach. In such a study, all participants are made physiologically dependent on the opioid in a 4- to 6-week open-label phase. Only those who tolerate the drug and find it helpful are included in the randomized study. Dr. Kolodny is codirector of opioid policy research at Brandeis University, Waltham, Mass.
“Critics of EERW have correctly described this methodology as ‘cooking the books,’ ” Dr. Kolodny writes.
He noted that the agency’s decision to rely on EERW trials for opioids was “based on discussions at private meetings between FDA officials and pharmaceutical company executives hosted by an organization called Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials.” The 2013 meetings were reported in an article published in the Washington Post.
Little sign of change
Among NDAs for chronic pain, the investigators found that eight (20.5%) included pooled safety reviews that reported systematic assessment of diversion. Seven (17.9%) reported systematic measurement of nonmedical use, and 15 (38.5%) assessed incident tolerance.
The study revealed that eight of nine products that were approved for acute pain were supported by at least one pivotal trial. The median duration of these 19 trials was 1 day, and they enrolled a median of 329 patients.
The investigators noted that the findings “underscore the evidence gaps that have limited clinicians’ and patients’ understanding and appreciation of the inherent risks of prescription opioid analgesics.”
Dr. Alexander, who has been an FDA advisory committee chairman and currently serves as a consultant to plaintiffs who are suing opioid manufacturers in federal multidistrict litigation, said the study “is a story about missed opportunities to improve the safety and to improve the regulatory review of these products.”
Coinvestigator Peter Lurie, MD, who was an official at the FDA from 2009 to 2017, said that “there’s not a lot of signs that things are changing” at the agency.
The study shows that the FDA has “accepted what the companies have been presenting,” said Dr. Lurie, who is president of the Center for Science in the Public Interest.
The FDA “absolutely has the authority” to require manufacturers to undertake more rigorous trials, but agency culture keeps it from making such demands, especially if doing so means a new applicant might have to conduct trials that weren’t previously required, Dr. Lurie said in an interview.
“FDA is pretty rigorous about trying to establish a level playing field. That’s a virtuous thing, but it becomes problematic when that prevents change,” said Dr. Lurie.
The most recent FDA guidance to manufacturers, issued in 2019, does not provide advice on criteria for endpoints, study duration, or which populations are most likely to benefit from opioid treatment. The agency also does not require drug manufacturers to formally collect data on safety, tolerance, overdose symptoms, or constipation.
The guidance does suggest that the agency would likely take into account public health considerations when evaluating opioids, such as the risk to the overall population for overdose and diversion.
‘Overwhelming evidence’
Dr. Kolodny said that, as far as he is aware, “this is the first scientific publication in a peer-reviewed journal demonstrating clearly the problems with FDA’s opioid approval process.”
The article offers “overwhelming evidence that they are improperly approving the most dangerous medications – medications that killed more people than any other medication on the market,” added Dr. Kolodny, who is also president of Physicians for Responsible Opioid Prescribing.
Asked to respond to the study findings, FDA spokesperson Charles Kohler said the agency “does not comment on specific studies but evaluates them as part of the body of evidence to further our understanding about a particular issue and assist in our mission to protect public health.”
A version of this article originally appeared on Medscape.com.
More U.S. states cap insulin cost, but activists will ‘fight harder’
Twelve U.S. states have now passed laws aimed at making insulin more affordable – and more than 30 are considering such legislation – but they all have gaps that still put the cost of this basic and essential medication out of reach for many with diabetes.
The laws only apply to health insurance through state-regulated plans, and not to the majority of health plans that cover most Americans: Medicare, Medicaid, the Veterans Affairs health system, or self-funded employer-sponsored plans.
Overall, Hannah Crabtree, an activist who writes the blog Data for Insulin, estimates state laws that limit copays, deductibles, or other out-of-pocket costs for insulin cover an average of 27% of people with diabetes across the United States.
And while diabetes activists have applauded state actions, most want more help for the under- and uninsured.
“Our chapter will be fighting harder next legislative session for the uninsured,” said Mindie Hooley, the leader of the Utah #insulin4all chapter, which successfully lobbied legislators to pass a bill signed by the state’s governor on March 30.
“With so many losing their jobs because of the pandemic, there’s no better time than now to fight for these patients who don’t have insurance,” Ms. Hooley said in an interview.
The American Diabetes Association has also been lobbying for state caps as one of many avenues for making insulin more affordable, said Stephen Habbe, the ADA’s director for state government affairs.
One in four insulin users report rationing the medication, Mr. Habbe said.
The state laws “can really provide important relief in terms of affordability for their insulin costs, which we know can be critical in terms of preserving their life and helping to prevent complications that can potentially be disabling or even deadly,” he said in an interview.
Activists with T1 International, which created the #insulin4all campaign, are working nationwide to convince state legislators to back measures that limit out-of-pocket costs for insulin, or for other diabetes medications and supplies.
Colorado, Connecticut, Delaware, Illinois, Maine, New Hampshire, New Mexico, New York, Utah, Virginia, Washington, and West Virginia have enacted such limits, with caps ranging from $25 to $100.
Insulin makers unfazed, blame insurers, PBMs for high prices
The three insulin manufacturers in the United States – Eli Lilly, Novo Nordisk, and Sanofi– have not overtly fought against the laws, although in July, the Pharmaceutical Research and Manufacturers of America did sue to block a related Minnesota law that provides a free emergency supply of insulin.
And the nonprofit news organization FairWarning reported in August that a lobbyist from Eli Lilly had attempted to push a Tennessee legislator to keep the uninsured from being eligible for any out-of-pocket limits.
The insulin makers have also not lowered prices in response to the mounting number of state laws.
They see no need, said Tara O’Neill Hayes, director of human welfare policy at the American Action Forum, a center right–leaning Washington, D.C., think tank.
“You’re going to do what you can get away with,” Ms. O’Neill Hayes said in an interview. “To the extent that they can keep their prices high and people are still buying, they have limited incentives to lower those costs.”
The insulin market is dysfunctional, she added. “The increasing cost of insulin seems primarily to be the result of a lack of competition in the market and convoluted drug pricing and insurance practices,” Ms. O’Neill Hayes and colleagues wrote in a report in April on federal and state attempts to address insulin affordability.
Novo Nordisk, however, maintains that drugmakers are not solely to blame.
“Everyone in the health care system has a role to play in affordability,” said Ken Inchausti, Novo Nordisk’s senior director for corporate communications. State legislation “attempts to address a systemic issue in [U.S.] health care: How benefit design can make medicines unaffordable for many, especially for those in high-deductible health plans,” he said in an interview.
“Efforts to place copay caps on insurance plans covering insulin can certainly help lower out-of-pocket costs,” said Mr. Inchausti.
Sanofi spokesperson Jon Florio said the company supports actions that increase affordable access to insulin. However, “while we support capped copays, we feel this should not be limited to just one class of medicines,” he said. Mr. Florio also noted that Sanofi provides out-of-pocket caps to anyone with commercial insurance and that anyone without insurance can buy one or multiple Sanofi insulins for a fixed price of $99 per month, up to 10 boxes of pens and/or 10-mL vials.
And Sanofi will take part in the Centers for Medicare & Medicaid Services’ new insulin demonstration program. Starting in 2021, CMS will cap insulin copays at $35 for people in Part D plans that participate.
Eli Lilly spokesperson Brad Jacklin said the company “believes in the common goal of ensuring affordable access to insulin and other life-saving medicines because nobody should have to forgo or ration because of cost.”
Lilly supports efforts “that more directly affect patients’ cost-sharing based on their health care coverage,” he said. Insurers and pharmacy benefit managers (PBMs) should pass savings on to patients, Mr. Jacklin urged. Lilly caps some insulins at $35 for the uninsured or commercially insured. The company will also participate in the CMS program.
