User login
A tip of the cap
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Commentary: Antibiotics use and vaccine antibody levels
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
This study of antibiotic use in the first 2 years of life in a reasonably standardized primary care office raises issues about antibiotic stewardship that can be the basis for counseling against antibiotics for viral infections or mild uncomplicated acute otitis media (AOM) above 6 months of age. Even unintended and previously undescribed downstream effects of antibiotics should play a role in our decisions and are another nudge toward prudent antibiotic use – for example, watchful waiting (WW) for AOM.
Some families ask for antibiotics for almost any infection while others may want antibiotics only if really necessary. But maybe patient family wishes are not the main driver, considering a report in Pediatrics (2022;150[1]:e2021055613). They analyzed over 2 million AOM episodes from billing/enrollment records from the MarketScan commercial claims research databases. They reported that, despite WW being the management of choice per American Academy of Pediatrics guidelines for uncomplicated AOM in children over 1 year of age, WW use had not increased between 2015 and 2019. Further, they noted that WW was not related to patient factors or demographics but was associated with specialty and provider. For example, WW use was five times more likely by otolaryngologists than pediatricians and less likely by nonpediatricians than pediatricians. Further, some clinicians used WW a lot, while others almost not at all (high-volume antibiotic prescribers). Of note, having a fever significantly lowered the chance of WW.
Maturing data on antibiotic-related alterations in species distribution and quantity within children’s microbiome plus potential effects on antibody responses to vaccines are ideas families need to hear. I suggest sharing these as part of anticipatory guidance at well-child checks as early in life as is feasible.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
Antibiotics use and vaccine antibody levels
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).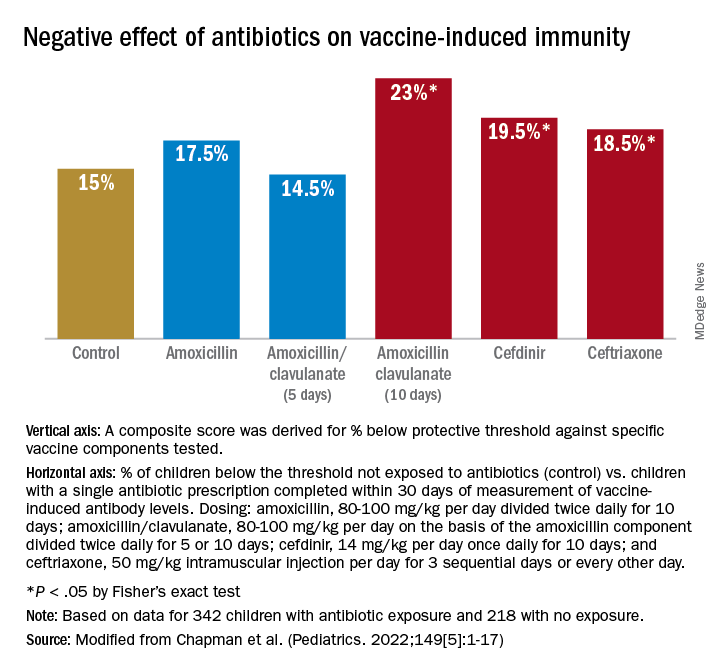
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).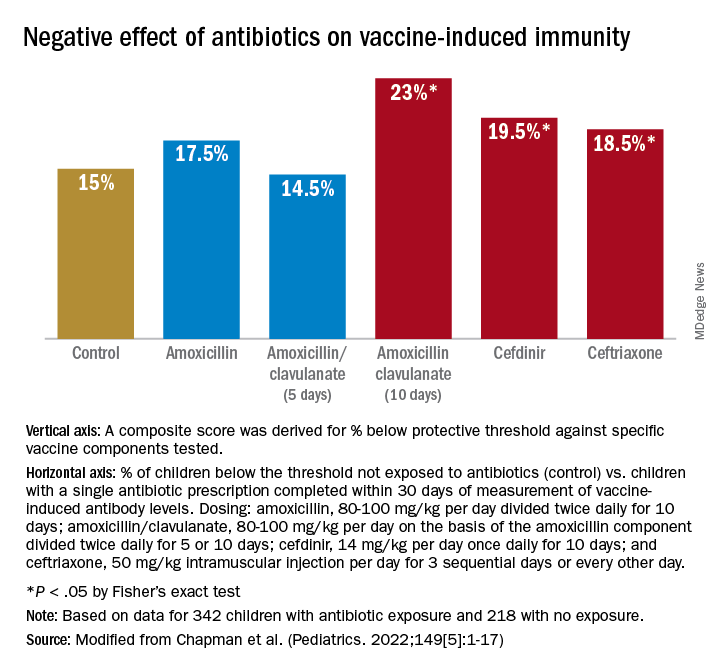
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
In this column I have previously discussed the microbiome and its importance to health, especially as it relates to infections in children. Given the appreciated connection between microbiome and immunity, my group in Rochester, N.Y., recently undertook a study of the effect of antibiotic usage on the immune response to routine early childhood vaccines. In mouse models, it was previously shown that antibiotic exposure induced a reduction in the abundance and diversity of gut microbiota that in turn negatively affected the generation and maintenance of vaccine-induced immunity.1,2 A study from Stanford University was the first experimental human trial of antibiotic effects on vaccine responses. Adult volunteers were given an antibiotic or not before seasonal influenza vaccination and the researchers identified specific bacteria in the gut that were reduced by the antibiotics given. Those normal bacteria in the gut microbiome were shown to provide positive immunity signals to the systemic immune system that potentiated vaccine responses.3
My group conducted the first-ever study in children to explore whether an association existed between antibiotic use and vaccine-induced antibody levels. In the May issue of Pediatrics we report results from 560 children studied.4 From these children, 11,888 serum antibody levels to vaccine antigens were measured. Vaccine-induced antibody levels were determined at various time points after primary vaccination at child age 2, 4, and 6 months and boosters at age 12-18 months for 10 antigens included in four vaccines: DTaP, Hib, IPV, and PCV. The antibody levels to vaccine components were measured to DTaP (diphtheria toxoid, pertussis toxoid, tetanus toxoid, pertactin, and filamentous hemagglutinin), Hib conjugate (polyribosylribitol phosphate), IPV (polio 2), and PCV (serotypes 6B, 14, and 23F). A total of 342 children with 1,678 antibiotic courses prescribed were compared with 218 children with no antibiotic exposures. The predominant antibiotics prescribed were amoxicillin, cefdinir, amoxicillin/clavulanate, and ceftriaxone, since most treatments were for acute otitis media.
Of possible high clinical relevance, we found that from 9 to 24 months of age, children with antibiotic exposure had a higher frequency of vaccine-induced antibody levels below protection compared with children with no antibiotic use, placing them at risk of contracting a vaccine-preventable infection for DTaP antigens DT, TT, and PT and for PCV serotype 14.
