User login
Official Newspaper of the American College of Surgeons
Breast cancer receptor change may predict outcomes
SAN FRANCISCO – A change in the status of any breast cancer tumor biomarker after neoadjuvant therapy was independently associated with a 37% decreased likelihood of recurrence in 5 years, a multivariate analysis showed.
The subtyping of breast cancer by receptor status changed in 41% of 398 samples between the initial tumor and residual disease after neoadjuvant chemotherapy.
In patients with any change in the status of estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2), after neoadjuvant chemotherapy, 63% were relapse free 5 years later as compared with 48% of patients with no receptor change, a significant difference.
Overall survival at 5 years, however, did not differ significantly based on receptor status change, Dr. Napa Parinyanitikul and her associates reported at a breast cancer symposium sponsored by the American Society of Clinical Oncology. At 5 years, 73% of patients with a receptor status change and 63% with no change were alive.
The study analyzed data on patients treated at her institution in 1992-2012 who had tumor biomarker results from pretreatment biopsies and from samples of residual disease after neoadjuvant chemotherapy. Most patients in the study were white, with clinical stage II or III disease.
Of the tumors, 49% were hormone receptor–positive and HER2 negative; 18% were HER2 positive, and 33% were negative for all three receptors (triple-negative breast cancer). Neoadjuvant chemotherapy consisted of a taxane-based regimen in 10%, an anthracycline-based regimen in 19%, an anthracycline/taxane-based regimen in 71%, and trastuzumab-based chemotherapy in 49%. The 88% of patients with hormone receptor-positive disease received adjuvant endocrine therapy with tamoxifen or an aromatase inhibitor.
After a median of 40 months of follow-up, 32% of women had died and 42% had a recurrence of breast cancer, reported Dr. Parinyanitikul, a fellow at the University of Texas MD Anderson Cancer Center, Houston.
The likelihood of receptor status changes differed significantly by the subtype of breast cancer. Of hormone receptor–positive cancers, 51% had a change in receptor status, compared with 27% of HER2-positive cancers and 22% of triple-negative breast cancers.
Other factors did not significantly affect the likelihood of receptor status change, including patient age or race, histology, tumor stage or grade, the presence of lymphovascular invasion, or the class of neoadjuvant chemotherapeutic agents.
Of ER-positive tumors, 11% changed to ER negative after neoadjuvant chemotherapy; of ER-negative tumors, 21% changed to ER positive. Of the PR-positive tumors, 35% changed to PR-negative; of PR-negative tumors, 12% changed to PR positive. Of HER2-positive tumors, 40% changed to HER2 negative; of HER2-negative tumors, 3% changed to HER2 positive. Among 35 patients treated with trastuzumab, the HER2 status changed in 16 (46%).
Patients who had tumors with an ER-negative status that did not change had the worst 5-year rates for overall survival (47%) and relapse-free survival (40%), compared with patients whose tumors had an ER-positive status did not change (81% overall survival and 63% relapse-free survival), patients whose ER status changed from positive to negative (67% and 66% survival rates, respectively), and patients whose ER status changed from negative to positive (75% and 59%, respectively).
Similarly, patients who had PR-negative tumors whose status did not change had significantly lower rates of overall survival (51%) and relapse-free survival (41%), compared with patients whose PR-positive tumor status did not change (87% and 67%, respectively), those who changed from PR positive to PR negative (78% and 73%, respectively), and patients whose PR-negative status changed to PR positive (69% and 55%, respectively).
Changes or lack of change in HER2 subgroups were not significantly associated with varying outcomes.
The investigators also looked at the absolute percent changes in ER or PR status using cutoffs in 10% increments from 10% to 50%. The 5-year overall survival rate was significantly greater in ER-positive patients who had at least a 20% change in ER status, compared with those with less than a 20% change (87% vs. 73%, respectively). The 5-year relapse-free survival rate also was significantly greater if the ER status changed by at least 20% (71%), compared with smaller ER changes (59%).
Of cancers that were hormone receptor–positive and HER2 negative before neoadjuvant chemotherapy, 20% changed to HER2-positive or triple-negative breast cancer after treatment, 12% of tumors that had been HER2 positive changed to triple negative tumors, and 2% of triple negative breast cancers changed to HER2-positive after treatment. These changes produced only one significant effect on outcomes: 5-year overall survival rates were significantly lower in patients who changed from HER2-positive to triple-negative breast cancer (23%), compared with those whose HER2-positive cancer did not change to triple negative (71%).
Larger prospective studies are needed to confirm the findings and to determine any impact of biomarker changes on long-term survival, she said.
Previous studies have reported discordance in hormone receptor status in up to 51% of breast cancers between the primary tumor and residual disease and changes in HER2 status in up to 43% of cases. Conclusions about associations between changes in receptor status and clinical outcomes have been inconsistent.
The symposium was cosponsored by the American Society of Breast Disease, the American Society of Breast Surgeons, the National Consortium of Breast Centers, the Society of Surgical Oncology, and the American Society for Radiation Oncology.
Dr. Parinyanitikul reported having no financial disclosures.
On Twitter @sherryboschert
Technical artifacts when testing receptor status in breast cancer complicate assessments of their potential ramifications on outcomes.

|
|
ER and PR status can change if you repeat the testing on the same specimen without any change in the actual marker status. In one "classic" study, the HER2 or ER status changed in 23% of samples after they were air-mailed from one center to another. You can’t conclude that it was the airplane flight that changed receptor status.
Similarly, in the current study, you can’t conclude that it was the chemotherapy that changed the receptor status, because part of this discordance is from the technical imprecision of the test. If a test is 90% accurate, for example, 10% of results on first testing will be "noise" and approximately 20% of results on repeat testing will be discordant.
The study also did not report the proportion of cases in which initial receptor status tests were conducted in one laboratory and the second test was conducted at a different center, as is often the case in the real world. That also introduces a very large, obvious cause for receptor discordance independent of therapy.
Dr. Lajos Pusztai is a professor of medicine and director of the Breast Medical Oncology Section at Yale University, New Haven, Conn. He made his remarks during a question-and-answer session at the meeting. Dr. Pusztai reported financial associations with BiPar Sciences/Sanofi, Bristol-Myers Squibb, Pfizer, AstraZeneca, Roche/Genentech, and Foundation Medicine.
Technical artifacts when testing receptor status in breast cancer complicate assessments of their potential ramifications on outcomes.

|
|
ER and PR status can change if you repeat the testing on the same specimen without any change in the actual marker status. In one "classic" study, the HER2 or ER status changed in 23% of samples after they were air-mailed from one center to another. You can’t conclude that it was the airplane flight that changed receptor status.
Similarly, in the current study, you can’t conclude that it was the chemotherapy that changed the receptor status, because part of this discordance is from the technical imprecision of the test. If a test is 90% accurate, for example, 10% of results on first testing will be "noise" and approximately 20% of results on repeat testing will be discordant.
The study also did not report the proportion of cases in which initial receptor status tests were conducted in one laboratory and the second test was conducted at a different center, as is often the case in the real world. That also introduces a very large, obvious cause for receptor discordance independent of therapy.
Dr. Lajos Pusztai is a professor of medicine and director of the Breast Medical Oncology Section at Yale University, New Haven, Conn. He made his remarks during a question-and-answer session at the meeting. Dr. Pusztai reported financial associations with BiPar Sciences/Sanofi, Bristol-Myers Squibb, Pfizer, AstraZeneca, Roche/Genentech, and Foundation Medicine.
Technical artifacts when testing receptor status in breast cancer complicate assessments of their potential ramifications on outcomes.

|
|
ER and PR status can change if you repeat the testing on the same specimen without any change in the actual marker status. In one "classic" study, the HER2 or ER status changed in 23% of samples after they were air-mailed from one center to another. You can’t conclude that it was the airplane flight that changed receptor status.
Similarly, in the current study, you can’t conclude that it was the chemotherapy that changed the receptor status, because part of this discordance is from the technical imprecision of the test. If a test is 90% accurate, for example, 10% of results on first testing will be "noise" and approximately 20% of results on repeat testing will be discordant.
The study also did not report the proportion of cases in which initial receptor status tests were conducted in one laboratory and the second test was conducted at a different center, as is often the case in the real world. That also introduces a very large, obvious cause for receptor discordance independent of therapy.
Dr. Lajos Pusztai is a professor of medicine and director of the Breast Medical Oncology Section at Yale University, New Haven, Conn. He made his remarks during a question-and-answer session at the meeting. Dr. Pusztai reported financial associations with BiPar Sciences/Sanofi, Bristol-Myers Squibb, Pfizer, AstraZeneca, Roche/Genentech, and Foundation Medicine.
SAN FRANCISCO – A change in the status of any breast cancer tumor biomarker after neoadjuvant therapy was independently associated with a 37% decreased likelihood of recurrence in 5 years, a multivariate analysis showed.
The subtyping of breast cancer by receptor status changed in 41% of 398 samples between the initial tumor and residual disease after neoadjuvant chemotherapy.
In patients with any change in the status of estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2), after neoadjuvant chemotherapy, 63% were relapse free 5 years later as compared with 48% of patients with no receptor change, a significant difference.
Overall survival at 5 years, however, did not differ significantly based on receptor status change, Dr. Napa Parinyanitikul and her associates reported at a breast cancer symposium sponsored by the American Society of Clinical Oncology. At 5 years, 73% of patients with a receptor status change and 63% with no change were alive.
The study analyzed data on patients treated at her institution in 1992-2012 who had tumor biomarker results from pretreatment biopsies and from samples of residual disease after neoadjuvant chemotherapy. Most patients in the study were white, with clinical stage II or III disease.
Of the tumors, 49% were hormone receptor–positive and HER2 negative; 18% were HER2 positive, and 33% were negative for all three receptors (triple-negative breast cancer). Neoadjuvant chemotherapy consisted of a taxane-based regimen in 10%, an anthracycline-based regimen in 19%, an anthracycline/taxane-based regimen in 71%, and trastuzumab-based chemotherapy in 49%. The 88% of patients with hormone receptor-positive disease received adjuvant endocrine therapy with tamoxifen or an aromatase inhibitor.
After a median of 40 months of follow-up, 32% of women had died and 42% had a recurrence of breast cancer, reported Dr. Parinyanitikul, a fellow at the University of Texas MD Anderson Cancer Center, Houston.
The likelihood of receptor status changes differed significantly by the subtype of breast cancer. Of hormone receptor–positive cancers, 51% had a change in receptor status, compared with 27% of HER2-positive cancers and 22% of triple-negative breast cancers.
Other factors did not significantly affect the likelihood of receptor status change, including patient age or race, histology, tumor stage or grade, the presence of lymphovascular invasion, or the class of neoadjuvant chemotherapeutic agents.
Of ER-positive tumors, 11% changed to ER negative after neoadjuvant chemotherapy; of ER-negative tumors, 21% changed to ER positive. Of the PR-positive tumors, 35% changed to PR-negative; of PR-negative tumors, 12% changed to PR positive. Of HER2-positive tumors, 40% changed to HER2 negative; of HER2-negative tumors, 3% changed to HER2 positive. Among 35 patients treated with trastuzumab, the HER2 status changed in 16 (46%).
Patients who had tumors with an ER-negative status that did not change had the worst 5-year rates for overall survival (47%) and relapse-free survival (40%), compared with patients whose tumors had an ER-positive status did not change (81% overall survival and 63% relapse-free survival), patients whose ER status changed from positive to negative (67% and 66% survival rates, respectively), and patients whose ER status changed from negative to positive (75% and 59%, respectively).
Similarly, patients who had PR-negative tumors whose status did not change had significantly lower rates of overall survival (51%) and relapse-free survival (41%), compared with patients whose PR-positive tumor status did not change (87% and 67%, respectively), those who changed from PR positive to PR negative (78% and 73%, respectively), and patients whose PR-negative status changed to PR positive (69% and 55%, respectively).
Changes or lack of change in HER2 subgroups were not significantly associated with varying outcomes.
The investigators also looked at the absolute percent changes in ER or PR status using cutoffs in 10% increments from 10% to 50%. The 5-year overall survival rate was significantly greater in ER-positive patients who had at least a 20% change in ER status, compared with those with less than a 20% change (87% vs. 73%, respectively). The 5-year relapse-free survival rate also was significantly greater if the ER status changed by at least 20% (71%), compared with smaller ER changes (59%).
Of cancers that were hormone receptor–positive and HER2 negative before neoadjuvant chemotherapy, 20% changed to HER2-positive or triple-negative breast cancer after treatment, 12% of tumors that had been HER2 positive changed to triple negative tumors, and 2% of triple negative breast cancers changed to HER2-positive after treatment. These changes produced only one significant effect on outcomes: 5-year overall survival rates were significantly lower in patients who changed from HER2-positive to triple-negative breast cancer (23%), compared with those whose HER2-positive cancer did not change to triple negative (71%).
Larger prospective studies are needed to confirm the findings and to determine any impact of biomarker changes on long-term survival, she said.
Previous studies have reported discordance in hormone receptor status in up to 51% of breast cancers between the primary tumor and residual disease and changes in HER2 status in up to 43% of cases. Conclusions about associations between changes in receptor status and clinical outcomes have been inconsistent.
The symposium was cosponsored by the American Society of Breast Disease, the American Society of Breast Surgeons, the National Consortium of Breast Centers, the Society of Surgical Oncology, and the American Society for Radiation Oncology.
Dr. Parinyanitikul reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A change in the status of any breast cancer tumor biomarker after neoadjuvant therapy was independently associated with a 37% decreased likelihood of recurrence in 5 years, a multivariate analysis showed.
