User login
Best Practices in HR+/HER2- Breast Cancer
Two out of three patients diagnosed with breast cancer are found to have the HR+/HER2- subtype, and over time, at least one third of patients with this subtype develop metastatic disease. But recent advances in the treatment of both early and metastatic HR+/HER2- disease have resulted in significant improvement in outcomes.
In this panel ReCAP, Drs Kathy Miller from Indiana University and Alexandra Thomas from Wake Forest University review how progress in treatment has affected outcomes across all stages of HR+/HER2- breast cancer.
They report that the use of trastuzumab deruxtecan in the metastatic setting improves overall survival. They also discuss how adjuvant use of abemaciclib in early-stage breast cancer improves disease-free survival, as evidenced by the latest updates of the monarchE trial, now providing 4 years of follow-up.
--
Ballvé-Lantero Professor of Oncology, Indiana University School of Medicine, Indianapolis, Indiana
Kathy D. Miller, MD, has disclosed the following relevant financial relationships:
Serve on independent Data Monitoring Committees for ongoing trials for: Merck; Genentech/Roche; AstraZeneca; Celcuity
Two out of three patients diagnosed with breast cancer are found to have the HR+/HER2- subtype, and over time, at least one third of patients with this subtype develop metastatic disease. But recent advances in the treatment of both early and metastatic HR+/HER2- disease have resulted in significant improvement in outcomes.
In this panel ReCAP, Drs Kathy Miller from Indiana University and Alexandra Thomas from Wake Forest University review how progress in treatment has affected outcomes across all stages of HR+/HER2- breast cancer.
They report that the use of trastuzumab deruxtecan in the metastatic setting improves overall survival. They also discuss how adjuvant use of abemaciclib in early-stage breast cancer improves disease-free survival, as evidenced by the latest updates of the monarchE trial, now providing 4 years of follow-up.
--
Ballvé-Lantero Professor of Oncology, Indiana University School of Medicine, Indianapolis, Indiana
Kathy D. Miller, MD, has disclosed the following relevant financial relationships:
Serve on independent Data Monitoring Committees for ongoing trials for: Merck; Genentech/Roche; AstraZeneca; Celcuity
Two out of three patients diagnosed with breast cancer are found to have the HR+/HER2- subtype, and over time, at least one third of patients with this subtype develop metastatic disease. But recent advances in the treatment of both early and metastatic HR+/HER2- disease have resulted in significant improvement in outcomes.
In this panel ReCAP, Drs Kathy Miller from Indiana University and Alexandra Thomas from Wake Forest University review how progress in treatment has affected outcomes across all stages of HR+/HER2- breast cancer.
They report that the use of trastuzumab deruxtecan in the metastatic setting improves overall survival. They also discuss how adjuvant use of abemaciclib in early-stage breast cancer improves disease-free survival, as evidenced by the latest updates of the monarchE trial, now providing 4 years of follow-up.
--
Ballvé-Lantero Professor of Oncology, Indiana University School of Medicine, Indianapolis, Indiana
Kathy D. Miller, MD, has disclosed the following relevant financial relationships:
Serve on independent Data Monitoring Committees for ongoing trials for: Merck; Genentech/Roche; AstraZeneca; Celcuity

Commentary: HER2+-targeted therapy, ovarian suppression, and adjuvant therapy in breast cancer, February 2023
The elevated risk for recurrence in young women with HR+ early breast cancer highlights the importance of aggressive endocrine therapy in the majority of patients in this population. Examples of approaches to maximize endocrine therapy benefit include the addition of ovarian suppression to either tamoxifen or an aromatase inhibitor (AI) as well as an extended duration of adjuvant endocrine therapy.4,5 Among 3047 premenopausal women included in SOFT study, at 12 years follow-up, the addition of ovarian function suppression (OFS) to tamoxifen significantly improved disease-free survival (DFS) compared with tamoxifen alone (hazard ratio 0.82; P = .03) with a more pronounced DFS benefit with exemestane plus OFS compared with tamoxifen (hazard ratio 0.69) (Francis et al). In the HER2- subgroup, those who received prior chemotherapy had 12-year OFS rates of 78.8% with tamoxifen, 81.1% with tamoxifen plus OFS and 84.4% with exemestane plus OFS. Furthermore, in the HER2- subgroup, women younger than 35 years had absolute improvements in 12-year OS of 9.1% with tamoxifen plus OFS and 16.5% with exemestane plus OFS compared with tamoxifen. These updated results provide further support for OFS added to tamoxifen or an AI (with more benefit seen with an AI) in the treatment of HR+ early breast cancer in young women who are at high risk for recurrence. Longer follow-up will be important to better define the treatment effect considering recurrence patterns for this subtype of breast cancer.
Various guidelines recommend the use of adjuvant bisphosphonates for postmenopausal patients with early breast cancer on the basis of disease-free and bone metastasis-free survival benefits.6 A regimen of zolendronic acid every 6 months for 3 years is commonly used in clinical practice. A substudy of ABCSG-12, including 725 premenopausal patients with HR+ early breast cancer on ovarian suppression randomly assigned to receive tamoxifen or anastrozole with or without zolendronic acid every 6 months, investigated the effect of shorter duration of bisphosphonate therapy on breast cancer outcomes (Beltran-Bless et al). After a median follow-up of 96 months, there was no statistically significant difference in DFS (hazard ratio 0.88; log-rank P = .642) or OS (stratified hazard ratio 1.16; log-rank P = .796) between patients who received ≤6 or ≥7 infusions. Rates of adverse events were increased in the patients who received ≥7 or ≤6 infusions (arthralgia, 20.1% vs 12.4%; nausea, 12.8% vs 7.3%; bone pain, 41.6% vs 34.9%). Modifications to adjuvant breast cancer regimens that can provide more ease for patients with less toxicity while maintaining efficacy are greatly desired to simultaneously support quality of life and disease outcomes.
Additional References
- Swain SM, Baselga J, Kim SB, et al; for the CLEOPATRA Study Group. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724-734. Doi: 10.1056/NEJMoa1413513
- Miles D, Ciruelos E, Schneeweiss A, et al; for the PERUSE investigators. Final results from the PERUSE study of first-line pertuzumab plus trastuzumab plus a taxane for HER2-positive locally recurrent or metastatic breast cancer, with a multivariable approach to guide prognostication. Ann Oncol. 2021;32:1245-1255. Doi: 10.1016/j.annonc.2021.06.024
- Hua X, Bi X-W, Zhao J-L, et al; for the South China Breast Cancer Group (SCBCG). Trastuzumab plus endocrine therapy or chemotherapy as first-line treatment for patients with hormone receptor-positive and HER2-positive metastatic breast cancer (SYSUCC-002). Clin Cancer Res. 2022;28:637-645. Doi: 10.1158/1078-0432.CCR-21-3435
- Kim H-A, Lee JW, Nam SJ, et al; for the Korean Breast Cancer Study Group. Adding ovarian suppression to tamoxifen for premenopausal breast Cancer: a randomized phase III trial. J Clin Oncol. 2020;38:434-443. Doi: 10.1200/JCO.19.00126
- Davies C, Pan H, Godwin J, et al; for the Adjuvant Tamoxifen: Longer Against Shorter (ATLAS) Collaborative Group. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. Doi: 10.1016/S0140-6736(12)61963-1
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet. 2015;386:1353-1361. Doi: 10.1016/S0140-6736(15)60908-4
The elevated risk for recurrence in young women with HR+ early breast cancer highlights the importance of aggressive endocrine therapy in the majority of patients in this population. Examples of approaches to maximize endocrine therapy benefit include the addition of ovarian suppression to either tamoxifen or an aromatase inhibitor (AI) as well as an extended duration of adjuvant endocrine therapy.4,5 Among 3047 premenopausal women included in SOFT study, at 12 years follow-up, the addition of ovarian function suppression (OFS) to tamoxifen significantly improved disease-free survival (DFS) compared with tamoxifen alone (hazard ratio 0.82; P = .03) with a more pronounced DFS benefit with exemestane plus OFS compared with tamoxifen (hazard ratio 0.69) (Francis et al). In the HER2- subgroup, those who received prior chemotherapy had 12-year OFS rates of 78.8% with tamoxifen, 81.1% with tamoxifen plus OFS and 84.4% with exemestane plus OFS. Furthermore, in the HER2- subgroup, women younger than 35 years had absolute improvements in 12-year OS of 9.1% with tamoxifen plus OFS and 16.5% with exemestane plus OFS compared with tamoxifen. These updated results provide further support for OFS added to tamoxifen or an AI (with more benefit seen with an AI) in the treatment of HR+ early breast cancer in young women who are at high risk for recurrence. Longer follow-up will be important to better define the treatment effect considering recurrence patterns for this subtype of breast cancer.
Various guidelines recommend the use of adjuvant bisphosphonates for postmenopausal patients with early breast cancer on the basis of disease-free and bone metastasis-free survival benefits.6 A regimen of zolendronic acid every 6 months for 3 years is commonly used in clinical practice. A substudy of ABCSG-12, including 725 premenopausal patients with HR+ early breast cancer on ovarian suppression randomly assigned to receive tamoxifen or anastrozole with or without zolendronic acid every 6 months, investigated the effect of shorter duration of bisphosphonate therapy on breast cancer outcomes (Beltran-Bless et al). After a median follow-up of 96 months, there was no statistically significant difference in DFS (hazard ratio 0.88; log-rank P = .642) or OS (stratified hazard ratio 1.16; log-rank P = .796) between patients who received ≤6 or ≥7 infusions. Rates of adverse events were increased in the patients who received ≥7 or ≤6 infusions (arthralgia, 20.1% vs 12.4%; nausea, 12.8% vs 7.3%; bone pain, 41.6% vs 34.9%). Modifications to adjuvant breast cancer regimens that can provide more ease for patients with less toxicity while maintaining efficacy are greatly desired to simultaneously support quality of life and disease outcomes.
