User login
Official Newspaper of the American College of Surgeons
Blood test charges vary widely among California hospitals
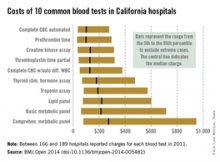
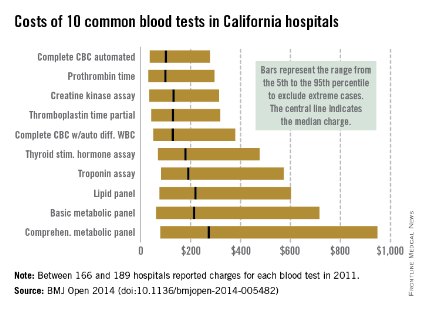
Charges for 10 common blood tests showed wide variation among hospitals in California, with the cost of one test ranging from $10 to more than $10,000, Dr. Renee Y. Hsia and her associates reported in BMJ Open.
In 2011, minimum charges for the examined blood tests ranged from $10 to $44. Maximum charges, with the exception of a creatine kinase assay at $628, were all more than $6,000. The highest charge for a lipid panel was $10,169 – more than a thousand times higher than the low of $10, according to Dr. Hsia and her associates (BMJ Open 2014 [doi: 10.1136/bmjopen-2014-005482]).
Large price differences remained after extreme cases were excluded (see graph). The test with the smallest variation between the 5th and 95th percentiles, an automated complete blood count, had a range of $37 to $278 (median, $100). A complete metabolic panel had the largest variation among the 10 blood tests, costing anywhere from $79 to $948 (median, $273).
Teaching hospitals charged significantly less than other hospitals for 7 of the 10 tests, and government hospitals charged less for 5 of the 10, but "it is notable how few characteristics were significant predictors of the charges patients faced. ... A hospital’s case mix and labor cost did not affect charges, nor did the competitiveness of the market or the percentage of uninsured people in the county," wrote Dr. Hsia of the University of California, San Francisco, and her associates.
The study used data from the California Office of Statewide Health Planning and Development. Of the 307 hospitals that reported charges in 2011, between 166 and 189 reported charges for each of the 10 tests included in the study.
Charges for 10 common blood tests showed wide variation among hospitals in California, with the cost of one test ranging from $10 to more than $10,000, Dr. Renee Y. Hsia and her associates reported in BMJ Open.
In 2011, minimum charges for the examined blood tests ranged from $10 to $44. Maximum charges, with the exception of a creatine kinase assay at $628, were all more than $6,000. The highest charge for a lipid panel was $10,169 – more than a thousand times higher than the low of $10, according to Dr. Hsia and her associates (BMJ Open 2014 [doi: 10.1136/bmjopen-2014-005482]).
Large price differences remained after extreme cases were excluded (see graph). The test with the smallest variation between the 5th and 95th percentiles, an automated complete blood count, had a range of $37 to $278 (median, $100). A complete metabolic panel had the largest variation among the 10 blood tests, costing anywhere from $79 to $948 (median, $273).
Teaching hospitals charged significantly less than other hospitals for 7 of the 10 tests, and government hospitals charged less for 5 of the 10, but "it is notable how few characteristics were significant predictors of the charges patients faced. ... A hospital’s case mix and labor cost did not affect charges, nor did the competitiveness of the market or the percentage of uninsured people in the county," wrote Dr. Hsia of the University of California, San Francisco, and her associates.
The study used data from the California Office of Statewide Health Planning and Development. Of the 307 hospitals that reported charges in 2011, between 166 and 189 reported charges for each of the 10 tests included in the study.
Charges for 10 common blood tests showed wide variation among hospitals in California, with the cost of one test ranging from $10 to more than $10,000, Dr. Renee Y. Hsia and her associates reported in BMJ Open.
In 2011, minimum charges for the examined blood tests ranged from $10 to $44. Maximum charges, with the exception of a creatine kinase assay at $628, were all more than $6,000. The highest charge for a lipid panel was $10,169 – more than a thousand times higher than the low of $10, according to Dr. Hsia and her associates (BMJ Open 2014 [doi: 10.1136/bmjopen-2014-005482]).
Large price differences remained after extreme cases were excluded (see graph). The test with the smallest variation between the 5th and 95th percentiles, an automated complete blood count, had a range of $37 to $278 (median, $100). A complete metabolic panel had the largest variation among the 10 blood tests, costing anywhere from $79 to $948 (median, $273).
Teaching hospitals charged significantly less than other hospitals for 7 of the 10 tests, and government hospitals charged less for 5 of the 10, but "it is notable how few characteristics were significant predictors of the charges patients faced. ... A hospital’s case mix and labor cost did not affect charges, nor did the competitiveness of the market or the percentage of uninsured people in the county," wrote Dr. Hsia of the University of California, San Francisco, and her associates.
The study used data from the California Office of Statewide Health Planning and Development. Of the 307 hospitals that reported charges in 2011, between 166 and 189 reported charges for each of the 10 tests included in the study.
FROM BMJ OPEN
Vagal nerve blockade effects on morbid obesity warrant further study
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
The findings suggest that vagal nerve blockade has little to offer when compared with other treatments for morbid obesity, according to Dr. David E. Arterburn and Dr. David P. Fisher.
