User login
Official Newspaper of the American College of Surgeons
Opioid management protocol lowered trauma patient pain medication use
BALTIMORE – A pain management protocol implemented in a trauma service reduced opioid intake in trauma patients while improving patient satisfaction, according to a retrospective study.
The opioid epidemic continues to grow every day, partly as a result of irresponsible overprescribing of opioid medication, according to Jessica Gross, MB BAO BCh, FACS, a trauma surgeon from Wake Forest (N.C.) Baptist Health at the American Association for the Surgery of Trauma annual meeting. Dr. Gross and her colleagues developed a pain management protocol (PMP) to provide adequate pain control while using fewer opioids in the postdischarge setting. They tested their PMP through a retrospective chart review of 498 patients admitted to the trauma service between January 2015 and December 2016, half of which were admitted before the PMP was initiated and half of which were admitted afterward.
The PMP involved a stepped approach to treating pain, with acetaminophen or ibuprofen as needed for mild pain, one 5-mg tablet of oxycodone/acetaminophen every 6 hours for moderate pain, two tablets for severe pain, and 50-100 mg of tramadol every 6 hours for breakthrough pain.
Counseling services for patients who were found to be in danger of substance use were provided in the hospital, and at discharge, patients received a weaning plan for their medication, according to Dr. Gross.
If the short-acting medications were found to be inadequate to control pain, patients were given slow-release pain medication as needed.
Average total medication, including at discharge and for refills, prescribed after PMP initiation was 1,242 morphine milligram equivalents (MME), compared with 2,421 MME prior to the protocol (P less than .0001).
After the protocol was implemented, Dr. Gross and her colleagues found the number of patients prescribed a refill dropped from 39.7% to 28.1%, with the size of those refills dropping from 1,032 MME to 213 MME on average.
“By having a comprehensive pain management protocol, we can reduce the amount of pain medications we prescribe for outpatient use, from discharge from the trauma service,” said Dr. Gross. “Additionally, we have shown that by having a protocol in place, we not only decreased the number of refills we were providing, but also the amount of pain medications that was prescribed within these refills.”
Through a Press Ganey survey analysis of patients during the month before and the month after the PMP implementation, investigators found a significant increase in patient satisfaction and overall pain management, according to Dr. Gross,
In addition, the main trauma floor where the PMP was implemented was recognized for the most improvement in overall hospital rating and pain management, compared with the previous year.
Discussant Oscar Guillamondegui MD,FACS, medical director of the trauma ICU at Vanderbilt University, Nashville, Tenn., acknowledged the importance of PMPs and the work investigators presented.
“I would consider this the next generation of ERAS [enhanced recovery after surgery], or ERAT [enhanced recovery after trauma] in pain perception modification,” said Dr. Guillamondegui. “Dr. Gross and the multidisciplinary group at Wake Forest have provided compelling evidence to help alleviate [the opioid epidemic].”
In a question-and-answer session following the presentation, attendees voiced concern over how a PMP would be used among patients who are more familiar with hospital systems, in particular concerning self-reported pain levels.
“Most of us employed at acute care centers are not working in utopia. Many of our patients are heroin addicts, are very bright, and know how to identify 10 on those silly smiley faces so that they get more medicine,” said Charles Lucas, MD, FACS, professor of surgeon at Wayne State University, Detroit. Dr. Lucas also pointed out that even when patients report false levels of pain, doctors still are required to put it into the electronic medical record for fear of repercussions,
In response, Dr. Gross said doctors on the floor reviewed patients to make sure they were receiving all doses of pain medications. If doctors felt the patient’s pain regimen was adequate, despite the patient reporting otherwise, no changes were made.
Certain limitations include not being able to confirm whether patients received prescription medication elsewhere, nor any concrete data on patient satisfaction after discharge other than an inference based on fewer refills and lower refill MME.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
BALTIMORE – A pain management protocol implemented in a trauma service reduced opioid intake in trauma patients while improving patient satisfaction, according to a retrospective study.
The opioid epidemic continues to grow every day, partly as a result of irresponsible overprescribing of opioid medication, according to Jessica Gross, MB BAO BCh, FACS, a trauma surgeon from Wake Forest (N.C.) Baptist Health at the American Association for the Surgery of Trauma annual meeting. Dr. Gross and her colleagues developed a pain management protocol (PMP) to provide adequate pain control while using fewer opioids in the postdischarge setting. They tested their PMP through a retrospective chart review of 498 patients admitted to the trauma service between January 2015 and December 2016, half of which were admitted before the PMP was initiated and half of which were admitted afterward.
The PMP involved a stepped approach to treating pain, with acetaminophen or ibuprofen as needed for mild pain, one 5-mg tablet of oxycodone/acetaminophen every 6 hours for moderate pain, two tablets for severe pain, and 50-100 mg of tramadol every 6 hours for breakthrough pain.
Counseling services for patients who were found to be in danger of substance use were provided in the hospital, and at discharge, patients received a weaning plan for their medication, according to Dr. Gross.
If the short-acting medications were found to be inadequate to control pain, patients were given slow-release pain medication as needed.
Average total medication, including at discharge and for refills, prescribed after PMP initiation was 1,242 morphine milligram equivalents (MME), compared with 2,421 MME prior to the protocol (P less than .0001).
After the protocol was implemented, Dr. Gross and her colleagues found the number of patients prescribed a refill dropped from 39.7% to 28.1%, with the size of those refills dropping from 1,032 MME to 213 MME on average.
“By having a comprehensive pain management protocol, we can reduce the amount of pain medications we prescribe for outpatient use, from discharge from the trauma service,” said Dr. Gross. “Additionally, we have shown that by having a protocol in place, we not only decreased the number of refills we were providing, but also the amount of pain medications that was prescribed within these refills.”
Through a Press Ganey survey analysis of patients during the month before and the month after the PMP implementation, investigators found a significant increase in patient satisfaction and overall pain management, according to Dr. Gross,
In addition, the main trauma floor where the PMP was implemented was recognized for the most improvement in overall hospital rating and pain management, compared with the previous year.
Discussant Oscar Guillamondegui MD,FACS, medical director of the trauma ICU at Vanderbilt University, Nashville, Tenn., acknowledged the importance of PMPs and the work investigators presented.
“I would consider this the next generation of ERAS [enhanced recovery after surgery], or ERAT [enhanced recovery after trauma] in pain perception modification,” said Dr. Guillamondegui. “Dr. Gross and the multidisciplinary group at Wake Forest have provided compelling evidence to help alleviate [the opioid epidemic].”
In a question-and-answer session following the presentation, attendees voiced concern over how a PMP would be used among patients who are more familiar with hospital systems, in particular concerning self-reported pain levels.
“Most of us employed at acute care centers are not working in utopia. Many of our patients are heroin addicts, are very bright, and know how to identify 10 on those silly smiley faces so that they get more medicine,” said Charles Lucas, MD, FACS, professor of surgeon at Wayne State University, Detroit. Dr. Lucas also pointed out that even when patients report false levels of pain, doctors still are required to put it into the electronic medical record for fear of repercussions,
In response, Dr. Gross said doctors on the floor reviewed patients to make sure they were receiving all doses of pain medications. If doctors felt the patient’s pain regimen was adequate, despite the patient reporting otherwise, no changes were made.
Certain limitations include not being able to confirm whether patients received prescription medication elsewhere, nor any concrete data on patient satisfaction after discharge other than an inference based on fewer refills and lower refill MME.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
BALTIMORE – A pain management protocol implemented in a trauma service reduced opioid intake in trauma patients while improving patient satisfaction, according to a retrospective study.
The opioid epidemic continues to grow every day, partly as a result of irresponsible overprescribing of opioid medication, according to Jessica Gross, MB BAO BCh, FACS, a trauma surgeon from Wake Forest (N.C.) Baptist Health at the American Association for the Surgery of Trauma annual meeting. Dr. Gross and her colleagues developed a pain management protocol (PMP) to provide adequate pain control while using fewer opioids in the postdischarge setting. They tested their PMP through a retrospective chart review of 498 patients admitted to the trauma service between January 2015 and December 2016, half of which were admitted before the PMP was initiated and half of which were admitted afterward.