Additional References
- Swain SM, Baselga J, Kim SB, et al; for the CLEOPATRA Study Group. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724-734. Doi: 10.1056/NEJMoa1413513
- Miles D, Ciruelos E, Schneeweiss A, et al; for the PERUSE investigators. Final results from the PERUSE study of first-line pertuzumab plus trastuzumab plus a taxane for HER2-positive locally recurrent or metastatic breast cancer, with a multivariable approach to guide prognostication. Ann Oncol. 2021;32:1245-1255. Doi: 10.1016/j.annonc.2021.06.024
- Hua X, Bi X-W, Zhao J-L, et al; for the South China Breast Cancer Group (SCBCG). Trastuzumab plus endocrine therapy or chemotherapy as first-line treatment for patients with hormone receptor-positive and HER2-positive metastatic breast cancer (SYSUCC-002). Clin Cancer Res. 2022;28:637-645. Doi: 10.1158/1078-0432.CCR-21-3435
- Kim H-A, Lee JW, Nam SJ, et al; for the Korean Breast Cancer Study Group. Adding ovarian suppression to tamoxifen for premenopausal breast Cancer: a randomized phase III trial. J Clin Oncol. 2020;38:434-443. Doi: 10.1200/JCO.19.00126
- Davies C, Pan H, Godwin J, et al; for the Adjuvant Tamoxifen: Longer Against Shorter (ATLAS) Collaborative Group. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. Doi: 10.1016/S0140-6736(12)61963-1
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet. 2015;386:1353-1361. Doi: 10.1016/S0140-6736(15)60908-4
The elevated risk for recurrence in young women with HR+ early breast cancer highlights the importance of aggressive endocrine therapy in the majority of patients in this population. Examples of approaches to maximize endocrine therapy benefit include the addition of ovarian suppression to either tamoxifen or an aromatase inhibitor (AI) as well as an extended duration of adjuvant endocrine therapy.4,5 Among 3047 premenopausal women included in SOFT study, at 12 years follow-up, the addition of ovarian function suppression (OFS) to tamoxifen significantly improved disease-free survival (DFS) compared with tamoxifen alone (hazard ratio 0.82; P = .03) with a more pronounced DFS benefit with exemestane plus OFS compared with tamoxifen (hazard ratio 0.69) (Francis et al). In the HER2- subgroup, those who received prior chemotherapy had 12-year OFS rates of 78.8% with tamoxifen, 81.1% with tamoxifen plus OFS and 84.4% with exemestane plus OFS. Furthermore, in the HER2- subgroup, women younger than 35 years had absolute improvements in 12-year OS of 9.1% with tamoxifen plus OFS and 16.5% with exemestane plus OFS compared with tamoxifen. These updated results provide further support for OFS added to tamoxifen or an AI (with more benefit seen with an AI) in the treatment of HR+ early breast cancer in young women who are at high risk for recurrence. Longer follow-up will be important to better define the treatment effect considering recurrence patterns for this subtype of breast cancer.
Various guidelines recommend the use of adjuvant bisphosphonates for postmenopausal patients with early breast cancer on the basis of disease-free and bone metastasis-free survival benefits.6 A regimen of zolendronic acid every 6 months for 3 years is commonly used in clinical practice. A substudy of ABCSG-12, including 725 premenopausal patients with HR+ early breast cancer on ovarian suppression randomly assigned to receive tamoxifen or anastrozole with or without zolendronic acid every 6 months, investigated the effect of shorter duration of bisphosphonate therapy on breast cancer outcomes (Beltran-Bless et al). After a median follow-up of 96 months, there was no statistically significant difference in DFS (hazard ratio 0.88; log-rank P = .642) or OS (stratified hazard ratio 1.16; log-rank P = .796) between patients who received ≤6 or ≥7 infusions. Rates of adverse events were increased in the patients who received ≥7 or ≤6 infusions (arthralgia, 20.1% vs 12.4%; nausea, 12.8% vs 7.3%; bone pain, 41.6% vs 34.9%). Modifications to adjuvant breast cancer regimens that can provide more ease for patients with less toxicity while maintaining efficacy are greatly desired to simultaneously support quality of life and disease outcomes.
Additional References
- Swain SM, Baselga J, Kim SB, et al; for the CLEOPATRA Study Group. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724-734. Doi: 10.1056/NEJMoa1413513
- Miles D, Ciruelos E, Schneeweiss A, et al; for the PERUSE investigators. Final results from the PERUSE study of first-line pertuzumab plus trastuzumab plus a taxane for HER2-positive locally recurrent or metastatic breast cancer, with a multivariable approach to guide prognostication. Ann Oncol. 2021;32:1245-1255. Doi: 10.1016/j.annonc.2021.06.024
- Hua X, Bi X-W, Zhao J-L, et al; for the South China Breast Cancer Group (SCBCG). Trastuzumab plus endocrine therapy or chemotherapy as first-line treatment for patients with hormone receptor-positive and HER2-positive metastatic breast cancer (SYSUCC-002). Clin Cancer Res. 2022;28:637-645. Doi: 10.1158/1078-0432.CCR-21-3435
- Kim H-A, Lee JW, Nam SJ, et al; for the Korean Breast Cancer Study Group. Adding ovarian suppression to tamoxifen for premenopausal breast Cancer: a randomized phase III trial. J Clin Oncol. 2020;38:434-443. Doi: 10.1200/JCO.19.00126
- Davies C, Pan H, Godwin J, et al; for the Adjuvant Tamoxifen: Longer Against Shorter (ATLAS) Collaborative Group. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. Doi: 10.1016/S0140-6736(12)61963-1
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet. 2015;386:1353-1361. Doi: 10.1016/S0140-6736(15)60908-4
Commentary: A New Drug, and Pediatric Concerns, February 2023
I love registries! With large numbers of participants, registries can be very helpful to identify rare side effects and to assess the efficacy and safety of medications in populations that may not be fully represented in clinical trials. I also love dupilumab; it was revolutionary in the management of patients with AD.
Vittrup and colleagues have created a registry of 347 participants treated with dupilumab. This does not yet have the large number of participants needed to identify new issues that wouldn't have been detected in clinical trials, but the study is informative about real-life use. The dramatic improvement in the Eczema Area and Severity Index (EASI) score is consistent with the high efficacy of dupilumab. The high rate of treatment persistence is also consistent with dupilumab being a very effective and safe treatment (because if the drug wasn't working well or was causing a severe problem, patients would probably stop the treatment). Though the study reported persistent head and neck involvement, the residual involvement may be quite minimal.
The EASI-75 and Investigator Global Assessment response rates reported in dupilumab trials underestimate the value of this drug. With a 2-year persistence rate of nearly 90%, it's clear that dupilumab is making a huge difference in the lives of patients with AD.
Fatigue is a fascinating issue in AD. We might wonder if all the inflammation in patients with AD would directly cause fatigue. Almost certainly all the itching in AD adversely affects sleep and would cause tremendous fatigue. It surprised me that most of the children in the study by Rangel and colleagues were reported as having no or mild fatigue; severe fatigue was very uncommon. It leaves me wondering whether the assessments of fatigue fully capture what's happening. Also, since the fatigue score was reported by the parents, I (as the parent of a child with AD) am wondering whether the parents were projecting, with the score more reflective of the parents' fatigue than with that of the child; alternatively, perhaps the child's hyperactivity leaves parents thinking there is no fatigue when there actually is (and possibly even causing the perceived hyperactivity).
The lack of a control group without AD is another major limitation in our ability to interpret the study findings. Is fatigue more common or less common in children with AD than in children without AD? I cannot tell from these findings. Does fatigue warrant, as the authors suggest, more attention in clinical practice? I don't know. If we are already treating our patients based on patients' global impressions of how they are doing — combined, of course, with our observations of their objective disease severity — I'm not sure how asking about fatigue would change anything, even if future studies were to definitively show that AD is associated with fatigue.
I hate new drugs (well, maybe not hate, but I worry about unknown long-term risks). Clinical trials that help a drug get approved can tell us a lot about a drug's efficacy, but these studies are generally limited in what they tell us about a drug's safety. Clinical trials are generally not powered enough (not enough participants and not followed for long enough) to be informative about rare risks. I love long-term studies of new drugs in large numbers of people because those studies can be very reassuring about the risks of medications. Studying nearly 10,000 patients for 5 years is quite reassuring, confirming my impression that dupilumab has a remarkable, excellent safety profile (Owji et al). Blocking interleukin 4 and interleukin 13 seems to be very specific to AD. Finding no association to cancer is what I would have expected; being able to share this information with patients is likely to be reassuring to them.
Oh, lord help me, another study that claims we should change our disease management because they've identified an increased risk for something. When you compare 70,000 patients with 270,000 controls, you have huge power to detect statistically significant associations of no clinical consequence. Let's assume for the moment that the detected association the authors found between AD and juvenile idiopathic arthritis (JIA) is real. The odds ratio is 2; the odds ratio for smoking causing cancer is on the order of 100.
In this study, over 99% of individuals in both AD and control groups did not have JIA. The difference between rates of JIA in patients with AD compared with controls was 0.3%! The authors conclude "it is important to inquire actively about symptoms not directly linked to the patients' skin disease"; based on the findings of this study, I would conclude that we don't need to worry about JIA in patients with AD even if there is a (marginally) higher prevalence of JIA in this group.
I love registries! With large numbers of participants, registries can be very helpful to identify rare side effects and to assess the efficacy and safety of medications in populations that may not be fully represented in clinical trials. I also love dupilumab; it was revolutionary in the management of patients with AD.