Meanwhile, a PhRMA-sponsored website www.letstalkaboutcost.org said that, because they do not share savings, insurers and PBMs are responsible for high insulin costs.
Manufacturer assistance programs for patients with diabetes and other chronic diseases, on the other hand, can save individuals $300-$500 a year, PhRMA said in August.
PBMs point back at insulin manufacturers
PBMs, however, point back at drug companies. “PBMs have been able to moderate insulin costs for most consumers with insurance,” said J.C. Scott, president and CEO of the Pharmaceutical Care Management Association, the PBM trade group, in a statement.
The rising cost of insulin is caused by a lack of competition and overuse of patent extensions, PCMA maintains.
Health insurers, which, in tandem with PBMs, give insulins formulary preference based on a discounted price, are most likely to feel the impact of laws limiting out-of-pocket costs.
If they have to make up the shortfall from a patient’s reduced payment for a prescription, they will likely raise premiums, said Ms. O’Neill Hayes.
And if patients pay the same price for insulin – regardless of who makes it – drugmakers won’t have much incentive to offer discounts or rebates for formulary placement, she said. Again, that would likely lead to higher premiums.
David Allen, a spokesperson for America’s Health Insurance Plans, said in an interview that AHIP believes lack of competition has driven up insulin prices.
“High prices for insulin correspond with high health insurance costs for insulin,” he said. When CMS starts requiring drugmakers to discount their insulins for Medicare that will allow “health plans to use those savings to reduce out-of-pocket [costs] for seniors.”
He did not respond to a question as to why health insurers were not already passing savings on to commercially insured patients, especially in states with out-of-pocket limits.
Mr. Allen did say that AHIP’s plans “stand ready to work with state policymakers to remove barriers to lower insulin prices for Americans.”
Utah savings hopefully saving lives already
In Utah, legislators tuned out the blame game, and instead were keen to listen to patients, who had many stories about how the high cost of insulin had hurt them, said Ms. Hooley.
She noted an estimated 50,000 Utahans rely on insulin to stay alive.
Ms. Hooley and her chapter convinced legislators to pass a bill that gives insurers the option to cap patient copays at $30 per month, or to put insulin on its lowest formulary tier and waive any patient deductible. That aspect of the law does not go into effect until January 2021, but insurers are already starting to move insulin to the lowest formulary tier.
That has helped some people immediately. One state resident said her most recent insulin prescription cost $7 – instead of the usual $200.
The uninsured are not left totally high and dry either. Starting June 1, anyone in the state could buy through a state bulk-purchasing program, which guaranteed a 60% discount.
Ms. Hooley said she’d recently heard about a patient who usually spent $300 per prescription but was able to buy insulin for $100 through the program.
“Although $100 is still too much, it is nice knowing the Utah Insulin Savings Program is saving lives,” Ms. Hooley concluded.
A version of this article originally appeared on Medscape.com.
Twelve U.S. states have now passed laws aimed at making insulin more affordable – and more than 30 are considering such legislation – but they all have gaps that still put the cost of this basic and essential medication out of reach for many with diabetes.
The laws only apply to health insurance through state-regulated plans, and not to the majority of health plans that cover most Americans: Medicare, Medicaid, the Veterans Affairs health system, or self-funded employer-sponsored plans.
Overall, Hannah Crabtree, an activist who writes the blog Data for Insulin, estimates state laws that limit copays, deductibles, or other out-of-pocket costs for insulin cover an average of 27% of people with diabetes across the United States.
And while diabetes activists have applauded state actions, most want more help for the under- and uninsured.
“Our chapter will be fighting harder next legislative session for the uninsured,” said Mindie Hooley, the leader of the Utah #insulin4all chapter, which successfully lobbied legislators to pass a bill signed by the state’s governor on March 30.
“With so many losing their jobs because of the pandemic, there’s no better time than now to fight for these patients who don’t have insurance,” Ms. Hooley said in an interview.
The American Diabetes Association has also been lobbying for state caps as one of many avenues for making insulin more affordable, said Stephen Habbe, the ADA’s director for state government affairs.
One in four insulin users report rationing the medication, Mr. Habbe said.
The state laws “can really provide important relief in terms of affordability for their insulin costs, which we know can be critical in terms of preserving their life and helping to prevent complications that can potentially be disabling or even deadly,” he said in an interview.
Activists with T1 International, which created the #insulin4all campaign, are working nationwide to convince state legislators to back measures that limit out-of-pocket costs for insulin, or for other diabetes medications and supplies.
Colorado, Connecticut, Delaware, Illinois, Maine, New Hampshire, New Mexico, New York, Utah, Virginia, Washington, and West Virginia have enacted such limits, with caps ranging from $25 to $100.
Insulin makers unfazed, blame insurers, PBMs for high prices
The three insulin manufacturers in the United States – Eli Lilly, Novo Nordisk, and Sanofi– have not overtly fought against the laws, although in July, the Pharmaceutical Research and Manufacturers of America did sue to block a related Minnesota law that provides a free emergency supply of insulin.
And the nonprofit news organization FairWarning reported in August that a lobbyist from Eli Lilly had attempted to push a Tennessee legislator to keep the uninsured from being eligible for any out-of-pocket limits.
The insulin makers have also not lowered prices in response to the mounting number of state laws.
They see no need, said Tara O’Neill Hayes, director of human welfare policy at the American Action Forum, a center right–leaning Washington, D.C., think tank.
“You’re going to do what you can get away with,” Ms. O’Neill Hayes said in an interview. “To the extent that they can keep their prices high and people are still buying, they have limited incentives to lower those costs.”
The insulin market is dysfunctional, she added. “The increasing cost of insulin seems primarily to be the result of a lack of competition in the market and convoluted drug pricing and insurance practices,” Ms. O’Neill Hayes and colleagues wrote in a report in April on federal and state attempts to address insulin affordability.
Novo Nordisk, however, maintains that drugmakers are not solely to blame.
“Everyone in the health care system has a role to play in affordability,” said Ken Inchausti, Novo Nordisk’s senior director for corporate communications. State legislation “attempts to address a systemic issue in [U.S.] health care: How benefit design can make medicines unaffordable for many, especially for those in high-deductible health plans,” he said in an interview.
“Efforts to place copay caps on insurance plans covering insulin can certainly help lower out-of-pocket costs,” said Mr. Inchausti.
Sanofi spokesperson Jon Florio said the company supports actions that increase affordable access to insulin. However, “while we support capped copays, we feel this should not be limited to just one class of medicines,” he said. Mr. Florio also noted that Sanofi provides out-of-pocket caps to anyone with commercial insurance and that anyone without insurance can buy one or multiple Sanofi insulins for a fixed price of $99 per month, up to 10 boxes of pens and/or 10-mL vials.
And Sanofi will take part in the Centers for Medicare & Medicaid Services’ new insulin demonstration program. Starting in 2021, CMS will cap insulin copays at $35 for people in Part D plans that participate.
Eli Lilly spokesperson Brad Jacklin said the company “believes in the common goal of ensuring affordable access to insulin and other life-saving medicines because nobody should have to forgo or ration because of cost.”
Lilly supports efforts “that more directly affect patients’ cost-sharing based on their health care coverage,” he said. Insurers and pharmacy benefit managers (PBMs) should pass savings on to patients, Mr. Jacklin urged. Lilly caps some insulins at $35 for the uninsured or commercially insured. The company will also participate in the CMS program.
Meanwhile, a PhRMA-sponsored website www.letstalkaboutcost.org said that, because they do not share savings, insurers and PBMs are responsible for high insulin costs.
Manufacturer assistance programs for patients with diabetes and other chronic diseases, on the other hand, can save individuals $300-$500 a year, PhRMA said in August.