The PMP involved a stepped approach to treating pain, with acetaminophen or ibuprofen as needed for mild pain, one 5-mg tablet of oxycodone/acetaminophen every 6 hours for moderate pain, two tablets for severe pain, and 50-100 mg of tramadol every 6 hours for breakthrough pain.
Counseling services for patients who were found to be in danger of substance use were provided in the hospital, and at discharge, patients received a weaning plan for their medication, according to Dr. Gross.
If the short-acting medications were found to be inadequate to control pain, patients were given slow-release pain medication as needed.
Average total medication, including at discharge and for refills, prescribed after PMP initiation was 1,242 morphine milligram equivalents (MME), compared with 2,421 MME prior to the protocol (P less than .0001).
After the protocol was implemented, Dr. Gross and her colleagues found the number of patients prescribed a refill dropped from 39.7% to 28.1%, with the size of those refills dropping from 1,032 MME to 213 MME on average.
“By having a comprehensive pain management protocol, we can reduce the amount of pain medications we prescribe for outpatient use, from discharge from the trauma service,” said Dr. Gross. “Additionally, we have shown that by having a protocol in place, we not only decreased the number of refills we were providing, but also the amount of pain medications that was prescribed within these refills.”
Through a Press Ganey survey analysis of patients during the month before and the month after the PMP implementation, investigators found a significant increase in patient satisfaction and overall pain management, according to Dr. Gross,
In addition, the main trauma floor where the PMP was implemented was recognized for the most improvement in overall hospital rating and pain management, compared with the previous year.
Discussant Oscar Guillamondegui MD,FACS, medical director of the trauma ICU at Vanderbilt University, Nashville, Tenn., acknowledged the importance of PMPs and the work investigators presented.
“I would consider this the next generation of ERAS [enhanced recovery after surgery], or ERAT [enhanced recovery after trauma] in pain perception modification,” said Dr. Guillamondegui. “Dr. Gross and the multidisciplinary group at Wake Forest have provided compelling evidence to help alleviate [the opioid epidemic].”
In a question-and-answer session following the presentation, attendees voiced concern over how a PMP would be used among patients who are more familiar with hospital systems, in particular concerning self-reported pain levels.
“Most of us employed at acute care centers are not working in utopia. Many of our patients are heroin addicts, are very bright, and know how to identify 10 on those silly smiley faces so that they get more medicine,” said Charles Lucas, MD, FACS, professor of surgeon at Wayne State University, Detroit. Dr. Lucas also pointed out that even when patients report false levels of pain, doctors still are required to put it into the electronic medical record for fear of repercussions,
In response, Dr. Gross said doctors on the floor reviewed patients to make sure they were receiving all doses of pain medications. If doctors felt the patient’s pain regimen was adequate, despite the patient reporting otherwise, no changes were made.
Certain limitations include not being able to confirm whether patients received prescription medication elsewhere, nor any concrete data on patient satisfaction after discharge other than an inference based on fewer refills and lower refill MME.
Investigators reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
AT THE AAST ANNUAL MEETING
Key clinical point:
Major finding: Average prescription fell to 1,242 morphine milligram equivalents (MME) per prescription, compared with 2,421 MME per prescription prior to the protocol.
Data Source: Retrospective chart review of 498 trauma patients from Jan. 1, 2015, and Dec. 31, 2016.
Disclosures: Investigators reported no relevant financial disclosures.
Sen. Collins deals likely fatal blow to GOP’s health bill
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Consider adding chemotherapy after GI surgery
Adjuvant chemotherapy was associated with improved overall survival rates at 3 years in patients who had surgery for gastroesophageal cancer, based on retrospective data from more than 10,000 adults.
Preoperative chemoradiotherapy and resection has shown benefits in patients with gastroesophageal adenocarcinoma, but the potential benefits of adjuvant chemotherapy (AC) after surgery in these patients has not been well studied, wrote Ali A. El Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2805).
The researchers reviewed data from 10,086 patients in the National Cancer Database during 2006-2013. Of these, 814 (8%) received adjuvant chemotherapy after surgery and 9,272 (94%) received no additional intervention beyond postoperative observation. The average age of the patients was 61 years, and 88% were men.
The average survival rates at 3 years after surgery were 40 months for the adjuvant group and 34 months for the observation group (hazard ratio, 0.79). The overall survival rates in the adjuvant group were 94%, 54%, and 38% at 1,3, and 5 years, respectively, compared with rates of 88%, 47%, and 34%, in the observation group.
The findings were limited in part by the retrospective nature of the study, the researchers said. In addition, “the estimated effect of AC on overall survival is subject to selection bias and immortal time bias given that the study was observational,” they noted.
However, the results support the addition of chemotherapy for gastroesophageal surgery patients, and “provide compelling motivation to explore the potential benefit of adjuvant chemotherapy in a randomized clinical trial,” they said. “A two-arm phase 2 trial design using recurrence-free survival as a primary endpoint is an appealing first step,” they added.
The researchers had no financial conflicts to disclose.
The study findings “seem to indicate that additional systemic chemotherapy could be advantageous for patients treated with neoadjuvant chemoradiotherapy for resectable gastroesophageal cancer,” wrote David Cunningham, MD, FMedSci, and Elizabeth C. Smyth, MB, BCh., MSc., in an accompanying editorial.
“The small percentage of patients treated with adjuvant chemotherapy is reassuring; neoadjuvant chemoradiotherapy and surgery followed by adjuvant chemotherapy is not a treatment approach endorsed by current national or international guidelines,” they noted. The findings suggest that the 4% increase in overall survival at 3 years is promising because most gastroesophageal cancer recurrences arise within 3 years of surgery, they said. “However, these results require validation in the form of a randomized clinical trial,” they emphasized (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2792).
Dr. Cunningham and Ms. Smyth are affiliated with the department of gastrointestinal oncology and lymphoma at the Royal Marsden Hospital, London. Dr. Cunningham disclosed institutional research funding from Amgen, AstraZeneca, Bayer, Celgene, MedImmune, Merck Serono, Merrimack, and Sanofi. Ms. Smyth disclosed honoraria for advisory roles with Five Prime Therapeutics, Bristol-Myers Squibb, and Gritstone Oncology.
The study findings “seem to indicate that additional systemic chemotherapy could be advantageous for patients treated with neoadjuvant chemoradiotherapy for resectable gastroesophageal cancer,” wrote David Cunningham, MD, FMedSci, and Elizabeth C. Smyth, MB, BCh., MSc., in an accompanying editorial.
“The small percentage of patients treated with adjuvant chemotherapy is reassuring; neoadjuvant chemoradiotherapy and surgery followed by adjuvant chemotherapy is not a treatment approach endorsed by current national or international guidelines,” they noted. The findings suggest that the 4% increase in overall survival at 3 years is promising because most gastroesophageal cancer recurrences arise within 3 years of surgery, they said. “However, these results require validation in the form of a randomized clinical trial,” they emphasized (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2792).
Dr. Cunningham and Ms. Smyth are affiliated with the department of gastrointestinal oncology and lymphoma at the Royal Marsden Hospital, London. Dr. Cunningham disclosed institutional research funding from Amgen, AstraZeneca, Bayer, Celgene, MedImmune, Merck Serono, Merrimack, and Sanofi. Ms. Smyth disclosed honoraria for advisory roles with Five Prime Therapeutics, Bristol-Myers Squibb, and Gritstone Oncology.
The study findings “seem to indicate that additional systemic chemotherapy could be advantageous for patients treated with neoadjuvant chemoradiotherapy for resectable gastroesophageal cancer,” wrote David Cunningham, MD, FMedSci, and Elizabeth C. Smyth, MB, BCh., MSc., in an accompanying editorial.
“The small percentage of patients treated with adjuvant chemotherapy is reassuring; neoadjuvant chemoradiotherapy and surgery followed by adjuvant chemotherapy is not a treatment approach endorsed by current national or international guidelines,” they noted. The findings suggest that the 4% increase in overall survival at 3 years is promising because most gastroesophageal cancer recurrences arise within 3 years of surgery, they said. “However, these results require validation in the form of a randomized clinical trial,” they emphasized (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2792).