Vittrup and colleagues have created a registry of 347 participants treated with dupilumab. This does not yet have the large number of participants needed to identify new issues that wouldn't have been detected in clinical trials, but the study is informative about real-life use. The dramatic improvement in the Eczema Area and Severity Index (EASI) score is consistent with the high efficacy of dupilumab. The high rate of treatment persistence is also consistent with dupilumab being a very effective and safe treatment (because if the drug wasn't working well or was causing a severe problem, patients would probably stop the treatment). Though the study reported persistent head and neck involvement, the residual involvement may be quite minimal.
The EASI-75 and Investigator Global Assessment response rates reported in dupilumab trials underestimate the value of this drug. With a 2-year persistence rate of nearly 90%, it's clear that dupilumab is making a huge difference in the lives of patients with AD.
Fatigue is a fascinating issue in AD. We might wonder if all the inflammation in patients with AD would directly cause fatigue. Almost certainly all the itching in AD adversely affects sleep and would cause tremendous fatigue. It surprised me that most of the children in the study by Rangel and colleagues were reported as having no or mild fatigue; severe fatigue was very uncommon. It leaves me wondering whether the assessments of fatigue fully capture what's happening. Also, since the fatigue score was reported by the parents, I (as the parent of a child with AD) am wondering whether the parents were projecting, with the score more reflective of the parents' fatigue than with that of the child; alternatively, perhaps the child's hyperactivity leaves parents thinking there is no fatigue when there actually is (and possibly even causing the perceived hyperactivity).
The lack of a control group without AD is another major limitation in our ability to interpret the study findings. Is fatigue more common or less common in children with AD than in children without AD? I cannot tell from these findings. Does fatigue warrant, as the authors suggest, more attention in clinical practice? I don't know. If we are already treating our patients based on patients' global impressions of how they are doing — combined, of course, with our observations of their objective disease severity — I'm not sure how asking about fatigue would change anything, even if future studies were to definitively show that AD is associated with fatigue.
I hate new drugs (well, maybe not hate, but I worry about unknown long-term risks). Clinical trials that help a drug get approved can tell us a lot about a drug's efficacy, but these studies are generally limited in what they tell us about a drug's safety. Clinical trials are generally not powered enough (not enough participants and not followed for long enough) to be informative about rare risks. I love long-term studies of new drugs in large numbers of people because those studies can be very reassuring about the risks of medications. Studying nearly 10,000 patients for 5 years is quite reassuring, confirming my impression that dupilumab has a remarkable, excellent safety profile (Owji et al). Blocking interleukin 4 and interleukin 13 seems to be very specific to AD. Finding no association to cancer is what I would have expected; being able to share this information with patients is likely to be reassuring to them.
Oh, lord help me, another study that claims we should change our disease management because they've identified an increased risk for something. When you compare 70,000 patients with 270,000 controls, you have huge power to detect statistically significant associations of no clinical consequence. Let's assume for the moment that the detected association the authors found between AD and juvenile idiopathic arthritis (JIA) is real. The odds ratio is 2; the odds ratio for smoking causing cancer is on the order of 100.
In this study, over 99% of individuals in both AD and control groups did not have JIA. The difference between rates of JIA in patients with AD compared with controls was 0.3%! The authors conclude "it is important to inquire actively about symptoms not directly linked to the patients' skin disease"; based on the findings of this study, I would conclude that we don't need to worry about JIA in patients with AD even if there is a (marginally) higher prevalence of JIA in this group.
I love registries! With large numbers of participants, registries can be very helpful to identify rare side effects and to assess the efficacy and safety of medications in populations that may not be fully represented in clinical trials. I also love dupilumab; it was revolutionary in the management of patients with AD.
Vittrup and colleagues have created a registry of 347 participants treated with dupilumab. This does not yet have the large number of participants needed to identify new issues that wouldn't have been detected in clinical trials, but the study is informative about real-life use. The dramatic improvement in the Eczema Area and Severity Index (EASI) score is consistent with the high efficacy of dupilumab. The high rate of treatment persistence is also consistent with dupilumab being a very effective and safe treatment (because if the drug wasn't working well or was causing a severe problem, patients would probably stop the treatment). Though the study reported persistent head and neck involvement, the residual involvement may be quite minimal.
The EASI-75 and Investigator Global Assessment response rates reported in dupilumab trials underestimate the value of this drug. With a 2-year persistence rate of nearly 90%, it's clear that dupilumab is making a huge difference in the lives of patients with AD.
Fatigue is a fascinating issue in AD. We might wonder if all the inflammation in patients with AD would directly cause fatigue. Almost certainly all the itching in AD adversely affects sleep and would cause tremendous fatigue. It surprised me that most of the children in the study by Rangel and colleagues were reported as having no or mild fatigue; severe fatigue was very uncommon. It leaves me wondering whether the assessments of fatigue fully capture what's happening. Also, since the fatigue score was reported by the parents, I (as the parent of a child with AD) am wondering whether the parents were projecting, with the score more reflective of the parents' fatigue than with that of the child; alternatively, perhaps the child's hyperactivity leaves parents thinking there is no fatigue when there actually is (and possibly even causing the perceived hyperactivity).
The lack of a control group without AD is another major limitation in our ability to interpret the study findings. Is fatigue more common or less common in children with AD than in children without AD? I cannot tell from these findings. Does fatigue warrant, as the authors suggest, more attention in clinical practice? I don't know. If we are already treating our patients based on patients' global impressions of how they are doing — combined, of course, with our observations of their objective disease severity — I'm not sure how asking about fatigue would change anything, even if future studies were to definitively show that AD is associated with fatigue.