PBMs point back at insulin manufacturers
PBMs, however, point back at drug companies. “PBMs have been able to moderate insulin costs for most consumers with insurance,” said J.C. Scott, president and CEO of the Pharmaceutical Care Management Association, the PBM trade group, in a statement.
The rising cost of insulin is caused by a lack of competition and overuse of patent extensions, PCMA maintains.
Health insurers, which, in tandem with PBMs, give insulins formulary preference based on a discounted price, are most likely to feel the impact of laws limiting out-of-pocket costs.
If they have to make up the shortfall from a patient’s reduced payment for a prescription, they will likely raise premiums, said Ms. O’Neill Hayes.
And if patients pay the same price for insulin – regardless of who makes it – drugmakers won’t have much incentive to offer discounts or rebates for formulary placement, she said. Again, that would likely lead to higher premiums.
David Allen, a spokesperson for America’s Health Insurance Plans, said in an interview that AHIP believes lack of competition has driven up insulin prices.
“High prices for insulin correspond with high health insurance costs for insulin,” he said. When CMS starts requiring drugmakers to discount their insulins for Medicare that will allow “health plans to use those savings to reduce out-of-pocket [costs] for seniors.”
He did not respond to a question as to why health insurers were not already passing savings on to commercially insured patients, especially in states with out-of-pocket limits.
Mr. Allen did say that AHIP’s plans “stand ready to work with state policymakers to remove barriers to lower insulin prices for Americans.”
Utah savings hopefully saving lives already
In Utah, legislators tuned out the blame game, and instead were keen to listen to patients, who had many stories about how the high cost of insulin had hurt them, said Ms. Hooley.
She noted an estimated 50,000 Utahans rely on insulin to stay alive.
Ms. Hooley and her chapter convinced legislators to pass a bill that gives insurers the option to cap patient copays at $30 per month, or to put insulin on its lowest formulary tier and waive any patient deductible. That aspect of the law does not go into effect until January 2021, but insurers are already starting to move insulin to the lowest formulary tier.
That has helped some people immediately. One state resident said her most recent insulin prescription cost $7 – instead of the usual $200.
The uninsured are not left totally high and dry either. Starting June 1, anyone in the state could buy through a state bulk-purchasing program, which guaranteed a 60% discount.
Ms. Hooley said she’d recently heard about a patient who usually spent $300 per prescription but was able to buy insulin for $100 through the program.
“Although $100 is still too much, it is nice knowing the Utah Insulin Savings Program is saving lives,” Ms. Hooley concluded.
A version of this article originally appeared on Medscape.com.
Twelve U.S. states have now passed laws aimed at making insulin more affordable – and more than 30 are considering such legislation – but they all have gaps that still put the cost of this basic and essential medication out of reach for many with diabetes.
The laws only apply to health insurance through state-regulated plans, and not to the majority of health plans that cover most Americans: Medicare, Medicaid, the Veterans Affairs health system, or self-funded employer-sponsored plans.
Overall, Hannah Crabtree, an activist who writes the blog Data for Insulin, estimates state laws that limit copays, deductibles, or other out-of-pocket costs for insulin cover an average of 27% of people with diabetes across the United States.
And while diabetes activists have applauded state actions, most want more help for the under- and uninsured.
“Our chapter will be fighting harder next legislative session for the uninsured,” said Mindie Hooley, the leader of the Utah #insulin4all chapter, which successfully lobbied legislators to pass a bill signed by the state’s governor on March 30.
“With so many losing their jobs because of the pandemic, there’s no better time than now to fight for these patients who don’t have insurance,” Ms. Hooley said in an interview.
The American Diabetes Association has also been lobbying for state caps as one of many avenues for making insulin more affordable, said Stephen Habbe, the ADA’s director for state government affairs.
One in four insulin users report rationing the medication, Mr. Habbe said.
The state laws “can really provide important relief in terms of affordability for their insulin costs, which we know can be critical in terms of preserving their life and helping to prevent complications that can potentially be disabling or even deadly,” he said in an interview.
Activists with T1 International, which created the #insulin4all campaign, are working nationwide to convince state legislators to back measures that limit out-of-pocket costs for insulin, or for other diabetes medications and supplies.
Colorado, Connecticut, Delaware, Illinois, Maine, New Hampshire, New Mexico, New York, Utah, Virginia, Washington, and West Virginia have enacted such limits, with caps ranging from $25 to $100.
Insulin makers unfazed, blame insurers, PBMs for high prices
The three insulin manufacturers in the United States – Eli Lilly, Novo Nordisk, and Sanofi– have not overtly fought against the laws, although in July, the Pharmaceutical Research and Manufacturers of America did sue to block a related Minnesota law that provides a free emergency supply of insulin.
And the nonprofit news organization FairWarning reported in August that a lobbyist from Eli Lilly had attempted to push a Tennessee legislator to keep the uninsured from being eligible for any out-of-pocket limits.
The insulin makers have also not lowered prices in response to the mounting number of state laws.
They see no need, said Tara O’Neill Hayes, director of human welfare policy at the American Action Forum, a center right–leaning Washington, D.C., think tank.
“You’re going to do what you can get away with,” Ms. O’Neill Hayes said in an interview. “To the extent that they can keep their prices high and people are still buying, they have limited incentives to lower those costs.”
The insulin market is dysfunctional, she added. “The increasing cost of insulin seems primarily to be the result of a lack of competition in the market and convoluted drug pricing and insurance practices,” Ms. O’Neill Hayes and colleagues wrote in a report in April on federal and state attempts to address insulin affordability.
Novo Nordisk, however, maintains that drugmakers are not solely to blame.
“Everyone in the health care system has a role to play in affordability,” said Ken Inchausti, Novo Nordisk’s senior director for corporate communications. State legislation “attempts to address a systemic issue in [U.S.] health care: How benefit design can make medicines unaffordable for many, especially for those in high-deductible health plans,” he said in an interview.
“Efforts to place copay caps on insurance plans covering insulin can certainly help lower out-of-pocket costs,” said Mr. Inchausti.
Sanofi spokesperson Jon Florio said the company supports actions that increase affordable access to insulin. However, “while we support capped copays, we feel this should not be limited to just one class of medicines,” he said. Mr. Florio also noted that Sanofi provides out-of-pocket caps to anyone with commercial insurance and that anyone without insurance can buy one or multiple Sanofi insulins for a fixed price of $99 per month, up to 10 boxes of pens and/or 10-mL vials.
And Sanofi will take part in the Centers for Medicare & Medicaid Services’ new insulin demonstration program. Starting in 2021, CMS will cap insulin copays at $35 for people in Part D plans that participate.
Eli Lilly spokesperson Brad Jacklin said the company “believes in the common goal of ensuring affordable access to insulin and other life-saving medicines because nobody should have to forgo or ration because of cost.”
Lilly supports efforts “that more directly affect patients’ cost-sharing based on their health care coverage,” he said. Insurers and pharmacy benefit managers (PBMs) should pass savings on to patients, Mr. Jacklin urged. Lilly caps some insulins at $35 for the uninsured or commercially insured. The company will also participate in the CMS program.
Meanwhile, a PhRMA-sponsored website www.letstalkaboutcost.org said that, because they do not share savings, insurers and PBMs are responsible for high insulin costs.
Manufacturer assistance programs for patients with diabetes and other chronic diseases, on the other hand, can save individuals $300-$500 a year, PhRMA said in August.
PBMs point back at insulin manufacturers
PBMs, however, point back at drug companies. “PBMs have been able to moderate insulin costs for most consumers with insurance,” said J.C. Scott, president and CEO of the Pharmaceutical Care Management Association, the PBM trade group, in a statement.
The rising cost of insulin is caused by a lack of competition and overuse of patent extensions, PCMA maintains.
Health insurers, which, in tandem with PBMs, give insulins formulary preference based on a discounted price, are most likely to feel the impact of laws limiting out-of-pocket costs.
