User login
Psychiatrist alleges plagiarism by journal editor
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
Feds look to retrofit factories to increase COVID vaccine production
The Biden administration is exploring whether factories can be retrofitted to produce more of the Pfizer/BioNTech and Moderna COVID-19 mRNA vaccines to speed up vaccination of the vast majority of Americans.
The announcement comes as the nation is on track to see 479,000-514,000 deaths by the end of February, said Rochelle Walensky, MD, the director of the Centers for Disease Control and Prevention.
Dr. Walensky, speaking to reporters Wednesday in the first briefing from the White House COVID-19 Response Team, said that 1.6 million COVID-19 shots had been administered each day over the past week and that 3.4 million Americans have been fully vaccinated with two doses.
More than 500 million doses will be needed to vaccinate every American older than 16 years, Andy Slavitt, the senior advisor to the COVID-19 response team, told reporters. Pfizer and Moderna are due to deliver an additional 200 million doses near the end of March, and President Biden is seeking to purchase another 200 million doses from the companies, said Mr. Slavitt.
But it may not be enough. Whether companies can retrofit factories to produce vaccines is “something that’s under active exploration,” Mr. Slavitt said.
“This is a national emergency,” said Jeff Zients, the White House COVID-19 response coordinator. “Everything is on the table across the whole supply chain,” he said. He noted that the administration was also buying low-dead-space syringes to help extract an additional sixth dose from every Pfizer vial.
Mr. Slavitt said the team had identified 12 areas in which Mr. Biden was authorized to use the Defense Production Act to spur the manufacture of items such as masks and COVID-19 diagnostics.
More sequencing needed
As new variants emerge, vaccine makers and the CDC are racing to stay a step ahead. “RNA viruses mutate all the time – that’s what they do, that’s their business,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and Mr. Biden’s chief medical adviser, in the briefing.
Three concerning variants have emerged: the B117, which is circulating widely in the United Kingdom; the B1.351 in South Africa; and the P.1 in Brazil. As of Jan. 26, no cases involving the B1.351 variant have been detected in the United States; one person with the P.1 variant was identified in Minnesota. The CDC has identified 308 cases of the U.K. variant in 26 states, said Dr. Walensky.
The United States is dismally behind in surveillance and sequencing of variants, said Zients. “We are 43rd in the world at genomic sequencing,” which he said was “totally unacceptable.”
Dr. Walensky said the CDC is working on improving data collection and sequencing, but she said more money is needed to “do the amount of sequencing and surveillance that we need in order to be able to detect these when they first start to emerge.”
Both she and Mr. Zients called on Congress to pass Mr. Biden’s proposed American Rescue package, which includes more money for sequencing.
Dr. Fauci said the National Institutes of Health was collaborating with the CDC to determine whether other newly emerging variants pose any threat – such as increased transmissibility or lethality or some other functional characteristic. Scientists will also monitor “in real-time” whether current vaccines continue to make neutralizing antibodies against these mutants.
“With the U.K. variant, what we’re seeing is a very slight, if at all, impact on vaccine-induced antibodies and very little impact on anything else,” he said. With the South African variant, there is “a multifold diminution in the in vitro neutralization by vaccine-induced antibodies,” but “it still is well within the cushion of protection” for the current vaccines.
But, he added, “we have to be concerned looking forward of what the further evolution of this might be.” The anti-COVID monoclonal antibodies – bamlanivimab and the combination of casirivimab and imdevimab – are “more seriously inhibited by this South African strain,” which is spurring development of new monoclonals.
Dr. Fauci also noted that the Johnson & Johnson/Janssen vaccine that is in development – for which phase 3 data may be released within days – was tested in South Africa and Brazil in addition to the United States. The comparative data could help researchers and clinicians make better-informed decisions about what vaccine to use if the South African variant “seeds itself in the U.S.”
A version of this article first appeared on Medscape.com.
The Biden administration is exploring whether factories can be retrofitted to produce more of the Pfizer/BioNTech and Moderna COVID-19 mRNA vaccines to speed up vaccination of the vast majority of Americans.
The announcement comes as the nation is on track to see 479,000-514,000 deaths by the end of February, said Rochelle Walensky, MD, the director of the Centers for Disease Control and Prevention.
Dr. Walensky, speaking to reporters Wednesday in the first briefing from the White House COVID-19 Response Team, said that 1.6 million COVID-19 shots had been administered each day over the past week and that 3.4 million Americans have been fully vaccinated with two doses.
More than 500 million doses will be needed to vaccinate every American older than 16 years, Andy Slavitt, the senior advisor to the COVID-19 response team, told reporters. Pfizer and Moderna are due to deliver an additional 200 million doses near the end of March, and President Biden is seeking to purchase another 200 million doses from the companies, said Mr. Slavitt.
But it may not be enough. Whether companies can retrofit factories to produce vaccines is “something that’s under active exploration,” Mr. Slavitt said.
“This is a national emergency,” said Jeff Zients, the White House COVID-19 response coordinator. “Everything is on the table across the whole supply chain,” he said. He noted that the administration was also buying low-dead-space syringes to help extract an additional sixth dose from every Pfizer vial.
Mr. Slavitt said the team had identified 12 areas in which Mr. Biden was authorized to use the Defense Production Act to spur the manufacture of items such as masks and COVID-19 diagnostics.
More sequencing needed
As new variants emerge, vaccine makers and the CDC are racing to stay a step ahead. “RNA viruses mutate all the time – that’s what they do, that’s their business,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and Mr. Biden’s chief medical adviser, in the briefing.
Three concerning variants have emerged: the B117, which is circulating widely in the United Kingdom; the B1.351 in South Africa; and the P.1 in Brazil. As of Jan. 26, no cases involving the B1.351 variant have been detected in the United States; one person with the P.1 variant was identified in Minnesota. The CDC has identified 308 cases of the U.K. variant in 26 states, said Dr. Walensky.
The United States is dismally behind in surveillance and sequencing of variants, said Zients. “We are 43rd in the world at genomic sequencing,” which he said was “totally unacceptable.”
Dr. Walensky said the CDC is working on improving data collection and sequencing, but she said more money is needed to “do the amount of sequencing and surveillance that we need in order to be able to detect these when they first start to emerge.”
Both she and Mr. Zients called on Congress to pass Mr. Biden’s proposed American Rescue package, which includes more money for sequencing.
Dr. Fauci said the National Institutes of Health was collaborating with the CDC to determine whether other newly emerging variants pose any threat – such as increased transmissibility or lethality or some other functional characteristic. Scientists will also monitor “in real-time” whether current vaccines continue to make neutralizing antibodies against these mutants.
“With the U.K. variant, what we’re seeing is a very slight, if at all, impact on vaccine-induced antibodies and very little impact on anything else,” he said. With the South African variant, there is “a multifold diminution in the in vitro neutralization by vaccine-induced antibodies,” but “it still is well within the cushion of protection” for the current vaccines.
But, he added, “we have to be concerned looking forward of what the further evolution of this might be.” The anti-COVID monoclonal antibodies – bamlanivimab and the combination of casirivimab and imdevimab – are “more seriously inhibited by this South African strain,” which is spurring development of new monoclonals.
Dr. Fauci also noted that the Johnson & Johnson/Janssen vaccine that is in development – for which phase 3 data may be released within days – was tested in South Africa and Brazil in addition to the United States. The comparative data could help researchers and clinicians make better-informed decisions about what vaccine to use if the South African variant “seeds itself in the U.S.”
A version of this article first appeared on Medscape.com.
The Biden administration is exploring whether factories can be retrofitted to produce more of the Pfizer/BioNTech and Moderna COVID-19 mRNA vaccines to speed up vaccination of the vast majority of Americans.
The announcement comes as the nation is on track to see 479,000-514,000 deaths by the end of February, said Rochelle Walensky, MD, the director of the Centers for Disease Control and Prevention.
Dr. Walensky, speaking to reporters Wednesday in the first briefing from the White House COVID-19 Response Team, said that 1.6 million COVID-19 shots had been administered each day over the past week and that 3.4 million Americans have been fully vaccinated with two doses.
