User login
Melatonin as a sleep aid: Are you prescribing it correctly?
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
Difficulty achieving regular restorative sleep is a common symptom of many psychiatric illnesses and can pose a pharmaceutical challenge, particularly for patients who have contraindications to benzodiazepines or sedative-hypnotics. Melatonin is commonly used to treat insomnia and circadian rhythm disorders in hospitalized patients because it is largely considered safe, nonhabit forming, unlikely to interact with other medications, and possibly protective against delirium.1 We support its short-term use in patients with sleep disruption, even if they do not meet the diagnostic criteria for insomnia or a circadian rhythm sleep-wake disorder. However, this use should be guided by consideration of the known physiological actions of melatonin, and not by an assumption that it acts as a simple sedative-hypnotic.
How melatonin works
Melatonin is an endogenous neurohormone involved in circadian rhythm regulation (sleep/wake regulation), a fundamental process in the functioning of the CNS and in the development of psychiatric disorders.2 Melatonin is commonly described as a sleep-promoting neurotransmitter, but it is more accurately described as a “darkness hormone.”3 With an onset at dusk and offset at sunrise, melatonin is the signal for biological night, not the signal for sleep. Melanopsin-containing retina neurons sensitive to blue light sense the diminishing light of the evening and communicate this cue to the brain’s master clock in the suprachiasmatic nucleus (SCN) of the hypothalamus (via the retinohypothalamic pathway). The SCN then releases its inhibition on the pineal gland, allowing it to release melatonin into the bloodstream and CSF. The timing of this release is known as the dim-light melatonin onset (DLMO).
Selecting the optimal timing and dose
Studies in laboratory and home settings have consistently shown that the DLMO precedes the onset of sleep by approximately 2 to 4 hours.4 Thus, we recommend scheduling melatonin administration for 2 to 4 hours before the intended bedtime.
Lower doses better replicate physiological levels of melatonin. A lower dose is also less likely to lead to a compromise of the entrainment process and the induction of a delayed sleep phase due to the lingering presence of melatonin, or the phase-delaying effects of a strong melatonin signal much later than the ideal DLMO. Giving higher doses at bedtime will induce sleep but may cause a circadian phase delay, effectively “jet lagging” the patient. We recommend prescribing low-dose melatonin (LDM; 0.5 to 1 mg) 2 to 4 hours before the intended bedtime rather than higher doses (≥5 mg) given at bedtime as is common practice and recommended by many melatonin manufacturers. LDM better simulates the natural release and function of melatonin and avoids potential adverse circadian phase delays. T
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
1. Joseph SG. Melatonin supplementation for the prevention of hospital-associated delirium. Ment Health Clin. 2018;7(4):143-146. doi:10.9740/mhc.2017.07.143
2. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39. doi:10.1016/j.smrv.2004.05.002
3. Tallavajhula S, Rodgers JJ, Slater JD. Sleep and sleep-wake disorders. In: Arciniengas DB, Yudofsky SC, Hales RE, eds. Textbook of Neuropsychiatry and Clinical Neurosciences. American Psychiatric Association Publishing; 2018:373-393.
4. Sletten TL, Vincenzi S, Redman JR, et al. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137. doi:10.3389/fneur.2010.00137
Proposal for a new diagnosis: Acute anxiety disorder
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Mr. F, age 42, says he has always been a very anxious person and has chronically found his worrying to negatively affect his life. He says that over the last month his anxiety has been “off the charts” and he is worrying “24/7” due to taking on new responsibilities at his job and his son being diagnosed with lupus. He says his constant worrying is significantly impairing his ability to focus at his job, and he is considering taking a mental health leave from work. His wife reports that she is extremely frustrated because Mr. F has been isolating himself from family and friends; he admits this is true and attributes it to being preoccupied by his worries.
Mr. F endorses chronic insomnia, muscle tension, and irritability associated with anxiety; these have all substantially worsened over the last month. He admits that recently he has occasionally thought it would be easier if he weren’t alive. Mr. F denies having problems with his energy or motivation levels and insists that he generally feels very anxious, but not depressed. He says he drinks 1 alcoholic drink per week and denies any other substance use. Mr. F is overweight and has slightly elevated cholesterol but denies any other health conditions. He takes melatonin to help him sleep but does not take any prescribed medications.
Although this vignette provides limited details, on the surface it appears that Mr. F is experiencing an exacerbation of chronic generalized anxiety disorder (GAD). However, in this article, I propose establishing a new diagnosis: “acute anxiety disorder,” which would encapsulate severe exacerbations of a pre-existing anxiety disorder. Among the patients I have encountered for whom this diagnosis would fit, most have pre-existing GAD or panic disorder.
A look at the differential diagnosis
It is important to determine whether Mr. F is using any substances or has a medical condition that could be contributing to his anxiety. Other psychiatric diagnoses that could be considered include:
Adjustment disorder. This diagnosis would make sense if Mr. F didn’t have an apparent chronic history of symptoms that meet criteria for GAD.
Major depressive disorder with anxious distress. Many patients experiencing a major depressive episode meet the criteria for the specifier “with anxious distress,” even those who do not have a comorbid anxiety disorder.1 However, it is not evident from this vignette that Mr. F is experiencing a major depressive episode.
Continue to: Panic disorder and GAD...
Panic disorder and GAD. It is possible for a patient with GAD to develop panic disorder, which, at times, occurs after experiencing significant life stressors. Panic disorder requires the presence of recurrent panic attacks. Mr. F describes experiencing chronic, intense symptoms of anxiety rather than the discreet episodes of acute symptoms that characterize panic attacks.
Acute stress disorder. This diagnosis involves psychological symptoms that occur in response to exposure to actual or threatened death, serious injury, or sexual violation. Mr. F was not exposed to any of these stressors.
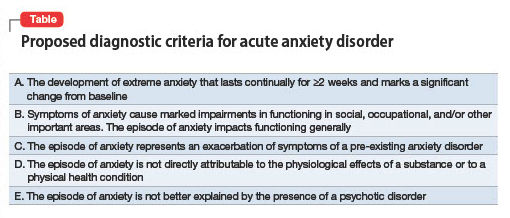
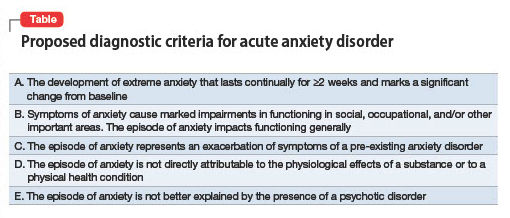
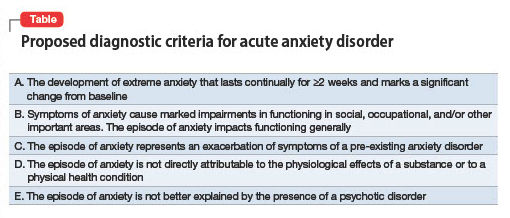
Why this new diagnosis would be helpful
A new diagnosis, acute anxiety disorder, would indicate that a patient is currently experiencing an acute exacerbation of a chronic anxiety disorder that is leading to a significant decrease in their baseline functioning. My proposed criteria for acute anxiety disorder appear in the Table. Here are some reasons this diagnosis would be helpful:
Signifier of severity. Anxiety disorders such as GAD are generally not considered severe conditions and not considered to fall under the rubric of SPMI (severe and persistent mental illness).2 Posttraumatic stress disorder is the anxiety disorder–like condition most often found in the SPMI category. A diagnosis of acute anxiety disorder would indicate a patient is experiencing an episode of anxiety that is distinct from their chronic anxiety condition due to its severe impact on functional capabilities. Acute anxiety disorder would certainly not qualify as a “SPMI diagnosis” that would facilitate someone being considered eligible for supplemental security income, but it might be a legitimate justification for someone to receive short-term disability.
Treatment approach. The pharmacologic treatment of anxiety disorders usually involves a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI). However, these medications can sometimes briefly increase anxiety when they are started. Individuals with acute anxiety are the most vulnerable to the possibility of experiencing increased anxiety when starting an SSRI or SNRI and may benefit from a slower titration of these medications. In light of this and the length of time required for SSRIs or SNRIs to exert a positive effect (typically a few weeks), patients with acute anxiety are best served by treatment with a medication with an immediate onset of action, such as a benzodiazepine or a sleep medication (eg, zolpidem). Benzodiazepines and hypnotics such as zolpidem are best prescribed for as-needed use because they carry a risk of dependence. One might consider prescribing mirtazapine or pregabalin (both of which are used off-label to treat anxiety) because these medications also have a relatively rapid onset of action and can treat both anxiety and insomnia (particularly mirtazapine).
Research considerations. It would be helpful to study which treatments are most effective for the subset of patients who experience acute anxiety disorder as I define it. Perhaps psychotherapy treatment protocols could be adapted or created. Treatment with esketamine or IV ketamine might be further studied as a treatment for acute anxiety because some evidence suggests ketamine is efficacious for this indication.3
1. Otsubo T, Hokama C, Sano N, et al. How significant is the assessment of the DSM-5 ‘anxious distress’ specifier in patients with major depressive disorder without comorbid anxiety disorders in the continuation/maintenance phase? Int J Psychiatry Clin Pract. 2021;25(4):385-392. doi:10.1080/13651501.2021.1907415
2. Butler H, O’Brien AJ. Access to specialist palliative care services by people with severe and persistent mental illness: a retrospective cohort study. Int J Ment Health Nurs. 2018;27(2):737-746. doi:10.1111/inm.12360
3. Glue P, Neehoff SM, Medlicott NJ, et al. Safety and efficacy of maintenance ketamine treatment in patients with treatment-refractory generalised anxiety and social anxiety disorders. J Psychopharmacol. 2018;32(6):663-667. doi:10.1177/0269881118762073
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Mr. F, age 42, says he has always been a very anxious person and has chronically found his worrying to negatively affect his life. He says that over the last month his anxiety has been “off the charts” and he is worrying “24/7” due to taking on new responsibilities at his job and his son being diagnosed with lupus. He says his constant worrying is significantly impairing his ability to focus at his job, and he is considering taking a mental health leave from work. His wife reports that she is extremely frustrated because Mr. F has been isolating himself from family and friends; he admits this is true and attributes it to being preoccupied by his worries.
Mr. F endorses chronic insomnia, muscle tension, and irritability associated with anxiety; these have all substantially worsened over the last month. He admits that recently he has occasionally thought it would be easier if he weren’t alive. Mr. F denies having problems with his energy or motivation levels and insists that he generally feels very anxious, but not depressed. He says he drinks 1 alcoholic drink per week and denies any other substance use. Mr. F is overweight and has slightly elevated cholesterol but denies any other health conditions. He takes melatonin to help him sleep but does not take any prescribed medications.