The treatment does not appear to be much more effective than an intensive lifestyle program, which in one study was shown to be associated with an 8.6% weight loss. Also, other procedures – including adjustable gastric banding, Roux-en-Y gastric bypass, and vertical sleeve gastrectomy – are associated with excess weight loss of between 50% and 68%, and thus are "clearly more effective for initial weight loss than vagal nerve blockade," Dr. Arterburn and Dr. Fisher wrote in an editorial (JAMA 2014;312:898-9).
The clinically important 8.6% rate of serious adverse events associated with intra-abdominal surgery and vagal nerve blockade in the study is also of concern, as are costs, which were not addressed by the authors, they noted.
"Although vagal nerve blockade therapy is an innovative approach, it does not appear to be a sustained, effective treatment for severe obesity," Dr. Arterburn and Dr. Fisher concluded.
Dr. Arterburn is with Group Health Research Institute, Seattle. He reported receiving institutional grants from the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Department of Veterans Affairs, and the Informed Medical Decisions Foundation, and receiving payment for travel expenses from the Informed Medical Decisions Foundation. Dr. Fisher is with the Permanente Medical Group, Kaiser Permanente Northern California, Bariatric Surgery Center, Richmond, Calif. He reported receiving institutional grants from the National Institutes of Health.
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
Intra-abdominal vagal nerve blockade to treat morbid obesity didn’t meet prespecified efficacy objectives in the randomized, double-blind ReCharge study, but treated patients did experience significantly greater weight loss than did those who underwent a sham procedure.
Mean excess weight loss was 24.4% (9.2% of initial body weight loss) in 162 patients who had a body mass index of 40-45 kg/m2 or 35-40 kg/m2 plus one or more obesity-related conditions, who underwent vagal nerve block therapy, compared with 15.9% (6% of initial body weight loss) in 77 patients in the sham group, for a mean between-group difference of 8.5 percentage points.
The difference was statistically significant, but it was less than the prespecified 10-point superiority margin, Dr. Sayeed Ikramuddin of the University of Minnesota, Minneapolis, and colleagues reported online Sept. 2 in JAMA.
At 12 months, 20% or more excess weight loss was achieved by 52% of patients in the vagal nerve block group, compared with 32% of patients in the sham procedure group. A total of 25% or more excess weight loss was achieved by 38% and 23% of patients in the groups, respectively, the investigators said (JAMA 2014;312:915-22).
Patients in the treatment group experienced more heartburn and dyspepsia, abdominal and other nonspecific pain, dysphagia, nausea, and eructation or belching than those in the control group. But these side effects were generally mild or moderate in severity. Serious adverse events associated with vagal nerve blockade occurred in 3.7% of treatment group patients, which was well below the 15% upper threshold for safety in the trial.
Additional study is needed to compare vagal nerve block with other obesity treatments, and to assess long-term durability and safety of the procedure, the investigators concluded.
This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
FROM JAMA
Major finding: At 12 months, 20% or more excess weight loss was achieved by 52% and 32% of patients in the treatment and control groups, respectively.
Data source: The randomized, double-blind ReCharge Study involving 239 patients.
Disclosures: This study was supported by EnteroMedics, which makes the vagal nerve blockade device used in the study. Dr. Ikramudden reported serving on the advisory board for Novo Nordisk and Medica, serving as a consultant for Metamodix and on an expert panel for OptumHealth, and receiving grant support from USGI Medical, ReShape Medical, and Covidien.
Sleeve gastrectomy replacing other bariatric surgery
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
Sleeve gastrectomy appears to be replacing other types of bariatric surgery in Michigan, even among subgroups of patients in whom its use is controversial, according to a Research Letter to the Editor published in the Sept. 3 issue of JAMA.
To examine time trends in the use of various bariatric procedures, investigators reviewed the medical records of 43,732 adults who had bariatric surgery and were enrolled in a statewide database between June 2006 and December 2013. They found that the relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, which represents an increase of 61%, said Dr. Bradley N. Reames of the department of surgery and the Center for Healthcare Outcomes and Policy, University of Michigan, Ann Arbor, and his associates.
At the same time, the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%, they said (JAMA 2014;312:959-61).
"Moreover, despite controversy regarding the optimal procedure for patients with gastroesophageal reflux disease and type 2 diabetes, sleeve gastrectomy has become the predominant procedure in both groups," Dr. Reames and his associates said.
The long-term outcomes after sleeve gastrectomy are not yet clear, so this trend "may reflect the favorable perioperative safety profile and emerging evidence of successful weight loss at 2-3 years after" the procedure, they added.
Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
FROM JAMA
Major finding: The relative use of sleeve gastrectomy rose from 6.0% of all procedures in 2008 to 67.3% 5 years later, while the use of Roux-en-Y gastric bypass dropped from 58.0% to 27.4% of all procedures, and the use of laparoscopic adjustable gastric banding decreased from 34.5% to 4.6%.
Data Source: An analysis of data regarding 43,732 adults who had bariatric surgery and were registered in a statewide database in Michigan between 2006 and 2013.
Disclosures: Dr. Reames’s work is supported by the National Cancer Institute. He and his associates reported no relevant financial conflicts of interest.
No mortality benefit from bilateral mastectomy, vs. breast-conserving surgery with radiation
The use of bilateral mastectomy has increased significantly in California, but the results from an observational cohort study show it achieves similar mortality reductions to breast-conserving surgery plus radiation, while unilateral mastectomy is associated with higher mortality.