More than 500 million doses will be needed to vaccinate every American older than 16 years, Andy Slavitt, the senior advisor to the COVID-19 response team, told reporters. Pfizer and Moderna are due to deliver an additional 200 million doses near the end of March, and President Biden is seeking to purchase another 200 million doses from the companies, said Mr. Slavitt.
But it may not be enough. Whether companies can retrofit factories to produce vaccines is “something that’s under active exploration,” Mr. Slavitt said.
“This is a national emergency,” said Jeff Zients, the White House COVID-19 response coordinator. “Everything is on the table across the whole supply chain,” he said. He noted that the administration was also buying low-dead-space syringes to help extract an additional sixth dose from every Pfizer vial.
Mr. Slavitt said the team had identified 12 areas in which Mr. Biden was authorized to use the Defense Production Act to spur the manufacture of items such as masks and COVID-19 diagnostics.
More sequencing needed
As new variants emerge, vaccine makers and the CDC are racing to stay a step ahead. “RNA viruses mutate all the time – that’s what they do, that’s their business,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and Mr. Biden’s chief medical adviser, in the briefing.
Three concerning variants have emerged: the B117, which is circulating widely in the United Kingdom; the B1.351 in South Africa; and the P.1 in Brazil. As of Jan. 26, no cases involving the B1.351 variant have been detected in the United States; one person with the P.1 variant was identified in Minnesota. The CDC has identified 308 cases of the U.K. variant in 26 states, said Dr. Walensky.
The United States is dismally behind in surveillance and sequencing of variants, said Zients. “We are 43rd in the world at genomic sequencing,” which he said was “totally unacceptable.”
Dr. Walensky said the CDC is working on improving data collection and sequencing, but she said more money is needed to “do the amount of sequencing and surveillance that we need in order to be able to detect these when they first start to emerge.”
Both she and Mr. Zients called on Congress to pass Mr. Biden’s proposed American Rescue package, which includes more money for sequencing.
Dr. Fauci said the National Institutes of Health was collaborating with the CDC to determine whether other newly emerging variants pose any threat – such as increased transmissibility or lethality or some other functional characteristic. Scientists will also monitor “in real-time” whether current vaccines continue to make neutralizing antibodies against these mutants.
“With the U.K. variant, what we’re seeing is a very slight, if at all, impact on vaccine-induced antibodies and very little impact on anything else,” he said. With the South African variant, there is “a multifold diminution in the in vitro neutralization by vaccine-induced antibodies,” but “it still is well within the cushion of protection” for the current vaccines.
But, he added, “we have to be concerned looking forward of what the further evolution of this might be.” The anti-COVID monoclonal antibodies – bamlanivimab and the combination of casirivimab and imdevimab – are “more seriously inhibited by this South African strain,” which is spurring development of new monoclonals.
Dr. Fauci also noted that the Johnson & Johnson/Janssen vaccine that is in development – for which phase 3 data may be released within days – was tested in South Africa and Brazil in addition to the United States. The comparative data could help researchers and clinicians make better-informed decisions about what vaccine to use if the South African variant “seeds itself in the U.S.”
A version of this article first appeared on Medscape.com.
Are there COVID-19–related ‘long-haul’ skin issues?
– as a result of infection with or exposure to the SARS-CoV-2 virus, but some dermatologists question if the skin signs and symptoms are truly related.
In their commentary in the Lancet Infectious Diseases, Esther P. Freeman, MD, PhD, and colleagues who lead and participate in the American Academy of Dermatology’s international registry said their analysis “revealed a previously unreported subset of patients who experience long-haul symptoms in dermatology-dominant COVID-19.”
Some of the data was presented at the 29th European Academy of Dermatology and Venereology in late October 2020, but has since been updated with more cases.
Dermatologists who spoke with this news organization said it has not been settled that some skin manifestations – such as pernio/chilblains rashes, seen primarily in nonhospitalized patients, and described in the registry – are definitively caused by COVID. They also noted that in some cases, patients who initially test negative for COVID-19 by polymerase chain reaction (PCR) sometimes do not ever develop antibodies, which could mean they were never actually exposed to SARS-CoV-2.
“I still question whether the perniosis is directly related to infection with SARS-CoV-2 or not,” said Anthony Fernandez, MD, PhD, director of medical and inpatient dermatology and assistant professor of dermatopathology at the Cleveland Clinic. His uncertainty is driven by the lack of seroconversion and that few cases were seen over the summer in the United States – suggesting that it may still be a result of cold temperatures.
“I’m not sure there is a definitive correct answer, definitely not that everyone would agree on,” said Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn.
Dr. Freeman, however, believed that pernio and especially persistent lesions are caused by an immune response to COVID.
In an interview, she noted the multiple cases of patients in the registry who did seroconvert and that, while a registry is not a perfect means of getting an answer, it is good for generating questions. Taken collectively, the cases in the registry can “tell a story for further hypotheses,” said Dr. Freeman, who is director of global health dermatology at Massachusetts General Hospital and assistant professor of dermatology at Harvard University, both in Boston.
“We were noticing this signal across the world” that patients “developed these toe lesions and they never got better,” said Dr. Freeman. Generally, people who experience pernio, also described as COVID toes or “COVID fingers,” recover in 4-8 weeks. But in the registry, “we did have this subset of patients who really were experiencing these very longstanding symptoms,” she added.
Two patients with lab-confirmed COVID have had long-lasting pernio of 133 days and 150 days. “I’m caring for a cohort in Boston who have had long COVID of the skin and symptoms for over 10 months,” Dr. Freeman said.
Pernio dominates
The registry – a collaboration between the AAD and the International League of Dermatological Societies – was launched in April 2020. Any medical professional can enter case information. From April to October, 1,030 total cases and 331 laboratory-confirmed or suspected COVID-19 cases with dermatological manifestations were entered from 41 countries.
Most of the cases were just recorded at a single time point, which is an acknowledged limitation of the study.
Dr. Freeman and colleagues reached out to registry participants in June and August to get updates on COVID lab test results and sign and symptom duration. Overall, 234 total and 96 lab-confirmed COVID infections had more lengthy data about sign and symptom duration.
Pernio lasted a median of 15 days in patients with suspected disease and 12 days for those with lab-confirmed COVID, compared with a median of 7 days for morbilliform eruptions, 4 days for urticarial eruptions, and 20 days for papulosquamous eruptions – all in patients with lab-confirmed disease.
Of the 103 cases of pernio, 7 had symptoms lasting more than 60 days. Only two of those seven patients had lab-confirmed COVID. Initially, the one patient tested negative with nasopharyngeal PCR, and serum IgM and IgG. Six weeks after pernio onset, the patient – still experiencing fatigue and pernio – seroconverted to anti–SARS-CoV-2 IgM positivity.
The other long-haul patient, after a negative PCR, tested positive for SARS-CoV-2 serum IgG 1 month after pernio onset.
Robust immune response?
Dr. Freeman said these patients might have a very high interferon response initially to the virus, which makes for a mild to nonexistent disease, but could create inflammation elsewhere. “I almost view the toes as an innocent bystander of a robust immune response to SARS-CoV-2.”
Although he has not seen extended pernio or other skin manifestations in his patients, Dr. Fernandez said the interferon hypothesis is “fair,” and “the best that’s out there.” Dr. Fernandez is currently studying cutaneous manifestations of COVID-19 as a principal investigator of a trial sponsored by the Clinical and Translational Science Collaborative of Cleveland.
Dr. Ko said in an interview that she has not observed long-haul skin issues in her patients, but Yale colleagues have.
In a study, she and Yale colleagues published in September, SARS-CoV-2 spike protein was detected in perniotic lesions, but not nuclear protein or viral RNA. The test they used – immunohistochemistry – can be nonspecific, which muddied results.
She does not think there is replicating virus in the skin or the lesions. Instead, said Dr. Ko, “either there is viral spike protein that has somehow become disassociated from actively replicating virus that somehow got deposited in endothelial cells,” or the staining “was spurious,” or some other protein is cross-reacting. “And the people who are unlucky enough to have that protein in their endothelial cells can manifest this COVID-toe, COVID-finger phenomenon.”
To her, it’s an unsolved mystery. “The weird thing is, we’ve never before had this much perniosis,” Dr. Ko said.