The subtyping of breast cancer by receptor status changed in 41% of 398 samples between the initial tumor and residual disease after neoadjuvant chemotherapy.
In patients with any change in the status of estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2), after neoadjuvant chemotherapy, 63% were relapse free 5 years later as compared with 48% of patients with no receptor change, a significant difference.
Overall survival at 5 years, however, did not differ significantly based on receptor status change, Dr. Napa Parinyanitikul and her associates reported at a breast cancer symposium sponsored by the American Society of Clinical Oncology. At 5 years, 73% of patients with a receptor status change and 63% with no change were alive.
The study analyzed data on patients treated at her institution in 1992-2012 who had tumor biomarker results from pretreatment biopsies and from samples of residual disease after neoadjuvant chemotherapy. Most patients in the study were white, with clinical stage II or III disease.
Of the tumors, 49% were hormone receptor–positive and HER2 negative; 18% were HER2 positive, and 33% were negative for all three receptors (triple-negative breast cancer). Neoadjuvant chemotherapy consisted of a taxane-based regimen in 10%, an anthracycline-based regimen in 19%, an anthracycline/taxane-based regimen in 71%, and trastuzumab-based chemotherapy in 49%. The 88% of patients with hormone receptor-positive disease received adjuvant endocrine therapy with tamoxifen or an aromatase inhibitor.
After a median of 40 months of follow-up, 32% of women had died and 42% had a recurrence of breast cancer, reported Dr. Parinyanitikul, a fellow at the University of Texas MD Anderson Cancer Center, Houston.
The likelihood of receptor status changes differed significantly by the subtype of breast cancer. Of hormone receptor–positive cancers, 51% had a change in receptor status, compared with 27% of HER2-positive cancers and 22% of triple-negative breast cancers.
Other factors did not significantly affect the likelihood of receptor status change, including patient age or race, histology, tumor stage or grade, the presence of lymphovascular invasion, or the class of neoadjuvant chemotherapeutic agents.
Of ER-positive tumors, 11% changed to ER negative after neoadjuvant chemotherapy; of ER-negative tumors, 21% changed to ER positive. Of the PR-positive tumors, 35% changed to PR-negative; of PR-negative tumors, 12% changed to PR positive. Of HER2-positive tumors, 40% changed to HER2 negative; of HER2-negative tumors, 3% changed to HER2 positive. Among 35 patients treated with trastuzumab, the HER2 status changed in 16 (46%).
Patients who had tumors with an ER-negative status that did not change had the worst 5-year rates for overall survival (47%) and relapse-free survival (40%), compared with patients whose tumors had an ER-positive status did not change (81% overall survival and 63% relapse-free survival), patients whose ER status changed from positive to negative (67% and 66% survival rates, respectively), and patients whose ER status changed from negative to positive (75% and 59%, respectively).
Similarly, patients who had PR-negative tumors whose status did not change had significantly lower rates of overall survival (51%) and relapse-free survival (41%), compared with patients whose PR-positive tumor status did not change (87% and 67%, respectively), those who changed from PR positive to PR negative (78% and 73%, respectively), and patients whose PR-negative status changed to PR positive (69% and 55%, respectively).
Changes or lack of change in HER2 subgroups were not significantly associated with varying outcomes.
The investigators also looked at the absolute percent changes in ER or PR status using cutoffs in 10% increments from 10% to 50%. The 5-year overall survival rate was significantly greater in ER-positive patients who had at least a 20% change in ER status, compared with those with less than a 20% change (87% vs. 73%, respectively). The 5-year relapse-free survival rate also was significantly greater if the ER status changed by at least 20% (71%), compared with smaller ER changes (59%).
Of cancers that were hormone receptor–positive and HER2 negative before neoadjuvant chemotherapy, 20% changed to HER2-positive or triple-negative breast cancer after treatment, 12% of tumors that had been HER2 positive changed to triple negative tumors, and 2% of triple negative breast cancers changed to HER2-positive after treatment. These changes produced only one significant effect on outcomes: 5-year overall survival rates were significantly lower in patients who changed from HER2-positive to triple-negative breast cancer (23%), compared with those whose HER2-positive cancer did not change to triple negative (71%).
Larger prospective studies are needed to confirm the findings and to determine any impact of biomarker changes on long-term survival, she said.
Previous studies have reported discordance in hormone receptor status in up to 51% of breast cancers between the primary tumor and residual disease and changes in HER2 status in up to 43% of cases. Conclusions about associations between changes in receptor status and clinical outcomes have been inconsistent.
The symposium was cosponsored by the American Society of Breast Disease, the American Society of Breast Surgeons, the National Consortium of Breast Centers, the Society of Surgical Oncology, and the American Society for Radiation Oncology.
Dr. Parinyanitikul reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
Major finding: Receptor status changed in 41% of breast cancers after neoadjuvant chemotherapy. Relapse within 5 years was significantly less likely in patients with a receptor change (63%) than in those with no receptor change (48%).
Data source: A retrospective study of 398 women with data on ER, PR, and HER2 status in the primary tumor and in residual disease after neoadjuvant chemotherapy.
Disclosures: Dr. Parinyanitikul reported having no financial disclosures.
Losartan shown effective in Marfan syndrome
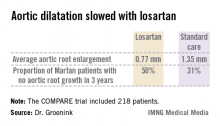
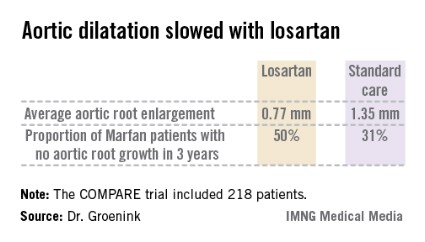
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall.
Dr. Groenink said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect obtainable with other angiotensin II receptor antagonists, though he suspects it’s a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible.
"I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better the results," he explained.
Marfan syndrome is a genetic connective tissue disorder affecting multiple organ systems. The prognosis is mainly determined by the aortic complications, including dilatation, aneurysm formation, and possible acute dissection. Affected individuals tend to be tall, long-limbed, and have distinctively long, thin fingers. The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
The COMPARE trial was funded by the Dutch Heart Association. Dr. Groenink reported having no relevant financial interests.
*CORRECTION 11/14/13: The first version of this story had Dr. Groenink's name misspelled.

|
Bruce Jancin/IMNG Medical Media
|
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.

|
Bruce Jancin/IMNG Medical Media
|
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.

|
Bruce Jancin/IMNG Medical Media
|
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall.
Dr. Groenink said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect obtainable with other angiotensin II receptor antagonists, though he suspects it’s a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible.
"I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better the results," he explained.
Marfan syndrome is a genetic connective tissue disorder affecting multiple organ systems. The prognosis is mainly determined by the aortic complications, including dilatation, aneurysm formation, and possible acute dissection. Affected individuals tend to be tall, long-limbed, and have distinctively long, thin fingers. The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
The COMPARE trial was funded by the Dutch Heart Association. Dr. Groenink reported having no relevant financial interests.
*CORRECTION 11/14/13: The first version of this story had Dr. Groenink's name misspelled.
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall.
Dr. Groenink said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect obtainable with other angiotensin II receptor antagonists, though he suspects it’s a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible.
"I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better the results," he explained.
Marfan syndrome is a genetic connective tissue disorder affecting multiple organ systems. The prognosis is mainly determined by the aortic complications, including dilatation, aneurysm formation, and possible acute dissection. Affected individuals tend to be tall, long-limbed, and have distinctively long, thin fingers. The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
The COMPARE trial was funded by the Dutch Heart Association. Dr. Groenink reported having no relevant financial interests.
*CORRECTION 11/14/13: The first version of this story had Dr. Groenink's name misspelled.
AT THE ESC CONGRESS 2013
Major finding: The rate of aortic root enlargement during 3 years of prospective follow-up was 0.77 mm in losartan-treated patients with Marfan syndrome, significantly less than the 1.35 mm in patients on standard-of-care treatment with no losartan.
Data source: The COMPARE trial was a randomized, prospective, open-label multicenter study in which 218 patients with Marfan syndrome were randomized to losartan at a target dose of 100 mg or to no losartan and followed for 3 years with the aortic root dilatation rate as measured by MRI the primary endpoint.
Disclosures: The COMPARE trial was supported by the Dutch Heart Association. Dr. Groenink reported having no financial conflicts.
Two studies document a rise in gun wounds, homicides
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that state passed a law making it legal to carry a concealed weapon without a permit or training. In one New Jersey trauma center, the rate of deaths among gunshot wound victims rose from 8% in 2000 to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds
Data source: A retrospective review of 6,323 gunshot wounds treated at one New Jersey trauma center from 2000-2011, and a retrospective review of data in southern Arizona 2 years before and after a 2010 law repealed concealed-carry limits.
Disclosures: Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
Hospice usage up but not delivered soon enough, study finds
LEBANON, N.H. – Medicare patients with advanced cancer are more likely to receive hospice care than in previous years, although it is still too late in their treatment to deliver the full benefits of palliative care, according to a report issued by the Dartmouth Institute for Health Policy and Clinical Practice.
The report also states that geography and the treatment styles favored by individual health systems, rather than patient preferences, drive the level of intensive, end-of-life treatments used.
The findings are part of the Dartmouth Atlas Project, which uses Medicare data to examine how health care resources are allocated nationally. The report is the institute’s first longitudinal analysis of trends in end-of-life care for advanced cancer patients across regions, academic medical centers, and National Cancer Institute–designated cancer centers.
Controlling for patient age, sex, race, tumor type, and non–cancer-related comorbidities, the investigators found that, when compared with similar data collected from 2003 to 2007 and published by the institute in 2010, the number of advanced cancer patients on Medicare dying in the hospital decreased by an average of 28.8% during 2003-2007 to 24.7% in 2010. An increase from 54.6% to 61.3% in the number of patients who were enrolled in hospice in the last month of life was also found. The number of patients for whom hospice was initiated during the last 3 days of life increased from 8.3% during 2003-2007 to 10.9% in 2010.
When asked in an interview about the importance of starting hospice sooner in terminal care, Dr. Lorenzo Norris, director of psycho-oncology services at George Washington University Medical Center in Washington, said, "The biggest misconception is that hospice is strictly for end of life. Palliative care is just good medicine. If you limit the hospice care to the last 3 days, you’ve already limited the options a patient has. If you offer palliative care 5 or 6 months out, you can start reducing symptom burdens and increase a patient’s quality of life, which is very important because during that last year to 6 months is when patients are finishing unresolved financial and relationship issues. Palliative care allows them to more fully engage in their life."
When viewed according to the medical center delivering the care, between 13% and 50% of Medicare patients with advanced cancer died in a hospital in 2010, rather than in a hospice setting – typically the patient’s home. These figures include data from NCI-designated cancer centers. Hospice treatment in the last month of life for patients treated in mid- and northwestern states such as Oregon and Iowa trended as much as nearly 50% higher than in places such as Alaska and New York City.
Addressing the reasons for regional variations in care, Dr. Ira Byock, director of palliative medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., wrote in an accompanying editorial that, "Previous research has also shown that regional supply of health care resources, such as hospital and intensive care beds and imaging equipment, is one driver of the intensity of care, irrespective of the patient’s particular condition or illness level."
The analysts found the overall rate of ICU admissions for treatments such as intubation, a feeding tube, or cardiopulmonary resuscitation during the last month of life increased from 23.7% in the period between 2003 and 2007 to 28.8% in 2010. The number of days patients spent in the ICU in the last month of life varied more than fivefold across all centers, the analysts wrote.
"Our research continues to find that patients with advanced cancer are often receiving aggressive care until their final days, when we know that most patients would prefer care directed toward a better quality of life through hospice and palliative services. The increase in patients admitted to hospice care only days before death suggests that hospice services are often provided too late to provide much benefit," Dr. David C. Goodman, coprincipal investigator for the Dartmouth Atlas Project, said in a statement.
When asked why some oncologists are not referring their patients to hospice sooner, Dr. Clifford Hudis, president of the American Society of Clinical Oncology said, "There are many circumstances, based on culture, family dynamics, and patient’s wishes, where it is hard to communicate the value of hospice services. Some patients remain fearful of the very word and, in some situations, there is an unwillingness to acknowledge the severity of illnesses. These barriers can often be overcome through an increase in communication between doctors and patients about care goals and wishes."
When asked about the potential economic implications of the data, Dr. Goodman said, "The goal of better end-of-life care is to improve patient well-being. Often, it is less expensive to provide good care that patients want, [rather] than the usual care that patients receive."
The report also indicated that the number of patients who saw 10 or more different physicians during the last six months of their lives rose from 46.2% to 58.5%. The analysts interpreted this to mean "more patients may have experienced fragmented care."
In a statement Dr. Hudis encouraged the oncology community to "keep striving to deliver the right care at the right time." In an e-mail interview, Dr. Hudis wrote that, "The overall trend is a good one because it is concordant with the overall goals of ASCO: to make sure that every patient has access to the highest quality care throughout their disease experience."
Dr. Goodman and Dr. Byock report no relevant disclosures. The report was principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders including the WellPoint Foundation, the United Health Foundation, and the California HealthCare Foundation.
LEBANON, N.H. – Medicare patients with advanced cancer are more likely to receive hospice care than in previous years, although it is still too late in their treatment to deliver the full benefits of palliative care, according to a report issued by the Dartmouth Institute for Health Policy and Clinical Practice.
The report also states that geography and the treatment styles favored by individual health systems, rather than patient preferences, drive the level of intensive, end-of-life treatments used.