In an analysis of data from nearly 190,000 patients in the population-based California Cancer Registry, no significant differences were found in all-cause mortality between patients who underwent bilateral mastectomy and those who had breast-conserving surgery with radiation (HR, 1.02 [95%CI, 0.94-1.11]); however, unilateral mastectomy was linked to 35% higher all-cause mortality than was breast-conserving surgery with radiation (HR, 1.35 [95% CI, 1.32-1.39]).
Dr. Allison W. Kurian of Stanford (Calif.)University and colleagues also found the rate of bilateral mastectomy had increased 14.3% each year, from 2% of all patients in 1998 to 12.3% in 2011, with it more commonly used among non-Hispanic white women, those with private insurance, and those who received care at a National Cancer Institute–designated cancer center, according to a paper published Sept. 2 in JAMA [doi:10.1001/jama.2014.10707].
"In a time of increasing concern over treatment, the risk-benefit ratio of bilateral mastectomy warrants careful consideration and raises the larger question of how physicians and society should respond to a patient’s preference for a morbid, costly intervention of dubious effectiveness," the authors wrote.
In an accompanying editorial, Dr. Lisa A. Newman of the comprehensive cancer center, University of Michigan, Ann Arbor, said the findings refute patient assumptions that bilateral mastectomy represents their best chance for a cure, and for eliminating the perceived cancer threat to the unaffected breast, and advocated a more calm and considered approach to treatment decision making (JAMA 2014 Sept. 2 [doi:10.1001/jama.2014.11308]).
"Physicians should not permit excessive treatment delays to compromise outcomes, but the initial few weeks surrounding the diagnosis are more effectively utilized by time invested in patient education and procedures that contribute to comprehensive treatment planning as opposed to hastily coordinating impulsive, irreversible surgical plans," Dr. Newman wrote.
The study was supported by the Jan Weimer Junior Faculty Chair in Breast Oncology, the Suzanne Pride Bryan Fund for Breast Cancer Research at Stanford Cancer Institute, and the National Cancer Institute. Two authors reported grants from Genentech for other work, but there were no other conflicts of interest disclosed.
The use of bilateral mastectomy has increased significantly in California, but the results from an observational cohort study show it achieves similar mortality reductions to breast-conserving surgery plus radiation, while unilateral mastectomy is associated with higher mortality.
In an analysis of data from nearly 190,000 patients in the population-based California Cancer Registry, no significant differences were found in all-cause mortality between patients who underwent bilateral mastectomy and those who had breast-conserving surgery with radiation (HR, 1.02 [95%CI, 0.94-1.11]); however, unilateral mastectomy was linked to 35% higher all-cause mortality than was breast-conserving surgery with radiation (HR, 1.35 [95% CI, 1.32-1.39]).
Dr. Allison W. Kurian of Stanford (Calif.)University and colleagues also found the rate of bilateral mastectomy had increased 14.3% each year, from 2% of all patients in 1998 to 12.3% in 2011, with it more commonly used among non-Hispanic white women, those with private insurance, and those who received care at a National Cancer Institute–designated cancer center, according to a paper published Sept. 2 in JAMA [doi:10.1001/jama.2014.10707].
"In a time of increasing concern over treatment, the risk-benefit ratio of bilateral mastectomy warrants careful consideration and raises the larger question of how physicians and society should respond to a patient’s preference for a morbid, costly intervention of dubious effectiveness," the authors wrote.
In an accompanying editorial, Dr. Lisa A. Newman of the comprehensive cancer center, University of Michigan, Ann Arbor, said the findings refute patient assumptions that bilateral mastectomy represents their best chance for a cure, and for eliminating the perceived cancer threat to the unaffected breast, and advocated a more calm and considered approach to treatment decision making (JAMA 2014 Sept. 2 [doi:10.1001/jama.2014.11308]).
"Physicians should not permit excessive treatment delays to compromise outcomes, but the initial few weeks surrounding the diagnosis are more effectively utilized by time invested in patient education and procedures that contribute to comprehensive treatment planning as opposed to hastily coordinating impulsive, irreversible surgical plans," Dr. Newman wrote.
The study was supported by the Jan Weimer Junior Faculty Chair in Breast Oncology, the Suzanne Pride Bryan Fund for Breast Cancer Research at Stanford Cancer Institute, and the National Cancer Institute. Two authors reported grants from Genentech for other work, but there were no other conflicts of interest disclosed.
The use of bilateral mastectomy has increased significantly in California, but the results from an observational cohort study show it achieves similar mortality reductions to breast-conserving surgery plus radiation, while unilateral mastectomy is associated with higher mortality.
In an analysis of data from nearly 190,000 patients in the population-based California Cancer Registry, no significant differences were found in all-cause mortality between patients who underwent bilateral mastectomy and those who had breast-conserving surgery with radiation (HR, 1.02 [95%CI, 0.94-1.11]); however, unilateral mastectomy was linked to 35% higher all-cause mortality than was breast-conserving surgery with radiation (HR, 1.35 [95% CI, 1.32-1.39]).
Dr. Allison W. Kurian of Stanford (Calif.)University and colleagues also found the rate of bilateral mastectomy had increased 14.3% each year, from 2% of all patients in 1998 to 12.3% in 2011, with it more commonly used among non-Hispanic white women, those with private insurance, and those who received care at a National Cancer Institute–designated cancer center, according to a paper published Sept. 2 in JAMA [doi:10.1001/jama.2014.10707].