If they have to make up the shortfall from a patient’s reduced payment for a prescription, they will likely raise premiums, said Ms. O’Neill Hayes.
And if patients pay the same price for insulin – regardless of who makes it – drugmakers won’t have much incentive to offer discounts or rebates for formulary placement, she said. Again, that would likely lead to higher premiums.
David Allen, a spokesperson for America’s Health Insurance Plans, said in an interview that AHIP believes lack of competition has driven up insulin prices.
“High prices for insulin correspond with high health insurance costs for insulin,” he said. When CMS starts requiring drugmakers to discount their insulins for Medicare that will allow “health plans to use those savings to reduce out-of-pocket [costs] for seniors.”
He did not respond to a question as to why health insurers were not already passing savings on to commercially insured patients, especially in states with out-of-pocket limits.
Mr. Allen did say that AHIP’s plans “stand ready to work with state policymakers to remove barriers to lower insulin prices for Americans.”
Utah savings hopefully saving lives already
In Utah, legislators tuned out the blame game, and instead were keen to listen to patients, who had many stories about how the high cost of insulin had hurt them, said Ms. Hooley.
She noted an estimated 50,000 Utahans rely on insulin to stay alive.
Ms. Hooley and her chapter convinced legislators to pass a bill that gives insurers the option to cap patient copays at $30 per month, or to put insulin on its lowest formulary tier and waive any patient deductible. That aspect of the law does not go into effect until January 2021, but insurers are already starting to move insulin to the lowest formulary tier.
That has helped some people immediately. One state resident said her most recent insulin prescription cost $7 – instead of the usual $200.
The uninsured are not left totally high and dry either. Starting June 1, anyone in the state could buy through a state bulk-purchasing program, which guaranteed a 60% discount.
Ms. Hooley said she’d recently heard about a patient who usually spent $300 per prescription but was able to buy insulin for $100 through the program.
“Although $100 is still too much, it is nice knowing the Utah Insulin Savings Program is saving lives,” Ms. Hooley concluded.
A version of this article originally appeared on Medscape.com.
Petition seeks to oust AAD president-elect, citing private equity conflicts
A make him too conflicted for the job.
The petition, created anonymously, appeared in early August and is seeking 1,500 signatures – calculated as the number needed to initiate a vote to recall Mark Kaufmann, MD. Dr. Kaufmann was voted president-elect of the AAD and its sister organization, the AAD Association, in April. He takes the position in 2021 and would become president in 2022.
The petition objects to the fact that Dr. Kaufmann is the chief medical officer of Advanced Dermatology and Cosmetic Surgery (ADCS), the nation’s largest private equity–backed dermatology group. It claims that he took the position in July, after being elected, which it portrays as dishonest.
The petition said Dr. Kaufmann “will have concurrent fiduciary responsibilities to both the AAD and a corporation whose interests may or may not be aligned with the AAD.” Even if Dr. Kaufmann chose to recuse himself from some decisions, that would be a disservice to the AAD, said the petition, which added that he “cannot serve two masters simultaneously.”
Several efforts were made to reach Dr. Kaufmann for a comment, with no responses at press time. At press time, ACDS had not responded to a request for comment.
In response to questions, Bruce H. Thiers, MD, president of the AAD/A, said that the organization has no policy barring officers from holding capital in a private equity (PE)–backed corporation, but that any elected officer is subject to the organization’s “fiduciary duties and obligations.”
The AAD/A shared a 7-page administrative regulation on disclosure of outside interests and management of conflicts of interest. The policy notes that employment by a private equity group is considered a potential conflict of interest, but so is employment by a government agency, solo practice, academic medical center, or multiple other models. Key leaders, including the president, president-elect, and immediate past president, are required to divest themselves of any direct financial relationships with industry during their entire term.
Members who do not disclose potential conflicts each year and who fail to update their disclosure within 30 days of acquiring a new financial relationship “will lose the right to hold office, serve in the governance structure and, except in unusual circumstances approved in advance by the Board of Directors, to participate in Academy programs,” according to the policy.
Petitioners lament conflicts, private equity
At press time, the petition had more than 1,100 signatures. Most who signed indicated in their comments that they believed that Dr. Kaufmann’s association with private equity disqualifies him.
“I believe private equity should not have a place at the table of the governing body of the AAD,” commented Cynthia Abbott, MD, an Atlanta dermatologist. In his comment, Ron Birnbaum, MD a Los Angeles–based dermatologist, wrote, “I oppose the movement to PE-based purchase and consolidation of practices,” adding that he had not voted for Dr. Kaufmann in April. Dr. Kaufmann “might resolve the conflict of interest by resigning from the job of CMO of ADCS,” wrote Dr. Birnbaum.
“I have great respect for Dr. Kaufmann but am very troubled by the influence of PE infiltration into dermatology,” Mark Gaughan, MD, a dermatologist in Durango, Colo., wrote in the petition.
The petition seeks 1,500 signatures – which is 10% of the AAD membership. That’s key because, as per AAD administrative rules, members can initiate the removal of a board member through a petition that is signed by 10% of voting members or by a two-thirds vote of entire board of directors.
Dr. Thiers said the AAD/A’s “administrative regulations do not cover the removal of an elected officer prior to the start of his or her term.” Thus, it’s not even clear that Dr. Kaufmann could be recalled before he took office in 2021.
Dr. Kaufmann previously served on the AAD/A board of directors for 4 years and is currently deputy chair of the AAD/A’s Patient Access and Payer Relations Committee. He is chair of the AAD’s Workgroup on Innovation in Payment and Delivery Actinic Keratosis Alternative Payment Model Development and is a member of numerous other AAD/A committees, including: the AAD budget committee; the AAD appointment selection committee; the Resource-Based Relative Value Scale and Current Procedural Terminology committee; the work group on innovation in payment and delivery; the work group on ICD-10; and the work group on rapid response team Medicare Physician Fee Schedule.
Since March 2019, Dr. Kaufmann has also served as the chief medical officer of Florham Park, N.J.–based MoleSafe, a company that provides full-body skin cancer screening directly to patients.
In an interview, former AAD president Daniel Siegel, MD, said that he believes the petition is an unwarranted attack. “Mark is an honest upstanding individual who has, in the almost 2 decades I’ve known and worked with him, always put the interests of the specialty and the AAD ahead of any personal interests,” said Dr. Siegel of the department of dermatology at State University of New York, Brooklyn. Dr. Siegel also disclosed that he is chief compliance officer for the Florida-based Skin and Cancer Associates, a large group of practices owned by private equity.
Dr. Kaufmann is “an objective person who has no difficulty declaring a conflict where there is one,” Dr. Siegel said.
But Sailesh Konda, MD, a critic of private equity in dermatology, who signed the petition, said in an interview that he believed the “membership is rightfully concerned and responding to these new conflicts of interest with a valid petition.”
“This is readily apparent with a petition signed by more than 1,000 dermatologists,” added Dr. Konda of the department of dermatology at the University of Florida in Gainesville.
It might be hard to erase all potential conflicts at the AAD. Some members work for industry, some for academia, and some for government agencies – all of which come with their own biases.
But the AAD will not publicly release disclosures for members, board members, or officers. Those disclosures are compiled in an internal AAD database, but the organization leaves it up to each individual to decide what they will make public.
Second anonymous conflict petition
It is not clear what will happen with the Dr. Kaufmann recall effort, but it is not the first time that a petition has taken aim at an AAD official. An October 2019 petition – also submitted by an anonymous dermatologist – sought to remove Scott M. Dinehart, MD, from the AAD board.
The petition noted Dr. Dinehart’s involvement in creating the American Dermatology Board of Physician Assistants, a group that aims to offer board certification to PAs who work with dermatologists. Dr. Dinehart’s “concurrent relationships with both organizations is a major conflict of interest,” said the petition, which garnered some 4,200 signatures – far in excess of what is required to initiate a removal vote.
