User login
Official Newspaper of the American College of Surgeons
‘Right to try’ bill passes House
Terminal patients who have exhausted all approved drug options would be able to seek out investigational treatments – even if they do not qualify for clinical trials – under a bill passed in the U.S. House, despite opposition from more than 100 patient and physician groups.
The Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina
For an unapproved drug to be made available to patients, it must have an active application that is not subject to any kind of clinical hold. Sponsors and manufacturers must notify the Food and Drug Administration when an unapproved drug is made available to the patient.
The bill also includes safeguards to prevent manufacturers from purposefully misbranding or mislabeling drugs.
H.R. 5247 provides liability protections to manufacturers, sponsors, physicians, clinical investigators, and hospitals that participate in providing experimental drugs to terminal patients through this new alternative pathway, although it does not shield them from liability stemming from reckless misconduct, gross negligence, or any other intentional violations. It requires sponsors and manufacturers to report all adverse events to the FDA.
It also provides certainty to manufacturers as to how the FDA will use patient outcomes from the use of treatments outside of clinical trials when it is evaluating the applications on these new drugs.
Rep. Michael Burgess (R-Tex.), the House Energy & Commerce Health Subcommittee chairman and a physician, spoke in support of the bill during a debate on the House floor.
“Mr. Speaker, as a physician, I understand that access to investigational drugs and therapies is a deeply personal priority for those seeking treatment for their loved ones with serious, life-threatening conditions,” he said. “To my friends on the other side of the aisle, I have a simple question: Why do you not want to allow these patients to exercise their right to fight for their future?”
Rep. Frank Pallone (D-N.J.), the top-ranking Democrat on the House Energy & Commerce Committee, responded by asking, “if this is such a patient-centered bill, then why does every major patient organization overwhelmingly oppose it?”
In a March 19 letter to congressional leaders, a coalition of more than 100 physician and patient advocacy groups called the alternative pathway laid out in legislation “less safe” for patients than the FDA’s current expanded access process.
“This alternative pathway would allow for a 7-day lag between access to investigational therapies (as well as potential ensuing adverse effects) and FDA notification. FDA also is prohibited from halting access to these experimental therapies short of placing a clinical hold on all clinical research on the therapy in question, which is a blunt and disproportionate measure. The legislation would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program,” the groups wrote.
The groups that signed the letter included the American Society of Clinical Oncology, the Cystic Fibrosis Foundation, Friends of Cancer Research, the Leukemia & Lymphoma Society, the National Comprehensive Cancer Network, the National Organization for Rare Disorders, the Platelet Disorder Support Association, and Vietnam Veterans of America.
“The current compassionate use program at the Food and Drug Administration does make a good faith effort to help patients who do not qualify for clinical trials,” Rep. Burgess said. “But ‘right to try’ would actually offer patients an alternative pathway to access eligible investigational drugs, so long as they are certified by a physician who is in good standing and abides by the rules laid out in the bill.”
But Rep. Pallone noted that a review by the Government Accountability Office found that the FDA approves 99% of the requests submitted to the agency. Of the nearly 1,700 requests the FDA received in 2017, just 9 were not approved. However, the agency also adjusted applications for 11% of the patients in order to improve patient safety protections and that type of review should be allowed to continue, he said.
Patient groups expressed disappointment following the House vote. “The House has voted for a proposal that would create a less-safe, redundant pathway for accessing investigational therapies outside of clinical trials,” the National Organization for Rare Disorders said in a statement. “We hope the Senate will recognize that patients deserve legislation that will genuinely increase access. For example, senators should focus on legislation that reduces the financial disincentives companies encounter in offering their therapy through expanded access.”
The Senate passed a version of “right to try” in 2017 through the unanimous consent process (S. 204). No schedule has been set yet to either combine the two bills in committee or for the Senate to take up the House bill. President Trump voiced support for “right to try” legislation during his 2018 State of the Union address.
Terminal patients who have exhausted all approved drug options would be able to seek out investigational treatments – even if they do not qualify for clinical trials – under a bill passed in the U.S. House, despite opposition from more than 100 patient and physician groups.
The Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina
For an unapproved drug to be made available to patients, it must have an active application that is not subject to any kind of clinical hold. Sponsors and manufacturers must notify the Food and Drug Administration when an unapproved drug is made available to the patient.
The bill also includes safeguards to prevent manufacturers from purposefully misbranding or mislabeling drugs.
H.R. 5247 provides liability protections to manufacturers, sponsors, physicians, clinical investigators, and hospitals that participate in providing experimental drugs to terminal patients through this new alternative pathway, although it does not shield them from liability stemming from reckless misconduct, gross negligence, or any other intentional violations. It requires sponsors and manufacturers to report all adverse events to the FDA.
It also provides certainty to manufacturers as to how the FDA will use patient outcomes from the use of treatments outside of clinical trials when it is evaluating the applications on these new drugs.
Rep. Michael Burgess (R-Tex.), the House Energy & Commerce Health Subcommittee chairman and a physician, spoke in support of the bill during a debate on the House floor.
“Mr. Speaker, as a physician, I understand that access to investigational drugs and therapies is a deeply personal priority for those seeking treatment for their loved ones with serious, life-threatening conditions,” he said. “To my friends on the other side of the aisle, I have a simple question: Why do you not want to allow these patients to exercise their right to fight for their future?”
Rep. Frank Pallone (D-N.J.), the top-ranking Democrat on the House Energy & Commerce Committee, responded by asking, “if this is such a patient-centered bill, then why does every major patient organization overwhelmingly oppose it?”
In a March 19 letter to congressional leaders, a coalition of more than 100 physician and patient advocacy groups called the alternative pathway laid out in legislation “less safe” for patients than the FDA’s current expanded access process.
“This alternative pathway would allow for a 7-day lag between access to investigational therapies (as well as potential ensuing adverse effects) and FDA notification. FDA also is prohibited from halting access to these experimental therapies short of placing a clinical hold on all clinical research on the therapy in question, which is a blunt and disproportionate measure. The legislation would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program,” the groups wrote.
The groups that signed the letter included the American Society of Clinical Oncology, the Cystic Fibrosis Foundation, Friends of Cancer Research, the Leukemia & Lymphoma Society, the National Comprehensive Cancer Network, the National Organization for Rare Disorders, the Platelet Disorder Support Association, and Vietnam Veterans of America.
“The current compassionate use program at the Food and Drug Administration does make a good faith effort to help patients who do not qualify for clinical trials,” Rep. Burgess said. “But ‘right to try’ would actually offer patients an alternative pathway to access eligible investigational drugs, so long as they are certified by a physician who is in good standing and abides by the rules laid out in the bill.”
But Rep. Pallone noted that a review by the Government Accountability Office found that the FDA approves 99% of the requests submitted to the agency. Of the nearly 1,700 requests the FDA received in 2017, just 9 were not approved. However, the agency also adjusted applications for 11% of the patients in order to improve patient safety protections and that type of review should be allowed to continue, he said.
Patient groups expressed disappointment following the House vote. “The House has voted for a proposal that would create a less-safe, redundant pathway for accessing investigational therapies outside of clinical trials,” the National Organization for Rare Disorders said in a statement. “We hope the Senate will recognize that patients deserve legislation that will genuinely increase access. For example, senators should focus on legislation that reduces the financial disincentives companies encounter in offering their therapy through expanded access.”
The Senate passed a version of “right to try” in 2017 through the unanimous consent process (S. 204). No schedule has been set yet to either combine the two bills in committee or for the Senate to take up the House bill. President Trump voiced support for “right to try” legislation during his 2018 State of the Union address.
Terminal patients who have exhausted all approved drug options would be able to seek out investigational treatments – even if they do not qualify for clinical trials – under a bill passed in the U.S. House, despite opposition from more than 100 patient and physician groups.
The Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina
For an unapproved drug to be made available to patients, it must have an active application that is not subject to any kind of clinical hold. Sponsors and manufacturers must notify the Food and Drug Administration when an unapproved drug is made available to the patient.
The bill also includes safeguards to prevent manufacturers from purposefully misbranding or mislabeling drugs.
H.R. 5247 provides liability protections to manufacturers, sponsors, physicians, clinical investigators, and hospitals that participate in providing experimental drugs to terminal patients through this new alternative pathway, although it does not shield them from liability stemming from reckless misconduct, gross negligence, or any other intentional violations. It requires sponsors and manufacturers to report all adverse events to the FDA.
It also provides certainty to manufacturers as to how the FDA will use patient outcomes from the use of treatments outside of clinical trials when it is evaluating the applications on these new drugs.
Rep. Michael Burgess (R-Tex.), the House Energy & Commerce Health Subcommittee chairman and a physician, spoke in support of the bill during a debate on the House floor.
“Mr. Speaker, as a physician, I understand that access to investigational drugs and therapies is a deeply personal priority for those seeking treatment for their loved ones with serious, life-threatening conditions,” he said. “To my friends on the other side of the aisle, I have a simple question: Why do you not want to allow these patients to exercise their right to fight for their future?”
Rep. Frank Pallone (D-N.J.), the top-ranking Democrat on the House Energy & Commerce Committee, responded by asking, “if this is such a patient-centered bill, then why does every major patient organization overwhelmingly oppose it?”
In a March 19 letter to congressional leaders, a coalition of more than 100 physician and patient advocacy groups called the alternative pathway laid out in legislation “less safe” for patients than the FDA’s current expanded access process.
“This alternative pathway would allow for a 7-day lag between access to investigational therapies (as well as potential ensuing adverse effects) and FDA notification. FDA also is prohibited from halting access to these experimental therapies short of placing a clinical hold on all clinical research on the therapy in question, which is a blunt and disproportionate measure. The legislation would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program,” the groups wrote.
The groups that signed the letter included the American Society of Clinical Oncology, the Cystic Fibrosis Foundation, Friends of Cancer Research, the Leukemia & Lymphoma Society, the National Comprehensive Cancer Network, the National Organization for Rare Disorders, the Platelet Disorder Support Association, and Vietnam Veterans of America.
“The current compassionate use program at the Food and Drug Administration does make a good faith effort to help patients who do not qualify for clinical trials,” Rep. Burgess said. “But ‘right to try’ would actually offer patients an alternative pathway to access eligible investigational drugs, so long as they are certified by a physician who is in good standing and abides by the rules laid out in the bill.”
But Rep. Pallone noted that a review by the Government Accountability Office found that the FDA approves 99% of the requests submitted to the agency. Of the nearly 1,700 requests the FDA received in 2017, just 9 were not approved. However, the agency also adjusted applications for 11% of the patients in order to improve patient safety protections and that type of review should be allowed to continue, he said.
Patient groups expressed disappointment following the House vote. “The House has voted for a proposal that would create a less-safe, redundant pathway for accessing investigational therapies outside of clinical trials,” the National Organization for Rare Disorders said in a statement. “We hope the Senate will recognize that patients deserve legislation that will genuinely increase access. For example, senators should focus on legislation that reduces the financial disincentives companies encounter in offering their therapy through expanded access.”
The Senate passed a version of “right to try” in 2017 through the unanimous consent process (S. 204). No schedule has been set yet to either combine the two bills in committee or for the Senate to take up the House bill. President Trump voiced support for “right to try” legislation during his 2018 State of the Union address.
Same-day discharge for hysterectomy
There is an increased focus on reducing the costs of health care delivery, and one major driver of surgical cost is length of hospitalization. A minimally invasive surgical approach to hysterectomy is a strategy that significantly enhances recovery and shortens hospital stay, although many patients who can safely be considered for same-day discharge (SDD), including many with cancer, are still admitted to the hospital overnight. Much has been published on the predictors and pathways for successful same-day discharge after minimally invasive hysterectomy, and in this column we will review how to best predict who is a good candidate for SDD and how to optimize the success of this approach with respect to safety and patient satisfaction.
What are the benefits to SDD?
Certainly, decreased hospitalization costs are an attractive feature of SDD following hysterectomy, although surgeons should also be mindful that patient-centered outcomes, such as pain control, managing nausea, and patient satisfaction, also are considered with equal emphasis. Several studies have shown that, in appropriate candidates and when proactive pathways are used, patient satisfaction is preserved with SDD following hysterectomy.1
Choosing patient candidates
Same day discharge is most successfully accomplished in patients of good general baseline health.2 Diabetic patients, particularly those on insulin, are generally not good candidates for SDD because it is important to monitor and intervene in blood glucose changes that are influenced by a nothing-by-mouth status and surgical stress. We recommend observing patients overnight with a history of pulmonary disease who may have transient increased postoperative O2 needs. Similarly, patients with significant cardiac disease (including heart failure and coronary disease) may benefit from prolonged overnight observation.
Particular caution should be paid to patients with obstructive sleep apnea, which may be occult but anticipated in patients with very high body mass indexes (greater than 40 kg/m2). General anesthetic drugs, the trauma of intubation, and opioids all couple with the underlying airway compromise such that these patients are at risk for postoperative apnea, which, in severe cases, can result in anoxia and death. These patients should be considered for continuous pulse-ox monitoring for at least 12-24 hours postoperatively and are not good candidates for same-day discharge.
Patients who have baseline anticoagulation that has been stopped or bridged preoperatively should have prolonged observation with recheck of their postoperative hemoglobin prior to discharge.