"In a time of increasing concern over treatment, the risk-benefit ratio of bilateral mastectomy warrants careful consideration and raises the larger question of how physicians and society should respond to a patient’s preference for a morbid, costly intervention of dubious effectiveness," the authors wrote.
In an accompanying editorial, Dr. Lisa A. Newman of the comprehensive cancer center, University of Michigan, Ann Arbor, said the findings refute patient assumptions that bilateral mastectomy represents their best chance for a cure, and for eliminating the perceived cancer threat to the unaffected breast, and advocated a more calm and considered approach to treatment decision making (JAMA 2014 Sept. 2 [doi:10.1001/jama.2014.11308]).
"Physicians should not permit excessive treatment delays to compromise outcomes, but the initial few weeks surrounding the diagnosis are more effectively utilized by time invested in patient education and procedures that contribute to comprehensive treatment planning as opposed to hastily coordinating impulsive, irreversible surgical plans," Dr. Newman wrote.
The study was supported by the Jan Weimer Junior Faculty Chair in Breast Oncology, the Suzanne Pride Bryan Fund for Breast Cancer Research at Stanford Cancer Institute, and the National Cancer Institute. Two authors reported grants from Genentech for other work, but there were no other conflicts of interest disclosed.
FROM JAMA
Key clinical point: There is no mortality benefit associated with bilateral mastectomy, compared with breast-conserving surgery, and a higher mortality associated uniquely with unilateral mastectomy.
Major finding: Compared with breast-conserving surgery with radiation, bilateral mastectomy was not associated with a mortality difference (HR, 1.02 [95%CI, 0.94-1.11]), whereas unilateral mastectomy was associated with higher mortality (HR, 1.35 [95% CI, 1.32-1.39]).
Data source: An observational cohort study using data from 189,734 patients in the population-based California Cancer Registry.
Disclosures: The study was supported by the Jan Weimer Junior Faculty Chair in Breast Oncology, the Suzanne Pride Bryan Fund for Breast Cancer Research at Stanford Cancer Institute, and the National Cancer Institute. Two authors reported grants from Genentech for other work, but there were no other conflicts of interest disclosed.
CMS extends Open Payment review and dispute deadline – again
The Centers for Medicare & Medicaid Services is extending the deadlines for the review and dispute process for its Open Payments system to Sept. 10. It is the second announced delay in the past month.
The agency is altering the deadline because scheduled maintenance on the Open Payments system has interrupted its availability recently. (The next service disruption is set for Sept. 5.) The deadline is being extended to "allow ample time in the review, dispute, and correction process," the agency announced on Aug. 28.
The new window for the review and dispute process now closes Sept. 10, with the correction period now going from Sept. 11 to Sept. 25. The CMS still plans to publish information on Sept. 30.
The CMS reactivated the system in early August after technical glitches that caused data to be linked to the wrong physician forced Open Payments offline for several days. When it was back online, the review and dispute deadline was extended to Sept. 8 from the previous Aug. 27 deadline.
The Open Payments Program, created by the Affordable Care Act, aims to add transparency to the financial relationship between the health care industry and physicians and teaching hospitals. However, the system has had numerous technical issues and the agency has previously said that about a third of payment information will not be available when information is released to the public on Sept. 30.
The Centers for Medicare & Medicaid Services is extending the deadlines for the review and dispute process for its Open Payments system to Sept. 10. It is the second announced delay in the past month.
The agency is altering the deadline because scheduled maintenance on the Open Payments system has interrupted its availability recently. (The next service disruption is set for Sept. 5.) The deadline is being extended to "allow ample time in the review, dispute, and correction process," the agency announced on Aug. 28.
The new window for the review and dispute process now closes Sept. 10, with the correction period now going from Sept. 11 to Sept. 25. The CMS still plans to publish information on Sept. 30.
The CMS reactivated the system in early August after technical glitches that caused data to be linked to the wrong physician forced Open Payments offline for several days. When it was back online, the review and dispute deadline was extended to Sept. 8 from the previous Aug. 27 deadline.
The Open Payments Program, created by the Affordable Care Act, aims to add transparency to the financial relationship between the health care industry and physicians and teaching hospitals. However, the system has had numerous technical issues and the agency has previously said that about a third of payment information will not be available when information is released to the public on Sept. 30.
The Centers for Medicare & Medicaid Services is extending the deadlines for the review and dispute process for its Open Payments system to Sept. 10. It is the second announced delay in the past month.
The agency is altering the deadline because scheduled maintenance on the Open Payments system has interrupted its availability recently. (The next service disruption is set for Sept. 5.) The deadline is being extended to "allow ample time in the review, dispute, and correction process," the agency announced on Aug. 28.
The new window for the review and dispute process now closes Sept. 10, with the correction period now going from Sept. 11 to Sept. 25. The CMS still plans to publish information on Sept. 30.
The CMS reactivated the system in early August after technical glitches that caused data to be linked to the wrong physician forced Open Payments offline for several days. When it was back online, the review and dispute deadline was extended to Sept. 8 from the previous Aug. 27 deadline.
The Open Payments Program, created by the Affordable Care Act, aims to add transparency to the financial relationship between the health care industry and physicians and teaching hospitals. However, the system has had numerous technical issues and the agency has previously said that about a third of payment information will not be available when information is released to the public on Sept. 30.