Dr. Cunningham and Ms. Smyth are affiliated with the department of gastrointestinal oncology and lymphoma at the Royal Marsden Hospital, London. Dr. Cunningham disclosed institutional research funding from Amgen, AstraZeneca, Bayer, Celgene, MedImmune, Merck Serono, Merrimack, and Sanofi. Ms. Smyth disclosed honoraria for advisory roles with Five Prime Therapeutics, Bristol-Myers Squibb, and Gritstone Oncology.
Adjuvant chemotherapy was associated with improved overall survival rates at 3 years in patients who had surgery for gastroesophageal cancer, based on retrospective data from more than 10,000 adults.
Preoperative chemoradiotherapy and resection has shown benefits in patients with gastroesophageal adenocarcinoma, but the potential benefits of adjuvant chemotherapy (AC) after surgery in these patients has not been well studied, wrote Ali A. El Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2805).
The researchers reviewed data from 10,086 patients in the National Cancer Database during 2006-2013. Of these, 814 (8%) received adjuvant chemotherapy after surgery and 9,272 (94%) received no additional intervention beyond postoperative observation. The average age of the patients was 61 years, and 88% were men.
The average survival rates at 3 years after surgery were 40 months for the adjuvant group and 34 months for the observation group (hazard ratio, 0.79). The overall survival rates in the adjuvant group were 94%, 54%, and 38% at 1,3, and 5 years, respectively, compared with rates of 88%, 47%, and 34%, in the observation group.
The findings were limited in part by the retrospective nature of the study, the researchers said. In addition, “the estimated effect of AC on overall survival is subject to selection bias and immortal time bias given that the study was observational,” they noted.
However, the results support the addition of chemotherapy for gastroesophageal surgery patients, and “provide compelling motivation to explore the potential benefit of adjuvant chemotherapy in a randomized clinical trial,” they said. “A two-arm phase 2 trial design using recurrence-free survival as a primary endpoint is an appealing first step,” they added.
The researchers had no financial conflicts to disclose.
Adjuvant chemotherapy was associated with improved overall survival rates at 3 years in patients who had surgery for gastroesophageal cancer, based on retrospective data from more than 10,000 adults.
Preoperative chemoradiotherapy and resection has shown benefits in patients with gastroesophageal adenocarcinoma, but the potential benefits of adjuvant chemotherapy (AC) after surgery in these patients has not been well studied, wrote Ali A. El Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (JAMA Oncol. 2017 Sep 21. doi: 10.1001/jamaoncol.2017.2805).
The researchers reviewed data from 10,086 patients in the National Cancer Database during 2006-2013. Of these, 814 (8%) received adjuvant chemotherapy after surgery and 9,272 (94%) received no additional intervention beyond postoperative observation. The average age of the patients was 61 years, and 88% were men.
The average survival rates at 3 years after surgery were 40 months for the adjuvant group and 34 months for the observation group (hazard ratio, 0.79). The overall survival rates in the adjuvant group were 94%, 54%, and 38% at 1,3, and 5 years, respectively, compared with rates of 88%, 47%, and 34%, in the observation group.
The findings were limited in part by the retrospective nature of the study, the researchers said. In addition, “the estimated effect of AC on overall survival is subject to selection bias and immortal time bias given that the study was observational,” they noted.
However, the results support the addition of chemotherapy for gastroesophageal surgery patients, and “provide compelling motivation to explore the potential benefit of adjuvant chemotherapy in a randomized clinical trial,” they said. “A two-arm phase 2 trial design using recurrence-free survival as a primary endpoint is an appealing first step,” they added.
The researchers had no financial conflicts to disclose.
FROM JAMA ONCOLOGY
Key clinical point: Patients undergoing surgery for gastroesophageal cancer may benefit from additional chemotherapy.
Major finding: Overall survival rates improved in patients who received adjuvant chemotherapy, compared with those who did not (40 months vs. 34 months, respectively).
Data source: A review of 10,086 adults in the National Cancer Database who underwent gastroesophageal cancer surgery during 2006-2013.
Disclosures: The researchers had no financial conflicts to disclose.
Battling physician burnout delivers monetary benefits for health care organizations
The financial impact of physician burnout can provide a guide to help organizations address the problem, according to a special communication published online in JAMA Internal Medicine.
Approximately half of U.S. physicians experience some degree of professional burnout, but health care organizations have done little to respond, wrote Tait Shanafelt, MD, of Stanford (Calif.) University, and colleagues (JAMA Intern Med. 2017 Sep 25. doi: 10.1001/jamainternmed.2017.4340).
The researchers cited “a lack of awareness regarding the economic costs of physician burnout” and a lack of confidence that anything can be done as key factors in why the organizational response to burnout has been so limited.
The business end of physician burnout includes the costs associated with physician turnover and decreased productivity, as well as “financial risks to the organization’s long-term viability due to the relationship between burnout and lower quality of care, decreased patient satisfaction, and problems with patient safety,” the researchers said.
Organizations can combat physician burnout, the authors noted, and the effort is financially worthwhile, as well as morally and ethically important. “Burnout is primarily a system-level problem driven by excess job demands and inadequate resources and support, not an individual problem triggered by personal limitations,” they wrote.
The researchers developed a model outlining “Typical Steps in an Organization’s Journey Toward Expertise in Physician Well-being.” The steps begin with strategies that have a minor impact, including awareness of the problem of physician burnout and a focus on individual interventions such as mindfulness training, exercise, and nutrition.
However, the “transformative” changes in an organization include developing a “culture of wellness,” strategic investment in physician well-being, the presence of a “chief well-being officer” at the executive level, and accountability for physician wellness shared among organizational leaders.
The cost of such strategies varies among institutions, and the researchers provided worksheets to calculate the organizational cost of burnout and the return on investment if intervention steps are taken.
For example, an organization employing 450 physicians could potentially spend $1 million per year on an intervention to reduce physician burnout from 50% to 40%. The intervention investment could yield organizational cost savings of $1.125 million per year, with a 12.5% return on investment, as well as the potential financial benefits of improved patient satisfaction and quality of care.
“Understanding the business case to reduce burnout and promote engagement, as well as overcoming the misperception that nothing meaningful can be done, are key steps for organizations to begin to take action,” the researchers concluded.
“Improvement is possible, investment is justified, and return on investment measurable,” they said.
Dr. Shanafelt is a coinventor of the Physician Well-Being Index, Medical Student Well-Being Index, and Well-Being Index; copyright and licensing rights for these tools belong to the Mayo Clinic, and Dr. Shanafelt receives part of the royalties. The researchers had no other financial conflicts to disclose.
The financial impact of physician burnout can provide a guide to help organizations address the problem, according to a special communication published online in JAMA Internal Medicine.
Approximately half of U.S. physicians experience some degree of professional burnout, but health care organizations have done little to respond, wrote Tait Shanafelt, MD, of Stanford (Calif.) University, and colleagues (JAMA Intern Med. 2017 Sep 25. doi: 10.1001/jamainternmed.2017.4340).
The researchers cited “a lack of awareness regarding the economic costs of physician burnout” and a lack of confidence that anything can be done as key factors in why the organizational response to burnout has been so limited.
The business end of physician burnout includes the costs associated with physician turnover and decreased productivity, as well as “financial risks to the organization’s long-term viability due to the relationship between burnout and lower quality of care, decreased patient satisfaction, and problems with patient safety,” the researchers said.
Organizations can combat physician burnout, the authors noted, and the effort is financially worthwhile, as well as morally and ethically important. “Burnout is primarily a system-level problem driven by excess job demands and inadequate resources and support, not an individual problem triggered by personal limitations,” they wrote.
The researchers developed a model outlining “Typical Steps in an Organization’s Journey Toward Expertise in Physician Well-being.” The steps begin with strategies that have a minor impact, including awareness of the problem of physician burnout and a focus on individual interventions such as mindfulness training, exercise, and nutrition.