Although this vignette provides limited details, on the surface it appears that Mr. F is experiencing an exacerbation of chronic generalized anxiety disorder (GAD). However, in this article, I propose establishing a new diagnosis: “acute anxiety disorder,” which would encapsulate severe exacerbations of a pre-existing anxiety disorder. Among the patients I have encountered for whom this diagnosis would fit, most have pre-existing GAD or panic disorder.
A look at the differential diagnosis
It is important to determine whether Mr. F is using any substances or has a medical condition that could be contributing to his anxiety. Other psychiatric diagnoses that could be considered include:
Adjustment disorder. This diagnosis would make sense if Mr. F didn’t have an apparent chronic history of symptoms that meet criteria for GAD.
Major depressive disorder with anxious distress. Many patients experiencing a major depressive episode meet the criteria for the specifier “with anxious distress,” even those who do not have a comorbid anxiety disorder.1 However, it is not evident from this vignette that Mr. F is experiencing a major depressive episode.
Continue to: Panic disorder and GAD...
Panic disorder and GAD. It is possible for a patient with GAD to develop panic disorder, which, at times, occurs after experiencing significant life stressors. Panic disorder requires the presence of recurrent panic attacks. Mr. F describes experiencing chronic, intense symptoms of anxiety rather than the discreet episodes of acute symptoms that characterize panic attacks.
Acute stress disorder. This diagnosis involves psychological symptoms that occur in response to exposure to actual or threatened death, serious injury, or sexual violation. Mr. F was not exposed to any of these stressors.
Why this new diagnosis would be helpful
A new diagnosis, acute anxiety disorder, would indicate that a patient is currently experiencing an acute exacerbation of a chronic anxiety disorder that is leading to a significant decrease in their baseline functioning. My proposed criteria for acute anxiety disorder appear in the Table. Here are some reasons this diagnosis would be helpful:
Signifier of severity. Anxiety disorders such as GAD are generally not considered severe conditions and not considered to fall under the rubric of SPMI (severe and persistent mental illness).2 Posttraumatic stress disorder is the anxiety disorder–like condition most often found in the SPMI category. A diagnosis of acute anxiety disorder would indicate a patient is experiencing an episode of anxiety that is distinct from their chronic anxiety condition due to its severe impact on functional capabilities. Acute anxiety disorder would certainly not qualify as a “SPMI diagnosis” that would facilitate someone being considered eligible for supplemental security income, but it might be a legitimate justification for someone to receive short-term disability.
Treatment approach. The pharmacologic treatment of anxiety disorders usually involves a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI). However, these medications can sometimes briefly increase anxiety when they are started. Individuals with acute anxiety are the most vulnerable to the possibility of experiencing increased anxiety when starting an SSRI or SNRI and may benefit from a slower titration of these medications. In light of this and the length of time required for SSRIs or SNRIs to exert a positive effect (typically a few weeks), patients with acute anxiety are best served by treatment with a medication with an immediate onset of action, such as a benzodiazepine or a sleep medication (eg, zolpidem). Benzodiazepines and hypnotics such as zolpidem are best prescribed for as-needed use because they carry a risk of dependence. One might consider prescribing mirtazapine or pregabalin (both of which are used off-label to treat anxiety) because these medications also have a relatively rapid onset of action and can treat both anxiety and insomnia (particularly mirtazapine).
Research considerations. It would be helpful to study which treatments are most effective for the subset of patients who experience acute anxiety disorder as I define it. Perhaps psychotherapy treatment protocols could be adapted or created. Treatment with esketamine or IV ketamine might be further studied as a treatment for acute anxiety because some evidence suggests ketamine is efficacious for this indication.3
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Mr. F, age 42, says he has always been a very anxious person and has chronically found his worrying to negatively affect his life. He says that over the last month his anxiety has been “off the charts” and he is worrying “24/7” due to taking on new responsibilities at his job and his son being diagnosed with lupus. He says his constant worrying is significantly impairing his ability to focus at his job, and he is considering taking a mental health leave from work. His wife reports that she is extremely frustrated because Mr. F has been isolating himself from family and friends; he admits this is true and attributes it to being preoccupied by his worries.
Mr. F endorses chronic insomnia, muscle tension, and irritability associated with anxiety; these have all substantially worsened over the last month. He admits that recently he has occasionally thought it would be easier if he weren’t alive. Mr. F denies having problems with his energy or motivation levels and insists that he generally feels very anxious, but not depressed. He says he drinks 1 alcoholic drink per week and denies any other substance use. Mr. F is overweight and has slightly elevated cholesterol but denies any other health conditions. He takes melatonin to help him sleep but does not take any prescribed medications.
Although this vignette provides limited details, on the surface it appears that Mr. F is experiencing an exacerbation of chronic generalized anxiety disorder (GAD). However, in this article, I propose establishing a new diagnosis: “acute anxiety disorder,” which would encapsulate severe exacerbations of a pre-existing anxiety disorder. Among the patients I have encountered for whom this diagnosis would fit, most have pre-existing GAD or panic disorder.
A look at the differential diagnosis
It is important to determine whether Mr. F is using any substances or has a medical condition that could be contributing to his anxiety. Other psychiatric diagnoses that could be considered include:
Adjustment disorder. This diagnosis would make sense if Mr. F didn’t have an apparent chronic history of symptoms that meet criteria for GAD.
Major depressive disorder with anxious distress. Many patients experiencing a major depressive episode meet the criteria for the specifier “with anxious distress,” even those who do not have a comorbid anxiety disorder.1 However, it is not evident from this vignette that Mr. F is experiencing a major depressive episode.
Continue to: Panic disorder and GAD...
Panic disorder and GAD. It is possible for a patient with GAD to develop panic disorder, which, at times, occurs after experiencing significant life stressors. Panic disorder requires the presence of recurrent panic attacks. Mr. F describes experiencing chronic, intense symptoms of anxiety rather than the discreet episodes of acute symptoms that characterize panic attacks.
Acute stress disorder. This diagnosis involves psychological symptoms that occur in response to exposure to actual or threatened death, serious injury, or sexual violation. Mr. F was not exposed to any of these stressors.
Why this new diagnosis would be helpful
A new diagnosis, acute anxiety disorder, would indicate that a patient is currently experiencing an acute exacerbation of a chronic anxiety disorder that is leading to a significant decrease in their baseline functioning. My proposed criteria for acute anxiety disorder appear in the Table. Here are some reasons this diagnosis would be helpful:
Signifier of severity. Anxiety disorders such as GAD are generally not considered severe conditions and not considered to fall under the rubric of SPMI (severe and persistent mental illness).2 Posttraumatic stress disorder is the anxiety disorder–like condition most often found in the SPMI category. A diagnosis of acute anxiety disorder would indicate a patient is experiencing an episode of anxiety that is distinct from their chronic anxiety condition due to its severe impact on functional capabilities. Acute anxiety disorder would certainly not qualify as a “SPMI diagnosis” that would facilitate someone being considered eligible for supplemental security income, but it might be a legitimate justification for someone to receive short-term disability.
Treatment approach. The pharmacologic treatment of anxiety disorders usually involves a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI). However, these medications can sometimes briefly increase anxiety when they are started. Individuals with acute anxiety are the most vulnerable to the possibility of experiencing increased anxiety when starting an SSRI or SNRI and may benefit from a slower titration of these medications. In light of this and the length of time required for SSRIs or SNRIs to exert a positive effect (typically a few weeks), patients with acute anxiety are best served by treatment with a medication with an immediate onset of action, such as a benzodiazepine or a sleep medication (eg, zolpidem). Benzodiazepines and hypnotics such as zolpidem are best prescribed for as-needed use because they carry a risk of dependence. One might consider prescribing mirtazapine or pregabalin (both of which are used off-label to treat anxiety) because these medications also have a relatively rapid onset of action and can treat both anxiety and insomnia (particularly mirtazapine).
Research considerations. It would be helpful to study which treatments are most effective for the subset of patients who experience acute anxiety disorder as I define it. Perhaps psychotherapy treatment protocols could be adapted or created. Treatment with esketamine or IV ketamine might be further studied as a treatment for acute anxiety because some evidence suggests ketamine is efficacious for this indication.3
1. Otsubo T, Hokama C, Sano N, et al. How significant is the assessment of the DSM-5 ‘anxious distress’ specifier in patients with major depressive disorder without comorbid anxiety disorders in the continuation/maintenance phase? Int J Psychiatry Clin Pract. 2021;25(4):385-392. doi:10.1080/13651501.2021.1907415
2. Butler H, O’Brien AJ. Access to specialist palliative care services by people with severe and persistent mental illness: a retrospective cohort study. Int J Ment Health Nurs. 2018;27(2):737-746. doi:10.1111/inm.12360
3. Glue P, Neehoff SM, Medlicott NJ, et al. Safety and efficacy of maintenance ketamine treatment in patients with treatment-refractory generalised anxiety and social anxiety disorders. J Psychopharmacol. 2018;32(6):663-667. doi:10.1177/0269881118762073
1. Otsubo T, Hokama C, Sano N, et al. How significant is the assessment of the DSM-5 ‘anxious distress’ specifier in patients with major depressive disorder without comorbid anxiety disorders in the continuation/maintenance phase? Int J Psychiatry Clin Pract. 2021;25(4):385-392. doi:10.1080/13651501.2021.1907415
2. Butler H, O’Brien AJ. Access to specialist palliative care services by people with severe and persistent mental illness: a retrospective cohort study. Int J Ment Health Nurs. 2018;27(2):737-746. doi:10.1111/inm.12360
3. Glue P, Neehoff SM, Medlicott NJ, et al. Safety and efficacy of maintenance ketamine treatment in patients with treatment-refractory generalised anxiety and social anxiety disorders. J Psychopharmacol. 2018;32(6):663-667. doi:10.1177/0269881118762073
Neurosurgical treatment of OCD: Patient selection, safety, and access
Obsessive-compulsive disorder (OCD) is typically a severe, chronic illness in which patients have recurrent, unwanted thoughts, urges, and compulsions.1 It causes significant morbidity and lost potential over time, and is the world’s 10th-most disabling disorder in terms of lost income and decreased quality of life, and the fifth-most disabling mental health condition.2 Patients with OCD (and their clinicians) are often desperate for an efficacious treatment, but we must ensure that those who are not helped by traditional psychotherapeutic and/or pharmacologic treatments are appropriate for safe neurosurgical intervention.
Pros and cons of neurosurgical therapies
Most patients with OCD are effectively treated with cognitive-behavioral therapy and pharmacotherapy in the form of selective serotonin reuptake inhibitors, clomipramine, or second-generation antipsychotics. However, up to 5% of individuals with OCD will have symptoms refractory to these traditional therapies.3 These cases require more aggressive forms of therapy, including radiofrequency ablation surgeries and deep brain stimulation (DBS). The efficacy of both therapies is similar at 40% to 60%.4,5 While these treatments can be life-changing for patients fortunate to receive them, they are not without issue.