COPPS-2 curtails colchicine enthusiasm in cardiac surgery
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
FROM THE ESC CONGRESS 2014
Key clinical point: Perioperative use of colchicine should be considered only in well-selected patients.
Major finding: Perioperative colchicine use cut the incidence of postpericardiotomy syndrome, but not postoperative atrial fibrillation or pericardial/pleural effusion.
Data source: Double-blind, randomized clinical trial in 360 consecutive candidates for heart surgery.
Disclosures: COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Movement training may lower stress fracture risk
SEATTLE – Correcting jumping and landing techniques may prevent lower-limb stress fractures in active young people, based on the results of a prospective study of 1,772 cadets at the United States Military Academy in West Point, N.Y.
Scores on the Landing Error Scoring System (LESS), which assesses 17 components of jumping and landing, were predictive of lower extremity stress fractures in the study, which was reported at the annual meeting of the American Orthopaedic Society for Sports Medicine.
Based on the results, freshman at West Point are now being screened for movement problems that are corrected when necessary. "We’ve seen a pretty impressive reduction – on average 30%-40% – in stress fractures, said lead investigator Kenneth Cameron, Ph.D., director of orthopedic research at Keller Army Community Hospital in West Point.
The reductions have not yet reached statistical significance because the program is fairly new, said Dr. Cameron, who added that the findings might prove useful for preventing post-traumatic osteoarthritis, anterior cruciate ligament tears, and other injuries.
For the study, cadets were instructed to jump off a 30-cm high box, then to leap as high as they could. Subjects were about 19 years old, on average, and had a body mass index of about 24 kg/m2 in men and 23 kg/m2 in women. The investigators videotaped the cadets and graded their movements using the LESS criteria.
Overall, there were 94 first-time fractures in the cohort, giving a cumulative incidence of 5.3%. Stress fractures were three times more likely in women, about one-third of the study population (incidence rate ratio = 2.86; 95% confidence interval, 1.88-4.34; P less than .001).
Controlling for sex and year of entry into the cohort, cadets who consistently landed flat footed or heel to toe were more than twice as likely (IRR = 2.32; 95% CI, 1.35-3.97; P = .002) to have a lower-extremity stress fracture during 4 years of follow-up. Similarly, a higher rate of stress fractures was noted in those who consistently landed asymmetrically (IRR = 2.53; 95% CI, 1.35-4.77; P = .004). Each additional movement error increased the incidence rate of lower-extremity stress fracture by 15% (IRR = 1.15; 95% CI, 1.02-1.31; P = .025).
"Typically, we don’t focus on changing movement patterns" when people have stress fractures, so most "move just as badly if not worse" and are at risk for another injury, he said. "Strength training isn’t enough; there’s a neuromuscular control issue, as well."
In stress fracture, "we see excessive motion in the frontal plane and transverse plane, and not much [side] plane motion. We also see hamstring and quadriceps weakness. Instead of flexing [the hip, knee, and ankle] to absorb force, [subjects] focus on compensatory movements," like internal rotation and abduction.
Hitting the floor with abnormal ankle flexion, stance width, and trunk flexion also increases the stress fracture risk.
The work was funded by the Department of Defense and National Institutes of Health, among others. Dr. Cameron had no relevant disclosures.
SEATTLE – Correcting jumping and landing techniques may prevent lower-limb stress fractures in active young people, based on the results of a prospective study of 1,772 cadets at the United States Military Academy in West Point, N.Y.
Scores on the Landing Error Scoring System (LESS), which assesses 17 components of jumping and landing, were predictive of lower extremity stress fractures in the study, which was reported at the annual meeting of the American Orthopaedic Society for Sports Medicine.
Based on the results, freshman at West Point are now being screened for movement problems that are corrected when necessary. "We’ve seen a pretty impressive reduction – on average 30%-40% – in stress fractures, said lead investigator Kenneth Cameron, Ph.D., director of orthopedic research at Keller Army Community Hospital in West Point.
The reductions have not yet reached statistical significance because the program is fairly new, said Dr. Cameron, who added that the findings might prove useful for preventing post-traumatic osteoarthritis, anterior cruciate ligament tears, and other injuries.
For the study, cadets were instructed to jump off a 30-cm high box, then to leap as high as they could. Subjects were about 19 years old, on average, and had a body mass index of about 24 kg/m2 in men and 23 kg/m2 in women. The investigators videotaped the cadets and graded their movements using the LESS criteria.
Overall, there were 94 first-time fractures in the cohort, giving a cumulative incidence of 5.3%. Stress fractures were three times more likely in women, about one-third of the study population (incidence rate ratio = 2.86; 95% confidence interval, 1.88-4.34; P less than .001).
Controlling for sex and year of entry into the cohort, cadets who consistently landed flat footed or heel to toe were more than twice as likely (IRR = 2.32; 95% CI, 1.35-3.97; P = .002) to have a lower-extremity stress fracture during 4 years of follow-up. Similarly, a higher rate of stress fractures was noted in those who consistently landed asymmetrically (IRR = 2.53; 95% CI, 1.35-4.77; P = .004). Each additional movement error increased the incidence rate of lower-extremity stress fracture by 15% (IRR = 1.15; 95% CI, 1.02-1.31; P = .025).