Dr. Fernandez is not convinced yet, noting that, in Cleveland, more pernio cases were observed in March and April than in the summer. “If it is a manifestation of the infection then you also need the right environment, the cold weather for this manifestation to present,” he said. “Or, it really isn’t a direct manifestation of COVID-19 but may be more related to other factors,” such as lifestyle changes related to limitations implemented to help mitigate the spread of the disease.
“To me the jury is still out whether or not the perniotic lesions really can tell us something about a patient’s exposure and infection with SARS-CoV-2,” he said.
Dr. Freeman reported receiving a grant from the International League of Dermatological Societies and nonfinancial support from the AAD for the study. Dr. Ko reported no conflicts. Dr. Fernadnez had no disclosures.
– as a result of infection with or exposure to the SARS-CoV-2 virus, but some dermatologists question if the skin signs and symptoms are truly related.
In their commentary in the Lancet Infectious Diseases, Esther P. Freeman, MD, PhD, and colleagues who lead and participate in the American Academy of Dermatology’s international registry said their analysis “revealed a previously unreported subset of patients who experience long-haul symptoms in dermatology-dominant COVID-19.”
Some of the data was presented at the 29th European Academy of Dermatology and Venereology in late October 2020, but has since been updated with more cases.
Dermatologists who spoke with this news organization said it has not been settled that some skin manifestations – such as pernio/chilblains rashes, seen primarily in nonhospitalized patients, and described in the registry – are definitively caused by COVID. They also noted that in some cases, patients who initially test negative for COVID-19 by polymerase chain reaction (PCR) sometimes do not ever develop antibodies, which could mean they were never actually exposed to SARS-CoV-2.
“I still question whether the perniosis is directly related to infection with SARS-CoV-2 or not,” said Anthony Fernandez, MD, PhD, director of medical and inpatient dermatology and assistant professor of dermatopathology at the Cleveland Clinic. His uncertainty is driven by the lack of seroconversion and that few cases were seen over the summer in the United States – suggesting that it may still be a result of cold temperatures.
“I’m not sure there is a definitive correct answer, definitely not that everyone would agree on,” said Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn.
Dr. Freeman, however, believed that pernio and especially persistent lesions are caused by an immune response to COVID.
In an interview, she noted the multiple cases of patients in the registry who did seroconvert and that, while a registry is not a perfect means of getting an answer, it is good for generating questions. Taken collectively, the cases in the registry can “tell a story for further hypotheses,” said Dr. Freeman, who is director of global health dermatology at Massachusetts General Hospital and assistant professor of dermatology at Harvard University, both in Boston.
“We were noticing this signal across the world” that patients “developed these toe lesions and they never got better,” said Dr. Freeman. Generally, people who experience pernio, also described as COVID toes or “COVID fingers,” recover in 4-8 weeks. But in the registry, “we did have this subset of patients who really were experiencing these very longstanding symptoms,” she added.
Two patients with lab-confirmed COVID have had long-lasting pernio of 133 days and 150 days. “I’m caring for a cohort in Boston who have had long COVID of the skin and symptoms for over 10 months,” Dr. Freeman said.
Pernio dominates
The registry – a collaboration between the AAD and the International League of Dermatological Societies – was launched in April 2020. Any medical professional can enter case information. From April to October, 1,030 total cases and 331 laboratory-confirmed or suspected COVID-19 cases with dermatological manifestations were entered from 41 countries.
Most of the cases were just recorded at a single time point, which is an acknowledged limitation of the study.
Dr. Freeman and colleagues reached out to registry participants in June and August to get updates on COVID lab test results and sign and symptom duration. Overall, 234 total and 96 lab-confirmed COVID infections had more lengthy data about sign and symptom duration.
Pernio lasted a median of 15 days in patients with suspected disease and 12 days for those with lab-confirmed COVID, compared with a median of 7 days for morbilliform eruptions, 4 days for urticarial eruptions, and 20 days for papulosquamous eruptions – all in patients with lab-confirmed disease.
Of the 103 cases of pernio, 7 had symptoms lasting more than 60 days. Only two of those seven patients had lab-confirmed COVID. Initially, the one patient tested negative with nasopharyngeal PCR, and serum IgM and IgG. Six weeks after pernio onset, the patient – still experiencing fatigue and pernio – seroconverted to anti–SARS-CoV-2 IgM positivity.
The other long-haul patient, after a negative PCR, tested positive for SARS-CoV-2 serum IgG 1 month after pernio onset.
Robust immune response?
Dr. Freeman said these patients might have a very high interferon response initially to the virus, which makes for a mild to nonexistent disease, but could create inflammation elsewhere. “I almost view the toes as an innocent bystander of a robust immune response to SARS-CoV-2.”
Although he has not seen extended pernio or other skin manifestations in his patients, Dr. Fernandez said the interferon hypothesis is “fair,” and “the best that’s out there.” Dr. Fernandez is currently studying cutaneous manifestations of COVID-19 as a principal investigator of a trial sponsored by the Clinical and Translational Science Collaborative of Cleveland.
Dr. Ko said in an interview that she has not observed long-haul skin issues in her patients, but Yale colleagues have.
In a study, she and Yale colleagues published in September, SARS-CoV-2 spike protein was detected in perniotic lesions, but not nuclear protein or viral RNA. The test they used – immunohistochemistry – can be nonspecific, which muddied results.
She does not think there is replicating virus in the skin or the lesions. Instead, said Dr. Ko, “either there is viral spike protein that has somehow become disassociated from actively replicating virus that somehow got deposited in endothelial cells,” or the staining “was spurious,” or some other protein is cross-reacting. “And the people who are unlucky enough to have that protein in their endothelial cells can manifest this COVID-toe, COVID-finger phenomenon.”
To her, it’s an unsolved mystery. “The weird thing is, we’ve never before had this much perniosis,” Dr. Ko said.
Dr. Fernandez is not convinced yet, noting that, in Cleveland, more pernio cases were observed in March and April than in the summer. “If it is a manifestation of the infection then you also need the right environment, the cold weather for this manifestation to present,” he said. “Or, it really isn’t a direct manifestation of COVID-19 but may be more related to other factors,” such as lifestyle changes related to limitations implemented to help mitigate the spread of the disease.
“To me the jury is still out whether or not the perniotic lesions really can tell us something about a patient’s exposure and infection with SARS-CoV-2,” he said.
Dr. Freeman reported receiving a grant from the International League of Dermatological Societies and nonfinancial support from the AAD for the study. Dr. Ko reported no conflicts. Dr. Fernadnez had no disclosures.
– as a result of infection with or exposure to the SARS-CoV-2 virus, but some dermatologists question if the skin signs and symptoms are truly related.
In their commentary in the Lancet Infectious Diseases, Esther P. Freeman, MD, PhD, and colleagues who lead and participate in the American Academy of Dermatology’s international registry said their analysis “revealed a previously unreported subset of patients who experience long-haul symptoms in dermatology-dominant COVID-19.”
Some of the data was presented at the 29th European Academy of Dermatology and Venereology in late October 2020, but has since been updated with more cases.
Dermatologists who spoke with this news organization said it has not been settled that some skin manifestations – such as pernio/chilblains rashes, seen primarily in nonhospitalized patients, and described in the registry – are definitively caused by COVID. They also noted that in some cases, patients who initially test negative for COVID-19 by polymerase chain reaction (PCR) sometimes do not ever develop antibodies, which could mean they were never actually exposed to SARS-CoV-2.
“I still question whether the perniosis is directly related to infection with SARS-CoV-2 or not,” said Anthony Fernandez, MD, PhD, director of medical and inpatient dermatology and assistant professor of dermatopathology at the Cleveland Clinic. His uncertainty is driven by the lack of seroconversion and that few cases were seen over the summer in the United States – suggesting that it may still be a result of cold temperatures.
“I’m not sure there is a definitive correct answer, definitely not that everyone would agree on,” said Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn.
Dr. Freeman, however, believed that pernio and especially persistent lesions are caused by an immune response to COVID.
In an interview, she noted the multiple cases of patients in the registry who did seroconvert and that, while a registry is not a perfect means of getting an answer, it is good for generating questions. Taken collectively, the cases in the registry can “tell a story for further hypotheses,” said Dr. Freeman, who is director of global health dermatology at Massachusetts General Hospital and assistant professor of dermatology at Harvard University, both in Boston.