Only a limited number of institutions offer these neurosurgical techniques, and for many patients, those locations may be inaccessible. Patients may not experience relief simply due to where they live, difficult logistics, and the high cost requisite to receive care. If fortunate enough to live near a participating institution or have the means to travel to one, the patient and clinician must then choose the best option based on the nuances of the patient’s situation.
Ablation techniques, such as gamma knife or magnetic resonance–guided ultrasound, are simpler and more cost-effective. A drawback of this approach, however, is that it is irreversible. Lesioned structures are irreparable, as are the adverse effects of the surgery, which, while rare, may include a persistent minimally conscious state or necrotic cysts.4 A benefit of this approach is that there is no need for lengthy follow-up as seen with DBS.
DBS is more complicated. In addition to having to undergo an open neurosurgical procedure, these patients require long-term follow-up and monitoring. A positive aspect is the device can be turned off or removed. However, the amount of follow-up and adjustments is significant. These patients need access to clinicians skilled in DBS device management.
Finally, we must consider the chronically ill patient’s perspective after successful treatment. While the patient’s symptoms may improve, their lives and identities likely developed around their symptoms. Bosanac et al6 describe this reality well in a case study in which a patient with OCD was “burdened with normality” after successful DBS treatment. He was finally able to work, build meaningful relationships, and approach previously unattainable social milestones. This was an overwhelming experience for him, and he and his family needed guidance into the world in which most of us find comfort.
As ablation techniques, DBS, and other cutting-edge therapies for OCD come to the forefront of modern care, clinicians must remember to keep patient safety first. Verify follow-up care before committing patients to invasive and irreversible treatments. While general access is currently poor, participating institutions should consider advertising and communicating that there is an accessible network available for these chronically ill individuals.
1. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
2. World Health Organization. The Global Burden of Disease: 2004 Update. World Health Organization; 2008.
3. Jenike MA, Rauch SL. Managing the patient with treatment-resistant obsessive compulsive disorder: current strategies. J Clin Psychiatry. 1994;55 Suppl:11-17.
4. Rasmussen SA, Noren G, Greenberg BD, et al. Gamma ventral capsulotomy in intractable obsessive-compulsive disorder. Biol Psychiatry. 2018;84(5):355-364.
5. Kumar KK, Appelboom, G, Lamsam L, et al. Comparative effectiveness of neuroablation and deep brain stimulation for treatment-resistant obsessive-compulsive disorder: a meta-analytic study. J Neurol Neurosurg Psychiatry. 2019;90(4):469-473.
6. Bosanac P, Hamilton BE, Lucak J, et al. Identity challenges and ‘burden of normality’ after DBS for severe OCD: a narrative case study. BMC Psychiatry. 2018;18(1):186.
Obsessive-compulsive disorder (OCD) is typically a severe, chronic illness in which patients have recurrent, unwanted thoughts, urges, and compulsions.1 It causes significant morbidity and lost potential over time, and is the world’s 10th-most disabling disorder in terms of lost income and decreased quality of life, and the fifth-most disabling mental health condition.2 Patients with OCD (and their clinicians) are often desperate for an efficacious treatment, but we must ensure that those who are not helped by traditional psychotherapeutic and/or pharmacologic treatments are appropriate for safe neurosurgical intervention.
Pros and cons of neurosurgical therapies
Most patients with OCD are effectively treated with cognitive-behavioral therapy and pharmacotherapy in the form of selective serotonin reuptake inhibitors, clomipramine, or second-generation antipsychotics. However, up to 5% of individuals with OCD will have symptoms refractory to these traditional therapies.3 These cases require more aggressive forms of therapy, including radiofrequency ablation surgeries and deep brain stimulation (DBS). The efficacy of both therapies is similar at 40% to 60%.4,5 While these treatments can be life-changing for patients fortunate to receive them, they are not without issue.
Only a limited number of institutions offer these neurosurgical techniques, and for many patients, those locations may be inaccessible. Patients may not experience relief simply due to where they live, difficult logistics, and the high cost requisite to receive care. If fortunate enough to live near a participating institution or have the means to travel to one, the patient and clinician must then choose the best option based on the nuances of the patient’s situation.
Ablation techniques, such as gamma knife or magnetic resonance–guided ultrasound, are simpler and more cost-effective. A drawback of this approach, however, is that it is irreversible. Lesioned structures are irreparable, as are the adverse effects of the surgery, which, while rare, may include a persistent minimally conscious state or necrotic cysts.4 A benefit of this approach is that there is no need for lengthy follow-up as seen with DBS.
DBS is more complicated. In addition to having to undergo an open neurosurgical procedure, these patients require long-term follow-up and monitoring. A positive aspect is the device can be turned off or removed. However, the amount of follow-up and adjustments is significant. These patients need access to clinicians skilled in DBS device management.
Finally, we must consider the chronically ill patient’s perspective after successful treatment. While the patient’s symptoms may improve, their lives and identities likely developed around their symptoms. Bosanac et al6 describe this reality well in a case study in which a patient with OCD was “burdened with normality” after successful DBS treatment. He was finally able to work, build meaningful relationships, and approach previously unattainable social milestones. This was an overwhelming experience for him, and he and his family needed guidance into the world in which most of us find comfort.
As ablation techniques, DBS, and other cutting-edge therapies for OCD come to the forefront of modern care, clinicians must remember to keep patient safety first. Verify follow-up care before committing patients to invasive and irreversible treatments. While general access is currently poor, participating institutions should consider advertising and communicating that there is an accessible network available for these chronically ill individuals.
Obsessive-compulsive disorder (OCD) is typically a severe, chronic illness in which patients have recurrent, unwanted thoughts, urges, and compulsions.1 It causes significant morbidity and lost potential over time, and is the world’s 10th-most disabling disorder in terms of lost income and decreased quality of life, and the fifth-most disabling mental health condition.2 Patients with OCD (and their clinicians) are often desperate for an efficacious treatment, but we must ensure that those who are not helped by traditional psychotherapeutic and/or pharmacologic treatments are appropriate for safe neurosurgical intervention.
Pros and cons of neurosurgical therapies
Most patients with OCD are effectively treated with cognitive-behavioral therapy and pharmacotherapy in the form of selective serotonin reuptake inhibitors, clomipramine, or second-generation antipsychotics. However, up to 5% of individuals with OCD will have symptoms refractory to these traditional therapies.3 These cases require more aggressive forms of therapy, including radiofrequency ablation surgeries and deep brain stimulation (DBS). The efficacy of both therapies is similar at 40% to 60%.4,5 While these treatments can be life-changing for patients fortunate to receive them, they are not without issue.
Only a limited number of institutions offer these neurosurgical techniques, and for many patients, those locations may be inaccessible. Patients may not experience relief simply due to where they live, difficult logistics, and the high cost requisite to receive care. If fortunate enough to live near a participating institution or have the means to travel to one, the patient and clinician must then choose the best option based on the nuances of the patient’s situation.
Ablation techniques, such as gamma knife or magnetic resonance–guided ultrasound, are simpler and more cost-effective. A drawback of this approach, however, is that it is irreversible. Lesioned structures are irreparable, as are the adverse effects of the surgery, which, while rare, may include a persistent minimally conscious state or necrotic cysts.4 A benefit of this approach is that there is no need for lengthy follow-up as seen with DBS.
DBS is more complicated. In addition to having to undergo an open neurosurgical procedure, these patients require long-term follow-up and monitoring. A positive aspect is the device can be turned off or removed. However, the amount of follow-up and adjustments is significant. These patients need access to clinicians skilled in DBS device management.
Finally, we must consider the chronically ill patient’s perspective after successful treatment. While the patient’s symptoms may improve, their lives and identities likely developed around their symptoms. Bosanac et al6 describe this reality well in a case study in which a patient with OCD was “burdened with normality” after successful DBS treatment. He was finally able to work, build meaningful relationships, and approach previously unattainable social milestones. This was an overwhelming experience for him, and he and his family needed guidance into the world in which most of us find comfort.
As ablation techniques, DBS, and other cutting-edge therapies for OCD come to the forefront of modern care, clinicians must remember to keep patient safety first. Verify follow-up care before committing patients to invasive and irreversible treatments. While general access is currently poor, participating institutions should consider advertising and communicating that there is an accessible network available for these chronically ill individuals.
1. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
2. World Health Organization. The Global Burden of Disease: 2004 Update. World Health Organization; 2008.
3. Jenike MA, Rauch SL. Managing the patient with treatment-resistant obsessive compulsive disorder: current strategies. J Clin Psychiatry. 1994;55 Suppl:11-17.
4. Rasmussen SA, Noren G, Greenberg BD, et al. Gamma ventral capsulotomy in intractable obsessive-compulsive disorder. Biol Psychiatry. 2018;84(5):355-364.
5. Kumar KK, Appelboom, G, Lamsam L, et al. Comparative effectiveness of neuroablation and deep brain stimulation for treatment-resistant obsessive-compulsive disorder: a meta-analytic study. J Neurol Neurosurg Psychiatry. 2019;90(4):469-473.
6. Bosanac P, Hamilton BE, Lucak J, et al. Identity challenges and ‘burden of normality’ after DBS for severe OCD: a narrative case study. BMC Psychiatry. 2018;18(1):186.
1. Ruscio AM, Stein DJ, Chiu WT, et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53-63.
2. World Health Organization. The Global Burden of Disease: 2004 Update. World Health Organization; 2008.
3. Jenike MA, Rauch SL. Managing the patient with treatment-resistant obsessive compulsive disorder: current strategies. J Clin Psychiatry. 1994;55 Suppl:11-17.
4. Rasmussen SA, Noren G, Greenberg BD, et al. Gamma ventral capsulotomy in intractable obsessive-compulsive disorder. Biol Psychiatry. 2018;84(5):355-364.
5. Kumar KK, Appelboom, G, Lamsam L, et al. Comparative effectiveness of neuroablation and deep brain stimulation for treatment-resistant obsessive-compulsive disorder: a meta-analytic study. J Neurol Neurosurg Psychiatry. 2019;90(4):469-473.
6. Bosanac P, Hamilton BE, Lucak J, et al. Identity challenges and ‘burden of normality’ after DBS for severe OCD: a narrative case study. BMC Psychiatry. 2018;18(1):186.