Patients who live alone or are very elderly with baseline frailty are poor candidates for SDD and may benefit from nursing observation overnight while they metabolize their anesthesia. Patients who have chronic opioid dependency present a greater challenge to control postoperative pain; these patients are generally less good candidates for SDD.
Studies have shown that the indication for the procedure (for example, cancer with staging, fibroids, endometriosis) is less critical in determining who is a good candidate for SDD.3 However, successful SDD rates are highest in more straightforward cases with few or no prior surgeries, small uteri (less than 14 weeks), a surgical duration of less than 3 hours, and a surgical start time before 2 p.m. Longer, more complex cases are typically associated with more blood loss, higher risk for occult complications, and more time under anesthesia (and in Trendelenburg), which can exacerbate airway edema. In preparation for such cases, it might be wise to prepare patients for the possibility that they may not be good candidates for discharge on the same day. In general, most SDD pathways exclude patients with very high BMI (greater than 50 kg/m2) because of concern for airway patency and because these cases may be more complex with higher underlying risk. In addition, many of these patients have diabetes and require perioperative metabolic interventions.
Patient preparation
A key component to successful SDD is setting patient expectations. Patients should be informed at their preoperative visit that, unless there is an unexpected occurrence or response to the surgery, they will be discharged to home the same day. This allows them to prepare their home (including transportation needs) in advance. They should be provided with information about what to expect that first night after surgery (including potential residual drowsiness or nausea from anesthesia and immediate postoperative pain).
On the day of surgery, under the influence of anesthesia and pain medication, patients will have difficulty retaining complex discharge instructions. The preoperative visit is critically important because it’s the best time to provide them with this information, including postoperative activity limitations, wound and dressing care, and follow-up instructions. This is also the best time to provide prescriptions for postoperative pain, nausea, and constipation prophylaxis with detailed instructions about best use. Patients should be encouraged to fill these prescriptions preoperatively so that they have these medications on hand on the evening of their discharge.
Many programs utilize a combination of educational strategies (in person, written, video) to maximize the likelihood of retention.1 It is also important to offer an opportunity for patients to ask questions about this information after they have received it (for example, by phoning the patients prior to their procedure).
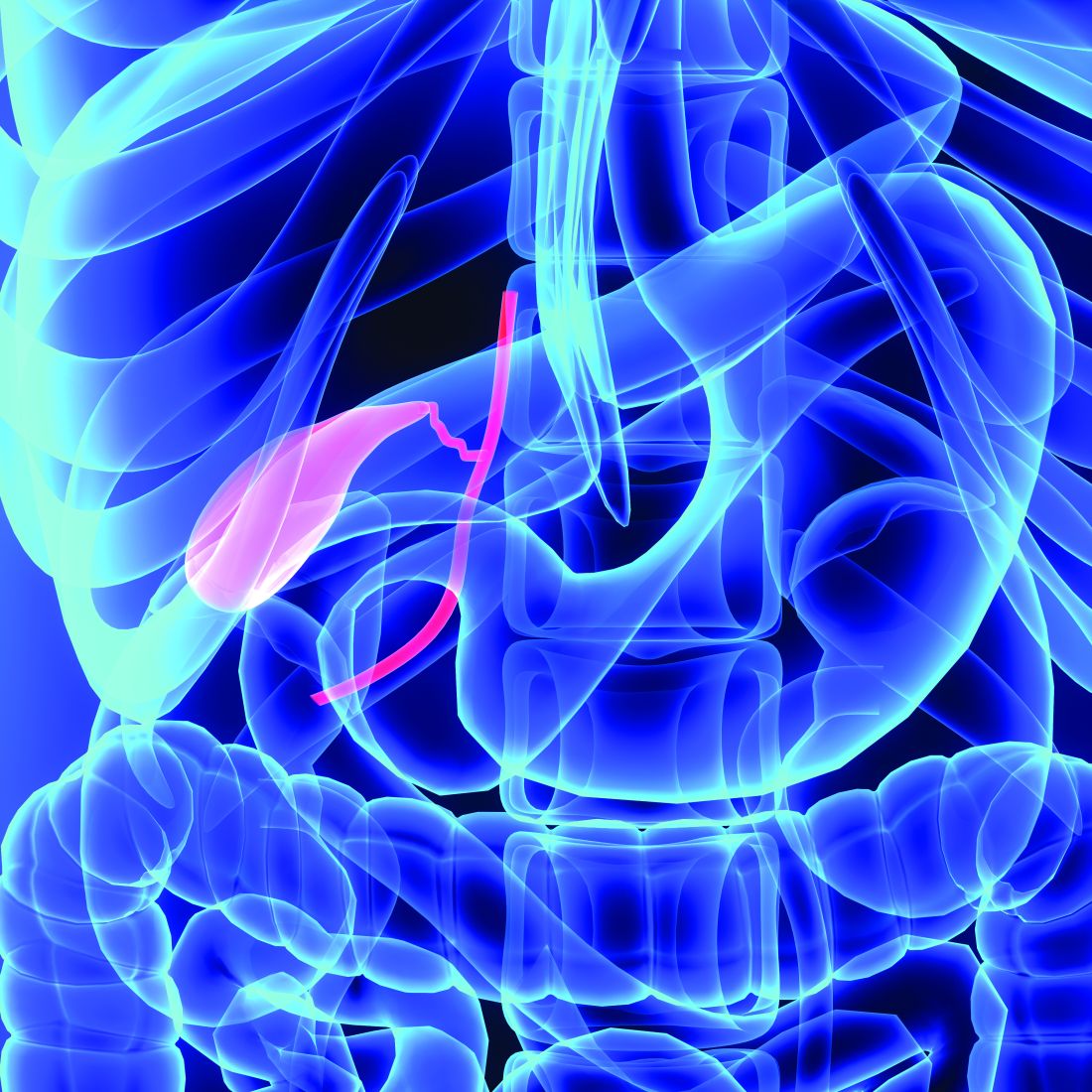
Preoperative strategies
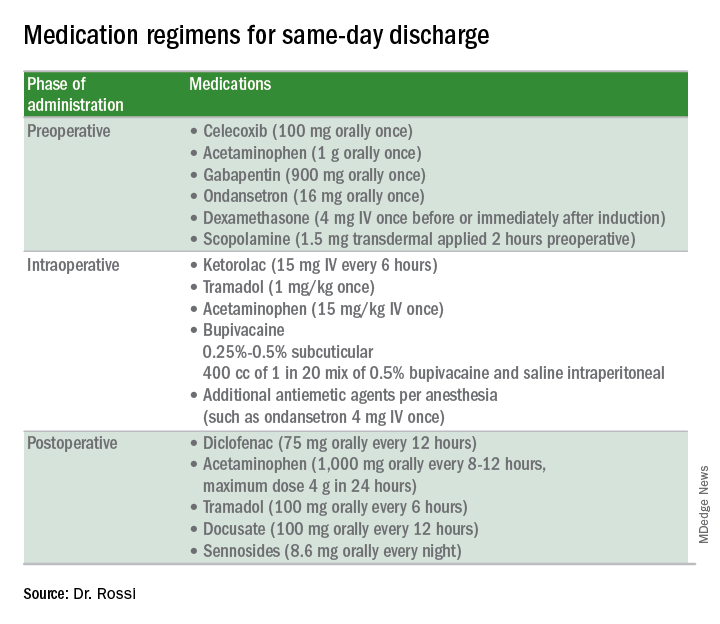
Intraoperative strategies
Consider in-and-out catheterization rather than placement of an indwelling catheter for anticipated short cases without complex bladder dissection.5 Minimize blood loss and maximally evacuate blood and clots with suction because hemoperitoneum can induce nausea and pain.
Pain from retained gas under the diaphragm can be reduced by bathing the diaphragms with 400 cc of dilute local anesthetic made by mixing 50 mL of 0.5% bupivacaine in 1000 mL normal saline prior to removal of pneumoperitoneum and while still in Trendelenburg. Ensure there is minimal retained intraperitoneal CO2 at the completion of the surgery by asking the anesthesiologists to perform positive pressure ventilations prior to fascial closure. Consider injecting port sites (including the peritoneal and fascial layers) with a mixture of immediate and long-acting local anesthetics. Request that the anesthesia staff administer intraoperative doses of IV ketorolac, acetaminophen, and tramadol (in preference to opioids) and an aggressive perioperative cocktail of antiemetics.
Management in the recovery room
Surgeons should ensure that recovery room staff are well versed in the pathway for patients who are selected for SDD to ensure proactive implementation of analgesic and antiemetic regimens and to fast-track the various tasks and education required for discharge.5
Patients should be started on their home postoperative medication regimen in the recovery room, including an anti-inflammatory such as diclofenac, sublingual tramadol (in preference to an opioid, such as hydrocodone), docusate, and sennosides. IV opioids should be avoided because they can result in somnolence and nausea.
If placed intraoperatively, the Foley catheter should be removed early to allow adequate time to void. Backfilling the bladder prior to removal can hasten the urge to void and help objectively document completeness of evacuation. All patients should be seen by the anesthesiologist and/or surgeon prior to discharge.
For patients who are discharged same day, a follow-up phone call on postoperative day 1 is valuable to ensure that they have continued their successful postoperative transition to the home and to intervene early if there are concerns for patient satisfaction.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Fountain CR et al. Promoting same-day discharge for gynecologic oncology patients in minimally invasive hysterectomy. J Minim Invasive Gynecol. 2017 Sep-Oct;24(6):932-9.
2. Rivard C et al. Factors influencing same-day hospital discharge and risk factors for readmission after robotic surgery in the gynecologic oncology patient population. J Minim Invasive Gynecol. 2015 Feb;22(2):219-26.
3. Lee SJ et al. The feasibility and safety of same-day discharge after robotic-assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014 Jun;133(3):552-5.
4. Elia N et al. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology. 2005 Dec;103(6):1296-304.
5. Donnez O et al. Low pain score after total laparoscopic hysterectomy and same-day discharge within less than 5 hours: Results of a prospective observational study. J Minim Invasive Gynecol. 2015 Nov-Dec;22(7):1293-9.
There is an increased focus on reducing the costs of health care delivery, and one major driver of surgical cost is length of hospitalization. A minimally invasive surgical approach to hysterectomy is a strategy that significantly enhances recovery and shortens hospital stay, although many patients who can safely be considered for same-day discharge (SDD), including many with cancer, are still admitted to the hospital overnight. Much has been published on the predictors and pathways for successful same-day discharge after minimally invasive hysterectomy, and in this column we will review how to best predict who is a good candidate for SDD and how to optimize the success of this approach with respect to safety and patient satisfaction.
What are the benefits to SDD?
Certainly, decreased hospitalization costs are an attractive feature of SDD following hysterectomy, although surgeons should also be mindful that patient-centered outcomes, such as pain control, managing nausea, and patient satisfaction, also are considered with equal emphasis. Several studies have shown that, in appropriate candidates and when proactive pathways are used, patient satisfaction is preserved with SDD following hysterectomy.1
Choosing patient candidates
Same day discharge is most successfully accomplished in patients of good general baseline health.2 Diabetic patients, particularly those on insulin, are generally not good candidates for SDD because it is important to monitor and intervene in blood glucose changes that are influenced by a nothing-by-mouth status and surgical stress. We recommend observing patients overnight with a history of pulmonary disease who may have transient increased postoperative O2 needs. Similarly, patients with significant cardiac disease (including heart failure and coronary disease) may benefit from prolonged overnight observation.
Particular caution should be paid to patients with obstructive sleep apnea, which may be occult but anticipated in patients with very high body mass indexes (greater than 40 kg/m2). General anesthetic drugs, the trauma of intubation, and opioids all couple with the underlying airway compromise such that these patients are at risk for postoperative apnea, which, in severe cases, can result in anoxia and death. These patients should be considered for continuous pulse-ox monitoring for at least 12-24 hours postoperatively and are not good candidates for same-day discharge.
Patients who have baseline anticoagulation that has been stopped or bridged preoperatively should have prolonged observation with recheck of their postoperative hemoglobin prior to discharge.
Patients who live alone or are very elderly with baseline frailty are poor candidates for SDD and may benefit from nursing observation overnight while they metabolize their anesthesia. Patients who have chronic opioid dependency present a greater challenge to control postoperative pain; these patients are generally less good candidates for SDD.
Studies have shown that the indication for the procedure (for example, cancer with staging, fibroids, endometriosis) is less critical in determining who is a good candidate for SDD.3 However, successful SDD rates are highest in more straightforward cases with few or no prior surgeries, small uteri (less than 14 weeks), a surgical duration of less than 3 hours, and a surgical start time before 2 p.m. Longer, more complex cases are typically associated with more blood loss, higher risk for occult complications, and more time under anesthesia (and in Trendelenburg), which can exacerbate airway edema. In preparation for such cases, it might be wise to prepare patients for the possibility that they may not be good candidates for discharge on the same day. In general, most SDD pathways exclude patients with very high BMI (greater than 50 kg/m2) because of concern for airway patency and because these cases may be more complex with higher underlying risk. In addition, many of these patients have diabetes and require perioperative metabolic interventions.
Patient preparation
A key component to successful SDD is setting patient expectations. Patients should be informed at their preoperative visit that, unless there is an unexpected occurrence or response to the surgery, they will be discharged to home the same day. This allows them to prepare their home (including transportation needs) in advance. They should be provided with information about what to expect that first night after surgery (including potential residual drowsiness or nausea from anesthesia and immediate postoperative pain).