However, the “transformative” changes in an organization include developing a “culture of wellness,” strategic investment in physician well-being, the presence of a “chief well-being officer” at the executive level, and accountability for physician wellness shared among organizational leaders.
The cost of such strategies varies among institutions, and the researchers provided worksheets to calculate the organizational cost of burnout and the return on investment if intervention steps are taken.
For example, an organization employing 450 physicians could potentially spend $1 million per year on an intervention to reduce physician burnout from 50% to 40%. The intervention investment could yield organizational cost savings of $1.125 million per year, with a 12.5% return on investment, as well as the potential financial benefits of improved patient satisfaction and quality of care.
“Understanding the business case to reduce burnout and promote engagement, as well as overcoming the misperception that nothing meaningful can be done, are key steps for organizations to begin to take action,” the researchers concluded.
“Improvement is possible, investment is justified, and return on investment measurable,” they said.
Dr. Shanafelt is a coinventor of the Physician Well-Being Index, Medical Student Well-Being Index, and Well-Being Index; copyright and licensing rights for these tools belong to the Mayo Clinic, and Dr. Shanafelt receives part of the royalties. The researchers had no other financial conflicts to disclose.
The financial impact of physician burnout can provide a guide to help organizations address the problem, according to a special communication published online in JAMA Internal Medicine.
Approximately half of U.S. physicians experience some degree of professional burnout, but health care organizations have done little to respond, wrote Tait Shanafelt, MD, of Stanford (Calif.) University, and colleagues (JAMA Intern Med. 2017 Sep 25. doi: 10.1001/jamainternmed.2017.4340).
The researchers cited “a lack of awareness regarding the economic costs of physician burnout” and a lack of confidence that anything can be done as key factors in why the organizational response to burnout has been so limited.
The business end of physician burnout includes the costs associated with physician turnover and decreased productivity, as well as “financial risks to the organization’s long-term viability due to the relationship between burnout and lower quality of care, decreased patient satisfaction, and problems with patient safety,” the researchers said.
Organizations can combat physician burnout, the authors noted, and the effort is financially worthwhile, as well as morally and ethically important. “Burnout is primarily a system-level problem driven by excess job demands and inadequate resources and support, not an individual problem triggered by personal limitations,” they wrote.
The researchers developed a model outlining “Typical Steps in an Organization’s Journey Toward Expertise in Physician Well-being.” The steps begin with strategies that have a minor impact, including awareness of the problem of physician burnout and a focus on individual interventions such as mindfulness training, exercise, and nutrition.
However, the “transformative” changes in an organization include developing a “culture of wellness,” strategic investment in physician well-being, the presence of a “chief well-being officer” at the executive level, and accountability for physician wellness shared among organizational leaders.
The cost of such strategies varies among institutions, and the researchers provided worksheets to calculate the organizational cost of burnout and the return on investment if intervention steps are taken.
For example, an organization employing 450 physicians could potentially spend $1 million per year on an intervention to reduce physician burnout from 50% to 40%. The intervention investment could yield organizational cost savings of $1.125 million per year, with a 12.5% return on investment, as well as the potential financial benefits of improved patient satisfaction and quality of care.
“Understanding the business case to reduce burnout and promote engagement, as well as overcoming the misperception that nothing meaningful can be done, are key steps for organizations to begin to take action,” the researchers concluded.
“Improvement is possible, investment is justified, and return on investment measurable,” they said.
Dr. Shanafelt is a coinventor of the Physician Well-Being Index, Medical Student Well-Being Index, and Well-Being Index; copyright and licensing rights for these tools belong to the Mayo Clinic, and Dr. Shanafelt receives part of the royalties. The researchers had no other financial conflicts to disclose.
FROM JAMA INTERNAL MEDICINE
‘Very daring study’ of neoadjuvant AI/CDKi combo in early BC is hypothesis generating
MADRID – For women with luminal breast cancer who are not initially candidates for breast-conserving surgery, neoadjuvant therapy with an aromatase inhibitor and a cyclin-dependent kinases 4/6 (CDK4/6) inhibitor offered a slightly higher residual cancer burden prior to surgery, but a significantly better safety profile than conventional chemotherapy with similar near-term safety outcomes, results of a phase 2 parallel group, noncomparative trial suggested.
Among 60 patients evaluable for response in an interim analysis of the UNICANCER NeoPAL trial, one patient (3.3%) treated with a combination of letrozole (Femara) and palbociclib (Ibrance) had a residual cancer burden (RCB) score of 0 (equivalent to a pathologic complete response; pCR), whereas three patients (10%) treated with FEC 100 chemotherapy (5-fluorouracil, epirubicin, and cyclophosphamide) had RCB 0 or I, reported Paul-Henri Cottu, MD, of the Institut Curie in Paris.
Following the interim analysis, the independent data monitoring committee for the NeoPAL trial recommended halting accrual; accrual was stopped in November 2016, after 106 patients had been randomized.
The IDMC also recommended that patients in the letrozole/palbociclib arm who did not have an RCB of 0 or I be offered adjuvant chemotherapy.
“Please note that 70% of those patients refused adjuvant chemotherapy,” Dr. Cottu said.
The investigators set out to test whether letrozole and palbociclib, which have been shown to have synergistic antiproliferative activity against advanced luminal breast cancer, could have similar benefits in the neoadjuvant setting.
They screened for women with luminal breast cancer who had newly diagnosed stage II or III breast cancer with biopsy-proven endocrine receptor–positive, human epidermal growth factor receptor 2–negative tumors, using the Prosigna test, based on the PAM50 gene signature assay. Women with node-positive luminal A or luminal B disease were enrolled and randomized to receive either letrozole 2.5 mg and palbociclib 125 mg daily for 3 out of every 4 weeks over 19 weeks, or three cycles of FEC 100, followed by three cycles of docetaxel 100 mg/m2 every 3 weeks, followed by surgery.
An interim analysis was planned after 30 patients were evaluable for RCB in the experimental arm, and, as prespecified, the trial was stopped for futility when fewer than five patients had an RCB of 0 or I.
The safety analysis, conducted with all 106 patients randomized, showed that letrozole/palbocilib was associated with more frequent grade 3 neutropenia (23% vs. 10% of patients with FEC), but less grade 4 neutropenia (1% vs. 11%, respectively), and no febrile neutropenia vs. 6% in the chemotherapy arm.
There were 2 serious adverse events with the AI/CDK-inhibitor combination vs. 17 with chemotherapy. Dose reductions or interruptions were less frequent with letrozole/palbociclib (10 and 16), and only two patients in the experimental arm required premature cessation of therapy vs. seven in the chemotherapy arm.
The final response analysis in 103 patients showed that the rate of RCB 0 or I was 7.7% with letrozole/palbociclib and 15.7% with chemotherapy. Respective rates of RCB II-III were 92.3% and 84.3%.
Clinical response rates were similar in each study arm, with approximately 30% complete responses and 44% partial responses.
In each arm, slightly less than one-third of patients underwent mastectomy, and a little more than two-thirds were able to have breast-conserving surgery after neoadjuvant therapy.
The patients will be followed out to at least 3 years to see whether those patients in the letrozole/palbociclib arm who turned down subsequent chemotherapy will have worse survival than patients who decided to undergo it, Dr. Cottu said.
Invited discussant Nadia Harbeck, MD, PhD, of the University of Munich called the NeoPAL trial “a very daring study.”
“This is not a practice-changing trial, but it’s a very, very interesting hypothesis-generating trial,” she said.
She said that the choice of RCB was probably not the best endpoint in a trial of endocrine-based therapy vs. chemotherapy.
“I think the challenge remains to identify those patients with luminal early breast cancer for whom an endocrine-based approach – not endocrine, but endocrine-based – will improve outcome, either replacing chemotherapy in the intermediate-risk setting or as an add-on in high-risk disease,” she said.
The study was funded by Pfizer and Nanostring. Dr. Cottu disclosed advisory board participation and travel support from Pfizer and others, and research support from Roche, Novartis, and AstraZeneca. Dr. Harbeck disclosed advising and consulting fees from Pfizer, Nanostring, and other companies.