Commentary: IL-Targeted Therapies and Nail Dystrophy in PsA, September 2022
Recent publications on psoriatic arthritis (PsA) have focused on targeted therapies, particularly those targeting interleukin (IL) 17 and 23. Bimekizumab is a novel biologic that dually inhibits IL-17A and IL-17F. Coates and colleagues reported 3-year results from the phase 2b BE ACTIVE trial that included 206 adults with active PsA randomly assigned to receive bimekizumab or placebo for 48 weeks, of which 184 patients were enrolled in the open-label extension phase for a further 104 weeks of treatment. They report that at least 20% improvement in American College of Rheumatology score was maintained by 64.1% of patients at week 152 compared with 72.3% of patients at week 48. By week 152, 89.3% of patients had reported one or more treatment-emergent adverse event (TEAE), with serious TEAE being reported by 10.7% of patients. Fungal infections are of special interest when inhibiting both IL-17A and IL-17F. It was observed that 9.7% had fungal infections (all mild-to-moderate and localized), of which 4.6% had candidiasis. Thus, bimekizumab shows promise as a new therapy for PsA.
In addition to improving signs and symptoms, clinically meaningful improvement in health-related quality of life is an important goal of treatment. Two studies reported improvement in patient reported outcomes on treatment with IL-23 inhibitors.
An analysis of data from the phase 3 DISCOVER 2 trial included 738 biologic-naive patients with active PsA and inadequate response to standard treatments. These patients were randomly assigned to receive 100 mg guselkumab every 4 weeks (Q4W) or every 8 weeks (Q8W) or placebo. Curtis and colleagues showed that a significantly higher proportion of patients receiving guselkumab Q4W/Q8W vs placebo reported achieving minimally important differences (MID) in the EuroQol 5-Dimension 5-Level (EQ-5D-5L) Index (56.0%/56.0% vs 43.4%; P < .006) and Visual Analog Scale (EQ-VAS) score (62.8%/63.5% vs 44.4%; P < .0001) at week 24, with more than 60% of patients reporting improvements at week 52.
Similarly, analyses of data by Kristensen and colleagues from two phase 3 trials, KEEPsAKE-1 and KEEPsAKE-2, included adults with PsA and inadequate response/intolerance to disease-modifying antirheumatic drugs or biologics. The patients were randomly assigned to receive risankizumab or placebo for 24 weeks and only risankizumab during weeks 24-52. At week 24, patients receiving risankizumab vs placebo were significantly more likely to report achieving MID in Patient's Global Assessment of Disease Activity (PtGA) in both KEEPsAKE-1 (odds ratio [OR] 2.0; P < .001) and KEEPsAKE-2 (OR 1.9; P < .01) studies, with further improvement at week 52. Improvement was also seen on the Patient's Assessment of Pain, Health Assessment Questionnaire – Disability Index, Short-Form 36 Physical and Mental Component Summary scores, EQ-5D-5L, Functional Assessment of Chronic Illness Therapy – Fatigue, and Work Productivity and Activity Impairment.
An interesting insight from two studies showed the importance of nail disease in predicting treatment response. A post hoc analysis by Helliwell and colleagues of the phase 3 SEAM-PsA trial of 851 biologic/methotrexate-naive patients with active PsA who were randomly assigned to receive methotrexate monotherapy, etanercept monotherapy, or methotrexate + etanercept combination therapy showed that the presence of both dactylitis and nail disease at baseline were significantly associated with the achievement of minimal disease activity (OR 1.4; P = .0457; and OR 1.8; P = .0233, respectively), as well as low PsA Disease Activity Score (OR 1.8; P = .0014; and OR 1.8; P = .0168, respectively).
Similarly, a post hoc analysis by Baraliakos and colleagues of the phase 3b MAXIMISE trial of 473 adult patients with PsA and axial manifestations who were randomly assigned to receive secukinumab (150 or 300 mg) or placebo showed that the presence vs the absence of nail dystrophy was associated with the achievement of significantly better Assessment of SpondyloArthritis International Society 20 response in the 300 mg secukinumab group (OR 5.0; 95% CI 1.47-17.19).
Recent publications on psoriatic arthritis (PsA) have focused on targeted therapies, particularly those targeting interleukin (IL) 17 and 23. Bimekizumab is a novel biologic that dually inhibits IL-17A and IL-17F. Coates and colleagues reported 3-year results from the phase 2b BE ACTIVE trial that included 206 adults with active PsA randomly assigned to receive bimekizumab or placebo for 48 weeks, of which 184 patients were enrolled in the open-label extension phase for a further 104 weeks of treatment. They report that at least 20% improvement in American College of Rheumatology score was maintained by 64.1% of patients at week 152 compared with 72.3% of patients at week 48. By week 152, 89.3% of patients had reported one or more treatment-emergent adverse event (TEAE), with serious TEAE being reported by 10.7% of patients. Fungal infections are of special interest when inhibiting both IL-17A and IL-17F. It was observed that 9.7% had fungal infections (all mild-to-moderate and localized), of which 4.6% had candidiasis. Thus, bimekizumab shows promise as a new therapy for PsA.
In addition to improving signs and symptoms, clinically meaningful improvement in health-related quality of life is an important goal of treatment. Two studies reported improvement in patient reported outcomes on treatment with IL-23 inhibitors.
An analysis of data from the phase 3 DISCOVER 2 trial included 738 biologic-naive patients with active PsA and inadequate response to standard treatments. These patients were randomly assigned to receive 100 mg guselkumab every 4 weeks (Q4W) or every 8 weeks (Q8W) or placebo. Curtis and colleagues showed that a significantly higher proportion of patients receiving guselkumab Q4W/Q8W vs placebo reported achieving minimally important differences (MID) in the EuroQol 5-Dimension 5-Level (EQ-5D-5L) Index (56.0%/56.0% vs 43.4%; P < .006) and Visual Analog Scale (EQ-VAS) score (62.8%/63.5% vs 44.4%; P < .0001) at week 24, with more than 60% of patients reporting improvements at week 52.
Similarly, analyses of data by Kristensen and colleagues from two phase 3 trials, KEEPsAKE-1 and KEEPsAKE-2, included adults with PsA and inadequate response/intolerance to disease-modifying antirheumatic drugs or biologics. The patients were randomly assigned to receive risankizumab or placebo for 24 weeks and only risankizumab during weeks 24-52. At week 24, patients receiving risankizumab vs placebo were significantly more likely to report achieving MID in Patient's Global Assessment of Disease Activity (PtGA) in both KEEPsAKE-1 (odds ratio [OR] 2.0; P < .001) and KEEPsAKE-2 (OR 1.9; P < .01) studies, with further improvement at week 52. Improvement was also seen on the Patient's Assessment of Pain, Health Assessment Questionnaire – Disability Index, Short-Form 36 Physical and Mental Component Summary scores, EQ-5D-5L, Functional Assessment of Chronic Illness Therapy – Fatigue, and Work Productivity and Activity Impairment.
An interesting insight from two studies showed the importance of nail disease in predicting treatment response. A post hoc analysis by Helliwell and colleagues of the phase 3 SEAM-PsA trial of 851 biologic/methotrexate-naive patients with active PsA who were randomly assigned to receive methotrexate monotherapy, etanercept monotherapy, or methotrexate + etanercept combination therapy showed that the presence of both dactylitis and nail disease at baseline were significantly associated with the achievement of minimal disease activity (OR 1.4; P = .0457; and OR 1.8; P = .0233, respectively), as well as low PsA Disease Activity Score (OR 1.8; P = .0014; and OR 1.8; P = .0168, respectively).
Similarly, a post hoc analysis by Baraliakos and colleagues of the phase 3b MAXIMISE trial of 473 adult patients with PsA and axial manifestations who were randomly assigned to receive secukinumab (150 or 300 mg) or placebo showed that the presence vs the absence of nail dystrophy was associated with the achievement of significantly better Assessment of SpondyloArthritis International Society 20 response in the 300 mg secukinumab group (OR 5.0; 95% CI 1.47-17.19).
Recent publications on psoriatic arthritis (PsA) have focused on targeted therapies, particularly those targeting interleukin (IL) 17 and 23. Bimekizumab is a novel biologic that dually inhibits IL-17A and IL-17F. Coates and colleagues reported 3-year results from the phase 2b BE ACTIVE trial that included 206 adults with active PsA randomly assigned to receive bimekizumab or placebo for 48 weeks, of which 184 patients were enrolled in the open-label extension phase for a further 104 weeks of treatment. They report that at least 20% improvement in American College of Rheumatology score was maintained by 64.1% of patients at week 152 compared with 72.3% of patients at week 48. By week 152, 89.3% of patients had reported one or more treatment-emergent adverse event (TEAE), with serious TEAE being reported by 10.7% of patients. Fungal infections are of special interest when inhibiting both IL-17A and IL-17F. It was observed that 9.7% had fungal infections (all mild-to-moderate and localized), of which 4.6% had candidiasis. Thus, bimekizumab shows promise as a new therapy for PsA.
In addition to improving signs and symptoms, clinically meaningful improvement in health-related quality of life is an important goal of treatment. Two studies reported improvement in patient reported outcomes on treatment with IL-23 inhibitors.
An analysis of data from the phase 3 DISCOVER 2 trial included 738 biologic-naive patients with active PsA and inadequate response to standard treatments. These patients were randomly assigned to receive 100 mg guselkumab every 4 weeks (Q4W) or every 8 weeks (Q8W) or placebo. Curtis and colleagues showed that a significantly higher proportion of patients receiving guselkumab Q4W/Q8W vs placebo reported achieving minimally important differences (MID) in the EuroQol 5-Dimension 5-Level (EQ-5D-5L) Index (56.0%/56.0% vs 43.4%; P < .006) and Visual Analog Scale (EQ-VAS) score (62.8%/63.5% vs 44.4%; P < .0001) at week 24, with more than 60% of patients reporting improvements at week 52.
Similarly, analyses of data by Kristensen and colleagues from two phase 3 trials, KEEPsAKE-1 and KEEPsAKE-2, included adults with PsA and inadequate response/intolerance to disease-modifying antirheumatic drugs or biologics. The patients were randomly assigned to receive risankizumab or placebo for 24 weeks and only risankizumab during weeks 24-52. At week 24, patients receiving risankizumab vs placebo were significantly more likely to report achieving MID in Patient's Global Assessment of Disease Activity (PtGA) in both KEEPsAKE-1 (odds ratio [OR] 2.0; P < .001) and KEEPsAKE-2 (OR 1.9; P < .01) studies, with further improvement at week 52. Improvement was also seen on the Patient's Assessment of Pain, Health Assessment Questionnaire – Disability Index, Short-Form 36 Physical and Mental Component Summary scores, EQ-5D-5L, Functional Assessment of Chronic Illness Therapy – Fatigue, and Work Productivity and Activity Impairment.
