User login
Official Newspaper of the American College of Surgeons
Survey reveals heavy EMR burden on surgical residents
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
AT THE ACS CLINICAL CONGRESS
Medicare pay cut may loom in wake of tax bill passage
requiring that any spending increases be offset by other spending cuts.
At issue is the Senate bill’s repeal of the Affordable Care Act requirement that every individual have health insurance – the individual mandate.
In a Nov. 14 letter to the majority and minority leaders of the both the House and Senate, the American Medical Association, the American Academy of Family Physicians, the American Hospital Association, and the Federation of American Hospitals called on Congress to maintain the individual mandate. The four health provider groups were joined in the letter by America’s Health Insurance Plans and the Blue Cross Blue Shield Association.
“Eliminating the individual mandate by itself likely will result in a significant increase in premiums, which would in turn substantially increase the number of uninsured Americans,” the organizations warned.
The American College of Physicians also urged the Senate to not end the individual mandate, after the bill was passed out of the Senate Finance Committee along party lines.
“We are concerned that the bill approved by the Senate Budget Committee on a party-line vote would repeal the Affordable Care Act’s requirement that persons purchase qualified health insurance coverage. ... which will destabilize the individual insurance market and lead to 13 million Americans losing coverage, double-digit premium increases, and insurers dropping out of the individual insurance market, according to the Congressional Budget Office and other independent analyses,” the American College of Physicians wrote in a Nov. 30 letter to Senate Majority Leader Mitch McConnell (R-Ky.) and Senate Minority Leader Charles Schumer (D-N.Y.).
ACP leaders also voiced concern about the looming cuts to Medicare that could result from the bill, noting that the Congressional Budget Office estimated that $25 billion will be cut from Medicare as part of a larger sequestration – a 4% pay cut to the fee schedule – that would result if offsets are not found to keep the deficit from increasing.
The ACP noted that, along with other pay cuts on the books from other legislative action, physicians would be losing nearly 7% of their pay from the fee schedule, beginning in 2018.
The next step in the process is for a House and Senate conference committee to resolve differences between the two versions of the tax reform bills. Both chambers would then vote on a compromise bill. At some point, there would to be a vote to waive the pay-as-you-go rules to prevent the Medicare cuts from going into effect. However, such a vote requires 60 votes in the Senate and a simple majority in the House, neither of which are guaranteed.
“It’s hard to say right now whether or not that can be worked out,” Julius Hobson, a Washington-based health care lobbyist, said in an interview. “There is desire on the part of the Republican leadership in the two chambers, and I suspect it might pass the Senate. The problem may well be in the House with the conservatives, particularly the House Freedom Caucus, and whether they will go along with that.”
Mr. Hobson noted that GOP leadership has said they plan to move on to entitlement reform after tax reform is finished. So, even if the cuts are spared by a pay-as-you-go rules waiver, they could still come into effect in some way when GOP tackles Medicare, Medicaid, and Social Security reform.
“It looks interesting to be saving cuts in Medicare on the one hand, but on the other hand, reform really means cuts,” he said.
requiring that any spending increases be offset by other spending cuts.
At issue is the Senate bill’s repeal of the Affordable Care Act requirement that every individual have health insurance – the individual mandate.
In a Nov. 14 letter to the majority and minority leaders of the both the House and Senate, the American Medical Association, the American Academy of Family Physicians, the American Hospital Association, and the Federation of American Hospitals called on Congress to maintain the individual mandate. The four health provider groups were joined in the letter by America’s Health Insurance Plans and the Blue Cross Blue Shield Association.
“Eliminating the individual mandate by itself likely will result in a significant increase in premiums, which would in turn substantially increase the number of uninsured Americans,” the organizations warned.
The American College of Physicians also urged the Senate to not end the individual mandate, after the bill was passed out of the Senate Finance Committee along party lines.
“We are concerned that the bill approved by the Senate Budget Committee on a party-line vote would repeal the Affordable Care Act’s requirement that persons purchase qualified health insurance coverage. ... which will destabilize the individual insurance market and lead to 13 million Americans losing coverage, double-digit premium increases, and insurers dropping out of the individual insurance market, according to the Congressional Budget Office and other independent analyses,” the American College of Physicians wrote in a Nov. 30 letter to Senate Majority Leader Mitch McConnell (R-Ky.) and Senate Minority Leader Charles Schumer (D-N.Y.).
ACP leaders also voiced concern about the looming cuts to Medicare that could result from the bill, noting that the Congressional Budget Office estimated that $25 billion will be cut from Medicare as part of a larger sequestration – a 4% pay cut to the fee schedule – that would result if offsets are not found to keep the deficit from increasing.
The ACP noted that, along with other pay cuts on the books from other legislative action, physicians would be losing nearly 7% of their pay from the fee schedule, beginning in 2018.
The next step in the process is for a House and Senate conference committee to resolve differences between the two versions of the tax reform bills. Both chambers would then vote on a compromise bill. At some point, there would to be a vote to waive the pay-as-you-go rules to prevent the Medicare cuts from going into effect. However, such a vote requires 60 votes in the Senate and a simple majority in the House, neither of which are guaranteed.
“It’s hard to say right now whether or not that can be worked out,” Julius Hobson, a Washington-based health care lobbyist, said in an interview. “There is desire on the part of the Republican leadership in the two chambers, and I suspect it might pass the Senate. The problem may well be in the House with the conservatives, particularly the House Freedom Caucus, and whether they will go along with that.”
Mr. Hobson noted that GOP leadership has said they plan to move on to entitlement reform after tax reform is finished. So, even if the cuts are spared by a pay-as-you-go rules waiver, they could still come into effect in some way when GOP tackles Medicare, Medicaid, and Social Security reform.
“It looks interesting to be saving cuts in Medicare on the one hand, but on the other hand, reform really means cuts,” he said.
requiring that any spending increases be offset by other spending cuts.
At issue is the Senate bill’s repeal of the Affordable Care Act requirement that every individual have health insurance – the individual mandate.
In a Nov. 14 letter to the majority and minority leaders of the both the House and Senate, the American Medical Association, the American Academy of Family Physicians, the American Hospital Association, and the Federation of American Hospitals called on Congress to maintain the individual mandate. The four health provider groups were joined in the letter by America’s Health Insurance Plans and the Blue Cross Blue Shield Association.
“Eliminating the individual mandate by itself likely will result in a significant increase in premiums, which would in turn substantially increase the number of uninsured Americans,” the organizations warned.
The American College of Physicians also urged the Senate to not end the individual mandate, after the bill was passed out of the Senate Finance Committee along party lines.
“We are concerned that the bill approved by the Senate Budget Committee on a party-line vote would repeal the Affordable Care Act’s requirement that persons purchase qualified health insurance coverage. ... which will destabilize the individual insurance market and lead to 13 million Americans losing coverage, double-digit premium increases, and insurers dropping out of the individual insurance market, according to the Congressional Budget Office and other independent analyses,” the American College of Physicians wrote in a Nov. 30 letter to Senate Majority Leader Mitch McConnell (R-Ky.) and Senate Minority Leader Charles Schumer (D-N.Y.).
ACP leaders also voiced concern about the looming cuts to Medicare that could result from the bill, noting that the Congressional Budget Office estimated that $25 billion will be cut from Medicare as part of a larger sequestration – a 4% pay cut to the fee schedule – that would result if offsets are not found to keep the deficit from increasing.
The ACP noted that, along with other pay cuts on the books from other legislative action, physicians would be losing nearly 7% of their pay from the fee schedule, beginning in 2018.
The next step in the process is for a House and Senate conference committee to resolve differences between the two versions of the tax reform bills. Both chambers would then vote on a compromise bill. At some point, there would to be a vote to waive the pay-as-you-go rules to prevent the Medicare cuts from going into effect. However, such a vote requires 60 votes in the Senate and a simple majority in the House, neither of which are guaranteed.
“It’s hard to say right now whether or not that can be worked out,” Julius Hobson, a Washington-based health care lobbyist, said in an interview. “There is desire on the part of the Republican leadership in the two chambers, and I suspect it might pass the Senate. The problem may well be in the House with the conservatives, particularly the House Freedom Caucus, and whether they will go along with that.”
Mr. Hobson noted that GOP leadership has said they plan to move on to entitlement reform after tax reform is finished. So, even if the cuts are spared by a pay-as-you-go rules waiver, they could still come into effect in some way when GOP tackles Medicare, Medicaid, and Social Security reform.
“It looks interesting to be saving cuts in Medicare on the one hand, but on the other hand, reform really means cuts,” he said.
Major venous injury tied to adverse events in aortic reconstruction
Although uncommon, major venous injury during surgery for aortic reconstruction can result in massive blood loss resulting in increased morbidity and mortality, according to the results of a retrospective review conducted by Sachinder S. Hans, MD, and colleagues, and reported online in the Annals of Vascular Surgery.
Of 945 patients undergoing major aortic reconstruction, 723 (76.5%) underwent open abdominal aortic aneurysm (AAA) repair/iliac aneurysm repair; 222 patients (23.5%) underwent aortofemoral grafting (AFG). The number of units of packed red blood cells transfused, location of injured vessel, type of repair, postoperative morbidity, and mortality were collected in a vascular registry on a continuous basis. All patients identified with iliac vein/inferior vena cava/femoral vein injury had follow-up noninvasive venous examination of the lower extremities.
A total of 17 of 945 patients (1.9%) suffered 18 major venous injuries during aortic reconstruction according to Dr. Hans and his colleagues at St. John Macomb Hospital, Warren, Mich. These injuries comprised four inferior vena cava injuries, 10 iliac vein injuries, and four left renal vein injuries (Ann Vasc Surg. 2017. doi: 10.1016/j.avsg.2017.08.004).
Overall, 16 of the 18 injuries occurred during open AAA repair (7 for ruptured AAA, and 9 for intact). Two of the patients with venous injury died (11.8%), one from uncontrolled bleeding from a tear in the right iliac during repair of a ruptured AAA, and the second from disseminated intravascular complication following repair of ruptured AAA. The remaining two major venous injuries occurred during redo AFG (1 out of 6 total) and primary AFG (1 out of 216 total).