I hate new drugs (well, maybe not hate, but I worry about unknown long-term risks). Clinical trials that help a drug get approved can tell us a lot about a drug's efficacy, but these studies are generally limited in what they tell us about a drug's safety. Clinical trials are generally not powered enough (not enough participants and not followed for long enough) to be informative about rare risks. I love long-term studies of new drugs in large numbers of people because those studies can be very reassuring about the risks of medications. Studying nearly 10,000 patients for 5 years is quite reassuring, confirming my impression that dupilumab has a remarkable, excellent safety profile (Owji et al). Blocking interleukin 4 and interleukin 13 seems to be very specific to AD. Finding no association to cancer is what I would have expected; being able to share this information with patients is likely to be reassuring to them.
Oh, lord help me, another study that claims we should change our disease management because they've identified an increased risk for something. When you compare 70,000 patients with 270,000 controls, you have huge power to detect statistically significant associations of no clinical consequence. Let's assume for the moment that the detected association the authors found between AD and juvenile idiopathic arthritis (JIA) is real. The odds ratio is 2; the odds ratio for smoking causing cancer is on the order of 100.
In this study, over 99% of individuals in both AD and control groups did not have JIA. The difference between rates of JIA in patients with AD compared with controls was 0.3%! The authors conclude "it is important to inquire actively about symptoms not directly linked to the patients' skin disease"; based on the findings of this study, I would conclude that we don't need to worry about JIA in patients with AD even if there is a (marginally) higher prevalence of JIA in this group.
Infant with red eyelid lesion
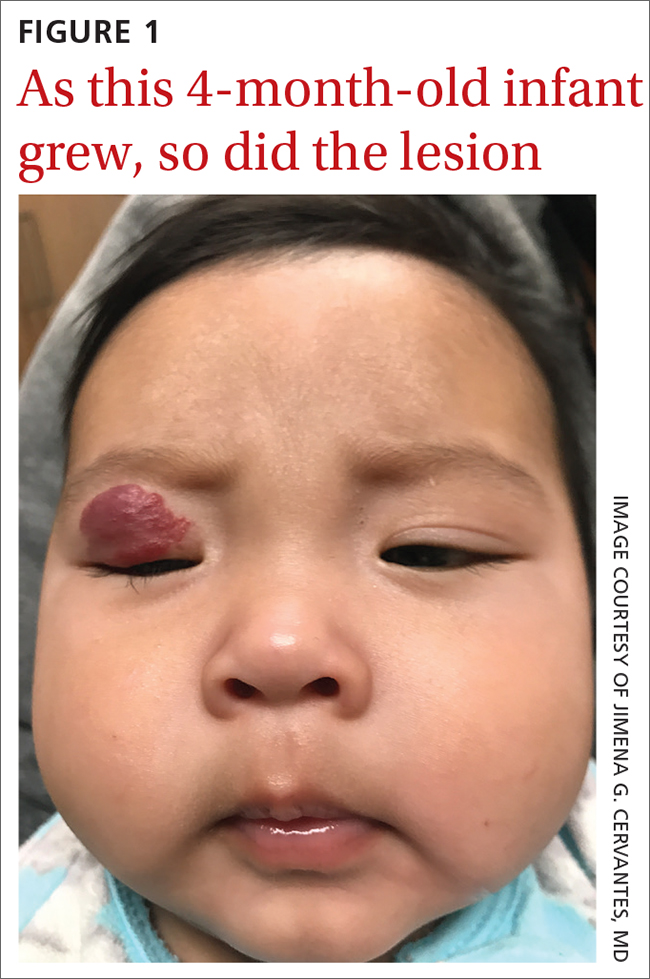
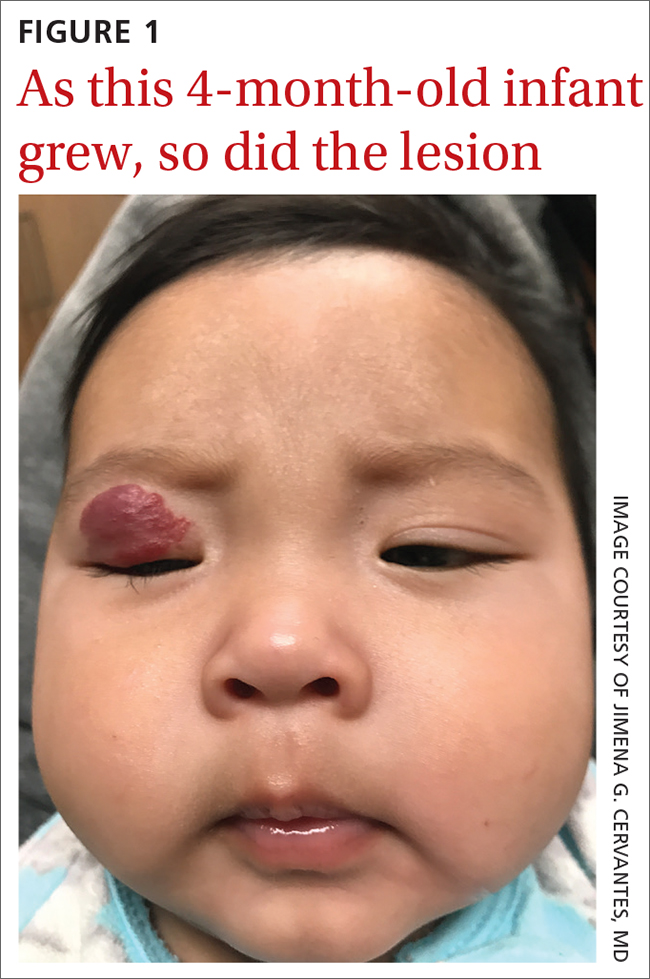
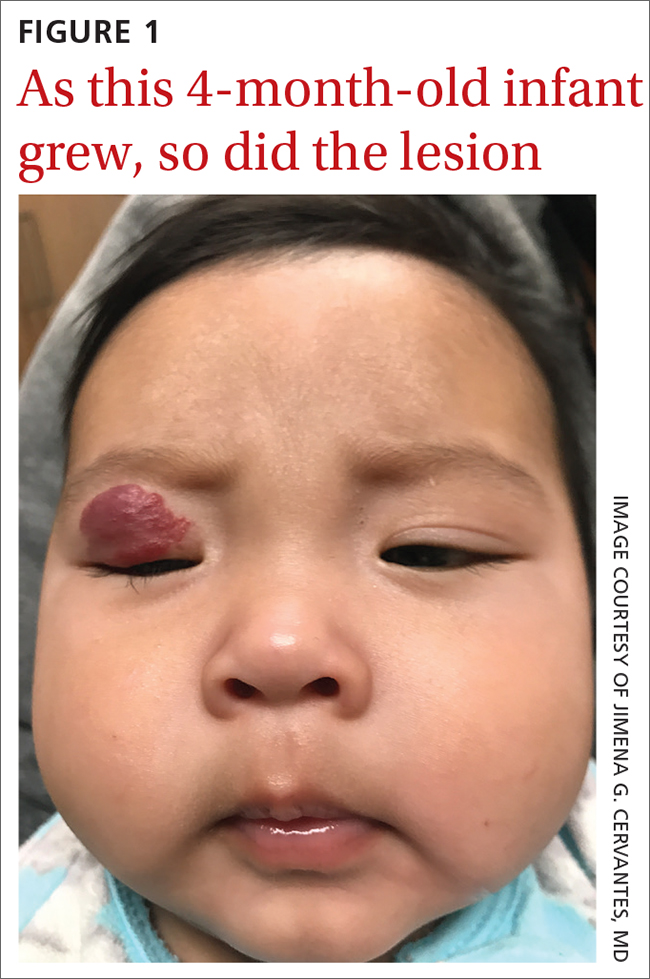
A 4-MONTH-OLD HISPANIC INFANT was brought to her pediatrician by her parents for evaluation of a dark red lesion over her right eyelid. The mother said that the lesion appeared when the child was 4 weeks old and started as a small red dot. As the baby grew, so did the red dot. The mother said the lesion appeared redder and darker when the baby got fussy and cried. The mother noted that some of the child’s eyelashes on the affected eyelid had fallen out. The infant was still able to use her eyes to follow the movements of her parents and siblings.
The mother denied any complications during pregnancy and delivered the child vaginally. No one else in the family had a similar lesion. When asked, the mother said that when her daughter was born, she was missing hair on her scalp and had dark spots on her lower backside. The mother had taken the baby to all wellness checks. The child was up to date on her vaccines, had no known drug allergies, and was otherwise healthy.
The pediatrician referred the baby to our skin clinic for further evaluation and treatment of the right eyelid lesion. Skin examination showed a 2.1-cm focal/localized, vascular, violaceous/dark red plaque over the right upper eyelid with an irregular border causing mild drooping of the right eyelid and some missing eyelashes (FIGURE 1). Multiple hyperpigmented patches on the upper and lower back were clinically consistent with Mongolian spots. Hair thinning was observed on the posterior and left posterior scalp.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infantile hemangioma
The diagnosis of an infantile hemangioma was made clinically, based on the lesion’s appearance and when it became noticeable (during the child’s first few weeks of life).
Infantile hemangiomas are the most common benign tumors of infancy, and the majority are not present at birth.1,2 Infantile periocular hemangioma, which our patient had, is typically unilateral and involves the upper eyelid.1 Infantile hemangiomas appear in the first few weeks of life with an area of pallor and later a faint red patch, which the mother first noted in our patient. Lesions grow rapidly in the first 3 to 6 months.2 Superficial lesions appear as bright red papules or patches that may have a flat or rough surface and are sharply demarcated, while deep lesions tend to be bluish and dome shaped.1,2
Infantile hemangiomas continue to grow until 9 to 12 months of age, at which time the growth rate slows to parallel the growth of the child. Involution typically begins by the time the child is 1 year old. Most infantile hemangiomas do not improve significantly after 3.5 years of age.3
Differential includes congenital hemangiomas, pyogenic granulomas
Clinical presentation, histology, and lesion evolution distinguish infantile hemangioma from other diagnoses, notably the following:
Congenital hemangiomas (CH) are fully formed vascular tumors present at birth; they occur less frequently than infantile hemangiomas. CHs are divided into 2 categories: rapidly involuting CHs and noninvoluting CHs.4
Continue to: Pyogenic granulomas
Pyogenic granulomas are usually small (< 1 cm), sessile or pedunculated red papules or nodules. They are friable, bleed easily, and grow rapidly.
Capillary malformations can manifest at birth as flat, red/purple, cutaneous patches with irregular borders that are painless and can spontaneously bleed; they can be found in any part of the body but mainly occur in the cervicofacial area.5 Capillary malformations are commonly known as stork bites on the nape of the neck or angel kisses if found on the forehead. Lateral lesions, known as port wine stains, persist and do not resolve without treatment.5
Tufted angioma and kaposiform hemangioendothelioma manifest as expanding ecchymotic firm masses with purpura and accompanying lymphedema.4 Magnetic resonance imaging, including magnetic resonance angiography, is recommended for management and treatment.4
Venous malformations can be noted at birth as a dark blue or purple discoloration and manifest as a deep mass.5 Venous malformations grow with the patient and have a rapid growth phase during puberty, pregnancy, or traumatic injury.5
Arteriovenous malformations (AVMs) may be present at birth as a slight blush hypervascular lesion. AVMs can be quiescent for many years and grow with the patient. AVMs have a palpable warmth, pulse, or thrill due to high vascular flow.5
Continue to: Individualize treatment when it's needed
Individualize treatment when it’s needed
The majority of infantile hemangiomas do not require treatment because they can resolve spontaneously over time.2 That said, children with periocular infantile hemangiomas may require treatment because the lesions may result in amblyopia and visual impairment if not properly treated.6 Treatment should be individualized, depending on the size, rate of growth, morphology, number, and location of the lesions; existing or potential complications; benefits and adverse events associated with the treatment; age of the patient; level of parental concern; and the physician’s comfort level with the various treatment options.
Predictive factors for ocular complications in patients with periocular infantile hemangiomas are diameter > 1 cm, a deep component, and upper eyelid involvement. Patients at risk for ocular complications should be promptly referred to an ophthalmologist, and treatment should be strongly considered.6 Currently, oral propranolol is the treatment of choice for high-risk and complicated infantile hemangiomas.2 This is a very safe treatment. Only rarely do the following adverse effects occur: bronchospasm, bradycardia, hypotension, nightmares, cold hands, and hypoglycemia. If these adverse effects do occur, they are reversible with discontinuation of propranolol. Hypoglycemia can be prevented by giving propranolol during or right after feeding.