For time points where antibody levels were determined within 30 days of completion of a course of antibiotics (recent antibiotic use), individual antibiotics were analyzed for effect on antibody levels below protective levels. Across all vaccine antigens measured, we found that all antibiotics had a negative effect on antibody levels and percentage of children achieving the protective antibody level threshold. Amoxicillin use had a lower association with lower antibody levels than the broader spectrum antibiotics, amoxicillin clavulanate (Augmentin), cefdinir, and ceftriaxone. For children receiving amoxicillin/clavulanate prescriptions, it was possible to compare the effect of shorter versus longer courses and we found that a 5-day course was associated with subprotective antibody levels similar to 10 days of amoxicillin, whereas 10-day amoxicillin/clavulanate was associated with higher frequency of children having subprotective antibody levels (Figure).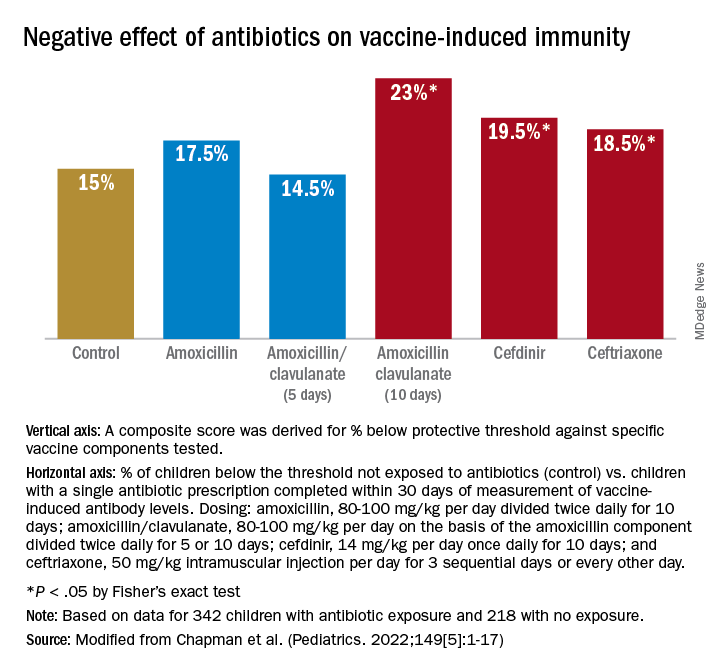
We examined whether accumulation of antibiotic courses in the first year of life had an association with subsequent vaccine-induced antibody levels and found that each antibiotic prescription was associated with a reduction in the median antibody level. For DTaP, each prescription was associated with 5.8% drop in antibody level to the vaccine components. For Hib the drop was 6.8%, IPV was 11.3%, and PCV was 10.4% – all statistically significant. To determine if booster vaccination influenced this association, a second analysis was performed using antibiotic prescriptions up to 15 months of age. We found each antibiotic prescription was associated with a reduction in median vaccine-induced antibody levels for DTaP by 18%, Hib by 21%, IPV by 19%, and PCV by 12% – all statistically significant.
Our study is the first in young children during the early age window where vaccine-induced immunity is established. Antibiotic use was associated with increased frequency of subprotective antibody levels for several vaccines used in children up to 2 years of age. The lower antibody levels could leave children vulnerable to vaccine preventable diseases. Perhaps outbreaks of vaccine-preventable diseases, such as pertussis, may be a consequence of multiple courses of antibiotics suppressing vaccine-induced immunity.
A goal of this study was to explore potential acute and long-term effects of antibiotic exposure on vaccine-induced antibody levels. Accumulated antibiotic courses up to booster immunization was associated with decreased vaccine antibody levels both before and after booster, suggesting that booster immunization was not sufficient to change the negative association with antibiotic exposure. The results were similar for all vaccines tested, suggesting that the specific vaccine formulation was not a factor.
The study has several limitations. The antibiotic prescription data and measurements of vaccine-induced antibody levels were recorded and measured prospectively; however, our analysis was done retrospectively. The group of study children was derived from my private practice in Rochester, N.Y., and may not be broadly representative of all children. The number of vaccine antibody measurements was limited by serum availability at some sampling time points in some children; and sometimes, the serum samples were collected far apart, which weakened our ability to perform longitudinal analyses. We did not collect stool samples from the children so we could not directly study the effect of antibiotic courses on the gut microbiome.
Our study adds new reasons to be cautious about overprescribing antibiotics on an individual child basis because an adverse effect extends to reduction in vaccine responses. This should be explained to parents requesting unnecessary antibiotics for colds and coughs. When antibiotics are necessary, the judicious choice of a narrow-spectrum antibiotic or a shorter duration of a broader spectrum antibiotic may reduce adverse effects on vaccine-induced immunity.
References
1. Valdez Y et al. Influence of the microbiota on vaccine effectiveness. Trends Immunol. 2014;35(11):526-37.
2. Lynn MA et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe. 2018;23(5):653-60.e5.
3. Hagan T et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell. 2019;178(6):1313-28.e13.
4. Chapman T et al. Antibiotic use and vaccine antibody levels. Pediatrics. 2022;149(5);1-17. doi: 10.1542/peds.2021-052061.
It’s time to shame the fat shamers
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
Career pivots: A new perspective on psychiatry
Psychiatrists practice a field of medicine that relies on one’s clinical perspective to interpret observable behaviors originating from the brains of others. In this manner, psychiatry and photography are similar. And digital technology has changed them both.
In photography, there are many technical aspects for one to master when framing and capturing a shot. The length of exposure. The amount of light needed. The speed of the film, which is its sensitivity to light. The aperture that controls how much light falls on the film. The movement of the subject across the film during the exposure. Despite the fact that physical film has mostly yielded to electronic sensors over the past couple decades, these basic aspects of photography remain.
But perspective is the critical ingredient. This is what brings the greatest impact to photography. The composition, or the subject of the photograph and how its elements – foreground, background, shapes, patterns, texture, shadow, motion, leading lines, and focal points – are arranged. The most powerful way to improve the composition – more powerful than fancy camera bells and whistles – is to move. One step to the left or right, one step forward or back. Stand on your toes, or crouch to your knees. Pivot this way or that. A simple change in perspective dramatically changes the nature and the energy of the captured image.
In fact, many physicians are changing what they actually do for a living. Pivoting their clinical perspectives. And applying those perspectives to other areas. The latest catalyst fueling these career pivots, these changes in perspectives, has been the incredible global impact of the tiny little coronavirus known as SARS-CoV-2. The COVID-19 pandemic that began two years ago has disrupted the entire planet. The virus has caused us all to change our perspective, to see our world differently, and our place in it.
The virus has exposed defects in our health care delivery system. And physicians have necessarily reacted, injecting changes in what they do and how they do it. Many of these changes rely on digital technology, building upon the groundwork laid over the past couple of decades to convert our paper processes into electronic processes, and our manual work flows into digital work flows. This groundwork is no small thing, as it relies on conventions and standards, such as DICOM, LOINC, AES, CDA, UMLS, FHIR, ICD, NDC, USCDI, and SNOMED-CT. Establishing, maintaining, and evolving health care standards requires organized groups of people to come together to share their diverse perspectives. This is but one of many places where physicians are using their unique clinical perspective to share what they see with others.
This column will focus on these professional pivots that physicians make when they take a step to the left or right to change their perspective and share their viewpoints in different settings with diverse groups of people. Some of these pivots are small, while others are career changing. But the theme that knits them together is about taking what one has learned while helping others achieve better health, and using that perspective to make a difference.
Dr. Daviss is chief medical officer for Optum Maryland and immediate past president of the Maryland-DC Society of Addiction Medicine, and former medical director and senior medical advisor at SAMHSA. He is coauthor of the 2011 book, Shrink Rap: Three Psychiatrists Explain Their Work. Psychiatrists and other physicians may share their own experience with pivots they have made with Dr. Daviss via email ([email protected]) or Twitter (@HITshrink). The opinions expressed are solely those of the author and do not necessarily reflect those of his employer or organizations with which he is associated.
Psychiatrists practice a field of medicine that relies on one’s clinical perspective to interpret observable behaviors originating from the brains of others. In this manner, psychiatry and photography are similar. And digital technology has changed them both.
In photography, there are many technical aspects for one to master when framing and capturing a shot. The length of exposure. The amount of light needed. The speed of the film, which is its sensitivity to light. The aperture that controls how much light falls on the film. The movement of the subject across the film during the exposure. Despite the fact that physical film has mostly yielded to electronic sensors over the past couple decades, these basic aspects of photography remain.
But perspective is the critical ingredient. This is what brings the greatest impact to photography. The composition, or the subject of the photograph and how its elements – foreground, background, shapes, patterns, texture, shadow, motion, leading lines, and focal points – are arranged. The most powerful way to improve the composition – more powerful than fancy camera bells and whistles – is to move. One step to the left or right, one step forward or back. Stand on your toes, or crouch to your knees. Pivot this way or that. A simple change in perspective dramatically changes the nature and the energy of the captured image.
In fact, many physicians are changing what they actually do for a living. Pivoting their clinical perspectives. And applying those perspectives to other areas. The latest catalyst fueling these career pivots, these changes in perspectives, has been the incredible global impact of the tiny little coronavirus known as SARS-CoV-2. The COVID-19 pandemic that began two years ago has disrupted the entire planet. The virus has caused us all to change our perspective, to see our world differently, and our place in it.