MADRID – For women with luminal breast cancer who are not initially candidates for breast-conserving surgery, neoadjuvant therapy with an aromatase inhibitor and a cyclin-dependent kinases 4/6 (CDK4/6) inhibitor offered a slightly higher residual cancer burden prior to surgery, but a significantly better safety profile than conventional chemotherapy with similar near-term safety outcomes, results of a phase 2 parallel group, noncomparative trial suggested.
Among 60 patients evaluable for response in an interim analysis of the UNICANCER NeoPAL trial, one patient (3.3%) treated with a combination of letrozole (Femara) and palbociclib (Ibrance) had a residual cancer burden (RCB) score of 0 (equivalent to a pathologic complete response; pCR), whereas three patients (10%) treated with FEC 100 chemotherapy (5-fluorouracil, epirubicin, and cyclophosphamide) had RCB 0 or I, reported Paul-Henri Cottu, MD, of the Institut Curie in Paris.
Following the interim analysis, the independent data monitoring committee for the NeoPAL trial recommended halting accrual; accrual was stopped in November 2016, after 106 patients had been randomized.
The IDMC also recommended that patients in the letrozole/palbociclib arm who did not have an RCB of 0 or I be offered adjuvant chemotherapy.
“Please note that 70% of those patients refused adjuvant chemotherapy,” Dr. Cottu said.
The investigators set out to test whether letrozole and palbociclib, which have been shown to have synergistic antiproliferative activity against advanced luminal breast cancer, could have similar benefits in the neoadjuvant setting.
They screened for women with luminal breast cancer who had newly diagnosed stage II or III breast cancer with biopsy-proven endocrine receptor–positive, human epidermal growth factor receptor 2–negative tumors, using the Prosigna test, based on the PAM50 gene signature assay. Women with node-positive luminal A or luminal B disease were enrolled and randomized to receive either letrozole 2.5 mg and palbociclib 125 mg daily for 3 out of every 4 weeks over 19 weeks, or three cycles of FEC 100, followed by three cycles of docetaxel 100 mg/m2 every 3 weeks, followed by surgery.
An interim analysis was planned after 30 patients were evaluable for RCB in the experimental arm, and, as prespecified, the trial was stopped for futility when fewer than five patients had an RCB of 0 or I.
The safety analysis, conducted with all 106 patients randomized, showed that letrozole/palbocilib was associated with more frequent grade 3 neutropenia (23% vs. 10% of patients with FEC), but less grade 4 neutropenia (1% vs. 11%, respectively), and no febrile neutropenia vs. 6% in the chemotherapy arm.
There were 2 serious adverse events with the AI/CDK-inhibitor combination vs. 17 with chemotherapy. Dose reductions or interruptions were less frequent with letrozole/palbociclib (10 and 16), and only two patients in the experimental arm required premature cessation of therapy vs. seven in the chemotherapy arm.
The final response analysis in 103 patients showed that the rate of RCB 0 or I was 7.7% with letrozole/palbociclib and 15.7% with chemotherapy. Respective rates of RCB II-III were 92.3% and 84.3%.
Clinical response rates were similar in each study arm, with approximately 30% complete responses and 44% partial responses.
In each arm, slightly less than one-third of patients underwent mastectomy, and a little more than two-thirds were able to have breast-conserving surgery after neoadjuvant therapy.
The patients will be followed out to at least 3 years to see whether those patients in the letrozole/palbociclib arm who turned down subsequent chemotherapy will have worse survival than patients who decided to undergo it, Dr. Cottu said.
Invited discussant Nadia Harbeck, MD, PhD, of the University of Munich called the NeoPAL trial “a very daring study.”
“This is not a practice-changing trial, but it’s a very, very interesting hypothesis-generating trial,” she said.
She said that the choice of RCB was probably not the best endpoint in a trial of endocrine-based therapy vs. chemotherapy.
“I think the challenge remains to identify those patients with luminal early breast cancer for whom an endocrine-based approach – not endocrine, but endocrine-based – will improve outcome, either replacing chemotherapy in the intermediate-risk setting or as an add-on in high-risk disease,” she said.
The study was funded by Pfizer and Nanostring. Dr. Cottu disclosed advisory board participation and travel support from Pfizer and others, and research support from Roche, Novartis, and AstraZeneca. Dr. Harbeck disclosed advising and consulting fees from Pfizer, Nanostring, and other companies.
MADRID – For women with luminal breast cancer who are not initially candidates for breast-conserving surgery, neoadjuvant therapy with an aromatase inhibitor and a cyclin-dependent kinases 4/6 (CDK4/6) inhibitor offered a slightly higher residual cancer burden prior to surgery, but a significantly better safety profile than conventional chemotherapy with similar near-term safety outcomes, results of a phase 2 parallel group, noncomparative trial suggested.
Among 60 patients evaluable for response in an interim analysis of the UNICANCER NeoPAL trial, one patient (3.3%) treated with a combination of letrozole (Femara) and palbociclib (Ibrance) had a residual cancer burden (RCB) score of 0 (equivalent to a pathologic complete response; pCR), whereas three patients (10%) treated with FEC 100 chemotherapy (5-fluorouracil, epirubicin, and cyclophosphamide) had RCB 0 or I, reported Paul-Henri Cottu, MD, of the Institut Curie in Paris.
Following the interim analysis, the independent data monitoring committee for the NeoPAL trial recommended halting accrual; accrual was stopped in November 2016, after 106 patients had been randomized.
The IDMC also recommended that patients in the letrozole/palbociclib arm who did not have an RCB of 0 or I be offered adjuvant chemotherapy.
“Please note that 70% of those patients refused adjuvant chemotherapy,” Dr. Cottu said.
The investigators set out to test whether letrozole and palbociclib, which have been shown to have synergistic antiproliferative activity against advanced luminal breast cancer, could have similar benefits in the neoadjuvant setting.
They screened for women with luminal breast cancer who had newly diagnosed stage II or III breast cancer with biopsy-proven endocrine receptor–positive, human epidermal growth factor receptor 2–negative tumors, using the Prosigna test, based on the PAM50 gene signature assay. Women with node-positive luminal A or luminal B disease were enrolled and randomized to receive either letrozole 2.5 mg and palbociclib 125 mg daily for 3 out of every 4 weeks over 19 weeks, or three cycles of FEC 100, followed by three cycles of docetaxel 100 mg/m2 every 3 weeks, followed by surgery.
An interim analysis was planned after 30 patients were evaluable for RCB in the experimental arm, and, as prespecified, the trial was stopped for futility when fewer than five patients had an RCB of 0 or I.
The safety analysis, conducted with all 106 patients randomized, showed that letrozole/palbocilib was associated with more frequent grade 3 neutropenia (23% vs. 10% of patients with FEC), but less grade 4 neutropenia (1% vs. 11%, respectively), and no febrile neutropenia vs. 6% in the chemotherapy arm.
There were 2 serious adverse events with the AI/CDK-inhibitor combination vs. 17 with chemotherapy. Dose reductions or interruptions were less frequent with letrozole/palbociclib (10 and 16), and only two patients in the experimental arm required premature cessation of therapy vs. seven in the chemotherapy arm.
The final response analysis in 103 patients showed that the rate of RCB 0 or I was 7.7% with letrozole/palbociclib and 15.7% with chemotherapy. Respective rates of RCB II-III were 92.3% and 84.3%.
Clinical response rates were similar in each study arm, with approximately 30% complete responses and 44% partial responses.
In each arm, slightly less than one-third of patients underwent mastectomy, and a little more than two-thirds were able to have breast-conserving surgery after neoadjuvant therapy.
The patients will be followed out to at least 3 years to see whether those patients in the letrozole/palbociclib arm who turned down subsequent chemotherapy will have worse survival than patients who decided to undergo it, Dr. Cottu said.
Invited discussant Nadia Harbeck, MD, PhD, of the University of Munich called the NeoPAL trial “a very daring study.”
“This is not a practice-changing trial, but it’s a very, very interesting hypothesis-generating trial,” she said.
She said that the choice of RCB was probably not the best endpoint in a trial of endocrine-based therapy vs. chemotherapy.