The following risk factors were also observed: The majority of the patients experiencing major venous injury were men (83%; P = .002), and the presence of periarterial inflammation (P = .006) and associated iliac aneurysm (P = .05) were significantly associated with major venous injury among the AAA patients.
The researchers suggested the following tips to lessen the likelihood of major venous injury: “Prevention of major venous injury is not always possible; however, keeping dissection plane close to arterial wall, avoiding passage of vessel loops or tapes around the neck of the aorta and iliac bifurcation, particularly in patients with surrounding inflammation and ligating venous tributaries crossing the aorta as they are joining the inferior vena cava may help reduce incidence of such injuries.”
They also suggested that surgeons should be cognizant of the serious complication that major venous injury was for patients undergoing aortic reconstruction, and to be aware that “the incidence of such injury is higher during the repair of ruptured AAA and redo aortofemoral grafting.”
The authors received no study funding and reported that they had no conflicts.
Although uncommon, major venous injury during surgery for aortic reconstruction can result in massive blood loss resulting in increased morbidity and mortality, according to the results of a retrospective review conducted by Sachinder S. Hans, MD, and colleagues, and reported online in the Annals of Vascular Surgery.
Of 945 patients undergoing major aortic reconstruction, 723 (76.5%) underwent open abdominal aortic aneurysm (AAA) repair/iliac aneurysm repair; 222 patients (23.5%) underwent aortofemoral grafting (AFG). The number of units of packed red blood cells transfused, location of injured vessel, type of repair, postoperative morbidity, and mortality were collected in a vascular registry on a continuous basis. All patients identified with iliac vein/inferior vena cava/femoral vein injury had follow-up noninvasive venous examination of the lower extremities.
A total of 17 of 945 patients (1.9%) suffered 18 major venous injuries during aortic reconstruction according to Dr. Hans and his colleagues at St. John Macomb Hospital, Warren, Mich. These injuries comprised four inferior vena cava injuries, 10 iliac vein injuries, and four left renal vein injuries (Ann Vasc Surg. 2017. doi: 10.1016/j.avsg.2017.08.004).
Overall, 16 of the 18 injuries occurred during open AAA repair (7 for ruptured AAA, and 9 for intact). Two of the patients with venous injury died (11.8%), one from uncontrolled bleeding from a tear in the right iliac during repair of a ruptured AAA, and the second from disseminated intravascular complication following repair of ruptured AAA. The remaining two major venous injuries occurred during redo AFG (1 out of 6 total) and primary AFG (1 out of 216 total).
The following risk factors were also observed: The majority of the patients experiencing major venous injury were men (83%; P = .002), and the presence of periarterial inflammation (P = .006) and associated iliac aneurysm (P = .05) were significantly associated with major venous injury among the AAA patients.
The researchers suggested the following tips to lessen the likelihood of major venous injury: “Prevention of major venous injury is not always possible; however, keeping dissection plane close to arterial wall, avoiding passage of vessel loops or tapes around the neck of the aorta and iliac bifurcation, particularly in patients with surrounding inflammation and ligating venous tributaries crossing the aorta as they are joining the inferior vena cava may help reduce incidence of such injuries.”
They also suggested that surgeons should be cognizant of the serious complication that major venous injury was for patients undergoing aortic reconstruction, and to be aware that “the incidence of such injury is higher during the repair of ruptured AAA and redo aortofemoral grafting.”
The authors received no study funding and reported that they had no conflicts.
Although uncommon, major venous injury during surgery for aortic reconstruction can result in massive blood loss resulting in increased morbidity and mortality, according to the results of a retrospective review conducted by Sachinder S. Hans, MD, and colleagues, and reported online in the Annals of Vascular Surgery.
Of 945 patients undergoing major aortic reconstruction, 723 (76.5%) underwent open abdominal aortic aneurysm (AAA) repair/iliac aneurysm repair; 222 patients (23.5%) underwent aortofemoral grafting (AFG). The number of units of packed red blood cells transfused, location of injured vessel, type of repair, postoperative morbidity, and mortality were collected in a vascular registry on a continuous basis. All patients identified with iliac vein/inferior vena cava/femoral vein injury had follow-up noninvasive venous examination of the lower extremities.
A total of 17 of 945 patients (1.9%) suffered 18 major venous injuries during aortic reconstruction according to Dr. Hans and his colleagues at St. John Macomb Hospital, Warren, Mich. These injuries comprised four inferior vena cava injuries, 10 iliac vein injuries, and four left renal vein injuries (Ann Vasc Surg. 2017. doi: 10.1016/j.avsg.2017.08.004).
Overall, 16 of the 18 injuries occurred during open AAA repair (7 for ruptured AAA, and 9 for intact). Two of the patients with venous injury died (11.8%), one from uncontrolled bleeding from a tear in the right iliac during repair of a ruptured AAA, and the second from disseminated intravascular complication following repair of ruptured AAA. The remaining two major venous injuries occurred during redo AFG (1 out of 6 total) and primary AFG (1 out of 216 total).
The following risk factors were also observed: The majority of the patients experiencing major venous injury were men (83%; P = .002), and the presence of periarterial inflammation (P = .006) and associated iliac aneurysm (P = .05) were significantly associated with major venous injury among the AAA patients.
The researchers suggested the following tips to lessen the likelihood of major venous injury: “Prevention of major venous injury is not always possible; however, keeping dissection plane close to arterial wall, avoiding passage of vessel loops or tapes around the neck of the aorta and iliac bifurcation, particularly in patients with surrounding inflammation and ligating venous tributaries crossing the aorta as they are joining the inferior vena cava may help reduce incidence of such injuries.”
They also suggested that surgeons should be cognizant of the serious complication that major venous injury was for patients undergoing aortic reconstruction, and to be aware that “the incidence of such injury is higher during the repair of ruptured AAA and redo aortofemoral grafting.”
The authors received no study funding and reported that they had no conflicts.
FROM THE ANNALS OF VASCULAR SURGERY
Key clinical point:
Major finding: A total of 17/945 patients suffered major venous injuries during aortic reconstruction.
Data source: A retrospective review of 945 patients undergoing aortic reconstruction at two sites.
Disclosures: The authors received no study funding and reported that they had no conflicts.
ASCO larynx-preservation guidelines reflect important practice changes
The latest edition of the clinical practice guideline on larynx preservation strategies for the treatment of laryngeal cancer from the American Society of Clinical Oncology (ASCO) emphasizes that larynx preservation in patients with early stage disease does not compromise survival compared with total laryngectomy.
“The nuances of treatment selection, assessments of pretreatment voice and swallowing, and public awareness of new organ-preservation treatment and decision making have increased to the point that careful and individualized discussion with patients and families with the multidisciplinary treatment team is a critical element of modern care,” wrote Arlene A. Forastiere, MD, of Johns Hopkins Medicine in Baltimore, and her colleagues. The report was published in the Journal of Clinical Oncology.
Changes since the last guideline on the subject, issued in 2006, include evidence-based support for the use of endoscopic resection in patients with limited stage (T1 and T2) disease, and as an initial total laryngectomy therapy both in patients with stage T4a disease, and in those with severe laryngeal dysfunction prior to treatment.
Also new since the last guideline are recommendations for the use of positron-emission tomography imaging for evaluating the status of regional nodes after treatment, as well as guidance on the best techniques for evaluating voice and swallowing function.
While the initial recommendation that all patients with T1 and T2 laryngeal cancer should be treated with the intent to preserve the larynx has not changed, there is a new recommendation (1.3) stating that surgery may be more effective than radiotherapy for initial larynx preservation therapy, although this recommendation is based on retrospective data and may be affected by patient selection factors, the authors acknowledged. The new recommendation also notes that in an experienced operator’s hands, endoscopic resections can have outcomes that are equal to or better than those with open partial laryngectomy.
The initial recommendation stating that “[e]very effort should be made to avoid combining surgery with radiation therapy because functional outcomes may be compromised by combined-modality therapy; single-modality treatment is effective for limited-stage, invasive cancer of the larynx” remains unchanged.
There is also an updated recommendation that tumor-free margins should be the goal when surgery with larynx preservation intent is performed (1.4).
“Surgery that anticipates the need for postoperative [radiation therapy] to treat close or involved tumor margins or widespread dysplasia is not an acceptable treatment approach,” the guideline authors noted.
There are two other new recommendations including the opinion, based on evidence of benefits vs. harms, that total laryngectomy rather than larynx preservation may be associated with better survival and quality of life in patients with extensive T3 lesions, large T4 lesions, or in those who have poor pretreatment laryngeal function.
The third new recommendation is that “[a]s part of a comprehensive pretreatment evaluation, all patients should undergo a baseline assessment of voice and swallowing function, voice (use and requirements), and counseling with regard to the potential effect of treatment options on voice, swallowing, and quality of life.”
Among the updated recommendations are the following:
• An emphasis on the importance of considering a multiplicity of factors when choosing therapy for patients with limited-stage disease (1.7).
• The option of specialized organ-preservation procedures for a small number of patients with T3 or T4 primary site disease (2.4).
• A strong recommendation for the use of concurrent chemoradiotherapy compared with radiotherapy alone or sequential therapy (2.5).
• Elective neck dissection is not required for patients with clinically involved regional cervical nodes treated with definitive radiotherapy of chemoradiotherapy who have complete clinical, radiologic, and metabolic imaging (3.3).
• “Selection of therapy for an individual patient requires assessment by the multidisciplinary team as well as consideration of voice and swallowing function; patient comorbidity, psychosocial situation, and preferences; and local therapeutic expertise” (4.2).
The guideline development process was supported by ASCO. Dr, Forastiere disclosed employment and stock ownership in NantHealth. Many of her coauthors disclosed institutional funding, consultation/advising, travel support and expenses, honoraria, and or patents/royalties with multiple entities.
The latest edition of the clinical practice guideline on larynx preservation strategies for the treatment of laryngeal cancer from the American Society of Clinical Oncology (ASCO) emphasizes that larynx preservation in patients with early stage disease does not compromise survival compared with total laryngectomy.