The virus has exposed defects in our health care delivery system. And physicians have necessarily reacted, injecting changes in what they do and how they do it. Many of these changes rely on digital technology, building upon the groundwork laid over the past couple of decades to convert our paper processes into electronic processes, and our manual work flows into digital work flows. This groundwork is no small thing, as it relies on conventions and standards, such as DICOM, LOINC, AES, CDA, UMLS, FHIR, ICD, NDC, USCDI, and SNOMED-CT. Establishing, maintaining, and evolving health care standards requires organized groups of people to come together to share their diverse perspectives. This is but one of many places where physicians are using their unique clinical perspective to share what they see with others.
This column will focus on these professional pivots that physicians make when they take a step to the left or right to change their perspective and share their viewpoints in different settings with diverse groups of people. Some of these pivots are small, while others are career changing. But the theme that knits them together is about taking what one has learned while helping others achieve better health, and using that perspective to make a difference.
Dr. Daviss is chief medical officer for Optum Maryland and immediate past president of the Maryland-DC Society of Addiction Medicine, and former medical director and senior medical advisor at SAMHSA. He is coauthor of the 2011 book, Shrink Rap: Three Psychiatrists Explain Their Work. Psychiatrists and other physicians may share their own experience with pivots they have made with Dr. Daviss via email ([email protected]) or Twitter (@HITshrink). The opinions expressed are solely those of the author and do not necessarily reflect those of his employer or organizations with which he is associated.
Psychiatrists practice a field of medicine that relies on one’s clinical perspective to interpret observable behaviors originating from the brains of others. In this manner, psychiatry and photography are similar. And digital technology has changed them both.
In photography, there are many technical aspects for one to master when framing and capturing a shot. The length of exposure. The amount of light needed. The speed of the film, which is its sensitivity to light. The aperture that controls how much light falls on the film. The movement of the subject across the film during the exposure. Despite the fact that physical film has mostly yielded to electronic sensors over the past couple decades, these basic aspects of photography remain.
But perspective is the critical ingredient. This is what brings the greatest impact to photography. The composition, or the subject of the photograph and how its elements – foreground, background, shapes, patterns, texture, shadow, motion, leading lines, and focal points – are arranged. The most powerful way to improve the composition – more powerful than fancy camera bells and whistles – is to move. One step to the left or right, one step forward or back. Stand on your toes, or crouch to your knees. Pivot this way or that. A simple change in perspective dramatically changes the nature and the energy of the captured image.
In fact, many physicians are changing what they actually do for a living. Pivoting their clinical perspectives. And applying those perspectives to other areas. The latest catalyst fueling these career pivots, these changes in perspectives, has been the incredible global impact of the tiny little coronavirus known as SARS-CoV-2. The COVID-19 pandemic that began two years ago has disrupted the entire planet. The virus has caused us all to change our perspective, to see our world differently, and our place in it.
The virus has exposed defects in our health care delivery system. And physicians have necessarily reacted, injecting changes in what they do and how they do it. Many of these changes rely on digital technology, building upon the groundwork laid over the past couple of decades to convert our paper processes into electronic processes, and our manual work flows into digital work flows. This groundwork is no small thing, as it relies on conventions and standards, such as DICOM, LOINC, AES, CDA, UMLS, FHIR, ICD, NDC, USCDI, and SNOMED-CT. Establishing, maintaining, and evolving health care standards requires organized groups of people to come together to share their diverse perspectives. This is but one of many places where physicians are using their unique clinical perspective to share what they see with others.
This column will focus on these professional pivots that physicians make when they take a step to the left or right to change their perspective and share their viewpoints in different settings with diverse groups of people. Some of these pivots are small, while others are career changing. But the theme that knits them together is about taking what one has learned while helping others achieve better health, and using that perspective to make a difference.
Dr. Daviss is chief medical officer for Optum Maryland and immediate past president of the Maryland-DC Society of Addiction Medicine, and former medical director and senior medical advisor at SAMHSA. He is coauthor of the 2011 book, Shrink Rap: Three Psychiatrists Explain Their Work. Psychiatrists and other physicians may share their own experience with pivots they have made with Dr. Daviss via email ([email protected]) or Twitter (@HITshrink). The opinions expressed are solely those of the author and do not necessarily reflect those of his employer or organizations with which he is associated.
Screening for anxiety in young children
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
On April 12, 2022, the U.S. Preventive Services Task Force released the draft of a recommendation statement titled Screening for Anxiety in Children and Adolescents. Based on their observation that 7.8% of children and adolescents have a current anxiety disorder and their analysis of the magnitude of the net benefit, the Task Force plans on recommending that children ages 8-18 years be screened for the condition. However, the group could not find evidence to support screening for children 7 years and younger.
Over more than 4 decades of general pediatric practice, it became obvious to me that anxiety was driving a high percentage of my office visits. Most often in young children it was parental anxiety that was prompting the phone call or office visit. In older childhood and adolescence it was patient anxiety that began to play a larger role.
Over the last 2 decades the level of anxiety in all age groups has seemed to increase. How large a role the events of Sept. 11, 2001, and other terrorist attacks were playing in this phenomenon is unclear to me. However, I suspect they were significant. More recently the pandemic and the failure of both political parties to forge a working arrangement have fueled even more anxiety in many demographic segments. It may be safe to say that everyone is anxious to one degree or another.
Broad-based anxiety in the general population and the incidence of anxiety disorders severe enough to disrupt a child’s life are certainly two different kettles of fish. However, the factors that have raised the level of anxiety across all age groups certainly hasn’t made things any easier for the child who has inherited or developed an anxiety disorder.
Glancing at the 600-page evidence synthesis that accompanies the task force’s report it is clear that they have taken their challenge seriously. However, I wonder whether looking at the 7-and-under age group with a different lens might have resulted in the inclusion of younger children in their recommendation.
I understand that to support their recommendations the U.S. Preventive Services Task Forces must rely on data from peer-reviewed studies that have looked at quantifiable outcomes. However, I suspect the task force would agree that its recommendations shouldn’t prevent the rest of us from using our own observations and intuition when deciding whether to selectively screen our younger patients for anxiety disorders.
Although it may not generate a measurable data point, providing the parents of a 5-year-old whose troubling behavior is in part the result of an anxiety disorder is invaluable. Do we need to screen all 5-year-olds? The task force says probably not given the current state of our knowledge and I agree. But, the fact that almost 8% of the pediatric population carries the diagnosis and my anecdotal observations suggest that as pediatricians we should be learning more about anxiety disorders and their wide variety of presentations. Then we should selectively screen more of our patients. In fact, I suspect we might help our patients and ourselves by questioning more parents about their own mental health histories even before we have any inkling that their child has a problem. While the degree to which anxiety disorders are inheritable and the exact mechanism is far from clear, I think this history might be a valuable piece of information to learn as early as the prenatal get-acquainted visit. A simple question to a new or expecting parent about what worries them most about becoming a parent would be a good opener. Your reassurance that you expect parents to be worried and welcome hearing about their concerns should be a step in building a strong foundation for a family-provider relationship.
Anxiety happens and unfortunately so do anxiety disorders. We need to be doing a better job of acknowledging and responding to these two realities.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
*This column was updated on 5/4/2022.
Smartphone diagnosis in infant seizures could be highly effective
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
This video transcript has been edited for clarity.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner, reporting from the American Epilepsy Society meeting.
Today, I have the pleasure of speaking with Dr. Chethan Rao, a child and adolescent neurology resident from the Mayo Clinic in Jacksonville, Fla. Dr. Rao has a particular interest in pediatric epilepsy. Welcome, Dr. Rao.
Chethan Rao, DO: Thank you, Dr. Wilner. It’s a pleasure to be here, and thanks for taking the time to highlight our work.
Dr. Wilner: You had a very interesting paper at the meeting that I wanted to talk about, focused on infantile spasms and smartphone video. Before we dive into the paper, tell us: What are infantile spasms, and why is it important to diagnose them early?
Dr. Rao: Infantile spasms, also known as epileptic spasms, are 1- to 2-second seizures, and they typically consist of sudden stiffening of the body with brief bending forward or backward of the arms, legs, and head. They usually happen around age 3-8 months, and they typically occur in clusters, most often after awakening from sleep.
The incidence is about 1 in 2,000-3,000 children. Many kids with spasms go on to develop seizures that are very difficult to treat, like Lennox-Gastaut epilepsy, and many go on to have developmental delays as well.