The findings are part of the Dartmouth Atlas Project, which uses Medicare data to examine how health care resources are allocated nationally. The report is the institute’s first longitudinal analysis of trends in end-of-life care for advanced cancer patients across regions, academic medical centers, and National Cancer Institute–designated cancer centers.
Controlling for patient age, sex, race, tumor type, and non–cancer-related comorbidities, the investigators found that, when compared with similar data collected from 2003 to 2007 and published by the institute in 2010, the number of advanced cancer patients on Medicare dying in the hospital decreased by an average of 28.8% during 2003-2007 to 24.7% in 2010. An increase from 54.6% to 61.3% in the number of patients who were enrolled in hospice in the last month of life was also found. The number of patients for whom hospice was initiated during the last 3 days of life increased from 8.3% during 2003-2007 to 10.9% in 2010.
When asked in an interview about the importance of starting hospice sooner in terminal care, Dr. Lorenzo Norris, director of psycho-oncology services at George Washington University Medical Center in Washington, said, "The biggest misconception is that hospice is strictly for end of life. Palliative care is just good medicine. If you limit the hospice care to the last 3 days, you’ve already limited the options a patient has. If you offer palliative care 5 or 6 months out, you can start reducing symptom burdens and increase a patient’s quality of life, which is very important because during that last year to 6 months is when patients are finishing unresolved financial and relationship issues. Palliative care allows them to more fully engage in their life."
When viewed according to the medical center delivering the care, between 13% and 50% of Medicare patients with advanced cancer died in a hospital in 2010, rather than in a hospice setting – typically the patient’s home. These figures include data from NCI-designated cancer centers. Hospice treatment in the last month of life for patients treated in mid- and northwestern states such as Oregon and Iowa trended as much as nearly 50% higher than in places such as Alaska and New York City.
Addressing the reasons for regional variations in care, Dr. Ira Byock, director of palliative medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., wrote in an accompanying editorial that, "Previous research has also shown that regional supply of health care resources, such as hospital and intensive care beds and imaging equipment, is one driver of the intensity of care, irrespective of the patient’s particular condition or illness level."
The analysts found the overall rate of ICU admissions for treatments such as intubation, a feeding tube, or cardiopulmonary resuscitation during the last month of life increased from 23.7% in the period between 2003 and 2007 to 28.8% in 2010. The number of days patients spent in the ICU in the last month of life varied more than fivefold across all centers, the analysts wrote.
"Our research continues to find that patients with advanced cancer are often receiving aggressive care until their final days, when we know that most patients would prefer care directed toward a better quality of life through hospice and palliative services. The increase in patients admitted to hospice care only days before death suggests that hospice services are often provided too late to provide much benefit," Dr. David C. Goodman, coprincipal investigator for the Dartmouth Atlas Project, said in a statement.
When asked why some oncologists are not referring their patients to hospice sooner, Dr. Clifford Hudis, president of the American Society of Clinical Oncology said, "There are many circumstances, based on culture, family dynamics, and patient’s wishes, where it is hard to communicate the value of hospice services. Some patients remain fearful of the very word and, in some situations, there is an unwillingness to acknowledge the severity of illnesses. These barriers can often be overcome through an increase in communication between doctors and patients about care goals and wishes."
When asked about the potential economic implications of the data, Dr. Goodman said, "The goal of better end-of-life care is to improve patient well-being. Often, it is less expensive to provide good care that patients want, [rather] than the usual care that patients receive."
The report also indicated that the number of patients who saw 10 or more different physicians during the last six months of their lives rose from 46.2% to 58.5%. The analysts interpreted this to mean "more patients may have experienced fragmented care."
In a statement Dr. Hudis encouraged the oncology community to "keep striving to deliver the right care at the right time." In an e-mail interview, Dr. Hudis wrote that, "The overall trend is a good one because it is concordant with the overall goals of ASCO: to make sure that every patient has access to the highest quality care throughout their disease experience."
Dr. Goodman and Dr. Byock report no relevant disclosures. The report was principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders including the WellPoint Foundation, the United Health Foundation, and the California HealthCare Foundation.
LEBANON, N.H. – Medicare patients with advanced cancer are more likely to receive hospice care than in previous years, although it is still too late in their treatment to deliver the full benefits of palliative care, according to a report issued by the Dartmouth Institute for Health Policy and Clinical Practice.
The report also states that geography and the treatment styles favored by individual health systems, rather than patient preferences, drive the level of intensive, end-of-life treatments used.
The findings are part of the Dartmouth Atlas Project, which uses Medicare data to examine how health care resources are allocated nationally. The report is the institute’s first longitudinal analysis of trends in end-of-life care for advanced cancer patients across regions, academic medical centers, and National Cancer Institute–designated cancer centers.
Controlling for patient age, sex, race, tumor type, and non–cancer-related comorbidities, the investigators found that, when compared with similar data collected from 2003 to 2007 and published by the institute in 2010, the number of advanced cancer patients on Medicare dying in the hospital decreased by an average of 28.8% during 2003-2007 to 24.7% in 2010. An increase from 54.6% to 61.3% in the number of patients who were enrolled in hospice in the last month of life was also found. The number of patients for whom hospice was initiated during the last 3 days of life increased from 8.3% during 2003-2007 to 10.9% in 2010.
When asked in an interview about the importance of starting hospice sooner in terminal care, Dr. Lorenzo Norris, director of psycho-oncology services at George Washington University Medical Center in Washington, said, "The biggest misconception is that hospice is strictly for end of life. Palliative care is just good medicine. If you limit the hospice care to the last 3 days, you’ve already limited the options a patient has. If you offer palliative care 5 or 6 months out, you can start reducing symptom burdens and increase a patient’s quality of life, which is very important because during that last year to 6 months is when patients are finishing unresolved financial and relationship issues. Palliative care allows them to more fully engage in their life."
When viewed according to the medical center delivering the care, between 13% and 50% of Medicare patients with advanced cancer died in a hospital in 2010, rather than in a hospice setting – typically the patient’s home. These figures include data from NCI-designated cancer centers. Hospice treatment in the last month of life for patients treated in mid- and northwestern states such as Oregon and Iowa trended as much as nearly 50% higher than in places such as Alaska and New York City.
Addressing the reasons for regional variations in care, Dr. Ira Byock, director of palliative medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., wrote in an accompanying editorial that, "Previous research has also shown that regional supply of health care resources, such as hospital and intensive care beds and imaging equipment, is one driver of the intensity of care, irrespective of the patient’s particular condition or illness level."
The analysts found the overall rate of ICU admissions for treatments such as intubation, a feeding tube, or cardiopulmonary resuscitation during the last month of life increased from 23.7% in the period between 2003 and 2007 to 28.8% in 2010. The number of days patients spent in the ICU in the last month of life varied more than fivefold across all centers, the analysts wrote.
"Our research continues to find that patients with advanced cancer are often receiving aggressive care until their final days, when we know that most patients would prefer care directed toward a better quality of life through hospice and palliative services. The increase in patients admitted to hospice care only days before death suggests that hospice services are often provided too late to provide much benefit," Dr. David C. Goodman, coprincipal investigator for the Dartmouth Atlas Project, said in a statement.
When asked why some oncologists are not referring their patients to hospice sooner, Dr. Clifford Hudis, president of the American Society of Clinical Oncology said, "There are many circumstances, based on culture, family dynamics, and patient’s wishes, where it is hard to communicate the value of hospice services. Some patients remain fearful of the very word and, in some situations, there is an unwillingness to acknowledge the severity of illnesses. These barriers can often be overcome through an increase in communication between doctors and patients about care goals and wishes."
When asked about the potential economic implications of the data, Dr. Goodman said, "The goal of better end-of-life care is to improve patient well-being. Often, it is less expensive to provide good care that patients want, [rather] than the usual care that patients receive."
The report also indicated that the number of patients who saw 10 or more different physicians during the last six months of their lives rose from 46.2% to 58.5%. The analysts interpreted this to mean "more patients may have experienced fragmented care."
In a statement Dr. Hudis encouraged the oncology community to "keep striving to deliver the right care at the right time." In an e-mail interview, Dr. Hudis wrote that, "The overall trend is a good one because it is concordant with the overall goals of ASCO: to make sure that every patient has access to the highest quality care throughout their disease experience."
Dr. Goodman and Dr. Byock report no relevant disclosures. The report was principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders including the WellPoint Foundation, the United Health Foundation, and the California HealthCare Foundation.
EXPERT ANALYSIS FROM THE DARTMOUTH ATLAS PROJECT
High-volume, low-mortality hospitals have lowest postsurgical readmissions
Hospitals that conduct a high volume of surgical procedures and have a low 30-day mortality rate have lower readmission rates, according to a new study. Even so, about one in seven patients discharged after major surgery is readmitted in the first 30 days, the authors found.
The researchers also showed that strictly following surgical process measures – such as infection control techniques – was only weakly associated with reduced readmissions.
The results are not terribly surprising, according to the authors, Dr. Thomas C. Tsai and his colleagues from Harvard University, Brigham and Women’s Hospital, and the Veterans Affairs Boston Healthcare System. The researchers could not specifically determine why the higher-volume, lower-mortality hospitals had lower readmission rates, but they speculated that these facilities have systems in place to protect surgical patients from bad outcomes that might bring them back to the hospital. Their study was published Sept. 18 in the New England Journal of Medicine (2013;369:1134-42).
The Medicare program now penalizes hospitals for excess readmissions after discharge for heart failure, heart attack, and pneumonia. For fiscal year 2013, which ends on Oct. 1, hospitals will be penalized 1% of their total Medicare billings if readmissions are too high. In fiscal 2014, chronic obstructive pulmonary disease and coronary artery bypass grafting will be added to the list of monitored conditions. The penalty rises to 2% in fiscal year 2014 and 3% in fiscal 2015. In coming years, the Centers for Medicare and Medicaid Services is expected to add more surgical procedures to the readmission penalty list.
The researchers analyzed national Medicare data, which comprised 479,471 discharges from 3,004 hospitals. These hospitals accounted for 90% of the discharges for the six major procedures studied: coronary artery bypass grafting, pulmonary lobectomy, endovascular repair of abdominal aortic aneurysm, open repair of AAA, colectomy, and hip replacement. The authors also analyzed Hospital Quality Alliance (HQA) surgical care scores. The HQA score is calculated based on how well hospitals perform on process measures established by the Surgical Care Improvement Project.
The three measures of surgical quality included the HQA score, procedure volume, and 30-day mortality. The primary outcome measure was a hospital-level composite of the six procedure-specific, risk-adjusted readmission rates at 30 days. The authors compared the characteristics of patients who were readmitted within 30 days with those who were not, and compared the characteristics of hospitals that had composite readmission rates above the median with those that had rates below the median.
The median composite risk-adjusted 30-day readmission rate was 13%. Patients who were readmitted tended to be older (78 years vs. 77 years) and had more comorbidities. The hospitals with readmission rates below the median were more likely to be nonprofit, nonteaching, and located in the West. They also had a higher number of full-time nurses per 1,000 patient-days and a lower proportion of Medicaid patients.
There was no significant difference between urban and rural hospitals.
The authors used multivariate models to gauge the impact of quality measures on readmission rates. After accounting for hospital characteristics, they found that hospitals with the highest volume of procedures had a readmission rate just under the median, compared with those with the lowest procedure volumes, which had a readmission rate of close to 17%.
Hospitals in the lowest quartile for mortality rates had a 13% readmission rate, compared with 14% for those in the highest mortality quartile.
Overall, there was no significant difference in readmissions between the hospitals that performed the best on the HQA score and those that were the poorest performers. That might be because there was only a very small variation in performance on the HQA score – with a median of 99% for high performers and 92% for low performers, said the authors.
Policymakers should be reassured by their consistent findings that readmissions are linked to certain quality measures – volume and mortality, the investigators said. But a direct link is still not definitive, said Dr. Tsai and his colleagues. Previous studies have indicated that volume did help reduce readmissions, while others have shown no relationship.
But those studies were conducted before the widespread use of minimally invasive procedures and process measures aimed at reducing postsurgical complications, the authors said.
The authors reported no relevant conflicts of interest.
On Twitter @aliciaault
Readmissions have clearly become a tremendous focus for payers and oversight agencies. The Readmission Reduction Program put forth by the Centers for Medicare and Medicaid Services (CMS) will potentially penalize hospitals up to 3% for high readmission rates in fiscal year 2015. This penalty is higher than for any other CMS pay-for-performance programs. The main CMS measure compares hospitals on risk-adjusted all-cause hospital-wide readmissions.
The study by Tsai and his colleagues concluded that surgical readmission rates are a relevant and valid approach to measure surgical quality. However, this has been the topic of much debate in the surgical community, and admittedly, my thinking has evolved on this topic.
Readmissions have gained momentum because they are undoubtedly costly, but they also certainly adversely affect quality of life for the patient. Readmission quality metrics were initially pioneered for medical admissions. Medical readmissions were thought to be caused by issues with the transition from the inpatient team to the outpatient physicians; thus there was potentially a systems-based intervention that could be implemented. Hospitals were able to reduce readmission rates with early postdischarge follow-up visits to intervene (e.g., weigh patients, assess symptoms, and adjust diuretics for heart failure patients) and better coordination of care.
Surgeons have argued that readmissions after medical admissions differ considerably from readmissions after surgery. Surgical readmissions are almost entirely caused by postoperative complications, whereas readmissions after medical admissions are due to worsening of the clinical problem or issues with coordination of care. Thus, surgeons have suggested that surgical readmissions are not preventable with a change in postoperative follow-up visits or an improvement in coordination of care. Thus, some may argue that readmissions are unavoidable and simply an aggregate measure of postdischarge postoperative complications. Some also suggest that surgeons are penalized twice: once for the postoperative complication and again for the readmission that is likely related to the complication.