"Typically, we don’t focus on changing movement patterns" when people have stress fractures, so most "move just as badly if not worse" and are at risk for another injury, he said. "Strength training isn’t enough; there’s a neuromuscular control issue, as well."
In stress fracture, "we see excessive motion in the frontal plane and transverse plane, and not much [side] plane motion. We also see hamstring and quadriceps weakness. Instead of flexing [the hip, knee, and ankle] to absorb force, [subjects] focus on compensatory movements," like internal rotation and abduction.
Hitting the floor with abnormal ankle flexion, stance width, and trunk flexion also increases the stress fracture risk.
The work was funded by the Department of Defense and National Institutes of Health, among others. Dr. Cameron had no relevant disclosures.
SEATTLE – Correcting jumping and landing techniques may prevent lower-limb stress fractures in active young people, based on the results of a prospective study of 1,772 cadets at the United States Military Academy in West Point, N.Y.
Scores on the Landing Error Scoring System (LESS), which assesses 17 components of jumping and landing, were predictive of lower extremity stress fractures in the study, which was reported at the annual meeting of the American Orthopaedic Society for Sports Medicine.
Based on the results, freshman at West Point are now being screened for movement problems that are corrected when necessary. "We’ve seen a pretty impressive reduction – on average 30%-40% – in stress fractures, said lead investigator Kenneth Cameron, Ph.D., director of orthopedic research at Keller Army Community Hospital in West Point.
The reductions have not yet reached statistical significance because the program is fairly new, said Dr. Cameron, who added that the findings might prove useful for preventing post-traumatic osteoarthritis, anterior cruciate ligament tears, and other injuries.
For the study, cadets were instructed to jump off a 30-cm high box, then to leap as high as they could. Subjects were about 19 years old, on average, and had a body mass index of about 24 kg/m2 in men and 23 kg/m2 in women. The investigators videotaped the cadets and graded their movements using the LESS criteria.
Overall, there were 94 first-time fractures in the cohort, giving a cumulative incidence of 5.3%. Stress fractures were three times more likely in women, about one-third of the study population (incidence rate ratio = 2.86; 95% confidence interval, 1.88-4.34; P less than .001).
Controlling for sex and year of entry into the cohort, cadets who consistently landed flat footed or heel to toe were more than twice as likely (IRR = 2.32; 95% CI, 1.35-3.97; P = .002) to have a lower-extremity stress fracture during 4 years of follow-up. Similarly, a higher rate of stress fractures was noted in those who consistently landed asymmetrically (IRR = 2.53; 95% CI, 1.35-4.77; P = .004). Each additional movement error increased the incidence rate of lower-extremity stress fracture by 15% (IRR = 1.15; 95% CI, 1.02-1.31; P = .025).
"Typically, we don’t focus on changing movement patterns" when people have stress fractures, so most "move just as badly if not worse" and are at risk for another injury, he said. "Strength training isn’t enough; there’s a neuromuscular control issue, as well."
In stress fracture, "we see excessive motion in the frontal plane and transverse plane, and not much [side] plane motion. We also see hamstring and quadriceps weakness. Instead of flexing [the hip, knee, and ankle] to absorb force, [subjects] focus on compensatory movements," like internal rotation and abduction.
Hitting the floor with abnormal ankle flexion, stance width, and trunk flexion also increases the stress fracture risk.
The work was funded by the Department of Defense and National Institutes of Health, among others. Dr. Cameron had no relevant disclosures.
AT THE AOSSM 2014 ANNUAL MEETING
Key clinical point: Movement evaluation and training may prevent orthopedic injury.
Major finding: People who land flat-footed or heel-to-toe in jump tests are more than twice as likely to develop lower-extremity stress fractures (IRR = 2.32; 95% CI, 1.35-3.97; P = .002).
Data Source: Prospective cohort study of nearly 1,800 young adults.
Disclosures: The lead investigator has no disclosures. The National Institutes of Health and Department of Defense funded the work.
Advice for surviving a billing audit
CHICAGO – The first rule of a billing audit, according to Dr. Brent Moody: "Don’t take it personally."
Audits are about money, and "there’s always going to be a winner and a loser," he said at the American Academy of Dermatology summer meeting.
To raise the odds of winding up on the winning side of an audit or billing investigation, Dr. Moody advised taking the following steps.
Consider retaining legal counsel. The need for an attorney depends on the size, scope, and seriousness of the audit.
"You may be able to handle it on your own" if a small number of records are requested, he said. But a Recovery Audit Contractor (RAC) audit request for dozens or hundreds of chart records could indicate a more serious audit investigation. "If they come back to you with a big recoupment or a really broad request, you may want to think about getting legal help."
Legal counsel is strongly recommended if audit investigations evolve into allegations of False Claims Act (FCA) violations or qui tam lawsuits, said Dr. Moody, a Nashville dermatologist and the chair of the public policy committee for the American College of Mohs Surgery. The federal FCA law sets criminal and civil penalties for falsely billing the government, overrepresenting the amount of a delivered product, or understating an obligation to the government. Qui tam lawsuits are civil claims under the FCA in which whistle-blowers are rewarded if the claims uncover fraud and recover funds for the government. Both types of cases can mean the involvement of federal authorities, seized documents or equipment, and potential criminal charges.
FCA violations or qui tam lawsuits "are serious issues. You need legal help, and you need it right away," he said.