An interesting insight from two studies showed the importance of nail disease in predicting treatment response. A post hoc analysis by Helliwell and colleagues of the phase 3 SEAM-PsA trial of 851 biologic/methotrexate-naive patients with active PsA who were randomly assigned to receive methotrexate monotherapy, etanercept monotherapy, or methotrexate + etanercept combination therapy showed that the presence of both dactylitis and nail disease at baseline were significantly associated with the achievement of minimal disease activity (OR 1.4; P = .0457; and OR 1.8; P = .0233, respectively), as well as low PsA Disease Activity Score (OR 1.8; P = .0014; and OR 1.8; P = .0168, respectively).
Similarly, a post hoc analysis by Baraliakos and colleagues of the phase 3b MAXIMISE trial of 473 adult patients with PsA and axial manifestations who were randomly assigned to receive secukinumab (150 or 300 mg) or placebo showed that the presence vs the absence of nail dystrophy was associated with the achievement of significantly better Assessment of SpondyloArthritis International Society 20 response in the 300 mg secukinumab group (OR 5.0; 95% CI 1.47-17.19).
Commentary: Early Intervention and Pregnancy Concerns in RA, September 2022
The potential to prevent clinical rheumatoid arthritis (RA) in patients at risk of developing arthritis is of long-standing interest in the rheumatology community. Other studies have addressed the potential for early treatment with glucocorticoids, hydroxychloroquine, or biologics to prevent arthritis, with mixed results. Few published studies have assessed the efficacy of methotrexate in the prevention of arthritis. A randomized controlled trial by Krijbolder and colleagues of adults with arthralgias deemed to be at risk for progression to RA evaluated the use of a single intramuscular steroid injection combined with 1 year of oral methotrexate, compared with placebo, for preventing the development of RA according to the 2010 American College of Rheumatology classification criteria. Although no difference was seen between the groups in development of RA, those treated with methotrexate did have lower levels of joint inflammation seen on MRI and better functional status as per Health Assessment Questionnaire score.
Su and colleagues also looked at the impact of different medications on the development of RA. Using a national health insurance database in Taiwan (between 1997 and 2013), they studied the use of biguanides and sulfonylureas in patients with diabetes and the risk for incident RA. In over 90,000 patients with diabetes, a longer duration of sulfonylurea or biguanide prescription within the first 3 years of diabetes diagnosis was associated with a lower risk for RA compared with non-use. However, use of any antihyperglycemic agents was also associated with lower risk for RA incidence. Limited information is available on both the severity of diabetes and activity of RA, so even a potential mechanism in terms of reduction of blood glucose or inflammation is hard to determine, and more detailed studies are needed.
The safety of different treatments during pregnancy, as well as the effect of both RA and its treatment on pregnancy outcomes, have been areas of research interest in terms of counseling patients with RA about pregnancy planning and management of medications. Gerardi and colleagues followed 63 patients with RA prospectively during pregnancy. They found that although the general understanding is that inflammatory arthritis improves during pregnancy, the percentage of patients with moderate and high disease activity increased slightly, and 37% of patients experienced a flare. Flares were associated with elevated C-reactive protein (CRP) levels and use of multiple prior biologic disease-modifying antirheumatic drugs (bDMARD) (suggesting overall more active arthritis), as well as bDMARD discontinuation in early pregnancy. Similarly, preterm delivery was associated with elevated CRP, higher Disease Activity Score-28 scores, and flares. The study findings provide further support for the importance of controlling maternal disease activity in favoring a better RA course as well as better pregnancy outcomes.
Smeele and colleagues recently published an analysis of the PreCARA cohort study looking at birthweight in pregnant patients with RA. RA is associated with children being born small for gestational age. In this cohort study of 188 pregnant patients with RA, the treatment protocol before pregnancy included hydroxychloroquine, sulfasalazine, prednisone, and anti–tumor necrosis factor (TNF) agents (adalimumab, infliximab, etanercept, and certolizumab). Anti-TNF medications were stopped at 20, 20, 28, or 38 weeks, respectively, according to the European Alliance of Associations for Rheumatology (EULAR) recommendations. In terms of gestational age at delivery and congenital malformations, no difference was seen between patients who used anti-TNF agents during pregnancy and those who did not. Anti-TNF use during pregnancy was associated, however, with increased birthweight and a lower percentage of infants who were small for gestational age. These findings are in keeping with those of prior studies, although larger studies would be helpful in determining whether there are critical periods during pregnancy that have a significant effect on birthweight or whether overall control of inflammation is the predominant factor.
The potential to prevent clinical rheumatoid arthritis (RA) in patients at risk of developing arthritis is of long-standing interest in the rheumatology community. Other studies have addressed the potential for early treatment with glucocorticoids, hydroxychloroquine, or biologics to prevent arthritis, with mixed results. Few published studies have assessed the efficacy of methotrexate in the prevention of arthritis. A randomized controlled trial by Krijbolder and colleagues of adults with arthralgias deemed to be at risk for progression to RA evaluated the use of a single intramuscular steroid injection combined with 1 year of oral methotrexate, compared with placebo, for preventing the development of RA according to the 2010 American College of Rheumatology classification criteria. Although no difference was seen between the groups in development of RA, those treated with methotrexate did have lower levels of joint inflammation seen on MRI and better functional status as per Health Assessment Questionnaire score.
Su and colleagues also looked at the impact of different medications on the development of RA. Using a national health insurance database in Taiwan (between 1997 and 2013), they studied the use of biguanides and sulfonylureas in patients with diabetes and the risk for incident RA. In over 90,000 patients with diabetes, a longer duration of sulfonylurea or biguanide prescription within the first 3 years of diabetes diagnosis was associated with a lower risk for RA compared with non-use. However, use of any antihyperglycemic agents was also associated with lower risk for RA incidence. Limited information is available on both the severity of diabetes and activity of RA, so even a potential mechanism in terms of reduction of blood glucose or inflammation is hard to determine, and more detailed studies are needed.
The safety of different treatments during pregnancy, as well as the effect of both RA and its treatment on pregnancy outcomes, have been areas of research interest in terms of counseling patients with RA about pregnancy planning and management of medications. Gerardi and colleagues followed 63 patients with RA prospectively during pregnancy. They found that although the general understanding is that inflammatory arthritis improves during pregnancy, the percentage of patients with moderate and high disease activity increased slightly, and 37% of patients experienced a flare. Flares were associated with elevated C-reactive protein (CRP) levels and use of multiple prior biologic disease-modifying antirheumatic drugs (bDMARD) (suggesting overall more active arthritis), as well as bDMARD discontinuation in early pregnancy. Similarly, preterm delivery was associated with elevated CRP, higher Disease Activity Score-28 scores, and flares. The study findings provide further support for the importance of controlling maternal disease activity in favoring a better RA course as well as better pregnancy outcomes.
Smeele and colleagues recently published an analysis of the PreCARA cohort study looking at birthweight in pregnant patients with RA. RA is associated with children being born small for gestational age. In this cohort study of 188 pregnant patients with RA, the treatment protocol before pregnancy included hydroxychloroquine, sulfasalazine, prednisone, and anti–tumor necrosis factor (TNF) agents (adalimumab, infliximab, etanercept, and certolizumab). Anti-TNF medications were stopped at 20, 20, 28, or 38 weeks, respectively, according to the European Alliance of Associations for Rheumatology (EULAR) recommendations. In terms of gestational age at delivery and congenital malformations, no difference was seen between patients who used anti-TNF agents during pregnancy and those who did not. Anti-TNF use during pregnancy was associated, however, with increased birthweight and a lower percentage of infants who were small for gestational age. These findings are in keeping with those of prior studies, although larger studies would be helpful in determining whether there are critical periods during pregnancy that have a significant effect on birthweight or whether overall control of inflammation is the predominant factor.
The potential to prevent clinical rheumatoid arthritis (RA) in patients at risk of developing arthritis is of long-standing interest in the rheumatology community. Other studies have addressed the potential for early treatment with glucocorticoids, hydroxychloroquine, or biologics to prevent arthritis, with mixed results. Few published studies have assessed the efficacy of methotrexate in the prevention of arthritis. A randomized controlled trial by Krijbolder and colleagues of adults with arthralgias deemed to be at risk for progression to RA evaluated the use of a single intramuscular steroid injection combined with 1 year of oral methotrexate, compared with placebo, for preventing the development of RA according to the 2010 American College of Rheumatology classification criteria. Although no difference was seen between the groups in development of RA, those treated with methotrexate did have lower levels of joint inflammation seen on MRI and better functional status as per Health Assessment Questionnaire score.
Su and colleagues also looked at the impact of different medications on the development of RA. Using a national health insurance database in Taiwan (between 1997 and 2013), they studied the use of biguanides and sulfonylureas in patients with diabetes and the risk for incident RA. In over 90,000 patients with diabetes, a longer duration of sulfonylurea or biguanide prescription within the first 3 years of diabetes diagnosis was associated with a lower risk for RA compared with non-use. However, use of any antihyperglycemic agents was also associated with lower risk for RA incidence. Limited information is available on both the severity of diabetes and activity of RA, so even a potential mechanism in terms of reduction of blood glucose or inflammation is hard to determine, and more detailed studies are needed.
The safety of different treatments during pregnancy, as well as the effect of both RA and its treatment on pregnancy outcomes, have been areas of research interest in terms of counseling patients with RA about pregnancy planning and management of medications. Gerardi and colleagues followed 63 patients with RA prospectively during pregnancy. They found that although the general understanding is that inflammatory arthritis improves during pregnancy, the percentage of patients with moderate and high disease activity increased slightly, and 37% of patients experienced a flare. Flares were associated with elevated C-reactive protein (CRP) levels and use of multiple prior biologic disease-modifying antirheumatic drugs (bDMARD) (suggesting overall more active arthritis), as well as bDMARD discontinuation in early pregnancy. Similarly, preterm delivery was associated with elevated CRP, higher Disease Activity Score-28 scores, and flares. The study findings provide further support for the importance of controlling maternal disease activity in favoring a better RA course as well as better pregnancy outcomes.
Smeele and colleagues recently published an analysis of the PreCARA cohort study looking at birthweight in pregnant patients with RA. RA is associated with children being born small for gestational age. In this cohort study of 188 pregnant patients with RA, the treatment protocol before pregnancy included hydroxychloroquine, sulfasalazine, prednisone, and anti–tumor necrosis factor (TNF) agents (adalimumab, infliximab, etanercept, and certolizumab). Anti-TNF medications were stopped at 20, 20, 28, or 38 weeks, respectively, according to the European Alliance of Associations for Rheumatology (EULAR) recommendations. In terms of gestational age at delivery and congenital malformations, no difference was seen between patients who used anti-TNF agents during pregnancy and those who did not. Anti-TNF use during pregnancy was associated, however, with increased birthweight and a lower percentage of infants who were small for gestational age. These findings are in keeping with those of prior studies, although larger studies would be helpful in determining whether there are critical periods during pregnancy that have a significant effect on birthweight or whether overall control of inflammation is the predominant factor.