“I think the challenge remains to identify those patients with luminal early breast cancer for whom an endocrine-based approach – not endocrine, but endocrine-based – will improve outcome, either replacing chemotherapy in the intermediate-risk setting or as an add-on in high-risk disease,” she said.
The study was funded by Pfizer and Nanostring. Dr. Cottu disclosed advisory board participation and travel support from Pfizer and others, and research support from Roche, Novartis, and AstraZeneca. Dr. Harbeck disclosed advising and consulting fees from Pfizer, Nanostring, and other companies.
AT ESMO 2017
Key clinical point:
Major finding: One patient (3.3%) assigned to letrozole/palbociclib had a residual cancer burden score of 0 or I, compared with three patients (10%) assigned to chemotherapy.
Data source: Interim analysis of a phase 2 parallel group trial with 60 patients evaluable for response and 106 evaluable for safety.
Disclosures: The study was funded by Pfizer and Nanostring. Dr. Cottu disclosed advisory board participation and travel support from Pfizer and others and research support from Roche, Novartis, and AstraZeneca. Dr. Harbeck disclosed advising and consulting fees from Pfizer, Nanostring, and other companies.
Can arterial switch operation impact cognitive deficits?
With dramatic advances of neonatal repair of complex cardiac disease, the population of adults with congenital heart disease (CHD) has increased dramatically, and while studies have shown an increased risk of neurodevelopmental and psychological disorders in these patients, few studies have evaluated their cognitive and psychosocial outcomes. Now, a review of young adults who had an arterial switch operation for transposition of the great arteries in France has found that they have almost twice the rate of cognitive difficulties and more than triple the rate of cognitive impairment as healthy peers.
“Despite satisfactory outcomes in most adults with transposition of the great arteries (TGA), a substantial proportion has cognitive or psychologic difficulties that may reduce their academic success and quality of life,” said lead author David Kalfa, MD, PhD, of Morgan Stanley Children’s Hospital of New York-Presbyterian, Columbia University Medical Center and coauthors in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2017;154:1028-35).
The study involved a review of 67 adults aged 18 and older born with TGA between 1984 and 1985 who had an arterial switch operation (ASO) at two hospitals in France: Necker Children’s Hospital in Paris and Marie Lannelongue Hospital in Le Plessis-Robinson. The researchers performed a matched analysis with 43 healthy subjects for age, gender, and education level.
The researchers found that 69% of the TGA patients had an intelligence quotient in the normal range of 85-115. The TGA patients had lower quotients for mean full-scale (94.9 plus or minus 15.3 vs. 103.4 plus or minus 12.3 in healthy subjects; P = 0.003), verbal (96.8 plus or minus 16.2 vs. 102.5 plus or minus 11.5; P =.033) and performance intelligence (93.7 plus or minus 14.6 vs. 103.8 plus or minus 14.3; P less than .001).
The TGA patients also had higher rates of cognitive difficulties, measured as intelligence quotient less than or equal to –1 standard deviation, and cognitive impairment, measured as intelligence quotient less than or equal to –2 standard deviation; 31% vs. 16% (P = .001) for the former and 6% vs. 2% (P = .030) for the latter.
TGA patients with cognitive difficulties had lower educational levels and were also more likely to repeat grades in school, Dr. Kalfa and coauthors noted. “Patients reported an overall satisfactory health-related quality of life,” Dr. Kalfa and coauthors said of the TGA group; “however, those with cognitive or psychologic difficulties reported poorer quality of life.” The researchers identified three predictors of worse outcomes: lower parental socioeconomic and educational status; older age at surgery; and longer hospital stays.
“Our findings suggest that the cognitive morbidities commonly reported in children and adolescents with complex CHD persist into adulthood in individuals with TGA after the ASO,” Dr. Kalfa and coauthors said. Future research should evaluate specific cognitive domains such as attention, memory, and executive functions. “This consideration is important for evaluation of the whole [adult] CHD population because specific cognitive impairments are increasingly documented into adolescence but remain rarely investigated in adulthood,” the researchers said.
Dr. Kalfa and coauthors reported having no financial disclosures.
The findings by Dr. Kalfa and coauthors may point the way to improve cognitive outcomes in children who have the arterial switch operation, said Ryan R. Davies, MD, of A.I duPont Hospital for Children in Wilmington, Del., in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:1036-7.) “Modifiable factors may exist both during the perioperative stage (perfusion strategies, intensive care management) and over the longer term (early neurocognitive assessments and interventions,” Dr. Davies said.
That parental socioeconomic status is associated with cognitive performance suggests early intervention and education “may pay long-term dividends,” Dr. Davies said. Future studies should focus on the impact of specific interventions and identify modifiable developmental factors, he said.
Dr. Kalfa and coauthors have provided an “important start” in that direction, Dr. Davies said. “They have shown that the neurodevelopmental deficits seen early in children with CHD persist into adulthood,” he said. “There are also hints here as to where interventions may be effective in ameliorating those deficits.”
Dr. Davies reported having no financial disclosures.
The findings by Dr. Kalfa and coauthors may point the way to improve cognitive outcomes in children who have the arterial switch operation, said Ryan R. Davies, MD, of A.I duPont Hospital for Children in Wilmington, Del., in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:1036-7.) “Modifiable factors may exist both during the perioperative stage (perfusion strategies, intensive care management) and over the longer term (early neurocognitive assessments and interventions,” Dr. Davies said.
That parental socioeconomic status is associated with cognitive performance suggests early intervention and education “may pay long-term dividends,” Dr. Davies said. Future studies should focus on the impact of specific interventions and identify modifiable developmental factors, he said.
Dr. Kalfa and coauthors have provided an “important start” in that direction, Dr. Davies said. “They have shown that the neurodevelopmental deficits seen early in children with CHD persist into adulthood,” he said. “There are also hints here as to where interventions may be effective in ameliorating those deficits.”
Dr. Davies reported having no financial disclosures.
The findings by Dr. Kalfa and coauthors may point the way to improve cognitive outcomes in children who have the arterial switch operation, said Ryan R. Davies, MD, of A.I duPont Hospital for Children in Wilmington, Del., in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:1036-7.) “Modifiable factors may exist both during the perioperative stage (perfusion strategies, intensive care management) and over the longer term (early neurocognitive assessments and interventions,” Dr. Davies said.
That parental socioeconomic status is associated with cognitive performance suggests early intervention and education “may pay long-term dividends,” Dr. Davies said. Future studies should focus on the impact of specific interventions and identify modifiable developmental factors, he said.
Dr. Kalfa and coauthors have provided an “important start” in that direction, Dr. Davies said. “They have shown that the neurodevelopmental deficits seen early in children with CHD persist into adulthood,” he said. “There are also hints here as to where interventions may be effective in ameliorating those deficits.”
Dr. Davies reported having no financial disclosures.
With dramatic advances of neonatal repair of complex cardiac disease, the population of adults with congenital heart disease (CHD) has increased dramatically, and while studies have shown an increased risk of neurodevelopmental and psychological disorders in these patients, few studies have evaluated their cognitive and psychosocial outcomes. Now, a review of young adults who had an arterial switch operation for transposition of the great arteries in France has found that they have almost twice the rate of cognitive difficulties and more than triple the rate of cognitive impairment as healthy peers.
“Despite satisfactory outcomes in most adults with transposition of the great arteries (TGA), a substantial proportion has cognitive or psychologic difficulties that may reduce their academic success and quality of life,” said lead author David Kalfa, MD, PhD, of Morgan Stanley Children’s Hospital of New York-Presbyterian, Columbia University Medical Center and coauthors in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2017;154:1028-35).
The study involved a review of 67 adults aged 18 and older born with TGA between 1984 and 1985 who had an arterial switch operation (ASO) at two hospitals in France: Necker Children’s Hospital in Paris and Marie Lannelongue Hospital in Le Plessis-Robinson. The researchers performed a matched analysis with 43 healthy subjects for age, gender, and education level.