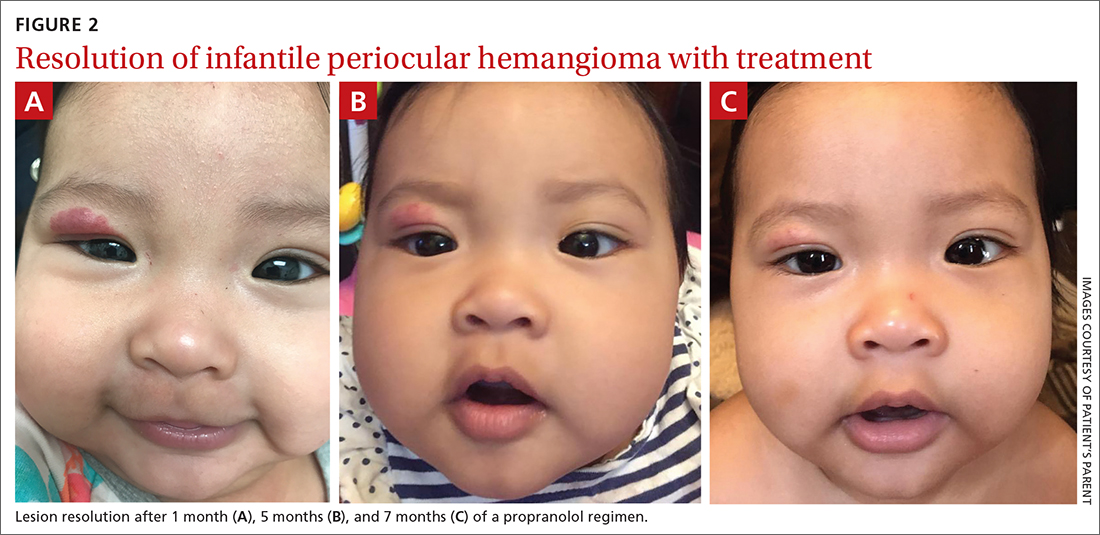
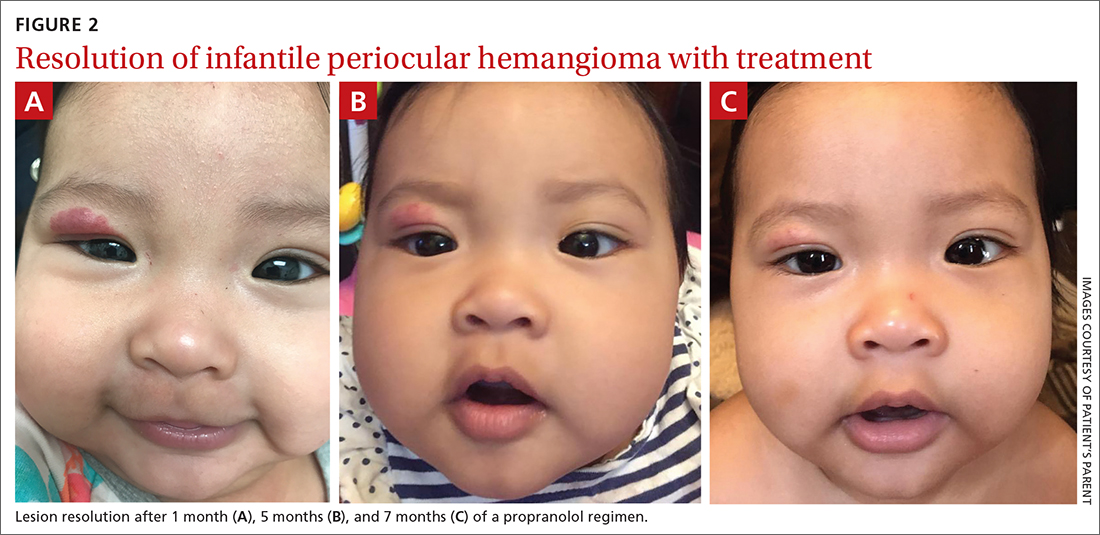
Our patient was started on propranolol 1 mg/kg/d for 1 month. The medication was administered by syringe for precise measurement. After the initial dose was tolerated, this was increased to 2 mg/kg/d for 1 month, then continued sequentially another month on 2.5 mg/kg/d, 2 months on 3 mg/kg/d, and finally 2 months on 3.4 mg/kg/d. All doses were divided twice per day between feedings.
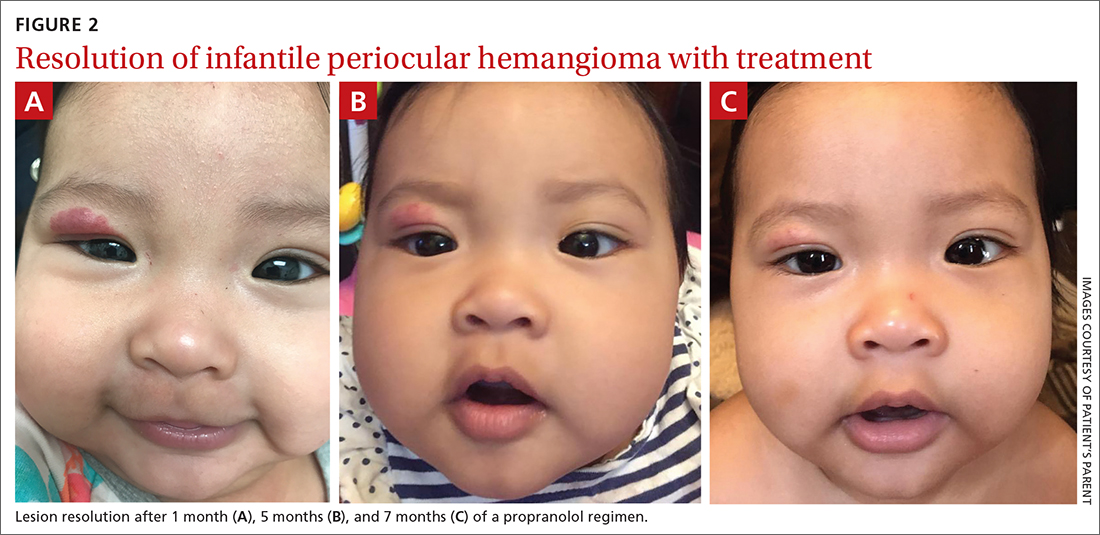
After 7 months of total treatment time (FIGURE 2), we began titrating down the patient’s dose over the next several months. After 3 months, treatment was stopped altogether. At the time treatment was completed, only a faint pink blush remained.
1. Tavakoli M, Yadegari S, Mosallaei M, et al. Infantile periocular hemangioma. J Ophthalmic Vis Res. 2017;12:205-211. doi: 10.4103/jovr.jovr_66_17
2. Leung AKC, Lam JM, Leong KF, et al. Infantile hemangioma: an updated review. Curr Pediatr Rev. 2021;17:55-69. doi: 10.2174/1573396316666200508100038
3. Couto RA, Maclellan RA, Zurakowski D, et al. Infantile hemangioma: clinical assessment of the involuting phase and implications for management. Plast Reconstr Surg. 2012;130:619-624. doi: 10.1097/PRS.0b013e31825dc129
4. Wildgruber M, Sadick M, Müller-Wille R, et al. Vascular tumors in infants and adolescents. Insights Imaging. 2019;10:30. doi: 10.1186/s13244-019-0718-6
5. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. 2012;2012:645678. doi: 10.1155/2012/645678
6. Samuelov L, Kinori M, Rychlik K, et al. Risk factors for ocular complications in periocular infantile hemangiomas. Pediatr Dermatol. 2018;35:458-462. doi: 10.1111/pde.13525
A 4-MONTH-OLD HISPANIC INFANT was brought to her pediatrician by her parents for evaluation of a dark red lesion over her right eyelid. The mother said that the lesion appeared when the child was 4 weeks old and started as a small red dot. As the baby grew, so did the red dot. The mother said the lesion appeared redder and darker when the baby got fussy and cried. The mother noted that some of the child’s eyelashes on the affected eyelid had fallen out. The infant was still able to use her eyes to follow the movements of her parents and siblings.
The mother denied any complications during pregnancy and delivered the child vaginally. No one else in the family had a similar lesion. When asked, the mother said that when her daughter was born, she was missing hair on her scalp and had dark spots on her lower backside. The mother had taken the baby to all wellness checks. The child was up to date on her vaccines, had no known drug allergies, and was otherwise healthy.
The pediatrician referred the baby to our skin clinic for further evaluation and treatment of the right eyelid lesion. Skin examination showed a 2.1-cm focal/localized, vascular, violaceous/dark red plaque over the right upper eyelid with an irregular border causing mild drooping of the right eyelid and some missing eyelashes (FIGURE 1). Multiple hyperpigmented patches on the upper and lower back were clinically consistent with Mongolian spots. Hair thinning was observed on the posterior and left posterior scalp.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infantile hemangioma
The diagnosis of an infantile hemangioma was made clinically, based on the lesion’s appearance and when it became noticeable (during the child’s first few weeks of life).
Infantile hemangiomas are the most common benign tumors of infancy, and the majority are not present at birth.1,2 Infantile periocular hemangioma, which our patient had, is typically unilateral and involves the upper eyelid.1 Infantile hemangiomas appear in the first few weeks of life with an area of pallor and later a faint red patch, which the mother first noted in our patient. Lesions grow rapidly in the first 3 to 6 months.2 Superficial lesions appear as bright red papules or patches that may have a flat or rough surface and are sharply demarcated, while deep lesions tend to be bluish and dome shaped.1,2
Infantile hemangiomas continue to grow until 9 to 12 months of age, at which time the growth rate slows to parallel the growth of the child. Involution typically begins by the time the child is 1 year old. Most infantile hemangiomas do not improve significantly after 3.5 years of age.3
Differential includes congenital hemangiomas, pyogenic granulomas
Clinical presentation, histology, and lesion evolution distinguish infantile hemangioma from other diagnoses, notably the following:
Congenital hemangiomas (CH) are fully formed vascular tumors present at birth; they occur less frequently than infantile hemangiomas. CHs are divided into 2 categories: rapidly involuting CHs and noninvoluting CHs.4
Continue to: Pyogenic granulomas
Pyogenic granulomas are usually small (< 1 cm), sessile or pedunculated red papules or nodules. They are friable, bleed easily, and grow rapidly.
Capillary malformations can manifest at birth as flat, red/purple, cutaneous patches with irregular borders that are painless and can spontaneously bleed; they can be found in any part of the body but mainly occur in the cervicofacial area.5 Capillary malformations are commonly known as stork bites on the nape of the neck or angel kisses if found on the forehead. Lateral lesions, known as port wine stains, persist and do not resolve without treatment.5
Tufted angioma and kaposiform hemangioendothelioma manifest as expanding ecchymotic firm masses with purpura and accompanying lymphedema.4 Magnetic resonance imaging, including magnetic resonance angiography, is recommended for management and treatment.4
Venous malformations can be noted at birth as a dark blue or purple discoloration and manifest as a deep mass.5 Venous malformations grow with the patient and have a rapid growth phase during puberty, pregnancy, or traumatic injury.5
Arteriovenous malformations (AVMs) may be present at birth as a slight blush hypervascular lesion. AVMs can be quiescent for many years and grow with the patient. AVMs have a palpable warmth, pulse, or thrill due to high vascular flow.5
Continue to: Individualize treatment when it's needed
Individualize treatment when it’s needed
The majority of infantile hemangiomas do not require treatment because they can resolve spontaneously over time.2 That said, children with periocular infantile hemangiomas may require treatment because the lesions may result in amblyopia and visual impairment if not properly treated.6 Treatment should be individualized, depending on the size, rate of growth, morphology, number, and location of the lesions; existing or potential complications; benefits and adverse events associated with the treatment; age of the patient; level of parental concern; and the physician’s comfort level with the various treatment options.