On the day of surgery, under the influence of anesthesia and pain medication, patients will have difficulty retaining complex discharge instructions. The preoperative visit is critically important because it’s the best time to provide them with this information, including postoperative activity limitations, wound and dressing care, and follow-up instructions. This is also the best time to provide prescriptions for postoperative pain, nausea, and constipation prophylaxis with detailed instructions about best use. Patients should be encouraged to fill these prescriptions preoperatively so that they have these medications on hand on the evening of their discharge.
Many programs utilize a combination of educational strategies (in person, written, video) to maximize the likelihood of retention.1 It is also important to offer an opportunity for patients to ask questions about this information after they have received it (for example, by phoning the patients prior to their procedure).
Preoperative strategies
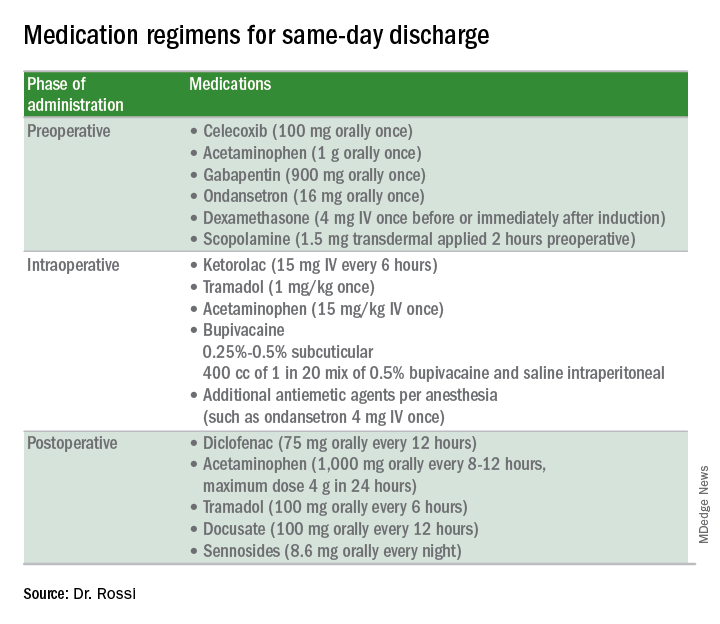
Intraoperative strategies
Consider in-and-out catheterization rather than placement of an indwelling catheter for anticipated short cases without complex bladder dissection.5 Minimize blood loss and maximally evacuate blood and clots with suction because hemoperitoneum can induce nausea and pain.
Pain from retained gas under the diaphragm can be reduced by bathing the diaphragms with 400 cc of dilute local anesthetic made by mixing 50 mL of 0.5% bupivacaine in 1000 mL normal saline prior to removal of pneumoperitoneum and while still in Trendelenburg. Ensure there is minimal retained intraperitoneal CO2 at the completion of the surgery by asking the anesthesiologists to perform positive pressure ventilations prior to fascial closure. Consider injecting port sites (including the peritoneal and fascial layers) with a mixture of immediate and long-acting local anesthetics. Request that the anesthesia staff administer intraoperative doses of IV ketorolac, acetaminophen, and tramadol (in preference to opioids) and an aggressive perioperative cocktail of antiemetics.
Management in the recovery room
Surgeons should ensure that recovery room staff are well versed in the pathway for patients who are selected for SDD to ensure proactive implementation of analgesic and antiemetic regimens and to fast-track the various tasks and education required for discharge.5
Patients should be started on their home postoperative medication regimen in the recovery room, including an anti-inflammatory such as diclofenac, sublingual tramadol (in preference to an opioid, such as hydrocodone), docusate, and sennosides. IV opioids should be avoided because they can result in somnolence and nausea.
If placed intraoperatively, the Foley catheter should be removed early to allow adequate time to void. Backfilling the bladder prior to removal can hasten the urge to void and help objectively document completeness of evacuation. All patients should be seen by the anesthesiologist and/or surgeon prior to discharge.
For patients who are discharged same day, a follow-up phone call on postoperative day 1 is valuable to ensure that they have continued their successful postoperative transition to the home and to intervene early if there are concerns for patient satisfaction.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Fountain CR et al. Promoting same-day discharge for gynecologic oncology patients in minimally invasive hysterectomy. J Minim Invasive Gynecol. 2017 Sep-Oct;24(6):932-9.
2. Rivard C et al. Factors influencing same-day hospital discharge and risk factors for readmission after robotic surgery in the gynecologic oncology patient population. J Minim Invasive Gynecol. 2015 Feb;22(2):219-26.
3. Lee SJ et al. The feasibility and safety of same-day discharge after robotic-assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014 Jun;133(3):552-5.
4. Elia N et al. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology. 2005 Dec;103(6):1296-304.
5. Donnez O et al. Low pain score after total laparoscopic hysterectomy and same-day discharge within less than 5 hours: Results of a prospective observational study. J Minim Invasive Gynecol. 2015 Nov-Dec;22(7):1293-9.
There is an increased focus on reducing the costs of health care delivery, and one major driver of surgical cost is length of hospitalization. A minimally invasive surgical approach to hysterectomy is a strategy that significantly enhances recovery and shortens hospital stay, although many patients who can safely be considered for same-day discharge (SDD), including many with cancer, are still admitted to the hospital overnight. Much has been published on the predictors and pathways for successful same-day discharge after minimally invasive hysterectomy, and in this column we will review how to best predict who is a good candidate for SDD and how to optimize the success of this approach with respect to safety and patient satisfaction.
What are the benefits to SDD?
Certainly, decreased hospitalization costs are an attractive feature of SDD following hysterectomy, although surgeons should also be mindful that patient-centered outcomes, such as pain control, managing nausea, and patient satisfaction, also are considered with equal emphasis. Several studies have shown that, in appropriate candidates and when proactive pathways are used, patient satisfaction is preserved with SDD following hysterectomy.1
Choosing patient candidates
Same day discharge is most successfully accomplished in patients of good general baseline health.2 Diabetic patients, particularly those on insulin, are generally not good candidates for SDD because it is important to monitor and intervene in blood glucose changes that are influenced by a nothing-by-mouth status and surgical stress. We recommend observing patients overnight with a history of pulmonary disease who may have transient increased postoperative O2 needs. Similarly, patients with significant cardiac disease (including heart failure and coronary disease) may benefit from prolonged overnight observation.
Particular caution should be paid to patients with obstructive sleep apnea, which may be occult but anticipated in patients with very high body mass indexes (greater than 40 kg/m2). General anesthetic drugs, the trauma of intubation, and opioids all couple with the underlying airway compromise such that these patients are at risk for postoperative apnea, which, in severe cases, can result in anoxia and death. These patients should be considered for continuous pulse-ox monitoring for at least 12-24 hours postoperatively and are not good candidates for same-day discharge.
Patients who have baseline anticoagulation that has been stopped or bridged preoperatively should have prolonged observation with recheck of their postoperative hemoglobin prior to discharge.
Patients who live alone or are very elderly with baseline frailty are poor candidates for SDD and may benefit from nursing observation overnight while they metabolize their anesthesia. Patients who have chronic opioid dependency present a greater challenge to control postoperative pain; these patients are generally less good candidates for SDD.
Studies have shown that the indication for the procedure (for example, cancer with staging, fibroids, endometriosis) is less critical in determining who is a good candidate for SDD.3 However, successful SDD rates are highest in more straightforward cases with few or no prior surgeries, small uteri (less than 14 weeks), a surgical duration of less than 3 hours, and a surgical start time before 2 p.m. Longer, more complex cases are typically associated with more blood loss, higher risk for occult complications, and more time under anesthesia (and in Trendelenburg), which can exacerbate airway edema. In preparation for such cases, it might be wise to prepare patients for the possibility that they may not be good candidates for discharge on the same day. In general, most SDD pathways exclude patients with very high BMI (greater than 50 kg/m2) because of concern for airway patency and because these cases may be more complex with higher underlying risk. In addition, many of these patients have diabetes and require perioperative metabolic interventions.
Patient preparation
A key component to successful SDD is setting patient expectations. Patients should be informed at their preoperative visit that, unless there is an unexpected occurrence or response to the surgery, they will be discharged to home the same day. This allows them to prepare their home (including transportation needs) in advance. They should be provided with information about what to expect that first night after surgery (including potential residual drowsiness or nausea from anesthesia and immediate postoperative pain).
On the day of surgery, under the influence of anesthesia and pain medication, patients will have difficulty retaining complex discharge instructions. The preoperative visit is critically important because it’s the best time to provide them with this information, including postoperative activity limitations, wound and dressing care, and follow-up instructions. This is also the best time to provide prescriptions for postoperative pain, nausea, and constipation prophylaxis with detailed instructions about best use. Patients should be encouraged to fill these prescriptions preoperatively so that they have these medications on hand on the evening of their discharge.
Many programs utilize a combination of educational strategies (in person, written, video) to maximize the likelihood of retention.1 It is also important to offer an opportunity for patients to ask questions about this information after they have received it (for example, by phoning the patients prior to their procedure).
Preoperative strategies
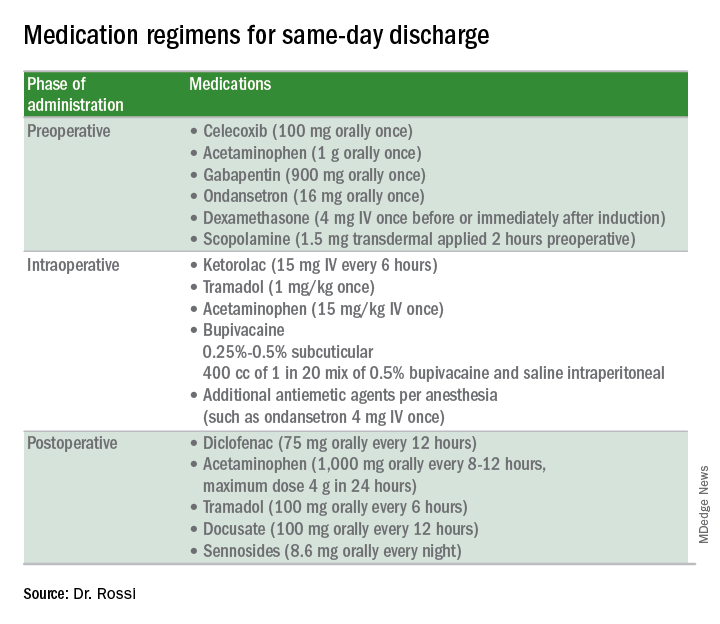
Intraoperative strategies
Consider in-and-out catheterization rather than placement of an indwelling catheter for anticipated short cases without complex bladder dissection.5 Minimize blood loss and maximally evacuate blood and clots with suction because hemoperitoneum can induce nausea and pain.
Pain from retained gas under the diaphragm can be reduced by bathing the diaphragms with 400 cc of dilute local anesthetic made by mixing 50 mL of 0.5% bupivacaine in 1000 mL normal saline prior to removal of pneumoperitoneum and while still in Trendelenburg. Ensure there is minimal retained intraperitoneal CO2 at the completion of the surgery by asking the anesthesiologists to perform positive pressure ventilations prior to fascial closure. Consider injecting port sites (including the peritoneal and fascial layers) with a mixture of immediate and long-acting local anesthetics. Request that the anesthesia staff administer intraoperative doses of IV ketorolac, acetaminophen, and tramadol (in preference to opioids) and an aggressive perioperative cocktail of antiemetics.
Management in the recovery room
Surgeons should ensure that recovery room staff are well versed in the pathway for patients who are selected for SDD to ensure proactive implementation of analgesic and antiemetic regimens and to fast-track the various tasks and education required for discharge.5
Patients should be started on their home postoperative medication regimen in the recovery room, including an anti-inflammatory such as diclofenac, sublingual tramadol (in preference to an opioid, such as hydrocodone), docusate, and sennosides. IV opioids should be avoided because they can result in somnolence and nausea.
If placed intraoperatively, the Foley catheter should be removed early to allow adequate time to void. Backfilling the bladder prior to removal can hasten the urge to void and help objectively document completeness of evacuation. All patients should be seen by the anesthesiologist and/or surgeon prior to discharge.
For patients who are discharged same day, a follow-up phone call on postoperative day 1 is valuable to ensure that they have continued their successful postoperative transition to the home and to intervene early if there are concerns for patient satisfaction.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Fountain CR et al. Promoting same-day discharge for gynecologic oncology patients in minimally invasive hysterectomy. J Minim Invasive Gynecol. 2017 Sep-Oct;24(6):932-9.
2. Rivard C et al. Factors influencing same-day hospital discharge and risk factors for readmission after robotic surgery in the gynecologic oncology patient population. J Minim Invasive Gynecol. 2015 Feb;22(2):219-26.
3. Lee SJ et al. The feasibility and safety of same-day discharge after robotic-assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014 Jun;133(3):552-5.
4. Elia N et al. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology. 2005 Dec;103(6):1296-304.
5. Donnez O et al. Low pain score after total laparoscopic hysterectomy and same-day discharge within less than 5 hours: Results of a prospective observational study. J Minim Invasive Gynecol. 2015 Nov-Dec;22(7):1293-9.