“The nuances of treatment selection, assessments of pretreatment voice and swallowing, and public awareness of new organ-preservation treatment and decision making have increased to the point that careful and individualized discussion with patients and families with the multidisciplinary treatment team is a critical element of modern care,” wrote Arlene A. Forastiere, MD, of Johns Hopkins Medicine in Baltimore, and her colleagues. The report was published in the Journal of Clinical Oncology.
Changes since the last guideline on the subject, issued in 2006, include evidence-based support for the use of endoscopic resection in patients with limited stage (T1 and T2) disease, and as an initial total laryngectomy therapy both in patients with stage T4a disease, and in those with severe laryngeal dysfunction prior to treatment.
Also new since the last guideline are recommendations for the use of positron-emission tomography imaging for evaluating the status of regional nodes after treatment, as well as guidance on the best techniques for evaluating voice and swallowing function.
While the initial recommendation that all patients with T1 and T2 laryngeal cancer should be treated with the intent to preserve the larynx has not changed, there is a new recommendation (1.3) stating that surgery may be more effective than radiotherapy for initial larynx preservation therapy, although this recommendation is based on retrospective data and may be affected by patient selection factors, the authors acknowledged. The new recommendation also notes that in an experienced operator’s hands, endoscopic resections can have outcomes that are equal to or better than those with open partial laryngectomy.
The initial recommendation stating that “[e]very effort should be made to avoid combining surgery with radiation therapy because functional outcomes may be compromised by combined-modality therapy; single-modality treatment is effective for limited-stage, invasive cancer of the larynx” remains unchanged.
There is also an updated recommendation that tumor-free margins should be the goal when surgery with larynx preservation intent is performed (1.4).
“Surgery that anticipates the need for postoperative [radiation therapy] to treat close or involved tumor margins or widespread dysplasia is not an acceptable treatment approach,” the guideline authors noted.
There are two other new recommendations including the opinion, based on evidence of benefits vs. harms, that total laryngectomy rather than larynx preservation may be associated with better survival and quality of life in patients with extensive T3 lesions, large T4 lesions, or in those who have poor pretreatment laryngeal function.
The third new recommendation is that “[a]s part of a comprehensive pretreatment evaluation, all patients should undergo a baseline assessment of voice and swallowing function, voice (use and requirements), and counseling with regard to the potential effect of treatment options on voice, swallowing, and quality of life.”
Among the updated recommendations are the following:
• An emphasis on the importance of considering a multiplicity of factors when choosing therapy for patients with limited-stage disease (1.7).
• The option of specialized organ-preservation procedures for a small number of patients with T3 or T4 primary site disease (2.4).
• A strong recommendation for the use of concurrent chemoradiotherapy compared with radiotherapy alone or sequential therapy (2.5).
• Elective neck dissection is not required for patients with clinically involved regional cervical nodes treated with definitive radiotherapy of chemoradiotherapy who have complete clinical, radiologic, and metabolic imaging (3.3).
• “Selection of therapy for an individual patient requires assessment by the multidisciplinary team as well as consideration of voice and swallowing function; patient comorbidity, psychosocial situation, and preferences; and local therapeutic expertise” (4.2).
The guideline development process was supported by ASCO. Dr, Forastiere disclosed employment and stock ownership in NantHealth. Many of her coauthors disclosed institutional funding, consultation/advising, travel support and expenses, honoraria, and or patents/royalties with multiple entities.
The latest edition of the clinical practice guideline on larynx preservation strategies for the treatment of laryngeal cancer from the American Society of Clinical Oncology (ASCO) emphasizes that larynx preservation in patients with early stage disease does not compromise survival compared with total laryngectomy.
“The nuances of treatment selection, assessments of pretreatment voice and swallowing, and public awareness of new organ-preservation treatment and decision making have increased to the point that careful and individualized discussion with patients and families with the multidisciplinary treatment team is a critical element of modern care,” wrote Arlene A. Forastiere, MD, of Johns Hopkins Medicine in Baltimore, and her colleagues. The report was published in the Journal of Clinical Oncology.
Changes since the last guideline on the subject, issued in 2006, include evidence-based support for the use of endoscopic resection in patients with limited stage (T1 and T2) disease, and as an initial total laryngectomy therapy both in patients with stage T4a disease, and in those with severe laryngeal dysfunction prior to treatment.
Also new since the last guideline are recommendations for the use of positron-emission tomography imaging for evaluating the status of regional nodes after treatment, as well as guidance on the best techniques for evaluating voice and swallowing function.
While the initial recommendation that all patients with T1 and T2 laryngeal cancer should be treated with the intent to preserve the larynx has not changed, there is a new recommendation (1.3) stating that surgery may be more effective than radiotherapy for initial larynx preservation therapy, although this recommendation is based on retrospective data and may be affected by patient selection factors, the authors acknowledged. The new recommendation also notes that in an experienced operator’s hands, endoscopic resections can have outcomes that are equal to or better than those with open partial laryngectomy.
The initial recommendation stating that “[e]very effort should be made to avoid combining surgery with radiation therapy because functional outcomes may be compromised by combined-modality therapy; single-modality treatment is effective for limited-stage, invasive cancer of the larynx” remains unchanged.
There is also an updated recommendation that tumor-free margins should be the goal when surgery with larynx preservation intent is performed (1.4).
“Surgery that anticipates the need for postoperative [radiation therapy] to treat close or involved tumor margins or widespread dysplasia is not an acceptable treatment approach,” the guideline authors noted.
There are two other new recommendations including the opinion, based on evidence of benefits vs. harms, that total laryngectomy rather than larynx preservation may be associated with better survival and quality of life in patients with extensive T3 lesions, large T4 lesions, or in those who have poor pretreatment laryngeal function.
The third new recommendation is that “[a]s part of a comprehensive pretreatment evaluation, all patients should undergo a baseline assessment of voice and swallowing function, voice (use and requirements), and counseling with regard to the potential effect of treatment options on voice, swallowing, and quality of life.”
Among the updated recommendations are the following:
• An emphasis on the importance of considering a multiplicity of factors when choosing therapy for patients with limited-stage disease (1.7).
• The option of specialized organ-preservation procedures for a small number of patients with T3 or T4 primary site disease (2.4).
• A strong recommendation for the use of concurrent chemoradiotherapy compared with radiotherapy alone or sequential therapy (2.5).
• Elective neck dissection is not required for patients with clinically involved regional cervical nodes treated with definitive radiotherapy of chemoradiotherapy who have complete clinical, radiologic, and metabolic imaging (3.3).
• “Selection of therapy for an individual patient requires assessment by the multidisciplinary team as well as consideration of voice and swallowing function; patient comorbidity, psychosocial situation, and preferences; and local therapeutic expertise” (4.2).
The guideline development process was supported by ASCO. Dr, Forastiere disclosed employment and stock ownership in NantHealth. Many of her coauthors disclosed institutional funding, consultation/advising, travel support and expenses, honoraria, and or patents/royalties with multiple entities.
FROM JCO
Potential postthyroidectomy quality improvement metrics arise from study
of U.S. hospitals, suggesting to the authors that these measures could be used for quality improvement metrics.
In the study, published Nov. 29 in JAMA Surgery, hospitals with significantly lower rates of hypocalcemia were more likely to conduct postoperative parathyroid hormone level measurement as well as to prescribe vitamin D, calcium supplements, or both. Hospitals with lower RLN injury rates more frequently used energy devices and intraoperative nerve monitoring.
“Causation cannot be proven by this, but the confidence that these practice parameters are important is high,” senior author Bruce Hall, MD, PhD, vice president and chief quality officer at BJC Healthcare, and professor of surgery at Washington University, St. Louis, said in an interview. Dr. Hall is consulting director for the American College of Surgeon’s National Surgical Quality Improvement Program (NSQIP), which provided data for the analysis (JAMA Surg. 2017 Nov 29. doi: 10.1001/jamasurg.2017.4593).
The researchers examined data from 14,540 patients who underwent thyroidectomies at 98 hospitals between Jan. 1, 2013, and Dec. 31, 2015. These included 13,242 operations at 96 hospitals with complete hypocalcemia data, 13,144 operations at 95 hospitals with complete RLN data, and 13,197 operations at 95 hospitals with complete hematoma data. The primary outcome was the 30-day incidence of hypocalcemia, RLN, and hematoma. The researchers also measured 30-day mortality, surgical site infections, and hospital readmissions.
A total of 3.3% of patients experienced clinically severe hypocalcemia (0.6% after partial thyroidectomy, 4.7% after total or subtotal thyroidectomy). Another 5.7% experienced RLN (4.2% after partial, 6.6% after total or subtotal). Hematoma occurred in 1.3% of cases, but there were no significant variations in rates of hematoma across participating institutions.
For hypocalcemia and RLN injury, there were hospital outliers both on the low end of complication rates and on the high end of complication rates, defined by odds ratios with 95% confidence ratios that were greater than 1 for high outliers, or lower than 1 for low outliers. There were no outliers with respect to hematoma, suggesting that it may not be a useful barometer of hospital performance.
With respect to hypocalcemia rates, four hospitals were low outliers, and seven were high. Eight hospitals were low outliers with respect to RLN injury, and 14 were high outliers.
In the analysis of postoperative hypocalcemia, both low and high outliers measured postoperative calcium with similar frequency (68.4% vs. 71.0%; P =.09). However, high performance outliers were more likely to prescribe postoperative calcium, vitamin D, or both (76.6% vs. 66.8%; P less than .001).
Among RLN outliers, intraoperative nerve monitoring was more common in the top performing hospitals (55.7% vs. 37.7%; P less than .001), as was the use of energy devices (69.1% vs. 55.2%; P less than .001).
There was one high outlier when it came to surgical site infections, and one high and one low outlier with respect to morbidity outcomes. There were no hospital readmission outliers.
No source of funding was disclosed. Dr. Liu and Dr. Hall reported having no financial disclosures.
of U.S. hospitals, suggesting to the authors that these measures could be used for quality improvement metrics.
In the study, published Nov. 29 in JAMA Surgery, hospitals with significantly lower rates of hypocalcemia were more likely to conduct postoperative parathyroid hormone level measurement as well as to prescribe vitamin D, calcium supplements, or both. Hospitals with lower RLN injury rates more frequently used energy devices and intraoperative nerve monitoring.