Decide whether to fight or pay. Complying with a recoupment will reduce hassle and more quickly resolve an audit. An appeal makes sense if the request is erroneous or unfair. Appealing within 30 days halts the recoupment but does not stop interest from accruing.
A letter of rebuttal – a formal statement as to why the recoupment should not take place – is ideal when the wrong doctor or practice has been audited or the audit violates state rules on look-back timelines. Health providers have 15 days to rebut upon notice of an impending recoupment action. Another option is to negotiate by paying the recoupment sum, but getting the auditors to agree that no further look-backs will occur from a certain time frame.
Do your audit homework. Audit resources and information are available from the American Medical Association and state medical societies. The American Academy of Dermatology provides a RAC audit toolkit, and many other medical organizations can provide answers to common audit questions and attorney referral lists.
Be civil to your auditor. While challenging, remaining cordial and respectful to auditors during the audit process can ultimately work in the physician’s favor. "At the end of the day, they are just people doing a job," Dr. Moody said. "Talk to them and try to figure out exactly what they are looking for. You don’t want to fight the wrong battle."
On Twitter @legal_med
CHICAGO – The first rule of a billing audit, according to Dr. Brent Moody: "Don’t take it personally."
Audits are about money, and "there’s always going to be a winner and a loser," he said at the American Academy of Dermatology summer meeting.
To raise the odds of winding up on the winning side of an audit or billing investigation, Dr. Moody advised taking the following steps.
Consider retaining legal counsel. The need for an attorney depends on the size, scope, and seriousness of the audit.
"You may be able to handle it on your own" if a small number of records are requested, he said. But a Recovery Audit Contractor (RAC) audit request for dozens or hundreds of chart records could indicate a more serious audit investigation. "If they come back to you with a big recoupment or a really broad request, you may want to think about getting legal help."
Legal counsel is strongly recommended if audit investigations evolve into allegations of False Claims Act (FCA) violations or qui tam lawsuits, said Dr. Moody, a Nashville dermatologist and the chair of the public policy committee for the American College of Mohs Surgery. The federal FCA law sets criminal and civil penalties for falsely billing the government, overrepresenting the amount of a delivered product, or understating an obligation to the government. Qui tam lawsuits are civil claims under the FCA in which whistle-blowers are rewarded if the claims uncover fraud and recover funds for the government. Both types of cases can mean the involvement of federal authorities, seized documents or equipment, and potential criminal charges.
FCA violations or qui tam lawsuits "are serious issues. You need legal help, and you need it right away," he said.
Decide whether to fight or pay. Complying with a recoupment will reduce hassle and more quickly resolve an audit. An appeal makes sense if the request is erroneous or unfair. Appealing within 30 days halts the recoupment but does not stop interest from accruing.
A letter of rebuttal – a formal statement as to why the recoupment should not take place – is ideal when the wrong doctor or practice has been audited or the audit violates state rules on look-back timelines. Health providers have 15 days to rebut upon notice of an impending recoupment action. Another option is to negotiate by paying the recoupment sum, but getting the auditors to agree that no further look-backs will occur from a certain time frame.
Do your audit homework. Audit resources and information are available from the American Medical Association and state medical societies. The American Academy of Dermatology provides a RAC audit toolkit, and many other medical organizations can provide answers to common audit questions and attorney referral lists.
Be civil to your auditor. While challenging, remaining cordial and respectful to auditors during the audit process can ultimately work in the physician’s favor. "At the end of the day, they are just people doing a job," Dr. Moody said. "Talk to them and try to figure out exactly what they are looking for. You don’t want to fight the wrong battle."
On Twitter @legal_med
CHICAGO – The first rule of a billing audit, according to Dr. Brent Moody: "Don’t take it personally."
Audits are about money, and "there’s always going to be a winner and a loser," he said at the American Academy of Dermatology summer meeting.
To raise the odds of winding up on the winning side of an audit or billing investigation, Dr. Moody advised taking the following steps.
Consider retaining legal counsel. The need for an attorney depends on the size, scope, and seriousness of the audit.
"You may be able to handle it on your own" if a small number of records are requested, he said. But a Recovery Audit Contractor (RAC) audit request for dozens or hundreds of chart records could indicate a more serious audit investigation. "If they come back to you with a big recoupment or a really broad request, you may want to think about getting legal help."
Legal counsel is strongly recommended if audit investigations evolve into allegations of False Claims Act (FCA) violations or qui tam lawsuits, said Dr. Moody, a Nashville dermatologist and the chair of the public policy committee for the American College of Mohs Surgery. The federal FCA law sets criminal and civil penalties for falsely billing the government, overrepresenting the amount of a delivered product, or understating an obligation to the government. Qui tam lawsuits are civil claims under the FCA in which whistle-blowers are rewarded if the claims uncover fraud and recover funds for the government. Both types of cases can mean the involvement of federal authorities, seized documents or equipment, and potential criminal charges.
FCA violations or qui tam lawsuits "are serious issues. You need legal help, and you need it right away," he said.
Decide whether to fight or pay. Complying with a recoupment will reduce hassle and more quickly resolve an audit. An appeal makes sense if the request is erroneous or unfair. Appealing within 30 days halts the recoupment but does not stop interest from accruing.