Creation of a National Virtual Tumor Board Through the National TeleOncology Service
Background
There is unequal access to subspecialty oncology expertise across the Veterans Affairs (VA) network. To address this need, the VA established National TeleOncology (NTO), which provides multiple virtual services (asynchronous [electronic consult] and synchronous [phone, video to home, video to facility]) to over 20 VA sites. Beyond these care modalities, a virtual tumor board was conceived to provide a forum for multidisciplinary review of patient cases. We describe the creation of the first NTO virtual tumor board, encompassing malignant hematology diagnoses.
Observations
Tumor boards are considered a standard of care. While challenging to quantify nationally, multiple single institution experiences have established the importance of tumor boards across different measures. A panel of stakeholders were convened to discuss the creation of a virtual tumor board. Best practices and standard operating procedures were created based on guidance from relevant literature and internal VA experience. Participants from specialties including medical oncology, surgical oncology, radiology, pathology, transplant, and palliative care were engaged from eight different VA medical centers across the nation. On March 2, 2022, the initial tumor board was held allowing for synchronous virtual review of patient pathology and imaging. Thus far 6 tumor boards have been convened, reviewing 11 patients originating from 6 different VA sites.
Results
A participant survey was conducted after 4 sessions, which indicated that all who completed the survey (n = 9) found the sessions beneficial or somewhat beneficial, and 55% found the sessions highly applicable to their practice. The most recent tumor board had 33 participants (physicians, nurses, advanced practice practitioners, and pharmacists).
Conclusions
The establishment of a national VA tumor board represents a novel approach to the review of oncology cases across the VA network. The goal of this tumor board is to leverage the diverse knowledge base that exists within the VA to deliver equitable care regardless of veteran location. Along with improving our general understanding of tumor board application, we believe that the NTO tumor board establishes a unique forum for additional tumor types, continued medical education opportunities, and the review of VA clinical trial opportunities.
Background
There is unequal access to subspecialty oncology expertise across the Veterans Affairs (VA) network. To address this need, the VA established National TeleOncology (NTO), which provides multiple virtual services (asynchronous [electronic consult] and synchronous [phone, video to home, video to facility]) to over 20 VA sites. Beyond these care modalities, a virtual tumor board was conceived to provide a forum for multidisciplinary review of patient cases. We describe the creation of the first NTO virtual tumor board, encompassing malignant hematology diagnoses.
Observations
Tumor boards are considered a standard of care. While challenging to quantify nationally, multiple single institution experiences have established the importance of tumor boards across different measures. A panel of stakeholders were convened to discuss the creation of a virtual tumor board. Best practices and standard operating procedures were created based on guidance from relevant literature and internal VA experience. Participants from specialties including medical oncology, surgical oncology, radiology, pathology, transplant, and palliative care were engaged from eight different VA medical centers across the nation. On March 2, 2022, the initial tumor board was held allowing for synchronous virtual review of patient pathology and imaging. Thus far 6 tumor boards have been convened, reviewing 11 patients originating from 6 different VA sites.
Results
A participant survey was conducted after 4 sessions, which indicated that all who completed the survey (n = 9) found the sessions beneficial or somewhat beneficial, and 55% found the sessions highly applicable to their practice. The most recent tumor board had 33 participants (physicians, nurses, advanced practice practitioners, and pharmacists).
Conclusions
The establishment of a national VA tumor board represents a novel approach to the review of oncology cases across the VA network. The goal of this tumor board is to leverage the diverse knowledge base that exists within the VA to deliver equitable care regardless of veteran location. Along with improving our general understanding of tumor board application, we believe that the NTO tumor board establishes a unique forum for additional tumor types, continued medical education opportunities, and the review of VA clinical trial opportunities.
Background
There is unequal access to subspecialty oncology expertise across the Veterans Affairs (VA) network. To address this need, the VA established National TeleOncology (NTO), which provides multiple virtual services (asynchronous [electronic consult] and synchronous [phone, video to home, video to facility]) to over 20 VA sites. Beyond these care modalities, a virtual tumor board was conceived to provide a forum for multidisciplinary review of patient cases. We describe the creation of the first NTO virtual tumor board, encompassing malignant hematology diagnoses.
Observations
Tumor boards are considered a standard of care. While challenging to quantify nationally, multiple single institution experiences have established the importance of tumor boards across different measures. A panel of stakeholders were convened to discuss the creation of a virtual tumor board. Best practices and standard operating procedures were created based on guidance from relevant literature and internal VA experience. Participants from specialties including medical oncology, surgical oncology, radiology, pathology, transplant, and palliative care were engaged from eight different VA medical centers across the nation. On March 2, 2022, the initial tumor board was held allowing for synchronous virtual review of patient pathology and imaging. Thus far 6 tumor boards have been convened, reviewing 11 patients originating from 6 different VA sites.
Results
A participant survey was conducted after 4 sessions, which indicated that all who completed the survey (n = 9) found the sessions beneficial or somewhat beneficial, and 55% found the sessions highly applicable to their practice. The most recent tumor board had 33 participants (physicians, nurses, advanced practice practitioners, and pharmacists).
Conclusions
The establishment of a national VA tumor board represents a novel approach to the review of oncology cases across the VA network. The goal of this tumor board is to leverage the diverse knowledge base that exists within the VA to deliver equitable care regardless of veteran location. Along with improving our general understanding of tumor board application, we believe that the NTO tumor board establishes a unique forum for additional tumor types, continued medical education opportunities, and the review of VA clinical trial opportunities.
Development of an Informatics Infrastructure and Frontend Dashboard for Monitoring Clinical Operations of the National TeleOncology Service
Background
Since inception, the Veterans Affairs (VA) National TeleOncology (NTO) service has monitored clinical operations through data tools produced by the Veterans Health Administration Support Service Center (VSSC). Unfortunately, pertinent data are spread across multiple reports, making it difficult to continually harmonize needed information. Further, the VSSC does not account for NTO’s hub and spoke clinical model, leading to inaccuracies when attempting to analyze unique encounters. To address these challenges, NTO partnered with the VA Salt Lake City Health Care System Informatics, Decision-Enhancement, and Analytic Sciences Center (IDEAS) to develop an informatics architecture and frontend NTO Clinical Operations Dashboard (NCOD). Here, we summarize our dashboard development process and the finalized key reporting components of the NCOD.
Methods
The VA Corporate Data Warehouse (CDW) serves as the primary data source for the NCOD. SQL Server Integration Services was used to build the backend data architecture. Data from the CDW were isolated into a staging data mart for reporting purposes using an extract, transform, load (ETL) approach. The frontend user interface was developed using Power BI. We used a participatory approach1 in determining reporting requirements. Stakeholders included the IDEAS dashboard development team and potential end users from NTO, including leadership, program managers, support assistants, and telehealth coordinators.
Results
The NCOD ETL is scheduled to refresh the data nightly to provide end users with a near real-time experience. The NCOD is comprised of the following four data views: clinic availability, team productivity, patient summary, and encounter summary. The clinic availability view summarizes clinic capacity, no shows, overbookings, and percent utilization. Relative value unit- based productivity is summarized in the team productivity view. The patient summary view presents aggregated data for veterans served by NTO, including geographic distribution, with patient-level drill down displaying demographics, cancer characteristics, and treatment history. Lastly, the encounter view displays utilization trends by modality, while accurately accounting for the hub and spoke clinical model.
Conclusions
An informatics architecture and frontend information display that is capable of synthesizing EHR data into a consumable format has been pivotal in obtaining accurate and timely insight into the demand and capacity of services provided by NTO.
- Esquer Rochin MA, Gutierrez-Garcia JO, Rosales JH, Rodriguez LF. Design and evaluation of a dashboard to support the comprehension of the progression.
Background
Since inception, the Veterans Affairs (VA) National TeleOncology (NTO) service has monitored clinical operations through data tools produced by the Veterans Health Administration Support Service Center (VSSC). Unfortunately, pertinent data are spread across multiple reports, making it difficult to continually harmonize needed information. Further, the VSSC does not account for NTO’s hub and spoke clinical model, leading to inaccuracies when attempting to analyze unique encounters. To address these challenges, NTO partnered with the VA Salt Lake City Health Care System Informatics, Decision-Enhancement, and Analytic Sciences Center (IDEAS) to develop an informatics architecture and frontend NTO Clinical Operations Dashboard (NCOD). Here, we summarize our dashboard development process and the finalized key reporting components of the NCOD.
Methods
The VA Corporate Data Warehouse (CDW) serves as the primary data source for the NCOD. SQL Server Integration Services was used to build the backend data architecture. Data from the CDW were isolated into a staging data mart for reporting purposes using an extract, transform, load (ETL) approach. The frontend user interface was developed using Power BI. We used a participatory approach1 in determining reporting requirements. Stakeholders included the IDEAS dashboard development team and potential end users from NTO, including leadership, program managers, support assistants, and telehealth coordinators.
Results
The NCOD ETL is scheduled to refresh the data nightly to provide end users with a near real-time experience. The NCOD is comprised of the following four data views: clinic availability, team productivity, patient summary, and encounter summary. The clinic availability view summarizes clinic capacity, no shows, overbookings, and percent utilization. Relative value unit- based productivity is summarized in the team productivity view. The patient summary view presents aggregated data for veterans served by NTO, including geographic distribution, with patient-level drill down displaying demographics, cancer characteristics, and treatment history. Lastly, the encounter view displays utilization trends by modality, while accurately accounting for the hub and spoke clinical model.
Conclusions
An informatics architecture and frontend information display that is capable of synthesizing EHR data into a consumable format has been pivotal in obtaining accurate and timely insight into the demand and capacity of services provided by NTO.
Background
Since inception, the Veterans Affairs (VA) National TeleOncology (NTO) service has monitored clinical operations through data tools produced by the Veterans Health Administration Support Service Center (VSSC). Unfortunately, pertinent data are spread across multiple reports, making it difficult to continually harmonize needed information. Further, the VSSC does not account for NTO’s hub and spoke clinical model, leading to inaccuracies when attempting to analyze unique encounters. To address these challenges, NTO partnered with the VA Salt Lake City Health Care System Informatics, Decision-Enhancement, and Analytic Sciences Center (IDEAS) to develop an informatics architecture and frontend NTO Clinical Operations Dashboard (NCOD). Here, we summarize our dashboard development process and the finalized key reporting components of the NCOD.
Methods
The VA Corporate Data Warehouse (CDW) serves as the primary data source for the NCOD. SQL Server Integration Services was used to build the backend data architecture. Data from the CDW were isolated into a staging data mart for reporting purposes using an extract, transform, load (ETL) approach. The frontend user interface was developed using Power BI. We used a participatory approach1 in determining reporting requirements. Stakeholders included the IDEAS dashboard development team and potential end users from NTO, including leadership, program managers, support assistants, and telehealth coordinators.