Dr. Wilner: Are these subtle? In other words, could a parent have a child like that and not really recognize that this is something abnormal? Or are they so dramatic that parents say: “We’re going to the emergency room?”
Dr. Rao: One of the problems that we encounter often is that in this age group of infants, they have benign sleep myoclonus; they have Sandifer syndrome related to reflux. Those can be very difficult mimics of spasms. They’re not the most clear-cut, but they look usually different enough from normal baby movements that they get parents to seek medical attention.
Dr. Wilner: You mentioned that the infantile spasms really are a type of epilepsy and symptomatic, usually, of some underlying neurologic condition. Why is it so important to diagnose them early?
Dr. Rao: Great question. Many studies have looked at developmental outcomes based on when spasms were diagnosed and treated, and all of them have replicated time over time that the earlier you get to treatment for the spasms, the better the outcomes are for seizure control and for development.
For this reason, infantile spasm is considered a neurologic urgency in our world. Like I said, accurate diagnosis is often complicated by these potential mimics. Prompt EEG is one of the most important things for confirmation of diagnosis.
Dr. Wilner: But to get that EEG, it has to get all the way to the neurologist, right? It’s not something they’re going to do in the ER. I saw a statistic: There are millions, if not billions, of smartphones out there. Where does the smartphone come in?
Dr. Rao: Absolutely. One of the things that we have on our side these days is that almost everyone has a smartphone at their disposal. One of the recent polls in 2021 showed that more than 95% of adults of childbearing age have smartphones with video access. As some other studies have shown in the adult world, we all really have an epilepsy monitoring unit minus the EEG in our own pockets.
It’s definitely a useful tool, as that first screening video can be used in adjunct to history and physical. There have been many of studies on the adult epilepsy side showing the predictive value of smartphone video for differentiating things like epileptic seizures and nonepileptic spells. What we wanted to do is use smartphone video to pin the diagnosis early of infantile spasms and get it treated as quickly as possible.
Dr. Wilner: I’m a fan. Every now and then, I do have a patient who brings in a video of some spell. I’m an adult neurologist. The patient had a spell, and you ask them – of course they don’t remember – and you ask the witness, who usually is not a trained observer. There have been one or two occasions where I thought: “Well, I don’t know if that was really a seizure.” Then they show me the video and it’s like, “Wow, that is definitely a convulsion.” A picture definitely can be worth a thousand words.
You studied this systematically for your poster. Tell me about what you did.
Dr. Rao: Since the poster, we’ve actually expanded the study, so I’ll give you the updated version. We looked at 101 infants retrospectively at two large children’s health care centers: Nemours Children’s, associated with Mayo Clinic in Jacksonville, Fla., and Texas Children’s Hospital in Houston. We narrowed it down to 80 patients whom we included. Of these, 43 had smartphone video capture when they first presented and 37 had no video when they first presented.
We found a 17-day difference by median in the time to diagnosis and treatment. In other words, the video group was diagnosed and treated 17 days by median, compared with the no-video group. Although 17 days may not sound like a big number, in this context it can make a huge difference. That’s been shown by one of these key studies in our field called the UK Infantile Spasms Study. The 2-week difference made about a 10-point difference on the developmental scale that they use – so pretty significant.
Dr. Wilner: Let me think about this for a minute. Was that because the parents brought the child in with their video and the doctor said, “Hey, that’s infantile spasms. Here’s your shot of ACTH [or whatever they’re using these days].” Or was it because the parents who were attentive enough to use video brought their kids in sooner?
Or was this the time from when they brought the child in to treatment? Is that the time you looked at? So it wasn’t just that these were more attentive parents and more likely to use the video – you’re looking at the time from presentation with or without video until treatment, is that right?
Dr. Rao: We looked to the time from the start of the spasms, as reported by the parents, to the time of diagnosis and then the start of spasms to the time of treatment. What you asked was a fantastic question. We wanted to know who these parents are who are taking videos versus the ones that are not.
We looked at the race/ethnicity data and socioeconomic status data. There were no significant differences between the video and nonvideo group. That would not explain the difference in our results here.
Dr. Wilner: Do you have plans to follow these approximately 40 children 5 years from now and see who’s riding a bicycle and who’s still stuck in the stroller? Is there going to be a difference?
Dr. Rao: Because time to diagnosis and time to treatment were our primary outcomes, long-term follow-up may not really help as much in this study. We did have a couple of other ideas for future studies. One that we wanted to look at was kids who have risk factors for developing spasms, such as trisomy 21, tuberous sclerosis, and congenital cortical malformations; those kids are at a much higher risk for developing spasms around 3-8 months of life.
In giving targeted counseling to those families about how they can use smartphone video to minimize the time to diagnosis and treatment, we think we may be able to learn more and maybe do that prospectively.
The other interesting idea is using artificial intelligence technology for spasm detection in some of these smartphone videos. They’re already using it for different seizure types. It could be an efficient first pass when we get a whole bunch of smartphone videos to determine which ones we need to pursue further steps – to see whether we need to get long-term EEG monitoring or not.
Dr. Wilner: As an epileptologist, I was going to say that we have smartphone EKG. All we need now is smartphone EEG, and then you’ll have all the information you need on day one. It may be a ways away.
As a bottom line, would it be fair to say that parents should not hesitate to take a video of any suspiciously abnormal behavior and bring it to their family doctor or pediatric neurologist?
Dr. Rao: Yes. I was happy to see the Tuberous Sclerosis Alliance put out a promotional video that had some steps for when parents see things that are suspicious for spasms, and they do recommend using smartphone video and promptly showing it to their doctors. I think the difference that we hope to provide in this study is that we can now quantify the effect of having that smartphone video when they first present.
My takeaway from this study that I would like to show is encouraging the use of smartphone video as an adjunct tool and for providers to ask for the videos, but also for these pediatric centers to develop an infrastructure – either a secure, monitored email address like we have at our center or a patient portal – where parents can submit video concerning for spasms.
Dr. Wilner: Save the trip to the doctor. Get that video out there first.
Dr. Rao: Especially in the pandemic world, right?
Dr. Wilner: Yes. I understand that you are a neurology resident. To wrap up, what’s the next step for you?
Dr. Rao: I’m finishing up my child neurology residency this year, and I’m moving out to Stanford for pediatric epilepsy fellowship. We’re preparing this project we’re talking about for submission soon, and we’re working on another project, which is a systematic review of genetic testing and the presurgical workup for pediatric drug-resistant focal epilepsy.
Dr. Wilner: Excellent. That’s pretty exciting. Good luck to you. I want to thank you very much for telling us about your research.
Dr. Rao: It was a pleasure speaking with you, and I look forward to the next time.
Dr. Wilner: I’m Dr Andrew Wilner, reporting for Medscape. Thanks for watching.
A version of this article first appeared on Medscape.com.
Review of new drugs that may be used during pregnancy
In 2021, the Food and Drug Administration approved 50 new drugs, but 24 will not be described here because they would probably not be used in pregnancy. The 24 are Aduhelm (aducanumab) to treat Alzheimer’s disease; Azstarys (serdexmethylphenidate and dexmethylphenidate), a combination CNS stimulant indicated for the treatment of ADHD; Cabenuva (cabotegravir and rilpivirine) to treat HIV; Voxzogo (vosoritide) for children with achondroplasia and open epiphyses; Qelbree (viloxazine) used in children aged 6-17 years to treat ADHD; and Pylarify (piflufolastat) for prostate cancer. Other anticancer drugs that will not be covered are Cosela (trilaciclib), Cytalux (pafolacianine), Exkivity (mobocertinib); Fotivda (tivozanib), Jemperli (dostarlimab-gxly), Lumakras (sotorasib), Pepaxto (melphalan flufenamide), Rybrevant (amivantamab-vmjw), Rylaze (asparaginase erwinia chrysanthemi), Scemblix (asciminib), Tepmetko (tepotinib), Tivdak (tisotumab vedotin-tftv), Truseltiq (infigratinib), Ukoniq (umbralisib), and Zynlonta (loncastuximab tesirine-lpyl).