The researchers found that 69% of the TGA patients had an intelligence quotient in the normal range of 85-115. The TGA patients had lower quotients for mean full-scale (94.9 plus or minus 15.3 vs. 103.4 plus or minus 12.3 in healthy subjects; P = 0.003), verbal (96.8 plus or minus 16.2 vs. 102.5 plus or minus 11.5; P =.033) and performance intelligence (93.7 plus or minus 14.6 vs. 103.8 plus or minus 14.3; P less than .001).
The TGA patients also had higher rates of cognitive difficulties, measured as intelligence quotient less than or equal to –1 standard deviation, and cognitive impairment, measured as intelligence quotient less than or equal to –2 standard deviation; 31% vs. 16% (P = .001) for the former and 6% vs. 2% (P = .030) for the latter.
TGA patients with cognitive difficulties had lower educational levels and were also more likely to repeat grades in school, Dr. Kalfa and coauthors noted. “Patients reported an overall satisfactory health-related quality of life,” Dr. Kalfa and coauthors said of the TGA group; “however, those with cognitive or psychologic difficulties reported poorer quality of life.” The researchers identified three predictors of worse outcomes: lower parental socioeconomic and educational status; older age at surgery; and longer hospital stays.
“Our findings suggest that the cognitive morbidities commonly reported in children and adolescents with complex CHD persist into adulthood in individuals with TGA after the ASO,” Dr. Kalfa and coauthors said. Future research should evaluate specific cognitive domains such as attention, memory, and executive functions. “This consideration is important for evaluation of the whole [adult] CHD population because specific cognitive impairments are increasingly documented into adolescence but remain rarely investigated in adulthood,” the researchers said.
Dr. Kalfa and coauthors reported having no financial disclosures.
With dramatic advances of neonatal repair of complex cardiac disease, the population of adults with congenital heart disease (CHD) has increased dramatically, and while studies have shown an increased risk of neurodevelopmental and psychological disorders in these patients, few studies have evaluated their cognitive and psychosocial outcomes. Now, a review of young adults who had an arterial switch operation for transposition of the great arteries in France has found that they have almost twice the rate of cognitive difficulties and more than triple the rate of cognitive impairment as healthy peers.
“Despite satisfactory outcomes in most adults with transposition of the great arteries (TGA), a substantial proportion has cognitive or psychologic difficulties that may reduce their academic success and quality of life,” said lead author David Kalfa, MD, PhD, of Morgan Stanley Children’s Hospital of New York-Presbyterian, Columbia University Medical Center and coauthors in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2017;154:1028-35).
The study involved a review of 67 adults aged 18 and older born with TGA between 1984 and 1985 who had an arterial switch operation (ASO) at two hospitals in France: Necker Children’s Hospital in Paris and Marie Lannelongue Hospital in Le Plessis-Robinson. The researchers performed a matched analysis with 43 healthy subjects for age, gender, and education level.
The researchers found that 69% of the TGA patients had an intelligence quotient in the normal range of 85-115. The TGA patients had lower quotients for mean full-scale (94.9 plus or minus 15.3 vs. 103.4 plus or minus 12.3 in healthy subjects; P = 0.003), verbal (96.8 plus or minus 16.2 vs. 102.5 plus or minus 11.5; P =.033) and performance intelligence (93.7 plus or minus 14.6 vs. 103.8 plus or minus 14.3; P less than .001).
The TGA patients also had higher rates of cognitive difficulties, measured as intelligence quotient less than or equal to –1 standard deviation, and cognitive impairment, measured as intelligence quotient less than or equal to –2 standard deviation; 31% vs. 16% (P = .001) for the former and 6% vs. 2% (P = .030) for the latter.
TGA patients with cognitive difficulties had lower educational levels and were also more likely to repeat grades in school, Dr. Kalfa and coauthors noted. “Patients reported an overall satisfactory health-related quality of life,” Dr. Kalfa and coauthors said of the TGA group; “however, those with cognitive or psychologic difficulties reported poorer quality of life.” The researchers identified three predictors of worse outcomes: lower parental socioeconomic and educational status; older age at surgery; and longer hospital stays.
“Our findings suggest that the cognitive morbidities commonly reported in children and adolescents with complex CHD persist into adulthood in individuals with TGA after the ASO,” Dr. Kalfa and coauthors said. Future research should evaluate specific cognitive domains such as attention, memory, and executive functions. “This consideration is important for evaluation of the whole [adult] CHD population because specific cognitive impairments are increasingly documented into adolescence but remain rarely investigated in adulthood,” the researchers said.
Dr. Kalfa and coauthors reported having no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A substantial proportion of young adults who had transposition of the great arteries have cognitive or psychological difficulties.
Major finding: Cognitive difficulties were significantly more frequent in the study population than the general population, 31% vs. 16%.
Data source: Age-, gender-, and education level–matched population of 67 young adults with transposition of the great arteries and 43 healthy subjects.
Disclosures: Dr. Kalfa and coauthors reported having no financial disclosures.
Diagnostic laparoscopy pinpoints postop abdominal pain in bariatric patients
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
FROM OBESITY SURGERY
Key clinical point:
Major finding: In the study group, 57% of patients had a positive diagnostic laparoscopy results identifying the source of their chronic abdominal pain.
Data source: Retrospective review of post–bariatric surgery patients who underwent diagnostic laparoscopy (DL) during 2003-2015.
Disclosures: The investigators had no relevant financial disclosures to report.
Residents getting unprecedented attention from employers
Half of final-year residents surveyed this April had received 100 or more job solicitations during their training, according to physician-recruiting firm Merritt Hawkins.
Among the 935 survey responses the company received, 70% of physicians in their final year of residency had gotten more than 50 job offers: 20% received 51-100, and 50% received more than 100. The numbers were even higher for those in primary care: 76% had received at least 51 job solicitations, and 55% reported more than 100 offers, Merritt Hawkins said in its 2017 Survey of Final-Year Medical Residents.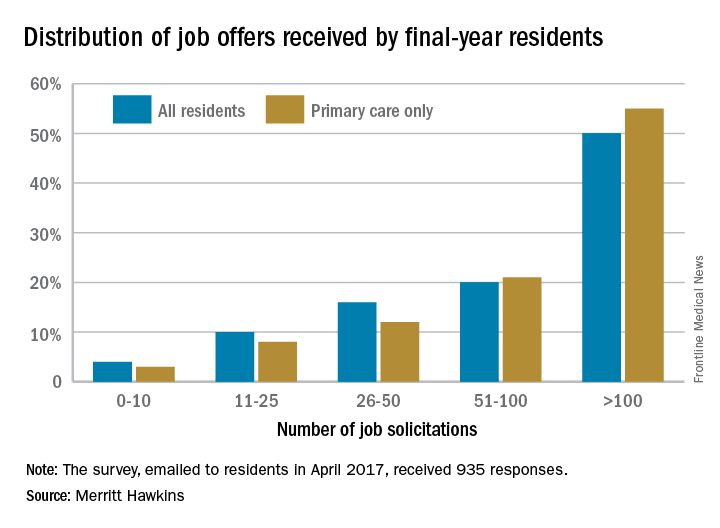
The 50% of all residents who received 100 or more job solicitations is the highest at that level since the survey began in 1991 (it is generally conducted every 2 or 3 years), with much lower figures seen as recently as 2008 – only 6% got that many offers – and 2006, when the number was 16%.
That primary care physicians are even more in demand shows their importance “as leaders of interdisciplinary clinical teams [and] managers of care and resources in emerging quality-driven delivery models such as ACOs [accountable care organizations],” the company said.
Demand for specialists is slightly lower, with 46% of residents in internal medicine, surgical, or diagnostic specialties getting more than 100 job offers and 64% getting more than 50. Current trends in mental health services, however, led Merritt Hawkins to single out psychiatry for special mention: 78% of final-year psychiatry residents had received more than 50 job solicitations – even more than primary care – although the number at the over-100 level, 48%, was lower, according to the report.
Half of final-year residents surveyed this April had received 100 or more job solicitations during their training, according to physician-recruiting firm Merritt Hawkins.