That led to a unanimous decision by the AAD/A board to present the membership with a resolution to remove Dr. Dinehart. Some 6,400 votes were cast, with 97% approving Dr. Dinehart’s removal.
He is no longer a member of the AAD/A board.
A make him too conflicted for the job.
The petition, created anonymously, appeared in early August and is seeking 1,500 signatures – calculated as the number needed to initiate a vote to recall Mark Kaufmann, MD. Dr. Kaufmann was voted president-elect of the AAD and its sister organization, the AAD Association, in April. He takes the position in 2021 and would become president in 2022.
The petition objects to the fact that Dr. Kaufmann is the chief medical officer of Advanced Dermatology and Cosmetic Surgery (ADCS), the nation’s largest private equity–backed dermatology group. It claims that he took the position in July, after being elected, which it portrays as dishonest.
The petition said Dr. Kaufmann “will have concurrent fiduciary responsibilities to both the AAD and a corporation whose interests may or may not be aligned with the AAD.” Even if Dr. Kaufmann chose to recuse himself from some decisions, that would be a disservice to the AAD, said the petition, which added that he “cannot serve two masters simultaneously.”
Several efforts were made to reach Dr. Kaufmann for a comment, with no responses at press time. At press time, ACDS had not responded to a request for comment.
In response to questions, Bruce H. Thiers, MD, president of the AAD/A, said that the organization has no policy barring officers from holding capital in a private equity (PE)–backed corporation, but that any elected officer is subject to the organization’s “fiduciary duties and obligations.”
The AAD/A shared a 7-page administrative regulation on disclosure of outside interests and management of conflicts of interest. The policy notes that employment by a private equity group is considered a potential conflict of interest, but so is employment by a government agency, solo practice, academic medical center, or multiple other models. Key leaders, including the president, president-elect, and immediate past president, are required to divest themselves of any direct financial relationships with industry during their entire term.
Members who do not disclose potential conflicts each year and who fail to update their disclosure within 30 days of acquiring a new financial relationship “will lose the right to hold office, serve in the governance structure and, except in unusual circumstances approved in advance by the Board of Directors, to participate in Academy programs,” according to the policy.
Petitioners lament conflicts, private equity
At press time, the petition had more than 1,100 signatures. Most who signed indicated in their comments that they believed that Dr. Kaufmann’s association with private equity disqualifies him.
“I believe private equity should not have a place at the table of the governing body of the AAD,” commented Cynthia Abbott, MD, an Atlanta dermatologist. In his comment, Ron Birnbaum, MD a Los Angeles–based dermatologist, wrote, “I oppose the movement to PE-based purchase and consolidation of practices,” adding that he had not voted for Dr. Kaufmann in April. Dr. Kaufmann “might resolve the conflict of interest by resigning from the job of CMO of ADCS,” wrote Dr. Birnbaum.
“I have great respect for Dr. Kaufmann but am very troubled by the influence of PE infiltration into dermatology,” Mark Gaughan, MD, a dermatologist in Durango, Colo., wrote in the petition.
The petition seeks 1,500 signatures – which is 10% of the AAD membership. That’s key because, as per AAD administrative rules, members can initiate the removal of a board member through a petition that is signed by 10% of voting members or by a two-thirds vote of entire board of directors.
Dr. Thiers said the AAD/A’s “administrative regulations do not cover the removal of an elected officer prior to the start of his or her term.” Thus, it’s not even clear that Dr. Kaufmann could be recalled before he took office in 2021.
Dr. Kaufmann previously served on the AAD/A board of directors for 4 years and is currently deputy chair of the AAD/A’s Patient Access and Payer Relations Committee. He is chair of the AAD’s Workgroup on Innovation in Payment and Delivery Actinic Keratosis Alternative Payment Model Development and is a member of numerous other AAD/A committees, including: the AAD budget committee; the AAD appointment selection committee; the Resource-Based Relative Value Scale and Current Procedural Terminology committee; the work group on innovation in payment and delivery; the work group on ICD-10; and the work group on rapid response team Medicare Physician Fee Schedule.
Since March 2019, Dr. Kaufmann has also served as the chief medical officer of Florham Park, N.J.–based MoleSafe, a company that provides full-body skin cancer screening directly to patients.
In an interview, former AAD president Daniel Siegel, MD, said that he believes the petition is an unwarranted attack. “Mark is an honest upstanding individual who has, in the almost 2 decades I’ve known and worked with him, always put the interests of the specialty and the AAD ahead of any personal interests,” said Dr. Siegel of the department of dermatology at State University of New York, Brooklyn. Dr. Siegel also disclosed that he is chief compliance officer for the Florida-based Skin and Cancer Associates, a large group of practices owned by private equity.
Dr. Kaufmann is “an objective person who has no difficulty declaring a conflict where there is one,” Dr. Siegel said.
But Sailesh Konda, MD, a critic of private equity in dermatology, who signed the petition, said in an interview that he believed the “membership is rightfully concerned and responding to these new conflicts of interest with a valid petition.”
“This is readily apparent with a petition signed by more than 1,000 dermatologists,” added Dr. Konda of the department of dermatology at the University of Florida in Gainesville.
It might be hard to erase all potential conflicts at the AAD. Some members work for industry, some for academia, and some for government agencies – all of which come with their own biases.
But the AAD will not publicly release disclosures for members, board members, or officers. Those disclosures are compiled in an internal AAD database, but the organization leaves it up to each individual to decide what they will make public.
Second anonymous conflict petition
It is not clear what will happen with the Dr. Kaufmann recall effort, but it is not the first time that a petition has taken aim at an AAD official. An October 2019 petition – also submitted by an anonymous dermatologist – sought to remove Scott M. Dinehart, MD, from the AAD board.
The petition noted Dr. Dinehart’s involvement in creating the American Dermatology Board of Physician Assistants, a group that aims to offer board certification to PAs who work with dermatologists. Dr. Dinehart’s “concurrent relationships with both organizations is a major conflict of interest,” said the petition, which garnered some 4,200 signatures – far in excess of what is required to initiate a removal vote.
That led to a unanimous decision by the AAD/A board to present the membership with a resolution to remove Dr. Dinehart. Some 6,400 votes were cast, with 97% approving Dr. Dinehart’s removal.
He is no longer a member of the AAD/A board.
A make him too conflicted for the job.
The petition, created anonymously, appeared in early August and is seeking 1,500 signatures – calculated as the number needed to initiate a vote to recall Mark Kaufmann, MD. Dr. Kaufmann was voted president-elect of the AAD and its sister organization, the AAD Association, in April. He takes the position in 2021 and would become president in 2022.
The petition objects to the fact that Dr. Kaufmann is the chief medical officer of Advanced Dermatology and Cosmetic Surgery (ADCS), the nation’s largest private equity–backed dermatology group. It claims that he took the position in July, after being elected, which it portrays as dishonest.
The petition said Dr. Kaufmann “will have concurrent fiduciary responsibilities to both the AAD and a corporation whose interests may or may not be aligned with the AAD.” Even if Dr. Kaufmann chose to recuse himself from some decisions, that would be a disservice to the AAD, said the petition, which added that he “cannot serve two masters simultaneously.”
Several efforts were made to reach Dr. Kaufmann for a comment, with no responses at press time. At press time, ACDS had not responded to a request for comment.
In response to questions, Bruce H. Thiers, MD, president of the AAD/A, said that the organization has no policy barring officers from holding capital in a private equity (PE)–backed corporation, but that any elected officer is subject to the organization’s “fiduciary duties and obligations.”