While this was my initial inclination, I do now believe there is value in readmission as a quality measure. There are likely many opportunities for hospitals to reduce readmissions and cost by dealing with more complications in the outpatient setting. For example, if a hospital has a high readmission rate and they find it is caused by surgical site infection (SSI), they could implement an outpatient system to deal with SSIs without needing to readmit patients. Hospitals have had success with this approach and have been able to insert PICC lines for antibiotics, open incisions, debride wounds, and place negative pressure wound therapy in the outpatient clinic.
In 2014, the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) will provide hospitals with risk-adjusted readmission rates. Since the CMS measure only provides an overall, hospital-wide rate, hospitals will need to examine their readmission performance for surgical patients overall and for individual surgeries to identify targeted opportunities for improvement. The ACS NSQIP will fill this need. Moreover, since the ACS NSQIP data abstractors record the reason for the readmission and other patient variables, ACS NSQIP hospitals will be able to better understand why the readmission happened and develop strategies to reduce readmissions. Hospitals will also be able to share experiences and best practices through the ACS NSQIP community to drive down readmission rates.
While readmission may not initially make intuitive sense as a surgical quality measure, it will likely prompt improvements in care for the patients and reduce costs for payers and hospitals, making it a worthwhile focus for quality improvement efforts.
Dr. Karl Bilimoria is an ACS Faculty Scholar and a surgical oncologist at Northwestern Memorial Hospital, Chicago, and an assistant professor of surgery at the Northwestern University Feinberg School of Medicine. He is also director of the Surgical Outcomes and Quality Improvement Center at Northwestern University.
Readmissions have clearly become a tremendous focus for payers and oversight agencies. The Readmission Reduction Program put forth by the Centers for Medicare and Medicaid Services (CMS) will potentially penalize hospitals up to 3% for high readmission rates in fiscal year 2015. This penalty is higher than for any other CMS pay-for-performance programs. The main CMS measure compares hospitals on risk-adjusted all-cause hospital-wide readmissions.
The study by Tsai and his colleagues concluded that surgical readmission rates are a relevant and valid approach to measure surgical quality. However, this has been the topic of much debate in the surgical community, and admittedly, my thinking has evolved on this topic.
Readmissions have gained momentum because they are undoubtedly costly, but they also certainly adversely affect quality of life for the patient. Readmission quality metrics were initially pioneered for medical admissions. Medical readmissions were thought to be caused by issues with the transition from the inpatient team to the outpatient physicians; thus there was potentially a systems-based intervention that could be implemented. Hospitals were able to reduce readmission rates with early postdischarge follow-up visits to intervene (e.g., weigh patients, assess symptoms, and adjust diuretics for heart failure patients) and better coordination of care.
Surgeons have argued that readmissions after medical admissions differ considerably from readmissions after surgery. Surgical readmissions are almost entirely caused by postoperative complications, whereas readmissions after medical admissions are due to worsening of the clinical problem or issues with coordination of care. Thus, surgeons have suggested that surgical readmissions are not preventable with a change in postoperative follow-up visits or an improvement in coordination of care. Thus, some may argue that readmissions are unavoidable and simply an aggregate measure of postdischarge postoperative complications. Some also suggest that surgeons are penalized twice: once for the postoperative complication and again for the readmission that is likely related to the complication.
While this was my initial inclination, I do now believe there is value in readmission as a quality measure. There are likely many opportunities for hospitals to reduce readmissions and cost by dealing with more complications in the outpatient setting. For example, if a hospital has a high readmission rate and they find it is caused by surgical site infection (SSI), they could implement an outpatient system to deal with SSIs without needing to readmit patients. Hospitals have had success with this approach and have been able to insert PICC lines for antibiotics, open incisions, debride wounds, and place negative pressure wound therapy in the outpatient clinic.
In 2014, the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) will provide hospitals with risk-adjusted readmission rates. Since the CMS measure only provides an overall, hospital-wide rate, hospitals will need to examine their readmission performance for surgical patients overall and for individual surgeries to identify targeted opportunities for improvement. The ACS NSQIP will fill this need. Moreover, since the ACS NSQIP data abstractors record the reason for the readmission and other patient variables, ACS NSQIP hospitals will be able to better understand why the readmission happened and develop strategies to reduce readmissions. Hospitals will also be able to share experiences and best practices through the ACS NSQIP community to drive down readmission rates.
While readmission may not initially make intuitive sense as a surgical quality measure, it will likely prompt improvements in care for the patients and reduce costs for payers and hospitals, making it a worthwhile focus for quality improvement efforts.
Dr. Karl Bilimoria is an ACS Faculty Scholar and a surgical oncologist at Northwestern Memorial Hospital, Chicago, and an assistant professor of surgery at the Northwestern University Feinberg School of Medicine. He is also director of the Surgical Outcomes and Quality Improvement Center at Northwestern University.
Readmissions have clearly become a tremendous focus for payers and oversight agencies. The Readmission Reduction Program put forth by the Centers for Medicare and Medicaid Services (CMS) will potentially penalize hospitals up to 3% for high readmission rates in fiscal year 2015. This penalty is higher than for any other CMS pay-for-performance programs. The main CMS measure compares hospitals on risk-adjusted all-cause hospital-wide readmissions.
The study by Tsai and his colleagues concluded that surgical readmission rates are a relevant and valid approach to measure surgical quality. However, this has been the topic of much debate in the surgical community, and admittedly, my thinking has evolved on this topic.
Readmissions have gained momentum because they are undoubtedly costly, but they also certainly adversely affect quality of life for the patient. Readmission quality metrics were initially pioneered for medical admissions. Medical readmissions were thought to be caused by issues with the transition from the inpatient team to the outpatient physicians; thus there was potentially a systems-based intervention that could be implemented. Hospitals were able to reduce readmission rates with early postdischarge follow-up visits to intervene (e.g., weigh patients, assess symptoms, and adjust diuretics for heart failure patients) and better coordination of care.
Surgeons have argued that readmissions after medical admissions differ considerably from readmissions after surgery. Surgical readmissions are almost entirely caused by postoperative complications, whereas readmissions after medical admissions are due to worsening of the clinical problem or issues with coordination of care. Thus, surgeons have suggested that surgical readmissions are not preventable with a change in postoperative follow-up visits or an improvement in coordination of care. Thus, some may argue that readmissions are unavoidable and simply an aggregate measure of postdischarge postoperative complications. Some also suggest that surgeons are penalized twice: once for the postoperative complication and again for the readmission that is likely related to the complication.
While this was my initial inclination, I do now believe there is value in readmission as a quality measure. There are likely many opportunities for hospitals to reduce readmissions and cost by dealing with more complications in the outpatient setting. For example, if a hospital has a high readmission rate and they find it is caused by surgical site infection (SSI), they could implement an outpatient system to deal with SSIs without needing to readmit patients. Hospitals have had success with this approach and have been able to insert PICC lines for antibiotics, open incisions, debride wounds, and place negative pressure wound therapy in the outpatient clinic.
In 2014, the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) will provide hospitals with risk-adjusted readmission rates. Since the CMS measure only provides an overall, hospital-wide rate, hospitals will need to examine their readmission performance for surgical patients overall and for individual surgeries to identify targeted opportunities for improvement. The ACS NSQIP will fill this need. Moreover, since the ACS NSQIP data abstractors record the reason for the readmission and other patient variables, ACS NSQIP hospitals will be able to better understand why the readmission happened and develop strategies to reduce readmissions. Hospitals will also be able to share experiences and best practices through the ACS NSQIP community to drive down readmission rates.
While readmission may not initially make intuitive sense as a surgical quality measure, it will likely prompt improvements in care for the patients and reduce costs for payers and hospitals, making it a worthwhile focus for quality improvement efforts.
Dr. Karl Bilimoria is an ACS Faculty Scholar and a surgical oncologist at Northwestern Memorial Hospital, Chicago, and an assistant professor of surgery at the Northwestern University Feinberg School of Medicine. He is also director of the Surgical Outcomes and Quality Improvement Center at Northwestern University.
Hospitals that conduct a high volume of surgical procedures and have a low 30-day mortality rate have lower readmission rates, according to a new study. Even so, about one in seven patients discharged after major surgery is readmitted in the first 30 days, the authors found.
The researchers also showed that strictly following surgical process measures – such as infection control techniques – was only weakly associated with reduced readmissions.
The results are not terribly surprising, according to the authors, Dr. Thomas C. Tsai and his colleagues from Harvard University, Brigham and Women’s Hospital, and the Veterans Affairs Boston Healthcare System. The researchers could not specifically determine why the higher-volume, lower-mortality hospitals had lower readmission rates, but they speculated that these facilities have systems in place to protect surgical patients from bad outcomes that might bring them back to the hospital. Their study was published Sept. 18 in the New England Journal of Medicine (2013;369:1134-42).
The Medicare program now penalizes hospitals for excess readmissions after discharge for heart failure, heart attack, and pneumonia. For fiscal year 2013, which ends on Oct. 1, hospitals will be penalized 1% of their total Medicare billings if readmissions are too high. In fiscal 2014, chronic obstructive pulmonary disease and coronary artery bypass grafting will be added to the list of monitored conditions. The penalty rises to 2% in fiscal year 2014 and 3% in fiscal 2015. In coming years, the Centers for Medicare and Medicaid Services is expected to add more surgical procedures to the readmission penalty list.
The researchers analyzed national Medicare data, which comprised 479,471 discharges from 3,004 hospitals. These hospitals accounted for 90% of the discharges for the six major procedures studied: coronary artery bypass grafting, pulmonary lobectomy, endovascular repair of abdominal aortic aneurysm, open repair of AAA, colectomy, and hip replacement. The authors also analyzed Hospital Quality Alliance (HQA) surgical care scores. The HQA score is calculated based on how well hospitals perform on process measures established by the Surgical Care Improvement Project.
The three measures of surgical quality included the HQA score, procedure volume, and 30-day mortality. The primary outcome measure was a hospital-level composite of the six procedure-specific, risk-adjusted readmission rates at 30 days. The authors compared the characteristics of patients who were readmitted within 30 days with those who were not, and compared the characteristics of hospitals that had composite readmission rates above the median with those that had rates below the median.
The median composite risk-adjusted 30-day readmission rate was 13%. Patients who were readmitted tended to be older (78 years vs. 77 years) and had more comorbidities. The hospitals with readmission rates below the median were more likely to be nonprofit, nonteaching, and located in the West. They also had a higher number of full-time nurses per 1,000 patient-days and a lower proportion of Medicaid patients.
There was no significant difference between urban and rural hospitals.
The authors used multivariate models to gauge the impact of quality measures on readmission rates. After accounting for hospital characteristics, they found that hospitals with the highest volume of procedures had a readmission rate just under the median, compared with those with the lowest procedure volumes, which had a readmission rate of close to 17%.
Hospitals in the lowest quartile for mortality rates had a 13% readmission rate, compared with 14% for those in the highest mortality quartile.
Overall, there was no significant difference in readmissions between the hospitals that performed the best on the HQA score and those that were the poorest performers. That might be because there was only a very small variation in performance on the HQA score – with a median of 99% for high performers and 92% for low performers, said the authors.
Policymakers should be reassured by their consistent findings that readmissions are linked to certain quality measures – volume and mortality, the investigators said. But a direct link is still not definitive, said Dr. Tsai and his colleagues. Previous studies have indicated that volume did help reduce readmissions, while others have shown no relationship.
But those studies were conducted before the widespread use of minimally invasive procedures and process measures aimed at reducing postsurgical complications, the authors said.
The authors reported no relevant conflicts of interest.
On Twitter @aliciaault
Hospitals that conduct a high volume of surgical procedures and have a low 30-day mortality rate have lower readmission rates, according to a new study. Even so, about one in seven patients discharged after major surgery is readmitted in the first 30 days, the authors found.
The researchers also showed that strictly following surgical process measures – such as infection control techniques – was only weakly associated with reduced readmissions.
The results are not terribly surprising, according to the authors, Dr. Thomas C. Tsai and his colleagues from Harvard University, Brigham and Women’s Hospital, and the Veterans Affairs Boston Healthcare System. The researchers could not specifically determine why the higher-volume, lower-mortality hospitals had lower readmission rates, but they speculated that these facilities have systems in place to protect surgical patients from bad outcomes that might bring them back to the hospital. Their study was published Sept. 18 in the New England Journal of Medicine (2013;369:1134-42).
The Medicare program now penalizes hospitals for excess readmissions after discharge for heart failure, heart attack, and pneumonia. For fiscal year 2013, which ends on Oct. 1, hospitals will be penalized 1% of their total Medicare billings if readmissions are too high. In fiscal 2014, chronic obstructive pulmonary disease and coronary artery bypass grafting will be added to the list of monitored conditions. The penalty rises to 2% in fiscal year 2014 and 3% in fiscal 2015. In coming years, the Centers for Medicare and Medicaid Services is expected to add more surgical procedures to the readmission penalty list.
The researchers analyzed national Medicare data, which comprised 479,471 discharges from 3,004 hospitals. These hospitals accounted for 90% of the discharges for the six major procedures studied: coronary artery bypass grafting, pulmonary lobectomy, endovascular repair of abdominal aortic aneurysm, open repair of AAA, colectomy, and hip replacement. The authors also analyzed Hospital Quality Alliance (HQA) surgical care scores. The HQA score is calculated based on how well hospitals perform on process measures established by the Surgical Care Improvement Project.