“Causation cannot be proven by this, but the confidence that these practice parameters are important is high,” senior author Bruce Hall, MD, PhD, vice president and chief quality officer at BJC Healthcare, and professor of surgery at Washington University, St. Louis, said in an interview. Dr. Hall is consulting director for the American College of Surgeon’s National Surgical Quality Improvement Program (NSQIP), which provided data for the analysis (JAMA Surg. 2017 Nov 29. doi: 10.1001/jamasurg.2017.4593).
The researchers examined data from 14,540 patients who underwent thyroidectomies at 98 hospitals between Jan. 1, 2013, and Dec. 31, 2015. These included 13,242 operations at 96 hospitals with complete hypocalcemia data, 13,144 operations at 95 hospitals with complete RLN data, and 13,197 operations at 95 hospitals with complete hematoma data. The primary outcome was the 30-day incidence of hypocalcemia, RLN, and hematoma. The researchers also measured 30-day mortality, surgical site infections, and hospital readmissions.
A total of 3.3% of patients experienced clinically severe hypocalcemia (0.6% after partial thyroidectomy, 4.7% after total or subtotal thyroidectomy). Another 5.7% experienced RLN (4.2% after partial, 6.6% after total or subtotal). Hematoma occurred in 1.3% of cases, but there were no significant variations in rates of hematoma across participating institutions.
For hypocalcemia and RLN injury, there were hospital outliers both on the low end of complication rates and on the high end of complication rates, defined by odds ratios with 95% confidence ratios that were greater than 1 for high outliers, or lower than 1 for low outliers. There were no outliers with respect to hematoma, suggesting that it may not be a useful barometer of hospital performance.
With respect to hypocalcemia rates, four hospitals were low outliers, and seven were high. Eight hospitals were low outliers with respect to RLN injury, and 14 were high outliers.
In the analysis of postoperative hypocalcemia, both low and high outliers measured postoperative calcium with similar frequency (68.4% vs. 71.0%; P =.09). However, high performance outliers were more likely to prescribe postoperative calcium, vitamin D, or both (76.6% vs. 66.8%; P less than .001).
Among RLN outliers, intraoperative nerve monitoring was more common in the top performing hospitals (55.7% vs. 37.7%; P less than .001), as was the use of energy devices (69.1% vs. 55.2%; P less than .001).
There was one high outlier when it came to surgical site infections, and one high and one low outlier with respect to morbidity outcomes. There were no hospital readmission outliers.
No source of funding was disclosed. Dr. Liu and Dr. Hall reported having no financial disclosures.
of U.S. hospitals, suggesting to the authors that these measures could be used for quality improvement metrics.
In the study, published Nov. 29 in JAMA Surgery, hospitals with significantly lower rates of hypocalcemia were more likely to conduct postoperative parathyroid hormone level measurement as well as to prescribe vitamin D, calcium supplements, or both. Hospitals with lower RLN injury rates more frequently used energy devices and intraoperative nerve monitoring.
“Causation cannot be proven by this, but the confidence that these practice parameters are important is high,” senior author Bruce Hall, MD, PhD, vice president and chief quality officer at BJC Healthcare, and professor of surgery at Washington University, St. Louis, said in an interview. Dr. Hall is consulting director for the American College of Surgeon’s National Surgical Quality Improvement Program (NSQIP), which provided data for the analysis (JAMA Surg. 2017 Nov 29. doi: 10.1001/jamasurg.2017.4593).
The researchers examined data from 14,540 patients who underwent thyroidectomies at 98 hospitals between Jan. 1, 2013, and Dec. 31, 2015. These included 13,242 operations at 96 hospitals with complete hypocalcemia data, 13,144 operations at 95 hospitals with complete RLN data, and 13,197 operations at 95 hospitals with complete hematoma data. The primary outcome was the 30-day incidence of hypocalcemia, RLN, and hematoma. The researchers also measured 30-day mortality, surgical site infections, and hospital readmissions.
A total of 3.3% of patients experienced clinically severe hypocalcemia (0.6% after partial thyroidectomy, 4.7% after total or subtotal thyroidectomy). Another 5.7% experienced RLN (4.2% after partial, 6.6% after total or subtotal). Hematoma occurred in 1.3% of cases, but there were no significant variations in rates of hematoma across participating institutions.
For hypocalcemia and RLN injury, there were hospital outliers both on the low end of complication rates and on the high end of complication rates, defined by odds ratios with 95% confidence ratios that were greater than 1 for high outliers, or lower than 1 for low outliers. There were no outliers with respect to hematoma, suggesting that it may not be a useful barometer of hospital performance.
With respect to hypocalcemia rates, four hospitals were low outliers, and seven were high. Eight hospitals were low outliers with respect to RLN injury, and 14 were high outliers.
In the analysis of postoperative hypocalcemia, both low and high outliers measured postoperative calcium with similar frequency (68.4% vs. 71.0%; P =.09). However, high performance outliers were more likely to prescribe postoperative calcium, vitamin D, or both (76.6% vs. 66.8%; P less than .001).
Among RLN outliers, intraoperative nerve monitoring was more common in the top performing hospitals (55.7% vs. 37.7%; P less than .001), as was the use of energy devices (69.1% vs. 55.2%; P less than .001).
There was one high outlier when it came to surgical site infections, and one high and one low outlier with respect to morbidity outcomes. There were no hospital readmission outliers.
No source of funding was disclosed. Dr. Liu and Dr. Hall reported having no financial disclosures.
FROM JAMA SURGERY
Key clinical point: Prescription of postoperative calcium, vitamin D, or both, and greater use of intraoperative nerve monitoring may lead to fewer adverse events after thyroidectomy.
Major finding: Both low and high outliers on 30-day rates of postoperative hypocalcemia measured postoperative calcium with similar frequency (68.4% vs. 71.0%; P =.09). However, high performance outliers were more likely to prescribe postoperative calcium, vitamin D, or both (76.6% vs. 66.8%; P less than .001).
Data source: Retrospective analysis of 14,540 patients at 98 hospitals in the American College of Surgeon’s National Surgical Quality Improvement Program.
Disclosures: No source of funding was disclosed. Dr. Liu and Dr. Hall reported having no financial disclosures.
Pancreatic surgery: Similar outcomes with primary anastomosis, allografts
Pancreatic tumor involvement with the superior mesenteric vein/portal vein (SMV/PV) is common and requires exploration and resection, which has now become an integral part of routine surgical treatment. The short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts was found to be comparable to that of reconstruction with primary end-to-end anastomosis, according to the results of a study performed by Dyre Kleive, MD, and his colleagues.
In order to assess the optimal method of reconstructing the portal vein during pancreatic surgery, Dr. Kleive and his colleagues performed a retrospective review of all patients undergoing pancreatic surgery with venous resection and reconstruction at a single center between January 2006 and December 2015.
A total of 857 patients underwent open pancreatic surgery during the study period, of whom 171 (20%) had vascular resection and reconstruction. The study population comprised 42 patients treated with cold-stored interposition cadaveric allografts for reconstruction and 71 patients who had primary end-to-end anastomosis instead. Patients with other forms of reconstruction were excluded, according to an online report in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.09.003).
Early failure at the reconstruction site was defined as the presence of thrombosis or no flow or low flow within the first 30 days after surgery.
Patients in the allograft group had statistically significantly longer mean operative times, more intraoperative bleeding, more frequent use of neoadjuvant therapy, and a longer length of tumor-vein involvement than the anastomosis group.
However, there was no statistically significant difference in the number of patients with major complications (42.9% for allografts vs. 36.6% for anastomosis) or early failure at the reconstruction site (9.5% for allografts vs. 8.5% for anastomosis) between the two groups, Dr Kleive and his colleagues reported.
The proportion of patients with grade C stenosis at last available imaging scan was significantly higher in the allograft group (26/42 [61.9%] vs. 13 of 66 [19.7%] for the anastomosis group; P less than .01). A subgroup analysis of 10 patients in the allograft group showed the presence of donor-specific antibodies in all patients. This could indicate that graft rejection was a contributing factor to the statistically higher development of severe stenosis in allograft vs. anastomosis patients, the authors suggested.
“This study shows that the short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts is comparable to that of reconstruction with primary end-to-end anastomosis,” the researchers concluded.
Dr. Kleive and his colleagues reported that they had no conflicts of interest.
Pancreatic tumor involvement with the superior mesenteric vein/portal vein (SMV/PV) is common and requires exploration and resection, which has now become an integral part of routine surgical treatment. The short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts was found to be comparable to that of reconstruction with primary end-to-end anastomosis, according to the results of a study performed by Dyre Kleive, MD, and his colleagues.
In order to assess the optimal method of reconstructing the portal vein during pancreatic surgery, Dr. Kleive and his colleagues performed a retrospective review of all patients undergoing pancreatic surgery with venous resection and reconstruction at a single center between January 2006 and December 2015.
A total of 857 patients underwent open pancreatic surgery during the study period, of whom 171 (20%) had vascular resection and reconstruction. The study population comprised 42 patients treated with cold-stored interposition cadaveric allografts for reconstruction and 71 patients who had primary end-to-end anastomosis instead. Patients with other forms of reconstruction were excluded, according to an online report in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.09.003).
Early failure at the reconstruction site was defined as the presence of thrombosis or no flow or low flow within the first 30 days after surgery.
Patients in the allograft group had statistically significantly longer mean operative times, more intraoperative bleeding, more frequent use of neoadjuvant therapy, and a longer length of tumor-vein involvement than the anastomosis group.
However, there was no statistically significant difference in the number of patients with major complications (42.9% for allografts vs. 36.6% for anastomosis) or early failure at the reconstruction site (9.5% for allografts vs. 8.5% for anastomosis) between the two groups, Dr Kleive and his colleagues reported.
The proportion of patients with grade C stenosis at last available imaging scan was significantly higher in the allograft group (26/42 [61.9%] vs. 13 of 66 [19.7%] for the anastomosis group; P less than .01). A subgroup analysis of 10 patients in the allograft group showed the presence of donor-specific antibodies in all patients. This could indicate that graft rejection was a contributing factor to the statistically higher development of severe stenosis in allograft vs. anastomosis patients, the authors suggested.