The AAD/A shared a 7-page administrative regulation on disclosure of outside interests and management of conflicts of interest. The policy notes that employment by a private equity group is considered a potential conflict of interest, but so is employment by a government agency, solo practice, academic medical center, or multiple other models. Key leaders, including the president, president-elect, and immediate past president, are required to divest themselves of any direct financial relationships with industry during their entire term.
Members who do not disclose potential conflicts each year and who fail to update their disclosure within 30 days of acquiring a new financial relationship “will lose the right to hold office, serve in the governance structure and, except in unusual circumstances approved in advance by the Board of Directors, to participate in Academy programs,” according to the policy.
Petitioners lament conflicts, private equity
At press time, the petition had more than 1,100 signatures. Most who signed indicated in their comments that they believed that Dr. Kaufmann’s association with private equity disqualifies him.
“I believe private equity should not have a place at the table of the governing body of the AAD,” commented Cynthia Abbott, MD, an Atlanta dermatologist. In his comment, Ron Birnbaum, MD a Los Angeles–based dermatologist, wrote, “I oppose the movement to PE-based purchase and consolidation of practices,” adding that he had not voted for Dr. Kaufmann in April. Dr. Kaufmann “might resolve the conflict of interest by resigning from the job of CMO of ADCS,” wrote Dr. Birnbaum.
“I have great respect for Dr. Kaufmann but am very troubled by the influence of PE infiltration into dermatology,” Mark Gaughan, MD, a dermatologist in Durango, Colo., wrote in the petition.
The petition seeks 1,500 signatures – which is 10% of the AAD membership. That’s key because, as per AAD administrative rules, members can initiate the removal of a board member through a petition that is signed by 10% of voting members or by a two-thirds vote of entire board of directors.
Dr. Thiers said the AAD/A’s “administrative regulations do not cover the removal of an elected officer prior to the start of his or her term.” Thus, it’s not even clear that Dr. Kaufmann could be recalled before he took office in 2021.
Dr. Kaufmann previously served on the AAD/A board of directors for 4 years and is currently deputy chair of the AAD/A’s Patient Access and Payer Relations Committee. He is chair of the AAD’s Workgroup on Innovation in Payment and Delivery Actinic Keratosis Alternative Payment Model Development and is a member of numerous other AAD/A committees, including: the AAD budget committee; the AAD appointment selection committee; the Resource-Based Relative Value Scale and Current Procedural Terminology committee; the work group on innovation in payment and delivery; the work group on ICD-10; and the work group on rapid response team Medicare Physician Fee Schedule.
Since March 2019, Dr. Kaufmann has also served as the chief medical officer of Florham Park, N.J.–based MoleSafe, a company that provides full-body skin cancer screening directly to patients.
In an interview, former AAD president Daniel Siegel, MD, said that he believes the petition is an unwarranted attack. “Mark is an honest upstanding individual who has, in the almost 2 decades I’ve known and worked with him, always put the interests of the specialty and the AAD ahead of any personal interests,” said Dr. Siegel of the department of dermatology at State University of New York, Brooklyn. Dr. Siegel also disclosed that he is chief compliance officer for the Florida-based Skin and Cancer Associates, a large group of practices owned by private equity.
Dr. Kaufmann is “an objective person who has no difficulty declaring a conflict where there is one,” Dr. Siegel said.
But Sailesh Konda, MD, a critic of private equity in dermatology, who signed the petition, said in an interview that he believed the “membership is rightfully concerned and responding to these new conflicts of interest with a valid petition.”
“This is readily apparent with a petition signed by more than 1,000 dermatologists,” added Dr. Konda of the department of dermatology at the University of Florida in Gainesville.
It might be hard to erase all potential conflicts at the AAD. Some members work for industry, some for academia, and some for government agencies – all of which come with their own biases.
But the AAD will not publicly release disclosures for members, board members, or officers. Those disclosures are compiled in an internal AAD database, but the organization leaves it up to each individual to decide what they will make public.
Second anonymous conflict petition
It is not clear what will happen with the Dr. Kaufmann recall effort, but it is not the first time that a petition has taken aim at an AAD official. An October 2019 petition – also submitted by an anonymous dermatologist – sought to remove Scott M. Dinehart, MD, from the AAD board.
The petition noted Dr. Dinehart’s involvement in creating the American Dermatology Board of Physician Assistants, a group that aims to offer board certification to PAs who work with dermatologists. Dr. Dinehart’s “concurrent relationships with both organizations is a major conflict of interest,” said the petition, which garnered some 4,200 signatures – far in excess of what is required to initiate a removal vote.
That led to a unanimous decision by the AAD/A board to present the membership with a resolution to remove Dr. Dinehart. Some 6,400 votes were cast, with 97% approving Dr. Dinehart’s removal.
He is no longer a member of the AAD/A board.
Convalescent plasma actions spark trial recruitment concerns
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
Addiction specialist charged in $681 million treatment fraud case
The federal government has charged a Florida addiction medicine specialist in what it says was a scheme to defraud Medicare and private insurers, charging them roughly $681 million over about a decade for lab tests, office visits, therapy sessions, and other services that were either unnecessary or never delivered.
The Department of Justice and the Attorney for the Southern District of Florida are prosecuting Michael Ligotti, DO, 46, saying that he preyed on individuals seeking substance abuse treatment. They have yet to issue a formal indictment.
“The substance abuse treatment fraud allegedly perpetrated by the defendant sacrificed the genuine care of vulnerable patients at a time when they urgently needed a trusted health care provider,” U.S. Attorney Ariana Fajardo Orshan, Southern District of Florida, said in a statement.
“Health care providers who allow greed to take precedence over their Hippocratic Oath and participate in these schemes are criminals and will be held accountable for their unscrupulous conduct,” she added.
Dr. Ligotti was charged July 31. The prosecutors were seeking to detain him until trial. However, a judge approved his bond today and he is free on bond, according to Ligotti’s attorney, Ben Curtis.
“As is always the case with any criminal matter, the burden of proof rests entirely with the government,” Mr. Curtis said in an interview.
“In this instance, we do not believe the US Department of Justice’s claims – and that is exactly what they are at this point, just one-sided claims – will reconcile with actual evidence at a future trial,” he said.
Mr. Curtis added that Dr. Ligotti “looks forward to establishing his innocence.”
Unnecessary urine tests
The government alleges that Dr. Ligotti played a central role in a scheme in which Medicare and private insurers paid about $121 million to cover some $680 million in charges from 2011 to 2020.
According to the prosecutors, Dr. Ligotti received a fee for becoming a “purported” medical director of about 50 addiction treatment facilities and sober homes – and that he issued 136 separate standing orders for medically unnecessary urinalysis (UA) tests.
The labs allegedly paid occasional kickbacks to the facilities and homes, and those facilities in turn were required to have their patients treated by Dr. Ligotti’s clinic, Whole Health, which is based in Delray Beach, Fla.
This allowed Dr. Ligotti to “bill hundreds of millions of dollars in additional fraudulent treatments, including unnecessary and expensive UAs, costly blood tests, nonexistent therapy sessions, office visits, and other unnecessary services, regardless of whether such treatment and testing were medically necessary and/or actually provided,” alleges the government.
Urine tests have been exploited before by addiction treatment clinics as a revenue generator. Kaiser Health News reported in 2017 that a single nurse practitioner at one pain clinic in Tennessee generated $1 million in billings to Medicare for drug-related urine tests in a single year.
Also in 2017, The New York Times reported that a single patient had been billed $260,000 for urine tests by his treatment center.
The federal government alleges that Dr. Ligotti also “billed for psychiatric services and therapy sessions that never happened, and that he and his staff were not qualified to conduct.”
In addition, they assert that Dr. Ligotti improperly prescribed controlled substances, including large quantities of buprenorphine/Suboxone, often exceeding the number of patients he was legally authorized to treat or giving it to patients who did not require the medications.