The three measures of surgical quality included the HQA score, procedure volume, and 30-day mortality. The primary outcome measure was a hospital-level composite of the six procedure-specific, risk-adjusted readmission rates at 30 days. The authors compared the characteristics of patients who were readmitted within 30 days with those who were not, and compared the characteristics of hospitals that had composite readmission rates above the median with those that had rates below the median.
The median composite risk-adjusted 30-day readmission rate was 13%. Patients who were readmitted tended to be older (78 years vs. 77 years) and had more comorbidities. The hospitals with readmission rates below the median were more likely to be nonprofit, nonteaching, and located in the West. They also had a higher number of full-time nurses per 1,000 patient-days and a lower proportion of Medicaid patients.
There was no significant difference between urban and rural hospitals.
The authors used multivariate models to gauge the impact of quality measures on readmission rates. After accounting for hospital characteristics, they found that hospitals with the highest volume of procedures had a readmission rate just under the median, compared with those with the lowest procedure volumes, which had a readmission rate of close to 17%.
Hospitals in the lowest quartile for mortality rates had a 13% readmission rate, compared with 14% for those in the highest mortality quartile.
Overall, there was no significant difference in readmissions between the hospitals that performed the best on the HQA score and those that were the poorest performers. That might be because there was only a very small variation in performance on the HQA score – with a median of 99% for high performers and 92% for low performers, said the authors.
Policymakers should be reassured by their consistent findings that readmissions are linked to certain quality measures – volume and mortality, the investigators said. But a direct link is still not definitive, said Dr. Tsai and his colleagues. Previous studies have indicated that volume did help reduce readmissions, while others have shown no relationship.
But those studies were conducted before the widespread use of minimally invasive procedures and process measures aimed at reducing postsurgical complications, the authors said.
The authors reported no relevant conflicts of interest.
On Twitter @aliciaault
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: Hospitals with the highest surgical volume and lowest 30-day mortality rates had the lowest 30-day readmission rates for six major surgical procedures.
Data source: A bivariate and multivariate analysis of Medicare data on 479,471 discharges from 3,004 hospitals.
Disclosures: The authors reported no relevant conflicts of interest.
How was your night, Doc? The limits of disclosure in preop
This morning I had the usual 7:30 a.m. elective surgical case scheduled. As I usually do, I went to see my patient at around 7 a.m. to review the procedure, answer any new questions that may have come up, and mark the incision site. My patient greeted me very cheerfully with the following questions, "How was your night? Did you sleep OK? Are you feeling good this morning? No arguments at home, I hope?" I readily answered, as I almost always do, when discussing things with patients in the preop area, that I am feeling good and ready for things to go well with the case.
I have been asked such questions many times over the years. However, for some reason the interchange with my patient this morning raised additional questions for me: Is it really acceptable for patients to ask such questions? Do I have an obligation to disclose such things? Do patients really want to know the answers or are they simply making nervous conversation?
In recent years, there have been a number of articles questioning whether surgeons should be required to disclose a lack of sleep to their elective surgical patients so that the patient can make a "truly informed" decision about what the risks of their surgery are. Thus far, there have been no such requirements at any hospital in the United States that I know of. But my patient’s questions raised a number of practical issues for me with such disclosure. We had already had a conversation in my office when I originally obtained consent for the procedure. I had carefully reviewed risks, benefits, and alternatives to the operation, and I had answered a list of the patient’s questions. Since I was actually the patient’s third opinion, it was clear that the patient already had significant background knowledge about the operation. The patient had signed the consent form before leaving my office.
At some point, before, during, or after my conversation with the patient, he had decided to trust me enough to allow me to do the operation. Subsequently, while home in the days prior to the surgery date, the patient had the opportunity to change his mind, but he actually came to the hospital on the morning of surgery. He had thus actively expressed his confidence in me by showing up for surgery. In this context, I believe that the patient’s questions were really a friendly way of expressing some degree of anxiety about the operation rather than an actual second guessing of my capacity to optimally perform the surgery. In this context, I believe that it is more important that I try to alleviate the patient’s concerns than that I give an expansive discourse on whatever stressful issues may be going on in my personal life.
Of particular importance is the issue of how much I have slept. I do not believe that I should discuss any concerns I may have with lack of sleep with my patient unless I have decided that I am not the best person to perform the surgery. I do not think that I would be doing my patient a service by, for example, saying that I didn’t sleep well and studies show that I might have altered judgment and asking the patient to sign a document that I have disclosed this fact. Such a disclosure seems to be designed to protect the surgeon and the institution rather than the patient.
However, if I believe that my lack of sleep, my personal stressors, or any other distraction will significantly hinder my ability to perform the operation safely, then I should not simply disclose these issues to the patient. Rather, I should explain why I should NOT be doing the surgery and either postpone the case or find someone else to do it if the patient requests this and if it is possible. Although some commentators have suggested that a sleep-deprived surgeon is the worst person to be able to assess his or her abilities to optimally perform an operation, I am convinced that we need to depend on the surgeon to make this assessment. Three central required components of professionalism are the exercise of self-regulation, the capacity to make decisions that are altruistic, and the discipline to abide by ethical standards. The issue of self-regulation is absolutely critical to the professionalism of any surgeon. The professionalism of the surgeon is the basis for patients trusting us to operate on them and make decisions in the operating room on their behalf. To mandate a separate disclosure to the patient about the amount of sleep the surgeon got the night before, or any other distracting issue, would be to cast doubt on the professionalism of the surgeon at the very time that patients most need to trust their surgeons.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
This morning I had the usual 7:30 a.m. elective surgical case scheduled. As I usually do, I went to see my patient at around 7 a.m. to review the procedure, answer any new questions that may have come up, and mark the incision site. My patient greeted me very cheerfully with the following questions, "How was your night? Did you sleep OK? Are you feeling good this morning? No arguments at home, I hope?" I readily answered, as I almost always do, when discussing things with patients in the preop area, that I am feeling good and ready for things to go well with the case.
I have been asked such questions many times over the years. However, for some reason the interchange with my patient this morning raised additional questions for me: Is it really acceptable for patients to ask such questions? Do I have an obligation to disclose such things? Do patients really want to know the answers or are they simply making nervous conversation?
In recent years, there have been a number of articles questioning whether surgeons should be required to disclose a lack of sleep to their elective surgical patients so that the patient can make a "truly informed" decision about what the risks of their surgery are. Thus far, there have been no such requirements at any hospital in the United States that I know of. But my patient’s questions raised a number of practical issues for me with such disclosure. We had already had a conversation in my office when I originally obtained consent for the procedure. I had carefully reviewed risks, benefits, and alternatives to the operation, and I had answered a list of the patient’s questions. Since I was actually the patient’s third opinion, it was clear that the patient already had significant background knowledge about the operation. The patient had signed the consent form before leaving my office.
At some point, before, during, or after my conversation with the patient, he had decided to trust me enough to allow me to do the operation. Subsequently, while home in the days prior to the surgery date, the patient had the opportunity to change his mind, but he actually came to the hospital on the morning of surgery. He had thus actively expressed his confidence in me by showing up for surgery. In this context, I believe that the patient’s questions were really a friendly way of expressing some degree of anxiety about the operation rather than an actual second guessing of my capacity to optimally perform the surgery. In this context, I believe that it is more important that I try to alleviate the patient’s concerns than that I give an expansive discourse on whatever stressful issues may be going on in my personal life.
Of particular importance is the issue of how much I have slept. I do not believe that I should discuss any concerns I may have with lack of sleep with my patient unless I have decided that I am not the best person to perform the surgery. I do not think that I would be doing my patient a service by, for example, saying that I didn’t sleep well and studies show that I might have altered judgment and asking the patient to sign a document that I have disclosed this fact. Such a disclosure seems to be designed to protect the surgeon and the institution rather than the patient.
However, if I believe that my lack of sleep, my personal stressors, or any other distraction will significantly hinder my ability to perform the operation safely, then I should not simply disclose these issues to the patient. Rather, I should explain why I should NOT be doing the surgery and either postpone the case or find someone else to do it if the patient requests this and if it is possible. Although some commentators have suggested that a sleep-deprived surgeon is the worst person to be able to assess his or her abilities to optimally perform an operation, I am convinced that we need to depend on the surgeon to make this assessment. Three central required components of professionalism are the exercise of self-regulation, the capacity to make decisions that are altruistic, and the discipline to abide by ethical standards. The issue of self-regulation is absolutely critical to the professionalism of any surgeon. The professionalism of the surgeon is the basis for patients trusting us to operate on them and make decisions in the operating room on their behalf. To mandate a separate disclosure to the patient about the amount of sleep the surgeon got the night before, or any other distracting issue, would be to cast doubt on the professionalism of the surgeon at the very time that patients most need to trust their surgeons.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
This morning I had the usual 7:30 a.m. elective surgical case scheduled. As I usually do, I went to see my patient at around 7 a.m. to review the procedure, answer any new questions that may have come up, and mark the incision site. My patient greeted me very cheerfully with the following questions, "How was your night? Did you sleep OK? Are you feeling good this morning? No arguments at home, I hope?" I readily answered, as I almost always do, when discussing things with patients in the preop area, that I am feeling good and ready for things to go well with the case.
I have been asked such questions many times over the years. However, for some reason the interchange with my patient this morning raised additional questions for me: Is it really acceptable for patients to ask such questions? Do I have an obligation to disclose such things? Do patients really want to know the answers or are they simply making nervous conversation?
In recent years, there have been a number of articles questioning whether surgeons should be required to disclose a lack of sleep to their elective surgical patients so that the patient can make a "truly informed" decision about what the risks of their surgery are. Thus far, there have been no such requirements at any hospital in the United States that I know of. But my patient’s questions raised a number of practical issues for me with such disclosure. We had already had a conversation in my office when I originally obtained consent for the procedure. I had carefully reviewed risks, benefits, and alternatives to the operation, and I had answered a list of the patient’s questions. Since I was actually the patient’s third opinion, it was clear that the patient already had significant background knowledge about the operation. The patient had signed the consent form before leaving my office.
At some point, before, during, or after my conversation with the patient, he had decided to trust me enough to allow me to do the operation. Subsequently, while home in the days prior to the surgery date, the patient had the opportunity to change his mind, but he actually came to the hospital on the morning of surgery. He had thus actively expressed his confidence in me by showing up for surgery. In this context, I believe that the patient’s questions were really a friendly way of expressing some degree of anxiety about the operation rather than an actual second guessing of my capacity to optimally perform the surgery. In this context, I believe that it is more important that I try to alleviate the patient’s concerns than that I give an expansive discourse on whatever stressful issues may be going on in my personal life.
Of particular importance is the issue of how much I have slept. I do not believe that I should discuss any concerns I may have with lack of sleep with my patient unless I have decided that I am not the best person to perform the surgery. I do not think that I would be doing my patient a service by, for example, saying that I didn’t sleep well and studies show that I might have altered judgment and asking the patient to sign a document that I have disclosed this fact. Such a disclosure seems to be designed to protect the surgeon and the institution rather than the patient.
However, if I believe that my lack of sleep, my personal stressors, or any other distraction will significantly hinder my ability to perform the operation safely, then I should not simply disclose these issues to the patient. Rather, I should explain why I should NOT be doing the surgery and either postpone the case or find someone else to do it if the patient requests this and if it is possible. Although some commentators have suggested that a sleep-deprived surgeon is the worst person to be able to assess his or her abilities to optimally perform an operation, I am convinced that we need to depend on the surgeon to make this assessment. Three central required components of professionalism are the exercise of self-regulation, the capacity to make decisions that are altruistic, and the discipline to abide by ethical standards. The issue of self-regulation is absolutely critical to the professionalism of any surgeon. The professionalism of the surgeon is the basis for patients trusting us to operate on them and make decisions in the operating room on their behalf. To mandate a separate disclosure to the patient about the amount of sleep the surgeon got the night before, or any other distracting issue, would be to cast doubt on the professionalism of the surgeon at the very time that patients most need to trust their surgeons.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
Sling surgery bests physiotherapy as initial treatment
Among women who had moderate to severe stress urinary incontinence, those who underwent midurethral-sling surgery as the first line of treatment showed significantly more improvement 1 year later than did women whose initial treatment was physiotherapy, according to a report published online Sept. 18 in the New England Journal of Medicine.
In a randomized Dutch trial involving 460 patients, 49 experienced gynecologists and urologists, and 83 certified pelvic physiotherapists, 1-year rates of both subjective and objective improvement, as well as rates of subjective and objective cure, were markedly higher for women who had immediate surgery than for those who had immediate physiotherapy, reported Dr. Julien Labrie of the University of Utrecht (the Netherlands) Medical Center and his associates.
Improvement in all secondary outcomes also was significantly better with initial surgery than with initial physiotherapy. These included urogenital symptoms, disease-specific quality of life, and the development of new urinary symptoms. However, all 65 adverse events that occurred in the study were related to surgery, including intraoperative bladder perforations, vaginal epithelial perforations, excessive blood loss, and four cases in which reoperation was required.
"Our findings suggest that women with this condition should be counseled regarding both pelvic-floor muscle training and midurethral-sling surgery as initial treatment options. Information on expected outcomes with both interventions, as well as on the potential, albeit infrequent, complications of surgery, will allow for individualized decision making by each woman and her health care provider," the investigators noted.
Dr. Labrie and his colleagues performed this study because standard practice is to recommend physiotherapy as first-line treatment, and to proceed to surgery only if that fails. Yet outcomes from midurethral-sling surgery and physiotherapy have never been directly compared.