Skytrofa (lonapegsomatropin-tcgd) will not be described below because it is indicated to treat short stature and is unlikely to be used in pregnancy. Nextstellis (drospirenone and estetrol) is used to prevent pregnancy.
Typically, for new drugs there will be no published reports describing their use in pregnant women. That information will come much later. In the sections below, the indications, effects on pregnant animals, and the potential for harm of a fetus/embryo are described. However, the relevance of animal data to human pregnancies is not great.
Adbry (tralokinumab) (molecular weight [MW], 147 kilodaltons), is indicated for the treatment of moderate to severe atopic dermatitis in adult patients whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. The drug did not harm fetal monkeys at doses that were 10 times the maximum recommended human dose.
Besremi (ropeginterferon alfa-2b-njft) (MW, 60 kDa) is an interferon alfa-2b indicated for the treatment of adults with polycythemia vera. It is given by subcutaneous injection every 2 weeks. Animal studies assessing reproductive toxicity have not been conducted. The manufacturer states that the drug may cause fetal harm and should be assumed to have abortifacient potential.
Brexafemme (ibrexafungerp) (MW, 922) is indicated for the treatment of vulvovaginal candidiasis. The drug was teratogenic in pregnant rabbits but not in pregnant rats. The manufacturer recommends females with reproductive potential should use effective contraception during treatment and for 4 days after the final dose.
Bylvay (odevixibat) (MW unknown) is indicated for the treatment of pruritus in patients aged 3 months and older. There are no human data regarding its use in pregnant women. The drug was teratogenic in pregnant rabbits. Although there are no data, the drug has low absorption following oral administration and breastfeeding is not expected to result in exposure of the infant.
Empaveli (pegcetacoplan) (MW, 44 kDa) is used to treat paroxysmal nocturnal hemoglobinuria. When the drug was given to pregnant cynomolgus monkeys there was an increase in abortions and stillbirths.
Evkeeza (evinacumab-dgnb) (MW, 146k) is used to treat homozygous familial hypercholesterolemia. The drug was teratogenic in rabbits but not rats.
Fexinidazole (MW not specified) is indicated to treat human African trypanosomiasis caused by the parasite Trypanosoma brucei gambiense. Additional information not available.
Kerendia (finerenone) (MW, 378), is indicated to reduce the risk of kidney and heart complications in chronic kidney disease associated with type 2 diabetes. The drug was teratogenic in rats.
Korsuva (difelikefalin) (MW, 679) is a kappa opioid–receptor agonist indicated for the treatment of moderate to severe pruritus associated with chronic kidney disease in adults undergoing hemodialysis. No adverse effects were observed in pregnant rats and rabbits. The limited human data on use of Korsuva in pregnant women are not sufficient to evaluate a drug associated risk for major birth defects or miscarriage.
Leqvio (inclisiran) (MW, 17,285) is indicated to treat heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease as an add-on therapy. The drug was not teratogenic in rats and rabbits.
Livmarli (maralixibat) (MW, 710) is indicated for the treatment of cholestatic pruritus associated with Alagille syndrome. Because systemic absorption is low, the recommended clinical dose is not expected to result in measurable fetal exposure. No effects on fetal rats were observed.
Livtencity (maribavir) (MW, 376) is used to treat posttransplant cytomegalovirus infection that has not responded to other treatment. Embryo/fetal survival was reduced in rats but not in rabbits at doses less then the human dose.
Lupkynis (voclosporin) (MW, 1,215) is used to treat nephritis. Avoid use of Lupkynis in pregnant women because of the alcohol content of the drug formulation. The drug was embryocidal and feticidal in rats and rabbits but with no treatment-related fetal malformations or variations.
Lybalvi (olanzapine and samidorphan) (MW, 312 and 505) is a combination drug used to treat schizophrenia and bipolar disorder. It was fetal toxic in pregnant rats and rabbits but with no evidence of malformations. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including this drug, during pregnancy. Health care providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit the Reproductive Psychiatry Resource and Information Center of the MGH Center for Women’s Mental Health.
Nexviazyme (avalglucosidase alfa-ngpt) (MW, 124k) is a hydrolytic lysosomal glycogen-specific enzyme indicated for the treatment of patients aged 1 year and older with late-onset Pompe disease. The drug was not teratogenic in mice and rabbits.
Nulibry (fosdenopterin) (MW, 480) is used to reduce the risk of mortality in molybdenum cofactor deficiency type A. Studies have not been conducted in pregnant animals.
Ponvory (ponesimod) (MW, 461) is used to treat relapsing forms of multiple sclerosis. The drug caused severe adverse effects in pregnant rats and rabbits.
Qulipta (atogepant) (MW, 604) is indicated to prevent episodic migraines. It is embryo/fetal toxic in rats and rabbits.
Saphnelo (anifrolumab-fnia) (MW, 148k) is used to treat moderate to severe systemic lupus erythematosus along with standard therapy. In pregnant cynomolgus monkeys, there was no evidence of embryotoxicity or fetal malformations with exposures up to approximately 28 times the exposure at the maximum recommended human dose.
Tavneos (avacopan) (MW, 582) is indicated to treat severe active antineutrophil cytoplasmic autoantibody–associated vasculitis in combination with standard therapy including glucocorticoids. There appears to be an increased risk for hepatotoxicity. The drug caused no defects in hamsters and rabbits, but in rabbits there was an increase in abortions.
Tezspire (tezepelumab-ekko) (MW, 147k) is indicated to treat severe asthma as an add-on maintenance therapy. No adverse fetal effects were observed in pregnant cynomolgus monkeys.
Verquvo (vericiguat) (MW, 426) is used to mitigate the risk of cardiovascular death and hospitalization for chronic heart failure. The drug was teratogenic in pregnant rabbits but not rats.
Vyvgart (efgartigimod alfa-fcab) (MW, 54k) is indicated to treat generalized myasthenia gravis. The drug did not cause birth defects in rats and rabbits.
Welireg (belzutifan) (MW, 383) is used to treat von Hippel–Lindau disease. In pregnant rats, the drug caused embryo-fetal lethality, reduced fetal body weight, and caused fetal skeletal malformations at maternal exposures of at least 0.2 times the human exposures.
Zegalogue (dasiglucagon) (MW, 3,382) is used to treat severe hypoglycemia. The drug did not cause birth defects in pregnant rats and rabbits.
Breastfeeding
It is not known if the above drugs will be in breast milk, but the safest course for an infant is to not breast feed if the mother is taking any of the above drugs.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2021, the Food and Drug Administration approved 50 new drugs, but 24 will not be described here because they would probably not be used in pregnancy. The 24 are Aduhelm (aducanumab) to treat Alzheimer’s disease; Azstarys (serdexmethylphenidate and dexmethylphenidate), a combination CNS stimulant indicated for the treatment of ADHD; Cabenuva (cabotegravir and rilpivirine) to treat HIV; Voxzogo (vosoritide) for children with achondroplasia and open epiphyses; Qelbree (viloxazine) used in children aged 6-17 years to treat ADHD; and Pylarify (piflufolastat) for prostate cancer. Other anticancer drugs that will not be covered are Cosela (trilaciclib), Cytalux (pafolacianine), Exkivity (mobocertinib); Fotivda (tivozanib), Jemperli (dostarlimab-gxly), Lumakras (sotorasib), Pepaxto (melphalan flufenamide), Rybrevant (amivantamab-vmjw), Rylaze (asparaginase erwinia chrysanthemi), Scemblix (asciminib), Tepmetko (tepotinib), Tivdak (tisotumab vedotin-tftv), Truseltiq (infigratinib), Ukoniq (umbralisib), and Zynlonta (loncastuximab tesirine-lpyl).
Skytrofa (lonapegsomatropin-tcgd) will not be described below because it is indicated to treat short stature and is unlikely to be used in pregnancy. Nextstellis (drospirenone and estetrol) is used to prevent pregnancy.
Typically, for new drugs there will be no published reports describing their use in pregnant women. That information will come much later. In the sections below, the indications, effects on pregnant animals, and the potential for harm of a fetus/embryo are described. However, the relevance of animal data to human pregnancies is not great.
Adbry (tralokinumab) (molecular weight [MW], 147 kilodaltons), is indicated for the treatment of moderate to severe atopic dermatitis in adult patients whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. The drug did not harm fetal monkeys at doses that were 10 times the maximum recommended human dose.
