User login
Dermoscopy
The 21st Century ED: Past Predictions and Current Trends
In the October 2006 editorial, “A Design for the 21st Century,” I suggested that the first consideration in designing a new ED should be how long it is likely to remain in service before being replaced or substantially renovated, and then to consider which conditions are most likely to continue to present or increase in importance during the first several decades of the 21st century (Emerg Med. 2006;37[10]:7). I envisioned “increasing patient volume, an aging population, new and emerging viral infections, an even higher incidence of bacterial resistance, and more immunocompromised patients resulting from organ transplants and greater use of chemotherapy.” A decade after these predictions were made, how are they holding up?
Since 2006, there have been over 40 epidemics worldwide and although most have not affected this country, easy travel and global emergency medicine missions have brought several distant viral illnesses to US EDs as well. In 2009, EDs throughout the country had to deal with a potentially disastrous epidemic of H1N1 influenza, and in the years since we have been challenged by MERS (2012), dengue fever (2013-), Ebola (2014), and now Zika and chikungunya—not to mention outbreaks of “older” bacterial and viral illnesses such as pertussis (2012), and measles (2014-2015). Though several of the newer viruses mentioned are mosquito borne, pathogens transmitted from human to human, or human to surface to human, along with the increasing incidence of antibiotic resistance (MRSA, Clostridium difficile, Carbapenem-resistant Enterobacteriaceae, etc) make the need for greater numbers of ED negative-pressure rooms undeniable.
One important design feature not specifically considered in 2006, but made apparent by the Ebola experience in 2014, is a need for the shortest possible route between the ambulance and non-ambulance ED entry points/triage and isolation facilities. As noted in 2006, a separate entrance and air handling for a designated infection-control unit in the ED is essential if it must be sealed off from the rest of the hospital and/or main ED.
The second major ED design issue considered in 2006 was the increasing numbers of elderly patients who will present to our EDs during the first half of this century. Isolation rooms and private rooms in the ED will help manage the rapidly rising number of elderly patients with contagious diseases, along with other conditions such as dementia and delirium. Significant needs of the elderly also include measures to prevent or mitigate falls, catheter-related UTIs, and bedsores.
One epidemic in the elderly that we are already facing is a significant increase in the number of trauma cases. In some Level I trauma centers, over 34% of trauma activations are for patients 55 years old and older. The 2003-2012 Oregon Trauma Registry Report containing data on 84,099 patients from 44 trauma hospitals, notes that the rate of trauma increased from 200.7 to 244.6 per 100,000 during that period, almost exclusively occurring in patients 55 years old or older who represented 21% of cases in 2003 and 34% by 2012—a rise largely attributed to a 159% increase in trauma due to falls (http://public.health.oregon.gov/providerpartnerresources/emstraumasystems/traumasystems/documents/reports/otr-report.pdf). In another study, Hsia et al reported that 27% of 430,081 patients admitted to California acute care hospitals for trauma-related diagnoses between January 1, 1999 and December 31, 2008 were older than 65 years (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121677/), and in Houston, Texas, 13% of 15,223 trauma patients admitted to one of its two level I trauma centers between January 2005 and December 2008 were 65 years old or older, according to Adams et al (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3836632/). The Adams paper noted that trauma centers were originally designed to care for seriously ill patients without age-specific guidelines, but in patients 65 years or older there was a negligible amount of penetrating trauma, and a marked increase in blunt trauma, especially falls, while fatality rates, organ failure, and thromboembolic complications correlated with increasing age. Clearly EDs designed for the 21st century must be built not only to handle increasing numbers of trauma cases in the elderly, but for changing etiologies, characteristics, and comorbidities.
When I wrote “A Design for the 21st Century” in 2006, I was in the midst of actually designing an expansion to our (circa 1997) ED to increase capacity by 1/3. Readers who would like to see how the considerations presented here (and others) shaped the unit we opened in 2009, can view the short video below.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In the October 2006 editorial, “A Design for the 21st Century,” I suggested that the first consideration in designing a new ED should be how long it is likely to remain in service before being replaced or substantially renovated, and then to consider which conditions are most likely to continue to present or increase in importance during the first several decades of the 21st century (Emerg Med. 2006;37[10]:7). I envisioned “increasing patient volume, an aging population, new and emerging viral infections, an even higher incidence of bacterial resistance, and more immunocompromised patients resulting from organ transplants and greater use of chemotherapy.” A decade after these predictions were made, how are they holding up?
Since 2006, there have been over 40 epidemics worldwide and although most have not affected this country, easy travel and global emergency medicine missions have brought several distant viral illnesses to US EDs as well. In 2009, EDs throughout the country had to deal with a potentially disastrous epidemic of H1N1 influenza, and in the years since we have been challenged by MERS (2012), dengue fever (2013-), Ebola (2014), and now Zika and chikungunya—not to mention outbreaks of “older” bacterial and viral illnesses such as pertussis (2012), and measles (2014-2015). Though several of the newer viruses mentioned are mosquito borne, pathogens transmitted from human to human, or human to surface to human, along with the increasing incidence of antibiotic resistance (MRSA, Clostridium difficile, Carbapenem-resistant Enterobacteriaceae, etc) make the need for greater numbers of ED negative-pressure rooms undeniable.
One important design feature not specifically considered in 2006, but made apparent by the Ebola experience in 2014, is a need for the shortest possible route between the ambulance and non-ambulance ED entry points/triage and isolation facilities. As noted in 2006, a separate entrance and air handling for a designated infection-control unit in the ED is essential if it must be sealed off from the rest of the hospital and/or main ED.
The second major ED design issue considered in 2006 was the increasing numbers of elderly patients who will present to our EDs during the first half of this century. Isolation rooms and private rooms in the ED will help manage the rapidly rising number of elderly patients with contagious diseases, along with other conditions such as dementia and delirium. Significant needs of the elderly also include measures to prevent or mitigate falls, catheter-related UTIs, and bedsores.
One epidemic in the elderly that we are already facing is a significant increase in the number of trauma cases. In some Level I trauma centers, over 34% of trauma activations are for patients 55 years old and older. The 2003-2012 Oregon Trauma Registry Report containing data on 84,099 patients from 44 trauma hospitals, notes that the rate of trauma increased from 200.7 to 244.6 per 100,000 during that period, almost exclusively occurring in patients 55 years old or older who represented 21% of cases in 2003 and 34% by 2012—a rise largely attributed to a 159% increase in trauma due to falls (http://public.health.oregon.gov/providerpartnerresources/emstraumasystems/traumasystems/documents/reports/otr-report.pdf). In another study, Hsia et al reported that 27% of 430,081 patients admitted to California acute care hospitals for trauma-related diagnoses between January 1, 1999 and December 31, 2008 were older than 65 years (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121677/), and in Houston, Texas, 13% of 15,223 trauma patients admitted to one of its two level I trauma centers between January 2005 and December 2008 were 65 years old or older, according to Adams et al (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3836632/). The Adams paper noted that trauma centers were originally designed to care for seriously ill patients without age-specific guidelines, but in patients 65 years or older there was a negligible amount of penetrating trauma, and a marked increase in blunt trauma, especially falls, while fatality rates, organ failure, and thromboembolic complications correlated with increasing age. Clearly EDs designed for the 21st century must be built not only to handle increasing numbers of trauma cases in the elderly, but for changing etiologies, characteristics, and comorbidities.