A letter of rebuttal – a formal statement as to why the recoupment should not take place – is ideal when the wrong doctor or practice has been audited or the audit violates state rules on look-back timelines. Health providers have 15 days to rebut upon notice of an impending recoupment action. Another option is to negotiate by paying the recoupment sum, but getting the auditors to agree that no further look-backs will occur from a certain time frame.
Do your audit homework. Audit resources and information are available from the American Medical Association and state medical societies. The American Academy of Dermatology provides a RAC audit toolkit, and many other medical organizations can provide answers to common audit questions and attorney referral lists.
Be civil to your auditor. While challenging, remaining cordial and respectful to auditors during the audit process can ultimately work in the physician’s favor. "At the end of the day, they are just people doing a job," Dr. Moody said. "Talk to them and try to figure out exactly what they are looking for. You don’t want to fight the wrong battle."
On Twitter @legal_med
EXPERT ANALYSIS FROM THE AAD 2014 SUMMER ACADEMY
Physicians in group practice setting make more
Physicians in medical groups and other organized systems of care delivery saw a slight increase in compensation, according to annual survey data released by the American Medical Group Management Association.
In general, findings show average percentage increases in compensation in 2013 were slightly higher than in 2012, with the overall weighted average increase in 2013 being 2.9%, up from 1.6% in the previous year. Results were based on a survey conducted on behalf of the American Medical Group Management Association (AMGA) by Sullivan, Cotter and Associates, with 289 medical groups representing about 73,700 providers submitting valid survey responses. AMGA released the survey results on Aug. 20.
Individual specialties showing the biggest median total compensation increase year-over-year include gastroenterology (a 9.0% increase to $471,336), cardiac/thoracic surgery (8.2% to $569,073), emergency medicine (5.2% to $316,739), and neurology (5.1% to $268,096). Total compensation includes the total compensation of the individual provider, including base, variable, and administrative compensation, plus all voluntary salary reductions.
Four specialties saw compensation decreases during this time period, including allergy/immunology (a 1.3% decrease to $267,338), rheumatologic disease (–0.5% to $239,112), cardiology-cath lab (–0.4% to $544,733), and endocrinology (–0.2% to $233,769).
Overall, AMGA reported that 68% of specialties reported increases in compensation in 2013, with primary care specialists reporting a 3.8% increase in 2013, up from 2.8% in 2012. Other specialists saw compensation increase on average 1.8%, up from 1.6%, and surgical specialists saw an average increase of 3.0%, up from 0.5%.
Physicians in medical groups and other organized systems of care delivery saw a slight increase in compensation, according to annual survey data released by the American Medical Group Management Association.
In general, findings show average percentage increases in compensation in 2013 were slightly higher than in 2012, with the overall weighted average increase in 2013 being 2.9%, up from 1.6% in the previous year. Results were based on a survey conducted on behalf of the American Medical Group Management Association (AMGA) by Sullivan, Cotter and Associates, with 289 medical groups representing about 73,700 providers submitting valid survey responses. AMGA released the survey results on Aug. 20.
Individual specialties showing the biggest median total compensation increase year-over-year include gastroenterology (a 9.0% increase to $471,336), cardiac/thoracic surgery (8.2% to $569,073), emergency medicine (5.2% to $316,739), and neurology (5.1% to $268,096). Total compensation includes the total compensation of the individual provider, including base, variable, and administrative compensation, plus all voluntary salary reductions.
Four specialties saw compensation decreases during this time period, including allergy/immunology (a 1.3% decrease to $267,338), rheumatologic disease (–0.5% to $239,112), cardiology-cath lab (–0.4% to $544,733), and endocrinology (–0.2% to $233,769).
Overall, AMGA reported that 68% of specialties reported increases in compensation in 2013, with primary care specialists reporting a 3.8% increase in 2013, up from 2.8% in 2012. Other specialists saw compensation increase on average 1.8%, up from 1.6%, and surgical specialists saw an average increase of 3.0%, up from 0.5%.
Physicians in medical groups and other organized systems of care delivery saw a slight increase in compensation, according to annual survey data released by the American Medical Group Management Association.
In general, findings show average percentage increases in compensation in 2013 were slightly higher than in 2012, with the overall weighted average increase in 2013 being 2.9%, up from 1.6% in the previous year. Results were based on a survey conducted on behalf of the American Medical Group Management Association (AMGA) by Sullivan, Cotter and Associates, with 289 medical groups representing about 73,700 providers submitting valid survey responses. AMGA released the survey results on Aug. 20.
Individual specialties showing the biggest median total compensation increase year-over-year include gastroenterology (a 9.0% increase to $471,336), cardiac/thoracic surgery (8.2% to $569,073), emergency medicine (5.2% to $316,739), and neurology (5.1% to $268,096). Total compensation includes the total compensation of the individual provider, including base, variable, and administrative compensation, plus all voluntary salary reductions.
Four specialties saw compensation decreases during this time period, including allergy/immunology (a 1.3% decrease to $267,338), rheumatologic disease (–0.5% to $239,112), cardiology-cath lab (–0.4% to $544,733), and endocrinology (–0.2% to $233,769).
Overall, AMGA reported that 68% of specialties reported increases in compensation in 2013, with primary care specialists reporting a 3.8% increase in 2013, up from 2.8% in 2012. Other specialists saw compensation increase on average 1.8%, up from 1.6%, and surgical specialists saw an average increase of 3.0%, up from 0.5%.
VIDEO: Federal health IT chief DeSalvo talks meaningful use
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.