“This study shows that the short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts is comparable to that of reconstruction with primary end-to-end anastomosis,” the researchers concluded.
Dr. Kleive and his colleagues reported that they had no conflicts of interest.
Pancreatic tumor involvement with the superior mesenteric vein/portal vein (SMV/PV) is common and requires exploration and resection, which has now become an integral part of routine surgical treatment. The short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts was found to be comparable to that of reconstruction with primary end-to-end anastomosis, according to the results of a study performed by Dyre Kleive, MD, and his colleagues.
In order to assess the optimal method of reconstructing the portal vein during pancreatic surgery, Dr. Kleive and his colleagues performed a retrospective review of all patients undergoing pancreatic surgery with venous resection and reconstruction at a single center between January 2006 and December 2015.
A total of 857 patients underwent open pancreatic surgery during the study period, of whom 171 (20%) had vascular resection and reconstruction. The study population comprised 42 patients treated with cold-stored interposition cadaveric allografts for reconstruction and 71 patients who had primary end-to-end anastomosis instead. Patients with other forms of reconstruction were excluded, according to an online report in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.09.003).
Early failure at the reconstruction site was defined as the presence of thrombosis or no flow or low flow within the first 30 days after surgery.
Patients in the allograft group had statistically significantly longer mean operative times, more intraoperative bleeding, more frequent use of neoadjuvant therapy, and a longer length of tumor-vein involvement than the anastomosis group.
However, there was no statistically significant difference in the number of patients with major complications (42.9% for allografts vs. 36.6% for anastomosis) or early failure at the reconstruction site (9.5% for allografts vs. 8.5% for anastomosis) between the two groups, Dr Kleive and his colleagues reported.
The proportion of patients with grade C stenosis at last available imaging scan was significantly higher in the allograft group (26/42 [61.9%] vs. 13 of 66 [19.7%] for the anastomosis group; P less than .01). A subgroup analysis of 10 patients in the allograft group showed the presence of donor-specific antibodies in all patients. This could indicate that graft rejection was a contributing factor to the statistically higher development of severe stenosis in allograft vs. anastomosis patients, the authors suggested.
“This study shows that the short-term outcome of SMV/PV reconstruction with interposed cold-stored cadaveric venous allografts is comparable to that of reconstruction with primary end-to-end anastomosis,” the researchers concluded.
Dr. Kleive and his colleagues reported that they had no conflicts of interest.
FROM THE JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISEASES
Key clinical point:
Major finding: There was no statistically significant difference in the number of patients with major complications or early failure at the reconstruction site between the allograft and the anastomosis groups.
Data source: A retrospective review of all 171 patients undergoing pancreatic surgery with venous resection and reconstruction at a single center between January 2006 and December 2015.
Disclosures: The authors reported that they had no conflicts of interest.
CMS looking to evolve QPP to measure outcomes, not processes
WASHINGTON – The Quality Payment Program, the value-based payment scheme created under the Medicare Access and CHIP Reauthorization Act, will focus on measuring clinical outcomes – instead of processes – if Seema Verma, administrator of the Centers for Medicare & Medicaid Services, has her way.
“I think the concept of paying for value is a good concept,” Ms. Verma told attendees at the annual meeting of the federal Office of the National Coordinator for Health Information Technology on Dec. 1. “A lot of the measures in terms of how we are evaluating providers aren’t necessarily around outcomes. There are a lot of process measures.”
“Many of us have used the health care system and can attest that it is also a lot of times confusing,” she said. “We don’t know where to go for our care. Who is the best doctor? We don’t always have the information about cost or quality or value, and it is difficult to navigate the health care system.”
She said she wants to “make sure that the data that we have at CMS is available to our beneficiaries, whether it be information about their claims data, information about quality, information about the health plan that they may pick, information about their provider directory, information about the quality ratings if they are seeking hospice care.”
Getting to that point will require addressing an ongoing and familiar problem for physicians: interoperability of health care IT systems.
Improved interoperability would allow for greater patient empowerment by providing patients with better access to their own medical data, she said, noting that the data also belongs to the patient.
“That is our information and the patient should have that,” Ms. Verma said. “When we talk about patient empowerment and patients first, this is what we are talking about. This is what I mean. I want to make sure the beneficiaries who are using the Medicaid program, the Medicare program have this information. That is important.”
She also noted that improved interoperability will allow for greater use of data across the health care spectrum, including in the area of drug pricing.
“We have some very high-cost new drugs coming,” she noted. “We are having discussions about how to pay for these drugs in a different way. Maybe we are going [toward] value-based pricing or indication-based pricing [and] so paying for the drug based on the outcomes.”
WASHINGTON – The Quality Payment Program, the value-based payment scheme created under the Medicare Access and CHIP Reauthorization Act, will focus on measuring clinical outcomes – instead of processes – if Seema Verma, administrator of the Centers for Medicare & Medicaid Services, has her way.
“I think the concept of paying for value is a good concept,” Ms. Verma told attendees at the annual meeting of the federal Office of the National Coordinator for Health Information Technology on Dec. 1. “A lot of the measures in terms of how we are evaluating providers aren’t necessarily around outcomes. There are a lot of process measures.”
“Many of us have used the health care system and can attest that it is also a lot of times confusing,” she said. “We don’t know where to go for our care. Who is the best doctor? We don’t always have the information about cost or quality or value, and it is difficult to navigate the health care system.”
She said she wants to “make sure that the data that we have at CMS is available to our beneficiaries, whether it be information about their claims data, information about quality, information about the health plan that they may pick, information about their provider directory, information about the quality ratings if they are seeking hospice care.”
Getting to that point will require addressing an ongoing and familiar problem for physicians: interoperability of health care IT systems.
Improved interoperability would allow for greater patient empowerment by providing patients with better access to their own medical data, she said, noting that the data also belongs to the patient.
“That is our information and the patient should have that,” Ms. Verma said. “When we talk about patient empowerment and patients first, this is what we are talking about. This is what I mean. I want to make sure the beneficiaries who are using the Medicaid program, the Medicare program have this information. That is important.”
She also noted that improved interoperability will allow for greater use of data across the health care spectrum, including in the area of drug pricing.
“We have some very high-cost new drugs coming,” she noted. “We are having discussions about how to pay for these drugs in a different way. Maybe we are going [toward] value-based pricing or indication-based pricing [and] so paying for the drug based on the outcomes.”
WASHINGTON – The Quality Payment Program, the value-based payment scheme created under the Medicare Access and CHIP Reauthorization Act, will focus on measuring clinical outcomes – instead of processes – if Seema Verma, administrator of the Centers for Medicare & Medicaid Services, has her way.
“I think the concept of paying for value is a good concept,” Ms. Verma told attendees at the annual meeting of the federal Office of the National Coordinator for Health Information Technology on Dec. 1. “A lot of the measures in terms of how we are evaluating providers aren’t necessarily around outcomes. There are a lot of process measures.”
“Many of us have used the health care system and can attest that it is also a lot of times confusing,” she said. “We don’t know where to go for our care. Who is the best doctor? We don’t always have the information about cost or quality or value, and it is difficult to navigate the health care system.”
She said she wants to “make sure that the data that we have at CMS is available to our beneficiaries, whether it be information about their claims data, information about quality, information about the health plan that they may pick, information about their provider directory, information about the quality ratings if they are seeking hospice care.”
Getting to that point will require addressing an ongoing and familiar problem for physicians: interoperability of health care IT systems.
Improved interoperability would allow for greater patient empowerment by providing patients with better access to their own medical data, she said, noting that the data also belongs to the patient.
“That is our information and the patient should have that,” Ms. Verma said. “When we talk about patient empowerment and patients first, this is what we are talking about. This is what I mean. I want to make sure the beneficiaries who are using the Medicaid program, the Medicare program have this information. That is important.”
She also noted that improved interoperability will allow for greater use of data across the health care spectrum, including in the area of drug pricing.
“We have some very high-cost new drugs coming,” she noted. “We are having discussions about how to pay for these drugs in a different way. Maybe we are going [toward] value-based pricing or indication-based pricing [and] so paying for the drug based on the outcomes.”
AT ONC 2017
5 big ways the tax bill could affect health policy
Having failed to repeal and replace the Affordable Care Act, Congress is now working on a tax overhaul. But it turns out the tax bills in the House and Senate also aim to reshape health care.
Here are five big ways the tax bill could affect health policy:
1. Repeal the requirement for most people to have health insurance or pay a tax penalty
Republicans tried and failed to end the so-called individual mandate this year when they attempted to advance their health overhaul legislation. Now the idea is back, at least in the Senate’s version of the tax bill. The measure would not technically remove the requirement for people to have insurance, but it would eliminate the fine people would face if they choose to remain uninsured.
The Congressional Budget Office has estimated that dropping the requirement would result in 13 million fewer people having insurance over 10 years.
It also estimates that premiums would rise 10% more per year than they would without this change. That is because healthier people would be most likely to drop insurance in the absence of a fine, so insurers would have to raise premiums to compensate for a sicker group of customers. Those consumers, in turn, would be left with fewer affordable choices, according to the CBO.
State insurance officials are concerned that insurers will drop out of the individual market entirely if there is no requirement for healthy people to sign up, but they still have to sell to people who know they will need medical care.
Ironically, the states most likely to see this kind of insurance-market disruption are those that are reliably Republican. An analysis by the Los Angeles Times suggested that the states with the fewest insurers and the highest premiums – including Alaska, Iowa, Missouri, Nebraska, Nevada, and Wyoming – would be the ones left with either no coverage options or options too expensive for most consumers in the individual market.
2. Repeal the medical expense deduction
The House-passed tax bill, although not the Senate’s, would eliminate taxpayers’ ability to deduct medical expenses that exceed 10% of their adjusted gross income.
The medical expense deduction is not widely used – just under 9 million tax filers took it on their 2015 tax returns, according to the Internal Revenue Service. But those who do use it generally have very high medical expenses, often for a disabled child, a serious chronic illness, or expensive long-term care not covered by health insurance.
Among those most vehemently against getting rid of the deduction is the senior advocacy group AARP. Eliminating the deduction, the group said in a statement, “amounts to a health tax on millions of Americans with high medical costs – especially middle income seniors.”