When I wrote “A Design for the 21st Century” in 2006, I was in the midst of actually designing an expansion to our (circa 1997) ED to increase capacity by 1/3. Readers who would like to see how the considerations presented here (and others) shaped the unit we opened in 2009, can view the short video below.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In the October 2006 editorial, “A Design for the 21st Century,” I suggested that the first consideration in designing a new ED should be how long it is likely to remain in service before being replaced or substantially renovated, and then to consider which conditions are most likely to continue to present or increase in importance during the first several decades of the 21st century (Emerg Med. 2006;37[10]:7). I envisioned “increasing patient volume, an aging population, new and emerging viral infections, an even higher incidence of bacterial resistance, and more immunocompromised patients resulting from organ transplants and greater use of chemotherapy.” A decade after these predictions were made, how are they holding up?
Since 2006, there have been over 40 epidemics worldwide and although most have not affected this country, easy travel and global emergency medicine missions have brought several distant viral illnesses to US EDs as well. In 2009, EDs throughout the country had to deal with a potentially disastrous epidemic of H1N1 influenza, and in the years since we have been challenged by MERS (2012), dengue fever (2013-), Ebola (2014), and now Zika and chikungunya—not to mention outbreaks of “older” bacterial and viral illnesses such as pertussis (2012), and measles (2014-2015). Though several of the newer viruses mentioned are mosquito borne, pathogens transmitted from human to human, or human to surface to human, along with the increasing incidence of antibiotic resistance (MRSA, Clostridium difficile, Carbapenem-resistant Enterobacteriaceae, etc) make the need for greater numbers of ED negative-pressure rooms undeniable.
One important design feature not specifically considered in 2006, but made apparent by the Ebola experience in 2014, is a need for the shortest possible route between the ambulance and non-ambulance ED entry points/triage and isolation facilities. As noted in 2006, a separate entrance and air handling for a designated infection-control unit in the ED is essential if it must be sealed off from the rest of the hospital and/or main ED.
The second major ED design issue considered in 2006 was the increasing numbers of elderly patients who will present to our EDs during the first half of this century. Isolation rooms and private rooms in the ED will help manage the rapidly rising number of elderly patients with contagious diseases, along with other conditions such as dementia and delirium. Significant needs of the elderly also include measures to prevent or mitigate falls, catheter-related UTIs, and bedsores.
One epidemic in the elderly that we are already facing is a significant increase in the number of trauma cases. In some Level I trauma centers, over 34% of trauma activations are for patients 55 years old and older. The 2003-2012 Oregon Trauma Registry Report containing data on 84,099 patients from 44 trauma hospitals, notes that the rate of trauma increased from 200.7 to 244.6 per 100,000 during that period, almost exclusively occurring in patients 55 years old or older who represented 21% of cases in 2003 and 34% by 2012—a rise largely attributed to a 159% increase in trauma due to falls (http://public.health.oregon.gov/providerpartnerresources/emstraumasystems/traumasystems/documents/reports/otr-report.pdf). In another study, Hsia et al reported that 27% of 430,081 patients admitted to California acute care hospitals for trauma-related diagnoses between January 1, 1999 and December 31, 2008 were older than 65 years (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121677/), and in Houston, Texas, 13% of 15,223 trauma patients admitted to one of its two level I trauma centers between January 2005 and December 2008 were 65 years old or older, according to Adams et al (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3836632/). The Adams paper noted that trauma centers were originally designed to care for seriously ill patients without age-specific guidelines, but in patients 65 years or older there was a negligible amount of penetrating trauma, and a marked increase in blunt trauma, especially falls, while fatality rates, organ failure, and thromboembolic complications correlated with increasing age. Clearly EDs designed for the 21st century must be built not only to handle increasing numbers of trauma cases in the elderly, but for changing etiologies, characteristics, and comorbidities.
When I wrote “A Design for the 21st Century” in 2006, I was in the midst of actually designing an expansion to our (circa 1997) ED to increase capacity by 1/3. Readers who would like to see how the considerations presented here (and others) shaped the unit we opened in 2009, can view the short video below.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: A better way to treat large intraventricular hemorrhages
LOS ANGELES – For intraventricular hemorrhages of at least 20 mL, alteplase (Activase – Genentech) delivered directly into the clot by external ventricular drain almost doubles the odds of achieving a modified Rankin Score of 0-3 by 6 months.
More clot is removed – and patients with large intraventricular hemorrhages (IVHs) do better – with more vigorous alteplase dosing and when more than one drain is used.
The findings come from the Clot Lysis Evaluation of Accelerated Resolution (CLEAR III) trial, which randomized 249 IVH patients to 1 mg alteplase every 8 hours for up to 12 doses, and 251 to saline on the same schedule, delivered by external ventricular drain. The intervention didn’t make much difference with small hemorrhages.
In a video interview at the International Stroke Conference, investigator Dr. Issam Awad, a professor of surgery and neurology and director of neurovascular surgery at the University of Chicago, explained how to do the technique correctly for larger clots, and the expected benefits.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – For intraventricular hemorrhages of at least 20 mL, alteplase (Activase – Genentech) delivered directly into the clot by external ventricular drain almost doubles the odds of achieving a modified Rankin Score of 0-3 by 6 months.
More clot is removed – and patients with large intraventricular hemorrhages (IVHs) do better – with more vigorous alteplase dosing and when more than one drain is used.
The findings come from the Clot Lysis Evaluation of Accelerated Resolution (CLEAR III) trial, which randomized 249 IVH patients to 1 mg alteplase every 8 hours for up to 12 doses, and 251 to saline on the same schedule, delivered by external ventricular drain. The intervention didn’t make much difference with small hemorrhages.
In a video interview at the International Stroke Conference, investigator Dr. Issam Awad, a professor of surgery and neurology and director of neurovascular surgery at the University of Chicago, explained how to do the technique correctly for larger clots, and the expected benefits.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – For intraventricular hemorrhages of at least 20 mL, alteplase (Activase – Genentech) delivered directly into the clot by external ventricular drain almost doubles the odds of achieving a modified Rankin Score of 0-3 by 6 months.