Besremi (ropeginterferon alfa-2b-njft) (MW, 60 kDa) is an interferon alfa-2b indicated for the treatment of adults with polycythemia vera. It is given by subcutaneous injection every 2 weeks. Animal studies assessing reproductive toxicity have not been conducted. The manufacturer states that the drug may cause fetal harm and should be assumed to have abortifacient potential.
Brexafemme (ibrexafungerp) (MW, 922) is indicated for the treatment of vulvovaginal candidiasis. The drug was teratogenic in pregnant rabbits but not in pregnant rats. The manufacturer recommends females with reproductive potential should use effective contraception during treatment and for 4 days after the final dose.
Bylvay (odevixibat) (MW unknown) is indicated for the treatment of pruritus in patients aged 3 months and older. There are no human data regarding its use in pregnant women. The drug was teratogenic in pregnant rabbits. Although there are no data, the drug has low absorption following oral administration and breastfeeding is not expected to result in exposure of the infant.
Empaveli (pegcetacoplan) (MW, 44 kDa) is used to treat paroxysmal nocturnal hemoglobinuria. When the drug was given to pregnant cynomolgus monkeys there was an increase in abortions and stillbirths.
Evkeeza (evinacumab-dgnb) (MW, 146k) is used to treat homozygous familial hypercholesterolemia. The drug was teratogenic in rabbits but not rats.
Fexinidazole (MW not specified) is indicated to treat human African trypanosomiasis caused by the parasite Trypanosoma brucei gambiense. Additional information not available.
Kerendia (finerenone) (MW, 378), is indicated to reduce the risk of kidney and heart complications in chronic kidney disease associated with type 2 diabetes. The drug was teratogenic in rats.
Korsuva (difelikefalin) (MW, 679) is a kappa opioid–receptor agonist indicated for the treatment of moderate to severe pruritus associated with chronic kidney disease in adults undergoing hemodialysis. No adverse effects were observed in pregnant rats and rabbits. The limited human data on use of Korsuva in pregnant women are not sufficient to evaluate a drug associated risk for major birth defects or miscarriage.
Leqvio (inclisiran) (MW, 17,285) is indicated to treat heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease as an add-on therapy. The drug was not teratogenic in rats and rabbits.
Livmarli (maralixibat) (MW, 710) is indicated for the treatment of cholestatic pruritus associated with Alagille syndrome. Because systemic absorption is low, the recommended clinical dose is not expected to result in measurable fetal exposure. No effects on fetal rats were observed.
Livtencity (maribavir) (MW, 376) is used to treat posttransplant cytomegalovirus infection that has not responded to other treatment. Embryo/fetal survival was reduced in rats but not in rabbits at doses less then the human dose.
Lupkynis (voclosporin) (MW, 1,215) is used to treat nephritis. Avoid use of Lupkynis in pregnant women because of the alcohol content of the drug formulation. The drug was embryocidal and feticidal in rats and rabbits but with no treatment-related fetal malformations or variations.
Lybalvi (olanzapine and samidorphan) (MW, 312 and 505) is a combination drug used to treat schizophrenia and bipolar disorder. It was fetal toxic in pregnant rats and rabbits but with no evidence of malformations. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including this drug, during pregnancy. Health care providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit the Reproductive Psychiatry Resource and Information Center of the MGH Center for Women’s Mental Health.
Nexviazyme (avalglucosidase alfa-ngpt) (MW, 124k) is a hydrolytic lysosomal glycogen-specific enzyme indicated for the treatment of patients aged 1 year and older with late-onset Pompe disease. The drug was not teratogenic in mice and rabbits.
Nulibry (fosdenopterin) (MW, 480) is used to reduce the risk of mortality in molybdenum cofactor deficiency type A. Studies have not been conducted in pregnant animals.
Ponvory (ponesimod) (MW, 461) is used to treat relapsing forms of multiple sclerosis. The drug caused severe adverse effects in pregnant rats and rabbits.
Qulipta (atogepant) (MW, 604) is indicated to prevent episodic migraines. It is embryo/fetal toxic in rats and rabbits.
Saphnelo (anifrolumab-fnia) (MW, 148k) is used to treat moderate to severe systemic lupus erythematosus along with standard therapy. In pregnant cynomolgus monkeys, there was no evidence of embryotoxicity or fetal malformations with exposures up to approximately 28 times the exposure at the maximum recommended human dose.
Tavneos (avacopan) (MW, 582) is indicated to treat severe active antineutrophil cytoplasmic autoantibody–associated vasculitis in combination with standard therapy including glucocorticoids. There appears to be an increased risk for hepatotoxicity. The drug caused no defects in hamsters and rabbits, but in rabbits there was an increase in abortions.
Tezspire (tezepelumab-ekko) (MW, 147k) is indicated to treat severe asthma as an add-on maintenance therapy. No adverse fetal effects were observed in pregnant cynomolgus monkeys.
Verquvo (vericiguat) (MW, 426) is used to mitigate the risk of cardiovascular death and hospitalization for chronic heart failure. The drug was teratogenic in pregnant rabbits but not rats.
Vyvgart (efgartigimod alfa-fcab) (MW, 54k) is indicated to treat generalized myasthenia gravis. The drug did not cause birth defects in rats and rabbits.
Welireg (belzutifan) (MW, 383) is used to treat von Hippel–Lindau disease. In pregnant rats, the drug caused embryo-fetal lethality, reduced fetal body weight, and caused fetal skeletal malformations at maternal exposures of at least 0.2 times the human exposures.
Zegalogue (dasiglucagon) (MW, 3,382) is used to treat severe hypoglycemia. The drug did not cause birth defects in pregnant rats and rabbits.
Breastfeeding
It is not known if the above drugs will be in breast milk, but the safest course for an infant is to not breast feed if the mother is taking any of the above drugs.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2021, the Food and Drug Administration approved 50 new drugs, but 24 will not be described here because they would probably not be used in pregnancy. The 24 are Aduhelm (aducanumab) to treat Alzheimer’s disease; Azstarys (serdexmethylphenidate and dexmethylphenidate), a combination CNS stimulant indicated for the treatment of ADHD; Cabenuva (cabotegravir and rilpivirine) to treat HIV; Voxzogo (vosoritide) for children with achondroplasia and open epiphyses; Qelbree (viloxazine) used in children aged 6-17 years to treat ADHD; and Pylarify (piflufolastat) for prostate cancer. Other anticancer drugs that will not be covered are Cosela (trilaciclib), Cytalux (pafolacianine), Exkivity (mobocertinib); Fotivda (tivozanib), Jemperli (dostarlimab-gxly), Lumakras (sotorasib), Pepaxto (melphalan flufenamide), Rybrevant (amivantamab-vmjw), Rylaze (asparaginase erwinia chrysanthemi), Scemblix (asciminib), Tepmetko (tepotinib), Tivdak (tisotumab vedotin-tftv), Truseltiq (infigratinib), Ukoniq (umbralisib), and Zynlonta (loncastuximab tesirine-lpyl).
Skytrofa (lonapegsomatropin-tcgd) will not be described below because it is indicated to treat short stature and is unlikely to be used in pregnancy. Nextstellis (drospirenone and estetrol) is used to prevent pregnancy.
Typically, for new drugs there will be no published reports describing their use in pregnant women. That information will come much later. In the sections below, the indications, effects on pregnant animals, and the potential for harm of a fetus/embryo are described. However, the relevance of animal data to human pregnancies is not great.
Adbry (tralokinumab) (molecular weight [MW], 147 kilodaltons), is indicated for the treatment of moderate to severe atopic dermatitis in adult patients whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. The drug did not harm fetal monkeys at doses that were 10 times the maximum recommended human dose.
Besremi (ropeginterferon alfa-2b-njft) (MW, 60 kDa) is an interferon alfa-2b indicated for the treatment of adults with polycythemia vera. It is given by subcutaneous injection every 2 weeks. Animal studies assessing reproductive toxicity have not been conducted. The manufacturer states that the drug may cause fetal harm and should be assumed to have abortifacient potential.