“We were noticing this signal across the world” that patients “developed these toe lesions and they never got better,” said Dr. Freeman. Generally, people who experience pernio, also described as COVID toes or “COVID fingers,” recover in 4-8 weeks. But in the registry, “we did have this subset of patients who really were experiencing these very longstanding symptoms,” she added.
Two patients with lab-confirmed COVID have had long-lasting pernio of 133 days and 150 days. “I’m caring for a cohort in Boston who have had long COVID of the skin and symptoms for over 10 months,” Dr. Freeman said.
Pernio dominates
The registry – a collaboration between the AAD and the International League of Dermatological Societies – was launched in April 2020. Any medical professional can enter case information. From April to October, 1,030 total cases and 331 laboratory-confirmed or suspected COVID-19 cases with dermatological manifestations were entered from 41 countries.
Most of the cases were just recorded at a single time point, which is an acknowledged limitation of the study.
Dr. Freeman and colleagues reached out to registry participants in June and August to get updates on COVID lab test results and sign and symptom duration. Overall, 234 total and 96 lab-confirmed COVID infections had more lengthy data about sign and symptom duration.
Pernio lasted a median of 15 days in patients with suspected disease and 12 days for those with lab-confirmed COVID, compared with a median of 7 days for morbilliform eruptions, 4 days for urticarial eruptions, and 20 days for papulosquamous eruptions – all in patients with lab-confirmed disease.
Of the 103 cases of pernio, 7 had symptoms lasting more than 60 days. Only two of those seven patients had lab-confirmed COVID. Initially, the one patient tested negative with nasopharyngeal PCR, and serum IgM and IgG. Six weeks after pernio onset, the patient – still experiencing fatigue and pernio – seroconverted to anti–SARS-CoV-2 IgM positivity.
The other long-haul patient, after a negative PCR, tested positive for SARS-CoV-2 serum IgG 1 month after pernio onset.
Robust immune response?
Dr. Freeman said these patients might have a very high interferon response initially to the virus, which makes for a mild to nonexistent disease, but could create inflammation elsewhere. “I almost view the toes as an innocent bystander of a robust immune response to SARS-CoV-2.”
Although he has not seen extended pernio or other skin manifestations in his patients, Dr. Fernandez said the interferon hypothesis is “fair,” and “the best that’s out there.” Dr. Fernandez is currently studying cutaneous manifestations of COVID-19 as a principal investigator of a trial sponsored by the Clinical and Translational Science Collaborative of Cleveland.
Dr. Ko said in an interview that she has not observed long-haul skin issues in her patients, but Yale colleagues have.
In a study, she and Yale colleagues published in September, SARS-CoV-2 spike protein was detected in perniotic lesions, but not nuclear protein or viral RNA. The test they used – immunohistochemistry – can be nonspecific, which muddied results.
She does not think there is replicating virus in the skin or the lesions. Instead, said Dr. Ko, “either there is viral spike protein that has somehow become disassociated from actively replicating virus that somehow got deposited in endothelial cells,” or the staining “was spurious,” or some other protein is cross-reacting. “And the people who are unlucky enough to have that protein in their endothelial cells can manifest this COVID-toe, COVID-finger phenomenon.”
To her, it’s an unsolved mystery. “The weird thing is, we’ve never before had this much perniosis,” Dr. Ko said.
Dr. Fernandez is not convinced yet, noting that, in Cleveland, more pernio cases were observed in March and April than in the summer. “If it is a manifestation of the infection then you also need the right environment, the cold weather for this manifestation to present,” he said. “Or, it really isn’t a direct manifestation of COVID-19 but may be more related to other factors,” such as lifestyle changes related to limitations implemented to help mitigate the spread of the disease.
“To me the jury is still out whether or not the perniotic lesions really can tell us something about a patient’s exposure and infection with SARS-CoV-2,” he said.
Dr. Freeman reported receiving a grant from the International League of Dermatological Societies and nonfinancial support from the AAD for the study. Dr. Ko reported no conflicts. Dr. Fernadnez had no disclosures.
FROM THE LANCET INFECTIOUS DISEASES
President Biden signs 10 new orders to help fight COVID-19
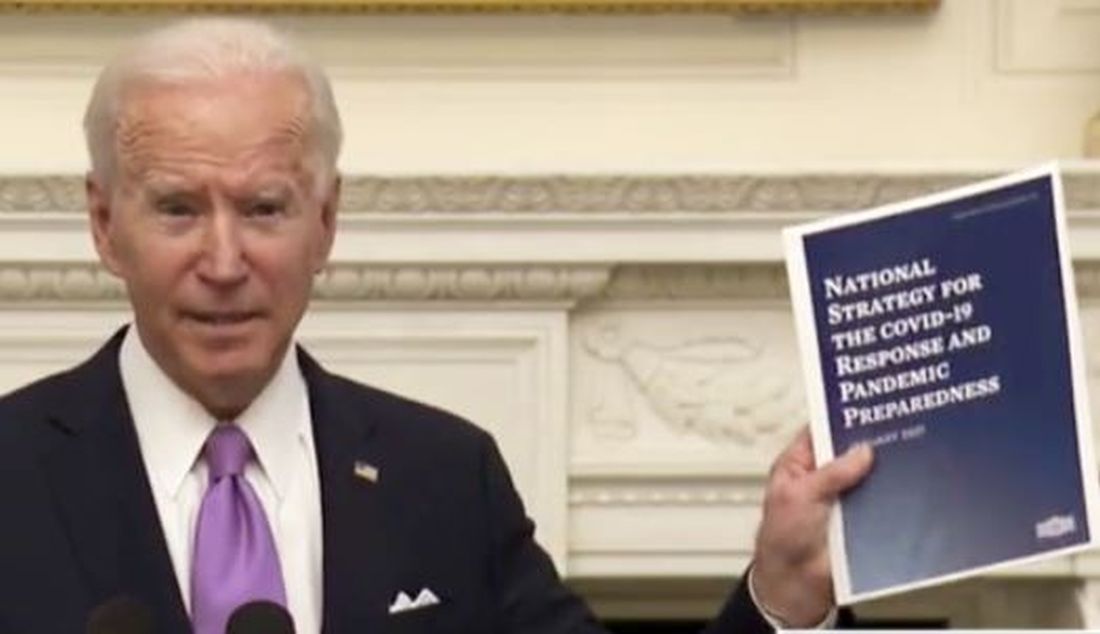
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
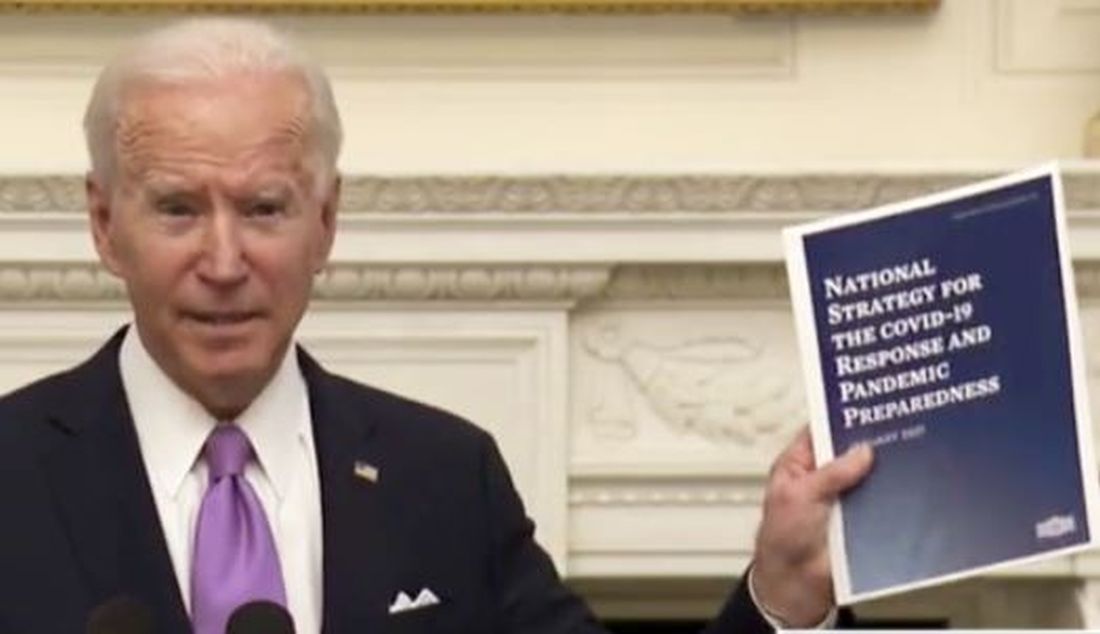
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
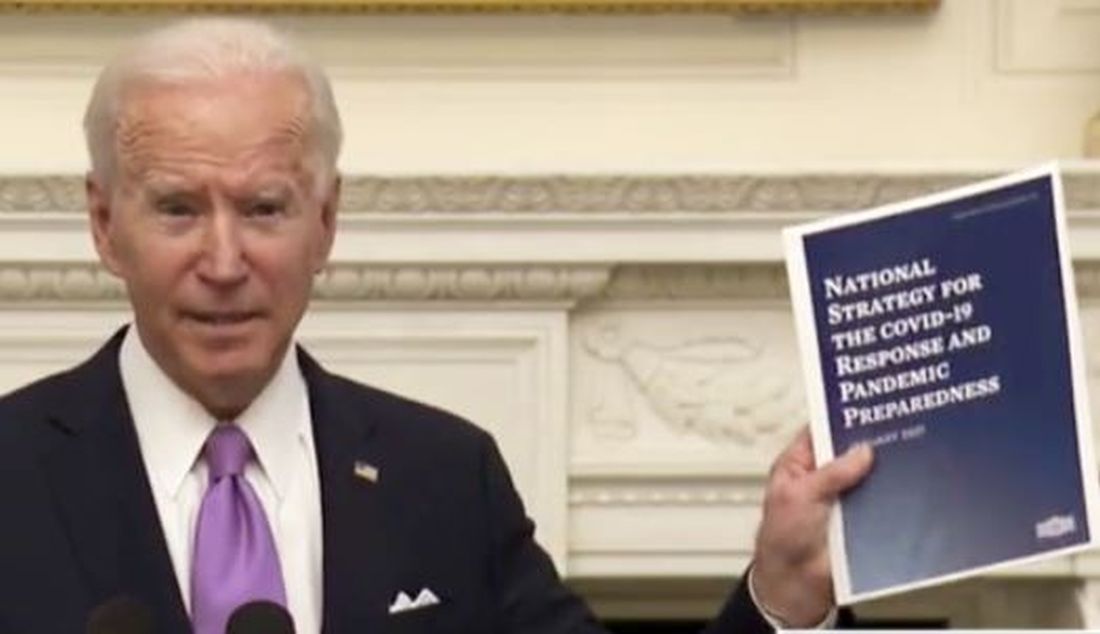
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
Feds to states: Give COVID-19 vaccine to 65+ and those with comorbidities
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
New coalition demands urgent action on COVID-19 mental health crisis
Fourteen mental health organizations have formed a coalition to press federal and state officials to tackle the ongoing and growing mental health crisis that is accompanying the COVID-19 pandemic.
The coalition is offering a road map, A Unified Vision for Transforming Mental Health and Substance Abuse Care, which spells out “immediate and long-term changes that will lead to a mental health care system capable of saving our nation,” they said in a statement.