More clot is removed – and patients with large intraventricular hemorrhages (IVHs) do better – with more vigorous alteplase dosing and when more than one drain is used.
The findings come from the Clot Lysis Evaluation of Accelerated Resolution (CLEAR III) trial, which randomized 249 IVH patients to 1 mg alteplase every 8 hours for up to 12 doses, and 251 to saline on the same schedule, delivered by external ventricular drain. The intervention didn’t make much difference with small hemorrhages.
In a video interview at the International Stroke Conference, investigator Dr. Issam Awad, a professor of surgery and neurology and director of neurovascular surgery at the University of Chicago, explained how to do the technique correctly for larger clots, and the expected benefits.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE INTERNATIONAL STROKE CONFERENCE
VIDEO: Intracranial warfarin bleeds smaller with prothrombin complex instead of FFP
LOS ANGELES – The international normalized ratio fell to 1.2 or less within 3 hours among 18 of 27 (67%) patients who received four-factor prothrombin complex concentrate (octaplex [Octapharma]) for warfarin-related intracranial hemorrhages, but only 2 of 23 (9%) who received fresh frozen plasma, according to a randomized trial from Germany.
Hematoma expansion was reduced by 16.9 mL (P = .026) at 3 hours and 16.4 mL (P = .018) at 24 hours in the prothrombin complex concentrate (PCC) group.
All the patients presented within 12 hours of symptom onset with an INR of at least 2; they received fresh frozen plasma (FFP) or four-factor PCC within an hour of their cerebral CT. There were eight deaths in the FFP group, including five due to hematoma expansion. The five deaths in the PCC group occurred after day 5, and one was thought to be because of hematoma expansion. Patients were 76 years old, on average, and the majority were men; both groups received vitamin K.
The findings make a case for PCC at a time when it’s unclear how best to handle warfarin-related intracranial bleeds, and whether the extra cost of PCC is worth it. Investigator Dr. Thorsten Steiner, a professor of neurology at the University of Heidelberg (Germany), addressed the relevant issues, including PCC safety, in a video interview at the International Stroke Conference sponsored by the American Heart Association. The investigator-initiated trial was funded by Octapharma, and Dr. Steiner reported receiving a research grant from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – The international normalized ratio fell to 1.2 or less within 3 hours among 18 of 27 (67%) patients who received four-factor prothrombin complex concentrate (octaplex [Octapharma]) for warfarin-related intracranial hemorrhages, but only 2 of 23 (9%) who received fresh frozen plasma, according to a randomized trial from Germany.
Hematoma expansion was reduced by 16.9 mL (P = .026) at 3 hours and 16.4 mL (P = .018) at 24 hours in the prothrombin complex concentrate (PCC) group.
All the patients presented within 12 hours of symptom onset with an INR of at least 2; they received fresh frozen plasma (FFP) or four-factor PCC within an hour of their cerebral CT. There were eight deaths in the FFP group, including five due to hematoma expansion. The five deaths in the PCC group occurred after day 5, and one was thought to be because of hematoma expansion. Patients were 76 years old, on average, and the majority were men; both groups received vitamin K.
The findings make a case for PCC at a time when it’s unclear how best to handle warfarin-related intracranial bleeds, and whether the extra cost of PCC is worth it. Investigator Dr. Thorsten Steiner, a professor of neurology at the University of Heidelberg (Germany), addressed the relevant issues, including PCC safety, in a video interview at the International Stroke Conference sponsored by the American Heart Association. The investigator-initiated trial was funded by Octapharma, and Dr. Steiner reported receiving a research grant from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – The international normalized ratio fell to 1.2 or less within 3 hours among 18 of 27 (67%) patients who received four-factor prothrombin complex concentrate (octaplex [Octapharma]) for warfarin-related intracranial hemorrhages, but only 2 of 23 (9%) who received fresh frozen plasma, according to a randomized trial from Germany.
Hematoma expansion was reduced by 16.9 mL (P = .026) at 3 hours and 16.4 mL (P = .018) at 24 hours in the prothrombin complex concentrate (PCC) group.
All the patients presented within 12 hours of symptom onset with an INR of at least 2; they received fresh frozen plasma (FFP) or four-factor PCC within an hour of their cerebral CT. There were eight deaths in the FFP group, including five due to hematoma expansion. The five deaths in the PCC group occurred after day 5, and one was thought to be because of hematoma expansion. Patients were 76 years old, on average, and the majority were men; both groups received vitamin K.
The findings make a case for PCC at a time when it’s unclear how best to handle warfarin-related intracranial bleeds, and whether the extra cost of PCC is worth it. Investigator Dr. Thorsten Steiner, a professor of neurology at the University of Heidelberg (Germany), addressed the relevant issues, including PCC safety, in a video interview at the International Stroke Conference sponsored by the American Heart Association. The investigator-initiated trial was funded by Octapharma, and Dr. Steiner reported receiving a research grant from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE INTERNATIONAL STROKE CONFERENCE
VIDEO: Herpes gladiatorum may be misdiagnosed as impetigo
WAIKOLOA, HAWAII – Athletes who wrestle, play rugby, or engage in any sport “where there’s a grinding of skin on skin” are at risk for herpes simplex gladiatorum, according to Dr. Andrew Krakowski.
The risk is exacerbated by the occlusive uniforms worn by athletes, which maintain a high moisture content – creating an environment hospitable to the spread of viruses, explained Dr. Krakowski, chief medical officer at DermOne, West Conshohocken, Pa.
In an interview at the Hawaii Dermatology Seminar, the dermatologist explained how HSV gladiatorum differs in appearance from classic vesicular herpes simplex, and how dermatologists and primary care physicians may misdiagnose these rashes as impetigo – or miss the diagnosis altogether.
He also provides recommendations on how to treat this condition when it is diagnosed and outlines measures to reduce the spread of the virus.
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. Krakowski is a consultant to Galderma and Valeant.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Athletes who wrestle, play rugby, or engage in any sport “where there’s a grinding of skin on skin” are at risk for herpes simplex gladiatorum, according to Dr. Andrew Krakowski.
The risk is exacerbated by the occlusive uniforms worn by athletes, which maintain a high moisture content – creating an environment hospitable to the spread of viruses, explained Dr. Krakowski, chief medical officer at DermOne, West Conshohocken, Pa.
In an interview at the Hawaii Dermatology Seminar, the dermatologist explained how HSV gladiatorum differs in appearance from classic vesicular herpes simplex, and how dermatologists and primary care physicians may misdiagnose these rashes as impetigo – or miss the diagnosis altogether.