FDA updates breast implant–associated lymphoma cases, risk
(BIA-ALCL), including nine deaths.
This figure includes all medical device reports received by the agency between 2011 and September 2017. The FDA recently provided an update on ALCL linked to breast implants and an estimate of lifetime risk of developing ALCL.
Based on available medical literature, the lifetime risk of developing BIA-ALCL for patients with textured breast implants ranges from 1 in 3,817 to 1 in 30,000, according to the update.
Of the 272 reports with data on surface type, 242 were textured implants and 30 were smooth implants. In addition, 413 reports include information on the implant fill type: 234 used silicone gel and 179 were saline filled.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association. We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health. “As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
The possible association between breast implants and the development of anaplastic large cell lymphoma (ALCL) was first identified in 2011. At that time, there were not enough cases of to determine what factors increased a patient’s risk of developing the disease. As more information became available, the World Health Organization designated BIA-ALCL as a T-cell lymphoma that can develop following breast implants.
(BIA-ALCL), including nine deaths.
This figure includes all medical device reports received by the agency between 2011 and September 2017. The FDA recently provided an update on ALCL linked to breast implants and an estimate of lifetime risk of developing ALCL.
Based on available medical literature, the lifetime risk of developing BIA-ALCL for patients with textured breast implants ranges from 1 in 3,817 to 1 in 30,000, according to the update.
Of the 272 reports with data on surface type, 242 were textured implants and 30 were smooth implants. In addition, 413 reports include information on the implant fill type: 234 used silicone gel and 179 were saline filled.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association. We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health. “As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
The possible association between breast implants and the development of anaplastic large cell lymphoma (ALCL) was first identified in 2011. At that time, there were not enough cases of to determine what factors increased a patient’s risk of developing the disease. As more information became available, the World Health Organization designated BIA-ALCL as a T-cell lymphoma that can develop following breast implants.
(BIA-ALCL), including nine deaths.
This figure includes all medical device reports received by the agency between 2011 and September 2017. The FDA recently provided an update on ALCL linked to breast implants and an estimate of lifetime risk of developing ALCL.
Based on available medical literature, the lifetime risk of developing BIA-ALCL for patients with textured breast implants ranges from 1 in 3,817 to 1 in 30,000, according to the update.
Of the 272 reports with data on surface type, 242 were textured implants and 30 were smooth implants. In addition, 413 reports include information on the implant fill type: 234 used silicone gel and 179 were saline filled.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association. We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health. “As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
The possible association between breast implants and the development of anaplastic large cell lymphoma (ALCL) was first identified in 2011. At that time, there were not enough cases of to determine what factors increased a patient’s risk of developing the disease. As more information became available, the World Health Organization designated BIA-ALCL as a T-cell lymphoma that can develop following breast implants.
Study links RA flares after joint replacement to disease activity, not medications
Patients with the most severe cases of rheumatoid arthritis are more likely to suffer flares after knee or hip replacement surgery, a new study finds, and it doesn’t seem to matter whether they stop taking biologics before their operation.
“We found that the majority of patients had active disease at the time of surgery, contrary to prior statements that RA patients have inactive disease at the time they go for hip or knee replacement. In fact, the majority – 65% of the patients – reported a flare of RA within 6 weeks of surgery,” lead author Susan M. Goodman, MD, of Cornell University and the Hospital for Special Surgery, New York, said in an interview. “Surprisingly, although more of the flaring patients were taking potent biologics that had been withheld preoperatively, the major risk factor for flares was their baseline disease activity.”
According to Dr. Goodman, the researchers launched the study to better understand how medical decisions prior to joint replacement surgery affect the progress of RA afterward.
In terms of continuing RA drug treatment, she said, “the decision really hinges on the risk of infection versus the risk of flare, and we didn’t know the usual course of events for these patients.”
In addition, she said, “many doctors incorrectly think that the majority of patients with RA have ‘burnt-out’ or inactive disease at the time of hip or knee replacement surgery.”
For the study, the researchers prospectively followed 120 patients who were to undergo joint replacement surgery. (The researchers initially approached 354 patients, of whom 169 declined to participate. Another 65 were dropped from the study for various reasons, including 42 who did not sufficiently fill out questionnaires and were deleted from the final analysis.)
The researchers tracked the patients before surgery and for 6 weeks after surgery. A majority of the patients were female (83%) and white (81%), with a mean age of 62 and a median RA symptom duration of 15 years. A total of 44% underwent hip replacement surgery while the rest underwent knee replacement surgery. Just over half of the patients were taking biologics, which were stopped prior to surgery, while glucocorticoids and methotrexate were usually continued.
Just under two-thirds of the patients flared within the first 6 weeks after surgery. The researchers didn’t find any connection between the flares and stopping biologics or using methotrexate. They did, however, link higher baseline RA activity to postsurgery flaring (odds ratio, 2.11; P = .015).
Dr. Goodman said that she and her colleagues continue to collect data to better understand flares and the link to disease severity. “The long-term implications of this are not yet known. We would like to know the effect on long-term functional outcome and complication rate.”
The National Institutes of Health, the Weill Cornell Clinical Translational Science Center, and the Block Family Foundation supported the study. Dr. Goodman disclosed receiving research funding from Novartis and Roche.
SOURCE: Goodman S et al. J Rheumatol. 2018 Mar 15. doi: 10.3899/jrheum.170366
Patients with the most severe cases of rheumatoid arthritis are more likely to suffer flares after knee or hip replacement surgery, a new study finds, and it doesn’t seem to matter whether they stop taking biologics before their operation.
“We found that the majority of patients had active disease at the time of surgery, contrary to prior statements that RA patients have inactive disease at the time they go for hip or knee replacement. In fact, the majority – 65% of the patients – reported a flare of RA within 6 weeks of surgery,” lead author Susan M. Goodman, MD, of Cornell University and the Hospital for Special Surgery, New York, said in an interview. “Surprisingly, although more of the flaring patients were taking potent biologics that had been withheld preoperatively, the major risk factor for flares was their baseline disease activity.”
According to Dr. Goodman, the researchers launched the study to better understand how medical decisions prior to joint replacement surgery affect the progress of RA afterward.
In terms of continuing RA drug treatment, she said, “the decision really hinges on the risk of infection versus the risk of flare, and we didn’t know the usual course of events for these patients.”
In addition, she said, “many doctors incorrectly think that the majority of patients with RA have ‘burnt-out’ or inactive disease at the time of hip or knee replacement surgery.”
For the study, the researchers prospectively followed 120 patients who were to undergo joint replacement surgery. (The researchers initially approached 354 patients, of whom 169 declined to participate. Another 65 were dropped from the study for various reasons, including 42 who did not sufficiently fill out questionnaires and were deleted from the final analysis.)
The researchers tracked the patients before surgery and for 6 weeks after surgery. A majority of the patients were female (83%) and white (81%), with a mean age of 62 and a median RA symptom duration of 15 years. A total of 44% underwent hip replacement surgery while the rest underwent knee replacement surgery. Just over half of the patients were taking biologics, which were stopped prior to surgery, while glucocorticoids and methotrexate were usually continued.
Just under two-thirds of the patients flared within the first 6 weeks after surgery. The researchers didn’t find any connection between the flares and stopping biologics or using methotrexate. They did, however, link higher baseline RA activity to postsurgery flaring (odds ratio, 2.11; P = .015).
Dr. Goodman said that she and her colleagues continue to collect data to better understand flares and the link to disease severity. “The long-term implications of this are not yet known. We would like to know the effect on long-term functional outcome and complication rate.”
The National Institutes of Health, the Weill Cornell Clinical Translational Science Center, and the Block Family Foundation supported the study. Dr. Goodman disclosed receiving research funding from Novartis and Roche.
SOURCE: Goodman S et al. J Rheumatol. 2018 Mar 15. doi: 10.3899/jrheum.170366
Patients with the most severe cases of rheumatoid arthritis are more likely to suffer flares after knee or hip replacement surgery, a new study finds, and it doesn’t seem to matter whether they stop taking biologics before their operation.
“We found that the majority of patients had active disease at the time of surgery, contrary to prior statements that RA patients have inactive disease at the time they go for hip or knee replacement. In fact, the majority – 65% of the patients – reported a flare of RA within 6 weeks of surgery,” lead author Susan M. Goodman, MD, of Cornell University and the Hospital for Special Surgery, New York, said in an interview. “Surprisingly, although more of the flaring patients were taking potent biologics that had been withheld preoperatively, the major risk factor for flares was their baseline disease activity.”
According to Dr. Goodman, the researchers launched the study to better understand how medical decisions prior to joint replacement surgery affect the progress of RA afterward.
In terms of continuing RA drug treatment, she said, “the decision really hinges on the risk of infection versus the risk of flare, and we didn’t know the usual course of events for these patients.”
In addition, she said, “many doctors incorrectly think that the majority of patients with RA have ‘burnt-out’ or inactive disease at the time of hip or knee replacement surgery.”
For the study, the researchers prospectively followed 120 patients who were to undergo joint replacement surgery. (The researchers initially approached 354 patients, of whom 169 declined to participate. Another 65 were dropped from the study for various reasons, including 42 who did not sufficiently fill out questionnaires and were deleted from the final analysis.)
The researchers tracked the patients before surgery and for 6 weeks after surgery. A majority of the patients were female (83%) and white (81%), with a mean age of 62 and a median RA symptom duration of 15 years. A total of 44% underwent hip replacement surgery while the rest underwent knee replacement surgery. Just over half of the patients were taking biologics, which were stopped prior to surgery, while glucocorticoids and methotrexate were usually continued.
Just under two-thirds of the patients flared within the first 6 weeks after surgery. The researchers didn’t find any connection between the flares and stopping biologics or using methotrexate. They did, however, link higher baseline RA activity to postsurgery flaring (odds ratio, 2.11; P = .015).
Dr. Goodman said that she and her colleagues continue to collect data to better understand flares and the link to disease severity. “The long-term implications of this are not yet known. We would like to know the effect on long-term functional outcome and complication rate.”
The National Institutes of Health, the Weill Cornell Clinical Translational Science Center, and the Block Family Foundation supported the study. Dr. Goodman disclosed receiving research funding from Novartis and Roche.
SOURCE: Goodman S et al. J Rheumatol. 2018 Mar 15. doi: 10.3899/jrheum.170366
FROM JOURNAL OF RHEUMATOLOGY
Key clinical point:
Major finding: Sixty-five percent of RA patients developed flares after joint replacement surgery, and it was more common in those with higher baseline RA activity (odds ratio, 2.11; P = .015).
Study details: Prospective study of 120 patients with RA who underwent hip replacement (44%) or knee replacement (56%).
Disclosures: The National Institutes of Health, the Weill Cornell Clinical Translational Science Center, and the Block Family Foundation supported the study. The lead author disclosed receiving research funding from Novartis and Roche.
Source: Goodman S et al. J Rheumatol. 2018 Mar 15. doi: 10.3899/jrheum.170366.
VIDEO: Andexanet alfa effectively reverses factor Xa anticoagulant
ORLANDO – Andexanet alfa, a new agent that reverses the anticoagulant effect of direct factor Xa inhibitors, showed an acceptable level of efficacy and safety in 227 patients who received the drug in the agent’s pivotal trial.
These results, which placed andexanet in the same ballpark for efficacy and safety as idarucizumab (Praxbind), approved in 2015 for reversing the anticoagulant dabigatran (Pradaxa), suggest that andexanet is likely on track for its own Food and Drug Administration marketing approval, Stuart Connolly, MD, said at the annual meeting of the American College of Cardiology.
Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa) previously announced that it expected Food and Drug Administration action on its marketing application by May 2018.
Andexanet reversal “has similar efficacy and safety as seen with other reversal agents” for other types of anticoagulants, said Dr. Connolly, a professor of medicine and an electrophysiologist at McMaster University in Hamilton, Ont. In the trial results he reported, andexanet treatment of patients who were bleeding while on treatment with a direct factor Xa inhibitor had an 83% rate of hemostatic efficacy and an 11% rate of thrombotic events. By comparison, idarucizumab, the FDA-approved reversal agent for the anticoagulant dabigatran, produced a 68% hemostatic efficacy and a 6% rate of thrombotic events in the idarucizumab pivotal trial, RE-VERSE AD (N Engl J Med. 2015 Aug 6;373[6]:511-20).
The Prospective, Open-Label Study of Andexanet Alfa in Patients Receiving a Factor Xa Inhibitor Who Have Acute Major Bleeding (ANNEXA-4) enrolled 227 patients at any of 60 centers, with efficacy data available from 132 of the patients. About 60% of the patients had an intracranial bleed, and about 30% had a gastrointestinal bleed, and their average age was 77 years. Roughly three-quarters of patients were on an anticoagulant for atrial fibrillation, with the rest treated for venous thromboembolism, with 4% having both conditions. The most commonly used direct factor Xa inhbitors in these patients were apixaban (Eliquis) in 105 and rivaroxaban (Xarelto) in 75. The ANNEXA-4 study has not enrolled patients treated with a direct factor Xa inhibitor anticoagulant and undergoing surgery, a setting that will be the subject of a future study, Dr. Connolly said.