The group includes CEOs from the American Psychiatric Association, the American Psychological Association, the Massachusetts Association for Mental Health, Meadows Mental Health Policy Institute, Mental Health America, the National Association for Behavioral Healthcare, the National Alliance on Mental Illness, the National Council for Behavioral Health, One Mind, Peg’s Foundation, the Steinberg Institute, The Kennedy Forum, the Treatment Advocacy Center, and the Well Being Trust.
They have been meeting in weekly sessions since the beginning of the pandemic. The groups have come together in the spirit of previous efforts to address major health crises, including the 1970s war on cancer and the campaign to curtail the HIV/AIDS epidemic in the 1980s, they report.
The coalition reported that since the pandemic began the prevalence of depression symptoms has jumped threefold, overdose deaths have increased in 40 states, and 25% of young adults have had suicidal ideation.
“It requires immediate action by the new administration, as well as state and local governments in all 50 states, and an acknowledged, consistent commitment to fix what’s broken in our system of care,” Daniel H. Gillison Jr, CEO of the National Alliance on Mental Illness, said in a statement.
SAMHSA chief ‘grateful’
Elinore McCance-Katz, MD, PhD, who is the assistant secretary for mental health and substance use and leads the Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services, applauded the coalition.
“I am very grateful that these organizations are stepping up and putting out a report like this,” Dr. McCance-Katz told this news organization. “I hope that they will continue this kind of advocacy and leadership on these issues going forward,” she said, adding that the need for mental health care and substance use disorders will be much greater going forward because of the pandemic.
Seven policy areas
The group’s 17-page strategic plan emphasizes interventions and methods that have already been tried and tested, focusing on seven policy areas:
- Early identification and prevention, especially for families and young people, by, for instance, bringing telehealth into schools and community centers.
- Rapid deployment of emergency crisis response and prevention, including speeding up the implementation of the new 988 number for the National Suicide Prevention Lifeline.
- Leveling inequities in access to care by addressing social and political constructs and historical systemic injustices such as racism.
- Integrating physical and mental health care and substance use services to ensure “whole-person” well-being.
- Achieving parity in payment by health plans for mental health and substance-use coverage.
- Assuring evidence-based standards of treatments and care.
- Increasing the number and diversity of the mental health care workforce, peer support, and community-based programs.
and will be even more so in the near future as the effects of the pandemic continue to ripple out.
SAMHSA received $425 million in the first COVID-19 relief package signed into law in March – the CARES Act. The money was distributed to states and used for direct care for people with serious mental illness and substance-use disorders who could not otherwise get care because of virus-related restrictions, and for boosting support for mental health support lines, said Dr. McCance-Katz.
A senior SAMHSA spokesperson said the agency is “hopeful that we will see additional resources in the upcoming stimulus for mental health and substance abuse” that Congress is still working on.
“We need bold steps from our government and the business community alike,” former Rep. Patrick J. Kennedy, founder of The Kennedy Forum, said in the statement from the new coalition. “We encourage all state governments to engage with mental health leaders, bring them into pandemic-related responses, and actively facilitate their communication with communities across the country,” said Mr. Kennedy, who is a part of the new coalition.
Mr. Kennedy is also cochair of the Action Alliance’s Mental Health and Suicide Prevention National Response to COVID-19, which unveiled its own six-priority Action Plan earlier in December.
A version of this article first appeared on Medscape.com.
Fourteen mental health organizations have formed a coalition to press federal and state officials to tackle the ongoing and growing mental health crisis that is accompanying the COVID-19 pandemic.
The coalition is offering a road map, A Unified Vision for Transforming Mental Health and Substance Abuse Care, which spells out “immediate and long-term changes that will lead to a mental health care system capable of saving our nation,” they said in a statement.
The group includes CEOs from the American Psychiatric Association, the American Psychological Association, the Massachusetts Association for Mental Health, Meadows Mental Health Policy Institute, Mental Health America, the National Association for Behavioral Healthcare, the National Alliance on Mental Illness, the National Council for Behavioral Health, One Mind, Peg’s Foundation, the Steinberg Institute, The Kennedy Forum, the Treatment Advocacy Center, and the Well Being Trust.
They have been meeting in weekly sessions since the beginning of the pandemic. The groups have come together in the spirit of previous efforts to address major health crises, including the 1970s war on cancer and the campaign to curtail the HIV/AIDS epidemic in the 1980s, they report.
The coalition reported that since the pandemic began the prevalence of depression symptoms has jumped threefold, overdose deaths have increased in 40 states, and 25% of young adults have had suicidal ideation.
“It requires immediate action by the new administration, as well as state and local governments in all 50 states, and an acknowledged, consistent commitment to fix what’s broken in our system of care,” Daniel H. Gillison Jr, CEO of the National Alliance on Mental Illness, said in a statement.