He also provides recommendations on how to treat this condition when it is diagnosed and outlines measures to reduce the spread of the virus.
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. Krakowski is a consultant to Galderma and Valeant.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Athletes who wrestle, play rugby, or engage in any sport “where there’s a grinding of skin on skin” are at risk for herpes simplex gladiatorum, according to Dr. Andrew Krakowski.
The risk is exacerbated by the occlusive uniforms worn by athletes, which maintain a high moisture content – creating an environment hospitable to the spread of viruses, explained Dr. Krakowski, chief medical officer at DermOne, West Conshohocken, Pa.
In an interview at the Hawaii Dermatology Seminar, the dermatologist explained how HSV gladiatorum differs in appearance from classic vesicular herpes simplex, and how dermatologists and primary care physicians may misdiagnose these rashes as impetigo – or miss the diagnosis altogether.
He also provides recommendations on how to treat this condition when it is diagnosed and outlines measures to reduce the spread of the virus.
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. Krakowski is a consultant to Galderma and Valeant.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
ISC: Imaging supplants clocks for targeting stroke reperfusion
LOS ANGELES – Can brain imaging surpass the clock for identifying acute ischemic stroke patients who will benefit from thrombolytic or thrombectomy treatment?
That’s what experts now envision, based on early findings from several studies. Although the evidence is not yet definitive enough to justify using imaging as a replacement for time-from-stroke-onset in routine practice, the results so far are encouraging and have led to the start or planning of several phase III trials that will try to nail down a role for imaging, either CT or MR, to identify acute ischemic stroke patients who qualify for reperfusion therapy.
“What we’re trying to do is move away from using the clock as a surrogate marker and instead use imaging as the surrogate,” Dr. Jenny P. Tsai said in an interview at the International Stroke Conference.
The linchpin of this new approach is that clocking time elapsed from the onset of stroke symptoms to initiation of thrombolytic or endovascular treatment makes no allowance for patient-to-patient variations in collateral cerebral circulation, a factor that appears to make a big difference in whether patients can be many more hours removed from the start of their stroke and still have salvageable brain tissue. And relying on time since stroke symptom onset gives a seriously flawed estimate of a stroke’s duration when patients have an unwitnessed stroke.
The alternative is to use either CT perfusion imaging or a combination of MR perfusion and diffusion-weighted imaging “to get effective reperfusion treatments to patients who present at later time windows,” said Dr. Gregory W. Albers, professor of neurology at Stanford (Calif.) University and director of the Stanford Stroke Center. He called these two new approaches to gauging a patient’s suitability for reperfusion therapy “the next big thing in imaging” for stroke.
Using CT perfusion to assess target mismatch
Dr. Tsai presented an analysis of thrombectomy reperfusion done in 181 patients enrolled in the CT Perfusion to Predict Response to Recanalization in Ischemic Stroke Project (CRISP), which included a total of 201 acute ischemic stroke patients with large cerebral-artery occlusions treated at six U.S. centers. Her analysis excluded nine patients who presented more than 18 hours after their stroke onset, six patients who did not have successful CT perfusion assessment, and five additional patients excluded for other reasons. The 181 patients analyzed included 125 with a target mismatch in CT perfusion, indicating that salvageable tissue remained in the area of their stroke. Among these 125 patients, 111 underwent successful reperfusion by thrombectomy.
The researchers identified good treatment outcomes as patients with a modified Rankin Scale score of 2 or less 90 days after treatment. A multivariate analysis showed that among these 111 patients, achievement of a good 90-day outcome had no statistically significant relationship with time-to-treatment out to at least the first 8 hours following stroke onset, reported Dr. Tsai, a neurologist at the Stanford Stroke Center. The data also showed a nonsignificant relationship between good outcomes and time from stroke onset to treatment beyond 8 hours, but the confidence interval for this nonsignificant relationship became very wide at later times as the analysis focused on fewer and fewer patients.
“In patients with large-artery occlusions who have a target mismatch profile [on perfusion CT] and achieve successful reperfusion there is no significant association between onset-to-reperfusion-time and the probability of a good functional outcome,” suggesting that “CT perfusion is a biomarker of good outcomes beyond 6 hours” after stroke onset, Dr. Tsai concluded. CT perfusion has the advantage of being more widely available than MRI is, she added. Last year, her associates at Stanford reported similar findings using perfusion-diffusion mismatch in the cerebral area around a stroke visualized with MRI (Neurology. 2015 Aug 25;85[8]:708-15).
“MRI is not readily available” at all U.S. centers that treat stroke patients, while CT perfusion imaging is much more ubiquitous, but the findings reported by Dr. Tsai require confirmation in the several prospective, randomized trials now underway and testing this approach, Dr. Albers said.
Using MRI in unwitnessed strokes
A second challenge for using reperfusion therapy in stroke patients are patients who have unwitnessed strokes, with a completely unknown elapsed time from onset to presentation. The ability of MRI to help identify patients with unwitnessed stroke who can safely receive intravenous thrombolytic therapy with alteplase (tissue plasminogen activator, Activase) underwent testing in the MR WITNESS (Study of Intravenous Thrombolysis With Alteplase in MRI-Selected Patients) trial.
The study enrolled 80 patients with an unwitnessed acute, ischemic stroke at 10 U.S. centers. Patients had to be in a position to receive alteplase within 4.5 hours of when their stroke was first identified; 57 (71%) of the participants had wake-up strokes. All patients underwent two types of MRI to identify them as potential candidates for safe administration of alteplase: diffusion weighted imaging, to identify that a stroke had occurred, and fluid-attenuated inversion recovery (FLAIR) assessment, to identify strokes that had occurred during the prior 4 hours.
This phase II study’s primary safety endpoint was the incidence of symptomatic intracerebral hemorrhage following alteplase treatment, which occurred in 1 of the 80 patients (1.25%), not a statistically significant difference when compared with the historical standard, the 2.4% rate seen in stroke patients treated with intravenous alteplase 3 to 4.5 hours after their known stroke onset in the ECASS III (European Cooperative Acute Stroke Study) (N Engl J Med. 2008 Sept 25;359[13]:1317-29). The rate of asymptomatic intracerebral hemorrhage was not significantly different between the new study and ECASS III, reported Dr. Lee H. Schwamm, director of TeleStroke & Acute Stroke Services at the Massachusetts General Hospital in Boston.
Based on this result, “we know this approach is safe, and we saw a signal of efficacy, but we really don’t know how effective it will be” until this approach to assessing unwitnessed-stroke patients by imaging undergoes testing in a phase III trial, cautioned Dr. Schwamm at the meeting, sponsored by the American Heart Association.