Their study involved women aged 35-80 years whose stress urinary incontinence was classified as moderate or severe according to the Sandvik index. These subjects were randomly assigned to receive either initial surgery (230 women) or initial physiotherapy (230 women) at four university medical centers and 19 general hospitals over a 2-year period.
Both retropubic and transobturator midurethral-sling surgical approaches were allowed. Physiotherapy included an average of nine sessions delivered over 18 weeks, and could include biofeedback assistance or functional electrostimulation therapy.
The women were allowed to cross over to the other group if they were not satisfied with their assigned treatment, as "is consistent with usual clinical practice." The data were analyzed on an intention-to-treat basis. However, because approximately half of the physiotherapy group crossed over to surgery after a mean of 31 weeks, the investigators also performed a post hoc per-protocol analysis.
The primary outcome was subjective improvement in symptoms of stress urinary incontinence at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I) scale. In the intention-to-treat analysis, the rate of this outcome was 90.8% with immediate surgery, significantly higher than the 64.4% rate with immediate physiotherapy, Dr. Labrie and his associates reported (New Engl. J. Med. 2013;369:1124-33 [doi: 10.1056/NEJMoa1210627]).
The pattern was the same when outcomes were assessed objectively using a cough stress test.
Both study groups showed improvement over time in urogenital symptoms as measured by the Urogenital Distress Inventory (UDI) and in disease-specific quality of life as measured by the Incontinence Impact Questionnaire (IIQ). The improvements were significantly greater in the immediate-surgery group for incontinence and overactive bladder, "but with only moderate effect sizes," the authors said.
Similarly, improvements were significantly greater in the immediate-surgery group for subscores regarding patients’ mobility and embarrassment, "but again with only moderate effect sizes," the researchers said.
In the post hoc per-protocol analysis, they compared the 103 women who only had physiotherapy, the 99 who had physiotherapy but crossed over to surgery, and the 215 who only had surgery. At 1 year, improvement in the physiotherapy-only group was lower by approximately 62% than in the crossover group and by 59% in the surgery-only group.
Adverse events, which occurred only in women who underwent surgery, included 6 cases of bladder perforation, 10 cases of vaginal epithelial perforation, 6 reoperations for tape exposure, 1 reoperation to loosen a too-tight synthetic sling, 20 hematomas, 18 cases of new-onset urge urinary incontinence, and 3 cases of excessive blood loss.
This study may have been limited by selection bias, because "women with a preference for surgery may have been more likely to participate in the study, because they otherwise would have received initial physiotherapy according to Dutch guidelines," Dr. Labrie and his associates said.
The study was supported by the Netherlands Organization for Health Research and Development (ZonMW) and was performed "without the support or involvement of manufacturers of midurethral slings." Several coauthors reported financial ties to Ethicon, American Medical Systems, and AMS. The remainder of the authors reported no relevant financial conflicts of interest.
Among women who had moderate to severe stress urinary incontinence, those who underwent midurethral-sling surgery as the first line of treatment showed significantly more improvement 1 year later than did women whose initial treatment was physiotherapy, according to a report published online Sept. 18 in the New England Journal of Medicine.
In a randomized Dutch trial involving 460 patients, 49 experienced gynecologists and urologists, and 83 certified pelvic physiotherapists, 1-year rates of both subjective and objective improvement, as well as rates of subjective and objective cure, were markedly higher for women who had immediate surgery than for those who had immediate physiotherapy, reported Dr. Julien Labrie of the University of Utrecht (the Netherlands) Medical Center and his associates.
Improvement in all secondary outcomes also was significantly better with initial surgery than with initial physiotherapy. These included urogenital symptoms, disease-specific quality of life, and the development of new urinary symptoms. However, all 65 adverse events that occurred in the study were related to surgery, including intraoperative bladder perforations, vaginal epithelial perforations, excessive blood loss, and four cases in which reoperation was required.
"Our findings suggest that women with this condition should be counseled regarding both pelvic-floor muscle training and midurethral-sling surgery as initial treatment options. Information on expected outcomes with both interventions, as well as on the potential, albeit infrequent, complications of surgery, will allow for individualized decision making by each woman and her health care provider," the investigators noted.
Dr. Labrie and his colleagues performed this study because standard practice is to recommend physiotherapy as first-line treatment, and to proceed to surgery only if that fails. Yet outcomes from midurethral-sling surgery and physiotherapy have never been directly compared.
Their study involved women aged 35-80 years whose stress urinary incontinence was classified as moderate or severe according to the Sandvik index. These subjects were randomly assigned to receive either initial surgery (230 women) or initial physiotherapy (230 women) at four university medical centers and 19 general hospitals over a 2-year period.
Both retropubic and transobturator midurethral-sling surgical approaches were allowed. Physiotherapy included an average of nine sessions delivered over 18 weeks, and could include biofeedback assistance or functional electrostimulation therapy.
The women were allowed to cross over to the other group if they were not satisfied with their assigned treatment, as "is consistent with usual clinical practice." The data were analyzed on an intention-to-treat basis. However, because approximately half of the physiotherapy group crossed over to surgery after a mean of 31 weeks, the investigators also performed a post hoc per-protocol analysis.
The primary outcome was subjective improvement in symptoms of stress urinary incontinence at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I) scale. In the intention-to-treat analysis, the rate of this outcome was 90.8% with immediate surgery, significantly higher than the 64.4% rate with immediate physiotherapy, Dr. Labrie and his associates reported (New Engl. J. Med. 2013;369:1124-33 [doi: 10.1056/NEJMoa1210627]).
The pattern was the same when outcomes were assessed objectively using a cough stress test.
Both study groups showed improvement over time in urogenital symptoms as measured by the Urogenital Distress Inventory (UDI) and in disease-specific quality of life as measured by the Incontinence Impact Questionnaire (IIQ). The improvements were significantly greater in the immediate-surgery group for incontinence and overactive bladder, "but with only moderate effect sizes," the authors said.
Similarly, improvements were significantly greater in the immediate-surgery group for subscores regarding patients’ mobility and embarrassment, "but again with only moderate effect sizes," the researchers said.
In the post hoc per-protocol analysis, they compared the 103 women who only had physiotherapy, the 99 who had physiotherapy but crossed over to surgery, and the 215 who only had surgery. At 1 year, improvement in the physiotherapy-only group was lower by approximately 62% than in the crossover group and by 59% in the surgery-only group.
Adverse events, which occurred only in women who underwent surgery, included 6 cases of bladder perforation, 10 cases of vaginal epithelial perforation, 6 reoperations for tape exposure, 1 reoperation to loosen a too-tight synthetic sling, 20 hematomas, 18 cases of new-onset urge urinary incontinence, and 3 cases of excessive blood loss.
This study may have been limited by selection bias, because "women with a preference for surgery may have been more likely to participate in the study, because they otherwise would have received initial physiotherapy according to Dutch guidelines," Dr. Labrie and his associates said.
The study was supported by the Netherlands Organization for Health Research and Development (ZonMW) and was performed "without the support or involvement of manufacturers of midurethral slings." Several coauthors reported financial ties to Ethicon, American Medical Systems, and AMS. The remainder of the authors reported no relevant financial conflicts of interest.
Among women who had moderate to severe stress urinary incontinence, those who underwent midurethral-sling surgery as the first line of treatment showed significantly more improvement 1 year later than did women whose initial treatment was physiotherapy, according to a report published online Sept. 18 in the New England Journal of Medicine.
In a randomized Dutch trial involving 460 patients, 49 experienced gynecologists and urologists, and 83 certified pelvic physiotherapists, 1-year rates of both subjective and objective improvement, as well as rates of subjective and objective cure, were markedly higher for women who had immediate surgery than for those who had immediate physiotherapy, reported Dr. Julien Labrie of the University of Utrecht (the Netherlands) Medical Center and his associates.
Improvement in all secondary outcomes also was significantly better with initial surgery than with initial physiotherapy. These included urogenital symptoms, disease-specific quality of life, and the development of new urinary symptoms. However, all 65 adverse events that occurred in the study were related to surgery, including intraoperative bladder perforations, vaginal epithelial perforations, excessive blood loss, and four cases in which reoperation was required.
"Our findings suggest that women with this condition should be counseled regarding both pelvic-floor muscle training and midurethral-sling surgery as initial treatment options. Information on expected outcomes with both interventions, as well as on the potential, albeit infrequent, complications of surgery, will allow for individualized decision making by each woman and her health care provider," the investigators noted.
Dr. Labrie and his colleagues performed this study because standard practice is to recommend physiotherapy as first-line treatment, and to proceed to surgery only if that fails. Yet outcomes from midurethral-sling surgery and physiotherapy have never been directly compared.
Their study involved women aged 35-80 years whose stress urinary incontinence was classified as moderate or severe according to the Sandvik index. These subjects were randomly assigned to receive either initial surgery (230 women) or initial physiotherapy (230 women) at four university medical centers and 19 general hospitals over a 2-year period.
Both retropubic and transobturator midurethral-sling surgical approaches were allowed. Physiotherapy included an average of nine sessions delivered over 18 weeks, and could include biofeedback assistance or functional electrostimulation therapy.
The women were allowed to cross over to the other group if they were not satisfied with their assigned treatment, as "is consistent with usual clinical practice." The data were analyzed on an intention-to-treat basis. However, because approximately half of the physiotherapy group crossed over to surgery after a mean of 31 weeks, the investigators also performed a post hoc per-protocol analysis.
The primary outcome was subjective improvement in symptoms of stress urinary incontinence at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I) scale. In the intention-to-treat analysis, the rate of this outcome was 90.8% with immediate surgery, significantly higher than the 64.4% rate with immediate physiotherapy, Dr. Labrie and his associates reported (New Engl. J. Med. 2013;369:1124-33 [doi: 10.1056/NEJMoa1210627]).
The pattern was the same when outcomes were assessed objectively using a cough stress test.
Both study groups showed improvement over time in urogenital symptoms as measured by the Urogenital Distress Inventory (UDI) and in disease-specific quality of life as measured by the Incontinence Impact Questionnaire (IIQ). The improvements were significantly greater in the immediate-surgery group for incontinence and overactive bladder, "but with only moderate effect sizes," the authors said.
Similarly, improvements were significantly greater in the immediate-surgery group for subscores regarding patients’ mobility and embarrassment, "but again with only moderate effect sizes," the researchers said.
In the post hoc per-protocol analysis, they compared the 103 women who only had physiotherapy, the 99 who had physiotherapy but crossed over to surgery, and the 215 who only had surgery. At 1 year, improvement in the physiotherapy-only group was lower by approximately 62% than in the crossover group and by 59% in the surgery-only group.
Adverse events, which occurred only in women who underwent surgery, included 6 cases of bladder perforation, 10 cases of vaginal epithelial perforation, 6 reoperations for tape exposure, 1 reoperation to loosen a too-tight synthetic sling, 20 hematomas, 18 cases of new-onset urge urinary incontinence, and 3 cases of excessive blood loss.
This study may have been limited by selection bias, because "women with a preference for surgery may have been more likely to participate in the study, because they otherwise would have received initial physiotherapy according to Dutch guidelines," Dr. Labrie and his associates said.
The study was supported by the Netherlands Organization for Health Research and Development (ZonMW) and was performed "without the support or involvement of manufacturers of midurethral slings." Several coauthors reported financial ties to Ethicon, American Medical Systems, and AMS. The remainder of the authors reported no relevant financial conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: A total of 90.8% of women in the immediate-surgery group reported significant subjective improvement in stress urinary incontinence after 1 year, compared with only 64.4% of women in the immediate-physiotherapy group.
Data source: A national, multicenter, randomized clinical trial involving 460 women with moderate to severe stress urinary incontinence who underwent immediate midurethral-sling surgery or immediate physiotherapy and were followed for 1 year.
Disclosures: The study was supported by the Netherlands Organization for Health Research and Development (ZonMW), and was performed "without the support or involvement of manufacturers of midurethral slings." Several coauthors reported financial ties to Ethicon, American Medical Systems, and AMS. The remainder of the authors reported no relevant financial conflicts of interest.
Prophylactic beta-blockers and noncardiac surgery: It's complicated!
AMSTERDAM – Results of a new Danish national study suggest the effects of prophylactic beta-blocker therapy in patients with ischemic heart disease undergoing noncardiac surgery are considerably more heterogeneous than portrayed in current pro-prophylaxis practice guidelines or, at the opposite extreme, in a recent highly critical meta-analysis.
"This is an extraordinarily confusing area at the moment," Dr. Charlotte Andersson observed in presenting the Danish national registry findings at the annual congress of the European Society of Cardiology.
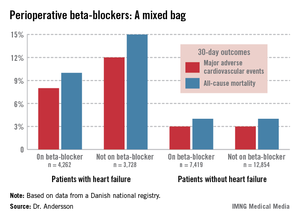
She reported on 28,263 adults with ischemic heart disease who underwent noncardiac surgery during 2004-2009. Hip or knee replacements were the most common operations, accounting for roughly one-third of the total. Patients were followed for 30 days postoperatively for the composite endpoint of acute myocardial infarction, ischemic stroke, or cardiovascular death, as well as for 30-day all-cause mortality.
In short, the effects of prophylactic beta-blocker therapy depended upon the type of background ischemic heart disease a surgical patient had.
"Our data suggest a beneficial effect of beta-blockers among patients with heart failure, perhaps a beneficial effect as well among patients with an MI within the previous 2 years, but no beneficial effect among patients with a more distant MI, and perhaps even harm associated with beta-blocker therapy among patients with neither heart failure nor a history of MI," according to Dr. Andersson of the University of Copenhagen.