Among the 935 survey responses the company received, 70% of physicians in their final year of residency had gotten more than 50 job offers: 20% received 51-100, and 50% received more than 100. The numbers were even higher for those in primary care: 76% had received at least 51 job solicitations, and 55% reported more than 100 offers, Merritt Hawkins said in its 2017 Survey of Final-Year Medical Residents.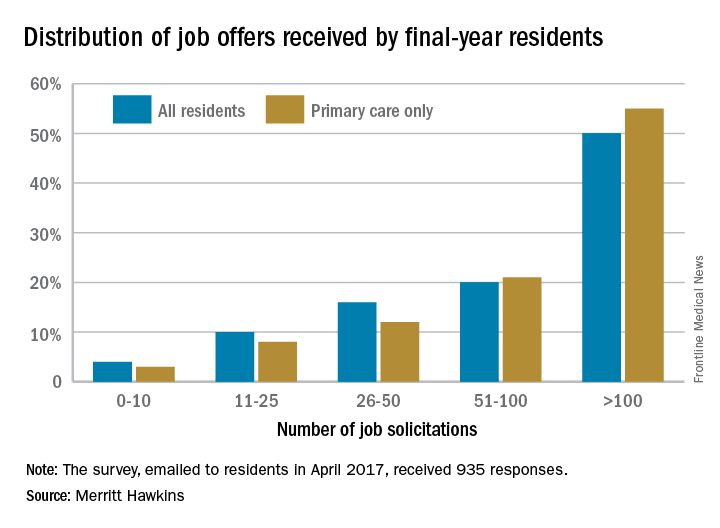
The 50% of all residents who received 100 or more job solicitations is the highest at that level since the survey began in 1991 (it is generally conducted every 2 or 3 years), with much lower figures seen as recently as 2008 – only 6% got that many offers – and 2006, when the number was 16%.
That primary care physicians are even more in demand shows their importance “as leaders of interdisciplinary clinical teams [and] managers of care and resources in emerging quality-driven delivery models such as ACOs [accountable care organizations],” the company said.
Demand for specialists is slightly lower, with 46% of residents in internal medicine, surgical, or diagnostic specialties getting more than 100 job offers and 64% getting more than 50. Current trends in mental health services, however, led Merritt Hawkins to single out psychiatry for special mention: 78% of final-year psychiatry residents had received more than 50 job solicitations – even more than primary care – although the number at the over-100 level, 48%, was lower, according to the report.
Half of final-year residents surveyed this April had received 100 or more job solicitations during their training, according to physician-recruiting firm Merritt Hawkins.
Among the 935 survey responses the company received, 70% of physicians in their final year of residency had gotten more than 50 job offers: 20% received 51-100, and 50% received more than 100. The numbers were even higher for those in primary care: 76% had received at least 51 job solicitations, and 55% reported more than 100 offers, Merritt Hawkins said in its 2017 Survey of Final-Year Medical Residents.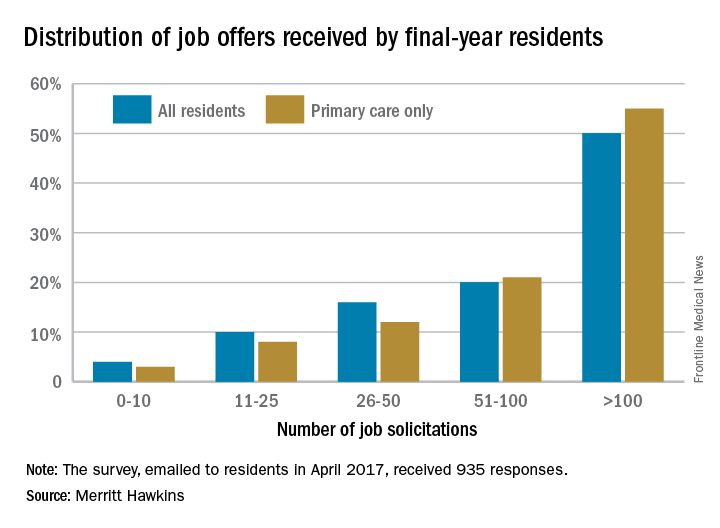
The 50% of all residents who received 100 or more job solicitations is the highest at that level since the survey began in 1991 (it is generally conducted every 2 or 3 years), with much lower figures seen as recently as 2008 – only 6% got that many offers – and 2006, when the number was 16%.
That primary care physicians are even more in demand shows their importance “as leaders of interdisciplinary clinical teams [and] managers of care and resources in emerging quality-driven delivery models such as ACOs [accountable care organizations],” the company said.
Demand for specialists is slightly lower, with 46% of residents in internal medicine, surgical, or diagnostic specialties getting more than 100 job offers and 64% getting more than 50. Current trends in mental health services, however, led Merritt Hawkins to single out psychiatry for special mention: 78% of final-year psychiatry residents had received more than 50 job solicitations – even more than primary care – although the number at the over-100 level, 48%, was lower, according to the report.
Patients with severe obesity may have difficulty grading pain
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
FROM SURGERY FOR OBESITY AND RELATED DISEASES
ACS releases quality and safety manual
The American College of Surgeons (ACS) is pleased to announce that the Optimal Resources for Surgical Quality and Safety manual is now available for purchase. This manual is intended to serve as a trusted resource for surgical leaders seeking to improve patient care in their institutions, departments, and practices. It introduces key concepts in quality, safety, and reliability and explores the essential elements that all hospitals should have in place to ensure the delivery of patient-centered care.
Specific topics covered include the following: the domains and phases of surgical care, peer and case review, responsibilities of the surgical quality officer, institutional infrastructure, privileging and credentialing, high reliability, applications to the unique surgical disciplines, data analytics, clinical practice guidelines, quality collaboratives, and education and training. The manual also includes a look at some of the “soft skills” that influence quality and safety in health care, as well as the individual surgeon’s responsibility to patients, colleagues, and the next generation of surgeons.
Optimal Resources for Surgical Quality and Safety is available on the ACS website at facs.org/quality-programs/about/optimal-resources-manual for $44.95 (includes shipping) for single copies (up to a quantity of nine) or $39.95 (includes shipping) per copy for 10 copies or more.
The American College of Surgeons (ACS) is pleased to announce that the Optimal Resources for Surgical Quality and Safety manual is now available for purchase. This manual is intended to serve as a trusted resource for surgical leaders seeking to improve patient care in their institutions, departments, and practices. It introduces key concepts in quality, safety, and reliability and explores the essential elements that all hospitals should have in place to ensure the delivery of patient-centered care.
Specific topics covered include the following: the domains and phases of surgical care, peer and case review, responsibilities of the surgical quality officer, institutional infrastructure, privileging and credentialing, high reliability, applications to the unique surgical disciplines, data analytics, clinical practice guidelines, quality collaboratives, and education and training. The manual also includes a look at some of the “soft skills” that influence quality and safety in health care, as well as the individual surgeon’s responsibility to patients, colleagues, and the next generation of surgeons.
Optimal Resources for Surgical Quality and Safety is available on the ACS website at facs.org/quality-programs/about/optimal-resources-manual for $44.95 (includes shipping) for single copies (up to a quantity of nine) or $39.95 (includes shipping) per copy for 10 copies or more.
The American College of Surgeons (ACS) is pleased to announce that the Optimal Resources for Surgical Quality and Safety manual is now available for purchase. This manual is intended to serve as a trusted resource for surgical leaders seeking to improve patient care in their institutions, departments, and practices. It introduces key concepts in quality, safety, and reliability and explores the essential elements that all hospitals should have in place to ensure the delivery of patient-centered care.
Specific topics covered include the following: the domains and phases of surgical care, peer and case review, responsibilities of the surgical quality officer, institutional infrastructure, privileging and credentialing, high reliability, applications to the unique surgical disciplines, data analytics, clinical practice guidelines, quality collaboratives, and education and training. The manual also includes a look at some of the “soft skills” that influence quality and safety in health care, as well as the individual surgeon’s responsibility to patients, colleagues, and the next generation of surgeons.
Optimal Resources for Surgical Quality and Safety is available on the ACS website at facs.org/quality-programs/about/optimal-resources-manual for $44.95 (includes shipping) for single copies (up to a quantity of nine) or $39.95 (includes shipping) per copy for 10 copies or more.