Dr. Ligotti may not be practicing any longer. His clinic’s website features a message that the practice will be closed as of Aug. 7.
This article first appeared on Medscape.com.
The federal government has charged a Florida addiction medicine specialist in what it says was a scheme to defraud Medicare and private insurers, charging them roughly $681 million over about a decade for lab tests, office visits, therapy sessions, and other services that were either unnecessary or never delivered.
The Department of Justice and the Attorney for the Southern District of Florida are prosecuting Michael Ligotti, DO, 46, saying that he preyed on individuals seeking substance abuse treatment. They have yet to issue a formal indictment.
“The substance abuse treatment fraud allegedly perpetrated by the defendant sacrificed the genuine care of vulnerable patients at a time when they urgently needed a trusted health care provider,” U.S. Attorney Ariana Fajardo Orshan, Southern District of Florida, said in a statement.
“Health care providers who allow greed to take precedence over their Hippocratic Oath and participate in these schemes are criminals and will be held accountable for their unscrupulous conduct,” she added.
Dr. Ligotti was charged July 31. The prosecutors were seeking to detain him until trial. However, a judge approved his bond today and he is free on bond, according to Ligotti’s attorney, Ben Curtis.
“As is always the case with any criminal matter, the burden of proof rests entirely with the government,” Mr. Curtis said in an interview.
“In this instance, we do not believe the US Department of Justice’s claims – and that is exactly what they are at this point, just one-sided claims – will reconcile with actual evidence at a future trial,” he said.
Mr. Curtis added that Dr. Ligotti “looks forward to establishing his innocence.”
Unnecessary urine tests
The government alleges that Dr. Ligotti played a central role in a scheme in which Medicare and private insurers paid about $121 million to cover some $680 million in charges from 2011 to 2020.
According to the prosecutors, Dr. Ligotti received a fee for becoming a “purported” medical director of about 50 addiction treatment facilities and sober homes – and that he issued 136 separate standing orders for medically unnecessary urinalysis (UA) tests.
The labs allegedly paid occasional kickbacks to the facilities and homes, and those facilities in turn were required to have their patients treated by Dr. Ligotti’s clinic, Whole Health, which is based in Delray Beach, Fla.
This allowed Dr. Ligotti to “bill hundreds of millions of dollars in additional fraudulent treatments, including unnecessary and expensive UAs, costly blood tests, nonexistent therapy sessions, office visits, and other unnecessary services, regardless of whether such treatment and testing were medically necessary and/or actually provided,” alleges the government.
Urine tests have been exploited before by addiction treatment clinics as a revenue generator. Kaiser Health News reported in 2017 that a single nurse practitioner at one pain clinic in Tennessee generated $1 million in billings to Medicare for drug-related urine tests in a single year.
Also in 2017, The New York Times reported that a single patient had been billed $260,000 for urine tests by his treatment center.
The federal government alleges that Dr. Ligotti also “billed for psychiatric services and therapy sessions that never happened, and that he and his staff were not qualified to conduct.”
In addition, they assert that Dr. Ligotti improperly prescribed controlled substances, including large quantities of buprenorphine/Suboxone, often exceeding the number of patients he was legally authorized to treat or giving it to patients who did not require the medications.
Dr. Ligotti may not be practicing any longer. His clinic’s website features a message that the practice will be closed as of Aug. 7.
This article first appeared on Medscape.com.
The federal government has charged a Florida addiction medicine specialist in what it says was a scheme to defraud Medicare and private insurers, charging them roughly $681 million over about a decade for lab tests, office visits, therapy sessions, and other services that were either unnecessary or never delivered.
The Department of Justice and the Attorney for the Southern District of Florida are prosecuting Michael Ligotti, DO, 46, saying that he preyed on individuals seeking substance abuse treatment. They have yet to issue a formal indictment.
“The substance abuse treatment fraud allegedly perpetrated by the defendant sacrificed the genuine care of vulnerable patients at a time when they urgently needed a trusted health care provider,” U.S. Attorney Ariana Fajardo Orshan, Southern District of Florida, said in a statement.
“Health care providers who allow greed to take precedence over their Hippocratic Oath and participate in these schemes are criminals and will be held accountable for their unscrupulous conduct,” she added.
Dr. Ligotti was charged July 31. The prosecutors were seeking to detain him until trial. However, a judge approved his bond today and he is free on bond, according to Ligotti’s attorney, Ben Curtis.
“As is always the case with any criminal matter, the burden of proof rests entirely with the government,” Mr. Curtis said in an interview.
“In this instance, we do not believe the US Department of Justice’s claims – and that is exactly what they are at this point, just one-sided claims – will reconcile with actual evidence at a future trial,” he said.
Mr. Curtis added that Dr. Ligotti “looks forward to establishing his innocence.”
Unnecessary urine tests
The government alleges that Dr. Ligotti played a central role in a scheme in which Medicare and private insurers paid about $121 million to cover some $680 million in charges from 2011 to 2020.
According to the prosecutors, Dr. Ligotti received a fee for becoming a “purported” medical director of about 50 addiction treatment facilities and sober homes – and that he issued 136 separate standing orders for medically unnecessary urinalysis (UA) tests.
The labs allegedly paid occasional kickbacks to the facilities and homes, and those facilities in turn were required to have their patients treated by Dr. Ligotti’s clinic, Whole Health, which is based in Delray Beach, Fla.
This allowed Dr. Ligotti to “bill hundreds of millions of dollars in additional fraudulent treatments, including unnecessary and expensive UAs, costly blood tests, nonexistent therapy sessions, office visits, and other unnecessary services, regardless of whether such treatment and testing were medically necessary and/or actually provided,” alleges the government.
Urine tests have been exploited before by addiction treatment clinics as a revenue generator. Kaiser Health News reported in 2017 that a single nurse practitioner at one pain clinic in Tennessee generated $1 million in billings to Medicare for drug-related urine tests in a single year.
Also in 2017, The New York Times reported that a single patient had been billed $260,000 for urine tests by his treatment center.
The federal government alleges that Dr. Ligotti also “billed for psychiatric services and therapy sessions that never happened, and that he and his staff were not qualified to conduct.”
In addition, they assert that Dr. Ligotti improperly prescribed controlled substances, including large quantities of buprenorphine/Suboxone, often exceeding the number of patients he was legally authorized to treat or giving it to patients who did not require the medications.
Dr. Ligotti may not be practicing any longer. His clinic’s website features a message that the practice will be closed as of Aug. 7.
This article first appeared on Medscape.com.