The study population included 7,990 patients with heart failure, 53% of whom were on beta-blockers when they underwent noncardiac surgery. Those on beta-blockers fared significantly better in terms of the study endpoints (see graphic).
In contrast, 30-day outcomes in the 37% of patients without heart failure were identical regardless of whether or not they were on beta-blockers at surgery.
In a multivariate analysis, the use of beta-blockers in noncardiac surgery patients with heart failure was associated with a 22% reduction in major adverse cardiovascular events (MACEs) and an 18% reduction in all-cause mortality compared with no use of beta-blockers, both of which were statistically significant advantages. The analysis was adjusted for patient demographics, acute versus elective surgery, chronic obstructive pulmonary disease, diabetes, atrial fibrillation, peripheral artery disease, cancer, anemia, smoking, alcohol consumption, cerebrovascular disease, and American Society of Anesthesiologists score.
Among the 1,664 patients with an MI within the past 2 years, being on a beta-blocker at the time of surgery was associated with an adjusted highly significant 46% reduction in MACE and a 20% decrease in all-cause mortality, compared with no use of beta-blockers.
For the 1,679 patients with an MI 2-5 years prior to surgery, being on a beta-blocker was associated with a 29% reduction in the risk of MACE and a 26% reduction in 30-day all-cause mortality.
Among the 5,018 patients with an MI more than 5 years earlier, the use of beta-blockers at surgery was associated with a 35% greater risk of MACE than in nonusers of beta-blockers as well as a 33% increase in all-cause mortality. These differences in adverse outcomes rates barely missed achieving statistical significance.
Perhaps the most striking study finding was that patients with no prior MI or heart failure who were on a beta-blocker at the time of noncardiac surgery had a 44% increased risk of 30-day MACE and a 30% higher all-cause mortality, compared with those not on a beta-blocker, with both differences being significant.
Session cochair Dr. Elmir Omerovic thanked Dr. Andersson for a presentation that "really adds important new information" and asked whether she had been surprised by the findings.
"Yes, I have to say I was surprised by the increased risk in patients without prior MI or heart failure, because the ESC [European Society of Cardiology] guidelines state as a class I recommendation that all patients with ischemic heart disease undergoing noncardiac surgery should be on a beta-blocker. Perhaps we should reevaluate beta-blockers in noncardiac surgery," Dr. Andersson replied.
Current American College of Cardiology/American Heart Association guidelines also endorse perioperative beta-blockade in patients with coronary artery disease undergoing vascular or intermediate-risk noncardiac surgery.
She noted that in drawing up the current guidelines, the ESC and ACC/AHA committees relied heavily on strongly positive randomized clinical trials whose validity has recently been called into question in a major research scandal. Indeed, the lead investigator in those studies, Dr. Don Poldermans – who also happened to be chairperson of the ESC guidelines-writing task force – has been dismissed from the faculty at Erasmus University in Rotterdam.
Dr. Omerovic, of Sahlgrenska University, Gothenburg, Sweden, asked for Dr. Andersson’s thoughts regarding a new meta-analysis by investigators at Imperial College London which excluded the suspect Dutch clinical trials. The investigators concluded that initiation of perioperative beta-blocker therapy was associated with a 27% increase in 30-day all-cause mortality, a 27% reduction in nonfatal MI, a 73% increase in stroke, and a 51% increase in hypotension.
"Patient safety being paramount, guidelines for perioperative beta-blocker initiation should be retracted without further delay," the meta-analysts argued (Heart 2013 July 31 [doi: 10.1136/heartjnl-2013-304262]).
"I read that meta-analysis with great interest," Dr. Andersson said. "I think there definitely is a heterogeneity in the effects of perioperative beta-blockers, and it depends on your baseline risk. Most of the studies in the meta-analysis included many patients at lower risk."
Dr. Andersson’s study was funded by the Danish Medical Research Foundation. She reported having no financial conflicts of interest.
Dr. Jun Chiong, FCCP, comments: There are similar studies published regarding preoperative beta-blockers. Most studies are from large databases and not randomized. The results are varied. Important factors such as severity of comorbid conditions prior to surgery (eg, uncontrolled diabetic, noncompliance), amount of blood loss, and surgical technique (not just the organ involved) are often not factored in. I applaud the authors for reporting a significant finding from such a large database. I hope this will encourage investigators to initiate a large, well-controlled, randomized study.
Dr. Jun Chiong, FCCP, comments: There are similar studies published regarding preoperative beta-blockers. Most studies are from large databases and not randomized. The results are varied. Important factors such as severity of comorbid conditions prior to surgery (eg, uncontrolled diabetic, noncompliance), amount of blood loss, and surgical technique (not just the organ involved) are often not factored in. I applaud the authors for reporting a significant finding from such a large database. I hope this will encourage investigators to initiate a large, well-controlled, randomized study.
Dr. Jun Chiong, FCCP, comments: There are similar studies published regarding preoperative beta-blockers. Most studies are from large databases and not randomized. The results are varied. Important factors such as severity of comorbid conditions prior to surgery (eg, uncontrolled diabetic, noncompliance), amount of blood loss, and surgical technique (not just the organ involved) are often not factored in. I applaud the authors for reporting a significant finding from such a large database. I hope this will encourage investigators to initiate a large, well-controlled, randomized study.
AMSTERDAM – Results of a new Danish national study suggest the effects of prophylactic beta-blocker therapy in patients with ischemic heart disease undergoing noncardiac surgery are considerably more heterogeneous than portrayed in current pro-prophylaxis practice guidelines or, at the opposite extreme, in a recent highly critical meta-analysis.
"This is an extraordinarily confusing area at the moment," Dr. Charlotte Andersson observed in presenting the Danish national registry findings at the annual congress of the European Society of Cardiology.
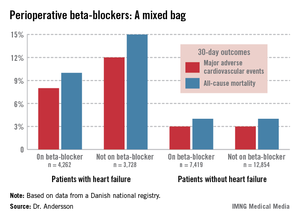
She reported on 28,263 adults with ischemic heart disease who underwent noncardiac surgery during 2004-2009. Hip or knee replacements were the most common operations, accounting for roughly one-third of the total. Patients were followed for 30 days postoperatively for the composite endpoint of acute myocardial infarction, ischemic stroke, or cardiovascular death, as well as for 30-day all-cause mortality.
In short, the effects of prophylactic beta-blocker therapy depended upon the type of background ischemic heart disease a surgical patient had.
"Our data suggest a beneficial effect of beta-blockers among patients with heart failure, perhaps a beneficial effect as well among patients with an MI within the previous 2 years, but no beneficial effect among patients with a more distant MI, and perhaps even harm associated with beta-blocker therapy among patients with neither heart failure nor a history of MI," according to Dr. Andersson of the University of Copenhagen.
The study population included 7,990 patients with heart failure, 53% of whom were on beta-blockers when they underwent noncardiac surgery. Those on beta-blockers fared significantly better in terms of the study endpoints (see graphic).
In contrast, 30-day outcomes in the 37% of patients without heart failure were identical regardless of whether or not they were on beta-blockers at surgery.
In a multivariate analysis, the use of beta-blockers in noncardiac surgery patients with heart failure was associated with a 22% reduction in major adverse cardiovascular events (MACEs) and an 18% reduction in all-cause mortality compared with no use of beta-blockers, both of which were statistically significant advantages. The analysis was adjusted for patient demographics, acute versus elective surgery, chronic obstructive pulmonary disease, diabetes, atrial fibrillation, peripheral artery disease, cancer, anemia, smoking, alcohol consumption, cerebrovascular disease, and American Society of Anesthesiologists score.
Among the 1,664 patients with an MI within the past 2 years, being on a beta-blocker at the time of surgery was associated with an adjusted highly significant 46% reduction in MACE and a 20% decrease in all-cause mortality, compared with no use of beta-blockers.
For the 1,679 patients with an MI 2-5 years prior to surgery, being on a beta-blocker was associated with a 29% reduction in the risk of MACE and a 26% reduction in 30-day all-cause mortality.
Among the 5,018 patients with an MI more than 5 years earlier, the use of beta-blockers at surgery was associated with a 35% greater risk of MACE than in nonusers of beta-blockers as well as a 33% increase in all-cause mortality. These differences in adverse outcomes rates barely missed achieving statistical significance.
Perhaps the most striking study finding was that patients with no prior MI or heart failure who were on a beta-blocker at the time of noncardiac surgery had a 44% increased risk of 30-day MACE and a 30% higher all-cause mortality, compared with those not on a beta-blocker, with both differences being significant.
Session cochair Dr. Elmir Omerovic thanked Dr. Andersson for a presentation that "really adds important new information" and asked whether she had been surprised by the findings.
"Yes, I have to say I was surprised by the increased risk in patients without prior MI or heart failure, because the ESC [European Society of Cardiology] guidelines state as a class I recommendation that all patients with ischemic heart disease undergoing noncardiac surgery should be on a beta-blocker. Perhaps we should reevaluate beta-blockers in noncardiac surgery," Dr. Andersson replied.
Current American College of Cardiology/American Heart Association guidelines also endorse perioperative beta-blockade in patients with coronary artery disease undergoing vascular or intermediate-risk noncardiac surgery.
She noted that in drawing up the current guidelines, the ESC and ACC/AHA committees relied heavily on strongly positive randomized clinical trials whose validity has recently been called into question in a major research scandal. Indeed, the lead investigator in those studies, Dr. Don Poldermans – who also happened to be chairperson of the ESC guidelines-writing task force – has been dismissed from the faculty at Erasmus University in Rotterdam.
Dr. Omerovic, of Sahlgrenska University, Gothenburg, Sweden, asked for Dr. Andersson’s thoughts regarding a new meta-analysis by investigators at Imperial College London which excluded the suspect Dutch clinical trials. The investigators concluded that initiation of perioperative beta-blocker therapy was associated with a 27% increase in 30-day all-cause mortality, a 27% reduction in nonfatal MI, a 73% increase in stroke, and a 51% increase in hypotension.
"Patient safety being paramount, guidelines for perioperative beta-blocker initiation should be retracted without further delay," the meta-analysts argued (Heart 2013 July 31 [doi: 10.1136/heartjnl-2013-304262]).
"I read that meta-analysis with great interest," Dr. Andersson said. "I think there definitely is a heterogeneity in the effects of perioperative beta-blockers, and it depends on your baseline risk. Most of the studies in the meta-analysis included many patients at lower risk."
Dr. Andersson’s study was funded by the Danish Medical Research Foundation. She reported having no financial conflicts of interest.
AMSTERDAM – Results of a new Danish national study suggest the effects of prophylactic beta-blocker therapy in patients with ischemic heart disease undergoing noncardiac surgery are considerably more heterogeneous than portrayed in current pro-prophylaxis practice guidelines or, at the opposite extreme, in a recent highly critical meta-analysis.
"This is an extraordinarily confusing area at the moment," Dr. Charlotte Andersson observed in presenting the Danish national registry findings at the annual congress of the European Society of Cardiology.
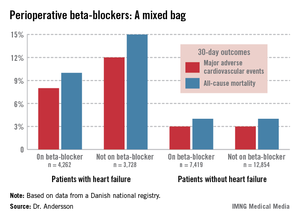
She reported on 28,263 adults with ischemic heart disease who underwent noncardiac surgery during 2004-2009. Hip or knee replacements were the most common operations, accounting for roughly one-third of the total. Patients were followed for 30 days postoperatively for the composite endpoint of acute myocardial infarction, ischemic stroke, or cardiovascular death, as well as for 30-day all-cause mortality.
In short, the effects of prophylactic beta-blocker therapy depended upon the type of background ischemic heart disease a surgical patient had.
"Our data suggest a beneficial effect of beta-blockers among patients with heart failure, perhaps a beneficial effect as well among patients with an MI within the previous 2 years, but no beneficial effect among patients with a more distant MI, and perhaps even harm associated with beta-blocker therapy among patients with neither heart failure nor a history of MI," according to Dr. Andersson of the University of Copenhagen.
The study population included 7,990 patients with heart failure, 53% of whom were on beta-blockers when they underwent noncardiac surgery. Those on beta-blockers fared significantly better in terms of the study endpoints (see graphic).
In contrast, 30-day outcomes in the 37% of patients without heart failure were identical regardless of whether or not they were on beta-blockers at surgery.
In a multivariate analysis, the use of beta-blockers in noncardiac surgery patients with heart failure was associated with a 22% reduction in major adverse cardiovascular events (MACEs) and an 18% reduction in all-cause mortality compared with no use of beta-blockers, both of which were statistically significant advantages. The analysis was adjusted for patient demographics, acute versus elective surgery, chronic obstructive pulmonary disease, diabetes, atrial fibrillation, peripheral artery disease, cancer, anemia, smoking, alcohol consumption, cerebrovascular disease, and American Society of Anesthesiologists score.
Among the 1,664 patients with an MI within the past 2 years, being on a beta-blocker at the time of surgery was associated with an adjusted highly significant 46% reduction in MACE and a 20% decrease in all-cause mortality, compared with no use of beta-blockers.
For the 1,679 patients with an MI 2-5 years prior to surgery, being on a beta-blocker was associated with a 29% reduction in the risk of MACE and a 26% reduction in 30-day all-cause mortality.
Among the 5,018 patients with an MI more than 5 years earlier, the use of beta-blockers at surgery was associated with a 35% greater risk of MACE than in nonusers of beta-blockers as well as a 33% increase in all-cause mortality. These differences in adverse outcomes rates barely missed achieving statistical significance.