Predictive factors for ocular complications in patients with periocular infantile hemangiomas are diameter > 1 cm, a deep component, and upper eyelid involvement. Patients at risk for ocular complications should be promptly referred to an ophthalmologist, and treatment should be strongly considered.6 Currently, oral propranolol is the treatment of choice for high-risk and complicated infantile hemangiomas.2 This is a very safe treatment. Only rarely do the following adverse effects occur: bronchospasm, bradycardia, hypotension, nightmares, cold hands, and hypoglycemia. If these adverse effects do occur, they are reversible with discontinuation of propranolol. Hypoglycemia can be prevented by giving propranolol during or right after feeding.
Our patient was started on propranolol 1 mg/kg/d for 1 month. The medication was administered by syringe for precise measurement. After the initial dose was tolerated, this was increased to 2 mg/kg/d for 1 month, then continued sequentially another month on 2.5 mg/kg/d, 2 months on 3 mg/kg/d, and finally 2 months on 3.4 mg/kg/d. All doses were divided twice per day between feedings.
After 7 months of total treatment time (FIGURE 2), we began titrating down the patient’s dose over the next several months. After 3 months, treatment was stopped altogether. At the time treatment was completed, only a faint pink blush remained.
A 4-MONTH-OLD HISPANIC INFANT was brought to her pediatrician by her parents for evaluation of a dark red lesion over her right eyelid. The mother said that the lesion appeared when the child was 4 weeks old and started as a small red dot. As the baby grew, so did the red dot. The mother said the lesion appeared redder and darker when the baby got fussy and cried. The mother noted that some of the child’s eyelashes on the affected eyelid had fallen out. The infant was still able to use her eyes to follow the movements of her parents and siblings.
The mother denied any complications during pregnancy and delivered the child vaginally. No one else in the family had a similar lesion. When asked, the mother said that when her daughter was born, she was missing hair on her scalp and had dark spots on her lower backside. The mother had taken the baby to all wellness checks. The child was up to date on her vaccines, had no known drug allergies, and was otherwise healthy.
The pediatrician referred the baby to our skin clinic for further evaluation and treatment of the right eyelid lesion. Skin examination showed a 2.1-cm focal/localized, vascular, violaceous/dark red plaque over the right upper eyelid with an irregular border causing mild drooping of the right eyelid and some missing eyelashes (FIGURE 1). Multiple hyperpigmented patches on the upper and lower back were clinically consistent with Mongolian spots. Hair thinning was observed on the posterior and left posterior scalp.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infantile hemangioma
The diagnosis of an infantile hemangioma was made clinically, based on the lesion’s appearance and when it became noticeable (during the child’s first few weeks of life).
Infantile hemangiomas are the most common benign tumors of infancy, and the majority are not present at birth.1,2 Infantile periocular hemangioma, which our patient had, is typically unilateral and involves the upper eyelid.1 Infantile hemangiomas appear in the first few weeks of life with an area of pallor and later a faint red patch, which the mother first noted in our patient. Lesions grow rapidly in the first 3 to 6 months.2 Superficial lesions appear as bright red papules or patches that may have a flat or rough surface and are sharply demarcated, while deep lesions tend to be bluish and dome shaped.1,2
Infantile hemangiomas continue to grow until 9 to 12 months of age, at which time the growth rate slows to parallel the growth of the child. Involution typically begins by the time the child is 1 year old. Most infantile hemangiomas do not improve significantly after 3.5 years of age.3
Differential includes congenital hemangiomas, pyogenic granulomas
Clinical presentation, histology, and lesion evolution distinguish infantile hemangioma from other diagnoses, notably the following:
Congenital hemangiomas (CH) are fully formed vascular tumors present at birth; they occur less frequently than infantile hemangiomas. CHs are divided into 2 categories: rapidly involuting CHs and noninvoluting CHs.4
Continue to: Pyogenic granulomas
Pyogenic granulomas are usually small (< 1 cm), sessile or pedunculated red papules or nodules. They are friable, bleed easily, and grow rapidly.
Capillary malformations can manifest at birth as flat, red/purple, cutaneous patches with irregular borders that are painless and can spontaneously bleed; they can be found in any part of the body but mainly occur in the cervicofacial area.5 Capillary malformations are commonly known as stork bites on the nape of the neck or angel kisses if found on the forehead. Lateral lesions, known as port wine stains, persist and do not resolve without treatment.5
Tufted angioma and kaposiform hemangioendothelioma manifest as expanding ecchymotic firm masses with purpura and accompanying lymphedema.4 Magnetic resonance imaging, including magnetic resonance angiography, is recommended for management and treatment.4
Venous malformations can be noted at birth as a dark blue or purple discoloration and manifest as a deep mass.5 Venous malformations grow with the patient and have a rapid growth phase during puberty, pregnancy, or traumatic injury.5
Arteriovenous malformations (AVMs) may be present at birth as a slight blush hypervascular lesion. AVMs can be quiescent for many years and grow with the patient. AVMs have a palpable warmth, pulse, or thrill due to high vascular flow.5
Continue to: Individualize treatment when it's needed
Individualize treatment when it’s needed
The majority of infantile hemangiomas do not require treatment because they can resolve spontaneously over time.2 That said, children with periocular infantile hemangiomas may require treatment because the lesions may result in amblyopia and visual impairment if not properly treated.6 Treatment should be individualized, depending on the size, rate of growth, morphology, number, and location of the lesions; existing or potential complications; benefits and adverse events associated with the treatment; age of the patient; level of parental concern; and the physician’s comfort level with the various treatment options.
Predictive factors for ocular complications in patients with periocular infantile hemangiomas are diameter > 1 cm, a deep component, and upper eyelid involvement. Patients at risk for ocular complications should be promptly referred to an ophthalmologist, and treatment should be strongly considered.6 Currently, oral propranolol is the treatment of choice for high-risk and complicated infantile hemangiomas.2 This is a very safe treatment. Only rarely do the following adverse effects occur: bronchospasm, bradycardia, hypotension, nightmares, cold hands, and hypoglycemia. If these adverse effects do occur, they are reversible with discontinuation of propranolol. Hypoglycemia can be prevented by giving propranolol during or right after feeding.
Our patient was started on propranolol 1 mg/kg/d for 1 month. The medication was administered by syringe for precise measurement. After the initial dose was tolerated, this was increased to 2 mg/kg/d for 1 month, then continued sequentially another month on 2.5 mg/kg/d, 2 months on 3 mg/kg/d, and finally 2 months on 3.4 mg/kg/d. All doses were divided twice per day between feedings.
After 7 months of total treatment time (FIGURE 2), we began titrating down the patient’s dose over the next several months. After 3 months, treatment was stopped altogether. At the time treatment was completed, only a faint pink blush remained.
1. Tavakoli M, Yadegari S, Mosallaei M, et al. Infantile periocular hemangioma. J Ophthalmic Vis Res. 2017;12:205-211. doi: 10.4103/jovr.jovr_66_17
2. Leung AKC, Lam JM, Leong KF, et al. Infantile hemangioma: an updated review. Curr Pediatr Rev. 2021;17:55-69. doi: 10.2174/1573396316666200508100038
3. Couto RA, Maclellan RA, Zurakowski D, et al. Infantile hemangioma: clinical assessment of the involuting phase and implications for management. Plast Reconstr Surg. 2012;130:619-624. doi: 10.1097/PRS.0b013e31825dc129
4. Wildgruber M, Sadick M, Müller-Wille R, et al. Vascular tumors in infants and adolescents. Insights Imaging. 2019;10:30. doi: 10.1186/s13244-019-0718-6
5. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. 2012;2012:645678. doi: 10.1155/2012/645678
6. Samuelov L, Kinori M, Rychlik K, et al. Risk factors for ocular complications in periocular infantile hemangiomas. Pediatr Dermatol. 2018;35:458-462. doi: 10.1111/pde.13525
1. Tavakoli M, Yadegari S, Mosallaei M, et al. Infantile periocular hemangioma. J Ophthalmic Vis Res. 2017;12:205-211. doi: 10.4103/jovr.jovr_66_17
2. Leung AKC, Lam JM, Leong KF, et al. Infantile hemangioma: an updated review. Curr Pediatr Rev. 2021;17:55-69. doi: 10.2174/1573396316666200508100038
3. Couto RA, Maclellan RA, Zurakowski D, et al. Infantile hemangioma: clinical assessment of the involuting phase and implications for management. Plast Reconstr Surg. 2012;130:619-624. doi: 10.1097/PRS.0b013e31825dc129
4. Wildgruber M, Sadick M, Müller-Wille R, et al. Vascular tumors in infants and adolescents. Insights Imaging. 2019;10:30. doi: 10.1186/s13244-019-0718-6
5. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. 2012;2012:645678. doi: 10.1155/2012/645678
6. Samuelov L, Kinori M, Rychlik K, et al. Risk factors for ocular complications in periocular infantile hemangiomas. Pediatr Dermatol. 2018;35:458-462. doi: 10.1111/pde.13525
Metabolic syndromes worsen outcomes in BC patients treated with neoadjuvant chemotherapy
Key clinical point: The presence of metabolic syndromes (MetS) worsened survival outcomes and increased disease recurrence risk in patients with breast cancer (BC) who received neoadjuvant chemotherapy (NAC).