Future work will also examine whether similar results can be obtained by CT imaging, which would “open this approach to every U.S. emergency department,” Dr. Schwamm said. Although the MR diffusion-weighted imaging and FLAIR analyses used in the current study do not require anything more than standard MRI equipment and software, it remains less available than CT imaging at most U.S. hospitals, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Traditionally, we have used a clock to identify patients who are eligible to receive reperfusion therapy, but now researchers are trying to extend patient eligibility with imaging. The Stanford (Calif.) team is trying to identify good candidates for reperfusion treatment who present with acute ischemic strokes beyond the traditional time window of 6 hours. The researchers at Massachusetts General Hospital, Boston, and their collaborators are trying to apply a similar approach to patients who have unwitnessed strokes and so have an unknown elapsed time from the start of their stroke.
The rationale behind the Stanford work is that some patients will have salvageable neurons beyond the traditional treatment time window and that this tissue can be identified by MR and CT perfusion imaging.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Bruce I. Ovbiagele |
The workers in Boston and their collaborators used MR diffusion weighted imaging to confirm that a patient has had a stroke, and then use MR fluid attenuated inversion recovery (FLAIR) to determine if the stroke had occurred within the previous 4 hours. If a stroke has not been going on long enough to produce a positive FLAIR image, it means that the patient is still eligible for thrombolytic therapy. This could be huge for U.S. clinical practice because so many patients have unwitnessed strokes. We definitely need a larger efficacy study, but the results Dr. Schwamm reported are highly encouraging.
CT is more widely available right now in U.S. practice than is MRI, so ideally we would like to be able to use CT imaging.
Dr. Bruce I. Ovbiagele is professor and chairman of neurology at the Medical University of South Carolina in Charleston. He had no disclosures. He made these comments in an interview.
Traditionally, we have used a clock to identify patients who are eligible to receive reperfusion therapy, but now researchers are trying to extend patient eligibility with imaging. The Stanford (Calif.) team is trying to identify good candidates for reperfusion treatment who present with acute ischemic strokes beyond the traditional time window of 6 hours. The researchers at Massachusetts General Hospital, Boston, and their collaborators are trying to apply a similar approach to patients who have unwitnessed strokes and so have an unknown elapsed time from the start of their stroke.
The rationale behind the Stanford work is that some patients will have salvageable neurons beyond the traditional treatment time window and that this tissue can be identified by MR and CT perfusion imaging.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Bruce I. Ovbiagele |
The workers in Boston and their collaborators used MR diffusion weighted imaging to confirm that a patient has had a stroke, and then use MR fluid attenuated inversion recovery (FLAIR) to determine if the stroke had occurred within the previous 4 hours. If a stroke has not been going on long enough to produce a positive FLAIR image, it means that the patient is still eligible for thrombolytic therapy. This could be huge for U.S. clinical practice because so many patients have unwitnessed strokes. We definitely need a larger efficacy study, but the results Dr. Schwamm reported are highly encouraging.
CT is more widely available right now in U.S. practice than is MRI, so ideally we would like to be able to use CT imaging.
Dr. Bruce I. Ovbiagele is professor and chairman of neurology at the Medical University of South Carolina in Charleston. He had no disclosures. He made these comments in an interview.
Traditionally, we have used a clock to identify patients who are eligible to receive reperfusion therapy, but now researchers are trying to extend patient eligibility with imaging. The Stanford (Calif.) team is trying to identify good candidates for reperfusion treatment who present with acute ischemic strokes beyond the traditional time window of 6 hours. The researchers at Massachusetts General Hospital, Boston, and their collaborators are trying to apply a similar approach to patients who have unwitnessed strokes and so have an unknown elapsed time from the start of their stroke.
The rationale behind the Stanford work is that some patients will have salvageable neurons beyond the traditional treatment time window and that this tissue can be identified by MR and CT perfusion imaging.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Bruce I. Ovbiagele |
The workers in Boston and their collaborators used MR diffusion weighted imaging to confirm that a patient has had a stroke, and then use MR fluid attenuated inversion recovery (FLAIR) to determine if the stroke had occurred within the previous 4 hours. If a stroke has not been going on long enough to produce a positive FLAIR image, it means that the patient is still eligible for thrombolytic therapy. This could be huge for U.S. clinical practice because so many patients have unwitnessed strokes. We definitely need a larger efficacy study, but the results Dr. Schwamm reported are highly encouraging.
CT is more widely available right now in U.S. practice than is MRI, so ideally we would like to be able to use CT imaging.
Dr. Bruce I. Ovbiagele is professor and chairman of neurology at the Medical University of South Carolina in Charleston. He had no disclosures. He made these comments in an interview.
LOS ANGELES – Can brain imaging surpass the clock for identifying acute ischemic stroke patients who will benefit from thrombolytic or thrombectomy treatment?
That’s what experts now envision, based on early findings from several studies. Although the evidence is not yet definitive enough to justify using imaging as a replacement for time-from-stroke-onset in routine practice, the results so far are encouraging and have led to the start or planning of several phase III trials that will try to nail down a role for imaging, either CT or MR, to identify acute ischemic stroke patients who qualify for reperfusion therapy.
“What we’re trying to do is move away from using the clock as a surrogate marker and instead use imaging as the surrogate,” Dr. Jenny P. Tsai said in an interview at the International Stroke Conference.
The linchpin of this new approach is that clocking time elapsed from the onset of stroke symptoms to initiation of thrombolytic or endovascular treatment makes no allowance for patient-to-patient variations in collateral cerebral circulation, a factor that appears to make a big difference in whether patients can be many more hours removed from the start of their stroke and still have salvageable brain tissue. And relying on time since stroke symptom onset gives a seriously flawed estimate of a stroke’s duration when patients have an unwitnessed stroke.
The alternative is to use either CT perfusion imaging or a combination of MR perfusion and diffusion-weighted imaging “to get effective reperfusion treatments to patients who present at later time windows,” said Dr. Gregory W. Albers, professor of neurology at Stanford (Calif.) University and director of the Stanford Stroke Center. He called these two new approaches to gauging a patient’s suitability for reperfusion therapy “the next big thing in imaging” for stroke.
Using CT perfusion to assess target mismatch
Dr. Tsai presented an analysis of thrombectomy reperfusion done in 181 patients enrolled in the CT Perfusion to Predict Response to Recanalization in Ischemic Stroke Project (CRISP), which included a total of 201 acute ischemic stroke patients with large cerebral-artery occlusions treated at six U.S. centers. Her analysis excluded nine patients who presented more than 18 hours after their stroke onset, six patients who did not have successful CT perfusion assessment, and five additional patients excluded for other reasons. The 181 patients analyzed included 125 with a target mismatch in CT perfusion, indicating that salvageable tissue remained in the area of their stroke. Among these 125 patients, 111 underwent successful reperfusion by thrombectomy.