Perhaps the most striking study finding was that patients with no prior MI or heart failure who were on a beta-blocker at the time of noncardiac surgery had a 44% increased risk of 30-day MACE and a 30% higher all-cause mortality, compared with those not on a beta-blocker, with both differences being significant.
Session cochair Dr. Elmir Omerovic thanked Dr. Andersson for a presentation that "really adds important new information" and asked whether she had been surprised by the findings.
"Yes, I have to say I was surprised by the increased risk in patients without prior MI or heart failure, because the ESC [European Society of Cardiology] guidelines state as a class I recommendation that all patients with ischemic heart disease undergoing noncardiac surgery should be on a beta-blocker. Perhaps we should reevaluate beta-blockers in noncardiac surgery," Dr. Andersson replied.
Current American College of Cardiology/American Heart Association guidelines also endorse perioperative beta-blockade in patients with coronary artery disease undergoing vascular or intermediate-risk noncardiac surgery.
She noted that in drawing up the current guidelines, the ESC and ACC/AHA committees relied heavily on strongly positive randomized clinical trials whose validity has recently been called into question in a major research scandal. Indeed, the lead investigator in those studies, Dr. Don Poldermans – who also happened to be chairperson of the ESC guidelines-writing task force – has been dismissed from the faculty at Erasmus University in Rotterdam.
Dr. Omerovic, of Sahlgrenska University, Gothenburg, Sweden, asked for Dr. Andersson’s thoughts regarding a new meta-analysis by investigators at Imperial College London which excluded the suspect Dutch clinical trials. The investigators concluded that initiation of perioperative beta-blocker therapy was associated with a 27% increase in 30-day all-cause mortality, a 27% reduction in nonfatal MI, a 73% increase in stroke, and a 51% increase in hypotension.
"Patient safety being paramount, guidelines for perioperative beta-blocker initiation should be retracted without further delay," the meta-analysts argued (Heart 2013 July 31 [doi: 10.1136/heartjnl-2013-304262]).
"I read that meta-analysis with great interest," Dr. Andersson said. "I think there definitely is a heterogeneity in the effects of perioperative beta-blockers, and it depends on your baseline risk. Most of the studies in the meta-analysis included many patients at lower risk."
Dr. Andersson’s study was funded by the Danish Medical Research Foundation. She reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2013
Major finding: Patients with heart failure who were on beta-blocker therapy at the time of noncardiac surgery had a 22% reduction in 30-day major adverse cardiovascular events, compared with those not on a beta-blocker perioperatively. In stark contrast, patients with ischemic heart disease but no history of heart failure or MI had a 44% greater risk of such events if they were on a perioperative beta-blocker.
Data source: This was a Danish national registry study that included more than 28,000 patients with ischemic heart disease who underwent noncardiac surgery.
Disclosures: Dr. Andersson’s study was funded by the Danish Medical Research Foundation. She reported having no financial conflicts of interest.
Gun deaths rise as gun ownership climbs
More guns means more gun deaths, according to a study comparing gun ownership and fatalities among 27 developed nations. The report was published online Sept. 18 in the American Journal of Medicine.
There is "a significant, positive correlation between guns per capita per country and the rate of firearm-related deaths" (r = 0.80; P less than .0001). On linear regression, gun ownership was a strong and independent predictor of firearm mortality (P less than .0001), wrote Dr. Sripal Bangalore of New York University and Dr. Franz Messerli of Columbia University, both in New York.
"Although correlation is not synonymous with causation, it seems conceivable that abundant gun availability facilitates firearm-related deaths ... the [finding] debunks the widely quoted hypothesis ... that countries with higher gun ownership are safer than those with low gun ownership," they said.
The team didn’t find a significant correlation between guns per capita and national crime rates, which argues "against the notion of more guns translating into less crime," they said (Am. J. Med. 2013 Sept 18).
Mental illness correlated weakly with firearm deaths (r = 0.52, P = .05), and did not correlate with national crime rates.
"In having almost as many guns as it has people, prevalence of private gun ownership was the highest in the [United States]" at 88.8 guns/100 people; the United States also had the highest firearm death rate at 10.2/100,000. In contrast, Japan, with the lowest gun ownership rate of 0.6/100 people, had the lowest rate of firearm-related deaths at 0.06/100,000, the researchers wrote.
In addition to the United States and Japan, the study included Canada, Australia, and most European nations, among others. Data on gun ownership was culled from the 2007 Small Arms Survey; national firearm-related death figures came from the World Health Organization and other sources; and crime rates were pulled from the United Nations Surveys of Crime Trends. National rates of major depressive disorder – also from the World Health Organization – were used as proxies for a country’s mental illness burden.
"Others have suggested that violence is often due to the perpetrator’s mental illness and therefore, lack of treatment for mental illness may be more of a pressing problem than mere availability of guns. [Although] there is little question that the combination of mental illness and easy access to guns may prove to be synergistic in their lethality ... the predictive power of mental illness burden was of borderline significance," the authors noted.
The study was an attempt to inject evidence into the gun control debate. Although "the association between gun ownership, mental illness, and firearm-related deaths has been hotly debated ... many of [the] arguments from both sides are based on little or no evidence," they said.
The study was published early following the Sept. 16 shootings at the Washington (D.C.) Navy Yard. Several doctors’ groups have repeatedly called for gun control, including the American Academy of Family Physicians, American Academy of Pediatrics, and American College of Emergency Physicians.
The investigators have no financial disclosures. Their project received no external funding.
It’s difficult to draw any real conclusions from this study; there’s not enough granularity to understand if these correlations have any true significance in terms of actual practice. Given its scope, the study is a necessarily superficial treatment of what is otherwise a very complex subject.
For instance, the crime rate analysis does not distinguish between violent and other types of crime, and the paper does not distinguish between suicide and homicide in its death rates. Although only a weak association was found between mental illness and gun deaths, it’s well documented that gun access increases the likelihood that depressed patients will use a firearm in suicide.
The paper also doesn’t take into account social scenarios that impact gun violence, such as the status of the economy in the different countries. For these and other reasons, the paper is methodologically flawed.
The correlation between higher per capita gun ownership and the incidence of firearm-related death isn’t surprising. We have known for a long time that higher access to guns makes them more likely to be used in a variety of situations.
Dr. John Milne is chairman of emergency medicine at the Swedish Medical Center in Issaquah, Wash. He reported no financial conflicts of interest.
It’s difficult to draw any real conclusions from this study; there’s not enough granularity to understand if these correlations have any true significance in terms of actual practice. Given its scope, the study is a necessarily superficial treatment of what is otherwise a very complex subject.
For instance, the crime rate analysis does not distinguish between violent and other types of crime, and the paper does not distinguish between suicide and homicide in its death rates. Although only a weak association was found between mental illness and gun deaths, it’s well documented that gun access increases the likelihood that depressed patients will use a firearm in suicide.
The paper also doesn’t take into account social scenarios that impact gun violence, such as the status of the economy in the different countries. For these and other reasons, the paper is methodologically flawed.
The correlation between higher per capita gun ownership and the incidence of firearm-related death isn’t surprising. We have known for a long time that higher access to guns makes them more likely to be used in a variety of situations.
Dr. John Milne is chairman of emergency medicine at the Swedish Medical Center in Issaquah, Wash. He reported no financial conflicts of interest.
It’s difficult to draw any real conclusions from this study; there’s not enough granularity to understand if these correlations have any true significance in terms of actual practice. Given its scope, the study is a necessarily superficial treatment of what is otherwise a very complex subject.
For instance, the crime rate analysis does not distinguish between violent and other types of crime, and the paper does not distinguish between suicide and homicide in its death rates. Although only a weak association was found between mental illness and gun deaths, it’s well documented that gun access increases the likelihood that depressed patients will use a firearm in suicide.
The paper also doesn’t take into account social scenarios that impact gun violence, such as the status of the economy in the different countries. For these and other reasons, the paper is methodologically flawed.
The correlation between higher per capita gun ownership and the incidence of firearm-related death isn’t surprising. We have known for a long time that higher access to guns makes them more likely to be used in a variety of situations.
Dr. John Milne is chairman of emergency medicine at the Swedish Medical Center in Issaquah, Wash. He reported no financial conflicts of interest.
More guns means more gun deaths, according to a study comparing gun ownership and fatalities among 27 developed nations. The report was published online Sept. 18 in the American Journal of Medicine.
There is "a significant, positive correlation between guns per capita per country and the rate of firearm-related deaths" (r = 0.80; P less than .0001). On linear regression, gun ownership was a strong and independent predictor of firearm mortality (P less than .0001), wrote Dr. Sripal Bangalore of New York University and Dr. Franz Messerli of Columbia University, both in New York.
"Although correlation is not synonymous with causation, it seems conceivable that abundant gun availability facilitates firearm-related deaths ... the [finding] debunks the widely quoted hypothesis ... that countries with higher gun ownership are safer than those with low gun ownership," they said.
The team didn’t find a significant correlation between guns per capita and national crime rates, which argues "against the notion of more guns translating into less crime," they said (Am. J. Med. 2013 Sept 18).
Mental illness correlated weakly with firearm deaths (r = 0.52, P = .05), and did not correlate with national crime rates.
"In having almost as many guns as it has people, prevalence of private gun ownership was the highest in the [United States]" at 88.8 guns/100 people; the United States also had the highest firearm death rate at 10.2/100,000. In contrast, Japan, with the lowest gun ownership rate of 0.6/100 people, had the lowest rate of firearm-related deaths at 0.06/100,000, the researchers wrote.
In addition to the United States and Japan, the study included Canada, Australia, and most European nations, among others. Data on gun ownership was culled from the 2007 Small Arms Survey; national firearm-related death figures came from the World Health Organization and other sources; and crime rates were pulled from the United Nations Surveys of Crime Trends. National rates of major depressive disorder – also from the World Health Organization – were used as proxies for a country’s mental illness burden.
"Others have suggested that violence is often due to the perpetrator’s mental illness and therefore, lack of treatment for mental illness may be more of a pressing problem than mere availability of guns. [Although] there is little question that the combination of mental illness and easy access to guns may prove to be synergistic in their lethality ... the predictive power of mental illness burden was of borderline significance," the authors noted.
The study was an attempt to inject evidence into the gun control debate. Although "the association between gun ownership, mental illness, and firearm-related deaths has been hotly debated ... many of [the] arguments from both sides are based on little or no evidence," they said.
The study was published early following the Sept. 16 shootings at the Washington (D.C.) Navy Yard. Several doctors’ groups have repeatedly called for gun control, including the American Academy of Family Physicians, American Academy of Pediatrics, and American College of Emergency Physicians.
The investigators have no financial disclosures. Their project received no external funding.
More guns means more gun deaths, according to a study comparing gun ownership and fatalities among 27 developed nations. The report was published online Sept. 18 in the American Journal of Medicine.
There is "a significant, positive correlation between guns per capita per country and the rate of firearm-related deaths" (r = 0.80; P less than .0001). On linear regression, gun ownership was a strong and independent predictor of firearm mortality (P less than .0001), wrote Dr. Sripal Bangalore of New York University and Dr. Franz Messerli of Columbia University, both in New York.
"Although correlation is not synonymous with causation, it seems conceivable that abundant gun availability facilitates firearm-related deaths ... the [finding] debunks the widely quoted hypothesis ... that countries with higher gun ownership are safer than those with low gun ownership," they said.
The team didn’t find a significant correlation between guns per capita and national crime rates, which argues "against the notion of more guns translating into less crime," they said (Am. J. Med. 2013 Sept 18).
Mental illness correlated weakly with firearm deaths (r = 0.52, P = .05), and did not correlate with national crime rates.
"In having almost as many guns as it has people, prevalence of private gun ownership was the highest in the [United States]" at 88.8 guns/100 people; the United States also had the highest firearm death rate at 10.2/100,000. In contrast, Japan, with the lowest gun ownership rate of 0.6/100 people, had the lowest rate of firearm-related deaths at 0.06/100,000, the researchers wrote.
In addition to the United States and Japan, the study included Canada, Australia, and most European nations, among others. Data on gun ownership was culled from the 2007 Small Arms Survey; national firearm-related death figures came from the World Health Organization and other sources; and crime rates were pulled from the United Nations Surveys of Crime Trends. National rates of major depressive disorder – also from the World Health Organization – were used as proxies for a country’s mental illness burden.
"Others have suggested that violence is often due to the perpetrator’s mental illness and therefore, lack of treatment for mental illness may be more of a pressing problem than mere availability of guns. [Although] there is little question that the combination of mental illness and easy access to guns may prove to be synergistic in their lethality ... the predictive power of mental illness burden was of borderline significance," the authors noted.
The study was an attempt to inject evidence into the gun control debate. Although "the association between gun ownership, mental illness, and firearm-related deaths has been hotly debated ... many of [the] arguments from both sides are based on little or no evidence," they said.
The study was published early following the Sept. 16 shootings at the Washington (D.C.) Navy Yard. Several doctors’ groups have repeatedly called for gun control, including the American Academy of Family Physicians, American Academy of Pediatrics, and American College of Emergency Physicians.
The investigators have no financial disclosures. Their project received no external funding.
FROM THE AMERICAN JOURNAL OF MEDICINE
Major finding: There is a significant, positive correlation between a county’s per capita gun ownership rate and its rate of firearm-related deaths (r = 0.80, P less than.001).
Data source: Comparison of gun ownership, fatalities, and other measures among 27 developed nations.
Disclosures: The authors have no financial disclosures; their project received no external funding.
Orthopaedic surgeons’ ‘Choosing Wisely’ list centers on osteoarthritis treatments
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.