SAMHSA chief ‘grateful’
Elinore McCance-Katz, MD, PhD, who is the assistant secretary for mental health and substance use and leads the Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services, applauded the coalition.
“I am very grateful that these organizations are stepping up and putting out a report like this,” Dr. McCance-Katz told this news organization. “I hope that they will continue this kind of advocacy and leadership on these issues going forward,” she said, adding that the need for mental health care and substance use disorders will be much greater going forward because of the pandemic.
Seven policy areas
The group’s 17-page strategic plan emphasizes interventions and methods that have already been tried and tested, focusing on seven policy areas:
- Early identification and prevention, especially for families and young people, by, for instance, bringing telehealth into schools and community centers.
- Rapid deployment of emergency crisis response and prevention, including speeding up the implementation of the new 988 number for the National Suicide Prevention Lifeline.
- Leveling inequities in access to care by addressing social and political constructs and historical systemic injustices such as racism.
- Integrating physical and mental health care and substance use services to ensure “whole-person” well-being.
- Achieving parity in payment by health plans for mental health and substance-use coverage.
- Assuring evidence-based standards of treatments and care.
- Increasing the number and diversity of the mental health care workforce, peer support, and community-based programs.
and will be even more so in the near future as the effects of the pandemic continue to ripple out.
SAMHSA received $425 million in the first COVID-19 relief package signed into law in March – the CARES Act. The money was distributed to states and used for direct care for people with serious mental illness and substance-use disorders who could not otherwise get care because of virus-related restrictions, and for boosting support for mental health support lines, said Dr. McCance-Katz.
A senior SAMHSA spokesperson said the agency is “hopeful that we will see additional resources in the upcoming stimulus for mental health and substance abuse” that Congress is still working on.
“We need bold steps from our government and the business community alike,” former Rep. Patrick J. Kennedy, founder of The Kennedy Forum, said in the statement from the new coalition. “We encourage all state governments to engage with mental health leaders, bring them into pandemic-related responses, and actively facilitate their communication with communities across the country,” said Mr. Kennedy, who is a part of the new coalition.
Mr. Kennedy is also cochair of the Action Alliance’s Mental Health and Suicide Prevention National Response to COVID-19, which unveiled its own six-priority Action Plan earlier in December.
A version of this article first appeared on Medscape.com.
Fourteen mental health organizations have formed a coalition to press federal and state officials to tackle the ongoing and growing mental health crisis that is accompanying the COVID-19 pandemic.
The coalition is offering a road map, A Unified Vision for Transforming Mental Health and Substance Abuse Care, which spells out “immediate and long-term changes that will lead to a mental health care system capable of saving our nation,” they said in a statement.
The group includes CEOs from the American Psychiatric Association, the American Psychological Association, the Massachusetts Association for Mental Health, Meadows Mental Health Policy Institute, Mental Health America, the National Association for Behavioral Healthcare, the National Alliance on Mental Illness, the National Council for Behavioral Health, One Mind, Peg’s Foundation, the Steinberg Institute, The Kennedy Forum, the Treatment Advocacy Center, and the Well Being Trust.
They have been meeting in weekly sessions since the beginning of the pandemic. The groups have come together in the spirit of previous efforts to address major health crises, including the 1970s war on cancer and the campaign to curtail the HIV/AIDS epidemic in the 1980s, they report.
The coalition reported that since the pandemic began the prevalence of depression symptoms has jumped threefold, overdose deaths have increased in 40 states, and 25% of young adults have had suicidal ideation.
“It requires immediate action by the new administration, as well as state and local governments in all 50 states, and an acknowledged, consistent commitment to fix what’s broken in our system of care,” Daniel H. Gillison Jr, CEO of the National Alliance on Mental Illness, said in a statement.
SAMHSA chief ‘grateful’
Elinore McCance-Katz, MD, PhD, who is the assistant secretary for mental health and substance use and leads the Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services, applauded the coalition.
“I am very grateful that these organizations are stepping up and putting out a report like this,” Dr. McCance-Katz told this news organization. “I hope that they will continue this kind of advocacy and leadership on these issues going forward,” she said, adding that the need for mental health care and substance use disorders will be much greater going forward because of the pandemic.
Seven policy areas
The group’s 17-page strategic plan emphasizes interventions and methods that have already been tried and tested, focusing on seven policy areas:
- Early identification and prevention, especially for families and young people, by, for instance, bringing telehealth into schools and community centers.
- Rapid deployment of emergency crisis response and prevention, including speeding up the implementation of the new 988 number for the National Suicide Prevention Lifeline.
- Leveling inequities in access to care by addressing social and political constructs and historical systemic injustices such as racism.
- Integrating physical and mental health care and substance use services to ensure “whole-person” well-being.
- Achieving parity in payment by health plans for mental health and substance-use coverage.
- Assuring evidence-based standards of treatments and care.
- Increasing the number and diversity of the mental health care workforce, peer support, and community-based programs.
and will be even more so in the near future as the effects of the pandemic continue to ripple out.
SAMHSA received $425 million in the first COVID-19 relief package signed into law in March – the CARES Act. The money was distributed to states and used for direct care for people with serious mental illness and substance-use disorders who could not otherwise get care because of virus-related restrictions, and for boosting support for mental health support lines, said Dr. McCance-Katz.
A senior SAMHSA spokesperson said the agency is “hopeful that we will see additional resources in the upcoming stimulus for mental health and substance abuse” that Congress is still working on.
“We need bold steps from our government and the business community alike,” former Rep. Patrick J. Kennedy, founder of The Kennedy Forum, said in the statement from the new coalition. “We encourage all state governments to engage with mental health leaders, bring them into pandemic-related responses, and actively facilitate their communication with communities across the country,” said Mr. Kennedy, who is a part of the new coalition.
Mr. Kennedy is also cochair of the Action Alliance’s Mental Health and Suicide Prevention National Response to COVID-19, which unveiled its own six-priority Action Plan earlier in December.
A version of this article first appeared on Medscape.com.
COVID-related harm to HCWs must be tracked more rigorously: NAS panel
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.
Proposed HIPAA overhaul to ease access to patient health info
The Department of Health & Human Services is proposing an overhaul of HIPAA that will make it easier to access patients’ personal health information, including the health records of patients with mental illness. The proposal would also do away with the requirement that all patients sign a notice of privacy practices.
The changes are contained in a 357-page proposed rule, which was unveiled by federal officials Dec. 10. Roger Severino, director of HHS’ Office for Civil Rights, said in a briefing that the sweeping proposal would empower patients, reduce the administrative burden for health care providers, and pave the way to better-coordinated care.
HHS estimated that the rule could save $3.2 billion over 5 years, but it’s not clear how much of that would accrue to clinical practices.
The most obvious cost-saving aspect for medical and dental practices is the proposal that practitioners would no longer have to provide and collect signed notifications of privacy practices.
“This has been a tremendous waste of time and effort and has caused massive confusion,” said Mr. Severino. He said some patients thought they were waiving privacy rights and that, in some cases, physicians refused to administer care unless patients signed the notices. “That was never the intent.”
Requiring that patients sign the form and that practices keep copies for 6 years is an “unnecessary burden,” said Mr. Severino. “We’ve lost whole forests from this regulation.”
Under the new proposal, health care providers would merely have to let patients know where to find their privacy policies.
Sharing mental health info
The rule would also ease the standard for sharing information about a patient who is in a mental health crisis, such as an exacerbation of a serious mental illness or a crisis related to a substance use disorder, including an overdose.
Currently, clinicians can choose to disclose protected health information – to a family member, a caregiver, a law enforcement official, a doctor, or an insurer – if they believe that doing so is advisable in their “professional judgment.” The rule proposes to ease that to a “good faith” belief that a disclosure would be in the best interest of the patient. In both instances, the patient can still object and block the disclosure.
As an example, HHS said that, in the case of a young adult who had experienced an overdose of opioids, a licensed health care professional could make the determination to “disclose relevant information to a parent who is involved in the patient’s treatment and who the young adult would expect, based on their relationship, to participate in or be involved with the patient’s recovery from the overdose.”