Clinicians administered andexanet alfa as a bolus followed by a 2-hour continuous infusion, with hemostatic efficacy assessed 12 hours after the start of treatment. The results showed that factor Xa inhibition fell by about 75%-90% within minutes of starting the bolus and remained depressed at that level during the infusion but then began recovering by 2 hours after the stop of infusion. Andexanet is a factor Xa “decoy” molecule that acts by latching onto the inhibitor molecules and thereby preventing them from interacting with actual factor Xa, but andexanet also has a short half life and hence the effect quickly reduces once treatment stops.
“There is no doubt that andexanet rapidly decreases anti–factor Xa activity,” he said.
Adjudicated efficacy results were available for 132 patients and showed good or excellent hemostasis achieved on andexanet in 109 patients (83%), Dr. Connolly reported. The effect on hemostasis was consistent regardless of patient age, sex, bleeding site, type of anticoagulant, and dosage tested.
Thrombotic events during the 30 days following treatment occurred in 24 of 227 patients (11%) who received andexanet and were evaluable for safety. Notably, no clustering of thrombotic events occurred early, even among the 129 patients who restarted on an anticoagulant during the 30 days after treatment. Among the 129 patients who restarted on an anticoagulant, 9 (7%) had a thrombotic event during the 30-day follow-up, compared with 15 events among 98 patients (15%) who did not restart on an anticoagulant.
Dr. Connolly acknowledged that a limitation of the ANNEXA-4 study is the absence of a control group, but he added that he and his associates believed randomizing patients with a serious bleed to placebo control would not have been “practical, feasible, or ethical.”
ANNEXA-4 is sponsored by Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa). Dr. Connolly has been a consultant to Portola, and also to Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, and Sanofi-Aventis. Dr. Kirtane has received research support from several device manufacturers.
SOURCE: Connolly S. ACC 2018.
Treatment with andexanet alfa produced good or excellent hemostasis in 83% of patients in the ANNEXA-4 study, which is what matters when patients are bleeding. Clinicians want to know that you can restore coagulation to a level where you can stop bleeding, and that’s what the results show.
The lack of a reversal agent until now for direct-acting factor Xa inhibitor drugs has probably been a modest but real obstacle to widespread adoption of these agents. We can look at the example of another new oral anticoagulant, dabigatran (Pradaxa), which works by a different mechanism, specifically by inhibiting thrombin. After a reversal agent for dabigatran, idarucizumab (Praxbind) received Food and Drug Administration approval and became available in late 2015, an uptick in dabigatran prescriptions occurred. That experience shows that patients and providers want the safety net of a reversal agent. They want to know that, if there is bleeding or need for urgent surgery, there is a way to facilitate restoration of hemostasis.
It’s the same with direct factor Xa inhibitors: Some patients are concerned about the lack of a reversal agent, and having such an agent may help increase access to these agents for such patients. I think that, once andexanet becomes available for routine U.S. practice, we’ll see an uptick in prescribing of direct factor Xa inhibitors. Also, some patients who have opted for treatment with warfarin will switch to a safer class of drugs, the direct factor X a inhibitors. A myth exists that reversal agents can easily negate the anticoagulant effect of warfarin. The reality is that, despite having treatments that reverse warfarin’s effect, this is often not an easy process in actual practice.
On the safety side, there was no indication in the ANNEXA-4 results of rebound thrombosis with andexanet alfa treatment. Patients receiving a direct factor Xa inhibitor are prothrombotic – that’s why they are on an anticoagulant – so their risk for a thrombotic event is always there, especially when they are not fully anticoagulated, such as when a reversal agent is administered. We need to look to restarting treatment with an anticoagulant because these patients have a high thrombotic risk.
Gregory Piazza, MD , is a cardiologist at Brigham and Women’s Hospital in Boston. He has been an advisor to Portola Pharmaceuticals, the company developing andexanet alfa, as well as to Bayer and Pfizer, and he has received research funding from Bristol-Myers Squibb, Janssen, and Daiichi Sankyo. He made these comments in an interview .
Treatment with andexanet alfa produced good or excellent hemostasis in 83% of patients in the ANNEXA-4 study, which is what matters when patients are bleeding. Clinicians want to know that you can restore coagulation to a level where you can stop bleeding, and that’s what the results show.
The lack of a reversal agent until now for direct-acting factor Xa inhibitor drugs has probably been a modest but real obstacle to widespread adoption of these agents. We can look at the example of another new oral anticoagulant, dabigatran (Pradaxa), which works by a different mechanism, specifically by inhibiting thrombin. After a reversal agent for dabigatran, idarucizumab (Praxbind) received Food and Drug Administration approval and became available in late 2015, an uptick in dabigatran prescriptions occurred. That experience shows that patients and providers want the safety net of a reversal agent. They want to know that, if there is bleeding or need for urgent surgery, there is a way to facilitate restoration of hemostasis.
It’s the same with direct factor Xa inhibitors: Some patients are concerned about the lack of a reversal agent, and having such an agent may help increase access to these agents for such patients. I think that, once andexanet becomes available for routine U.S. practice, we’ll see an uptick in prescribing of direct factor Xa inhibitors. Also, some patients who have opted for treatment with warfarin will switch to a safer class of drugs, the direct factor X a inhibitors. A myth exists that reversal agents can easily negate the anticoagulant effect of warfarin. The reality is that, despite having treatments that reverse warfarin’s effect, this is often not an easy process in actual practice.
On the safety side, there was no indication in the ANNEXA-4 results of rebound thrombosis with andexanet alfa treatment. Patients receiving a direct factor Xa inhibitor are prothrombotic – that’s why they are on an anticoagulant – so their risk for a thrombotic event is always there, especially when they are not fully anticoagulated, such as when a reversal agent is administered. We need to look to restarting treatment with an anticoagulant because these patients have a high thrombotic risk.
Gregory Piazza, MD , is a cardiologist at Brigham and Women’s Hospital in Boston. He has been an advisor to Portola Pharmaceuticals, the company developing andexanet alfa, as well as to Bayer and Pfizer, and he has received research funding from Bristol-Myers Squibb, Janssen, and Daiichi Sankyo. He made these comments in an interview .
Treatment with andexanet alfa produced good or excellent hemostasis in 83% of patients in the ANNEXA-4 study, which is what matters when patients are bleeding. Clinicians want to know that you can restore coagulation to a level where you can stop bleeding, and that’s what the results show.
The lack of a reversal agent until now for direct-acting factor Xa inhibitor drugs has probably been a modest but real obstacle to widespread adoption of these agents. We can look at the example of another new oral anticoagulant, dabigatran (Pradaxa), which works by a different mechanism, specifically by inhibiting thrombin. After a reversal agent for dabigatran, idarucizumab (Praxbind) received Food and Drug Administration approval and became available in late 2015, an uptick in dabigatran prescriptions occurred. That experience shows that patients and providers want the safety net of a reversal agent. They want to know that, if there is bleeding or need for urgent surgery, there is a way to facilitate restoration of hemostasis.
It’s the same with direct factor Xa inhibitors: Some patients are concerned about the lack of a reversal agent, and having such an agent may help increase access to these agents for such patients. I think that, once andexanet becomes available for routine U.S. practice, we’ll see an uptick in prescribing of direct factor Xa inhibitors. Also, some patients who have opted for treatment with warfarin will switch to a safer class of drugs, the direct factor X a inhibitors. A myth exists that reversal agents can easily negate the anticoagulant effect of warfarin. The reality is that, despite having treatments that reverse warfarin’s effect, this is often not an easy process in actual practice.
On the safety side, there was no indication in the ANNEXA-4 results of rebound thrombosis with andexanet alfa treatment. Patients receiving a direct factor Xa inhibitor are prothrombotic – that’s why they are on an anticoagulant – so their risk for a thrombotic event is always there, especially when they are not fully anticoagulated, such as when a reversal agent is administered. We need to look to restarting treatment with an anticoagulant because these patients have a high thrombotic risk.
Gregory Piazza, MD , is a cardiologist at Brigham and Women’s Hospital in Boston. He has been an advisor to Portola Pharmaceuticals, the company developing andexanet alfa, as well as to Bayer and Pfizer, and he has received research funding from Bristol-Myers Squibb, Janssen, and Daiichi Sankyo. He made these comments in an interview .
ORLANDO – Andexanet alfa, a new agent that reverses the anticoagulant effect of direct factor Xa inhibitors, showed an acceptable level of efficacy and safety in 227 patients who received the drug in the agent’s pivotal trial.
These results, which placed andexanet in the same ballpark for efficacy and safety as idarucizumab (Praxbind), approved in 2015 for reversing the anticoagulant dabigatran (Pradaxa), suggest that andexanet is likely on track for its own Food and Drug Administration marketing approval, Stuart Connolly, MD, said at the annual meeting of the American College of Cardiology.
Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa) previously announced that it expected Food and Drug Administration action on its marketing application by May 2018.
Andexanet reversal “has similar efficacy and safety as seen with other reversal agents” for other types of anticoagulants, said Dr. Connolly, a professor of medicine and an electrophysiologist at McMaster University in Hamilton, Ont. In the trial results he reported, andexanet treatment of patients who were bleeding while on treatment with a direct factor Xa inhibitor had an 83% rate of hemostatic efficacy and an 11% rate of thrombotic events. By comparison, idarucizumab, the FDA-approved reversal agent for the anticoagulant dabigatran, produced a 68% hemostatic efficacy and a 6% rate of thrombotic events in the idarucizumab pivotal trial, RE-VERSE AD (N Engl J Med. 2015 Aug 6;373[6]:511-20).
The Prospective, Open-Label Study of Andexanet Alfa in Patients Receiving a Factor Xa Inhibitor Who Have Acute Major Bleeding (ANNEXA-4) enrolled 227 patients at any of 60 centers, with efficacy data available from 132 of the patients. About 60% of the patients had an intracranial bleed, and about 30% had a gastrointestinal bleed, and their average age was 77 years. Roughly three-quarters of patients were on an anticoagulant for atrial fibrillation, with the rest treated for venous thromboembolism, with 4% having both conditions. The most commonly used direct factor Xa inhbitors in these patients were apixaban (Eliquis) in 105 and rivaroxaban (Xarelto) in 75. The ANNEXA-4 study has not enrolled patients treated with a direct factor Xa inhibitor anticoagulant and undergoing surgery, a setting that will be the subject of a future study, Dr. Connolly said.
Clinicians administered andexanet alfa as a bolus followed by a 2-hour continuous infusion, with hemostatic efficacy assessed 12 hours after the start of treatment. The results showed that factor Xa inhibition fell by about 75%-90% within minutes of starting the bolus and remained depressed at that level during the infusion but then began recovering by 2 hours after the stop of infusion. Andexanet is a factor Xa “decoy” molecule that acts by latching onto the inhibitor molecules and thereby preventing them from interacting with actual factor Xa, but andexanet also has a short half life and hence the effect quickly reduces once treatment stops.
“There is no doubt that andexanet rapidly decreases anti–factor Xa activity,” he said.
Adjudicated efficacy results were available for 132 patients and showed good or excellent hemostasis achieved on andexanet in 109 patients (83%), Dr. Connolly reported. The effect on hemostasis was consistent regardless of patient age, sex, bleeding site, type of anticoagulant, and dosage tested.
Thrombotic events during the 30 days following treatment occurred in 24 of 227 patients (11%) who received andexanet and were evaluable for safety. Notably, no clustering of thrombotic events occurred early, even among the 129 patients who restarted on an anticoagulant during the 30 days after treatment. Among the 129 patients who restarted on an anticoagulant, 9 (7%) had a thrombotic event during the 30-day follow-up, compared with 15 events among 98 patients (15%) who did not restart on an anticoagulant.
Dr. Connolly acknowledged that a limitation of the ANNEXA-4 study is the absence of a control group, but he added that he and his associates believed randomizing patients with a serious bleed to placebo control would not have been “practical, feasible, or ethical.”
ANNEXA-4 is sponsored by Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa). Dr. Connolly has been a consultant to Portola, and also to Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, and Sanofi-Aventis. Dr. Kirtane has received research support from several device manufacturers.
SOURCE: Connolly S. ACC 2018.
ORLANDO – Andexanet alfa, a new agent that reverses the anticoagulant effect of direct factor Xa inhibitors, showed an acceptable level of efficacy and safety in 227 patients who received the drug in the agent’s pivotal trial.
These results, which placed andexanet in the same ballpark for efficacy and safety as idarucizumab (Praxbind), approved in 2015 for reversing the anticoagulant dabigatran (Pradaxa), suggest that andexanet is likely on track for its own Food and Drug Administration marketing approval, Stuart Connolly, MD, said at the annual meeting of the American College of Cardiology.
Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa) previously announced that it expected Food and Drug Administration action on its marketing application by May 2018.
Andexanet reversal “has similar efficacy and safety as seen with other reversal agents” for other types of anticoagulants, said Dr. Connolly, a professor of medicine and an electrophysiologist at McMaster University in Hamilton, Ont. In the trial results he reported, andexanet treatment of patients who were bleeding while on treatment with a direct factor Xa inhibitor had an 83% rate of hemostatic efficacy and an 11% rate of thrombotic events. By comparison, idarucizumab, the FDA-approved reversal agent for the anticoagulant dabigatran, produced a 68% hemostatic efficacy and a 6% rate of thrombotic events in the idarucizumab pivotal trial, RE-VERSE AD (N Engl J Med. 2015 Aug 6;373[6]:511-20).