3. Trigger major cuts to the Medicare program
The tax bill includes no specific Medicare changes, but budget analysts point out that passing it in its current form would trigger another law to kick in. That measure requires cuts to federal programs if the federal budget deficit is increased.
Because the tax bills in both the House and Senate would add an additional $1.5 trillion to the deficit over the next 10 years, both would result in automatic cuts under the Statutory Pay-As-You-Go Act of 2010 (PAYGO). According to the CBO, if Congress passes the tax bill and does not waive the PAYGO law, federal officials “would be required to issue a sequestration order within 15 days of the end of the session of Congress to reduce spending in fiscal year 2018 by the resultant total of $136 billion.”
Cuts to Medicare are limited under the PAYGO law, so the Medicare reduction would be limited to 4% of program spending, which is roughly $25 billion of that total. Cuts of a similar size would be required in future years. Most of that would likely come from payments to providers.
4. Change tax treatment for graduate students and those paying back student loans
The House bill, though not the Senate’s, would for the first time require graduate students to pay tax on the value of tuition that universities do not require them to pay.
Currently, graduate students in many fields, including science, often are paid a small stipend for teaching while they pursue advanced degrees. Many are technically charged tuition, but it is “waived” as long as they are working for the university.
The House tax bill would eliminate that waiver and require them to pay taxes on the full value of the tuition they don’t have to pay, which would result in many students with fairly low incomes seeing very large tax bills.
At the same time, the House tax bill would eliminate the deduction for interest paid on student loans. This would disproportionately affect young doctors.
According to the Association of American Medical Colleges, 75% of the medical school class of 2017 graduated with student loan debt, with nearly half owing $200,000 or more.
5. Change or eliminate the tax credit for rare disease drug development
Congress created the so-called Orphan Drug Credit in 1983, as part of a package of incentives intended to entice drugmakers to study and develop drugs to treat rare diseases, defined as those affecting fewer than 200,000 people. With such a small potential market, it does not otherwise make financial sense for the companies to spend the millions of dollars necessary to develop treatments for such ailments.
To date, about 500 drugs have come to market using the incentives, although in some cases drugmakers have manipulated the credit for extra financial gain.
The House tax bill would eliminate the tax credit; the Senate bill would scale it back. Sen. Orrin Hatch (R-Utah), chairman of the tax-writing Finance Committee, is one of the original sponsors of the orphan drug law.
The drug industry has been relatively quiet about the potential loss of the credit, but the National Organization for Rare Disorders called the change “wholly unacceptable” and said it “would directly result in 33% fewer orphan drugs coming to market.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Having failed to repeal and replace the Affordable Care Act, Congress is now working on a tax overhaul. But it turns out the tax bills in the House and Senate also aim to reshape health care.
Here are five big ways the tax bill could affect health policy:
1. Repeal the requirement for most people to have health insurance or pay a tax penalty
Republicans tried and failed to end the so-called individual mandate this year when they attempted to advance their health overhaul legislation. Now the idea is back, at least in the Senate’s version of the tax bill. The measure would not technically remove the requirement for people to have insurance, but it would eliminate the fine people would face if they choose to remain uninsured.
The Congressional Budget Office has estimated that dropping the requirement would result in 13 million fewer people having insurance over 10 years.
It also estimates that premiums would rise 10% more per year than they would without this change. That is because healthier people would be most likely to drop insurance in the absence of a fine, so insurers would have to raise premiums to compensate for a sicker group of customers. Those consumers, in turn, would be left with fewer affordable choices, according to the CBO.
State insurance officials are concerned that insurers will drop out of the individual market entirely if there is no requirement for healthy people to sign up, but they still have to sell to people who know they will need medical care.
Ironically, the states most likely to see this kind of insurance-market disruption are those that are reliably Republican. An analysis by the Los Angeles Times suggested that the states with the fewest insurers and the highest premiums – including Alaska, Iowa, Missouri, Nebraska, Nevada, and Wyoming – would be the ones left with either no coverage options or options too expensive for most consumers in the individual market.
2. Repeal the medical expense deduction
The House-passed tax bill, although not the Senate’s, would eliminate taxpayers’ ability to deduct medical expenses that exceed 10% of their adjusted gross income.
The medical expense deduction is not widely used – just under 9 million tax filers took it on their 2015 tax returns, according to the Internal Revenue Service. But those who do use it generally have very high medical expenses, often for a disabled child, a serious chronic illness, or expensive long-term care not covered by health insurance.
Among those most vehemently against getting rid of the deduction is the senior advocacy group AARP. Eliminating the deduction, the group said in a statement, “amounts to a health tax on millions of Americans with high medical costs – especially middle income seniors.”
3. Trigger major cuts to the Medicare program
The tax bill includes no specific Medicare changes, but budget analysts point out that passing it in its current form would trigger another law to kick in. That measure requires cuts to federal programs if the federal budget deficit is increased.
Because the tax bills in both the House and Senate would add an additional $1.5 trillion to the deficit over the next 10 years, both would result in automatic cuts under the Statutory Pay-As-You-Go Act of 2010 (PAYGO). According to the CBO, if Congress passes the tax bill and does not waive the PAYGO law, federal officials “would be required to issue a sequestration order within 15 days of the end of the session of Congress to reduce spending in fiscal year 2018 by the resultant total of $136 billion.”
Cuts to Medicare are limited under the PAYGO law, so the Medicare reduction would be limited to 4% of program spending, which is roughly $25 billion of that total. Cuts of a similar size would be required in future years. Most of that would likely come from payments to providers.
4. Change tax treatment for graduate students and those paying back student loans
The House bill, though not the Senate’s, would for the first time require graduate students to pay tax on the value of tuition that universities do not require them to pay.
Currently, graduate students in many fields, including science, often are paid a small stipend for teaching while they pursue advanced degrees. Many are technically charged tuition, but it is “waived” as long as they are working for the university.
The House tax bill would eliminate that waiver and require them to pay taxes on the full value of the tuition they don’t have to pay, which would result in many students with fairly low incomes seeing very large tax bills.
At the same time, the House tax bill would eliminate the deduction for interest paid on student loans. This would disproportionately affect young doctors.
According to the Association of American Medical Colleges, 75% of the medical school class of 2017 graduated with student loan debt, with nearly half owing $200,000 or more.
5. Change or eliminate the tax credit for rare disease drug development
Congress created the so-called Orphan Drug Credit in 1983, as part of a package of incentives intended to entice drugmakers to study and develop drugs to treat rare diseases, defined as those affecting fewer than 200,000 people. With such a small potential market, it does not otherwise make financial sense for the companies to spend the millions of dollars necessary to develop treatments for such ailments.
To date, about 500 drugs have come to market using the incentives, although in some cases drugmakers have manipulated the credit for extra financial gain.
The House tax bill would eliminate the tax credit; the Senate bill would scale it back. Sen. Orrin Hatch (R-Utah), chairman of the tax-writing Finance Committee, is one of the original sponsors of the orphan drug law.
The drug industry has been relatively quiet about the potential loss of the credit, but the National Organization for Rare Disorders called the change “wholly unacceptable” and said it “would directly result in 33% fewer orphan drugs coming to market.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Having failed to repeal and replace the Affordable Care Act, Congress is now working on a tax overhaul. But it turns out the tax bills in the House and Senate also aim to reshape health care.
Here are five big ways the tax bill could affect health policy:
1. Repeal the requirement for most people to have health insurance or pay a tax penalty
Republicans tried and failed to end the so-called individual mandate this year when they attempted to advance their health overhaul legislation. Now the idea is back, at least in the Senate’s version of the tax bill. The measure would not technically remove the requirement for people to have insurance, but it would eliminate the fine people would face if they choose to remain uninsured.
The Congressional Budget Office has estimated that dropping the requirement would result in 13 million fewer people having insurance over 10 years.
It also estimates that premiums would rise 10% more per year than they would without this change. That is because healthier people would be most likely to drop insurance in the absence of a fine, so insurers would have to raise premiums to compensate for a sicker group of customers. Those consumers, in turn, would be left with fewer affordable choices, according to the CBO.
State insurance officials are concerned that insurers will drop out of the individual market entirely if there is no requirement for healthy people to sign up, but they still have to sell to people who know they will need medical care.
Ironically, the states most likely to see this kind of insurance-market disruption are those that are reliably Republican. An analysis by the Los Angeles Times suggested that the states with the fewest insurers and the highest premiums – including Alaska, Iowa, Missouri, Nebraska, Nevada, and Wyoming – would be the ones left with either no coverage options or options too expensive for most consumers in the individual market.
2. Repeal the medical expense deduction
The House-passed tax bill, although not the Senate’s, would eliminate taxpayers’ ability to deduct medical expenses that exceed 10% of their adjusted gross income.
The medical expense deduction is not widely used – just under 9 million tax filers took it on their 2015 tax returns, according to the Internal Revenue Service. But those who do use it generally have very high medical expenses, often for a disabled child, a serious chronic illness, or expensive long-term care not covered by health insurance.
Among those most vehemently against getting rid of the deduction is the senior advocacy group AARP. Eliminating the deduction, the group said in a statement, “amounts to a health tax on millions of Americans with high medical costs – especially middle income seniors.”
3. Trigger major cuts to the Medicare program
The tax bill includes no specific Medicare changes, but budget analysts point out that passing it in its current form would trigger another law to kick in. That measure requires cuts to federal programs if the federal budget deficit is increased.
Because the tax bills in both the House and Senate would add an additional $1.5 trillion to the deficit over the next 10 years, both would result in automatic cuts under the Statutory Pay-As-You-Go Act of 2010 (PAYGO). According to the CBO, if Congress passes the tax bill and does not waive the PAYGO law, federal officials “would be required to issue a sequestration order within 15 days of the end of the session of Congress to reduce spending in fiscal year 2018 by the resultant total of $136 billion.”
Cuts to Medicare are limited under the PAYGO law, so the Medicare reduction would be limited to 4% of program spending, which is roughly $25 billion of that total. Cuts of a similar size would be required in future years. Most of that would likely come from payments to providers.