Brexafemme (ibrexafungerp) (MW, 922) is indicated for the treatment of vulvovaginal candidiasis. The drug was teratogenic in pregnant rabbits but not in pregnant rats. The manufacturer recommends females with reproductive potential should use effective contraception during treatment and for 4 days after the final dose.
Bylvay (odevixibat) (MW unknown) is indicated for the treatment of pruritus in patients aged 3 months and older. There are no human data regarding its use in pregnant women. The drug was teratogenic in pregnant rabbits. Although there are no data, the drug has low absorption following oral administration and breastfeeding is not expected to result in exposure of the infant.
Empaveli (pegcetacoplan) (MW, 44 kDa) is used to treat paroxysmal nocturnal hemoglobinuria. When the drug was given to pregnant cynomolgus monkeys there was an increase in abortions and stillbirths.
Evkeeza (evinacumab-dgnb) (MW, 146k) is used to treat homozygous familial hypercholesterolemia. The drug was teratogenic in rabbits but not rats.
Fexinidazole (MW not specified) is indicated to treat human African trypanosomiasis caused by the parasite Trypanosoma brucei gambiense. Additional information not available.
Kerendia (finerenone) (MW, 378), is indicated to reduce the risk of kidney and heart complications in chronic kidney disease associated with type 2 diabetes. The drug was teratogenic in rats.
Korsuva (difelikefalin) (MW, 679) is a kappa opioid–receptor agonist indicated for the treatment of moderate to severe pruritus associated with chronic kidney disease in adults undergoing hemodialysis. No adverse effects were observed in pregnant rats and rabbits. The limited human data on use of Korsuva in pregnant women are not sufficient to evaluate a drug associated risk for major birth defects or miscarriage.
Leqvio (inclisiran) (MW, 17,285) is indicated to treat heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease as an add-on therapy. The drug was not teratogenic in rats and rabbits.
Livmarli (maralixibat) (MW, 710) is indicated for the treatment of cholestatic pruritus associated with Alagille syndrome. Because systemic absorption is low, the recommended clinical dose is not expected to result in measurable fetal exposure. No effects on fetal rats were observed.
Livtencity (maribavir) (MW, 376) is used to treat posttransplant cytomegalovirus infection that has not responded to other treatment. Embryo/fetal survival was reduced in rats but not in rabbits at doses less then the human dose.
Lupkynis (voclosporin) (MW, 1,215) is used to treat nephritis. Avoid use of Lupkynis in pregnant women because of the alcohol content of the drug formulation. The drug was embryocidal and feticidal in rats and rabbits but with no treatment-related fetal malformations or variations.
Lybalvi (olanzapine and samidorphan) (MW, 312 and 505) is a combination drug used to treat schizophrenia and bipolar disorder. It was fetal toxic in pregnant rats and rabbits but with no evidence of malformations. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including this drug, during pregnancy. Health care providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit the Reproductive Psychiatry Resource and Information Center of the MGH Center for Women’s Mental Health.
Nexviazyme (avalglucosidase alfa-ngpt) (MW, 124k) is a hydrolytic lysosomal glycogen-specific enzyme indicated for the treatment of patients aged 1 year and older with late-onset Pompe disease. The drug was not teratogenic in mice and rabbits.