Move over supplements, here come medical foods
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
Big pharma sues to block Minnesota insulin affordability law
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
#WhiteCoats4BlackLives: A ‘platform for good’
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
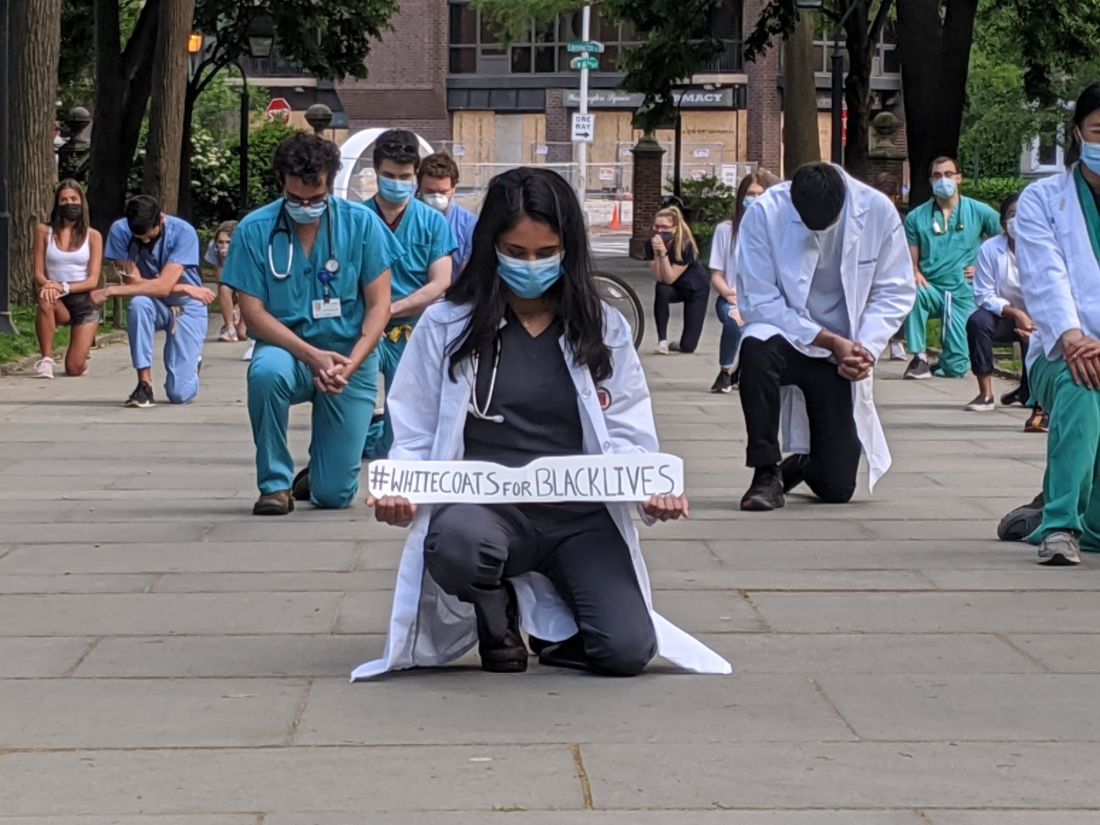
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
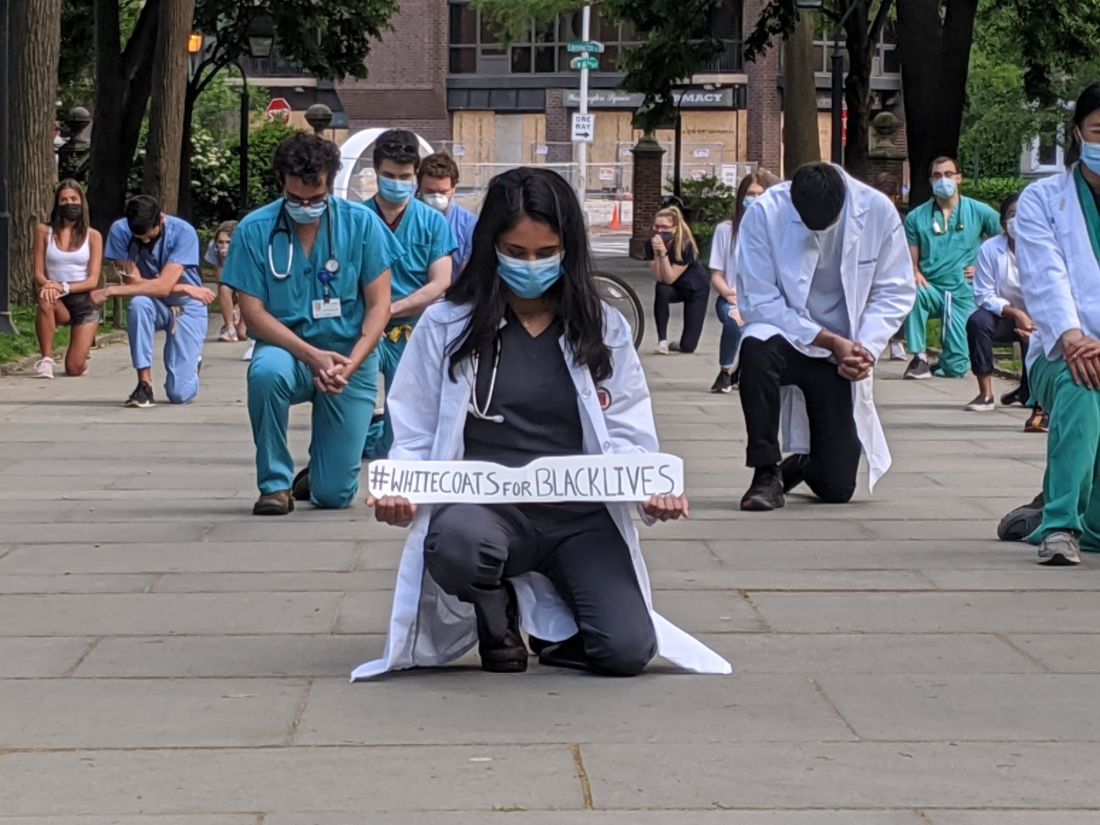
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
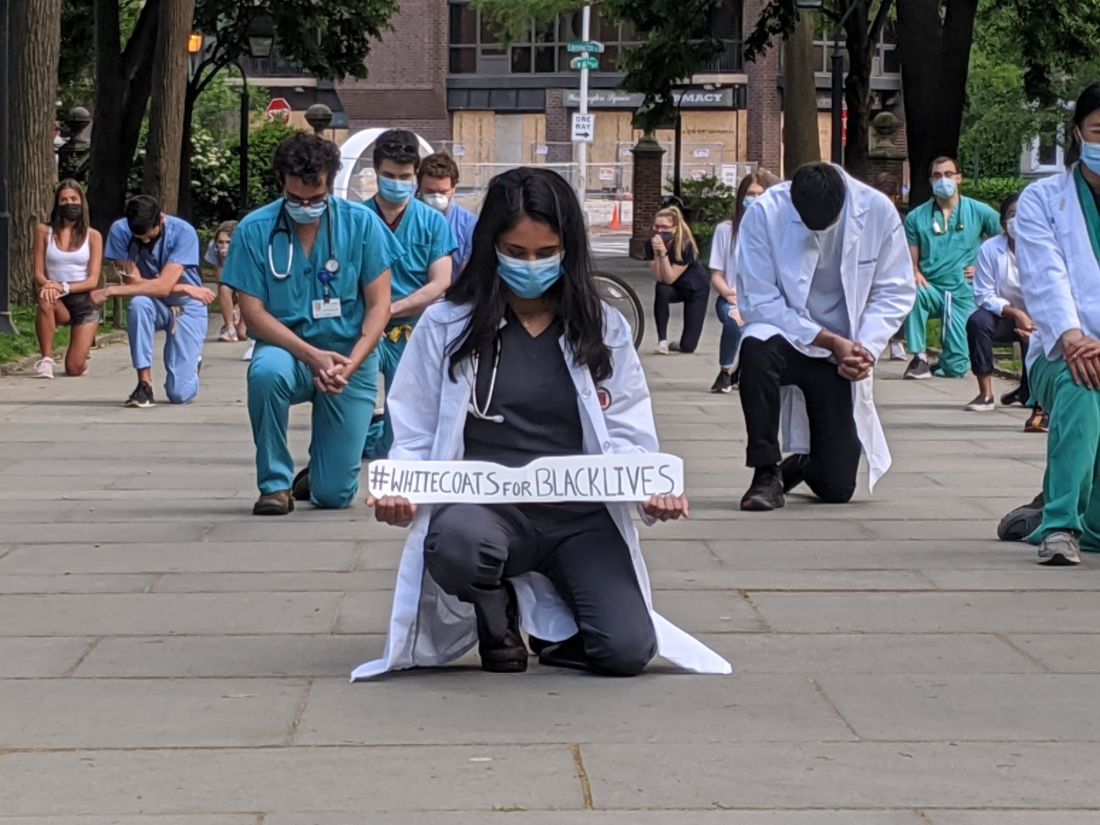
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.