4. Change tax treatment for graduate students and those paying back student loans
The House bill, though not the Senate’s, would for the first time require graduate students to pay tax on the value of tuition that universities do not require them to pay.
Currently, graduate students in many fields, including science, often are paid a small stipend for teaching while they pursue advanced degrees. Many are technically charged tuition, but it is “waived” as long as they are working for the university.
The House tax bill would eliminate that waiver and require them to pay taxes on the full value of the tuition they don’t have to pay, which would result in many students with fairly low incomes seeing very large tax bills.
At the same time, the House tax bill would eliminate the deduction for interest paid on student loans. This would disproportionately affect young doctors.
According to the Association of American Medical Colleges, 75% of the medical school class of 2017 graduated with student loan debt, with nearly half owing $200,000 or more.
5. Change or eliminate the tax credit for rare disease drug development
Congress created the so-called Orphan Drug Credit in 1983, as part of a package of incentives intended to entice drugmakers to study and develop drugs to treat rare diseases, defined as those affecting fewer than 200,000 people. With such a small potential market, it does not otherwise make financial sense for the companies to spend the millions of dollars necessary to develop treatments for such ailments.
To date, about 500 drugs have come to market using the incentives, although in some cases drugmakers have manipulated the credit for extra financial gain.
The House tax bill would eliminate the tax credit; the Senate bill would scale it back. Sen. Orrin Hatch (R-Utah), chairman of the tax-writing Finance Committee, is one of the original sponsors of the orphan drug law.
The drug industry has been relatively quiet about the potential loss of the credit, but the National Organization for Rare Disorders called the change “wholly unacceptable” and said it “would directly result in 33% fewer orphan drugs coming to market.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Drug prices a key focus of Senate HELP examination of Azar nomination
WASHINGTON Escalating drug prices topped the agenda as members of the Senate Health, Education, Labor & Pensions Committee interviewed Alex Azar regarding his nomination as secretary of the Department of Health & Human Services.
Mr. Azar, a former HHS deputy secretary and general counsel during the Bush Administration and a former president of Eli Lilly’s U.S. operations, outlined his priorities to the Senate HELP committee during the Nov. 29 hearing.
Drug prices were the focus of many senators’ questions, and while many contentious questions came from panel Democrats, Sen. Rand Paul (R-Ky.) signaled he was not yet on board with his approval for Mr. Azar’s nomination.
“I think many [Americans] perceive [that drug companies use] their economic might to manipulate the system to maximize profits,” Sen. Paul said. “It’s not like they are selling a cheaper product to more people. They are using government to maximize their profits. Do you acknowledge that, under the current system, Big Pharma uses their economic clout to manipulate the patent system to increase drug prices?”
“There are clearly abuses, Senator, in the system, and that is why one of the steps that I mentioned ... that I believe we have to go after, is the gaming of that,” Mr. Azar responded. He suggested that although Hatch-Waxman rules give innovators a time frame to exclusively sell products “there should be a certain moment” when full generic competition should begin.
Sen. Paul also challenged Mr. Azar on the notion of drug importation.
There has not been a successful path to certify that drugs being imported are “safe and reliable,” Mr. Azar noted.
Sen. Paul countered that “you would have to sit there and say that the European Union has unsafe drugs. It would be unsafe for Americans to buy drugs from the European Union or from Canada or Australia. It’s just frankly not true.”
Sen. Paul told Mr. Azar that if he cannot come up with a way to reimport drugs as a means of addressing the high cost of pharmaceuticals in the United States, “I can’t support you.”
Sen. Paul continued that a lot of people have talked about how they are going to change the system, particularly patent issues that stand in the way of generic competition, and “you’ve got some convincing to make me believe that you are going to represent the American people and not Big Pharma, and I know that’s insulting, and I don’t mean it to be because I am sure you are an honest and upright person. But we all have our doubts because Big Pharma manipulates the system to keep prices high. ... We’ve got to fix it. We can’t tepidly go at it. We have to really fix it, and you need to convince those of us who are skeptical that you will be part of fixing it and won’t be beholden to Big Pharma.”
Regarding his other priorities, Mr. Azar noted that, through his “experience helping to implement [Medicare] Part D and with my extensive knowledge of how insurance, manufacturers, pharmacy, and government programs work together, I believe I can bring the skills and experiences to the table that can help us address these issues, while still encouraging discovery so Americans have access to high-quality care.”
He called for making health care “more affordable, more available, and more tailored to what individuals want and need. … Under the status quo, premiums have been skyrocketing year after year, and choices have been dwindling. We must address these challenges for those who have insurance coverage and for those who have been pushed out or left out of the insurance market by the Affordable Care Act.”
Mr. Azar signaled that he will continue the push toward value-based care and will use the power of Medicare to lead the rest of the health care delivery system to follow suit.
“We can better channel the power of health information technology and leverage what is best in our programs and in the private competitive marketplace to ensure the individual patient is the center of decision making and his or her needs are being met with greater transparency and accountability.”
Regarding the opioid crisis, Mr. Azar said that “we must heed President Trump’s call to action and tackle the scourge of the opioid epidemic that is destroying so many individuals, families, and communities. We need aggressive prevention, education, regulatory, and enforcement efforts to stop overprescribing and overuse of these legal and illegal drugs. And we need compassionate treatment for those suffering from dependence and addiction.”
Mr. Azar also was challenged on women’s health issues, particularly the ability of employers to exclude health insurance coverage of contraception because of religious objections. He noted that there needs to be a balance between the medical needs of the patient and the rights of an organization to follow its conscience.
When queried about making contraception available over the counter, he noted that the regulations regarding OTC conversion are outdated, and he was encouraged that FDA Commissioner Scott Gottlieb, MD, is looking into that.
Mr. Azar also committed during the hearing to working with improving interoperability of electronic health records as well as working with physicians to reduce the associated documentation burden.
He voiced his support of reforming the Affordable Care Act, adding that, “if it remains the law, my goal is to implement a way that leads to affordable insurance, leads to choice of insurance that leads to real access and not a meaningless insurance care, and insurance that has the benefits that people want, not what we say in D.C. for them.”
He also expressed support for the use of block grants to help fund Medicaid.
Mr. Azar’s appearance before the HELP committee was a courtesy as the Senate Finance Committee holds jurisdiction over his nomination. No confirmation hearing had been scheduled at press time.
WASHINGTON Escalating drug prices topped the agenda as members of the Senate Health, Education, Labor & Pensions Committee interviewed Alex Azar regarding his nomination as secretary of the Department of Health & Human Services.
Mr. Azar, a former HHS deputy secretary and general counsel during the Bush Administration and a former president of Eli Lilly’s U.S. operations, outlined his priorities to the Senate HELP committee during the Nov. 29 hearing.
Drug prices were the focus of many senators’ questions, and while many contentious questions came from panel Democrats, Sen. Rand Paul (R-Ky.) signaled he was not yet on board with his approval for Mr. Azar’s nomination.
“I think many [Americans] perceive [that drug companies use] their economic might to manipulate the system to maximize profits,” Sen. Paul said. “It’s not like they are selling a cheaper product to more people. They are using government to maximize their profits. Do you acknowledge that, under the current system, Big Pharma uses their economic clout to manipulate the patent system to increase drug prices?”
“There are clearly abuses, Senator, in the system, and that is why one of the steps that I mentioned ... that I believe we have to go after, is the gaming of that,” Mr. Azar responded. He suggested that although Hatch-Waxman rules give innovators a time frame to exclusively sell products “there should be a certain moment” when full generic competition should begin.
Sen. Paul also challenged Mr. Azar on the notion of drug importation.
There has not been a successful path to certify that drugs being imported are “safe and reliable,” Mr. Azar noted.
Sen. Paul countered that “you would have to sit there and say that the European Union has unsafe drugs. It would be unsafe for Americans to buy drugs from the European Union or from Canada or Australia. It’s just frankly not true.”
Sen. Paul told Mr. Azar that if he cannot come up with a way to reimport drugs as a means of addressing the high cost of pharmaceuticals in the United States, “I can’t support you.”
Sen. Paul continued that a lot of people have talked about how they are going to change the system, particularly patent issues that stand in the way of generic competition, and “you’ve got some convincing to make me believe that you are going to represent the American people and not Big Pharma, and I know that’s insulting, and I don’t mean it to be because I am sure you are an honest and upright person. But we all have our doubts because Big Pharma manipulates the system to keep prices high. ... We’ve got to fix it. We can’t tepidly go at it. We have to really fix it, and you need to convince those of us who are skeptical that you will be part of fixing it and won’t be beholden to Big Pharma.”
Regarding his other priorities, Mr. Azar noted that, through his “experience helping to implement [Medicare] Part D and with my extensive knowledge of how insurance, manufacturers, pharmacy, and government programs work together, I believe I can bring the skills and experiences to the table that can help us address these issues, while still encouraging discovery so Americans have access to high-quality care.”
He called for making health care “more affordable, more available, and more tailored to what individuals want and need. … Under the status quo, premiums have been skyrocketing year after year, and choices have been dwindling. We must address these challenges for those who have insurance coverage and for those who have been pushed out or left out of the insurance market by the Affordable Care Act.”
Mr. Azar signaled that he will continue the push toward value-based care and will use the power of Medicare to lead the rest of the health care delivery system to follow suit.
“We can better channel the power of health information technology and leverage what is best in our programs and in the private competitive marketplace to ensure the individual patient is the center of decision making and his or her needs are being met with greater transparency and accountability.”
Regarding the opioid crisis, Mr. Azar said that “we must heed President Trump’s call to action and tackle the scourge of the opioid epidemic that is destroying so many individuals, families, and communities. We need aggressive prevention, education, regulatory, and enforcement efforts to stop overprescribing and overuse of these legal and illegal drugs. And we need compassionate treatment for those suffering from dependence and addiction.”
Mr. Azar also was challenged on women’s health issues, particularly the ability of employers to exclude health insurance coverage of contraception because of religious objections. He noted that there needs to be a balance between the medical needs of the patient and the rights of an organization to follow its conscience.
When queried about making contraception available over the counter, he noted that the regulations regarding OTC conversion are outdated, and he was encouraged that FDA Commissioner Scott Gottlieb, MD, is looking into that.