Nulibry (fosdenopterin) (MW, 480) is used to reduce the risk of mortality in molybdenum cofactor deficiency type A. Studies have not been conducted in pregnant animals.
Ponvory (ponesimod) (MW, 461) is used to treat relapsing forms of multiple sclerosis. The drug caused severe adverse effects in pregnant rats and rabbits.
Qulipta (atogepant) (MW, 604) is indicated to prevent episodic migraines. It is embryo/fetal toxic in rats and rabbits.
Saphnelo (anifrolumab-fnia) (MW, 148k) is used to treat moderate to severe systemic lupus erythematosus along with standard therapy. In pregnant cynomolgus monkeys, there was no evidence of embryotoxicity or fetal malformations with exposures up to approximately 28 times the exposure at the maximum recommended human dose.
Tavneos (avacopan) (MW, 582) is indicated to treat severe active antineutrophil cytoplasmic autoantibody–associated vasculitis in combination with standard therapy including glucocorticoids. There appears to be an increased risk for hepatotoxicity. The drug caused no defects in hamsters and rabbits, but in rabbits there was an increase in abortions.
Tezspire (tezepelumab-ekko) (MW, 147k) is indicated to treat severe asthma as an add-on maintenance therapy. No adverse fetal effects were observed in pregnant cynomolgus monkeys.
Verquvo (vericiguat) (MW, 426) is used to mitigate the risk of cardiovascular death and hospitalization for chronic heart failure. The drug was teratogenic in pregnant rabbits but not rats.
Vyvgart (efgartigimod alfa-fcab) (MW, 54k) is indicated to treat generalized myasthenia gravis. The drug did not cause birth defects in rats and rabbits.
Welireg (belzutifan) (MW, 383) is used to treat von Hippel–Lindau disease. In pregnant rats, the drug caused embryo-fetal lethality, reduced fetal body weight, and caused fetal skeletal malformations at maternal exposures of at least 0.2 times the human exposures.
Zegalogue (dasiglucagon) (MW, 3,382) is used to treat severe hypoglycemia. The drug did not cause birth defects in pregnant rats and rabbits.
Breastfeeding
It is not known if the above drugs will be in breast milk, but the safest course for an infant is to not breast feed if the mother is taking any of the above drugs.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Indications and techniques for multifetal pregnancy reduction
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.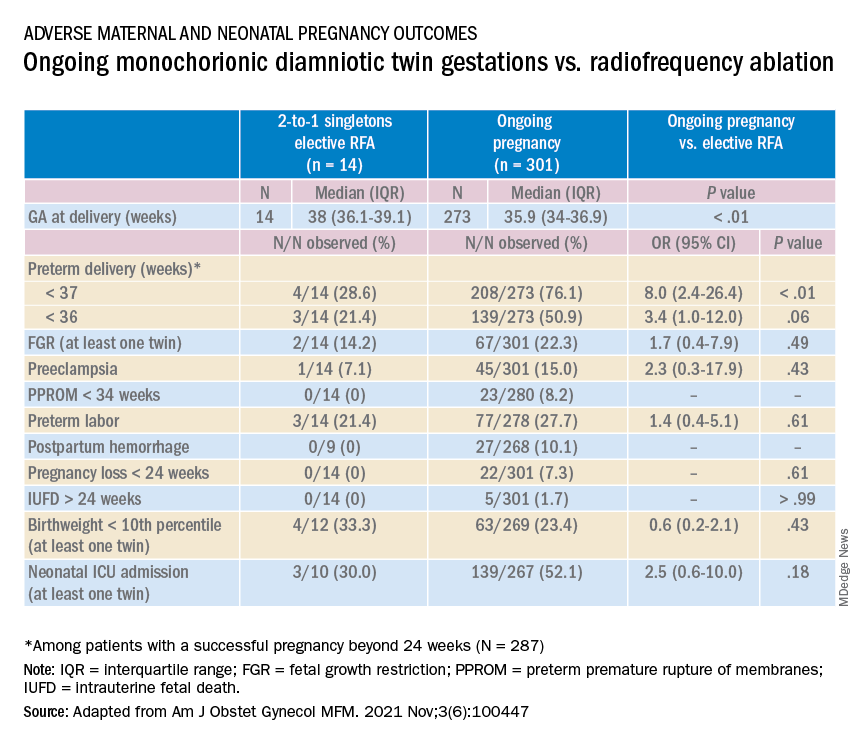
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.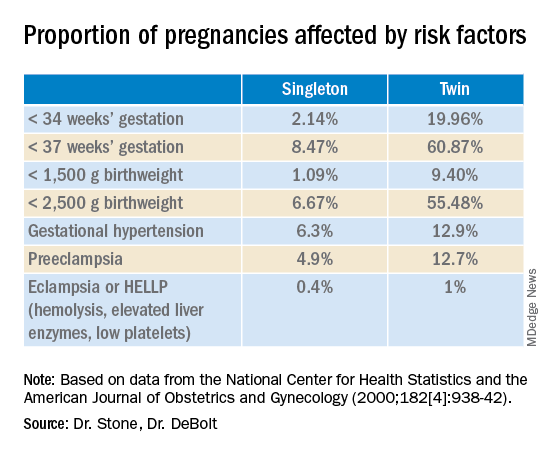
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.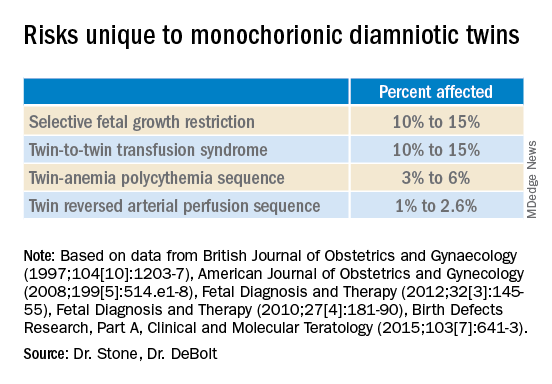
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.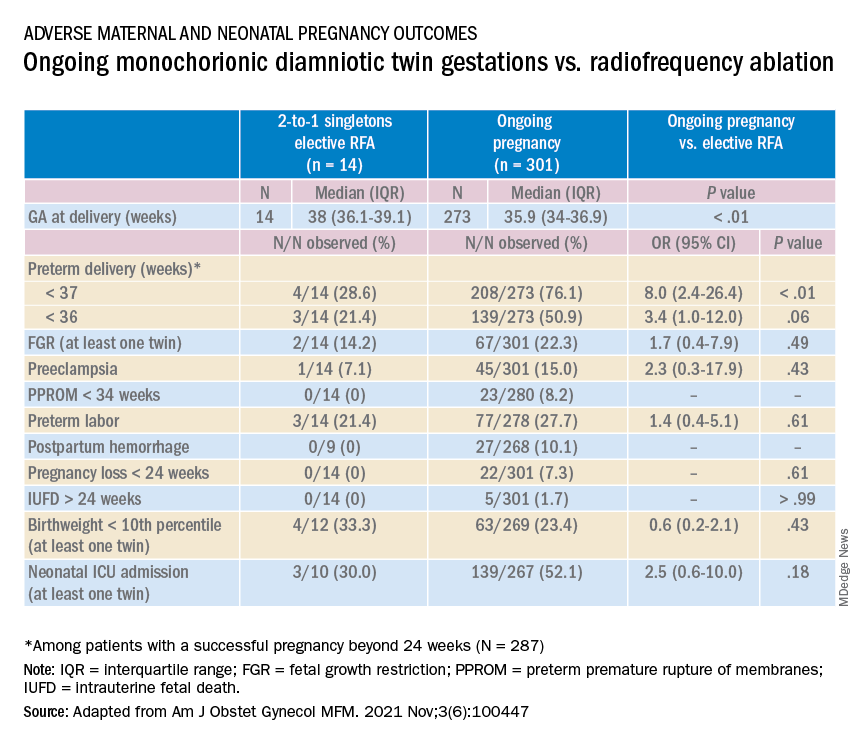
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.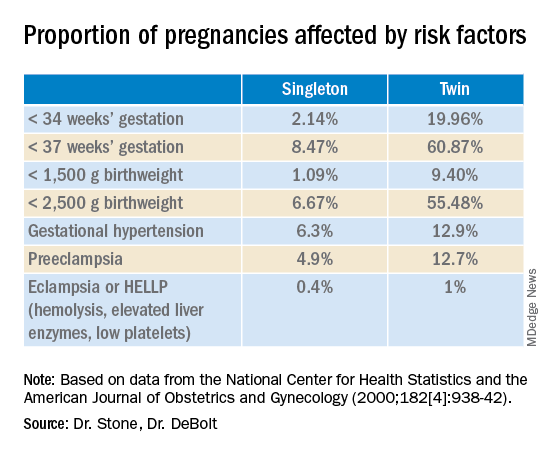
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.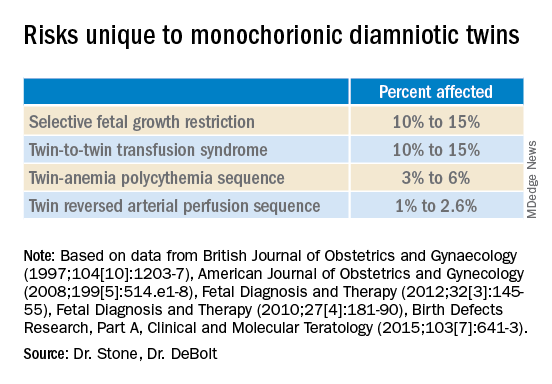
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.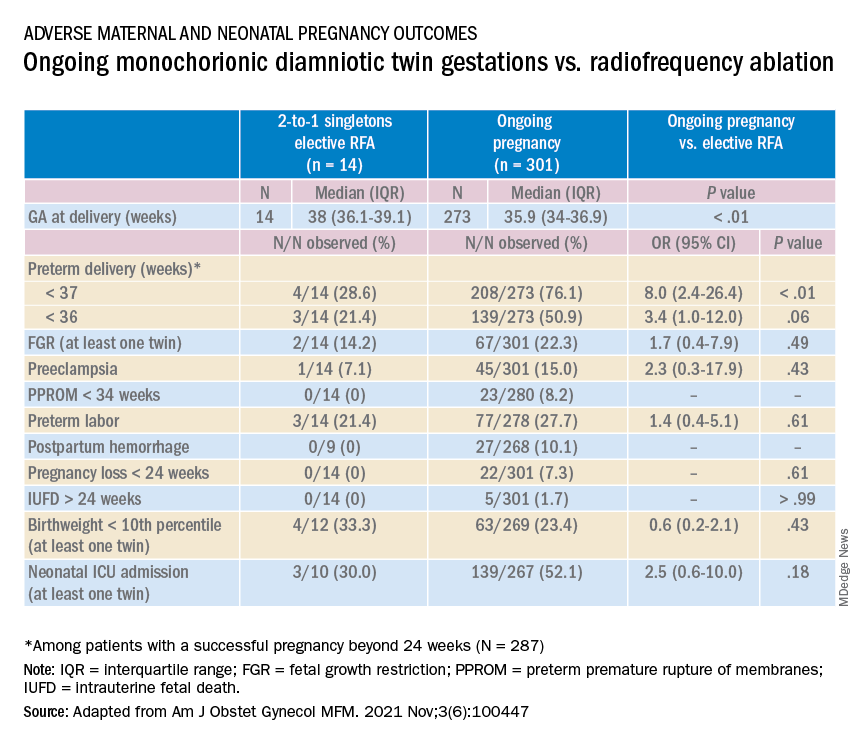
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.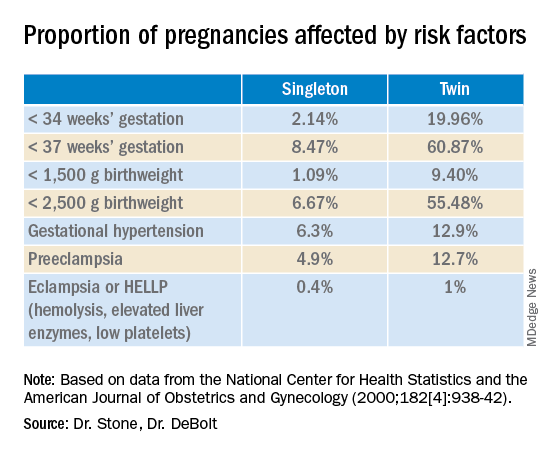
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.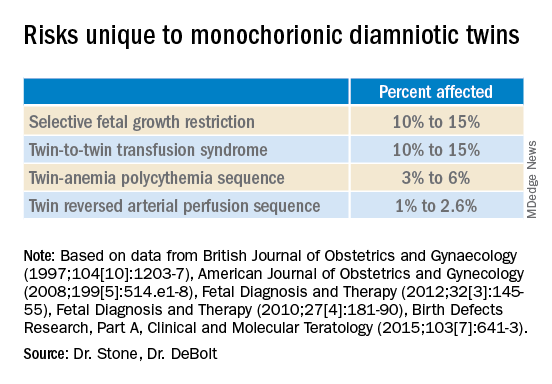
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Managing maternal mortality with multifetal pregnancy reduction
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.