HHS is also proposing to let clinicians disclose information in cases in which an individual might be a threat to himself or others, provided the harm is “serious and reasonably foreseeable.”
Currently, information can only be disclosed if it appears there is a “serious and imminent” threat to health or safety. If an individual experienced suicidal ideation, for instance, a health care professional could notify family that the individual is at risk.
Fast, no-cost access
The rule also aims to make it easier for patients to get access to their own health care information quickly – within 15 days of a request – instead of the 30 days currently allowed, and sometimes at no cost.
The 30-day time frame is “a relic of a pre-Internet age that should be dispensed with,” said Mr. Severino.
Patients can also request that a treating physician get his or her records from a clinician who had previously treated the individual. The request would be fulfilled within 15 days, although extensions might be possible.
“That takes away the burden of coordination from the patient and puts it on those parties that are responsible for the actual provision of care and that are better positioned to do that coordination,” Mr. Severino said.
Health care professionals will also have to share with patients a fee schedule for records requests. However, if records are shared through a patient portal with view, download, and transmit capabilities, the provider can’t charge the patient for the time it took to upload the information into the system.
“We do not believe a patient’s personal medical record should be profit centers for providers,” Mr. Severino said.
Patients will be allowed to take photos with a smartphone of personal health information – such as an x-ray or sonogram – while receiving care.
The rule is open for public comment until mid-February. After that, it will become final in 180 days. The agency said it would not begin enforcement until 240 days after the final rule was published.
A version of this article originally appeared on Medscape.com.
The Department of Health & Human Services is proposing an overhaul of HIPAA that will make it easier to access patients’ personal health information, including the health records of patients with mental illness. The proposal would also do away with the requirement that all patients sign a notice of privacy practices.
The changes are contained in a 357-page proposed rule, which was unveiled by federal officials Dec. 10. Roger Severino, director of HHS’ Office for Civil Rights, said in a briefing that the sweeping proposal would empower patients, reduce the administrative burden for health care providers, and pave the way to better-coordinated care.
HHS estimated that the rule could save $3.2 billion over 5 years, but it’s not clear how much of that would accrue to clinical practices.
The most obvious cost-saving aspect for medical and dental practices is the proposal that practitioners would no longer have to provide and collect signed notifications of privacy practices.
“This has been a tremendous waste of time and effort and has caused massive confusion,” said Mr. Severino. He said some patients thought they were waiving privacy rights and that, in some cases, physicians refused to administer care unless patients signed the notices. “That was never the intent.”
Requiring that patients sign the form and that practices keep copies for 6 years is an “unnecessary burden,” said Mr. Severino. “We’ve lost whole forests from this regulation.”
Under the new proposal, health care providers would merely have to let patients know where to find their privacy policies.
Sharing mental health info
The rule would also ease the standard for sharing information about a patient who is in a mental health crisis, such as an exacerbation of a serious mental illness or a crisis related to a substance use disorder, including an overdose.
Currently, clinicians can choose to disclose protected health information – to a family member, a caregiver, a law enforcement official, a doctor, or an insurer – if they believe that doing so is advisable in their “professional judgment.” The rule proposes to ease that to a “good faith” belief that a disclosure would be in the best interest of the patient. In both instances, the patient can still object and block the disclosure.
As an example, HHS said that, in the case of a young adult who had experienced an overdose of opioids, a licensed health care professional could make the determination to “disclose relevant information to a parent who is involved in the patient’s treatment and who the young adult would expect, based on their relationship, to participate in or be involved with the patient’s recovery from the overdose.”
HHS is also proposing to let clinicians disclose information in cases in which an individual might be a threat to himself or others, provided the harm is “serious and reasonably foreseeable.”
Currently, information can only be disclosed if it appears there is a “serious and imminent” threat to health or safety. If an individual experienced suicidal ideation, for instance, a health care professional could notify family that the individual is at risk.
Fast, no-cost access
The rule also aims to make it easier for patients to get access to their own health care information quickly – within 15 days of a request – instead of the 30 days currently allowed, and sometimes at no cost.
The 30-day time frame is “a relic of a pre-Internet age that should be dispensed with,” said Mr. Severino.
Patients can also request that a treating physician get his or her records from a clinician who had previously treated the individual. The request would be fulfilled within 15 days, although extensions might be possible.
“That takes away the burden of coordination from the patient and puts it on those parties that are responsible for the actual provision of care and that are better positioned to do that coordination,” Mr. Severino said.
Health care professionals will also have to share with patients a fee schedule for records requests. However, if records are shared through a patient portal with view, download, and transmit capabilities, the provider can’t charge the patient for the time it took to upload the information into the system.
“We do not believe a patient’s personal medical record should be profit centers for providers,” Mr. Severino said.
Patients will be allowed to take photos with a smartphone of personal health information – such as an x-ray or sonogram – while receiving care.
The rule is open for public comment until mid-February. After that, it will become final in 180 days. The agency said it would not begin enforcement until 240 days after the final rule was published.
A version of this article originally appeared on Medscape.com.
The Department of Health & Human Services is proposing an overhaul of HIPAA that will make it easier to access patients’ personal health information, including the health records of patients with mental illness. The proposal would also do away with the requirement that all patients sign a notice of privacy practices.
The changes are contained in a 357-page proposed rule, which was unveiled by federal officials Dec. 10. Roger Severino, director of HHS’ Office for Civil Rights, said in a briefing that the sweeping proposal would empower patients, reduce the administrative burden for health care providers, and pave the way to better-coordinated care.
HHS estimated that the rule could save $3.2 billion over 5 years, but it’s not clear how much of that would accrue to clinical practices.
The most obvious cost-saving aspect for medical and dental practices is the proposal that practitioners would no longer have to provide and collect signed notifications of privacy practices.
“This has been a tremendous waste of time and effort and has caused massive confusion,” said Mr. Severino. He said some patients thought they were waiving privacy rights and that, in some cases, physicians refused to administer care unless patients signed the notices. “That was never the intent.”
Requiring that patients sign the form and that practices keep copies for 6 years is an “unnecessary burden,” said Mr. Severino. “We’ve lost whole forests from this regulation.”
Under the new proposal, health care providers would merely have to let patients know where to find their privacy policies.
Sharing mental health info
The rule would also ease the standard for sharing information about a patient who is in a mental health crisis, such as an exacerbation of a serious mental illness or a crisis related to a substance use disorder, including an overdose.
Currently, clinicians can choose to disclose protected health information – to a family member, a caregiver, a law enforcement official, a doctor, or an insurer – if they believe that doing so is advisable in their “professional judgment.” The rule proposes to ease that to a “good faith” belief that a disclosure would be in the best interest of the patient. In both instances, the patient can still object and block the disclosure.
As an example, HHS said that, in the case of a young adult who had experienced an overdose of opioids, a licensed health care professional could make the determination to “disclose relevant information to a parent who is involved in the patient’s treatment and who the young adult would expect, based on their relationship, to participate in or be involved with the patient’s recovery from the overdose.”
HHS is also proposing to let clinicians disclose information in cases in which an individual might be a threat to himself or others, provided the harm is “serious and reasonably foreseeable.”
Currently, information can only be disclosed if it appears there is a “serious and imminent” threat to health or safety. If an individual experienced suicidal ideation, for instance, a health care professional could notify family that the individual is at risk.
Fast, no-cost access
The rule also aims to make it easier for patients to get access to their own health care information quickly – within 15 days of a request – instead of the 30 days currently allowed, and sometimes at no cost.
The 30-day time frame is “a relic of a pre-Internet age that should be dispensed with,” said Mr. Severino.
Patients can also request that a treating physician get his or her records from a clinician who had previously treated the individual. The request would be fulfilled within 15 days, although extensions might be possible.
“That takes away the burden of coordination from the patient and puts it on those parties that are responsible for the actual provision of care and that are better positioned to do that coordination,” Mr. Severino said.
Health care professionals will also have to share with patients a fee schedule for records requests. However, if records are shared through a patient portal with view, download, and transmit capabilities, the provider can’t charge the patient for the time it took to upload the information into the system.
“We do not believe a patient’s personal medical record should be profit centers for providers,” Mr. Severino said.
Patients will be allowed to take photos with a smartphone of personal health information – such as an x-ray or sonogram – while receiving care.