Major finding: The MetS group had a significantly lower likelihood of achieving pathological complete response than the non-MetS group (odds ratio [OR] 0.316; P = .028), with the risk for death (OR 2.587; P = .004) and disease recurrence (OR 2.228; P = .007) being significantly higher in patients with vs without MetS.
Study details: Findings are from a retrospective study including 221 women with BC who received preoperative NAC, of which 22.2% of patients were included in the MetS group.
Disclosures: This study was supported by the Beijing Medical Award Foundation. The authors declared no conflicts of interest.
Source: Zhou Z et al. Metabolic syndrome is a risk factor for breast cancer patients receiving neoadjuvant chemotherapy: A case-control study. Front Oncol. 2023;12:1080054 (Jan 4). Doi: 10.3389/fonc.2022.1080054
Key clinical point: The presence of metabolic syndromes (MetS) worsened survival outcomes and increased disease recurrence risk in patients with breast cancer (BC) who received neoadjuvant chemotherapy (NAC).
Major finding: The MetS group had a significantly lower likelihood of achieving pathological complete response than the non-MetS group (odds ratio [OR] 0.316; P = .028), with the risk for death (OR 2.587; P = .004) and disease recurrence (OR 2.228; P = .007) being significantly higher in patients with vs without MetS.
Study details: Findings are from a retrospective study including 221 women with BC who received preoperative NAC, of which 22.2% of patients were included in the MetS group.
Disclosures: This study was supported by the Beijing Medical Award Foundation. The authors declared no conflicts of interest.
Source: Zhou Z et al. Metabolic syndrome is a risk factor for breast cancer patients receiving neoadjuvant chemotherapy: A case-control study. Front Oncol. 2023;12:1080054 (Jan 4). Doi: 10.3389/fonc.2022.1080054
Key clinical point: The presence of metabolic syndromes (MetS) worsened survival outcomes and increased disease recurrence risk in patients with breast cancer (BC) who received neoadjuvant chemotherapy (NAC).
Major finding: The MetS group had a significantly lower likelihood of achieving pathological complete response than the non-MetS group (odds ratio [OR] 0.316; P = .028), with the risk for death (OR 2.587; P = .004) and disease recurrence (OR 2.228; P = .007) being significantly higher in patients with vs without MetS.
Study details: Findings are from a retrospective study including 221 women with BC who received preoperative NAC, of which 22.2% of patients were included in the MetS group.
Disclosures: This study was supported by the Beijing Medical Award Foundation. The authors declared no conflicts of interest.
Source: Zhou Z et al. Metabolic syndrome is a risk factor for breast cancer patients receiving neoadjuvant chemotherapy: A case-control study. Front Oncol. 2023;12:1080054 (Jan 4). Doi: 10.3389/fonc.2022.1080054
Metastatic BC: Not worth changing the 4-weekly schedule of pegylated liposomal doxorubicin
Key clinical point: Recent phase 2 trials have recommended a 2-weekly schedule of pegylated liposomal doxorubicin (PLD) in patients with heavily treated metastatic breast cancer (BC); however, it failed to demonstrate any advantage in terms of efficacy or safety over the registered 4-weekly regimen of PLD.
Major finding: The median progression-free survival was 3.0 and 3.4 months in the 2-weekly and 4-weekly PLD schedule groups, respectively, with a weighted hazard ratio of 1.12 (P = .54). The rate of adverse events also appeared comparable between both the groups.
Study details: Findings are from a retrospective study including 191 heavily pretreated patients with metastatic BC who received a 2-weekly (n = 95) or the registered 4-weekly (n = 96) schedule of PLD.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Bischoff H et al. A propensity score-weighted study comparing a two- versus four-weekly pegylated liposomal doxorubicin regimen in metastatic breast cancer. Breast Cancer Res Treat. 2022 (Dec 23). Doi: 10.1007/s10549-022-06844-5
Key clinical point: Recent phase 2 trials have recommended a 2-weekly schedule of pegylated liposomal doxorubicin (PLD) in patients with heavily treated metastatic breast cancer (BC); however, it failed to demonstrate any advantage in terms of efficacy or safety over the registered 4-weekly regimen of PLD.
Major finding: The median progression-free survival was 3.0 and 3.4 months in the 2-weekly and 4-weekly PLD schedule groups, respectively, with a weighted hazard ratio of 1.12 (P = .54). The rate of adverse events also appeared comparable between both the groups.
Study details: Findings are from a retrospective study including 191 heavily pretreated patients with metastatic BC who received a 2-weekly (n = 95) or the registered 4-weekly (n = 96) schedule of PLD.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Bischoff H et al. A propensity score-weighted study comparing a two- versus four-weekly pegylated liposomal doxorubicin regimen in metastatic breast cancer. Breast Cancer Res Treat. 2022 (Dec 23). Doi: 10.1007/s10549-022-06844-5
Key clinical point: Recent phase 2 trials have recommended a 2-weekly schedule of pegylated liposomal doxorubicin (PLD) in patients with heavily treated metastatic breast cancer (BC); however, it failed to demonstrate any advantage in terms of efficacy or safety over the registered 4-weekly regimen of PLD.
Major finding: The median progression-free survival was 3.0 and 3.4 months in the 2-weekly and 4-weekly PLD schedule groups, respectively, with a weighted hazard ratio of 1.12 (P = .54). The rate of adverse events also appeared comparable between both the groups.
Study details: Findings are from a retrospective study including 191 heavily pretreated patients with metastatic BC who received a 2-weekly (n = 95) or the registered 4-weekly (n = 96) schedule of PLD.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Bischoff H et al. A propensity score-weighted study comparing a two- versus four-weekly pegylated liposomal doxorubicin regimen in metastatic breast cancer. Breast Cancer Res Treat. 2022 (Dec 23). Doi: 10.1007/s10549-022-06844-5
Early autologous fat grafting associated with increased BC recurrence risk
Key clinical point: Autologous fat grafting (AFG) in the second stage of a 2-stage prosthetic breast reconstruction was linked to a higher risk for breast cancer (BC) recurrence when performed within a year after mastectomy.
Major finding: Patients who did vs did not undergo AFG within 1 year after the primary operation had a significantly increased risk for disease recurrence (hazard ratio 5.701; 95% CI 1.164-27.927). However, delaying the fat grafting beyond 12 months after mastectomy did not affect survival outcomes.
Study details: Findings are from a retrospective cohort study including 267 patients with unilateral invasive BC who underwent total mastectomy and immediate tissue-expander-based reconstruction, of which 203 patients underwent the second-stage operation within 12 months of mastectomy and 64 patients underwent the operation after 12 months of mastectomy.
Disclosures: This study did not report the source of funding. The authors declared no conflicts of interest.
Source: Lee KT et al. Association of fat graft with breast cancer recurrence in implant-based reconstruction: Does the timing matter? Ann Surg Oncol. 2022;30(2):1087-1097 (Dec 10). Doi: 10.1245/s10434-022-12389-0
Key clinical point: Autologous fat grafting (AFG) in the second stage of a 2-stage prosthetic breast reconstruction was linked to a higher risk for breast cancer (BC) recurrence when performed within a year after mastectomy.
Major finding: Patients who did vs did not undergo AFG within 1 year after the primary operation had a significantly increased risk for disease recurrence (hazard ratio 5.701; 95% CI 1.164-27.927). However, delaying the fat grafting beyond 12 months after mastectomy did not affect survival outcomes.
Study details: Findings are from a retrospective cohort study including 267 patients with unilateral invasive BC who underwent total mastectomy and immediate tissue-expander-based reconstruction, of which 203 patients underwent the second-stage operation within 12 months of mastectomy and 64 patients underwent the operation after 12 months of mastectomy.
Disclosures: This study did not report the source of funding. The authors declared no conflicts of interest.
Source: Lee KT et al. Association of fat graft with breast cancer recurrence in implant-based reconstruction: Does the timing matter? Ann Surg Oncol. 2022;30(2):1087-1097 (Dec 10). Doi: 10.1245/s10434-022-12389-0
Key clinical point: Autologous fat grafting (AFG) in the second stage of a 2-stage prosthetic breast reconstruction was linked to a higher risk for breast cancer (BC) recurrence when performed within a year after mastectomy.
Major finding: Patients who did vs did not undergo AFG within 1 year after the primary operation had a significantly increased risk for disease recurrence (hazard ratio 5.701; 95% CI 1.164-27.927). However, delaying the fat grafting beyond 12 months after mastectomy did not affect survival outcomes.
Study details: Findings are from a retrospective cohort study including 267 patients with unilateral invasive BC who underwent total mastectomy and immediate tissue-expander-based reconstruction, of which 203 patients underwent the second-stage operation within 12 months of mastectomy and 64 patients underwent the operation after 12 months of mastectomy.
Disclosures: This study did not report the source of funding. The authors declared no conflicts of interest.
Source: Lee KT et al. Association of fat graft with breast cancer recurrence in implant-based reconstruction: Does the timing matter? Ann Surg Oncol. 2022;30(2):1087-1097 (Dec 10). Doi: 10.1245/s10434-022-12389-0
Meta-analysis compares adjuvant chemotherapy regimens for resected early-stage TNBC
Key clinical point: In patients with early-stage triple-negative breast cancer (TNBC), adding capecitabine to classic anthracycline/taxane-based adjuvant chemotherapy improved overall survival (OS) and carboplatin/paclitaxel was the most effective regimen for improving disease-free survival (DFS).
Major finding: Adjuvant chemotherapy with anthracyclines/taxanes plus capecitabine vs anthracyclines significantly improved OS outcomes (hazard ratio [HR] 0.56; 95% CI 0.36-0.87; probability for ranking the first 29%), whereas carboplatin/paclitaxel vs anthracyclines was the best regimen for improving DFS outcomes (HR 0.51; 95% CI 0.30-0.86; probability for ranking the first 41%).