The researchers identified good treatment outcomes as patients with a modified Rankin Scale score of 2 or less 90 days after treatment. A multivariate analysis showed that among these 111 patients, achievement of a good 90-day outcome had no statistically significant relationship with time-to-treatment out to at least the first 8 hours following stroke onset, reported Dr. Tsai, a neurologist at the Stanford Stroke Center. The data also showed a nonsignificant relationship between good outcomes and time from stroke onset to treatment beyond 8 hours, but the confidence interval for this nonsignificant relationship became very wide at later times as the analysis focused on fewer and fewer patients.
“In patients with large-artery occlusions who have a target mismatch profile [on perfusion CT] and achieve successful reperfusion there is no significant association between onset-to-reperfusion-time and the probability of a good functional outcome,” suggesting that “CT perfusion is a biomarker of good outcomes beyond 6 hours” after stroke onset, Dr. Tsai concluded. CT perfusion has the advantage of being more widely available than MRI is, she added. Last year, her associates at Stanford reported similar findings using perfusion-diffusion mismatch in the cerebral area around a stroke visualized with MRI (Neurology. 2015 Aug 25;85[8]:708-15).
“MRI is not readily available” at all U.S. centers that treat stroke patients, while CT perfusion imaging is much more ubiquitous, but the findings reported by Dr. Tsai require confirmation in the several prospective, randomized trials now underway and testing this approach, Dr. Albers said.
Using MRI in unwitnessed strokes
A second challenge for using reperfusion therapy in stroke patients are patients who have unwitnessed strokes, with a completely unknown elapsed time from onset to presentation. The ability of MRI to help identify patients with unwitnessed stroke who can safely receive intravenous thrombolytic therapy with alteplase (tissue plasminogen activator, Activase) underwent testing in the MR WITNESS (Study of Intravenous Thrombolysis With Alteplase in MRI-Selected Patients) trial.
The study enrolled 80 patients with an unwitnessed acute, ischemic stroke at 10 U.S. centers. Patients had to be in a position to receive alteplase within 4.5 hours of when their stroke was first identified; 57 (71%) of the participants had wake-up strokes. All patients underwent two types of MRI to identify them as potential candidates for safe administration of alteplase: diffusion weighted imaging, to identify that a stroke had occurred, and fluid-attenuated inversion recovery (FLAIR) assessment, to identify strokes that had occurred during the prior 4 hours.
This phase II study’s primary safety endpoint was the incidence of symptomatic intracerebral hemorrhage following alteplase treatment, which occurred in 1 of the 80 patients (1.25%), not a statistically significant difference when compared with the historical standard, the 2.4% rate seen in stroke patients treated with intravenous alteplase 3 to 4.5 hours after their known stroke onset in the ECASS III (European Cooperative Acute Stroke Study) (N Engl J Med. 2008 Sept 25;359[13]:1317-29). The rate of asymptomatic intracerebral hemorrhage was not significantly different between the new study and ECASS III, reported Dr. Lee H. Schwamm, director of TeleStroke & Acute Stroke Services at the Massachusetts General Hospital in Boston.
Based on this result, “we know this approach is safe, and we saw a signal of efficacy, but we really don’t know how effective it will be” until this approach to assessing unwitnessed-stroke patients by imaging undergoes testing in a phase III trial, cautioned Dr. Schwamm at the meeting, sponsored by the American Heart Association.
Future work will also examine whether similar results can be obtained by CT imaging, which would “open this approach to every U.S. emergency department,” Dr. Schwamm said. Although the MR diffusion-weighted imaging and FLAIR analyses used in the current study do not require anything more than standard MRI equipment and software, it remains less available than CT imaging at most U.S. hospitals, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
LOS ANGELES – Can brain imaging surpass the clock for identifying acute ischemic stroke patients who will benefit from thrombolytic or thrombectomy treatment?
That’s what experts now envision, based on early findings from several studies. Although the evidence is not yet definitive enough to justify using imaging as a replacement for time-from-stroke-onset in routine practice, the results so far are encouraging and have led to the start or planning of several phase III trials that will try to nail down a role for imaging, either CT or MR, to identify acute ischemic stroke patients who qualify for reperfusion therapy.
“What we’re trying to do is move away from using the clock as a surrogate marker and instead use imaging as the surrogate,” Dr. Jenny P. Tsai said in an interview at the International Stroke Conference.
The linchpin of this new approach is that clocking time elapsed from the onset of stroke symptoms to initiation of thrombolytic or endovascular treatment makes no allowance for patient-to-patient variations in collateral cerebral circulation, a factor that appears to make a big difference in whether patients can be many more hours removed from the start of their stroke and still have salvageable brain tissue. And relying on time since stroke symptom onset gives a seriously flawed estimate of a stroke’s duration when patients have an unwitnessed stroke.
The alternative is to use either CT perfusion imaging or a combination of MR perfusion and diffusion-weighted imaging “to get effective reperfusion treatments to patients who present at later time windows,” said Dr. Gregory W. Albers, professor of neurology at Stanford (Calif.) University and director of the Stanford Stroke Center. He called these two new approaches to gauging a patient’s suitability for reperfusion therapy “the next big thing in imaging” for stroke.
Using CT perfusion to assess target mismatch
Dr. Tsai presented an analysis of thrombectomy reperfusion done in 181 patients enrolled in the CT Perfusion to Predict Response to Recanalization in Ischemic Stroke Project (CRISP), which included a total of 201 acute ischemic stroke patients with large cerebral-artery occlusions treated at six U.S. centers. Her analysis excluded nine patients who presented more than 18 hours after their stroke onset, six patients who did not have successful CT perfusion assessment, and five additional patients excluded for other reasons. The 181 patients analyzed included 125 with a target mismatch in CT perfusion, indicating that salvageable tissue remained in the area of their stroke. Among these 125 patients, 111 underwent successful reperfusion by thrombectomy.
The researchers identified good treatment outcomes as patients with a modified Rankin Scale score of 2 or less 90 days after treatment. A multivariate analysis showed that among these 111 patients, achievement of a good 90-day outcome had no statistically significant relationship with time-to-treatment out to at least the first 8 hours following stroke onset, reported Dr. Tsai, a neurologist at the Stanford Stroke Center. The data also showed a nonsignificant relationship between good outcomes and time from stroke onset to treatment beyond 8 hours, but the confidence interval for this nonsignificant relationship became very wide at later times as the analysis focused on fewer and fewer patients.