Results
The NCOD ETL is scheduled to refresh the data nightly to provide end users with a near real-time experience. The NCOD is comprised of the following four data views: clinic availability, team productivity, patient summary, and encounter summary. The clinic availability view summarizes clinic capacity, no shows, overbookings, and percent utilization. Relative value unit- based productivity is summarized in the team productivity view. The patient summary view presents aggregated data for veterans served by NTO, including geographic distribution, with patient-level drill down displaying demographics, cancer characteristics, and treatment history. Lastly, the encounter view displays utilization trends by modality, while accurately accounting for the hub and spoke clinical model.
Conclusions
An informatics architecture and frontend information display that is capable of synthesizing EHR data into a consumable format has been pivotal in obtaining accurate and timely insight into the demand and capacity of services provided by NTO.
- Esquer Rochin MA, Gutierrez-Garcia JO, Rosales JH, Rodriguez LF. Design and evaluation of a dashboard to support the comprehension of the progression.
- Esquer Rochin MA, Gutierrez-Garcia JO, Rosales JH, Rodriguez LF. Design and evaluation of a dashboard to support the comprehension of the progression.
Myeloid Neoplasm Masquerading as Hypereosinophilia and Sweet Syndrome
Introduction
Hypereosinophilia can be seen in many medical conditions, including myeloproliferative disorders, and can lead to serious complications if untreated. Sweet syndrome is a rare and painful cutaneous inflammatory condition that has been linked to underlying malignancies.
Case Presentation
A 72-year-old male presented with 6-month history of painful maculopapular rash, night sweats, fever, and weight loss. He was treated with antibiotics and steroids with no improvement. A skin biopsy demonstrated neutrophilic dermatosis consistent with sweet syndrome. Laboratory studies a showed hemoglobin 7.1g/dl, WBC 12.9x103/uL, 30% eosinophils, absolute eosinophil count 3x109/L, and normal platelets. Infectious and immunological work up was negative. CT scan revealed splenomegaly. Bone marrow biopsy showed 100% hypercellularity, trilineage atypia, eosinophils 43% (normal, 1-5%) and 3-4% blasts positive for CD34 and CD117. FISH studies detected loss of PDGFRB signal, cytogenetics revealed a complex karyotype. He was diagnosed with a high-risk (based on IPSS-R) MDS/MPN cross-over with peripheral eosinophilia and is planned to undergo HSCT.
Discussion
Hematologic malignancies are associated with several paraneoplastic syndromes including sweet syndrome, also known as acute febrile neutrophilic dermatosis. The literature describes sweet syndrome occurring mostly with AML but can also be seen with other malignancies like MDS and solid tumor. The distinction between sweet syndrome and infectious or immune-mediated rash can be challenging as it requires histopathologic evaluation and is usually mistreated. Hypereosinophilia is defined as persistent eosinophil count of at least 1.5x109/L. It can be idiopathic or associated with allergic, rheumatologic, infectious, or neoplastic conditions. Clonal hypereosinophilia is most frequently associated with chronic myeloid neoplasms such as myeloproliferative neoplasm (MPN) or overlapping MDS/MPN, and more less frequently with AML. Hypereosinophilia related to hematological malignancies has been linked to gene rearrangements involving PDGFRA, PDGFRB, FGFR1, and JAK2. Patients with documented rearrangements or mutations in PDGFRB are treated with imatinib, which is a potent kinase inhibitor. However, patients with high-risk MDS/MPN with associated eosinophilia are typically treated as MDS and should undergo allogenic HSCT if eligible.
Conclusions
Both hypereosinophlia and sweet syndrome have been linked to myeloid neoplasms. Early recognition of either phenomenon as a paraneoplastic syndrome is important for early diagnosis and treatment.
Introduction
Hypereosinophilia can be seen in many medical conditions, including myeloproliferative disorders, and can lead to serious complications if untreated. Sweet syndrome is a rare and painful cutaneous inflammatory condition that has been linked to underlying malignancies.
Case Presentation
A 72-year-old male presented with 6-month history of painful maculopapular rash, night sweats, fever, and weight loss. He was treated with antibiotics and steroids with no improvement. A skin biopsy demonstrated neutrophilic dermatosis consistent with sweet syndrome. Laboratory studies a showed hemoglobin 7.1g/dl, WBC 12.9x103/uL, 30% eosinophils, absolute eosinophil count 3x109/L, and normal platelets. Infectious and immunological work up was negative. CT scan revealed splenomegaly. Bone marrow biopsy showed 100% hypercellularity, trilineage atypia, eosinophils 43% (normal, 1-5%) and 3-4% blasts positive for CD34 and CD117. FISH studies detected loss of PDGFRB signal, cytogenetics revealed a complex karyotype. He was diagnosed with a high-risk (based on IPSS-R) MDS/MPN cross-over with peripheral eosinophilia and is planned to undergo HSCT.
Discussion
Hematologic malignancies are associated with several paraneoplastic syndromes including sweet syndrome, also known as acute febrile neutrophilic dermatosis. The literature describes sweet syndrome occurring mostly with AML but can also be seen with other malignancies like MDS and solid tumor. The distinction between sweet syndrome and infectious or immune-mediated rash can be challenging as it requires histopathologic evaluation and is usually mistreated. Hypereosinophilia is defined as persistent eosinophil count of at least 1.5x109/L. It can be idiopathic or associated with allergic, rheumatologic, infectious, or neoplastic conditions. Clonal hypereosinophilia is most frequently associated with chronic myeloid neoplasms such as myeloproliferative neoplasm (MPN) or overlapping MDS/MPN, and more less frequently with AML. Hypereosinophilia related to hematological malignancies has been linked to gene rearrangements involving PDGFRA, PDGFRB, FGFR1, and JAK2. Patients with documented rearrangements or mutations in PDGFRB are treated with imatinib, which is a potent kinase inhibitor. However, patients with high-risk MDS/MPN with associated eosinophilia are typically treated as MDS and should undergo allogenic HSCT if eligible.
Conclusions
Both hypereosinophlia and sweet syndrome have been linked to myeloid neoplasms. Early recognition of either phenomenon as a paraneoplastic syndrome is important for early diagnosis and treatment.
Introduction
Hypereosinophilia can be seen in many medical conditions, including myeloproliferative disorders, and can lead to serious complications if untreated. Sweet syndrome is a rare and painful cutaneous inflammatory condition that has been linked to underlying malignancies.
Case Presentation
A 72-year-old male presented with 6-month history of painful maculopapular rash, night sweats, fever, and weight loss. He was treated with antibiotics and steroids with no improvement. A skin biopsy demonstrated neutrophilic dermatosis consistent with sweet syndrome. Laboratory studies a showed hemoglobin 7.1g/dl, WBC 12.9x103/uL, 30% eosinophils, absolute eosinophil count 3x109/L, and normal platelets. Infectious and immunological work up was negative. CT scan revealed splenomegaly. Bone marrow biopsy showed 100% hypercellularity, trilineage atypia, eosinophils 43% (normal, 1-5%) and 3-4% blasts positive for CD34 and CD117. FISH studies detected loss of PDGFRB signal, cytogenetics revealed a complex karyotype. He was diagnosed with a high-risk (based on IPSS-R) MDS/MPN cross-over with peripheral eosinophilia and is planned to undergo HSCT.
Discussion
Hematologic malignancies are associated with several paraneoplastic syndromes including sweet syndrome, also known as acute febrile neutrophilic dermatosis. The literature describes sweet syndrome occurring mostly with AML but can also be seen with other malignancies like MDS and solid tumor. The distinction between sweet syndrome and infectious or immune-mediated rash can be challenging as it requires histopathologic evaluation and is usually mistreated. Hypereosinophilia is defined as persistent eosinophil count of at least 1.5x109/L. It can be idiopathic or associated with allergic, rheumatologic, infectious, or neoplastic conditions. Clonal hypereosinophilia is most frequently associated with chronic myeloid neoplasms such as myeloproliferative neoplasm (MPN) or overlapping MDS/MPN, and more less frequently with AML. Hypereosinophilia related to hematological malignancies has been linked to gene rearrangements involving PDGFRA, PDGFRB, FGFR1, and JAK2. Patients with documented rearrangements or mutations in PDGFRB are treated with imatinib, which is a potent kinase inhibitor. However, patients with high-risk MDS/MPN with associated eosinophilia are typically treated as MDS and should undergo allogenic HSCT if eligible.
Conclusions
Both hypereosinophlia and sweet syndrome have been linked to myeloid neoplasms. Early recognition of either phenomenon as a paraneoplastic syndrome is important for early diagnosis and treatment.
Gastrointestinal Stromal Tumor Arising From the Small Intestine in a Heart Transplant Recipient on Hemodialysis and Chronic Immunosuppression: A Case Report
Background
Gastrointestinal stromal tumors (GISTs) are rare mesenchymal tumors with worse prognosis if arising from the small bowel. Surgery remains the mainstay of treatment for patients with resectable tumors. Imatinib has become the standard treatment in cKIT-positive GISTs with significant morbidity in neoadjuvant, adjuvant, and palliative settings. There are limited data on efficacy and safety of imatinib in dialysis patients, and chemotherapy dosing is challenging in dialysis patients with multiple comorbidities.
Presentation
A 68-year-old male with a history of orthotopic heart transplantation on sirolimus with prednisone, cardiac allograft vasculopathy, plus ESRD on peritoneal dialysis (PD), presented with lower abdominal pain and fever. Abdominal imaging revealed a right lower quadrant (RLQ) mass with concern for bowel perforation.
Diagnosis and Treatment
The patient underwent exploratory laparoscopy with small bowel resection, excision of the mesenteric small bowel mass, drainage and washout of intraabdominal abscess, removal of PD catheter, and transition to hemodialysis. Pathology revealed a 14.5-cm high-grade GIST with mixed spindle and epithelioid types involving the ileal wall and mesentery, consistent with pT4 primary tumor and stage IIIB disease. Molecular testing was positive for c-KIT and DOG-1 mutations.
After a prolonged recovery, repeat abdominal imaging demonstrated metastatic liver disease and a new RLQ lesion. The patient was started on palliative imatinib 100 mg daily with subsequent increase to 200 mg daily. He was monitored closely for toxicities but reported only mild nausea controlled with ondansetron. Hemodialysis was continued 3 times per week. Follow up scans 3 months later showed improvement in RLQ mass and hepatic lesions. The patient remains on the current dose 15 months after the diagnosis.