Study details: Findings are from a network meta-analysis of 27 randomized phase 3 trials that compared adjuvant chemotherapy regimens in patients with resected, stage I-III TNBC.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Petrelli F et al. Adjuvant chemotherapy for resected triple negative breast cancer patients: A network meta-analysis. Breast. 2022;67:8-13 (Dec 15). Doi: 10.1016/j.breast.2022.12.004
Key clinical point: In patients with early-stage triple-negative breast cancer (TNBC), adding capecitabine to classic anthracycline/taxane-based adjuvant chemotherapy improved overall survival (OS) and carboplatin/paclitaxel was the most effective regimen for improving disease-free survival (DFS).
Major finding: Adjuvant chemotherapy with anthracyclines/taxanes plus capecitabine vs anthracyclines significantly improved OS outcomes (hazard ratio [HR] 0.56; 95% CI 0.36-0.87; probability for ranking the first 29%), whereas carboplatin/paclitaxel vs anthracyclines was the best regimen for improving DFS outcomes (HR 0.51; 95% CI 0.30-0.86; probability for ranking the first 41%).
Study details: Findings are from a network meta-analysis of 27 randomized phase 3 trials that compared adjuvant chemotherapy regimens in patients with resected, stage I-III TNBC.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Petrelli F et al. Adjuvant chemotherapy for resected triple negative breast cancer patients: A network meta-analysis. Breast. 2022;67:8-13 (Dec 15). Doi: 10.1016/j.breast.2022.12.004
Key clinical point: In patients with early-stage triple-negative breast cancer (TNBC), adding capecitabine to classic anthracycline/taxane-based adjuvant chemotherapy improved overall survival (OS) and carboplatin/paclitaxel was the most effective regimen for improving disease-free survival (DFS).
Major finding: Adjuvant chemotherapy with anthracyclines/taxanes plus capecitabine vs anthracyclines significantly improved OS outcomes (hazard ratio [HR] 0.56; 95% CI 0.36-0.87; probability for ranking the first 29%), whereas carboplatin/paclitaxel vs anthracyclines was the best regimen for improving DFS outcomes (HR 0.51; 95% CI 0.30-0.86; probability for ranking the first 41%).
Study details: Findings are from a network meta-analysis of 27 randomized phase 3 trials that compared adjuvant chemotherapy regimens in patients with resected, stage I-III TNBC.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Petrelli F et al. Adjuvant chemotherapy for resected triple negative breast cancer patients: A network meta-analysis. Breast. 2022;67:8-13 (Dec 15). Doi: 10.1016/j.breast.2022.12.004
Overall survival improved with chemotherapy in ER-negative/HER2-negative, T1abN0 BC
Key clinical point: Treatment with adjuvant chemotherapy significantly improved overall survival (OS) outcomes in patients with estrogen receptor-negative (ER−)/human epidermal growth factor receptor 2-negative (HER2−), T1abN0 breast cancer (BC).
Major finding: After a median follow-up of 7.7 years, a significant improvement was observed in OS with vs without chemotherapy in the overall cohort of patients with T1abN0 BC (hazard ratio 0.35; P = .02), along with both subgroups of patients with T1a (log-rank P = .001) and T1b (P = .001) BC.
Study details: Findings are from a nationwide, retrospective cohort study including 296 patients with ER− /HER2−, T1abN0 BC, of which 79.4% of patients received adjuvant chemotherapy.
Disclosures: This study was supported by the Danish Cancer Society, Denmark, and other sources. Some authors declared receiving personal fees, speaker honorarium, or research grants from various sources.
Source: Hassing CMS et al. Adjuvant chemotherapy in patients with ER-negative/HER2-negative, T1abN0 breast cancer: A nationwide study. Breast Cancer Res Treat. 2022 (Dec 28). Doi: 10.1007/s10549-022-06839-2
Key clinical point: Treatment with adjuvant chemotherapy significantly improved overall survival (OS) outcomes in patients with estrogen receptor-negative (ER−)/human epidermal growth factor receptor 2-negative (HER2−), T1abN0 breast cancer (BC).
Major finding: After a median follow-up of 7.7 years, a significant improvement was observed in OS with vs without chemotherapy in the overall cohort of patients with T1abN0 BC (hazard ratio 0.35; P = .02), along with both subgroups of patients with T1a (log-rank P = .001) and T1b (P = .001) BC.
Study details: Findings are from a nationwide, retrospective cohort study including 296 patients with ER− /HER2−, T1abN0 BC, of which 79.4% of patients received adjuvant chemotherapy.
Disclosures: This study was supported by the Danish Cancer Society, Denmark, and other sources. Some authors declared receiving personal fees, speaker honorarium, or research grants from various sources.
Source: Hassing CMS et al. Adjuvant chemotherapy in patients with ER-negative/HER2-negative, T1abN0 breast cancer: A nationwide study. Breast Cancer Res Treat. 2022 (Dec 28). Doi: 10.1007/s10549-022-06839-2
Key clinical point: Treatment with adjuvant chemotherapy significantly improved overall survival (OS) outcomes in patients with estrogen receptor-negative (ER−)/human epidermal growth factor receptor 2-negative (HER2−), T1abN0 breast cancer (BC).
Major finding: After a median follow-up of 7.7 years, a significant improvement was observed in OS with vs without chemotherapy in the overall cohort of patients with T1abN0 BC (hazard ratio 0.35; P = .02), along with both subgroups of patients with T1a (log-rank P = .001) and T1b (P = .001) BC.
Study details: Findings are from a nationwide, retrospective cohort study including 296 patients with ER− /HER2−, T1abN0 BC, of which 79.4% of patients received adjuvant chemotherapy.
Disclosures: This study was supported by the Danish Cancer Society, Denmark, and other sources. Some authors declared receiving personal fees, speaker honorarium, or research grants from various sources.
Source: Hassing CMS et al. Adjuvant chemotherapy in patients with ER-negative/HER2-negative, T1abN0 breast cancer: A nationwide study. Breast Cancer Res Treat. 2022 (Dec 28). Doi: 10.1007/s10549-022-06839-2
ERBB2 mRNA expression predicts prognosis in trastuzumab emtansine-treated advanced HER2+ BC patients
Key clinical point: In patients with advanced human epidermal growth factor receptor 2-positive (HER2+ or ERBB2+) breast cancer (BC) treated with trastuzumab emtansine, the pre-established levels of ERBB2 mRNA expression according to the HER2DX standardized assay served as an important prognostic biomarker in predicting survival outcomes.
Major finding: High, medium, and low levels of ERBB2 mRNA expression were associated with overall response rates of 56%, 29%, and 0%, respectively, with high ERBB2 mRNA expression being associated with both better progression-free survival (P < .001) and overall survival (P = .007) outcomes.
Study details: Findings are from a study including 87 patients with HER2+ advanced BC who received treatment with trastuzumab emtansine.
Disclosures: This study was funded by Hospital Clinic, Dipartimento di Scienze Chirurgiche, Oncologiche e Gastroenterologiche, University of Padova, Italy, and other sources. The authors declared serving as consultants; receiving advisory, lecture, or consulting fees; or having other ties with several sources.
Source: Brasó-Maristany F et al. HER2DX ERBB2 mRNA expression in advanced HER2-positive breast cancer treated with T-DM1. J Natl Cancer Inst. 2022 (Dec 28). Doi: 10.1093/jnci/djac227
Key clinical point: In patients with advanced human epidermal growth factor receptor 2-positive (HER2+ or ERBB2+) breast cancer (BC) treated with trastuzumab emtansine, the pre-established levels of ERBB2 mRNA expression according to the HER2DX standardized assay served as an important prognostic biomarker in predicting survival outcomes.
Major finding: High, medium, and low levels of ERBB2 mRNA expression were associated with overall response rates of 56%, 29%, and 0%, respectively, with high ERBB2 mRNA expression being associated with both better progression-free survival (P < .001) and overall survival (P = .007) outcomes.
Study details: Findings are from a study including 87 patients with HER2+ advanced BC who received treatment with trastuzumab emtansine.
Disclosures: This study was funded by Hospital Clinic, Dipartimento di Scienze Chirurgiche, Oncologiche e Gastroenterologiche, University of Padova, Italy, and other sources. The authors declared serving as consultants; receiving advisory, lecture, or consulting fees; or having other ties with several sources.
Source: Brasó-Maristany F et al. HER2DX ERBB2 mRNA expression in advanced HER2-positive breast cancer treated with T-DM1. J Natl Cancer Inst. 2022 (Dec 28). Doi: 10.1093/jnci/djac227
Key clinical point: In patients with advanced human epidermal growth factor receptor 2-positive (HER2+ or ERBB2+) breast cancer (BC) treated with trastuzumab emtansine, the pre-established levels of ERBB2 mRNA expression according to the HER2DX standardized assay served as an important prognostic biomarker in predicting survival outcomes.
Major finding: High, medium, and low levels of ERBB2 mRNA expression were associated with overall response rates of 56%, 29%, and 0%, respectively, with high ERBB2 mRNA expression being associated with both better progression-free survival (P < .001) and overall survival (P = .007) outcomes.
Study details: Findings are from a study including 87 patients with HER2+ advanced BC who received treatment with trastuzumab emtansine.
Disclosures: This study was funded by Hospital Clinic, Dipartimento di Scienze Chirurgiche, Oncologiche e Gastroenterologiche, University of Padova, Italy, and other sources. The authors declared serving as consultants; receiving advisory, lecture, or consulting fees; or having other ties with several sources.
Source: Brasó-Maristany F et al. HER2DX ERBB2 mRNA expression in advanced HER2-positive breast cancer treated with T-DM1. J Natl Cancer Inst. 2022 (Dec 28). Doi: 10.1093/jnci/djac227