“In patients with large-artery occlusions who have a target mismatch profile [on perfusion CT] and achieve successful reperfusion there is no significant association between onset-to-reperfusion-time and the probability of a good functional outcome,” suggesting that “CT perfusion is a biomarker of good outcomes beyond 6 hours” after stroke onset, Dr. Tsai concluded. CT perfusion has the advantage of being more widely available than MRI is, she added. Last year, her associates at Stanford reported similar findings using perfusion-diffusion mismatch in the cerebral area around a stroke visualized with MRI (Neurology. 2015 Aug 25;85[8]:708-15).
“MRI is not readily available” at all U.S. centers that treat stroke patients, while CT perfusion imaging is much more ubiquitous, but the findings reported by Dr. Tsai require confirmation in the several prospective, randomized trials now underway and testing this approach, Dr. Albers said.
Using MRI in unwitnessed strokes
A second challenge for using reperfusion therapy in stroke patients are patients who have unwitnessed strokes, with a completely unknown elapsed time from onset to presentation. The ability of MRI to help identify patients with unwitnessed stroke who can safely receive intravenous thrombolytic therapy with alteplase (tissue plasminogen activator, Activase) underwent testing in the MR WITNESS (Study of Intravenous Thrombolysis With Alteplase in MRI-Selected Patients) trial.
The study enrolled 80 patients with an unwitnessed acute, ischemic stroke at 10 U.S. centers. Patients had to be in a position to receive alteplase within 4.5 hours of when their stroke was first identified; 57 (71%) of the participants had wake-up strokes. All patients underwent two types of MRI to identify them as potential candidates for safe administration of alteplase: diffusion weighted imaging, to identify that a stroke had occurred, and fluid-attenuated inversion recovery (FLAIR) assessment, to identify strokes that had occurred during the prior 4 hours.
This phase II study’s primary safety endpoint was the incidence of symptomatic intracerebral hemorrhage following alteplase treatment, which occurred in 1 of the 80 patients (1.25%), not a statistically significant difference when compared with the historical standard, the 2.4% rate seen in stroke patients treated with intravenous alteplase 3 to 4.5 hours after their known stroke onset in the ECASS III (European Cooperative Acute Stroke Study) (N Engl J Med. 2008 Sept 25;359[13]:1317-29). The rate of asymptomatic intracerebral hemorrhage was not significantly different between the new study and ECASS III, reported Dr. Lee H. Schwamm, director of TeleStroke & Acute Stroke Services at the Massachusetts General Hospital in Boston.
Based on this result, “we know this approach is safe, and we saw a signal of efficacy, but we really don’t know how effective it will be” until this approach to assessing unwitnessed-stroke patients by imaging undergoes testing in a phase III trial, cautioned Dr. Schwamm at the meeting, sponsored by the American Heart Association.
Future work will also examine whether similar results can be obtained by CT imaging, which would “open this approach to every U.S. emergency department,” Dr. Schwamm said. Although the MR diffusion-weighted imaging and FLAIR analyses used in the current study do not require anything more than standard MRI equipment and software, it remains less available than CT imaging at most U.S. hospitals, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: New CT and MR techniques provide alternatives to time-from-stroke-onset to select acute ischemic stroke patients for reperfusion therapies.
Major finding: CT perfusion identified ischemic stroke patients who could undergo effective thrombectomy more than 6 hours after their stroke onset.
Data source: The CRISP study, which enrolled 201 patients at six U.S. centers.
Disclosures: Dr. Tsai and Dr. Schwamm had no disclosures. Dr. Albers has been a consultant to iSchemaView and Covidien/Medtronic and has an ownership interest in iSchemaView.
VIDEO: Genetic tests, clinical data sharpen pigmented lesion diagnosis
WAIKOLOA, HAWAII – While many pigmented lesions analyzed in the dermatopathology lab are easily classifiable as benign or malignant, a certain percentage of cases are “very challenging to all examiners” – and in those cases, newer testing methods such as immunostaining or genetic testing can provide useful information, according to Dr. Whitney High.
Morphologic analysis of pigmented lesions under the microscope to determine whether a lesion is benign or malignant has limitations, said Dr. High, director of dermatopathology at the University of Colorado at Denver, Aurora. “We don’t really actually know. We haven’t genetically queried the cells.”
In a video interview at the Hawaii Dermatology Seminar, Dr. High emphasized, however, that no test is 100% sensitive and 100% specific. In fact, such tests should be considered adjunctive – requiring “some type of physician oversight or guidance to decide what is a significant result, what is an insignificant result, what is a confounded result, [and] what is a discrepant result.”
Clinical information is also useful, Dr. High said, noting that when this information is not provided, “I don’t really have any feeling from the clinician as to whether the lesion is new, growing, changing, [or] doing anything suspicious.”
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. High had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – While many pigmented lesions analyzed in the dermatopathology lab are easily classifiable as benign or malignant, a certain percentage of cases are “very challenging to all examiners” – and in those cases, newer testing methods such as immunostaining or genetic testing can provide useful information, according to Dr. Whitney High.
Morphologic analysis of pigmented lesions under the microscope to determine whether a lesion is benign or malignant has limitations, said Dr. High, director of dermatopathology at the University of Colorado at Denver, Aurora. “We don’t really actually know. We haven’t genetically queried the cells.”
In a video interview at the Hawaii Dermatology Seminar, Dr. High emphasized, however, that no test is 100% sensitive and 100% specific. In fact, such tests should be considered adjunctive – requiring “some type of physician oversight or guidance to decide what is a significant result, what is an insignificant result, what is a confounded result, [and] what is a discrepant result.”
Clinical information is also useful, Dr. High said, noting that when this information is not provided, “I don’t really have any feeling from the clinician as to whether the lesion is new, growing, changing, [or] doing anything suspicious.”
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. High had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – While many pigmented lesions analyzed in the dermatopathology lab are easily classifiable as benign or malignant, a certain percentage of cases are “very challenging to all examiners” – and in those cases, newer testing methods such as immunostaining or genetic testing can provide useful information, according to Dr. Whitney High.
Morphologic analysis of pigmented lesions under the microscope to determine whether a lesion is benign or malignant has limitations, said Dr. High, director of dermatopathology at the University of Colorado at Denver, Aurora. “We don’t really actually know. We haven’t genetically queried the cells.”
In a video interview at the Hawaii Dermatology Seminar, Dr. High emphasized, however, that no test is 100% sensitive and 100% specific. In fact, such tests should be considered adjunctive – requiring “some type of physician oversight or guidance to decide what is a significant result, what is an insignificant result, what is a confounded result, [and] what is a discrepant result.”
Clinical information is also useful, Dr. High said, noting that when this information is not provided, “I don’t really have any feeling from the clinician as to whether the lesion is new, growing, changing, [or] doing anything suspicious.”