Conclusion
To our knowledge, this is the first case of a small intestinal GIST in a heart transplant recipient treated with dose-reduced imatinib with concurrent dialysis and immunosuppression. Treatment decision-making was complex given concern for cardiotoxicity with pre-existing cardiac disease and drug-drug interactions with immunosuppressive agents. While some literature suggests standard dose imatinib with dialysis, no large-scale studies evaluated pharmacokinetics of imatinib with creatinine clearance < 20 mL/min. There is a need for further studies to determine dosing strategies for such patients.
Background
Gastrointestinal stromal tumors (GISTs) are rare mesenchymal tumors with worse prognosis if arising from the small bowel. Surgery remains the mainstay of treatment for patients with resectable tumors. Imatinib has become the standard treatment in cKIT-positive GISTs with significant morbidity in neoadjuvant, adjuvant, and palliative settings. There are limited data on efficacy and safety of imatinib in dialysis patients, and chemotherapy dosing is challenging in dialysis patients with multiple comorbidities.
Presentation
A 68-year-old male with a history of orthotopic heart transplantation on sirolimus with prednisone, cardiac allograft vasculopathy, plus ESRD on peritoneal dialysis (PD), presented with lower abdominal pain and fever. Abdominal imaging revealed a right lower quadrant (RLQ) mass with concern for bowel perforation.
Diagnosis and Treatment
The patient underwent exploratory laparoscopy with small bowel resection, excision of the mesenteric small bowel mass, drainage and washout of intraabdominal abscess, removal of PD catheter, and transition to hemodialysis. Pathology revealed a 14.5-cm high-grade GIST with mixed spindle and epithelioid types involving the ileal wall and mesentery, consistent with pT4 primary tumor and stage IIIB disease. Molecular testing was positive for c-KIT and DOG-1 mutations.
After a prolonged recovery, repeat abdominal imaging demonstrated metastatic liver disease and a new RLQ lesion. The patient was started on palliative imatinib 100 mg daily with subsequent increase to 200 mg daily. He was monitored closely for toxicities but reported only mild nausea controlled with ondansetron. Hemodialysis was continued 3 times per week. Follow up scans 3 months later showed improvement in RLQ mass and hepatic lesions. The patient remains on the current dose 15 months after the diagnosis.
Conclusion
To our knowledge, this is the first case of a small intestinal GIST in a heart transplant recipient treated with dose-reduced imatinib with concurrent dialysis and immunosuppression. Treatment decision-making was complex given concern for cardiotoxicity with pre-existing cardiac disease and drug-drug interactions with immunosuppressive agents. While some literature suggests standard dose imatinib with dialysis, no large-scale studies evaluated pharmacokinetics of imatinib with creatinine clearance < 20 mL/min. There is a need for further studies to determine dosing strategies for such patients.
Background
Gastrointestinal stromal tumors (GISTs) are rare mesenchymal tumors with worse prognosis if arising from the small bowel. Surgery remains the mainstay of treatment for patients with resectable tumors. Imatinib has become the standard treatment in cKIT-positive GISTs with significant morbidity in neoadjuvant, adjuvant, and palliative settings. There are limited data on efficacy and safety of imatinib in dialysis patients, and chemotherapy dosing is challenging in dialysis patients with multiple comorbidities.
Presentation
A 68-year-old male with a history of orthotopic heart transplantation on sirolimus with prednisone, cardiac allograft vasculopathy, plus ESRD on peritoneal dialysis (PD), presented with lower abdominal pain and fever. Abdominal imaging revealed a right lower quadrant (RLQ) mass with concern for bowel perforation.
Diagnosis and Treatment
The patient underwent exploratory laparoscopy with small bowel resection, excision of the mesenteric small bowel mass, drainage and washout of intraabdominal abscess, removal of PD catheter, and transition to hemodialysis. Pathology revealed a 14.5-cm high-grade GIST with mixed spindle and epithelioid types involving the ileal wall and mesentery, consistent with pT4 primary tumor and stage IIIB disease. Molecular testing was positive for c-KIT and DOG-1 mutations.
After a prolonged recovery, repeat abdominal imaging demonstrated metastatic liver disease and a new RLQ lesion. The patient was started on palliative imatinib 100 mg daily with subsequent increase to 200 mg daily. He was monitored closely for toxicities but reported only mild nausea controlled with ondansetron. Hemodialysis was continued 3 times per week. Follow up scans 3 months later showed improvement in RLQ mass and hepatic lesions. The patient remains on the current dose 15 months after the diagnosis.
Conclusion
To our knowledge, this is the first case of a small intestinal GIST in a heart transplant recipient treated with dose-reduced imatinib with concurrent dialysis and immunosuppression. Treatment decision-making was complex given concern for cardiotoxicity with pre-existing cardiac disease and drug-drug interactions with immunosuppressive agents. While some literature suggests standard dose imatinib with dialysis, no large-scale studies evaluated pharmacokinetics of imatinib with creatinine clearance < 20 mL/min. There is a need for further studies to determine dosing strategies for such patients.
Team-based Genetic Consultation: An Effective System of Care for Delivery of Precision Oncology Services
Objectives
US Department of Veterans Affairs (VA) patients with genetics referrals are 1.5 times more likely to have multiple cancer screening and preventive procedures if they completed their genetic consultations, but only when completed under a VA traditional model staffed by a team of clinical geneticists and genetic counselors versus a VA nontraditional, centralized telehealth model staffed by genetic counselors working independently. We sought to understand the reasons for these differences in cancer screening and prevention uptake.
Methods
We reviewed randomly selected medical records of patients with cancer genetics referrals stratified by model (142 records from each model). We conducted semi-structured interviews with 15 genetics providers and 36 referring clinicians from 13 VA facilities using purposive sampling. We analyzed annotated medical records and interview transcripts using a rapid assessment process. We characterized annotations as personalized recommendations (eg, begin colonoscopy at age 30 then every 1-2 years), options (eg, consider bilateral mastectomy), and generic messages (eg, refer to guidelines or another provider).
Results
Cancer screening or prevention was documented in 80 traditional-model records (141 annotations) and 106 nontraditional-model records (143 annotations). Personalized recommendations comprised 69% (97/141) of annotations within traditional-model records and 30% (43/143) within nontraditional-model records. Generic messages comprised 17% (24/141) of annotations in traditional-model records and 51% (73/143) in nontraditional-model records. From interview data, referring clinicians expected a broad range of services from genetics providers, including management and screening recommendations, and stated their role was to follow through on recommendations made. Under the traditional model, geneticists formulated recommendations documented by genetic counselors. Under the nontraditional model, scope of practice limited how genetic counselors addressed cancer screening and prevention.
Conclusions/Impacts
Personalized recommendations were typical of traditional-model records, whereas nontraditional-model records usually had generic messages. Compared with the nontraditional model, the traditional model was more patient-centered and better meets expectations of referring clinicians, which might explain in part the differences in patient uptake of cancer screening and preventive procedures.
As the demand for genetic services grows, the VA should promote team-based care under the traditional model for a more patient-centered, coordinated, and effective system of care for precision oncology.
Objectives
US Department of Veterans Affairs (VA) patients with genetics referrals are 1.5 times more likely to have multiple cancer screening and preventive procedures if they completed their genetic consultations, but only when completed under a VA traditional model staffed by a team of clinical geneticists and genetic counselors versus a VA nontraditional, centralized telehealth model staffed by genetic counselors working independently. We sought to understand the reasons for these differences in cancer screening and prevention uptake.
Methods
We reviewed randomly selected medical records of patients with cancer genetics referrals stratified by model (142 records from each model). We conducted semi-structured interviews with 15 genetics providers and 36 referring clinicians from 13 VA facilities using purposive sampling. We analyzed annotated medical records and interview transcripts using a rapid assessment process. We characterized annotations as personalized recommendations (eg, begin colonoscopy at age 30 then every 1-2 years), options (eg, consider bilateral mastectomy), and generic messages (eg, refer to guidelines or another provider).
Results
Cancer screening or prevention was documented in 80 traditional-model records (141 annotations) and 106 nontraditional-model records (143 annotations). Personalized recommendations comprised 69% (97/141) of annotations within traditional-model records and 30% (43/143) within nontraditional-model records. Generic messages comprised 17% (24/141) of annotations in traditional-model records and 51% (73/143) in nontraditional-model records. From interview data, referring clinicians expected a broad range of services from genetics providers, including management and screening recommendations, and stated their role was to follow through on recommendations made. Under the traditional model, geneticists formulated recommendations documented by genetic counselors. Under the nontraditional model, scope of practice limited how genetic counselors addressed cancer screening and prevention.
Conclusions/Impacts
Personalized recommendations were typical of traditional-model records, whereas nontraditional-model records usually had generic messages. Compared with the nontraditional model, the traditional model was more patient-centered and better meets expectations of referring clinicians, which might explain in part the differences in patient uptake of cancer screening and preventive procedures.
As the demand for genetic services grows, the VA should promote team-based care under the traditional model for a more patient-centered, coordinated, and effective system of care for precision oncology.
Objectives
US Department of Veterans Affairs (VA) patients with genetics referrals are 1.5 times more likely to have multiple cancer screening and preventive procedures if they completed their genetic consultations, but only when completed under a VA traditional model staffed by a team of clinical geneticists and genetic counselors versus a VA nontraditional, centralized telehealth model staffed by genetic counselors working independently. We sought to understand the reasons for these differences in cancer screening and prevention uptake.
Methods
We reviewed randomly selected medical records of patients with cancer genetics referrals stratified by model (142 records from each model). We conducted semi-structured interviews with 15 genetics providers and 36 referring clinicians from 13 VA facilities using purposive sampling. We analyzed annotated medical records and interview transcripts using a rapid assessment process. We characterized annotations as personalized recommendations (eg, begin colonoscopy at age 30 then every 1-2 years), options (eg, consider bilateral mastectomy), and generic messages (eg, refer to guidelines or another provider).
Results
Cancer screening or prevention was documented in 80 traditional-model records (141 annotations) and 106 nontraditional-model records (143 annotations). Personalized recommendations comprised 69% (97/141) of annotations within traditional-model records and 30% (43/143) within nontraditional-model records. Generic messages comprised 17% (24/141) of annotations in traditional-model records and 51% (73/143) in nontraditional-model records. From interview data, referring clinicians expected a broad range of services from genetics providers, including management and screening recommendations, and stated their role was to follow through on recommendations made. Under the traditional model, geneticists formulated recommendations documented by genetic counselors. Under the nontraditional model, scope of practice limited how genetic counselors addressed cancer screening and prevention.
Conclusions/Impacts
Personalized recommendations were typical of traditional-model records, whereas nontraditional-model records usually had generic messages. Compared with the nontraditional model, the traditional model was more patient-centered and better meets expectations of referring clinicians, which might explain in part the differences in patient uptake of cancer screening and preventive procedures.
As the demand for genetic services grows, the VA should promote team-based care under the traditional model for a more patient-centered, coordinated, and effective system of care for precision oncology.