Mr. Azar also committed during the hearing to working with improving interoperability of electronic health records as well as working with physicians to reduce the associated documentation burden.
He voiced his support of reforming the Affordable Care Act, adding that, “if it remains the law, my goal is to implement a way that leads to affordable insurance, leads to choice of insurance that leads to real access and not a meaningless insurance care, and insurance that has the benefits that people want, not what we say in D.C. for them.”
He also expressed support for the use of block grants to help fund Medicaid.
Mr. Azar’s appearance before the HELP committee was a courtesy as the Senate Finance Committee holds jurisdiction over his nomination. No confirmation hearing had been scheduled at press time.
WASHINGTON Escalating drug prices topped the agenda as members of the Senate Health, Education, Labor & Pensions Committee interviewed Alex Azar regarding his nomination as secretary of the Department of Health & Human Services.
Mr. Azar, a former HHS deputy secretary and general counsel during the Bush Administration and a former president of Eli Lilly’s U.S. operations, outlined his priorities to the Senate HELP committee during the Nov. 29 hearing.
Drug prices were the focus of many senators’ questions, and while many contentious questions came from panel Democrats, Sen. Rand Paul (R-Ky.) signaled he was not yet on board with his approval for Mr. Azar’s nomination.
“I think many [Americans] perceive [that drug companies use] their economic might to manipulate the system to maximize profits,” Sen. Paul said. “It’s not like they are selling a cheaper product to more people. They are using government to maximize their profits. Do you acknowledge that, under the current system, Big Pharma uses their economic clout to manipulate the patent system to increase drug prices?”
“There are clearly abuses, Senator, in the system, and that is why one of the steps that I mentioned ... that I believe we have to go after, is the gaming of that,” Mr. Azar responded. He suggested that although Hatch-Waxman rules give innovators a time frame to exclusively sell products “there should be a certain moment” when full generic competition should begin.
Sen. Paul also challenged Mr. Azar on the notion of drug importation.
There has not been a successful path to certify that drugs being imported are “safe and reliable,” Mr. Azar noted.
Sen. Paul countered that “you would have to sit there and say that the European Union has unsafe drugs. It would be unsafe for Americans to buy drugs from the European Union or from Canada or Australia. It’s just frankly not true.”
Sen. Paul told Mr. Azar that if he cannot come up with a way to reimport drugs as a means of addressing the high cost of pharmaceuticals in the United States, “I can’t support you.”
Sen. Paul continued that a lot of people have talked about how they are going to change the system, particularly patent issues that stand in the way of generic competition, and “you’ve got some convincing to make me believe that you are going to represent the American people and not Big Pharma, and I know that’s insulting, and I don’t mean it to be because I am sure you are an honest and upright person. But we all have our doubts because Big Pharma manipulates the system to keep prices high. ... We’ve got to fix it. We can’t tepidly go at it. We have to really fix it, and you need to convince those of us who are skeptical that you will be part of fixing it and won’t be beholden to Big Pharma.”
Regarding his other priorities, Mr. Azar noted that, through his “experience helping to implement [Medicare] Part D and with my extensive knowledge of how insurance, manufacturers, pharmacy, and government programs work together, I believe I can bring the skills and experiences to the table that can help us address these issues, while still encouraging discovery so Americans have access to high-quality care.”
He called for making health care “more affordable, more available, and more tailored to what individuals want and need. … Under the status quo, premiums have been skyrocketing year after year, and choices have been dwindling. We must address these challenges for those who have insurance coverage and for those who have been pushed out or left out of the insurance market by the Affordable Care Act.”
Mr. Azar signaled that he will continue the push toward value-based care and will use the power of Medicare to lead the rest of the health care delivery system to follow suit.
“We can better channel the power of health information technology and leverage what is best in our programs and in the private competitive marketplace to ensure the individual patient is the center of decision making and his or her needs are being met with greater transparency and accountability.”
Regarding the opioid crisis, Mr. Azar said that “we must heed President Trump’s call to action and tackle the scourge of the opioid epidemic that is destroying so many individuals, families, and communities. We need aggressive prevention, education, regulatory, and enforcement efforts to stop overprescribing and overuse of these legal and illegal drugs. And we need compassionate treatment for those suffering from dependence and addiction.”
Mr. Azar also was challenged on women’s health issues, particularly the ability of employers to exclude health insurance coverage of contraception because of religious objections. He noted that there needs to be a balance between the medical needs of the patient and the rights of an organization to follow its conscience.
When queried about making contraception available over the counter, he noted that the regulations regarding OTC conversion are outdated, and he was encouraged that FDA Commissioner Scott Gottlieb, MD, is looking into that.
Mr. Azar also committed during the hearing to working with improving interoperability of electronic health records as well as working with physicians to reduce the associated documentation burden.
He voiced his support of reforming the Affordable Care Act, adding that, “if it remains the law, my goal is to implement a way that leads to affordable insurance, leads to choice of insurance that leads to real access and not a meaningless insurance care, and insurance that has the benefits that people want, not what we say in D.C. for them.”
He also expressed support for the use of block grants to help fund Medicaid.
Mr. Azar’s appearance before the HELP committee was a courtesy as the Senate Finance Committee holds jurisdiction over his nomination. No confirmation hearing had been scheduled at press time.
AT A SENATE HELP COMMITTEE HEARING
HealthCare.gov seeing more action this fall
Four weeks into the open enrollment for 2018, the number of health insurance plans selected through HealthCare.gov is up by 30% over the first 4 weeks of the 2017 sign-up period, according to data from the Centers for Medicare & Medicaid Services.
From Nov. 1 to Nov. 25 of this year, 2.78 million plans for 2018 were selected on the 39 state marketplaces that use the HealthCare.gov platform, the CMS reported Nov. 29, compared with the 2.14 million plans for 2017 selected from Nov. 1 to Nov. 26 of last year.
Last year, the enrollment numbers were released only every 2 weeks, so direct week-to-week comparisons are not possible. Looking at 2-week periods, however, shows that, despite a drop in the number of selections from the first to the second biweekly period this year, weeks 3 and 4 were still up considerably over last year.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” the CMS noted. Also, “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”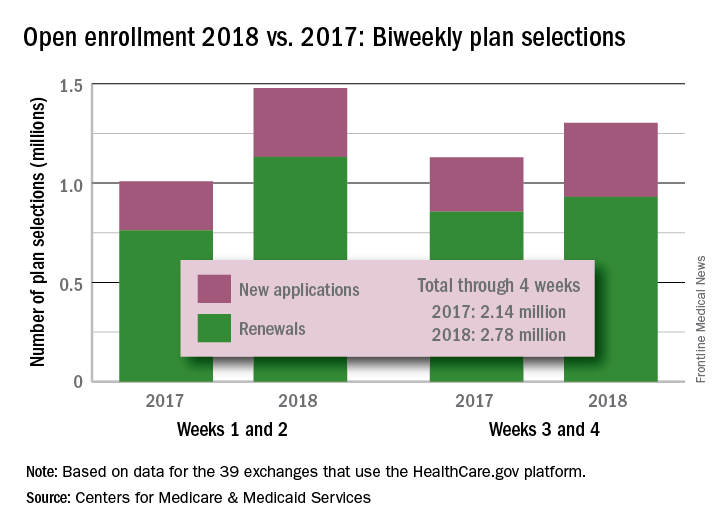
Four weeks into the open enrollment for 2018, the number of health insurance plans selected through HealthCare.gov is up by 30% over the first 4 weeks of the 2017 sign-up period, according to data from the Centers for Medicare & Medicaid Services.
From Nov. 1 to Nov. 25 of this year, 2.78 million plans for 2018 were selected on the 39 state marketplaces that use the HealthCare.gov platform, the CMS reported Nov. 29, compared with the 2.14 million plans for 2017 selected from Nov. 1 to Nov. 26 of last year.
Last year, the enrollment numbers were released only every 2 weeks, so direct week-to-week comparisons are not possible. Looking at 2-week periods, however, shows that, despite a drop in the number of selections from the first to the second biweekly period this year, weeks 3 and 4 were still up considerably over last year.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” the CMS noted. Also, “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”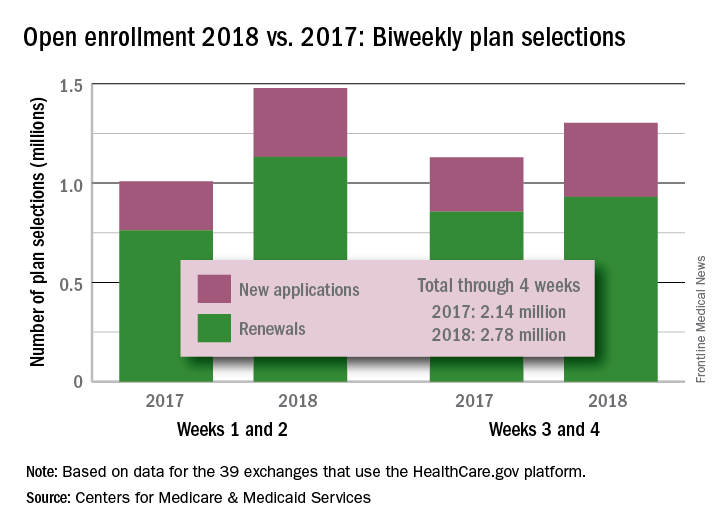
Four weeks into the open enrollment for 2018, the number of health insurance plans selected through HealthCare.gov is up by 30% over the first 4 weeks of the 2017 sign-up period, according to data from the Centers for Medicare & Medicaid Services.
From Nov. 1 to Nov. 25 of this year, 2.78 million plans for 2018 were selected on the 39 state marketplaces that use the HealthCare.gov platform, the CMS reported Nov. 29, compared with the 2.14 million plans for 2017 selected from Nov. 1 to Nov. 26 of last year.
Last year, the enrollment numbers were released only every 2 weeks, so direct week-to-week comparisons are not possible. Looking at 2-week periods, however, shows that, despite a drop in the number of selections from the first to the second biweekly period this year, weeks 3 and 4 were still up considerably over last year.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” the CMS noted. Also, “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”