The Prospective, Open-Label Study of Andexanet Alfa in Patients Receiving a Factor Xa Inhibitor Who Have Acute Major Bleeding (ANNEXA-4) enrolled 227 patients at any of 60 centers, with efficacy data available from 132 of the patients. About 60% of the patients had an intracranial bleed, and about 30% had a gastrointestinal bleed, and their average age was 77 years. Roughly three-quarters of patients were on an anticoagulant for atrial fibrillation, with the rest treated for venous thromboembolism, with 4% having both conditions. The most commonly used direct factor Xa inhbitors in these patients were apixaban (Eliquis) in 105 and rivaroxaban (Xarelto) in 75. The ANNEXA-4 study has not enrolled patients treated with a direct factor Xa inhibitor anticoagulant and undergoing surgery, a setting that will be the subject of a future study, Dr. Connolly said.
Clinicians administered andexanet alfa as a bolus followed by a 2-hour continuous infusion, with hemostatic efficacy assessed 12 hours after the start of treatment. The results showed that factor Xa inhibition fell by about 75%-90% within minutes of starting the bolus and remained depressed at that level during the infusion but then began recovering by 2 hours after the stop of infusion. Andexanet is a factor Xa “decoy” molecule that acts by latching onto the inhibitor molecules and thereby preventing them from interacting with actual factor Xa, but andexanet also has a short half life and hence the effect quickly reduces once treatment stops.
“There is no doubt that andexanet rapidly decreases anti–factor Xa activity,” he said.
Adjudicated efficacy results were available for 132 patients and showed good or excellent hemostasis achieved on andexanet in 109 patients (83%), Dr. Connolly reported. The effect on hemostasis was consistent regardless of patient age, sex, bleeding site, type of anticoagulant, and dosage tested.
Thrombotic events during the 30 days following treatment occurred in 24 of 227 patients (11%) who received andexanet and were evaluable for safety. Notably, no clustering of thrombotic events occurred early, even among the 129 patients who restarted on an anticoagulant during the 30 days after treatment. Among the 129 patients who restarted on an anticoagulant, 9 (7%) had a thrombotic event during the 30-day follow-up, compared with 15 events among 98 patients (15%) who did not restart on an anticoagulant.
Dr. Connolly acknowledged that a limitation of the ANNEXA-4 study is the absence of a control group, but he added that he and his associates believed randomizing patients with a serious bleed to placebo control would not have been “practical, feasible, or ethical.”
ANNEXA-4 is sponsored by Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa). Dr. Connolly has been a consultant to Portola, and also to Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, and Sanofi-Aventis. Dr. Kirtane has received research support from several device manufacturers.
SOURCE: Connolly S. ACC 2018.
REPORTING FROM ACC 18
Key clinical point:
Major finding: Hemostatic efficacy of andexanet alfa was 83%, and thrombotic events occurred in 11%.
Study details: ANNEXA-4, a single arm cohort study with 227 patients.
Disclosures: ANNEXA-4 is sponsored by Portola Pharmaceuticals, the company developing andexanet alfa (AndexXa). Dr. Connolly has been a consultant to Portola and also to Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, and Sanofi-Aventis.
Source: Connolly S. ACC 2018.
Women in medicine shout #MeToo about sexual harassment at work
Annette Katz didn’t expect to be part of a major social movement. She didn’t set out to take on a major health organization. But that all began to change when a coworker saw her fighting back tears and joined Katz to report to her union what amounted to a criminal sexual offense at a Cleveland Veterans Affairs Medical Center in 2012 and 2013.
Four years later, Katz, a licensed practical nurse at the hospital, testified in a court deposition that a male nursing assistant had shoved her into a linen closet and groped her and subjected her to an onslaught of lewd comments.
In speaking out and taking legal action, Katz joined a growing group of women who are combating sexual harassment in the medical field at every level, from patients’ bedsides to the executive boardroom.
Much as the #MeToo moment has raised awareness of sexual harassment in business, politics, media, and Hollywood, it is prompting women in medicine to take on a health system where workers have traditionally been discouraged from making waves and where hierarchies are ever-present and all-commanding. While the health care field overall has far more women than men, in many stations of power the top of the pyramid is overwhelmingly male, with women occupying the vast base.
In a recent survey, 30% of women on medical faculties reported experiencing sexual harassment at work within the past 2 years, said Reshma Jagsi, MD, who conducted the poll. That share is comparable to results in other sectors and, as elsewhere, in medicine it had been mostly taboo to discuss before last year.
“We know harassment is more common in fields where there are strong power differentials,” said Dr. Jagsi, director of the Center for Bioethics and Social Sciences in Medicine at the University of Michigan, Ann Arbor. “And we know medicine is very hierarchical.”
Workers in the health care and social assistance field reported 4,738 cases of sexual harassment from fiscal 2005 through 2015, eclipsed only by fields such as hospitality and manufacturing, where men make up a greater proportion of the workforce, according to data gathered by the Equal Employment Opportunity Commission.
A Kaiser Health News review of dozens of legal cases across the U.S. shows similar patterns in the waves of harassment cases that have cropped up in other fields, from entertainment to sports to journalism: The harassers are typically male. The alleged harasser supervises or outranks the alleged victim. There are slaps on the butt, lewd comments, and requests for sex. When superiors are confronted with reports of bad behavior, the victims, mostly women, are disbelieved, demoted, or fired.
But recently, physicians have taken to Twitter using the #MeTooMedicine tag, sharing anecdotes and linking to blogs that chronicle powerful doctors harassing them or disrobing at professional conferences.
Women who work in cardiology recently told the cardiology trade publication TCTMD that they felt the problem was particularly widespread in their specialty, where females account for 14% of the physicians. A Los Angeles anesthesiologist made waves in a blog post urging “prettier” women to adopt a “professional-looking, even severe, hair style” to be taken seriously and to consider self-defense classes.
Among those speaking out is Jennifer Gunter, MD, a San Francisco obstetrician-gynecologist, who recently wrote a blog post about being groped in 2014 by a prominent colleague at a medical conference – even naming him.
“I think nothing will change unless people are able to name people and institutions are held accountable,” she said in an interview. “I don’t think without massive public discourse and exposure that things will change.”
Lawsuits, many settled or still making their way through the courts, describe encounters.
A Florida nurse claimed that in 2014, a surgeon made lewd comments about her breasts, asking her in a room full of people if he should “refer to her as ‘JJ’ or ‘Jugs,’ ” the nurse’s lawsuit says. The nurse said she “responded that she wished to be called by her name.”
In other cases: A phlebotomist in New York alleged in a lawsuit that a doctor in her medical practice gave her a box of Valentine’s Day candy and moved in for an unwanted kiss on the mouth. A Florida medical resident alleged that a supervising doctor told her she looked like a “slutty whore.” A Nebraska nurse claimed that a doctor she traveled with to a professional conference offered to buy her a bikini, if he could see her in it, and an extra night in a hotel, if they could share the room. She declined.
A Pennsylvania nurse described the unsatisfying response she got after reporting that a colleague had pressed his pelvis against her and flipped through her phone for “naked pictures.” A supervisor to whom she reported the conduct expressed exasperation, saying “I can’t deal with this” and “What do you want?”
Kayla Behbahani, DO, chief psychiatry resident at University of Massachusetts Memorial Medical Center, did not file a lawsuit but recently wrote about sexual harassment by a subordinate. In an interview, she said her instincts were to pity the man, and also to follow a dictate that’s drilled into medical students: Don’t make waves. So, she disclosed the harassment only after another woman’s complaint launched an investigation.
“As a professional, I come from a culture where you go with the flow,” Dr. Behbahani said. “You deal with what you’re dealt. In that regard, it was a dilemma for me.”
Annette Katz, the Veterans Affairs nurse, initially didn’t complain about the harassment. A single mother with two children, she needed her job. Her attacker, MD Garrett, was also a nursing assistant but had more seniority, was a veteran, and was friends with her boss.
“I really did feel that I would lose my job,” Ms. Katz said in an interview. “I would be that troublemaker.”
But as the abuse escalated, she went to the VA inspector general and the Cleveland police.
She estimated that five times Mr. Garrett pushed her into a closet where he would ask for sex. She would “tell him ‘no’ and fight my way out of [his] grip,” her statement said. He shoved her into an unconscious patient’s bathroom and would “try to restrain me, but I eventually could break free.”
After one such assault, a colleague noticed tears in Ms. Katz’s eyes. The coworker shared with Ms. Katz that she, too, had been a target of Mr. Garrett’s lewd behavior.
Ms. Katz and the colleague filed complaints in March 2013 with their union, the police, and with their managers. That July, Mr. Garrett was indicted by a grand jury and later pleaded guilty to three counts of sexual imposition and one count of unlawful restraint. He was also dismissed from his job.
Reached by phone, Mr. Garrett said he agreed to the plea because he was facing multiple felonies and didn’t know what a jury would do. He said that even though he pleaded guilty to four misdemeanors, he did not commit the crimes of which he was accused. “There was no harassment; she and I were friends,” he said.
In 2013, Ms. Katz sued the VA, alleging that it failed to protect her from harassment and retaliated against her by refusing to give her a job-site transfer before firing her for not showing up to work.
The VA attorneys argued that the department had no direct knowledge of harassing behavior before Ms. Katz reported it, and that once it was informed, immediate action was taken. Veterans Affairs Deputy Press Secretary Lydia Blaha said in an email that anyone engaged in sexual harassment is swiftly held accountable.
The U.S. Department of Veterans Affairs agreed in February to pay $161,500 to settle Ms. Katz’s lawsuit.
Ms. Katz said it was costly and emotional to press on with her legal case but hopes it helps other women see that seeking justice is worthwhile. “I do think there are a lot of women who just suffer in silence,” she said.
Dr. Gunter, the San Francisco physician-blogger, said that needed change will come only when people who are more established across all professions stand up for those who are more junior. “Speaking quietly, going to HR – if that worked, we wouldn’t be here,” she said.
It’s ironic, she said, that as a gynecologist she’s trained to believe patients’ claims about sexual assault. In the workplace, though, it’s well known that raising such matters can backfire. She added: “Physicians should be setting a standard on this.”
KHN’s coverage of these topics is supported by the John A. Hartford Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Annette Katz didn’t expect to be part of a major social movement. She didn’t set out to take on a major health organization. But that all began to change when a coworker saw her fighting back tears and joined Katz to report to her union what amounted to a criminal sexual offense at a Cleveland Veterans Affairs Medical Center in 2012 and 2013.
Four years later, Katz, a licensed practical nurse at the hospital, testified in a court deposition that a male nursing assistant had shoved her into a linen closet and groped her and subjected her to an onslaught of lewd comments.
In speaking out and taking legal action, Katz joined a growing group of women who are combating sexual harassment in the medical field at every level, from patients’ bedsides to the executive boardroom.
Much as the #MeToo moment has raised awareness of sexual harassment in business, politics, media, and Hollywood, it is prompting women in medicine to take on a health system where workers have traditionally been discouraged from making waves and where hierarchies are ever-present and all-commanding. While the health care field overall has far more women than men, in many stations of power the top of the pyramid is overwhelmingly male, with women occupying the vast base.
In a recent survey, 30% of women on medical faculties reported experiencing sexual harassment at work within the past 2 years, said Reshma Jagsi, MD, who conducted the poll. That share is comparable to results in other sectors and, as elsewhere, in medicine it had been mostly taboo to discuss before last year.
“We know harassment is more common in fields where there are strong power differentials,” said Dr. Jagsi, director of the Center for Bioethics and Social Sciences in Medicine at the University of Michigan, Ann Arbor. “And we know medicine is very hierarchical.”
Workers in the health care and social assistance field reported 4,738 cases of sexual harassment from fiscal 2005 through 2015, eclipsed only by fields such as hospitality and manufacturing, where men make up a greater proportion of the workforce, according to data gathered by the Equal Employment Opportunity Commission.
A Kaiser Health News review of dozens of legal cases across the U.S. shows similar patterns in the waves of harassment cases that have cropped up in other fields, from entertainment to sports to journalism: The harassers are typically male. The alleged harasser supervises or outranks the alleged victim. There are slaps on the butt, lewd comments, and requests for sex. When superiors are confronted with reports of bad behavior, the victims, mostly women, are disbelieved, demoted, or fired.
But recently, physicians have taken to Twitter using the #MeTooMedicine tag, sharing anecdotes and linking to blogs that chronicle powerful doctors harassing them or disrobing at professional conferences.
Women who work in cardiology recently told the cardiology trade publication TCTMD that they felt the problem was particularly widespread in their specialty, where females account for 14% of the physicians. A Los Angeles anesthesiologist made waves in a blog post urging “prettier” women to adopt a “professional-looking, even severe, hair style” to be taken seriously and to consider self-defense classes.
Among those speaking out is Jennifer Gunter, MD, a San Francisco obstetrician-gynecologist, who recently wrote a blog post about being groped in 2014 by a prominent colleague at a medical conference – even naming him.
“I think nothing will change unless people are able to name people and institutions are held accountable,” she said in an interview. “I don’t think without massive public discourse and exposure that things will change.”
Lawsuits, many settled or still making their way through the courts, describe encounters.
A Florida nurse claimed that in 2014, a surgeon made lewd comments about her breasts, asking her in a room full of people if he should “refer to her as ‘JJ’ or ‘Jugs,’ ” the nurse’s lawsuit says. The nurse said she “responded that she wished to be called by her name.”