The Hawaii Dermatology Seminar is provided by Global Academy for Medical Education/Skin Disease Education Foundation. SDEF and this news organization are owned by the same parent company.
Dr. High had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: New microscopy tools improve melanoma detection
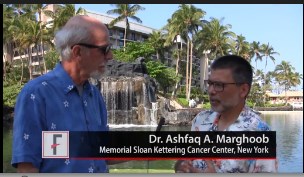
WAIKOLOA, HAWAII – Armed with dermoscopy and reflective confocal microscopy, dermatologists have been “pushing the envelope and becoming better and better at detecting melanoma and limiting the number of benign lesions being removed,” said Dr. Ashfaq A. Marghoob.
Dermoscopy – now used by about 75% of dermatologists in the United States – has lowered the benign-to-malignant ratio to about 5:1, Dr. Marghoob explained. That’s five benign nevi removed for every one melanoma found.
In an interview at the Hawaii Dermatology Seminar, Dr. Marghoob of Memorial Sloan Kettering Cancer Center, New York, discussed the impact that new technologies such as reflectance confocal microscopy are having on finding melanomas and differentiating them from benign nevi.
The Hawaii Dermatology Seminar is provided by the Global Academy for Medical Education/Skin Disease Education Foundation. The SDEF and this news organization are owned by the same parent company.
Dr. Marghoob had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Armed with dermoscopy and reflective confocal microscopy, dermatologists have been “pushing the envelope and becoming better and better at detecting melanoma and limiting the number of benign lesions being removed,” said Dr. Ashfaq A. Marghoob.
Dermoscopy – now used by about 75% of dermatologists in the United States – has lowered the benign-to-malignant ratio to about 5:1, Dr. Marghoob explained. That’s five benign nevi removed for every one melanoma found.
In an interview at the Hawaii Dermatology Seminar, Dr. Marghoob of Memorial Sloan Kettering Cancer Center, New York, discussed the impact that new technologies such as reflectance confocal microscopy are having on finding melanomas and differentiating them from benign nevi.
The Hawaii Dermatology Seminar is provided by the Global Academy for Medical Education/Skin Disease Education Foundation. The SDEF and this news organization are owned by the same parent company.
Dr. Marghoob had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAIKOLOA, HAWAII – Armed with dermoscopy and reflective confocal microscopy, dermatologists have been “pushing the envelope and becoming better and better at detecting melanoma and limiting the number of benign lesions being removed,” said Dr. Ashfaq A. Marghoob.
Dermoscopy – now used by about 75% of dermatologists in the United States – has lowered the benign-to-malignant ratio to about 5:1, Dr. Marghoob explained. That’s five benign nevi removed for every one melanoma found.
In an interview at the Hawaii Dermatology Seminar, Dr. Marghoob of Memorial Sloan Kettering Cancer Center, New York, discussed the impact that new technologies such as reflectance confocal microscopy are having on finding melanomas and differentiating them from benign nevi.
The Hawaii Dermatology Seminar is provided by the Global Academy for Medical Education/Skin Disease Education Foundation. The SDEF and this news organization are owned by the same parent company.
Dr. Marghoob had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF HAWAII DERMATOLOGY SEMINAR
VIDEO: Novel tools measure disease progression in MS
NEW ORLEANS – The visual system is relevant and accessible for the study of multiple sclerosis and can aid in the measurement of neuronal and axonal injury.
Capturing primary neuronal loss in the afferent visual pathway was among the topics addressed during a session focused on novel methods for measuring disease progression in MS at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
In this video interview at the meeting, session chair Dr. Fiona Costello of the University of Calgary, Alta., discussed the presentation on the visual pathway, as well as presentations on the use of microRNA biomarkers and the use of MRI as an outcome measure in progressive MS.
“The gestalt is that the field is moving in a new direction; the field is looking for not only a better understanding of what causes disability in MS, but also more reliable, objective, accessible means of capturing the same thing that is relevant and meaningful to patients and their caretakers,” she said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The visual system is relevant and accessible for the study of multiple sclerosis and can aid in the measurement of neuronal and axonal injury.
Capturing primary neuronal loss in the afferent visual pathway was among the topics addressed during a session focused on novel methods for measuring disease progression in MS at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
In this video interview at the meeting, session chair Dr. Fiona Costello of the University of Calgary, Alta., discussed the presentation on the visual pathway, as well as presentations on the use of microRNA biomarkers and the use of MRI as an outcome measure in progressive MS.
“The gestalt is that the field is moving in a new direction; the field is looking for not only a better understanding of what causes disability in MS, but also more reliable, objective, accessible means of capturing the same thing that is relevant and meaningful to patients and their caretakers,” she said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The visual system is relevant and accessible for the study of multiple sclerosis and can aid in the measurement of neuronal and axonal injury.
Capturing primary neuronal loss in the afferent visual pathway was among the topics addressed during a session focused on novel methods for measuring disease progression in MS at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
In this video interview at the meeting, session chair Dr. Fiona Costello of the University of Calgary, Alta., discussed the presentation on the visual pathway, as well as presentations on the use of microRNA biomarkers and the use of MRI as an outcome measure in progressive MS.
“The gestalt is that the field is moving in a new direction; the field is looking for not only a better understanding of what causes disability in MS, but also more reliable, objective, accessible means of capturing the same thing that is relevant and meaningful to patients and their caretakers,” she said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACTRIMS FORUM 2016
MAVERIC Precision Oncology Program
Federal Practitioner talks one-on-one with Louis Fiore, MD, MPH, the executive director of the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC), which the VA created as 1 of 3 epidemiological research centers. At MAVERIC Fiore is spearheading a precision oncology program, which is developing precision oncology best practices; enhancing patient and provider engagement; and fostering collaboration among the VA, National Cancer Institute, academia, and other health care systems to provide cancer patients with access to clinical trial participation.
Federal Practitioner talks one-on-one with Louis Fiore, MD, MPH, the executive director of the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC), which the VA created as 1 of 3 epidemiological research centers. At MAVERIC Fiore is spearheading a precision oncology program, which is developing precision oncology best practices; enhancing patient and provider engagement; and fostering collaboration among the VA, National Cancer Institute, academia, and other health care systems to provide cancer patients with access to clinical trial participation.
Federal Practitioner talks one-on-one with Louis Fiore, MD, MPH, the executive director of the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC), which the VA created as 1 of 3 epidemiological research centers. At MAVERIC Fiore is spearheading a precision oncology program, which is developing precision oncology best practices; enhancing patient and provider engagement; and fostering collaboration among the VA, National Cancer Institute, academia, and other health care systems to provide cancer patients with access to clinical trial participation.