The rule is open for public comment until mid-February. After that, it will become final in 180 days. The agency said it would not begin enforcement until 240 days after the final rule was published.
A version of this article originally appeared on Medscape.com.
Kennedy, NIMH demand urgent action on COVID-19 mental health toll
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
FDA gives guidance on allergy, pregnancy concerns for Pfizer COVID vaccine
stating that it is safe for people with any history of allergies, but not for those who might have a known history of severe allergic reaction to any component of the vaccine.
The warning is included in the FDA’s information sheet for health care providers, but questions are arising as to whether the vaccine – which was authorized for emergency use by the FDA on Friday – should not be given to anyone with a history of allergies.
Sara Oliver, MD, an epidemic intelligence service officer with the Centers for Disease Control and Prevention reported at a Dec. 11 meeting of the agency’s Advisory Committee on Immunization Practices that two U.K. health care workers with a history of significant allergic reactions had a reaction to the Pfizer vaccine. A third health care worker with no history of allergies developed tachycardia, Dr. Oliver said.
“I want to reassure the public that although there were these few reactions in Great Britain, these were not seen in the larger clinical trial datasets,” said Peter Marks, MD, PhD, director of the Center for Biologics Evaluation and Research at the FDA, during a press briefing on Dec. 12.
The Pfizer vaccine “is one that we’re comfortable giving to patients who have had other allergic reactions besides those other than severe allergic reactions to a vaccine or one of its components,” he said.
Dr. Marks suggested that individuals let their physicians know about any history of allergic reactions. He also noted that the federal government will be supplying vaccine administration sites, at least initially, with epinephrine, diphenhydramine, hydrocortisone, and other medications needed to manage allergic reactions.
The FDA is going to monitor side effects such as allergic reactions very closely, “but I think we still need to learn more and that’s why we’re going to be taking precautions. We may have to modify things as we move forward,” said Dr. Marks.
Dr. Oliver said that on Dec. 12 the CDC convened an external panel with experience in vaccine safety, immunology, and allergies “to collate expert knowledge regarding possible cases,” and that the FDA is getting more data from U.K. regulatory authorities.
Pregnancy concerns
Agency officials had little to say, however, about the safety or efficacy of the vaccine for pregnant or breastfeeding women.
The FDA’s information to health care professionals noted that “available data on Pfizer-BioNTech COVID-19 vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.”
Additionally, the agency stated, “data are not available to assess the effects of Pfizer-BioNTech COVID-19 vaccine on the breastfed infant or on milk production/excretion.”
Dr. Marks said that, for pregnant women and people who are immunocompromised, “it will be something that providers will need to consider on an individual basis.” He suggested that individuals consult with physicians to weigh the potential benefits and potential risks.
“Certainly, COVID-19 in a pregnant woman is not a good thing,” Dr. Marks said.
An individual might decide to go ahead with vaccination. “But that’s not something we’re recommending, that’s something we’re leaving up to the individual,” he said.
A version of this article originally appeared on Medscape.com.
stating that it is safe for people with any history of allergies, but not for those who might have a known history of severe allergic reaction to any component of the vaccine.
The warning is included in the FDA’s information sheet for health care providers, but questions are arising as to whether the vaccine – which was authorized for emergency use by the FDA on Friday – should not be given to anyone with a history of allergies.
Sara Oliver, MD, an epidemic intelligence service officer with the Centers for Disease Control and Prevention reported at a Dec. 11 meeting of the agency’s Advisory Committee on Immunization Practices that two U.K. health care workers with a history of significant allergic reactions had a reaction to the Pfizer vaccine. A third health care worker with no history of allergies developed tachycardia, Dr. Oliver said.
“I want to reassure the public that although there were these few reactions in Great Britain, these were not seen in the larger clinical trial datasets,” said Peter Marks, MD, PhD, director of the Center for Biologics Evaluation and Research at the FDA, during a press briefing on Dec. 12.
The Pfizer vaccine “is one that we’re comfortable giving to patients who have had other allergic reactions besides those other than severe allergic reactions to a vaccine or one of its components,” he said.
Dr. Marks suggested that individuals let their physicians know about any history of allergic reactions. He also noted that the federal government will be supplying vaccine administration sites, at least initially, with epinephrine, diphenhydramine, hydrocortisone, and other medications needed to manage allergic reactions.
The FDA is going to monitor side effects such as allergic reactions very closely, “but I think we still need to learn more and that’s why we’re going to be taking precautions. We may have to modify things as we move forward,” said Dr. Marks.
Dr. Oliver said that on Dec. 12 the CDC convened an external panel with experience in vaccine safety, immunology, and allergies “to collate expert knowledge regarding possible cases,” and that the FDA is getting more data from U.K. regulatory authorities.
Pregnancy concerns
Agency officials had little to say, however, about the safety or efficacy of the vaccine for pregnant or breastfeeding women.
The FDA’s information to health care professionals noted that “available data on Pfizer-BioNTech COVID-19 vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.”
Additionally, the agency stated, “data are not available to assess the effects of Pfizer-BioNTech COVID-19 vaccine on the breastfed infant or on milk production/excretion.”
Dr. Marks said that, for pregnant women and people who are immunocompromised, “it will be something that providers will need to consider on an individual basis.” He suggested that individuals consult with physicians to weigh the potential benefits and potential risks.
“Certainly, COVID-19 in a pregnant woman is not a good thing,” Dr. Marks said.
An individual might decide to go ahead with vaccination. “But that’s not something we’re recommending, that’s something we’re leaving up to the individual,” he said.
A version of this article originally appeared on Medscape.com.
stating that it is safe for people with any history of allergies, but not for those who might have a known history of severe allergic reaction to any component of the vaccine.
The warning is included in the FDA’s information sheet for health care providers, but questions are arising as to whether the vaccine – which was authorized for emergency use by the FDA on Friday – should not be given to anyone with a history of allergies.
Sara Oliver, MD, an epidemic intelligence service officer with the Centers for Disease Control and Prevention reported at a Dec. 11 meeting of the agency’s Advisory Committee on Immunization Practices that two U.K. health care workers with a history of significant allergic reactions had a reaction to the Pfizer vaccine. A third health care worker with no history of allergies developed tachycardia, Dr. Oliver said.
“I want to reassure the public that although there were these few reactions in Great Britain, these were not seen in the larger clinical trial datasets,” said Peter Marks, MD, PhD, director of the Center for Biologics Evaluation and Research at the FDA, during a press briefing on Dec. 12.
The Pfizer vaccine “is one that we’re comfortable giving to patients who have had other allergic reactions besides those other than severe allergic reactions to a vaccine or one of its components,” he said.
Dr. Marks suggested that individuals let their physicians know about any history of allergic reactions. He also noted that the federal government will be supplying vaccine administration sites, at least initially, with epinephrine, diphenhydramine, hydrocortisone, and other medications needed to manage allergic reactions.
The FDA is going to monitor side effects such as allergic reactions very closely, “but I think we still need to learn more and that’s why we’re going to be taking precautions. We may have to modify things as we move forward,” said Dr. Marks.
Dr. Oliver said that on Dec. 12 the CDC convened an external panel with experience in vaccine safety, immunology, and allergies “to collate expert knowledge regarding possible cases,” and that the FDA is getting more data from U.K. regulatory authorities.
Pregnancy concerns
Agency officials had little to say, however, about the safety or efficacy of the vaccine for pregnant or breastfeeding women.
The FDA’s information to health care professionals noted that “available data on Pfizer-BioNTech COVID-19 vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.”
Additionally, the agency stated, “data are not available to assess the effects of Pfizer-BioNTech COVID-19 vaccine on the breastfed infant or on milk production/excretion.”
Dr. Marks said that, for pregnant women and people who are immunocompromised, “it will be something that providers will need to consider on an individual basis.” He suggested that individuals consult with physicians to weigh the potential benefits and potential risks.
“Certainly, COVID-19 in a pregnant woman is not a good thing,” Dr. Marks said.
An individual might decide to go ahead with vaccination. “But that’s not something we’re recommending, that’s something we’re leaving up to the individual,” he said.
A version of this article originally appeared on Medscape.com.