In other cases: A phlebotomist in New York alleged in a lawsuit that a doctor in her medical practice gave her a box of Valentine’s Day candy and moved in for an unwanted kiss on the mouth. A Florida medical resident alleged that a supervising doctor told her she looked like a “slutty whore.” A Nebraska nurse claimed that a doctor she traveled with to a professional conference offered to buy her a bikini, if he could see her in it, and an extra night in a hotel, if they could share the room. She declined.
A Pennsylvania nurse described the unsatisfying response she got after reporting that a colleague had pressed his pelvis against her and flipped through her phone for “naked pictures.” A supervisor to whom she reported the conduct expressed exasperation, saying “I can’t deal with this” and “What do you want?”
Kayla Behbahani, DO, chief psychiatry resident at University of Massachusetts Memorial Medical Center, did not file a lawsuit but recently wrote about sexual harassment by a subordinate. In an interview, she said her instincts were to pity the man, and also to follow a dictate that’s drilled into medical students: Don’t make waves. So, she disclosed the harassment only after another woman’s complaint launched an investigation.
“As a professional, I come from a culture where you go with the flow,” Dr. Behbahani said. “You deal with what you’re dealt. In that regard, it was a dilemma for me.”
Annette Katz, the Veterans Affairs nurse, initially didn’t complain about the harassment. A single mother with two children, she needed her job. Her attacker, MD Garrett, was also a nursing assistant but had more seniority, was a veteran, and was friends with her boss.
“I really did feel that I would lose my job,” Ms. Katz said in an interview. “I would be that troublemaker.”
But as the abuse escalated, she went to the VA inspector general and the Cleveland police.
She estimated that five times Mr. Garrett pushed her into a closet where he would ask for sex. She would “tell him ‘no’ and fight my way out of [his] grip,” her statement said. He shoved her into an unconscious patient’s bathroom and would “try to restrain me, but I eventually could break free.”
After one such assault, a colleague noticed tears in Ms. Katz’s eyes. The coworker shared with Ms. Katz that she, too, had been a target of Mr. Garrett’s lewd behavior.
Ms. Katz and the colleague filed complaints in March 2013 with their union, the police, and with their managers. That July, Mr. Garrett was indicted by a grand jury and later pleaded guilty to three counts of sexual imposition and one count of unlawful restraint. He was also dismissed from his job.
Reached by phone, Mr. Garrett said he agreed to the plea because he was facing multiple felonies and didn’t know what a jury would do. He said that even though he pleaded guilty to four misdemeanors, he did not commit the crimes of which he was accused. “There was no harassment; she and I were friends,” he said.
In 2013, Ms. Katz sued the VA, alleging that it failed to protect her from harassment and retaliated against her by refusing to give her a job-site transfer before firing her for not showing up to work.
The VA attorneys argued that the department had no direct knowledge of harassing behavior before Ms. Katz reported it, and that once it was informed, immediate action was taken. Veterans Affairs Deputy Press Secretary Lydia Blaha said in an email that anyone engaged in sexual harassment is swiftly held accountable.
The U.S. Department of Veterans Affairs agreed in February to pay $161,500 to settle Ms. Katz’s lawsuit.
Ms. Katz said it was costly and emotional to press on with her legal case but hopes it helps other women see that seeking justice is worthwhile. “I do think there are a lot of women who just suffer in silence,” she said.
Dr. Gunter, the San Francisco physician-blogger, said that needed change will come only when people who are more established across all professions stand up for those who are more junior. “Speaking quietly, going to HR – if that worked, we wouldn’t be here,” she said.
It’s ironic, she said, that as a gynecologist she’s trained to believe patients’ claims about sexual assault. In the workplace, though, it’s well known that raising such matters can backfire. She added: “Physicians should be setting a standard on this.”
KHN’s coverage of these topics is supported by the John A. Hartford Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Annette Katz didn’t expect to be part of a major social movement. She didn’t set out to take on a major health organization. But that all began to change when a coworker saw her fighting back tears and joined Katz to report to her union what amounted to a criminal sexual offense at a Cleveland Veterans Affairs Medical Center in 2012 and 2013.
Four years later, Katz, a licensed practical nurse at the hospital, testified in a court deposition that a male nursing assistant had shoved her into a linen closet and groped her and subjected her to an onslaught of lewd comments.
In speaking out and taking legal action, Katz joined a growing group of women who are combating sexual harassment in the medical field at every level, from patients’ bedsides to the executive boardroom.
Much as the #MeToo moment has raised awareness of sexual harassment in business, politics, media, and Hollywood, it is prompting women in medicine to take on a health system where workers have traditionally been discouraged from making waves and where hierarchies are ever-present and all-commanding. While the health care field overall has far more women than men, in many stations of power the top of the pyramid is overwhelmingly male, with women occupying the vast base.
In a recent survey, 30% of women on medical faculties reported experiencing sexual harassment at work within the past 2 years, said Reshma Jagsi, MD, who conducted the poll. That share is comparable to results in other sectors and, as elsewhere, in medicine it had been mostly taboo to discuss before last year.
“We know harassment is more common in fields where there are strong power differentials,” said Dr. Jagsi, director of the Center for Bioethics and Social Sciences in Medicine at the University of Michigan, Ann Arbor. “And we know medicine is very hierarchical.”
Workers in the health care and social assistance field reported 4,738 cases of sexual harassment from fiscal 2005 through 2015, eclipsed only by fields such as hospitality and manufacturing, where men make up a greater proportion of the workforce, according to data gathered by the Equal Employment Opportunity Commission.
A Kaiser Health News review of dozens of legal cases across the U.S. shows similar patterns in the waves of harassment cases that have cropped up in other fields, from entertainment to sports to journalism: The harassers are typically male. The alleged harasser supervises or outranks the alleged victim. There are slaps on the butt, lewd comments, and requests for sex. When superiors are confronted with reports of bad behavior, the victims, mostly women, are disbelieved, demoted, or fired.
But recently, physicians have taken to Twitter using the #MeTooMedicine tag, sharing anecdotes and linking to blogs that chronicle powerful doctors harassing them or disrobing at professional conferences.
Women who work in cardiology recently told the cardiology trade publication TCTMD that they felt the problem was particularly widespread in their specialty, where females account for 14% of the physicians. A Los Angeles anesthesiologist made waves in a blog post urging “prettier” women to adopt a “professional-looking, even severe, hair style” to be taken seriously and to consider self-defense classes.
Among those speaking out is Jennifer Gunter, MD, a San Francisco obstetrician-gynecologist, who recently wrote a blog post about being groped in 2014 by a prominent colleague at a medical conference – even naming him.
“I think nothing will change unless people are able to name people and institutions are held accountable,” she said in an interview. “I don’t think without massive public discourse and exposure that things will change.”
Lawsuits, many settled or still making their way through the courts, describe encounters.
A Florida nurse claimed that in 2014, a surgeon made lewd comments about her breasts, asking her in a room full of people if he should “refer to her as ‘JJ’ or ‘Jugs,’ ” the nurse’s lawsuit says. The nurse said she “responded that she wished to be called by her name.”
In other cases: A phlebotomist in New York alleged in a lawsuit that a doctor in her medical practice gave her a box of Valentine’s Day candy and moved in for an unwanted kiss on the mouth. A Florida medical resident alleged that a supervising doctor told her she looked like a “slutty whore.” A Nebraska nurse claimed that a doctor she traveled with to a professional conference offered to buy her a bikini, if he could see her in it, and an extra night in a hotel, if they could share the room. She declined.
A Pennsylvania nurse described the unsatisfying response she got after reporting that a colleague had pressed his pelvis against her and flipped through her phone for “naked pictures.” A supervisor to whom she reported the conduct expressed exasperation, saying “I can’t deal with this” and “What do you want?”
Kayla Behbahani, DO, chief psychiatry resident at University of Massachusetts Memorial Medical Center, did not file a lawsuit but recently wrote about sexual harassment by a subordinate. In an interview, she said her instincts were to pity the man, and also to follow a dictate that’s drilled into medical students: Don’t make waves. So, she disclosed the harassment only after another woman’s complaint launched an investigation.
“As a professional, I come from a culture where you go with the flow,” Dr. Behbahani said. “You deal with what you’re dealt. In that regard, it was a dilemma for me.”
Annette Katz, the Veterans Affairs nurse, initially didn’t complain about the harassment. A single mother with two children, she needed her job. Her attacker, MD Garrett, was also a nursing assistant but had more seniority, was a veteran, and was friends with her boss.
“I really did feel that I would lose my job,” Ms. Katz said in an interview. “I would be that troublemaker.”
But as the abuse escalated, she went to the VA inspector general and the Cleveland police.
She estimated that five times Mr. Garrett pushed her into a closet where he would ask for sex. She would “tell him ‘no’ and fight my way out of [his] grip,” her statement said. He shoved her into an unconscious patient’s bathroom and would “try to restrain me, but I eventually could break free.”
After one such assault, a colleague noticed tears in Ms. Katz’s eyes. The coworker shared with Ms. Katz that she, too, had been a target of Mr. Garrett’s lewd behavior.
Ms. Katz and the colleague filed complaints in March 2013 with their union, the police, and with their managers. That July, Mr. Garrett was indicted by a grand jury and later pleaded guilty to three counts of sexual imposition and one count of unlawful restraint. He was also dismissed from his job.
Reached by phone, Mr. Garrett said he agreed to the plea because he was facing multiple felonies and didn’t know what a jury would do. He said that even though he pleaded guilty to four misdemeanors, he did not commit the crimes of which he was accused. “There was no harassment; she and I were friends,” he said.
In 2013, Ms. Katz sued the VA, alleging that it failed to protect her from harassment and retaliated against her by refusing to give her a job-site transfer before firing her for not showing up to work.
The VA attorneys argued that the department had no direct knowledge of harassing behavior before Ms. Katz reported it, and that once it was informed, immediate action was taken. Veterans Affairs Deputy Press Secretary Lydia Blaha said in an email that anyone engaged in sexual harassment is swiftly held accountable.
The U.S. Department of Veterans Affairs agreed in February to pay $161,500 to settle Ms. Katz’s lawsuit.
Ms. Katz said it was costly and emotional to press on with her legal case but hopes it helps other women see that seeking justice is worthwhile. “I do think there are a lot of women who just suffer in silence,” she said.
Dr. Gunter, the San Francisco physician-blogger, said that needed change will come only when people who are more established across all professions stand up for those who are more junior. “Speaking quietly, going to HR – if that worked, we wouldn’t be here,” she said.
It’s ironic, she said, that as a gynecologist she’s trained to believe patients’ claims about sexual assault. In the workplace, though, it’s well known that raising such matters can backfire. She added: “Physicians should be setting a standard on this.”
KHN’s coverage of these topics is supported by the John A. Hartford Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Trauma surgeon shares story of involuntary commitment, redemption
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Survey: Litigation fears drive response to FDA power morcellator warnings
ORLANDO – A 2014 Food and Drug Administration Safety Communication warning about the risk of disseminating occult cancerous tissue when using power morcellation led to a sharp decline in its use among physicians in a large health care system, a survey and records review showed.
Of 126 ob.gyns. in the Charlotte, N.C., metro area who received the 24-question e-mail survey, 58% responded, and while 75% reported that they always or sometimes used power morcellation prior to receiving the FDA communication, more than 80% reported rarely or never using it after receiving the communication, Gerald Bernard Taylor, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Fear of litigation was cited as the reason for the change in practice by 45.7% of ob.gyns., followed by lack of access to power morcellators (34.7%), and concerns about undiagnosed malignancy (11.8%) and patient safety (5.7%), said Dr. Taylor of the Carolinas HealthCare System in Charlotte.
“We also heard from physicians about the guidelines,” he added, referring to informed consent protocols developed by a group of “key opinion leaders in gynecologic oncology and minimally invasive gynecology.” Many institutions developed moratoriums against the use of power morcellation in the wake of the FDA communication, but the Carolinas HealthCare System chose to commission these opinion leaders to address the issue, he explained.
“Interestingly enough, some [survey respondents] were not aware that the guidelines were available. Most (74.6%) thought that they were helpful when they actually reviewed them, and a few said that they were not helpful,” he said, noting that most of those who found the guidelines helpful said they felt that way because the guidelines “provide a standard of care and a possible defense against litigation.”
Analyses with respect to changes in practice after the FDA communication are ongoing but suggest that changes occurred mainly in the approach to myomectomies rather than in hysterectomy routes, Dr. Taylor said.
“We’re looking to see if there was increased use of minilaparotomy, and we are looking at the use of concealed morcellation bags right now,” he said.
The FDA Safety Communication was issued April 17, 2014 and stated that power morcellation used for hysterectomy or myomectomy in women with uterine fibroids “poses a risk of spreading unsuspected cancerous tissue, notably uterine sarcomas, beyond the uterus.”
“Health care providers and patients should carefully consider available alternative treatment options for symptomatic uterine fibroids. Based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids,” the communication stated.
A Nov. 24, 2014 update stated that “laparoscopic power morcellators are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal or are candidates for en bloc tissue removal, for example, through the vagina or minilaparotomy incision,” and “in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.”
The update also urged manufacturers of new and existing laparoscopic power morcellators to include the contraindications and a boxed warning in their product labeling and recommended that doctors share the information with their patients.
On Dec. 24, 2017, the FDA issued an updated assessment reinforcing their earlier communications. This latest update was based on a review of recent medical studies that, according to the FDA, suggested that “approximately 1 in 225 to 1 in 580 women who undergo surgery (hysterectomy or myomectomy) for presumed benign uterine growths (‘fibroids’) may have ‘occult’ or hidden uterine cancers known as sarcomas.” The FDA also said that “this is generally consistent with the 1 in 350 incidence estimated by the FDA in a 2014 review. The FDA also estimates the rate of occult leiomyosarcoma, a particularly aggressive type of sarcoma, to be approximately 1 in 495 to 1 in 1,100, again in general agreement with our previous assessment of 1 in 498.”
The FDA acknowledged that some health organizations have reported a lower estimate of risk but maintained its findings and recommendations, noting that it will continue to review new and relevant data.
Dr. Taylor reported having no disclosures.
SOURCE: Taylor GB et al. SGS 2018, Oral Poster 19.
ORLANDO – A 2014 Food and Drug Administration Safety Communication warning about the risk of disseminating occult cancerous tissue when using power morcellation led to a sharp decline in its use among physicians in a large health care system, a survey and records review showed.
Of 126 ob.gyns. in the Charlotte, N.C., metro area who received the 24-question e-mail survey, 58% responded, and while 75% reported that they always or sometimes used power morcellation prior to receiving the FDA communication, more than 80% reported rarely or never using it after receiving the communication, Gerald Bernard Taylor, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Fear of litigation was cited as the reason for the change in practice by 45.7% of ob.gyns., followed by lack of access to power morcellators (34.7%), and concerns about undiagnosed malignancy (11.8%) and patient safety (5.7%), said Dr. Taylor of the Carolinas HealthCare System in Charlotte.
“We also heard from physicians about the guidelines,” he added, referring to informed consent protocols developed by a group of “key opinion leaders in gynecologic oncology and minimally invasive gynecology.” Many institutions developed moratoriums against the use of power morcellation in the wake of the FDA communication, but the Carolinas HealthCare System chose to commission these opinion leaders to address the issue, he explained.
“Interestingly enough, some [survey respondents] were not aware that the guidelines were available. Most (74.6%) thought that they were helpful when they actually reviewed them, and a few said that they were not helpful,” he said, noting that most of those who found the guidelines helpful said they felt that way because the guidelines “provide a standard of care and a possible defense against litigation.”
Analyses with respect to changes in practice after the FDA communication are ongoing but suggest that changes occurred mainly in the approach to myomectomies rather than in hysterectomy routes, Dr. Taylor said.
“We’re looking to see if there was increased use of minilaparotomy, and we are looking at the use of concealed morcellation bags right now,” he said.
The FDA Safety Communication was issued April 17, 2014 and stated that power morcellation used for hysterectomy or myomectomy in women with uterine fibroids “poses a risk of spreading unsuspected cancerous tissue, notably uterine sarcomas, beyond the uterus.”
“Health care providers and patients should carefully consider available alternative treatment options for symptomatic uterine fibroids. Based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids,” the communication stated.
A Nov. 24, 2014 update stated that “laparoscopic power morcellators are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal or are candidates for en bloc tissue removal, for example, through the vagina or minilaparotomy incision,” and “in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.”
The update also urged manufacturers of new and existing laparoscopic power morcellators to include the contraindications and a boxed warning in their product labeling and recommended that doctors share the information with their patients.
On Dec. 24, 2017, the FDA issued an updated assessment reinforcing their earlier communications. This latest update was based on a review of recent medical studies that, according to the FDA, suggested that “approximately 1 in 225 to 1 in 580 women who undergo surgery (hysterectomy or myomectomy) for presumed benign uterine growths (‘fibroids’) may have ‘occult’ or hidden uterine cancers known as sarcomas.” The FDA also said that “this is generally consistent with the 1 in 350 incidence estimated by the FDA in a 2014 review. The FDA also estimates the rate of occult leiomyosarcoma, a particularly aggressive type of sarcoma, to be approximately 1 in 495 to 1 in 1,100, again in general agreement with our previous assessment of 1 in 498.”
The FDA acknowledged that some health organizations have reported a lower estimate of risk but maintained its findings and recommendations, noting that it will continue to review new and relevant data.
Dr. Taylor reported having no disclosures.
SOURCE: Taylor GB et al. SGS 2018, Oral Poster 19.
ORLANDO – A 2014 Food and Drug Administration Safety Communication warning about the risk of disseminating occult cancerous tissue when using power morcellation led to a sharp decline in its use among physicians in a large health care system, a survey and records review showed.
Of 126 ob.gyns. in the Charlotte, N.C., metro area who received the 24-question e-mail survey, 58% responded, and while 75% reported that they always or sometimes used power morcellation prior to receiving the FDA communication, more than 80% reported rarely or never using it after receiving the communication, Gerald Bernard Taylor, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Fear of litigation was cited as the reason for the change in practice by 45.7% of ob.gyns., followed by lack of access to power morcellators (34.7%), and concerns about undiagnosed malignancy (11.8%) and patient safety (5.7%), said Dr. Taylor of the Carolinas HealthCare System in Charlotte.
“We also heard from physicians about the guidelines,” he added, referring to informed consent protocols developed by a group of “key opinion leaders in gynecologic oncology and minimally invasive gynecology.” Many institutions developed moratoriums against the use of power morcellation in the wake of the FDA communication, but the Carolinas HealthCare System chose to commission these opinion leaders to address the issue, he explained.
“Interestingly enough, some [survey respondents] were not aware that the guidelines were available. Most (74.6%) thought that they were helpful when they actually reviewed them, and a few said that they were not helpful,” he said, noting that most of those who found the guidelines helpful said they felt that way because the guidelines “provide a standard of care and a possible defense against litigation.”
Analyses with respect to changes in practice after the FDA communication are ongoing but suggest that changes occurred mainly in the approach to myomectomies rather than in hysterectomy routes, Dr. Taylor said.
“We’re looking to see if there was increased use of minilaparotomy, and we are looking at the use of concealed morcellation bags right now,” he said.
The FDA Safety Communication was issued April 17, 2014 and stated that power morcellation used for hysterectomy or myomectomy in women with uterine fibroids “poses a risk of spreading unsuspected cancerous tissue, notably uterine sarcomas, beyond the uterus.”
“Health care providers and patients should carefully consider available alternative treatment options for symptomatic uterine fibroids. Based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids,” the communication stated.
A Nov. 24, 2014 update stated that “laparoscopic power morcellators are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal or are candidates for en bloc tissue removal, for example, through the vagina or minilaparotomy incision,” and “in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.”
The update also urged manufacturers of new and existing laparoscopic power morcellators to include the contraindications and a boxed warning in their product labeling and recommended that doctors share the information with their patients.
On Dec. 24, 2017, the FDA issued an updated assessment reinforcing their earlier communications. This latest update was based on a review of recent medical studies that, according to the FDA, suggested that “approximately 1 in 225 to 1 in 580 women who undergo surgery (hysterectomy or myomectomy) for presumed benign uterine growths (‘fibroids’) may have ‘occult’ or hidden uterine cancers known as sarcomas.” The FDA also said that “this is generally consistent with the 1 in 350 incidence estimated by the FDA in a 2014 review. The FDA also estimates the rate of occult leiomyosarcoma, a particularly aggressive type of sarcoma, to be approximately 1 in 495 to 1 in 1,100, again in general agreement with our previous assessment of 1 in 498.”
The FDA acknowledged that some health organizations have reported a lower estimate of risk but maintained its findings and recommendations, noting that it will continue to review new and relevant data.
Dr. Taylor reported having no disclosures.
SOURCE: Taylor GB et al. SGS 2018, Oral Poster 19.
REPORTING FROM SGS 2018
Key clinical point: Litigation fears drove decline in power morcellation after FDA warning.
Study details: A survey of 126 physicians.
Disclosures: Dr. Taylor reported having no disclosures.
Source: Taylor GB et al. SGS 2018, Oral Poster 19.
Bile spillage during lap cholecystectomy comes with a price
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Bile spillage that happens during laparoscopic gallbladder removal is a known problem, but a large study has put some numbers to quantify the risks to patients.
A research team at Massachusetts General Hospital, Boston, conducted a prospective study of 1,001 such operations to look at the impact of bile spillage. They found that wound infection rates in cases involving bile spillage were almost three times higher than were those without spillage and resulting hospital stays were 50% longer, according to an article in the Journal of the American College of Surgeons.
The study involved adults who had laparoscopic and laparoscopic converted to open cholecystectomy at the academic hospital during May 2010-March 2017. The latter category accounted for 95 patients, a 9.5% conversion rate. Overall, bile was spilled in 591 patients (59%), with empyema in 86 (8.6%), hydrops in 62 (6.2%), and clear bile spillage in the remainder. Bile spillage along with gallstone spillage occurred in 202 patients (20.2%), with recovery of all spilled gallstones in 145 (71.8%) of those cases.
Overall, the surgical site infection (SSI) rate was 2.4% (n = 8) in patients with no bile spillage vs. 7.1% (n = 30) for those with bile spillage. Median hospital length of stay was 2 days for the nonspillage patients vs. 3 days for those with spillage. The 30-day readmission rates were 5.9% for the nonspillage group vs. 9.6% for the spillage group.
The bile spillage rate in this study was considerably higher than previous studies had reported, the researchers noted. A retrospective study of 1,127 patients reported a spillage rate of 11.6% (World J Surg. 1999;23:1186-90). “One needs to notice that a retrospective review of medical records almost certainly underappreciates the rate of bile spillage,” the investigators wrote. A Mayo Clinic study reported a bile spillage rate of 29% and an increased risk of intra-abdominal abscesses (J Gastrointest Surg. 1997;1:85-90). The complex and acute nature of the cases at Mass General may explain their higher spillage rates, the researchers suggested.
This study identifies bile spillage, along with conversion to open surgery and patient ASA class 2 or higher as the only independent predictors of SSI. The study also found no link between empyema and hydrops with SSI, although the small number of cases may preclude an representative sample.
Nonetheless, surgeons must face the question of how to decrease SSI in laparoscopic cholecystectomy with bile spillage, study authors wrote. “First, surgeons should acknowledge that gallbladder perforations and bile spillage come at a price,” they said, “and thus should be cautious and try to avoid them.”
When bile is spilled, liberal peritoneal irrigation may be futile; this study showed similar SSI rates after bile spillage, regardless of peritoneal irrigation. “We could consider modifying perioperative antibiotic coverage,” the investigators wrote, but they acknowledged a need for more research to validate its benefit.
The investigators reported having no financial disclosures.
SOURCE: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Bile spillage during laparoscopic cholecystectomy increases the patient’s risk for surgical site infection.
Major finding: Surgical site infection rates were 7.1% in cases in which bile spillage occurred vs. 2.4% in cases that had no bile spillage.
Data source: Prospective analysis of 1,001 laparoscopic or laparoscopic converted to open operations in adults during May 2010-March 2017.
Disclosures: Dr. Velmahos and coauthors reported having no financial disclosures.
Source: Peponis T et al. J Am Coll Surg. 2018 Mar 1. doi: 10.1016/j.jamcollsurg.2017.11.025.
Match Day 2018: Surgery increases positions and matches
Surgery helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled 3% more residency slots than it did in 2017, according to the National Resident Matching Program (NRMP).
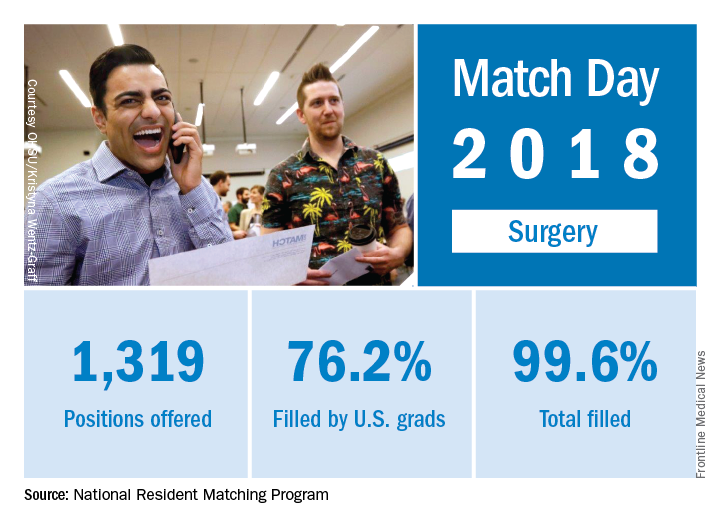
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions and PGY-1 positions filled (up 4.7% and 4.9%, respectively), and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Surgery helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled 3% more residency slots than it did in 2017, according to the National Resident Matching Program (NRMP).
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions and PGY-1 positions filled (up 4.7% and 4.9%, respectively), and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Surgery helped to make the 2018 Main Residency Match the largest ever as the specialty offered and filled 3% more residency slots than it did in 2017, according to the National Resident Matching Program (NRMP).
The 2018 Match also set new highs for total positions offered (up 4.4% over last year), total positions and PGY-1 positions filled (up 4.7% and 4.9%, respectively), and total applicants (up 1.7%). “The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.